Abstract
Introduction
Ischemic strokes and their recurrence create an immense disease burden globally. Therefore, preventing recurrent strokes by promoting medication adherence is crucial to reduce morbidity and mortality. In addition, understanding the barriers to medication adherence related to the social determinants of health (SDoH) could promote equity among persons with ischemic stroke.
Objective
To explore the barriers to medication adherence among patients with ischemic stroke through the SDoH.
Methods
This systematic review included studies published between January 2018 and December 2022 identified through PubMed, MEDLINE, Web of Science, and CINAHL Plus Full Text. The descriptions of the studies were systematically summarized and discussed based on the SDoH from the US Healthy People 2030 initiative.
Results
Eight studies met the inclusion criteria and were included in this review. The most common barrier to adherence was inappropriate medication beliefs, medication side effects, and patient-physician relationship, which relate to the dimensions of healthcare access and quality. Health literacy and health perception, dependent on education access and quality, frequently influenced adherence. Other social determinants, such as financial strain and social and community context, were found to alter adherence behaviors. No study addressed the neighborhood and built environment domain. We found that cognitive impairment is another factor that impacts adherence outcomes among stroke patients.
Conclusion
Multifaceted approaches are needed to address the SDoH to improve medication adherence among patients with ischemic stroke. This review emphasized strategies, including patient education, provider-patient communication, social support, health literacy, technology, and policy advocacy to enhance adherence.
Keywords: ischemic stroke, medication adherence, social determinants of health, systematic review
Introduction
Stroke is the leading cause of death and disability worldwide.1 The report from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) in 2019 shows that there were 12.2 million incident cases of stroke, and 6.55 million of those were fatal.2 Globally, ischemic stroke (IS) constituted 62.4% of all incident strokes in 2019. At the same time, 27.9% and 9.7% were intracerebral and subarachnoid hemorrhages, respectively.2 In the United States (US), more than 795,000 people have a stroke, and more than 76% are first strokes;3 moreover, 87% of all strokes in the US are IS.3 Consequently, the US spent almost $53 billion between 2017 and 2018, including healthcare services, medication to treat strokes, and missed days at work.3
Previous studies have reported on the prognosis and risk of stroke recurrence in patients with a history of stroke. For example, cognitive impairment was found frequently in patients with multiple lacunar infarction recurrences,4 while in cardioembolic stroke, early recurrent embolization emerged as the most important predictor of in-hospital mortality.5 A study by Flach et al in the United Kingdom, which includes 6,052 patients with a first-ever stroke, shows that the risk of stroke recurrence in five years ranged between 10% to 18% from 1995 to 2005. When accounting for death as a competing risk, the 5-year recurrence rate was 8.7%, and the 10-year recurrence was 11.2%.6 Han et al included 1185 Chinese individuals who experienced initial stroke events. Their results revealed that the overall rate of recurrent stroke within one year and five years was 5.7% overall within one year, 6.9% in men and 4.6% in women, and 22.5% within five years, with 24.0% in men and 20.2% in women, respectively.7 Another study from Germany aimed to determine the frequency and timing of recurrent strokes. The results showed that the risk of recurrence was 1.2% in the first 30 days, 3.4% within 90 days, 7.4% within one year, and 19.4% within five years.8 Moreover, the mortality rate from a recurrent stroke was higher than the first stroke.9 Thus, stroke recurrence prevention is essential.10
Adherence to a stroke-preventive medication has been reported to be a promising way to prevent stroke recurrence.11 However, medication adherence rates in stroke patients are poor. Multiple studies have reported that between 40% to 50% of stroke patients do not adhere to their medication.12,13 This result is consistent with a meta-analysis of 63 observational studies, which found that the overall medication adherence rate of patients with stroke was only 64.1%.14 Previous studies have found factors that impact medication adherence. For example, financial problems,15,16 education,17,18 social support,19–21 health literacy,22,23 or sociodemographic factors such as age24,25 and gender.22,24,26 Thus, it is essential to understand the factors that influence medication adherence comprehensively. That knowledge could benefit future interventional research studies that can incorporate these factors and help improve medication adherence rates and health outcomes in IS patients.
In this systematic review, the social determinants of health model (SDoH) framework retrieved from the US Department of Health and Human Services Healthy People 2030 initiative was used to guide data synthesis to understand barriers to medication adherence in patients with IS.27 SDoH are considered conditions in the environment where people live that involve a wide range of health, functioning, and quality-of-life outcomes and risks.28 SDoH can be grouped into five domains; (1) Economic Stability, (2) Education Access and Quality, (3) Health Care Access and Quality, (4) Neighborhood and Built Environment, and (5) Social and Community Context.28 Briefly, in the data synthesis process, themes have been extracted from the key findings of the included studies by examining the similarities and differences between the main findings based on the five domains in SDoH. Moreover, sub-themes will then be abstracted according to the more specific target of the corresponding findings as needed, similar to how qualitative researchers produce themes.29 Therefore, we explored the barriers to medication adherence among patients with IS through the SDoH framework.
Methods
Identify Relevant Studies
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines30 in this systematic review to present the literature’s identification, screening, exclusion, and inclusion flow diagram. Four electronic databases, PubMed, MEDLINE, Web of Science, and CINAHL Plus Full Text, were systematically searched on November 21, 2022, to identify preliminary studies published between January 2018 and December 2022, reporting barriers to medication adherence in patients with IS to capture the most recent studies at the time the visionary goal of Healthy People 2030 announced. The researcher combined the search terms: (Ischemic Stroke* OR Ischemic Stroke* OR Cryptogenic Ischemic Stroke* OR Cryptogenic Stroke* OR Cryptogenic Embolism Stroke* OR Wake up Stroke* OR Acute Ischemic Stroke* OR Embolic Stroke* OR Cardioembolic Stroke* OR Cardio-embolic Stroke* OR Thrombotic Stroke* OR Acute Thrombotic Stroke* OR Lacunar Stroke* OR Lacunar Syndrome* OR Lacunar Infarction* OR Lacunar Infarct*) AND (Medication Adherence OR Medication Non-adherence OR Medication Non-compliance OR Medication Persistence OR Medication Compliance OR Medication NonCompliance) OR AB=(Medication Adherence OR Medication Non-adherence OR Medication Non-compliance OR Medication Persistence OR Medication Compliance OR Medication NonCompliance) AND (Barrier*) using Boolean phrases. In addition, reference lists of the included studies were manually searched to obtain relevant studies. All references identified were stored in EndNote. The detailed search strategy is shown in Supplementary Table 1.
