Abstract
In this brief review, the authors describe the main characteristics of trauma systems in Latin America's 2 most populous countries, Mexico and Brazil. Trauma is a common health problem and the major cause of death in the young populations in both countries. Mexico and Brazil have well-organized systems based on system designation and prehospital triage. The highest level trauma hospitals are only available in the biggest cities, with residents of the smaller cities having less access to quality care. Both countries can provide adequate musculoskeletal trauma and polytrauma care, but the systems are not universally equal and, therefore, not ideal. The lack of consistency and standardization of the systems across each country must be addressed to improve patient outcomes across each country.
Keywords: accident prevention, developing countries, emergency care, public health, traffic accidents, trauma
1. Introduction
Latin America is a region composed by 19 different countries, where its northern limit is the Mexican northern border and Chile and Argentina as the southern limit. The 2 most populous Latin American countries, comprising almost one-third of the overall population, are Mexico and Brazil. Both countries are classified as the emergent economy countries, particularly within Latin America. In this brief review, the authors explain the main characteristics of both countries’ trauma systems, including prehospital care, main trauma providers, hospital care, and improvement projects.
2. Mexican trauma system
2.1. Introduction
Mexico is a country with an emerging economy and has more than 131,995,765 inhabitants.[1] This makes Mexico the 11th most populous country in the world.[1] Of this population, only 117 million have access to public health services, while the other 15 million people either have no such access or they have to pay for public health services themselves. This situation makes trauma a major public health problem.
One of the largest sources of traumatic injuries in Mexico is traffic accidents. In 2015 alone, there were 378,232 traffic accidents in urban areas, representing the main cause of death in the population between 15 and 29 years old (Fig. 1). These accidents led to 4601 deaths and 73,576 injuries.[2] Moreover, in 2011 unintentional trauma led to 158,799 emergency department visits.[3] These numbers imply a high demand of emergency services across the country. Trauma is now the leading cause of death among older children and young adults in Mexico.[4,5] Unintentional traumatic injuries cause 17.7% of all disabilities in Mexico, and 63.56% of this population with disabilities is between 16 and 45 years old (Fig. 2).[6,7]
Figure 1.
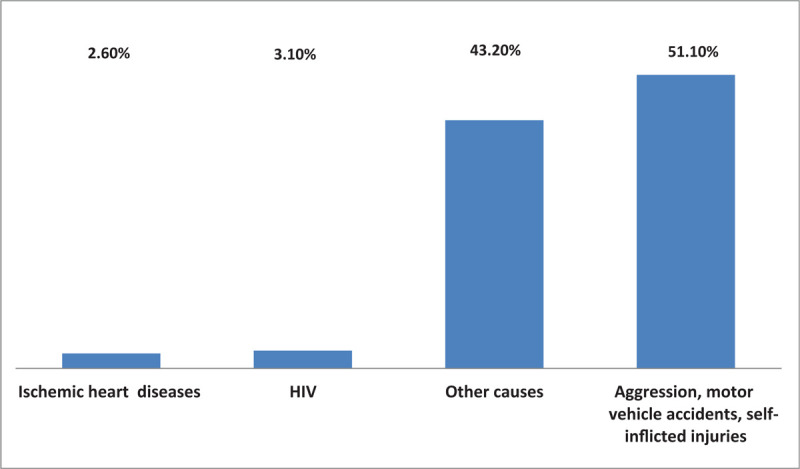
Main causes of death in male population from 15 to 29 years.
Figure 2.
