Abstract
Objectives The authors examined the structural differences in the paranasal sinus region at sphenoid sinus in the pediatric population.
Methods Paranasal sinus computed tomography (PNSCT) images of 86 pediatric subjects (30 males, 56 females) were included. In 13 to 15 years of age group ( n =34) and ≥16 years of age group ( n =52), sphenoid sinus pneumatization (SSP), optic canal and carotid canal classifications and dehiscence evaluation were performed.
Results In both sexes, type 1 and type 2 SS pneumatization were observed more frequently on both the right and left sides. On the right side, type 2> type 1; on the left side type 1> type 2 optic canals were detected in both gender. Type 3 optic canals were detected in 8.8 to 14.7% of the 13 to 15 years of age group; and 11.5 to 17.3% of ≥16 years of age group. Type 4 optic canals were detected in 2.9% of the 13 to 15 years of age group and 1.9% of the ≥16 years of age group bilaterally. Optic canal dehiscence was detected in 26.5% of the 13 to 15 years of age group and 17.3% of the ≥16 years of age group. Type 1 and type 2 carotid canals are most common in children, the percentages for type 3 carotid canals were 1.8 to 3.6% in children.
Conclusion In pneumatized SS, optic canal classifications got increased values which showed protrusion into the sphenoid sinus wall. Therefore, in children, the surgeons must be very careful for optic canal being nearer to the sphenoid sinus walls.
Keywords: sphenoid sinus, pneumatization, optic canal, carotid canal, PNSCT
Introduction
The development of paranasal sinuses (PNS) begins in fetal life. Face development continues after birth with the development of the cranium and matures around the age of 12. 1 Some anatomical variations can be seen during the development process. These variations seen in the development process may disrupt normal airflow and mucociliary activity, leading to a tendency to sinusitis. If the patient needs surgery at a later time, it may cause difficulties during surgical procedures. 2 3
Kim et al found that the incidence of anatomical abnormalities in pediatric chronic sinusitis cases was higher than in the control group. 4 Nowadays, surgical treatment is appropriate for selected pediatric cases of chronic sinusitis that develops secondary to anatomical variations, albeit rarely, and functional endoscopic sinus surgery (FESC) has been used more frequently in children than open surgery, just as in adults. 5 6 7 In the preoperative evaluation, the radiologist's accurate assessment of anatomical variation and dangerous areas is very important for the surgeon who will perform FESC.
In our study, we examine the structural differences in the PNS region at sphenoid sinus (SS) in the pediatric population. In particular, we investigated the SS aeration, the width and classification of the optic canal and carotid canal, and their relationship with the SS wall. We should mention that the studies on this subject have mostly been done on adults. 8
Materials and Methods
This retrospective study was conducted at Kırıkkale University Faculty of Medicine, Pediatrics, Otorhinolaryngology and Radiology Departments according to the principles of the Declaration of Helsinki. Paranasal sinus computed tomography (PNSCT) images were obtained from the database of the V University Faculty of Medicine Radiology Department, Kirikkale University. Ethics committee approval was obtained from Kırıkkale University Non-invasive Research Ethics Committee (Date: August 21, 2019, Number: 2019.08.02). There is no need to take informed consent, because the data was evaluated retrospectively.
Subjects
This study was performed retrospectively. PNSCT images of 86 pediatric subjects (30 males, 56 females), were selected from a digital radiology database of all PNSCT in Kırıkkale University Faculty of Medicine Radiology Department between 2019 January to 2014 January. There were a total of 466 PNSCT in our database and only 86 PNSCT were included into the study according to the inclusion criteria.
Mean ages of the males were 15.96±1.32 years (ranged from 13 to 17 years); and of the females were 15.58±1.33 years (ranged from 13 to 17 years).
Analyses were also performed in age groups of 13 to 15 years ( n =34) and ≥16 years of age group ( n =52). In 13 to 15 years of age group, the mean ages were 14.29±0.87 years (ranged from 13 to 15 years). In ≥16 years of age group, the mean ages were 16.65±0.48 years (ranged from 16 to 17 years).
The age groups were created in children who underwent PNSCT examination and most of our children who took PNSCT examinations were ≥13 years of age. Therefore the age groups were created as early in adolescence (13–15 years of age) and late in adolescence (≥16 years of age) in our PNSCT images in children.
Inclusion Criteria
Children aged ≥13 years and <18 years.
In children, PNSCT examination was not performed frequently. Most of the patients' PNSCT indication was mainly suspecting sinusitis or nasal septal deviation. Normal (no sinusitis and no other pathologies) or nasal septal deviation reported cases were included ( Table 1 ).
