Abstract
Objectives:
We examine the mediation effects of prenatal stress on the associations between intimate partner violence (IPV) experience and the most common forms of substance use (i.e., cigarette smoking, alcohol drinking, and marijuana use) among pregnant Black women.
Design:
Cross-sectional.
Sample:
Black women (N = 203) from metropolitan Detroit, Michigan and Columbus, Ohio, were recruited between 8 and 29 weeks of gestation.
Measurements:
Women were asked about IPV experience during 12 months prior to the start of the pregnancy, perceived stress during pregnancy, and substance use during pregnancy.
Results:
Intimate partner violence prior to pregnancy was positively associated with cigarette smoking and marijuana use but not with alcohol use during pregnancy. IPV prior to pregnancy was also positively associated with higher levels of perceived stress during pregnancy after controlling for covariates. Path analysis indicated that IPV had an indirect effect on marijuana use through perceived stress (standardized indirect effect = 0.026, SE = 0.020, 95% CI = 0.005–0.064, p =.017).
Conclusions:
Perceived stress during pregnancy partially mediated the association between previous experience of IPV and marijuana use among pregnant Black women. Interventions are needed to reduce IPV that would lower stress during pregnancy and consequently substance abuse to improve pregnancy outcomes and maternal and newborn health.
Keywords: Black/African American, intimate partner violence, perceived stress, pregnant women, substance use
1 ∣. BACKGROUND
National Intimate Partner and Sexual Violence Survey (NISVS) data indicate that 36.4% of U. S. women experience intimate partner violence (IPV) in their lifetime (Smith et al., 2018). According to NISVS data, 43.7% of Black women experienced lifetime IPV; a higher rate than is seen for White women (34.6%; Black et al., 2011). Women who experience IPV before pregnancy are more likely to encounter IPV during pregnancy (Silva et al., 2011). The higher risk of adverse birth outcomes (e.g., preterm birth [PTB]; <37 completed weeks of gestation) for Black women underlines the importance of studying IPV in pregnancy among these women. IPV prior to and during pregnancy is significantly associated with adverse birth out0comes (Alhusen et al., 2015; Silverman et al., 2006). Evidence also indicates that adverse birth outcomes are significantly associated with psychological stress and substance use (Corsi et al., 2019; Sealy-Jefferson et al., 2019). To our knowledge, there has not been any study regarding the effects of IPV before pregnancy on psychological well-being and substance use in the context of pregnancy or on the mechanisms linking history of IPV and substance use among pregnant Black women.
There are known to be bidirectional associations between IPV and substance use (Nowotny & Graves, 2013). Substance use is either the risk factor or the consequence of IPV (Cafferky et al., 2016). Studies have demonstrated that IPV against women is associated with both recreational and non-recreational substance use (Carbone-López et al., 2006). In a study with 241 urban women receiving emergency department care, different types of substance use were associated with different types of IPV; heroin or cocaine users were more likely to be exposed to injurious IPV and women with sexual IPV experience were more likely to use crack cocaine (Gilbert et al., 2012). The estimated prevalence of lifetime IPV in women with substance abuse was 60%–75% (El-Bassel et al., 2000). The association between IPV and substance use may differ by race/ethnicity. Nowotny and Graves (2013) reported an association between IPV and substance use in White and Latina women but not in African American women. In a sample of 33,225 Black mothers interviewed at 2–9 months postpartum, those who experienced IPV were more likely to smoke during the 3 months prior to pregnancy compared to women who did not experience IPV (29.6% and 14.9%, respectively; Cheng et al., 2015). Another study conducted in a nationally representative U. S. sample of women reported that physical IPV experience was associated with alcohol use during pregnancy (Deutsch, 2019). In another study of 101 pregnant women (37.6% Black) in the state of Indiana, IPV before pregnancy was found to be associated with marijuana use (Miller-Graff et al., 2018). Women may use marijuana to self-medicate for physical and emotional pains caused by IPV (Gilbert et al., 2000). Substance use may be a coping strategy of pregnant women who experience IPV before pregnancy (Flanagan et al., 2014). However, substance use as a coping strategy has a negative impact on both the pregnant women and their newborns' health outcomes (Forray, 2016; Shankaran et al., 2007). To date, no study has explored the associations between IPV and substance use (cigarette smoking, alcohol, and marijuana use) in a sample of pregnant Black women.
While women who experience IPV may worry for their safety and may have a sense of helplessness to control the situation, which, in turn, may cause a higher level of psychological stress (Karakurt et al., 2014), published studies on the associations between IPV and perceived stress among pregnant Black women in the United States could not be identified. However, IPV against pregnant women has been related to depressive symptoms. A study conducted in California State among 2,250 pregnant and postpartum women reported that 7% of women had co-occurrence of depressive symptoms and IPV (Connelly et al., 2013). In another study conducted in the New York City among 930 pregnant adolescents, researchers found that IPV during pregnancy was related to higher levels of depressive symptoms (Thomas et al., 2019).
