Abstract
Study Objectives:
This study aimed to estimate the 12-month prevalence of diagnosed sleep disorders among veterans with and without serious mental illnesses (SMI) in Veterans Affairs health record data in 2019. We also examined diagnosed sleep disorders across a 9-year period and explored associations with demographic and health factors.
Methods:
This study used health record data from VISN 4 of the Veterans Health Administration from 2011 to 2019. SMI diagnoses included schizophrenia and bipolar spectrum diagnoses as well as major depression with psychosis. Sleep diagnoses included insomnias, hypersomnias, sleep-related breathing disorders, circadian rhythm sleep-wake disorders, and sleep-related movement disorders. Demographic and health-related factors were also collected from the record.
Results:
In 2019, 21.8% of veterans with SMI were diagnosed with a sleep disorder. This is a significantly higher proportion than for veterans without SMI, 15.1% of whom were diagnosed with a sleep disorder. Sleep disorder rates were highest in veterans with a chart diagnosis of major depression with psychosis. From 2011 to 2019, the overall prevalence of sleep disorders in veterans with SMI more than doubled (10.2%–21.8%), suggesting improvements in the detection and diagnosis of sleep concerns for this group.
Conclusions:
Our findings suggest that identification and diagnosis of sleep disorders for veterans with SMI has improved over the past decade, though diagnoses still likely underrepresent actual prevalence of clinically relevant sleep concerns. Sleep concerns may be at particularly high risk of going untreated in veterans with schizophrenia-spectrum disorders.
Citation:
Bonfils KA, Longenecker JM, Soreca I, et al. Sleep disorders in veterans with serious mental illnesses: prevalence in Veterans Affairs health record data. J Clin Sleep Med. 2023;19(9):1651–1660.
Keywords: sleep disorder, serious mental illness, schizophrenia, bipolar disorder, sleep apnea, insomnia, psychosis, veterans
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study assessed the prevalence of sleep disorders in veterans with and without serious mental illnesses and explored relevant demographic and health information. Additionally, we assessed changes in sleep disorder diagnoses from 2011 to 2019.
Study Impact: We found that veterans with serious mental illnesses had higher rates of comorbid sleep disorder diagnoses than veterans without serious mental illnesses. Additionally, there was a two-fold increase in the diagnosis of sleep disorders in veterans with serious mental illnesses from 2011 to 2019, though prevalence rates still likely represent an underestimate of clinically relevant sleep concerns.
INTRODUCTION
Approximately 4% to 5% of veterans receiving health care through Veterans Affairs (VA) services are diagnosed with a serious mental illness (SMI).1 This group includes schizophrenia-spectrum and severe mood diagnoses (ie, bipolar I and II, major depression with psychosis), which are linked to poor physical health outcomes,2 increased mortality,3 and heightened health care spending.4 Yet veterans with SMI experience barriers to accessing and engaging with health care above and beyond those faced by veterans without SMI, and physical and mental health complaints may go untreated or unrecognized.5–7 One domain in which concerns may be at particular risk of being overlooked in treatment is sleep disturbance.8 Many people with SMI experience significant disruptions to their sleep, which are linked to increased symptomatology, risk for suicide attempt, and reduced quality of life9–11; indeed, SMI symptomatology and sleep disturbance are hypothesized to bidirectionally aggravate symptom expression and impact treatment outcomes for this group.12 Sleep disturbance refers to problems falling or staying asleep (ie, insomnia or insomnia-like symptoms), prolonged sleep and excessive daytime sleepiness (ie, hypersomnia or hypersomnia-like symptoms), or delayed or irregular sleep phase (circadian rhythm abnormalities), among other sleep abnormalities.13,14 Studies have identified rates of sleep disturbance as high as 25% to 80% in people with SMI,13,15–17 as compared to 15% to 30% in the general population.18 Of note, clinical research of people with SMI has generated sleep disorders prevalence estimates that are substantially higher than those produced by record-based studies.19,20 Coupled with data indicating that formal sleep assessment and evidence-based treatment for sleep in SMI are underutilized,21 these findings suggest that sleep disturbance among individuals with SMI is underrecognized in clinical practice.
As such, further work is needed to promote our understanding of the prevalence of sleep diagnoses in persons with SMI in everyday clinical practice. One method of inquiry with particular relevance to these issues is health record data. Health record data offers valuable insight into prevalence of sleep diagnoses in a real-world context. As the largest integrated health care system in the United States, VA health record data offers a unique opportunity to better understand care provided to veterans and identify areas for potential improvement. The Veterans’ Health Administration is comprised of both large medical centers and community-based outpatient health care facilities where veterans receive care across a continuum of physical and mental health conditions. Organization and availability of services may vary across facilities, similar to the private sector; however, VA utilizes national rollouts to ensure availability of high-quality, evidence-based care for veterans, including in the realms of sleep and mental health care. For example, competency-based provider training for cognitive behavioral therapy for insomnia was rolled out across VA in 2011.22 Thus, examination of VA medical records is a prime opportunity to better understand sleep and SMI diagnoses among veterans.
Considering that veterans with SMI have multiple known risk factors for sleep disorders (eg, physical and mental comorbidities, obesity23,24), improving the identification, evaluation, and treatment of sleep disorders is needed for this high-risk group. VA health record data has been used to examine veteran sleep disorder diagnoses and comorbidities in prior research. Two studies have investigated prevalence of sleep disorder diagnoses across VA facilities nationwide. The first examined data from 2000 to 2010.25 This study found lifetime prevalence rates from 0.01% (circadian rhythm disorders) to 4.5% (sleep apnea), with 9.7% of all veterans meeting criteria for at least one sleep disorder diagnosis at some point during the study period.25 The second examined data from 2012 to 2018 and found in 2018 prevalence rates ranging from 1.7% (hypersomnias) to 22.2% (sleep-related breathing disorders).26 While substantial, these rates are lower than rates in clinical research, which suggest up to one-third of the population have at least one sleep disorder.18 Similar discrepancies are found in SMI-specific health record studies; one study with data from 2001 to 2011 found 13.7% of veterans with SMI had diagnoses of sleep apnea,20 in contrast to rates of 25% to 50% suggested by clinical research using polysomnography.17,27
The discrepancy between record-based and clinical research for those with SMI likely has numerous contributing factors. First, clinician surveys in European countries suggest that clinicians less commonly use formal sleep assessments in diagnosis and treatment of people with psychosis, which may contribute to underrecognition of these issues in practice.21,28 This aligns with findings that suggest that people with SMI diagnoses are a vulnerable group at risk of having medical issues overlooked.6 Second, patient-related factors may play a role, as patients in this population may underreport sleep concerns. Further, both providers and patients with SMI (eg, experiencing psychotic, depressive, or manic symptoms) may mistakenly view sleep disturbance as a minor or secondary issue within the context of a person’s illness, despite evidence that sleep problems exacerbate psychotic and affective symptoms.8,29 Third, inaccurate or stigmatizing views toward patients with SMI may be held by some providers, which can affect evaluation of and treatment provided to those patients.30 One recent study demonstrated that almost three-quarters of patients with comorbid SMI and sleep disorders did not receive treatment for sleep disorders, despite over half of patients raising sleep-related concerns to their providers.8 Indeed, clinician surveys suggest that clinicians may view patients with SMI as unmotivated or unable to engage in sleep interventions.21,28 Lastly, one methodological factor worth mentioning is that many clinical studies of sleep disturbance may occur in settings where patients are already registering these concerns (ie, sleep clinics31) or may utilize convenience sampling procedures wherein participants who opt into the study may do so because they already have concerns about their sleep or are interested in learning more.16 This could bias estimates from clinical research upwards, contributing to the gap in prevalence estimates with medical record studies.
