Abstract
Study Objectives:
Near-infrared light exhibits several therapeutic properties, but little is known about the benefits to sleep and daytime function. The purpose of this study was to investigate the effects of red and near-infrared exposure before bed on sleep and next-day function.
Methods:
Thirty adults (30–60 y) with a self-reported sleep complaint but without a sleep disorder participated in a randomized, sham-controlled study for a duration of 5 weeks. After a 2-week baseline period, participants wore either a cervical red light/near-infrared–emitting collar (combined: 660 nm, 740 nm, 810 nm, and 870 nm) or sham device every other night before bed for 3 weeks. Sleep was measured using actigraphy and sleep diaries. Mood and performance were assessed using weekly self-reported surveys and debrief interviews.
Results:
Objective sleep parameters, as measured by actigraphy, did not differ between the active or sham groups, but improved self-reported sleep, as well as perceived improvements in relaxation and mood, were observed among active but not sham users. Both active and sham users improved in Insomnia Severity Index score by the end of the trial.
Conclusions:
Red and near-infrared exposure to the head and neck before bed may offer potential therapeutic benefits to sleep and daytime function, but further work needs to be done to determine optimal dose parameters, wavelengths, and milliwatt power level.
Clinical Trial Registration:
Registry: ClinicalTrials.gov; Name: Phase II Study—Trial of a Phototherapy Light Device to Improve Sleep Health (PHOTONS); URL: https://clinicaltrials.gov/ct2/show/NCT05116358; Identifier: NCT05116358.
Citation:
Kennedy KER, Wills CCA, Holt C, Grandner MA. A randomized, sham-controlled trial of a novel near-infrared phototherapy device on sleep and daytime function. J Clin Sleep Med. 2023;19(9):1669–1675.
Keywords: sleep, wearables, phototherapy, near infrared, insomnia, actigraphy
BRIEF SUMMARY
Current Knowledge/Study Rationale: There are few interventions specifically designed to treat subclinical sleep complaints. This study aims to assess the efficacy of a cervical red and near-infrared–emitting device on sleep and daytime function.
Study Impact: In this randomized, sham-controlled study, we show that red and near-infrared phototherapy targeted at the neck before bed improved perceived relaxation, sleep quality, and next-day function.
INTRODUCTION
The population prevalence of suboptimal sleep quality is relatively high, with over 25% of the population sleeping for less than the recommended minimum of 7 hours per night, and approximately 15% regularly reporting trouble falling or staying asleep.1,2 Although some of these cases may represent sleep disorders, most of the individuals who report some problem with sleep likely do not meet criteria for a sleep disorder. Still, poor sleep quality is associated with poor cardiometabolic health,3 mental health,4 and daytime functioning.5 Despite the high prevalence of these problems and identified associated risks, there are still few interventions that are specifically designed to address subclinical sleep quality.
A wearable device that emits red and near-infrared (NIR) light may be beneficial for sleep and mood. While photo-biomodulation, or phototherapy, for sleep typically focuses on the presence or absence of light entering the eye to regulate sleep timing and mood,6 NIR and red light applied to the skin may create a cascade of effects that improve sleep and daytime function through skin warming and other pathways.7
NIR therapy has been shown to improve chronic pain,8,9 and has been effective and comparable to exercise training in fibromyalgia treatment.10 It promotes capillary growth in skeletal muscle11 and exhibits anti-inflammatory effects by attenuating circulating levels of prostaglandin-2.12
Some of the observed improvements in pain may also result from the ability of NIR to improve cardiovascular function. This may occur through increased vasodilation via the direct application of heat and upregulation of nitric oxide (NO).13,14 NIR wavelengths are absorbed by cytochrome c oxidase (CCO), the terminal enzyme of the electron transport chain housed within the mitochondria.15 This results in an increased rate of respiration and thus increased adenosine triphosphate (ATP) production.16 In the process of increasing metabolism within the cell, NO photo-dissociates from CCO.17
Previous studies have not focused on the benefits of NIR therapy on sleep quality specifically, despite evidence that this approach may influence related pathways. NIR devices are already commercially available to the general public. Therefore, if these devices do demonstrate benefits for subclinical sleep quality, they may represent a novel approach for improving sleep health.
One way that NIR therapy may also support sleep health is through effects on relaxation. Although relaxation is typically insufficient to treat sleep disorders,18 other interventions focused on relaxation have been shown to generally improve sleep quality.19–21 Relaxation from direct heat may help to decrease cortisol levels, thus reducing nocturnal arousals.22 NIR may also decrease circulating levels of norepinephrine, one of the main neurotransmitters involved in arousal.23 Last, direct skin warming and NO have both been shown to promote non–rapid eye movement (non-REM) sleep.24,25
The objective of the present study was to determine whether an NIR device worn before bed improved sleep quality, reduced sleep onset, increased total sleep time, modified estimated sleep architecture, and/or was associated with improved daytime function following use.
