Abstract:
Customized photorefractive keratectomy with minimal tissue ablation combined with corneal cross-linking seems to be a long-term safe and effective strategy for anatomical and visual management of keratoconus, postsurgical ectasia, and other ectasia management. Multiple published studies, many with long-term follow-up, have supported the Athens Protocol and its various forms as a means to manage corneal ectatic disorders, which not only stabilize corneal shapes but also improve functional vision.
Key Words: ectasia, keratoconus, corneal cross-linking, excimer ablation, PRK, Athens Protocol
Over the past 2 decades, corneal cross-linking (CXL) has emerged to become the predominant intervention strategy for corneal stabilization in keratoconus and other ectasia disorders.1,2 However, visual rehabilitation, even in cases stabilized by CXL, has proven challenging, especially in patients unable to be fitted or to tolerate contact lenses. However, as CXL offered promise for long-term arrest of keratoconus progression, speculation arose whether such post-CXL stability might then also enable refractive excimer laser intervention.1 Initially, customized excimer laser surface ablation was used sequentially at 6 months to a year after CXL, thereby aiming to improve visual function through improving corneal curvature asymmetry and irregularity.3,4
Subsequently, attempts were made to combine ectasia-stabilizing CXL with excimer corneal reshaping procedures in the same treatment session.6–9 In the initial reports, surface excimer ablation was described as photorefractive keratectomy (PRK) but in essence served more as phototherapeutic keratectomy (PTK), customized to regularize the ectasia-induced corneal refractive irregularity changes.4,5
Subsequent publications documented that visual function improved whether these 2 procedures were performed sequentially or at the same sitting.7 This combined PRK-CXL technique, termed “the Athens Protocol”, specifically aimed to structurally stabilize and refractively optimize the 5-mm zone of the central anterior cornea,9 seeking to reduce irregular astigmatism and central refractive coma. This strategy has proven pivotal in improvement of uncorrected and corrected distance visual acuity (UDVA and spectacle CDVA, respectively), as well as reduction of keratometric asymmetry indices.10 Several peer reviewed studies have now reported outcomes of the original or modified version of the Athens Protocol with similar stabilization and visual function improvement ranging from short-term to over a decade of follow-up (Table 1).10–15
TABLE 1.
Compilation of a Large Group22 of Publications Documenting Clinical Data of Keratoconus Treatment With Combined Customized Surface Ablation and Corneal Cross-linking, Some With Very Long-Term Follow-Up
| Reference | Authors | Year | Protocol | Study Design | Cases | Follow-Up | UDVA | CDVA | SE | Keratometry Change | Complications |
| 3 | Wong JJ, et al | 2006 | Topo-PRK + CXL sequential | Case series | 7 | 12 m | 20/100–20/30 | 20/50–20/22 | 2.14 D | Kmax reduced 3 D | None |
| 4 | Kanellopoulos AJ, et al | 2007 | Topo-PRK + CXL sequential | Case report | 1 | 18 m | 20/100–20/20 | 20/50–20/15 | 5.25 D | Steep K reduced 5.5 D | None |
| 6 | Ewald M, et al | 2008 | Topo-PRK + CXL | Case series | 45 | 19 m | 20/400–20/100 | 27/32 >2.25 logMAR | 6.4 D | 53 D to 44 D (9 D) | 1 case PK |
| 7 | Kanellopoulos AJ, | 2009 | Topo-PRK + CXL | Comp. Case series | 198 | 36 m | 0.96–0.3 | 0.39–0.16 | 3.2 D | 3.5 D flatten | 2 cases haze |
| 13 | Kymionis GD, et al | 2009 | Topo-PRK + CXL | Case series | 23 | 24–48 m | Improved 0.38 | Improved 0.1 | NR | 3.4 D flatten | None |
| 14 | Stojanovic A et al | 2010 | Topo-PRK + CXL | Case series | 12 | 12 m | 20/1000–20/125 | 20/57–20/35 | NR | 3.62 D flatten | None |
