Abstract
Objectives
In psoriatic arthritis (PsA), self-management is important for patient function and quality of life. Behaviour change can be difficult, patients could benefit from high-quality support to initiate change. Our aim was to codesign the project as theory-informed, evidence-based, patient-focused, materials supporting healthy lifestyle changes for patients diagnosed with PsA.
Methods
Development of the materials was overseen by a steering group of patients with PsA, psychologists, rheumatologists, a design team and researchers. First, a literature review was performed to establish the evidence base for behaviours and potential interventions in PsA, including diet, weight, alcohol, smoking, exercise, anxiety, depression and stress. An initial roundtable of patients with PsA prioritised areas and content ideas. Draft materials including a website and downloadable materials were produced. A second roundtable of patients with PsA collected feedback on the draft content and design. A third roundtable was held with patients with PsA and a fourth with clinicians to refine the materials and ensuring that they were evidence based, accessible, interesting, and helpful to initiate and maintain change. A final evaluation survey was performed to review the draft website before launching the final materials.
Results
15 candidate topics were prioritised. A website and set of postcards summarising the topics were developed by the design team and refined following feedback from the roundtable groups.
Conclusion
This project created patient-focused resources to support behaviour change. It addresses common concerns of patients with PsA about how they may optimise their health by providing practical and brief interventions to challenge and support them to make changes.
Keywords: psoriatic arthritis, patient reported outcome measures, psychology
WHAT IS ALREADY KNOWN ON THIS TOPIC
There is a lack of evidence to support how best to manage the psychological and physical concerns of patients living with psoriatic arthritis (PsA).
WHAT THIS STUDY ADDS
This project created patient-focused materials and a website designed for use in clinical practice. They address the common concerns of patients living with PsA and provide information about how they may be able to optimise their health by using these practical and brief interventions to challenge them to make personal change/s.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Future research is needed to test the impact of the resource.
Introduction
Around 3% of the population will develop psoriasis, the inflammatory skin condition.1 Some 15%–30% of people with psoriasis will develop psoriatic arthritis (PsA).2 PsA can present with a range of signs and symptoms, including assorted musculoskeletal manifestations. PsA is associated with other conditions that can have a negative impact on quality of life, including depression, metabolic syndrome and increased cardiovascular disease risk.3–5 In addition, patients living with (PsA) are at greater risk of being overweight, sedentary consuming alcohol above recommended levels, smoking, reporting poor sleep, fatigue and anxiety.6 7 Without modification (and they may be modifiable), these health behaviours further increase cardiovascular morbidity and mortality risk.3–5
Given the complexity of PsA, it is critical that those living with it are supported to self-manage. Self-management aims to empower and enhance peoples’ well-being. It puts an emphasis on sharing the responsibility for management of a condition between healthcare professionals and the individual. Supporting people to self-manage enables people with long-term conditions to live well and can reduce peoples’ need for using health services.8
Our understanding about how patients who live with PsA manage and cope with their condition remains limited,9 and evidence of how best to support and manage the psychological and physical concerns of patients living with PsA is lacking. Osborne et al proposed that self-management is most effective when closely aligned to clinical practice.10 For patients living with PsA, such management where possible should strongly involve the combination of the patient, the patient’s PsA healthcare team, the patients’ families and friends.11 The evidence base for effective healthcare professional led interventions to change behaviour is extremely limited. However, there is evidence that behaviour change interventions can support non-pharmacological management for other types of arthritis and improve outcomes.12 13
We aimed to identify what was already known about the health behaviours of patients living with PsA and used behaviour change theories, literature and expert insight to develop resources to support patients living with PsA and their clinicians to encourage change. The learning resources created were developed with patients living with PsA, clinicians, researchers and psychologists and designed to be distributed to clinicians and patients to address these lifestyle issues. In the absence of a strong evidence base for healthcare professional led interventions to change behaviour in PsA, evidence-based self-management strategies were used from other long-term conditions, for example, motivational interviewing techniques for improving outcomes in long-term conditions, including physical activity, reducing alcohol use and weight loss.14–17
Methods
Our process followed six steps; these are illustrated in figure 1. The development of the materials was overseen by a steering group of patients living with PsA, psychologists, rheumatologists and researchers in the UK who also formed the author group (LoH, LaH, CB, SK, SM, DO, IS, MS, LCC). There was wider stakeholder involvement from public contributors living with PsA and clinicians at various stages of design. The steering group chair (LCC) oversaw the process to ensure accountability and transparency. The steering group ran as a collaborative effort between the patients with a lived experience of the disease and those who care for them.
