Abstract
Aims
Aseptic loosening is the most common cause of failure following cemented total knee arthroplasty (TKA), and has been linked to poor cementation technique. We aimed to develop a consensus on the optimal technique for component cementation in TKA.
Methods
A UK-based, three-round, online modified Delphi Expert Consensus Study was completed focusing on cementation technique in TKA. Experts were identified as having a minimum of five years’ consultant experience in the NHS and fulfilling any one of the following criteria: a ‘high volume’ knee arthroplasty practice (> 150 TKAs per annum) as identified from the National joint Registry of England, Wales, Northern Ireland and the Isle of Man; a senior author of at least five peer reviewed articles related to TKA in the previous five years; a surgeon who is named trainer for a post-certificate of comletion of training fellowship in TKA.
Results
In total, 81 experts (round 1) and 80 experts (round 2 and 3) completed the Delphi Study. Four domains with a total of 24 statements were identified. 100% consensus was reached within the cement preparation, pressurization, and cement curing domains. 90% consensus was reached within the cement application domain. Consensus was not reached with only one statement regarding the handling of cement during initial application to the tibial and/or femoral bone surfaces.
Conclusion
The Cementing Techniques In Knee Surgery (CeTIKS) Delphi consensus study presents comprehensive recommendations on the optimal technique for component cementing in TKA. Expert opinion has a place in the hierarchy of evidence and, until better evidence is available these recommendations should be considered when cementing a TKA.
Cite this article: Bone Jt Open 2023;4(9):682–688.
Keywords: Knee arthroplasty, Cementation, Cementing technique, Aseptic loosening, cementing techniques, Knee Surgery, total knee arthroplasty (TKA), knee arthroplasty, National Joint Registry, cemented total knee arthroplasty, bone cement, tourniquets, knee
Introduction
Lower limb arthroplasty is a cost-effective intervention which significantly improves the quality of life for patients with hip and knee osteoarthritis.1,2 Total knee arthroplasty (TKA) and total hip arthroplasty (THA) are performed in almost equal numbers according to the 2022 19th annual report of the National Joint Registry (NJR), which collects data for England, Wales, Northern Island, the Isle of Man, and Guernsey.3 The same report demonstrates that only 30.7% of all THAs are fully cemented compared to 95.3% of all TKAs.3 Despite the disparity of cementing rates between THA and TKA, there remains very limited literature or consensus on the optimal cementing technique for TKA. In comparison, there are well-recognized and improved cementing techniques for THA which have evolved over time.4,5
Failure after TKA may be for many different reasons.6,7 Early implants commonly failed as a result of polyethylene delamination, leading to wear and subsequent osteolysis. Following improvements in polyethylene technology, implant design, and surgical techniques, this is now rare and superseded by other failure modes.3,8 As other causes of TKA failure have been progressively addressed, aseptic loosening has become the most common failure mode and indication for revision surgery in the UK. This is mirrored in registry data from Australia and New Zealand.3,9 A recent data analysis from the New Zealand Joint Registry has shown the lifetime risk of aseptic loosening to be as high as 5.9% for females and 6.4% for males under the age of 50 years.1 Aseptic loosening can present as both early and late failures of TKA. Aseptic loosening of the tibial component is seen more frequently than femoral loosening, and has been linked to poor cementing technique.10-12
Since the inception of the NJR, there has been a year-on-year increase in the number of TKAs performed and this trend is predicted to continue.3 Given the number of TKAs performed, the morbidity associated with a failing TKA, and the healthcare costs associated with revision TKA, it is imperative to optimize longevity of this procedure. As poor cementing may be correlated with the risk of aseptic loosening, it seems intuitive to ensure optimal cementing techniques, but there is a paucity of evidence to guide what this may entail. Current UK guidelines related to TKA include the 2020 National Institute for Health and Care Excellence (NICE) arthroplasty guidance,13 and the best practice for knee arthroplasty surgery document.14 While valuable, neither of these documents include any guidance on the optimal cementing technique to be used when performing TKA.
