Abstract
Certain dental procedures produce high levels of aerosols containing pathogenic microorganisms, posing a risk for the transmission of infections in dental settings. This study aimed to assess the effectiveness of various aerosol mitigation interventions during clinical dental procedures in real-world environments. A systematic literature search was conducted in PubMed/MEDLINE, Scopus, Web of Science, and Embase for English studies up to March 2023 according to the PRISMA guidelines. Only peer-reviewed controlled clinical trials (CCT) or randomized controlled trials (RCT) studies involving human subjects were included. The risk of bias of selected researches were evaluated by two independent authors using the Cochrane Collaboration tool. The literature search yielded 3491 articles, of which 42 studies met the inclusion criteria and were included in this study. Most studies evaluated bacterial contamination in bio-aerosols, while the viral and fungal contamination was assessed in only three studies. Overall, various approaches have been applied in reducing aerosol contamination in clinical scenarios, including high-volume evacuators (HVE), mouse rinses and rubber dams, air cleaning systems, and high-efficiency particulate air (HEPA) filters. The available evidence suggests that various aerosol mitigation strategies could be implemented to decrease the risk of cross-infection during clinical dental procedures in real-world environments. However, further clinical trials are necessary to establish statistical validity in measuring aerosol contamination and mitigation, as well as to evaluate the risk of infection transmission for viral and fungal contamination.
Keywords: Aerosol contamination, Aerosol mitigation, Dental environments, Acute respiratory syndrome coronavirus
1. Introduction
The production of aerosols in dental clinics is a significant health concern, as these aerosols generated during dental procedures may contain harmful viral, bacterial, and fungal organisms (Meng et al., 2020, Mosaddad et al., 2019). Aerosol-generating procedures (AGPs), including ultrasonic scalers, air abrasion, polishing teeth, opening teeth for drainage, cementation of fixed prosthesis, placement of dental implant, and tooth extraction, are commonly used in dental practice. An aerosol is defined as a suspension of solid or liquid particles in the air, consisting of droplet nuclei less than 5 μm in diameter, which could remain suspended in the air and be transported by air currents (Tellier, 2009, Judson and Munster, 2019). Aerosols created with liquids produce a wide range of droplet sizes. Studies have shown that droplets (particulate matter greater than 5 µm) generated by AGPs usually fall quickly within 1 m of the source as a splatter. In contrast, aerosols generated during AGPs can remain suspended for a prolonged period and spread over a distance of up to 1.8 m (Jones and Brosseau, 2015, Leggat and Kedjarune, 2001).
It has been three years since the Coronavirus Disease 2019 (COVID-19) was declared by the World Health Organization (WHO) as a global pandemic (LaCaille et al., 2021). Furthermore, the emergence and rapid spread of the Omicron variant have raised greater public health concerns worldwide (Karim and Karim, 2021). The oral cavity contains over 700 microbial species, including the highly infectious SARS-CoV-2, which can be spread through AGPs, posing a risk of infection transmission in dental clinics where close contact occurs between patients and dental healthcare providers (To et al., 2020). The COVID-19 pandemic increased public concerns in terms of the level of aerosol contamination in dental environments with the spread of the virus between dentists and patients. Because of concerns about the spread of COVID-19, patients may be in pain but in fear of attending for urgent treatment, leading to delayed treatment and exacerbation of non-urgent problems. In addition, dental professionals in many countries have restricted or even stopped routine care because of regulatory restrictions and fear of spreading COVID-19 in clinical practice.
Since preventing aerosol transmission has been a long-standing concern in the dental community, multiple precautions have been standard practiced during the clinical practice of dentistry (Harrel and Molinari, 2004). Based on evidence-informed infection control, the layering of infection control steps reduces risk with the ultimate aim of breaking the transmission chain, preventing cross-infection, and ensuring safe and effective dental practice. Potential aerosol mitigation strategies, including rubber dam isolation, HVE, HEPA filters, anti-suction turbine handpieces, UV lights, mouth rinses before dental procedures, and appropriate application of personal protective equipment by dentists have been proposed in the literature based on data derived from mannequin experiments (Eliades and Koletsi, 2020, Hallier et al., 2010). Findings demonstrated a significant reduction in the level of hazardous aerosols generated during dental procedures after using the approaches mentioned above.
Several studies have systematically summarized certain aerosol mitigation strategies in specific conditions. For instance, a previous study assessed the generation of splatter and aerosol using rotary handpieces and concluded that high-speed handpieces displayed higher aerosol contamination than low-speed ones (Al-Yaseen et al., 2022). Another study investigated the efficacy of pre-procedural mouth rinses and indicated that pre-procedural mouth rinses could be a promising measure in reducing the number of microorganisms in the dental environment (Marui et al., 2019). In addition, a previous review summarized the current evidence of interventions in reducing aerosolized microbes in the clinical practice of dentistry (Koletsi et al., 2020). However, none of them separated experimental and clinical studies and systematically evaluated the effectiveness of aerosol mitigation strategies in real-world dental environments. Nevertheless, clinical trials need to be addressed before the strategies mentioned above can be put into real-world applications.
It is therefore crucial for dentists to adopt best practices in reducing the risk of infectious diseases spreading through aerosols during the COVID-19 pandemic by evaluating the effectiveness of aerosol mitigation interventions in real-world dental environments. Accordingly, this study aimed to conduct a comprehensive evaluation of the effectiveness of aerosol mitigation interventions used to reduce contamination in aerosols during dental practice in real-world environments.
2. Materials and methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement and registered in the International Prospective Register of Systematic Reviews under registration number CRD42022382985 (Moher et al., 2015). As this study did not involve human or animal subjects, ethics approval was not required.
The question of this study was established according to the PICO framework, with (P) representing the participants, (I) indicating the intervention, (C) representing the comparison, and (O) standing for the outcome (Schardt et al., 2007). Do various aerosol mitigation interventions (I) result in effective reduction (percentage reduction or colony-forming units) in volume and level of contaminated aerosols (O) for patients and dental health providers undergoing AGPs in a dental environment? (P) In addition, the costs for the aerosol mitigation interventions and the acceptability and feasibility of the intervention to dental healthcare providers and their patients were also measured. Results from selected studies were to be compared (C) to participants who did not receive aerosol mitigation strategies.
2.1. Search strategy
A detailed literature search in PubMed/MEDLINE, Scopus, Web of Science, and Embase was performed according to the PRISMA guidelines for peer-reviewed studies published until March 2023. The search terms were predetermined and related to aerosol generation and mitigation strategies in the dental environment. Table 1 presents the specific search strategies utilized for each database. Gray literature was searched in the ClinicalTrials.gov and Open Access Theses and Dissertations. In addition, the electronic search of the databases was complemented by a manual search in reference lists of chosen articles to improve completeness.
Table 1.
Electronic databases used and search strategies.