Table 1. The indications for PNSCT examination and final diagnosis report of PNSCT in the children.
| Indication for PNSCT examination | Final diagnosis report of PNSCT | Children number ( n =86) |
|---|---|---|
| Suspicion of nasal septal deviation | Nasal septal deviation | 36 |
| Suspicion of rhinosinusitis | Normal CT report, no rhinosinusitis | 27 |
| Headache, etiology? | Normal CT report, no intranasal pathology | 5 |
| Allergic rhinitis, intranasal pathology? | Normal CT report, no intranasal pathology | 15 |
| Halitosis, intranasal pathology? | Normal CT report, no intranasal pathology | 1 |
| Foreign body in the nasal cavity? | Normal CT report, no intranasal pathology, no foreign body | 1 |
| Epistaxis history, intranasal pathology ? | Normal CT report, no intranasal pathology | 1 |
Exclusion Criteria
Subjects with previous trauma or surgery history, sinonasal tumor, acute and chronic rhinosinusitis, sinonasal polyposis, CSF leak, and marked facial deformity were not included in the study.
CT Imaging and Analysis
All of the scans were obtained with routine PNS-computed tomography imaging in the supine position, with no contrast or sedation being used for the procedures. The images were acquired using a 64-slice CT (MSCT; Brilliance 64, Philips Medical System, Best, the Netherlands). All of the scans were obtained using the following parameters: tube voltage=120kV, effective mAs=350, slice thickness=1.00mm, field of view=180mm and image matrix=768×768. The images were transferred to a commercially available workstation, and the raw data was reconstructed using bone algorithms. After scanning, the coronal, axial, and sagittal images were reconstructed with a slice thickness of 1.00mm. The coronal and axial plan was often preferred.
The following measurements were performed 8 :
-
Sphenoid sinus pneumatization (SSP): it was classified as types 1 to 3 at coronal plane ( Fig. 1 ):
“Type 1: SSP extends medially to the Vidian canal.
Type 2: SSP extends medially to the foramen rotundum.
Type 3: SSP extends laterally to the foramen rotundum.”
Optic canal width: “At coronal plane, both optic canals were measured as mm at the widest site internally without including bone structure.” ( Fig. 2A ).
Optic canal dehiscence: “It was classified at coronal plane as absent, right, left or bilateral” ( Fig. 2B and C ).
-
Optic canal classification: “Both optic canals were classified according to the relationship with the SS wall” ( Fig. 2D ):
“Type 1: No indentation.
Type 2: Indentation to SS wall.
Type 3: Protrudation to SS wall.
Type 4: Extends laterally to the SS and posterior ethmoid cell.”
Carotid canal width: At coronal plane, both carotid canals were measured at the level associated with the SS wall as mm at the widest site internally without including bone structure ( Fig. 3A ).
Carotid canal dehiscence: it was classified at coronal plane as absent, right, left or bilateral ( Fig. 3B ).
-
Carotid canal classification: Both carotid canals were classified according to the relationship with the SS wall ( Fig. 3C ).
“Type 1: No indentation.
Type 2: Indentation to SS wall.
Type 3: Protrudation to SS wall.”
Fig. 1.

Coronal PNSCT shows sphenoid sinus pneumatization (type 2) ( long arrow ) extending medially to the foramen rotundum ( short arrow ). PNSCT, paranasal sinus computed tomography.
Fig. 2.