Given the lack of evidence, obtaining a balanced perspective from a large cross-section of experienced knee arthroplasty surgeons who are actively involved in performing, training, and research in TKA is important. Such consensus group methodologies are defined as a systematic means to assess, develop, and define levels of agreement between individuals. In the hierarchy of evidence, expert consensus opinion has a place, particularly in the absence of more robust data. With this background in mind the aim of our study was to develop comprehensive recommendations for Cementing Technique in Knee Surgery (CeTIKS) using a modified Delphi technique with expert knee surgeons across the UK.
Methods
Design of the modified Delphi study
The Delphi technique is a validated form of consensus methodology used in formulating an opinion within a group of experts. A three-round, modified Delphi consensus design was completed. A systematic literature search was performed during the initial phase of the CeTIKS study to identify any evidence related to TKA cementing technique. The information gathered from the literature search was only intended to formulate themes and questions for the formulation of the Delphi consensus. As the current literature on cementing techniques is limited, the literature review was not sent to the experts in order to prevent introducing confounders and leading experts into answers. Based on this data, we categorized TKA cementing into four key stages: 1) surface preparation; 2) cement application; 3) pressurization; and 4) cement curing.
These key stages were considered question domains and expanded into 25 statements as part of round 1 of the Delphi process.
Inclusion and exclusion criteria
Our criteria for expert inclusion were five years or more of national registry data as an orthopaedic consultant, and at least one of the following: 150 or more TKAs per year (identified from the NJR); five or more peer-reviewed publications in the last five years related to knee arthroplasty; and named trainer on a post-CCT knee arthroplasty fellowship in the UK.
The number of experts included in Delphi consensus studies varies in the literature, however a minimum of 30 experts in each round is required for vigorous analysis.15 We aimed for wide participation across the UK to ensure validity and reliability of the consensus process. Following identification, all suitable experts were invited by email to contribute to the CeTIKS study. The invitation included an information letter describing the study process and what participation involved. Participants were asked to confirm their consent to participate as well as their name, degree, institution, and email address. Individual responses from the experts remained confidential and were blinded to the principal investigators. Participation in this study was voluntary, and participants were offered no financial incentive or reimbursement. The senior authors of the study (CPC, PMS) were not included in the study group in order to remain impartial.
Development of Delphi statements
Four domains with a total of 25 statements were created. Round 1 focused on open-ended questions allowing experts to describe their individual cementing techniques. After establishing key themes from round 1, round 2 focused on direct and closed statements. Finally, round 3 explored in more detail those remaining statements for which expert consensus had not already been achieved. At the end of each section, there was a free-text box where experts could add suggestions relating to the statements that could be evaluated in subsequent rounds. In each subsequent round, experts were presented with the percentage consensus from the previous round and a reminder of their own previous response.
Delivery of the Delphi survey
The CeTIKS Delphi study survey was delivered electronically using an online web-based survey platform, Google Forms. The email included a covering letter to the experts and an electronic link to the survey. Only invited experts had access to the survey, and experts could only complete each round once.
Invited experts who failed to respond were contacted via email with a maximum of three invites at weekly intervals, and were also reminded via email to their secretary. Each round lasted for four weeks. All three rounds were completed in 2022. Expert responses were blinded prior to analysis by the principal investigators.
Data analysis
Analysis of the expert responses for each round were undertaken by the principal investigators before the statements were agreed for subsequent rounds. As there is no universal agreement on what defines consensus, we mirrored that of recent literature and used a threshold of 70% agreement.16 We defined this as accepting consensus prior to submitting the first survey. This threshold was further categorized with the consensus criteria used during the second International Consensus Meeting on Prosthetic Joint Infection (PJI) at Philadelphia in 2018.16
Results
The CeTIKS Delphi consensus study received expert representation from across the UK (Figure 1, Table I). A total of 81 experts completed round 1, with 80 experts completing the following 2 rounds of the study. One expert withdrew from the study after completing the first round. 100% consensus was reached within the cement preparation, pressurization, and cement curing domains. 90% consensus was reached within the cement application domain. All domains, statements, and results are shown in Tables II and V.
Fig. 1.