Figure 1.

Flowchart of resource development process.
Scope
The planned scope of the project was adult PsA. It did not extend into PsA in childhood as this is commonly considered as a subtype within juvenile idiopathic arthritis and children may have different needs than adults.
User involvement
Patient involvement was central to the project. From the design, through all stages, to conclusion. Involvement of people affected by PsA was key to ensuring the relevance and quality of project. Steering group, Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) patient research partners included those with lived experience of PsA (DO and IS). Patient and public contributors involved in the roundtable groups were recruited through the GRAPPA network and patient support groups as well as social media and snowballing through these groups. Three of the four roundtables and the final evaluation survey included design input from patients with lived experience of PsA. Patient and public involvement in the project followed good practice based, on guidance from the UK Standards for Public Involvement and National Institute for Healthcare Research. For example, for payments and recognition of involvement.18 19 Clinicians directly involved in PsA care were recruited through specialist interest groups for health professionals and the GRAPPA Network/British Psoriatic Arthritis ConsorTium (Brit-PACT).
Project methods
Step 1: Literature review
A review of the literature examined the evidence for the current burden of diet, weight, alcohol, smoking, exercise, anxiety, depression, and stress in PsA. The review also aimed to identify evidence for any interventions and the success of these (eg, weight loss in patients with stable PsA). All members of the steering group including the patient research partners were involved in identifying topics and relevant search terms for each topic.
Step 2: Engagement forum
A patient engagement forum established priorities for the project. In December 2020, an initial roundtable group of patients living with PsA was led by steering group members (LCC, LoH, LaH, CB) to identify priority behaviours and ideas for content. LaH and CB welcomed the patients to the group and used their experience as psychologists to create a safe space for patients to feel comfortable to discuss and disclose their experiences and opinions on the topics. This enabled the patients to feel as comfortable as possible when discussing potentially sensitive issues such as intimacy. The patients were reassured they only needed to share their views on what they felt happy disclosing. DOS and IS observed the groups. The literature review results were presented. The contributors were then asked to provide feedback and insight into the topics they felt were most important, suggest any additional missing topics and help generate ideas around the information they would hope to see that included in the final materials.
Step 3: Development of content
The psychologists (CB and LaH) designed the materials to be compatible with the motivational interviewing stages and used theCapability, Opportunity, Motivation – changing Behaviour model (COM-B) to articulate how the intervention design targeted the three drivers of behaviour: capability, opportunity and motivation. Table 1 provides a summary of the psychologically informed design features used.20–22
Table 1.
Summary of the psychologically informed design features
| COM-B component | Design features |
| Physical capability | n/a |
| Psychological capability |
|
| Physical opportunity |
|
| Social opportunity | n/a |
| Reflective motivation |
|
| Automatic motivation |
|
Step 4: Resource design
The steering group partnered with a design agency to translate the information and topics into engaging materials using good health literacy principles. The design team created a draft website and downloadable postcards. In June 2021, a second roundtable group comprising PsA patients was setup. This enabled the patients to provide their views on the draft content of the materials, including the design, website name/logo and layout of the resources and website. The steering group refined their work based on same.