| 15 | Lin DT, et al | 2012 | Topo-PRK + CXL | Case series | 66 | 6 m | 58% 20/40 or better | 92% 20/40 or better | NR | NR | None |
| 10 | Kanellopoulos AJ et al | 2014 | Topo-PRK + CXL | Case series | 231 | 36 m | 0.38 | 0.2 | NR | 46.56–44.44 | None |
| 15 | Kapasi et al | 2012 | Topo-PRK + CXL | Case series | 17 | 1 m | 0.33 lines better | Not reported | NR | NR | None |
| 15 | Tuwairqi WS, et al | 2012 | Topo-PRK + CXL | Case series | 22 | 12 m | Improved | Improved | NR | Reduced | 15 |
| 15 | Alessio et al | 2013 | Topo-PRK + CXL | Case series | 17 | 24 m | 0.44 | 0.003 | NR | 2.07 flatten | NR |
| 9 | Kanellopoulos AJ, et al | 2011 | Topo-PRK + CXL | Case series | 32 | 27 m | 27/32 >2.25 logMAR | 27/32 >2.25 logMAR | 2.3 D | 3.34 D flatten | None |
| 15 | Sakla H, et al | 2016 | Topo-PRK + CXL | Case series | 85 | 12 m | 0.86–0.46 improved | 0.41–0.11 improved | 1.71 D | Steep 48.1–46.05 D | None |
| 13 | Grenzelos MA et al | 2017 | Topo-PRK + CXL | Case series | 55 | 12 m | 0.59 improved | 0.12 improved | NR | Steep K reduced 4.03 D | 7.3% haze |
| 15 | Ohana | 2018 | Topo-PRK + CXL | Case series | 98 | 25.3 m | 1.23 logMAR improved | Not improved | NR | 4.03 D flatten | 5% haze |
| 15 | Iqbal M et al | 2019 | Topo-PRK + CXL | Case series | 67 | 24 m | 0.68 logMAR improved | NR | 2.31 D | Mean K reduced 0.36 D | 1 keratitis |
| 15 | Gore et al | 2018 | Wavefront-PRK + CXL | Case series | 47 | 24 m | NR | 0.13 logMAR improved | NR | Steep K reduced 5.4 D | NR |
| 15 | Nattis et al | 2018 | Topo-PRK + CXL sequential | Case series | 56 | 6 m | NR | 93% 20/40 or better | NR | No change | NR |
| 13 | Kymionis GD, et al | 2012 | PTK + CXL | Case series | 19 | 12 m | 0.36 improved | 0.12 improved | NR | steep K: reduced 2.07 D | NR |
| 15 | Assaf A, et al | 2015 | Topo-PRK + CXL sequential | Case series | 22 | 10.9 m | 0.87 improved | 0.34 | NR | meanK reduced 1.75 D | None |
| 16 | Kanellopoulos AJ, | 2019 | Topo-PRK + CXL | Case series | 144 | 128 m | 0.19–0.55 | 0.59–0.81 | Kmax reduced 7.6 D | 3.5% hyperopic shift | |
| 11 | Kanellopoulos AJ, et al | 2019 | Topo-PRK + CXL pediatric | Case series | 39 | 48 m | 0.51–0.65 | 0.71–0.81 | NR | Kmax reduced 8.7 D | 2 late haze |
| 15 | Kaiserman I, et al | 2019 | PTK + CXL | Case report | 20 | 27.5 m | 0.95–0.22 | 0.24–0.13 | NR | Kmax 48.18–45.97 | None |
The impressive similarities in improvement of UDVA, CDVA, and corneal flattening underline the efficacy in ectasia stabilization along with the improvement of visual function.
SUMMARY OF THE ATHENS PROTOCOL TECHNIQUE, ADVANTAGES, CONCERNS, AND COMPLICATIONS
Patient selection: any patient with keratoconus with documented progression and agreeable residual corneal thickness described below is potentially a candidate. A typical patient in our practice is a young man in his early 20s, typically a vigorous eye rubber and usually sleeping face down and with his eyes, usually, the most progressed on the knuckles of his hand. The limit of stromal tissue removal by the excimer laser ablation from the thinnest corneal area was initially set at 50 μm,6 as measured initially by scanning-slit tomography and later by Scheimpflug and/or OCT tomography, a limit that we set because it seemed to offer substantial stromal remodeling with minimum tissue removal in treatment design and has been retained and adapted by most subsequent technique modifications.
Customized corneal surface ablation was topography-guided by most investigators, whereas wavefront-guided by a few others.12–15 Topography-guided customization of the excimer ablation is driven by topography-captured data, and even when set to correct no refractive error, it provides an ablation algorithm attempting to flatten the ectatic, steeper corneal area and steepen the adjacent and usually superior flatter corneal area within the central 5 to 6.5 mm of the cornea (Fig. 1).
