Abstract
Objective
The number of primary hip arthroplasty (PHA) has increased sharply in recent years. Whether the epidemiological characteristics and trends of PHA have changed are unknown. This study aims to analyze the epidemiological characteristics and trends of those patients are urgent for public health institutions.
Methods
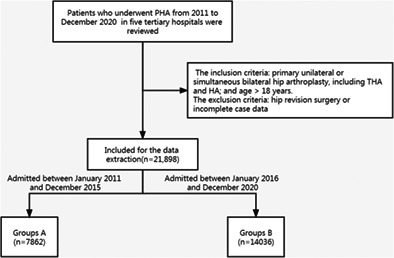
The data of patients who underwent PHA in five tertiary hospitals from January 2011 to December 2020 were retrospectively reviewed. A total of 21,898 patients were included, most of whom were aged 60–69 years (25.1% males and 31.5% females). According to the hospitalization date, the patients were divided into two groups (Group A and Group B). The patients admitted between January 2011 and December 2015 were designated as Group A (7862), and those admitted between January 2016 and December 2020 were designated as Group B (14036). The patient data of the two groups, including sex, age, disease causes, body mass index (BMI), comorbidities, surgical procedures, hospital stay duration, and hospitalization costs, were analyzed by Pearson chi‐Square test, Student t test or Mann–Whitney U test.
Results
More women were included in Group B than in Group A (58.5% vs 52.5%, P < 0.001). The mean age of Group B was less than that of Group A (62.27 ± 14.77 vs 60.69 ± 14.44 years, P < 0.001). Femoral head necrosis was the primary pathogenic factor in both groups, with a higher proportion in Group B than in Group A (55.5% vs 45.5%, P < 0.001). Significant differences were found between the two groups in BMI, comorbidities, surgical procedures, hospital stay duration, and hospitalization costs. Total hip arthroplasty (THA) was the most common surgical procedure in both groups, with a higher proportion in Group B than in Group A (89.8% vs 79.3%, P < 0.001). The proportion of patients with one or more comorbidities was significantly higher in Group B than in Group A (69.2% vs 59.9%, P < 0.001). In addition, Group B had a shorter hospital stay duration and higher hospitalization costs than Group A.
Conclusion
Femoral head necrosis was the primary etiology for PHA in this study, followed by femoral neck fracture and hip osteoarthritis. Patients who underwent PHA exhibited a higher percentage of femoral head necrosis; underwent THA more often; and had larger BMIs, more comorbidities, higher medical costs, and younger age in the past decade.
Keywords: Epidemiology, Femur head necrosis, Hip arthroplasty, Primary hip arthroplasty, Total hip arthroplasty
Epidemiological characteristics and trends of primary‐hip‐arthroplasty.
Introduction
The hip joint is one of the largest weight‐bearing joints in the human body and is located at the junction of the torso and lower limbs. It plays an essential role in sitting, walking, and lying down. The number of hip joint diseases is expected to increase due to the increased aging population worldwide. 1 Hip arthroplasty is one of the most commonly performed elective surgical procedures in China. The volume of primary THA, including total hip arthroplasty (THA) and hemiarthroplasty (HA), has risen dramatically over the past several decades. The number of hip arthroplasties will continue to increase among the aging population due to increased unfavorable risk factors (obesity and osteoarthritis). 2 Hip arthroplasty has become a serious public concern since it is associated with an enormous economic burden on health care systems and an increased number of revision procedures.
Hip arthroplasty involves the reconstruction of the joint to eliminate clinical symptoms and restore the joint function of patients. It also has the advantages of fewer complications and rapid recovery after surgery. The mode of hip arthroplasty has changed due to the continuous improvement of medical technology. THA and HA are used for femoral neck fracture, femoral head necrosis, hip osteoarthritis, hip dysplasia, rheumatoid arthritis, ankylosing spondylitis, traumatic arthritis, and infectious arthritis. More than 400,000 THAs are performed each year in China. 3 The estimated prevalence of THA in adults aged 50 years and older in the United States was 2.34% in 2010. 4
Although few epidemiological investigations of hip arthroplasty cover all ages, most are single‐center studies with small sample sizes and shorter periods, and none are comparative studies. Therefore, a large‐scale multicenter study is necessary to investigate the characteristics of patients undergoing hip arthroplasty in China. This study retrospectively analyzed the data of inpatients who underwent PHA in five tertiary hospitals in China during the past 10 years. Moreover, the changing trends of sex, age, causes, body mass index (BMI), concomitant diseases, surgical procedures, duration of hospital stay, and hospitalization costs were analyzed to provide epidemiological data for hip diseases. This study aims to analyze the epidemiological characteristics and trends of those patients are urgent for public health institutions. We proposed hypotheses as: (i) the femoral head necrosis is still the primary etiology for PHA; (ii) THA is a growing proportion of surgery in patients of PHA; and (iii) The age of PHA patients exhibits a younger trend.
