Abstract
Background
The introduction of immunotherapy in the treatment of non-small cell lung cancer (NSCLC) has resulted in a radical change in patients’ treatment responses and survival rates. The increased percentage of long survivors, improved toxicity profiles compared to chemotherapy, and the possible applications for different NSCLC scenarios, have led to immune checkpoint inhibitors (ICIs) becoming the cornerstone of NSCLC treatment. Therefore, the objective of this review is to describe the current and future perspectives of NSCLC treatment.
Methods
A systematic review according to the PRISMA criteria has been performed based on clinical trials with immunotherapy in NSCLC from the start of these treatments until June 2022.
Results
The use of ICIs is widespread across both first- and second-line treatments with anti-PD-1, anti-PD-L1, and anti-CTLA-4 drugs. New indications for immunotherapy in NSCLC have focused on adjuvant (atezolizumab) and neoadjuvant (nivolumab), with ICIs now present in all stages of NSCLC treatment. Given the promising results seen in clinical trials, new ICIs [anti- lymphocyte activation gene-3 (LAG-3) or IDO1] currently under development, will soon be used as standard treatment for NSCLC.
Conclusions
Immunotherapy is the mainstay of NSCLC treatment in all stages, including adjuvant, neoadjuvant and advanced tumors. The development of new molecules will revolutionize the treatment of NSCLC in the coming years.
Keywords: non-small cell lung cancer (NSCLC), immune checkpoint inhibitors (ICIs), anti-PD-1, anti-PD-L1, anti-CTLA-4
Highlight box.
Key findings
• Immunotherapy has been established as the mainstay of NSCLC treatment for all stages (adjuvant, neoadjuvant and advanced). atezolizumab is standardized for adjuvant treatment after surgery and chemotherapy in stages II–III and nivolumab for neoadjuvant treatment in stages IB–IIIA.
What is known and what is new?
• Immunotherapy (alone or in combination with chemotherapy) is the standard treatment for advanced or metastatic NSCLC in both first and second line.
• ICIs become the standard in NSCLC for adjuvant and neoadjuvant treatment. New ICIs in development [anti- lymphocyte activation gene-3 (LAG-3) or IDO1] are currently under study in different clinical trials, being the future of NSCLC treatment.
What is the implication, and what should change now?
• Unless certain contraindications, treatment of NSCLC at all stages should include immunotherapy. New clinical trials will assess the role of ICIs in non-chemotherapy combinations to improve treatment efficacy and reduce toxicity.
Introduction
Currently, over half of patients with non-small cell lung cancer (NSCLC) are diagnosed in advanced stages (stages IIIB/C or IV), which have no curative treatment options (1). Of neoplasms, lung cancer has the highest mortality rate worldwide (2,3). Although most NSCLC tumors are diagnosed as localized or locally advanced, more than 80% of patients develop metastases as the disease progresses (4). NSCLC treatment has undergone a revolution since the introduction of immunotherapy and immune checkpoint inhibitors (ICIs) in 2015 (5). Prior to this, standard treatment regimens for advanced or metastatic NSCLC involved platinum doublets, which provided an overall survival (OS) of 6–12 months (6,7). Following the introduction of ICIs, the median survival of NSCLC patients has doubled, with 5-year survival rates of approximately 20–30% in cases that are in the metastatic stage (8). In 2015, the Food and Drug Administration (FDA) approved pembrolizumab and nivolumab as second-line treatments for NSCLC (9). This has resulted in radical improvements in patient survival and quality of life.
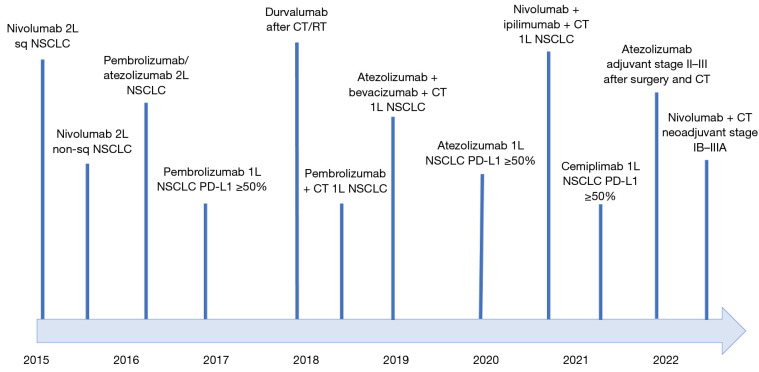
Immunotherapy using ICIs is based on three key pillars that involve acting on three immune system cellular receptors: PD-1, PD-L1, and CTLA-4 (10,11) (Table 1). Due to their importance, anti-PD-1 drugs have traditionally been the most commonly used for NSCLC treatment. However, drugs that target all three receptors have potential applications in the treatment of different NSCLC case presentations. These drugs, in monotherapy and combination with chemotherapy (CT) or each other, have been shown to improve patient survival and treatment response (12). Their toxicity profiles are similar to that of classic CT (13). Currently, 6 ICIs have been approved by the FDA for the treatment of NSCLC: ipilimumab, nivolumab, pembrolizumab, durvalumab, atezolizumab, and cemiplimab (14) (Figure 1). New ICIs are currently being studied alongside new immunotherapy modalities, such as oncolytic viruses or CAR-T cells (15,16).
Table 1. Main immune checkpoints antibodies and their principal indications for the treatment of solid tumors.
| Immune checkpoint inhibitors | Immunoglobulin type | Target molecule | Tumour type |
|---|---|---|---|
| Ipilimumab (MDX-010) | IgG-1κ | CTLA-4 | Advanced melanoma (alone second-line or in combination with nivolumab in first-line) |
| Advanced renal cancer (in combination with nivolumab in first-line) | |||
| Advanced lung cancer (in combination with chemotherapy and nivolumab in first-line) | |||
| Advanced pleural mesothelioma (in combination with nivolumab in first-line) | |||
| Advanced dMMR colorectal cancer (in combination with nivolumab in first-line) | |||
| Advanced squamous oesophageal cancer (in combination with nivolumab with PD-L1 ≥1%) | |||
| Pembrolizumab (MK-3475) | IgG-4κ | PD-1 | Advanced melanoma and adjuvant (alone) |
| First-line metastatic NSCLC (alone in first PD-L1 ≥50% or in combination with CT in PD-L1 <50%) | |||
| Second line metastatic NSCLC (alone with PD-L1 ≥1%) | |||
| Refractory Hodgkin lymphoma (alone) | |||
| Advanced bladder cancer (alone in second-line) | |||
| Advanced head and neck cancer (in first line in combination with CT in CPS ≥1 or monotherapy in CPS ≥50%) | |||
| Advanced renal cancer (in combination with lenvatinib or axitinib) or in adjuvant | |||
| All dMMR solid tumours (alone in first-line) | |||
| Advanced oesophageal cancer (plus CT in CPS ≥10%) | |||
| Advanced triple negative breast cancer (plus CT in CPS ≥10% or PD-L1+) | |||
| Neoadjuvant and adjuvant triple negative breast cancer (plus CT) | |||
| Advanced endometrial cancer (second-line with lenvatinib) | |||
| Advanced cervical cancer (first-line with CT +/− bevacizumab in CPS ≥1) | |||
| Nivolumab (MDX-1106) | IgG4 | PD-1 | Advanced melanoma (plus CT or alone) and adjuvant (alone) |
| First-line metastatic NSCLC (plus nivolumab and CT) | |||
| Second-line metastatic NSCLC (alone) | |||
| Advanced pleural mesothelioma (in combination with ipilimumab) | |||
| Advanced renal cancer (first-line with ipilimumab or cabozantinib and second-line alone) | |||
| Refractory Hodgkin lymphoma (alone) | |||
| Advanced bladder cancer (alone in second-line) | |||
| Advanced head and neck cancer (alone in second-line) | |||
| Advanced dMMR colorectal cancer (in combination with ipilimumab) | |||
| Advanced oesophageal cancer (plus CT or alone or plus ipilimumab) | |||
| Neoadjuvant in NSCLC plus CT (stage IB–III) | |||
| Atezolizumab (MPDL3280A) | IgG1 | PD-L1 | Advanced bladder cancer (alone in second line) |
| Metastatic NSCLC (in first-line in combination with CT and bevacizumab or in second-line alone) | |||
| Adjuvant NSCLC (stage II–III) after surgery and CT | |||
| Advanced SCLC (in first-line plus CT) | |||
| Durvalumab (MEDI4736) | IgG1 | PD-L1 | Locally advanced unresectable non-small cell lung cancer (after CT/RT with PD-L1 ≥1% in tumour cells) |
| Advanced SCLC (in first-line plus CT) | |||
| Avelumab (MSB0010718C) | IgG1 | PD-L1 | Metastatic Merkel cell carcinoma (alone) |
| Advanced urothelial cancer in maintenance after CT in first-line | |||
| Advanced renal cancer (plus axitinib in first-line) | |||
| Cemiplimab (REGN-2810) | IgG4 | PD-1 | Advanced squamous cell carcinoma (first-line alone) |
| Advanced nasal-cell carcinoma (after or not tolerance to vismodegib) | |||
| Advanced NSCLC (alone in first-line in PD-L1 ≥50%) | |||
| Dostarlimab (TSR-042) | IgG4 | PD-1 | Advanced dMMR endometrial cancer (alone in second-line) |
| Relatlimab (BMS-986016) | IgG4 | LAG-3 | Advanced melanoma (in combination with nivolumab in first-line)† |
†, only approved by FDA. dMMR, deficiency of the mismatch repair; CPS, Combined Positive Score; NSCLC, non-small cell lung cancer; CT, chemotherapy; SCLC, small cell lung cancer; RT, radiotherapy; FDA, Food and Drug Administration; LAG-3, lymphocyte activation gene-3.