| Database | Search strategy |
|---|---|
| MEDLINE/PubMed | (“aerosol s”[All Fields] OR “aerosolic”[All Fields] OR “aerosolization”[All Fields] OR “aerosolizations”[All Fields] OR “aerosolize”[All Fields] OR “aerosolized”[All Fields] OR “aerosolizer”[All Fields] OR “aerosolizes”[All Fields] OR “aerosolizing”[All Fields] OR “aerosols”[MeSH Terms] OR “aerosols”[All Fields] OR “aerosol”[All Fields] OR “bio-aerosol”[All Fields] OR (“emission”[All Fields] OR “emission s”[All Fields] OR “emissions”[All Fields] OR “emissive”[All Fields]) OR (“air pollution”[MeSH Terms] OR (“air”[All Fields] AND “pollution”[All Fields]) OR “air pollution”[All Fields])) AND (“dental health services”[MeSH Terms] OR (“dental”[All Fields] AND “health”[All Fields] AND “services”[All Fields]) OR “dental health services”[All Fields] OR “dental”[All Fields] OR “dentally”[All Fields] OR “dentals”[All Fields] OR (“dentist s”[All Fields] OR “dentists”[MeSH Terms] OR “dentists”[All Fields] OR “dentist”[All Fields]) OR (“dentistry”[MeSH Terms] OR “dentistry”[All Fields] OR “dentistry s”[All Fields])) AND ((“high”[All Fields] AND (“volum”[All Fields] OR “volume”[All Fields] OR “volumes”[All Fields] OR “voluming”[All Fields]) AND (“evacuate”[All Fields] OR “evacuated”[All Fields] OR “evacuates”[All Fields] OR “evacuating”[All Fields] OR “evacuation”[All Fields] OR “evacuations”[All Fields] OR “evacuator”[All Fields] OR “evacuators”[All Fields])) OR (“rubber dams”[MeSH Terms] OR (“rubber”[All Fields] AND “dams”[All Fields]) OR “rubber dams”[All Fields] OR (“rubber”[All Fields] AND “dam”[All Fields]) OR “rubber dam”[All Fields]) OR (“air filters”[MeSH Terms] OR (“air”[All Fields] AND “filters”[All Fields]) OR “air filters”[All Fields] OR (“air”[All Fields] AND “filter”[All Fields]) OR “air filter”[All Fields]) OR (“air ionization”[MeSH Terms] OR (“air”[All Fields] AND “ionization”[All Fields]) OR “air ionization”[All Fields]) OR (“ultraviolet”[All Fields] OR “ultraviolets”[All Fields]) OR (“disinfect”[All Fields] OR “disinfectable”[All Fields] OR “disinfectants”[Pharmacological Action] OR “disinfectants”[MeSH Terms] OR “disinfectants”[All Fields] OR “disinfectant”[All Fields] OR “disinfected”[All Fields] OR “disinfecting”[All Fields] OR “disinfection”[MeSH Terms] OR “disinfection”[All Fields] OR “disinfections”[All Fields] OR “disinfective”[All Fields] OR “disinfects”[All Fields])) |
| Scopus | (TITLE-ABS-KEY(aerosol) OR TITLE-ABS-KEY(aerosolization) OR TITLE-ABS-KEY(aerosolizations) OR TITLE-ABS-KEY(aerosolize) OR TITLE-ABS-KEY(aerosolized) OR TITLE-ABS-KEY(aerosolizer) OR TITLE-ABS-KEY(aerosolizes) OR TITLE-ABS-KEY(aerosolizing) OR TITLE-ABS-KEY(aerosols) OR TITLE-ABS-KEY(aerosolic) OR TITLE-ABS-KEY(bio-aerosol) OR TITLE-ABS-KEY(emission) OR TITLE-ABS-KEY(emissions) OR TITLE-ABS-KEY(emissive) OR TITLE-ABS-KEY(air pollution)) AND (TITLE-ABS-KEY(dental health services) OR TITLE-ABS-KEY(dental) OR TITLE-ABS-KEY(dentally) OR TITLE-ABS-KEY(dentals) OR TITLE-ABS-KEY(dentists) OR TITLE-ABS-KEY(dentist) OR TITLE-ABS-KEY(dentistry)) AND (TITLE-ABS-KEY(high volume evacuation) OR TITLE-ABS-KEY(high volume evacuate) OR TITLE-ABS-KEY(rubber dam) OR TITLE-ABS-KEY(suction) OR TITLE-ABS-KEY(air filter) OR TITLE-ABS-KEY(high efficiency particulate air) OR TITLE-ABS-KEY(air ionization) OR TITLE-ABS-KEY(ozone) OR TITLE-ABS-KEY(ultraviolet) OR TITLE-ABS-KEY(fumigation) OR TITLE-ABS-KEY(rinse) OR TITLE-ABS-KEY(reduction) OR TITLE-ABS-KEY(disinfection) OR TITLE-ABS-KEY(decontamination) OR TITLE-ABS-KEY(mitigation)) |
| Web of Science | TS= (aerosol OR aerosols OR aerosolization OR aerosolizations OR aerosolize OR bio-aerosol OR aerosol transmission OR aerosol generating procedures OR inhalation transmission OR contact transmission OR emissions OR nosocomial transmission OR air pollution) AND TS= (dental OR dental health services OR dentally OR dentals OR dentists OR dentist OR dentistry) AND TS= (high volume evacuation OR high volume evacuate OR rubber dam OR suction OR air filter OR high efficiency particulate air OR air ionization OR ozone OR ultraviolet OR fumigation OR rinse OR reduction OR disinfection OR decontamination OR mitigation) |
| Embase | ('aerosol'/exp OR aerosol OR 'aerosols'/exp OR aerosols OR 'bio aerosol' OR 'aerosol transmission'/exp OR 'aerosol transmission' OR (('aerosol'/exp OR aerosol) AND ('transmission'/exp OR transmission)) OR 'aerosol generating procedures'/exp OR 'aerosol generating procedures' OR (('aerosol'/exp OR aerosol) AND generating AND ('procedures'/exp OR procedures)) OR 'inhalation transmission' OR (('inhalation'/exp OR inhalation) AND ('transmission'/exp OR transmission)) OR 'contact transmission' OR (('contact'/exp OR contact) AND ('transmission'/exp OR transmission)) OR emissions OR 'nosocomial transmission'/exp OR 'nosocomial transmission' OR (nosocomial AND ('transmission'/exp OR transmission)) OR 'air pollution'/exp OR 'air pollution' OR (('air'/exp OR air) AND ('pollution'/exp OR pollution))) AND ('dental'/exp OR dental) AND ('high volume evacuation' OR (high AND ('volume'/exp OR volume) AND ('evacuation'/exp OR evacuation)) OR 'high volume evacuate' OR (high AND ('volume'/exp OR volume) AND evacuate) OR 'rubber dam'/exp OR 'rubber dam' OR (('rubber'/exp OR rubber) AND ('dam'/exp OR dam)) OR 'suction'/exp OR suction OR 'air filter'/exp OR 'air filter' OR (('air'/exp OR air) AND ('filter'/exp OR filter)) OR 'high efficiency particulate air' OR (high AND ('efficiency'/exp OR efficiency) AND particulate AND ('air'/exp OR air)) OR 'air ionization'/exp OR 'air ionization' OR (('air'/exp OR air) AND ('ionization'/exp OR ionization)) OR 'ozone'/exp OR ozone OR 'ultraviolet'/exp OR ultraviolet OR 'fumigation'/exp OR fumigation OR rinse OR 'reduction'/exp OR reduction OR 'disinfection'/exp OR disinfection OR 'decontamination'/exp OR decontamination OR 'mitigation'/exp OR mitigation) |
2.2. Eligibility criteria
Publications fulfilling the following inclusion criteria were selected: (1) RCT or CCT conducted in real-world dental or hospital environments relevant to dental procedures and investigations; (2) studies that investigate various aerosol mitigation interventions relevant to clinical dentistry; (3) articles written in English.
The following exclusion criteria were applied to the search results: (1) review articles, randomized and pseudo-randomized (alternation) split-mouth studies, experimental studies conducted in an environment not related to clinical settings; (2) researches that evaluate aerosol generation but where these are not related to single dental procedure and are performed in an environmental level; (3) studies written in languages other than English.
2.3. Study selection and data collection process
The information retrieved from the database was compiled, and any duplicate entries were removed. Two authors evaluated the title and abstract independently according to the eligibility criteria. Articles that were deemed ineligible by the two investigators were excluded, while articles that were deemed eligible by one investigator but ineligible by the other were retained for full-text assessment. Two reviewers worked collaboratively to analyze all the articles that were not excluded. Studies that met the eligibility criteria were selected for data extraction. If a discrepancy arose, a decision was made by consensus with a third author through further discussion.
Data from the selected articles were meticulously retrieved and gathered. The following variables were extracted: author(s), publication year, country, number of participants, type of study, type of aerosol mitigation intervention, method of aerosol assessment, type of microorganism, summary of aerosol reduction, and main findings. A meta-analysis was not feasible in this systematic review because of the differences in sample characteristics, study settings, assessment of aerosols, and outcome characterization. Instead, a systematic narrative synthesis approach was adopted to thematically explore the results and methods in accordance with the research questions proposed.
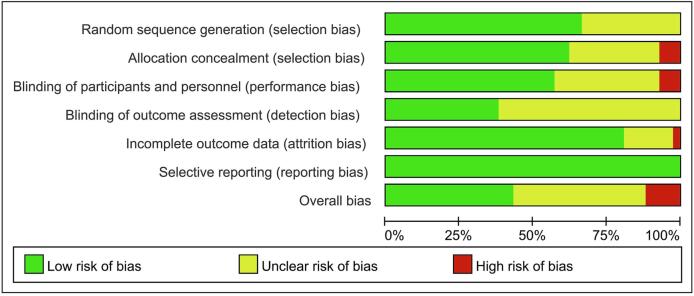
2.4. Quality assessment and risk of bias
The risk of bias in experimental studies was evaluated independently, in accordance with the Cochrane Collaboration’s tool, using Review Manager software version 5.4 (The Cochrane Collaboration, Copenhagen, Denmark) (Cumpston et al., 2019). This tool performed the quality assessment based on several criteria: allocation concealment, random sequence generation, blinding of outcome assessment, blinding of participants and personnel, incomplete outcome data, and selective reporting. Based on these criteria, each study's risk of bias was categorized as having a low risk, some concerns, or a high risk of bias.