Study Selection
Titles and abstracts were screened for eligible studies. The full text was then assessed to decide whether it was relevant. Finally, inclusion criteria were implemented to guarantee that only studies considered relevant to our objective were included. Similarly, exclusion criteria were used to eliminate literature not affiliated with the review (Table 1).
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Quality Assessment
The quality assessment aims to assess a study’s methodological quality and determine the extent to which a study has addressed the possibility of bias in its design, conduct, and analysis. In this study, two researchers assessed the methodological quality of studies independently using the Joanna Briggs Institute (JBI) critical appraisal tools designed for systematic review, including the JBI critical appraisal checklist for analytical cross-sectional studies and qualitative research.31,32
Data Extraction
The standardized chart for data extraction (Supplementary Table 2) developed for this review included the following data for each study: Reference, country, year, study design, the sample size of the target population (n), age (year), the study aims, medication adherence measurement, key findings, themes (barriers to medication adherence) based on SDoH domains and summarize/further research implications.
Data Synthesis
In this review, the convergent integrated analysis framework suggested by JBI for systematic reviews was utilized for the data synthesis of the included studies.29 In the data synthesis process, themes will be extracted from the key findings of the included studies by examining the similarities and differences between the main findings base on five domains in SDoH: 1) Economic Stability, 2) Education Access and Quality, 3) Health Care Access and Quality, 4) Neighborhood and Built Environment, 5) Social and Community Context. Moreover, sub-themes will then be abstracted according to the more specific target of the corresponding findings as needed, similar to how qualitative researchers produce themes.29
Results
Search Results
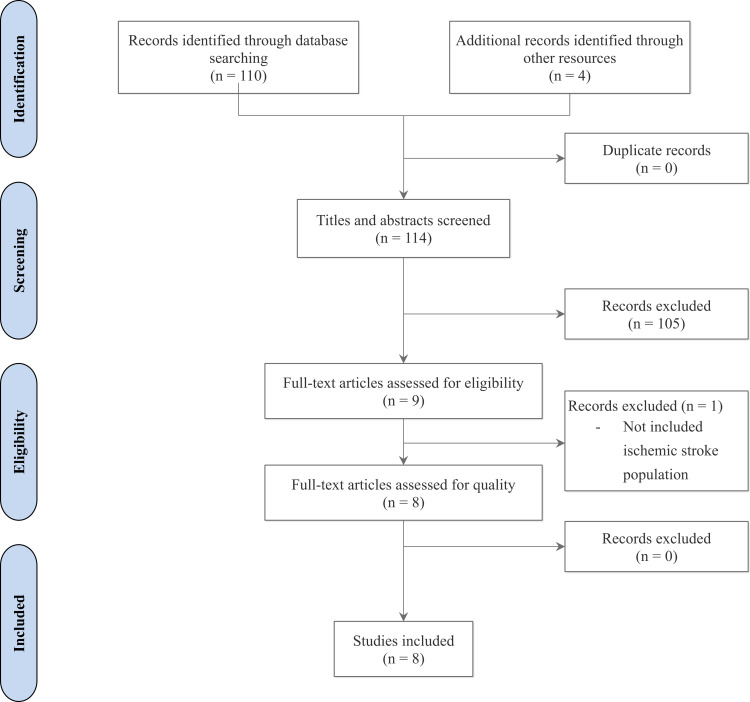
Following the PRISMA guidelines,33 a total of 114 articles were initially identified, with four additional ones found from other resources. No duplicate articles were identified. Subsequently, the remaining articles were screened by their titles and abstracts based on the inclusion and exclusion criteria (see Table 1). At this stage, 105 articles did not meet the inclusion criteria and were excluded, leaving nine articles eligible for full-text screening. During the full-text screening phase, one article was excluded as it did not include the IS population. Consequently, eight studies were included in the quality appraisal (see Figure 1).
Figure 1.
PRISMA flow chart.
Notes: Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873–880.33
Description of Included Studies
Table 2 shows that most included studies were published in 2020 (n = 3, 37.5%). Two articles were conducted in India (25%). Each with one study (12.5%) was conducted in China, French, Lebanon, Singapore, the Republic of Korea, and Greece. The majority of the study design was cross-sectional (n = 7, 87.5%). One was a qualitative study (n = 1, 12.5%). Most of the studies studied on IS population (n = 7, 58.33%). Sample size ranged from 1 to 50 (n = 1, 12.5%), 50 to 100 (n = 1, 12.5%), 100 to 200 (n = 3, 37.5%), 200 to 300 (n = 2, 25%), and more than 300 (n = 1, 12.5%). Among the validated scales used to measure medication adherence was the shortened Medication Adherence Report Scale (MARS-5) (n = 3, 37.5%), the 8-item Morisky Medication Adherence Scale (MMAS) (n = 1, 12.5%), and the Lebanese Medication Adherence Scale (LMAS-14) (n = 1, 12.5%).
Table 2.