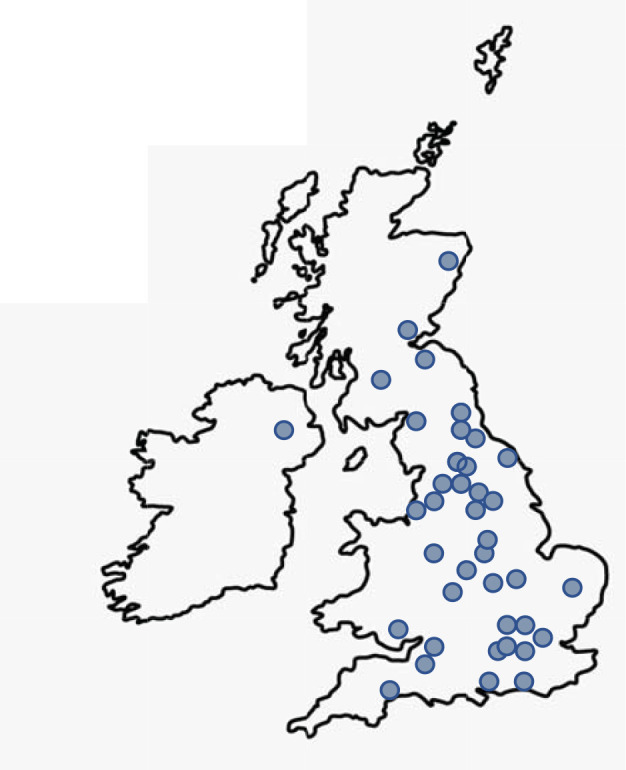
Distribution of experts across the UK.
Table I.
Expert demographics.
| Variable | Value |
|---|---|
| Mean years in practice as consultant knee surgeon (range) | 15 (5 to 30) |
| Mean primary TKAs/year (range) | 147 (10 to 500) |
| Mean revision TKAs/year (range) | 19 (0 to 70) |
| Registrar or fellowship trainer, n (%) | 75 (94) |
| Committee member for a Society, n (%) | 25 (31) |
TKA, total knee arthroplasty.
Table II.
Consensus statements on surface preparation.
| Statement | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) |
|---|---|---|---|
| I recommend pulsed lavage to clean the prepared bone surfaces prior to cementing | 99 | 99 | - |
| I recommend preparation of a sclerotic tibial surface (drill/jig pin/K-wire/saw/burr/other) | 99 | 100 | - |
| I recommend drying the bone surfaces prior to cementing (suction/swab/intraosseous) | 100 | 100 | - |
| If a tourniquet is used, it should remain inflated while cementing | 97 | 97 | 98 |
| If wetting surgical gloves prior to handling cement, wet cement surfaces should be dried prior to implant insertion | - | 64 | 92 |
| I recommend filling the femoral intramedullary jig entry point | 73 | 78 | - |
K-wire, Kirschner wire.
Table V.
Consensus statements on cement curing.
| Statement | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) |
|---|---|---|---|
| While the cement cures, the leg is preferably placed between hyperextension and 30° flexion (but NOT hyperextension or deep flexion) | 68 | 72 | - |
| While the cement is curing, it is acceptable to clear cement from the notch and/or wash the joint (taking care to avoid movement at the joint) | 50 | 87 | - |
| I recommend waiting until the cement is partly cured or fully cured before closing the joint | 88 | 90 | - |
Table III.
Consensus statements on cement application.
| Statement | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) |
|---|---|---|---|
| I recommend high- or medium-viscosity cement (but NOT low-viscosity) for routine primary knee arthroplasty | 88 | 98 | - |
| I recommend using antibiotic-loaded cement for primary knee arthroplasty | 100 | 100 | - |
| When mixing cement I recommend using a vacuum-assisted device | 95 | 96 | - |
| For routine primary knee arthroplasty I recommend cementing all components with a single cement mix (the desired number of cement packs are combined and mixed in one go) | 90 | 90 | |
| I recommend applying cement to the tibial bone and tibial implant | - | - | 75 |
| I recommend applying cement to the femoral bone and femoral implant | - | - | 78 |
| Where applicable, I recommend applying cement to the tibial flat surface and keel canal | 88 | 100 | - |
| If blood and/or fat contaminates the cement surface prior to implant insertion I would recommend to wash and/or dry then continue with insertion of the implant | 96 | 99 | - |
| Initial application of cement to the tibial bone should be with an instrument (cement gun, syringe, spatula, osteotome, etc) and not touched by hand | 64 | - | 65 |
| Initial application of cement to the femoral bone should be with an instrument (cement gun, syringe, spatula, osteotome, etc) and not touched by hand | 64 | - | 50 |
Table IV.
