Abstract
Background:
Avascular necrosis of the femoral head typically occurs in the young population. Core decompression in the precollapse stage provides pain relief and preservation of the femoral head. The results of core decompression vary considerably despite the early diagnosis. Clinicians concur that primary treatment should focus on preserving the natural surface of the joint. This study investigated the predictive risk factors of failure in femoral head decompression.
Methods:
We retrospectively reviewed 135 patients and 207 hips (77 male (127 hips) and 58 female (80 hips)) who underwent core decompression (mean age: 34.7 years [age range: 21-71]) from April 2010 to December 2017. All patients were followed by a mean of 57 months. All hips were in the precollapse stage (Ficat I, II).
Results:
A total of 207 hips were treated with core decompression surgery, and the overall success rate was 58%. The higher grade of Kerboul, Ficat, ARCO classifications, multifocal avascular necrosis of the femoral head, smoking, opium, and corticosteroids were significantly associated with a higher failure rate after core decompression in univariate analysis. In multivariate logistic regression analysis, the Kerboul and Ficat classifications, alcohol consumption, and multifocal avascular necrosis of the femoral head were significantly correlated with core decompression failure. The most common predictive factors in core decompression failure were Ficat II, Kerboul stage 3, multifocal avascular necrosis of the femoral head, and alcohol consumption.
Conclusion:
In conclusion, we had an overall 58 % success rate in core decompression of femoral head avascular necrosis. Based on the results of this study, imaging evaluation and imaging-based classifications are the most valuable predictor factors for the success of core decompression. Consistent with previous reports, corticosteroid was not a significant predictor of core decompression failure.
Key Words: Avascular necrosis, Core decompression, Femoral head, Predictors
Introduction
Osteonecrosis/avascular necrosis of the femoral head is a pathologic condition arising from the disruption of blood circulation supplying the bone. Mainly young patients are involved with this disorder. 1-3 Multiple factors, including trauma, corticosteroids, smoking, alcohol, rheumatoid diseases, immunosuppressive drugs, and many other etiologic factors, have been considered risk factors for developing this pathology. Avascular necrosis is not associated with pain or motion limitation in the early stages, but as the condition progresses, painful hip motion establishes. 4 If the ischemia is not managed timely, the collapse of the femoral head will be inevitable, requiring total hip arthroplasty. 5-13 The goal of numerous treatments for osteonecrosis is to halt the progression of the damage to prevent the collapse of the femoral head. These treatments range from bisphosphonate therapy, hyperbaric oxygen, electrical stimulation, extracorporeal shock wave therapy, bone marrow mononuclear cell implantation, core decompression, and eventually total hip arthroplasty. 14-21
Core decompression surgery is considered a safe and effective treatment for patients in precollapse stages. Core decompression is usually performed by drilling and eliminating a segment from a necrotic lesion. 22,23 Modifications in technique have been suggested, such as multiple drillings, insertion of a porous tantalum implant, combined with bone grafting, or application of growth factors and bone-marrow cells. 24-30 This surgery relieves intraosseous pressure caused by venous congestion, allowing improved vascularity and possibly slowing the progression of the disease. 2,3,25,27,31 Despite the promising results of core decompression, some patients will require total hip replacement within 4 to 5 years. In this study, we aimed to investigate the risk factors associated with the failure/success of core decompression surgery in patients with femoral head avascular necrosis.
Materials and Methods
Study design
This study reviewed 140 patients (214 hips) with femoral head avascular necrosis who had core decompression surgery in our orthopedic department from April 2010 to December 2017. The diagnosis of avascular necrosis was established based on radiologic evaluation and clinical assessment. Patients whose medical records or radiologic images were missing were excluded from the study. Radiographs such as anterior-posterior (AP) and lateral views and MRI scans of patients were obtained and re-evaluated by an expert radiologist to assess the required parameters of the study. The variables were then analyzed to determine the correlation of different risk factors with surgical failure. The mean duration of follow-up was 4.8 ± 1.2 years (range: 6 months - 8 years). A total of 5 patients were lost to follow-up, and 135 patients (207 hips) entered the analysis.
