Abstract
Individual-level behavior can be influenced by injunctive and descriptive social network norms surrounding that behavior. There is a need to understand how the influence of social norms within an individual’s social networks may influence individual-level sexual behavior. We aimed to typologize the network-level norms of sexual behaviors within the social networks of Black sexual and gender minoritized groups (SGM) assigned male at birth. Survey data were collected in Chicago, Illinois, USA, between 2018 and 2019 from Black SGM. A total of 371 participants provided individual-level information about sociodemographic characteristics and HIV vulnerability from sex (i.e., condomless sex, group sex, use of alcohol/drugs to enhance sex) and completed an egocentric network inventory assessing perceptions of their social network members’ (alters’) injunctive and descriptive norms surrounding sexual behaviors with increased HIV vulnerability. We used Latent Profile Analysis (LPA) to identify network-level norms based on the proportion of alters’ approval of the participant engaging in condomless sex, group sex, and use of drugs to enhance sex (i.e., injunctive norms) and alters’ engagement in these behaviors (i.e., descriptive norms). We then used binomial regression analyses to examine associations between network-level norm profiles and individual-level HIV vulnerability from sex. The results of our LPA indicated that our sample experienced five distinct latent profiles of network-level norms: (1) low HIV vulnerability network norm, (2) moderately high HIV vulnerability network norm, (3) high HIV vulnerability network norm, (4) condomless sex dominant network norm, and (5) approval of drug use during sex dominant network norm. Condomless anal sex, group sex, and using drugs to enhance sex were positively and significantly associated with higher HIV vulnerability social network norm profiles, relative to low HIV vulnerability norm profiles. To mitigate Black SGM’s HIV vulnerability, future HIV risk reduction strategies can consider using network-level intervention approaches such as opinion leaders, segmentation, induction, or alteration, through an intersectionality framework.
Keywords: Social network analysis, Latent class analysis, Sexual and gender minorities, African Americans, Minority health disparities, HIV
Introduction
Despite the availability of biomedical HIV prevention strategies such as pre-exposure prophylaxis (PrEP), antiretroviral treatment (ART), and Treatment as Prevention (TasP), Black sexual and gender minoritized groups assigned male at birth such as cisgender sexual minoritized men (SMM) and transgender women (TW), continue to be subpopulations at exacerbated vulnerability to HIV in the US (Centers for Disease Control Prevention, 2021; Hess et al., 2017; Matthews et al., 2016). Due largely in part to the benefits of PrEP, ART, and TasP, HIV incidence decreased among White SMM from 2010 to 2019 but did not for Black SMM (Kanny et al., 2019). While 1 in 257 US White heterosexual men will be diagnosed with HIV in their lifetimes and 1 in 11 for white SMM, this rate is 1 in 2 for Black SMM (Hess et al., 2017; Matthews et al., 2016). Alarmingly, a 2021 Centers for Disease Control and Prevention (CDC) surveillance study found that 62% of Black transgender women were living with HIV (Centers for Disease Control Prevention, 2021) and a simulation study by Matthews et al. (2016) found that up to 61% of Black SMM are predicted to be diagnosed with HIV by age 40 years (Matthews et al., 2016).
Structurally, Black SMM and TW experience co-occurring and intersecting discrimination from racism, homophobia, transphobia, biphobia, and HIV-related stigma (Arnold et al., 2014; Cahill et al., 2017; Purdie-Vaughns & Eibach, 2008; Quinn et al., 2019), which can compound to create a new type of discrimination, as best described using the Intersectionality Framework (Bauer, 2014; Bowleg, 2008, 2012, 2013; Callander et al., 2019; Crenshaw, 2017; Duncan et al., 2019, 2020, 2021; English et al., 2020; Feelemyer et al., 2021; Quinn et al., 2019). Social network-based interventions may surmount intersecting structural and systemic oppressions faced by Black sexual minority men and transgender women to mitigate health disparities. Social networks can disseminate information, channel peer/personal influence, and enable attitudinal or behavioral change (Huang et al., 2016; Jaganath et al., 2012; Pagkas-Bather et al., 2020; Rosengren et al., 2016; Rössler, 2017; Wang & Muessig, 2017). This suggests that until health equity in HIV incidence and supranormal levels in the implementation of biomedical strategies are reached, researchers must consider investigating the reduction in individual-level HIV sexual vulnerability behaviors (e.g., condomless sex, group sex, using drugs or alcohol to enhance sex) among Black sexual and gender minoritized groups (SGM), including SMM and TW, using social network approaches which can account for intersectional stigma.
An approach to promote social justice and health equity for Black SMM and TW is to provide SMM and TW with HIV status-neutral care, which confers protection to HIV acquisition (i.e., PrEP and condoms) or prevention of HIV transmission (i.e., ART and condoms) through equitable access pathways for HIV care (Gardner et al., 2011; Myers et al., 2018). However, HIV status-neutral care is not yet widely available and until it is, opportunities to address individual-level sexual behaviors with vulnerability to HIV must be addressed. Previous research surrounding HIV-related health disparities among Black SGM has extensively examined individual-level factors, without prioritizing the multilevel influences of HIV vulnerability and related health disparities (Baral et al., 2013; Bronfenbrenner, 1977), such as those at the network level. For example, the majority of research has been at the individual level and has identified sex-related behaviors associated with HIV vulnerability including sex without using a condom consistently and correctly (De Santis, 2009; Operario et al., 2011), engaging in group sex (Friedman et al., 2008; Prestage et al., 2009), and using drugs or alcohol during sex (Morgan et al., 2016; Washington et al., 2021). There were some differences among these behaviors by race (with Black SMM reporting less risk behaviors relative to White SMM) but due to health disparities and structural oppression, the adverse consequences of sexual vulnerability behaviors disproportionately impact Black SMM (Maulsby et al., 2014; Millett et al., 2007, 2012). This necessitates an examination of health inequities and disparities at higher levels (Halkitis et al., 2013). As Black SGM continue to experience poor HIV outcomes relative to other racial groups due to multilevel influences, HIV vulnerability must account for an individual’s social networks and norms surrounding sexual behaviors. This is a current gap in our understanding of health disparities. Social networks can impact behaviors through various mediating pathways: one of these pathways include through social influence which can be transmitted through networks (Kohler et al., 2001), social network norms (Bandura & Walters, 1977; Marsden, 2006), and an individual’s perceived engagement of their network members in a behavior (Valente et al., 2013).
Although social network behavioral norms have been posited to guide individual-level HIV vulnerability (Bandura, 1994, 2001; Centers for Disease Control & Prevention, 2021; De et al., 2007; Dearing et al., 1994; Latkin et al., 2003, 2010; Sheehan et al., 2019), much of previous research has focused on either the influences of specific network members and sexual partners and less so on the overall influence of the norms of their social networks (Holloway et al., 2015; Tobin & Latkin, 2008). Social networks can be composed of several spheres of influence, including family members, friends, and sexual partners (Miller et al., 2005). Networks can facilitate an environment in which individuals may share norms and behaviors; however, it is unclear how an individual may internalize the diverse and potentially conflicting injunctive and descriptive norms of their social networks. To identify an individual’s network norm, it may be useful to characterize the different typologies of network norms within the social networks of Black SGM. While injunctive norms are behaviors which individuals believe are approved by others within their social networks, descriptive norms are the perceived behaviors that occur within a social network (Baumeister & Vohs, 2007; Cialdini et al., 1990; Kincaid, 2004). Both types of norms have shown to influence individual-level HIV risk behaviors (Bandura, 1994; Latkin et al., 2003, 2010; Sheehan et al., 2019). For example, previous research on descriptive norms has identified that Black SMM who had an “enabler,” or an individual who would not disapprove of the respondent’s HIV sexual vulnerability behavior (i.e., condomless sex, group sex, or drug use during sex), in their social networks were more likely to engage in that behavior, relative to Black SMM who did not have an enabler in their social networks (Schneider et al., 2013). Network characteristics may also be important for consideration: Black SMM with a greater proportion of family members in their social networks were more likely to discourage group sex and drug use during sex to members of their sexual networks (Schneider et al., 2012). This also suggests there may be a threshold effect occurring in networks: individuals may only adopt a norm or behavior once a threshold of their network adopts that norm or behavior (Montgomery & Chung, 1999; Valente, 1996).
These foundational social network norm studies relied on a variable-centered approach as social network sexual norms have yet to be examined synchronously in the context of a person-centered approach such as Latent Profile Analysis (LPA). LPA is a method to identify patterns of social network injunctive and descriptive sexual norms among Black SGM who may be at heightened sexual vulnerability to HIV, using a person-centered approach. Latent class analysis has previously been used in social network research among people from low-income neighborhoods to identify social support patterns within social support networks (Bohnert et al., 2010) and young SMM to identify sexual partner typologies (Janulis et al., 2018). Additionally, LCA aligns with the Intersectionality theory as it allows for overlapping experiences to be captured at the person level and identifies the resulting unique typology. The present study aimed to examine profiles of injunctive sexual norms (i.e., Black SGM network members approve of the individual engaging in condomless sex, group sex, or using drugs or alcohol to enhance sex), and descriptive sexual norms (i.e., Black SGM network members engage in condomless sex, group sex, or using drugs or alcohol to enhance sex) within the social networks of Black SGM. We hypothesize that Black SGM will have distinct network profiles of social network norms surrounding approval and engagement of these sexual behaviors and these norms will be associated with increased individual-level HIV vulnerability behaviors of condomless sex, group sex, and using drugs or alcohol to enhance sex.
Method
Participants
Data were from the baseline wave of the Neighborhoods and Networks (N2) Cohort Study, a prospective longitudinal study of Black SGM (baseline data were collected from January 2018 to December 2019). Black SGM were recruited via peer referral sampling in Chicago, Illinois, United States (US). Trained interviewers obtained participant’s written consent and then, used interviewer-administered computer-assisted assessments to collect information about participants. Assessments were conducted in a private room at the study site and lasted 1–2 hours in length. Additional study information can be found elsewhere (Duncan et al., 2019). Participants were provided $150 for their time and transportation to the study site, and participants were provided $20 for each referral, with a maximum of 6 referrals possible. Participants provided individual-level information surrounding their sociodemographic characteristics, relationship characteristics, HIV sexual vulnerability behaviors, HIV status neutral treatment and care. Participants were also asked to name up to 5 alters whom they considered to be a part of their confidant networks and then, administered an egocentric network inventory which assessed the (1) participant’s perception of each confidant alter’s sociodemographic characteristics, (2) confidant alter’s relationship characteristics with the participant, (3) participant’s perception of the confidant alter’s sexual vulnerability to HIV, and (4) participant’s perception of the confidant alter’s approval of the participant engaging in HIV vulnerability behaviors.
