Abstract
Objective
To examine indirect spillover effects of Affordable Care Act (ACA) Medicaid expansions to working‐age adults on health care coverage, spending, and utilization by older low‐income Medicare beneficiaries.
Data Sources
2010–2018 Health and Retirement Study survey data linked to annual Medicare beneficiary summary files.
Study Design
We estimated individual‐level difference‐in‐differences models of total spending for inpatient, institutional outpatient, physician/professional provider services; inpatient stays, outpatient visits, physician visits; and Medicaid and Part A and B Medicare coverage. We compared changes in outcomes before and after Medicaid expansion in expansion versus nonexpansion states.
Data Collection/Extraction Methods
The sample included low‐income respondents aged 69 and older with linked Medicare data, enrolled in full‐year traditional Medicare, and residing in the community.
Principal Findings
ACA Medicaid expansion was associated with a 9.8 percentage point increase in Medicaid coverage (95% CI: 0.020–0.176), a 4.4 percentage point increase in having any institutional outpatient spending (95% CI: 0.005–0.083), and a positive but statistically insignificant 2.4 percentage point change in Part B enrollment (95% CI: −0.003 to 0.050, p = 0.079).
Conclusions
ACA Medicaid expansion was associated with more institutional outpatient spending among older low‐income Medicare beneficiaries. Increased care costs should be weighed against potential benefits from increased realized access to care.
Keywords: access/demand/utilization of services, aging/elderly/geriatrics, health policy/politics/law/regulation, Medicaid, Medicare
What is known on this topic
Medicaid expansion to working‐age adults under the Affordable Care Act (ACA) had spillover effects on low‐income older traditional Medicare beneficiaries, who became more likely to participate in Medicaid.
While Medicaid expansion could also increase health care use by older low‐income adults, prior work examined self‐reported measures of utilization or used area‐level measures of eligibility.
What this study adds
Using individual‐level eligibility measures linked to administrative data on coverage and spending, this study finds Medicaid expansion was associated with increased total outpatient spending in Medicare and Part B enrollment.
Increases in institutional outpatient care use and spending occur among persons never eligible for ACA Medicaid expansion and are consistent with indirect spillover effects of increased insurance coverage.
1. INTRODUCTION
Medicaid expansion under the Affordable Care Act (ACA) and prior reforms directly impacted low‐income adults aged 19–64, but also had spillover effects to other groups. 1 , 2 , 3 , 4 One group not directly targeted by the policy change is older low‐income adults; following ACA Medicaid expansion, those living in expansion states were more likely to have supplemental Medicaid coverage in addition to Medicare. 5 , 6 Coverage gains among older low‐income adults can have important impacts since, historically, their Medicaid take‐up has been low. 7 , 8
ACA Medicaid expansions to working‐age adults may increase Medicaid coverage among older low‐income adults for several reasons. Medicaid expansion may be a “welcome mat” for previously‐eligible groups, by increasing program awareness or enrollment assistance from states, providers, and others, or reducing stigma associated with participation. In addition, ACA Medicaid may be an “on‐ramp” to dual eligibility by raising Medicaid coverage among the near elderly. 5 , 9 , 10 , 11 For example, 64‐year‐olds in 2014 may benefit from Medicaid coverage as a direct result of the ACA expansion and remain enrolled upon aging into Medicare at age 65 in 2015.
These different pathways to Medicaid eligibility may have different effects on health care use and spending among duals, an issue of significant interest to policy makers. 12 Under standard welcome mat mechanisms, duals' health care use and spending could increase, since Medicaid lowers out‐of‐pocket costs by covering Medicare Part A and B cost‐sharing and some services that Medicare does not. 13 Alternatively, if expansion increases coverage through on‐ramp effects, duals may age into Medicare with reduced health care demand because near‐elderly Medicaid coverage helped address chronic conditions and reduce pent‐up demand. 14 , 15 , 16 , 17 , 18 The latter effect can be thought of as a direct, but delayed, effect of Medicaid expansion on the targeted group, as opposed to an indirect spillover effect to another population. Prior studies of the effects of ACA Medicaid expansion on health care use by low‐income older adults found differing effects. Two studies report that the ACA Medicaid expansion had no effects on primary care or long‐term care use by Medicare beneficiaries, while another found that Medicaid expansion increased self‐reported use of office visits by older low‐income older adults in poor health. 6 , 19 , 20 These studies included adults aged 65–68 who were exposed to both standard welcome mat effects and on‐ramp effects.
In this study, we isolate ACA Medicaid expansion's indirect spillover effects on health care coverage (i.e., Medicaid, Medicare Parts A and B), use, and spending while on Medicare by studying Medicare beneficiaries whose age made them ineligible for any direct benefits from ACA Medicaid expansion. In addition, because we use data from Health and Retirement Study (HRS) surveys linked to Medicare administrative data, our study makes three additional contributions to the ACA Medicaid spillovers literature. First, we use administrative measures of Medicaid coverage and health care spending and utilization, unlike prior analyses that rely on self‐reports. 6 Second, we use respondent‐level information on income, as opposed to ZIP code level income, to identify beneficiaries likely to be affected by spillover effects of Medicaid expansion. 10 , 11 , 19 Finally, we provide new evidence on the association between ACA Medicaid expansion and Medicare Part A and B enrollment, which may serve as mechanisms for increased spending.
2. MATERIALS AND METHODS
We used data from the HRS, a nationally representative survey of approximately 20,000 adults aged 50 and older, which collects information about income, assets, health insurance, and other respondent characteristics every 2 years. We used the RAND HRS longitudinal file 2018 (V1) linked to restricted‐use HRS data. 21 We used Medicare administrative files (for respondents who gave HRS consent to access Medicare data) to define coverage, spending, and utilization. We linked annual Medicare beneficiary summary files from 2010 to 2018 to survey waves 10–14. Since the survey data apply to even years and the Medicare data are annual, we applied respondent traits other than age from the survey to the preceding odd‐numbered year of Medicare data; we measured age from the annual beneficiary summary files.