Consensus statements on pressurization.
| Statement | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) |
|---|---|---|---|
| I recommend insertion and impaction of the tibial tray | 96 | 100 | - |
| I recommend insertion and impaction of the femoral component | 99 | 100 | - |
| I recommend pressurizing the tibial component mainly with an impactor | 85 | 98 | - |
| I recommend pressurizing the femoral component mainly with an impactor | 90 | 100 | - |
| I recommend using an actual size insert while the cement cures | 99 | 99 | - |
There were only two statements where consensus was not reached, relating to the initial application of cement to the tibial and femoral bone surfaces: ‘Initial application of cement to the [tibial/femoral] bone should be with an instrument (cement gun, syringe, spatula, osteotome, etc.) and not touched by hand’. This specifically relates to whether or not cement should be handled at any timepoint prior to impaction of implants, and consensus may not have been reached due to the ambiguity of the statement wording.
Discussion
To the best of our knowledge, this is the first national consensus agreement on cementing techniques in TKA. With this consensus, we are able to provide comprehensive recommendations for each step in the cementing process of the tibial and femoral components when performing primary cemented TKA.
The NJR reports the prosthesis time incidence rates (PTIR) per 1,000 prosthesis years for each indication for revision of cemented TKA, which ascertains that the most common cause of failure of cemented TKA is now aseptic loosening.3 The PTIR for aseptic loosening or lysis is 0.96 (95% CI 0.94 to 0.98), which is substantial when considering 74,172 cemented TKAs were implanted in the UK during 2021.3 Although aseptic loosening may be of multifactorial aetiology, poor cementing technique has been shown to influence this. Aseptic loosening is not only a common cause of late TKA failures, but can also be associated with early failure, with evidence that up to 11% of revision TKAs performed within one year of the index surgery failed by this mode.17 A recent study suggested that early TKA loosening occurs at the tibial cement implant interface, and that the cementing process including choice of cement, application of cement, and the cement mantle have been directly linked with these early failures.17 It is well documented that the outcome of revision TKA is worse than primary TKA, and that revision TKA is associated with patient morbidity, mortality, high healthcare costs, and failure rates.18,19 It is therefore essential to strive for implant longevity and prevent early failures of primary TKA whenever possible. The authors believe that a reproducible and effective cementing technique is integral to this.
There are almost equal numbers of TKAs and THAs performed annually in the UK, and for THA there are well-accepted systematic steps for cementing, particularly the femoral stems. These described steps include pulsatile lavage of the femoral canal, use of epinephrine-soaked swabs, vacuum cement mixing, retrograde cement introduction, cement pressurization, and the use of stem centralizers.4 In contrast to THA, there has been no widely accepted or published recommendations for a systematic approach to cementing a TKA, and we believe our study should provide a framework for this.
Surface preparation prior to any cementing technique is essential to ensure adequate cement penetration within the cancellous bone, which has been shown to play an important role in reducing micromotion of the implant. Consensus was agreed on using pulsed lavage to clear bone debris, blood, and fat; appropriately drying the cut bone surfaces prior to cementing; drilling sclerotic bone to ensure adequate penetration; and inflating a tourniquet prior to cementing (if one is used) to ensure bone surfaces are dry.
It was agreed that pulsed lavage is superior to other techniques such as irrigation with a syringe. This has also been demonstrated in both cadaveric and clinical studies which have shown improved cement penetration depth, better bone-cement interface strength, and significantly better pull-out force when pulsed lavage was used.20-22
Drilling sclerotic bone has been shown to increase cement penetration on postoperative radiographs in clinical studies as well as improving pull-out strength in cadaveric studies,23,24 but as yet, there are no clinical studies showing that this improves implant survivorship. The heterogenous nature of TKA failure means such a study may be difficult or impossible.
Drying the bone surfaces can be achieved using simple suction, swabs, or intraosseous negative pressure suction catheters. Although some studies have recommended use of negative pressure suction, it has yet to be proven to be of any clinical benefit.25-27 Whichever technique is chosen, it was agreed that it is essential to ensure there is no debris, soft-tissue, fat, or blood blocking the cancellous bone surface prior to cement application.