METHODS
Participants
Healthy adults aged 30–60 years (n = 30) were recruited locally from Tucson, Arizona. Recruitment was achieved through flyers and social media advertising. Inclusion criteria were that participants needed to be fluent in English, have access to a mobile device (ie, smartphone) and a residential mailing address, and exhibit a score ≥ 8 on the Insomnia Severity Index (ISI). Individuals were excluded if they had a diagnosed sleep or psychiatric disorder (assessed using self-reported medical history), met apparent criteria for a sleep disorder (assessed using the Sleep Disorder Symptoms Checklist-25 [SDSCL-25]29 administered during the screening interview), took medications that interfered with sleep, or had a medical condition that prevented them from participating in the study. They were also excluded if they were shift workers or had unusual sleep timing, regularly smoked tobacco or cannabis, were pregnant, or were using any other phototherapy devices. Participants were asked to restrict alcohol consumption to no more than 2 drinks within 4 hours of sleep and consume no caffeine after 12 pm while participating in the study.
Measures
Phototherapy device
The phototherapy device (CeraZ Technologies LLC, Boca Raton, FL) consisted of a neoprene collar designed to be worn around the neck (Figure 1 and Figure 2), connected to a controller and 36-V power supply. The power supply was connected to a 120/VAC power outlet during use. The collar was fitted with 48 light-emitting diodes that emit 660-nm, 740-nm, 810-nm, and 870-nm wavelengths of red and NIR light at 40 mW each (48 light-emitting diodes × 40 mW each = 1,920 mW total = 192 lumens). This combination of wavelengths was chosen to cover a broad spectrum of potentially therapeutic red and NIR light.
Figure 1. The phototherapy collar.

Figure 2. The phototherapy device.
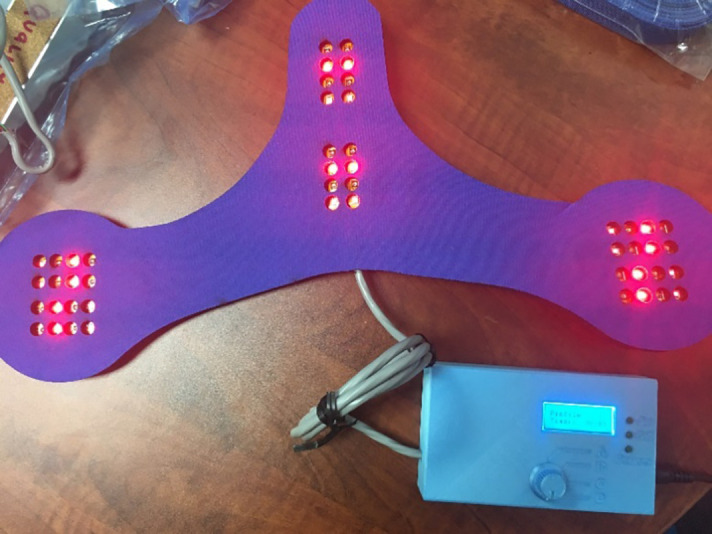
Participants wore the device every other night for 25 minutes’ duration in the 1 hour prior to their targeted bedtime. They could watch television, read, listen to music, or pursue other typical prebed relaxation rituals during this time. The activity performed while wearing the device was recorded in the morning sleep diary the next day. The sham devices were identical except that they did not emit any light.
Oura ring
The Oura Ring Heritage Generation 2 (OURA, Oulu, Finland) measures and approximates sleep vs wake and sleep stages via accelerometry (for movement) and photoplethysmography (for heart rate).26 Rings are waterproof, ceramic, and connected to a mobile app that uses a proprietary algorithm to estimate sleep. Previous studies have shown that these devices perform well in capturing sleep vs wake in adults without sleep disorders.26,27 Data on assessment of sleep stages suggest that these devices roughly approximate polysomnographic sleep stages but are not equivalent to polysomnography.26 The ring is designed to be worn continuously, apart from during charging. The ring transmits user data to the app at regular intervals throughout the day via Bluetooth, although manual synchronizations can also be triggered by the user through the app. Participants’ data were accessed by study personnel via the Oura Teams dashboard.