Our main sample included HRS respondents aged 69 and older in our study period. Because the earliest ACA Medicaid expansions occurred in 2014, this ensures that persons aged 64 or less in that year (who may have experienced direct benefits from expansion Medicaid) were excluded from our analysis, allowing us to focus on indirect spillovers only. Since we used Medicare administrative data, our analysis was limited to respondents with linked Medicare data enrolled in traditional Medicare for the full year (because we required fee‐for‐service claims to measure annual spending/utilization), thus excluding decedents. We focused on respondents with Medicaid‐countable income at or below 135% of the federal poverty level (FPL), which includes persons eligible for full Medicaid through the aged, blind, disabled pathway, as well as those eligible for partial Medicaid through three Medicare Savings Programs using standard income thresholds. We defined Medicaid‐countable income following Medicaid's income counting rules, which include separate disregards for earned and unearned income. We excluded a small number of respondents residing in nursing homes who may qualify through other Medicaid eligibility pathways, and thus focus on community‐dwelling Medicare beneficiaries. Finally, we excluded respondents living in states that expanded Medicaid under the ACA in 2015 and 2016, due to concerns about staggered treatment implementation and the limited number of HRS respondents in those states. 22
Primary outcomes were constructed from annual Medicare beneficiary summary files and included Medicaid participation (any Medicaid participation and number of months enrolled in Medicaid that year) and full‐year enrollment in Medicare Parts A and B. We constructed measures of spending and utilization for three types of health care defined from Medicare claims: (1) inpatient spending and stays; (2) institutional outpatient spending and visits; and (3) physician/professional provider spending and physician office visits. 23 Inpatient care is covered under Part A Medicare while the other two categories are covered under Part B. Institutional outpatient care is measured by claims from hospital outpatient departments, rural health clinics, federally qualified health centers, among others. Total spending on these three service types is more than 70% of all spending for low‐income persons in the beneficiary summary files. Spending was defined as the sum of Medicare reimbursements, beneficiary payment obligations (including Medicaid contributions to cost‐sharing), and reimbursements by a payer other than Medicare (e.g., employer coverage, VA coverage, workers compensation, but not including Medicaid), and expressed in constant dollars adjusted by the annual medical consumer price index. For each service type, we examined indicators of whether the respondent had any spending (or utilization) of that service type and continuous measures of the log of spending (or visits) conditional on having any spending (or visits).
The main independent variable was an indicator for whether the respondent lived in an expansion state after it expanded Medicaid under the ACA. 24 Covariates included indicators for single year of respondent age, sex, and, to account for well‐known disparities in access and health care use tied to socioeconomic traits and structural factors such as systemic racism, we controlled for education (less than high school, high school degree/GED, some college, and college degree or more), self‐reported race (White, Black/African American, and other race, as coded by the RAND file), and self‐reported Hispanic ethnicity. 25 The other race category included people who identified as American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, or other races. We included state indicators to account for unobserved time‐invariant differences across states and year indicators to control for temporal shocks common to all states.
We estimated difference‐in‐differences (DD) models following this specification:
| (1) |
EXPANSION indicates that individual i lived in one of the 27 states (including DC) that expanded Medicaid in 2014, POST indicates 2014 or later. β is the DD estimate of the association of the ACA Medicaid expansion and the outcome of interest, Y ist; γ s , and τ t represent state and year fixed effects, respectively. We used survey weights in all analyses, and we clustered regression standard errors at the state level.
To support our identifying assumption, we tested that pre‐period trends in outcomes were parallel in the two groups of states using an event study specification. To rule out changes in the sample driven by ACA expansion, we modeled indicators of the availability of Medicare claims, community residence, full‐year Medicare enrollment, and full‐year traditional Medicare enrollment. We also modeled spending measures specific to Medicare reimbursements only. We estimated DD models of primary outcomes for all respondents aged 65 and up to show how results change when delayed direct effects are included, and for respondents who met their state's eligibility criteria for the Qualified Medicare Beneficiary (QMB) program that covers all Medicare cost‐sharing. We tested the robustness of our main results by including potentially endogenous covariates (marital status, income, employment, the number of chronic conditions, and the number of activity of daily living [ADL] limitations), and by excluding respondents with spouses residing in nursing facilities (because that may affect own eligibility), and living in states that either provided Medicaid to childless low‐income adults in 2010–2013 26 , 27 or enacted early, albeit modest, Medicaid expansions under the ACA. 28
Analysis of restricted data was approved by the HRS at the University of Michigan and the CMS Privacy Board. This study was approved by the Protection of Human Subjects Committee at William & Mary under protocol #PHSC‐2022‐07‐25‐15748.
3. RESULTS
Table 1 reports results from Equation (1). Table A1 reports summary statistics for the analytical sample and differences by expansion status for reference. Relative to those living in nonexpansion states, older low‐income adults in expansion states were 9.8 percentage points (or 23%) more likely to have any Medicaid coverage (p = 0.015) after the ACA Medicaid expansions and 2.4 percentage points more likely to be enrolled in Part B for a full year, although the latter association was not statistically significant (p = 0.079). Relative to those in nonexpansion states, older low‐income adults in expansion states were 4.4–4.6 percentage points (about 6%) more likely to have any institutional outpatient spending or visits after the ACA Medicaid expansion (p = 0.026, p = 0.020). Medicaid expansion was not associated with statistically significant changes in the amount of institutional outpatient spending or use conditional on having any spending or use, or with physician/professional provider spending or the number of physician office visits.
TABLE 1.
