Introduction
Textbook outcome is a multidimensional quality measurement, which comprises the desirable short-term outcomes after surgery. This composite measure is reached when a patient meets all predefined requirements, resulting in a broader reflection of quality of care than single outcome measures. This aids clinicians in daily practice, giving insight into the quality of the entire surgical pathway from surgery to postoperative outcomes. Textbook outcome also provides an opportunity to evaluate variation between hospitals in a more objective manner, as it provides higher event rates and more power to detect differences than single outcomes.
Textbook outcome has been evaluated in different surgical fields, and confirmed to be a feasible parameter for assessment of short-term outcomes1–8. A recent study provided a consensus-based definition specifically for colorectal liver metastases used for nationwide auditing in the Netherlands. Textbook outcome for colorectal liver metastases, as described by de Graaff et al.9, consists of five short-term postoperative outcome measures from surgery to 1 month after discharge. The aim of this study was to assess the association between textbook outcome and overall and disease-free survival in patients with colorectal liver metastases.
Methods
The study was approved by the local ethics authorities of Erasmus Medical Centre (MEC-2020-0294). All patients who underwent surgery for colorectal liver metastases at Erasmus MC Cancer Institute between 2009 and 2020 were identified from a retrospective database. Patients were excluded when resection margins or data on postoperative outcomes such as death or readmission were missing, when they underwent thermal ablation only, or when they underwent adjuvant hepatic arterial infusion pump chemotherapy in the context of the PUMP trial10.
The primary outcome of this study was the association between textbook outcome after colorectal liver metastasis surgery and long-term overall and disease-free survival. Secondary outcomes were the association between recurrence-free interval and textbook outcome, and predictors of textbook outcome. Full methods, including the statistical analysis plan, are available in the supplementary material.
Results
During the study interval, a total of 591 patients were eligible for inclusion. Of these, 495 (83.8 per cent) achieved a textbook outcome after resection of colorectal liver metastases. Patient characteristics are summarized in Table S1.
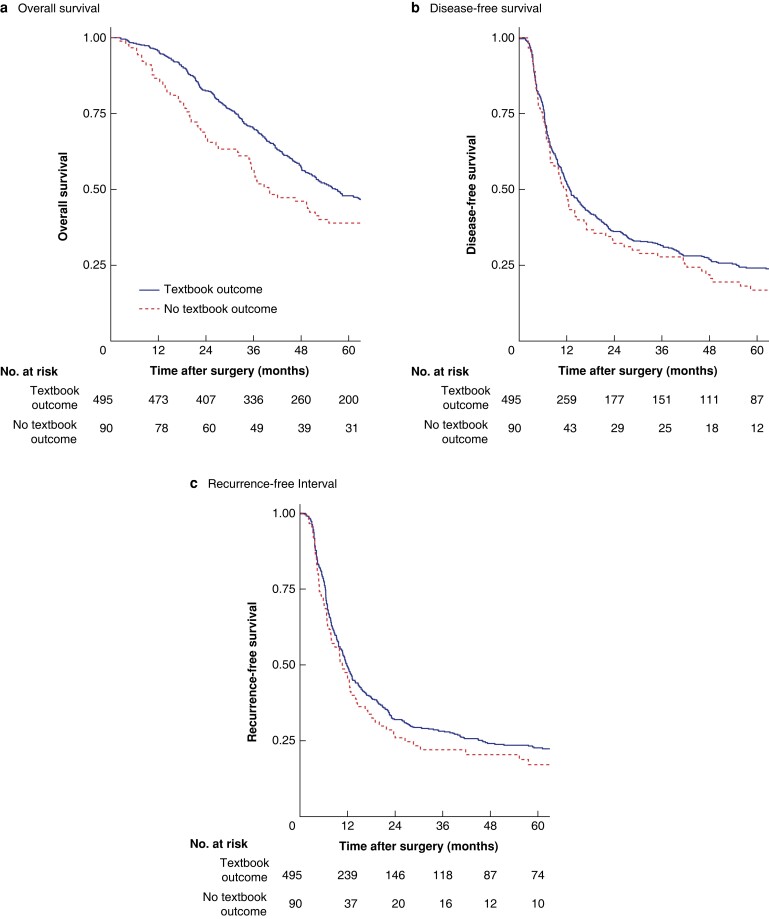
Median overall survival was 51 (i.q.r. 29–103) months for patients who a achieved textbook outcome compared with 39 (19–80) months for those who did not, resulting in a survival benefit of 12 months. Median follow-up for survivors was 91 (i.q.r. 67–111) months. Patients who achieved a textbook outcome had a superior 5-year overall survival rate of 43 (95 per cent c.i. 38 to 48) per cent, compared with 35 (26 to 48) per cent for those who did not (P = 0.013) (Fig. 1a). A textbook outcome was associated with improved overall survival in multivariable regression analysis (adjusted HR for death 0.71, 95 per cent c.i. 0.52 to 0.95; P = 0.021). Neither Charlson Co-morbidity Index score (adjusted HR 1.06, 0.77 to 1.47; P = 0.708) nor ASA grade above II (adjusted HR 1.40, 0.99 to 1.99; P = 0.059) was associated with impaired overall survival. The full results are shown in Table 1.