Sleep diary
The sleep diary28 was a brief questionnaire designed to be completed within 30 minutes of waking each morning during the study period. It included questions about time to bed and nighttime arousals from the previous night, as well as self-perceived daytime sleepiness and general quality of sleep.
Expectancy questionnaires
Participants were asked about their initial impressions upon their first interaction with the device. They were asked questions about how comfortable the device was, and whether they anticipated that there would be any problems during use. They were also asked about their expectations of how much the device would improve their sleep, ability to relax, daytime mood, energy, and performance on a scale of 0 to 100. They were asked to rate these parameters again upon completion of the study.
Weekly surveys
Surveys were administered the first night of device use and every week thereafter until completion of the study and included demographics items, the SDSCL-25,29 an instrument that assesses symptoms of common sleep disorders; the Systematic Assessment for Treatment of Emergent Effects (SAFTEE),30 a survey that is routinely administered during clinical trials to assess for adverse effects; the ISI,31 a 7-item instrument that assesses for symptoms of insomnia, the Positive and Negative Affect Scale (PANAS);32 consisting of 2 scales that measure both positive and negative mood; the Perceived Stress Scale (PSS),33 which assesses perceived stress; the Fatigue Severity Scale (FSS),34 which asks about current fatigue severity; the Profile of Mood States (POMS),35 which assesses mood; the Circadian Energy Scale (CIRENS),36 which assesses chronotype; and the Pittsburgh Sleep Quality Index (PSQI),37 which assesses recent perceived sleep quality.
Procedure
Baseline period
Participants completed a 2-week baseline period consisting of Oura ring use and sleep diary completion. This established current sleep behavior prior to introducing the intervention.
Intervention period
Following the baseline period, participants continued to use the Oura ring and complete sleep diaries while wearing the phototherapy device every other night for 3 weeks. Weekly surveys were completed during the intervention, and a debrief interview was conducted upon completion.
Statistical analyses
All statistical analyses were completed using STATA SE 17.0 (StataCorp LLC, College Station, TX). Mean weekly sleep diary and Oura data were computed, and the baseline (pre) and intervention (post) averages were compared using paired t tests. The first-night survey (prior to device use) and final weekly survey (at the end of the intervention period) were compared using paired t tests. The initial expectancy (pre) estimates of improvements in sleep, relaxation, daytime mood, performance, and energy levels were compared to scores provided during the debrief interview (post) using paired t tests. All primary outcome data were adjusted using a Holm-Bonferroni correction to account for multiple comparisons.
Exploratory post hoc analyses comparing the baseline period (pre) with the third week of the intervention only (post) were also conducted to detect any potential cumulative effects of device use.
RESULTS
Characteristics of the sample
Characteristics of the sample are reported in Table 1. The sample comprised mostly White, middle-class females with a mean age of 51.18 (±10.50) years.
Table 1.
Characteristics of the sample.
| Demographics | Sham | Active |
|---|---|---|
| Age, y | 55 ± 7.51 | 49 ± 11.06 |
| Sex | ||
| Female | 80% | 90% |
| Male | 20% | 10% |
| Race/ethnicity | ||
| White | 90% | 85% |
| Hispanic/Latino | 0% | 10% |
| Black (African) | 10% | 0% |
| Asian | 0% | 5% |
| Financial status | ||
| Lower middle | 20% | 25% |
| Middle | 40% | 35% |
| Upper middle | 40% | 40% |
| Sleep satisfaction | ||
| 0–19% | 10% | 10% |
| 20–39% | 50% | 5% |
| 40–59% | 30% | 35% |
| 60–79% | 10% | 40% |
| 80–100% | 0% | 10% |
Age is reported as mean ± standard deviation.
Primary outcomes
Subjective ratings
There was a trend toward perceived improvements in daytime performance following participation in the study among active, but not control, participants, but there were no significant differences between groups before or after applying a Holm-Bonferroni correction (Table 2). There were within-group improvements in perceived relaxation and daytime mood among active, but not control, participants (Table 3).
Table 2.
Between-group differences in self-reported perception of the device before and after use.
| Subjective Rating (%) | P | ||
|---|---|---|---|
| Measure | Sham Group | Active Group | |
| Sleep | −21.5 (30.9) | −3.65 (23.7) | .090 |
| Relax | 5.5 (21.7) | 17.5 (23.1) | .183 |
| Daytime | −25.0 (23.7) | −10.6 (27.6) | .170 |
| Perform | −26.0 (30.2) | −5.8 (24.4) | .058 |
| Energy | −18.7 (25.7) | −6.8 (25.1) | .233 |
Data are presented as mean (standard deviation); t tests were performed on change scores pre- and postintervention.
Table 3.