Step 5: User feedback
Following the design and production of the materials, there was a two-stage evaluation, from two round table group interviews and surveys, conducted by steering group members MS and SM. Between July 2021 and August 2021, two separate group interviews/focus groups were conducted with patients living with PsA and clinicians using qualitative interview methods to evaluate the materials and ensure that they were accessible, interesting and helpful to initiate and maintain change. Participants were paid for their time to review static elements of the website prototype and discuss questions about the proposed website in a group interview. Critical feedback from each group was used to refine the final materials and website where possible.
The user feedback survey was then performed to review the functional website prototype before launch. It ran for 6 weeks from 12 January 2022. Two paid surveys were developed on the platform Qualtrics—one for clinicians who work with patients living with PsA and one for patients living with PsA. The survey used scale/rank questions, followed by open ended questions to determine usability, acceptability of design and content, with questions asking about recommendation to a friend/family, and whether they were considering making health behaviour changes after looking at the resource. It included both positives/benefits and any major barriers/challenges to use,which could also inform future research.
Step 6: Dissemination
To ensure the outputs from the project got to the people who need to make use of them (patients, public members and healthcare professionals) as quickly as possible and to maximise the benefits of the new resources the steering group worked closely with patient and clinician groups to promote them. A launch campaign was created and used by the groups involved on social media.
Results
Literature review
The literature review to inform the outputs of this project combined a number of different phases. An initial literature search, combining terms for patient behaviours or lifestyle and PsA and focused on retrieving systematic reviews, was conducted in MEDLINE (via OVID) on 17 November 2020. The purpose of this search was to inform the initial topics list that was discussed during the focus groups held in December 2020. A copy of the search strategy is found in online supplemental table S1. Following the focus groups, and building on the initial MEDLINE search strategy, revised and expanded search strategies were developed (not restricted by publication type) and were run in the Cochrane Central Register of Controlled Trials (CENTRAL) (via Cochrane Library, Wiley), CINAHL (via EBSCOhost), AMED (via OVID), EMBASE (via OVID), Global Health (via OVID), MEDLINE (via OVID), PsycINFO (via OVID) on the 28 May 2021. The search results, from 17 November 2020 and the 28 May 2021, combined with the use of backward citation searching of identified references and known references obtained from experts in the steering group all informed the development of the project materials. Where guideline or systematic review-level evidence was not available for a topic, the best available evidence identified was used along with expert knowledge. A copy of the search strategies for all the databases searched on 28 May 2021 is found in online supplemental table S1.
rmdopen-2023-003190supp001.pdf (193.3KB, pdf)
Engagement forum
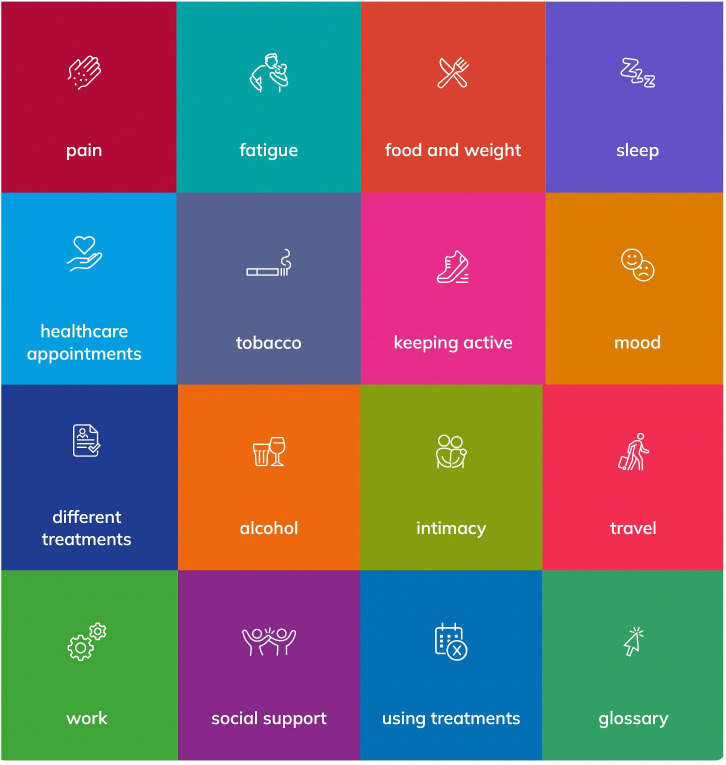
Table 2 details the concept development roundtable groups that were conducted. The PsA groups comprised of a mix of age groups, backgrounds and stages of PsA. These discussions probed for increased understanding, acceptability and views on the value of these new materials as part of self-management and as part of high-quality clinical care. Also, suggestions were given on the topic, content for materials, naming the website and the types of materials (eg, postcards). Suggestions for topics from the focus groups were added to the literature review. Following the steering group and roundtable input, 15 candidate topics were prioritised. The topics emerging from the roundtable groups are listed in table 3. A draft website and downloadable postcards summarising each of the topics was developed by the design team and refined following feedback from the roundtable groups and steering group. The website developed as part of the resources is called ‘informatree’. Figure 2 shows an example of how the topics are represented on the informatree website.
