Abstract
We performed a scoping review of articles published from 1 January 2000 to 4 January 2022 to characterize inequities in antibiotic prescribing and use across healthcare settings in the United States to inform antibiotic stewardship interventions and research. We included 34 observational studies, 21 cross-sectional survey studies, 4 intervention studies, and 2 systematic reviews. Most studies (55 of 61 [90%]) described the outpatient setting, 3 articles were from dentistry, 2 were from long-term care, and 1 was from acute care. Differences in antibiotic prescribing were found by patient's race and ethnicity, sex, age, socioeconomic factors, geography, clinician's age and specialty, and healthcare setting, with an emphasis on outpatient settings. Few studies assessed stewardship interventions. Clinicians, antibiotic stewardship experts, and health systems should be aware that prescribing behavior varies according to both clinician- and patient-level markers. Prescribing differences likely represent structural inequities; however, no studies reported underlying drivers of inequities in antibiotic prescribing.
Keywords: antibiotic prescribing, antibiotic stewardship, health disparities, health equity
Antibiotic prescribing differences by patient's race and ethnicity, sex, age, socioeconomic factors, geography, clinician's age and specialty, and healthcare setting likely represent healthcare inequities. Most studies in this scoping review did not have a prespecified health equity objective.
Antibiotics are among the most commonly prescribed medications in the United States (US) [1, 2]. Providing equitable healthcare is one of the National Academy of Medicine's (formerly the Institute of Medicine [IOM]) 6 domains of healthcare quality, and advancing health equity is a public health priority [3]. Consistent with the IOM, the Centers for Disease Control and Prevention (CDC) [4] is committed to integrating health equity efforts, including improvement of health equity science, across the agency [5]. Disparities in disease prevalence and diagnosis, access to care, and healthcare quality have been documented related to patients’ race and ethnicity, income, insurance status, and location of residence [6]. However, there are limited studies exploring characteristics of populations experiencing antibiotic-related inequities (markers) and the factors that cause or perpetuate the inequity (drivers) to ensure equitable access to high-quality medicines (pharmacoequity) (Table 1). Inequities in overprescribing may impact health outcomes, resulting in more antibiotic resistance or antibiotic-associated adverse events in some populations. The potential for undertreatment of infections is also a concern that could disproportionately affect certain populations and lead to poor outcomes.
Table 1.
Definitions of Health Equity Terms
| Term | Definition |
|---|---|
| Health equity | The state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving health equity requires focused and ongoing societal efforts to address historical and contemporary injustices; overcome economic, social, and other obstacles to health and healthcare; and eliminate preventable health disparities.a |
| Health disparity | Preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by populations that have been socially, economically, geographically, and environmentally disadvantaged.a |
| Health inequity | Particular types of health disparities that stem from unfair and unjust systems, policies, and practices and limit access to the opportunities and resources needed to live the healthiest life possible.a |
| Pharmacoequity | A health equity goal that ensures that “individuals, regardless of race, ethnicity, and socioeconomic status, have access to the highest-quality medications required to manage their health needs” (Essien et al, 2021b). |
| Markers of health inequity | Characteristics of subpopulations experiencing a health inequity. Examples are race, ethnicity, and nationality.a |
| Drivers of health inequity | Factors that create, perpetuate, or exacerbate a health inequity. Examples are racism and other systems of oppression and discrimination, residential segregation, inequity in income, and inequity in health insurance coverage.a |
Centers for Disease Control and Prevention. What is health equity? 2022. Available at: https://www.cdc.gov/healthequity/whatis/index.html. Accessed 8 December 2022.
Essien UR, Dusetzina SB, Gellad WF. A policy prescription for reducing health disparities—achieving pharmacoequity. JAMA 2021; 326:1793–4.
Achieving health equity requires focused and ongoing societal efforts to address historical and contemporary injustices; overcome economic, social, and other obstacles to health and healthcare; and eliminate preventable health disparities. We conducted a scoping review of published literature with 2 objectives: (1) characterize inequities or types of disparities that contribute to inequities in antibiotic prescribing and use across US healthcare settings, and (2) assess gaps in knowledge to identify research priorities to improve healthcare quality.
METHODS
Scope of Review
We conducted a scoping exercise to assess the landscape of published literature including heterogeneous studies by healthcare setting, populations, and study designs as well as to identify gaps in knowledge [7]. We followed the scoping review methodology and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping review reporting [7–9]. The primary review question was: What is the scope of the published literature on health equity markers and drivers in antibiotic prescribing, use, and stewardship in the US? Table 1 includes definitions of health equity terms used throughout this study.
Eligibility Criteria, Search Strategy, and Source Selection
Eligible studies were written in English, geographically focused on the US, and evaluated antibiotic prescribing, use, or stewardship (aiming to improve prescribing) and included information about at least 1 marker of inequity and its relationship to antibiotic prescribing. Potential markers were identified from social determinants of health literature and expert knowledge and included age, race, ethnicity, income, education, social vulnerability [4], geography, rurality, homelessness, immigrant status, gender identity, sexual orientation, substance use, or chronic health conditions/comorbid conditions. We included peer-reviewed systematic reviews, randomized controlled trials, and observational studies. We included studies using multivariate models, trend analyses, or spatial analyses including at least 1 marker of inequity and excluded studies using only descriptive statistics without controlling for other possible confounding factors. We did not exclude qualitative or mixed-methods studies. We excluded guidelines, professional society position statements, study protocol descriptions, stewardship implementation methods, and professional education literature focused on delivery of education to healthcare providers. We also excluded studies focused on animal use or environmental sampling and articles describing antimicrobial susceptibility.
A comprehensive search strategy was employed in collaboration with the CDC library that included Medline, Embase, and Scopus databases for publications from 1 January 2000 to 4 January 2022. Search criteria included titles, abstracts, and keywords of original research articles published based on our eligibility criteria. Health equity search terms were selected based on “MEDLINE/PubMed Health Disparities and Minority Health Search Strategy,” available on the National Library of Medicine's website (search terms are shown in Supplementary Table 1) [10]. We applied a “backward snowballing” technique with systematic reviews identified through the initial search by reviewing references and including relevant articles [11]. We also solicited input from known experts (n = 2) in this field for relevant articles.