Fig. 1.
Survival and recurrence outcomes for patients with and without a textbook outcome
Kaplan–Meier survival curves showing a overall survival, b disease-free survival, and c recurrence-free interval for patients with and without a textbook outcome. aP = 0.013, bP = 0.280, and cP = 0.290 (log rank test).
Table 1.
Univariable and multivariable Cox regression analyses for overall survival
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| HR | P | HR | P | |
| Textbook outcome | 0.71 (0.55, 0.93) | 0.014 | 0.71 (0.52, 0.95) | 0.021 |
| Female sex | 0.87 (0.70, 1.08) | 0.207 | 0.90 (0.70, 1.15) | 0.403 |
| Age at CRLM resection (years) | 1.02 (1.01, 1.03) | 0.002 | 1.02 (1.01, 1.04) | < 0.001 |
| Charlson Co-morbidity Index score ≥2 | 1.05 (0.78, 1.40) | 0.764 | 1.06 (0.77, 1.47) | 0.708 |
| ASA fitness grade > II | 1.48 (1.08, 2.01) | 0.013 | 1.40 (0.99, 1.99) | 0.059 |
| Primary tumour location | ||||
| Right side | 1.00 (reference) | |||
| Left side | 0.69 (0.52, 0.90) | 0.007 | 0.74 (0.55, 0.99) | 0.044 |
| Rectum | 0.72 (0.54, 0.95) | 0.021 | 0.72 (0.53, 0.98) | 0.034 |
| Nodal involvement (N+) | 1.62 (1.30, 2.01) | < 0.001 | 1.56 (1.23, 1.98) | < 0.001 |
| DFI < 1 year | 1.41 (1.10, 1.80) | 0.006 | 1.36 (1.01, 1.82) | 0.042 |
| CEA (µg/L) | 1.00 (1.00, 1.00) | 0.554 | 1.00 (1.00, 1.00) | 0.511 |
| > 1 CRLM treated | 1.33 (1.07, 1.66) | 0.010 | 1.31 (1.00, 1.71) | 0.050 |
| CRLM size > 5 cm | 1.26 (0.97, 1.65) | 0.086 | 1.26 (0.91, 1.74) | 0.157 |
| Neoadjuvant chemotherapy | 1.20 (0.98, 1.47) | 0.081 | 1.08 (0.82, 1.41) | 0.585 |
| Extrahepatic disease | 1.31 (0.97, 1.77) | 0.081 | 1.45 (1.04, 2.03) | 0.029 |
Values in parentheses are 95% confidence intervals. CRLM, colorectal liver metastasis; DFI, disease-free interval; CEA, carcinoembryonic antigen.
No differences were found in disease-free survival at 5 years between patients who achieved a textbook outcome and those who did not (21 (18 to 25) versus 15 (9 to 25) per cent; P = 0.280) (Fig. 1b). Full results, including exploratory analyses, are available in the supplementary material.
Discussion
Textbook outcome is a composite quality measure that has the potential to aid clinicians in daily practice by giving insight into the perioperative pathway. Textbook outcome was independent of preoperative status of the patient, demonstrated by indices such as ASA grade and Charlson Co-morbidity Index scores. Achieving a textbook outcome was associated with better overall survival. This illustrates the association between improved short-term outcomes and long-term survival and the importance of reducing postoperative complications.
Recently, Neary et al.11 investigated the association between textbook outcome after surgery for colorectal liver metastases and long-term overall survival, using an alternative definition of textbook outcome. In the present study, achieving a textbook outcome was associated with improved long-term overall survival after resection of colorectal liver metastases. The survival benefit at 12 months highlights the importance of the perioperative phase. Pursuing a textbook outcome during this interval has the potential to ultimately lead to improved survival rates. Improvement of individual parameters and, therefore, textbook outcome will further enhance the quality of care in surgery for colorectal liver metastases.