Measures
Participant’s Sociodemographic and Background Characteristics
Participants provided information about their age (in years), gender (cisgender man or transgender woman, non-binary, or other), sexual orientation (gay/homosexual/lesbian, bisexual, straight/heterosexual, or other), relationship status (not single or single), ethnicity (Hispanic/Latine or not Hispanic/Latine), education (high school degree or no high school degree), employment status (employed full-time or not employed full-time), income ($20,000 a year or less, or above $20,000 a year), housing instability in the past year (history of housing instability or did not experience housing instability), number of sexual partners in the past 6 months, self-reported HIV serostatus (HIV negative or living with HIV), and adherence to ART or PrEP.
Confidant Network Member’s Sociodemographic Characteristics
Participants provided information surrounding each alter’s gender (cisgender man, cisgender woman, or another transgender identity) age, ethnicity (Hispanic/Latine or not Hispanic/Latine), and race (Black or not Black).
Alter’s Relationship Characteristics
Participants indicated the relationship type with their alter: family (i.e., immediate, extended, and god parent/sibling), romantic or sexual partner (current or former), chosen family [i.e., play, House Ball (i.e., “a kinship system that is organized to meet the needs of its members for social solidarity and mentoring” (Arnold & Bailey, 2009; Murrill et al., 2008; Phillips et al., 2011), gay sibling, friend, or different relationship (e.g., counselor, minister, therapist). Participants described their emotional closeness to and how often they communicated with the alter.
Alter’s Sexual Vulnerability to HIV
Participants described 3 descriptive and 3 injunctive norms for each confidant alter. Participants indicated descriptive norms such as condomless sex (yes, or no/don’t know), use of drugs or alcohol to enhance sex (yes, or no/don’t know), or engagement in group sex (yes, or no/don’t know). Participants were asked to indicate the alter’s approval (i.e., injunctive norm) of the participant engaging in condomless sex (yes, or no/don’t know), using drugs or alcohol to enhance sex (yes, or no/don’t know), or engaging in group sex (yes, or no/don’t know).
Network Proportions of Sexual Behavior and Approval of Participant Engaging in Behavior
We calculated proportion of networks that responded “yes” to each of the sexual vulnerability behaviors and approval of the participant engaging in sexual vulnerability behaviors.
Individual-Level HIV Vulnerability Behaviors
Participants indicated if they engaged in condomless sex in the past 6 months, if they had ever had group sex (sex between three or more people) in the past 6 months, and if they used drugs or alcohol to enhance sex in the past 6 months.
Analysis
In line with intersectionality theory, we used LPA to identify latent profiles (Wilson & Urick, 2022). Previous studies have also used LPA to construct network norm profiles surrounding HIV sexual vulnerability, based on an individual’s sexual partner network, but have not assessed the impact of social network-level norms (Dangerfield et al., 2018). We used the tidyLPA package on the R environment to examine latent profiles until the best fitting profile emerged. We used the following indices to identify the optimal profile solution: Bayes information criterion (BIC), Akaike’s information criterion (AIC), Entropy, Bootstrap likelihood ratio test (BLRT), Prob. Min/Prob. Max, and the unique sample size of each profile. Lower values of BIC and AIC indicate a more parsimonious fit (Akaike, 1974; Akaike, 1980; Schwarz, 1978). Entropy values closer to 1 indicate the model’s ability to discriminate between profiles (Celeux & Soromenho, 1996). The BLRT assesses if model fit is superior relative to the model with one profile less (Lo et al., 2001; McLachlan & Peel, 2004). We also considered the Prob. Min (minimum of the diagonal of the average latent profile probabilities for most likely profile membership, by assigned profile) and Prob. Max (maximum of the diagonal of the average latent profile probabilities for most likely profile membership, by assigned profile) as these indices signify greater classification as values increase (Jung & Wickrama, 2008). Finally, we considered the sample size of each profile (Min n), as models with profiles that are less than or equal to 25 members could indicate a spurious finding (Jung & Wickrama, 2008).
After identifying the most parsimonious latent profile solution, we used bivariate associations to examine the relationship between network profile membership and other measures. We used binomial regression models to assess the associations between the network-level LPA profiles, and five individual-level HIV sexual vulnerability outcomes (condomless anal sex in the past 6 months, condomless insertive anal sex in the past 6 months, condomless receptive anal sex in the past 6 months, group sex in the past 6 months, and the use of drugs or alcohol to enhance sex in the past 6 months).
Results
Analytic Sample
Study staff recruited and enrolled 412 Black SGM into the parent study. Of participants, 377 reported sex in the past 6 months and named up to 5 confidant network alters (n = 1036 alters). There were missing data for 2 participants’ confidant networks, so information from 375 participants and 1016 social network alters was included in the LPA. There were missing data for 2 participants’ sexual orientation and 2 participants’ laboratory-confirmed HIV serostatus. We used listwise deletion to identify the final sample size (n = 371).
Latent Profile Analysis for Identifying Injunctive and Descriptive Sex Behavior Norms
We assessed several fit criteria in the selection of the latent profile model of the most parsimonious fit (Pastor et al., 2007). Based on BIC and AIC values which were lowest in the 5-profile model solution, we identified the 5-profile model solution as the best fit to the data. In accordance with the BLRT values, the 5-profile model solution was identified as superior to the 4-profile solution (BLRT = 230.09; BLRT p-value < 0.01). Although the BLRT suggested that the 6-profile solution was a significantly better fit to the data relative to the 5-profile solution, the minimum proportion of participants who were grouped into the smallest size group was 0, indicating that this model contains a group which is a spurious finding or may not have converged. Additional information about latent profile model fit indices can be found in Supplemental Table 1. Figure 1 visualizes the mean probability of being included in each social network norm profile. Social network sexual norms were categorized as: (1) Low HIV vulnerability network norm (low injunctive and descriptive norm of sexual behaviors), (2) Moderately high HIV vulnerability network norm (high injunctive and descriptive norms of group sex and using drugs to enhance sex, and moderately high injunctive and descriptive norms of condomless sex), (3) High HIV vulnerability network norm (high injunctive and descriptive norms of condomless sex and drug use to enhance sex, and moderately high injunctive and descriptive norms of group sex), (4) Approval of drugs to enhance sex dominant network norm (high injunctive norm of participant engaging in using drugs or alcohol to enhance sex but low injunctive and descriptive norms of all other behaviors), and (5) Condomless sex dominant network norm (high descriptive norm of condomless sex; low injunctive and descriptive norm of other behaviors).
Fig. 1.
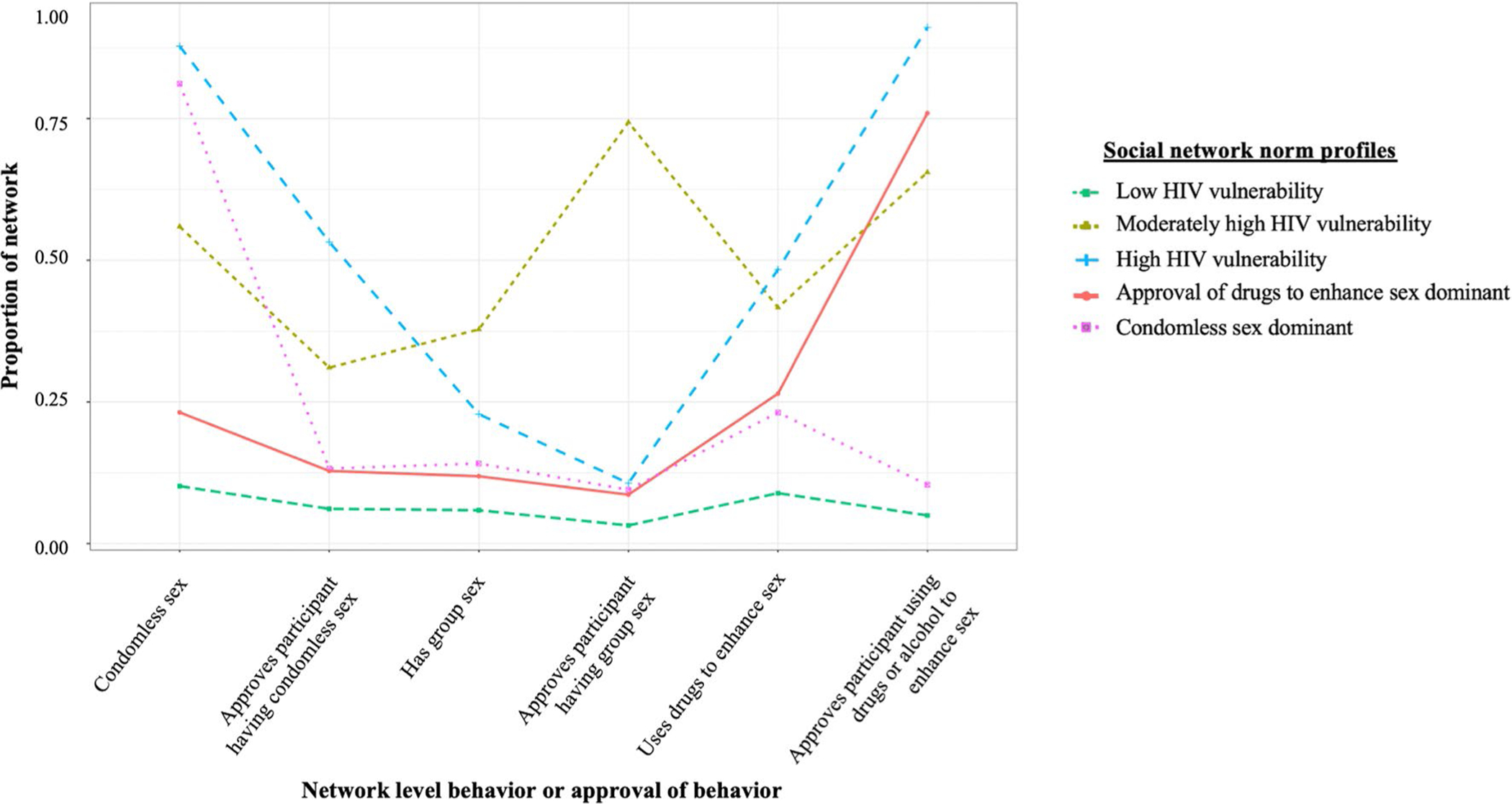
Five profile latent class distribution of HIV network perceptions among Black sexual and gender minoritized groups
Comparison of Participant Background Information, by Network Norm Profilel
Participants were a mean age of 26 years old (± 4 years). The majority of participants identified as a cisgender man (87%), gay/homosexual/lesbian (61%), not Hispanic/Latine (93%), and single (62%). The majority of participants reported an income less than $20,000 a year (66%), had more than a high school diploma (49%), did not experience housing instability in the past year (69%), were HIV negative (67%), and were not adherent (i.e., missed a dose in the past 30 days) to PrEP or ART (90%). Approximately half of participants reported full-time employment. Participants reported a mean of 3.7 (± 3.8) sexual partners and 17% reported selling or exchanging sex for money, drugs, food and/or shelter in the past 6 months. Approximately half of participants were employed in the past week. The majority of participants reported condomless anal sex in the past 6 months (84%), and 95% engaged in insertive anal sex of which 52% reported condomless insertive anal sex, and 96% engaged in receptive anal sex of which 46% reported condomless receptive anal sex (Tables 1 and 2). Slightly less than half of participants engaged in group sex (45%), and the majority of participants reported the use of alcohol or drugs during sex to enhance the experience (58%). Additional participant background information, by network norm profile, can be found in Table 1.