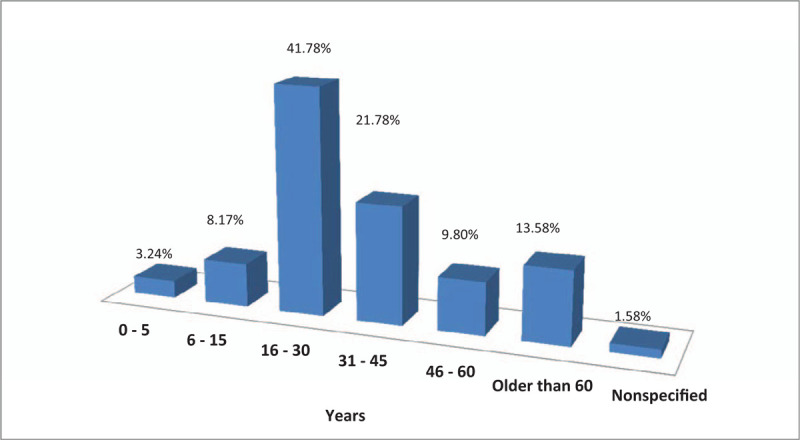
Distribution of trauma deaths per age range.
In Mexico, however, only 2.7% of the gross domestic product is designated to health services, which is the lowest rate among countries in the Organization of Cooperation and Economic Growth. While 77.8% of the population depends on the public health care system, of the other 22.2%, only 7% have private medical insurance.[7]
The objective of this section is to describe the trauma systems in Mexico, and to outline the main characteristics, strengths, and abilities. Understanding these conditions will allow for improvements in the systems and future outcomes of trauma patients in Mexico.
2.2. Systems review
Based on the methodology described by Colquhoun et al,[8] we performed a scoping review to analyze the trauma care systems (TCS) of Mexico. We included all available information written in the last 30 years in Spanish and English languages. We searched the PubMed, Cochrane, Medigraphic, and Scopus databases, plus local government data. We included and analyzed the following topics: health care providers, prehospital care, hospital trauma care, improvement projects, and the effects of implemented precautionary measures.
After excluding unrelated articles, repeated bibliography, or articles older than 30 years, we obtained 72 articles and statistical files. After analyzing and selecting relevant articles we ended up with 24 relevant references. Subsequently, we performed an analysis of the current status and existing improvement recommendations. Finally, we identified the main problems and the most suitable improvements.
2.3. Findings
In Mexico, public trauma care services are provided by several institutions (Fig. 3)[7]: the Mexican Institute of Social Security (IMSS), Institute of Social Security for Government Employees (ISSSTE), Secretary of Health (SSA), Institutes of Health for Petroleum Employees (PEMEX), Army Health System (SEDENA), Secretary of Marine Health System (SEMAR), and private hospitals.
Figure 3.
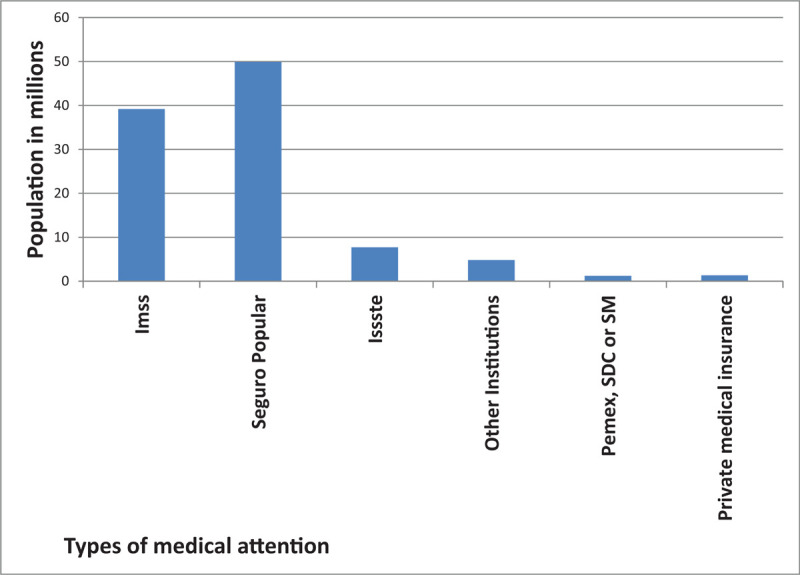
Amount of population affiliated with the different types of medical attention. Seguro Popular = Popular Insurance, SDC = Secretaria de la Defensa Nacional (Military Secretary), SM = Secretaria de Marina (Navy Secretary).