The use of tourniquets in TKA helps provide a bloodless field which improves intraoperative visualization and delivers dry bone surfaces for cement application. A recent Cochrane review by Ahmed at al28 concluded that the use of a tourniquet in TKA was associated with minimal short-term clinical benefits but a significantly increased risk of perioperative complications, including venous thromboembolism, infection, reoperation, and postoperative pain. Despite the evident early benefits of not using a tourniquet, there remains concern about the long-term effects due to blood contamination of the bone-cement interface, leading to poor implant fixation and decreased implant survival. The question of whether or not to use a tourniquet remains controversial, and this study was not designed to address it. However, of those experts who used tourniquets, there was a consensus that as a minimum it should be inflated for the cementing process.
When considering cement application, the following consensus was achieved: the cement should be medium- or high-viscosity and loaded with antibiotics; it should be mixed in a vacuum device; it should be applied to both the back side of the tibial/femoral implants as well as the surface of both bones; the tibial surface and keel should both be cemented; and any blood, water, or fat on the surface of the cement should be dried prior to implantation.
There was no consensus that the initial application of the cement should be performed by hand, instruments, or a cement gun. It is of interest that the experts felt low-viscosity cement should not be used, as a study by Wyatt et al29 suggested that the viscosity of the cement does not influence the long-term revision rates in TKA. It was felt important to apply cement to both the back side of the component and the cut surface of the bone; this is supported by evidence.30-32
It has also recently been shown that fat between the implant and the bone cement can result in a reduction of resistance to pull-out of the tibial tray to near zero.31 Applying cement to the back of the tibial tray can prevent the back side of the tray being contaminated with fat, and therefore improve the pull-out strength even if fat was to inadvertently contaminate the interface between the cement on the back of the prosthesis and the cement on the cut bone surface.
Applying cement to the back side of the components at the earliest possible stage while the cement is ‘wetter’ has been shown to increase strength characteristics compared to its application at a later, ‘doughier’ phase.33 No consensus was reached on how the initial application of cement should be carried out, and we note that there is little evidence guiding this. However, the use of an instrument may allow easier cement application during the ‘wet phase’, and use of a cement gun has been shown to improve both cement penetration and mantle compared to hand packing or spatula application.34,35
When considering the pressurization stage of cementing, the following consensus was reached: both the tibial and femoral implants should be pressurized with impactors; the knee should be held in a fixed position while the cement partly or fully cures; and holding the hyperextension or deep flexion should be avoided.
Keeping the knee in a fixed position while the cement cures following implantation of the components is a logical step aiming to minimize micromotion between the interfaces. This consensus opinion is supported by a recent cadaveric study of four different contemporary TKA designs, which showed that knee motion during cement polymerization resulted in significant decreases in the implant fixation strength.36
The Delphi technique is a well-recognized consensus methodology used to formulate an opinion within a group of experts. It is often used when there is uncertainty and an absence of higher levels of evidence, but we recognize the limitations of this research method and our study: first, there is no definition of an expert within the literature. To address this, we used inclusion criteria in line with other recent Delphi studies and covered a range of attributes considered to represent expertise. Likewise, there is no rigid definition of consensus within the literature, but in our study protocol we pre-determined 70% agreement in line with previous studies.15,16 Considering this ambiguity, and to minimize bias, the threshold was further categorized using the consensus criteria used during the second International Consensus Meeting on Prosthetic Joint Infection (PJI) in Philadelphia in 2018.
We acknowledge that this study was carried out entirely within the UK and with UK surgeons. We recognize that TKA is a common procedure around the world, and that this study does not justify recommendations for cementing techniques outside the UK. However, we believe TKA failure modes are universal, and registry data from outside the UK support this. It is therefore important that cementing techniques are considered in healthcare settings outside the UK; this consensus may provide a relevant framework.
Finally, participant dropout has been reported to be a difficulty with the Delphi technique,37 however, in our study only a single expert did not complete each round, and this is unlikely to influence the outcome.
In conclusion, there has been recent justified enthusiasm into researching implant design, patient-specific instrumentation, and robotics, with the aim of improved accuracy, outcomes, and satisfaction levels following TKA. However, with all these recent advancements in TKA, it should not be overlooked that a meticulous cementing technique at the time of implantation remains fundamental to preventing aseptic loosening, and therefore early failure of TKA. This study provides the most comprehensive recommendations on cementing techniques in TKA from a large group of UK experts. We believe these recommendations should be considered by surgeons who perform TKA surgery as well as best practice documents.
