ABSTRACT
School-based HPV vaccination programs have improved vaccine uptake among adolescents globally. However, school-based HPV vaccination strategies in the United States (US) have mainly focused on school-entry mandates for vaccination, which have passed in only five states/jurisdictions. Many schools and school-based health centers (SBHCs) already provide health services to medically underserved adolescents and opportunities to improve disparities in HPV vaccine education and uptake are underexplored. This qualitative study of clinic and community members assessed potential opportunities within and outside schools to increase HPV vaccination. Data were generated from a larger mixed-methods study designed to understand experiences with HPV vaccination evidence-based strategies in medically underserved communities. The parent study included interviews and focus groups conducted with clinic (providers, clinic leaders, staff) and community (racial/ethnic minority parents, advocates, payers, policy representatives) members in Los Angeles and New Jersey between December 2020-January 2022. We created a reduced dataset of text related to schools/SBHCs (30 in-depth interviews, 7 focus groups) and conducted a directed content analysis. Participants indicated that schools and SBHCs are ideal venues for reaching medically underserved adolescents experiencing barriers to primary care access. Parents/providers expressed mutual interest in HPV vaccine administration/education in schools, but some advocates/policy participants experienced challenges due to increasing politicization of vaccines. Participants highlighted policies for expanding HPV vaccine education and administration in schools, including minor consent and increasing SBHC funding for HPV vaccines. More research is needed to explore existing infrastructure, partner motivation, and opportunities to improve HPV vaccination among medically underserved adolescents within schools beyond vaccine mandates.
KEYWORDS: HPV vaccination, school-based strategies, underserved adolescents, vaccine policy
Introduction
In the United States (US), the Advisory Committee on Immunization Practices recommends routine HPV vaccination for adolescents ages 11–12 starting as early as age 9.1 The adolescent HPV vaccination rates in the US remain lower than those of most high income countries,2 with only 62% of US adolescents (ages 13–17) up to date with HPV vaccines in 2021.3 Although provider verified HPV vaccine uptake among some racial minority groups appear to be ~ 9% higher than their White counterparts, they are also ~ 9% less likely to complete the HPV vaccine.4 Uninsured adolescents are particularly vulnerable, given lower HPV vaccine uptake and completion than insured counterparts.5 Low HPV vaccination rates are particularly concerning for medically underserved populations who live in geographic areas with a shortage of primary care services and may face economic, cultural, or language barriers to healthcare6 and experience disproportionately higher HPV-associated cancer burden compared to other groups.7,8
School-based HPV vaccination programs have improved uptake among adolescents globally and are standard in many countries.2 School-based vaccine education, outreach, and delivery are key strategies recommended by the World Health Organization to introduce the HPV vaccine into national vaccination programs.9 Australia has been delivering HPV vaccines along with other adolescent vaccines in schools as a part of its national vaccination program since its inception in 2007, and reached a completion rate of 81% in girls and 78% in boys aged 15 years in 2020.10 Similarly, Rwanda achieved a 94% completion rate by 2019 after the introduction of a school-based campaign in 2011.2 However, school-based HPV vaccination strategies in the US have mainly focused on vaccine policy mandates for school entry, which were met with resistance in most states due to concerns about adolescent sexual promiscuity11 and pushback from anti-vaccine groups.12 As of 2022, HPV vaccine mandates for school entry exist in only five US states/jurisdictions.13 Other school-based strategies for HPV vaccination remain underexplored in the US but may be a viable avenue for improving HPV vaccine education and uptake.
Schools and school-based health centers (SBHCs) in the US serve as an important safety-net for essential health and social services for medically underserved adolescents. School-based strategies for HPV vaccination could help overcome logistical barriers of vaccine administration in communities with greater social needs and barriers to health care.14,15 SBHCs have higher proportions of under-insured students, racial/ethnic minority students, and students with unmet health needs.16,17 Furthermore, many communities received increased health information and vaccination services directly from schools during the COVID-19 pandemic,18 potentially creating new opportunities to address HPV vaccination within schools. However, how partnerships with schools and SBHCs can mitigate disproportional uptake of HPV vaccines among medically underserved adolescents remains unclear.
Partnerships with schools for HPV vaccine education and SBHCs for vaccine administration could be key to achieving higher and more equitable vaccine coverage among medically disadvantaged adolescents who may not receive the vaccine otherwise. Therefore, we examined perspectives of clinic and community members regarding opportunities for school-based strategies in the US (e.g., motivation, infrastructure, policies, community partnerships), other than school entry mandates, to inform planning for HPV vaccine improvement within medically underserved communities.