3. Results
3.1. Study selection
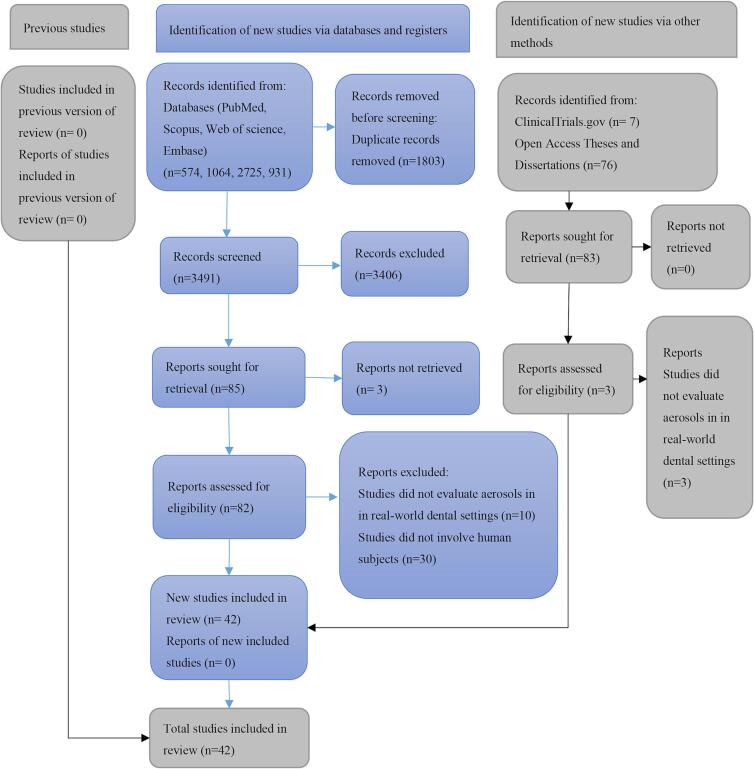
5294 articles were identified after the database screening: 574 from PubMed/MEDLINE, 1064 from Scopus, 2725 from Web of Science, and 931 from Embase. None of the 73 references obtained from the gray literature met the eligibility criteria. After removing duplicates, 3491 studies remained, of which 3406 were excluded after reviewing titles and abstracts. After considering full texts, 40 studies were excluded since these studies did not meet the inclusion criteria. Lastly, 42 studies were selected in the present study. Fig. 1 presents the selection process.
Fig. 1.
3.2. Study characteristics
Data from the 42 included studies are presented in Table 2 and Table 3. Table 2 focused on the assessment of bio-aerosols using bacterial culture, while Table 3 summarized the characteristics of studies that evaluated aerosols using multiple aerosol samplers. The majority of the studies were performed in America and India, while the rest came from around the world. Out of 42 studies, 16 were CCT and the remaining 26 were RCT. The number of participants ranges from 1 to 93. Overall, the use of mouse rises was the main type of aerosol mitigation intervention for the assessment of bio-aerosols. The application of HVE was widely used for the evaluation of aerosols via bacterial culture or aerosol samplers in the selected studies. In addition, HEPA filters, air cleaning systems, dental instruments, rubber dams, and saliva ejectors were also tested in several researches. In terms of aerosol assessment methodology, bacterial culture after natural sedimentation was the most widely used method in 29 studies. Other specific instruments like an optical aerosol spectrometer or various particle sizer were also applied. Most studies evaluated bacterial contamination in aerosols, while the viral and fungal contamination was assessed in only three studies.
Table 2.
Summary characteristics of the included studies assessing bio-aerosols.
| Author(s) | Country | Number of participants | Type of study | Type of aerosol mitigation intervention | Method of aerosol assessment | Type of microorganism |
|---|---|---|---|---|---|---|
| Al-Amad et al 2017 | United Arab Emirates | 52 | RCT | Rubber dam | Bacterial culture | Bacterial |
| Ashokkumar et al 2023 | India | 45 | RCT | Mouth rinses (CHX and herbal formulation) | Bacterial culture | Bacterial |
| Das et al 2022 | India | 80 |
RCT | Mouth rinses (no rinse group, water, 0.2% Chlorhexidine gluconate, herbal mouthwash) | bacterial culture | Bacterial |
| Desarda et al 2014 | India | 80 | RCT | HVE | Bacterial culture | Bacterial |
| Devker et al 2012 | India | 90 | CCT | HVE and mouth rinses (bis-biguanide) | Bacterial culture | Bacterial |
| Feres et al 2010 | Brazil | 60 | RCT | Mouth rinses (0.05 percent cetylpyridinium chloride, 0.12 percent chlorhexidine, water, no rinsing) | bacterial culture | Bacterial |
| Fine et al 1992 | America | 18 | RCT | Mouth rinses (antiseptic mouthwash, 5% hydroalcohol control rinse) | bacterial culture | Bacterial |
| Fine et al 1993 | America | 18 | RCT | Mouth rinses | Bacterial culture | Bacterial |
| Gupta et al 2014 | India | 24 | RCT | Mouth rinses (0.2% CHX gluconate, herbal mouthwash and water) | Bacterial culture | Bacterial |
| Hallier et al 2010 | BRITISH | 2 | RCT | Air cleaning system | Bacterial culture | Bacterial |
| Holloman et al 2015 | America | 50 | RCT | HVE (Isolite Systems and SE) | Bacterial culture | Bacterial |
| Jawade et al 2016 | India | 30 | RCT | Different ultrasonic liquid (distilled water, 2% povidone iodine and 0.12% CHX) | Bacterial culture | Bacterial |
| King et al 1997 | America | 12 | CCT | HEPA filter | Bacterial culture | Bacterial |
| Logothetis et al 1995 | America | 18 | RCT | Mouth rinses (chlorhexidine, antiseptic mouthwash, water) | bacterial culture | Bacterial |
| Mamajiwala et al 2018 | India | 60 | RCT | Irrigant through DUWL (chlorhexidine (CHX), cinnamon (CIN)) | bacterial culture | Bacterial |
| Muzzin et al 1999 | 30 | RCT | aerosol reduction device | bacterial culture | Bacterial | |
| Nayak et al 2020 | India | 30 | RCT | Mouth rinses (0.2% CHX gluconate, Befresh™ herbal mouthwash and water) | Bacterial culture | Bacterial |
| Nisha et al 2021 | India | 90 | RCT | Mouth rinses (0.12% CHX, 0.75% BA and water) | Bacterial culture | Bacterial |
| Nisha et al 2022 | India | 90 | RCT | Mouth rinses (0.12% chlorhexidine, 1.5% hydrogen peroxide, distilled water) | bacterial culture | Bacterial |
| Paul et al 2020 | India | 60 | RCT | Mouth rinses (94.5% aloe vera to 0.2% CHX gluconate and 1% povidone–iodine) | Bacterial culture | Bacterial |
| Prasanth et al 2010 | India | N/A | CCT | HVE with sterile water, distilled water, 0.5% sodium hypochlorite | Bacterial culture | Bacterial |
| Reddy et al 2012 | India | 30 | RCT | Mouth rinses (sterile water, non-tempered chlorhexidine, tempered chlorhexidine) | bacterial culture | Bacterial |
| Retamal-Valdes et al 2017 | Brazil | 60 | RCT | Mouth rinses (cetylpyridinium chloride, zinc lactate and sodium fluoride, water, 0.12% CHX digluconate) | Bacterial culture and checkerboard DNA–DNA hybridization | Bacterial |
| Santa et al 2022 | Brazil | N/A | CCT | Individual biosafety capsule in dentistry | Bacterial culture | Bacterial and virus |
| Santos et al 2014 | Brazil | 23 | RCT | Mouth rinses (distilled water, 0.12% chlorhexidine) | bacterial culture | Bacterial |
| Sethi et al 2019 | India | 60 | RCT | Ultrasonic coolant (distilled water, chlorhexidine, cinnamon extract) | bacterial culture | Bacterial |
| Shetty et al 2013 | India | 60 | CCT | Mouth rinses (CHX digluconate, tea tree oil or distilled water) | Bacterial culture | Bacterial |
| Takenaka et al 2022 | Japan | 10 | RCT | HVE and mouth rinses | Bacterial culture | Bacterial |
| Toroğlu et al 2001 | Turkey | N/A | CCT | Mouth rinsed (CHX) | Bacterial culture | Bacterial |
BA: boric acid; CCT: controlled clinical trials; CHX: chlorhexidine; EOSD: extra-oral suction device; HEPA: high-efficiency particulate air; HSS: high-speed suction; HVE: high-volume evacuators; N/A: not applicable; RCT: randomized controlled trials; SE: saliva ejector.