The Characteristics of the Included Studies
| Characteristic | Number* | Percentage (%) |
|---|---|---|
| Publication year | ||
| 2022 | 2 | 25 |
| 2021 | 2 | 25 |
| 2020 | 3 | 37.5 |
| 2019 | 1 | 12.5 |
| Country | ||
| India | 2 | 25 |
| China | 1 | 12.5 |
| French | 1 | 12.5 |
| Lebanon | 1 | 12.5 |
| Singapore | 1 | 12.5 |
| Republic of Korea | 1 | 12.5 |
| Greece | 1 | 12.5 |
| Study design | ||
| Cross-sectional study | 7 | 87.5 |
| Qualitative study | 1 | 12.5 |
| Target population | ||
| Ischemic stroke | 7 | 58.33 |
| Transient ischemic attack | 3 | 25 |
| Acute ischemic stroke | 1 | 8.33 |
| Hemorrhagic stroke | 1 | 8.33 |
| Sample size (n) | ||
| 1–50 | 1 | 12.5 |
| > 50–100 | 1 | 12.5 |
| > 100–200 | 3 | 37.5 |
| > 200–300 | 2 | 25 |
| > 300 | 1 | 12.5 |
| Medication adherence measurement | ||
| The shortened Medication Adherence Report Scale (MARS-5) | 3 | 37.5 |
| The 8-item Morisky Medication Adherence Scale (MMAS) | 1 | 12.5 |
| The Lebanese Medication Adherence Scale (LMAS-14) | 1 | 12.5 |
| Semi-structured interview | 1 | 12.5 |
| Self-report** | 1 | 12.5 |
| A medication adherence assessment questionnaire was developed based on the patients’ common problems | 1 | 12.5 |
Notes: *The number of included studies in which one study may contribute to > 1 characteristic. **Self-reported medication adherence was defined as the consumption of at least > 80% of their medications for the last two weeks, based on the patient’s last prescription.
Assessment of Methodological Quality
The methodological quality of the included studies was evaluated by the JBI critical appraisal checklist for analytical cross-sectional studies and qualitative research.29 The results show that contents about the methodological quality were clearly reported in the included studies (all above 50%), thus minimizing the risk of bias in study design, conduct, and analysis (Supplementary Table 3).
Description of Barriers to Medication Adherence in Patients with Ischemic Stroke
A summary of the findings of the barrier to medication adherence theme based on the SDoH domain is provided in Table 3. Scrutiny of Table 3 can be placed into four major domains of SDoH: 1) Economic Stability (including financial restrain theme), 2) Education Access and Quality (including health behavior and health literacy themes), 3) Health Care Access and Quality (including lack of health information, medication side effects, medication belief, patient-physician relationship, polypharmacy, accessible to healthcare themes), and 4) Social and Community Context (including medication management due to social context theme). For Neighborhood and Built Environment, no review results fell into this domain. Moreover, the review results highlighted cognitive impairment, which does not fall into any SDoH domain. Given that cognitive impairment can impact social determinants of health by limiting persons’ ability to access healthcare and work, leading to financial difficulties and inadequate housing, the cognitive impairment domain was considered to be included and falls under “others”.
Table 3.
Barriers to Medication Adherence Theme Based on the Social Determinant of Health Domain
| Reference | Social Determinants of Health (SDoH) Domains | Others* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Economic Stability | Education Access and Quality | Health Care Access and Quality | Social and Community Context | Neighborhood and Built Environment | ||||||||
| Theme Based on SDoH | ||||||||||||
| Financial Restrain | Health Behavior | Health Literacy and Health Perception | Lack of Health Information | Medication Side Effects | Medication Belief | Patient-Physician Relationship | Polypharmacy | Accessible to Healthcare | Medication Management Due to Social Context | N/A | Cognitive Impairment | |
| [34] | X | X | X | X | X | N/A | ||||||
| [35] | X | X | N/A | |||||||||
| [36] | X | X | N/A | |||||||||
| [37] | X | X | X | N/A | ||||||||
| [38] | X | X | N/A | X | ||||||||
| [39] | X | X | X | X | X | N/A | X | |||||
| [40] | X | X | X | N/A | ||||||||
| [41] | X | X | N/A | |||||||||
Note: *Not fall into the SDoH domain.
Abbreviation: N/A, not applicable.
Economic Stability
Financial Restrain
Economic stability has been shown to be the factor that impacts people’s health in many ways. People with reliable incomes are less likely to live in poverty and, thus, are healthier.27 In the current review, two included studies found that financial restraints are barriers to medication adherence in patients with IS.35,38 A cross-sectional study by Saade et al assessed medication adherence for secondary stroke prevention among Lebanese stroke survivors and identified the barriers to non-compliance. Patients who reported concern about medication costs were more likely to be non-adherent to their medications.35 Similarly, a study by Shani et al determined the factors associated with medication adherence among 240 stroke survivors. The result showed that patients with financial constraints were more likely to report non-adherence to stroke medication.38 These findings suggested that to improve medication adherence, establishing financial aid or medical insurance to purchase medications is critical to improving medication adherence to prevent future strokes.
Education Access and Quality
People with higher education were more likely to live longer and healthier.27 Access to good quality education provides more opportunities for individuals to get safe and high-paying jobs. In the future, they are less likely to have health problems such as heart disease, depression, or diabetes.27 In this review, there are two themes in this domain: 1) health behavior, 2) health literacy, and health perception.
Health Behavior
Health behavior refers to the actions of individuals that impact health, which can be positive such as eating well and exercising, or negative such as smoking and drinking.27 One included study investigated medication adherence among 250 acute ischemic stroke patients and identified the factors influencing their medication adherence.37 The result demonstrated that non-smokers were more likely to adhere to medication compared to patients who smoked.37 Therefore, we suggest that post-stroke care should concentrate on encouraging lifestyle modifications, such as smoking cessation, in order to improve the medication adherence of patients with stroke.
Health Literacy and Health Perception
Health literacy was described by Hewitt (2012) as the ability to understand and use healthcare information to make health decisions appropriately and follow instructions for treatments.42 A prospective study that determined the barriers to medication adherence for secondary prevention in patients with IS revealed that patients with low health literacy and difficulty understanding the doctor were more likely not to take their medications regularly.39 This study suggested that healthcare professionals, caregivers, and patients should work together to help patients understand their health condition and medication more to enhance medication adherence.
Additionally, health perception, defined as an individual’s personal beliefs and understanding regarding their health status, was associated with medication adherence in the included studies.34,40 One qualitative study explored barriers and facilitators to adherence to medications after stroke and found that a lack of understanding about the disease negatively impacted medication adherence. One of the participants stated that “I didn’t know it was a stroke until I woke up in. I knew after [.], But I was still out of it, so I didn’t understand anything”.34 Another included study conducted by Ruksakulpiwat et al found that patients with IS who report a higher perception of illness score, which indicated that if the patient viewed the illness as more dangerous, they were more likely to report non-adherence to medication.40 Therefore, incorporating IS perceptions in future interventions is important to enhance adherence and patient outcomes.