Patients and Methods
Inclusion and Exclusion Criteria
The local ethical review committee approved this study (NO. 2015‐002‐1). The data of patients who underwent PHA from January 2011 to December 2020 in five tertiary hospitals, including the Third Hospital of Hebei Medical University, the Affiliated Hospital of Qingdao University, Wuhan Union Hospital, the First People's Hospital of Shanghai Jiao Tong University, and the Second Affiliated Hospital of Wenzhou Medical University, were reviewed. A total of 21,898 patients were included. The inclusion criteria were patients with primary unilateral or simultaneous bilateral hip arthroplasty, including THA and HA. The exclusion criteria were as follows: (i) hip revision surgery; and (ii) incomplete case data, for example, incomplete baseline information, specific surgical procedure unknown. According to the hospitalization date, the patients were divided into groups (Groups A and B). Group A patients (7862) were admitted between January 2011 and December 2015, while Group B patients (14036) were admitted between January 2016 and December 2020.
Patient Characteristics
The patients' data, including sex, age, disease causes, BMI, comorbidities, surgical procedures, length of hospital stay, and hospitalization costs, were also reviewed. The surgical procedures were classified into unilateral THA, unilateral HA, simultaneous THA, and simultaneous HA. In addition, BMI was defined as underweight (≤18.5 kg/m2), normal (18.5 to 23.9 kg/m2), overweight (24.0 to 27.9 kg/m2), and obese (≥28 kg/m2). 5
Statistical Analysis
SPSS 23.0 software (IBM, Armonk, NY, USA) was used for all statistical analyses. A P value < 0.05 was considered statistically significant. Continuous variables corresponding to a normal distribution are expressed as the mean ± standard deviation, while the nonnormally distributed variables are expressed as the median with quartiles. Categorical variables are expressed as frequencies and percentages. Student's t test or the Mann–Whitney U test was used for continuous variable analysis, while the chi‐square test or Fisher's exact test was used for categorical analysis.
Results
Epidemiological Characteristics
In this study, 21,898 patients (10,467 males and 11,431 females) who underwent hip arthroplasty were included. The mean age of these patients was 62.26 ± 14.58 years. Most patients were aged 60–69 years (28.8%, 6298/21,898), followed by patients aged 50–59 years (21.7%, 4748/21,898). The pathogenies of PHA in this study included femoral head necrosis(51.9%, 11,370/21,898), femoral neck fracture (30.3% 6637/21,898), hip osteoarthritis (2%, 437/21,898), hip hypoplasia(5.6%, 1218/21,898), traumatic arthritis(2%, 437/21,898), femoral intertrochanteric fracture(1.1%, 232/21,898), ankylosing spondylitis (0.9%, 207/21,898), rheumatoid arthritis (0.4%, 85/21,898), and femoral head fracture (0.3%, 62/11,898). The number of patients who underwent unilateral THA, simultaneous THA, unilateral HA, and simultaneous HA was 18,844 (86.1%, 18,844/21,898), 2022 (9.2%, 2022/21,898), 1030 (4.7%, 1030/21,898), and 2 (0.00%, 2/21,898), respectively. A total of 14,430 patients (65.8%) had internal diseases, mainly hypertension, diabetes, coronary heart disease, cerebrovascular disease, and arrhythmia. A total of 7034 patients (32.1%) had one disease, 3668 patients (16.8%) had two diseases, and 3728 patients (17%) had three or more diseases. The median hospitalization duration was 12 days. The median hospitalization cost was 68,130.94 yuan, with an interquartile range of 30,491.00 yuan (6503–290,968 yuan) (Table 1).
TABLE 1.