While discrepancies between health record and clinical research participant rates of sleep disorder diagnoses have been consistent for those with SMI, there is some evidence that trends in the diagnosis of sleep disorders are changing over time. For example, 13.7% of veterans with SMI had sleep apnea diagnoses in health record data from 2001 to 2011,20 as compared to only 4% to 5% using data from 1998 to 2001.19 Similarly, in non-SMI research, Alexander and colleagues25 identified a nearly six-fold increase in sleep disorder diagnoses among all veterans from 2000 to 2010, and Folmer and colleagues26 identified a four-fold increase in sleep-related breathing disorders and modest increase in insomnia diagnoses from 2012 to 2018. These data suggest two things. First, estimates of sleep disorder prevalence from older health records likely are not representative of current rates of sleep disorder diagnosis in VA health care. Second, trends in diagnosis and treatment of sleep disorders among veterans are changing, including among veterans with SMI, but the field has yet to characterize these changes in veterans with SMI.
As such, this study had three main aims. First, we aimed to estimate the 12-month prevalence of diagnosed sleep disorders among veterans with SMI in VA Veteran Integrated Service Network (VISN) 4 health record data from 2019, the most recent year of data available to us at the time of this writing, and, notably, prior to the onset of the COVID-19 global pandemic. Second, we aimed to examine yearly rates of diagnosed sleep disorders over a 9-year span of time (2011–2019) in veterans with SMI. Lastly, we aimed to explore demographic and health factors year by year. We expected to see higher rates of diagnosed sleep disorders in veterans with SMI in 2019 than those reported in earlier VA data19,20 and that, from 2011 to 2019, rates of diagnosed sleep disorders would have increased.
METHODS
Study population and procedures
US veterans receiving care in VISN 4 of the Veterans Health Administration during calendar years 2011 to 2019 were the target population for this study. Veterans were included in the sample for each year during which they had at least one clinical encounter at a VISN 4 facility. VISN 4 facilities include large VA hospitals in Pittsburgh and Philadelphia as well as seven smaller medical centers and community-based outpatient clinics in Pennsylvania, Delaware, and parts of Ohio, West Virginia, New York, and New Jersey. Veterans were excluded from the sample for a given year if medical record data indicated that the veteran received the majority of their VA care at a non-VISN 4 facility. Data for eligible veterans came from electronic health records and were accessed via the VA Corporate Data Warehouse. The data underlying this article cannot be shared publicly due to the sensitive and identifiable nature of said data. All procedures were approved by the VA Pittsburgh Healthcare System Institutional Review Board (IRBNet 1617272).
Diagnoses
Relevant diagnoses were assigned based on health record data for both SMI and sleep disorders. Defined SMI diagnoses included schizophrenia-spectrum disorders, bipolar disorders, and major depressive disorder with psychotic features. Defined sleep diagnoses were designed to follow Alexander and colleagues25 and included insomnias, hypersomnias, sleep-related breathing disorders, circadian rhythm sleep-wake disorders, and sleep-related movement disorders. For both categories, codes from the outpatient International Classification of Diseases, Ninth and Tenth Revisions32,33 were used. A full list of relevant International Classification of Diseases codes for each diagnostic group is available upon request from the authors. A diagnosis was considered to be present for a given calendar year when the veteran was assigned an International Classification of Diseases code relevant to that diagnosis at least twice within a 390-day period; the second, confirmatory diagnosis may have been made outside the calendar year. Further, the two diagnoses had to have occurred at least 30 days apart for the veteran to be assigned that diagnosis (ie, the 30/390 criteria34). This approach limits inclusion of rule-out or provisional diagnoses while also allowing inclusion of veterans who may only attend annual appointments.25,34 For both SMI and sleep diagnoses, we also defined broader groups based on the 30/390 criteria, such that any SMI or sleep diagnosis could serve as the confirmatory second diagnosis (ie, if a veteran was diagnosed with schizoaffective disorder at the start of one year and bipolar disorder at the end of the year, they would not meet criteria to be included in either the schizophrenia-spectrum or bipolar groups but would be included in a broader SMI group). Similar procedures were followed to define a broader sleep diagnosis group. These broad groups were defined in order to capture veterans with health concerns relevant to SMI or sleep diagnoses but who perhaps were undergoing differential diagnosis during a given calendar year.
Other demographic and health-related data
Demographic factors were defined for each year of data as available including veteran sex, race, marital status, and age. We further examined comorbid physical health conditions, collapsed across categories corresponding to relevant body systems (see Table 1). Of note, while we characterized a wide range of chronic comorbidities across multiple body systems, four categories were chosen for additional analyses based on their relevance to sleep and SMI diagnoses: endocrine, circulatory, respiratory (with breathing-related sleep disorders excluded), and digestive systems.35 Comorbidities were dichotomized to indicate presence/absence of diagnoses in the relevant category per year of data. Lastly, body mass index (BMI) was defined per year of data, such that the last instance from which this value could be calculated in the calendar year was utilized for each veteran.
Table 1.