Methods
Study design and sample
Data for this qualitative study was generated as part of a larger National Cancer Institute-funded study focused on examining clinic and community members’ perspectives and experiences with implementation of evidence-based strategies (EBS) to improve HPV vaccination in safety-net health care settings. Methods and conceptual framework for the larger parent study were previously reported.19 Briefly, key stakeholder groups relevant to HPV vaccination (clinicians, advocates, payers, policy representatives) were purposively recruited from HPV vaccination coalitions and other networks in Los Angeles (LA) and New Jersey (NJ). The parents were recruited from community-based organizations that serve medically underserved adolescent populations in LA and NJ. The geographic areas were chosen based on the study team locations and the diverse populations they serve. For the larger study, 58 semi-structured, in-depth interviews and 7 parent focus groups (2 English, 3 Spanish, 2 Mandarin) were completed via Zoom between December 2020-January 2022. In-depth interview is a qualitative data collection method that “seeks to foster learning about individual experiences and perspectives on a given set of issues,”20 and was used to understand the complexities of HPV vaccination for medically underserved adolescents. Focus groups were conducted to elicit knowledge and experiences of HPV vaccination from multiple parents.20 In the larger study, the Practice Change Model informed interview and focus group guide development to elicit internal and external factors that impact implementation of EBS in clinics.21 For example, the guide probed about the participants’ positive and negative experiences with HPV vaccines, perspectives on opportunities to improve HPV vaccination, as well as external factors such as encounters with misinformation and negative media. For this analysis, we focused on quotes from the transcripts that specifically discussed testing in schools or SBHCs. This reduced the dataset to 30 interviews and 7 focus groups in which school-based testing was discussed.
Verbal consent was obtained from all participants and all data were collected, uploaded, de-identified, and stored in a password-protected data storage system to protect the participants’ privacy and confidentiality. Interviews were transcribed verbatim and translated to English (if needed) using a professional third-party transcription service with certified transcriptionists and translators, and members of the research team reviewed the transcripts for any errors. The Consolidated Criteria for Reporting Qualitative Research Checklist is available in the supplementary material.22 This study was approved by the University of Southern California’s Institutional Review Board (Protocol # UP-20-00541) and Rutgers University under exempt status. The IRB classified the study as exempt under CFR §46.104 because it involved only interview procedures, and the information obtained was recorded in such a way that the identity of the participants could not be ascertained. Therefore, the IRB approved a waiver of written consent and authorized a verbal consent process.23
Data analysis
We used the qualitative data collected in the parent study to conduct a directed content analysis focused on HPV vaccination opportunities in school settings.24 Our interdisciplinary research team members hold master’s and doctoral degrees with qualitative experience in health services, social work, nursing, and anthropology, who met regularly to practice systematic reflexivity by sharing their preconceptions, exploring their roles in research and inherent bias, and how they changed over time.25,26 First, we formulated our research question: What are potential school-based opportunities and strategies to improve HPV vaccination among medically underserved adolescents? Second, we selected an analytic sample using data (interview and focus group transcripts) from the parent study by compiling a reduced sample subset included in this study with all texts related to schools and SBHCs using Atlas.ti software (Version 9). This resulted in a dataset of 30 individual in-depth interviews and 7 focus groups. We organized the themes according to predetermined categories of the Consolidated Framework for Implementation Research,27 focusing on the domains of individuals (parents, advocates, and community members), inner setting (schools and SBHCs), and outer setting (policy/payer influences) (Figure 1). We assessed for barriers and facilitators in each domain to identify motivation and opportunities to improve HPV vaccination in school-based settings. Then, we coded the data, constructed themes through comparison and contrast, and organized themes in an iterative manner through a series of meetings where we defined and named the themes together to establish credibility. We kept records of our discussions to bolster trustworthiness of our interpretation and had discussions to resolve any coding discrepancies. We also discussed whether saturation was reached at each level of analysis in which “no new categories or themes emerge.”20,25
Figure 1.
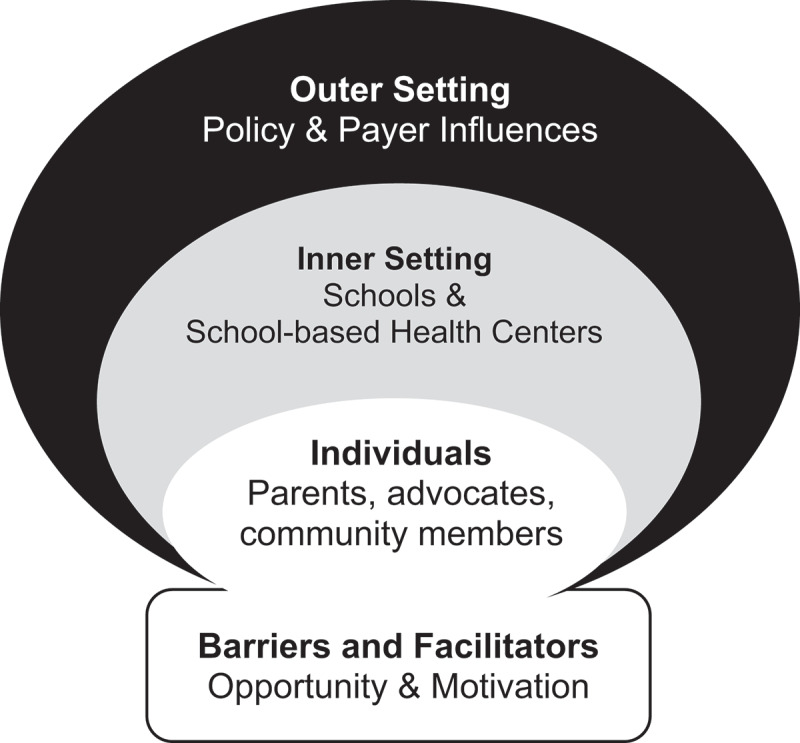
Conceptual model adapted from the updated Consolidated framework for implementation research (CFIR 2.0)27.