Within-group statistically significant changes across all measures.
| Measure | Sham Group | Active Group | ||
|---|---|---|---|---|
| Mean (SD) | P | Mean (SD) | P | |
| Survey data | ||||
| ISI item 7 | −0.75 (0.89) | 0.048 | −0.70 (1.09) | .009 |
| ISI total | −2.38 (2.20) | 0.019 | −1.70 (3.39) | .037 |
| SDS insomnia | −1.44 (1.51) | 0.021 | −1.35 (2.25) | .015 |
| POMS depression | – | – | −0.22 (0.42) | .029 |
| Oura | ||||
| REM (%) | – | – | −0.01 (0.02) | .034 |
| Diary | ||||
| Karolinska Sleepiness Scale | −0.56 (0.62) | 0.019 | −0.57 (0.85) | .008 |
| Sleep latency (min) | – | – | −6.33 (7.30) | .001 |
| Sufficient | – | – | 0.07 (1.51) | .044 |
| Refreshed | 0.35 (0.50) | 0.057 | 0.71 (0.71) | <.0001 |
| Sleep quality | 0.37 (0.52) | 0.051 | 0.59 (0.77) | .003 |
| Subjective rating (%) | ||||
| Sleep | −21.50 (30.92) | 0.055 | – | – |
| Relax | – | – | 17.50 (23.14) | .003 |
| Daytime | – | – | 17.50 (23.14) | .003 |
| Perform | −18.70 (25.73) | 0.047 | – | – |
| Energy | −26.00 (30.17) | 0.023 | – | – |
Data are presented as mean (SD); t tests were performed on change scores pre- and postintervention. ISI = Insomnia Severity Index, POMS = Profile of Mood States, REM = rapid eye movement, SD = standard deviation, SDS = Sleep Disorders Symptoms Checklist-25.
Insomnia severity
There were no between-group differences in ISI score before or after applying a Holm-Bonferroni correction (Table 4). However, as seen in Table 3, there were significant within-group improvements (specifically item 7, which asks, “To what extend do you feel that your current sleep problems interfere with daytime function?”) in both the active and control groups.
Table 4.
Between-group differences in survey results.
| Survey Data Measure | Sham Group | Active Group | P |
|---|---|---|---|
| SAFTEE total score | 13.80 (45.18) | −9.40 (11.05) | .036* |
| SAFTEE (other) | 4.10 (8.71) | −2.90 (3.80) | .005* |
| ISI | −2.38 (2.12) | −1.70 (3.39) | .608 |
| PANAS positive | −1.38 (6.76) | −0.25 (5.41) | .647 |
| PANAS negative | −0.88 (2.78) | −3.00 (4.71) | .246 |
| Perceived Stress Scale | −0.75 (5.90) | −0.40 (6.28) | .893 |
| Fatigue Severity Scale | 2.75 (7.32) | −2.10 (6.14) | .085 |
| POMS tension | −0.25 (0.97) | −0.13 (0.57) | .674 |
| POMS depression | −0.17 (0.41) | −0.22 (0.42) | .788 |
| POMS anger | −0.09 (0.89) | −0.16 (0.44) | .787 |
| POMS vigor | 0.04 (0.91) | 0.11 (0.71) | .838 |
| POMS fatigue | 0.03 (1.15) | −0.38 (0.95) | .347 |
| POMS confusion | −0.38 (0.73) | −0.12 (0.42) | .254 |
| Pittsburgh Sleep Quality Index | −0.88 (1.25) | −0.95 (2.61) | .939 |
| SDSCL-25 insomnia | −1.44 (1.51) | −1.35 (2.25) | .910 |
| SDSCL-25 circadian | −0.67 (0.87) | −0.35 (1.18) | .479 |
| SDSCL-25 narcolepsy | 0.00 (0.00) | −0.25 (0.72) | .309 |
| SDSCL-25 sleep apnea | −0.89 (1.05) | −0.60 (1.19) | .537 |
| SDSCL-25 RLS | 0.00 (0.50) | −0.05 (0.51) | .808 |
| SDSCL-25 parasomnias | −0.22 (0.44) | −0.40 (0.68) | .481 |
| SDSCL-25 grind teeth | 0.11 (0.33) | −0.15 (0.67) | 0.281 |
Data are presented as mean (standard deviation); t tests were performed on change scores pre- and postintervention. *Statistically significant. ISI = Insomnia Severity Index, PANAS = Positive and Negative Affect Score, POMS = Profile of Mood States, SDSCL-25 = Sleep Disorder Symptoms Checklist-25.
