Abstract
Discovery of the genetics/genomics underpinnings of health, risk for disease, sickness, and treatment response have the prospects of improving recognition and management of at risk individuals; improving screening, prognostics, and therapeutic decision-making; expanding targeted therapies; and improving the accuracy of medication dosing and selection based on drug metabolism genetic variation. Thus, genetics/genomics science, information, and technologies influence the entire health care continuum and are fundamental to the nursing profession. Translating the benefits of genetics and genomics into health care requires that nurses are knowledgeable about and able to integrate this information and technology into their practice. This chapter explores the development of essential nursing competences in genetics and genomics and outcome indicators. Included is an overview of projects aimed at measuring and/or supporting adoption and integration of such competencies. Included as well is an update reviewing current evidence of the state of genomics nursing education in the United States and recommendations for next steps.
INTRODUCTION
The entire health care continuum is being impacted by research developments in genetics and genomics that are rapidly being integrated into practice. This rapid translation has moved genetics from specialty services into mainstream health care as the clinical utility of genetics and genomics expands. No longer are genetic applications limited to the 10–20 million Americans estimated to have or have been diagnosed with a genetic condition (National Institutes of Health, 2010). Current applications include identifying people at risk of disease; using genomic information and technology to screen, diagnose, inform prognosis, and guide treatment; informing drug selection; and expanding knowledge of the biologic underpinnings of disease leading to new treatments. The area of pharmacogenomics, or knowledge of variation in drug response and toxicity because of genetic variation, has experienced exceptional growth and alludes to the massive extent of potential genomic applications. The U.S. population stands at approximately 307,000,000 with each individual having a realistic probability of being prescribed a medication at some point in their lifespan (United States Census Bureau, 2009). Medications are now on the market whose dose, inhibitors, and/or inducers already are or may be optimized in the future based on genetic and genomic information.
A look back at the field of infectious disease provides a model of the process for current genetic/genomic information translation. At one time, the specialty of infectious disease was commonplace. Antimicrobials were first developed and introduced into health care by infectious disease specialists. But the reduction in morbidity and mortality of infections occurred as all health care providers were trained in the prevention and therapy of infections (Kass, 1987). This transition into routine health care has not eliminated the need for infectious disease specialists. Complex infections, drug resistance, and new infectious diseases have all illustrated the continuing need of the specialty. The field of genetics and genomics is striving for a similar conclusion, an improvement in health outcomes through the integration of genomic information and technology into mainstream health care. That successful conclusion is hinged on a genomically competent health care workforce and served to inspire the projects reviewed in this chapter.
Until recently, genetic services have been predominately consultation services for prenatal, dysmorphology, congenital, and/or single gene disorders services. In certain conditions, long-term care may be provided such as the case of metabolic genetic syndromes. Genetic health care professionals have had specific training in this field and can be nurses, physicians, or genetic counselors. As the genetic and genomic contribution to common diseases has been illuminated, the genetic specialists may have begun to practice closely with other health care providers, including working in general health care services to assist in integration of this knowledge (Drury, Bethea, Guilbert, & Qureshi, 2007). In addition, there has been continued expansion of genetic services’ scope of practice in the laboratory, diagnostic, counseling, case management, and treatment services for a wide range of conditions including adult onset disorders such as cancer and cardiovascular diseases.
As the clinical utility of genomic information and technology continues to increase, there are insufficient numbers of genetic health care professionals to meet the demand. In addition, as genomic applications continue to expand, many genetic providers lack the specialty training needed to use the new approaches. Cancer care and genomic tumor profiling to inform therapeutic decisions represents an application where this is clearly demonstrated. The therapeutic decisions associated with genomic prognostic indicators such as tumor profiles falls into the domain of the oncologist and further patient education about the prescribed therapies is in the oncology nursing domain. This illustrates the need for genomic competency of all health professionals including nurses.
An influencing factor of genomic applications in care is the insurance coverage where genetic and/or genomic services and tests coverage differ significantly. One study conducted in Illinois found that the extent of coverage varied, testing criteria differed depending on the insurance carrier, and different provider types had varied levels of reimbursement for their services (Latchaw, Ormond, Smith, Richardson, & Wicklund, 2010). Nurses serve as advocates for insurance coverage and therefore are central to assuring that genetic and genomic translation does not further expand health care inequality (Calzone et al., 2010).
BACKGROUND
Genetic/Genomic Nursing Integration Efforts
Nurses are the largest segment of the health care provider community in the United States with more than 3 million licensed registered nurses of which more than 2.5 million are actively practicing (U.S. Department of Health and Human Services, 2010). Nurses practice in every health care setting and continue to hold the distinction of being trusted by the public as the most honest and ethical health care providers. This credibility positions nurses to be effective change agents, as illustrated by the success of the End-of-Life Nursing Education Consortium (ELNEC; Ferrell, Virani, & Malloy, 2006). This initiative has sponsored train-the-trainer seminars that have reached more than 4,500 nurses across the country. The results have included content integration into the academic curricula, clinical care translation including expansion of palliative care, professional nursing organization dissemination, and establishment of ELNEC efforts internationally (Malloy, Paice, Virani, Ferrell, & Bednash, 2008). Such an educational model is valuable when contemplating strategies to educate such a large and diverse nursing workforce in genetics and genomics.
As the largest health care profession, nurses are vital to the successful translation of genetics/genomics into health care and should not serve as a translation barrier (Calzone et al., 2010). Yet, nurses have limited competency in this foundational science that is hindering their ability to integrate this into their practice and academic programs preparing the next generation of the profession. This insufficient competency can result in decreased capability to provide education in genetics/genomics to patients and families; perform assessments that identify people at risk for diseases; facilitate referrals to genetic specialists; know how to interpret genetic test results; understand the potential toxicities of genetically targeted therapies; recognize inhibitors or inducers of medications based on genetic drug metabolism; handle the ethical, legal, and social components of genetic/genomic information and technology; and provide sufficient information consent for research that includes genomics (Calzone et al., 2010; Feetham, Thomson, & Hinshaw, 2005).