Results
Table 1 describes the diverse participant groups, their organizations, and characteristics, including the language that the interview/focus group was conducted in. Clinicians primarily represented providers and staff working in academic and community-based Federally Qualified Health Centers (FQHCs). Parents of adolescent children with varying HPV vaccine status participated in focus groups in LA and depth interviews in NJ, due to participants’ availability during the pandemic. Advocates worked in governmental/non-governmental immunization and cancer-focused organizations. Policy participants included policymakers and policy implementers working in school district wellness programs or health departments, and payers represented health plans that serve medically underserved adolescents. Overall, participants identified school-based settings as fertile opportunities to engage underserved adolescents and parents to improve HPV vaccination. They also highlighted challenges, such as politicization of vaccines and limited data interoperability between state immunization registries and SBHCs. Our participants pointed to existing policies and funding for HPV vaccination in schools and suggested community partnership opportunities for expanding its education and administration. These and other major themes are described in detail below and in Table 2.
Table 1.
Summary of participants by region and organization (n = 37).
| Participant Group | Participant ID | Region | Organization | N |
|---|---|---|---|---|
| Clinicians | P1 | Los Angeles | FQHC | 7 |
| P2 | New Jersey | Private pediatric practice | ||
| P3 | New Jersey | Academic health system FQHC | ||
| P4 | New Jersey | Academic health system FQHC | ||
| P5 | New Jersey | Academic health system pediatric FQHC | ||
| P6 | Los Angeles | Pediatric vaccine mobile program | ||
| P7 | Los Angeles | FQHC | ||
| Advocates | P8 | Los Angeles | Nonprofit organization | 5 |
| P9 | Los Angeles | Statewide cancer control coalition | ||
| P10 | Los Angeles | School-based health nonprofit organization | ||
| P11 | New Jersey | Statewide immunization coalition | ||
| P12 | New Jersey | Nonprofit foundation | ||
| Policy | P13 | Los Angeles | State immunization registry | 7 |
| P14 | Los Angeles | Statewide cancer control coalition | ||
| P15 | Los Angeles | County-State immunization program | ||
| P16 | Los Angeles | School district wellness center | ||
| P17 | New Jersey | State school-based health nonprofit | ||
| P18 | New Jersey | State legislator’s office | ||
| P19 | New Jersey | State department of health | ||
| Payer | P20 | Los Angeles | State Medicaid managed care organization | 5 |
| P21 | Los Angeles | County Medicaid plan | ||
| P22 | Los Angeles | Healthcare policy consulting firm | ||
| P23 | New Jersey | Medicaid managed care organization | ||
| P24 | New Jersey | State Medicaid organization | ||
| Parents FG | FG1 | Los Angeles | English | 7 |
| FG2 | Los Angeles | Spanish | ||
| FG3 | Los Angeles | Mandarin | ||
| FG4 | Los Angeles | English | ||
| FG5 | Los Angeles | Spanish | ||
| FG6 | Los Angeles | Spanish | ||
| FG7 | Los Angeles | Mandarin | ||
| Individual Parents | P25 | New Jersey | English | 6 |
| P26 | New Jersey | English | ||
| P27 | New Jersey | English | ||
| P28 | New Jersey | English | ||
| P29 | New Jersey | English | ||
| P30 | New Jersey | English | ||
| Total | 37 | |||
Table 2.
Emerging themes and supporting quotes based on the domains of updated Consolidated framework for implementation research (CFIR 2.0).
| CFIR domains | Emerging themes | Supporting quotes |
|---|---|---|
| Individuals (Parents, advocates, and community members) |
Theme 1: Parents are accepting of HPV vaccine information from schools and SBHCs |
|
| Theme 2: New community partnerships could provide opportunities for HPV vaccine education and administration in schools |
|
|
| Inner setting (schools and SBHCs) | Theme 3: Schools and SBHCs serve as healthcare safety-net for adolescents in marginalized communities |
|
| Theme 4: Engagement with schools will require leadership support to address vaccine stigma and politicization of vaccines |
|
|
| Outer setting (Policy/payer influences) | Theme 5: Raising awareness about minor consent policies among adolescents and providers could be an opportunity for HPV vaccine administration |
|
| Theme 6: Funding for HPV vaccine administration in SBHCs is limited |
|
|
| Theme 7: Limited data interoperability between SBHCs and state immunization registries present challenges to vaccination |
|
Individuals (Parents, advocates, and community members)
Themes 1 and 2 include school-based opportunities to improve HPV vaccination from the perspectives of parents, advocates, and community members working in safety-net clinic settings.
Theme 1: parents are accepting of HPV vaccine information from schools and SBHCs
While some advocates and policy participants anticipated that parents would react negatively toward HPV vaccine administration or education in schools, both LA and NJ parents shared positive experiences about how their adolescents received the HPV vaccine in a SBHC or expressed a desire to receive HPV vaccine information from schools. One parent from NJ discussed how their child’s SBHC identified a missed opportunity for the HPV vaccine during a sick visit and reached out to the parent to receive their consent.