Demographic characteristics.
| Characteristic | n (out of total population from 2011–2019) | % | |
|---|---|---|---|
| Sex | Female | 38,469 | 6.7 |
| Male | 535,925 | 93.3 | |
| Race | Black | 72,394 | 12.6 |
| White | 446,618 | 77.8 | |
| Mixed | 8,912 | 1.6 | |
| Other/unknown | 46,499 | 8.1 | |
| Marital status (first instance/y) | Married | 310,093 | 54.0 |
| Not married | 234,131 | 40.8 | |
| Unknown | 30,170 | 5.3 | |
| SMI (ever) | Overall SMI group | 22,487 | 3.9 |
| SZ | 10,607 | 1.8 | |
| Bipolar | 12,486 | 2.2 | |
| Dep | 1,748 | 0.3 | |
| Sleep (ever) | Overall sleep group | 83,030 | 14.5 |
| Breathing | 56,676 | 9.9 | |
| Circadian | 2,753 | 0.5 | |
| Hypersomnia | 397 | 0.1 | |
| Insomnia | 40,518 | 7.1 | |
| Movement | 4,930 | 0.9 | |
| Body systems (ever) | BS3 Endocrine | 353,239 | 78.4 |
| BS7 Circulatory | 330,009 | 73.2 | |
| BS8 Respiratory | 150,439 | 33.4 | |
| BS9 Digestive | 193,291 | 42.9 | |
| Mean | SD | ||
| Age (first instance/y) | 60.3 | 17.8 | |
Demographic characteristics are presented with the number and percentage of the veteran population within the 9-year period. SMI = serious mental illness, SZ = schizophrenia, Dep = major depression with psychosis.
Analyses
Consistent with previous reports on sleep disorder prevalence in VA health record data,25,26 prevalence rates for SMI and sleep disorders were calculated for each year of data such that the number of veterans in any year meeting criteria for the diagnostic category of interest was divided by the total number of eligible veterans receiving care in a VISN 4 facility in that year. Prevalence in each year was calculated for each SMI and sleep disorder diagnostic category. Additionally, prevalence of sleep disorders among veterans with SMI was calculated for each year of data. To examine absolute change in prevalence, we subtracted the relevant prevalence rate in 2011 from the prevalence rate in the year of interest. To compare prevalence in 2011 and 2019, we conducted a 2-sample proportion test. Lastly, we characterized veterans in 2019 (the most recent year of data) by demographic factors and comorbid conditions and examined changes in age and BMI year by year for veterans with SMI with and without comorbid sleep conditions. In 2019 data, we further examined statistically whether veterans with SMI with and without sleep disorders differed by sex, race, age, BMI, and presence of physical comorbidities using a series of chi-square and independent samples t tests. Findings were considered significant at P < .05. These methods were reviewed by a professional epidemiologist and deemed appropriate to enable conclusions regarding project aims (M. Y. Boudreaux-Kelly, personal communication, April 13, 2023).
RESULTS
Across the study period, 573,974 unique veterans received care in a VISN 4 facility and met inclusion criteria. Data from each veteran could have been included in one or multiple years; as such, yearly veteran samples were smaller than the total for the 9-year span and varied from year to year, with the sample sizes ranging from 245,132 in 2011 to 259,685 in 2019. See Table 1 for a demographic breakdown of the full veteran sample along with presence of SMI and sleep diagnoses and comorbid conditions.
In 2019, 4.0% of veterans were diagnosed with an SMI, and 21.8% of those veterans were also diagnosed with a sleep disorder. This is a significantly higher proportion than for those veterans without SMI, 15.1% of whom were diagnosed with a sleep disorder (x2 [2, n = 259,675] = 341.6, P < .001). Bipolar disorders were the most common form of SMI, diagnosed in 2.3% of veterans, followed by schizophrenia-spectrum disorders, diagnosed in 1.7% of veterans; major depressive disorder with psychosis was the least common SMI, diagnosed in only 0.2% of veterans in 2019. In the overall SMI group as well as more specific diagnostic groups, sleep-related breathing disorders were the most common sleep disorders, with prevalence rates ranging from 11.1% in veterans with schizophrenia-spectrum disorders to 23.2% in veterans with major depressive disorder with psychosis. Insomnia was the second most common sleep disorder, ranging from 8.1% in veterans with schizophrenia-spectrum disorders to 16.4% in veterans with major depressive disorder with psychosis. When rates of overall sleep diagnoses are compared between veterans with schizophrenia-spectrum disorders, bipolar disorders, and major depressive disorder with psychosis in 2019, results indicate that sleep disorders are diagnosed at significantly higher rates in veterans with major depressive disorder with psychosis (34.5%), followed by veterans with bipolar disorders (25.2%), and least commonly in veterans with schizophrenia-spectrum disorders (16.2%; x2 [2, n = 10,956] = 173.5, P < .001).
Regarding demographic factors, among veterans with SMI (n = 10,486) in 2019, White veterans (n = 7,363, 70.2%) were more likely to be diagnosed with sleep disorders than veterans identifying as a racial minority (n = 3,123, 29.8%; x2 [1, n = 10,486] = 4.5, P = .034); sleep disorder diagnoses did not differ between male (n = 9,009, 85.9%) and female (n = 1,477, 14.1%) veterans with SMI (x2 [1, n = 10,486] = 2.6, P = .109). In terms of age, veterans with SMI and sleep disorders were, on average, about 1 year younger (M = 56.8, SD = 12.7) than veterans with SMI without sleep disorders (M = 57.7, SD = 14.2; t(3,993) = –3.1, P = .002). Regarding comorbidities, in 2019, veterans with SMI who were diagnosed with sleep disorders had higher rates of comorbidities in endocrine (x2 [1, n = 10,486] = 297.1, P < .001), circulatory (x2 [1, n = 10,486] = 191.8, P < .001), respiratory (x2 [1, n = 10,486] = 144.0, P < .001), and digestive systems (x2 [1, n = 10,486] = 183.1, P < .001) than veterans with SMI without sleep disorders. Lastly, in 2019, veterans with SMI and sleep disorders had significantly higher BMI (M = 33.1, SD = 6.9) than veterans with SMI without sleep disorders (M = 29.3, SD = 6.0; t(3325.9) = 23.1, P < .001).