Figure 1.
Development of the different ICIs along the last 10 years to nowadays in NSCLC. 2L, second-line; sq, squamous; NSCLC, non-small cell lung cancer; 1L, first-line; CT, chemotherapy; RT, radiotherapy; ICIs, immune checkpoint inhibitors.
The objective of this review was to describe and assess the present and future immunotherapy treatments available for NSCLC to garner a greater understanding of the revolution the oncology field is experiencing regarding the treatment of lung cancer. The systematic review was conducted and carried out using the quality standards detailed in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4218/rc).
Methods
Search strategy
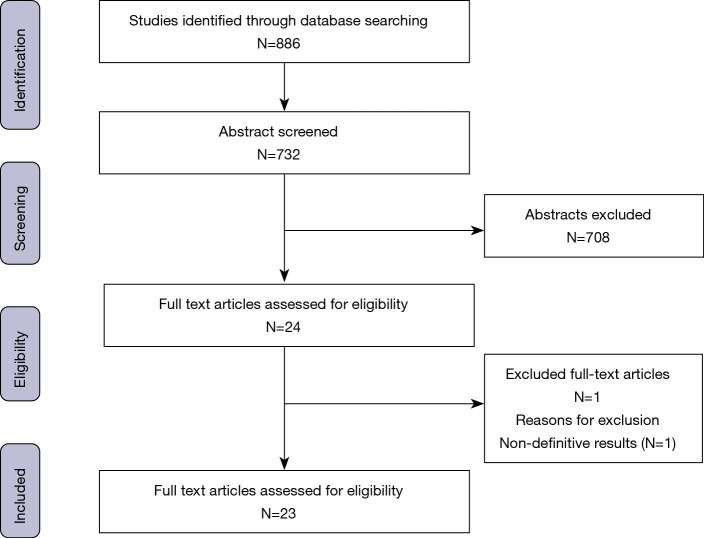
The clinical trials and studies included were found through searching several databases: PubMed, COCHRANE, Science Direct, EMBASE, and the clinical trial registry (www.clinicaltrials.gov). Studies and trials presented at the American Society of Clinical Oncology (ASCO) and European Society of Medical Oncology (ESMO) conferences were also included.
The studies selected for inclusion in this review involved the clinical trials and approval of the main ICIs, the approval records of the drugs, their indications by the FDA and the European Medicines Agency (EMA), and reviews and articles on immunotherapy as a treatment for lung cancer. No publication date parameters were used during the database searches; all studies published before June 30, 2022, were included. Studies based on clinical practice data have not been collected for publication due to the recent use of immunotherapy, so the review has been based on validated studies in this field that have allowed the approval of immunotherapy in the different scenarios of NSCLC.
Various text and medical subject headings (MeSH) combinations were used during the search: “Lung cancer OR lung OR NSCLC”, “Immunotherapy OR immune checkpoint inhibitors OR ICI”, “clinical trials OR approved drugs OR review”. Several combinations were used to search the databases: [“(Lung Cancer OR NSCLC) “AND” (Immunotherapy OR immune checkpoint inhibitors OR ICI)” AND/OR “(clinical trials OR approved drugs OR review)”]. All studies that provided current evidence on the current or future treatment of lung cancer using immunotherapy were considered. Flow diagram is in the Figure 2.
Figure 2.
Flow diagram of selected included and excluded studies.
Study selection and data extraction
Initially, the studies reviewing the main clinical trials that resulted in the approval of immunotherapy drugs for the treatment of NSCLC were selected. Subsequently, existing literature reviews were selected, as well as studies that involved data analysis from different hospitals. Abstracts that, due to their novelty or importance, influenced the oncology field were also included. Most of these abstracts were derived from the ASCO and ESMO congresses.
Two independent reviewers (Olivares-Hernández and González del Portillo) completed the data extraction and examination. Following this, a third reviewer (Miramontes-González) compared the results and assessed the consistency of the results with the current literature.
Results
When considering the treatment of NSCLC, it is critical that the presence of driver mutations is assessed before beginning immune therapy (17). In healthcare practice, analysis of several tumor mutations is recommended due to the therapeutic implications associated with the use of certain drugs: EGFR, KRAS, ALK, ROS1, BRAF, NTRK1/2/3, MET, and RET (18). Tumors with these driver mutations present different clinical characteristics compared to tumors. Therefore, the treatment approach should not initially involve immunotherapy treatments (19).
Furthermore, PD-L1 levels must be assessed to determine the correct treatment option for NSCLC patients (20). PD-L1 levels can be assessed using different; pharmaceutical companies typically use different methods. Levels are determined by immunohistochemistry and are currently the most important predictive biomarker for immunotherapy responses (21). Other biomarkers have been assessed, such as the tumor mutation burden (TMB) or mismatch repair (MMR) system deficiency (22,23); however, PD-L1 is the only biomarker that has shown predictive value regarding the response of NSCLC to ICIs.
Locally and locally advanced stage treatment
Multiple recent investigations have studied the role of immunotherapy in the adjuvant and neoadjuvant treatment of NSCLC (24). The most important study regarding adjuvant treatment in operable stages is IMpower010 (NCT02486718) (25), in which the efficacy of maintenance atezolizumab treatment was evaluated 1 year after platinum-based adjuvant CT in patients with stage IB–III NSCLC who underwent surgery. One year of maintenance atezolizumab treatment was shown to be more beneficial compared to best supportive care (BSC) for patients with stage II–IIIA tumors with PD-L1 expressed on ≥1% of tumor cells. After a median follow-up of 32.2 months, disease-free survival (DFS) was higher in the treatment group compared to the BSC group [HR =0.66 (95% CI: 0.59–0.88)]. After 2 years, DFS in the atezolizumab group was 74.5% compared to 61.0% in the placebo group. Following this study, in October 2021, the FDA approved the use of atezolizumab for use in the maintenance treatment of stage II–III NSCLC with PD-L1 expressed on ≥1% of tumor cells, following treatment with surgery and adjuvant CT.