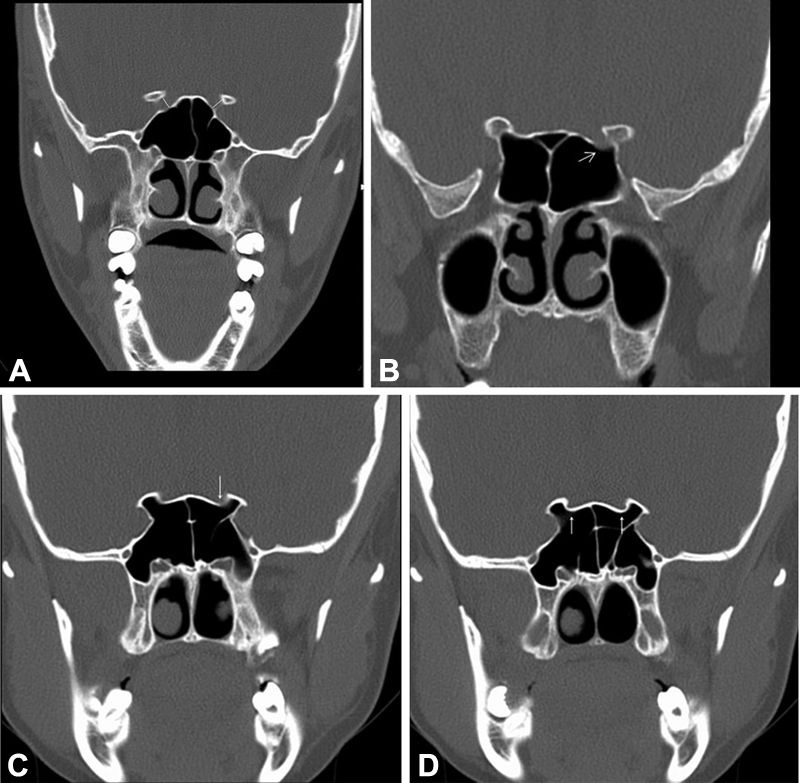
( A ) Coronal PNSCT shows the measurement of bilateral Optic canal width ( white lines ). ( B ) Coronal PNSCT shows left optic canal dehiscence ( white arrow ). ( C ) Coronal PNSCT shows left optic canal dehiscence ( white arrow ). ( D ) Coronal PNSCT shows, bilateral optic canal ( white arrow ) protrudation to sphenoid sinus wall (type 3). PNSCT, paranasal sinus computed tomography.
Fig. 3.

( A ) Coronal PNSCT shows the measurement of right carotid canal width ( white arrow ). ( B ) Coronal PNSCT shows left carotid canal dehiscence ( white arrow ). ( C ) Axial PNSCT shows bilateral carotid canal ( white arrows ) protrudation to sphenoid sinus wall (type 3). PNSCT, paranasal sinus computed tomography.
Statistical Analysis
SPSS for Windows 25.0 (SPSS, INC, an IBM Company, Chicago, Illinois, United States). Chi-square test, independent samples t -test, and Spearman's correlation rho efficient test were used.
p -Value <0.05 was considered as statistically significant.
Results
Analysis of the Results According to Gender
SS pneumatization : In both genders, type 1> type 2 SS pneumatization was detected ( p >0.05) ( Table 2 ).
Table 2. Sphenoid sinus pneumatization, carotid and optic canal classification values in males and females a .
| Male (n=30) | Female (n=56) | pa | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||||
| Type of the Sphenoid sinus pneumatization c | R | Type 1 | 11 | 36.7 | 30 | 53.6 |
p
=0.316
χ2 =2.303 |
||
| Type 2 | 11 | 36.7 | 16 | 28.6 | |||||
| Type 3 | 8 | 26.7 | 10 | 17.9 | |||||
| L | Type 1 | 13 | 43.3 | 28 | 50,0 |
p
=0.636
χ2 =0.904 |
|||
| Type 2 | 11 | 36.7 | 15 | 26,8 | |||||
| Type 3 | 6 | 20.0 | 13 | 23,2 | |||||
| Carotid canal classification at SS wall d | R | Type 1 | 18 | 60.0 | 44 | 78,6 |
p
=0.096
χ2 =4.693 |
||
| Type 2 | 12 | 40.0 | 11 | 19,6 | |||||
| Type 3 | 0 | 0.0 | 1 | 1,8 | |||||
| L | Type 1 | 20 | 66.7 | 44 | 78,6 |
p
=0.442
χ2 =1.631 |
|||
| Type 2 | 9 | 30.0 | 10 | 17,9 | |||||
| Type 3 | 1 | 3.3 | 2 | 3,6 | |||||
| Carotid canal dehiscence | Absent | 29 | 96.7 | 54 | 96.4 |
p
=0.954
χ2 =0.003 |
|||
| Right | 0 | 0.0 | 0 | 0.0 | |||||
| Left | 1 | 3.3 | 2 | 3.6 | |||||
| Bilateral | 0 | 0.0 | 0 | 0.0 | |||||
| Optic canal classification at SS wall e | R | Type 1 | 9 | 30.0 | 24 | 42,9 |
p
=0.635
χ2 =1.708 |
||
| Type 2 | 15 | 50.0 | 25 | 44,6 | |||||
| Type 3 | 5 | 16.7 | 6 | 10,7 | |||||
| Type 4 | 1 | 3.3 | 1 | 1,8 | |||||
| L | Type 1 | 14 | 46.7 | 24 | 42,9 |
p
=0.947
χ2 =0.365 |
|||
| Type 2 | 11 | 36.7 | 23 | 41,1 | |||||
| Type 3 | 4 | 13.3 | 8 | 14,3 | |||||
| Type 4 | 1 | 3.3 | 1 | 1,8 | |||||
| Optic canal dehiscence | Absent | 24 | 80.0 | 44 | 78.6 |
p
=0.826
χ2 =0.896 |
|||
| Right | 3 | 10.0 | 5 | 8.9 | |||||
| Left | 3 | 10.0 | 6 | 10.7 | |||||
| Bilateral | 0 | 0.0 | 1 | 1.8 | |||||
| Mean | Median | Std. dev. | Mean | Median | Std. dev. | p b | |||
| Carotid canal diameter (mm) | R | 4.61 | 4.70 | 0.54 | 4.22 | 4.20 | 0.51 | 0.002 | |
| L | 4.62 | 4.50 | 0.53 | 4.33 | 4.35 | 0.49 | 0.015 | ||
| Optic canal diameter (mm) | R | 3.56 | 3.60 | 0.48 | 3.35 | 3.30 | 0.36 | 0.028 | |
| L | 3.52 | 3.50 | 0.49 | 3.38 | 3.40 | 0.43 | 0.181 | ||
p-Value shows the results of Chi-square test.