General data of patients with hip arthroplasty from 2011 to 2020
| Variables | |
|---|---|
| Gender | |
| Male, n (%) | 10,467 (47.8) |
| Female, n (%) | 11,431 (52.2) |
| Age (Mean ± SD, years) | 62.26 ± 14.58 |
| BMI (Mean ± SD, kg/m2) | 23.73 ± 3.75 |
| ≤18.5, n (%) | 1778 (8.1) |
| 18.5–23.9, n (%) | 9821 (44.8) |
| 24–27.9, n (%) | 7801 (35.7) |
| ≥28, n (%) | 2498 (11.4) |
| Diagnosis | |
| Femoral head necrosis, n (%) | 11,370 (51.9) |
| Femoral neck fracture, n (%) | 6637 (30.3) |
| Hip osteoarthritis, n (%) | 1650 (7.5) |
| Hip hypoplasia, n (%) | 1218 (5.6) |
| Traumatic arthritis, n (%) | 437 (2.0) |
| Femoral intertrochanteric fracture, n (%) | 232 (1.1) |
| Ankylosing spondylitis, n (%) | 207 (0.9) |
| Rheumatoid arthritis, n (%) | 85 (0.4) |
| Femoral head fracture, n (%) | 62 (0.3) |
| Surgical side | |
| Left, n (%) | 10,273 (46.9) |
| Right, n (%) | 10,584 (48.3) |
| Both, n (%) | 1041 (4.8) |
| Operations | |
| Unilateral total hip arthroplasty, n (%) | 18 844 (86.1) |
| Unilateral hemiarthroplasty, n (%) | 2022 (9.2) |
| Simultaneous total hip arthroplasty, n (%) | 1030 (4.7) |
| Simultaneous hemiarthroplasty, n (%) | 2 (0.0) |
| Comorbidities | |
| 0, n (%) | 7468 (34.1) |
| 1, n (%) | 7034 (32.1) |
| 2, n (%) | 3668 (16.8) |
| ≥3, n (%) | 3728 (17) |
| Hospital stay, Median (Interquartile range) | 12 (8) |
| Hospitalization costs, Median (Interquartile range) | 68,130.94 (30,491.00) |
Abbreviation: BMI, body mass index.
Differences in Pathogenies between the Two Groups
In Group A, femoral head necrosis (45.5%, 3574/7862) was the most common pathogenesis of PHA, followed by femoral neck fracture (37%, 2907/7862) and hip osteoarthritis (7.1%, 577/7862). Similarly, in Group B, most patients had femoral head necrosis (55.5%, 7796/14,036), followed by femoral neck fracture (26.6%, 3730/14,036) and hip osteoarthritis (7.8%, 1095/14,036). The proportion of patients with femoral head necrosis was significantly higher in Group B than in Group A. In contrast, the proportion of patients with femoral neck fractures was significantly lower in Group B than in Group A.
BMI Results between the Two Groups
In Group A, most patients were overweight and obese (44.1%, 3467/7862), followed by normal‐weight patients (46. 3%, 3641/7862). Similarly, in Group B, most patients were overweight and obese (48.7%, 6832/14,036), followed by normal‐weight patients (44%, 6180/14,036). The proportion of overweight and obese patients was significantly higher in Group B than in Group A. The constituent ratio of BMI was significantly different between the two groups (X2 = 64.638, P < 0.05) (Table 2).
TABLE 2.
Comparison of gender composition ratio at all ages in group A and group B patients undergoing hip arthroplasty, n (%)
| Age Group | Group A | Total | Group B | Total | χ 2 | p value | ||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||
| 0–9 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | 0 (0.00) | 1 (0.0) | ‐ | ‐ |
| 10–19 | 8 (0.2) | 4 (0.1) | 12 (0.2) | 12 (0.2) | 9 (0.1) | 21 (0.2) | 0.290 | 0.590 a |
| 20–29 | 140 (3.9) | 74 (1.7) | 214 (2.7) | 264 (3.9) | 135 (1.9) | 399 (2.8) | 0.034 | 0.853 a |
| 30–39 | 257 (7.1) | 114 (2.7) | 371 (4.7) | 627 (9.2) | 259 (3.6) | 886 (6.3) | 0.280 | 0.597 a |
| 40–49 | 592 (16.3) | 308 (7.3) | 900 (11.4) | 1087 (15.9) | 556 (7.7) | 1643 (11.7) | 0.038 | 0.846 a |
| 50–59 | 863 (23.8) | 740 (17.5) | 1603 (20.4) | 1749 (25.6) | 1396 (19.4) | 3145 (22.4) | 1.353 | 0.245 a |
| 60–69 | 908 (25.0) | 1260 (29.8) | 2168 (27.6) | 1794 (26.2) | 2336 (32.5) | 4130 (29.5) | 1.406 | 0.236 a |
| 70–79 | 549 (15.1) | 1069 (25.3) | 1618 (20.6) | 896 (13.1) | 1647 (22.9) | 2543 (18.1) | 0.741 | 0.389 a |
| 80–89 | 280 (7.7) | 602 (14.2) | 882 (11.2) | 371 (5.4) | 752 (10.4) | 1123 (8.0) | 0.375 | 0.540 a |
| ≥90 | 33 (0.9) | 61 (1.4) | 94 (1.2) | 36 (0.5) | 109 (1.5) | 145 (1.0) | 2.934 | 0.087 a |
| Total | 3630 (100.0) | 4232 (100.0) | 7862 (100.0) | 6837 (100.0) | 7199 (100.0) | 14 036 (100.0) | 7.451 | 4.383 a |
Pearson Chi‐Square test.