They [child] received [HPV vaccine] at their school-based health center. He ha[d] visit[ed] there, when they had some problem, like flu. The procedure is, the doctor at the school, first contact the parents – if the parent allows the child to get [the HPV vaccine]. So, they contacted me … they told me the recommended ages in which they get [the HPV vaccine] so that’s why I said it’s okay. (P25, Parent, NJ)
Other parents suggested that receiving HPV vaccine information from schools could increase HPV vaccine uptake in their communities and mentioned established channels of communications, including e-mail and back-to-school events [FG1, LA]. A clinic leader who runs a mobile van for vaccination in schools shared how parents have responded positively to learning about HPV vaccine through their health educator in schools:
So, part of our HRSA grant gives us about 16 hours a week of a health educator … [she] first connects with the schools, and with the parent centers to provide them education about the vaccine. And what she’s discovered is, there is not a lot of hesitancy. (P6, Clinician, LA)
Although some advocates and policy participants had encountered or anticipated resistance from parents, most parents that we interviewed expressed having positive experiences, and a desire to receive HPV vaccine information from schools and SBHCs.
Theme 2: new community partnerships could provide opportunities for HPV vaccine education and administration in schools
Participants shared existing community partnerships with schools and identified new opportunities to explore for expanding HPV vaccine education and administration in schools. A clinic leader participant who used mobile vans to provide vaccinations in schools stated that investing in relationship building within middle schools and bundling the HPV vaccine with school-mandated adolescent vaccinations (Tdap and meningococcal vaccines) created a mutually beneficial partnership:
[After the initial COVID-19 stay-at-home orders were lifted] middle schools were calling us [for the] Tdap vaccine, which gets us the HPV vaccine. So, [because] we developed a relationship, and we continue to show up every six months and we were helping them with their Tdap numbers. It’s got to be a win-win, right? (P6, Clinician, LA)
A policy participant in LA explained how partnering with other local community-based organizations that already work in schools could be successful in targeting youth for HPV vaccination:
…we would love to partner with, for example, Planned Parenthood to say how do we pressure the schools to use our campaign to create more awareness because our campaign, even though it’s targeted for the LGBTQI community, it’s really targeted for youth. (P14, Policy, LA)
Inner setting (Schools and school-based health centers)
Themes 3 and 4 are related to internal organizational factors within schools/SBHCs that can serve as barriers and facilitators for HPV vaccination.
Theme 3: schools and SBHCs serve as a healthcare safety-net for adolescents in marginalized communities
Participants identified schools as important healthcare access points, especially for medically underserved adolescents who may not have a reliable source of primary care. They emphasized that SBHCs have an advantage of having contact with adolescents during an age period when their primary care visits decline compared to earlier in childhood [P11, Advocate, NJ]. Some participants wished for expanded access to SBHCs:
… doing whatever we can to make access to preventative healthcare easier for teens … I’m like, ‘Go find the universal access points where teens are going to be’ … That’s schools and probably concerts, right? So, if we can get campaigns at schools, not just SBHCs … And you make it easier for adolescents to access SBHCs. (P22, Payer, LA)
Administering HPV vaccines in SBHCs could also conserve resources and time for underserved adolescents with minimal impact on their school attendance and academic performance:
…where there are wellness centers on sites or SBHCs that offer vaccinations, the kids can leave class without telling their teacher, they just have to go to the wellness center…but then they get checked back in and they’re done within an hour, they don’t miss school, it’s really expeditious. (P16, Policy, LA)
Overall, there was a consensus that SBHCs would be an opportune place for HPV vaccine education and administration because of ease of access for underserved adolescents.
Theme 4: engagement with schools will require leadership support to address vaccine stigma and politicization of vaccines
Participants expressed a desire to partner with schools and SBHCs to improve HPV vaccination. However, advocacy and policy participants encountered reluctance from some school administrations about discussing HPV vaccines with students and parents because broader politicization of vaccines in their communities had created barriers to engaging with the topic. Hesitancy about reproductive health topics also contributed to censorship of HPV vaccine education for adolescent students in some schools. According to an advocate working with a school-based health nonprofit organization:
There is somewhat of conservatism as well, both on the [school-based] clinic administration or sometimes even the school campuses. The principals are very hesitant to talk about anything about reproductive health or even promoting minor consent services, and so we’re very limited on what could be said, what kind of health campaigns [we] can deliver around HPV. (P10, Advocate, LA)
A policy participant suggested that local advocacy and community partnerships would be key to engaging with schools, as was the case for tobacco control efforts:
…when I think of the tobacco control movement, we achieved so much in smaller specific cities. And I think [we should] model after that to think about what are the independent school districts [public and private] that we can work with. (P14, Policy, LA)
Participants expressed overall interest in providing HPV vaccine education and outreach in schools, but politicization of vaccines among parents had increased hesitancy among some school policy and district leaders. Grassroots advocacy efforts and community partnerships were suggested to address this barrier.
Outer setting (Policy/payer influences)
Themes 5 through 7 are related to external factors, especially outer influences from payers and policy members that impact opportunities for and existing strategies in school-based HPV vaccination.