Two researchers iteratively reviewed (C. K. and W. C. D.) relevant titles, abstracts, and eligible full texts from the search results. The first reviewer initially screened the titles and abstracts for relevance to antibiotic prescribing, use, or stewardship, and then screened for markers of inequity. The second reviewer conducted a confirmatory review of included full texts against eligibility criteria. Disagreements were resolved on study selection by consensus and discussion between the 2 reviewers.
Framework of Factors Contributing to Inequities in Antibiotic Prescribing in the US
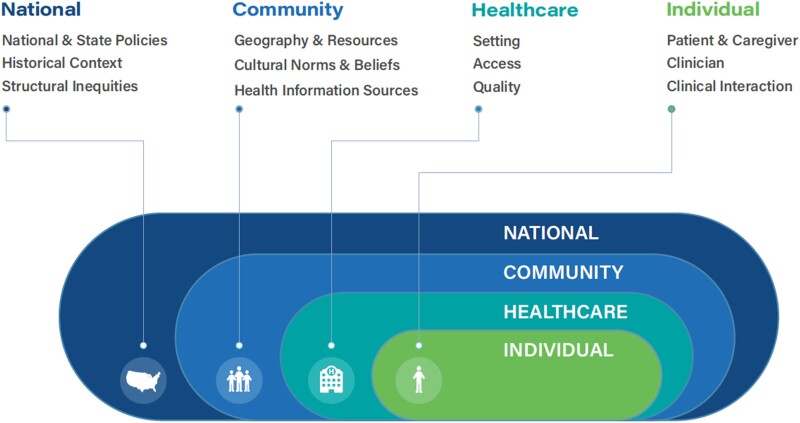
Based on the reviewed literature, we developed a nested capsule framework of factors contributing to health inequities in antibiotic prescribing in the US (Figure 1). Building on the socioecological model, the framework shows individual-, healthcare-, community-, and national-level factors potentially related to antibiotic prescribing inequities [12]. We used this framework to guide our search strategy and synthesis of the literature.
Figure 1.
Factors contributing to inequities in antibiotic prescribing in the United States.
Examples of individual factors that may be indicators of inequities include patient and caregiver markers such as age, race and ethnicity, sex, language, or health literacy. Clinician markers may include specialty and years of experience. Clinical interactions are influenced by patient expectations, clinician implicit bias, communication barriers, and cultural and power dynamics. Healthcare factors such as the type of clinical setting, healthcare access, workforce diversity, and healthcare quality including guideline-concordant care or availability of antibiotic stewardship expertise were another category. Community factors include factors like geography, availability of nonclinical resources, and health information sources. Although some factors, such as cultural norms and beliefs, can be considered individual factors, they can influence health behaviors of different groups of people and were included in community factors [13]. Finally, national factors include policies that combat antibiotic resistance, diversify the clinical and public health workforce, or affect access to health insurance. The historical and contemporaneous context of discriminatory treatment of people based on their race, ethnicity, sex, gender identity, age, or sexual orientation, which has negative health consequences, is also included under national factors [14–16].
Data Synthesis
Data on study design, methods, population, healthcare setting, key findings on equity markers and drivers, intersectionality of markers, and year of publication were charted using a standardized Microsoft Excel spreadsheet by the 2 reviewers. The table of extracted variables is shown in Supplementary Table 2. Results were synthesized by our framework categories both quantitatively (eg, enumeration of key concepts) and qualitatively (eg, summary of characteristics and themes).
RESULTS
Selection and Characteristics of Sources
After removing 388 duplicates, we screened 870 titles and abstracts; 431 studies were excluded that did not include antibiotic prescribing or use, leaving 439 studies for full text review. Of these, 61 were selected for inclusion (Supplementary Figure 1). Study designs included 34 observational studies, 21 cross-sectional survey studies, 4 intervention studies, and 2 systematic reviews. No qualitative or mixed-methods studies were identified. Data sources included Medicaid/Medicare, commercial claims, electronic health records, surveillance, and survey data, mainly from the National Ambulatory Medical Care Survey and/or the National Hospital Ambulatory Medical Care Survey.
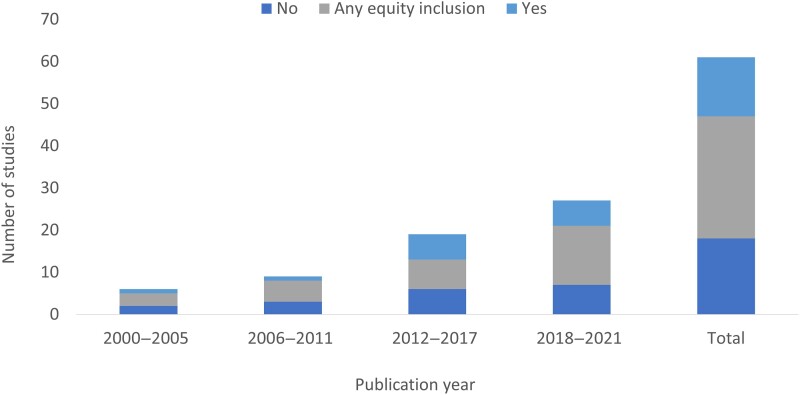
Most studies (55 of 61 [90%]) described the outpatient setting, 3 articles were from dentistry, 2 were from long-term care, and 1 was from acute care. The most common outcome assessed in the studies was antibiotic use or prescribing (83%) followed by inappropriate prescribing or guideline-concordant treatment (10%). Only 4 studies assessed antibiotic prescribing related to stewardship programs. The most common conditions reported were respiratory tract infections (n = 22; acute respiratory tract infections including upper respiratory tract infections and acute otitis media), skin and soft tissue infections (n = 5), and urinary tract infections (n = 3). Since 2000, the number of studies published on antibiotic prescribing has steadily increased along with studies with a specific equity objective (n = 14/61 [23%]) or studies assessing general patient or clinician characteristics with antibiotic prescribing or use (any equity inclusion; n = 29/61 [48%]) (Figure 2). Almost half (n = 20/43 [47%]) of the studies with an equity focus or any equity inclusion were published between 2018 and 2021, with 65% of those studies published in 2020 and 2021.