Concomitant Diseases between the Two Groups
Common medical comorbidities include hypertension, diabetes, coronary heart disease, arrhythmia, cerebrovascular disease, arrhythmia, and pulmonary disease. In Group A, 4715 (59.9%) of 7862 patients had internal diseases. A total of 2441 patients (31%) had one disease, 1138 patients (14.5%) had two diseases, and 1136 patients (14.4%) had three or more diseases. In Group B, 9715 (69.2%) of 14,036 patients had internal diseases. A total of 4593 patients (32.7%) had one disease, 2539 patients (18%) had two diseases, and 2592 patients (18.5%) had three or more diseases. The number of patients with internal diseases was significantly higher in Group B than in Group A (P < 0.001, Table 2).
Operation Time, Hospital Stay Duration, and Hospitalization Costs between the Two Groups
In Group A, 6237 patients (79.3%, 6237/7862) underwent unilateral THA, 1113 patients (14.2%, 1113/7862) underwent unilateral HA, 511 patients (6.5%, 511/7862) underwent simultaneous bilateral THA, and one patient (0.0%, 1/7862) underwent simultaneous bilateral HA. In Group B, 12,607 patients (89.8%, 12,607/14,036) underwent unilateral THA, 909 patients (6.5%, 909/14,036) underwent unilateral HA, 519 patients (3.7%, 519/14,036) underwent simultaneous bilateral THA, and one patient (0.0%, 1/14,036) underwent simultaneous bilateral HA. The constituent ratio of surgery was significantly different between the two groups (X2 = 470.643, P < 0.001).
The median hospitalization duration of patients in Group A was 15 days, with an interquartile range of 8 days (range, 1–95 days). The median hospitalization duration of patients in Group B was 11 days, with an interquartile range of 6 days (range, 1–76 days). Group B patients had a significantly shorter hospital stay duration than Group A patients (Z = −39.514, P = 0.001).
The median hospitalization costs of patients in Group A were 62,964.82 RMB, with an interquartile range of 26,909 RMB (range, 6503–290,968 RMB). The median hospitalization cost of patients in Group B was 71,019.58 RMB, with an interquartile range of 30,802 RMB (range, 10,303–250,170 RMB). The hospitalization costs were significantly higher in Group B than in Group A (Z = −19.410, P = 0.005).
Discussion
In this study, 21,898 patients (10,467 males and 11,431 females) who underwent hip arthroplasty were included. The mean age of these patients was 62.26 ± 14.58 years. The pathogenies of PHA in this study included femoral head necrosis (51.9%, 11,370/21,898), femoral neck fracture (30.3% 6637/21,898), hip osteoarthritis(2%, 437/21,898), hip hypoplasia (5.6%, 1218/21,898), traumatic arthritis(2%, 437/21898), femoral intertrochanteric fracture (1.1%, 232/21,898), ankylosing spondylitis (0.9%, 207/21,898), rheumatoid arthritis (0.4%, 85/21,898), and femoral head fracture (0.3%, 62/11898).