Objective sleep efficiency
There were no significant differences in sleep efficiency as measured using the Oura ring between active and sham groups before or after applying a Holm-Bonferroni correction (Table 5).
Table 5.
Between-group differences in Oura ring outcomes.
| Oura Measure | Group | P | |
|---|---|---|---|
| Sham | Active | ||
| Time in bed (min) | 3.02 (37.60) | 1.71 (37.56) | .929 |
| Total sleep time (min) | 7.26 (23.38) | 1.52 (21.80) | .512 |
| Sleep efficiency (%) | 0.75 (4.12) | −0.24 (2.69) | .541 |
| Light (min) | 4.68 (21.03) | 0.24 (20.55) | .584 |
| REM (min) | 5.30 (14.83) | −3.56 (10.86) | .073 |
| Deep (min) | −2.72 (11.01) | 4.84 (11.78) | .102 |
| Light (%) | −0.00 (0.03) | 0.00 (0.03) | .912 |
| REM (%) | 0.01 (0.03) | −0.01 (0.02) | .047* |
| Deep (%) | −0.01 (0.04) | 0.01 (0.04) | .262 |
| Total wake time (min) | −4.25 (26.90) | 0.18 (18.64) | .601 |
| Time to bed (time) | −0.05 (0.28) | −0.06 (0.52) | .960 |
| Time out of bed (time) | 0.01 (0.66) | −0.13 (0.60) | .574 |
Data are presented as mean (standard deviation); t tests were performed on change scores pre- and postintervention. *Statistically significant. REM = rapid eye movement.
Secondary outcomes
Sleep diary measures
There were no significant between-group differences in sleep diary variables (Table 6). Within-group improvements in perceived sleepiness, as assessed by Karolinska Sleepiness Score, perceived sense of feeling refreshed, and sleep quality were seen in both active and control groups (Table 3). Within-group improvements in perceived sleep-onset latency and sufficient sleep duration were seen in the active, but not control, group.
Table 6.
Between-group sleep diary outcomes.
| Diary Measure | Group | P | |
|---|---|---|---|
| Sham | Active | ||
| Karolinska Sleepiness Scale | −0.56 (0.62) | 0.57 (0.85) | .970 |
| Time to bed (time) | −0.12 (0.05) | 0.02 (0.01) | .240 |
| Time to sleep (time) | −0.00 (0.06) | 0.03 (0.15) | .583 |
| Sleep latency (min) | −1.50 (6.38) | −6.33 (7.30) | .086 |
| Sleep efficiency (%) | 1.64 (3.13) | 1.84 (13.67) | .964 |
| Total sleep time (min) | 0.00 (0.02) | 0.01 (0.03) | .507 |
| Number of awakenings | −0.02 (0.71) | −0.29 (0.77) | .344 |
| Wake after sleep onset (min) | −2.04 (18.71) | 0.64 (11.92) | .636 |
| Wake after sleep onset time out of bed (min) | −3.25 (8.44) | 0.33 (1.39) | .198 |
| Wake up time (time) | 0.01 (0.03) | 0.01 (0.03) | .990 |
| Time out of bed (time) | 0.00 (0.03) | 0.00 (0.02) | .834 |
| Sufficient | 0.04 (0.12) | 0.07 (1.51) | .594 |
| Refreshed | 0.35 (0.50) | 0.71 (0.71) | .164 |
| Sleep quality | 0.37 (0.52) | 0.59 (0.77) | .426 |
Data are presented as mean (standard deviation); t tests were performed on change scores pre- and postintervention.
Oura ring data
There were no significant differences in objective sleep measures using the Oura ring between sham and active groups. A spurious decrease in REM sleep among the active group when REM sleep was assessed as a percentage of total sleep minutes (Table 3 and Table 5) was not mirrored when REM sleep was assessed by total minutes.
Survey data
There were statistically significant improvements among users of the active devices, as compared with the control group, in SAFTEE scores pertaining to self-reported problems falling asleep, trouble thinking/concentrating, and anxiety (Table 4). There were significant within-group improvements in insomnia symptoms as assessed using the SDSCL-25 insomnia item in both active and control groups. There was a significant within-group improvement in POMS depression subscore among the active, but not control, group.
Exploratory analyses
To account for any potential cumulative effects of device use, change scores were calculated from the baseline period to the third week of the intervention only. There were no significant differences in sleep diary measures or Oura scores.
DISCUSSION
A red and NIR-emitting device worn around the neck before bed may offer some benefits to sleep and next-day function, but further investigation is required. Statistically significant improvements were mostly observed in within-group, self-reported (subjective) data and there were no differences between groups in terms of a priori primary outcomes.