Stress during pregnancy was positively associated with substance use in pregnant Black women (Jesse et al., 2006; Woods et al., 2010). Data in a sample of 1,522 pregnant women (7.6% Black) indicated that prenatal stress was significantly associated with depression, panic disorder, drug use, and domestic violence (Woods et al., 2010). Another study of 1,868 pregnant women (8.6% Black) indicated that Black women had a higher prevalence of depression and substance use (Connelly et al., 2013). Pregnant smokers were more likely to have depressive symptoms than non-smokers (Tojal & Costa, 2020). A study indicated that marijuana use in pregnant women (89% Black) was significantly associated with prenatal depression (Mark et al., 2016). According to the Stress-Coping Model, substance use is a coping response to psychological stress (Wills et al., 1996).
The study of IPV, stress, and substance abuse in pregnancy among Black women must also appreciate how racism permeates women's lives. Racism is a social stressor faced by pregnant Black women which can lead to both substance use and stress (Farahmand et al., 2020; Mendez et al., 2014; Slaughter-Acey et al., 2016). Exposure to traumatic events such as racism, IPV, stress, and substance use during pregnancy may increase risk of PTB because these experiences raise placental corticotropin-releasing hormone level, which, in turn, trigger the early parturition (Hogue & Bremner, 2005; Rich-Edwards et al., 2001). Critical Race Theory (CRT) is a methodology being employed to study race equity (Ford & Airhihenbuwa, 2010a). The concept of CRT is race consciousness, contemporary orientation, centering in the margins rather than in the mainstream, and theory-informed action (Ford & Airhihenbuwa, 2010a). Race consciousness is fundamental to CRT. Public Health Critical Race (PHCR) is the approach to apply CRT in public health to study racial disparities and health equity (Ford & Airhihenbuwa, 2010b). The PHCR approach is severely underutilized in studies of disparate outcomes in Black women. In race-conscious society, negative stereotypes had impact on psychological well-being of Black population (Williams & Williams-Morris, 2000). Our study takes a PHCR approach to examine the relationships of IPV, stress, and substance use in a cohort of pregnant Black women. Despite an abundance of research on each of the three connections (IPV and stress, stress and substance use, and IPV and substance use) in several populations, the mechanisms linking IPV and substance use have been largely unknown, particularly among pregnant Black population. Research has not examined perceived stress as a potential mediator on the associations between experiences of IPV before pregnancy and the most common forms of substance use (i.e., cigarette smoking, alcohol drinking, and marijuana use) during pregnancy among pregnant Black women. Violence against women has long-term effects on women's psychological well-being (Alejo, 2014). Therefore, this study focused on the impact of IPV before pregnancy on the perceived stress and substance use during pregnancy. We hypothesized that women who experienced IPV before pregnancy were more likely to report a higher level of psychological stress and were more likely to use substances. The purpose of this study was to examine the mediation effect of reported stress on the associations between IPV during the 12 months before pregnancy and substance use (cigarette smoking, alcohol use, or marijuana use) during pregnancy among Black women.
2 ∣. METHODS
2.1 ∣. Study design and sample
The data reported here were collected as part of the Biosocial Impact on Black Births (BIBB) study. The BIBB study research design has been reported elsewhere (Giurgescu et al., 2020). BIBB is a prospective study that aims to examine the role of maternal factors on birth outcomes among pregnant Black women. The sample of Black women in this study refers to Black women, also referred as African American women. We restricted the study to Black women because they are (1) at the highest risk of PTB (Martin et al., 2015), and (2) more likely to be exposed to social stressors (e.g., racism) compared to Whites (Slaughter-Acey et al., 2016). Although pathways by which social stressors increase risk of PTB have been demonstrated in previous studies among Black women (Mendez et al., 2014; Rich-Edwards et al., 2001; Slaughter-Acey et al., 2016), no data are available regarding the mediation effect of perceived stress on the relationship between historical IPV and perinatal substance use in this population. In addition, analytic techniques cannot accommodate extreme confounding likely to occur for factors such as racism. Moreover, outside of vital statistics-based studies, research has rarely included enough Black respondents to stratify on race and retain sufficient statistical power. The design with the intra-group examination will allow identification of unique factors, and lead to contextually tailored interventions for Black women. Using a cross-sectional design, a preliminary sample of 203 pregnant Black women of reproductive age (18–45 years old) were recruited from three selected prenatal care clinics in two metropolitan areas in the Midwest (i.e., Detroit, Michigan and Columbus, Ohio). Women were enrolled into the study if they self-identified as Black or African American (based on self-report), had singleton pregnancies, were less than 30 weeks of gestation, and were able to read and write in English. Women were excluded if they had plurality pregnancies with twins or more. Women were reimbursed with a $30 store gift card for their participation.