Health Care Access and Quality
Healthcare access and quality refer to the availability, affordability, and appropriateness of health services for people across their lifespans.27 In this review, there are six themes in this domain: 1) lack of health information, 2) medication side effects, 3) medication belief, 4) patient-physician relationship, 5) polypharmacy, and 6) accessibility to healthcare.
Lack of Health Information
In this review, a couple of the included studies reported that lacking health information was a factor that prevented stroke patients from adhering to their medication.34,40 A qualitative study identified three barriers preventing effective patient education which led to a lack of health information, including lack of consultation time, technical jargon, and individual cognitive impairment. One of the participants stated that
No. I did not ask him, but he did not tell me. […] they are not like those we had in the past who explained everything to us, what we had, explained the medicine to us, what it would do. [.] they do not have the time anymore.
Another participant stated,
They try to explain to me [what a stroke is], but it’s hard to explain to people who aren’t in the trade. And then, it’s difficult to explain because they use terms like. which aren’t familiar to us.34
The researcher suggests that providing information for patients at opportune moments, particularly by promoting discussion with primary care physicians throughout illness and recovery, is essential to ensure that patients understand their health and treatment, especially medication.
Medication Side Effects
Side effects from stroke medication have been reported as a factor impacting medication adherence in three included studies in this review.34,35,38 Viprey et al conducted a semi-structured interview with 36 patients with IS and Transient Ischemic Attack (TIA). They found that side effects of stroke medication prevent patients’ medication adherence. For example, one participant stated that the medication caused heartburn, so he/she stopped taking it.34 Similarly, a quantitative, cross-sectional study of 100 patients with IS showed that patients who reported concern about medication side effects were more likely not to adhere to their medication.35 This is consistent with another study by Shani et al which determined factors associated with medication adherence among 240 stroke survivors. The results showed that patients who reported experiencing side effects due to stroke medication were more likely to have non-adherence to their prescriptions than those without side effects.38 Accordingly, we suggest that establishing patient education regarding medications (eg, medication use, side effects) is important to improve medication adherence to prevent future stroke recurrence.
Medication Belief
Six studies have shown that medication beliefs were significantly associated with medication adherence.34,36,37,39–41 For example, a cohort study conducted by Fan et al determined whether beliefs about medication would mediate the relationship between trust in physicians and medication adherence. The result demonstrated that participants who were concerned about their medications and believed that doctors overuse them were likely not to take medications regularly.36 Likewise, Ruksakulpiwat et al stated that a high score on the IS medication-concerned questionnaire was a barrier to medication adherence.40 Therefore, results from these studies recommended that future interventions to improve medication adherence may benefit from addressing their beliefs about medication, and patients’ beliefs about IS medication should be included as one component in future interventions.
Patient-Physician Relationship
The Patient-Physician Relationship is one of several factors that impact medication adherence in patients with IS.36,39,41 A previous cohort study investigated the relationship between medication adherence, physician trust, and medication beliefs among stroke survivors.36 The results demonstrated that a lack of trust in physicians prevented IS patients from taking their medications regularly.36 Another study from Velusamy et al revealed that among 132 adult patients with IS white coat adherence, increased medication adherence around clinic visits negatively impacted medication adherence and patient-provider decision-making, and treatment planning, ultimately worsening patients’ outcomes.39 Therefore, we suggest that future interventions to improve medication adherence may benefit from improving stroke survivors’ trust in physicians. Furthermore, healthcare professionals, caregivers, and patients should work together to help patients understand their medication more to enhance medication adherence.
Polypharmacy
The use of multiple medications to treat diseases, known as polypharmacy, can lead to various problems, such as being costly and difficult to track and manage.43 We found that to be a factor causing medication non-adherence.44 In our review, Kim et al and Velusamy et al found that polypharmacy is a barrier to medication adherence in patients with IS.37,39 For example, Kim et al found that patients who took less frequent daily doses were more like to adhere to their medication than those who took more doses per day.37 Consistent with the result from Velusamy et al study, which showed that with increasing the frequency of daily medications, the less adherent they were to their medications.39 Medication reconciliation is needed to evaluate the possibility of decreasing the number of needed medications. We recommend that medication management strategies, such as medication-taking reminders utilizing mobile technology or medication management programs provided by healthcare professionals, could be used to facilitate patient taking their medication and improve medication adherence.
Accessibility to Healthcare
According to the Report on Health Insurance Coverage in the United States, people without insurance and access to healthcare are less likely to have a primary care provider. Therefore, they may not be able to receive the healthcare services and medications they need, which leads to poor health outcomes.45 In this review, a prospective study determined the barriers to medication adherence for secondary prevention in 132 patients with IS. The researcher found that patients with difficulties accessing the hospital were more likely not to adhere to their stroke medications.39
Social and Community Context
Medication Management Due to Social Context
The relationships and interactions with family, friends, or community members can impact health and well-being.27 Positive connections at home, work, and in the community can help reduce adverse health impacts. On the other hand, living in unsafe neighborhoods can harm health and safety.27 In our review, one included study found that social and community contexts negatively impact patients with IS and TIA health. The study by Viprey et al showed that patients had difficulties adhering to their medications because of their social context. Notably, one participant stated during the interview, “It is true that when you’ve, for example, have guests at home, you think more about taking care of the guests, you do not necessarily take care of your pills”.34 Hence, we recommend that having good relationships with friends and family can positively impact health and promote a regular medication management routine.
Others
Cognitive Impairment
One theme, cognitive impairment, did not fall into any domain of SDoH. Therefore, it was coded as “Others”. In this review, two studies found that cognitive impairment was a barrier to medication adherence in patients with stroke.38,39 Shani et al determined factors associated with medication adherence among stroke survivors and found that patients with memory issues were more likely to not be adherent to medications (OR = 0.34; 95% CI, 0.16–0.71).38 Similarly, another study determined the barriers to medication adherence for secondary prevention in patients with IS and found that forgetfulness was a factor that prevented patients from adhering to their medication.39 For patients with cognitive impairment encouraging healthcare professionals working with caregivers to help manage patients’ medication could enhance their medication adherence.