The sham-controlled study design was rigorous in that it assessed the efficacy of the phototherapy device above and beyond other aspects of the protocol that had the potential to improve sleep. The Oura ring is a sleep tracker that can provide regular feedback about sleep quality and duration and may have encouraged some participants to create more sleep opportunity for themselves than they did prior to using the device. Further, the period of mandatory sedentary activity for 25 minutes before bed every other night while wearing the collar (regardless of whether or not it emitted light) may have promoted relaxation for individuals who, prior to the study period, were not allocating sufficient wind-down time before bed. Many participants commented during the debrief interviews that they felt that these 2 activities alone may have improved their sleep. The within-group analyses indicated that both the control and active groups improved in several areas of sleep and mood, which led to fewer statistically significant differences between the 2 groups.
Gamma-amino butyric acid (GABA-ergic) neurons in the preoptic area of the mouse hypothalamus have been shown to respond to changes in ambient temperature.38 Excitation of these cells through warming of the environment or skin promotes a robust increase in non-REM sleep. Further, although a drop in core body temperature is known to promote sleep onset, Harding and colleagues38 observed that sleep onset preceded a decrease in core body temperature in these experiments. This points to a unique circuitry that involves skin warming and non-REM onset.39
A study by Igaki and colleagues40 investigated whether sleep was improved after warming the posterior cervical skin—similar to the area warmed in the present study—to approximately 40°C for 30 minutes before habitual bedtime for a period of 6 days. The application of heat to this area improved self-reported feelings of restfulness following subsequent sleep, and delta power, as measured using electroencephalography, increased in the first third of the sleep episodes. The application of heat in both this and the present study may have reduced somatic arousal, promoting parasympathetic nerve activity and perceived relaxation.
The devices used in the present study did not result in any reported adverse effects, although many participants commented that the prototype devices manufactured for this study could become mildly to moderately uncomfortable to wear. This discomfort may have counteracted some of the benefits potentially associated with device use.
Limitations
These findings must be understood within the context of the study limitations. First, this was a small sample of 30 individuals who were mostly White midlife females. As such, the study was underpowered but served as essential exploratory analyses. Second, the use of a commercial multisensory device that provides feedback via the associated app may have served as a sleep intervention that improved sleep in both experimental groups independent of the phototherapy device. The neoprene collar was noted by some participants to be somewhat uncomfortable during use due to rubbing along the jawline and this may have negated some of the potential benefits of phototherapy use. Last, the participants in this study were recruited locally in Tucson, Arizona, where baseline sun exposure is relatively high for residents. Given the importance of daylight exposure for sleep, results obtained in this locale may not necessarily translate to other locations.
CONCLUSIONS
This study used a novel, wearable phototherapy device targeted at improving sleep and next-day function. Usage protocols, including dose parameters, wavelengths, and milliwatt power level, are yet to be refined and were provided by the sponsor based on what was believed to be feasible to ensure adherence. The results of this study suggest that users generally felt that their subjective experience of relaxation and sleep improved, suggesting that cervical warming, or exposure to red and NIR phototherapy, shows promise for improving sleep health in the general population, perhaps through reduced somatic arousal and parasympathetic activation. Whether the effects are mediated by metabolic changes or fluctuations in NO are yet to be determined.
Future studies should explore the optimal frequency and duration of device use as well as modifications to the device structure to improve comfort and fit. Future investigations should also be conducted on larger sample sizes, should consider a crossover design paradigm, and should include a more diverse sample.
DISCLOSURE STATEMENT
Work for this study was performed in the Sleep and Health Research Program at the University of Arizona in Tucson, Arizona. This study was funded by a grant from CeraZ Technologies. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: M.A.G. was responsible for study conceptualization. K.E.R.K., C.C.A.W., and C.H. were responsible for all data collection. M.A.G. and K.E.R.K. were responsible for statistical analyses. K.E.R.K. and M.A.G. were responsible for manuscript preparation, with all authors reviewing and approving the final manuscript.