2.2 ∣. Data collection and management
The study was approved by the Institutional Review Board (IRB) of the two universities and of clinical sites. The principal investigator obtained an IRB waiver to access electronic medical records to determine eligibility of women for the study who received prenatal care at the participating sites. The trained research staff approached women who were eligible for the study, explained the study, and invited them to participate. Women completed an informed consent process prior to completing the questionnaires on an iPad. Questionnaire data were entered into Qualtrics Research Suite, a web-based platform for creating online surveys. Password-protected, customer-controlled survey data were captured in real time and stored on Qualtrics' secure and Transport Layer Security encrypted servers.
2.3 ∣. Measures
2.3.1 ∣. Intimate partner violence
The measure for IPV before pregnancy was a one-item question developed by our research team and used in our pilot study with pregnant Black women. Participants were asked a question: “During the 12 months before you got pregnant this time, did your husband or intimate partner hit, pushed, slapped, kicked, choked, or threatened your safety in any other way?” The IPV variable was coded 1 = Yes and 0 = No.
2.3.2 ∣. Substance use
Participants were asked three questions for each on whether they smoked cigarettes, used alcohol, or used marijuana during this pregnancy, or before pregnancy, respectively. Responses for each of these items were coded 1 = Yes and 0 = No.
2.3.3 ∣. Prenatal stress
The Perceived Stress Scale (PSS) measures prenatal stress during the prior month (e.g., “How often have you been upset because of something that happened unexpectedly?” “How often have you found that you could not cope with all the things that you had to do?”). The tool has 10 items on a five-point scale (0 = never to 4 = very often; Cohen et al., 1983). The total score can range from 0 to 36 with higher scores indicating higher levels of perceived stress. The Cronbach's alpha for this sample was 0.80.
2.3.4 ∣. Sociodemographic and obstetrical characteristics
Women completed questionnaires about their sociodemographic characteristics (e.g., age, level of education, marital status). Data on gestational age at data collection were collected by medical records abstraction.
2.4 ∣. Statistical analysis
First, descriptive statistics were calculated for the following variables: sociodemographic characteristics; experiences of IPV during the 12 months before pregnancy; cigarette smoking, alcohol drinking, and marijuana use during pregnancy; and perceived stress. Independent samples t test for continuous variables and chi-square test for categorical variables were used to examine differences in sociodemographic characteristics, cigarette smoking, alcohol drinking, marijuana use, perceived stress between women who experienced IPV and women who did not experience IPV during the 12 months before pregnancy. Multiple logistic regressions (with cigarette smoking, alcohol use, or marijuana use during pregnancy as the dependent variable) and multiple linear regressions (perceived stress during the pregnancy as the dependent variable) were performed after controlling for maternal age, level of education, marital status, and gestational age at data collection. Third, path analysis models were performed using analysis of a moment structures (AMOS) to test the mediation role of perceived stress during pregnancy on the association between IPV during the 12 months before pregnancy and marijuana use during pregnancy. Maternal age, level of education, marital status, and gestational age at data collection were included as the covariates in the path analyses. Variables used in the path analysis had a low percentage of missing data (e.g., 0.5%–3.4%). The proportions of missing data were 2.5% for IPV before pregnancy, 1.5% for cigarette smoking, 3.9% for alcohol use, 2.5% for marijuana use, 1.0% for PSS, and 3.4% for education variable, respectively. The average proportion of missing data for these variables of interest was less than 2.5%. We assumed that our data were missing completely at random (MCAR) and the Little's MCAR test supported our assumption (χ2 = 138.466, df = 117, p = .086). Missing data on continuous variables (e.g., perceived stress, age) are replaced with the mean of observed data for the variables while missing data on categorical variables (e.g., education and marital status) are replaced with the median of observed data for the variables. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 26.0 and AMOS version 26.0.
3 ∣. RESULTS
3.1 ∣. Sociodemographic characteristics and medical history
In all, 15 (7.6%) women reported experiencing IPV during the 12 months before pregnancy. There were no statistically significant differences in sociodemographic characteristics between women who experienced IPV during the 12 months before pregnancy and women who did not (see Table 1).
TABLE 1.