For more than 4 decades, there have been consistent calls for more genetics and, recently, genomics integration into the nursing curricula (Brantl & Esslinger, 1962). Despite these appeals, Anderson (1996) found in a review of the literature spanning 1983–1995 that genetic integration into academic nursing education remained scarce. Scanlon and Fibison (1995) further documented this finding in their national survey of 1,000 practicing nurses, in which 91% reported no training in genetics or the consequences of genetic information.
This issue is not unique to the United States but represents a universal issue for nursing around the globe. Recently, studies have begun to assess the health care impact associated with a genetically illiterate workforce. One study examined the non-genetic specialist health care encounter experiences of consumers and their family members who are affected with a genetic condition (Harvey et al., 2007). The Genetic Alliance, an advocacy organization of more than 600 genetic advocacy groups, served as the source for participant recruitment. Sixty-four percent of the 5,915 respondents indicated they had received no genetic education materials from their health care provider, which resulted in their pursuit of information and resources unaided. Respondents also rated their primary care physician’s ability to establish a treatment plan in collaboration with others, identify necessary services, and understand the medical and psychosocial implications of their genetic condition as fair (Harvey et al., 2007). These data provide insight into the health care implications of a workforce not yet competent in genetics.
There are many reasons that health care providers, including nurses, have genetic/genomic competency deficits. These include
limited comprehension of genetic/genomic relevancy to practice,
insufficient knowledge to understand emerging literature,
faculty are inadequately prepared to teach genetic/genomic content,
existing genetic/genomic competencies were long and complex,
changes in the field are occurring rapidly making it difficult to remain current, and
there were no regulations requiring integration of genetics and genomics (i.e., accreditation of academic programs or hospitals, and licensure examinations; Burke & Kirk, 2006; Calzone et al., 2010; Prows, Calzone, & Jenkins, 2006).
Focused Genetic/Genomic Nursing Competency Efforts
To address these competency deficits, the Genetic/Genomic Nursing Competency Initiative (GGNCI) was established by Calzone and Jenkins in 1995. GGNCI activities were focused at both organizational issues in addition to government and regulatory policies. Figure 8.1 summarizes the timeline associated with genetic integration activities. The GGNCI launched their initiative in September 1995 by hosting the Genetics Education in Nursing Workshop. Representatives from 23 professional nursing specialty organizations with a constituency of more than 400,000 members sent representatives to discuss the state of nursing knowledge in genetics and brainstorm strategies to address competency deficits. Consensus from the workshop was to develop a genetic core curriculum for practicing nurses.
FIGURE 8.1.
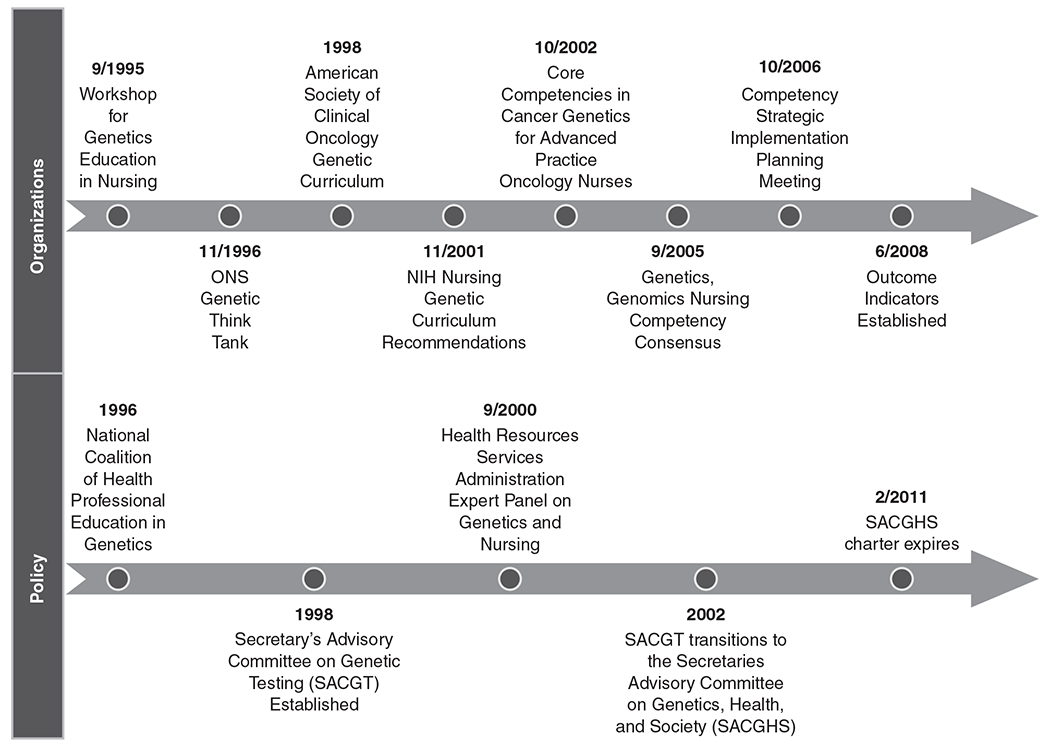
Timeline of U.S. genetic/genomic organizational and policy integration efforts.
Following this workshop, the Oncology Nursing Society (ONS) began to establish an action plan for their organization. A 2-day Think Tank on Cancer Genetics was convened in November, 1996. Participants in the Think Tank established levels for the roles of oncology nurses in genetics and confirmed the nursing role in genetic service delivery. ONS followed with Position Statements documenting Think Tank outcomes, published initially in 1997 and maintained and updated since that time (Oncology Nursing Society, 2009a, 2009b).