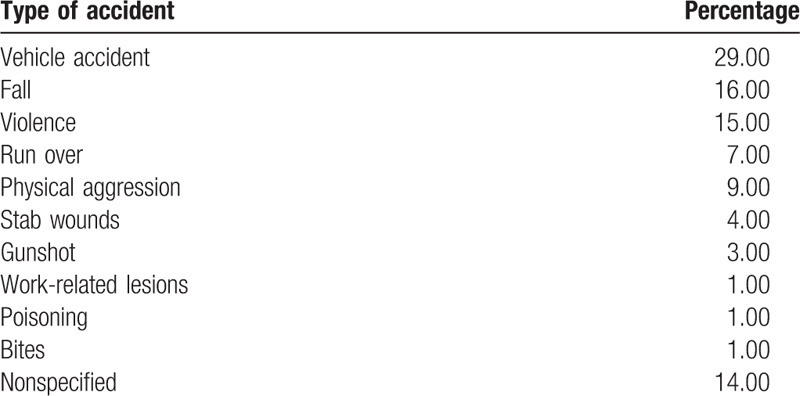
Around 29% of traumatic injuries are related to motor vehicle accidents (Table 1). Almost all these patients arrive to the hospital in ambulance. There are 3 types of ambulances in most cities: Red Cross, governmental, and private. For road traffic accidents, in most cities with more than 50,000 habitants all 3 types of ambulances may arrive at the scene, representing a waste of time and resources.
Table 1.
Causes of traumatic injury in Mexico.
Among the major problems with the Mexican prehospital emergency system, only 50% of the paramedics are salaried and thus have good training, while the rest are volunteers. The average response times for the major cities of Monterrey, Mexico City, and Queretaro is 23.13 minutes. Furthermore, there are still places where the emergency systems are not continually available.[6,9]
The trauma care centers in Mexico are divided into 3 levels. Level 1 centers are common health clinics with very limited resources, even for stabilizing patients with polytrauma; level 2 centers include general hospitals that can manage most common traumatic injuries; and level 3 trauma centers possess all of the resources needed to handle major traumatic injuries. While, in general, trauma management is efficient in big cities, there are still problems with coordinated prehospital care, such as the possibility of more than one ambulance arriving at the scene of an accident, and a lack of equipment in small hospitals and emergency centers.[10]
In Mexico, there are only 4 highest-level trauma centers in 3 cities (Monterrey, Puebla, and Mexico City). However, some private hospitals have the resources to treat polytrauma patients. Patients are referred to trauma centers based on a “red light” code to hospitals of the various hospital levels.[3,10] The first parameter for referral is the severity of the injuries (Fig. 4).[11] This decision is made by paramedics, but most of them have not taken the Prehospital Trauma Life Support (PHTLS) course. The patients designated as code red are taken to the best-equipped and closest hospitals; in the cities that have them, these patients are taken directly to a trauma center. The second parameter is the type of health care insurance. If a patient is in critical condition, the patient is initially stabilized in an emergency unit, and subsequent to the patient's stabilization, the patient can be referred to an appropriate hospital, either public or private. That decision is generally made independently of the severity of the injuries. For most cases at public hospitals, the patient must be referred to the closest second-level hospital, no matter the severity of the trauma. After evaluation at the second-level hospital, a patient can be referred to a third-level hospital if it is required. For private hospitals, the referral is based upon the patient's or family's choice.
Figure 4.