Discussion
Our review found that the SDoH can affect the ability and willingness of patients with stroke to adhere to medications. Unstable financial resources were found as a significant barrier for IS patients in adhering to their medication plans. This finding is in contrast to studies with socialized medicine access, such as one conducted in Sweden, which found no significant interaction between medication adherence to statin treatment after stroke and patients’ income.46 Similarly, a study of the socioeconomic status and the care after stroke in Canadian stroke patients revealed similar medication adherence rates across different income groups. They suggested that medication adherence may not be the primary reason for different health outcomes among people with varying income levels after a stroke.47
Despite the conflicting findings, evidence suggests that government health policies covering post-stroke medication costs can help reduce non-adherence. For example, a study conducted in the US found that implementing the Affordable Care Act, which increased health insurance coverage, was associated with a decrease in cost-related non-adherence to medication among adult stroke survivors. These findings suggested that expanding health insurance coverage could benefit stroke survivors in terms of their ability to afford and adhere to medication, resulting in positive health outcomes.48 Further investigations are needed to determine the specific factors contributing to the financial burden for stroke survivors and their impact on medication adherence. Additionally, examining the effectiveness of different government health policies and programs in reducing the financial burden and improving medication adherence among stroke survivors are essential elements to be addressed in future research.
Regarding health literacy, our findings indicate that low health literacy is a significant barrier to medication adherence among stroke patients, which is consistent with previous research demonstrating that health literacy is a strong predictor of medication adherence.49 One explanation could be that patients with low health literacy may have limited knowledge about their medications, which makes it difficult for them to understand the importance of adhering to them.50 Additionally, patients with low literacy may struggle with establishing routines that facilitate medication adherence.51 These findings highlight the need for increased access to health education to improve medication knowledge and better support for stroke patients in adhering to their medication regimens.
Our study also suggests that health behavior can be an important factor influencing medication adherence, consistent with previous studies examining the relationship between health behaviors and medication adherence.52,53 One possible explanation is that education significantly predicts health behaviors, such as substance use, physical activity, and diet.54 Different levels of education can also influence changes in health behaviors. For example, one study found that a group with higher educational attainment achieved higher smoking cessation rates two years after the intervention.55 Given that the reviewed studies did not examine the direct association between education and medication adherence, future studies need to focus more on how education plays a role in the relationship between health literacy, health behaviors, and medication adherence among stroke patients.
Healthy People 2030 focuses strongly on healthcare access and the quality of healthcare services.27 Our review presented healthcare access and quality factors incorporated with medication adherence through multilevel factors. Individual-level factors, such as medication side effects, medication belief, and polypharmacy, were relevant to medication adherence among stroke survivors. Regarding side effects, the findings were congruent with a previous study that reported a correlation between lower medication adherence and experiencing more drug-related side effects in patients with hypertension.56 Moreover, high worrying scores about taking medication has been shown to be a barrier to medication adherence which may affect stroke survivors’ beliefs about the medications.40 The finding reported that some stroke survivors, who perceived the act of taking medication as excessive, also held the belief that taking medication could be harmful to their bodies.36,57 Additionally, medication beliefs by stroke survivors were reported to have a greater significant impact than any other barriers to medication adherence.57 Others were medication frequency, where less frequency of daily doses was related to better medication adherence, which concurs with previous studies conducted in elderly populations.37,58 However, medication adherence resulting from timing issues can be improved by providing medication education, as indicated in a study among patients with hypertension, improving health outcomes.59
Given the interpersonal level, the results from the review highlighted that the physicians’ and patients’ interactions play a vital role in medication adherence. One of the barriers to achieving adherence is a lack of health information associated with ineffective communication between physicians and patients.34 Ineffective patient-provider communication hinders medication adherence among patients with hypertension, inflammatory arthritis, and multimorbidity.60–62 Furthermore, the review exploring communication skills and the patient-physician relationship by Drossman et al also emphasized that effective communication, trust in healthcare, and the physician’s time allocation can directly improve self-efficacy, health literacy, and medication adherence.62 This could potentially promote long-term behavioral adherence among patients with TIA and stroke as secondary or tertiary prevention.
In addition, considering the healthcare system level, our review identified the accessibility to healthcare, described as a geographic barrier to medication adherence. The previous literature has shown that innovations aiming to improve healthcare access, such as telemedicine, and medication delivery program, significantly improve adherence.63,64 The innovation facilitating healthcare access is vital to empowering patients to engage more in their health and self-management, improving health outcomes.
The relationships and interactions with family, friends, or community members can impact health and well-being.27 Positive connections at home, work, and in the community can help reduce adverse health impacts. However, in our review, one included study found that social and community contexts sometimes negatively impact patients with IS and TIA health. The study by Viprey et al showed that patients might have difficulties related to the practical management of medicines due to the social context.34
All of these point to the fact that social, cultural, and community contexts need to be incorporated into the medication management routines of patients. Patients should be encouraged to talk about their social, cultural, and community contexts to figure out how this may be used to improve medication adherence with their providers. For instance, a family member or a close friend could be part of the medication routine for the patient. This way, patients could be accountable to somebody closer, perhaps spatially and in terms of relations, than their physicians. In addition, these individuals may help remind patients of their medication routines and ensure that they comply with them. The study by Edward et al shows that utilizing family members, community support groups, and education based on community outreach, amongst other factors, are important facilitators of medication adherence. The healthcare providers included in the study also highlighted the importance of counseling family members, utilizing younger family members, and utilizing religious leaders to share information as important facilitators of medication adherence.65
Two included studies reveal that cognitive impairment is a barrier to medication adherence in patients with stroke.38,39 Shani et al investigated various factors associated with medication adherence among stroke survivors, finding that patients with memory issues have an increased likelihood of non-adherence to medication.38 A similar study explored the barriers to medication adherence in patients with IS, with forgetfulness being a factor in preventing patients from adhering to their medication.39 However, two contrasting studies note that cognitive impairment does not lead to increased non-medication adherence.66,67 Despite the conflicting conclusions on the effect of cognitive impairment on medication adherence, a study has been done to support such patients. A study conducted by Rohde et al found that aiding family members and caregivers significantly improves medication adherence in stroke patients suffering from cognitive impairment.68 Further investigation on the involvement of other methods of reminding patients, like alarms or medication reminder devices, should be investigated to assist cognitively impaired patients to compare it to the effectiveness of using humans as reminders.