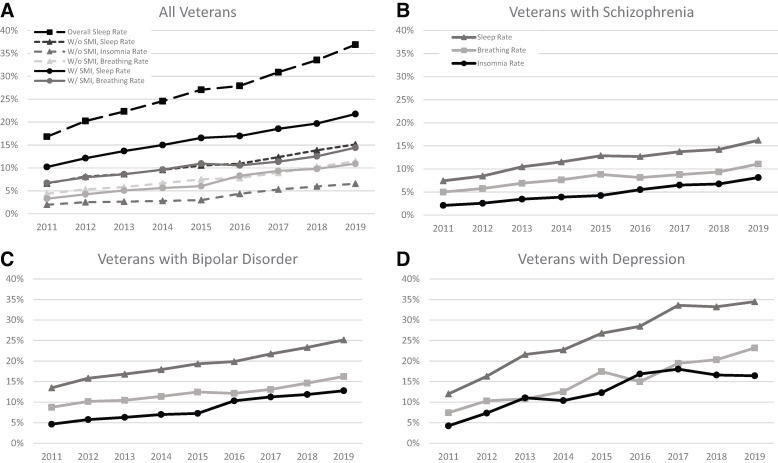
See Table 2 for prevalence rates of sleep disorders in veterans with SMI from 2011 to 2019. Overall, diagnoses of sleep disorders in this group in 2019 (21.8%) were more than double the rate in 2011 (10.2%; z = –22.4, P < .001). Across sleep disorder categories, similar increases in prevalence were seen year-by-year, as is represented in Figure 1A, though these increases are most notable for sleep-related breathing disorders and insomnia, with lower prevalence and smaller increases for circadian rhythm sleep-wake disorders, hypersomnias, and sleep-related movement disorders. Sleep-related breathing disorders were most prevalent across each year of data, followed by insomnia. Circadian rhythm sleep-wake disorders, hypersomnias, and sleep-related movement disorders were all relatively rare (rates from 0.02–1.22% across diagnoses and years). Similar patterns of increasing prevalence were seen across schizophrenia-spectrum disorders, bipolar disorders, and major depressive disorder with psychosis yearly from 2011 to 2019 (see Figure 1B, Figure 1C, and Figure 1D). Notably, increases in diagnoses of sleep disorders were also seen in veterans without SMI over this period, at relatively similar rates (ie, overall rate of sleep disorder diagnoses more than doubled during the study period; Figure 1A). While rates of sleep disorders were higher overall in veterans with SMI than in those without (21.8% vs 15.1% in 2019), veterans with schizophrenia-spectrum disorders are diagnosed with sleep disorders at a rate only marginally higher than veterans without SMI (16.2% vs 15.1% in 2019). Indeed, results suggest that veterans with schizophrenia-spectrum disorders have been diagnosed with sleep disorders at rates only 1% to 2% higher than veterans without any SMI consistently during the study period (schizophrenia-spectrum disorders range over time: 7.4–16.2%; non-SMI range: 6.6–15.1%). This is in contrast to veterans with bipolar disorders (range: 13.5–25.1%) and major depressive disorder with psychosis (range: 12.0–34.5%).
Table 2.
Yearly prevalence rates of sleep disorders in veterans with SMI.
| Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
| n | 245,132 | 257,878 | 257,041 | 257,231 | 258,158 | 258,142 | 258,523 | 259,682 | 259,685 |
| SMI group | 9,811 (4.0) | 10,537 (4.1) | 10,619 (4.1) | 10,758 (4.2) | 10,755 (4.2) | 10,129 (3.9) | 10,243 (4.0) | 10,312 (4.0) | 10,486 (4.0) |
| SMI and sleep (%) | 1,001 (10.2) | 1,278 (12.1) | 1,453 (13.7) | 1,613 (15.0) | 1,780 (16.6) | 1,719 (17.0) | 1,899 (18.5) | 2,030 (19.7) | 2,283 (21.8) |
| SMI and breathing (%) | 659 (6.7) | 837 (7.9) | 914 (8.6) | 1,035 (9.6) | 1,177 (10.9) | 1,069 (10.6) | 1,164 (11.4) | 1,293 (12.5) | 1,512 (14.4) |
| SMI and insomnia (%) | 322 (3.3) | 447 (4.2) | 538 (5.1) | 605 (5.6) | 648 (6.0) | 840 (8.3) | 958 (9.4) | 1,010 (9.8) | 1,145 (10.9) |
| SMI and movement (%) | 48 (0.5) | 58 (0.6) | 59 (0.6) | 49 (0.5) | 58 (0.5) | 73 (0.7) | 99 (1.0) | 103 (1.0) | 128 (1.2) |
| SMI and circadian (%) | 4 (0.0) | 2 (0.0) | 7 (0.1) | 8 (0.1) | 14 (0.1) | 27 (0.3) | 42 (0.4) | 62 (0.6) | 68 (0.7) |
| SMI and hypersomnia (%) | 4 (0.0) | 2 (0.0) | 3 (0.0) | 5 (0.1) | 7 (0.1) | 9 (0.1) | 19 (0.2) | 16 (0.2) | 19 (0.2) |
The number of veterans with corresponding diagnoses are presented as well as the yearly prevalence rates. SMI = serious mental illness.
Figure 1. Visualization of sleep disorder and SMI diagnoses by group year by year.
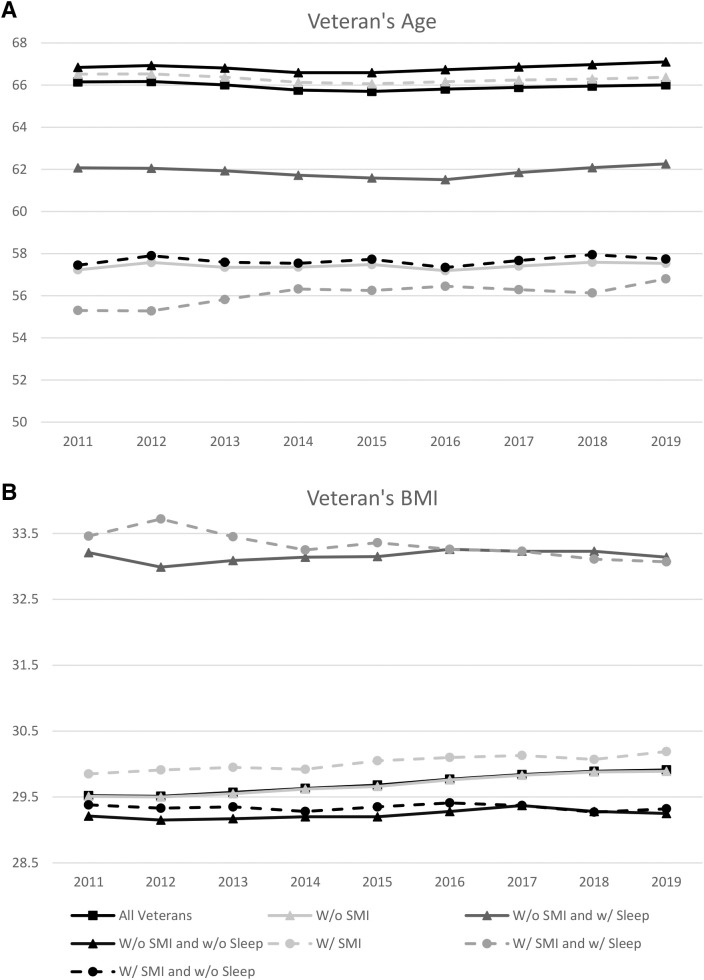
In examining the average age year-by-year, the average age of veterans with SMI was lower than the average age of all veterans (Figure 2A). Further, the average age of veterans with SMI and a sleep disorder was, on average, 1 to 2 years younger than those without sleep disorders. This pattern differs from that seen in veterans without SMI (Figure 2A), where the average age is similar to the average of all veterans, and those with a sleep disorder are 4 to 5 years younger than veterans without SMI and without a sleep disorder. Notably, veterans with SMI average 4 to 6 years younger than veterans without SMI but with sleep disorders.