Another interesting study regarding adjuvant therapy was the PEARLS/KEYNOTE-091 (NCT02504372) clinical trial (26). This study evaluated the efficacy of 1 year of maintenance pembrolizumab versus placebo in patients with stage IB–IIIA NSCLC that had been treated by surgery and possibly adjuvant CT. The pembrolizumab group had an average DFS of 53.6 versus 42.0 months in the placebo group [HR =0.76 (95% CI: 0.63–0.91)]. After 18 months, the DFS of the pembrolizumab group was 73.4% compared to 64.3% in the placebo group. There are several important differences between this study and the IMpower010 study. One is the IMpower010 study included more stage III participants, as well as a higher percentage of negative PD-L1 participants. While in the KEYNOTE-091 study, 14.1% of the patients did not receive adjuvant CT treatment. These are notable differences; therefore, the studies are hard to compare. Furthermore, the KEYNOTE-091 study is currently pending evaluation by the FDA.
Neoadjuvant therapy presents a challenge for the treatment of NSCLC due to over one-third of patients presenting with stage III or later at diagnosis (27). In stage IIIA tumors, over half of patients experience tumor recurrence despite surgical resection, with more than two-thirds relapsing at the systemic level (28). Because of these challenges, the combination of CT and neoadjuvant immunotherapy for the treatment of resectable stage III NSCLC has been an area of research interest. Compared to adjuvant treatment, the neoadjuvant treatment enables the early control of the disease at the systemic level (29). CheckMate-816 (NCT02998528) is the main study that has studied this treatment, evaluating the efficacy of neoadjuvant treatment with nivolumab plus platinum-based CT versus standard CT in resectable stage IB–IIIA NSCLC (30). The primary endpoints were event-free survival (EFS) and pathological complete response (pCR). The EFS of the nivolumab group was 31.6 months compared to 20.8 months in the CT-only group [HR =0.63 (95% CI: 0.43–0.91)]. The pCR in the nivolumab group was 24.0% vs. 2.2% in the CT-only group [odds ratio 13.94 (99% CI: 3.49–55.75)]. Following this study, in March 2022, the FDA approved the combination of CT and nivolumab as a neoadjuvant treatment for resectable stage IB–IIIA NSCLC. Several other investigating neoadjuvant therapies are currently underway, such as KEYNOTE-671 (NCT03425643) (31), which is investigating the combination of pembrolizumab with neoadjuvant CT and subsequent post-surgery maintenance pembrolizumab and IMpower030 trial (NCT03456063) (32), which is following a similar protocol using atezolizumab.
The PACIFIC trial is the most important and well-known studying involving patients with unresectable stage III (IIIB/C) NSCLC (33,34). This study evaluated the efficacy of durvalumab maintenance treatment after concomitant chemoradiation therapy (CT/RT). The progression-free survival (PFS) in the durvalumab group was 16.8 months compared to 5.6 months in the placebo group [HR =0.52 (95% CI: 0.42–0.65)]. After 18 months, the PFS rate was 44.2% in the durvalumab group versus 27% in the placebo group. Following the publication of this study, in February 2018, the FDA approved the use of durvalumab for the maintenance treatment of unresectable stage III NSCLC following non-progressed concomitant CT/RT treatment. The KEYLYNK-012 study is currently underway (35), comparing durvalumab with two experimental groups with concurrent CT/RT plus pembrolizumab, with subsequent maintenance with pembrolizumab +/− olaparib. The phase 2 KEYNOTE-799 (NCT03631784) trial evaluated patients with stage IIIA/B/C tumors that were initially unresectable but had surgical potential (36). The efficacy of pembrolizumab combined with neoadjuvant platinum-based CT followed by concomitant CT/RT with pembrolizumab and subsequent maintenance pembrolizumab was assessed in two cohorts separated based on histology. An objective response rate (ORR) of 72–74% was reported, with OS not reaching at the time of the study. However, the results indicate a potential treatment path for patients with stage III tumors that have the potential to be resected.
Advanced stage treatment
Following the FDA’s approval of nivolumab as the first neoadjuvant immunotherapy treatment for NSCLC on March 4, 2022, the progressive development of different therapeutic protocols for NSCLC treatment has led to the establishment of these protocols as a standard and fundamental component of NSCLC therapy (37). In recent years, immunotherapy has evolved from being a second- to first-line treatment. However, no patient with NSCLC (without driver mutations) can receive ICIs unless contraindicated. PD-L1 expression levels determine whether a patient should receive immunotherapy as a first- or second-line treatment (38).
First-line treatment for PD-L1 ≥50%
Pembrolizumab was the first drug approved for the treatment of patients with high PD-L1 expression (39). In October 2016, the FDA approved its use as a first-line monotherapy for NSCLC cases with PD-L1 expression ≥50%. This approval was based on the results of the KEYNOTE-024 (NCT02142738) study (40), which evaluated the efficacy of pembrolizumab versus platinum-based CT as first-line treatments for NSCLC with PD-L1 ≥50%. The pembrolizumab group had a PFS of 10.3 months compared to 6 months for the CT group [HR =0.50 (95% CI: 0.37–0.68)]. The ORR was 44.8% in the pembrolizumab group versus 27.8% in the CT group (41).
In May 2020, atezolizumab became the second drug to be approved as a monotherapy treatment for NSCLC with PD-L1 ≥50%. The IMpower110 study (NCT02409342) compared atezolizumab with standard CT in NSCLC patients with PD-L1 ≥1% (42). Of patients with PD-L1 ≥50%, those in the atezolizumab group had a PFS of 8.1 months compared to 5 months in the CT-only group [HR =0.63 (95% CI: 0.45–0.88)]. The ORR in the atezolizumab group was 38.3% compared to 28.6% in the CT-only group. In February 2021, Cemiplimab became the most recent drug to be approved as a monotherapy treatment for NSCLC with PD-L1 ≥50%, following the results of the EMPOWER-Lung 1 trial (NCT03088540) (43). This trial compared cemiplimab monotherapy with standard CT in patients with NSCLC and PD-L1 ≥50%. In the cemiplimab group, PFS was 8.2 months compared to 5.7 months in the CT group [HR =0.54 (95% CI: 0.43–0.68)]. Furthermore, ORR was 39% in the cemiplimab group versus 20% in the CT group.
Therefore, there are currently three approved drugs (all monotherapies) for the first-line treatment of NSCLC with PD-L1 ≥50%: pembrolizumab, atezolizumab, and cemiplimab. Due to the burden of lung cancer, such patients require rapid treatment responses. The combination of CT and ICIs enables more rapid responses compared to ICIs alone. Therefore, for highly symptomatic patients with intermediate or low PD-L1 expressions, other regimens should be considered as first-line treatments.
First-line treatment for PD-L1 <50%
Currently, the combination of platinum-doublet CT treatment with pembrolizumab is the recommended first-line treatment option for patients with PD-L1 <50%, barring specific contraindications or clinical suggestions where other treatment options may be more appropriate. The recommendation for this combination is based on two studies: KEYNOTE-189 and KEYNOTE-407 (44,45). The KEYNOTE-189 study evaluated the combination of 4 cycles of platinum-containing pembrolizumab and pemetrexed with subsequent maintenance pembrolizumab and pemetrexed maintenance versus standard first-line CT for non-squamous NSCLC, independent of PD-L1 expression (46). The PFS of the pembrolizumab group was 8.8 months compared to 4.9 months in the control group [HR =0.52 (95% CI: 0.43–0.64)]. Median OS was not reached in the pembrolizumab group, while it was 11.2 months in the control group [HR =0.49 (95% CI: 0.38–0.64)]. The ORR was 47.6% in the pembrolizumab group versus 18.9% in the control group.