The Institutional review board (IRB) of Tehran University of medical sciences reviewed and approved the study protocol and confirmed that there was no ethical concern with the study (Approval Code: IR.TUMS.IKHC.REC.1396.4076)
Variables
Medical records of patients were assessed for these variables:
• Demographics (age, gender, weight, height, and Body mass index (BMI))
• Past medical history (systemic lupus erythematosus, rheumatoid arthritis, lymphoma, inflammatory bowel disease, transplantation, and trauma)
• Drug history (weight gain agents, weight loss agents, corticosteroids, radiotherapy, and chemotherapy)
• Habitual history (smoking, alcohol, and opium)
• Imaging results (Ficat, ARCO, Kerboul, and multiple- versus uni-focal)
Classification
The first classification method used in our study was Ficat and Arlet system. In this classification system, stage 0 is defined as normal radiographs of the hip. Stage I is normal on radiographs but shows abnormalities on MRI. It may be accompanied by minor osteopenia changes. Stage II shows the development of sclerotic or cystic lesions categorized into two substages. Stage IIa reflects focal radiological changes, and stage IIb is associated with a crescent sign without femoral head flattening. Stage III is equivalent to flattening the femoral head or femoral head collapse while joint space is normal. Stage IV is femoral head collapse and osteoarthritis (joint space collapse and acetabular changes). 22 The ARCO classification system is also used to evaluate our cases which are demonstrated in [Table 1]. 32
Table 1.
The ARCO international classification of osteonecrosis of the femoral head
| Classification | ||
|---|---|---|
| 0 | biopsy results consistent with osteonecrosis; normal findings on all other tests | |
| I | Positive scintiscan or magnetic resonance image, or both | |
| I-A | < 15% involvement of femoral head | |
| I-B | 15 – 30% involvement of femoral head | |
| I-C | > 30% involvement of femoral head | |
| II | Radiographic abnormalities (mottled appearance of femoral head, osteosclerosis, cyst formation, and osteopenia); no crescent sign or evidence of collapse of femoral head on radiographs | |
| II-A | < 15% involvement of femoral head | |
| II-B | 15 – 30% involvement of femoral head | |
| II-C | > 30% involvement of femoral head | |
| III | Crescent sign | |
| III-A | < 15% involvement of femoral head or <2mm depression of femoral head | |
| III-B | 15 – 30% involvement of femoral head or 2 – 4 mm depression of femoral head | |
| III-C | > 30% involvement of femoral head or > 4 mm depression of femoral head | |
| IV | Osteoarthritis: Articular surface flattened radiographically and joint space shows narrowing; changes in acetabulum with evidence of osteosclerosis, cyst formation, and marginal osteophytes |
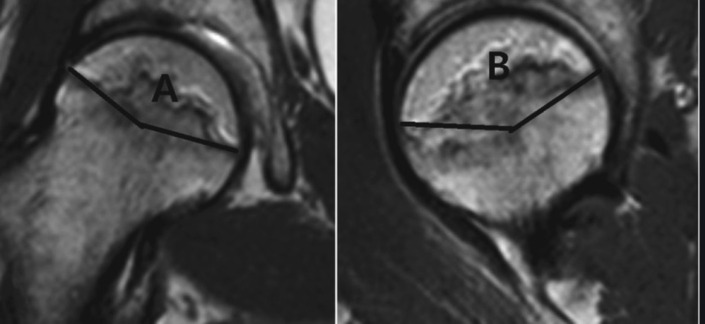
To assess the extent of necrosis in the femoral head, the Kerboul angle (combined necrotic angle) was used [Figure 1]. 33 To calculate this angle, the center of the femoral head is identified, and then two lines from this point to both borders of the necrotic area are drawn. The angle is measured on both AP and lateral radiographs. The sum of these two angles is the Kerboul angle, classified into three groups. Degrees of 160 and lower are considered small (Kerboul 1), degrees of 161 to 199 are medium (Kerboul 2), and degrees of 200 and higher are considered large involvements (Kerboul 3).
Figure 1.
Kerboul angle, Kerboul angle = A+B
The cases are also classified regarding multiple versus focal necrosis. Radiographs and MRIs are reevaluated for the detection of necrotic areas.
Failure of core decompression
A surgical failure is defined as the presence of the following conditions after six months of surgery: 1. Undergoing total hip arthroplasty due to severe symptoms, 2. Pain intensity of > 3 on the visual analog scale (VAS), and 3. Evidence of the necrosis progressing on imaging and further collapse.