Causes and Surgical Trends of Patients Undergoing Hip Arthroplasty
Femoral head necrosis (51.9%) was discovered as the primary pathogeny of PHA, followed by femoral neck fracture (30.3%), hip osteoarthritis (7.5%), hip hypoplasia (5.6%), traumatic arthritis (2.0%), femoral intertrochanteric fracture (1.1%), ankylosing spondylitis (0.9%), and femoral head fracture (0.3%), which was consistent with previous studies. 6 , 7 , 8 , 9 In addition, greater proportions of femoral head necrosis (55.5% vs 45.5), hip osteoarthritis (7.8% vs 7.1%), traumatic arthritis (2.1% vs 1.8%), hip hypoplasia (5.6% vs 5.5%), and femoral head fracture (0.3% vs 0.2%) were found in Group B than in Group A. To the best of our knowledge, few reports have assessed changes in the PHA procedure. Miller et al. 10 analyzed the data of patients with femoral neck fractures from the American Board of Orthopedic Surgery database between 1999 and 2011. The percentage of THA increased with time (from 0.7% in 1999 to 7.7% in 2011) and that of HA decreased with time. In this study, more unilateral THA was discovered in Group B than in Group A, and less unilateral HA was found in Group B than in Group A. The percentage of patients under 60 years old in Group B was 43.4%, which was higher than that in Group A (39.4%), which might be related to the increase in the proportion of THA.
Gender and Age Distribution in Patients Undergoing Hip Arthroplasty
The percentage of female patients who underwent PHA in this study was higher than that of male patients, which was consistent with previous studies. 11 , 12 , 13 Singh et al. 12 analyzed 6168 patients who underwent PHA from 1993 to 2005, where 52% were females and 48% were males. The mean age of the patients was 64.2 ± 13.8 years, which was similar to that in this study (62.26 ± 14.58 years). Namba et al. 14 retrospectively assessed 12,859 patients who underwent THA from 2008 to 2011, in which the median age was 67 years. More females were included than males (58% vs 42%). In this study, the average age of Group B was lower than that of Group A (60.7 vs 62.3, P < 0.001 in Table 3). Consistent with our study, Kurtz et al. found more demand in future young patients for primary total joint replacement surgery. 15
TABLE 3.
Comparison of general data between the two groups
| Variables | Group A | Group B | t/χ 2 /Z | P value |
|---|---|---|---|---|
| Gender | 13.020 | 0.001 a | ||
| Male, n (%) | 3630 (46.2) | 6837 (48.7) | ||
| Female, n (%) | 4232 (53.8) | 7199 (51.3) | ||
| Age(years), mean ± SD | 62.3 ± 14.8 | 60.7 ± 14.4 | 7.640 | <0.001 b |
| Diagnosis | 306.493 | 0.001 a | ||
| Femoral neck fracture, n (%) | 2907 (37) | 3730 (26.6) | ||
| Traumatic arthritis, n (%) | 145 (1.8) | 292 (2.1) | ||
| Rheumatoid arthritis, n (%) | 42 (0.5) | 43 (0.3) | ||
| Ankylosing spondylitis, n (%) | 82 (1.0) | 125 (0.9) | ||
| Femoral head necrosis, n (%) | 3574 (45.5) | 7796 (55.5) | ||
| Hip hypoplasia, n (%) | 429 (5.5) | 789 (5.6) | ||
| Primary arthritis, n (%) | 555 (7.1) | 1095 (7.8) | ||
| Femoral fracture, n (%) | 110 (1.4) | 122 (0.9) | ||
| Femoral head fracture, n (%) | 18 (0.2) | 44 (0.3) | ||
| BMI (kg/m2) | ||||
| ≤18.5, n (%) | 754 (9.6) | 1024 (7.3) | 64.638 | 0.001 a |
| 18.5‐23.9, n (%) | 3641 (46.3) | 6180 (44.0) | ||
| 24–27.9, n (%) | 2666 (33.9) | 5135 (36.6) | ||
| ≥28, n (%) | 801 (10.2) | 1697 (12.1) | ||
| Comorbidities | 216.338 | 0.001 a | ||
| 0, n (%) | 3147 (40.1) | 4321 (30.8) | ||
| 1, n (%) | 2441 (31) | 4593 (32.7) | ||
| 2, n (%) | 1138 (14.5) | 2539 (18) | ||
| ≥3, n (%) | 1136 (14.4) | 2592 (18.5) | ||
| Operations | ||||
| Unilateral total hip arthroplasty, n (%) | 6237 (79.3) | 12,607 (89.8) | 470.643 | 0.001 a |
| Unilateral hemiarthroplasty, n (%) | 1113 (14.2) | 909 (6.5) | ||
| Simultaneous total hip arthroplasty, n (%) | 511 (6.5) | 519 (3.7) | ||
| Simultaneous total hip arthroplasty, n (%) | 1 (0.0) | 1 (0.0) | ||
| Hospital stay, median (Interquartile range) | 15 (8) | 11 (6) | 39.514 | 0.001 c |
| Hospitalization cost, median (Interquartile range) | 62,694.82 (26909) | 71,019.58 (30802) | 19.410 | 0.005 c |
Pearson chi‐Square test.