Changes in coverage, spending, and utilization, associated with Medicaid expansion, 2010–2018, adults aged 69+, income ≤135% of the federal poverty line, 2010–2018 Health and Retirement Study.
| Dependent variable | DD estimate (standard error) | Pre‐period mean (mean of level shown for log‐transformed variables) | n |
|---|---|---|---|
| Has Medicaid coverage (any month) | 0.098** (0.039) | 0.427 | 7567 |
| Number of months of Medicaid coverage | 1.209** (0.471) | 4.931 | 7567 |
| Part A enrollment | 0.004 (0.005) | 0.983 | 7567 |
| Part B enrollment | 0.024* (0.013) | 0.970 | 7567 |
| Any inpatient spending | −0.002 (0.024) | 0.223 | 7567 |
| log (real inpatient spending), if any | 0.109 (0.112) | 20,036 | 1610 |
| Any inpatient stays | −0.002 (0.026) | 0.225 | 7567 |
| log (inpatient stays), if any | 0.135* (0.067) | 1.66 | 1633 |
| Any institutional outpatient spending | 0.044** (0.019) | 0.750 | 7567 |
| log (real institutional outpatient spending), if any | 0.136 (0.098) | 3038 | 5624 |
| Any institutional outpatient visits | 0.046** (0.019) | 0.752 | 7567 |
| log (institutional outpatient visits), if any | 0.011 (0.068) | 6.46 | 5633 |
| Any physician/professional provider spending | 0.023 (0.019) | 0.925 | 7567 |
| log (physician/professional provider spending), if any | −0.002 (0.054) | 4156 | 7021 |
| Any physician office visits | 0.001 (0.024) | 0.876 | 7567 |
| log (physician office visits), if any | −0.049 (0.054) | 9.88 | 6629 |
Note: The difference‐in‐differences (DD) estimate column presents the coefficient estimates for EXPANSION × POST from Equation (1) in the text. Each row reports a DD estimate from a separate regression estimated for 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. All regressions are weighted and include controls for single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black/African American, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. The DD estimates presented reflect absolute, not relative, effects. Standard errors are clustered by state.
p < 0.05;
p < 0.1.
We tested the identifying assumptions of the DD models by estimating event study models of inpatient and institutional outpatient spending/use and enrollment in Medicaid and Part B. Figures 1 and 2 show that the parallel trends assumption was supported for these spending and utilization outcomes. For inpatient stays (conditional on any), the event study results indicate significant increases in some, but not all, post‐period years relative to baseline. For institutional outpatient spending/use on the extensive margin, increases were observed in the first two years of ACA Medicaid expansion but were not statistically significant at the 5% level (Figure 2A,C; p < 0.10). Figures A1 and A2 present event study results for Medicaid and Part B enrollment.
FIGURE 1.
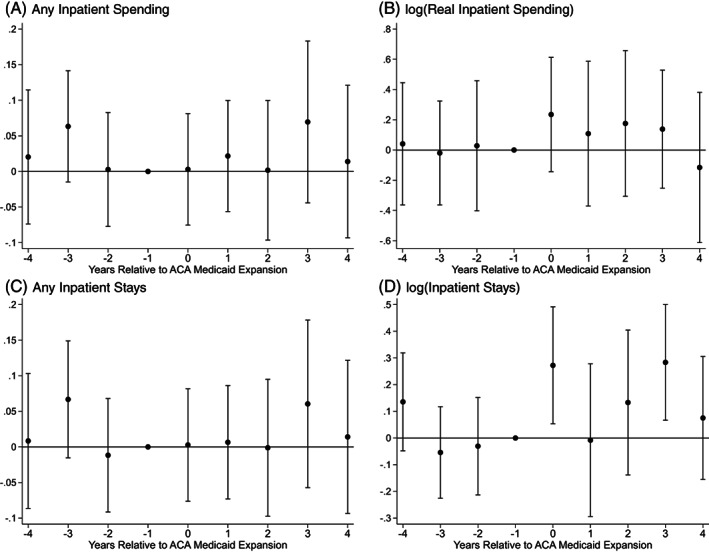
Event study estimates of relative changes over time in inpatient spending and utilization associated with Medicaid expansion, 2010–2018. Estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. Weighted coefficients and 95‐percent confidence intervals shown for EXPANSION × 4 YEARS PRE EXPANSION; EXPANSION × 3 YEARS PRE EXPANSION; EXPANSION × 2 YEARS PRE EXPANSION; EXPANSION × YEAR OF EXPANSION; EXPANSION × 1 YEAR POST EXPANSION; EXPANSION × 2 YEARS POST EXPANSION; EXPANSION × 3 YEARS POST EXPANSION; EXPANSION × 4 YEARS POST EXPANSION. The omitted category is EXPANSION × 1 YEAR PRE EXPANSION. Controls include single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black/African American, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. DV, dependent variable. The p‐values of F‐tests of the joint significance of pre‐trend coefficient estimates are as follows for Figures 1 (A) 0.31; (B) 0.98; (C) 0.18; (D) 0.32.
FIGURE 2.