Sample characteristics by experiences of IPV during the 12 months before pregnancy
| IPV during the 12 months before pregnancy | |||
|---|---|---|---|
| Variables | Total, N = 203 | No, n = 183 (92.4%) | Yes, n = 15 (7.6%) |
| M ± SD | M ± SD | M ± SD | |
| Age (years) | 26.9 ± 5.65 | 26.85 ± 5.71 | 26.13 ± 5.41 |
| Gestational age at data collection (weeks) | 15.6 ± 5.72 | 15.64 ± 5.82 | 15.87 ± 4.78 |
| Perceived stress | 18.96 ± 6.21 | 18.64 ± 6.11 | 22.67 ± 6.15 |
| N (%) | N (%) | N (%) | |
| Education | |||
| ≤High school | 124 (63.3) | 114 (63.3) | 9 (60.0) |
| >High school | 72 (36.7) | 66 (36.7) | 6 (40.0) |
| Marital status | |||
| Ever marrieda | 85 (43.4) | 80 (44.4) | 5 (33.3) |
| Never married | 111 (56.6) | 100 (55.6) | 10 (66.7) |
| Cigarette smoking before pregnancy | |||
| No | 134 (67.0) | 123 (67.2) | 9 (60.0) |
| Yes | 66 (33.0) | 60 (32.8) | 6 (40.0) |
| Cigarette smoking during pregnancy | |||
| No | 167 (83.5) | 156 (85.2) | 9 (60.0)* |
| Yes | 33 (16.5) | 27 (14.8) | 6 (40.0) |
| Marijuana use before pregnancy | |||
| No | 119 (59.5) | 109 (59.6) | 8 (53.3) |
| Yes | 81 (40.5) | 74 (40.4) | 7 (46.7) |
| Marijuana use during pregnancy | |||
| No | 165 (83.3) | 154 (85.1) | 9 (60.0)* |
| Yes | 33 (16.7) | 27 (14.9) | 6 (40.0) |
| Alcohol use before pregnancy | |||
| No | 103 (52.8) | 98 (55.1) | 4 (26.7)* |
| Yes | 92 (47.2) | 80 (44.9) | 11 (73.3) |
| Alcohol use during pregnancy | |||
| No | 195 (96.1) | 175 (96.7) | 13 (86.7) |
| Yes | 8 (3.9) | 6 (3.3) | 2 (13.3) |
| IPV during pregnancy | |||
| No | 187 (94.4) | 180 (98.4) | 7 (46.7)*** |
| Yes | 11 (5.6) | 3 (1.6) | 8 (53.3) |
Abbreviations: IPV, intimate partner violence; M, mean; SD, standard deviation.
Ever married means that women currently married, widowed, divorced, separated.
p <.05
p <.001.
3.2 ∣. Experiences of IPV, substance use, and psychological well-being
Women who reported experiencing IPV during the 12 months before pregnancy were more likely to smoke cigarettes (40.0% vs. 14.8%, p <.05); drink alcohol (13.3% vs. 3.3%, p =.06); use marijuana (40.0% vs. 14.9%, p <.05); and have higher levels of perceived stress (22.67 vs. 18.64, p <.05) during pregnancy compared to women who did not experience IPV. Women who used marijuana were more likely to report a higher level of perceived stress compared to women who did not (21.48 vs. 18.53, p =.011). IPV before pregnancy was significantly related to alcohol use during pregnancy; women used alcohol were more likely to report IPV than those who did not use alcohol (73.3% vs. 26.7%, p <.05). The prevalence of smoking cigarettes, drinking alcohol, and using marijuana decreased during pregnancy compared to the rates before pregnancy (see Tables 1 and 2).
TABLE 2.
Associations between experience of IPV before pregnancy, substance use, and perceived stress
| PSS scoreb M ± SD |
|
|---|---|
| Experiences of IPV before pregnancya | |
| No | 18.64 ± 6.11* |
| Yes | 22.67 ± 6.15 |
| Cigarette smoking during pregnancy | |
| No | 18.74 ± 6.18 |
| Yes | 20.00 ± 6.04 |
| Marijuana use during pregnancy | |
| No | 18.53 ± 6.08* |
| Yes | 21.48 ± 5.76 |
| Alcohol use during pregnancy | |
| No | 18.76 ± 6.10 |
| Yes | 22.38 ± 6.55 |
Abbreviations: IPV, intimate partner violence; M, mean; PSS, Perceived Stress Scale; SD, standard deviation.
Experience of IPV during the 12 months before pregnancy.
Perceived stress during the past month prior to data collection.
p <.05.
3.3 ∣. Multiple regression analysis
Multiple logistic regression analysis results indicated that women who experienced IPV during the 12 months before the pregnancy were approximately four times more likely to smoke cigarettes (odds ratio [OR] = 4.06; 95% CI = 1.31, 12.56; p <.05), and four times more likely to use marijuana during pregnancy (OR = 4.43; 95% CI = 1.37, 14.35; p <.05) compared to women who did not report experiencing IPV during the 12 months before pregnancy after controlling for maternal age, level of education, marital status, and gestational age at data collection (see Table 3).
TABLE 3.
Multiple logistic regression analysis for predictive effect of IPV on substance use
| Substance use during pregnancy | |||
|---|---|---|---|
| Cigarette smoking |
Marijuana use |
Alcohol use |
|
| Predictive variables | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) |
| IPV before pregnancya | 4.06 (1.31, 12.56)* | 4.43 (1.37, 14.35)* | 6.13 (0.91, 41.05) |
| Maternal age | 1.00 (0.93, 1.08) | 1.04 (0.97, 1.12) | 1.01 (0.86, 1.18) |
| Gestational age at data collection | 0.99 (0.92, 1.06) | 1.01 (0.94, 1.08) | 0.86 (0.71, 1.03) |
| Level of education | 0.95 (0.65, 1.39) | 0.57 (0.37, 0.88) | 1.22 (0.59, 2.52) |
| Marital status | 0.69 (0.32, 1.52) | 1.17 (0.52, 2.64) | 0.24 (0.04, 1.32) |
Note: Covariates in the multiple regression models are maternal age, gestational age at data collection, level of education, and marital status.