Figure 2.
Number of studies with a health equity and antibiotic prescribing focus by publication year. Any equity inclusion is defined as articles with the aim of assessing general patient and/or provider characteristics associated with any of the target outcomes (eg, antibiotic prescribing, inappropriate prescribing, stewardship) without an explicit equity-focused objective, but identifying equity-related results.
Individual Factors
Individual patient factors associated with antibiotic prescribing included race and ethnicity, age, sex, socioeconomic status, insurance status, comorbid conditions, and education (Table 2). While there was variability in prescribing across studies and in how race and ethnicity were defined, in general, people of racial or ethnic minority groups were less likely to be diagnosed with a condition warranting antibiotics (guideline concordant), less likely to receive antibiotics overall, and less likely to receive broad-spectrum antibiotics. Fleming-Dutra et al found that diagnosis of otitis media was 30% lower among Black children compared with children of other races or ethnicities, despite similar rates of otitis media visits between the 2 groups, and Black children were 41% less likely to receive a broad-spectrum antibiotic when diagnosed [17]. Similarly, Gerber et al found that Black children were 21%–40% less likely to be diagnosed with an acute respiratory tract infection, 25% less likely to receive an antibiotic, and 12% less likely to receive a broad-spectrum antibiotic from the same clinician compared to other children [18]. Kornblith et al also found that Black children were 28% less likely to receive antibiotics when they were indicated for acute respiratory tract infections [19]. Among hospitalized adults, Wurcel et al found that Black patients were less likely to receive first-line treatment for skin and soft tissue infections compared to White patients [20]. There were fewer studies overall that assessed inappropriate prescribing and guideline-concordant treatment by race and ethnicity (Supplementary Table 3). Four studies showed that inappropriate prescribing was more common among Black patients [21–24], while 1 study showed more guideline-concordant treatment prescribed [25]. Wattles et al [22] found that despite higher rates of antibiotic prescribing to White children, inappropriate prescribing was more common among Black children, but Gerber et al [18] found higher prescribing rates of broad-spectrum antibiotics to White children, possibly reflective of inappropriate prescribing.
Table 2.
Studies Showing Increased, Decreased, or No Associations With Markers Contributing to Health Inequities and Antibiotic Prescribing
| Factors and Equity Markers | Articles With Increased Association With Antibiotic Prescribing (No.) | Articles With Decreased Association With Antibiotic Prescribing (No.) | Articles With No Association (No.) | Total, No. |
|---|---|---|---|---|
| Community | ||||
| Geography | ||||
| Region | Southern (11) Northeast (2) Midwest (1) |
Western (1) Northeast (1) |
Region (2) | 18 |
| Rurality | Rural (8) Suburb (2) |
… | Rurality (3) | 13 |
| County characteristics | % poverty (5) % females (3) % White (2) % with obesity (2) % aged ≤2 y (1) % aged <65 y (1) % aged >65 y (1) |
… | … | 15 |
| Healthcare | ||||
| Setting | ||||
| Clinical setting | ED (3) Public clinic (1) |
ED (3) Hospital outpatient (1) |
Setting (1) | 9 |
| Access | ||||
| Clinician density | Prescribers per capita (2) | … | … | 2 |
| Quality | ||||
| Wait time | >2 h (1) | … | … | 1 |
| Individual | ||||
| Patient | ||||
| Race and ethnicity | White (5) Black (1) Hispanic (1) |
Black (8) Hispanic (3) Racial and ethnic minorities (2) Asian (2) |
Race (6) | 28 |
| Age | <2 y (3) <6 y (3) ≥5 y (1) 2–5 y (1) <18 y (1) ≥65 y (1) |
1–3 y, >6 y (1) 5–14 y (1) <18 y (1) |
Age (9) | 22 |
| Sex | Female (5) Male (2) |
Female (1) | Sex (9) | 17 |
| Income | Low income (1) High income (1) |
… | … | 1 |
| Insurance status | Private (5) Self-pay/uninsured (2) |
Self-pay/uninsured (4) Medicaid (3) Public and other (3) Private (1) |
Insurance (6) | 25 |
| Comorbid conditions | Presence (7) | … | Heart failure (1) Comorbid conditions (1) |
9 |
| Education | <High school (2) High school degree (1) |
… | … | 3 |
| Clinician | ||||
| Age | Advanced age (1) Born in 1960s (1) Older age (51–60 y) (1) |
Born in 1980s (1) | … | 4 |
| Sex | Male (1) | … | … | 1 |
| Years of experience | >20 y (1) | <10 y (1) | Experience (1) | 3 |
| Specialty | NP/PA (4) General/family medicine (2) Non–internal medicine (1) Dentists (1) Emergency medicine (1) Primary care (1) |
Pediatrician (3) ENT/surgery (1) Internal medicine (1) |
Specialty (3) | 18 |
Abbreviations: ED, emergency department; ENT, ear, nose, and throat; NP, nurse practitioner, PA, physician assistant.