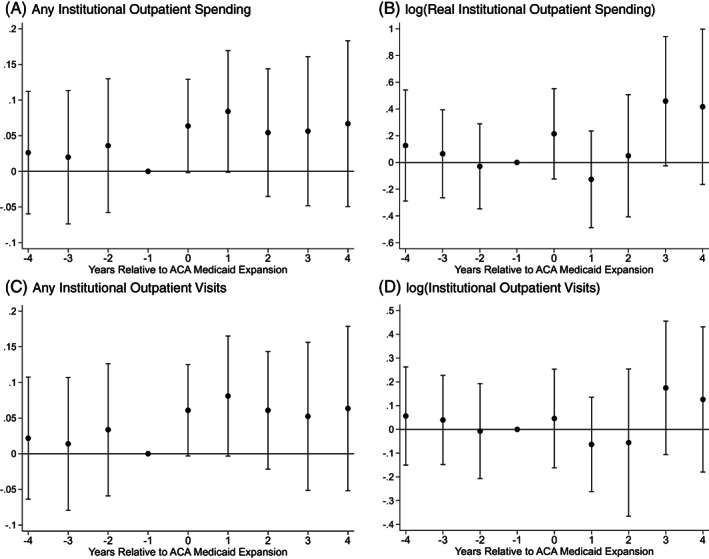
Event study estimates of relative changes over time in outpatient spending and utilization associated with Medicaid expansion, 2010–2018. Estimated on 2010–2018 Health and Retirement Survey respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. Weighted coefficients and 95‐percent confidence intervals shown for EXPANSION × 4 YEARS PRE EXPANSION; EXPANSION × 3 YEARS PRE EXPANSION; EXPANSION × 2 YEARS PRE EXPANSION; EXPANSION × YEAR OF EXPANSION; EXPANSION × 1 YEAR POST EXPANSION; EXPANSION × 2 YEARS POST EXPANSION; EXPANSION × 3 YEARS POST EXPANSION; EXPANSION × 4 YEARS POST EXPANSION. The omitted category is EXPANSION × 1 YEAR PRE EXPANSION. Controls include single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black/African American, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. DV, dependent variable. The p‐values of F‐tests of the joint significance of pre‐trend coefficient estimates are as follows for Figure 2 (A) 0.85; (B) 0.81; (C) 0.85; (D) 0.87.
Table A2 reports results from DD models of indicators for selection into the sample. Relative to nonexpansion state residents Medicaid expansion was not associated with a differential likelihood of having Medicare claims data, residing in the community, or having full‐year Medicare or traditional Medicare. Further, Table A2 shows that the finding for our primary measure of total outpatient institutional spending on the extensive margin is also observed for a binary measure of Medicare reimbursement alone.
Tables A3, A4 report results from sensitivity analyses that tested whether Table 1 results were robust to using different sample restrictions or including additional covariates. Most signs and magnitudes of the estimated associations between Medicaid expansion and study outcomes were similar to our main results. When we include 65–68‐year‐olds who may experience delayed direct effects (Table A3), estimated effects on the likelihood of having any institutional outpatient spending or utilization are slightly smaller and estimated less precisely (p < 0.10).
4. DISCUSSION
This study found that Medicaid expansion was associated with increases in outpatient care for older low‐income Medicare beneficiaries. Because we focused on adults too old to be directly impacted by the ACA Medicaid expansion to persons under age 65, these increases in utilization and spending are consistent with the spillover effects of new or more generous coverage, as opposed to delayed, direct effects of Medicaid expansion. We provide the first evidence that another indirect benefit of the Medicaid expansion to working‐age adults was increased Medicare Part B enrollment, reflecting new coverage for outpatient and physician care. We confirm prior work finding an increase in dual Medicare–Medicaid enrollment, which effectively increases insurance generosity. For Part B, Medicare enrollees face premiums ($134/month in 2018) and cost‐sharing (in 2018, a $183 annual deductible followed by 20% coinsurance). For most dual enrollees, Medicaid covers those financial obligations.
Our findings add to those reported in prior studies. Similar to Carey et al. 19 we did not observe changes in primary care as measured by physician office visits. In contrast, we also studied institutional outpatient care, and found that it increased for respondents in expansion states relative to those in nonexpansion states. We build on McInerney et al. 6 by providing evidence consistent with the hypothesis that indirect spillover effects on outpatient care are larger than direct, but delayed, effects and by using administrative measures of utilization and not self‐reports. Our results confirm their findings that ACA Medicaid expansion increased outpatient care for older adults responding to the National Health Interview Survey.
Our study has some limitations. Our analysis is limited to traditional Medicare beneficiaries. Although we used rich data on respondent socioeconomic characteristics and Medicare use, the number of low‐income older adults we studied was relatively small, which limits our power to detect significant effects. While we used annual measures from Medicare beneficiary summary files, measures of most respondent traits, including income, were available from surveys collected every 2 years; thus, available measures of income do not align with claims‐based measures for the years between surveys. Nonetheless, the paired survey and claims data offer an advantage over other studies that use area‐level income to identify eligible persons.
Spillover effects are important to document given the costs of Medicare and benefits to low‐income Medicare beneficiaries. Increased use of outpatient services covered by Part B will have fiscal implications for the federal budget, and household finances may also be impacted if Part B premiums rise in response. Our analysis did not examine whether ACA Medicaid expansions improved health status by increasing realized access to care, but such potential benefits must be weighed against Medicare costs. Event study models showed that Medicaid expansion was associated with immediate increases in some types of Part B spending on the extensive margin; however, estimated changes in use/spending 2–4 years after expansion are imprecise, which makes longer term implications for federal spending unclear. Future research using larger samples of Part B claims and focusing on the potential benefits to low‐income older adults is warranted.
ACKNOWLEDGMENTS
This research was supported by a grant from the Agency for Healthcare Research and Quality. The views in this paper are solely those of the authors. This study uses data from the Health and Retirement Study, which is sponsored by the National Institute on Aging (grant number NIA U01AG009740 and is conducted by the University of Michigan.
APPENDIX A.
TABLE A1.