FIGURE 1.
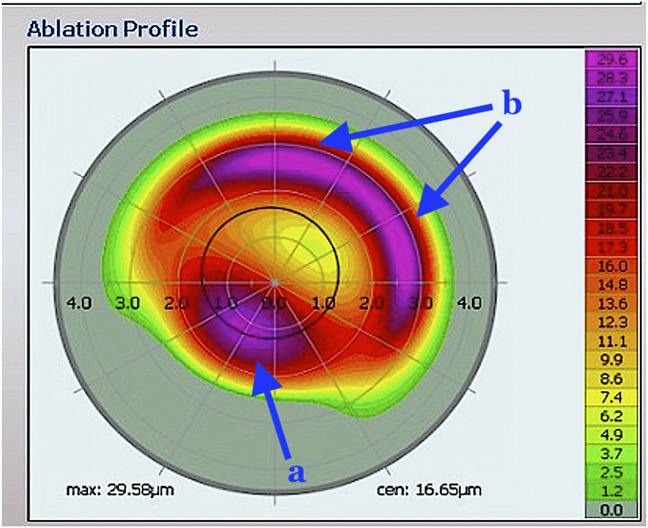
Topography-guided surface ablation used (EX500 excimer laser, WaveLight/Alcon, Erlangen, Germany) has a bimodal design: the blue arrow ‘a’ pointed to the part of the treatment ablating the cone area, so as to flatten it. Equally important to the normalization attempt is to steepen the area above the cone that invariably flattens in the ectasia process. Hence, the blue arrows ‘b’ point to the part of the treatment ablating away from the cone, usually superonasal, in a hyperopic-type arc. These 2 aspects of the customized topography-guided ablation achieve drastic normalization of the central ectatic cornea by flattening the cone and also steepening the cornea diametrically opposite to the cone—usually superonasal—that has flattened in the ectasia process.
Most such “therapeutic” excimer surface ablations performed in concert with CXL use higher fluence UV irradiance for a shorter time exposure, commonly termed “accelerated” CXL, usually for 5.5 to 7.0 joules total energy delivered.12–15 As a note here, the previous science of “accelerated cross-linking” and most of the published clinical results have cast more than substantial doubt on the photochemical basis of this concept. The Bunsen–Roscoe law of reciprocity is not applicable to this biological microenvironment nor to cross-linking in general. Molecular stromal oxygen concentration is likely the rate-limiting reagent, not UVA radiation. In addition, the higher the UV fluence, especially with continuous wave application promoting the more toxic type 1 photochemical CXL pathway instead of the preferred, the more efficient and much less toxic the type II pathway15B; thus, we have opted to use fluence of 6 mW/cm2 for over 15 minutes irradiance as the optimal time versus effect, as documented by the postoperative CXL, defined by the CXL “line” on anterior segment corneal OCT. The CXL procedure is invariably “epithelium-off” because even the Bowman layer plus the superficial corneal stroma has already been laser ablated before riboflavin solution soaking and UV light exposure, maximizing absorption and subsequent UV exposure. In some bilaterally rapidly advancing cases, we have applied this technique bilaterally. Apart from the obvious efficiency advantages of combining CXL + PRK as a single procedure and postoperative interval, the Athens Protocol technique and its modifications afford additional reported benefits as follows:
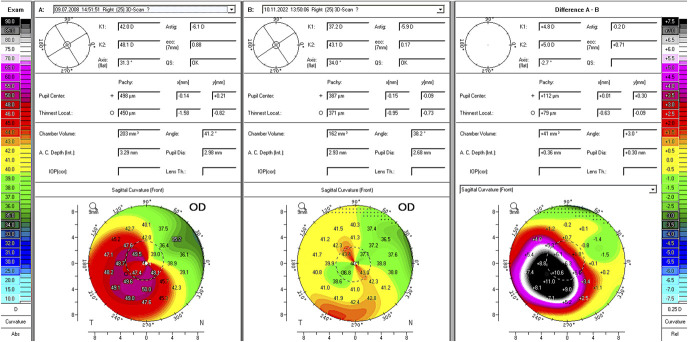
1. The overall normalization of an ectatic cornea should be measured, not only by the effective flattening of the apex but also by the simultaneous steepening of the superior to the cone-flattened area, thus enhancing central corneal symmetry and respective visual function. The index of height decentration (IHD) is an anterior corneal asymmetry index available in the topometric indices of most Scheimpflug tomography devices, and perhaps this change is best documented as we have reported. The example case in Figure 2 better illustrates this point. Based on the degree of corneal normalization, the combined technique seems to offer drastically higher efficacy in ectatic corneal normalization when compared to what would have been expected by applying CXL, followed by a normalization surface ablation at a later time. This enhanced effect seems to sustain stability even over 10-year follow-up.17
FIGURE 2.