p -Value shows the results of independent samples t -test.
Sphenoid sinus pneumatization (SSP): Type 1: SSP extends medially to the Vidian canal, Type 2: SSP extends medially to the foramen rotundum, Type 3: SSP extends laterally to the foramen rotundum.
Carotid canal classification: Type 1: no indentation, Type 2: indentation to SS wall, Type 3: protrudation to SS wall.
Optic canal classification: type 1: no indentation, type 2: indentation to SS wall, type 3: protrudation to SS wall, type 4: extends lateral to the sphenoid sinus and posterior ethmoid cell.
Carotid Canals
In both genders, type 1 >type 2 carotid canals were detected ( p >0.05) ( Table 2 ). Type 3 carotid canals were detected in 3.3% of the males; and 1.8 to 3.6% of the females. Carotid canal dehiscence was detected in 3.3% of the males (left side) and 3.6% of the females ( p >0.05) ( Table 2 ). In males, bilateral carotid canal diameters were higher than those in females ( p <0.05) ( Table 2 ).
Optic Canals
On the right side, type 2> type 1; on the left side type 1>type 2 optic canals were detected in both gender ( p >0.05) ( Table 2 ). Type 3 optic canals were detected in 13.3 to 16.7% of the males; and 10.7 to 14.3% of the females. Type 4 optic canals were detected in 3.3% of the males and 1.8% of the females bilaterally ( Table 2 ). Optic canal dehiscence was detected in 20.0% of the males (10.0% on the right side and 10.0% on the left side) and 21.4% of the females (8.9% on the right side, 10.7% on the left side, and 1.8% on bilateral sides) ( p >0.05) ( Table 2 ). In males, optic canal diameter was higher than those in females ( p <0.05) ( Table 2 ).
Analysis of the Results According to Age Groups (13–15 Years of Age and ≥16 Years of Age Group)
SS Pneumatization
In both age groups, type 1> type 2 SS pneumatization was detected ( p >0.05) ( Table 3 ).
Table 3. Sphenoid sinus pneumatization, carotid and optic canal classification values in age groups.