Means of demographic characteristics, coverage, spending and utilization, adults aged 69+, and income ≤135% of the federal poverty level: 2010–2018 health and retirement study.
| Variable | 2010–2018, n = 7567 summary statistic | 2010–2013, n = 4190 | ||
|---|---|---|---|---|
| Summary statistic | Difference between expansion and non‐expansion states (95% CI) | p‐value | ||
| Age, mean | 79.67 | 79.76 | 0.719 (0.18–1.26) | <0.01 |
| Less than high school, % | 41.90 | 44.2 | −14.1 (−17.5 to −10.7) | <0.001 |
| High school degree, % | 35.7 | 34.9 | 5.0 (1.7–8.3) | <0.01 |
| Some college, % | 15.0 | 13.8 | 6.7 (4.3–9.1) | <0.001 |
| College or more, % | 7.4 | 7.1 | 2.4 (0.5–4.2) | 0.013 |
| Female, % | 71.0 | 71.9 | 1.1 (−4.3 to 2.0) | 0.48 |
| Male, % | 29.0 | 28.1 | 1.1 (−2.0 to 4.3) | 0.48 |
| White, % | 75.0 | 75.8 | 7.7 (5.0–10.5) | <0.001 |
| Black, % | 16.2 | 16.6 | −6.5 (−8.8 to −4.2) | <0.001 |
| Other race, % | 8.8 | 7.6 | −1.3 (−3.1 to 0.6) | 0.19 |
| Hispanic, % | 16.8 | 16.8 | −6.5 (−9.0 to −4.0) | <0.001 |
| Non‐Hispanic, % | 83.2 | 83.2 | 6.5 (4.0–9.0) | <0.001 |
| Has Medicaid coverage, % | 42.6 | 42.7 | −8.1 (−11.5 to −4.7) | <0.001 |
| Number of months Medicaid coverage, mean | 4.90 | 4.93 | −0.95 (−1.4 to −0.5) | <0.001 |
| Part A enrollment, % | 98.3 | 98.3 | −1.8 (−2.6 to −1.0) | <.0001 |
| Part B enrollment, % | 96.4 | 97.0 | −0.7 (−2.0 to 0.7) | 0.33 |
| Any inpatient spending, % | 21.3 | 22.3 | −0.6 (−3.5 to 2.3) | 0.68 |
| Inpatient spending if any, mean | 19,672 | 20,036 | 2499 (−989–5988) | 0.16 |
| Any inpatient stays, % | 21.5 | 22.5 | −0.6 (−3.5–2.3) | 0.68 |
| Inpatient stays if any, mean | 1.65 | 1.66 | −0.13 (−0.31 to 0.06) | 0.18 |
| Any outpatient institutional spending, % | 75.5 | 75.0 | −1.1 (−4.0 to 1.9) | 0.48 |
| Outpatient institutional spending if any, mean | 3314 | 3038 | −66 (−745 to 614) | 0.85 |
| Any outpatient institutional visits, % | 75.6 | 75.2 | −1.1 (−4.1 to 1.9) | 0.47 |
| Outpatient institutional visits if any, mean | 6.88 | 6.46 | 1.2 (0.63–1.81) | <0.001 |
| Any physician/professional provider spending, % | 92.5 | 92.5 | −2.9 (−4.8 to −1.0) | <0.01 |
| Physician/professional provider spending if any, mean | 4101 | 4156 | 20.1 (−456 to 497) | 0.93 |
| Any physician office visits, % | 87.2 | 87.6 | −2.0 (−4.5 to 0.17) | 0.07 |
| Physician office visits if any, mean | 9.91 | 9.88 | −0.60 (−1.22 to 0.02) | 0.06 |
Note: Weighted means reported for Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018.
Abbreviation: CI, confidence interval.
TABLE A2.
Tests for changes in sample compositional and Medicare (only) spending associated with Medicaid expansion, adults aged 69+, and income ≤135% of the federal poverty level: 2010–2018 health and retirement study.
| Dependent variable | Difference‐in‐differences estimate (standard error) | Pre‐period mean (mean of level shown for log‐transformed variables) | n |
|---|---|---|---|
| Inclusion criteria | |||
| Medicare claims matched to survey a | −0.015 (0.012) | 0.930 | 15,441 |
| Resides in community b | −0.007 (0.009) | 0.916 | 13,802 |
| Has Medicare all year b | −0.0005 (0.0007) | 0.999 | 13,662 |
| Has traditional Medicare all year b | 0.041 (0.026) | 0.618 | 13,654 |
| Medicare spending only c | |||
| Any inpatient spending | −0.003 (0.024) | 0.222 | 7567 |
| log (real inpatient spending) if any | 0.098 (0.123) | 18,415 | 1604 |
| Any outpatient institutional spending | 0.050** (0.020) | 0.744 | 7567 |
| log (real outpatient institutional spending) if any | 0.096 (0.099) | 2393 | 5582 |
| Any physician/professional provider spending | 0.027 (0.018) | 0.912 | 7567 |
| log (physician/professional provider spending) if any | −0.0002 (0.053) | 3306 | 6938 |
Note: The difference‐in‐differences (DD) estimate column presents coefficient estimates and standard errors for EXPANSION × POST from separate regressions. Controls include single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic) and state and year fixed effects. The DD estimates presented reflect absolute, not relative, effects. Standard errors are clustered by state.
Estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older with income at or below 135% of the federal poverty level and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018.
Estimated on the sample in Note (a), conditional on meeting the restrictions shown in previous rows.
Models estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018.
p < 0.05.
TABLE A3.
Robustness checks of main results.