Theme 5: raising awareness about minor consent policies among adolescents and providers could be an opportunity for HPV vaccine administration
In California, minors aged 12 and older can consent to HPV vaccination without a parent or guardian’s consent,28 but not in NJ. LA participants felt that raising awareness about this policy among adolescents as well as providers could be an opportunity for HPV vaccine administration in SBHCs:
…I think the [school] district needs to embrace the fact that this is a service that can occur without parental consent and promote it and allow the teens to promote it. (P16, Policy, LA)
A participant from NJ discussed that a similar minor consent policy exists in NJ, but does not currently pertain to HPV vaccination:
In NJ, we do have a law about when a young person turns 16….they’re able to access a lot of services without their parental consent. And I think that HPV should be one of those things. (P19, Policy, NJ)
However, participants in both regions stressed that it would be important to protect adolescents’ privacy and educate adolescents, parents, and providers about minor consent for school-based HPV vaccine administration.
Theme 6: funding for HPV vaccine administration in SBHCs is limited
Participants indicated that establishing a financial infrastructure for HPV vaccine payment/reimbursement is crucial for routine administration of HPV vaccines in schools. At the time of data collection, participants in California mentioned how state-level reproductive health care funding mechanisms like the Family PACT (Planning, Access, Care and Treatment) program did not cover the HPV vaccine, which presented a financial barrier for SBHCs to provide HPV vaccination without billing the adolescents’ insurance [P16, Policy, LA]. Participants acknowledged that schools could partake in existing funding sources such as the Vaccines for Children (VFC) program to cover the cost of the vaccine instead of billing the adolescents’ primary insurance for reimbursement. One provider shared:
If school-based clinics were allowed – to give vaccinations or encourage to be part of the VFC program, that could make a difference [to improve HPV vaccination]. (P1, Clinician, LA)
One payer participant stated that school-based partnerships with FQHCs could ensure financial sustainability of SBHCs and expand long-term access to HPV vaccine administration infrastructure:
But increasingly, let’s say when a FQHC partner puts a FQ[HC] on a school site, they [want to] be able to sustain that. They [want to] be able to draw in enough revenue that they can keep the doors open. And so, they’re [going to] want to open that to folks other than schoolkids. I don’t have a problem with that, as long as you continue to make it easier for the kids to get there. (P22, Payer, LA)
Theme 7: limited data interoperability between SBHCs and state immunization registries present challenges to vaccination
Participants emphasized that SBHCs need the ability to reliably identify adolescents who need HPV vaccines. They anticipated the limited data interoperability between school-based clinic electronic health record (EHR) and state immunization registries would pose challenges to routinely tracking vaccination status. One clinician from LA stated:
So school campaigns and access might be a good way, but you also need to be able to easily get those records to know [who needs the vaccine] – [because] you don’t [want to] give it to somebody who’s already been vaccinated, and kids don’t carry their own [immunization record]. (P1, Clinician, LA)
Another clinician from NJ shared that reporting vaccinations to the state immunization registry was also cumbersome in their FQHC, and how SBHCs in their region face similar challenges due to limited data interoperability (P4, Clinician, NJ). In LA, efforts to build data infrastructure for ongoing monitoring and evaluation in SBHCs had begun:
But we need more data on who’s getting it [HPV vaccine in the SBHCs] and [only] the school district has all of that data … So, [we helped] modify their record system, so that they could inform their efforts. (P9, Advocate)
Participants emphasized that expanding data interoperability between the SBHCs’ EHRs and state immunization registries would allow identification of missed opportunities for HPV vaccination and enable a more targeted approach for outreach to students.
Discussion
This study is one of few that explores potential opportunities for school-based HPV vaccine education and administration for adolescents in the US. Our participants from diverse clinic and community groups stated that schools and SBHCs are vital venues for improving HPV vaccination in medically underserved communities, as found in other studies.29,30 While participants echoed known barriers for routine administration and education of HPV vaccination in schools such as politicization of vaccines in their communities and limited funding,31 they specifically identified a need to foster partnerships between the schools and SBHCs and the community to overcome barriers and capitalize on shared motivation. There was strong consensus that there are new opportunities and existing infrastructure to further engage schools and SBHCs. There are more than 2,500 SBHCs in the US and the numbers have been growing steadily.32 As of 2018, 36 states had policies that addressed availability of school nurses on campus during the school day or some days of the week.33 Acceptability and feasibility of engaging school nurses in HPV vaccine education has been observed in other studies.34,35
We found that parents and clinic members, especially providers, are mutually interested in engaging with one another in schools regarding HPV vaccination for adolescents. This finding is consistent with other US-based studies that found wide acceptance for HPV vaccine education and administration through schools among parents of adolescents who had not completed the HPV vaccine series.14,36 Some states, including NJ, require public schools to provide information about HPV vaccination to parents and caregivers in seventh grade.37 However, some of our participants anticipated that hesitancy among parents could be a barrier for school-based HPV vaccine strategies, which may have worsened during the COVID-19 pandemic due to politicization of vaccines.38,39 In another study our research team conducted in LA, we found that as much as 20% of parent participants who were predominantly racial/ethnic minorities reported high HPV vaccine hesitancy.40 These barriers point to the need to tailor the parent engagement strategies in school settings according to the needs of the community, and an opportunity for targeted messaging to racial/ethnic minority adolescents who may play a significant role in vaccine decision-making in their families.