Figure 2. Visualization of veterans’ age and BMI by group year by year.
Lastly, examination of BMI in veterans with and without SMI can be seen in Figure 2B. Trends are largely similar between these groups, with veterans with sleep disorders (with or without SMI) displaying the highest BMI (33+), while all other groups fall closer to the 29 to 30 range.
DISCUSSION
Results indicate that in 2019 VA VISN 4 health records, ∼22% of veterans with SMI were diagnosed with a sleep disorder, compared to ∼15% of veterans without SMI. Rates are highest among veterans with major depressive disorder with psychosis, followed by bipolar disorders and schizophrenia-spectrum disorders; veterans with schizophrenia-spectrum disorders are diagnosed at a rate near that of veterans without SMI. In the SMI group in 2019, breathing-related sleep disorders and insomnia were most commonly diagnosed, and those with a sleep disorder were more likely to exhibit comorbidities in endocrine, circulatory, respiratory, and digestive systems. Veterans with SMI and sleep disorders in 2019 were younger and had higher BMIs than veterans with SMI without sleep disorders. Lastly, and importantly, the overall prevalence of sleep disorders in veterans with SMI more than doubled from 2011 to 2019, suggesting improvements in the detection and diagnosis of sleep concerns for this group.
Our data indicate differences in the rates of diagnosed sleep disorders among veterans with schizophrenia-spectrum disorders, bipolar disorders, and major depressive disorder with psychosis. Veterans with major depressive disorder with psychosis were diagnosed at a rate approximately 10% higher than those with bipolar disorders, who were diagnosed at a rate nearly 10% higher than those with schizophrenia-spectrum disorders. These estimates align with findings from a meta-analysis examining the prevalence of obstructive sleep apnea in people with SMI—which found rates of 36% in major depressive disorder, 24% in bipolar disorders, and 15% in schizophrenia-spectrum disorders.27 While our data are examining sleep disorders more broadly (and our estimates for diagnosed sleep-related breathing disorders are considerably lower), the differences between groups follow the same pattern and are roughly equal intervals. This could suggest that sleep disorders occur less frequently in veterans with schizophrenia-spectrum disorders than in those with bipolar disorders and most frequently in veterans with major depressive disorder with psychosis. Indeed, sleep disturbance is a symptom of both bipolar and major depressive disorders.24 A large body of work links disruption in the circadian system to mood dysregulation,36 particularly for bipolar disorders,37 and some therapeutic approaches explicitly target the circadian system and/or sleep regularity to treat mood dysregulation with success.36 While the shared etiology of mood and sleep disorders is undoubtedly complex and in need of further research, several biological processes implicated in mood disorders are shared by those who experience circadian and sleep dysregulation.36 For example, prior work suggests altered serotonergic neurotransmission may play a role in both major depressive disorder and obstructive sleep apnea, potentially serving as a shared neurobiological pathway to the development of these disorders.27,38 Thus, sleep disorder prevalence may be higher in those with mood disorders, particularly those with prominent depressive symptoms.
However, recent transdiagnostic research examining clinically significant sleep disturbance in patients with schizophrenia-spectrum disorders and bipolar disorders suggests that these groups both endorse sleep disturbance (78% and 69%, respectively) at nearly double the rate of healthy control participants (39%).13 Indeed, ample work has established that people with schizophrenia-spectrum disorders experience sleep disturbance at a high rate9–11,13,16,17,39 and above typically reported prevalence rates for the general population.18 Furthermore, depression is common among those diagnosed with schizophrenia-spectrum disorders; up to 80% of people with these disorders experience clinically significant depressive symptoms over the course of the lifetime,40 and those with schizoaffective disorder (included here in our schizophrenia-spectrum disorder group) must endorse significant mood symptomatology meeting criteria for depressive and/or manic episodes.24 As such, given that the prevalence of sleep disorders for veterans with schizophrenia-spectrum disorders in our health record data is only marginally higher (∼1%) than in veterans without SMI, it is likely that sleep disorders are particularly underdiagnosed in this group.
There are several potential reasons for this possible underdiagnosis. First, providers may be more knowledgeable about sleep issues as potential comorbidities for those with mood disorders rather than schizophrenia-spectrum disorders or may be more likely to formally assess for sleep issues in this group. Importantly, sleep issues are included in the diagnostic criteria for both depression and mania,24 which likely increases discussions around sleep and chances for providers to note that sleep issues may be in need of additional treatment. Patients with schizophrenia-spectrum disorders who are experiencing more severe symptoms may also be at risk of having their sleep issues misconstrued by providers as secondary to disorder-specific symptomatology (eg, auditory or visual hallucinations), which may not be the case; indeed, research suggests that sleep disturbance and psychiatric symptomatology including psychosis can be bidirectionally influential, and untreated sleep problems may negatively influence psychotic symptoms.8,29 Patient-related factors likely also play a role in that patients may underreport sleep-related concerns, or misunderstandings in patient-provider communications may contribute to sleep concerns being missed.7 Further, sleep concerns are frequently reported by bed partners41; people with schizophrenia-spectrum disorders have live-in partners at a lower rate than those in the general population,42 which could contribute to underdiagnosis of sleep disorders in this group. Lastly, underdiagnosis in schizophrenia specifically may be related to inaccurate or stigmatizing views held by service providers, which can affect services provided to patients with schizophrenia-spectrum disorders.30 Indeed, a clinician survey of providers to patients with nonaffective psychosis found that providers frequently cited patients’ “lifestyle factors” as barriers to treatment, including perceived lack of motivation and capability to engage in sleep treatment,21 neither of which are borne out in the literature as patients with schizophrenia are able to engage in and benefit from sleep treatment.43 Of note, however, clinician surveys have primarily taken place in European countries and may not generalize to providers in the United States, so additional research is needed in this area. Overall, further work is needed to investigate how sleep concerns are discussed in health care visits for veterans with SMI and in particular for those with schizophrenia-spectrum disorders.