Finally, although our review could not identify any factors related to neighborhood and built environment impacting medication adherence among stroke survivors, the evidence showed that neighborhood violence and unhealthy built environments, measured by inaccessibility to exercise opportunities and pharmacies, were also associated with poorer medication adherence among people with other medical conditions.69,70 Exploring this factor may be crucial to prioritize attention in promoting medication adherence for stroke survivors in specific areas.
The systematic review has certain limitations that should be noted. Firstly, the inclusion criteria requiring studies to be in the English language acted as a limiting factor. As a result, qualified studies reported in other languages may have been omitted, potentially leading to a language bias in the review. Secondly, each of the included studies featured different sample sizes, target populations (with varying ischemic stroke types), study designs, and were conducted in different countries, using diverse measurements for medication adherence. These variations may have introduced heterogeneity, which could account for the differences observed in the study outcomes. Lastly, the use of the SDoH framework in this review may not encompass all barriers to medication adherence (eg, cognitive impairment). For future research, it is advisable to consider integrating the SDOH framework with other models to provide a more comprehensive understanding of the factors influencing medication adherence.
Conclusion
SDoH can have a significant impact on medication adherence among stroke patients. Factors such as finances, education, health literacy, healthcare quality, access to healthcare, social support, and cognitive status can influence the ability and willingness of stroke patients to follow their prescribed treatment regimen. Medication adherence is crucial for preventing recurrent strokes and improving quality of life. Therefore, to promote medication adherence, a multifaceted approach to address SDoH is needed. This review suggests possible strategies, including providing appropriate patient education, enhancing provider-patient communication and trust, facilitating social support, improving health literacy and health system navigation, utilizing technology to support medication management, and advocating for policies that reduce cost and improve access to medications and health services to enhance medication adherence among patients with IS.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Mahidol University, Thailand, supported the article processing charge.
Disclosure
The authors advise there are no conflicts of interest to declare.
References
- 1.Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54(2):171–179. doi: 10.1159/000506396 [DOI] [PubMed] [Google Scholar]
- 2.Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820. doi: 10.1016/S1474-4422(21)00252-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 4.Arboix A, Font A, Garro C, Garcia-Eroles L, Comes E, Massons J. Recurrent lacunar infarction following a previous lacunar stroke: a clinical study of 122 patients. J Neurol Neurosurg Psychiatry. 2007;78(12):1392–1394. doi: 10.1136/jnnp.2007.119776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arboix A, Oliveres M, Massons J, Pujades R, García‐Eroles L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: a multivariate analysis. Eur J Neurol. 1999;6(6):677–683. doi: 10.1046/j.1468-1331.1999.660677.x [DOI] [PubMed] [Google Scholar]
- 6.Flach C, Muruet W, Wolfe CD, Bhalla A, Douiri A. Risk and secondary prevention of stroke recurrence: a population-base cohort study. Stroke. 2020;51(8):2435–2444. doi: 10.1161/STROKEAHA.120.028992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han J, Mao W, Ni J, et al. Rate and determinants of recurrence at 1 year and 5 years after stroke in a low-income population in rural China. Front Neurol. 2020;11:2. doi: 10.3389/fneur.2020.00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stahmeyer JT, Stubenrauch S, Geyer S, Weissenborn K, Eberhard S. The frequency and timing of recurrent stroke: an analysis of routine health insurance data. Dtsch Arztebl Int. 2019;116(42):711–717. doi: 10.3238/arztebl.2019.0711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aarnio K, Haapaniemi E, Melkas S, Kaste M, Tatlisumak T, Putaala J. Long-term mortality after first-ever and recurrent stroke in young adults. Stroke. 2014;45(9):2670–2676. doi: 10.1161/STROKEAHA.114.005648 [DOI] [PubMed] [Google Scholar]
- 10.Coull A, Lovett J, Rothwell P. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ. 2004;328(7435):326. doi: 10.1136/bmj.37991.635266.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westberg A, Sjölander M, Glader E-L, Gustafsson M. Primary non-adherence to preventive drugs and associations with beliefs about medicines in stroke survivors. Patient Prefer Adherence. 2022;16:343–352. doi: 10.2147/ppa.s351001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kronish IM, Diefenbach MA, Edmondson DE, Phillips LA, Fei K, Horowitz CR. Key barriers to medication adherence in survivors of strokes and transient ischemic attacks. J Gen Intern Med. 2013;28:675–682. doi: 10.1007/s11606-012-2308-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang Y, Yang X, Li Z, et al. Persistence of secondary prevention medication and related factors for acute ischemic stroke and transient ischemic attack in China. Neurol Res. 2017;39(6):492–497. doi: 10.1080/01616412.2017.1312792 [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Gong Y, Zhao Y, Jiang N, Wang J, Yin X. Post-stroke medication adherence and persistence rates: a meta-analysis of observational studies. J Neurol. 2021;268:2090–2098. doi: 10.1007/s00415-019-09660-y [DOI] [PubMed] [Google Scholar]