Take home message
- Cementing technique has been linked to aseptic loosening of total knee arthroplasty (TKA), which leads to both early and late failure.
- This is the first consensus study which provides robust guidance and best practice for cementing techniques in TKA.
Author contributions
M. Hampton: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft.
V. Balachandar: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft.
C. P. Charalambous: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing.
P. M. Sutton: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Data sharing
All data generated or analyzed during this study are included in the published article and/or in the supplementary material.
Acknowledgements
The CeTIKS Study Group: Aaron Biing Yann Ng, Ajit Shetty, Alasdair J A Santini, Andrew Barnett, Andrew Gordon, Andrew Hamer, Andrew Port, Ben Bloch, David Johnson, Fazal Ali, Geoffrey Verne Johnson, Ivan Brenkel, Jim Holland, James Brian Newman, James Stoddard, Jeremy Mark Wilkinson, Jonathan Phillips, Mark Bowditch, Matt Dawson, Mohammad Tomouk, Stephen Blair, Paul Baker, Paul Haslam, Paul Jermin, Pedro Foguet, Peter Gallacher, Philip Turner, Philip Walsmley, David Sochart, Tim Broad, Richard Spencer Jones, Robert Kerry, Saif Salih, Sandeep Datir, Simon Buckley, Simon Jameson, Tim Harrison, Tim Spalding, Tom Symes, Amanda Hawkins, Carl Green, Peter Young, Chloe Scott, Adili Ajuied, Ajeya Raj Adhikari, Andrew Armitage, Anthony Joseph Gibbon, Antony Langley Smith, Anwar Jafri, Charles Willis-Owen, David John Deehan, David John Weir, George Pavlou, Graham Walsh, Guido Geutjens, Ian Carluke, James Smith, John Marshall Rowles, Kalid Abdlslam, Khalid Baloch, Nicholas John London, Paul Alistair Gibb, Richard Goddard, Samuel Rajaratnam, Sanjeev Anand, Sanjeev Sharma, Shankar Thiagarajah, Simon Coleridge, Veysi Tuna Veysi, Andrew Toms, Hugh Ben Waterson, Abin Alvand, Adrian Taylor, Ben Kendrick, Paul Allen, Kevin Wembridge, Jamie Arbuthnot.
Ethical review statement
No formal ethical review process was required for this study.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
Follow M. Hampton @Hampton_ortho
© 2023 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Matthew Hampton, Email: matthew.hampton@nhs.net.
Vivek Balachandar, Email: vbsheffield1@gmail.com.
Charalambos P. Charalambous, Email: cpcharalambous@uclan.ac.uk.
Paul M. Sutton, Email: paul.sutton2@nhs.net.
References
- 1. Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018;104(1S):S41–S46. doi: 10.1016/j.otsr.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 2. Khatib Y, Badge H, Xuan W, Naylor JM, Harris IA. Patient satisfaction and perception of success after total knee arthroplasty are more strongly associated with patient factors and complications than surgical or anaesthetic factors. Knee Surg Sports Traumatol Arthrosc. 2020;28(10):3156–3163. doi: 10.1007/s00167-019-05804-9. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Shlomo Y, Blom A, Bolton C, et al. London, UK: The National Joint Registry 19th Annual Report 2022. [PubMed] [Google Scholar]
- 4. Emara AK, Ng M, Krebs VE, Bloomfield M, Molloy RM, Piuzzi NS. Femoral stem cementation in hip arthroplasty: The know-how of a “lost” art. Curr Rev Musculoskelet Med. 2021;14(1):47–59. doi: 10.1007/s12178-020-09681-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ballard WT, Callaghan JJ, Sullivan PM, Johnston RC. The results of improved cementing techniques for total hip arthroplasty in patients less than fifty years old. A ten-year follow-up study. J Bone Joint Surg Am. 1994;76-A(7):959–964. doi: 10.2106/00004623-199407000-00001. [DOI] [PubMed] [Google Scholar]