Table 3.
Summary characteristics of the included studies assessing aerosols with various aerosol samplers.
| Author(s) | Country | Number of participants | Type of study | Type of aerosol mitigation intervention | Method of aerosol assessment | Type of microorganism |
|---|---|---|---|---|---|---|
| Barrett et al 2022 | America | 40 | RCT | EOSD | Handheld particle counter (Temtop PMD 33) | N/A |
| Cappare et al 2022 | Italy | 80 | RCT | HEPA 14 Filter | Particle counter system (Lasair III) | Bacterial |
| Choudhary et al., 2022a, Choudhary et al., 2022b | America | N/A | CCT | HVE, SE, HEPA and rubber dams | A viable virus aerosol sampler and 2 SKC BioSamplers | Bacterial and virus |
| Choudhary et al., 2022a, Choudhary et al., 2022b | America | N/A | CCT | HVE, Air cleaning systems and dental instruments | An optical aerosol spectrometer (Model 11C) and wearable particulate matter sensors (Applied Particle Technology) | N/A |
| Demirkol et al 2023 | Turkey | N/A | CCT | SE and HEPA | Particle counter | N/A |
| Dudding et al 2022 | United Kingdom | 41 | RCT | Dental instruments | Aerodynamic particle sizer | N/A |
| Emery et al 2023 | America | 18 | CCT | Riboflavin | Fluorescent tracer | N/A |
| Lahdentausta et al 2022 | Finland | 84 | CCT | Dental instruments | Optical Particle Sizer | N/A |
| Liu et al 2023 | China | N/A | CCT | HVE (oral spray suction machine) | Anderson six-stage sampler and the natural sedimentation method | Bacterial and virus |
| Makhsous et al 2021 | America | N/A | CCT | Local area HEPA filters and HVE (extra-oral suction device) | A network of 13 fixed sensors positioned within the operatory and one wearable sensor | N/A |
| Noordien et al 2021 | South Africa | 1 | RCT | HVE | Assess and quantify in cm2 | N/A |
| Suprono et al 2021 | America | 93 | CCT | Baseline, HVE, combination and post-treatment | An automatic colony counter | Bacterial |
| Yang et al 2021 | America | 1 | CCT | HVE and HSS | Three measurement meters (DustTrak 8534, PTrak 8525 and AeroTrak 9306) | N/A |
BA: boric acid; CCT: controlled clinical trials; CHX: chlorhexidine; EOSD: extra-oral suction device; HEPA: high-efficiency particulate air; HSS: high-speed suction; HVE: high-volume evacuators; N/A: not applicable; RCT: randomized controlled trials; SE: saliva ejector.
Table 4 summarizes the main findings of the included studies. Overall, mouth rinses before clinical procedures can reduce the majority of bacteria generated from AGPs. In addition, the effectiveness of HVE in the mitigation of aerosol particles has been demonstrated in current studies. The HEPA filters and various air cleaning systems also present promising results. However, using a rubber dam seems to be associated with more bacterial colony-forming units.
Table 4.
Main findings of the included studies.
| Author(s) | Summary of aerosol reduction | Conclusions |
|---|---|---|
| Al-Amad et al 2017 | The number of bacteria: Using a rubber dam > not using a rubber dam | The rubber dam seems to result in significantly higher aerosol levels on various areas of the dentist’s head, requiring that dentists cover their heads with suitable protective wear. |
| Ashokkumar et al 2023 | The number of bacteria: distilled water (control) > herbal formulation (test) > CHX (tTest) | The addition of antiseptic agents to the water source contributed to a significant reduction of the cultivable microbial counts in the aerosol and hence can be used to reduce the risk of cross-infection during ultrasonic scaling. |
| Barrett et al 2022 | The number of particles: HVE only > HVE and EOSD | The reduction of aerosols is enhanced when the EOSD is used in combination with traditional HVE. However, the increased noise level when using the device can have a negative impact on patients’ dental experience. |
| Capparè et al. 2022 | The test group on pollution abatement was 83% more than the control group. | The addition of PAC equipment to the already existing safety measures was found to be significantly effective in further microbiological risk reduction. |
| Choudhary et al., 2022a, Choudhary et al., 2022b | The bacteria identified were most consistent with either environmental or oral microbiota. | Aerosols generating from dental procedures pose a low health risk for bacterial and likely viral pathogens when common aerosol mitigation interventions. |
| Choudhary et al., 2022a, Choudhary et al., 2022b | The number of particles: tip HVE > Conical HVE tip HVE > ISOVAC HVE |
Dentists should consider using HVE rather than standard-tip evacuators to reduce aerosols generated during routine clinical practice. |
| Das et al 2022 | The number of bacteria: no rinse group (control) > water (test) > 0.2% Chlorhexidine gluconate (test) > herbal mouthwash (test) | 0.2% Chlorhexidine gluconate is superior in reducing the microbial load in aerosols produced during ultrasonic scaling. |
| Demirkol et al 2023 | The number of particles: only SE > ventilated room > SE and HEOS |
As the particle size increases, the rate of spread away from the dentist’s working area decreases. The HEPA filtered extra-oral suction unit is more effective on particles smaller than 0.5 µm. |
| Desarda et al 2014 | The number of bacteria: with HVE: 11.08 ± 2.25 without HVE: 12.14 ± 1.93 |
It was concluded that HVE, when used as a separate unit without any modification, is not effective in reducing aerosol counts and environmental contamination. |
| Devker et al 2012 | The number of bacteria: 0.2% CHX gluconate > HVE > 0.2% CHX gluconate and HVE |
Preprocedural rinse and high volume suction were effective when used alone as well as together in reducing the microbial load of the aerosols produced during ultrasonic scaling. |
| Dudding et al 2022 | The number of particles: Background: 12.7% 3-in-1 air + water syringe: 42.9% |
This study provides evidence for sources of aerosol generation during common dental procedures, enabling more informed evaluation of risk and appropriate mitigation strategies. |
| Emery et al 2023 | The percentages of contaminated: slow suction > high suction > in‐line funnel |
Riboflavin can be used with minimal risk during dental procedures and allows for the detection of droplet spread in clinical settings in real time. |
| Feres et al 2010 | The number of bacteria: water (conrol) > CPC (test), CHX (test); no rinsing (control) > CPC (test), CHX (test) | A commercial mouthrinse containing 0.05 percent CPC when used as a preprocedural mouthrinse was equally effective as CHX in reducing the levels of spatter bacteria generated during ultrasonic scaling. |
| Fine et al 1992 | The number of bacteria: 5% hydroalcohol (control) > antiseptic mouthwash (test) | This study indicates that preprocedural rinsing with an antiseptic mouthwash can significantly reduce the microbial content of aerosols generated during ultrasonic scaling and may have potential in-office use as part of an infection control regimen. |
| Fine et al 1993 | The number of bacteria: control > antimicrobial mouthrinse |
The pre-procedural use of an antimicrobial mouth rinse produces a significant reduction in number of viable bacteria in a dental aerosol produced by ultrasonic scaling 40 min later. |
| Gupta et al 2014 | The number of bacteria: group C > group B > group A |
A routine preprocedural mouth rinse could eliminate the majority of bacterial aerosols generated by the use of an ultrasonic unit, and that 0.2% CHX gluconate is more effective than herbal mouthwash. |
| Hallier et al 2010 | The number of bacteria: Without ACS > with ACS |
Potentially hazardous bioaerosols created during dental procedures can be significantly reduced using an air cleaning system. |
| Holloman et al 2015 | The number of bacteria: control group: 3.61(0.95) > test group: 3.30(0.88) | Neither device reduced aerosols and spatter effectively, and there was no significant difference in reduction between the 2 devices. Additional measures should be taken with these devices to reduce the likelihood of disease transmission. |
| Jawade et al 2016 | The number of bacteria: CHX gluconate: 27.17 ± 12.5 CFU distilled water: 124.5 ± 30.08 CFU povidone iodine: 60.43 ± 33.33 CFU |
CHX gluconate is more effective in reducing dental aerosols when compared to povidone iodine and distilled water. Povidone iodine showed better CFU reduction when compared with distilled water. |
| King et al 1997 | The number of bacteria: the ultrasonic sealer without the aerosol reduction device: 45.1 ± 28.9; the ultrasonic sealer with the aerosol reduction device: 2.6 ± 3.6 | An aerosol reduction device is effective in reducing the number of microorganisms generated during ultrasonic scaling, therefore decreasing the risk of disease transmission. |