Table 1.
Background information of participants stratified by latent profile, n = 375
| Low HIV vulnerability network norm (N = 140) | Approval of drugs to enhance sex network norm (N = 41) | Moderately high HIV vulnerability network norm (N = 81) | High HIV vulnerability network norm (N = 34) | Condomless sex network norm (N = 79) | Overall (N = 375) | Test statistic | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age | F = 2.17 | ||||||
| Mean (SD) | 25.6 (4.04) | 26.2 (4.00) | 26.8 (3.93) | 25.2 (3.78) | 25.1 (4.02) | 25.8 (4.01) | |
| Median [Min, Max] | 25.0 [18.0, 34.0] | 26.0 [19.0, 36.0] | 27.0 [19.0, 34.0] | 25.0 [19.0, 33.0] | 24.0 [17.0, 34.0] | 25.0 [17.0, 36.0] | |
| Gender | χ2 = 4.41 | ||||||
| Cis man | 118 (84.3%) | 33 (80.5%) | 72 (88.9%) | 31 (91.2%) | 72 (91.1%) | 326 (86.9%) | |
| Transgender or non-binary | 22 (15.7%) | 8 (19.5%) | 9 (11.1%) | 3 (8.8%) | 7 (8.9%) | 49 (13.1%) | |
| Sexual orientation† | χ2 = 9.42 | ||||||
| Gay, homosexual, or Lesbian | 88 (63.8%) | 22 (53.7%) | 46 (56.8%) | 24 (70.6%) | 45 (57.0%) | 225 (60.3%) | |
| Bisexual | 32 (23.2%) | 13 (31.7%) | 25 (30.9%) | 4 (11.8%) | 22 (27.8%) | 96 (25.7%) | |
| Different sexual orientation†† | 8 (5.8%) | 3 (7.3%) | 7 (8.6%) | 2 (5.9%) | 7 (8.9%) | 27 (7.2%) | |
| Straight or heterosexual | 10 (7.2%) | 3 (7.3%) | 3 (3.7%) | 4 (11.8%) | 5 (6.3%) | 25 (6.7%) | |
| Hispanic or Latine* | |||||||
| No | 134 (97.1%) | 39 (95.1%) | 72 (88.9%) | 33 (97.1%) | 70 (88.6%) | 348 (93.3%) | χ2 = 9.48 |
| Yes | 4 (2.9%) | 2 (4.9%) | 9 (11.1%) | 1 (2.9%) | 9 (11.4%) | 25 (6.7%) | |
| Relationship status | χ2 = 4.54 | ||||||
| Not single | 54 (38.6%) | 16 (39.0%) | 23 (28.4%) | 13 (38.2%) | 35 (44.3%) | 141 (37.6%) | |
| Single | 86 (61.4%) | 25 (61.0%) | 58 (71.6%) | 21 (61.8%) | 44 (55.7%) | 234 (62.4%) | |
| Education | χ2 = 14.49 | ||||||
| More than high school | 21 (51.2%) | 44 (54.3%) | 57 (40.7%) | 15 (44.1%) | 45 (57.0%) | 182 (48.5%) | |
| High school diploma or equivalent (for example, GED) | 13 (31.7%) | 33 (40.7%) | 59 (42.8%) | 15 (44.1%) | 21 (26.6%) | 141 (37.8%) | |
| No high school diploma | 7 (17.1%) | 4 (4.9%) | 23 (16.7%) | 4 (11.8%) | 13 (16.5%) | 51 (13.7%) | |
| Employment status | χ2 = 3.63 | ||||||
| No | 66 (47.1%) | 16 (39.0%) | 44 (54.3%) | 17 (50.0%) | 43 (54.4%) | 186 (49.6%) | |
| Yes | 74 (52.9%) | 25 (61.0%) | 37 (45.7%) | 17 (50.0%) | 36 (45.6%) | 189 (50.4%) | |
| Income | χ2 = 7.01 | ||||||
| Above $20,000 a year | 38 (27.1%) | 17 (41.5%) | 35 (43.2%) | 11 (32.4%) | 28 (35.4%) | 129 (34.4%) | |
| $20,000 or less a year | 102 (72.9%) | 24 (58.5%) | 46 (56.8%) | 23 (67.6%) | 51 (64.6%) | 246 (65.6%) | |
| History of unstable housing | χ2 = 5.00 | ||||||
| No | 90 (64.3%) | 31 (75.6%) | 54 (66.7%) | 27 (79.4%) | 58 (73.4%) | 260 (69.3%) | |
| Yes | 50 (35.7%) | 10 (24.4%) | 27 (33.3%) | 7 (20.6%) | 21 (26.6%) | 115 (30.7%) | |
| Proportion of network that participant has had sex with | F = 2.24 | ||||||
| Mean (SD) | 0.473 (0.218) | 0.450 (0.233) | 0.527 (0.169) | 0.561 (0.192) | 0.513 (0.234) | 0.499 (0.213) | |
| Median [Min, Max] | 0.500 [0,1.00] | 0.500 [0, 0.833] | 0.500 [0.200, 1.00] | 0.500 [0.167, 1.00] | 0.500 [0, 1.00] | 0.500 [0, 1.00] | |
| Number of sex partners in the past 6 months | F = 4.20 | ||||||
| Mean (SD) | 3.16 (3.73) | 3.07 (3.40) | 5.07 (4.02) | 2.85 (2.23) | 3.92 (4.21) | 3.70 (3.83) | |
| Median [Min, Max] | 2.00 [0, 29.0] | 2.00 [0, 16.0] | 4.00 [0, 18.0] | 2.50 [0, 9.00] | 3.00 [0, 18.0] | 2.00 [0, 29.0] | |
| Exchanged sex for money, drugs, food, or shelter | χ2 = 8.93 | ||||||
| No | 121 (86.4%) | 31 (75.6%) | 60 (74.1%) | 28 (82.4%) | 70 (88.6%) | 310 (82.7%) | |
| Yes | 19 (13.6%) | 10 (24.4%) | 21 (25.9%) | 6 (17.6%) | 9 (11.4%) | 65 (17.3%) | |
| HIV status | |||||||
| HIV Negative | 98 (70.0%) | 23 (56.1%) | 51 (63.0%) | 20 (58.8%) | 59 (74.7%) | 251 (66.9%) | χ2 = 6.50 |
| Living with HIV | 42 (30.0%) | 18 (43.9%) | 30 (37.0%) | 14 (41.2%( | 20 (25.3%) | 124 (33.1%) | |
| Adherent to PrEP or ART | χ2 = 2.82 | ||||||
| No | 123 (87.9%) | 35 (85.4%) | 75 (92.6%) | 31 (91.2%) | 73 (92.4%) | 337 (89.9%) | |
| Yes | 17 (12.1%) | 6 (14.6%) | 6 (7.4%) | 3 (8.8%) | 6 (7.6%) | 38 (10.1%) | |
| Engaged in insertive anal sex in past 6 months** | χ2 = 2.19 | ||||||
| Engaged in insertive anal sex | 133 (95.0%) | 39 (95.1%) | 79 (97.5%) | 31 (91.2%) | 75 (94.9%) | 357 (95.2%) | |
| Engaged in condomless insertive anal sex | 60 (42.9%) | 18 (43.9%) | 54 (66.7%) | 20 (58.8%) | 42 (53.2%) | 194 (51.7%) | χ2 = 13.24 |
| Engaged in receptive anal sex in past 6 months* | |||||||
| Engaged in receptive anal sex | 134 (95.7%) | 39 (95.1%) | 79 (97.5%) | 34 (100%) | 74 (93.7%) | 360 (96.0%) | χ2 = 3.14 |
| Engaged in condomless receptive anal sex | 55 (39.3%) | 19 (46.3%) | 37 (45.7%) | 24 (70.6%) | 37 (46.8%) | 172 (45.9%) | χ2 = 9.71 |
| Engaged in both insertive and receptive (versatile) anal sex in past 6 months* | |||||||
| Engaged in versatile anal sex | 38 (92.7%) | 78 (96.3%) | 130 (94.2%) | 31 (91.2%) | 73 (92.4%) | 350 (93.8%) | χ2 = 1.67 |
| Engaged in condomless versatile anal sex | 19 (46.3%) | 37 (45.7%) | 54 (39.1%) | 24 (70.6%) | 37 (46.8%) | 171 (45.8%) | χ2 = 10.93 |
| Had condomless sex in past 6 months* | χ2 = 11.03 | ||||||
| No | 34 (24.3%) | 7 (17.1%) | 8 (9.9%) | 3 (8.8%) | 10 (12.7%) | 62 (16.5%) | |
| Yes | 106 (75.7%) | 34 (82.9%) | 73 (90.1%) | 31 (91.2%) | 69 (87.3%) | 313 (83.5%) | |
| Had group sex in past 6 months*** | χ2 = 28.36 | ||||||
| No | 97 (69.3%) | 26 (63.4%) | 29 (35.8%) | 16 (47.1%) | 36 (45.6%) | 204 (54.4%) | |
| Yes | 43 (30.7%) | 15 (36.6%) | 52 (64.2%) | 18 (52.9%) | 43 (54.4%) | 171 (45.6%) | |
| Used drugs to enhance sex*** | χ2 = 25.84 | ||||||
| No | 79 (56.4%) | 15 (36.6%) | 20 (24.7%) | 9 (26.5%) | 34 (43.0%) | 157 (41.9%) | |
| Yes | 61 (43.6%) | 26 (63.4%) | 61 (75.3%) | 25 (73.5%) | 45 (57.0%) | 218 (58.1%) | |
p < 0.05
p < 0.01
p < 0.001
Missing information from 2 participants
Different sexual orientation included write in responses (i.e., “Transgender,” “Male,” “Female”), “Confused,” “Curious,” “Girl,” “Nothing,” “Open to all,” “Pansexual,” “Queer,” and “Trade.”
Table 2.