The KEYNOTE-407 used the same experimental design as the KEYNOTE-189 study but in patients with squamous NSCLC (47). The CT combination used was pembrolizumab plus paclitaxel or nab-paclitaxel and platinum, with subsequent pembrolizumab maintenance. The PFS of the pembrolizumab group was 6.4 months compared to 4.8 months in the placebo group [HR =0.56 (95% CI: 0.45–0.70)]. In the pembrolizumab group, OS was 15.9 versus 11.3 months in the placebo group [HR =0.64 (95% CI: 0.49–0.85)]. The ORR rates were 57.9% and 38.4% in the pembrolizumab and placebo groups, respectively. Based on these results, the FDA approved the use of a combination treatment of pembrolizumab plus CT as a first-line treatment in non-squamous NSCLC in August 2018 and for squamous tumors in October 2018.
Alternative treatments are available depending on the clinical and tumor characteristics of the patient. The IMpower150 study (NCT02366143) studied the efficacy of atezolizumab with platinum-doublet CT plus paclitaxel and bevacizumab, with subsequent atezolizumab and bevacizumab maintenance, as a first-line treatment for non-squamous NSCLC (48), regardless of PD-L1 expression. This treatment was compared with CT plus bevacizumab (49). In the atezolizumab group, OS in was 19.2 months compared to 14.7 months in the control group [HR =0.78 (95% CI: 0.64–0.96)]. PFS was 8.3 and 6.8 months [HR =0.62 (95% CI: 0.52–0.74)] and ORR was 63.5% and 48% in the atezolizumab and control groups, respectively. Following this study, the combination of CT (platinum plus paclitaxel) plus bevacizumab plus atezolizumab was approved by the FDA in December 2018 for the first-line treatment of non-squamous NSCLC.
Two cycles of nivolumab plus ipilimumab and CT is another first-line treatment option for NSCLC, as studied in the CheckMate 9LA clinical trial (NCT03215706) (50). This study demonstrated the superiority of a combined treatment approach using nivolumab and ipilimumab with CT, with subsequent nivolumab and ipilimumab maintenance compared with standard CT. Due to this study, the FDA approved this first-line treatment in May 2020 as a possible alternative to the combination of pembrolizumab with CT.
Second-line treatments
For patients who have not received first-line immunotherapy, second-line immunotherapy for NSCLC may be considered (51). There are three drugs approved for this indication after progression to first line with platinum doublet, which are nivolumab, pembrolizumab, and atezolizumab (52). The first drug approved by the FDA for the treatment of NSCLC (squamous histology) in the second line after progression to platinum in March 2015 was nivolumab. The CheckMate 017 study (NCT01642004) showed superiority of nivolumab versus the docetaxel control group both in terms of OS (9.2 vs. 6.0 months; HR =0.59, 95% CI: 0.44–0.79) and PFS (3.5 vs. 2.8 months, HR =0.62, 95% CI: 0.47–0.81) (53). Subsequently, in October 2015, the indication for non-squamous tumors was extended due to the results of the CheckMate 057 study (which compared nivolumab versus docetaxel) (54). The study showed OS superiority of nivolumab versus docetaxel (12.2 vs. 9.4 months; HR 0.73, 95% CI: 0.59–0.89). However, there was no improvement in terms of PFS (2.3 vs. 4.2 months).
In October 2016, pembrolizumab was approved as a second-line treatment for NSCLC with PD-L1 ≥1% following progression to platinum-based CT. The KEYNOTE-010 (NCT01905657) study investigated the efficacy of pembrolizumab versus docetaxel as second-line treatments following progression to platinum CT in tumors where PD-L1 ≥1% (55). Pembrolizumab was found to improve OS compared to CT alone. However, similar to the CheckMate 057 study, no improvement was observed regarding PFS. The most recent study in this area is the OAK clinical trial (56), which compared atezolizumab with docetaxel as second-line treatments for NSCLC, regardless of PD-L1 expression levels. OS was higher in the atezolizumab group OS for both PD-L1 negative and positive patients. Following this, the FDA approved the use of this indication in October 2016. The summary of the different clinical trials with immunotherapy in NSCLC is in the Table 2.
Table 2. Main clinical trials in immunotherapy to NSCLC with approved by the FDA.
| Trial | Phase | Stage | Histology | PD-L1 | Trial design | Results | Approved by FDA |
|---|---|---|---|---|---|---|---|
| IMpower010 | 3 | Adjuv IB–III | NSCLC | All | Atezolizumab vs. placebo post-surgery and CT | Follow 32.2 m (HR =0.66); DFS 74.5% vs. 61.0% (24 m) (II–IIIA and PD-L1 ≥1%) | Oct/21 stage II–III NSCLC PD-L1 ≥1% |
| CheckMate 816 | 3 | Neoadj IB–IIIA | NSCLC | All | Nivolumab + CT vs. CT | EFS 31.6 vs. 20.8 m; pCR 24.0% vs. 2.2% | March 2022 stage IB–IIIA NSCLC all PD-L1 |
| PACIFIC | 3 | Adjuv UR III | NSCLC | All | Durvalumab vs. placebo post CT/RT | PFS 16.8 vs. 5.6 m; PFS 44.2 vs. 27% (18 m) | Feb/18 UR stage III post CT/RT |
| KEYNOTE-024 | 3 | Advanced stages (1L) | NSCLC | PD-L1 ≥50% | Pembrolizumab vs. CT | PFS 10.3 vs. 6 m; ORR 44.8% vs. 27.8% | Oct/16 1L advanced NSCLC PD-L1 ≥50% |
| IMpower110 | 3 | Advanced stages (1L) | NSCLC | PD-L1+ | Atezolizumab vs. CT | PFS 8.1 vs. 5 m (PD-L1 ≥50%); ORR 38.3% vs. 28.6% | May/20 1L advanced NSCLC PD-L1 ≥50% |
| EMPOWER-Lung 1 | 3 | Advanced stages (1L) | NSCLC | All | Cemiplimab vs. CT | PFS 8.2 vs. 5.7 m (PD-L1 ≥50%); ORR 39% vs. 20% | Feb/21 1L advanced NSCLC PD-L1 ≥50% |
| KEYNOTE-189 | 3 | Advanced stages (1L) | Non-Sq NSCLC | All | Pembrolizumab + CT vs. CT | PFS 8.8 vs. 4.9 m; ORR 47.6% vs. 18.9% | August/18 1L advanced non-Sq NSCLC all PD-L1 |
| KEYNOTE-407 | 3 | Advanced stages (1L) | Sq NSCLC | All | Pembrolizumab + CT vs. CT | PFS 6.4 vs. 4.8 m; ORR 57.9 vs. 38.4% | Oct/18 1L advanced Sq NSCLC all PD-L1 |
| IMpower150 | 3 | Advanced stages (1L) | Non-Sq NSCLC | All | Atezolizumab + CT vs. CT | PFS 8.3 vs. 6.8 m; ORR 63.5 vs. 48% | Dec/18 1L advanced non-Sq NSCLC all PD-L1 |
| CheckMate9LA | 3 | Advanced stages (1L) | NSCLC | All | Nivolumab + ipilimumab + CT vs. CT | OS 14.1 vs. 10.7 m (HR =0.69: 0.55–0.87) | May/20 1L advanced NSCLC all PD-L1 |
| CheckMate 017 | 3 | Advanced stages (2L) | Sq NSCLC | All | Nivolumab vs. docetaxel | OS 9.2 vs. 6 m; PFS 3.5 vs. 2.8 m | March/2015 2L advanced NSCLC all PD-L1 |
| CheckMate 057 | 3 | Advanced stages (2L) | Non-Sq NSCLC | All | Nivolumab vs. docetaxel | OS 12.2 vs. 9.4 m; PFS 2.3 vs. 4.2 m | Oct/2015 2L advanced NSCLC all PD-L1 |
| KEYNOTE-010 | 3 | Advanced stages (2L) | NSCLC | PD-L1+ | Pembrolizumab vs. docetaxel | OS 12.7 vs. 8.5 m; PFS 4.0 vs. 4.0 m | Oct/16 2L advanced NSCLC PD-L1 ≥1% |
| OAK | 3 | Advanced stages (2L) | NSCLC | All | Atezolizumab vs. docetaxel | OS 13.8 vs. 9.6 (HR =0.73: 0.62–0.87) | Oct/16 2L advanced NSCLC all PD-L1 |
NSCLC, non-small cell lung cancer; FDA, Food and Drug Administration; adjuv, adjuvant; CT, chemotherapy; DFS, disease-free survival; neoadj, neoadjuvant; EFS, event-free survival; pCR, pathological complete response; sq, squamous; UR, unresectable; RT, radiotherapy; PFS, progression-free survival; 1L, first-line; ORR, objective response rate; OS, overall survival; 2L, second-line.