Statistics
Statistical analysis was conducted with IBM SPSS version 22.0 (Chicago, IL, USA). Data are presented as mean ± standard deviation (SD) or frequency (%) whenever necessary. The Student’s t-test was used to compare quantitative variables in the success and failure groups. Multivariate regression analysis was performed to determine independent predictors of surgical failure. A P-value of <0.05 was considered significant for all tests (two-sided).
Results
A total of 207 hips that have been treated with core decompression surgery were analyzed in our study. The overall failure rate in our study was 78/207 (42%)cases.
Demographics of the patients
75/135 (56%) were males, and 60/135 (44%) were females. The mean age of patients in our study was 35±5.9 years (age range: 21-71). The patients’ mean weight was 75±13 kg (weight range: 50-119). The mean height of patients was 173±9.3 cm (range: 155-90). The mean BMI of patients was 26 ± 2.8 kg/m2 (BMI range: 21-38). Analysis of demographic parameters revealed no significant difference between success and failure groups [Table 2].
Table 2.
Demographic factors among patients with surgical success and failure
| Factor | Mean | P-value | |
|---|---|---|---|
| Success | Failure | ||
| Age | 33.7±4.9 | 34.9±4.6 | 0.48 |
| Weight | 75.2±8.3 | 75.4±8.0 | 0.53 |
| Height | 172.4±6.7 | 172.8±7.1 | 0.70 |
| BMI | 25.3±4.6 | 25.8±4.2 | 0.69 |
Past medical history
There were some factors in the history of the patients in our study: systemic lupus erythematosus (24 patients, 12%), Rheumatoid arthritis (18 patients, 8.7%), lymphoma (10 patients, 4.8%), irritable bowel disease (4 patients, 1.9%), transplantation (13 patients, 6.3%), and trauma (13 patients, 6.3%). Analysis showed no association between past medical conditions and failure of core decompression surgery [Table 3].
Table 3.
Past medical history, drug history, and habitual history among patients in surgical success and failure groups
| Risk factor | Positive | Negative | P-value | ||
|---|---|---|---|---|---|
| Failure | Success | Failure | Success | ||
| Past medical history | |||||
| Systemic lupus erythematosus | 9 (37.5%) | 15 (62.5%) | 78 (42.6%) | 105 (57.4%) | 0.63 |
| Rheumatoid arthritis | 9 (50%) | 9 (50%) | 60 (38.2%) | 97 (61.8%) | 0.41 |
| Lymphoma | 3 (30%) | 7 (70%) | 66 (40.9%) | 97 (59.1%) | 0.52 |
| Irritibale bowel disease | 0 (0%) | 4 (100%) | 87 (42.9%) | 116 (57.1%) | 0.11 |
| Transplantation | 8 (61.5%) | 5 (38.5%) | 79 (40.7%) | 115 (59.3%) | 0.26 |
| Trauma | 6 (46.2%) | 7 (53.8%) | 81 (41.8%) | 113 (58.2%) | 0.71 |
| Drug history | |||||
| Weight gain drugs | 26 (59.1%) | 18 (40.9%) | 61 (37.4%) | 102 (62.6%) | 0.15 |
| Weight loss drugs | 2 (28.6%) | 5 (71.4%) | 85 (42.5%) | 115 (57.5%) | 0.76 |
| Corticosteroid | 56 (48.7%) | 59 (51.3%) | 31 (33.7%) | 61 (66.3%) | 0.03 |
| Radiotherapy | 0 (0%) | 1 (100%) | 87 (42.2%) | 119 (57.8%) | 0.95 |
| Chemotherapy | 3 (33.3%) | 6 (66.7%) | 84 (42.4%) | 114 (57.6%) | 0.73 |
| Habitual history | |||||
| Smoking | 47 (61.1%) | 30 (39.0%) | 40 (30.8%) | 90 (69.2%) | <0.0001 |
| Alcohol consumption | 30 (73.2%) | 11 (26.8%) | 57 (35.6%) | 103 (64.4%) | <0.0001 |
| Opium consumption | 17 (85%) | 3 (15%) | 70 (37.4%) | 117 (62.6%) | <0.0001 |
Drug history
Evaluation of drug/therapy history in patients revealed the following results: weight gain drugs (44 patients, 21%), weight loss drugs (7 patients, 3.4%), corticosteroids (115 patients, 56%), radiotherapy (1 patient, 0.4%), and chemotherapy (9 patients, 4.3%). Further analysis indicated that drugs or therapies received by patients do not correlate with failure except for the consumption of corticosteroids. The details are shown in [Table 3].