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; IPV, intimate partner violence.
Experience of IPV during the 12 months before pregnancy.
p <.05.
Multiple linear regression analysis results indicated that women who experienced IPV during the 12 months before pregnancy were also more likely to report higher levels of perceived stress during pregnancy (β = 4.17; 95% CI = 0.88, 7.46; p <.05) compared to women who did not experience IPV during the 12 months before pregnancy after controlling for maternal age, level of education, marital status, and gestational age at data collection. Results also indicated that women who used marijuana during pregnancy reported higher levels of perceived stress (β = 3.11; 95% CI = 0.77, 5.45; p <.05; see Table 4). Alcohol use during pregnancy did not show a statistically significant association with PSS (p >.05).
TABLE 4.
Multiple linear regression analysis for predictive effect of IPV on perceived stress
| PSSb | |
|---|---|
| Predictive variables | β (95% CI) |
| IPV during the 12 months before pregnancya | 4.17 (0.88, 7.46)* |
| Cigarette smoking during pregnancy | 1.40 (−1.03, 3.84) |
| Marijuana use during pregnancy | 3.11 (0.77, 5.45)* |
| Alcohol use during pregnancy | 3.51 (−0.98, 8.00) |
Note: Covariates in the multiple regression models are maternal age, gestational age at data collection, level of education, and marital status. Abbreviations: CI, confidence interval; IPV, intimate partner violence; PSS, Perceived Stress Scale; β unstandardized regression coefficient.
Experience of IPV during the 12 months before pregnancy.
Perceived stress during the past month prior to data collection.
p <.05.
3.4 ∣. Path analysis
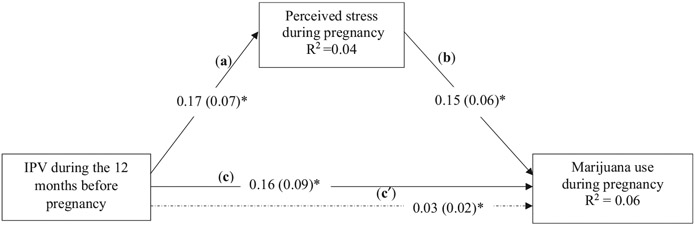
Path analysis results indicated that the standardized direct effect from IPV during the 12 months before pregnancy to perceived stress during pregnancy was 0.17 (SE = 0.07, p <.05), the standardized direct effect from IPV during the 12 months before pregnancy to marijuana use during pregnancy was 0.16 (SE = 0.09, p <.05), and the standardized direct effect from perceived stress to marijuana use during pregnancy was 0.15 (SE = 0.06, p <.05). Perceived stress during pregnancy partially mediated the association between IPV during the 12 months before pregnancy and marijuana use during pregnancy (see Figure 1); the standardized indirect effect was 0.026 (SE = 0.020, 95% CI = 0.005–0.064, p <.05).
FIGURE 1.
Standardized solutions of path analysis model. Control variables included maternal age, gestational age at data collection, level of education, and marital status. The number in the path (c′) from IPV to perceived stress using dash line is the indirect effect (standard indirect effect = 0.026, SE = 0.020, 95% CI = 0.005–0.064, p =.017). The overall hypothesized model yields χ2 to df ratio = 0.253 (p =.615), Goodness of Fit Index = 0.999, Normed Fit Index = 0.993, Comparative Fit Index = 1.000, Root Mean Square Error of Approximation (RMSEA) = 0.000. CI, confidence interval; IPV, intimate partner violence; SE, standard error. *p <.05
The model fit indices indicated a good fit in the path model. The hypothesized model yielded χ2 to df ratio = 0.253, (p >.05), Goodness of Fit Index = 0.999, Normed Fit Index = 0.993, Comparative Fit Index (CFI) = 1.000, and Root Mean Square Error of Approximation (RMSEA) = 0.000 suggesting that the hypothesized model fit to the data. It should be noticed that CFI = 1.000 and RMSEA = 0.000, indicating the model may be saturated or just-identified. The percentages of variance in marijuana use during pregnancy and perceived stress during pregnancy that were explained by the model were 4% and 6%, respectively.
4 ∣. DISCUSSION
The prevalence of IPV during the 12 months before pregnancy was 7.6% among pregnant Black women in our sample, a rate consistent with previous studies among Black women. In a study conducted in 30 states in the United States, Chisholm and colleagues found that 5.8% of pregnant Black women reported IPV (Chisholm et al., 2017). In the current study, we found that pregnant Black women who experienced IPV before pregnancy were also more likely to smoke cigarettes and use marijuana during pregnancy. These results are similar to results from the U.S. National Violence against Women Survey where exposure to IPV increases in the likelihood of substance use (Carbone-López et al., 2006). Data in the current study indicated that pregnant Black women who experienced IPV prior to pregnancy were more likely to report a higher level of perceived stress during pregnancy.