Table 2.
Round table groups
| Group number | Purpose of group | Contributors involved | Number of people | Date of group |
| Roundtable 1 | Concept development | Patients living with PsA | 14 (run as two sessions with 6 and 8 people) | December 2020 |
| Roundtable 2 | Concept development | Patients living with PsA | 10 | June 2021 |
| Roundtable 3 | User evaluation | Patients living with PsA | 5 | July 2021 |
| Roundtable 4 | User evaluation | Clinicians | 5 | August 2021 |
PsA, psoriatic arthritis.
Table 3.
Resource topics
| Topics | |
| 1 | Pain |
| 2 | Fatigue |
| 3 | Healthcare appointments |
| 4 | Tobacco |
| 5 | Different treatments |
| 6 | Alcohol |
| 7 | Work |
| 8 | Social support |
| 9 | Food and weight |
| 10 | Sleep |
| 11 | Keeping active |
| 12 | Mood |
| 13 | Intimacy |
| 14 | Travel |
| 15 | Using treatments |
Figure 2.
Example of topics from informatree website. The topics are shown as they are represented on the website and the order is not intended to imply the priority of any given topic over another.
User feedback
Table 2 details the user evaluation roundtable groups. Key messages from the evaluation group interviews with clinicians and patients living with PsA included suggested changes to the design, colours and functionality of informatree as well as specific feedback on the content of topics. For example, suggestions included changes to the language on the smoking and pain topics—with participants highlighting the important of rest and an empathetic tone. It was felt that the information on informatree had a basic level of information and could be useful for those newly diagnosed. Feedback included suggested improvements on the design, colours and wording on the resource. An example of the postcard for ‘keeping active’ is found in figure 3. The speech bubbles used in the resources were written in the first person and capture tips and advice provided by patients during coproduction of the content. These were either provided as direct quotes from individuals or ideas that were paraphrased for clarity of message and anonymity.
Figure 3.
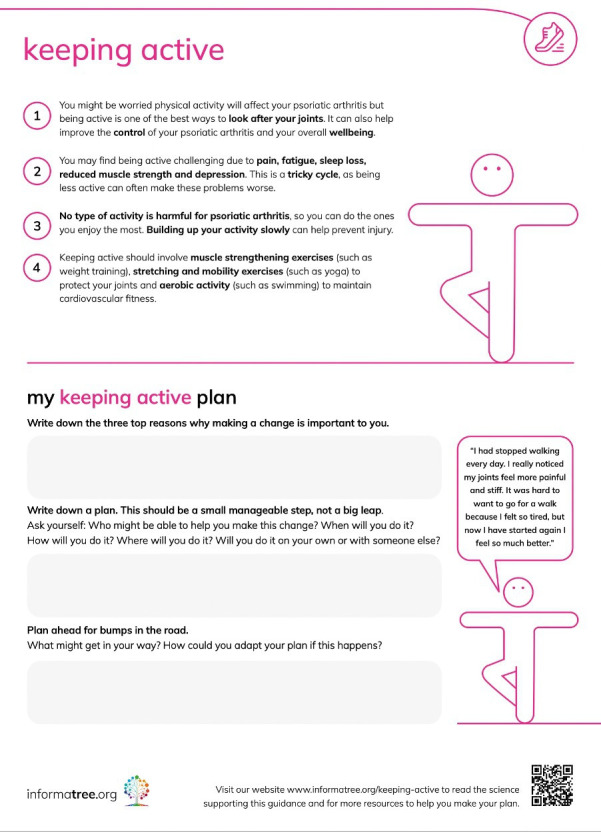
Example of downloadable postcard for keeping active topic.