Habitual history
Smoking was reported by 77 (37%) patients in our study. Alcohol consumption was positive in 41 patients (20%). Opium consumption was also observed in 20 (9.7%) patients. All these components of habitual history were significantly more prevalent in the failure group compared to successful cases. The details of these comparisons enlists in [Table 3].
Classifications based on imaging results
A total of 65 (31%) cases were categorized as Ficat stage I, while 142 (69%) cases were classified as Ficat stage II preoperatively. Kerboul angle calculations revealed that 66 (32%) patients in stage 1, 126 (61%) cases in stage 2, and 13 (6.28%) cases fall into stage 3. The results of ARCO classification for our cases were as follows: 1A (1 case, 0.4%), 1B (24 cases, 12%), 1C (26 cases, 13%), 2A (27 cases, 13%), 2B (63 cases, 30%) and 2C (66 cases, 32%). Evaluations showed that the lesion in
A total of 36 (17%) cases were multifocal, and 171 (83%) were unifocal. Analysis of the correlation between classifications and surgery outcomes has shown a significant positive association between the stage of avascular necrosis and the failure rate of surgery. Details are summarized in [Table 4].
Table 4.
Details of the results according to the classification of avascular necrosis, kerboul angle stage, and focality of the lesions
| Classification | Stage | Failure | Success | P-value |
|---|---|---|---|---|
| Ficat | 1 | 5 (7.7%) | 60 (92.3%) | 0.0001 |
| 2 | 82 (57.7%) | 60 (42.3%) | ||
| Kerboul | 1 | 6 (9.1%) | 60 (90.9%) | 0.0001 |
| 2 | 69 (54.8%) | 57 (45.2%) | ||
| 3 | 12 (92.3%) | 1 (7.7%) | ||
| ARCO | 1A | 0 (0%) | 1 (100%) | 0.0001 |
| 1B | 0 (0%) | 24 (100%) | ||
| 1C | 2 (7.7%) | 24 (92.3%) | ||
| 2A | 5 (18.5%) | 22 (81.5%) | ||
| 2B | 29 (46.0%) | 34 (54.0%) | ||
| 2C | 51 (77.3%) | 15 (22.7%) | ||
| Multifocal | Positive | 31 (86.1%) | 5 (13.9%) | 0.0001 |
| Negative | 56 (32.7%) | 115 (67.3%) |
To control the confounding factors, multivariate regression analysis was performed for variables with significant effects in univariate analysis. The regression analysis results revealed that alcohol consumption, Kerboul class, Ficat 2A class, and multifocal cases are independently and significantly correlated with failure of core decompression surgery (all P-values< 0.001).
Discussion
Femoral head avascular necrosis is an insidious condition that results in femoral head collapse. 34 Hence, timely diagnosis and effective intervention to prevent femoral head collapse are key principles in preserving the joint. The type of treatment plays a critical role in the final outcome. One of the main factors in choosing the treatment choice is the success rate of the procedure and the risk factors affecting its outcome. Core decompression surgery has been considered an effective and safe choice among joint-preserving surgery methods. We evaluated the success rate of this method in our patients and the factors that determine the surgery outcomes.
The primary outcome of our study was to determine the success/failure rate of core decompression. In our study, an overall success rate of 58% was achieved. Lee et al.8 and Song et al. 24 reported 56% and 68% success rates, respectively. It seems that the success rate in our study is comparable to those reported by previous studies. In the next step, we assessed the success rates in different stages of femoral head avascular necrosis classification systems. The most common staging method used in the literature is Ficat and Arlet classification. 22 In our study, the success rate in Ficat I and Ficat II stages was 93% and 46%, respectively, which are significantly different. Lavernia et al. 35 also reported that success rates in Ficat I, IIA, IIB, and III stages were 84%, 47%, 20%, and 0%, respectively.