Novel ICIs
Current immune therapies under development for the treatment of NSCLC go far beyond those that target the classic receptors (PD-1, PD-L1, and CTLA-4). In most cases, resistance to these drugs develops over time. Current clinical trials are showing promising results regarding new drugs against different molecular targets (57) (Table 3).
Table 3. Main clinical trials in research on the new molecular targets of ICIs in NSCLC.
| Trial | Phase | Drug | Trial design | Stage and indication |
|---|---|---|---|---|
| NCT03625323 | 2 | LAG-3: IMP321 (eftilagimod alpha) | Pembrolizumab + IMP321 | Untreated metastatic NSCLC |
| NCT04623775 | 2 | LAG-3: BMS-986016 (relatlimab) | Relatlimab + nivolumab + CT vs. nivolumab + CT | First line metastatic NSCLC |
| NCT04140500 | 1 | LAG-3: RO7247669 | Dose escalation study of bispecific antibody PD-1-LAG-3 | Metastatic NSCLC |
| NCT03322540 | 2 | IDO1: INCB024360 (epacadostat) | Epacadostat + pembrolizumab vs. pembrolizumab | First line metastatic NSCLC and high levels of PD-L1 |
| NCT04294810 | 3 | TIGIT: MTIG7192A (tiragolumab) | Tiragolumab + atezolizumab vs. atezolizumab | First line metastatic NSCLC with PD-L1 ≥50% |
| NCT04738487 | 3 | TIGIT: MK-7684A (vibostolimab) | Vibostolimab + pembrolizumab vs. pembrolizumab | Metastatic NSCLC with PD-L1 ≥1% |
| NCT03822351 | 2 | NKG2A: IPH2201 (monalizumab) | Durvalumab vs. durvalumab + oleclumab vs. durvalumab + monalizumab | Stage III NSCLC after treatment with CT/RT |
| CD73: MEDI-9447 (oleclumab) | ||||
| NCT03381274 | 1/2 | CD73: MEDI-9447 (oleclumab) | Oleclumab + osimertinib vs. MEDI9447 + AZD4635 | EGFRm NSCLC |
| NCT03549000 | 1 | CD73: NZV930 | NZV930 vs. NZV930 + PDR001 vs. NZV930 + NIR178 vs. NZV930 + PDR001 + NIR178 | Metastatic NSCLC |
| NCT02475213 | 1 | B7-H3: MGA271 (enoblituzumab) | Enoblituzumab + pembrolizumab | Metastatic NSCLC |
| NCT02381314 | 1 | B7-H3: MGA271 (enoblituzumab) | Enoblituzumab + ipilimumab | Metastatic NSCLC |
| NCT03729596 | 1/2 | B7-H3·: MGC018 | MGC018 vs. MGC018 + retifanlimab | Metastatic NSCLC |
| NCT04081688 | 1 | CD27: CDX-1127 (varlimumab) | Varlimumab + atezolizumab + SBRT | Metastatic NSCLC |
| NCT03708328 | 1 | TIM3: RO7121661 | Dose escalation study of bispecific antibody PD-1/TIM3 | Metastatic NSCLC |
ICIs, immune checkpoint inhibitors; NSCLC, non-small cell lung cancer; LAG-3, lymphocyte activation gene-3; CT, chemotherapy; RT, radiotherapy.
Lymphocyte activation gene-3 (LAG-3)
LAG-3 is a type I transmembrane protein primarily activated in T, NK, B, and plasmacytoid dendritic cells. LAG-3 is structurally similar to CD4 receptors; however, it binds to the MHC type II complex with greater affinity than CD4. A study has demonstrated a relationship between the PD-1 receptor and LAG-3, with the elimination or blocking of both molecules inducing lymphocyte infiltration in tumors (58). Several clinical trials investigating the efficacy of anti-LAG-3 drugs in the treatment of NSCLC are currently underway. One of the main studies is the phase 2 trial NCT03625323, which is investigating the use of pembrolizumab plus the anti-LAG-3 drug IMP321 in patients with previously untreated metastatic NSCLC (59). The first results are expected at the end of 2023. NCT04623775 is another phase 2 trial that is evaluating the efficacy of the combination of the anti-LAG-3 drug relatlimab with nivolumab plus CT as a first-line treatment for NSCLC. The combination of relatlimab and nivolumab has already been by the FDA as an effective treatment for previously untreated advanced melanoma (60). Therefore, it is one of the more promising treatments currently being studied (61). The first results from this study are expected in 2024.
Indoleamine 2,3-dioxygenase 1 (IDO1)
IDO1 plays a critical role in regulating immune escape. The abnormal activation of IDO1 leads to lower tryptophan reserves in tumor microenvironments, resulting in a decrease in T cells. Several IDO1 inhibitors are at different stages of development (62). The most promising anti-IDO1 drug is epacadostat, which is a highly selective inhibitor of IDO1 that decreases tryptophan metabolism (63). The phase 2 KEYNOTE-654-05/ECHO-305-05 (NCT03322540) clinical trial is evaluating the efficacy of epacadostat with pembrolizumab as a first-line treatment for NSCLC with elevated PD-L1 levels (64).
T-cell immunoreceptor with IG and ITIM domains (TIGIT)
TIGIT is a receptor expressed on activated T cells, NK cells, and regulatory T cells (Tregs). Blocking both PD-1 and TIGIT has shown anti-tumor potential in animal models (65). The phase 2 CITYSCAPE trial compared the combination of anti-TIGIT drug tiragolumab and atezolizumab versus atezolizumab alone as a first-line treatment for NSCLC with PD-L1 ≥50% (66). The tiragolumab group showed improvement in PFS and ORR compared to the control group. A phase 3 clinical trial is currently underway to further validate these results (NCT04294810). Vibostolimab is another promising anti-TIGIT drug. The phase 3 clinical trial NCT04738487 is currently evaluating the combination of this drug with pembrolizumab as a first-line treatment for NSCLC patients with positive PD-L1 expression (67).
CD73
CD73, also known as ecto-5'-nucleotidase, is an enzyme expressed on multiple immune cells (68). The immunosuppressive functions of Treg cells depend on the expression of CD73 (69). Blocking this receptor leads to an increase in tumor response. One of the main clinical trials in this field is the phase 2 COAST study (NCT03822351) (70). This clinical trial is evaluating the efficacy of a combined regimen of oleclumab and durvalumab in patients with stage III NSCLC following treatment with CT/RT. The preliminary results of the study demonstrated an improvement in PFS compared to durvalumab monotherapy.
B7-H3
The B7–H3 receptor is also known as CD276. In patients with NSCLC, it has been shown to play a cooperative role in immune evasion alongside Treg cells (71). Different studies have assessed the role of this receptor in the treatment of NSCLC. The drug enoblituzumab is currently being studied in multiple phase 1 studies evaluating its efficacy in combination with pembrolizumab (NCT02475213) and ipilimumab (NCT02381314) (72).
There are many other molecules within the field of ICIs that have promise, such as those that act on the T-cell Immunoglobulin and mucin-domain containing-3 (TIM-3) receptor (73), the NK Group 2 member A (NKG2A) molecule (74), and the V-domain immunoglobulin suppressor of T-cell activation (VISTA) (75). Trials assessing the efficacy of these molecules are currently underway. However, the results are expected to confirm that these drugs will play an important role in the further development of NSCLC treatment.