Confidant network member information, n = 1016
| Overall (N = 1016) |
|
|---|---|
|
| |
| Gender | |
| Cisgender man | 532 (52.4%) |
| Cisgender woman | 408 (40.2%) |
| Transgender or non-binary | 73(7.2%) |
| Missing | 3 (0.3%) |
| Age | |
| Mean (SD) | 31.3 (11.4) |
| Median [Min, Max] | 28.0 [15.0, 93.0] |
| Missing | 14 (1.4%) |
| Hispanic or Latine | 58 (5.7%) |
| Black | 948 (93.3%) |
| Relationship status | |
| In a committed relationship with one other person | 337 (33.2%) |
| Married | 90 (8.9%) |
| Single | 498 (49.0%) |
| Different relationship status* | 91 (9.%) |
| Relationship to participant | |
| Best Friend | 295 (29.0%) |
| Family | 263 (25.9%) |
| Friend | 162 (15.9%) |
| Current or Former Romantic/Sex partner/spouse | 127 (12.5%) |
| Chosen family | 55 (5.4%) |
| Different relationship** | 21 (2.1%) |
| Closeness | |
| Not close | 16 (1.6%) |
| Somewhat close | 169 (16.6%) |
| Very close | 831 (81.8%) |
| Communication frequency | |
| Several times a day | 247 (24.3%) |
| Every day | 361 (35.5%) |
| Several times a week | 258 (25.4%) |
| Once a week | 68 (6.7%) |
| Once every two weeks or less frequently | 82 (8.1%) |
| Has condomless sex | 460 (45.3%) |
| Approves of participant having condomless sex | 191 (18.8%) |
| Engages in group sex | 180 (17.7%) |
| Approves of participant engaging in group sex | 247 (24.3%) |
| Uses alcohol or drugs to enhance sex | 243 (23.9%) |
| Approves of participant using alcohol or drugs to enhance sex | 360 (35.4%) |
Includes don’t know, widowed, complicated, in a relationship with more than one person
Includes colleague, counselor, minister, therapist, among other relationship types
Confidant network characteristics—Participants reported a mean of 2.7 confidant network alters (± 1.25 alters) for a total of 1,016 alters. Alters were perceived as being mean age 31.3 years (± 11.4 years), and participants perceived alters to be cisgender men (52%), cis women (40%), or of transgender experience (7%). Alters were perceived as majority Black (93%), non-Hispanic/Latine (94%), unmarried (49%), and either a friend, family, or chosen family member of the participant (85%). Of alters, 13% were current or former sexual partners of participants. Participants reported being very close to alters (82%) and communicated with alters frequently, with 92% of participants reporting communicating with alters at least once a week, suggesting high potential for social influence. The majority of alters did not engage in the HIV vulnerability behaviors (condomless sex = 45%, group sex = 18%, use of drugs to enhance sex = 24%) or approve of participants engaging in these behaviors (condomless sex = 25%, group sex = 35%, use of alcohol or drugs to enhance sex = 24%). Additional information can be found in Table 2.
Binomial Regression Model Examining Condomless Anal Sex
Relative to participants who reported being in a relationship, participants who reported being single had lower likelihood of reporting condomless sex in the past 6 months (OR = 0.49, 95% CI 0.25–0.91, p = 0.027). Participants who reported having a higher number of sex partners in the past 6 months (OR = 1.27, 95% CI 1.09–1.53, p = 0.005) had higher likelihood of reporting condomless sex in the past 6 months. There was no statistical significance between latent profile and condomless sex. Additional information can be found in Table 3: Model 1a.
Table 3.
Results of the binomial regression models examining condom use
| Predictors | Model 1a: Condomless anal sex | Model 1b: Condomless insertive anal sex | Model 1c: Condomless receptive anal sex | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Odds Ratios | CI | p | Odds Ratios | CI | p | Odds Ratios | CI | p | |
|
| |||||||||
| (Intercept) | 1.05 | 0.11–10.07 | 0.968 | 1.04 | 0.16–6.73 | 0.963 | 0.71 | 0.11–4.80 | 0.729 |
| Age | 1.02 | 0.94–1.10 | 0.629 | 0.98 | 0.92–1.04 | 0.477 | 0.96 | 0.90–1.02 | 0.218 |
| Transgender | 1.16 | 0.41–3.59 | 0.785 | 0.35 | 0.15–0.79 | 0.013 | 3.83 | 1.69–9.22 | 0.002 |
| Sexual Orientation | |||||||||
| Ref=Gay | |||||||||
| Bisexual | 0.73 | 0.36–1.51 | 0.386 | 1.55 | 0.88–2.75 | 0.128 | 0.24 | 0.13–0.44 | < 0.001 |
| Different sexual orientation | 2.45 | 0.57–17.87 | 0.288 | 0.99 | 0.40–2.50 | 0.978 | 0.59 | 0.24–1.44 | 0.241 |
| Straight or heterosexual | 0.89 | 0.25–3.50 | 0.860 | 1.20 | 0.41–3.58 | 0.734 | 0.25 | 0.08–0.74 | 0.014 |
| Not in a relationship | 0.49 | 0.25–0.91 | 0.027 | 0.87 | 0.54–1.40 | 0.567 | 1.03 | 0.64–1.68 | 0.894 |
| No high school education | 1.58 | 0.66–4.22 | 0.330 | 1.67 | 0.82–3.46 | 0.162 | 0.99 | 0.48–2.03 | 0.981 |
| Not employed | 0.84 | 0.43–1.61 | 0.595 | 1.04 | 0.63–1.74 | 0.868 | 1.18 | 0.71–1.98 | 0.528 |
| Income is below $20,000 | 0.85 | 0.39–1.79 | 0.669 | 0.48 | 0.27–0.83 | 0.009 | 0.99 | 0.57–1.73 | 0.975 |
| Housing instability | 0.70 | 0.35–1.42 | 0.314 | 1.57 | 0.91–2.74 | 0.110 | 0.89 | 0.51–1.54 | 0.667 |
| Living with HIV | 1.39 | 0.74–2.64 | 0.308 | 1.06 | 0.65–1.73 | 0.813 | 1.63 | 0.99–2.70 | 0.058 |
| Using PrEP or ARTs | 1.39 | 0.67–3.05 | 0.391 | 0.88 | 0.50–1.54 | 0.644 | 1.01 | 0.56–1.79 | 0.984 |
| Proportion of network that participant has had sex with | 2.93 | 0.58–15.70 | 0.201 | 4.40 | 1.27–15.92 | 0.021 | 4.32 | 1.24–15.61 | 0.023 |
| Number of sexual partners in past 6 months | 1.27 | 1.09–1.53 | 0.005 | 1.00 | 0.94–1.07 | 0.971 | 1.06 | 0.99–1.14 | 0.096 |
| Exchanged/sold sex for money, drugs, food, or shelter | 1.11 | 0.43–3.27 | 0.844 | 1.11 | 0.57–2.22 | 0.758 | 0.98 | 0.49–1.95 | 0.960 |
| Network norm profile | |||||||||
| Ref = Low HIV vulnerability | |||||||||
| Moderately high HIV vulnerability | 2.36 | 1.00–6.11 | 0.061 | 2.40 | 1.28–4.57 | 0.007 | 1.31 | 0.69–2.47 | 0.406 |
| High vulnerability | 3.02 | 0.94–13.60 | 0.095 | 2.01 | 0.86–4.86 | 0.110 | 3.26 | 1.40–8.04 | 0.008 |
| Approval of drugs to enhance sex dominant | 1.58 | 0.62–4.47 | 0.362 | 1.05 | 0.48–2.29 | 0.908 | 1.53 | 0.68–3.44 | 0.304 |
| Condomless sex dominant | 2.10 | 0.96–4.91 | 0.072 | 1.28 | 0.69–2.37 | 0.433 | 1.56 | 0.84–2.93 | 0.161 |
| Observations | 371 | 353 | 356 | ||||||
| R2 Tjur | 0.127 | 0.122 | 0.157 | ||||||
Bold font indicates significant p-values
Binomial Regression Model Examining Condomless Insertive Anal Sex Among Participants Who Reported Insertive Anal Sex
Relative to participants who reported identifying as a cisgender man, participants who identified as a transgender woman or non-binary and were assigned male at birth (OR = 0.35, 95% CI 0.15–0.79, p = 0.013) and participants who reported an income below $20,000 (OR = 0.48, 95% CI 0.27–0.83, p = 0.009) had lower likelihood of reporting condomless insertive sex in the past 6 months. Participants who reported having sex with a larger proportion of their network (OR = 4.40; 95% CI 1.27–15.92; p = 0.021), and being in the moderately high HIV vulnerability network norm profile (OR = 2.40; 95% CI 1.28–4.57; p = 0.007) relative to the low HIV vulnerability network norm profile had positive and significant associations of engaging in condomless insertive anal sex in the past 6 months. Additional information can be found in Table 3: Model 1b.
Binomial Regression Model Examining Condomless Receptive Anal Sex Among Participants Who Reported Receptive Anal Sex
Relative to participants who reported identifying as a cisgender man, participants who identify as a transgender woman or non-binary and assigned male at birth (OR = 3.83, 95% CI 1.69–9.22, p = 0.002), participants who had sex with a larger portion of their social network (OR = 4.32, 95% CI 1.24–15.61, p = 0.023), and being in the high HIV vulnerability network norm profile (OR = 3.26; 95% CI 1.40–8.04, p = 0.008) relative to the low HIV vulnerability network norm profile had positive and significant associations of engaging in condomless receptive anal sex in the past 6 months. Participants who identified as bisexual (OR = 0.24, 95% CI 0.13–0.44, p < 0.001), or straight/heterosexual (OR = 0.25, 95% CI 0.08–0.74, p = 0.014), relative to gay, had negative and significant associations of engaging in condomless receptive anal sex in the past 6 months. Additional information can be found in Table 3: Model 1c.
Binomial Regression Model Examining Group Sex
Participants who reported not being in a relationship (OR = 1.81; 95% CI 1.07–3.08; p = 0.028), having sex with a larger proportion of their network (OR = 9.96; 95% CI 2.65–39.73; p = 0.001), having a higher number of sexual partners in the past 6 months (OR = 1.23; 95% CI 1.11–1.37; p < 0.001), and relative to the low HIV vulnerability network norm profile being in either the moderately high HIV vulnerability network norm profile (OR = 2.99; 95% CI 1.50–6.02; p = 0.002), high vulnerability network norm profile (OR = 3.13; 95% CI 1.29–7.72; p = 0.012), and the condomless sex network norm profile (OR = 3.08; 95% CI 1.58–6.10; p = 0.001), had positive and significant associations of engaging in group sex in the past 6 months. It may be of interest to note that although not significant at p < 0.05, exchanging or selling sex for money, drugs, food or shelter (OR = 2.10; 95% CI 1.00–4.51; p = 0.053) was found to be trending toward significance for association with group sex in the past 6 months. Additional information can be found in Table 4: Model 2.
Table 4.