At the same time, a Task Force on Cancer Genetic Education was established by the American Society of Clinical Oncology (ASCO). ASCO efforts focused on a multi-dimensional education initiative that began with the development of the Cancer Genetics and Cancer Predisposition Testing curriculum resource consisting of prepared slides and accompanying support materials (ASCO, 1998). Other efforts included establishing a detailed genetic curriculum as well as developing a position statement on inherited cancer predisposition genetic testing that has continued to be updated (American Society of Clinical Oncology, 1996, 2003; Robson, Storm, Weitzel, Wollins, & Offit, 2010).
In an effort to expand beyond oncology health care professionals and address genetic/genomic education issues for all health care disciplines, not specific to just nursing as in the GGNCI, the National Coalition for Health Professional Education in Genetics (NCHPEG) was established in 1996. A collaborative effort of the American Nurses Association, the American Medical Association, and the National Human Genome Research Institute, NCHPEG membership consists of more than 50 professional specialty health care provider organizations working on education in genetics and genomics. An early NCHPEG effort was to establish genetic core competencies applicable to all health care disciplines (Core Competency Working Group of the National Coalition for Health Professional Education in Genetics, 2001). Initially approved in 2000 and published in 2001, these competencies were not widely implemented as they were extensive (44 competencies), not health care discipline specific, and addressed genetics not genetics and genomics that applies more broadly to the entire nursing profession (Jenkins & Calzone, 2007).
Building on the NCHPEG efforts and responding to the primary Genetics Education in Nursing Workshop recommendations, Jenkins and colleagues (2001) conducted a project that established genetic curriculum content recommendations for nursing education. Using this core curriculum and the oncology specialty recommendations that genetic nursing practice occur at the advance practice level, Calzone and colleagues (2002) applied the Delphi technique to nurse expert responses to establish core competencies in cancer genetics for Advanced Practice Oncology Nurses that applied to any oncology nurse with a graduate degree. The limitations to this effort included application only to one specialty (i.e., oncology), advanced practice nurses, the large number of competencies identified (52), and the continuing emphasis on genetics and not genomics (Note: Genetics was the primary scientific focus at that time).
Policy Efforts
Policy recommendations and guidance are important when providing the justification for efforts to address health care professional competency in genetics. Such guidance was provided by an expert panel on Genetics Nursing September 2000, when the U.S. Department of Health and Human Service, Health Resources and Services Administration, Bureau of Health Professions convened a group of experts in nursing, medicine, genetics, and nursing education. This panel recommended federal funding for an interdisciplinary resource clearinghouse, creation of interdisciplinary programs and collaborative partnerships, regulatory environment enhancements, and attention to workforce issues (Expert Panel Report on Genetics and Nursing, 2000).
Additionally, policy efforts at the federal level highlighted ethical, legal, and social issues that require an educated workforce to be able to identify genetic testing associated policy issues and make recommendations to address those issues. The U.S. Department of Health and Human Services (DHHS) established the Secretary’s Advisory Committee on Genetic Testing (SACGT, 2006) in response to recommendations from two advisory groups (Task Force on Genetic Testing and the Joint National Institutes of Health (NIH)/Department of Energy Committee to Evaluate the Ethical, Legal, and Social Implications Program of the Human Genome Project) that evolved to a new committee in 2002, the Secretary’s Advisory Committee on Genetics, Health, and Society (SACGHS). Both committees advised the DHHS secretary on genetic testing plus human health and societal issues associated with genetic technologies (Secretary’s Advisory Committee on Genetics, 2010). Nurses have been active participants in these policy initiatives adding a biobehavioral, prevention, health promotion, and holistic perspective to the discussions. An informed and competent nurse can advocate and inform the developing genetic/genomic policies, standards, and practices influencing standards of care (Calzone et al., 2010).
Outcome Evaluation
Despite the potential benefits achieved by an informed health care workforce, evidence indicates that the progress of U.S. nursing competency in genetics and genomics remains limited (Edwards, Maradiegue, Seibert, Macri, & Sitzer, 2006; Hetteberg, Prows, Deets, Monsen, & Kenner, 1999; Prows et al., 2006).
Surveys done in 1996 and 2005 documented minimal change in the amount of genetic and genomic content in the curricula of basic preparatory nursing academic programs (Hetteberg et al., 1999; Prows et al., 2006) with only 30% of academic nursing programs reporting a curriculum thread in genetics/genomics (Prows et al., 2006). Similarly, a survey of advanced practice nurses documented comparable finding with the majority reporting minimal training and knowledge in genetics (Maradiegue, Edwards, Seibert, Macri, & Sitzer, 2005). Genetic and genomic content is nominally found within National Council Licensure Examination (NCLEX®) or certification examinations. Continuing education resources for practicing nurses are available but with only 30% of professional nursing organizations offering some form of genetic content (Monsen & Anderson, 1999). In summary, existing reviews indicate that the nursing profession continues to have deficits in understanding and using genetic and genomic information in health care despite existing resources, established competencies in genetics/genomics for all health professionals, and published model curricula (Prows, Glass, Nicol, Skirton, & Williams, 2005). These issues are not unique to the United States, but represent a problem shared globally (Iino et al., 2002; Kirk, Calzone, Arimori, & Tonkin, 2011; Kirk, Lea, & Skirton, 2008; Kirk, Tonkin, & Burke, 2008; Nicol, 2002).
There are many reasons for the lack of progress in nursing genetics/genomics education that influence the capacity of this diverse discipline to acknowledge the value of this information to care including:
The relevance of genetics/genomics to nursing practice is not fully appreciated. Most nurses view genetics as being relevant only to a few specialty nurses as opposed to the entire profession.
Competency expectations appear daunting, long, and complex challenging educators given packed curricula and practicing professionals with limited time and resources for continuing education.
Most nurses, including faculty, have not had a foundation in understanding the science of genetics resulting in insufficient numbers of faculty prepared to teach this content.