- 6. Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today--has anything changed after 10 years? J Arthroplasty. 2014;29(9):1774–1778. doi: 10.1016/j.arth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 7. Narkbunnam R, Chareancholvanich K. Causes of failure in total knee arthroplasty. J Med Assoc Thai. 2012;95(5):667–673. [PubMed] [Google Scholar]
- 8. Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97-A(9):715–720. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 9. Stone B, Nugent M, Young SW, Frampton C, Hooper GJ. The lifetime risk of revision following total knee arthroplasty: a New Zealand Joint Registry study. Bone Joint J. 2022;104-B(2):235–241. doi: 10.1302/0301-620X.104B2.BJJ-2021-0890.R1. [DOI] [PubMed] [Google Scholar]
- 10. Arsoy D, Pagnano MW, Lewallen DG, Hanssen AD, Sierra RJ. Aseptic tibial debonding as a cause of early failure in a modern total knee arthroplasty design. Clin Orthop Relat Res. 2013;471(1):94–101. doi: 10.1007/s11999-012-2467-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mulroy RD, Harris WH. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg Br. 1990;72-B(5):757–760. doi: 10.1302/0301-620X.72B5.2211749. [DOI] [PubMed] [Google Scholar]
- 12. Menken LG, Fleuriscar J, Weiner T, Berliner ZP, Rodriguez JA. Aseptic tibial implant loosening after total knee arthroplasty: Preventable? J Am Acad Orthop Surg. 2021;29(8):326–330. doi: 10.5435/JAAOS-D-20-00452. [DOI] [PubMed] [Google Scholar]
- 13.No authors listed Joint replacement (primary): hip, knee and shoulder. National Institute for Health and Care Excellence. Mar 29, 2022. [2 August 2023]. https://www.nice.org.uk/guidance/qs206 date last. accessed.
- 14.No authors listed GIRFT, BASK, and BOA Best Practice for Knee Arthroplasty Surgery Documentation. [2 August 2023]. https://www.boa.ac.uk/static/aea3c8b6-cb3f-48a0-bfb1f3c0ad1f5e29/girft-bask-boa-1pga4-summary-knee-july19b.pdf date last. accessed.
- 15. de Villiers MR, de Villiers PJT, Kent AP. The Delphi technique in health sciences education research. Med Teach. 2005;27(7):639–643. doi: 10.1080/13611260500069947. [DOI] [PubMed] [Google Scholar]
- 16. Parvizi J, Tan TL, Goswami K, et al. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J Arthroplasty. 2018;33(5):1309–1314. doi: 10.1016/j.arth.2018.02.078. [DOI] [PubMed] [Google Scholar]
- 17. van Otten TJM, van Loon CJM. Early aseptic loosening of the tibial component at the cement-implant interface in total knee arthroplasty: a narrative overview of potentially associated factors. Acta Orthop Belg. 2022;88(1):103–111. doi: 10.52628/88.1.13. [DOI] [PubMed] [Google Scholar]
- 18. Järvenpää J, Kettunen J, Miettinen H, Kröger H. The clinical outcome of revision knee replacement after unicompartmental knee arthroplasty versus primary total knee arthroplasty: 8-17 years follow-up study of 49 patients. Int Orthop. 2010;34(5):649–653. doi: 10.1007/s00264-009-0811-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Greidanus NV, Peterson RC, Masri BA, Garbuz DS. Quality of life outcomes in revision versus primary total knee arthroplasty. J Arthroplasty. 2011;26(4):615–620. doi: 10.1016/j.arth.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 20. Scheele C, Pietschmann MF, Schröder C, et al. Effect of lavage and brush preparation on cement penetration and primary stability in tibial unicompartmental total knee arthroplasty: An experimental cadaver study. Knee. 2017;24(2):402–408. doi: 10.1016/j.knee.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 21. Schlegel UJ, Püschel K, Morlock MM, Nagel K. An in vitro comparison of tibial tray cementation using gun pressurization or pulsed lavage. Int Orthop. 2014;38(5):967–971. doi: 10.1007/s00264-014-2303-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schlegel UJ, Siewe J, Delank KS, et al. Pulsed lavage improves fixation strength of cemented tibial components. Int Orthop. 2011;35(8):1165–1169. doi: 10.1007/s00264-010-1137-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahn JH, Jeong SH, Lee SH. The effect of multiple drilling on a sclerotic proximal tibia during total knee arthroplasty. Int Orthop. 2015;39(6):1077–1083. doi: 10.1007/s00264-014-2551-3. [DOI] [PubMed] [Google Scholar]