- 15.Osborn CY, Kripalani S, Goggins KM, Wallston KA. Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients. J Health Care Poor Underserved. 2017;28(1):499–513. doi: 10.1353/hpu.2017.0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Macquart de Terline D, Kane A, Kramoh KE, et al. Factors associated with poor adherence to medication among hypertensive patients in twelve low and middle income Sub-Saharan countries. PLoS One. 2019;14(7):e0219266. doi: 10.1371/journal.pone.0219266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mamaghani EA, Hasanpoor E, Maghsoodi E, Soleimani F. Barriers to medication adherence among hypertensive patients in deprived rural areas. Ethiop J Health Sci. 2020;30(1). doi: 10.4314/ejhs.v30i1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Driever EM, Brand PLP. Education makes people take their medication: myth or maxim? Breathe. 2020;16(1):190338. doi: 10.1183/20734735.0338-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu L, Wu S, Zhao S, Zhou H, Zhang S, Gao M. Association of social support and medication adherence in Chinese patients with type 2 diabetes mellitus. Int J Environ Res Public Health. 2017;14(12):1522. doi: 10.3390/ijerph14121522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chu H-Y, Huang H-C, Huang C-Y, et al. A predictive model for identifying low medication adherence among older adults with hypertension: a classification and regression tree model. Geriatr Nurs. 2021;42(6):1309–1315. doi: 10.1016/j.gerinurse.2021.08.011 [DOI] [PubMed] [Google Scholar]
- 21.Wan J, Wu Y, Ma Y, Tao X, Wang A. Predictors of poor medication adherence of older people with hypertension. Nurs Open. 2022;9(2):1370–1378. doi: 10.1002/nop2.1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heizomi H, Iraji Z, Vaezi R, Bhalla D, Morisky DE, Nadrian H. Gender differences in the associations between health literacy and medication adherence in hypertension: a population-based survey in Heris County, Iran. Vasc Health Risk Manag. 2020;16:157. doi: 10.2147/VHRM.S245052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pinhati RR, Ferreira RE, Carminatti M, et al. The prevalence and associated factors of nonadherence to antihypertensive medication in secondary healthcare. Int Urol Nephrol. 2021;53(8):1639–1648. doi: 10.1007/s11255-020-02755-w [DOI] [PubMed] [Google Scholar]
- 24.Chang S-M, I-C L, Chen Y-C, Hsuan C-F, Lin Y-J, Chuang H-Y. Behavioral factors associated with medication nonadherence in patients with hypertension. Int J Environ Res Public Health. 2021;18(18):9614. doi: 10.3390/ijerph18189614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wakai E, Ikemura K, Kato C, Okuda M. Effect of number of medications and complexity of regimens on medication adherence and blood pressure management in hospitalized patients with hypertension. PLoS One. 2021;16(6):e0252944. doi: 10.1371/journal.pone.0252944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adinkrah E, Bazargan M, Wisseh C, Assari S. Adherence to hypertension medications and lifestyle recommendations among underserved African American middle-aged and older adults. Int J Environ Res Public Health. 2020;17(18):6538. doi: 10.3390/ijerph17186538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.HHS. Social determinants of health. U.S. Department of health and human services, office of disease prevention and health promotion 2023; 2023. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health. Accessed August 24, 2023.
- 28.Gary F, Lotas M. A Population Health Approach to Health Disparities for Nurses: Care of Vulnerable Populations. Springer Publishing Company; 2022. [Google Scholar]
- 29.Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. JBI Rev Manual Joanna Brig Instit. 2017;5:217–269. [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873–880. doi: 10.1093/ptj/89.9.873 [DOI] [PubMed] [Google Scholar]
- 31.Aromataris EMZ. JBI Manual for Evidence Synthesis. Joanna Briggs Institute; 2020. [Google Scholar]
- 32.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. JBI Evid Implement. 2015;13(3):179–187. [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG; Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 34.Viprey M, Gouillet M, Puppo C, et al. A qualitative study of barriers and facilitators to adherence to secondary prevention medications among French patients suffering from stroke and transient ischemic attack. Patient Preference Adherence. 2020;14:1213–1223. doi: 10.2147/PPA.S257323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saade S, Kobeissy R, Sandakli S, et al. Medication adherence for secondary stroke prevention and its barriers among Lebanese survivors: a cross-sectional study. Clin Epidemiol Global Health. 2021;9:338–346. doi: 10.1016/j.cegh.2020.10.007 [DOI] [Google Scholar]
- 36.Fan QQ, Doshi K, Narasimhalu K, et al. Impact of beliefs about medication on the relationship between trust in physician with medication adherence after stroke. Patient Educ Couns. 2022;105(4):1025–1029. doi: 10.1016/j.pec.2021.07.016 [DOI] [PubMed] [Google Scholar]
- 37.Kim -G-G, Chae D-H, Park M-S, Yoo S-H. Factors influencing 1-year medication adherence of Korean ischemic stroke survivors. Int J Behav Med. 2020;27(2):225–234. doi: 10.1007/s12529-020-09854-z [DOI] [PubMed] [Google Scholar]
- 38.Shani SD, Sylaja PN, Sarma PS, Kutty VR. Facilitators and barriers to medication adherence among stroke survivors in India. J Clin Neurosci. 2021;88:185–190. doi: 10.1016/j.jocn.2021.03.019 [DOI] [PubMed] [Google Scholar]
- 39.Velusamy S, Varatharaj K, Kathirvel R, Venkatesan P, Varghese LJ. Determination of barriers in medication adherence for secondary prevention in stroke patients. Indian J Pharm Pharmacol. 2022;15(2):83–89. doi: 10.5530/ijopp.15.2.16 [DOI] [Google Scholar]
- 40.Ruksakulpiwat S, Liu Z, Yue S, Fan Y. The association among medication beliefs, perception of illness and medication adherence in ischemic stroke patients: a cross-sectional study in China. Patient Prefer Adherence. 2020;14:235. doi: 10.2147/PPA.S235107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheiloudaki E, Alexopoulos EC. Adherence to treatment in stroke patients. Int J Environ Res Public Health. 2019;16(2):196. doi: 10.3390/ijerph16020196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hewitt M. Facilitating State Health Exchange Communication Through the Use of Health Literate Practices: Workshop Summary. National Academies Press; 2012. [Google Scholar]
- 43.NIA. The dangers of polypharmacy and the case for deprescribing in older adults. 2022. Available from: https://www.nia.nih.gov/news/dangers-polypharmacy-and-case-deprescribing-older-adults. Accessed August 24, 2023.