State Boards of Nursing currently do not require competency in genetics/genomics as part of licensure or re-licensure (National Council of State Boards of Nursing, 2010; Prows et al., 2005)
These influencing factors represent challenges and opportunities. Challenges associated with the nursing workforce size and diversity in educational preparation requires a centralized approach with the creation of new resources and educational models for learning. Opportunities because nurses are central to health care delivery with the potential to be contributing change agents as illustrated by the End of Life Nursing Education Consortium and Geriatric initiatives (Kelly, Ersek, Virani, Malloy, & Ferrel, 2008; Sherman, Matzo, Rogers, McLaughlin, & Virani, 2002). Nurses, therefore, are the cornerstone for a focused effort to prepare the health care workforce in using genetics and genomics information in quality care.
Overcoming Barriers to Change
Success in a focused educational effort requires an understanding of best methods and strategies to overcome barriers and hindrances of change. The use of a strong theoretical underpinning such as a tested change theory (i.e., Rogers Diffusion of Innovations) was valuable to informing the process, to identify the reasons for lack of progress, and present mechanisms for moving forward that could garner greater success (Rogers, 2003). The literature delineates factors that can serve as successful facilitators for change such as a strong research evidence base. Five research phases have been identified in the translation of research into application. The phases are:
Basic research studies that explore different phenomena.
Methods development that involves the development of technology, instruments, or equipment needed for basic research.
Efficacy trials that assess whether there is any value to a given intervention.
Effectiveness trials that assess the extent of usefulness associated with one or more interventions.
Dissemination trials which explore the propagation and uptake of a given intervention (Sussman, Valente, Rohrbach, Skara, & Pentz, 2006).
The phases are not necessarily a linear progression and attention must be paid to the translation end-point from the onset of any research agenda to assure translation of research innovation to application (Glasgow, Lichtenstein, & Marcus, 2003). Furthermore, critical to any translational research are the validity criteria used including adequate sample representation, program implementation issues, decision-making considerations in light of existing guidelines, complexity of the innovation, and long-term sustainability evaluations (Glasgow & Emmons, 2007). Attention to data emerging from each of these phases informs and improves the quality of research discoveries when applied in health care and are appropriate for consideration when assessing the translation of genetics/genomics research into application.
The U.S. Institute of Medicine, an independent, non-governmental body aimed at providing unbiased advice to the public and policy makers, reported that several elements need to be in place for successful translation of discoveries that can improve health care and health outcomes (Glasgow, Lichtenstein, & Marcus, 2003):
Organizational support for change (i.e., hospitals, managed care organizations, medical groups, multi-specialty clinics, integrated delivery systems).
Evidence reports and practical implementation into clinical practice guidelines that improve application of evidence to health care delivery.
Use of information technology such as clinical decision support tools.
Alignment of payment policies with quality improvement (Institute of Medicine, 2001).
Key individuals are important variables in this change process including involvement of:
Key interdisciplinary stakeholders who are the end-users of the innovation such as health care providers and health care consumers.
Context adapters such as administrators or executives who can facilitate implementation of the innovation within the existing health care system.
Policy makers who establish policies, regulations, and the needed oversight for the protection of the public’s welfare (Sussman, 2006).
The engagement of such key individuals can be accelerated using opinion leaders, individuals who have both the respect and social ties within the health care environment who can help with the transmission of the information within their social network (Valente & Fasados, 2006). All of this is hinged on an educated health care workforce and an educated public who need a sufficient command of the scientific underpinnings of the innovation to understand the literature, the research, the potential application to practice, and the policy implications to contribute to the innovation dissemination and adoption (Institute of Medicine, 2001). Thus, it was identified that to have successful adoption of quality-based care that integrated genetic/genomic research into health care, a competency initiative for nursing workforce education was important to moving this identified goal forward.
ESTABLISHING THE ESSENTIAL GENETIC AND GENOMIC COMPETENCIES FOR NURSING
The competency initiative (GGNCI) began with the identification of Essential Nursing Competencies and Curricula Guidelines for Genetics and Genomics to guide academic curriculum content/learning activities and continuing education for practicing registered nurses. The Competencies were defined by a competency consensus panel and were framed by the domains of professional responsibilities and professional practice that includes assessment, identification, referral, and provision of education, care, and support. The second edition document includes competency specific outcome indicators consisting of specific areas of knowledge and clinical performance indicators. The consensus process used for competency development and endorsement was guided by the Diffusion of Innovations theory (Rogers, 2003).
Methods
There were two phases to the competency development process including establishing the essential competencies and identifying what to do with the document through the creation of a strategic implementation plan. Faculty response motivated the development of the corresponding competency outcome indicators. Figure 8.2 provides a flow diagram of the competency development process.
FIGURE 8.2.

Competency development Flow Diagram.
Phase 1
The essential genetic and genomic competencies for all U.S. registered nurses were defined in phase 1. The objectives for this phase were:
Create a steering committee made up of identified stakeholders including U.S. federal government, academic, and clinical nursing leaders. These leaders were instrumental in guiding the competency development and consensus process.
Funding for bringing together resources necessary for competency development, dissemination and implementation was obtained.
A consensus panel (see Table 8.1) representing academic, research, clinical, government agencies, and international representation was established to review and approve the draft competencies.
A consensus panel meeting brought together representatives of nursing organizations for final modification and sanction of the essential competencies.
Plans for dissemination of the essential competencies for endorsement by U.S. academic and clinical nursing organizations were made.
Publication of the final document in monograph and internet format facilitated wider distribution to the nursing community.
TABLE 8.1.