Engaging medically underserved adolescents in schools and SBHCs could expand access to HPV vaccines and address disparities in HPV-associated cancers. The role of schools as a safety-net healthcare provider was demonstrated during the COVID-19 pandemic, such as when school shutdowns disrupted access to healthy food for socioeconomically disadvantaged children and therapies for children with special needs.41 Previous studies have found that parents who struggle to take time off from work to take their children to appointments and uninsured parents are more willing to partake in school-based vaccination programs.42 Reaching the adolescents in schools where they spend most of their time could offset the burden for families with competing priorities including obtaining food and employment or barriers such as lack of transportation. Rodriguez and colleagues demonstrated the potential of school-based interventions to advance health equity in a rural, medically underserved area of Texas that significantly increased HPV vaccination and completion.43 Their intervention continued to improve HPV vaccine uptake through the COVID-19 pandemic and addressed transportation barriers by using mobile vans and telecommunications for community engagement.44 Strengthening the schools and SBHCs’ capacity to provide HPV vaccine administration and education through their expanded role during the pandemic and improving appointment compliance in SBHCs could be key for improving uptake among medically underserved adolescents.45,46
We have previously reported policy level strategies for improving HPV vaccination, such as raising awareness about minor consent policies in states where applicable.47 However, we found that funding sources for HPV vaccination often did not benefit medically underserved adolescents, which could create tension when minors consent to getting the HPV vaccine for themselves in SBHCs in some states. For example, in July 2022 shortly after we finished interviews and focus groups, the Family PACT program, which covers reproductive health education and services in California, including programs within SBHCs, changed its policy to cover the HPV vaccine for adults between ages 19–45, but not for adolescents.48 Similarly, NJ Plan First began covering the HPV vaccine in 2019 for individuals with incomes that are higher than traditional Medicaid eligibility, but the program excludes children.49 The federal VFC Program covers the cost of the HPV vaccine for children under age 19, but not all SBHCs are enrolled in VFC.50 These factors represent challenges that could be addressed through advocacy efforts and community partnerships as well as through state and local policy changes.
Strengths and limitations
Our study provides unique perspectives on school-based opportunities for HPV vaccination from diverse participants who serve medically underserved communities in two states but has some limitations. First, although several of our participants suggested different strategies for implementing HPV vaccination in schools, our interview guide did not specifically probe about school-based strategies. Secondly, while we were able to obtain perspectives from a wide spectrum of participants at the policy, payer, clinic and community levels, future research should directly solicit perspectives from higher-level school representatives (e.g., school district board members) as well as clinicians in SBHCs to validate opportunities found in our study. In addition, social desirability bias may have prevented some parent focus group participants from sharing negative opinions about HPV vaccination. Lastly, our participants were recruited from two states, with most participants from urban settings, which may limit generalizability of our results to other states and rural settings.
Conclusions
Schools and SBHCs are important safety-net institutions and engaging with medically underserved communities in these settings is vital to improving HPV vaccination among populations that are vulnerable to HPV-associated cancers. Parents and community members are open and willing to engage with each other in schools and SBHCs to improve adolescent HPV vaccination, and school infrastructure and policy-related strategies should be further explored to improve access to HPV vaccine education, delivery, and uptake for adolescents in medically underserved communities.
Acknowledgments
We thank Bibiana Martinez, Alec Allee-Munoz, and Jenna Howard for their contributions to data collection and initial analysis. The abstract of the preliminary analysis was presented as a poster at the 35th International Papillomavirus Conference on April 17-21, 2023.
Funding Statement
This work was supported by a National Cancer Institute Award [R37CA242541; PI: Tsui].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Abbreviations
- US
United States
- HPV
Human Papillomavirus
- FQHC
Federally Qualified Health Center
- EBS
Evidence-Based Strategies
- EHR
Electronic Health Record
- LA
Los Angeles
- NJ
New Jersey
- SBHC
School-Based Health Center
- VFC
Vaccines For Children
References
- 1.Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, Bocchini JA, Unger ER.. Human papillomavirus vaccination: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep. 2014;63(Rr–05):1–9. [PubMed] [Google Scholar]
- 2.Bruni L, Saura-Lázaro A, Montoliu A, Brotons M, Alemany L, Diallo MS, Afsar OZ, LaMontagne DS, Mosina L, Contreras M, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev Med. 2021;144:106399. doi: 10.1016/j.ypmed.2020.106399. [DOI] [PubMed] [Google Scholar]
- 3.Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Valier MR, Fredua B, Crowe SJ, Stokley S, Singleton JA. National vaccination coverage among adolescents aged 13–17 Years — National immunization survey-Teen, United States, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(35):1101–8. doi: 10.15585/mmwr.mm7135a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spencer JC, Calo WA, Brewer NT. Disparities and reverse disparities in HPV vaccination: a systematic review and meta-analysis. Prev Med. 2019;123:197–203. doi: 10.1016/j.ypmed.2019.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Valier MR, Fredua B, Crowe SJ, Stokley S, Singleton JA, Centers for Disease C, Prevention . National vaccination coverage among adolescents aged 13–17 Years — National immunization survey-Teen, United States, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(35):1101–8. doi: 10.15585/mmwr.mm7135a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Resources and Services Administration . What is a medically underserved area/Population (MUA/P)? 2023 Apr [accessed 2023 Jun 16]. https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation#mups.