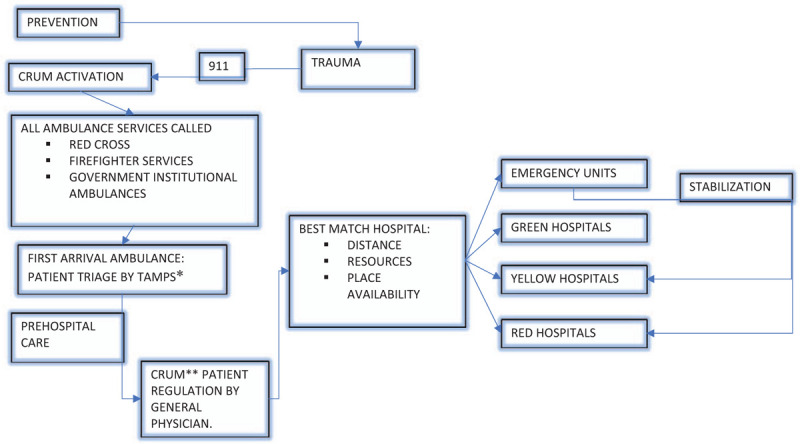
Step-by-step process for prehospital and hospital management of trauma patients by health services in Mexico. TAMPS∗ Medical Attention Pre Hospital Technicians CRUM∗∗ Medical Emergencies Regulatory Center.
There are several differences between hospitals upon the patient's arrival. Basic resources, such as IV fluids, oxygen, and x-rays, are present in the majority of level 1 units. In level 2 units, other medical personnel are available, such as vascular surgeons and anesthesiologists. Moreover, these centers typically have computed tomography scanners, external fixators, and blood banks, but during the night (between 9:00 pm and 7:00 am) such resources can be difficult to obtain. In general, public hospitals have established triage systems, and they are staffed with emergency doctors, orthopaedic surgeons, and general surgeons. Not all level 1 and 2 hospitals have Advanced Trauma Life Support (ATLS)-trained personnel,[10] particularly in rural areas. In hospitals with established residency programs, the residents generally handle initial management. In private hospitals, general practitioners perform the initial management, in conjunction with an intensive care unit if the hospital has one.
Several projects have been developed to improve trauma systems in Mexico; none of them have been applied in all states and units.[12–17] All the described projects have led to improvements in current trauma care, most of which focus on improving the training of involved health personnel, standardizing protocols, and improving material resources.
3. Discussion
In Mexico, the effectiveness of the public health system (PHS) is reduced due to a lack of ambulances and qualified personnel, the small number of emergency units, hospital overbooking with only 1.68 beds for each 1000 inhabitants,[18] long waiting times for surgery, and limited financial resources to treat patients which are common conditions in the public health services. Adding to these problems is the prehospital care system, system of medical urgency, which works through a telephone triage system to send all available ambulances to an accident zone. This has turned into a resource-consuming method, and it also requires significant time to attend to all needed emergency services. An improvement in this system will lead to lower costs and better patient outcomes, and provide faster medical attention.[19,20]
Another problem in Mexico's PHS is the universalization of health services. Seventy percent of the population lives in urban areas, while the other 30% lives in areas of fewer than 2500 habitants. As an effort to universalize the PHS, the Seguro Popular was implemented in 2006, improving PHS access from 35 million members in 2010 to 47.8 million in 2012.[18] Unfortunately, this measure is still insufficient for the universalization of health services in Mexico. The magnitude of Mexico's health service problems are still incompletely understood due to a lack of information and statistics, underscoring the need for more population-based research and data analysis.
In recent years, attention has been given to preventing trauma, specifically road traffic accidents. Such measures have lowered the incidence of traffic accidents from 476,279 in 2007 to 378,232 in 2015, which represents a decrease of 21%.[21] Efforts should be directed toward improving prevention strategies and the education of healthcare providers. All prehospital medical healthcare providers must be provided with PHTLS, and all the physicians involved in treating trauma patients should take the ATLS course.