| 13–15 y of age group (n=34) | ≥16 y of age group (n=52) | pa | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | n | % | ||||||
| Type of the sphenoid sinus pneumatization c | R | Type 1 | 16 | 47.1 | 25 | 48,1 |
p
=0.988
χ2 =0.024 |
||
| Type 2 | 11 | 32.4 | 16 | 30,8 | |||||
| Type 3 | 7 | 20.6 | 11 | 21,2 | |||||
| L | Type 1 | 13 | 38.2 | 28 | 53,8 |
p
=0.287
χ2 =2.498 |
|||
| Type 2 | 11 | 32.4 | 15 | 28,8 | |||||
| Type 3 | 10 | 29.4 | 9 | 17,3 | |||||
| Carotid canal classification at SS wall d | R | Type 1 | 26 | 76.5 | 36 | 69,2 |
p
=0.243
χ2 =2.476 |
||
| Type 2 | 7 | 20.6 | 16 | 30,8 | |||||
| Type 3 | 1 | 2.9 | 0 | 0,0 | |||||
| L | Type 1 | 25 | 73.5 | 39 | 75,0 |
p
=0.948
χ 2 =0.107 |
|||
| Type 2 | 8 | 23.5 | 11 | 21,2 | |||||
| Type 3 | 1 | 2.9 | 2 | 3,8 | |||||
| Carotid canal dehiscence | Absent | 33 | 97.1 | 50 | 96.2 |
p
=0.821
χ2 =0.510 |
|||
| Right | 0 | 0.0 | 0 | 0.0 | |||||
| Left | 1 | 2.9 | 2 | 3.8 | |||||
| Bilateral | 0 | 0.0 | 0 | 0.0 | |||||
| Optic canal classification at SS wall e | R | Type 1 | 15 | 44.1 | 18 | 34,6 |
p
=0.665
χ2 =1.574 |
||
| Type 2 | 13 | 38.2 | 27 | 51,9 | |||||
| Type 3 | 5 | 14.7 | 6 | 11,5 | |||||
| Type 4 | 1 | 2.9 | 1 | 1,9 | |||||
| L | Type 1 | 14 | 41.2 | 24 | 46,2 |
p
=0.932
χ2 =0.007 |
|||
| Type 2 | 16 | 47.1 | 18 | 34,6 | |||||
| Type 3 | 3 | 8.8 | 9 | 17,3 | |||||
| Type 4 | 1 | 2.9 | 1 | 1,9 | |||||
| Optic canal dehiscence | Absent | 25 | 73.5 | 43 | 82.7 |
p
=0.161
χ 2 =1.967 |
|||
| Right | 3 | 8.8 | 5 | 9.6 | |||||
| Left | 5 | 14.7 | 4 | 7.7 | |||||
| Bilateral | 1 | 2.9 | 0 | 0.0 | |||||
| Mean | Median | Std. dev. | Mean | Median | Std. dev. | p b | |||
| Carotid canal diameter (mm) | R | 4.21 | 4.15 | 0.52 | 4.45 | 4.50 | 0.55 | 0.049 | |
| L | 4.39 | 4.40 | 0.45 | 4.45 | 4.40 | 0.56 | 0.603 | ||
| Optic canal diameter (mm) | R | 3.40 | 3.35 | 0.39 | 3.45 | 3.50 | 0.43 | 0.614 | |
| L | 3.44 | 3.40 | 0.41 | 3.43 | 3.40 | 0.49 | 0.934 | ||
p -Value shows the results of Chi-square test.
p -Value shows the results of the independent samples t -test.
Sphenoid sinus pneumatization (SSP): Type 1: SSP extends medially to the Vidian canal, Type 2: SSP extends medially to the foramen rotundum, Type 3: SSP extends laterally to the foramen rotundum.
Carotid canal classification: Type 1: no indentation, Type 2: indentation to SS wall, Type 3: protrudation to SS wall.
Optic canal classification: Type 1: no indentation, Type 2: indentation to SS wall, Type 3: protrudation to SS wall, Type 4: extends lateral to the sphenoid sinus and posterior ethmoid cell.
Carotid Canals
In both genders, type 1 >type 2 carotid canals were detected ( p >0.05) ( Table 3 ). Type 3 carotid canals were detected in 2.9% of the 13 to 15 years of age group; and 3.8% of the ≥16 years of age group. Carotid canal dehiscence was detected in 2.9% of the 13 to 15 years of age group (left side) and 3.8% of the ≥16 years of age group ( p >0.05) ( Table 3 ). In ≥16 years of age group, right carotid canal width was higher than those in 13 to 15 years of age group ( p <0.05) ( Table 3 ).
Optic Canals
On the right side, type 1> type 2, on the left side type 2>type 1 optic canals were detected in 13 to 15 years of age group. In ≥16 years of age group, on the right side, type 2> type 1, on the left side type 1> type 2 optic canals were detected ( p >0.05) ( Table 3 ). Type 3 optic canals were detected in 8.8 to 14.7% of the 13 to 15 years of age group; and 11.5 to 17.3% of the ≥16 years of age group. Type 4 optic canals were detected in 2.9% of the 13 to 15 years of age group and 1.9% of ≥16 years of age group bilaterally ( Table 3 ). Optic canal dehiscence was detected in 26.5% of the 13 to 15 years of age group (8.8% on the right side, 14.7% on the left side, and 2.9% on bilateral sides) and 17.3% of the ≥16 years of age group (9.6% on the right side and 7.7% on the left side) ( p >0.05) ( Table 3 ). In both age groups, optic canal diameters were not different bilaterally ( p <0.05) ( Table 3 ).
Correlation Test Results
There were positive correlations between SSP ( p <0.05) and optic canal classification values of the right and left sides ( p <0.05) ( Table 4 ).