Our path analysis results indicate that IPV had an indirect effect on marijuana use through perceived stress. Over the past decade, substance use particularly opioid and marijuana use have increased in pregnant women (Salameh & Hall, 2020). Black women who experience IPV before pregnancy may experience psychological stress and may use marijuana as a coping strategy to alleviate the stress (Wills et al., 1996). However, in general, this coping strategy has limited effectiveness in alleviating psychological stress, which, in turn, may lead to detrimental psychological outcomes (e.g., depression). Consequently, this coping strategy may have negative impact on health outcomes for both pregnant women and their infants (Forray, 2016; Shankaran et al., 2007).
The significant strength of our current study is to take the PHCR approach to examine the relationships of IPV, stress, and substance use in a sample of pregnant Black women who historically have the highest prevalence of PTB. A number of research demonstrated that racism plays an important role in health disparities. Black women who experienced racism were more likely to report the experience of IPV (Waltermaurer et al., 2006). Black people's experience of racial discrimination may increase psychological stress; consequently, psychological stress may result in substance use as a coping mechanism. (Farahmand et al., 2020). Racial discrimination may increase both the IPV and stress and also the substance abuse; more future research is needed to model these associations. Among pregnant Black women, the response of physiologic pathways to the maternal stress may increase prematurity risk. IPV, psychological stress and substance use may increase risk for adverse birth outcomes (e.g., PTB) through maternal–placental–fetal endocrine systems that are involved in parturition. Future studies need to include racial discrimination into the model.
There are some limitations of this study that should be noted. First, we used a cross-sectional design; thus, causal inferences are precluded. However, we asked women about IPV prior to pregnancy and about substance use and perceived stress during the pregnancy, which may benefit the establishment of temporal associations. Second, our data are based on self-reports of women which may suffer from reporting bias due to social desirability and recall errors. We expect, however, that these biases would have been reduced by the use of an electronic tablet for data collection rather than face-to-face interviews. Third, our study sample was from two metropolitan areas in the Midwest; therefore, it may not be representative of pregnant Black women in other regions. Fourth, our sample size is relatively small with a low number of women reporting IPV (n = 15), thus constraining statistical power. Lastly, the use of a single-item (yes/no measures) to assess IPV is a weakness; further studies are needed to assess the validity of the single-item of IPV with multiple-item scales (Zhang et al., 2017).
Despite these limitations, there are important implications of our results for public health and clinical practice. Results of this study highlight the importance of assessing exposure to IPV before pregnancy in prenatal care visits rather than only current IPV, especially among pregnant Black women who use marijuana or smoke cigarettes. Our findings also have implications for IPV training for health care professionals caring for pregnant women. Health care providers may lack the skills to appropriately respond to IPV disclosure and may require training on screening and the necessary follow-up referrals.
Our study also has implications for future research about the need to assess patterns of IPV—before, during pregnancy, and even after pregnancy—and IPV's impact on mental health, and substance use. Studies using multi-item scales to assess IPV are especially needed to determine whether these findings can be replicated with a more comprehensive measure of IPV.
Our findings also suggest the importance of collecting state-level surveillance data on IPV and substance use among women of reproductive age. Finally, our findings support the need for interventions that integrate screening for all three risk factors: IPV prior to pregnancy, substance use, and psychological stress. In addition, information on stigma and perceived and actual experiences of racial discrimination should be collected. Educational interventions on pregnancy-specific stress-relief and coping strategies at the individual level, and IPV reduction/elimination at the family level could lead to improved psychological well-being and reductions in substance abuse among pregnant Black women.
ACKNOWLEDGMENTS
The study was supported by the National Institutes of Health (NIH; grant number NIH/NIMHD R01 MD01157502; Dr. Carmen Giurgescu is the Principal Investigator). The authors thank all researchers who contributed to data collections and all women participants for sharing their life experiences and perspectives. We thank hospital staff/authorities for their permission and support to interview women participants. We also thank Dr. Iqbal H. Shah for his valuable comments and suggestions.
Footnotes
CONFLICT OF INTEREST
Authors declare no conflict of interest.
DATA AVAILABILITY STATEMENT
The research data are not shared.