Consensus Panel Participant Organizations
| Nursing Organization Participants: Academy of Neonatal Nursing American Academy of Ambulatory Care Nursing American Academy of Nurse Practitioners American Academy of Nursing American Association of Colleges of Nursing American Association of Nurse Anesthetists American Nurses Association American Psychiatric Nurses Association American Society for Pain Management Nursing Asian American/Pacific Islander Nurses Association Association of Women’s Health, Obstetric and Neonatal Nurses Dermatology Nurses’ Association Developmental Disabilities Nurses Association National League for Nursing National Nursing Staff Development Organization National Organization of Nurse Practitioner Faculties Oncology Nursing Society Pediatric Endocrinology Nursing Society Philippine Nurses Association of America Sigma Theta Tau International Society of Pediatric Nurses The International Society of Psychiatric-Mental Health Nurses National Alaska Native American Indian Nurses Association National Association of Clinical Nurse Specialists National Association of Hispanic Nurses National Association of Neonatal Nurses National Association of Pediatric Nurse Practitioners |
| Medical Centers: Cincinnati Children’s Hospital Medical Center |
| Academic Programs: Johns Hopkins University School of Nursing Oregon Health and Science University University of Glamorgan, Wales University of Iowa University of Tennessee Health Science Center Virginia Commonwealth University |
| Governmental Agencies: Health Resources and Services Administration National Cancer Institute, NIH National Human Genome Research Institute, NIH National Institute of Nursing Research, NIH United Kingdom National Health Service, National Genetics Education and Development Centre |
| Regulatory Bodies: American Nurses Credentialing Center National Council of State Boards of Nursing National League for Nursing Accrediting Commission |
Steering Committee
The development of the competencies began with the assembly of a steering committee that included varied stakeholder representation that was an extremely lengthy process. To assure that this steering committee included adequate representation of the diverse nursing profession, a process of social network building, engaging leaders, disseminating knowledge to persuade them to adopt genetics and genomics and engage in this GGNCI effort was necessary. A snowballing effort to work through initial contacts to gain access to other key nursing leaders was repeated. Throughout this process, what was learned from these well-positioned leaders were key characteristics about the receiver, antecedent, and nursing social system characteristics all of which informed the optimal ways to engage and influence this massive and diverse discipline. After almost a year’s worth of effort, the final steering committee was compiled consisting of 15 key representatives from federal agencies and key nursing organizations, recognized academic educators, and genetic nurse experts. The committee’s responsibilities were to help guide the consensus panel, advise on the methods for establishing consensus, and provide expert review of each competency document draft as illustrated in Figure 8.2.
The consensus process for the Competencies involved soliciting feedback from a number of groups and consisted of the following:
Review and revision of the competency draft by the steering committee.
Review of the revised document by nursing representatives at a 2005 National Coalition for Health Professional Education in Genetics meeting.
Public comment from the nursing community at large was solicited using the American Nurses Association website http://nursingworld.org in August 2005.
Consensus panel (Table 8.1) convened on September 24–25, 2005, which was comprised of key stakeholders from the U.S. nursing community including academic, research, clinical, as well as minority nursing representation, and crucial regulatory bodies including certification and accrediting organizations, and the National Council of State Boards of Nursing.
Endorsement
All nursing professional organizations registered as a member of the Nursing Organizations Alliance were offered the opportunity to review, comment, and endorse the competencies. Each was contacted with first, a letter including the competencies, followed by a personal contact using standardized talking points established by members of the consensus panel and the steering committee. Fifty organizations have now endorsed the competencies. The GGNCI co-chairs received unsolicited endorsements from two schools of nursing: Johns Hopkins University School of the Nursing and Nell Hodgson Woodruff School of Nursing at Emory University. Both these schools indicated that, although they were not formally asked to endorse, they felt strongly enough about this effort to provide their endorsement. The Genetic Alliance, an advocacy genetic organization, also endorsed the competencies. A copy of the final Essential Nursing Competencies and Curricula Guidelines for Genetics and Genomics monograph can be found at http://www.genome.gov/Pages/Careers/HealthProfessionalEducation/geneticscompetency.pdf
Phase 2
The implementation of the competencies began with the assembly of an essentials advisory group that consisted of representation from each endorsing organization as well as clinical, research, academic, and government settings. The responsibility of the advisory group was to help develop a plan to guide implementation activities.
Strategic Plan
The first advisory group activity was to establish a 5-year Strategic Implementation Plan for the Essential Nursing Competencies and Curricula Guidelines for Genetics and Genomics. This plan was defined at a meeting held October 22–24, 2006. The final strategic plan focuses on four areas including recommended infrastructure, focus on practicing nurses, initiative focused on academics, and regulatory/quality control efforts (http://www.genome.gov/Pages/Health/HealthCareProvidersInfo/CompetencyStrategicPlan3-2-07.pdf). One of the priority recommendations was to establish outcome indicators for each of the essential competencies to facilitate faculty use of the competencies.
Outcome Indicator Development
As a separate second consensus initiative, a writing team consisting of members of the essentials advisory group drafted the outcome indicators that consist of two components: specific areas of knowledge and clinical performance indicators (Calzone, Jenkins, Prows, & Masny, 2011). The consensus process for approval of the outcome indicators involved soliciting feedback from a number of groups:
Creation, review, and revision of the document by the essentials advisory group.
Review by representatives at another convened group meeting for development of a Genetics/Genomics Toolkit for Faculty, with written comments accepted following the meeting and revisions incorporated.
Review by workshop attendees at American Association of Colleges of Nursing Baccalaureate and Master’s Education Conferences with revisions incorporated, and
Review and final approval by the essentials advisory group.
The outcome indicators were published in the second edition of the essential competencies that define specific knowledge areas and suggesting clinical performance indicators for each competency. Both the first and second editions of the essential competencies do not represent the opinions or position of the genetics specialty nursing community, a single nursing organization or government body. Instead, the competencies and outcome indicators were both developed through separate consecutive consensus building efforts using independent advisory panels of nurse leaders from organizations, clinical, research, and academic settings in collaboration with genetic nurse experts.
STATUS OF GENOMIC NURSING COMPETENCY
The competency document has been used to lobby for and guide the integration of genetics and genomics into the revision of the American Association Colleges of Nursing (AACN) Essentials of Baccalaureate Education for Professional Nursing Practice (American Association of Colleges of Nursing, 2008). The AACN Essentials are used by the Commission on Collegiate Nursing Education (CCNE) to establish nursing program accreditation standards, and since 2010, nursing programs undergoing CCNE accreditation review are evaluated to determine that efforts are ongoing for genetics/genomics to be included in the Baccalaureate curriculum.