Clinical case of a 24 year-old man with progressive keratoconus undergoing the Athens Protocol CXL in 2008. This image is a comparison of preoperative (left) to 14 years postoperative (middle) and difference preoperative minus postoperative (right) of the front sagittal curvature map captured by Scheimpflug tomography (Pentacam, Oculus Germany). The 2 aspects of the customized topography-guided ablation noted in Figure 1 underline in this case the drastic normalization of the ectatic cornea by flattening the cone (by maximally a drastic 11 diopters) and, as mentioned in Figure 1, also steepening the superonasal paracentral cornea diametrically opposite to the cone that has flattened in the ectasia process (by maximally 1.5 diopters). As a result, corneal power symmetry is drastically improved as noted in the difference (right) image that also underlines the accuracy of the excimer normalization delivery (the cone is flattened by over 11 diopters, whereas the flat superonasal area has effectively steepened from a minimum 35.2 D to 36.5 D also adding to the corneal refractive power normalization. Although this image suggests that the minimal corneal thickness has been reduced from 450 μm to 371 μm, Fig. 3 documents a 14-year postoperative minimal thickness of 400 μm as measured by anterior segment OCT—we have reported its superior accuracy to Scheimpflug tomography in corneal pachymetry measurement, especially after CXL.
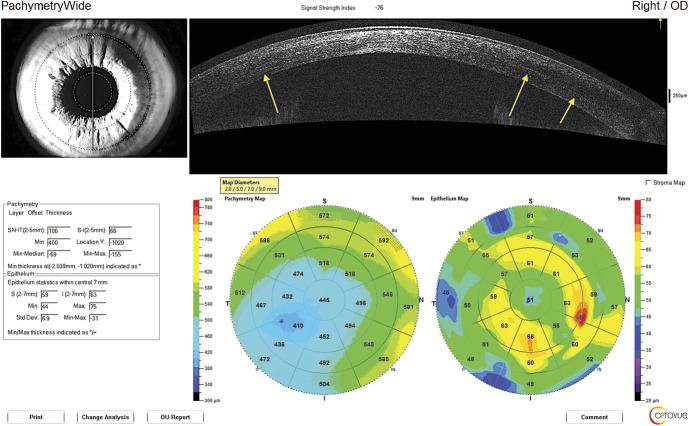
2. Uniform, deeper CXL effect—compared to what we have experienced when applying CXL alone—extending both below the 60% to 80% residual stromal thickness and broader, up to 9 mm corneal diameter, as evident on slit-lamp biomicroscopy and by anterior segment OCT “CXL demarcation line” is evident clinically even 14 years after successful treatment in the example case of Figures 2,3.
FIGURE 3.