The user feedback survey had a target number of 50 respondents. There were 14 responses from clinicians and 62 responses from patients (n=76) to the user feedback survey. Findings from the patients living with PsA survey supported this with 95% (n=59) identifying with the information on the website and would recommend it to friends, family or someone newly diagnosed with PsA. Ninety-eight per cent (n=61) of patients living with PsA felt they would be ready to make change compared with before reading the materials. Similarly, 93% (n=13) of clinicians who responded agreed that it covered the information their patients were interested in and that they would be able to identify with the information on the website. Eighty per cent (n=12) clinicians agreed that they would recommend this website to patients newly diagnosed, or with known PsA. Fifty per cent (n=7) of clinicians felt that the resources covered the right amount of depth, 30% (n=4) disagreed and 20% (n=3) neither agreed or disagreed.
The materials developed during the project are available (free of charge) for download as PDFs from the informatree website https://www.informatree.org and via the GRAPPA Network and Brit-PACT websites. They have also been promoted by the team and partner organisations including, the International Federation of Psoriatic disease Associations, the Psoriasis Association and Psoriasis and Psoriatic Arthritis Alliance. The postcards can also be printed from high-resolution PDFs to distribute to clinicians, thus aiding self-management links to clinical care.
Discussion
The advice offered in this resource was based on the most up-to-date evidence and information available and was consistent with best practice for providing health information on behaviour change. The resources give an overview of the current non-pharmacological interventions for PsA although against a growing but limited evidence base. Where available, clear links to the evidence resources were provided within the web resource. Where high-quality evidence was not available, the recommendations were based on clinical expertise and the experience of patients living with PsA.
There was a high level of patient and expert involvement in this initiative. All the key clinical (doctors, nurses and allied health professionals involved in caring for patients with PsA) and patient charity groups involved in the care of PsA in the UK were involved and patients with lived experience of PsA, and their carer’s, were included at every stage.
A limitation of the project was that the limited high-quality evidence base established by the literature review meant that there was often no or very limited evidence to base the resources on, and the steering group had to defer to expert opinion from within the steering group or use lower quality evidence. Although the resources created address common concerns of patients living with PsA, future research is needed to test the impact of the resource in clinical practice. The lack of available high-quality evidence to support effective methods for addressing lifestyle/behaviour change and patient self-management support to guide healthcare professionally led interventions in the clinical setting calls for additional research in this area.
The final resources created were produced in the English language. They have not been translated into other languages. They are intended to be used within the UK. While the authors acknowledge that even within the UK, translation into other languages may be helpful for non-English-speaking patients and communities to ensure they understand the information accurately. Unfortunately, this was not possible within the scope of this project. The resources can still be translated into other languages. However, if translated care would need to be given with the process to ensure the medical ‘jargon’ and wording is translated accurately and safely to make sense for the intended patients.
A potential weakness of this project is that the website is not a living document and the information provided in the resource was accurate up to May 2021. However, the project evaluation also highlighted the need for further in-depth research on the emotional and mental health aspects of living with PsA, which means that additions to the website in the future could be possible in future reviews.
In conclusion, this project has used a codesign approach to identify areas of unmet need, prioritised by patient and clinician groups, and to create resources to support individuals living with PsA.