Articles varied in specific populations studied by age: 25 (41%) articles focused on children and adolescents, 19 (31%) articles focused on adults (including 5 only on older adults and 2 only on adult women), and 17 (28%) articles on patients of all ages. Studies assessing age were also highly variable in their definitions of age groups, making comparisons across studies challenging. Younger children (aged <5 years) or older adults (aged ≥65 years) were generally more likely to receive antibiotics than their older-aged children or younger-aged adult comparison groups, respectively. Wattles et al found that children aged ≤2 years receiving Medicaid in Kentucky were more likely to receive an inappropriate antibiotic prescription than those aged 10–19 years (adjusted odds ratio, 1.39 [95% confidence interval, 1.37–1.41]) [22]. A study of women with uncomplicated urinary tract infection in the outpatient setting by Langner et al found that women aged ≥45 years were 3 times more likely to be given non-guideline-concordant care (overuse of fluoroquinolones and the underuse of first-line antibiotic agents) compared to younger women aged 18–44 years [25]. In a dental study, Suda et al found that while adults aged ≥65 years were more likely to be prescribed antibiotic prophylaxis, they were more likely to receive appropriate therapy compared with those aged 18–34 years [26].
Some studies showed that women were more likely than men to receive antibiotics, broad-spectrum antibiotics [27–31], and inappropriate treatment [26]. It is unclear whether these differences were clinically warranted, and many studies showed no differences by sex as recorded in health records [19, 32–38]. Gender identity may also be a marker of disparity but was not evaluated in included studies, which focused on sex at birth.
Three socioeconomic factors were identified and included in the review: income, education, and insurance type/status. The most common socioeconomic factors assessed were insurance type and status. People with private insurance were more likely to receive antibiotic prescriptions compared to people with public insurance (Medicare or Medicaid) [24, 38–40] or no insurance [24, 39].
Comorbid conditions were often measured as presence or absence of any chronic conditions or specific conditions identified such as asthma, renal disease, or substance use disorder. Congestive heart failure was associated with higher rates of antibiotic prescribing [41], and patients with at least 1 comorbid condition were more likely to receive an antibiotic prescription [22, 33, 40, 42–44]. Tobacco use was another individual factor associated with increased likelihood of antibiotic prescribing [38, 44].
Associations with antibiotic prescribing and clinician factors included clinician age, sex, years of experience, and specialty. Older physicians [24, 25, 45, 46], male clinicians [46], advanced practice clinicians [24, 31, 32], non–internal medicine clinicians [25, 38, 46, 47], and non–pediatric clinicians [34, 40, 48] had higher rates of antibiotic prescribing.
Healthcare Factors
A limited number of healthcare factors were measured in the studies and included clinical setting, clinician density as a proxy for access, and wait time as a measure for quality. Specific clinical settings varied across studies, but the most assessed setting associated with antibiotic prescribing was the emergency department (ED). Antibiotic prescribing in an ED was associated with longer duration of antibiotics [29], greatest increase in prescribing rates over time [49], and higher prescribing rates compared with a physician's office [49]. Studies found that higher clinician density, at the county level and per capita, was associated with higher antibiotic prescribing rates [50–52]. Waiting time longer than 2 hours in the ED was significantly associated with increased odds of receiving an antibiotic prescription [53].
Community Factors
Community-level factors explored in the studies were limited to geography (region and rurality) and county characteristics. Many studies showed a strong association between residence in the US Southern region and antibiotic prescribing across clinical settings, clinician specialty, and diagnoses [30, 36, 42, 49, 52, 54–59]. Hersh et al found that children living in the South were 82% more likely to be prescribed a broad-spectrum antibiotic than those living in the West census region [39]. Langner et al found that physicians in all other regions had a 29%–35% significantly higher likelihood of prescribing guideline-concordant treatment than physicians in the South Atlantic [25]. People living in rural areas were also more likely to receive an antibiotic prescription [21, 46, 54, 56, 60] and were more likely to receive inappropriate prescriptions [21, 22, 28, 31] than their urban counterparts. Five studies conducted county-level analyses of antibiotic prescribing and found that counties with high proportions of people with incomes below the federal poverty level [30, 52, 60, 61], women, [30, 50, 52] and people who are White [30, 50, 51] were associated with higher prescribing rates.
Methodologic Limitations
None of the studies assessed drivers of inequities in antibiotic prescribing. Also, interaction between health equity markers was assessed by only 1 study. Dantuluri et al included subgroup analyses of their primary analysis between rurality of residence and antibiotic prescribing for acute respiratory infections (ARI) and inappropriate prescribing for ARI among children aged ≤5 years enrolled in Tennessee's Medicaid program [21]. Interaction terms between race and rurality and median household income and rurality found that the strength of association between rurality and prescribing varied by race (significantly higher inappropriate prescribing among Black children) and median household income (significantly higher inappropriate prescribing among children from households with lower median income). Another gap in the studies’ assessment of interaction was the exclusion of at least 1 health equity marker by 4 studies in their multivariate models because they were not statistically significant in univariate analyses. Race and ethnicity [45, 49, 62], sex, [45, 62] region [42, 62], comorbid conditions [62], and insurance status [42] were excluded from some models, and interactions were not assessed.
DISCUSSION
In our review of the published literature examining the association between health equity markers and drivers with antibiotic prescribing in the US, differences in prescribing were found by patient's race and ethnicity, sex, age, socioeconomic factors (ie, income, insurance type/status, and education), geography, clinician's age and specialty, and healthcare setting, with an emphasis on outpatient settings. These differences likely represent healthcare inequities; however, no drivers of inequities in antibiotic prescribing were reported, and most studies did not have a prespecified health equity objective. Studies that specified a health equity objective were more recently published, which follows the growth of social justice movements [63], commitment to address racism as a public health problem by leading public health organizations [5, 64], and evidence of the coronavirus disease 2019 (COVID-19) pandemic exacerbating longstanding systemic health inequities [65, 66]. Within this context of health equity research, we found that prescribing rates and appropriateness varied by certain factors, and several gaps in knowledge were identified requiring future evaluation.