Anterior segment OCT corneal and epithelial thickness map (Optovue Solix, Visionix, CA) of the same case described in Figure 2. This technology documents a 14-year postoperative minimal thickness of 400 μm (instead of 372 μm noted on Scheimpflug tomography in Fig. 2), depicting an effective 50 μm thinning of the cone area from preoperative to 14 years postoperative. The yellow arrows underline the presence even after 14 years of a CXL demarcation line, and the epithelial map also underlines marked remodeling from what is customary in corneal ectasia.76
3. Less postoperative stromal scarring is associated with combined, same-day therapeutic excimer laser surface ablation with CXL, in comparison to sequential technique (CXL first and surface ablation several months later) cases.7
Excimer ablation of a thinned ectatic cornea remains of serious concern for the potential risk of further biomechanically weakening the residual stromal bed, thereby increasing the potential risk for further ectasia. Yet, the long-term combined procedure results fortunately do not identify such concerns as the corneal curvatures remain flattened and normalized (reductions ranging from 8 to 20 D), suggesting synergy of cone flattening and corneal curvature normalization, presumably consequent to the deeper and broader CXL effect.17 As noted above, we limit the minimum total corneal thickness of 400 μm as the absolute lower limit of performing the combined procedures.9 Additional technical details are as specified in our 10-year postoperative review.17
Although nearly half of the treated eyes remain variably ametropic because the excimer ablation limits cannot address the full refractive error, most cases experience improved ability to use visual rehabilitation with spectacles and/or contact lenses as soon as they reepithelialize, reporting improved rigid gas-permeable contact lens and even soft contact lens use and tolerance after PRK + CXL,17 as CDVA demonstrates significant visual improvement (Table 1). Complications associated with combined PRK + CXL techniques, although limited, have been reported.19
1. Delayed corneal reepithelization beyond that anticipated for PRK alone likely related to increased apoptosis as described above, although the complication rates of the Athens Protocol seem markedly lower than other procedures, such as corneal transplantation and the implantation of corneal ring segments. To promote more efficient reepithelialization, reduction of topical corticosteroids and addition of autologous platelet-rich plasma19 are beneficial.
2. Corneal stromal haze over the ablation areas can develop. We have reported an under 10% incidence in the combined cases versus over 20% in the sequential cases when CXL was performed months before the excimer surface ablation.7
Specifically for pediatric cases, we have reported a rare late-onset (over 1 year after the procedure) stromal haze occurrence, possibly in response to intense natural UV light exposure in southern Europe.11 Haze is common and has been reported at roughly 60% with epithelium-off standard cross-linking even without PRK.20
3. Potential deep stromal scarring associated with CXL is not specific to the Athens Protocol procedures and should be carefully observed and managed postoperatively.19
4. A potential progressive additional flattening effect developing years after treatment has been reported in <2% of cases.17 This may result in a significant hyperopic shift requiring revision of optical visual correction and/or additional refractive surgical intervention.
Potential Concerns and Precautions
Residual stromal thickness: The greatest limitation and safety consideration is the excimer ablation limit in an already thinned cornea. As previously noted, the total corneal thickness (including the epithelium) before PRK should be at least 400 μm at the thinnest apical region, a concern that in our opinion merits careful informed consent and patient education of the potential risks involved. The so-called “400-μm rule” has been addressed scientifically and clinically for the photochemistry, application of the Beer–Lambert law, and sensitivity of endothelial cells to UVA. This earlier thinking has been revisited, parsed, and modified over time. Perhaps future research with different technologies and modifications of techniques may well allow safe and effective treatment of patients with thinner corneas, thus expanding the pool of patients with advanced disease who could benefit. When limited corneal thickness does not allow for a normalizing surface stromal ablation, we limit the surface ablation to solely epithelial removal by the excimer laser (50 μm depth, 7 mm diameter). As a result, in the areas of epithelial thinning to <50 μm, the Bowman layer and even superficial stromal tissue may be ablated. In any event, a residual stromal thickness of at least 350 μm has been observed. This limit should not be exceeded out of concern that further reduction of stromal thickness and overall volume might not afford adequate structural stabilization by CXL and also that the UV penetrance during CXL closer to the endothelial level might induce endothelial cell loss.
Another potential CXL modification is the customized application of the UV irradiation at variable fluence and variable pattern profile, thereby using CXL as an enhanced flattening tool when compared to standard CXL with uniform UV light application.21
Continued vigorous eye rubbing: It is increasingly likely that vigorous eye rubbing, even during sleep, might contribute to development and progression of keratoconus and corneal ectasia.22,23 Thus, proper patient education and continued reinforcement of vigorous eye-rubbing avoidance can benefit ectasia stabilization and long-term prognosis.