REFERENCES
- Alejo K (2014). Long-term physical and mental health effects of domestic violence. Themis, 2(Article 5). Retrieved from http://scholarworks.sjsu.edu/themis/vol2/iss1/5 [Google Scholar]
- Alhusen JL, Ray E, Sharps P, & Bullock L (2015). Intimate partner violence during pregnancy: Maternal and neonatal outcomes. Journal of Women's Health, 24(1), 100–106. 10.1089/jwh.2014.4872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, & Stevens MR (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Cafferky BM, Mendez M, Anderson JR, & Stith SM (2016). Substance use and intimate partner violence: A meta-analytic review. Psychology of Violence, 8(1), 110–131. 10.1037/vio0000074 [DOI] [Google Scholar]
- Carbone-López K, Kruttschnitt C, & Macmillan R (2006). Patterns of intimate partner violence and their associations with physical health, psychological distress, and substance use. Public Health Report, 121(4), 382–392. 10.1177/003335490612100406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng D, Salimi S, Terplan M, & Chisolm MS (2015). Intimate partner violence and maternal cigarette smoking before and during pregnancy reply. Obstetrics and Gynecology, 125(6), 1493–1494. 10.1097/Aog.0000000000000877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm CA, Bullock L, & Ferguson JE (2017). Intimate partner violence and pregnancy: Epidemiology and impact. American Journal of Obstetrics and Gynecology, 217(2), 141–144. 10.1016/j.ajog.2017.05.042 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 386–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Connelly CD, Hazen AL, Baker-Ericzen MJ, Landsverk J, & Horwitz SM (2013). Is screening for depression in the perinatal period enough? The co-occurrence of depression, substance abuse, and intimate partner violence in culturally diverse pregnant women. Journal of Womens Health, 22(10), 844–852. 10.1089/jwh.2012.4121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi DJ, Walsh L, Weiss D, Hsu H, El-Chaar D, Hawken S, Fell DB, & Walker M (2019). Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. Journal of the American Medical Association, 322(2), 145–152. 10.1001/jama.2019.8734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutsch AR (2019). The importance of intimate partner violence in within-relationship and between-person risk for alcohol-exposed pregnancy. Alcoholism-Clinical and Experimental Research, 43(4), 679–689. 10.1111/acer.13968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Schilling R, & Wada T (2000). Drug abuse and partner violence among women in methadone treatment. Journal of Family Violence, 15(3), 209–228. 10.1023/A:1007532917759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farahmand P, Arshed A, & Bradley M (2020). Systemic racism and substance use disorders. Psychiatric Annals, 50(11), 494–498. 10.3928/00485713-20201008-01 [DOI] [Google Scholar]
- Flanagan JC, Jaquier V, Overstreet N, Swan SC, & Sullivan TP (2014). The mediating role of avoidance coping between intimate partner violence (IPV) victimization, mental health, and substance abuse among women experiencing bidirectional IPV. Psychiatry Research, 220(1–2), 391–396. 10.1016/j.psychres.2014.07.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford CL, & Airhihenbuwa CO (2010a). Critical Race Theory, race equity, and public health: Toward antiracism praxis. American Journal of Public Health, 100(Suppl 1), S30–S35. 10.2105/AJPH.2009.171058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford CL, & Airhihenbuwa CO (2010b). The public health critical race methodology: Praxis for antiracism research. Social Science & Medicine, 71(8), 1390–1398. 10.1016/j.socscimed.2010.07.030 [DOI] [PubMed] [Google Scholar]
- Forray A (2016). Substance use during pregnancy. F1000Research, 5, 887. 10.12688/fl000research.7645.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Chang M, Wu E, & Roy L (2012). Substance use and partner violence among urban women seeking emergency care. Psychology of Addictive Behaviors, 26(2), 226–235. 10.1037/a0025869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Schilling R, Wada T, & Bennet B (2000). Partner violence and sexual HIV risk behaviors among women in methadone treatment. AIDS and Behavior, 4(3), 261–269. 10.1023/A:1009568718804 [DOI] [Google Scholar]
- Giurgescu C, Zhang L, Price MA, Dailey RK, Frey HA, Walker DS, Zenk SN, Engeland CG, Anderson CM, & Misra DP (2020). Prenatal cigarette smoking as a mediator between racism and depressive symptoms: The Biosocial Impact on Black Births Study. Public Health Nursing, 37(5), 740–749. 10.1111/phn.12780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue CJ, & Bremner JD (2005). Stress model for research into preterm delivery among black women. American Journal of Obstetrics and Gynecology, 192(5 Suppl), S47–S55. 10.1016/j.ajog.2005.01.073 [DOI] [PubMed] [Google Scholar]
- Jesse DE, Graham M, & Swanson M (2006). Psychosocial and spiritual factors associated with smoking and substance use during pregnancy in African American and White low-income women. Journal of Obstetric, Gynecologic & Neonatal Nursing, 35(1), 68–77. 10.1111/j.1552-6909.2006.00010.x [DOI] [PubMed] [Google Scholar]