Student t test.
Mann‐Whitney U test.
Trends of BMI and Concomitant Diseases
Obesity is the most prevalent metabolic disease worldwide, affecting adults, children, and adolescents. 16 , 17 , 18 Studies have shown that obesity is a risk factor for osteoarthritis and increases the length of hospital stay among patients undergoing joint replacement. 19 Kuroda et al. 20 retrospectively evaluated patients who underwent THA in Japan from 2006 to 2013 and found that their BMI was 23.2 ± 3.5 kg/m2. In this study, the mean BMI of patients was 23.73 ± 3.75 kg/m2, which is consistent with that found by Kuroda et al. In addition, more overweight and obese patients were included in Group B than in Group A (48.7% vs 44.1%, in Table 2). Tayne et al. 21 investigated the predictive risk of 30‐day readmission in patients undergoing THA and found that obesity increased the incidence of surgical adverse events. Therefore, preoperative weight loss and reasonable diet control can improve the postoperative effects and help to restore normal activities.
In this study, 65.9% of the patients who underwent PHA presented with medical diseases, with hypertension and diabetes accounting for the highest proportion, followed by cardiovascular diseases, which was consistent with previous studies. 22 , 23 , 24 There were significantly more patients with one or more comorbidities in Group B than in Group A (69.2% vs 59.9%). Some comorbidities (such as diabetes) can increase the incidence of postoperative complications in patients undergoing orthopedic surgery, including mortality, infection, blood transfusion, pneumonia, and unconventional discharge, thus increasing the length of hospital stay and total hospital costs. 25 , 26 , 27 Therefore, perioperative management, intraoperative coordinated management, and postoperative evaluation should be performed in a multidisciplinary manner to improve the prognosis of those patients.
Comparison of Hospitalization Duration and Costs of Patients Undergoing Hip Arthroplasty
In this study, the median hospital stay for patients undergoing hip arthroplasty was 12 days, which was shorter than that reported by Wenwei et al. 28 (14 days). A longer hospitalization was found in Group B than in Group A. A study of 961 inpatients who underwent hip arthroplasty in nine general hospitals in Belgium in 2014 showed that the hospital stay duration was 9 days (range, 6.29–20.91 days), which was shorter than that of this study. 29 In this study, the median hospitalization cost of hip arthroplasty patients was 68,130.94 RMB. The hospitalization cost in Group B was higher than that in Group A (71,019.58 vs 62,694.82, P = 0.005). Kumar et al. 30 analyzed patients who underwent THA in the United States from 1997 to 2001 and found that the total hospitalization cost, including direct and indirect costs, was approximately $13,339.1. Frerichmann et al. 31 evaluated patients undergoing hip arthroplasty in Germany in 2007 and found that the average hospitalization costs were 7000.7 Euros. De Foor et al. 29 retrospectively assessed 961 inpatients who underwent hip arthroplasty in nine general hospitals in Belgium in 2014 and reported that the hospitalization cost was 8023.91 Euros (range, 6678.32–13,670.78 Euros). The cost of hospitalization reported in this study was significantly lower than that in Belgium and the United States but significantly higher than that in Germany. Although the hospital stay duration of Group B was shorter than that of Group A, the hospitalization costs of Group B were significantly higher. This could be due to an increase in the price of consumables, perioperative examination, and drug costs of patients with multiple diseases.
Strengths and Limitations
This study was a large‐scale multicenter study, and a sufficiently large number of patients (21,898 patients) from five tertiary hospitals were reviewed. Meanwhile a broad range of variables on epidemiological characteristics of PHA patients were extracted. There were several limitations in this study, as follows: (i) advances in surgical techniques and implants may have influenced the clinical outcomes due to the difference in hospitalization time between the two groups of patients; and (ii) we only conducted an epidemiological analysis of limited clinical data, and more variables (such as geographical factors, mortality, and indications for surgery) need to be collected and analyzed in our future studies.