Acknowledgments
We acknowledge the patients with PsA and healthcare professionals who helped shape the resources by promoting and participating in the roundtable groups and final evaluation survey including our partner organisations the Psoriasis Association, the Psoriasis and Psoriatic Arthritis Alliance and International Federation of Psoriasis Associations.
Footnotes
Twitter: @drlauracoates
Contributors: LoH: study design, literature search, figures, data collection and interpretation (engagement forum, resource creation and design, user feedback), writing—original and editing. LaH: study design, data collection and interpretation (engagement forum, resource creation and design, user feedback), writing—review and editing. CB: Study design, data collection and interpretation (engagement forum, resource creation and design, user feedback), writing—review and editing. SK: study design, literature search, writing—original draft and editing. SM: study design, literature search, data collection and interpretation (resource design, user feedback), writing—review and editing. DO'S: Study design, literature search, data interpretation (engagement forum, resource design, user feedback) writing—review and editing. IS: Study design, literature search, data interpretation (engagement forum, resource design, user feedback) writing—review and editing. MS: Study design, literature search, data collection and interpretation (resource design, user feedback), writing—review and editing. LCC: funding acquisition, study design, (engagement forum, resource creation and design, user feedback), writing—original draft and editing.
Funding: This project was funded by an independent Medical Education Grant from Pfizer. No conflicts of interest were envisaged where Pfizer could potentially benefit from the results of the project. SK was funded by Cancer Research UK (grant C49297/A27294).
Competing interests: LoH: none declared, CB has received funds for research and honoraria from the following pharmaceutical companies: Abbvie, Almirall, Amgen (was Celgene), Beiersdorf, Janssen, Novartis, Pfizer, UCB., LaH received consultancy fees from the University of Oxford for this work, SK: none declared, SM: none declared, DO: none declared, IS: none declared, MS: none declared, LCC has been paid as a speaker for AbbVie, Amgen, Biogen, Celgene, Eli Lilly, Galapagos, Gilead, GSK, Janssen, Medac, Novartis, Pfizer and UCB. LCC has worked as a paid consultant for AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Eli Lilly, Gilead, Galapagos, Janssen, Moonlake, Novartis, Pfizer and UCB., LCC has received grants/research support from AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Novartis, Pfizer and UCB. LCC is a member of the RMD Editorial board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was not sought for this project as the patient and public were involved solely in involvement activities. Their involvement informed the design of project (for example, the search strategy) and their opinions helped to co-produce the final materials. The Research Services Department at the University of Oxford were consulted and advised user feedback evaluation did not need ethical approval.
References
- 1.Coates LC, Savage L, Waxman R, et al. Comparison of screening questionnaires to identify Psoriatic arthritis in a primary-care population: a cross-sectional study. Br J Dermatol 2016;175:542–8. 10.1111/bjd.14604 [DOI] [PubMed] [Google Scholar]
- 2.Mease PJ, Gladman DD, Papp KA, et al. Prevalence of Rheumatologist-diagnosed Psoriatic arthritis in patients with psoriasis in European/North American Dermatology clinics. J Am Acad Dermatol 2013;69:729–35. 10.1016/j.jaad.2013.07.023 [DOI] [PubMed] [Google Scholar]
- 3.Peters MJ, van der Horst-Bruinsma IE, Dijkmans BA, et al. Cardiovascular risk profile of patients with Spondylarthropathies, particularly Ankylosing Spondylitis and Psoriatic arthritis. Semin Arthritis Rheum 2004;34:585–92. 10.1016/j.semarthrit.2004.07.010 [DOI] [PubMed] [Google Scholar]
- 4.Husted JA, Thavaneswaran A, Chandran V, et al. Cardiovascular and other Comorbidities in patients with Psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res (Hoboken) 2011;63:1729–35. 10.1002/acr.20627 [DOI] [PubMed] [Google Scholar]