- Karakurt G, Smith D, & Whiting J (2014). Impact of intimate partner violence on women's mental health. Journal of Family Violence, 29(7), 693–702. 10.1007/s10896-014-9633-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark K, Desai A, & Terplan M (2016). Marijuana use and pregnancy: Prevalence, associated characteristics, and birth outcomes. Archives of Womens Mental Health, 19(1), 105–111. 10.1007/S00737-015-0529-9 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman M, Curtin SC, & Matthews T (2015). Births: Final data for 2013. National Vital Statistics Reports (Vol. 64, No 1). National Center for Health Statistics. [PubMed] [Google Scholar]
- Mendez DD, Hogan VK, & Culhane JF (2014). Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity & Health, 19(5), 479–499. 10.1080/13557858.2013.846300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Graff L, Howell K, Grein K, & Keough K (2018). Women's cigarette and marijuana use in pregnancy: Identifying the role of past versus recent violence exposure. Journal of Interpersonal Violence, 088626051877906. 10.1177/0886260518779068 [DOI] [PubMed] [Google Scholar]
- Nowotny KM, & Graves JL (2013). Substance use and intimate partner violence victimization among White, African American, and Latina women. Journal of Interpersonal Violence, 28(17), 3301–3318. 10.1177/0886260513496903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards J, Krieger N, Majzoub J, Zierler S, Lieberman E, & Gillman M (2001). Maternal experiences of racism and violence as predictors of preterm birth: Rationale and study design. Paediatric and Perinatal Epidemiolgy, 15(Suppl 2), 124–135. 10.1046/j.1365-3016.2001.00013.x [DOI] [PubMed] [Google Scholar]
- Salameh TN, & Hall LA (2020). Depression, anxiety, and substance use disorders and treatment receipt among pregnant women in the United States: A systematic review of trend and population-based studies. Issues in Mental Health Nursing, 41(1), 7–23. 10.1080/01612840.2019.1667460 [DOI] [PubMed] [Google Scholar]
- Sealy-Jefferson S, Mustafaa FN, & Misra DP (2019). Early-life neighborhood context, perceived stress, and preterm birth in African American Women. SSM – Population Health, 7, 100362. 10.1016/j.ssmph.2019.10036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankaran S, Lester BM, Das A, Bauer CR, Bada HS, Lagasse L, & Higgins R (2007). Impact of maternal substance use during pregnancy on childhood outcome. Seminars in Fetal and Neonatal Medicine, 12(2), 143–150. 10.1016/j.siny.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva EP, Ludermir AB, de Araujo TVB, & Valongueiro SA (2011). Frequency and pattern of intimate partner violence before, during and after pregnancy. Revista De Saude Publica, 45(6), 1044–1053. [DOI] [PubMed] [Google Scholar]
- Silverman JG, Decker MR, Reed E, & Raj A (2006). Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: Associations with maternal and neonatal health. American Journal of Obstetrics and Gynecology, 195(1), 140–148. 10.1016/j.ajog.2005.12.052 [DOI] [PubMed] [Google Scholar]
- Slaughter-Acey JC, Sealy-Jefferson S, Helmkamp L, Caldwell CH, Osypuk TL, Platt RW, Straughen JK, Dailey-Okezie RK, Abeysekara P, & Misra DP (2016). Racism in the form of micro aggressions and the risk of preterm birth among black women. Annals of Epidemiology, 26(1), 7–13.e1. 10.1016/j.annepidem.2015.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, & Chen J (2018). The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data brief – Updated Release. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from https://stacks.cdc.gov/view/cdc/60893 [Google Scholar]
- Thomas JL, Lewis JB, Martinez I, Cunningham SD, Siddique M, Tobin JN, & Ickovics JR (2019). Associations between intimate partner violence profiles and mental health among low-income, urban pregnant adolescents. BMC Pregnancy and Childbirth, 19, 120. 10.1186/s12884-019-2256-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tojal C, & Costa R (2020). Anxiety and depression symptoms among pregnant women with different smoking habits. Psychology Health & Medicine, 25(4), 410–417. 10.1080/13548506.2019.1634820 [DOI] [PubMed] [Google Scholar]
- Waltermaurer E, Watson CA, & McNutt LA (2006). Black women's health: The effect of perceived racism and intimate partner violence. Violence against Women, 12(12), 1214–1222. 10.1177/1077801206293545 [DOI] [PubMed] [Google Scholar]
- Williams DR, & Williams-Morris R (2000). Racism and mental health: The African American experience. Ethnicity & Health, 5(3–4), 243–268. 10.1080/713667453 [DOI] [PubMed] [Google Scholar]
- Wills TA, McNamara G, Vaccaro D, & Hirky AE (1996). Escalated substance use: A longitudinal grouping analysis from early to middle adolescence. Journal of Abnormal Psychology, 105(2), 166–180. 10.1037/0021-843X.105.2.166 [DOI] [PubMed] [Google Scholar]
- Woods SM, Melville JL, Guo Y, Fan MY, & Gavin A (2010). Psychosocial stress during pregnancy. American Journal of Obstetrics and Gynecology, 202(1), 61.e1–61.e7. 10.1016/j.ajog.2009.07.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Li X, Wang B, Shen Z, Zhou Y, Xu J, Tang Z, & Bonita S (2017). Violence, stigma and mental health among female sex workers in China: A structural equation modeling. Women and Health, 57(6), 685–704. 10.1080/03630242.2016.1186781 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The research data are not shared.