Conclusion
In this study, 21,898 patients who underwent hip arthroplasty were included, whose epidemiological characteristics have changed in the past 10 years. The pathogenies of PHA in this study included femoral head necrosis (51.9%, 11,370/21,898), femoral neck fracture (30.3% 6637/21,898), hip osteoarthritis(2%, 437/21,898), hip hypoplasia(5.6%, 1218/21898), traumatic arthritis(2%, 437/2,1898), femoral intertrochanteric fracture(1.1%, 232/21,9898), ankylosing spondylitis (0.9%, 207/2,1898), rheumatoid arthritis (0.4%, 85/21,898), and femoral head fracture (0.3%, 62/11,898). The number of patients who underwent unilateral THA, simultaneous THA, unilateral HA, and simultaneous HA was 18,844 (86.1%, 18844/21,898), 2022 (9.2%, 2022/21,898), 1030 (4.7%, 1030/21,898), and 2 (0.00%, 2/21,898), respectively. Patients who underwent PHA exhibited a higher percentage of femoral head necrosis; underwent THA more often; and had larger BMIs, more comorbidities, higher medical costs, and younger age in the past decade.
Author Contributions
Yingze Zhang designed this study; Weiyi Sun wrote the manuscript; Kuo Zhao, Yanwei Wang, Kuishuai Xu and Lin Jin collected and analyzed the data; Wei Chen and Zhiyong Hou revised the manuscript; and Yingze Zhang approved the final version of the manuscript.
Conflict of Interest Statement
All authors declare that they have no conflicts of interest.
Ethical Statement
Implementation of this study was agreed by local ethical review committee.
Acknowledgments
We would like to thank ZZ J and YC W for their assistance in data collection. This study was funded by the National Key R&D Program of China (Grant No. 2019YFC0120600).
Weiyi Sun, Kuo Zhao and Yanwei Wang have made equal contributions to this study.
References
- 1. Sheth NP, Melnic CM, Rozell JC, Paprosky WG. Management of severe femoral bone loss in revision total hip arthroplasty. Orthop Clin North Am. 2015;46(3):329–42. [DOI] [PubMed] [Google Scholar]
- 2. lug A, Pfluger DH, Gramlich Y, Hoffmann R, Drees P, Kutzner KP. Future burden of primary and revision hip arthroplasty in Germany: a socio‐economic challenge. Arch Orthop Trauma Surg. 2021;141(11):2001–10. [DOI] [PubMed] [Google Scholar]
- 3. Cao J, Zhou Y, Xin W, Zhu J, Chen Y, Wang B, et al. Natural outcome of hemoglobin and functional recovery after the direct anterior versus the posterolateral approach for total hip arthroplasty: a randomized study. J Orthop Surg Res. 2020;15(1):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Patel I, Nham F, Zalikha AK, El‐Othmani MM. Epidemiology of total hip arthroplasty: demographics, comorbidities and outcomes. Arthroplasty. 2023;5(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gutin I, In BMI. We trust: reframing the body mass index as a measure of health. Soc Theory Health. 2018;16(3):256–71. 10.1057/s41285-017-0055-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tamaki T, Nakakita Y, Miura Y, Higashi H, Oinuma K, Shiratsuchi H. Radiographic factors to predict operation time of direct anterior total hip arthroplasty for dysplastic hips. Hip Int. 2021;31(1):90–6. [DOI] [PubMed] [Google Scholar]
- 7. Klasan A, Neri T, Oberkircher L, Malcherczyk D, Heyse TJ, Bliemel C. Complications after direct anterior versus Watson‐Jones approach in total hip arthroplasty: results from a matched pair analysis on 1408 patients. BMC Musculoskelet Disord. 2019;20(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nagase Y, Yasunaga H, Horiguchi H, Hashimoto H, Shoda N, Kadono Y, et al. Risk factors for pulmonary embolism and the effects of fondaparinux after Total hip and knee arthroplasty: a retrospective observational study with use of a National Database in Japan. J Bone Jt Surg Am. 2011;93(24):e146. [DOI] [PubMed] [Google Scholar]
- 9. Bozic KJ, Katz P, Cisternas M, et al. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Jt Surg Am. 2005;87(3):570–6. [DOI] [PubMed] [Google Scholar]
- 10. Miller BJ, Callaghan JJ, Cram P, et al. Changing trends in the treatment of femoral neck fractures:a review of the american board of Orthopaedic surgery database. J Bone Jt Surg Am. 2014;96(17):e149. [DOI] [PubMed] [Google Scholar]