4. Trauma system in Brazil
4.1. Introduction
In Brazil, trauma represents the third leading cause of death and 12.5% of deaths from all causes. Between the ages of 1 and 39 years, trauma is the leading cause of death, with a mortality rate of 70.5 cases per 100,000 inhabitants and male gender comprising 83.1% of the deaths.[22] Brazil has the fifth largest death rate in the world due to traffic injuries, with 28% resulting from motorbike accidents.[23]
Brazil is a large country, and just as large as its territory, is its health care inequality. The federal government provides universal access to health care. Every employed person has a tax deducted from his or her monthly checks for health care, and the coverage of the federal health system is universal to all, whether employed or unemployed. Around 10% to 15% of the population has private health insurance, either paid individually or by their employer, with different levels of coverage. Expensive plans cover everything in nice, modern hospitals and less expensive plans cover care in their own units.[24]
The 26 states of the Federation are divided into 5 regions, with the wealthier regions being in the south and southeast and poorer regions being in the north and northeast. The population of the northern region depends almost 100% on public health insurance, causing a huge overload on the public system. In the southern region, there are more patients who have private insurance and access to private hospitals, thereby easing the load on the public system. The burden on the PHS increases with national health crises that exacerbate unemployment and the subsequent loss of private insurance.[24,25]
The complexity of the public system is even larger considering that the financial support and administration are not done by one central unit, but by 3 different levels (federal, state, and municipality) that are unfortunately not well coordinated. In addition, the financial support varies according to how well the economy is going and is heavily influenced by politics.[25]
4.2. Sao Paulo: an example of the urban trauma care system
Sao Paulo city in its metropolitan areas has around 19 million inhabitants. Trauma care is divided in major and minor trauma. The state government with the support from the Municipality coordinates major trauma care. Severe accidents are first seen by rescue teams, whose responses are coordinated by a central station that directs them according to the expected severity of the injured patient. Paramedics on motorcycles are the first to arrive, and the central station can send an ambulance with paramedics or doctors or a helicopter with a doctor. After the initial assessment, the severity of the injury is determined and the patient triaged to an appropriate hospital.[26]
There are 5 level one trauma hospitals in the city: one in the north, one in the east, one in the south, one central, and one in the west region. In Sao Paulo, the west region hospital is the largest unit where the more severe cases are referred. In this unit, all the specialties, including trauma, vascular, neurologic, and thoracic surgeons, are present. For less severe injuries, the rescue team can take patients to smaller level 2 trauma centers or to private hospitals if they are insured. The trauma care in the 5 level 1 centers follows international guidelines for assessment and care. Unfortunately, they also suffer from weaker financial support from the government, which is also dependent upon the economy.
The care provided by private hospitals for elective cases is the same level as any other high-level hospital in North America or Europe, but these hospitals are not well prepared to treat severely injured patients because their volume is low and they do not have an emergency trauma team available 24/7.
Another issue that can be improved in Sao Paulo's trauma system is the referral mechanism. The communication between hospitals and the referral hierarchy could be improved. As hospitals are managed by different payors, the communication line can be lacking, and it is not uncommon for a patient to have to wait for days in the hospital due to lack of an implant.
4.3. Trauma care in small- and medium-sized cities
Trauma care in small- and medium-size cities is handled by municipally managed hospitals. If the city has a rescue system, the paramedics perform the first level of prehospital care, and then patients are transferred to the hospital, where they receive emergency care. In cases where there are no rescue systems, patients are transferred by the police or sometimes by family members. However, the major problem in the level 1 and level 2 hospitals is the definitive treatment. Due to an overload of patients and lack of resources such as operating room time, patients have to wait for days to have definitive fixation done. Delayed surgeries are quite common, and are associated with longer operating room times and greater complications. A better coordinated system is needed, with improved management and decreased political influence.
5. Conclusions
Trauma is a growing health problem worldwide. The morbidity and mortality of trauma is particularly high in third world countries and those with emerging economies, like those of Latin America, where about 90% of the burden of trauma occurs.[27] Furthermore, there are notable disparities in mortality rates for injured patients globally, with rates of 35% in high-income settings to 55% and 63% in middle- and low-income settings, respectively.[27]
Many studies have confirmed that proper TCS reduce morbidity and mortality. Likewise, population-based studies and trauma registry studies have shown a 15% to 20% reduction in the mortality of better organized systems.[19,28] For example, Nathens et al[20,29] published a population-based study demonstrating an 8% reduction of mortality in places with planned TCS in contrast compared to places without such planning.