Results of the binomial regression models examining group sex and using drugs to enhance sex
| Predictors | Model 2: Group sex |
Model 3: Used alcohol or drugs to enhance sex |
||||
|---|---|---|---|---|---|---|
| Odds Ratios | CI | p | Odds Ratios | CI | p | |
|
| ||||||
| (Intercept) | 0.01 | 0.00–0.10 | < 0.001 | 0.30 | 0.05–1.84 | 0.196 |
| Age | 1.05 | 0.98–1.12 | 0.180 | 0.99 | 0.93–1.06 | 0.840 |
| Transgender | 1.63 | 0.64–4.20 | 0.308 | 0.76 | 0.33–1.72 | 0.504 |
| Sexual Orientation | 1.46 | 0.79–2.71 | 0.233 | 1.50 | 0.85–2.68 | 0.163 |
| Ref = Gay | ||||||
| Bisexual | 1.16 | 0.44–3.03 | 0.761 | 1.13 | 0.46–2.82 | 0.792 |
| Different sexual orientation | 0.78 | 0.23–2.57 | 0.690 | 1.61 | 0.56–4.80 | 0.382 |
| Straight or heterosexual | 1.81 | 1.07–3.08 | 0.028 | 1.06 | 0.66–1.69 | 0.823 |
| Not in a relationship | 1.82 | 1.08–3.09 | 0.026 | 1.07 | 0.67–1.71 | 0.776 |
| No high school education | 0.78 | 0.36–1.69 | 0.540 | 0.98 | 0.50–1.96 | 0.964 |
| Not employed | 0.73 | 0.42–1.28 | 0.271 | 1.22 | 0.74–2.03 | 0.431 |
| Income is below $20,000 | 1.15 | 0.63–2.10 | 0.656 | 1.25 | 0.72–2.17 | 0.427 |
| Housing instability | 1.14 | 0.62–2.08 | 0.677 | 0.75 | 0.43–1.30 | 0.307 |
| Living with HIV | 0.85 | 0.49–1.45 | 0.543 | 0.94 | 0.57–1.53 | 0.794 |
| Using PrEP or ARTs | 0.89 | 0.48–1.67 | 0.727 | 0.83 | 0.47–1.44 | 0.501 |
| Proportion of network that participant has had sex with | 9.96 | 2.65–39.73 | 0.001 | 3.37 | 1.05–11.28 | 0.044 |
| Number of sexual partners in past 6 months | 1.23 | 1.11–1.37 | < 0.001 | 1.04 | 0.97–1.13 | 0.279 |
| Exchanged/sold sex for money, drugs, food, or shelter | 2.10 | 1.00–4.51 | 0.053 | 2.98 | 1.41–6.75 | 0.006 |
| Network norm profile | ||||||
| Ref = Low HIV vulnerability | ||||||
| Moderately high HIV vulnerability | 2.99 | 1.50–6.02 | 0.002 | 3.47 | 1.83–6.76 | < 0.001 |
| High vulnerability | 3.13 | 1.29–7.72 | 0.012 | 3.39 | 1.45–8.48 | 0.006 |
| Approval of drugs to enhance sex dominant | 1.51 | 0.61–3.60 | 0.361 | 2.38 | 1.10–5.31 | 0.030 |
| Condomless sex dominant | 3.08 | 1.58–6.10 | 0.001 | 1.68 | 0.93–3.06 | 0.088 |
| Observations | 371 | 371 | ||||
| R2 Tjur | 0.295 | 0.149 | ||||
Bold font indicates significant p-values
Binomial Regression Model Examining the Use of Alcohol or Drugs to Enhance Sex
Participants who reported having sex with a larger proportion of their network (OR = 3.37; 95% CI 1.05–11.28; p = 0.044), exchanging or selling sex for money, drugs, food or shelter (OR = 2.98; 95% CI 1.41–6.75; p = 0.006), and relative to the low HIV vulnerability network norm profile, being in either the moderately high HIV vulnerability network norm profile (OR = 3.47; 95% CI 1.83–6.76; p < 0.001), and high vulnerability network norm profile (OR = 3.39; 95% CI 1.45–8.48; p = 0.006), and approval of drugs to enhance sex group (OR = 2.38; 95% CI 1.08–5.12; p = 0.033), had positive and significant associations with using drugs or alcohol to enhance sex. Additional information can be found in Table 4: Model 3.
Discussion
Our study sought to identify if injunctive and descriptive social network norms would be typologized as latent profiles among Black SGM assigned male at birth, and our findings support our hypothesis. Our study found that Black SGM experienced one of five gradients of HIV risk and vulnerability within their social network sexual norm profiles: low HIV vulnerability norm, moderately high HIV vulnerability norm, high HIV vulnerability norm, approval of drug use dominant norm, and condomless sex dominant norm. Moderately high and high HIV vulnerability norm profiles were associated with condomless sex, group sex, and using drugs or alcohol to enhance sex in the past 6 months. Our findings suggest that social network norms can either exacerbate or mitigate the hazardous effects of intersectional discrimination on HIV-related outcomes.
Importantly, we found that social network norms surrounding engagement and approval of HIV sexual vulnerability behaviors were associated with individual-level sexual vulnerability to HIV. For example, Black SGM who were grouped into the higher HIV vulnerability social network norm profiles (i.e., moderately high and high) were more likely to report engaging in condomless insertive or receptive anal sex, group sex, and the use of drugs/alcohol to enhance sex in the past 6 months, relative to the low HIV vulnerability profile. As our analysis consisted of cross-sectional data, our findings can be interpreted in one of two ways. First, our findings may suggest that participants who perceive their networks to be higher in HIV vulnerability norm profiles could be engaging in higher HIV vulnerability behaviors because they believe the behavior is common. Second, our findings may suggest that participants are embedded in networks in which the norm is the acceptance of higher sexual vulnerability behaviors, and then, themselves engage in higher sexual vulnerability behaviors due to this peer influence. As our study is cross-sectional, perception of behaviors and peer influence cannot be disentangled statistically. However, participants were provided the option to indicate that they do not know if their social network alters engaged in a specific behavior or approved of the participant’s engagement in a specific behavior; thus, our study likely captures the latter option, peer influence (as they participants could indicate not knowing of descriptive norms). A future study could include a longitudinal study which collects data from sociocentric networks (i.e., entire closed networks) to assess peer influence using alter-provided data, instead of perceived data at the ego level.
Our study supports previous literature which suggests that there may be some threshold which must be reached for social network norms to be adopted by an individual (Montgomery & Chung, 1999; Valente, 1996). For example, Black SGM in the moderately high, high, and approval of drugs to enhance sex dominant HIV vulnerability network norm profiles had networks in which over 60% of their alters approved of the participant using drugs or alcohol to enhance sex—these individuals were more likely to report using drugs or alcohol to enhance sex in the past 6 months, relative to the low HIV vulnerability profile. Until health equity or supranormal efforts to increase PrEP and ART accessibility are reached in the USA, interventions to reduce HIV sexual vulnerability for Black SGM may consider network-level interventions as they may surmount structural oppression to reach health equity. Currently, HIV prevention providers and strategies are not equitably accessible to Black SGM, as suggested by research outlining racial gaps in biomedical prevention strategy uptake (Centers for Disease Control Prevention, 2021; Hess et al., 2017; Kanny et al., 2019; Matthews et al., 2016). HIV status-neutral care can also overcome intersectional discrimination faced by Black SMM and TW (Gardner et al., 2011; Myers et al., 2018). Until health equity is reached, social network interventions are needed. For example, SMM of Color were more likely to discuss PrEP and encourage PrEP use with friends they felt more emotionally close to them and interacted with them more frequently (Shrader et al., 2021b). Thus, if Black SGM do not have access to HIV prevention providers or strategies due to structural issues including intersectional discrimination, their social networks may fill this gap. In designing interventions to reduce sexual behaviors related to HIV vulnerability, it is important to consider how network norms can be changed in addition to structural barriers. The Diffusion of Innovation Theory posits that behaviors can spread throughout a network—Valente (1996) emphasized the importance of personal networks in the adoption of behaviors, with an individual’s network position in a network more important than the community’s behavioral norms (Valente & Rogers, 1995). The Diffusion of Innovations theory has also posited that mere exposure to a behavior or the absence of a behavior may be adequate enough for individuals to adopt this new behavior (Rogers & Kincaid, 1981), whereas more recent research suggests that homophily (i.e., similarities between individuals) may be critical in behavior adoption (McPherson et al., 2001). Thus, interventions should consider the utility of staff who are homophilous with the priority population on race, ethnicity, sexual orientation, and gender identity, among other characteristics.
There are generally four types of network-level interventions which can be used to elicit individual-level behavioral change: identification of network opinion leaders, segmentation (prioritizing specific groups of people through an intervention), induction (activating novel interactions between people within a network), and alteration (changing the network) (Pagkas-Bather et al., 2020, 2022; Valente, 2012). To date, there has been much research surrounding the positive effects of network-level interventions which use opinion leaders and social-networking applications to increase HIV self-testing (Huang et al., 2016; Lightfoot et al., 2018; Rosengren et al., 2016), opinion leaders and social media to increase HIV prevention information (Jaganath et al., 2012), and online social network applications to increase HIV prevention information (Tanner et al., 2018; Young, 2012; Young et al., 2014). PrEP Chicago, a social network intervention implemented among cisgender Black sexual minoritized men in Chicago, used a peer change agent approach (i.e., opinion leader workshop with telephonic booster sessions) to leverage existing social networks as pathways for HIV prevention strategy (i.e., PrEP) information diffusion, behavioral influence, social support, and empowerment (Schneider et al., 2021; Young et al., 2017). PrEP Chicago was successful in diffusing PrEP to Black SGM with high HIV susceptibility (Schneider et al., 2021). Interventions to reduce HIV vulnerability from sex can include enrolling sociocentric groups of friends to receive an intervention together (i.e., segmentation) (Kanamori et al., 2017, 2019), prioritizing behavior change in individuals who are central within a network (i.e., induction), and tailoring interventions to each network with the understanding that each individual views and responds to their network influence differently (segmentation and induction) (Dyal, 2015). Other interventions which have shown promise include the alteration or manipulation of networks; however, research such as this is sparse (Schneider et al., 2021). Future network-level interventions can consider altering networks to introduce individuals who do not engage in HIV vulnerability behaviors, removing these individuals who do engage or approve of HIV vulnerability behaviors from a network, or creating ties between network members (Kanamori et al., 2019).