Discussion
In addition to the different molecules currently being investigated, there are different treatment combinations that involve ICIs and other molecules that may have potential future applications. Cell therapy with CAR-T cells could play a role in the treatment of NSCLC in the coming years (76). One of the most promising possible treatment combinations involves poly (ADP-ribose) polymerase (iPARP) inhibitors and ICIs. Cell damage induced by tobacco and other carcinogens leads to alterations in DNA repair pathways. These routes could be used for NSCLC treatment in combination with immunotherapy. Three clinical trials are currently evaluating the combination of ICIs with iPARP for the treatment of NSCLC. The first of these is the phase 3 KEYLYNK-006 clinical trial. This trial is evaluating the efficacy of maintenance pembrolizumab with olaparib following CT versus pembrolizumab and pemetrexed in non-squamous NSCLC (77). Another is the phase 3 KEYLYNK-008 trial that is investigating the efficacy of maintenance with pembrolizumab and olaparib versus pembrolizumab monotherapy in patients with squamous NSCLC (78). The latest of these studies is the phase 2 ORION clinical trial, which is evaluating the efficacy of post-CT maintenance with durvalumab and olaparib in NSCLC. These studies have demonstrated significant potential future. Based on preclinical model results, iPARP is expected to become a standard treatment for NSCLC tumors.
It is important to highlight the role of cell therapy with CAR-T cells in NSCLC. NSCLC has multiple different molecular targets which can be acted upon with targeted drugs, such as the epidermal growth factor receptor (EGFR) (79), the anaplastic lymphoma kinase (ALK), or the human epidermal growth factor receptor 2 (HER2). Using CAR-T cell infusions, these targets can be acted upon with much greater selectivity than current drug options (80). Due to the importance of these targets in the development and lifecycle of NSCLC, cell therapy is of particular importance in its treatment compared to other solid neoplasms.
Conclusions
In conclusion, immune therapy is the present and future of NSCLC treatment. Optimal NSCLC treatment is not currently possible without immunotherapy. New molecular targets will enable the resolution of the resistance problem that occurs with PD-1, PDL1, and CTLA-4 inhibitors, as well as responses and survival that were unimaginable in NSCLC patients a decade ago. The combination of these molecules with other drugs, such as iPARPs, will also play a key role in the future of NSCLC treatment.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-4218/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4218/coif). JPMG serves as an unpaid editorial board member of Annals of Translational Medicine from June 2022 to May 2024. The other authors have no conflicts of interest to declare.
References
- 1.Nooreldeen R, Bach H. Current and Future Development in Lung Cancer Diagnosis. Int J Mol Sci 2021;22:8661. 10.3390/ijms22168661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 3.Siegel RL, Miller KD, Fuchs HE, et al. Cancer Statistics, 2021. CA Cancer J Clin 2021;71:7-33. 10.3322/caac.21654 [DOI] [PubMed] [Google Scholar]
- 4.Woodard GA, Jones KD, Jablons DM. Lung Cancer Staging and Prognosis. Cancer Treat Res 2016;170:47-75. 10.1007/978-3-319-40389-2_3 [DOI] [PubMed] [Google Scholar]
- 5.Tsao AS, Scagliotti GV, Bunn PA, Jr, et al. Scientific Advances in Lung Cancer 2015. J Thorac Oncol 2016;11:613-38. 10.1016/j.jtho.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 6.Brodowicz T, Krzakowski M, Zwitter M, et al. Cisplatin and gemcitabine first-line chemotherapy followed by maintenance gemcitabine or best supportive care in advanced non-small cell lung cancer: a phase III trial. Lung Cancer 2006;52:155-63. 10.1016/j.lungcan.2006.01.006 [DOI] [PubMed] [Google Scholar]
- 7.Griesinger F, Korol EE, Kayaniyil S, et al. Efficacy and safety of first-line carboplatin-versus cisplatin-based chemotherapy for non-small cell lung cancer: A meta-analysis. Lung Cancer 2019;135:196-204. 10.1016/j.lungcan.2019.07.010 [DOI] [PubMed] [Google Scholar]
- 8.Reck M, Remon J, Hellmann MD. First-Line Immunotherapy for Non-Small-Cell Lung Cancer. J Clin Oncol 2022;40:586-97. 10.1200/JCO.21.01497 [DOI] [PubMed] [Google Scholar]
- 9.Kwok G, Yau TC, Chiu JW, et al. Pembrolizumab (Keytruda). Hum Vaccin Immunother 2016;12:2777-89. 10.1080/21645515.2016.1199310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruiz-Cordero R, Devine WP. Targeted Therapy and Checkpoint Immunotherapy in Lung Cancer. Surg Pathol Clin 2020;13:17-33. 10.1016/j.path.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 11.Suresh K, Naidoo J, Lin CT, et al. Immune Checkpoint Immunotherapy for Non-Small Cell Lung Cancer: Benefits and Pulmonary Toxicities. Chest 2018;154:1416-23. 10.1016/j.chest.2018.08.1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Broderick SR. Adjuvant and Neoadjuvant Immunotherapy in Non-small Cell Lung Cancer. Thorac Surg Clin 2020;30:215-20. 10.1016/j.thorsurg.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 13.Kennedy LB, Salama AKS. A review of cancer immunotherapy toxicity. CA Cancer J Clin 2020;70:86-104. 10.3322/caac.21596 [DOI] [PubMed] [Google Scholar]
- 14.Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. 10.6004/jnccn.2022.0025 [DOI] [PubMed] [Google Scholar]
- 15.Guo ZS, Lu B, Guo Z, et al. Vaccinia virus-mediated cancer immunotherapy: cancer vaccines and oncolytics. J Immunother Cancer 2019;7:6. 10.1186/s40425-018-0495-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qu J, Mei Q, Chen L, et al. Chimeric antigen receptor (CAR)-T-cell therapy in non-small-cell lung cancer (NSCLC): current status and future perspectives. Cancer Immunol Immunother 2021;70:619-31. 10.1007/s00262-020-02735-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dantoing E, Piton N, Salaün M, et al. Anti-PD-1/PD-L1 Immunotherapy for Non-Small Cell Lung Cancer with Actionable Oncogenic Driver Mutations. Int J Mol Sci 2021;22:6288. 10.3390/ijms22126288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sankar K, Gadgeel SM, Qin A. Molecular therapeutic targets in non-small cell lung cancer. Expert Rev Anticancer Ther 2020;20:647-61. 10.1080/14737140.2020.1787156 [DOI] [PubMed] [Google Scholar]
- 19.da Cunha Santos G, Shepherd FA, Tsao MS. EGFR mutations and lung cancer. Annu Rev Pathol 2011;6:49-69. 10.1146/annurev-pathol-011110-130206 [DOI] [PubMed] [Google Scholar]
- 20.Patel SP, Kurzrock R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol Cancer Ther 2015;14:847-56. 10.1158/1535-7163.MCT-14-0983 [DOI] [PubMed] [Google Scholar]