Trauma care systems in Latin America, specifically Mexico and Brazil, provide adequate attention to simple trauma and polytrauma, but the systems are not ideal. The lack of universalization and standardization of systems across the various countries must be addressed, with authorities allocating greater resources for trauma care—one of the most common health problems. Nevertheless, there are some low-cost improvements to the system that can be implemented. More attention should be paid to preventing unintentional traumatic injuries to decrease mortality in Latin American populations.
Acknowledgements
The authors acknowledge the Mexican Federation of Orthopaedic and Trauma (FEMECOT) for support, and Adriana Echegoyen for her valuable cooperation.
References
- 1.INEGI. Número de habitantes [INEGI web site]. 2015. Available at: http://cuentame.inegi.org.mx/poblacion/habitantes.aspx?tema=P. [In Spanish]. Accessed September 19, 2019. [Google Scholar]
- 2.INEGI. Estadísticas a propósito del día mundial en recuerdo de las víctimas de los accidentes de tráfico (Tercer domingo del mes de Noviembre) [INEGI web site]. Available at: http://www.inegi.org.mx/saladeprensa/aproposito/2015/trafico0.pdf. Accessed on November 13, 2015. [In Spanish]. [Google Scholar]
- 3.Híjar-Medina MC. Los Accidentes Como Problema de Salud Pública En México. Mexico City: Intersistemas; 2014;[In Spanish]. [Google Scholar]
- 4.Almanza-Cruz S, Rea-Field G. A model system for emergency medicine for Mexico City. Gac Med Mex. 1990;126:423–430. in Spanish. [PubMed] [Google Scholar]
- 5.Smith GS, Barss P. Unintentional injuries in developing countries: the epidemiology of a neglected problem. Epidemiol Rev. 1991;13:228–266. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez GJI. Epidemiología del trauma en la ciudad de México. Asoc trauma Ciudad Mex. 2003;6:40–43. [In Spanish]. [Google Scholar]
- 7.INEGI. Encuesta Nacional de La Dinámica Demográfica 2014 [INEGI web site]. Available at: http://www.inegi.org.mx/saladeprensa/boletines/2015/especiales/especiales2015_07_1.pdf. Accessed on July 9, 2015. In Spanish. [Google Scholar]
- 8.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67:1291–1294. [DOI] [PubMed] [Google Scholar]
- 9.Fraga-Sastrías JM, Asensio-Lafuente E, Román-Morales F, et al. Sistemas médicos de emergencia en México. Una perspectiva prehospitalaria. Arch Med Urgencias México. 2010;2:25–34. in Spanish. [Google Scholar]
- 10.Arreola-Risa C, Mock C, Vega Rivera F, et al. Evaluating trauma care capabilities in Mexico with the World Health Organization's Guidelines for Essential Trauma Care publication. Rev Panam Salud Publica. 2006;19:94–103. [DOI] [PubMed] [Google Scholar]
- 11.Rodríguez-Cabrera R, Guevara-López U, Covarrubias-Gómez A, et al. Parámetros de práctica para el manejo del enfermo politraumatizado en el área de urgencias hospitalarias. Manejo del trauma ortopédico. Cir Ciruj. 2008;76:529–541. in Spanish. [Google Scholar]
- 12.Secretaría de Salud. Programa de Acción: Accidentes. 2002. Available at: http://www.salud.gob.mx/unidades/cdi/documentos/accidentes.pdf. In Spanish. Accessed September 24, 2019. [Google Scholar]
- 13.Díaz De MA, Ponce L, Olivares AB, Cruz F, Jesús V, Garduño CB. Trauma: Un problema de salud en México. Available at: https://www.anmm.org.mx/publicaciones/ultimas_publicaciones/TRAUMA.pdf. In Spanish. [Google Scholar]