In a related finding, our results suggest that among veterans with SMI, those identifying as a racial minority are less frequently diagnosed with sleep disorders than White veterans. This is inconsistent with research suggesting that sleep disturbance may in fact be more prevalent among Black patients.44 Notably, health care disparities are widespread among racial minorities. Health care systems and individual providers are both contributing factors that can be shifted to better serve patients of color.45 Our results suggest particular work is needed to understand sleep diagnosis disparities in veterans with SMI and to improve diagnostic and intervention services in VA for this group. Other demographic and health-related findings were consistent with expectations; lower age in veterans with SMI is likely related to well-established findings suggesting premature mortality in this group as compared to the general population,46 with one recent study suggesting that adults with SMI may die an average of 6.3 years earlier than matched controls.47 Higher BMI is also associated both with use of certain antipsychotic medications48 and with diagnoses of sleep apnea49 and as such was an expected finding in our SMI and sleep groups.
Regarding year-by-year sleep disorder prevalence rates, the 2-fold increase in sleep disorders among veterans with SMI from 2011 to 2019 is consistent with past findings suggesting that sleep disorders are being diagnosed more frequently among the broader veteran population25,26 and that sleep apnea diagnoses have increased in veterans with SMI.19,20 While the increase in sleep diagnoses was surely influenced by a number of factors, given the 9-year span of this examination and numerous historical factors occurring during this time that may have influenced diagnostic trends (eg, transition from the fourth edition, text revision to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, changes in administrative requirements that could have affected the medical record, changes in funding for and/or emphasis on various mental and physical health conditions or treatments in the VA system), it is a positive change nonetheless. One factor that likely influenced the increase of diagnoses over time specific to this area is VA rollouts of diagnostic and treatment programs targeting obstructive sleep apnea (eg, home sleep apnea tests50,51) and insomnia (eg, cognitive behavioral therapy for insomnia34,51). Though we are unable to causally examine which factors were most influential, our data suggest that sleep-focused treatment rollouts are likely having positive impacts on awareness and diagnosis of sleep disorders in veterans with and without SMI, as well as accessibility of diagnostic services.52
This study has some limitations. Notably, rates of diagnosed sleep disorders presented here are likely underestimated across categories, as not all veterans are assessed for sleep disorders, and diagnoses are only assigned in the record if sleep concerns are discussed in clinical encounters and providers appropriately evaluate, diagnose, and document these concerns.25,26 This is a limitation of all medical records research. Further, we took a conservative approach to confirming diagnoses found in the health records, requiring at least 2 instances of a qualifying diagnosis within 390 days but at least 30 days apart, consistent with some past research.25,34 Our approach aligned with Alexander and colleagues25 and was more stringent than the study by Folmer and colleagues,26 which required only a single diagnosis for inclusion and resulted in notably higher prevalence rates than reported here. We further excluded parasomnias from our data and thus cannot comment on the prevalence of parasomnias in veterans with SMI. Additionally, we are unable to comment on diagnostic services or treatment received, as this analysis was limited to examination of diagnostic codes in the health record. Future work is needed to examine how veterans with SMI are treated for sleep concerns as compared to veterans without SMI.
Importantly, while this study has a large sample and several years of data, results may have limited generalizability outside of the VA system or for nonveterans. The Veterans Health Administration is a large, integrated health care system designed to serve a unique population at higher risk of multiple physical and mental comorbidities.53 Veterans who receive care at VA facilities, specifically, are also older, have lower socioeconomic status, and use greater health care resources than their non-VA veteran counterparts and the general population.53 Further, VA health care is paid unique attention by the media and is subject to policy changes that may accompany changes in government administration or focus areas. Despite this, in recent years studies suggest that wait times for VA care are the same as or better than community care,54,55 and veterans perceive a greater degree of integration and/or continuity of care in the VA system.56 These VA-specific factors may have influenced results of this study. More broadly, health record data are extremely complex and subject to changes in service provision trends and administrative procedures. While steps were taken to overcome limitations of these records where possible, based on the naturalistic design of this study, we cannot determine the cause of changes in prevalence rates year by year or know the extent to which sleep concerns were reported but not diagnosed by providers. We were also unable to examine a number of factors that may have influenced diagnostic outcomes, such as medication side effects, provider differences, and treatment-seeking behaviors. Despite these limitations, we believe this work represents an advance in our understanding of sleep diagnoses in a large, real-world medical setting for people with SMI.
In sum, our findings suggest that in VA VISN 4 health record data, nearly 22% of veterans with SMI were also diagnosed with a sleep disorder in 2019, and rates of sleep disorders for veterans with SMI have doubled since 2011. More work is needed to understand prevalence of sleep disorders between veterans with schizophrenia-spectrum disorders, bipolar disorders, and major depressive disorder with psychosis—and whether concerns brought up in treatment are perceived similarly by providers across groups or whether other factors might influence how sleep concerns are diagnosed and treated. Additionally, work is needed to investigate diagnostic differences between veterans who identify as a racial minority and White veterans with SMI. Lastly, future work should investigate how veterans with SMI are treated for sleep concerns in VA.
DISCLOSURE STATEMENT
All authors have seen and approve this manuscript. The authors report no conflicts of interest. Research reported in this article was funded by the Veterans Health Foundation through a Gerald Goldstein Early Career Mental Health Research Award (Co-PIs: Bonfils & Longenecker) and pilot project funds (PI: Bramoweth) from the Department of Veterans Affairs VISN 4 Mental Illness Research, Education, and Clinical Center (Director: David Oslin; Associate Director: Gretchen L. Haas). Additional support was provided to K. Bonfils by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number U54GM115428. Lastly, Dr. Tighe was supported by Career Development/Capacity Building Award Number IK2 RX003393 from the United States Department of Veterans Affairs Rehabilitation R&D Service. The content of this article is solely the responsibility of the authors and does not necessarily represent the views of the U.S. Department of Veterans Affairs, the National Institutes of Health, or the United States Government.
ACKNOWLEDGMENTS
The authors wish to express their appreciation to Jon Walker, PhD, and Monique Kelly, PhD, honest brokers who assisted with data collection from the health record for this work.