- 24. van de Groes SAW, de Waal Malefijt MC, Verdonschot N. Influence of preparation techniques to the strength of the bone-cement interface behind the flange in total knee arthroplasty. Knee. 2013;20(3):186–190. doi: 10.1016/j.knee.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 25. Norton MR, Eyres KS. Irrigation and suction technique to ensure reliable cement penetration for total knee arthroplasty. J Arthroplasty. 2000;15(4):468–474. doi: 10.1054/arth.2000.2965. [DOI] [PubMed] [Google Scholar]
- 26. Hofmann AA, Goldberg TD, Tanner AM, Cook TM. Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty. 2006;21(3):353–357. doi: 10.1016/j.arth.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 27. Stannage K, Shakespeare D, Bulsara M. Suction technique to improve cement penetration under the tibial component in total knee arthroplasty. Knee. 2003;10(1):67–73. doi: 10.1016/s0968-0160(02)00084-4. [DOI] [PubMed] [Google Scholar]
- 28. Ahmed I, Chawla A, Underwood M, et al. Infographic: Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery. Bone Joint J. 2021;103-B(5):828–829. doi: 10.1302/0301-620X.103B5.BJJ-2021-0545. [DOI] [PubMed] [Google Scholar]
- 29. Wyatt RWB, Chang RN, Royse KE, Paxton EW, Namba RS, Prentice HA. The association between cement viscosity and revision risk after primary total knee arthroplasty. J Arthroplasty. 2021;36(6):1987–1994. doi: 10.1016/j.arth.2021.01.052. [DOI] [PubMed] [Google Scholar]
- 30. Rodríguez-Collell JR, Mifsut D, Ruiz-Sauri A, Rodríguez-Pino L, González-Soler EM, Valverde-Navarro AA. Improving the cementation of the tibial component in knee arthroplasty: a study of four techniques in the cadaver. Bone Joint Res. 2021;10(8):467–473. doi: 10.1302/2046-3758.108.BJR-2020-0524.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kelly BC, Owen JR, Shah SC, Johnson AJ, Golladay GJ, Kates SL. A biomechanical comparison of the effect of baseplate design and bone marrow fat infiltration on tibial baseplate pullout strength. J Arthroplasty. 2021;36(1):356–361. doi: 10.1016/j.arth.2020.07.049. [DOI] [PubMed] [Google Scholar]
- 32. Cawley DT, Kelly N, McGarry JP, Shannon FJ. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J. 2013;95-B(3):295–300. doi: 10.1302/0301-620X.95B3.29586. [DOI] [PubMed] [Google Scholar]
- 33. Billi F, Kavanaugh A, Schmalzried H, Schmalzried TP. Techniques for improving the initial strength of the tibial tray-cement interface bond. Bone Joint J. 2019;101-B(1_Supple_A):53–58. doi: 10.1302/0301-620X.101B1.BJJ-2018-0500.R1. [DOI] [PubMed] [Google Scholar]
- 34. Lutz MJ, Pincus PF, Whitehouse SL, Halliday BR. The effect of cement gun and cement syringe use on the tibial cement mantle in total knee arthroplasty. J Arthroplasty. 2009;24(3):461–467. doi: 10.1016/j.arth.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 35. Schlegel UJ, Bishop NE, Püschel K, Morlock MM, Nagel K. Comparison of different cement application techniques for tibial component fixation in TKA. Int Orthop. 2015;39(1):47–54. doi: 10.1007/s00264-014-2468-x. [DOI] [PubMed] [Google Scholar]
- 36. Martin JR, Wronski PT, Schilkowsky RM, Orfanos AV, Fehring TK, Mason JB. Chitranjan S. Ranawat Award: Motion during total knee cementing significantly decreases tibial implant fixation strength. J Arthroplasty. 2022;37(6S):S12–S18. doi: 10.1016/j.arth.2022.02.091. [DOI] [PubMed] [Google Scholar]
- 37. Barrett D, Heale R. What are Delphi studies? Evid Based Nurs. 2020;23(3):68–69. doi: 10.1136/ebnurs-2020-103303. [DOI] [PubMed] [Google Scholar]