| Include all respondents aged 65 and above | Include respondents meeting state‐specific eligibility requirements for the Qualified Medicare Beneficiary Program only | Add controls for potentially endogenous regressors | ||||
|---|---|---|---|---|---|---|
| Dependent variable | DD estimate (standard error) | n | DD estimate (standard error) | n | DD estimate (standard error) | n |
| Has Medicaid coverage (any month) | 0.105*** (0.030) | 8770 | 0.119** (0.045) | 3766 | 0.088** (0.036) | 7457 |
| Number of months of Medicaid coverage | 1.293*** (0.369) | 8770 | 1.556*** (0.530) | 3766 | 1.104** (0.431) | 7457 |
| Part A enrollment | 0.011** (0.005) | 8770 | 0.003 (0.013) | 3766 | 0.006 (0.005) | 7457 |
| Part B enrollment | 0.028* (0.014) | 8770 | 0.023** (0.009) | 3766 | 0.026** (0.013) | 7457 |
| Any inpatient spending | −0.006 (0.022) | 8770 | 0.035 (0.026) | 3766 | −0.003 (0.019) | 7457 |
| log (real inpatient spending), if any | 0.087 (0.090) | 1813 | 0.204 (0.171) | 798 | 0.125 (0.107) | 1580 |
| Any inpatient stays | −0.005 (0.022) | 8770 | 0.043 (0.026) | 3766 | −0.002 (0.020) | 7457 |
| log (inpatient stays), if any | 0.094* (0.055) | 1838 | 0.179* (0.104) | 809 | 0.134** (0.058) | 1603 |
| Any outpatient institutional spending | 0.034* (0.020) | 8770 | 0.059* (0.029) | 3766 | 0.050*** (0.016) | 7457 |
| log (real outpatient institutional spending), if any | 0.132 (0.094) | 6479 | 0.204 (0.125) | 2792 | 0.181** (0.084) | 5540 |
| Any outpatient institutional visits | 0.036* (0.020) | 8770 | 0.056* (0.029) | 3766 | 0.052*** (0.017) | 7457 |
| log (outpatient institutional visits), if any | 0.034 (0.055) | 6490 | 0.068 (0.093) | 2799 | 0.038 (0.065) | 5549 |
| Any physician/professional provider spending | 0.015 (0.020) | 8770 | 0.021 (0.016) | 3766 | 0.027 (0.016) | 7457 |
| log (physician/professional provider spending), if any | −0.078 (0.053) | 8043 | 0.103 (0.097) | 3533 | 0.029 (0.054) | 6915 |
| Any physician office visits | −0.021 (0.024) | 8770 | 0.029 (0.023) | 3766 | 0.001 (0.020) | 7457 |
| log (physician office visits), if any | −0.044 (0.069) | 7559 | 0.009 (0.088) | 3319 | −0.049 (0.054) | 6535 |
Note: The difference‐in‐differences (DD) estimate column presents coefficient estimates for EXPANSION × POST from separate regressions estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. All regressions are weighted and include controls for single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. See text for details on exclusions/inclusions. The DD estimates presented reflect absolute, not relative, effects. Standard errors are clustered by state.
p < 0.001;
p < 0.05;
p < 0.1.
TABLE A4.
Additional robustness checks of main results.
| Drop respondents with spouses residing in nursing facilities | Drop respondents in states with early Affordable Care Act expansions | Drop respondents in states with 2010–2013 expansions to childless adults | ||||
|---|---|---|---|---|---|---|
| Dependent variable | DD estimate (standard error) | n | DD estimate (standard error) | n | DD estimate (standard error) | n |
| Has Medicaid coverage (any month) | 0.098** (0.039) | 7534 | 0.149*** (0.038) | 6346 | 0.098** (0.041) | 6977 |
| Number of months of Medicaid coverage | 1.213** (0.473) | 7534 | 1.812*** (0.454) | 6346 | 1.231** (0.497) | 6977 |
| Part A enrollment | 0.004 (0.005) | 7534 | 0.004 (0.006) | 6346 | 0.007 (0.005) | 6977 |
| Part B enrollment | 0.024* (0.013) | 7534 | 0.031** (0.012) | 6346 | 0.022 (0.014) | 6977 |
| Any inpatient spending | −0.003 (0.024) | 7534 | 0.019 (0.024) | 6346 | −0.009 (0.026) | 6977 |
| log (real inpatient spending), if any | 0.106 (0.114) | 1604 | 0.015 (0.130) | 1362 | 0.096 (0.121) | 1472 |
| Any inpatient stays | −0.001 (0.026) | 7534 | 0.021 (0.025) | 6346 | −0.010 (0.027) | 6977 |
| log (inpatient stays), if any | 0.131* (0.069) | 1625 | 0.080 (0.072) | 1379 | 0.119 (0.071) | 1496 |
| Any outpatient institutional spending | 0.044** (0.019) | 7534 | 0.052** (0.021) | 6346 | 0.045** (0.021) | 6977 |
| log (real outpatient institutional spending), if any | 0.133 (0.098) | 5601 | 0.145 (0.123) | 4788 | 0.148 (0.109) | 5172 |
| Any outpatient institutional visits | 0.046** (0.019) | 7534 | 0.052** (0.021) | 6346 | 0.047** (0.021) | 6977 |
| log (outpatient institutional visits), if any | 0.012 (0.068) | 5610 | 0.009 (0.070) | 4795 | 0.019 (0.072) | 5181 |
| Any physician/professional provider spending | 0.024 (0.019) | 7534 | 0.033 (0.021) | 6346 | 0.018 (0.019) | 6977 |
| log (physician/professional provider spending), if any | −0.001 (0.054) | 6989 | −0.040 (0.059) | 5931 | −0.016 (0.057) | 6485 |
| Any physician office visits | 0.002 (0.024) | 7534 | 0.003 (0.026) | 6346 | −0.007 (0.024) | 6977 |
| log (physician office visits), if any | −0.049 (0.054) | 6602 | −0.083 (0.055) | 5594 | −0.043 (0.060) | 6126 |
Note: The difference‐in‐differences (DD) estimate columns present coefficient estimates for EXPANSION × POST from separate regressions estimated on 2010–2018 Health and Retirement Study respondents who are age 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. All regressions are weighted and include controls for single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black, other race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. See text for details on exclusions/inclusions. The DD estimates presented reflect absolute, not relative, effects. Standard errors are clustered by state.
p < 0.001;
p < 0.05;
p < 0.1.
FIGURE A1.