A survey to assess the impact of this regulatory development was conducted in 2008, using the stages of change framework to assess the intention of nursing faculty to integrate genetic and genomic curriculum content into entry level nursing education (Prochaska, Redding, & Evers, 2002). Most faculty participants were found to be in the contemplation stage with 35% planning to adopt curriculum changes within the next 6 months. Four percent were in the preparation stage and had plans to make changes within the next 30 days. Some faculty were in the action stage with 9% already reporting curriculum changes that included genetics/genomics for less than 6 months and 10% in maintenance stage with curriculum changes that included genetics/genomics for greater than 6 months (Jenkins & Calzone, 2012).
These data indicate that the CCNE policy change resulted in a rapid change in faculty attitudes and appreciation of genetics/genomics for nursing education and practice. More than half the surveyed faculty were already in some form of action to be able to meet the new CCNE accreditation standards. Clearly, the ability of the competencies to influence policy has resulted in immediate impact stimulating GGNCI to prioritize efforts aimed at influencing policy to stimulate change.
Genetics and Genomics in Nursing Practice Survey
Next steps were to establish a benchmark of genomic nursing competency. To address this issue, the GGNCI developed the Genetics and Genomics in Nursing Practice Survey (GGNPS) instrument in 2007. The GGNPS is a web-based survey instrument designed to evaluate the integration of genetics and genomics in nursing practice using family history as the critical benchmark for assessment of attitudes, practices, receptivity, confidence, and competency. Questions assessed the value nurses placed on family history and their understanding of the role of genetics in common diseases such as cancer, heart disease, diabetes, and psychiatric illnesses. Use of family history within the past 3 months was the measure used to assess current practice. Receptivity to genetics/genomics application was measured though evaluation of barriers to family history utilization and difficulties encountered in practice as a result of family history assessments or patient questions on genetics. Nurse confidence was evaluated using self-assessment exercises on use of family history and referral patterns. Competency in family history utilization was measured through questions regarding the extent of family history that should be collected and other knowledge questions. The survey instrument was tailored from a validated instrument used to assess Family Physicians (FP) competency in genomics (Jenkins, Woolford, Stevens, Kahn, & McBride, 2010). The FP instrument was developed by a multidisciplinary team consisting of family physicians, a behavioral scientist, online survey designers, and genetic/genomic experts as an online tool to assess FP practice. The domains for measurement were selected from the constructs of Rogers Diffusion of Innovations theory and considered FP use of family history as a benchmark for genetic/genomic competency. Each item was reviewed for content validity by outside content experts including a convenience sample of family physicians. A second phase of item analysis occurred through a pilot online survey with a different convenience sample of family physicians and factor analysis was then used to revise the instrument. The final FP instrument included assessments of genetic/genomic knowledge/competency, persuasion, and decision domains from the Diffusion of Innovations theory (Jenkins et al., 2010). Most of these questions were equally appropriate for nurses, thus they were replicated in the GGNPS nursing instrument using the same questions except leveled for scope of practice when applicable.
Two studies have now been completed using this instrument. The pilot study done in collaboration with the National Institutes of Health (including the Clinical Center and the National Cancer Institute) and the National Nursing Workforce study done in collaboration with the American Nurses Association (ANA). In total, 859 licensed registered nurses have completed the survey instrument. There are 239 in the pilot study consisting of nurses from a large single research institution and 620 from the National Nursing Workforce study done in collaboration with ANA. Findings from both the pilot (2008) and National Nursing Workforce studies (2011) were congruent revealing that most nurses completing the survey thought genomics was important but felt inadequately prepared to incorporate genomics into practice. In addition, knowledge gaps were found in all nurses regardless of education level indicating that all nurses would benefit from a broad-scale education intervention to assure genetic/genomic competency.
Next Steps
At this juncture, despite a burgeoning body of evidence regarding the genetics/genomics influences on health and illness, genomic competency of the nursing workforce remains limited and a national multifaceted education effort is indicated. In addition, the evidence specific to outcomes of genomically competent nursing practice and the impact on the public’s health is extremely limited, if not entirely absent. This paucity of outcome data is further hindering efforts to translate genetics/genomics discoveries into patient care as well as efforts to influence incorporation of genetics/genomics information into academic curricula, licensure examinations, schools of nursing, and health care organization accreditation.
Although some regulatory bodies have embraced genomics, this is not universal. For instance, academic accrediting bodies that have not yet integrated genomics (National League for Nursing Accrediting Commission), the National Council of State Boards of Nursing (NCSBN) that develops the National Council Licensure Examination for Registered Nurses (NCLEX®) licensing examination, and the accrediting bodies for health care facilities such as Joint Commission, are clear that modifications to existing requirements must be based on evidence that nursing care that incorporates genetic and genomic principles, information, and technology improves the public’s health. However, this kind of evidence-base remains sparse. The GGNCI is currently engaged in developing a state of the science effort to examine and evaluate the current state of the science regarding nursing care that incorporates genetic and genomic principles, information, and technology. GGNCI will then use that evidence base to identify the gaps and establish through consensus research priorities that will serve as the underpinning for the development of research that produces the essential outcome data needed to define outcomes associated with a genetic/genomically competent nurse, and ultimately how that influences the quality of the public’s health.
The generation of this research base may be a vehicle for influencing the regulatory environment including NCLEX® and the Joint Commission. Coupled with a nationwide genomic competency education initiative, this could serve as a model for other health care disciplines to replicate in advancing genomic competency to optimize health care outcomes.