The most studied and used platform for topography-guided PRK is that of the 400-Hz Eye-Q and EX500 excimer lasers (Alcon, Ft. Worth, TX, an WaveLight, Erlangen, Germany) and addresses reshaping the anterior corneal curvature as determined by the actual cone location about the corneal center.17 Severely eccentric or oblique cones may significantly normalize with this technique about the anterior corneal curvature but will still retain irregular posterior curvature that can functionally limit vision. The limitation of reshaping only the anterior corneal surface in these cases may be addressed by wavefront-guided or ray-tracing customization of the therapeutic surface ablation used in the Athens Protocol CXL and its other applied modifications. As such, ray-tracing seemingly affords potential normalization of total corneal aberrations with less tissue removal over the thinnest cone area, as by measuring the total dynamic eye aberrations (low and high) it defines the most ectatic corneas as “tilted” about the total eye optics. This serves to significantly reduce the actual ablation planned in area “a” of Figure 1 and increase the ablation depth in area “b” illustrated in Figure 1 that is not thinned by ectasia. We have reported this complex advantage of ray-tracing customization of the normalization surface ablation in the Athens Protocol in detail.24
CONCLUSIONS AND RECOMMENDATION
In summary, the preponderance of published evidence supports customized PRK with minimal tissue ablation combined with CXL to be a long-term safe and effective strategy for anatomical and visual management of keratoconus, surgical ectasia, and other keratoectasia management.9-17 Ever since 2013 US FDA approval of the Alcon/WaveLight platform for topography-guided LASIK, PRK treatments are performed off-label—treatment of naive myopic eyes—and subsequently with 2016 US FDA approval of CXL for keratoconus and ectasia, many American refractive surgeons have been trained in and used to the best of their ability, within the limits of US excimer lasers, the Athens Protocol as an off-labeled procedure, although US FDA parameters, capabilities, and indications for approved PRK technology are markedly different for devices from outside the United States. This protocol has been used internationally for almost 2 decades because dozens of instructional courses and “hands-on” treatment designing wet laboratories have been given at the AAO, ASCRS, and ESCRS over the last 18 years. Based on the increasing passage of time and weight of experience, many refractive surgical specialists consider the Athens Protocol and modifications thereof to no longer be investigational but rather standard for optimal management of corneal ectatic disorders.
The Future and Next Steps
As corneal cross-linking has changed the management paradigm for keratoconus, revisiting the keratoconus diagnostic criteria has also become increasingly crucial.25 To this end, utilization of modern corneal diagnostics such as Scheimpflug corneal tomography and anterior segment OCT corneal tomography and epithelial mapping, as well as high-frequency ultrasound corneal epithelial mapping, has also increased the sensitivity of detection for early signs of ectasia, even when visual function, slit-lamp biomicroscopy, and traditional corneal topography results seem normal. Corneal epithelial remodeling may be able to mask traditional topographic imaging signs in early corneal ectasia, as well as explain corneal topographic steepening that is not associated with ectasia progression but rather local epithelial thickening of the cone apex.25
Recent attention to keratoconus screening in first-degree and second-degree family members attests to these crucial concerns. As in so many medical contexts, prevention is the best therapy, such that earlier detection of keratoconus and other ectasias affords the best opportunity for arresting progression and optimizing vision in the beginning stages of these important corneal conditions. As such, early suspicion of ectasia enables earlier detection with potential to additionally optimize clinical management with life-long beneficial implications.
Footnotes
The authors have no funding or conflicts of interest to disclose. Consultant for Alcon, Ft. Worth, TX, USA and Glaukos, USA.
REFERENCES
- 1.Braun E, Kanellopoulos J, Pe L, et al. Riboflavin/ultraviolet A–induced collagen cross–linking in the management of keratoconus. Invest Ophthalmol Vis Sci. 2005;46:4964. [Google Scholar]
- 2.Greenstein SA, Fry KL, Hersh PS. Corneal topography indices after corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011; 37:1282–1290. [DOI] [PubMed] [Google Scholar]
- 3.Wong JJ, Papakostas AD, Kanellopoulos AJ, et al. Post–LASIK Ectasia: PRK Following Previous Stabilization and Effective Management With Riboflavin/Ultraviolet A–Induced Collagen Cross–Linking. Invest Ophthalmol Vis Sci. 2006;47:557. [Google Scholar]