While there was variability across study findings, we found that most associations with inequity markers were at the individual, healthcare, or community levels. Some differences in prescribing may be clinically indicated such as by sex or age but, based on these studies, appropriateness cannot be determined. However, patterns of prescribing disparities by race and ethnicity, place of residence (Southern region and rural) [67], socioeconomic status [68], and differential clinician treatment [69] reflect similar disparities to those documented in healthcare access [70], diabetes care and medication prescribing [71, 72], and pain management [73]. For instance, Black people were less likely than White people to receive antibiotics. Similarly, racial disparities have been found in pain management where Black people were less likely to be prescribed any pain medication and less likely to be prescribed opioids for severe pain compared to White people [74, 75]. During the COVID-19 pandemic, despite disproportionately higher rates of infections, hospitalizations, and death among people of race and ethnic minority groups, there were continued disparities in access and receipt of COVID-19 therapeutics including monoclonal antibodies and oral antivirals [76]. In cancer care research, disparities in outcomes in rural areas have been well characterized and are likely due to the impact of rurality on access to oncology infrastructure (eg, cancer prevention, diagnosis, and guideline-concordant treatment services), health insurance, and transportation, as well as higher rates of risk factors such as smoking and obesity [77]. Similarly, geographic disparities in antibiotic prescribing may be because people living in rural areas are more likely to receive care in an urgent care or ED setting [78] or by clinician specialties with higher rates of inappropriate prescribing [79–81].
Not all levels of markers and drivers of inequities were evaluated, particularly at the national and community levels. At the individual level, potential markers not studied include gender identity, sexual orientation, language, refugee and immigrant status, and health literacy, with limited studies on inequities by Hispanic origin. At the healthcare level, while antibiotic stewardship programs are required for inpatient settings, most studies evaluating health equity markers were limited to outpatient settings. We found higher prescribing associated with visits to EDs compared to physicians’ offices, an opportunity for stewardship interventions by health systems. An article by Goodman et al on antibiotic prescribing in the inpatient setting, published after our search period, found higher prescribing rates in the Southern region and to male patients and lower prescribing rates to people of racial and ethnic minority groups [82]. Wojcik et al conducted a systematic review of qualitative studies on inpatient prescribing behaviors describing the complex and dynamic context of physicians’ antibiotic prescribing [83]. Only 3 of 15 included studies were from the US. They suggested that changes to practice were needed on managing failures in communication and information provision, promoting distribution of responsibility for antibiotic decisions, and reducing fear of consequences from not prescribing. Future quantitative and qualitative studies evaluating markers and drivers of inequities in antibiotic prescribing are needed to address these knowledge gaps, especially in acute care settings. Additionally, evaluation of the intersectionality and interaction of equity markers is needed for focused interventions. For instance, studies have shown that rural status confers additional disadvantage in healthcare access and among rural populations, people of racial and ethnic minority groups have less access to healthcare and poorer health outcomes compared to rural White populations [70, 84]. Schulman et al found that a patient's race and sex independently influenced physicians’ management of chest pain, and race–sex interactions showed that Black women were significantly less likely than White men to be referred for cardiac catheterization [85].
This review has several limitations. First, studies included in this scoping review vary by study design, variable definition, outcomes measured, and populations and conditions studied, limiting comparability. However, we aimed to broadly report the scope of literature on this topic and emphasize the importance of including equity-related variables in future research. Second, our search did not yield any relevant qualitative studies, which may be a valuable methodology to assess health equity drivers in different settings. Third, many potential markers of inequities were not collected or analyzed, and markers were mainly assessed in outpatient settings, limiting the number of markers with data and interpretation of findings to other settings. Fourth, we did not assess the risk of bias of studies included in the review because it is not applicable to the scoping review methodology. As more health equity–focused research in antibiotic prescribing is published, a systematic review with a critical appraisal of studies should be considered. Fifth, while we employed a systematic literature search, it is possible that relevant studies [86, 87] were missed, and future updates should be considered to capture the growing literature on health equity and antibiotic prescribing. Additionally, our study period may have been too short to capture studies related to the COVID-19 pandemic. Future studies may also specifically explore the COVID-19 pandemic's impact on disparities in antibiotic prescribing.
Clinicians, antibiotic stewardship experts, and health systems should be aware that prescribing behavior varies according to both clinician- and patient-level markers. In addition to studying the best approaches to providing feedback, assessing the drivers of these differences is an important next step (Supplementary Table 4). Antibiotic prescribing quality improvement activities and interventions should consider clinician prescribing feedback that incorporates a health equity lens and more broadly consider equitable care of infectious diseases. Family practice and advanced practice clinicians and their professional organizations need to be engaged in antibiotic stewardship to address differences in quality of prescribing by clinician type.
Researchers should include specific health equity–related objectives to improve characterization of equity markers and expand understanding of potential systemic and structural drivers of inequities in all clinical settings. Data on relevant markers of health inequities should be collected and included a priori in statistical models, and interactions between inequity markers should be assessed [88]. Boyd et al outlined a standard for publishing about racial health inequities, which researchers should use as a guide when embarking on this work [89]. Moving beyond documenting inequities, antibiotic stewardship interventions should be designed to address drivers of health inequities and examine the potential effects of interventions across inequity markers to optimize antibiotic use and incorporate the patient’s perspective. Additional resources and partnerships (eg, professional societies, payers, and public health) to improve access to stewardship expertise, especially in the South and in rural areas, are needed. Incorporating health equity principles into guidance and regulatory requirements is an important step in improving equitable antibiotic prescribing, access, and use. A new Joint Commission accreditation standard aiming to reduce healthcare disparities was made effective January 2023 [90]. Combining stewardship activities for quality improvement with a focus on health equity will help health systems meet quality and equity standards while improving population health outcomes.
Supplementary Material
Contributor Information
Christine Kim, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Sarah Kabbani, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
William C Dube, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Melinda Neuhauser, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Sharon Tsay, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Adam Hersh, University of Utah, Salt Lake City, Utah, USA.
Jasmine R Marcelin, University of Nebraska Medical Center, Omaha, Nebraska, USA.