CONCLUSION
The translation of genetics and genomics into the clinical arena is progressing rapidly and has implications for the entire nursing profession. Genetics and genomics when integrated competently into health care have the potential to improve health outcomes. Yet, despite efforts in the United States and elsewhere around the world, genetic/genomic nursing competency continues to be limited. Failure of the nursing profession to understand the relevancy of genetics/genomics for health care, to have a sufficient scientific foundation in genetics to comprehend the literature, and to have the capacity to teach this material is contributing to this limited progress. This was a driving force behind the GGNCI whose primary aim is to prepare the nursing workforce to be competent in genetics and genomics. Additional evidence is needed on health outcomes associated with genomically competent nursing practice. Nurse scientists conducting translation research will document the outcomes associated with competency applying this new knowledge into health care. Progress in implementing the competencies and associated outcomes will have a global effect as we work together to optimize health care both nationally and internationally.
REFERENCES
- American Association of Colleges of Nursing. (2008). The essentials of baccalaureate education for professional nursing practice. Retrieved from http://www.aacn.nche.edu/Education/pdf/BaccEssentials08.pdf
- American Society of Clinical Oncology. (1996). Statement of the American Society of Clinical Oncology: Genetic testing for cancer susceptibility. Journal of Clinical Oncology, 14(5), 1730–1736. [DOI] [PubMed] [Google Scholar]
- American Society of Clinical Oncology. (1998). Cancer Genetics and Cancer Predisposition Testing: An ASCO Curriculum. Washington, DC: American Society of Clinical Oncology [Google Scholar]
- American Society of Clinical Oncology (2003). American Society of Clinical Oncology policy statement update: Genetic testing for cancer susceptibility. Journal of Clinical Oncology, 21(12), 2397–2406. [DOI] [PubMed] [Google Scholar]
- Anderson GW (1996). The evolution and status of genetics education in nursing in the United States 1983–1995. Image—Journal of Nursing Scholarship, 28(2), 101–106. [DOI] [PubMed] [Google Scholar]
- Brantl VM, & Esslinger PN (1962). Genetic implications for the nursing curriculum. Nursing Forum, 1(2), 90–100. [Google Scholar]
- Burke S, & Kirk M (2006). Genetics education in the nursing profession: Literature review. Journal of Advanced Nursing, 54(2), 228–237. [DOI] [PubMed] [Google Scholar]
- Calzone K, Jenkins J, & Masny A (2002). Core competencies in cancer genetics for the advanced practice oncology nurses. Oncology Nursing Forum, 29(4), 1327–1333. [DOI] [PubMed] [Google Scholar]
- Calzone KA, Cashion A, Feetham S, Jenkins J, Prows CA, Williams JK, & Wung SF (2010). Nurses transforming health care using genetics and genomics. Nursing Outlook, 58(1), 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzone KA, Jenkins J, Prows CA, & Masny A (2011). Establishing the outcome indicators for the essential nursing competencies and curricula guidelines for genetics and genomics. Journal of Professional Nursing, 27(3), 179–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Core Competency Working Group of the National Coalition for Health Professional Education in Genetics. (2001). Recommendations of core competencies in genetics essential for all health professionals. Genetics in Medicine, 3(2), 155–159. [DOI] [PubMed] [Google Scholar]
- Drury N, Bethea J, Guilbert P, & Qureshi N (2007). Genetics support to primary care practitioners—A demonstration project. Journal of Genetic Counseling, 16(5), 583–591. [DOI] [PubMed] [Google Scholar]
- Edwards QT, Maradiegue A, Seibert D, Macri C, & Sitzer L (2006). Faculty members’ perceptions of medical genetics and its integration into nurse practitioner curricula. Journal of Nursing Education, 45(3), 124–130. [DOI] [PubMed] [Google Scholar]
- Expert Panel Report on Genetics and Nursing. (2000). Report of the expert panel on genetics and nursing: Implications for education and practice (HRS00296 HRSA Publication Catalog). Washington, DC: U.S. Department of Health and Human Services, Human Resources and Services Administration. [Google Scholar]
- Feetham S, Thomson EJ, & Hinshaw AS (2005). Nursing leadership in genomics for health and society. Journal of Nursing Scholarship, 37(2), 102–110. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Virani R, & Malloy P (2006). Evaluation of the end-of-life nursing education consortium project in the USA. International Journal of Palliative Nursing, 12(6), 269–276. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, & Emmons KM (2007). How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health, 38, 413–433. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Lichtenstein E, & Marcus AC (2003). Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health, 93(8), 1261–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey EK, Fogel CE, Peyrot M, Christensen KD, Terry SF, & Mclnerney JD (2007). Providers’ knowledge of genetics: A survey of 5915 individuals and families with genetic conditions. Genetics in Medicine, 9(5), 259–267. [DOI] [PubMed] [Google Scholar]
- Hetteberg CG, Prows CA, Deets C, Monsen RB, & Kenner CA (1999). National survey of genetics content in basic nursing preparatory programs in the United States. Nursing Outlook, 47(4), 168–180. [DOI] [PubMed] [Google Scholar]
- Iino H, Tsukahara M, Murakami K, Lambert VA, Lambert CE, & Tsujino K (2002). Genetic education in baccalaureate and associate degree nursing programs in Japan. Nursing & Health Sciences, 4(4), 173–180. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Jenkins J, Woolford S, Stevens N, Kahn N, & McBride CM (2010). Family physicians’ likely adoption of genomic-related innovations. Case Studies in Business, Industry and Government Statistics, 3(2). Retrieved from http://legacy.bentley.edu/csbigs/documents/jenkins.pdf [Google Scholar]