A recent systematic review 36 on core decompression surgery also reported that success rates in stages I, II, and III were 78%, 59%, and 27%, respectively. As in our study, both mentioned studies also reported that the success rates were significantly different between different stages of the Ficat classification. In contrast, some studies claim no significant difference between Ficat stages regarding the success rate of surgery. Lee et al. 19 reported that the success rate in Ficat I and II stages were 67%. Song et al. 24 also reported that success rates in Ficat I and Ficat II stages were 79% and 77%, respectively. Our findings indicate that the disease stage is significantly correlated with surgical outcomes. Other classification methods also confirm these findings. In our study, ARCO I and ARCO II had 96% and 46% success rates, respectively. Kerboul 1, 2, and 3 groups had success rates of 91%, 45%, and 7.7%, respectively. Multifocal lesions had a success rate of 14%, while the unifocal disease was associated with a 67% success rate. A systematic review 36 also reported that success rates in ARCO I, II, and III stages were 95%, 78%, and 52%, respectively. Further analysis of the results also confirmed that higher Kerboul class, Ficat 2A class, and multifocal lesions are independent predictors of failure. Evaluation of other parameters in our study revealed that smoking, alcohol usage, opium, and corticosteroid consumption are risk factors for core decompression failure. However, multivariate regression analysis indicated that only alcohol consumption was an independent predictor of failure. The important point is that corticosteroid usage in our study was not a significant predictor of core decompression failure. Various studies have evaluated the risk factors and predictors of surgery failure. Unlike our study, Hyodo et al. 37 reported that age and BMI were predictors of core decompression failure. Tomaru et al. 38 also declared that gender and BMI>23.3 kg/m2 were risk factors for surgery failure, while in our study, there was no correlation between these parameters and surgery outcomes. Consistent with our findings, Lavernia et al. 35 confirmed that alcohol consumption was a predictor of core decompression failure but denied the correlation of the femoral head necrotic area with the success of surgery, which was proved in contrast to our findings. Smith et al. 39 also reported that Ficat significantly predicted surgical outcomes, but ARCO could not show any significant association. Scully et al. 40 suggested that age>37 years and Ficat were risk factors for failure, but corticosteroids were not correlated with surgery results. Consistent with our study, Amanatullah et al. 41 reported that the Kerboul angle was associated with the rate of failure/success of core decompression surgery.
The retrospective design of this study can be regarded as its main limitation. The retrospective design would limit the control of various parameters, which can confound the results. Prospective design can provide the researchers’ management of the dosage and duration of drug consumption(particularly corticosteroids and alcohol)by patients and assessment of the underlying conditions and the status of habits.
We had an overall 58 % success rate in core decompression of femoral head avascular necrosis. Based on the results of this study, imaging studies and imaging-based classifications are the most valuable predictors of the success of core decompression. The higher grade of the Kerboul and Ficat classifications, alcohol consumption, and multifocal avascular necrosis of the femoral head were significantly correlated with core decompression failure. Consistent with previous reports, corticosteroid consumption was not a significant predictor of core decompression failure.
Funding:
This research did not receive any specific funding.
Conflict of interests:
The authors declare that they have no relevant financial or non-financial interests to report.
References
- 1.Lieberman JR, Berry DJ, Montv MA, et al. Osteonecrosis of the Hip: Management in the Twenty-first Century. JBJS. 2002;84(5):834–53. [Google Scholar]
- 2.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88(5):1117–32. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 3.Mont MA, Ragland PS, Etienne G. Core decompression of the femoral head for osteonecrosis using percutaneous multiple small-diameter drilling. Clin Orthop Relat Res. 2004;(429):131–8. doi: 10.1097/01.blo.0000150128.57777.8e. [DOI] [PubMed] [Google Scholar]