In the present study, the textbook outcome rate was 84 per cent (495 of 591) in colorectal liver metastasis surgery, similar to that in the nationwide Dutch Hepato Biliary Audit study, which also used data from this centre. The textbook outcome definition used here was established in the DHBA through expert opinion and previously published definitions9. As textbook outcome is primarily meant for clinical auditing of short-term results, the parameters used in its definition should be readily available, preferably from standard reporting in electronic patient files. An international expert Delphi consensus on defining textbook outcome has been published recently12. In addition to the five parameters, Görgec et al.13 included intraoperative incidents of grade 2 or higher (Oslo classification), postoperative reinterventions, and postoperative bile leakage to their definition of textbook outcome, resulting in a lower rate of textbook outcome achievement of 67.4 per cent. The additional variables in this version of the definition are not registered consistently in routine practice, and the present authors were unable to retrieve these from electronic patient files. The measurements of Delphi consensus of textbook outcome in most patients led to a higher Clavien–Dindo grade and a prolonged hospital stay, both of which are included in the DHBA definition of textbook outcome. The Delphi consensus is an expert-driven consensus, in contrast to the data-driven definition of the DHBA9.
Achieving a textbook outcome in surgery for colorectal liver metastases was shown not to improve disease-free survival or recurrence-free interval. Including tumour-specific parameters in textbook outcome could potentially lead to a more significant difference in disease-free survival and, therefore, in finding associations between textbook outcome and disease recurrence. Adequate resection margins are the obvious tumour-specific parameters in liver surgery for colorectal liver metastases, and indeed the authors’ exploratory analyses using R0 versus R1/2 instead of R0/1 versus R2 as cut-off revealed an association between textbook outcome and disease-free survival. There is ongoing debate on intentional R1 resections (vascular R1 versus parenchymal R1, R1 after induction chemotherapy)14–16. Tumour-free resection margins are, if attainable, always the most favourable outcome of every resection. However, R1 resections may be performed intentionally when important anatomical structures are at risk, or could result from a chosen resection technique. Inability to achieve an R0 resection when R1 is deemed possible should not be a contraindication to resection but, in fact, is part of a modern, multidisciplinary approach to colorectal liver metastases.
The multivariable logistic regression analysis in this study revealed no predictors for achieving textbook outcome. In particular, there was no association between poor preoperative status (ASA grade and Charlson Co-morbidity Index score) and not achieving textbook outcome. This highlights the importance of the perioperative care pathway as achievement of textbook outcome in this study was not related to patient factors but depended on the perioperative factors associated with the care delivered.
Limitations of this study are related to its retrospective nature and setting in a tertiary referral centre. It may be possible that readmissions within 30 days after discharge were not registered adequately and/or communicated when patients were readmitted to the referring centres. The retrospective database did not distinguish between R1 and R2 resections, thereby reducing the potential for identifying differences in disease recurrence. Another limitation of this study was the lack of data on somatic mutations such as those in RAS, TP53, and BRAF.
Supplementary Material
Contributor Information
Kelly R Voigt, Department of Surgical Oncology and Gastrointestinal Surgery, Erasmus MC Cancer Institute, Rotterdam, the Netherlands.
Lissa Wullaert, Department of Surgical Oncology and Gastrointestinal Surgery, Erasmus MC Cancer Institute, Rotterdam, the Netherlands.
Michelle R de Graaff, Department of Surgery, University Medical Centre Groningen, Groningen, the Netherlands.
Cornelis Verhoef, Department of Surgical Oncology and Gastrointestinal Surgery, Erasmus MC Cancer Institute, Rotterdam, the Netherlands.
Dirk J Grünhagen, Department of Surgical Oncology and Gastrointestinal Surgery, Erasmus MC Cancer Institute, Rotterdam, the Netherlands.
Funding
The authors have no funding to declare.
Author contributions
Kelly Voigt (Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing—original draft), Lissa Wullaert (Conceptualization, Formal analysis, Investigation, Methodology, Visualization, Writing—original draft), Michelle de Graaff (Conceptualization, Formal analysis, Methodology, Validation, Visualization, Writing—review & editing), Kees Verhoef (Conceptualization, Formal analysis, Investigation, Supervision, Validation, Visualization, Writing—review & editing), and Dirk Grünhagen (Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing—review & editing).
Disclosure
The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS online.
Data availability
Data will be made available upon reasonable request.