- 21.Fournel L, Wu Z, Stadler N, et al. Cisplatin increases PD-L1 expression and optimizes immune check-point blockade in non-small cell lung cancer. Cancer Lett 2019;464:5-14. 10.1016/j.canlet.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 22.Olivares-Hernández A, Del Barco Morillo E, Parra Pérez C, et al. Influence of DNA Mismatch Repair (MMR) System in Survival and Response to Immune Checkpoint Inhibitors (ICIs) in Non-Small Cell Lung Cancer (NSCLC): Retrospective Analysis. Biomedicines 2022;10:360. 10.3390/biomedicines10020360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bodor JN, Boumber Y, Borghaei H. Biomarkers for immune checkpoint inhibition in non-small cell lung cancer (NSCLC). Cancer 2020;126:260-70. 10.1002/cncr.32468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanna NH, Schneider BJ, Temin S, et al. Therapy for Stage IV Non-Small-Cell Lung Cancer Without Driver Alterations: ASCO and OH (CCO) Joint Guideline Update. J Clin Oncol 2020;38:1608-32. 10.1200/JCO.19.03022 [DOI] [PubMed] [Google Scholar]
- 25.Felip E, Altorki N, Zhou C, et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB-IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. Lancet 2021;398:1344-57. 10.1016/S0140-6736(21)02098-5 [DOI] [PubMed] [Google Scholar]
- 26.Paz-Ares L, O`Brien MER, Mauer M, et al. Pembrolizumab (pembro) versus placebo for early-stage non-small cell lung cancer (NSCLC) following complete resection and adjuvant chemotherapy (chemo) when indicated: Randomized, triple-blind, phase III EORTC-1416- LCG/ETOP 8-15 e PEARLS/KEYNOTE-091 study. Ann Oncol 2022;33:451-3. 10.1016/j.annonc.2022.02.224 [DOI] [Google Scholar]
- 27.Kang J, Zhang C, Zhong WZ. Neoadjuvant immunotherapy for non-small cell lung cancer: State of the art. Cancer Commun (Lond) 2021;41:287-302. 10.1002/cac2.12153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jazieh AR, Zeitouni M, Alghamdi M, et al. Management guidelines for stage III non-small cell lung cancer. Crit Rev Oncol Hematol 2021;157:103144. 10.1016/j.critrevonc.2020.103144 [DOI] [PubMed] [Google Scholar]
- 29.Forde PM, Chaft JE, Smith KN, et al. Neoadjuvant PD-1 Blockade in Resectable Lung Cancer. N Engl J Med 2018;378:1976-86. 10.1056/NEJMoa1716078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Forde PM, Spicer J, Lu S, et al. Neoadjuvant nivolumab plus Chemotherapy in Resectable Lung Cancer. N Engl J Med 2022;386:1973-85. 10.1056/NEJMoa2202170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsuboi M, Luft A, Ursol G, et al. 1235TiP Perioperative pembrolizumab + platinum-based chemotherapy for resectable locally advanced non-small cell lung cancer: The phase III KEYNOTE-671 study. Ann Oncol 2020;31:S801-2. 10.1016/j.annonc.2020.08.1437 [DOI] [Google Scholar]
- 32.Peters S, Kim AW, Solomon B, et al. IMpower030: Phase III study evaluating neoadjuvant treatment of resectable stage II-IIIB non-small cell lung cancer (NSCLC) with atezolizumab (atezo) + chemotherapy. Ann Oncol 2019;30:II30. 10.1093/annonc/mdz064.014 [DOI] [Google Scholar]
- 33.Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:1919-29. 10.1056/NEJMoa1709937 [DOI] [PubMed] [Google Scholar]
- 34.Spigel DR, Faivre-Finn C, Gray JE, et al. Five-Year Survival Outcomes From the PACIFIC Trial: Durvalumab After Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. J Clin Oncol 2022;40:1301-11. 10.1200/JCO.21.01308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jabbour SK, Cho BC, Bria E, et al. Rationale and Design of the Phase III KEYLYNK-012 Study of Pembrolizumab and Concurrent Chemoradiotherapy Followed by Pembrolizumab With or Without Olaparib for Stage III Non-Small-Cell Lung Cancer. Clin Lung Cancer 2022;23:e342-6. 10.1016/j.cllc.2022.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jabbour SK, Lee KH, Frost N, et al. Pembrolizumab Plus Concurrent Chemoradiation Therapy in Patients With Unresectable, Locally Advanced, Stage III Non-Small Cell Lung Cancer: The Phase 2 KEYNOTE-799 Nonrandomized Trial. JAMA Oncol 2021. [Epub ahead of print]. doi: . 10.1001/jamaoncol.2021.2301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma P, Allison JP. The future of immune checkpoint therapy. Science 2015;348:56-61. 10.1126/science.aaa8172 [DOI] [PubMed] [Google Scholar]
- 38.Tsoukalas N, Kiakou M, Tsapakidis K, et al. PD-1 and PD-L1 as immunotherapy targets and biomarkers in non-small cell lung cancer. J BUON 2019;24:883-8. [PubMed] [Google Scholar]
- 39.Aguilar EJ, Ricciuti B, Gainor JF, et al. Outcomes to first-line pembrolizumab in patients with non-small-cell lung cancer and very high PD-L1 expression. Ann Oncol 2019;30:1653-9. 10.1093/annonc/mdz288 [DOI] [PubMed] [Google Scholar]
- 40.Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. 10.1056/NEJMoa1606774 [DOI] [PubMed] [Google Scholar]
- 41.Reck M, Rodríguez-Abreu D, Robinson AG, et al. Updated Analysis of KEYNOTE-024: Pembrolizumab Versus Platinum-Based Chemotherapy for Advanced Non-Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score of 50% or Greater. J Clin Oncol 2019;37:537-46. 10.1200/JCO.18.00149 [DOI] [PubMed] [Google Scholar]
- 42.Herbst RS, Giaccone G, de Marinis F, et al. atezolizumab for First-Line Treatment of PD-L1-Selected Patients with NSCLC. N Engl J Med 2020;383:1328-39. 10.1056/NEJMoa1917346 [DOI] [PubMed] [Google Scholar]
- 43.Sezer A, Kilickap S, Gümüş M, et al. Cemiplimab monotherapy for first-line treatment of advanced non-small-cell lung cancer with PD-L1 of at least 50%: a multicentre, open-label, global, phase 3, randomised, controlled trial. Lancet 2021;397:592-604. 10.1016/S0140-6736(21)00228-2 [DOI] [PubMed] [Google Scholar]
- 44.Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:2078-92. 10.1056/NEJMoa1801005 [DOI] [PubMed] [Google Scholar]
- 45.Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N Engl J Med 2018;379:2040-51. 10.1056/NEJMoa1810865 [DOI] [PubMed] [Google Scholar]
- 46.Rodríguez-Abreu D, Powell SF, Hochmair MJ, et al. Pemetrexed plus platinum with or without pembrolizumab in patients with previously untreated metastatic nonsquamous NSCLC: protocol-specified final analysis from KEYNOTE-189. Ann Oncol 2021;32:881-95. 10.1016/j.annonc.2021.04.008 [DOI] [PubMed] [Google Scholar]
- 47.Paz-Ares L, Vicente D, Tafreshi A, et al. A Randomized, Placebo-Controlled Trial of Pembrolizumab Plus Chemotherapy in Patients With Metastatic Squamous NSCLC: Protocol-Specified Final Analysis of KEYNOTE-407. J Thorac Oncol 2020;15:1657-69. 10.1016/j.jtho.2020.06.015 [DOI] [PubMed] [Google Scholar]
- 48.Socinski MA, Jotte RM, Cappuzzo F, et al. atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med 2018;378:2288-301. 10.1056/NEJMoa1716948 [DOI] [PubMed] [Google Scholar]
- 49.Socinski MA, Nishio M, Jotte RM, et al. IMpower150 Final Overall Survival Analyses for atezolizumab Plus Bevacizumab and Chemotherapy in First-Line Metastatic Nonsquamous NSCLC. J Thorac Oncol 2021;16:1909-24. 10.1016/j.jtho.2021.07.009 [DOI] [PubMed] [Google Scholar]
- 50.Paz-Ares L, Ciuleanu TE, Cobo M, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncol 2021;22:198-211. 10.1016/S1470-2045(20)30641-0 [DOI] [PubMed] [Google Scholar]
- 51.Geraci E, Chablani L. Immunotherapy as a second-line or later treatment modality for advanced non-small cell lung cancer: A review of safety and efficacy. Crit Rev Oncol Hematol 2020;152:103009. 10.1016/j.critrevonc.2020.103009 [DOI] [PubMed] [Google Scholar]