- 44.Kurczewska-Michalak M, Lewek P, Jankowska-Polańska B, et al. Polypharmacy management in the older adults: a scoping review of available interventions. Front Pharmacol. 2021;12. doi: 10.3389/fphar.2021.734045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berchick ER, Barnett JC, Upton RD. Health Insurance Coverage in the United States, 2018. US Department of Commerce, US Census Bureau; 2019. [Google Scholar]
- 46.Sjölander M, Eriksson M, Glader EL. Inequalities in medication adherence to statin treatment after stroke: a nationwide observational study. Eur Stroke J. 2016;1(2):101–107. doi: 10.1177/2396987316646026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang K, Khan N, Kwan A, Fang J, Yun L, Kapral MK. Socioeconomic status and care after stroke. Stroke. 2013;44(2):477–482. doi: 10.1161/STROKEAHA.112.672121 [DOI] [PubMed] [Google Scholar]
- 48.Levine DA, Burke JF, Shannon CF, Reale BK, Chen LM. Association of medication nonadherence among adult survivors of stroke after implementation of the US Affordable Care Act. JAMA Neurol. 2018;75(12):1538–1541. doi: 10.1001/jamaneurol.2018.2302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee Y-M, Yu HY, You M-A, Son Y-J. Impact of health literacy on medication adherence in older people with chronic diseases. Collegian. 2017;24(1):11–18. doi: 10.1016/j.colegn.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 50.Federman AD, Wolf MS, Sofianou A, et al. Self‐management behaviors in older adults with asthma: associations with health literacy. J Am Geriatr Soc. 2014;62(5):872–879. doi: 10.1111/jgs.12797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Federman AD, Wisnivesky JP, Wolf MS, Leventhal H, Halm EA. Inadequate health literacy is associated with suboptimal health beliefs in older asthmatics. J Asthma. 2010;47(6):620–626. doi: 10.3109/02770901003702816 [DOI] [PubMed] [Google Scholar]
- 52.Han E, Sohn HS, Lee J-Y, Jang S. Health behaviors and medication adherence in elderly patients. Am J Health Promot. 2017;31(4):278–286. doi: 10.4278/ajhp.150205-QUAN-709 [DOI] [PubMed] [Google Scholar]
- 53.Pellowski JA, Kalichman SC. Health behavior predictors of medication adherence among low health literacy people living with HIV/AIDS. J Health Psychol. 2016;21(9):1981–1991. doi: 10.1177/1359105315569617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brunello G, Fort M, Schneeweis N, Winter‐Ebmer R. The causal effect of education on health: what is the role of health behaviors? Health Econ. 2016;25(3):314–336. doi: 10.1002/hec.3141 [DOI] [PubMed] [Google Scholar]
- 55.Zhuang Y-L, Gamst AC, Cummins SE, Wolfson T, Zhu S-H. Comparison of smoking cessation between education groups: findings from 2 US National Surveys over 2 decades. Am J Public Health. 2015;105(2):373–379. doi: 10.2105/AJPH.2014.302222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tedla YG, Bautista LE. Drug side effect symptoms and adherence to antihypertensive medication. Am J Hypertens. 2016;29(6):772–779. doi: 10.1093/ajh/hpv185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence. 2018;12:1687–1698. doi: 10.2147/PPA.S169236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jin H, Kim Y, Rhie SJ. Factors affecting medication adherence in elderly people. Patient Prefer Adherence. 2016;10:2117–2125. doi: 10.2147/PPA.S118121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ayodapo A, Elegbede O, Omosanya O, Monsudi K. Patient education and medication adherence among hypertensives in a tertiary hospital, South Western Nigeria. Ethiop J Health Sci. 2020;30(2). doi: 10.4314/ejhs.v30i2.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tavakoly Sany SB, Behzhad F, Ferns G, Peyman N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res. 2020;20:1–10. doi: 10.1186/s12913-020-4901-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kelly A, Tymms K, de Wit M, et al. Patient and caregiver priorities for medication adherence in gout, osteoporosis, and rheumatoid arthritis: nominal group technique. Arthritis Care Res. 2020;72(10):1410–1419. doi: 10.1002/acr.24032 [DOI] [PubMed] [Google Scholar]
- 62.Drossman DA, Chang L, Deutsch JK, et al. A review of the evidence and recommendations on communication skills and the patient–provider relationship: a Rome foundation working team report. Gastroenterology. 2021;161(5):1670–1688. e7. doi: 10.1053/j.gastro.2021.07.037 [DOI] [PubMed] [Google Scholar]
- 63.Neil WP, Shiokari CE, Burchette RJ, Stapleton D, Ovbiagele B. Mail order pharmacy use and adherence to secondary prevention drugs among stroke patients. J Neurol Sci. 2018;390:117–120. doi: 10.1016/j.jns.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 64.Thakkar J, Kurup R, Laba T-L, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA Intern Med. 2016;176(3):340–349. doi: 10.1001/jamainternmed.2015.7667 [DOI] [PubMed] [Google Scholar]
- 65.Edward A, Campbell B, Manase F, Appel LJ. Patient and healthcare provider perspectives on adherence with antihypertensive medications: an exploratory qualitative study in Tanzania. BMC Health Serv Res. 2021;21(1):834. doi: 10.1186/s12913-021-06858-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wawruch M, Zatko D, Wimmer JG, et al. Patient‐related characteristics associated with non‐persistence with statin therapy in elderly patients following an ischemic stroke. Pharmacoepidemiol Drug Saf. 2017;26(2):201–207. doi: 10.1002/pds.4148 [DOI] [PubMed] [Google Scholar]
- 67.Wawruch M, Zatko D, Wimmer G, et al. Factors influencing non-persistence with antiplatelet medications in elderly patients after ischaemic stroke. Drugs Aging. 2016;33:365–373. doi: 10.1007/s40266-016-0365-2 [DOI] [PubMed] [Google Scholar]
- 68.Rohde D, Gaynor E, Large M, et al. Cognitive impairment and medication adherence post-stroke: a five-year follow-up of the ASPIRE-S cohort. PLoS One. 2019;14(10):e0223997. doi: 10.1371/journal.pone.0223997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Donneyong MM, Chang T-J, Jackson JW, et al. Structural and social determinants of health factors accounted for county-level variation in non-adherence to antihypertensive medication treatment. medRxiv. 2020;2020:4826. doi: 10.1101/2020.06.07.20124826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wilder ME, Kulie P, Jensen C, et al. The impact of social determinants of health on medication adherence: a systematic review and meta-analysis. J Gen Intern Med. 2021;36:1359–1370. doi: 10.1007/s11606-020-06447-0 [DOI] [PMC free article] [PubMed] [Google Scholar]