- 4.Yu X, Zhang D, Chen X, Yang J, Shi L, Pang Q. Effectiveness of various hip preservation treatments for non-traumatic osteonecrosis of the femoral head: A network meta-analysis of randomized controlled trials. J Orthop Sci. 2018;23(2):356–364. doi: 10.1016/j.jos.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Jamshidi MM, Moharrami A, Sharifpour S, Mafi AR, Mortazavi SJ. The Role of Spinopelvic Parameters in Total Hip Arthroplasty: A Current Concept Review. Journal of Orthopedic and Spine Trauma. 2022;8(2):40–3. [Google Scholar]
- 6.Mirghaderi SP, Sharifpour S, Moharrami A, et al. Determining the accuracy of preoperative total hip replacement 2D templating using the mediCAD® software. J Orthop Surg Res. 2022 Apr;17(1):222 . doi: 10.1186/s13018-022-03086-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mortazavi SMJ, Ghadimi E, Ardakani MV, et al. Risk factors of dislocation after total hip arthroplasty in patients with developmental dysplasia of the hip. Int Orthop. 2022;46(4):749–759. doi: 10.1007/s00264-021-05294-w. [DOI] [PubMed] [Google Scholar]
- 8.Mirghaderi SP, Baghdadi S, Salimi M, Shafiei SH. Scientometric Analysis of the Top 50 Most-Cited Joint Arthroplasty Papers: Traditional vs Altmetric Measures. Arthroplast Today. 2022;15:81–92. doi: 10.1016/j.artd.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mirghaderi SP, Hoveidaei AH, Sheikhbahaei E, Motififard M, Moradi N, Moradi M. Femoral Stem Dislocation Caused by Trunnionosis Along with Adverse Local Tissue Reaction; A Case Report and a New Technique of Head to Cone Cementing. Arch Bone Jt Surg. 2022;10(10):911–915. doi: 10.22038/ABJS.2022.61214.3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mirghaderi SP, Raeini AG, Gholamshahi H, Mortazavi SMJ, Shafiei SH, Sheikhvatan M. Content Validity and Reliability of the Persian Version of the Forgotten Joint Score Questionnaire in Patients Undergoing Total Hip Arthroplasty. Arthroplast Today. 2022;15:40–42. doi: 10.1016/j.artd.2022.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirghaderi SP, Sheikhbahaei E, Salimi M, et al. COVID-19 infection rate after urgent versus elective total hip replacement among unvaccinated individuals: A multicenter prospective cohort amid the COVID-19 pandemic. Ann Med Surg (Lond) 2022;80:104307. doi: 10.1016/j.amsu.2022.104307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moharrami A, Mirghaderi SP, Hoseini-Zare N, et al. Restoring femoral medial offset could reduce pelvic obliquity following primary total hip arthroplasty, an observational study. Int Orthop. 2022;46(12):2765–2774. doi: 10.1007/s00264-022-05506-x. [DOI] [PubMed] [Google Scholar]
- 13.Sheikhbahaei E, Mirghaderi SP, Moharrami A, Habibi D, Motififard M, Mortazavi SMJ. Incidence of Symptomatic COVID-19 in Unvaccinated Patients Within One Month After Elective Total Joint Arthroplasty: A Multicenter Study. Arthroplast Today. 2022;14:110–115. doi: 10.1016/j.artd.2022.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ebrahimpour A, Sadighi M, Hoveidaei AH, et al. Surgical Treatment for Bisphosphonate-related Atypical Femoral Fracture: A Systematic Review. Arch Bone Jt Surg. 2021;9(3):283–296. doi: 10.22038/abjs.2020.52698.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong YC, Luo RB, Lin T, Zhong HM, Shi JB. Efficacy of alendronate for preventing collapse of femoral head in adult patients with nontraumatic osteonecrosis. Biomed Res Int. 2014;2014:716538. doi: 10.1155/2014/716538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uzun G, Mutluoglu M, Ersen O, Yildiz S. Hyperbaric oxygen therapy in the treatment of osteonecrosis of the femoral head: a review of the current literature. Undersea Hyperb Med. 2016;43(3):189–99. [PubMed] [Google Scholar]
- 17.Oliaei S, SeyedAlinaghi S, Mehrtak M, et al. The effects of hyperbaric oxygen therapy (HBOT) on coronavirus disease-2019 (COVID-19): a systematic review. Eur J Med Res. 2021;26(1):96 . doi: 10.1186/s40001-021-00570-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Jabri T, Tan JYQ, Tong GY, et al. The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: a systematic review. BMC Musculoskelet Disord. 2017;18(1):319–319. doi: 10.1186/s12891-017-1663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee J-Y, Kwon J-W, Park J-S, et al. Osteonecrosis of Femoral Head Treated with Extracorporeal Shock Wave Therapy: Analysis of Short-term Clinical Outcomes of Treatment with Radiologic Staging. Hip Pelvis. 2015;27(4):250–257. doi: 10.5371/hp.2015.27.4.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yan ZQ, Chen YS, Li WJ, et al. Treatment of osteonecrosis of the femoral head by percutaneous decompression and autologous bone marrow mononuclear cell infusion. Chin J Traumatol. 2006;9(1):3–7. [PubMed] [Google Scholar]