- 4.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–895. [DOI] [PubMed] [Google Scholar]
- 5.Kanellopoulos AJ. The impact of keratoconus treatment with the Athens Protocol (partial topography-guided photorefractive keratectomy combined with higher-fluence corneal collagen cross-linking) on quality of life: a long-term study. Clin Ophthalmol. 2019;13:795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ewald M, Kanellopoulos J. Limited topography-guided surface ablation (TGSA) followed by stabilization with collagen cross-linking with UV irradiation and riboflavin (UVACCL) for keratoconus (KC). Invest Ophthalmol Vis Sci. 2008;49:4338. [Google Scholar]
- 7.Kanellopoulos AJ. Comparison of sequential vs. same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25:S812–S818. [DOI] [PubMed] [Google Scholar]
- 8.Kanellopoulos J, Asimellis G. Introduction of quantitative and qualitative cornea optical coherence tomography findings induced by collagen cross-linking for keratoconus: a novel effect measurement benchmark. Clin Ophthalmol. 2013;7:329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg. 2011;27:323–331. [DOI] [PubMed] [Google Scholar]
- 10.Kanellopoulos AJ, Asimellis G. Corneal refractive power and symmetry changes following normalization of ectasias treated with partial topography-guided PTK combined with higher-fluence CXL (the Athens Protocol). J Refract Surg. 2014;30:342–346. [DOI] [PubMed] [Google Scholar]
- 11.Kanellopoulos AJ, Vingopoulos F, Sideri AM. Long-term stability with the Athens protocol (Topography-Guided partial PRK combined with cross-linking) in pediatric patients with keratoconus. Cornea. 2019;38:1049–1057. [DOI] [PubMed] [Google Scholar]
- 12.Kankariya VP, Dube AB, Grentzelos MA, et al. Corneal cross-linking (CXL) combined with refractive surgery for the comprehensive management of keratoconus: CXL plus. Indian J Ophthalmol. 2020;68:2757–2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kymionis GD, Grentzelos MA, Portaliou DM, et al. Corneal collagen cross-linking (CXL) combined with refractive procedures for the treatment of corneal ectatic disorders: CXL plus. J Refract Surg. 2014;30:566–576. [DOI] [PubMed] [Google Scholar]
- 14.Ziaei M, Barsam A, Shamie N, et al. ; ASCRS Cornea Clinical Committee. Reshaping procedures for the surgical management of corneal ectasia. J Cataract Refractive Surg. 2015;41:842–872. [DOI] [PubMed] [Google Scholar]
- 15.Zhu AY, Jun AS, Soiberman US. Combined protocols for corneal collagen cross-linking with photorefractive surgery for refractive management of keratoconus: update on techniques and review of literature. Ophthalmol Ther. 2019;8:15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubinfeld RS, Caruso C, Ostacolo C. Corneal cross-linking: the science beyond the myths and misconceptions. Cornea. 2019;38:780–790. [DOI] [PubMed] [Google Scholar]
- 17.Kanellopoulos AJ. Ten-year outcomes of progressive keratoconus management with the Athens protocol (Topography-Guided partial-refraction PRK combined with CXL). J Refract Surg. 2019;35:478–483. [DOI] [PubMed] [Google Scholar]
- 18.Lim L, Lim EWL. Current perspectives in the management of keratoconus with contact lenses. Eye (Lond). 2020;34:2175–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho MY, Kanellopoulos AJ. Short and long-term complications of combined topography-guided photorefractive keratectomy and riboflavin/ultraviolet A corneal collagen cross-linking (the Athens protocol) in 412 keratoconus eyes. Invest Ophthalmol Vis Sci. 2011;52:5202.21508105 [Google Scholar]
- 20.Greenstein SA, Hersh PS. Corneal crosslinking for progressive keratoconus and corneal ectasia: summary of US multicenter and subgroup clinical trials. Translational Vis Sci Technology. 2021;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanellopoulos AJ. Management of progressive keratoconus with partial topography-guided PRK combined with refractive, customized CXL; a novel technique: the enhanced Athens protocol. Clin Ophthalmol. 2019;13:581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sahebjada S, Al-Mahrouqi HH, Moshegov S, et al. Eye rubbing in the aetiology of keratoconus: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2021;259:2057–2067. [DOI] [PubMed] [Google Scholar]
- 23.Mazharian A, Panthier C, Courtin R, et al. Incorrect sleeping position and eye rubbing in patients with unilateral or highly asymmetric keratoconus: a case-control study. Graefes Arch Clin Exp Ophthalmol. 2020;258:2431–2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanellopoulos AJ. Keratoconus management with customized photorefractive keratectomy by artificial intelligence ray-tracing optimization combined with higher fluence corneal crosslinking: the ray-tracing Athens protocol. Cornea. 2021;40:1181–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanellopoulos J, Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol. 2013;7:1539–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]