ABBREVIATIONS
- BMI
body mass index
- SMI
serious mental illness
- VA
Veterans Affairs
- VISN
Veteran Integrated Service Network
REFERENCES
- 1. Bowersox NW , Visnic S , McCarthy JF . Care for Veterans Health Administration Clients with Psychosis, FY2015: 17th Annual Report . Washington DC: : US Department of Veterans Affairs; ; 2016. . [Google Scholar]
- 2. Scott D , Happell B . The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness . Issues Ment Health Nurs. 2011. ; 32 ( 9 ): 589 – 597 . [DOI] [PubMed] [Google Scholar]
- 3. John A , McGregor J , Jones I , et al . Premature mortality among people with severe mental illness—new evidence from linked primary care data . Schizophr Res. 2018. ; 199 : 154 – 162 . [DOI] [PubMed] [Google Scholar]
- 4. Zulman DM , Chee CP , Wagner TH , et al . Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System . BMJ Open. 2015. ; 5 ( 4 ): e007771 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McCarthy JF , Blow FC , Valenstein M , et al . Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: evaluating accessibility and availability barriers . Health Serv Res. 2007. ; 42 ( 3 Pt 1 ): 1042 – 1060 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goldman LS . Medical illness in patients with schizophrenia . J Clin Psychiatry. 1999. ; 60 ( Suppl 21 ): 10 – 15 . [PubMed] [Google Scholar]
- 7. Bonfils KA , Fukui S , Adams EL , Hedrick HM , Salyers MP . Why are you here again? Concordance between consumers and providers about the primary concern in recurring psychiatric visits . Psychiatry Res. 2014. ; 220 ( 1–2 ): 541 – 548 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reeve S , Sheaves B , Freeman D . Sleep disorders in early psychosis: incidence, severity, and association with clinical symptoms . Schizophr Bull. 2019. ; 45 ( 2 ): 287 – 295 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kaskie RE , Graziano B , Ferrarelli F . Schizophrenia and sleep disorders: links, risks, and management challenges . Nat Sci Sleep. 2017. ; 9 : 227 – 239 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Klingaman EA , Palmer-Bacon J , Bennett ME , Rowland LM . Sleep disorders among people with schizophrenia: emerging research . Curr Psychiatry Rep. 2015. ; 17 ( 10 ): 79 . [DOI] [PubMed] [Google Scholar]
- 11. Li SX , Lam SP , Zhang J , et al . Sleep disturbances and suicide risk in an 8-year longitudinal study of schizophrenia-spectrum disorders . Sleep. 2016. ; 39 ( 6 ): 1275 – 1282 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yates NJ . Schizophrenia: the role of sleep and circadian rhythms in regulating dopamine and psychosis . Rev Neurosci. 2016. ; 27 ( 7 ): 669 – 687 . [DOI] [PubMed] [Google Scholar]
- 13. Laskemoen JF , Simonsen C , Büchmann C , et al . Sleep disturbances in schizophrenia spectrum and bipolar disorders—a transdiagnostic perspective . Compr Psychiatry. 2019. ; 91 : 6 – 12 . [DOI] [PubMed] [Google Scholar]
- 14. Laskemoen JF , Büchmann C , Barrett EA , et al . Do sleep disturbances contribute to cognitive impairments in schizophrenia spectrum and bipolar disorders? Eur Arch Psychiatry Clin Neurosci. 2020. ; 270 ( 6 ): 749 – 759 . [DOI] [PubMed] [Google Scholar]
- 15. Freeman D , Pugh K , Vorontsova N , Southgate L . Insomnia and paranoia . Schizophr Res. 2009. ; 108 ( 1–3 ): 280 – 284 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Palmese LB , DeGeorge PC , Ratliff JC , et al . Insomnia is frequent in schizophrenia and associated with night eating and obesity . Schizophr Res. 2011. ; 133 ( 1–3 ): 238 – 243 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Winkelman JW . Schizophrenia, obesity, and obstructive sleep apnea . J Clin Psychiatry. 2001. ; 62 ( 1 ): 8 – 11 . [DOI] [PubMed] [Google Scholar]
- 18. Grandner MA , Jackson NJ , Pigeon WR , Gooneratne NS , Patel NP . State and regional prevalence of sleep disturbance and daytime fatigue . J Clin Sleep Med. 2012. ; 8 ( 1 ): 77 – 86 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sharafkhaneh A , Giray N , Richardson P , Young T , Hirshkowitz M . Association of psychiatric disorders and sleep apnea in a large cohort . Sleep. 2005. ; 28 ( 11 ): 1405 – 1411 . [DOI] [PubMed] [Google Scholar]
- 20. Soreca I , Tighe CA , Bramoweth AD . The intersection of sleep apnea and severe mental illness in veterans . Psychosomatics. 2019. ; 60 ( 5 ): 481 – 487 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rehman A , Waite F , Sheaves B , Biello S , Freeman D , Gumley A . Clinician perceptions of sleep problems, and their treatment, in patients with non-affective psychosis . Psychosis. 2017. ; 9 ( 2 ): 129 – 139 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Manber R , Simpson N . Dissemination of CBT for insomnia . Curr Sleep Med Rep. 2016. ; 2 ( 3 ): 136 – 141 . [Google Scholar]
- 23. Rush T. LeardMann CA , Crum‐Cianflone NF . Obesity and associated adverse health outcomes among US military members and veterans: findings from the Millennium Cohort Study . Obesity (Silver Spring). 2016. ; 24 ( 7 ): 1582 – 1589 . [DOI] [PubMed] [Google Scholar]
- 24. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: : American Psychiatric Publishing; ; 2013. . [Google Scholar]
- 25. Alexander M , Ray MA , Hébert JR , et al . The National Veteran Sleep Disorder Study: descriptive epidemiology and secular trends, 2000–2010 . Sleep. 2016. ; 39 ( 7 ): 1399 – 1410 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Folmer RL , Smith CJ , Boudreau EA , et al . Prevalence and management of sleep disorders in the Veterans Health Administration . Sleep Med Rev. 2020. ; 54 : 101358 . [DOI] [PubMed] [Google Scholar]
- 27. Stubbs B , Vancampfort D , Veronese N , et al . The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: a systematic review and meta-analysis . J Affect Disord. 2016. ; 197 : 259 – 267 . [DOI] [PubMed] [Google Scholar]
- 28. Barrett EA , Aminoff SR , Simonsen C , Romm KL . Opening the curtains for better sleep in psychotic disorders—considerations for improving sleep treatment . Compr Psychiatry. 2020. ; 103 : 152207 . [DOI] [PubMed] [Google Scholar]
- 29. Waite F , Evans N , Myers E , et al . The patient experience of sleep problems and their treatment in the context of current delusions and hallucinations . Psychol Psychother. 2016. ; 89 ( 2 ): 181 – 193 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Corrigan PW , Mittal D , Reaves CM , et al . Mental health stigma and primary health care decisions . Psychiatry Res. 2014. ; 218 ( 1 ): 35 – 38 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mysliwiec V , Brock MS , Pruiksma KE , et al . A comprehensive evaluation of insomnia, obstructive sleep apnea and comorbid insomnia and obstructive sleep apnea in US military personnel . Sleep. 2022. ; 45 ( 12 ): zsac203 . [DOI] [PubMed] [Google Scholar]
- 32. World Health Organization . International Statistical Classification of Diseases and Related Health Problems. 9th ed. Geneva, Switzerland: : WHO; ; 1979. . [Google Scholar]
- 33. World Health Organization . International Statistical Classification of Diseases and Related Health Problems. 10th ed. Geneva, Switzerland: : WHO; ; 2016. . https://icd.who.int/browse10/2016/en . [Google Scholar]
- 34. Bramoweth AD , Tighe CA , Berlin GS . Insomnia and insomnia-related care in the Department of Veterans Affairs: an electronic health record analysis . Int J Environ Res Public Health. 2021. ; 18 ( 16 ): 8573 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. HCUP-US Tools & Software. https://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp . Accessed March 8, 2018. .