- 21.Pierce TP, Jauregui JJ, Elmallah RK, Lavernia CJ, Mont MA, Nace J. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr Rev Musculoskelet Med. 2015;8(3):228–32. doi: 10.1007/s12178-015-9280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ficat RP. Idiopathic bone necrosis of the femoral head Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67(1):3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 23.Kapadia BH, Banerjee S, Cherian JJ, Jauregui JJ, Mont MA. Principles of Core Decompression for Osteonecrosis of the Hip. In: Koo K-H, Mo., editor. Osteonecrosis. Springer Berlin Heidelberg; 2014. pp. 279–284. [Google Scholar]
- 24.Song WS, Yoo JJ, Kim Y-M, Kim HJ. Results of multiple drilling compared with those of conventional methods of core decompression. Clin Orthop Relat Res . 2007;454:139–46. doi: 10.1097/01.blo.0000229342.96103.73. [DOI] [PubMed] [Google Scholar]
- 25.Liu ZH, Guo WS, Li ZR, et al. Porous tantalum rods for treating osteonecrosis of the femoral head. Genet Mol Res. 2014;13(4):8342–52. doi: 10.4238/2014.October.20.10. [DOI] [PubMed] [Google Scholar]
- 26.Nadeau M, Séguin C, Theodoropoulos JS, Harvey EJ. Short term clinical outcome of a porous tantalum implant for the treatment of advanced osteonecrosis of the femoral head. Mcgill J Med. 2007;10(1):4–10. [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Li L, Shi ZJ, Wang J, Li ZH. Porous tantalum rod implant is an effective and safe choice for early-stage femoral head necrosis: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol. 2013;23(2):211–7. doi: 10.1007/s00590-012-0962-7. [DOI] [PubMed] [Google Scholar]
- 28.Steinberg ME, Larcom PG, Strafford B, et al. Core Decompression With Bone Grafting for Osteonecrosis of the Femoral Head. Clin Orthop Relat Res . 2001;(386):71–8. doi: 10.1097/00003086-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Li X, Xu X, Wu W. Comparison of bone marrow mesenchymal stem cells and core decompression in treatment of osteonecrosis of the femoral head: a meta-analysis. Int J Clin Exp Pathol. 2014;7(8):5024–30. [PMC free article] [PubMed] [Google Scholar]
- 30.Gangji V, Hauzeur JP, Matos C, De Maertelaer V, Toungouz M, Lambermont M. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells A pilot study. J Bone Joint Surg Am. 2004;86(6):1153–60. doi: 10.2106/00004623-200406000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;466(5):1093–103. doi: 10.1007/s11999-008-0184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardeniers J. A new international classification of osteonecrosis of the ARCO-committee on terminology and classification. ARCO news. 1992;4:41–46. [Google Scholar]
- 33.Kerboul M, Thomine J, Postel M, d’Aubigné RM. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56(2):291–6. [PubMed] [Google Scholar]
- 34.Mortazavi SMJ, Moharrami A, Shafiei H, Ebrahimzadeh MH, Karimi M. Unapproved Weight Gain Supplement as a Cause of Avascular Necrosis: A Cautionary Report. Arch Bone Jt Surg. 2019;7(6):561–565. [PMC free article] [PubMed] [Google Scholar]
- 35.Lavernia CJ, Sierra RJ. Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty. 2000;15(2):171–8. doi: 10.1016/s0883-5403(00)90132-3. [DOI] [PubMed] [Google Scholar]
- 36.Hua KC, Yang XG, Feng JT, et al. The efficacy and safety of core decompression for the treatment of femoral head necrosis: a systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):306 . doi: 10.1186/s13018-019-1359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hyodo K, Yoshioka T, Sugaya H, et al. Predicting risk factors of total hip arthroplasty conversion after concentrated autologous bone marrow aspirate transplantation for the treatment of idiopathic osteonecrosis of the femoral head: a retrospective review of 213 hips at a mean follow-up of 5 years. The Journal of Hip Surgery. 2017;1(01):007–013. [Google Scholar]
- 38.Tomaru Y, Yoshioka T, Sugaya H, et al. Ten-year results of concentrated autologous bone marrow aspirate transplantation for osteonecrosis of the femoral head: a retrospective study. BMC Musculoskelet Disord. 2019;20(1):410. doi: 10.1186/s12891-019-2797-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77(5):674–80. doi: 10.2106/00004623-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Scully SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 1998;80(9):1270–5. doi: 10.2106/00004623-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Amanatullah DF, Strauss EJ, Di Cesare PE. Current management options for osteonecrosis of the femoral head: part 1, diagnosis and nonoperative management. Am J Orthop (Belle Mead NJ). 2011;40(9):E186–92. [PubMed] [Google Scholar]