Condomless insertive sex, group sex, and the use of drugs to enhance sex were higher among participants with a higher number of sexual partners and who had sex with a higher proportion of their confidant networks. This may be due to participants having more opportunities to engage in these behaviors with their network members. Alternatively, sexual network members may have a higher influence on sexual behaviors relative to social network members (Kohler et al., 2001; Marsden, 2006; Valente et al., 2013). Dynamics surrounding event-level sexual behaviors remain unclear: future prospective studies can consider the utility of ecological momentary assessments (EMA), such as a sex diary in longitudinal research to further examine this relationship (Wray et al., 2016). EMA could account for specific event-level sexual behaviors, which could vary in HIV vulnerability depending on PrEP/ART use at that time and disclosure of status or PrEP use (Algarin et al., 2022; Shrader et al., 2021a). Additionally, future network-level interventions can also focus on dyadic interventions, as HIV transmission from primary partners accounts for up to 67% of new HIV diagnoses among men who have sex with men (Hess et al., 2017; Sullivan et al., 2009), often due to a low perceived risk of HIV acquisition from primary partners (Stephenson et al., 2015). Other studies have successfully leveraged the relationship between dyads of same sex male couples to promote engagement in HIV care (Stephenson et al., 2017, 2021) and couples HIV counseling and testing and adherence to safer sexual agreements (Stephenson et al., 2022). Our sample of Black SGM’s status-neutral biomedical prevention strategy use (i.e., PrEP or ART) was not associated with condomless sex, group sex, or the use of drugs or alcohol to enhance sex. This finding contradicts the highly stigmatizing concept of “risk compensation” in which individuals are theorized to discontinue condoms or increase the number of concurrent sexual partners when they begin PrEP or ART use (Pasipanodya et al., 2020) and supports those studies which find that PrEP use does not influence the discontinuation of condom use (Algarin et al., 2022; Goodman-Meza et al., 2019). HIV prevention researchers and healthcare providers can continue supporting Black SGM’s PrEP and ART use in a stigma-free manner, having established that PrEP and ART were not found to be associated with condomless sex, group sex, or the use of drugs or alcohol to enhance sex (Rojas Castro et al., 2019).
Although Black SMM and TW are oftentimes clustered into a homogenous group, our findings distinguish important considerations related to gender, sexual identity, income, and sex work when examining HIV-vulnerability related outcomes (Duncan et al., 2020). As aforementioned, HIV prevention interventions must consider addressing inequities in power and privilege to ensure that the comprehensive needs of Black SGM are addressed by meeting Black SGM where they are at by addressing basic needs first, and then addressing the individual’s unique HIV prevention needs. For example, considering the high rate of housing instability in our sample (31%), participants may be engaging in sex work to have their basic needs met. Previous interventions which have successfully done this include strengths-based case management such as ARTAS (Craw et al., 2008; Gardner et al., 2007, 2009) and ASK-PrEP (Ogunbajo et al., 2021; Reback et al., 2019), and client-centered care coordination (C4) models (Nelson et al., 2022; Whitfield et al., 2022). These interventions have a strong peer advocate and service navigation component—supporting the utility of network-based peer interventions. Future qualitative research can aim to explore opportunities to incorporate harm reduction strategies during sex work or the use of drugs to enhance sex.
Limitations
This study had several limitations that are important to note. First, we used convenience and peer referral to recruit participants. Thus, participants may also be present in other participants’ social networks. These sampling procedures can introduce dependencies within the data; however, because this was not a true respondent-driven sampling study, we did not use an estimator to adjust for any potential dependencies. As is typical with social network studies, our findings are not generalizable. Additionally, our data were self-reported by participants and collected by an interview-administered egocentric inventory. For this, our participants may incorrectly perceive the behaviors of others within their networks by overestimating their network members’ behaviors towards their own behaviors. Because the egocentric network inventories may not be as accurate as if other members of the participants’ social networks were assessed (Berkowitz, 2005; Lapinski & Rimal, 2005; Miller & McFarland, 1991), there may have been biases within our data. To address this, we included a “I don’t know” option so that participants are not forced into guessing their network members’ behaviors. In addition, participants may have been subject to recall bias due to the retrospective nature of this study and social desirability bias due to the sensitive nature of the questions. Further, we did not define the different experiences of transgender participants in our study: this may have resulted in less nuanced results and disguised important differences between people with differing gender identities. Finally, despite conducting several analyses, we did not correct for multiple comparisons, which may have increased the family-wise error rate and false discovery rate.
Supplementary Material
Public Health Implications.
As discrimination from racism, homophobia, and transphobia can intersect and compound to form a new type of discrimination, this may exacerbate racial, ethnic, and sexual minority health disparities, and disrupt HIV status neutral care equity (Duncan et al., 2020). This necessitates behavioral strategies such as the use of condoms, especially when engaging in group sex and drug use during sex, to reduce HIV transmission among Black SGM until PrEP and ART roll-out can be equitably accessed by Black SGM. By using a person-centered approach to construct social network HIV risk profiles, and identifying correlates of engaging in condomless sex, group sex, and the use of drugs/alcohol to enhance sex, our study demonstrated the importance of social network norms and socioecological context in individual-level HIV sexual vulnerability. In addition, as social network norms are an important convention in daily decision making, networks are also an opportunity to intervene. HIV prevention interventions for Black SGM many consider the enrollment of entire social networks, such as groups of friends, or perhaps intervene on specific members within social networks with high social influence or who may be late adopters for maximum impact. Thus, developing community-centered social network HIV prevention interventions, which focus on the reduction in sexual behaviors associated with HIV vulnerability, may be an effective approach to limiting HIV incidence in this community until biomedical prevention strategies are equitably available.
Acknowledgements
The Neighborhoods and Networks (N2) Cohort Study is funded through grants from the National Institute on Mental Health (Grant Number: R01MH112406; Principal Investigators: Dustin T. Duncan, ScD and John A. Schneider, MD, MPH) and a cooperative agreement with the Centers for Disease Control and Prevention under the Minority HIV/AIDS Research Initiative (Grant Number: U01PS005122; Principal Investigator: Dustin T. Duncan, ScD). The University of Chicago authors were supported in part by the National Institute on Drug Abuse (U2C DA050098). We thank the participants for engaging in this research. We would like to thank the CCHE services team for provision of testing, resource counseling, mental health and other health care services for study participants as part of the South Side Health Home (S2H2).
Funding
All authors report support from the National Institute on Mental Health (R01MH112406, PI: Duncan and Schneider), the Centers for Disease Control and Prevention under the Minority HIV/AIDS Research Initiative (U01PS005122, PI: Duncan). CS’s efforts were supported by the National Institute on Drug Abuse (R25DA026401; P30DA011041) and, along with JR, the National Institute of Allergy and Infectious Diseases (T32AI114398; PI: Howard). YC and JS were supporting by the National Institute on Drug Abuse (R03DA053161, PI: Chen and Schneider). RD’s efforts were supported by the National Institute of Mental Health (T32MH019139, PI: Sandfort). JK’s effort on this project was funded by NIH grants K01AA028199, R01DA054553, and R21DA053156. RM was supported by the National Institute on Drug Abuse (T32DA031099, PI: Hasin) and a grant from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention to the Center for Injury Epidemiology and Prevention at Columbia University (R49CE003096, PI: Branas). The University of Chicago authors were supported in part by the National Institute on Drug Abuse (U2CDA050098, PI: Schneider). We thank the participants for engaging in this research.
Footnotes
Declarations
Conflict of interest The authors declare that they have no conflicts of interests or competing interests.
Ethical Approval Columbia University (#AAAS7654) and the University of Chicago (IRB16-1419) provided ethical approval for this study.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s10508-023-02555-0.
Availability of Data and Material The data can be made available on a case-by-case basis upon written request to the senior author.
Code Availability The code can be made available on a case-by-case basis upon written request to the first author.
References
- Akaike H (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19(6), 716–723. 10.1109/TAC.1974.1100705 [DOI] [Google Scholar]
- Algarin AB, Shrader CH, Hackworth BT, & Ibanez GE (2022). Condom use likelihood within the context of PrEP and TasP among men who have sex with men in Florida: A short report. AIDS Care, 34(3), 294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold EA, & Bailey MM (2009). Constructing home and family: How the ballroom community supports African American GLBTQ youth in the face of HIV/AIDS. Journal of Gay & Lesbian Social Services, 21(2–3), 171–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold EA, Rebchook GM, & Kegeles SM (2014). ‘Triply cursed’: Racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Culture, Health & Sexuality, 16(6), 710–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology, 52(1), 1–26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- Bandura A, & Walters RH (1977). Social learning theory (Vol. 1). Englewood Cliffs: Prentice Hall. [Google Scholar]
- Bandura A (1994). Social cognitive theory and exercise of control over HIV infection. In DiClemente RJ & Peterson JL (Eds.), Preventing AIDS: Theories and methods of behavioral interventions (pp. 25–59). Springer. [Google Scholar]
- Baral S, Logie CH, Grosso A, Wirtz AL, & Beyrer C (2013). Modified social ecological model: A tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health, 13(1), 482. 10.1186/1471-2458-13-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer GR (2014). Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine (1982), 110, 10–17. 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Baumeister RF, & Vohs KD (2007). Encyclopedia of social psychology. Sage Publications, Inc. 10.4135/9781412956253 [DOI] [Google Scholar]
- Berkowitz AD (2005). An overview of the social norms approach. In Lederman L, Stewart L, Goodhart F & Laitman L (Eds.), Changing the culture of college drinking: A socially situated health communication campaign (pp. 193–214). Hampton Press. [Google Scholar]