- 52.Wu S, Wang L, Li W, et al. Comparison between the first-line and second-line immunotherapy drugs in the progression-free survival and overall survival in advanced non-small cell lung cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med 2021;10:1717-26. 10.21037/apm-20-449 [DOI] [PubMed] [Google Scholar]
- 53.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. 10.1056/NEJMoa1504627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. 10.1056/NEJMoa1507643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. 10.1016/S0140-6736(15)01281-7 [DOI] [PubMed] [Google Scholar]
- 56.Rittmeyer A, Barlesi F, Waterkamp D, et al. atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255-65. 10.1016/S0140-6736(16)32517-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mamdani H, Matosevic S, Khalid AB, et al. Immunotherapy in Lung Cancer: Current Landscape and Future Directions. Front Immunol 2022;13:823618. 10.3389/fimmu.2022.823618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.He Y, Yu H, Rozeboom L, et al. LAG-3 Protein Expression in Non-Small Cell Lung Cancer and Its Relationship with PD-1/PD-L1 and Tumor-Infiltrating Lymphocytes. J Thorac Oncol 2017;12:814-23. 10.1016/j.jtho.2017.01.019 [DOI] [PubMed] [Google Scholar]
- 59.Atkinson V, Khattak A, Haydon A, et al. Eftilagimod alpha, a soluble lymphocyte activation gene-3 (LAG-3) protein plus pembrolizumab in patients with metastatic melanoma. J Immunother Cancer 2020;8:e001681. 10.1136/jitc-2020-001681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tawbi HA, Schadendorf D, Lipson EJ, et al. Relatlimab and nivolumab versus nivolumab in Untreated Advanced Melanoma. N Engl J Med 2022;386:24-34. 10.1056/NEJMoa2109970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ruffo E, Wu RC, Bruno TC, et al. Lymphocyte-activation gene 3 (LAG-3): The next immune checkpoint receptor. Semin Immunol 2019;42:101305. 10.1016/j.smim.2019.101305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Horvath L, Thienpont B, Zhao L, et al. Overcoming immunotherapy resistance in non-small cell lung cancer (NSCLC) - novel approaches and future outlook. Mol Cancer 2020;19:141. 10.1186/s12943-020-01260-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Doi T, Fujiwara Y, Shitara K, et al. The safety and tolerability of epacadostat alone and in combination with pembrolizumab in patients with advanced solid tumors: results from a first-in-Japanese phase I study (KEYNOTE-434). Invest New Drugs 2021;39:152-62. 10.1007/s10637-020-00942-1 [DOI] [PubMed] [Google Scholar]
- 64.Long GV, Dummer R, Hamid O, et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab in patients with unresectable or metastatic melanoma (ECHO-301/KEYNOTE-252): a phase 3, randomised, double-blind study. Lancet Oncol 2019;20:1083-97. 10.1016/S1470-2045(19)30274-8 [DOI] [PubMed] [Google Scholar]
- 65.De Giglio A, Di Federico A, Nuvola G, et al. The Landscape of Immunotherapy in Advanced NSCLC: Driving Beyond PD-1/PD-L1 Inhibitors (CTLA-4, LAG-3, IDO, OX40, TIGIT, Vaccines). Curr Oncol Rep 2021;23:126. 10.1007/s11912-021-01124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cho BC, Abreu DR, Hussein M, et al. Tiragolumab plus atezolizumab versus placebo plus atezolizumab as a first-line treatment for PD-L1-selected non-small-cell lung cancer (CITYSCAPE): primary and follow-up analyses of a randomised, double-blind, phase 2 study. Lancet Oncol 2022;23:781-92. 10.1016/S1470-2045(22)00226-1 [DOI] [PubMed] [Google Scholar]
- 67.Niu J, Maurice-Dror C, Lee DH, et al. First-in-human phase 1 study of the anti-TIGIT antibody vibostolimab as monotherapy or with pembrolizumab for advanced solid tumors, including non-small-cell lung cancer. Ann Oncol 2022;33:169-80. 10.1016/j.annonc.2021.11.002 [DOI] [PubMed] [Google Scholar]
- 68.Ghalamfarsa G, Kazemi MH, Raoofi Mohseni S, et al. CD73 as a potential opportunity for cancer immunotherapy. Expert Opin Ther Targets 2019;23:127-42. 10.1080/14728222.2019.1559829 [DOI] [PubMed] [Google Scholar]
- 69.Han Y, Lee T, He Y, et al. The regulation of CD73 in non-small cell lung cancer. Eur J Cancer 2022;170:91-102. 10.1016/j.ejca.2022.04.025 [DOI] [PubMed] [Google Scholar]
- 70.Herbst RS, Majem M, Barlesi F, et al. COAST: An Open-Label, Phase II, Multidrug Platform Study of Durvalumab Alone or in Combination With Oleclumab or Monalizumab in Patients With Unresectable, Stage III Non-Small-Cell Lung Cancer. J Clin Oncol 2022:JCO2200227. 10.1200/JCO.22.00227 [DOI] [PubMed] [Google Scholar]
- 71.Yang S, Wei W, Zhao Q. B7-H3, a checkpoint molecule, as a target for cancer immunotherapy. Int J Biol Sci 2020;16:1767-73. 10.7150/ijbs.41105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aggarwal C, Prawira A, Antonia S, et al. Dual checkpoint targeting of B7-H3 and PD-1 with enoblituzumab and pembrolizumab in advanced solid tumors: interim results from a multicenter phase I/II trial. J Immunother Cancer 2022;10:e004424. 10.1136/jitc-2021-004424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Das M, Zhu C, Kuchroo VK. Tim-3 and its role in regulating anti-tumor immunity. Immunol Rev 2017;276:97-111. 10.1111/imr.12520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen Y, Xin Z, Huang L, et al. CD8(+) T Cells Form the Predominant Subset of NKG2A(+) Cells in Human Lung Cancer. Front Immunol 2019;10:3002. 10.3389/fimmu.2019.03002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hernandez-Martinez JM, Vergara E, Zatarain-Barrón ZL, et al. VISTA/PD-1H: a potential target for non-small cell lung cancer immunotherapy. J Thorac Dis 2018;10:6378-82. 10.21037/jtd.2018.11.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Srivastava S, Furlan SN, Jaeger-Ruckstuhl CA, et al. Immunogenic Chemotherapy Enhances Recruitment of CAR-T Cells to Lung Tumors and Improves Antitumor Efficacy when Combined with Checkpoint Blockade. Cancer Cell 2021;39:193-208.e10. 10.1016/j.ccell.2020.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gray JE, Owonikoko TK, Kato T, et al. Randomized phase III study of first-line pembrolizumab plus pemetrexed/platinum followed by pembrolizumab and maintenance olaparib versus pemetrexed in patients with metastatic nonsquamous non-small cell lung cancer (NSCLC): KEYLYNK-006. J Clin Oncol 2020;38. 10.1200/JCO.2020.38.15_suppl.TPS963233052757 [DOI] [Google Scholar]
- 78.Gray JE, Owonikoko TK, Kato T, et al. 1418TiP Randomized, placebo-controlled phase III study of 1L pembrolizumab (Pembro) plus carboplatin/taxane followed by pembro with or without maintenance olaparib in patients (Pts) with metastatic squamous non-small cell lung cancer (sqNSCLC): KEYLYNK-008. Ann Oncol 2020;31:S896. 10.1016/j.annonc.2020.08.1732 [DOI] [Google Scholar]
- 79.Feng K, Guo Y, Dai H, et al. Chimeric Antigen Receptor-Modified T Cells for the Immunotherapy of Patients With EGFR Expressing Advanced Relapsed/Refractory Non-Small Cell Lung Cancer. Sci China Life Sci 2016;59:468-79. 10.1007/s11427-016-5023-8 [DOI] [PubMed] [Google Scholar]
- 80.Jie Y, Liu G, Feng L, et al. PTK7-Targeting CAR T-Cells for the Treatment of Lung Cancer and Other Malignancies. Front Immunol 2021;12:665970. 10.3389/fimmu.2021.665970 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as