- Jenkins JF, & Calzone KA (2007). Establishing the essential nursing competencies for genetics and genomics. Journal of Nursing Scholarship, 39(1), 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins JF, & Calzone KA (2012). Are nursing faculty ready to integrate genomic content into curricula? Nurse Educator, 37(1), 25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins JF, Prows C, Dimond E, Monsen R, & Williams J (2001). Recommendations for educating nurses in genetics. Journal of Professional Nursing, 17(6), 283–290. [DOI] [PubMed] [Google Scholar]
- Kass EH (1987). History of the specialty of infectious diseases in the United States. Annals of Internal Medicine, 106(5), 745–756. [DOI] [PubMed] [Google Scholar]
- Kelly K, Ersek M, Virani R, Malloy P, & Ferrell B (2008). End-of-life nursing education consortium. Geriatric training program: Improving palliative care in community geriatric care settings. Journal of Gerontological Nursing, 34(5), 28–35. [DOI] [PubMed] [Google Scholar]
- Kirk M, Calzone K, Arimori N, & Tonkin E (2011). Genetics-genomics competencies and nursing regulation. Journal of Nursing Scholarship, 43(2), 107–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk M, Lea D, & Skirton H (2008). Genomic health care: Is the future now? Nursing & Health Sciences, 10(2), 85–92. [DOI] [PubMed] [Google Scholar]
- Kirk M, Tonkin E, & Burke S (2008). Engaging nurses in genetics: The strategic approach of the NHS National Genetics Education and Development Centre. Journal of Genetic Counseling, 17(2), 180–188. [DOI] [PubMed] [Google Scholar]
- Latchaw M, Ormond K, Smith M, Richardson J, & Wicklund C (2010). Health insurance coverage of genetic services in Illinois. Genetics in Medicine, 12(8), 525–531. [DOI] [PubMed] [Google Scholar]
- Malloy P, Paice J, Virani R, Ferrell BR, & Bednash GP (2008). End-of-life nursing education consortium: 5 years of educating graduate nursing faculty in excellent palliative care. Journal of Professional Nursing, 24(6), 352–357. [DOI] [PubMed] [Google Scholar]
- Maradiegue A, Edwards QT, Seibert D, Macri C, & Sitzer L (2005). Knowledge, perceptions, and attitudes of advanced practice nursing students regarding medical genetics. Journal of the American Academy of Nurse Practitioners, 17(11), 472–479. [DOI] [PubMed] [Google Scholar]
- Monsen RB, & Anderson G (1999). Continuing education for nurses that incorporates genetics. Journal of Continuing Education in Nursing, 30(1), 20–24. [DOI] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing. (2010). 2010 NCLEX examination candidate bulletin. Retrieved from https://www.ncsbn.org/2010_NCLEX_Candidate_Bulletin.pdf
- National Institutes of Health. (2010). NIH announces genetic testing registry. Retrieved from http://www.nih.gov/news/health/mar2010/od-18.htm
- Nicol MJ (2002). The teaching of genetics in New Zealand undergraduate nursing programmes. Nurse Education Today, 22(5), 401–408. [DOI] [PubMed] [Google Scholar]
- Oncology Nursing Society (2009a). Cancer predisposition genetic testing and risk assessment counseling. Retrieved from http://www.ons.org/Publications/Positions/Predisposition [PubMed]
- Oncology Nursing Society (2009b). The role of the oncology nurse in cancer genetic counseling. Retrieved from http://www.ons.org/Publications/Positions/GeneticCounseling
- Prochaska JO, Redding CA, & Evers KE (2002). The transtheoretical model and stages of change. In Glanz K, Rimer B, & Lewis FM (Eds.), Health behavior and health education: Theory research, and practice (3rd ed., pp. 97–122). San Francisco, CA: Josey-Boss. [Google Scholar]
- Prows C, Calzone K, Jenkins J (2006). Genetics content in nursing curriculum. Paper presented at the meeting of the National Coalition Health Professional Education in Genetics, Bethesda, MD. [Google Scholar]
- Prows CA, Glass M, Nicol MJ, Skirton H, & Williams J (2005). Genomics in nursing education. Journal of Nursing Scholarship, 37(3), 196–202. [DOI] [PubMed] [Google Scholar]
- Robson ME, Storm CD, Weitzel J, Wollins DS, & Offit K (2010). American Society of Clinical Oncology policy statement update: Genetic and genomic testing for cancer susceptibility. Journal of Clinical Oncology, 28(5), 893–901. [DOI] [PubMed] [Google Scholar]
- Rogers E (2003). Diffusion of Innovations (5th ed.). New York, NY: Free Press. [Google Scholar]
- Scanlon C, & Fibison W (1995). Managing genetic information: Implications for nursing practice. Washington, DC: American Nurses Association. [PubMed] [Google Scholar]
- Secretary’s Advisory Committee on Genetics, Health, and Society. (2006). Coverage and reimbursement of genetic tests and services: Report of the Secretary’s Advisory Committee on Genetics, Health, and Society. Washington, DC: Department of Health and Human Services. Retrieved from http://oba.od.nih.gov/oba/sacghs/reports/CR_report.pdf [Google Scholar]
- Secretary’s Advisory Committee on Genetics, Health, and Society. (2010). Secretary’s Advisory Committee on Genetics, Health, and Society. Retrieved from http://oba.od.nih.gov/SACGHS/sacghs_home.html
- Sherman DW, Matzo ML, Rogers S, McLaughlin M, & Virani R (2002). Achieving quality care at the end of life: A focus of the End-of-Life Nursing Education Consortium (ELNEC) curriculum. Journal of Professional Nursing, 18(5), 255–262. [DOI] [PubMed] [Google Scholar]
- Sussman S, Valente TW, Rohrbach LA, Skara S, & Pentz MA (2006). Translation in the health professions: Converting science into action. Evaluation and the Health Professions, 29(1), 7–32. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2009). National and state population estimates: Annual population estimates 2000 to 2009. Retrieved from http://www.census.gov/newsroom/releases/archives/population/cb10-81.html
- U.S. Department of Health and Human Services, Health Resources Services Administration. (2010). The registered nurse population: Findings from the 2008 national sample survey of registered nurses. Washington, DC: Retrieved from http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf [Google Scholar]
- Valente TW, & Fosados R (2006). Diffusion of innovations and network segmentation: The part played by people in the promoting health. Sexually Transmitted Diseases, 33(7, Suppl), S23–S31. [DOI] [PubMed] [Google Scholar]