- 7.Damgacioglu H, Wu C-F, Lin Y-Y, Ortiz AP, Sonawane K, Deshmukh AA. Contemporary Patterns in HPV-Associated cancer Incidence among young US men. J Gen Intern Med. 2022;38:817–9. doi: 10.1007/s11606-022-07755-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maguire RL, Vidal AC, Murphy SK, Hoyo C. Disparities in Cervical cancer Incidence and Mortality: Can Epigenetics Contribute to Eliminating disparities? Adv Cancer Res. 2017;133:129–56. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Guide to introducing HPV vaccine into national immunization programmes. Geneva: World Health Organization; 2016. [Google Scholar]
- 10.Hull B, Hendry A, Dey A, Brotherton J, Macartney K, Beard F. Annual immunisation coverage report 2020. Commun Dis Intell (2018). 2022;46. doi: 10.33321/cdi.2022.46.60. [DOI] [PubMed] [Google Scholar]
- 11.Daley E, Thompson E, Zimet G. Human Papillomavirus vaccination and school entry requirements: politically challenging, but not impossible. JAMA Pediatr. 2019;173(1):6–7. doi: 10.1001/jamapediatrics.2018.3327. [DOI] [PubMed] [Google Scholar]
- 12.Thompson EL, Daley EM, Washburn T, Salisbury-Keith K, Saslow D, Fontenot HB, Zimet GD. School-entry requirements for HPV vaccination: part of the patchwork for HPV-related cancer prevention. Hum Vaccin Immunother. 2021;17(7):1975–9. doi: 10.1080/21645515.2020.1851130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Conference of State Legislatures . HPV vaccine: state legislation and regulation; 2020. [updated 2020 May 26; accessed 2022 Sep 20]. https://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx.
- 14.Hansen CE, Okoloko E, Ogunbajo A, North A, Niccolai LM. Acceptability of school-based health centers for Human Papillomavirus vaccination visits: a mixed-Methods study. J Sch Health. 2017;87(9):705–14. doi: 10.1111/josh.12540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hofstetter AM, Schaffer S. Childhood and adolescent vaccination in alternative settings. Acad Pediatr. 2021;21(4, Supplement):S50–S6. doi: 10.1016/j.acap.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Rep. 2008;123(6):739–50. doi: 10.1177/003335490812300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94. doi: 10.1542/peds.2006-2314. [DOI] [PubMed] [Google Scholar]
- 18.Lee RC, Soto DW, Deva S, Macedo M, Shanker K, Rodriguez A, Alhajri D, Unger JB. Evaluation of a COVID-19 rapid antigen testing program in a supervised community distance learning setting for K-8 students. J Sch Health. 2022;92(5):445–51. doi: 10.1111/josh.13146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsui J, Shin M, Sloan K, Martinez B, Palinkas LA, Baezconde-Garbanati L, Cantor JC, Hudson SV, Crabtree BF. Understanding clinic and community member experiences with implementation of evidence-based strategies for HPV vaccination in safety-net primary care settings. Prev Sci. 2023. doi: 10.1007/s11121-023-01568-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiCicco-Bloom B, Crabtree B. The qualitative research interview. Med Educ. 2006;40(4):314–21. doi: 10.1111/j.1365-2929.2006.02418.x. [DOI] [PubMed] [Google Scholar]
- 21.Cohen D, McDaniel RR Jr., Crabtree BF, Ruhe MC, Weyer SM, Tallia A, Miller WL, Goodwin MA, Nutting P, Solberg LI, et al. A practice change model for quality improvement in primary care practice. J Healthc Manage. 2004;49(3):155–68. doi: 10.1097/00115514-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services. Exemptions ; 2018. [accessed 2023 July 4]. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/common-rule-subpart-a-46104/index.html.
- 24.Hsieh H-F, Shannon SE. Three Approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 25.Crabtree BF, Miller WL. Doing qualitative research. 3rd ed. Thousand Oaks (CA): Sage; 2023. [Google Scholar]
- 26.Galdas P. Revisiting bias in qualitative research: reflections on its relationship with funding and impact. Int J Qual. 2017;16(1):1609406917748992. doi: 10.1177/1609406917748992. [DOI] [Google Scholar]
- 27.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for implementation research based on user feedback. Implement Sci. 2022;17(1):75. doi: 10.1186/s13012-022-01245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.California School-Based Health Alliance . Consent; 2022. [accessed 2022 Oct 7]. https://www.schoolhealthcenters.org/resources/sbhc-operations/student-records-consent-and-confidentiality/consent/.