- 5.Gisondi P, Tessari G, Conti A, et al. Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study. Br J Dermatol 2007;157:68–73. 10.1111/j.1365-2133.2007.07986.x [DOI] [PubMed] [Google Scholar]
- 6.Nowowiejska J, Baran A, Flisiak I. Mutual relationship between sleep disorders, quality of life and Psychosocial aspects in patients with psoriasis. Front Psychiatry 2021;12:674460. 10.3389/fpsyt.2021.674460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta S, Syrimi Z, Hughes DM, et al. Comorbidities in Psoriatic arthritis: a systematic review and meta-analysis. Rheumatol Int 2021;41:275–84. 10.1007/s00296-020-04775-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morgan HM, Entwistle VA, Cribb A, et al. We need to talk about purpose: a critical interpretive synthesis of health and social care professionals' approaches to self-management support for people with long-term conditions. Health Expect 2017;20:243–59. 10.1111/hex.12453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howells L, Chisholm A, Cotterill S, et al. Impact of disease severity, illness beliefs, and coping strategies on outcomes in Psoriatic arthritis. Arthritis Care Res (Hoboken) 2018;70:295–302. 10.1002/acr.23330 [DOI] [PubMed] [Google Scholar]
- 10.Osborne RH, Jordan JE, Rogers A. A critical look at the role of self-management for people with arthritis and other chronic diseases. Nat Clin Pract Rheumatol 2008;4:224–5. 10.1038/ncprheum0765 [DOI] [PubMed] [Google Scholar]
- 11.Husni ME, Merola JF, Davin S. The Psychosocial burden of Psoriatic arthritis. Semin Arthritis Rheum 2017;47:351–60. 10.1016/j.semarthrit.2017.05.010 [DOI] [PubMed] [Google Scholar]
- 12.Larkin L, Gallagher S, Cramp F, et al. Behaviour change interventions to promote physical activity in rheumatoid arthritis: a systematic review. Rheumatol Int 2015;35:1631–40. 10.1007/s00296-015-3292-3 [DOI] [PubMed] [Google Scholar]
- 13.Marques A, Santos E, Nikiphorou E, et al. Effectiveness of self-management interventions in inflammatory arthritis: a systematic review informing the 2021 EULAR recommendations for the implementation of self-management strategies in patients with inflammatory arthritis. RMD Open 2021;7:e001647. 10.1136/rmdopen-2021-001647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Georgopoulou S, Prothero L, Lempp H, et al. Motivational interviewing: relevance in the treatment of rheumatoid arthritis Rheumatology (Oxford) 2016;55:1348–56. 10.1093/rheumatology/kev379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilbert AL, Lee J, Ehrlich-Jones L, et al. A randomized trial of a motivational interviewing intervention to increase lifestyle physical activity and improve self-reported function in adults with arthritis. Semin Arthritis Rheum 2018;47:732–40. 10.1016/j.semarthrit.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mbuagbaw L, Ye C, Thabane L. Motivational interviewing for improving outcomes in youth living with HIV. Cochrane Database Syst Rev 2012:CD009748. 10.1002/14651858.CD009748.pub2 [DOI] [PubMed] [Google Scholar]
- 17.West DS, DiLillo V, Bursac Z, et al. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care 2007;30:1081–7. 10.2337/dc06-1966 [DOI] [PubMed] [Google Scholar]
- 18.Involvement USfP . UK standards for public involvement. n.d. Available: https://sites.google.com/nihr.ac.uk/pi-standards/home
- 19.Research NIfH . PPI (patient and public involvement) resources for applicants to NIHR research programmes. n.d. Available: https://www.nihr.ac.uk/documents/ppi-patient-and-public-involvement-resources-for-applicants-to-nihr-research-programmes/23437#resources-for-ppi
- 20.Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions, 1st edn. Great Britain: Silverback Publishing, 2014. [Google Scholar]
- 21.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for Characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller W, Rollnick S. Motivational interviewing third edition: helping people change. New York: Guilford, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2023-003190supp001.pdf (193.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request.