| Lahdentausta et al 2022 | The number of particles: different dental procedures > background air turbine handpiece was highest |
Air turbine handpieces produced the highest levels of < 1 μm aerosols and total particle number concentrations. High- and low-speed dental handpieces and ultrasonic scalers elevated the aerosol concentration levels compared to the aerosol levels measured during oral examination. |
| Liu et al 2023 | The bioaerosol concentration: Without OSSM > with OSSM |
OSSM use in dental clinics can reduce the exposure concentrations of bioaerosols for healthcare workers during dental treatment and is beneficial for minimizing the risk of infectious diseases such as COVID-19. |
| Logothetis and Martinez-Welles, 1995 | The number of bacteria: water (conrol) > chlorhexidine (test); dantiseptic mouthwash (test) > chlorhexidine (test) | Bacterial counts collected during the treatment indicate that the chlorhexidine pretreatment rinse was significantly more effective than the other solutions in reducing bacterial aerosols. |
| Makhsous et al 2021 | The bioaerosol concentration: HEPA > EOSD |
The data collected found a slight reduction in particle count when EOSD units were turned on. |
| Mamajiwala et al 2018 | The number of bacteria: distilled water (conrol) > chlorhexidine (test); distilled water (control) > cinnamon (test) | Both CIN and CHX used as an irrigant through DUWL effectively helped in the reduction of bacterial count in dental aerosols. |
| Muzzin et al 1999 | The number of bacteria: without the aerosol reduction device (control) > with the aerosol reduction device (test) | The data suggest that the aerosol reduction device is effective in reducing the number of microorganisms generated during air polishing. |
| Nayak et al 2020 | The number of bacteria: water > Befresh™ (Sagar Pharmaceuticals) mouthwash > the CHX group |
This study proves that a regular preprocedural mouth rinse could significantly reduce the majority bacteria present in aerosols generated by the use of an ultrasonic unit, and Befresh™ mouth rinse was found to be equally effective in reducing the aerosol contamination to 0.2% CHX gluconate. |
| Nisha et al 2021 | The number of bacteria: group A > group B > group C |
Routine use of preprocedural mouthrinse could be a measure to reduce bacterial aerosols generated during ultrasonic scaling and 0.12% CHX gluconate is more effective than 0.75% BA mouthwash in reducing CFUs count. |
| Nisha et al 2022 | The number of bacteria: distilled water (control) > 1.5% hydrogen peroxide (test) > 0.12% chlorhexidine (test) | Preprocedural rinse using HP can effectively be used as a method to reduce dental aerosols generated during ultrasonic scaling. |
| Noordien et al 2021 | DASD + LV: in a 62% reduction HV + LV compared to LV alone: in a 53% reduction |
The DASD in conjunction with LV was more effective in reducing aerosol, droplets and splatter than HV plus LV. |
| Paul et al 2020 | The number of bacteria: PVP-1 > AV > CHX |
94.5% AV as a preprocedural rinse is better than 1% PVP–I and comparable to 0.2% CHX in reducing CFU count. |
| Prasanth et al 2010 | The number of colonies: stage 1 > stage 2 | The use of high volume suction apparatus and 0.5 percent sodium hypochlorite solution was significantly effective in reducing the microbial load. |
| Reddy et al 2012 | The number of bacteria: sterile water (control) > non tempered chlorhexidine (test) > tempered chlorhexidine (test) | Pre-procedural rinse can significantly reduce the viable microbial content of dental aerosols and tempered chlorhexidine was more effective than non-tempered chlorhexidine. |
| Retamal-Valdes et al 2017 | The number of bacteria: did not rinse or rinse with water > CPC + Zn + F or CHX | The mouthwash containing CPC + Zn + F, is effective in reducing viable bacteria in oral aerosol after a dental prophylaxis with ultrasonic scaler. |
| Santa et al 2022 | The number of bacteria: Without IBCD > with IBCD |
The use of the biosafety device is an effective means to reduce air contamination by more than 99% of bacterial contamination around the main droplet/aerosol source. |
| Santos et al 2014 | The number of bacteria: distilled water (control) > 0.12% chlorhexidine (test) | The prior use of 0.12% chlorhexidine as mouthwash significantly reduced contamination caused by aerosolized sodium bicarbonate during dental prophylaxis in the orthodontic clinic. |
| Sethi et al 2019 | The number of bacteria: distilled water (conrol) > chlorhexidine (test); distilled water (control) > cinnamon extract (test) | Both cinnamon and chlorhexidine used as an ultrasonic device coolant through DUWLs effectively helped in the reduction of bacterial count in dental aerosols. |
| Shetty et al 2013 | The number of bacteria: distilled water > tea tree oil > Chlorhexidine digluconate | This study showed that all the antiseptic mouthwashes significantly reduced the bacterial CFUs in aerosol samples. Chlorhexidine rinses were found to be superior to tea tree when used preprocedurally in reducing aerolized bacteria. |
| Suprono et al 2021 | The number of bacteria: HVE > HVE and intraoral suction device |
Significant reductions were founded in the amount of microbial aerosols when both HVE and an intraoral suction device were used. |
| Takenaka et al 2022 | The number of bacteria: With the eHVE 20 cm away > With the eHVE 10 cm away; No rinsing > mouth rinsing | Preprocedural mouth rinsing can reduce bacterial contamination where the extraoral HVE is positioned away from the mouth, depending on the procedure. Combining an extraoral HVE with preprocedural mouth rinsing can reduce bacterial contamination in dental offices. |
| Toroğlu et al 2001 | The number of bacteria: Debonding > Baseline Without CHX rinse > with CHX rinse (P > 0.05) |
Preprocedural CHX gluconate mouth rinse appears to be ineffective in decreasing the exposure to infectious agents. Therefore, barrier equipment should be used to prevent aerosol contamination. |
| Yang et al 2021 | the number of particles: SE + HSS > SE + HSS + HVS |
The increase of the level of aerosol with size less than 10 µm was minimal during dental procedures when using SE and HSS. Use of HVS further reduced aerosol levels below the ambient levels. |
AV: aloe vera; BA: boric acid; CCT: controlled clinical trials; CFUs: colony‑forming units; CHX: chlorhexidine; CPC: cetylpyridinium chloride; DASD: dental aerosol suction device; DUWLs: dental unit waterlines; EOSD: extra-oral suction device; HEPA: high-efficiency particulate air; HSS: high-speed suction; HVE: high-volume evacuators; IBCD: individual biosafety capsule in dentistry; LV: low-volume; PVP‑I: povidone‑iodine; RCT: randomized controlled trials; SE: saliva ejector.
3.3. Risk of bias
The risk of bias is presented in Fig. 2. More than half of the studies showed a low risk of bias regarding random sequence generation. Regarding the deviation from allocation concealment, 3 studies were considered high as the researchers and patients were both fully aware of the dental treatment received. Regarding the blinding of participants and personnel, 3 studies were considered a high risk of bias due to as the treatment methods received by patients were not concealed and researchers obtained knowledge of the treatment through testing. Most of the selected studies were regarded as having an unclear risk in the blinding of outcome assessment because the use of blinding during the results assessment process was not reported in the text. For the incomplete outcome data, most of them demonstrated a low risk of bias. All studies presented low a risk of bias in selective reporting. Overall, based on the Cochrane Collaboration tool, 18 studies were considered to have a low risk of bias, while 19 studies were rated as having unclear risk and 5 studies were deemed to have high risk of bias.
Fig. 2.
4. Discussion
Recent scientific evidence has demonstrated the relevant role of the oral cavity in the transmission of COVID-19 (Herrera et al., 2020). Given the increase in COVID-19 cases during the Omicron epidemic, it is crucial to implement effective strategies to mitigate aerosol contamination during dental procedures to protect both patients and dental health providers. To improve reliability, only studies involving human subjects and conducted in dental settings were included. As one of the first reviews to focus on aerosol generation interventions in real-world dental clinics, our study provides valuable insights into the effectiveness of different mitigation strategies.