Table 4. Correlation test results a .
| Type of the sphenoid sinus pneumatizationb | Carotid canal classification at SS wall c | Optic canal classification at SS walld |
||||||
|---|---|---|---|---|---|---|---|---|
| R | L | R | L | R | L | |||
| Type of the sphenoid sinus pneumatization b | R | r | 0.378 | 0.034 | 0.006 | 0.046 | 0.091 | |
| P | 0.000 | 0.755 | 0.954 | 0.675 | 0.407 | |||
| L | r | 0.378 | 0.019 | 0.084 | −0.032 | 0.105 | ||
| P | 0.000 | 0.859 | 0.441 | 0.771 | 0.334 | |||
| Carotid canal classification at SS wall c | R | r | 0.034 | 0.019 | 0.205 | 0.125 | 0.214 | |
| P | 0.755 | 0.859 | 0.058 | 0.253 | 0.048 | |||
| L | r | 0.006 | 0.084 | 0.205 | 0.014 | 0.084 | ||
| P | 0.954 | 0.441 | 0.058 | 0.898 | 0.443 | |||
| Optic canal classification at SS wall d |
R | r | 0.046 | −0.032 | 0.125 | 0.014 | 0.378 | |
| P | 0.675 | 0.771 | 0.253 | 0.898 | 0.000 | |||
| L | r | 0.091 | 0.105 | 0.214 | 0.084 | 0.378 | ||
| P | 0.407 | 0.334 | 0.048 | 0.443 | 0.000 | |||
| Carotid canal diameter (mm) | R | r | 0.116 | −0.071 | 0.050 | 0.123 | 0.111 | 0.050 |
| P | 0.286 | 0.519 | 0.651 | 0.258 | 0.311 | 0.647 | ||
| L | r | 0.121 | 0.060 | 0.144 | 0.087 | 0.045 | −0.027 | |
| P | 0.268 | 0.584 | 0.187 | 0.425 | 0.678 | 0.804 | ||
| Optic canal diameter (mm) | R | r | 0.089 | 0.082 | 0.274 | −0.021 | −0.177 | −0.160 |
| P | 0.415 | 0.454 | 0.011 | 0.847 | 0.102 | 0.142 | ||
| L | r | 0.084 | 0.112 | −0.016 | 0.026 | −0.107 | 0.008 | |
| p | 0.444 | 0.307 | 0.885 | 0.815 | 0.327 | 0.944 | ||
| Age | r | −0.111 | −0.078 | 0.108 | 0.058 | 0.071 | 0.017 | |
| p | 0.310 | 0.476 | 0.323 | 0.595 | 0.517 | 0.876 | ||
| Age group (Code 1: 13–15 y of age, Code 2: ≥16 y of age) | r | −0.005 | −0.170 | 0.069 | −0.013 | 0.050 | −0.003 | |
| p | 0.966 | 0.119 | 0.528 | 0.904 | 0.647 | 0.977 | ||
| Gender (Code 1: Male. Code 2: Female) |
r | −0.161 | −0.031 | −0.189 | −0.124 | −0.140 | 0.023 | |
| p | 0.139 | 0.774 | 0.081 | 0.255 | 0.197 | 0.830 | ||
p -Value shows the results of Spearman's correlation rho efficient test.
Sphenoid sinus pneumatization (SSP): Type 1: SSP extends medially to the Vidian canal, Type 2: SSP extends medially to the foramen rotundum, Type 3: SSP extends laterally to the foramen rotundum.
Carotid canal classification: Type 1: No indentation, Type 2: Indentation to SS wall, Type 3: Protrudation to SS wall.
Optic canal classification: Type 1: No indentation, Type 2: Indentation to SS wall, Type 3: Protrudation to SS wall, Type 4: Extends lateral to the sphenoid sinus and posterior ethmoid cell.
As carotid canal classification values get higher on the right side, left optic canal classification values ( p <0.05) and right optic canal diameter values ( p <0.05) also get higher ( Table 4 ).