- Bohnert AS, German D, Knowlton AR, & Latkin CA (2010). Friendship networks of inner-city adults: A latent class analysis and multi-level regression of supporter types and the association of supporter latent class membership with supporter and recipient drug use. Drug and Alcohol Dependence, 107(2–3), 134–140. 10.1016/j.drugalcdep.2009.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2008). When Black+ lesbian+ woman≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles, 59(5), 312–325. [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality—An important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2013). “Once you’ve blended the cake, you can’t take the parts back to the main ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles, 68(11), 754–767. [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. [Google Scholar]
- Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, & Mayer KH (2017). Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care, 29(11), 1351–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callander D, Duncan D, Park SH, Bowleg L, Brinkley-Rubinstein L, Theall K, & Hickson D (2019). P559 Incarceration, stress and sexual risk-taking: An intersectional analysis of black men who have sex with men in the deep south. Sexually Transmitted Infections, 95(Suppl 1), A252. [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13(2), 195–212. 10.1007/BF01246098 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2021). HIV Surveillance Report, 2019; vol 32. Retrieved Dec 10 from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-32.pdf [Google Scholar]
- Centers for Disease Control Prevention. (2021). HIV infection, risk, prevention and testing behaviors among transgender women—National HIV behavioral surveillance, 7 US cities, 2019–2020. HIV Surveillance Special Reports, 27, 15. [Google Scholar]
- Cialdini RB, Reno RR, & Kallgren CA (1990). A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology, 58(6), 1015–1026. [Google Scholar]
- Craw JA, Gardner LI, Marks G, Rapp RC, Bosshart J, Duffus WA, Rossman A, Coughlin SL, Gruber D, & Safford LA (2008). Brief strengths-based case management promotes entry into HIV medical care: Results of the antiretroviral treatment access study-II. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47(5), 597–606. [DOI] [PubMed] [Google Scholar]
- Crenshaw KW (2017). On intersectionality: Essential writings. The New Press. [Google Scholar]
- Dangerfield DT, Carmack CC, Gilreath TD, & Duncan DT (2018). Latent classes of sexual positioning practices and sexual risk among men who have sex with men in Paris, France. AIDS and Behavior, 22(12), 4001–4008. 10.1007/s10461-018-2267-2 [DOI] [PubMed] [Google Scholar]
- De P, Cox J, Boivin JF, Platt RW, & Jolly AM (2007). The importance of social networks in their association to drug equipment sharing among injection drug users: A review. Addiction, 102(11), 1730–1739. 10.1111/j.1360-0443.2007.01936.x [DOI] [PubMed] [Google Scholar]
- Dearing JW, Meyer G, & Rogers EM (1994). Diffusion theory and HIV risk behavior change. In DiClemente RJ & Peterson JL (Eds.), Preventing AIDS: Theories and methods of behavioral interventions (pp. 79–93). Springer. [Google Scholar]
- De Santis JP (2009). HIV infection risk factors among male-to-female transgender persons: A review of the literature. The Journal of the Association of Nurses in AIDS Care: JANAC, 20(5), 362–372. 10.1016/j.jana.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Duncan DT, Callander D, Bowleg L, Park SH, Brinkley-Rubinstein L, Theall KP, & Hickson DA (2020). Intersectional analysis of life stress, incarceration and sexual health risk practices among cisgender Black gay, bisexual and other men who have sex with men in the Deep South of the US: The MARI Study. Sexual Health, 17(1), 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Hickson DA, Goedel WC, Callander D, Brooks B, Chen Y-T, Hanson H, Eavou R, Khanna AS, & Chaix B (2019). The social context of HIV prevention and care among black men who have sex with men in three US Cities: The neighborhoods and networks (N2) cohort study. International Journal of Environmental Research and Public Health, 16(11), 1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Ransome Y, Park SH, Jackson SD, Kawachi I, Branas CC, Knox J, Al-Ajlouni YA, Mountcastle H, & Miles CH (2021). Neighborhood social cohesion, religious participation and sexual risk behaviors among cisgender black sexual minority men in the southern United States. Social Science & Medicine, 279, 113913. 10.1016/j.socscimed.2021.113913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyal SR (2015). Network influences on behavior: A summary of Tom Valente’s keynote address at Sunbelt XXXV: The Annual Meeting International Network for Social Network Analysis. Connect, 35(2), 52–57. 10.17266/35.2.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Carter JA, Forbes N, Bowleg L, Malebranche DJ, Talan AJ, & Rendina HJ (2020). Intersectional discrimination, positive feelings, and health indicators among Black sexual minority men. Health Psychology, 39(3), 220–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feelemyer J, Duncan DT, Dyer TV, Geller A, Scheidell JD, Young KE, Cleland CM, Turpin RE, Brewer RA, & Hucks-Ortiz C (2021). Longitudinal associations between police harassment and experiences of violence among Black men who have sex with men in six US cities: The HPTN 061 Study. Journal of Urban Health, 98(2), 172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Bolyard M, Khan M, Maslow C, Sandoval M, Mateu-Gelabert P, Krauss B, & Aral SO (2008). Group sex events and HIV/STI risk in an urban network. Journal of Acquired Immune Deficiency Syndromes, 49(4), 440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner LI, Marks G, Craw J, Metsch L, Strathdee S, Anderson-Mahoney P, & del Rio C (2009). Demographic, psychological, and behavioral modifiers of the Antiretroviral Treatment Access Study (ARTAS) intervention. AIDS Patient Care and STDs, 23(9), 735–742. [DOI] [PubMed] [Google Scholar]
- Gardner LI, Marks G, Metsch LR, Loughlin AM, O’Daniels C, Del Rio C, Anderson-Mahoney P, Wilkinson JD, & Group AS (2007). Psychological and behavioral correlates of entering care for HIV infection: The Antiretroviral Treatment Access Study (ARTAS). AIDS Patient Care and STDs, 21(6), 418–425. [DOI] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, & Burman WJ (2011). The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases, 52(6), 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman-Meza D, Beymer MR, Kofron RM, Amico KR, Psaros C, Bushman LR, Anderson PL, Bolan R, Jordan WC, & Rooney JF (2019). Effective use of pre-exposure prophylaxis (PrEP) Among stimulant users with multiple condomless sex partners: A longitudinal study of men who have sex with men in Los Angeles. AIDS Care, 31(10), 1228–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Wolitski RJ, & Millett GA (2013). A holistic approach to addressing HIV infection disparities in gay, bisexual, and other men who have sex with men. American Psychologist, 68(4), 261–273. [DOI] [PubMed] [Google Scholar]
- Hess KL, Hu X, Lansky A, Mermin J, & Hall HI (2017). Life-time risk of a diagnosis of HIV infection in the United States. Annals of Epidemiology, 27(4), 238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway IW, Pulsipher CA, Gibbs J, Barman-Adhikari A, & Rice E (2015). Network influences on the sexual risk behaviors of gay, bisexual and other men who have sex with men using geosocial networking applications. AIDS and Behavior, 19(2), 112–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang E, Marlin RW, Young SD, Medline A, & Klausner JD (2016). Using grindr, a smartphone social-networking application, to increase HIV self-testing among Black and Latino men who have sex with men in Los Angeles, 2014. AIDS Education and Prevention, 28(4), 341–350. 10.1521/aeap.2016.28.4.341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaganath D, Gill HK, Cohen AC, & Young SD (2012). Harnessing online peer education (HOPE): Integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care, 24(5), 593–600. 10.1080/09540121.2011.630355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janulis P, Feinstein BA, Phillips G, Newcomb ME, Birkett M, & Mustanski B (2018). Sexual partner typologies and the association between drug use and sexual risk behavior among young men who have sex with men. Archives of Sexual Behavior, 47(1), 259–271. 10.1007/s10508-016-0909-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung T, & Wickrama KA (2008). An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass, 2(1), 302–317. [Google Scholar]
- Kanamori M, De La Rosa M, Diez S, Weissman J, Trepka MJ, Sneij A, Schmidt P, & Rojas P (2017). Lessons learned and preliminary findings of Progreso en Salud, an HIV risk reduction intervention for Latina seasonal farmworkers. International Journal of Environmental Research and Public Health, 14(1), 32. 10.3390/ijerph14010032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanamori M, De La Rosa M, Shrader C-H, Munayco C, Doblecki-Lewis S, Prado G, Safren S, Trepka MJ, & Fujimoto K (2019). Progreso en Salud: Findings from two adapted social network HIV risk reduction interventions for Latina seasonal workers. International Journal of Environmental Research and Public Health, 16(22), 4530. 10.3390/ijerph16224530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanny D, Jeffries WL IV., Chapin-Bardales J, Denning P, Cha S, Finlayson T, Wejnert C, Abrego M, Al-Tayyib A, & Anderson B (2019). Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. Morbidity and Mortality Weekly Report, 68(37), 801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kincaid DL (2004). From innovation to social norm: Bounded normative influence. Journal of Health Communication, 9(S1), 37–57. [DOI] [PubMed] [Google Scholar]
- Kohler H-P, Behrman JR, & Watkins SC (2001). The density of social networks and fertility decisions: Evidence from South Nyanza District, Kenya. Demography, 38(1), 43–58. [DOI] [PubMed] [Google Scholar]
- Lapinski MK, & Rimal RN (2005). An explication of social norms. Communication Theory, 15(2), 127–147. [Google Scholar]
- Latkin CA, Forman V, Knowlton A, & Sherman S (2003). Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Social Science & Medicine, 56(3), 465–476. 10.1016/S0277-9536(02)00047-3 [DOI] [PubMed] [Google Scholar]
- Latkin C, Kuramoto S, Davey-Rothwell M, & Tobin K (2010). Social norms, social networks, and HIV risk behavior among injection drug users. AIDS and Behavior, 14(5), 1159–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightfoot MA, Campbell CK, Moss N, Treves-Kagan S, Agnew E, Kang Dufour MS, Scott H, Saʼid AM, & Lippman SA (2018). Using a social network strategy to distribute HIV self-test kits to African American and Latino MSM. JAIDS Journal of Acquired Immune Deficiency Syndromes, 79(1), 38–45. 10.1097/qai.0000000000001726 [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Marsden PV (2006). Network methods in social epidemiology. Methods in Social Epidemiology, 109, 186–204. [Google Scholar]
- Matthews DD, Herrick AL, Coulter RWS, Friedman MR, Mills TC, Eaton LA, Wilson PA, Stall RD, & The PST (2016). Running backwards: Consequences of current HIV incidence rates for the next generation of black MSM in the United States. AIDS and Behavior, 20(1), 7–16. 10.1007/s10461-015-1158-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, & Holtgrave D (2014). HIV among black men who have sex with men (MSM) in the United States: A review of the literature. AIDS and Behavior, 18(1), 10–25. 10.1007/s10461-013-0476-2 [DOI] [PubMed] [Google Scholar]
- McLachlan GJ, & Peel D (2004). Finite mixture models. Wiley. [Google Scholar]
- McPherson M, Smith-Lovin L, & Cook JM (2001). Birds of a feather: Homophily in social networks. Annual Review of Sociology, 27, 415–444. [Google Scholar]
- Miller M, Serner M, & Wagner M (2005). Sexual diversity among black men who have sex with men in an inner-city community. Journal of Urban Health, 82(1 Suppl 1), i26–34. 10.1093/jurban/jti021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DT, & McFarland C (1991). When social comparison goes awry: The case of pluralistic ignorance. In Suls J & Wills TA (Eds.), Social comparison: Contemporary theory and research (pp. 287–313). Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Millett GA, Flores SA, Peterson JL, & Bakeman R (2007). Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS, 21(15), 2083–2091. [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL 4th., Wilson PA, Rourke SB, Heilig CM, Elford J, & Fenton KA (2012). Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. The Lancet, 380(9839), 341–348. [DOI] [PubMed] [Google Scholar]