- 11. Wang XQ, Wu CS, Sun S, Wang J, Li W, Zhang W. A therapeutic effect analysis of femur first principle and combined anteversion technique during total hip arthroplasty. Zhonghua Waike Zazhi. 2018;56(4):279–83. [DOI] [PubMed] [Google Scholar]
- 12. Assaker A, Trivellin G, Vacchiano A, Cominelli D, Meyer A. Direct anterior total hip arthroplasty: a retrospective study. Acta Biomed. 2020;91(4S):98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Singh JA, Lewallen DG. Increasing obesity and comorbidity in patients undergoing primary total hip arthroplasty in the U.S.: a 13‐year study of time trends. Singh and Lewallen. BMC Musculoskelet Disord. 2014;15:441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Namba RS, Inacio MC, Pratt NL, et al. Postoperative opioid use as an early indication of total hip arthroplasty failure. Acta Orthop. 2016;87(Suppl 1):37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement:national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gómez‐Serrano M, Camafeita E, García‐Santos E, López JA, Rubio MA, Sánchez‐Pernaute A, et al. Proteome‐wide alterations on adipose tissue from obese patients as age‐, diabetes‐ and gender‐specific hallmarks. Sci Rep. 2016;6:25756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999‐2010. Jama. 2012;307(5):491–7. [DOI] [PubMed] [Google Scholar]
- 18. Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–209. [DOI] [PubMed] [Google Scholar]
- 19. Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta‐analysis. Osteoarthr Cartil. 2010;18(1):24–33. [DOI] [PubMed] [Google Scholar]
- 20. Kuroda K, Kabata T, Maeda T, Kajino Y, Watanabe S, Iwai S, et al. The value of computed tomography based navigation in revision total hip arthroplasty. Int Orthop. 2014;38(4):711–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tayne S, Merrill CA, Smith EL, Maxkey WC. Predictive risk factors for 30‐day readmissions following primary total joint replacement and modification of patient management. J Arthroplasty. 2014;29(10):1938–42. [DOI] [PubMed] [Google Scholar]
- 22. Zheng L, Baoguo X, Lin H. Clinical analysis of the efficacy of total hip arthroplasty and hemiarthroplasty on femoral neck fracture. Chin J Med Front. 2014;20(10):62–4. [Google Scholar]
- 23. Piano LP, Golmia RP, Scheinberg M. Total hip and knee joint replacement: perioperative clinical aspects. Einstein. 2010;8(3):350–3. [DOI] [PubMed] [Google Scholar]
- 24. Jones CA, Cox V, Jhangri GS, Suarez‐Almazor ME. Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthr Cartil. 2012;20(6):511–8. [DOI] [PubMed] [Google Scholar]
- 25. Higuera CA, Elsharkawy K, Klika AK, Barsoum WK. 2010 Mid‐America Orthopaedic Association Physician in Training Award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. 2011;469(5):1391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Röder C, Bach B, Berry DJ, Eggli S, Langenhahn R, Busato A. Obesity, age, sex, diagnosis, and fixation mode differently affect early cup failure in total hip arthroplasty: a matched case‐control study of 4420 patients. J Bone Jt Surg Am. 2010;92(10):1954–63. [DOI] [PubMed] [Google Scholar]
- 27. Bozic KJ, Lau E, Kurtz S, Ong K, Rubash H, Vail TP, et al. Patient‐related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Jt Surg Am. 2012;94(9):794–800. [DOI] [PubMed] [Google Scholar]
- 28. Wenwei L, Jing Y, Suwei Y, Fengqing W, Jin M. Evaluation of hospital stays and hospitalization costs of hospitalized patients undergoing hip arthroplasty before and after quality control for single disease. Chin J Health Stat. 2016;33(2):287–92. [Google Scholar]
- 29. De Foor J, Van Wilder P, Leclercq P, Pirson M. The hospital cost of hip replacement for old inpatients in Belgium. Eur Geriatr Med. 2019;10(1):67–78. [DOI] [PubMed] [Google Scholar]
- 30. Kumar S, Breuing R, Chahal R. Globalization of health care delivery in the United States through medical tourism. J Health Commun. 2012;17(2):177–98. [DOI] [PubMed] [Google Scholar]
- 31. Frerichmann U, Raschke MJ, Stöckle U, Lohmann R. Proximal femoral intertrochanteric fractures in the elderly. Data from health insurance providers on more than 23 million insured persons‐part 2. Unfallchirurg. 2007;110(7):610–6. [DOI] [PubMed] [Google Scholar]