- 29.Shah MD, Glenn BA, Chang LC, Chung PJ, Valderrama R, Uyeda K, Szilagyi PG. Reducing missed opportunities for Human Papillomavirus vaccination in school-based health centers: impact of an intervention. Acad Pediatr. 2020;20(8):1124–32. doi: 10.1016/j.acap.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Munn MS, Kay M, Page LC, Duchin JS. Completion of the Human Papillomavirus vaccination series among adolescent users and nonusers of school-based health centers. Public Health Rep. 2019;134(5):559–66. doi: 10.1177/0033354919867734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saulsberry L, Fowler EF, Nagler RH, Gollust SE. Perceptions of politicization and HPV vaccine policy support. Vaccine. 2019;37(35):5121–8. doi: 10.1016/j.vaccine.2019.05.062. [DOI] [PubMed] [Google Scholar]
- 32.Love HE, Schlitt J, Soleimanpour S, Panchal N, Behr C. Twenty years of school-based health care growth and expansion. Health Aff. 2019;38(5):755–64. doi: 10.1377/hlthaff.2018.05472. [DOI] [PubMed] [Google Scholar]
- 33.Chriqui J-CV, Piekarz-Porter E, Temkin D, Lao K, Steed H, Harper K, Leider J, Gabriel A. Using state policy to create healthy schools: coverage of the whole school, whole community, whole child framework in state statutes and regulations school year 2017-2018. Child Trends; 2019. https://www.childtrends.org/publications/using-policy-to-create-healthy-schools [Google Scholar]
- 34.Bozigar M, Faith TD, White AA, Drayton KD, Fabick A, Cartmell KB. A cross-sectional survey to evaluate potential for partnering with school nurses to promote Human Papillomavirus vaccination. Prev Chronic Dis. 2020;17:E111. doi: 10.5888/pcd17.190451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mattebo M, Gottvall M, Grandahl M. School nurses’ perceptions and experiences of delivering a school-based intervention to improve primary prevention of human papillomavirus among adolescents—A focus group study following a randomized controlled trial. J Sch Nurs. 2021;10598405211046174. doi: 10.1177/10598405211046174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vercruysse J, Chigurupati NL, Fung L, Apte, G., Pierre-Joseph, N., Perkins, R B.. Parents’ and providers’ attitudes toward school-located provision and school-entry requirements for HPV vaccines. Human Vaccines Immunother. 2016;12(6):1606–14. doi: 10.1080/21645515.2016.1140289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.New Jersey Department of Education . Summary of selected school health mandates and resources. 2019.
- 38.Sharfstein JM, Callaghan T, Carpiano RM, Sgaier SK, Brewer NT, Galvani AP, Lakshmanan R, McFadden SM, Reiss DR, Salmon DA, et al. Uncoupling vaccination from politics: a call to action. Lancet. 2021;398(10307):1211–12. doi: 10.1016/S0140-6736(21)02099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kates JT, Jennifer RA. The red/blue divide in COVID-19 vaccination rates continues: an update: KFF; 2022. [updated 2022 Jan 19; accessed 2023 February 20]. https://www.kff.org/policy-watch/the-red-blue-divide-in-covid-19-vaccination-rates-continues-an-update/.
- 40.Tsui J, Martinez B, Shin MB, Allee-Munoz A, Rodriguez I, Navarro J, Thomas-Barrios KR, Kast WM, Baezconde-Garbanati L. Understanding medical mistrust and HPV vaccine hesitancy among multiethnic parents in Los Angeles. J Behav Med. 2022;2:1–16. doi: 10.1007/s10865-022-00283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bylander J. How COVID-19 threatens the safety net for US children. Health Aff. 2020;39(10):1668–71. doi: 10.1377/hlthaff.2020.01576. [DOI] [PubMed] [Google Scholar]
- 42.Brown DS, Arnold SE, Asay G, Lorick SA, Cho B-H, Basurto-Davila R, Messonnier ML. Parent attitudes about school-located influenza vaccination clinics. Vaccine. 2014;32(9):1043–8. doi: 10.1016/j.vaccine.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 43.Kaul S, Do TQN, Hsu E, Schmeler KM, Montealegre JR, Rodriguez AM. School-based human papillomavirus vaccination program for increasing vaccine uptake in an underserved area in Texas. Papillomavirus Res. 2019;8:100189. doi: 10.1016/j.pvr.2019.100189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rodriguez AM, Do TQN, Jibaja-Weiss ML, Chen L, Schmeler KM, Montealegre JR, Kuo Y-F. Human Papillomavirus vaccinations during the COVID-19 pandemic in middle schools in the rio grande valley of Texas. Am J Public Health. 2022;112(9):1269–72. doi: 10.2105/AJPH.2022.306970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abdul-Raheem JN, Liu AJ, Collins ME. Reimagining the role of school-based health centers during the COVID-19 pandemic. J Sch Health. 2021;91(4):271–3. doi: 10.1111/josh.13000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oliver K, McCorkell C, Pister I, et al. Improving HPV vaccine delivery at school-based health centers. Human Vaccin Immunother. 2019;15(7–8):1870–7. doi: 10.1080/21645515.2019.1578596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sloan K, Shin M, Palinkas LA, Hudson SV, Crabtree BF, Cantor JC, Tsui J. Exploring HPV vaccination policy and payer strategies for opportunities to improve uptake in safety-net settings [Original research]. Front Public Health. 2023;11:11. doi: 10.3389/fpubh.2023.1099552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.California Department of Health Care Services . HPV vaccine added as Family PACT benefit. 2022. [updated 2022 July 1; accessed 2022 Oct 30]. https://files.medi-cal.ca.gov/pubsdoco/bulletins/artfull/fpact202207.aspx.
- 49.New Jersey Department of Human Services. N.J. Human services launches New Family planning benefit. 2019. [updated 2019 Oct 7; accessed 2022 Oct 31]. https://www.state.nj.us/humanservices/news/press/2019/approved/20191007.html.
- 50.Huber KG, Perkinson L, Katelyn’ Bollinger J, Melton M, Less E. Priorities and policy levers to support school-located vaccination. Health Affairs Forefront. 2022. doi: 10.1377/forefront.20220228.651782. [DOI] [Google Scholar]