ABBREVIATIONS
- ISI
Insomnia Severity Index
- NIR
near-infrared
- PANAS
Positive and Negative Affect Scale
- POMS
Profile of Mood States
- REM
rapid eye movement
- SDSCL-25
Sleep Disorder Symptoms Checklist-25
REFERENCES
- 1. Adjaye-Gbewonyo D . QuickStats: percentage of adults aged ≥18 years who sleep <7 hours on average in a 24-hour period, by sex and age group—National Health Interview Survey, United States, 2020 . MMWR Morb Mortal Wkly Rep. 2022. ; 71 ( 10 ): 393 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adjaye-Gbewonyo D , Ng AE , Black LI . Sleep difficulties in adults: United States, 2020 . NCHS Data Brief. 2022. : 436 : 1 – 8 . [PubMed] [Google Scholar]
- 3. Cappuccio FP , Miller MA . Sleep and cardio-metabolic disease . Curr Cardiol Rep. 2017. ; 19 ( 11 ): 110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scott AJ , Webb TL , Martyn-St James M , Rowse G , Weich S . Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials . Sleep Med Rev. 2021. ; 60 : 101556 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Killgore WD . Effects of sleep deprivation on cognition . Prog Brain Res. 2010. ; 185 : 105 – 129 . [DOI] [PubMed] [Google Scholar]
- 6. Brown TM , Brainard GC , Cajochen C , et al . Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults . PLoS Biol. 2022. ; 20 ( 3 ): e3001571 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maiello M , Losiewicz OM , Bui E , et al . Transcranial photobiomodulation with near-infrared light for generalized anxiety disorder: a pilot study . Photobiomodul Photomed Laser Surg. 2019. ; 37 ( 10 ): 644 – 650 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gale GD , Rothbart PJ , Li Y . Infrared therapy for chronic low back pain: a randomized, controlled trial . Pain Res Manag. 2006. ; 11 ( 3 ): 193 – 196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kingsley JD , Demchak T , Mathis R . Low-level laser therapy as a treatment for chronic pain . Front Physiol. 2014. ; 5 : 306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. da Silva MM , Albertini R , de Tarso Camillo de Carvalho P , et al . Randomized, blinded, controlled trial on effectiveness of photobiomodulation therapy and exercise training in the fibromyalgia treatment . Lasers Med Sci. 2018. ; 33 ( 2 ): 343 – 351 . [DOI] [PubMed] [Google Scholar]
- 11. Kuhlenhoelter AM , Kim K , Neff D , et al . Heat therapy promotes the expression of angiogenic regulators in human skeletal muscle . Am J Physiol Regul Integr Comp Physiol. 2016. ; 311 ( 2 ): R377 – R391 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Campana VR , Castel A , Vidal AE , Juri H , Palma JA . Prostaglandin E2 in experimental arthritis of rats irradiated with He-Ne laser . J Clin Laser Med Surg. 1993. ; 11 ( 2 ): 79 – 81 . [Google Scholar]
- 13. Brunt VE , Eymann TM , Francisco MA , Howard MJ , Minson CT . Passive heat therapy improves cutaneous microvascular function in sedentary humans via improved nitric oxide-dependent dilation . J Appl Physiol (1985). 2016. ; 121 ( 3 ): 716 – 723 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yokomizo S , Roessing M , Morita A , et al . Near-infrared II photobiomodulation augments nitric oxide bioavailability via phosphorylation of endothelial nitric oxide synthase . FASEB J. 2022. ; 36 ( 9 ): e22490 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Little AG , Lau G , Mathers KE , Leary SC , Moyes CD . Comparative biochemistry of cytochrome c oxidase in animals . Comp Biochem Physiol B Biochem Mol Biol. 2018. ; 224 : 170 – 184 . [DOI] [PubMed] [Google Scholar]
- 16. Eells JT , Henry MM , Summerfelt P , et al . Therapeutic photobiomodulation for methanol-induced retinal toxicity . Proc Natl Acad Sci USA. 2003. ; 100 ( 6 ): 3439 – 3444 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hamblin MR . Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation . Photochem Photobiol. 2018. ; 94 ( 2 ): 199 – 212 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Edinger JD , Arnedt JT , Bertisch SM , et al . Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline . J Clin Sleep Med. 2021. ; 17 ( 2 ): 255 – 262 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cordi MJ , Ackermann S , Rasch B . Effects of relaxing music on healthy sleep . Sci Rep. 2019. ; 9 ( 1 ): 9079 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tubbs AS , Kennedy KER , Alfonso-Miller P , Wills CCA , Grandner MAA . A randomized, double-blind, placebo-controlled trial of a polyphenol botanical blend on sleep and daytime functioning . Int J Environ Res Public Health. 2021. ; 18 ( 6 ): 3044 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wong KF , Perini F , Lin J , et al . Dissociable changes in sleep architecture with mindfulness and sleep hygiene intervention in older adults: secondary and exploratory analysis of polysomnography data from the Mindfulness Sleep Therapy (MIST) trial . Sleep Health. 2022. ; 8 ( 4 ): 364 – 372 . [DOI] [PubMed] [Google Scholar]