Discussion
The ongoing growth process in children is associated with differences in anatomical structures compared with adults. Attention is also required in the childhood age group when even very small anatomical variations are important for the success of the surgery and to avoid complications such as transsphenoidal surgical procedures. Veins are functional and have a vital importance. The paranasal sinus region through which the vessels and nerves are located has a special importance in this regard. Therefore, it is recommended to routinely examine PNS and neighboring structures with CT before transsphenoidal operations. 9
In this study, the relationship between the SS, carotid canal, and optic canal was investigated in children. In both sexes, type 1 and type 2 SS pneumatization were observed more frequently on both the right and left sides. In Asal et al's study 8 on adults, they reported that type 3 SS pneumatization bilaterally in males and in females, type 2 SS pneumatization on the right side and type 3 SS pneumatization on the left side were more common. Although this indicates that SS aeration is higher in adults than in children, there was no significant difference between 13 to 15 years and ≥16 age groups in the present study. In a study of 267 children with chronic rhinosinusitis symptoms who did not respond to medical treatment, it was reported that SS over-pneumatization was detected in 11.9% of cases. 10 In this study, in which we did not include acute and chronic rhinosinusitis cases, Type 3 SS pneumatization was found to be similar in both sexes between 17.9 and 26.7%. This suggests that in chronic rhinosinus cases, SS pneumatization may be affected and its aeration may have decreased.
In the present study, on the right side, type 2> type 1, on the left side type 1> type 2 optic canals were detected in both gender. Type 3 optic canals were detected in 13.3 to 16.7% of the males and 10.7 to 14.3% of the females. Type 4 optic canals were detected in 3.3% of the males and 1.8% of the females bilaterally. Optic canal dehiscence was detected in 20.0% of the males and 21.4% of the females. In males, optic canal diameter was higher than those in females. Type 3 optic canals were detected in 8.8 to 14.7% of 13 to 15 years of age group and 11.5 to 17.3% of ≥16 years of age group. Type 4 optic canals were detected in 2.9% of 13 to 15 years of age group and 1.9% of ≥16 years of age group bilaterally. Optic canal dehiscence was detected in 26.5% of 13 to 15 years of age group and 17.3% of ≥16 years of age group.
In adults, it was reported that optic canal protrudation values were 33.3% in males and 30.5% in females. Optic canal dehiscence was detected in 11.3% of males and 9.9% of females. 8 These results showed that from childhood to adulthood, optic canal classification values got increased and protrudation got a higher percentages.
There were positive correlations between SSP and optic canal classification values bilaterally. As carotid canal classification values get higher on the right side, left optic canal classification values and right optic canal diameter values also get higher. Our results showed that in pneumatized SS, optic canal classifications got increased values which showed protrusion into the SS wall.
In this study, it was shown that type 1 and type 2 carotid canals are most common in children, similar to those in adults. In adults, type 3 carotid canal is also the most rare. 8 However, in children, type 3 carotid canal is very rare in our study. The rates of encountering type 3 carotid canal in adults were 24 to 36%, 8 while in the present study, the percentages for type 3 carotid canals were 1.8 to 3.6% in children.
Surgical interventions involving the PNS region are not limited to FESC, and different surgical-endoscopic treatments, including transsphenoidal endoscopic surgery of pituitary adenomas, are also applied today in the pediatric population. 8 11 SS septation and pneumatization may present with many different variations. The close relationship of the SS with neurovascular structures, especially its relationship with the internal carotid artery (CA), should be examined before surgery. 12 13 14 Computed tomography (CT) appears to be the best imaging method for the lesions, variations, and preoperative evaluation of the SS, CA, and skull base. It has been evaluated as a gold standard especially for intervention to transsphenoidal pituitary tumors. 15 16 17
In this study, carotid canal dehiscence was found to be much rarer (3.3–3.6%) in children than in adults. 8 Since the SS, which is the last to develop and be aerated in the pediatric age, during the progress to adulthood, the volume of sinus will increase and carotid canal protrusion can be expected to increase as a result. In addition, it may be associated with the increasing frequency of bone-mineral disorders seen with increasing age or chronic diseases such as diabetes mellitus and hypertension that impair microvascular tissue nutrition.
In conclusion, type 3 optic canals were detected in 8.8 to 14.7% in younger children and 11.5 to 17.3% in older children. Therefore, in children, the surgeons must be very careful about the proximity of optic canal to the SS walls. Although type 3 carotid canals were detected rarely in children (1.8–3.6%), we recommend to evaluate PNS CT before surgery and to be aware of pneumatized sphenoid sinuses which are observed with higher optic canal classification values.
Conflict of Interest None declared.
Authors' Contributions
S.T. and M.İ. are the guarantors of integrity of the entire study and they did clinical studies.S.T., N.B.M., M.İ., A.G., and Z.Ş. studied concepts and design and did literature search. N.B.M. did the statistical analysis and manuscript editing. N.B.M. and S.T. prepared the manuscript.
Ethics Committee Approval
This study is retrospective. Ethics committee approval was obtained from Kırıkkale University Non-invasive Research Ethics Committee (Date: August 21, 2019, Number: 2019.08.02).