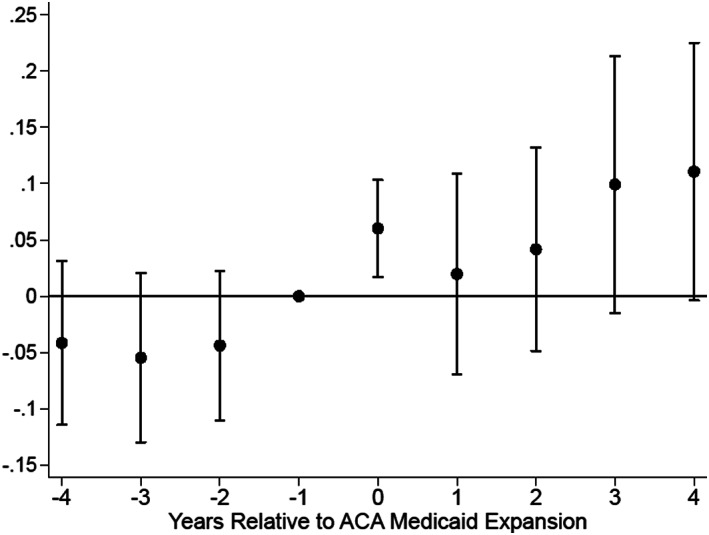
Event study of Medicaid enrollment, 2010–2018. Estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. Weighted coefficients and 95‐percent confidence intervals shown for EXPANSION × 4 YEARS PRE EXPANSION; EXPANSION × 3 YEARS PRE EXPANSION; EXPANSION × 2 YEARS PRE EXPANSION; EXPANSION × YEAR OF EXPANSION; EXPANSION × 1 YEAR POST EXPANSION; EXPANSION × 2 YEARS POST EXPANSION; EXPANSION × 3 YEARS POST EXPANSION; and EXPANSION × 4 YEARS POST EXPANSION The omitted category is EXPANSION × 1 YEAR PRE EXPANSION. Controls include single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black, Other Race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. The p‐value for individual interaction terms are 0.007 (year 0), p = 0.66 (year 1), 0.36 (year 2), 0.09 (year 3), and 0.06 (year 4). The p‐value of an F‐test of the joint significance of pre‐trend coefficient estimates is 0.55.
FIGURE A2.
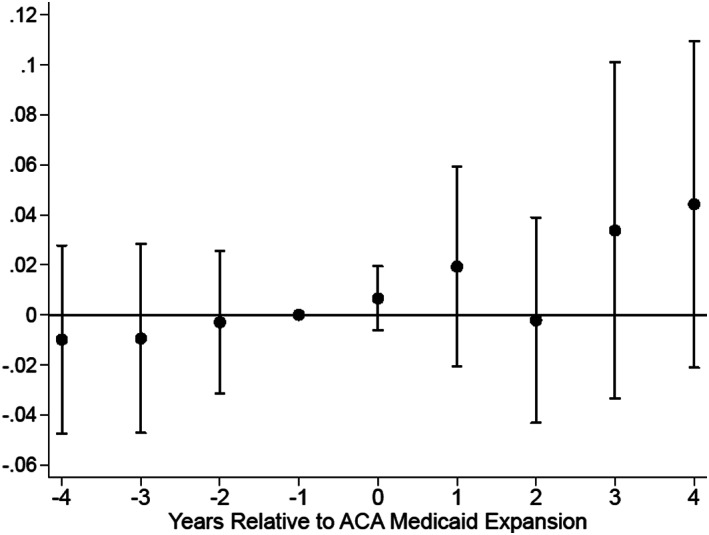
Event study part B Medicare enrollment, 2010–2018. Estimated on 2010–2018 Health and Retirement Study respondents who are aged 69 and older, have Medicare data, have full‐year traditional Medicare enrollment, have income at or below 135% of the federal poverty level, live in the community, and live in states that either expanded Medicaid in 2014 or did not expand Medicaid between 2014 and 2018. Weighted coefficients and 95‐percent confidence intervals shown for EXPANSION × 4 YEARS PRE EXPANSION; EXPANSION × 3 YEARS PRE EXPANSION; EXPANSION × 2 YEARS PRE EXPANSION; EXPANSION × YEAR OF EXPANSION; EXPANSION × 1 YEAR POST EXPANSION; EXPANSION × 2 YEARS POST EXPANSION; EXPANSION × 3 YEARS POST EXPANSION; and EXPANSION × 4 YEARS POST EXPANSION The omitted category is EXPANSION × 1 YEAR PRE EXPANSION. Controls include single year of respondent age, education (less than high school, some college, college or more; the omitted category is high school), sex, race (Black, Other Race; the omitted category is White), and Hispanic ethnicity (the omitted category is non‐Hispanic), and state and year fixed effects. p‐value for individual interaction terms are 0.30 (year 0), p = 0.34 (year 1), 0.92 (year 2), 0.32 (year 3), and 0.18 (year 4). The p‐value of an F‐test of the joint significance of pre‐trend coefficient estimates is 0.88.