References
- 1. Busweiler LA, Schouwenburg MG, van Berge Henegouwen MI, Kolfschoten NE, de Jong PC, Rozema Tet al. Textbook outcome as a composite measure in oesophagogastric cancer surgery. Br J Surg 2017;104:742–750 [DOI] [PubMed] [Google Scholar]
- 2. Karthaus EG, Lijftogt N, Busweiler LAD, Elsman BHP, Wouters MWJM, Vahl ACet al. Textbook outcome: a composite measure for quality of elective aneurysm surgery. Ann Surg 2017;266:898–904 [DOI] [PubMed] [Google Scholar]
- 3. Kolfschoten NE, Kievit J, Gooiker GA, van Leersum NJ, Snijders HS, Eddes EHet al. Focusing on desired outcomes of care after colon cancer resections; hospital variations in ‘textbook outcome’. Eur J Surg Oncol 2013;39:156–163 [DOI] [PubMed] [Google Scholar]
- 4. Poelemeijer YQM, Marang-van de Mheen PJ, Wouters M, Nienhuijs SW, Liem RSL. Textbook outcome: an ordered composite measure for quality of bariatric surgery. Obes Surg 2019;29:1287–1294 [DOI] [PubMed] [Google Scholar]
- 5. Salet N, Bremmer RH, Verhagen MAMT, Ekkelenkamp VE, Hansen BE, de Jonge PJFet al. Is textbook outcome a valuable composite measure for short-term outcomes of gastrointestinal treatments in the Netherlands using hospital information system data? A retrospective cohort study. BMJ Open 2018;8:e019405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van der Heide MFJ, de Jel DVC, Hoeijmakers F, Hoebers FJP, de Boer JP, Hamming-Vrieze Oet al. Defining high-quality integrated head and neck cancer care through a composite outcome measure: textbook outcome. Laryngoscope 2022;132:78–87 [DOI] [PubMed] [Google Scholar]
- 7. van der Kaaij RT, de Rooij MV, van Coevorden F, Voncken FEM, Snaebjornsson P, Boot Het al. Using textbook outcome as a measure of quality of care in oesophagogastric cancer surgery. Br J Surg 2018;105:561–569 [DOI] [PubMed] [Google Scholar]
- 8. van Roessel S, Mackay TM, van Dieren S, van der Schelling GP, Nieuwenhuijs VB, Bosscha Ket al. Textbook outcome: nationwide analysis of a novel quality measure in pancreatic surgery. Ann Surg 2020;271:155–162 [DOI] [PubMed] [Google Scholar]
- 9. de Graaff MR, Elfrink AKE, Buis CI, Swijnenburg RJ, Erdmann JI, Kazemier Get al. Defining textbook outcome in liver surgery and assessment of hospital variation: a nationwide population-based study. Eur J Surg Oncol 2022;48:2414–2423 [DOI] [PubMed] [Google Scholar]
- 10. Buisman FE, Homs MYV, Grünhagen DJ, Filipe WF, Bennink RJ, Besselink MGHet al. Adjuvant hepatic arterial infusion pump chemotherapy and resection versus resection alone in patients with low-risk resectable colorectal liver metastases—the multicenter randomized controlled PUMP trial. BMC Cancer 2019;19:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Neary C, O’Brien L, McCormack E, Kelly M, Bolger J, McEntee Get al. Defining a textbook outcome for the resection of colorectal liver metastases. J Surg Oncol 2023;127:616–624 [DOI] [PubMed] [Google Scholar]
- 12. Görgec B, Cacciaguerra AB, Pawlik TM, Aldrighetti LA, Alseidi AA, Cillo Uet al. An international expert Delphi consensus on defining textbook outcome in liver surgery (TOLS). Ann Surg 2022;277:821–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Görgec B, Benedetti Cacciaguerra A, Lanari J, Russolillo N, Cipriani F, Aghayan Det al. Assessment of textbook outcome in laparoscopic and open liver surgery. JAMA Surg 2021;156:e212064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Viganò L, Rubbia-Brandt L, De Rosa G, Majno P, Langella S, Toso Cet al. Nodular regenerative hyperplasia in patients undergoing liver resection for colorectal metastases after chemotherapy: risk factors, preoperative assessment and clinical impact. Ann Surg Oncol 2015;22:4149–4157 [DOI] [PubMed] [Google Scholar]
- 15. Viganò L, Costa G, Cimino MM, Procopio F, Donadon M, Del Fabbro Det al. R1 resection for colorectal liver metastases: a survey questioning surgeons about its incidence, clinical impact, and management. J Gastrointest Surg 2018;22:1752–1763 [DOI] [PubMed] [Google Scholar]
- 16. Ayez N, Lalmahomed ZS, Eggermont AM, Ijzermans JN, de Jonge J, van Montfort Ket al. Outcome of microscopic incomplete resection (R1) of colorectal liver metastases in the era of neoadjuvant chemotherapy. Ann Surg Oncol 2012;19:1618–1627 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available upon reasonable request.