There is no need to take informed consent, because the data were evaluated retrospectively.
There are no funds for this article.
References
- 1.Anderhuber W, Weiglein A, Wolf G. [Nasal cavities and paranasal sinuses in newborns and children] Acta Anat (Basel) 1992;144(02):120–126. [PubMed] [Google Scholar]
- 2.Mohebbi A, Ahmadi A, Etemadi M, Safdarian M, Ghourchian S. An epidemiologic study of factors associated with nasal septum deviation by computed tomography scan: a cross sectional study. BMC Ear Nose Throat Disord. 2012;12:15. doi: 10.1186/1472-6815-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cannavò S, Venturino M, Curtò L et al. Clinical presentation and outcome of pituitary adenomas in teenagers. Clin Endocrinol (Oxf) 2003;58(04):519–527. doi: 10.1046/j.1365-2265.2003.01748.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim H J, Jung Cho M, Lee J-W et al. The relationship between anatomic variations of paranasal sinuses and chronic sinusitis in children. Acta Otolaryngol. 2006;126(10):1067–1072. doi: 10.1080/00016480600606681. [DOI] [PubMed] [Google Scholar]
- 5.Siedek V, Stelter K, Betz C S, Berghaus A, Leunig A. Functional endoscopic sinus surgery–a retrospective analysis of 115 children and adolescents with chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol. 2009;73(05):741–745. doi: 10.1016/j.ijporl.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Eviatar E, Pitaro K, Gavriel H, Krakovsky D. Complications following powered endoscopic sinus surgery: an 11 year study on 1190 patients in a single institute in Israel. Isr Med Assoc J. 2014;16(06):338–340. [PubMed] [Google Scholar]
- 7.Arıcıgil M, Yücel A. Çocuklarda Endoskopik Sinüs Cerrahisi: 10 Yıllık Tecrübemiz. KBB-Forum. 2017;16(02):53–57. [Google Scholar]
- 8.Asal N, Bayar Muluk N, Inal M, Şahan M H, Doğan A, Arıkan O K. Carotid canal and optic canal at sphenoid sinus. Neurosurg Rev. 2019;42(02):519–529. doi: 10.1007/s10143-018-0995-4. [DOI] [PubMed] [Google Scholar]
- 9.Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base. 2008;18(01):9–15. doi: 10.1055/s-2007-992764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palabıyık F. Imaging of the anatomic variations and dangerous areas of the paranasal sinuses and nasal cavity in pediatric patients. IKSST Dergisi. 2018;10(01):36–42. [Google Scholar]
- 11.Locatelli D, Veiceschi P, Castelnuovo P et al. Transsphenoidal surgery for pituitary adenomas in pediatric patients: a multicentric retrospective study. Childs Nerv Syst. 2019;35(11):2119–2126. doi: 10.1007/s00381-019-04179-z. [DOI] [PubMed] [Google Scholar]
- 12.Johnson D M, Hopkins R J, Hanafee W N, Fisk J D. The unprotected parasphenoidal carotid artery studied by high-resolution computed tomography. Radiology. 1985;155(01):137–141. doi: 10.1148/radiology.155.1.3975391. [DOI] [PubMed] [Google Scholar]
- 13.Labib M A, Prevedello D M, Carrau Ret al. A road map to the internal carotid artery in expanded endoscopic endonasal approaches to the ventral cranial base Neurosurgery 20141003448–471., discussion 471 [DOI] [PubMed] [Google Scholar]
- 14.Kennedy D W, Zinreich S J, Hassab M H. The internal carotid artery as it relates to endonasal sphenoethmoidectomy. Am J Rhinol. 1990;4(01):7–12. [Google Scholar]
- 15.Cashman E C, Macmahon P J, Smyth D. Computed tomography scans of paranasal sinuses before functional endoscopic sinus surgery. World J Radiol. 2011;3(08):199–204. doi: 10.4329/wjr.v3.i8.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unlu A, Meco C, Ugur H C, Comert A, Ozdemir M, Elhan A. Endoscopic anatomy of sphenoid sinus for pituitary surgery. Clin Anat. 2008;21(07):627–632. doi: 10.1002/ca.20707. [DOI] [PubMed] [Google Scholar]
- 17.Kölln K A, Senior B A. Conventional and endoscopic approaches to the pituitary: an integrated anatomical and computerized tomography study. Eur Radiol. 2006;16:2092–2099. doi: 10.1007/s00330-006-0208-3. [DOI] [PubMed] [Google Scholar]