Mellor JM, McInerney M, Garrow RC, Sabik LM. The impact of Medicaid expansion on spending and utilization by older low‐income Medicare beneficiaries. Health Serv Res. 2023;58(5):1024‐1034. doi: 10.1111/1475-6773.14155
REFERENCES
- 1. Hamersma S, Kim M, Timpe B. The effect of parental Medicaid expansions on children's health insurance coverage. Contem Econ Policy. 2019;37(2):297‐311. doi: 10.1111/coep.12392 [DOI] [Google Scholar]
- 2. Hudson J, Moriya A. Medicaid expansion for adults had measurable ‘welcome mat’ effects on their children. Health Aff (Millwood). 2017;36(9):1643‐1651. doi: 10.1377/hlthaff.2017.0347 [DOI] [PubMed] [Google Scholar]
- 3. Kenney GM, Long SK, Luque A. Health reform In Massachusetts cut the uninsurance rate among children in half. Health Aff (Millwood). 2010;29(6):1242‐1247. doi: 10.1377/hlthaff.2010.0314 [DOI] [PubMed] [Google Scholar]
- 4. Sonier J, Boudreaux MH, Blewett LA. Medicaid “welcome‐mat” effect of Affordable Care Act implementation could be substantial. Health Aff (Millwood). 2013;32(7):1319‐1325. doi: 10.1377/hlthaff.2013.0360 [DOI] [PubMed] [Google Scholar]
- 5. McInerney M, Mellor JM, Sabik LM. Welcome mats and on‐ramps for older adults: the impact of the Affordable Care Act's Medicaid expansions on dual enrollment in Medicare and Medicaid. J Policy Anal Manag. 2020;40(1):12‐41. doi: 10.1002/pam.22259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McInerney M, McCormack G, Mellor JM, Sabik LM. Association of Medicaid expansion with Medicaid enrollment and health care use among older adults with low income and chronic condition limitations. JAMA Health Forum. 2022;3(6):e221373. doi: 10.1001/jamahealthforum.2022.1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pezzin LE, Kasper JD. Medicaid enrollment among elderly Medicare beneficiaries: individual determinants, effects of state policy, and impact on service use. Health Serv Res. 2002;37(4):827‐847. doi: 10.1034/j.1600-0560.2002.55.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ungaro R, Federman AD. Restrictiveness of eligibility determination and Medicaid enrollment by low‐income seniors. J Aging Soc Policy. 2009;21(4):338‐351. doi: 10.1080/08959420903166993 [DOI] [PubMed] [Google Scholar]
- 9. McInerney M, Winecoff R, Ayyagari P, Simon K, Bundorf MK. ACA Medicaid expansion associated with increased Medicaid participation and improved health among near‐elderly: evidence from the health and retirement study. Inquiry. 2020;57:004695802093522. doi: 10.1177/0046958020935229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barkowski S, Jun D, Zhang Y. Medicaid expansion spillover effects on health care consumption and coverage: evidence from Medicare administrative data. Melbourne Institute Working Paper Forthcoming. 2022. doi: 10.2139/ssrn.4047511 [DOI]
- 11. Bundorf MK, McInerney M, Simon K, Winecoff R. The Effect of Access to Health Insurance before Age 65 on Utilization and Outcomes among Medicare Beneficiaries. Mimeo; 2022. [Google Scholar]
- 12. Center for Medicare & Medicaid Services . Annual report of the boards of trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. Published 2022. 2022. Accessed August 3, 2022. https://www.cms.gov/files/document/2022-medicare-trustees-report.pdf
- 13. Musumeci M. Medicaid's role for Medicare beneficiaries. KFF Published February 17, 2017. Accessed August 3, 2022. https://www.kff.org/medicaid/issue-brief/medicaids-role-for-medicare-beneficiaries/
- 14. Card D, Dobkin C, Maestas N. The impact of nearly universal insurance coverage on health care utilization: evidence from Medicare. Am Econ Rev. 2008;98(5):2242‐2258. doi: 10.1257/aer.98.5.2242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Card D, Dobkin C, Maestas N. Does Medicare save lives? Q J Econ. 2009;124(2):597‐636. doi: 10.1162/qjec.2009.124.2.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357:143‐153. doi: 10.1056/NEJMsa067712 [DOI] [PubMed] [Google Scholar]
- 17. Chatterji P, Nguyen T, Yoruk BK. The effects of Medicare on health care utilization and spending among the elderly. Am J Health Econ. 2021;8(2):151‐180. doi: 10.1086/716544 [DOI] [Google Scholar]
- 18. McWilliams JM. Impact of Medicare coverage on basic clinical services for previously uninsured adults. JAMA Health Forum. 2003;290(6):757‐764. doi: 10.1001/jama.290.6.757 [DOI] [PubMed] [Google Scholar]
- 19. Carey CM, Miller S, Wherry LR. The impact of insurance expansions on the already insured: the Affordable Care Act and Medicare. Am Econ J Appl Econ. 2020;12(4):288‐318. doi: 10.1257/app.20190176 [DOI] [Google Scholar]
- 20. Van Houtven CH, McGarry BE, Jutkowitz E, Grabowski DC. Association of Medicaid expansion under the Patient Protection and Affordable Care Act with use of long‐term care. JAMA Netw Open. 2020;3(10):1‐10. doi: 10.1001/jamanetworkopen.2020.18728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health and Retirement Study, (HRS‐CMS Medicare Cross Reference) restricted dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI; 2021.
- 22. Goodman‐Bacon A. Difference‐in‐differences with variation in treatment timing. J Econom. 2021;225(2):254‐277. doi: 10.1016/j.jeconom.2021.03.014 [DOI] [Google Scholar]
- 23. Acumen LLC. MedRIC Documentation for HRS Data Requestors. Accessed June 14, 2016. https://hrs.isr.umich.edu/sites/default/files/rda-forms/MedRIC-Documentation-for-HRS-Data-Requestors.pdf
- 24. Status of State Action on the Medicaid Expansion Decision. KFF. Published January 10, 2020. Accessed August 3, 2022. https://www.kff.org/health‐reform/state‐indicator/state‐activity‐around‐expanding‐medicaid‐under‐the‐affordable‐care‐act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22
- 25. National Institute on Minority Health and Health Disparities . NIMHD Research Framework. Accessed on January 10, 2023. 2017. https://www.nimhd.nih.gov/about/overview/research-framework.html
- 26. Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947‐956. doi: 10.1056/nejmsa1612890 [DOI] [PubMed] [Google Scholar]
- 27. Ghosh A, Simon K, Sommers B. The effect of health insurance on prescription drug use among low‐income adults: evidence from recent Medicaid expansions. J Health Econ. 2019;63:64‐80. doi: 10.1016/j.jhealeco.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 28. Frean M, Gruber J, Sommers BD. Premium subsidies, the mandate, and Medicaid expansion: coverage effects of the Affordable Care Act. J Health Econ. 2017;53:72‐86. doi: 10.1016/j.jhealeco.2017.02.004 [DOI] [PubMed] [Google Scholar]