The clinical practice of dentistry is one of the most important representative areas against aerosolized particulates, including fungi, bacteria, and virus. As a byproduct of the dental practice, small particulates such as aerosols have been regarded as respiratory system–triggering proxies, which impose potential risk to dental health providers (Dawson et al., 2016). The aforementioned concerns are augmented concerning dental clinics, especially in the era of the pandemic. For example, the presence of SARS-CoV-2 in patients’ saliva presents an additional impact on its air suspension after AGPs (Azzi et al., 2020). The commonly used AGPs in the clinical practice of dentistry have been confirmed to produce droplets and aerosols which may present potential detriments to both patients and dentists. A recent systematic review comprehensively evaluated the aerosols generation of commonly applied dental activities in 83 studies, including low-speed handpieces, high-speed air-rotor, oral surgery, air polishing, ultrasonic scaling, hand scaling, and air–water syringes (Innes et al., 2021). The contamination in air as well as surfaces around the personnel was demonstrated from all procedures although the detection sensitivity was low. Accordingly, the identification of the microbial load after AGPs in general and the evaluation of the effectiveness of aerosol intervention strategies are critical concerns during the clinical practice of Dentistry.
Aerosol contamination can be measured with several methods. However, a previous review reported there was no generally accepted approach for measuring bio-aerosol contamination (Ghosh et al., 2015). Regarding the method used for aerosol assessment in this study, the majority of included papers selected natural sedimentation and bacterial culture as the approach to studying the aerosol components in dental environments. Bacterial culture collection points were established in diverse positions of the experimental area, and the positioned culture media was used to detect potential microbial particles carried therein. The collected culture media samples are then cultured under appropriate environmental conditions to facilitate microbial growth. Upon completion of the cultivation phase, laboratory technicians employ a microbial colony counter to quantitatively assess the formed microbial colonies. This quantitative data serves as a metric for evaluating the extent of bio-aerosol contamination. However, this method has some limitations since this approach would only be helpful if the positioned culture media was beyond an area expected to collect splatter. Moreover, small particles like aerosols may remain suspended for a long time. Accordingly, studies using this method would be more limited compared to direct aerosol capture via an aerosol sampler. Three articles (Barrett et al., 2022, Demirkol et al., 2023; Barrett et al., 2021) used air quality particle counters to measure the concentration of particles in the air since these devices can detect both airborne droplets and aerosols before they fall to the ground. Some specific methods, such as virus aerosol sampler, optical aerosol spectrometer, aerodynamic particle sizer, fluorescent tracer, and Anderson six-stage sampler were also used in several studies. Further investigations should focus on the effectiveness and accuracy of this newly developed equipment in monitoring aerosols in dental environments. Moreover, in this study, particles of less than 5 μm in diameter were considered aerosols based on the commonly held assumption. Nevertheless, recently researchers proposed that this classification was not supported by current scientific knowledge (Eliades and Koletsi, 2020). Accordingly, further multi-disciplinary researches are required to better elucidate the characteristics of aerosol and its potential influence during dental practice in real-world environments.
Although conventional protective equipment such as surgical masks and gloves are widely used in clinical practice among dental providers, there remain potential limitations. For example, due to the limited ability to filter particles and the presence of small defects in commonly used surgical masks, they may not be able to completely prevent the spread of aerosolized microorganisms. Moreover, the filtration efficiency of surgical masks decreases significantly when they become wet, and gloves may have small defects and can be torn during clinical use (Kohn et al., 2003). However, aerosols may remain suspended in clinical settings for up to 4 h after AGPs (Veena et al., 2015). Accordingly, dental health providers may be exposed when the protective equipment is removed.
A range of approaches to reducing aerosol concentrations has been evaluated in current studies, including rubber dams, HVE, HEPA filters, and air cleaning systems. As the most widely used device in reducing aerosols, HVE has been extensively evaluated in selected studies. Several current reviews have summarized the effectiveness of interventions to reduce aerosol generation in dental environments. For example, a previous systematic review containing RCT has been performed to assess the influence of mouth rinses used in dental clinics (Kumbargere et al., 2022). The reduction in the level of bacterial contamination in aerosols has been demonstrated in this study. Another systematic review summarized available data on pre-procedural oral rinse, rubber dam application, and HVE aimed at decreasing bio-aerosols (Samaranayake et al., 2021). Researchers concluded that HVE could be an obligatory requirement to reduce bio-aerosols during the clinical practice of dentistry, while pre-procedural oral rinses and rubber dams must be utilized when opportune. Overall, most studies concluded that HVE was effective in decreasing the microbial load of aerosols produced in AGPs. However, the use of HVE as a separate unit without any modification should be taken with caution since another study did not report positive results in reducing aerosol counts and environmental contamination (Desarda et al., 2014), and the positioning of HVE relative to the oral cavity was also critical for the effectiveness (Takenaka et al., 2022). Nevertheless, the combination of HVE with other approaches such as pre-procedural mouth rinsing or extra-oral suction devices. In addition, the effectiveness of a dedicated air cleaning system has also been assessed in many dental procedures including cavity preparation, extraction and ultrasonic scaling and showed promising results (Hallier et al., 2010). As the standard of care in dentistry, the rubber dam has been commonly applied in dental environments. Nevertheless, the results demonstrated significantly higher aerosol levels on various areas of the head after using the rubber dam, indicating the necessity of suitable protective wear for covering the head of dentists (Al-Amad et al., 2017). After evaluating the efficacy of reducing aerosols during anterior tooth preparation, Demirkol et al found that the HEPA-filtered extra-oral suction unit is more useful when measuring particles less than 0.5 µm, which can reduce the spread of viral and bacterial infections and cross-infection (Demirkol et al., 2023). Accordingly, the strategies mentioned above can be applied in clinical practice based on specific conditions.
This study has several limitations. First of all, selected studies did not measure the reduction in infection rates in COVID-19 since it can only be measured during an epidemic, which is difficult or even impossible to conduct. In addition, a meta-analysis was not feasible in this systematic review because of the differences in sample characteristics, study settings, aerosol measurement equipment, and outcome characterization and assessment in aerosols, and it was hard to compare the results with those of previous reviews since this is the first review focus on aerosol generation intervention strategies in real-world dental clinics. Finally, although there is evidence suggesting that certain interventions such as mouth rinse before procedures may reduce bacterial contamination in aerosols, there were many challenges to drawing conclusive conclusions from the available literature concerning the effectiveness of remaining interventions to reduce aerosol generation due to the various methods used in included studies.
5. Conclusions
In conclusion, after summarizing the current literature, a reduction in the level of bacterial contamination in aerosols of dental environments has been confirmed after several mitigation strategies, particularly in the context of the COVID-19 pandemic. Dental health providers should continue to implement measures to protect themselves and their patients, such as using appropriate personal protective equipment and implementing effective infection control practices. Further multi-disciplinary researches are required to investigate the most effective strategies for reducing aerosol generation and transmission of infectious agents during dental practice in real-world environments.
6. Data availability
Data will be made available from the corresponding author on reasonable request.
Funding
This research was funded by scientific research project of National Key Research and Development Program of China, grant number 2021YFC2400400 and Shanghai Municipal Health Commission, grant number 202040094.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
Data will be made available on request.