Lauri A Hicks, Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Disclaimer. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1. Chai G, Governale L, McMahon AW, Trinidad JP, Staffa J, Murphy D. Trends of outpatient prescription drug utilization in US children, 2002–2010. Pediatrics 2012; 130:23–31. [DOI] [PubMed] [Google Scholar]
- 2. Fuentes AV, Pineda MD, Venkata KCN. Comprehension of top 200 prescribed drugs in the US as a resource for pharmacy teaching, training and practice. Pharmacy (Basel) 2018; 6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Institute of Medicine Committee on Quality of Health Care in America . Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 4. Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry . CDC Social Vulnerability Index documentation 2020. 2022. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/SVI_documentation_2020.html. Accessed 3 November 2022.
- 5. Centers for Disease Control and Prevention . CDC declares racism and public health threat. Available at: https://www.cdc.gov/minorityhealth/racism-disparities/expert-perspectives/threat/index.html. Accessed 23 August 2023.
- 6. Agency for Healthcare Research and Quality . 2021 national healthcare quality and disparities report. 2023. Available at: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr21/index.html. Accessed 21 September 2022.
- 7. Peters MDJ, Marnie C, Colquhoun H, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev 2021; 10:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169:467–73. [DOI] [PubMed] [Google Scholar]
- 9. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Library of Medicine . MEDLINE/PubMed health disparities and minority health search strategy. Bethesda, MD: National Institutes of Health; 2021. [Google Scholar]
- 11. Wohlin C, Kalinowski M, Romero Felizardo K, Mendes E. Successful combination of database search and snowballing for identification of primary studies in systematic literature studies. Inf Softw Technol 2022; 147:106908. [Google Scholar]
- 12. Bronfenbrenner U. Ecological systems theory. In: Vasta R, ed. Six theories of child development: revised formulations and current issues. Jessica Kingsley Publishers; 1989:187–249. [Google Scholar]
- 13. McFerran B. Social norms, beliefs, and health. In: Roberto CA, Kawachi I, eds. Behavioral economics and public health. Oxford, UK: Oxford University Press; 2015:1–26. [Google Scholar]
- 14. Centers for Disease Control and Prevention . What is health equity? Available at: https://www.cdc.gov/healthequity/whatis/index.html. Accessed 21 September 2022.
- 15. American Psychological Association . Discrimination: what it is, and how to cope. 2019. Available at: https://www.apa.org/topics/racism-bias-discrimination/types-stress. Accessed 21 September 2022.
- 16. Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull 2009; 135:531–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fleming-Dutra KE, Shapiro DJ, Hicks LA, Gerber JS, Hersh AL. Race, otitis media, and antibiotic selection. Pediatrics 2014; 134:1059–66. [DOI] [PubMed] [Google Scholar]
- 18. Gerber JS, Prasad PA, Localio AR, et al. Racial differences in antibiotic prescribing by primary care pediatricians. Pediatrics 2013; 131:677–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kornblith AE, Fahimi J, Kanzaria HK, Wang RC. Predictors for under-prescribing antibiotics in children with respiratory infections requiring antibiotics. Am J Emerg Med 2018; 36:218–25. [DOI] [PubMed] [Google Scholar]
- 20. Wurcel AG, Essien UR, Ortiz C, et al. Variation by race in antibiotics prescribed for hospitalized patients with skin and soft tissue infections. JAMA Netw Open 2021; 4:e2140798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dantuluri KL, Bruce J, Edwards KM, et al. Rurality of residence and inappropriate antibiotic use for acute respiratory infections among young Tennessee children. Open Forum Infect 2021; 8:ofaa587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wattles BA, Jawad KS, Feygin Y, et al. Inappropriate outpatient antibiotic use in children insured by Kentucky Medicaid. Infect Control Hosp Epidemiol 2021;43:582–7. [DOI] [PubMed] [Google Scholar]
- 23. Tabidze IL, Nicholson TF, Mikati T, Benbow N, Mehta SD. Adherence to Centers for Disease Control and Prevention gonococcal treatment guidelines among Chicago health care providers, 2011–2012. Sex Transm Dis 2015; 42:422–8. [DOI] [PubMed] [Google Scholar]
- 24. Schmidt ML, Spencer MD, Davidson LE. Patient, provider, and practice characteristics associated with inappropriate antimicrobial prescribing in ambulatory practices. Infect Control Hosp Epidemiol 2018; 39:307–15. [DOI] [PubMed] [Google Scholar]
- 25. Langner JL, Chiang KF, Stafford RS. Current prescribing practices and guideline concordance for the treatment of uncomplicated urinary tract infections in women. Am J Obstet Gynecol 2021; 225:272.e1–11. [DOI] [PubMed] [Google Scholar]
- 26. Suda KJ, Calip GS, Zhou J, et al. Assessment of the appropriateness of antibiotic prescriptions for infection prophylaxis before dental procedures, 2011 to 2015. JAMA Netw 2019; 2:e193909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Okunseri C, Zheng C, Steinmetz CN, Okunseri E, Szabo A. Trends and racial/ethnic disparities in antibiotic prescribing practices of dentists in the United States. J Public Health Dent 2018; 78:109–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wattles BA, Vidwan NK, Feygin Y, Jawad KS, Creel LM, Smith MJ. Antibiotic prescribing to Kentucky Medicaid children, 2012–2017: prescribing is higher in rural areas. J Rural Health 2021; 12:12. [DOI] [PubMed] [Google Scholar]
- 29. Frost HM, Becker LF, Knepper BC, Shihadeh KC, Jenkins TC. Antibiotic prescribing patterns for acute otitis media for children 2 years and older. J Pediatr 2020; 220:109–15.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Volpi C, Shehadeh F, Mylonakis E. Correlation of antimicrobial prescription rate and county income in Medicare part D. Medicine (Baltimore) 2019; 98:e15914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Winders HR, Royer J, Younas M, et al. Temporal trends in ambulatory antibiotic prescription rates in South Carolina: impact of age, gender, and resident location. Infect Control Hosp Epidemiol 2020; 41:879–82. [DOI] [PubMed] [Google Scholar]
- 32. Wattles B, Vidwan N, Ghosal S, et al. Cefdinir use in the Kentucky Medicaid population: a priority for outpatient antimicrobial stewardship. J Pediatric Infect Dis Soc 2021; 10:157–60. [DOI] [PubMed] [Google Scholar]