- 14.Mock CN, Arreola-Rissa C, Vega F, et al. Fortaleciendo la atención del trauma en México y a nivel mundial: Proyecto Atención Esencial en Trauma. Trauma. 2004;7:5–14. in Spanish. [Google Scholar]
- 15.Mock C, Joshipura M, Goosen J, et al. Overview of the essential trauma care project. World J Surg. 2006;30:919–929. [DOI] [PubMed] [Google Scholar]
- 16.Arreola-Risa C, Mock CN, Lojero-Wheatly L, et al. Low-cost improvements in prehospital trauma care in a Latin American city. J Trauma. 2000;48:119–124. [DOI] [PubMed] [Google Scholar]
- 17.Arreola-Rissa C, Castilleja F, Mock CN, et al. En busca de la excelencia en la atención del trauma en México: ¿dónde estamos? ¿hacia dónde debemos ir? Trauma. 2001;4:81–84. In Spanish. [Google Scholar]
- 18.Consejo Nacional de Evaluación de la Política de Desarrollo Social Indicadores de Acceso Y Uso Efectivo de Los Servicios de Salud de Afiliados Al Seguro Popular. 2014;CONEVAL, Mexico City:in Spanish. [Google Scholar]
- 19.Jurkovich GJ, Mock C. Systematic review of trauma system effectiveness based on registry comparisons. J Trauma. 1999;47:S46–S55. [DOI] [PubMed] [Google Scholar]
- 20.Nathens AB, Jurkovich GJ, Cummings P, et al. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283:1990–1994. [DOI] [PubMed] [Google Scholar]
- 21.INEGI. Síntesis Metodológica de la Estadística de Accidentes de Tránsito Terrestre en Zonas Urbanas y Suburbanas. Aguascalientes, Mexico: [INEGI web site], August 2009. Available at: www.inegi.org.mx. [Google Scholar]
- 22.Ministério da Sa_ude: plano nacional de sa_ude—PNS, 2012–1015. Brasilia, DF: MS.2011. (Série B, Textos básicos de sau_de). Available at http://conselho.saude.gov.br/biblioteca/relatorios/plano_nacional_saude_2012_2015.pdf. [Google Scholar]
- 23.Ministério da Saúde. Agencia Saúde. Brasil é o quinto país no mundo em mortes por acidentes no trânsito, 2015. Disponível em: Available at: http://www.blog.saude.gov.br/35535-brasil-e-o-quinto-pais-no-mundo-em-mortes-por-acidentes-no-transito. [Google Scholar]
- 24.Pinto LP, Soranz DR. Ciencia Saude Coletiva. 2004;9:85.2.Furlan A, 2004 in https://educacao.uol.com.br/.../regioes-geoeconomicas-divisao-do-brasil-por-criterios. [Google Scholar]
- 25.Ministério da Saúde. Portaria n° 1.600, de 7 de julho de 2011. Reformula Política de Atenção às Urgências e institui a Rede de Atenção às Urgências (RAU) no Sistema Único de Saúde (SUS). Diário Oficial da União. Brasília, DF. Disponível em: Available at: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1600_07_07_2011.html. Accessed on July 7, 2011. [Google Scholar]
- 26.Ministerio da Saude, 2014. Available at: http://www.brasil.gov.br/saude/2014/01/sao-paulo-ganhara-novo-servico-para-atender-trauma. [Google Scholar]
- 27.MacLeod JBA. Guidelines for essential trauma care. J Trauma Acute Care Surg. 2005;58:652–653. [Google Scholar]
- 28.Mann NC, Mullins RJ, MacKenzie EJ, et al. Systematic review of published evidence regarding trauma system effectiveness. J Trauma. 1999;47:S25–S33. [DOI] [PubMed] [Google Scholar]
- 29.Nathens AB, Jurkovich GJ, Rivara FP, et al. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. [DOI] [PubMed] [Google Scholar]