- Montgomery MR, & Chung W (1999). Social networks and the diffusion of fertility control in the Republic of Korea. Dynamics of Values in Fertility Change, 179–209. [Google Scholar]
- Morgan E, Skaathun B, Michaels S, Young L, Khanna A, Friedman SR, Davis B, Pitrak D, Schneider J, & The UST (2016). Marijuana use as a sex-drug is associated with HIV risk among black MSM and their network. AIDS and Behavior, 20(3), 600–607. 10.1007/s10461-015-1195-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrill CS, Liu KL, Guilin V, Colón ER, Dean L, Buckley LA, Sanchez T, Finlayson TJ, & Torian LV (2008). HIV prevalence and associated risk behaviors in New York City’s house ball community. American Journal of Public Health, 98(6), 1074–1080. 10.2105/ajph.2006.108936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers JE, Braunstein SL, Xia Q, Scanlin K, Edelstein Z, Harriman G, Tsoi B, Andaluz A, Yu E, & Daskalakis D (2018). Redefining prevention and care: A status-neutral approach to HIV. Open Forum Infectious Diseases. 10.1093/ofid/ofy097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson LE, Wilton L, Whitfield DL, Williams GC, Mayer KH, Komárek A, Boyd DT, Beauchamp G, Fields SD, & Wheeler DP (2022). Client-centered care coordination (C4™) for HIV/STI prevention: A theoretical, conceptual, and methodological overview—HIV Preventions Trials Network (HPTN) 073. Sexuality Research and Social Policy, 19, 1365–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunbajo A, Storholm ED, Ober AJ, Bogart LM, Reback CJ, Flynn R, Lyman P, & Morris S (2021). Multilevel barriers to HIV PrEP uptake and adherence among black and Hispanic/ Latinx transgender women in southern California. AIDS and Behavior, 25(7), 2301–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Nemoto T, Iwamoto M, & Moore T (2011). Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS and Behavior, 15(3), 674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagkas-Bather J, Brewer R, & Bouris A (2022). Status-neutral interventions to support health equity for black sexual minority men. Current HIV/AIDS Reports, 19(4), 265–280. 10.1007/s11904-022-00610-4 [DOI] [PubMed] [Google Scholar]
- Pagkas-Bather J, Young LE, Chen Y-T, & Schneider JA (2020). Social network interventions for HIV transmission elimination. Current HIV/AIDS Reports, 17(5), 450–457. 10.1007/s11904-020-00524-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasipanodya EC, Li MJ, Jain S, Sun X, Tobin J, Ellorin E, Dube M, Daar ES, Corado K, Milam J, Blumenthal J, Morris SH, Moore DJ, & the California Collaborative Treatment, G. (2020). Greater levels of self-reported adherence to pre-exposure prophylaxis (PrEP) are associated with increased condomless sex among men who have sex with men. AIDS and Behavior, 24(11), 3192–3204. 10.1007/s10461-020-02881-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastor DA, Barron KE, Miller BJ, & Davis SL (2007). A latent profile analysis of college students’ achievement goal orientation. Contemporary Educational Psychology, 32(1), 8–47. 10.1016/j.cedpsych.2006.10.003 [DOI] [Google Scholar]
- Phillips G, Peterson J, Binson D, Hidalgo J, Magnus M, & Group YOCSIS (2011). House/ball culture and adolescent African-American transgender persons and men who have sex with men: A synthesis of the literature. AIDS Care, 23(4), 515–520. [DOI] [PubMed] [Google Scholar]
- Prestage GP, Hudson J, Down I, Bradley J, Corrigan N, Hurley M, Grulich AE, & McInnes D (2009). Gay men who engage in group sex are at increased risk of HIV infection and onward transmission. AIDS and Behavior, 13(4), 724–730. [DOI] [PubMed] [Google Scholar]
- Purdie-Vaughns V, & Eibach RP (2008). Intersectional invisibility: The distinctive advantages and disadvantages of multiple subordinate-group identities. Sex Roles, 59(5), 377–391. [Google Scholar]
- Quinn K, Bowleg L, & Dickson-Gomez J (2019). “The fear of being Black plus the fear of being gay”: The effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Social Science & Medicine, 232, 86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Clark KA, Rünger D, & Fehrenbacher AE (2019). A promising PrEP navigation intervention for transgender women and men who have sex with men experiencing multiple syndemic health disparities. Journal of Community Health, 44(6), 1193–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM, & Kincaid DL (1981). Communication networks: Toward a new paradigm for research. Free Press. [Google Scholar]
- Rojas Castro D, Delabre RM, & Molina JM (2019). Give PrEP a chance: Moving on from the “risk compensation” concept. Journal of the International AIDS Society, 22, e25351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren AL, Huang E, Daniels J, Young SD, Marlin RW, & Klausner JD (2016). Feasibility of using Grindr(TM) to distribute HIV self-test kits to men who have sex with men in Los Angeles, California. Sexual Health, 13, 389–392. 10.1071/SH15236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rössler P (2017). The international encyclopedia of media effects, 4 volume set. Wiley. [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, & Friedman S (2013). Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. American Journal of Public Health, 103(1), e28–e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider J, Michaels S, & Bouris A (2012). Family network proportion and HIV risk among black men who have sex with men. Journal of Acquired Immune Deficiency Syndromes (1999), 61(5), 627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JA, Young L, Ramachandran A, Michaels S, Cohen H, Robinson I, Alon L, Hill B, Nakasone S, Balenciaga M, Motley D, Bouris A, Khanna A, Ferreira M, Valente T, & Schumm P (2021). A pragmatic randomized controlled trial to increase PrEP uptake for HIV prevention: 55-week results from PrEPChicago. Journal of Acquired Immune Deficiency Syndromes, 86(1), 31–37. 10.1097/qai.0000000000002518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. 10.1214/aos/1176344136 [DOI] [Google Scholar]
- Sheehan DM, Miller RP, Trepka MJ, Smith LR, & Latkin C (2019). Role of social network sexual norms and behaviors on the HIV sexual risk behaviors of people who inject drugs in HPTN 037. AIDS and Behavior, 23(6), 1604–1611. 10.1007/s10461-019-02409-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrader C-H, Arroyo-Flores J, Skvoretz J, Fallon S, Gonzalez V, Safren S, Algarin A, Johnson A, Doblecki-Lewis S, & Kanamori M (2021a). PrEP use and PrEP use disclosure are associated with condom use during sex: A multilevel analysis of Latino MSM egocentric sexual networks. AIDS and Behavior, 25(5), 1636–1645. 10.1007/s10461-020-03080-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrader C-H, Arroyo-Flores J, Stoler J, Skvoretz J, Carrico A, Doblecki-Lewis S, & Kanamori M (2021b). The association between social and spatial closeness with PrEP conversations among Latino men who have sex with men. JAIDS Journal of Acquired Immune Deficiency Syndromes, 88(4), 366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Garofalo R, Sullivan PS, Hidalgo MA, Bazzi AR, Hoehnle S, Bratcher A, Finneran CA, & Mimiaga MJ (2021). Stronger Together: Results from a randomized controlled efficacy trial of a dyadic intervention to improve engagement in HIV care among serodiscordant male couples in three US cities. AIDS and Behavior, 25(8), 2369–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Suarez NA, Garofalo R, Hidalgo MA, Hoehnle S, Thai J, Mimiaga MJ, Brown E, Bratcher A, & Wimbly T (2017). Project Stronger Together: Protocol to test a dyadic intervention to improve engagement in HIV care among serodiscordant male couples in three US cities. JMIR Research Protocols, 6(8), e7884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Sullivan SP, Mitchell JW, Johnson BA, & Sullvian PS (2022). Efficacy of a telehealth delivered couples’ HIV counseling and testing (CHTC) intervention to improve formation and adherence to safer sexual agreements among male couples in the US: Results from a randomized control trial. AIDS and Behavior, 26(8), 2813–2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, White D, Darbes L, Hoff C, & Sullivan P (2015). HIV testing behaviors and perceptions of risk of HIV infection among MSM with main partners. AIDS and Behavior, 19(3), 553–560. 10.1007/s10461-014-0862-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, & Sanchez TH (2009). Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS, 23(9), 1153–1162. 10.1097/QAD.0b013e32832baa34 [DOI] [PubMed] [Google Scholar]
- Tanner AE, Song EY, Mann-Jackson L, Alonzo J, Schafer K, Ware S, Garcia JM, Arellano Hall E, Bell JC, Van Dam CN, & Rhodes SD (2018). Preliminary impact of the weCare social media intervention to support health for young men who have sex with men and transgender women with HIV. AIDS Patient Care and STDs, 32(11), 450–458. 10.1089/apc.2018.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, & Latkin CA (2008). An examination of social network characteristics of men who have sex with men who use drugs. Sexually Transmitted Infections, 84(6), 420–424. 10.1136/sti.2008.031591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW (1996). Social network thresholds in the diffusion of innovations. Social Networks, 18(1), 69–89. [Google Scholar]
- Valente TW (2012). Network interventions. Science, 337(6090), 49–53. 10.1126/science.1217330 [DOI] [PubMed] [Google Scholar]
- Valente TW, Fujimoto K, Soto D, Ritt-Olson A, & Unger JB (2013). A comparison of peer influence measures as predictors of smoking among predominately Hispanic/Latino high school adolescents. Journal of Adolescent Health, 52(3), 358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW, & Rogers EM (1995). The origins and development of the diffusion of innovations paradigm as an example of scientific growth. Science Communication, 16(3), 242–273. 10.1177/1075547095016003002 [DOI] [PubMed] [Google Scholar]
- Wang W, & Muessig KE (2017). Social network correlates of HIV risk-related behaviors among male migrants in China. BMC Public Health, 17(1), 459. 10.1186/s12889-017-4409-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington TA, Brocato J, Applewhite S, Dyson YD, & Ramos A (2021). Alcohol and condomless insertive anal intercourse among Black/Latino sexual-minority male non-PrEP users. Urban Social Work, 5(1), 43–59. [Google Scholar]
- Whitfield DL, Nelson LE, Komárek A, Turner D, Ni Z, Boyd DT, Taggart T, Ramos SR, Wilton L, & Beauchamp GG (2022). Implementation of client-centered care coordination for HIV prevention with black men who have sex with men: Activities, personnel costs, and outcomes—HPTN 073. Journal of Racial and Ethnic Health Disparities, 10, 183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson ASP, & Urick A (2022). An intersectional examination of the opportunity gap in science: A critical quantitative approach to latent class analysis. Social Science Research, 102, 102645. 10.1016/j.ssresearch.2021.102645 [DOI] [PubMed] [Google Scholar]
- Wray TB, Kahler CW, & Monti PM (2016). Using ecological momentary assessment (EMA) to study sex events among very high-risk men who have sex with men (MSM). AIDS and Behavior, 20(10), 2231–2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SD (2012). Analysis of online social networking peer health educators. Annual Review of Cybertherapy and Telemedicine, 181, 253–259. [PubMed] [Google Scholar]
- Young SD, Holloway I, Jaganath D, Rice E, Westmoreland D, & Coates T (2014). Project HOPE: Online social network changes in an HIV prevention randomized controlled trial for African American and Latino men who have sex with men. American Journal of Public Health, 104(9), 1707–1712. 10.2105/ajph.2014.301992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young LE, Schumm P, Alon L, Bouris A, Ferreira M, Hill B, Khanna AS, Valente TW, & Schneider JA (2017). PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clinical Trials, 15(1), 44–52. 10.1177/1740774517730012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