- 33. Grammatico-Guillon L, Shea K, Jafarzadeh SR, et al. Antibiotic prescribing in outpatient children: a cohort from a clinical data warehouse. Clin Pediatr (Phila) 2019; 58:681–90. [DOI] [PubMed] [Google Scholar]
- 34. Paul IM, Maselli JH, Hersh AL, Boushey HA, Nielson DW, Cabana MD. Antibiotic prescribing during pediatric ambulatory care visits for asthma. Pediatrics 2011; 127:1014–21. [DOI] [PubMed] [Google Scholar]
- 35. May L, Nguyen MH, Trajano R, et al. A multifaceted intervention improves antibiotic stewardship for skin and soft tissues infections. Am J Emerg Med 2021; 46:374–81. [DOI] [PubMed] [Google Scholar]
- 36. Vanderweil SG, Pelletier AJ, Hamedani AG, Gonzales R, Metlay JP, Camargo CA Jr. Declining antibiotic prescriptions for upper respiratory infections, 1993–2004. Acad Emerg Med 2007; 14:366–9. [DOI] [PubMed] [Google Scholar]
- 37. Stone S, Gonzales R, Maselli J, Lowenstein SR. Antibiotic prescribing for patients with colds, upper respiratory tract infections, and bronchitis: a national study of hospital-based emergency departments. Ann Emerg Med 2000; 36:320–7. [DOI] [PubMed] [Google Scholar]
- 38. Steinberg MB, Akincigil A, Kim EJ, Shallis R, Delnevo CD. Tobacco smoking as a risk factor for increased antibiotic prescription. Am J Prev Med 2016; 50:692–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics 2011; 128:1053–61. [DOI] [PubMed] [Google Scholar]
- 40. Howard LM, Thurm C, Dantuluri K, et al. Parenteral antibiotic use among ambulatory children in United States children's hospital emergency departments. Open Forum Infect 2020; 7:ofaa357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lim DW, Htun HL, Ong LS, Guo H, Chow A. Systematic review of determinants influencing antibiotic prescribing for uncomplicated acute respiratory tract infections in adult patients at the emergency department. Infect Control Hosp Epidemiol 2020;43:366–75. [DOI] [PubMed] [Google Scholar]
- 42. Ference EH, Min JY, Chandra RK, et al. Antibiotic prescribing by physicians versus nurse practitioners for pediatric upper respiratory infections. Ann Otol Rhinol Laryngol 2016; 125:982–91. [DOI] [PubMed] [Google Scholar]
- 43. Fischer MA, Mahesri M, Lii J, Linder JA. Non-visit-based and non-infection-related antibiotic use in the US: a cohort study of privately insured patients during 2016–2018. Open Forum Infect 2021; 8:ofab412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Olsen MA, Nickel KB, Fraser VJ, Wallace AE, Warren DK. Prevalence and predictors of postdischarge antibiotic use following mastectomy. Infect Control Hosp Epidemiol 2017; 38:1048–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Aspinall SL, Good CB, Metlay JP, Mor MK, Fine MJ. Antibiotic prescribing for presumed nonbacterial acute respiratory tract infections. Am J Emerg Med 2009; 27:544–51. [DOI] [PubMed] [Google Scholar]
- 46. Staub MB, Ouedraogo Y, Evans CD, et al. Analysis of a high-prescribing state's 2016 outpatient antibiotic prescriptions: implications for outpatient antimicrobial stewardship interventions. Infect Control Hosp Epidemiol 2020; 41:135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hendricksen M, Habtemariam D, D’Agata EMC, Mitchell SL. Factors associated with antimicrobial use in nursing home residents with advanced dementia. J Am Med Dir Assoc 2021; 22:178–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Frost HM, McLean HQ, Chow BDW. Variability in antibiotic prescribing for upper respiratory illnesses by provider specialty. J Pediatr 2018; 203:76–85.e8. [DOI] [PubMed] [Google Scholar]
- 49. Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med 2008; 168:1585–91. [DOI] [PubMed] [Google Scholar]
- 50. Hubbard CC, Evans CT, Calip GS, et al. Characteristics associated with opioid and antibiotic prescribing by dentists. Am J Prev Med 2021; 60:648–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Klein EY, Makowsky M, Orlando M, Hatna E, Braykov NP, Laxminarayan R. Influence of provider and urgent care density across different socioeconomic strata on outpatient antibiotic prescribing in the USA. J Antimicrob Chemother 2015; 70:1580–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis 2015; 60:1308–16. [DOI] [PubMed] [Google Scholar]
- 53. Xu KT, Roberts D, Sulapas I, Martinez O, Berk J, Baldwin J. Over-prescribing of antibiotics and imaging in the management of uncomplicated URIs in emergency departments. BMC Emerg Med 2013; 13:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Brown DW, Taylor R, Rogers A, Weiser R, Kelley M. Antibiotic prescriptions associated with outpatient visits for acute upper respiratory tract infections among adult Medicaid recipients in North Carolina. N C Med J 2003; 64:148–56. [PubMed] [Google Scholar]
- 55. Coco AS, Horst MA, Gambler AS. Trends in broad-spectrum antibiotic prescribing for children with acute otitis media in the United States, 1998–2004. BMC Pediatr 2009; 9:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Evans CT, Fitzpatrick MA, Poggensee L, et al. Outpatient prescribing of antibiotics and opioids by Veterans Health Administration providers, 2015–2017. Am J Prev Med 2021; 61:e235–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA 2003; 289:719–25. [DOI] [PubMed] [Google Scholar]
- 58. Zhang Y, Steinman MA, Kaplan CM. Geographic variation in outpatient antibiotic prescribing among older adults. Arch Intern Med 2012; 172:1465–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Alsan M, Morden NE, Gottlieb JD, Zhou W, Skinner J. Antibiotic use in cold and flu season and prescribing quality: a retrospective cohort study. Med Care 2015; 53:1066–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kilgore JT, Smith MJ. Outpatient pediatric antibiotic use: a systematic review. Curr Infect Dis Rep 2019; 21:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Watson JR, Wang L, Klima J, et al. Healthcare claims data: an underutilized tool for pediatric outpatient antimicrobial stewardship. Clin Infect Dis 2017; 64:1479–85. [DOI] [PubMed] [Google Scholar]
- 62. Fee C, Metlay JP, Camargo CA Jr, Maselli JH, Gonzales R. ED antibiotic use for acute respiratory illnesses since pneumonia performance measure inception. Am J Emerg Med 2010; 28:23–31. [DOI] [PubMed] [Google Scholar]
- 63. García JJ-L, Zulfacar SM. Black lives matter: a commentary on racism and public health. Am J Public Health 2015; 105:e27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. American Medical Association . AMA Board of Trustees pledges action against racism, police brutality. 2020. Available at: https://www.ama-assn.org/press-center/press-releases/ama-board-trustees-pledges-action-against-racism-police-brutality. Accessed 23 August 2023.