- 36. Scott MR , McClung CA . Circadian Rhythms in Mood Disorders . In: Circadian Clock in Brain Health and Disease . New York: : Springer International Publishing; ; 2021. : 153 – 168 . [Google Scholar]
- 37. Alloy LB , Ng TH , Titone MK , Boland EM . Circadian rhythm dysregulation in bipolar spectrum disorders . Curr Psychiatry Rep. 2017. ; 19 ( 4 ): 21 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schröder CM , O’Hara R . Depression and obstructive sleep apnea (OSA) . Ann Gen Psychiatry. 2005. ; 4 ( 1 ): 1 – 8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ferrarelli F . Sleep abnormalities in schizophrenia: state of the art and next steps . Am J Psychiatry. 2021. ; 178 ( 10 ): 903 – 913 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Upthegrove R , Marwaha S , Birchwood M . Depression and schizophrenia: cause, consequence, or trans-diagnostic issue? Schizophr Bull. 2017. ; 43 ( 2 ): 240 – 244 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Punjabi NM . The epidemiology of adult obstructive sleep apnea . Proc Am Thorac Soc. 2008. ; 5 ( 2 ): 136 – 143 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Agerbo E , Byrne M , Eaton WW , Mortensen PB . Marital and labor market status in the long run in schizophrenia . Arch Gen Psychiatry. 2004. ; 61 ( 1 ): 28 – 33 . [DOI] [PubMed] [Google Scholar]
- 43. Chiu VW , Ree M , Janca A , Iyyalol R , Dragovic M , Waters F . Sleep profiles and CBT-I response in schizophrenia and related psychoses . Psychiatry Res. 2018. ; 268 : 279 – 287 . [DOI] [PubMed] [Google Scholar]
- 44. Jehan S , Myers AK , Zizi F , et al . Sleep health disparity: the putative role of race, ethnicity and socioeconomic status . Sleep Med Disord. 2018. ; 2 ( 5 ): 127 – 133 . [PMC free article] [PubMed] [Google Scholar]
- 45. Alvidrez J , Castille D , Laude-Sharp M , Rosario A , Tabor D . The National Institute on Minority Health and Health Disparities research framework . Am J Public Health. 2019. ; 109 ( S1 ): S16 – S20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Olfson M , Gerhard T , Huang C , Crystal S , Stroup TS . Premature mortality among adults with schizophrenia in the United States . JAMA Psychiatry. 2015. ; 72 ( 12 ): 1172 – 1181 . [DOI] [PubMed] [Google Scholar]
- 47. Iturralde E , Slama N , Kline-Simon AH , Young-Wolff KC , Mordecai D , Sterling SA . Premature mortality associated with severe mental illness or substance use disorder in an integrated health care system . Gen Hosp Psychiatry. 2021. ; 68 : 1 – 6 . [DOI] [PubMed] [Google Scholar]
- 48. Rojo LE , Gaspar PA , Silva H , et al . Metabolic syndrome and obesity among users of second generation antipsychotics: a global challenge for modern psychopharmacology . Pharmacol Res. 2015. ; 101 : 74 – 85 . [DOI] [PubMed] [Google Scholar]
- 49. Gami AS , Caples SM , Somers VK . Obesity and obstructive sleep apnea . Endocrinol Metab Clin. 2003. ; 32 ( 4 ): 869 – 894 . [DOI] [PubMed] [Google Scholar]
- 50. Cairns A , Sarmiento K , Bogan R . Utility of home sleep apnea testing in high-risk veterans . Sleep Breath. 2017. ; 21 ( 3 ): 647 – 655 . [DOI] [PubMed] [Google Scholar]
- 51. Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea Work Group . VA/DoD Clinical Practice Guideline for the Management of Chronic Insomnia Disorder and Obstructive Sleep APNEA , Washington DC: : US Department of Veterans Affairs; ; 2019. . [Google Scholar]
- 52. Flemons WW , Douglas NJ , Kuna ST , Rodenstein DO , Wheatley J . Access to diagnosis and treatment of patients with suspected sleep apnea . Am J Respir Crit Care Med. 2004. ; 169 ( 6 ): 668 – 672 . [DOI] [PubMed] [Google Scholar]
- 53. Agha Z , Lofgren RP , VanRuiswyk JV , Layde PM . Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use . Arch Intern Med. 2000. ; 160 ( 21 ): 3252 – 3257 . [DOI] [PubMed] [Google Scholar]
- 54. Griffith KN , Ndugga NJ , Pizer SD . Appointment wait times for specialty care in Veterans Health Administration facilities vs community medical centers . JAMA Netw Open. 2020. ; 3 ( 8 ): e2014313 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Penn M , Bhatnagar S , Kuy S , et al . Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers . JAMA Netw Open. 2019. ; 2 ( 1 ): e187096 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Vanneman ME , Wagner TH , Shwartz M , et al . Veterans’ experiences with outpatient care: comparing the Veterans Affairs system with community-based care: study compares veterans’ experiences in VA-delivered and community-based outpatient care . Health Aff (Millwood). 2020. ; 39 ( 8 ): 1368 – 1376 . [DOI] [PMC free article] [PubMed] [Google Scholar]