References
- Al-Amad S.H., Awad M.A., Edher F.M., Shahramian K., Omran T.A. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J. Infect. Public Health. 2017;10(2):195–200. doi: 10.1016/j.jiph.2016.04.014. [DOI] [PubMed] [Google Scholar]
- Al-Yaseen W., Jones R., McGregor S., Wade W., Gallagher J., Harris R., et al. Aerosol and splatter generation with rotary handpieces used in restorative and orthodontic dentistry: a systematic review. BDJ Open. 2022;8(1):26. doi: 10.1038/s41405-022-00118-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashokkumar L., Lavu V., Palraj K.K., Rao S.R., Balaji S.K. Efficacy of chlorhexidine/herbal formulation for microbial reduction in aerosol generated following ultrasonic scaling - A double-blinded randomized controlled trial. J. Indian Soc. Periodontol. 2023;27(1):82–86. doi: 10.4103/jisp.jisp_478_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azzi L., Carcano G., Gianfagna F., Grossi P., Gasperina D.D., Genoni A., et al. Saliva is a reliable tool to detect SARS-CoV-2. J. Infect. 2020;81(1):e45–e50. doi: 10.1016/j.jinf.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett B., McGovern J., Catanzaro W., Coble S., Redden D., Fouad A.F. Clinical Efficacy of an Extraoral Dental Evacuation Device in Aerosol Elimination During Endodontic Access Preparation. J. Endod. 2022;48(12):1468–1475. doi: 10.1016/j.joen.2022.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capparè P., D'Ambrosio R., De Cunto R., Darvizeh A., Nagni M., Gherlone E. The Usage of an Air Purifier Device with HEPA 14 Filter during Dental Procedures in COVID-19 Pandemic: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health. 2022;19(9):5139. doi: 10.3390/ijerph19095139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhary S., Bach T., Wallace M.A., Stoeckel D.C., Thornhill M.H., Lockhart P.B. Assessment of Infectious Diseases Risks From Dental Aerosols in Real-World Settings. Open Forum. Infect. Dis. 2022;9(11):ofac617. doi: 10.1093/ofid/ofac617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhary S., Durkin M.J., Stoeckel D.C., Steinkamp H.M., Thornhill M.H., Lockhart P.B. Comparison of aerosol mitigation strategies and aerosol persistence in dental environments. Infect. Control Hosp. Epidemiol. 2022;43(12):1779–1784. doi: 10.1017/ice.2022.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumpston M., Li T., Page M.J., Chandler J., Welch V.A., Higgins J.P., et al., 2019. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10: ED000142. [DOI] [PMC free article] [PubMed]
- Das S.J., Kharbuli D., Alam S.T. Effects of preprocedural mouth rinse on microbial load in aerosols produced during the ultrasonic scaling: A randomized controlled trial. J Indian Soc Periodontol. 2022;26(5):478–484. doi: 10.4103/jisp.jisp_281_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson M., Soro V., Dymock D., Price R., Griffiths H., Dudding T., et al. Microbiological assessment of aerosol generated during debond of fixed orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2016;150(5):831–838. doi: 10.1016/j.ajodo.2016.04.022. [DOI] [PubMed] [Google Scholar]
- Demirkol N., Karagozoglu I., Kocer I.K. Efficiency of HEPA-filtered extra-oral suction unit on aerosols during prosthetic dental preparation: A pilot study. Clin. Oral Invest. 2023:1–8. doi: 10.1007/s00784-022-04850-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desarda H., Gurav A., Dharmadhikari C., Shete A., Gaikwad S., et al. Efficacy of High-volume Evacuator in Aerosol Reduction: Truth or Myth? A Clinical and Microbiological Study. J Dent Res Dent Clin Dent Prospects. 2014;8(3):176–179. doi: 10.5681/joddd.2014.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devker N.R., Mohitey J., Vibhute A., Chouhan V.S., Chavan P., Malagi S., et al. A study to evaluate and compare the efficacy of preprocedural mouthrinsing and high volume evacuator attachment alone and in combination in reducing the amount of viable aerosols produced during ultrasonic scaling procedure. J. Contemp. Dent. Pract. 2012;13(5):681–689. doi: 10.5005/jp-journals-10024-1209. [DOI] [PubMed] [Google Scholar]
- Dudding T., Sheikh S., Gregson F., Haworth J., Haworth S., Main B.G., et al. A clinical observational analysis of aerosol emissions from dental procedures. PLoS One. 2022;17(3):e0265076. doi: 10.1371/journal.pone.0265076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliades T., Koletsi D. Minimizing the aerosol-generating procedures in orthodontics in the era of a pandemic: Current evidence on the reduction of hazardous effects for the treatment team and patients. Am. J. Orthod. Dentofac. Orthop. 2020;158(3):330–342. doi: 10.1016/j.ajodo.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery M.A., Reed D., McCracken B. Novel use of riboflavin as a fluorescent tracer in the dissemination of aerosol and splatter in an open operatory dental clinic. Clin. Exp. Dent. Res. 2023:1–9. doi: 10.1002/cre2.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feres M., Figueiredo L.C., Faveri M., Stewart B., de Vizio W. The effectiveness of a preprocedural mouthrinse containing cetylpyridinium chloride in reducing bacteria in the dental office. J. Am. Dent. Assoc. 2010;141(4):415–422. doi: 10.14219/jada.archive.2010.0193. [DOI] [PubMed] [Google Scholar]
- Fine D.H., Mendieta C., Barnett M.L., Furgang D., Meyers R., Olshan A., et al. Efficacy of preprocedural rinsing with an antiseptic in reducing viable bacteria in dental aerosols. J. Periodontol. 1992;63(10):821–824. doi: 10.1902/jop.1992.63.10.821. [DOI] [PubMed] [Google Scholar]
- Fine D.H., Yip J., Furgang D., Barnett M.L., Olshan A.M., Vincent J. Reducing bacteria in dental aerosols: pre-procedural use of an antiseptic mouthrinse. J. Am. Dent. Assoc. 1993;124(5):56–58. doi: 10.14219/jada.archive.1993.0122. [DOI] [PubMed] [Google Scholar]
- Ghosh B., Lal H., Srivastava A. Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environ. Int. 2015;85:254–272. doi: 10.1016/j.envint.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta G., Mitra D., Ashok K.P., Gupta A., Soni S., Ahmed S. Efficacy of preprocedural mouth rinsing in reducing aerosol contamination produced by ultrasonic scaler: a pilot study. J. Periodontol. 2014;85(4):562–568. doi: 10.1902/jop.2013.120616. [DOI] [PubMed] [Google Scholar]
- Hallier C., Williams D.W., Potts A.J., Lewis M.A. A pilot study of bioaerosol reduction using an air cleaning system during dental procedures. Br. Dent. J. 2010;209(8):E14. doi: 10.1038/sj.bdj.2010.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrel S.K., Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004;135(4):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera D., Serrano J., Roldán S., Sanz M. Is the oral cavity relevant in SARS-CoV-2 pandemic? Clin. Oral Invest. 2020;24(8):2925–2930. doi: 10.1007/s00784-020-03413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloman J.L., Mauriello S.M., Pimenta L., Arnold R.R. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. J. Am. Dent. Assoc. 2015;146(1):27–33. doi: 10.1016/j.adaj.2014.10.001. [DOI] [PubMed] [Google Scholar]
- Innes N., Johnson I.G., Al-Yaseen W., Harris R., Jones R., Kc S., et al. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2021;105 doi: 10.1016/j.jdent.2020.103556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jawade R., Bhandari V., Ugale G., Taru S., Khaparde S., Kulkarni A., et al. Comparative Evaluation of Two Different Ultrasonic Liquid Coolants on Dental Aerosols. J. Clin. Diagn. Res. 2016;10(7):ZC53-7. doi: 10.7860/JCDR/2016/20017.8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.M., Brosseau L.M. Aerosol transmission of infectious disease. J. Occup. Environ. Med. 2015;57(5):501–508. doi: 10.1097/JOM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- Judson S.D., Munster V.J. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses. 2019;11(10):940. doi: 10.3390/v11100940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim S.S.A., Karim Q.A. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–2128. doi: 10.1016/S0140-6736(21)02758-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King T.B., Muzzin K.B., Berry C.W., Anders L.M. The effectiveness of an aerosol reduction device for ultrasonic scalers. J. Periodontol. 1997;68(1):45–49. doi: 10.1902/jop.1997.68.1.45. [DOI] [PubMed] [Google Scholar]
- Kohn W.G., Collins A.S., Cleveland J.L., Harte J.A., Eklund K.J., Malvitz D.M., et al. Guidelines for infection control in dental health-care settings–2003. MMWR Recomm. Rep. 2003 52(RR-17):1–61. [PubMed] [Google Scholar]