- 22. Oster H , Challet E , Ott V , et al . The functional and clinical significance of the 24-hour rhythm of circulating glucocorticoids . Endocr Rev. 2017. ; 38 ( 1 ): 3 – 45 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mitchell HA , Weinshenker D . Good night and good luck: norepinephrine in sleep pharmacology . Biochem Pharmacol. 2010. ; 79 ( 6 ): 801 – 809 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harding EC , Franks NP , Wisden W . The temperature dependence of sleep . Front Neurosci. 2019. ; 13 : 336 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Obal F Jr , Krueger JM . Biochemical regulation of non-rapid-eye-movement sleep . Front Biosci. 2003. ; 8 ( 4 ): d520 – d550 . [DOI] [PubMed] [Google Scholar]
- 26. de Zambotti M , Rosas L , Colrain IM , Baker FC . The sleep of the ring: comparison of the ŌURA sleep tracker against polysomnography . Behav Sleep Med. 2019. ; 17 ( 2 ): 124 – 136 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Asgari Mehrabadi M , Azimi I , Sarhaddi F , et al . Sleep tracking of a commercially available smart ring and Smartwatch against medical-grade actigraphy in everyday settings: instrument validation study . JMIR Mhealth Uhealth. 2020. ; 8 ( 10 ): e20465 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carney CE , Buysse DJ , Ancoli-Israel S , et al . The consensus sleep diary: standardizing prospective sleep self-monitoring . Sleep. 2012. ; 35 ( 2 ): 287 – 302 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Klingman KJ , Jungquist CR , Perlis ML . Introducing the Sleep Disorders Symptom Checklist-25: a primary care friendly and comprehensive screener for sleep disorders . Sleep Med Res. 2017. ; 8 ( 1 ): 17 – 25 . [Google Scholar]
- 30. Johnson BA , Ait-Daoud N , Roache JD . The COMBINE SAFTEE: a structured instrument for collecting adverse events adapted for clinical studies in the alcoholism field . J Stud Alcohol Suppl. 2005. ; 15 : 157 – 167 ; discussion 140. [DOI] [PubMed] [Google Scholar]
- 31. Morin CM , Belleville G , Bélanger L , Ivers H . The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response . Sleep. 2011. ; 34 ( 5 ): 601 – 608 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Watson D , Clark LA , Tellegen A . Development and validation of brief measures of positive and negative affect: the PANAS scales . J Pers Soc Psychol. 1988. ; 54 ( 6 ): 1063 – 1070 . [DOI] [PubMed] [Google Scholar]
- 33. Cohen S , Kamarck T , Mermelstein R . A global measure of perceived stress . J Health Soc Behav. 1983. ; 24 ( 4 ): 385 – 396 . [PubMed] [Google Scholar]
- 34. Krupp LB , LaRocca NG , Muir-Nash J , Steinberg AD . The Fatigue Severity Scale. Application to patients with multiple sclerosis and systemic lupus erythematosus . Arch Neurol. 1989. ; 46 ( 10 ): 1121 – 1123 . [DOI] [PubMed] [Google Scholar]
- 35. McNair DM . Manual Profile of Mood States. San Diego, CA: : Educational & Industrial Testing Service; ; 1971. . [Google Scholar]
- 36. Ottoni GL , Antoniolli E , Lara DR . The Circadian Energy Scale (CIRENS): two simple questions for a reliable chronotype measurement based on energy . Chronobiol Int. 2011. ; 28 ( 3 ): 229 – 237 . [DOI] [PubMed] [Google Scholar]
- 37. Buysse DJ , Reynolds CF 3rd , Monk TH , Berman SR , Kupfer DJ . The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research . Psychiatry Res. 1989. ; 28 ( 2 ): 193 – 213 . [DOI] [PubMed] [Google Scholar]
- 38. Harding EC , Yu X , Miao A , et al . A neuronal hub binding sleep initiation and body cooling in response to a warm external stimulus . Curr Biol. 2018. ; 28 ( 14 ): 2263 – 2273, e4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Peever J . Neuroscience: a ‘skin warming’ circuit that promotes sleep and body cooling . Curr Biol. 2018. ; 28 ( 14 ): R800 – R802 . [DOI] [PubMed] [Google Scholar]
- 40. Igaki M , Suzuki M , Sakamoto I , Ichiba T , Kuriyama K , Uchiyama M . Effects of bedtime periocular and posterior cervical cutaneous warming on sleep status in adult male subjects: a preliminary study . Sleep Biol Rhythms. 2018. ; 16 ( 1 ): 77 – 84 . [DOI] [PMC free article] [PubMed] [Google Scholar]