- 65. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020; 323:2466–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Romano SD, Blackstock AJ, Taylor EV, et al. Trends in racial and ethnic disparities in COVID-19 hospitalizations, by region—United States, March–December 2020. MMWR Morb Mortal Wkly Rep 2021; 70:560–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Martino SC, Mathews M, Agniel D, et al. National racial/ethnic and geographic disparities in experiences with health care among adult Medicaid beneficiaries. Health Serv Res 2019; 54(Suppl 1):287–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wasserman J, Palmer RC, Gomez MM, Berzon R, Ibrahim SA, Ayanian JZ. Advancing health services research to eliminate health care disparities. Am J Public Health 2019; 109(S1):S64–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Simon MS, Raychaudhuri S, Hamel LM, et al. A review of research on disparities in the care of Black and White patients with cancer in Detroit. Front Oncol 2021; 11:690390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, Bouye K. Racial/ethnic health disparities among rural adults—United States, 2012–2015. MMWR Surveill Summ 2017; 66:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci 2016; 351:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hanna J, Nargesi AA, Essien UR, et al. County-level variation in cardioprotective antihyperglycemic prescribing among Medicare beneficiaries. Am J Prev Cardiol 2022; 11:100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med 2019; 37:1770–7. [DOI] [PubMed] [Google Scholar]
- 74. Jordan A, Mathis M, Haeny A, Funaro M, Paltin D, Ransome Y. An evaluation of opioid use in Black communities: a rapid review of the literature. Harv Rev Psychiatry 2021; 29:108–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr 2015; 169:996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Wiltz JL, Feehan AK, Molinari NM, et al. Racial and ethnic disparities in receipt of medications for treatment of COVID-19—United States, March 2020–August 2021. MMWR Morb Mortal Wkly Rep 2022; 71:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Bhatia S, Landier W, Paskett ED, et al. Rural–urban disparities in cancer outcomes: opportunities for future research. J Natl Cancer Inst 2022; 114:940–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Greenwood-Ericksen MB, Kocher K. Trends in emergency department use by rural and urban populations in the United States. JAMA Netw 2019; 2:e191919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Barreto T, Jetty A, Eden AR, Petterson S, Bazemore A, Peterson LE. Distribution of physician specialties by rurality. J Rural Health 2021; 37:714–22. [DOI] [PubMed] [Google Scholar]
- 80. MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural Remote Health 2010; 10:1531. [PMC free article] [PubMed] [Google Scholar]
- 81. Randolph GD, Pathman DE. Trends in the rural-urban distribution of general pediatricians. Pediatrics 2001; 107:e18. [DOI] [PubMed] [Google Scholar]
- 82. Goodman KE, Baghdadi JD, Magder LS, et al. Patterns, predictors, and inter-center variability in empiric gram-negative antibiotic use across 928 U.S. hospitals. Clin Infect Dis 2022; 76:e1224–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Wojcik G, Ring N, McCulloch C, Willis DS, Williams B, Kydonaki K. Understanding the complexities of antibiotic prescribing behaviour in acute hospitals: a systematic review and meta-ethnography. Arch Public Health 2021; 79:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health 2016; 106:1463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med 1999; 340:618–26. [DOI] [PubMed] [Google Scholar]
- 86. Honcoop AC, Poitevien P, Kerns E, Alverson B, McCulloh RJ. Racial and ethnic disparities in bronchiolitis management in freestanding children’s hospitals. Acad Emerg Med 2021; 28:1043–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Mangione-Smith R, Elliott MN, Stivers T, McDonald L, Heritage J, McGlynn EA. Racial/ethnic variation in parent expectations for antibiotics: implications for public health campaigns. Pediatrics 2004; 113:e385–94. [DOI] [PubMed] [Google Scholar]
- 88. Clemans-Cope L, Garrett B, McMorrow S. How should we measure and interpret racial and ethnic disparities in health care? 2023. Available at: https://www.rwjf.org/en/insights/our-research/2023/01/how-should-we-measure-and-interpret-racial-and-ethnic-disparitie.html. Accessed 3 July 2023.
- 89. Boyd RW, Lindo EG, Weeks LD, McLemore MR. On racism: a new standard for publishing on racial health inequities. Health Affairs Blog. 2020. Available at: https://www.healthaffairs.org/do/10.1377/forefront.20200630.939347/full/. Accessed 23 August 2023.
- 90. The Joint Commission . New requirements to reduce health care disparities. Available at: https://www.jointcommission.org/standards/r3-report/r3-report-issue-36-new-requirements-to-reduce-health-care-disparities/#.Y9HarkHMI2w. Accessed 25 January 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.