- Koletsi D., Belibasakis G.N., Eliades T. Interventions to Reduce Aerosolized Microbes in Dental Practice: A Systematic Review with Network Meta-analysis of Randomized Controlled Trials. J. Dent. Res. 2020;99(11):1228–1238. doi: 10.1177/0022034520943574. [DOI] [PubMed] [Google Scholar]
- Kumbargere N.S., Eachempati P., Paisi M., Nasser M., Sivaramakrishnan G., Francis T., et al. Preprocedural mouth rinses for preventing transmission of infectious diseases through aerosols in dental healthcare providers. Cochrane Database Syst. Rev. 2022 doi: 10.1002/14651858.CD013826.pub2. 8(8):CD013826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaCaille L.J., Hooker S.A., Marshall E., LaCaille R.A., Owens R. Change in Perceived Stress and Health Behaviors of Emerging Adults in the Midst of the COVID-19 Pandemic. Ann. Behav. Med. 2021;55(11):1080–1088. doi: 10.1093/abm/kaab074. [DOI] [PubMed] [Google Scholar]
- Lahdentausta L., Sanmark E., Lauretsalo S., Korkee V., Nyman S., Atanasova N., et al. Aerosol concentrations and size distributions during clinical dental procedures. Heliyon. 2022;8(10):e11074. doi: 10.1016/j.heliyon.2022.e11074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leggat P.A., Kedjarune U. Bacterial aerosols in the dental clinic: a review. Int. Dent. J. 2001;51(1):39–44. doi: 10.1002/j.1875-595x.2001.tb00816.x. [DOI] [PubMed] [Google Scholar]
- Liu Z., Zhang P., Liu H., He J., Li Y., Yao G., et al. Estimating the restraint of SARS-CoV-2 spread using a conventional medical air-cleaning device: Based on an experiment in a typical dental clinical setting. Int. J. Hyg. Environ. Health. 2023;248 doi: 10.1016/j.ijheh.2023.114120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logothetis D.D., Martinez-Welles J.M. Reducing bacterial aerosol contamination with a chlorhexidine gluconate pre-rinse. J. Am. Dent. Assoc. 1995;126(12):1634–1639. doi: 10.14219/jada.archive.1995.0111. [DOI] [PubMed] [Google Scholar]
- Makhsous S., Segovia J.M., He J., Chan D., Lee L., Novosselov I.V., et al. Methodology for Addressing Infectious Aerosol Persistence in Real-Time Using Sensor Network. Sensors (Basel) 2021;21(11):3928. doi: 10.3390/s21113928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamajiwala A.S., Sethi K.S., Raut C.P., Karde P.A., Khedkar S.U. Comparative evaluation of chlorhexidine and cinnamon extract used in dental unit waterlines to reduce bacterial load in aerosols during ultrasonic scaling. Indian J. Dent. Res. 2018;29(6):749–754. doi: 10.4103/ijdr.IJDR_571_17. [DOI] [PubMed] [Google Scholar]
- Marui V.C., Souto M.L.S., Rovai E.S., Romito G.A., Chambrone L., Pannuti C.M. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: A systematic review. J. Am. Dent. Assoc. 2019;150(12):1015–1026.e1. doi: 10.1016/j.adaj.2019.06.024. [DOI] [PubMed] [Google Scholar]
- Meng L., Hua F., Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosaddad S.A., Tahmasebi E., Yazdanian A., Rezvani M.B., Seifalian A., Yazdanian M., et al. Oral microbial biofilms: an update. Eur. J. Clin. Microbiol. Infect. Dis. 2019;38(11):2005–2019. doi: 10.1007/s10096-019-03641-9. [DOI] [PubMed] [Google Scholar]
- Muzzin K.B., King T.B., Berry C.W. Assessing the clinical effectiveness of an aerosol reduction device for the air polisher. J. Am. Dent. Assoc. 1999;130(9):1354–1359. doi: 10.14219/jada.archive.1999.0407. [DOI] [PubMed] [Google Scholar]
- Nisha S., Shivamallu A.B., Gujjari S.K., Shashikumar P., Ali N.M., Kulkarni M. Efficacy of Preprocedural Boric Acid Mouthrinse in Reducing Viable Bacteria in Dental Aerosols Produced during Ultrasonic Scaling. Contemp Clin Dent. 2021;12(3):282–288. doi: 10.4103/ccd.ccd_374_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisha S., Karmakar S., Das S., Jana D., Ali N.M., Shashikumar P. Comparison of Chlorhexidine and Hydrogen Peroxide as Preprocedural Mouthrinse during Ultrasonic Scaling: A Triple-Blinded Randomized Controlled Clinical Trial. J. Pharm. Bioallied Sci. 2022;14(Suppl 1):S110–S114. doi: 10.4103/jpbs.jpbs_595_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noordien N., Mulder-van S.S., Mulder R. In Vivo Study of Aerosol, Droplets and Splatter Reduction in Dentistry. Viruses. 2021;13(10):1928. doi: 10.3390/v13101928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul B., Baiju R.M.P., Raseena N.B., Godfrey P.S., Shanimole P.I. Effect of aloe vera as a preprocedural rinse in reducing aerosol contamination during ultrasonic scaling. J Indian Soc Periodontol. 2020;24(1):37–41. doi: 10.4103/jisp.jisp_188_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasanth T., Mandlik V.B., Kumar S., Jha A.K., Kosala M. Evaluation of Aerosol and Water Contamination and Control of Cross Infection in Dental Clinics. Med. J. Armed Forces India. 2010;66(1):37–40. doi: 10.1016/S0377-1237(10)80090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy S., Prasad M.G., Kaul S., Satish K., Kakarala S., Bhowmik N. Efficacy of 0.2% tempered chlorhexidine as a pre-procedural mouth rinse: A clinical study. J Indian Soc Periodontol. 2012;16(2):213–217. doi: 10.4103/0972-124X.99264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retamal-Valdes B., Soares G.M., Stewart B., Figueiredo L.C., Faveri M., Miller S., et al. Effectiveness of a pre-procedural mouthwash in reducing bacteria in dental aerosols: randomized clinical trial. Braz. Oral Res. 2017;31:e21. doi: 10.1590/1807-3107BOR-2017.vol31.0021. [DOI] [PubMed] [Google Scholar]
- Samaranayake L.P., Fakhruddin K.S., Buranawat B., Panduwawala C. The efficacy of bio-aerosol reducing procedures used in dentistry: a systematic review. Acta Odontol. Scand. 2021;79(1):69–80. doi: 10.1080/00016357.2020.1839673. [DOI] [PubMed] [Google Scholar]
- Santos I.R., Moreira A.C., Costa M.G., Castellucci e Barbosa M.d., Effect of 0.12% chlorhexidine in reducing microorganisms found in aerosol used for dental prophylaxis of patients submitted to fixed orthodontic treatment. Dental Press. J. Orthod. 2014;19(3):95–101. doi: 10.1590/2176-9451.19.3.095-101.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schardt C., Adams M.B., Owens T., Keitz S., Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inf. Decis. Making. 2007;7:16. doi: 10.1186/1472-6947-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi K.S., Mamajiwala A., Mahale S., Raut C.P., Karde P. Comparative evaluation of the chlorhexidine and cinnamon extract as ultrasonic coolant for reduction of bacterial load in dental aerosols. J Indian Soc Periodontol. 2019;23(3):226–233. doi: 10.4103/jisp.jisp_517_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shetty S.K., Sharath K., Shenoy S., Sreekumar C., Shetty R.N., Biju T. Compare the effcacy of two commercially available mouthrinses in reducing viable bacterial count in dental aerosol produced during ultrasonic scaling when used as a preprocedural rinse. J. Contemp. Dent. Pract. 2013;14(5):848–851. doi: 10.5005/jp-journals-10024-1414. [DOI] [PubMed] [Google Scholar]
- Suprono M.S., Won J., Savignano R., Zhong Z., Ahmed A., Roque-Torres G., et al. A clinical investigation of dental evacuation systems in reducing aerosols. J. Am. Dent. Assoc. 2021;152(6):455–462. doi: 10.1016/j.adaj.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takenaka S., Sotozono M., Yashiro A., Saito R., Kornsombut N., Naksagoon T., et al. Efficacy of Combining an Extraoral High-Volume Evacuator with Preprocedural Mouth Rinsing in Reducing Aerosol Contamination Produced by Ultrasonic Scaling. Int. J. Environ. Res. Public Health. 2022;19(10):6048. doi: 10.3390/ijerph19106048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J. R. Soc. Interface. 2009;6 Suppl 6(Suppl 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To K.K., Tsang O.T., Yip C.C., Chan K.H., Wu T.C., Chan J.M., et al. Consistent Detection of 2019 Novel Coronavirus in Saliva. Clin. Infect. Dis. 2020;71(15):841–843. doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toroğlu M.S., Haytaç M.C., Köksal F. Evaluation of aerosol contamination during debonding procedures. Angle Orthod. 2001;71(4):299–306. doi: 10.1043/0003-3219(2001)071<0299:EOACDD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Veena H.R., Mahantesha S., Joseph P.A., Patil S.R., Patil S.H. Dissemination of aerosol and splatter during ultrasonic scaling: a pilot study. J. Infect. Public Health. 2015;8(3):260–265. doi: 10.1016/j.jiph.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Yang M., Chaghtai A., Melendez M., Hasson H., Whitaker E., Badi M., et al. Mitigating saliva aerosol contamination in a dental school clinic. BMC Oral Health. 2021;21(1):52. doi: 10.1186/s12903-021-01417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available from the corresponding author on reasonable request.
Data will be made available on request.