Abstract
Background
Conventional cannulated screws are commonly used for internal fixation in the treatment of vertical femoral neck fractures. However, the noticeably high rates of undesirable outcomes such as nonunion, malunion, avascular necrosis, and fixation failure still troubled the patients and surgeons. It is urgent to develop new cannulated screws to improve the above clinical problems. The purpose of this study was to design a novel magnesium-titanium hybrid cannulated screw and to further evaluate its biomechanical performance for the treatment of vertical femoral neck fractures.
Methods
A novel magnesium-titanium hybrid cannulated screw was designed, and the conventional titanium cannulated screw was also modeled. The finite element models for vertical femoral neck fractures with magnesium-titanium hybrid cannulated screws and conventional cannulated screws were respectively established. The hip joint contact force during walking gait calculated by a subject-specific musculoskeletal multibody dynamics model, was used as loads and boundary conditions for both finite element models. The stress and displacement distributions of the cannulated screws and the femur, the micromotion of the fracture surfaces of the femoral neck, and the overall stiffness were calculated and analyzed using finite element models. The biomechanical performance of the Magnesium–Titanium hybrid cannulated screws was evaluated.
Results
The maximum stresses of the magnesium-titanium hybrid cannulated screws and the conventional cannulated screws were 451.5 MPa and 476.8 MPa, respectively. The maximum stresses of the femur with the above different cannulated screws were 140.3 MPa and 164.8 MPa, respectively. The maximum displacement of the femur with the hybrid cannulated screws was 6.260 mm, lower than the femur with the conventional cannulated screws, which was 7.125 mm. The tangential micromotions in the two orthogonal directions at the fracture surface of the femoral neck with the magnesium-titanium hybrid cannulated screws were comparable to those with the conventional cannulated screws. The overall stiffness of the magnesium-titanium hybrid cannulated screw system was 490.17 N/mm, higher than that of the conventional cannulated screw system, which was 433.92 N/mm.
Conclusion
The magnesium-titanium hybrid cannulated screw had superior mechanical strength and fixation stability for the treatment of the vertical femoral neck fractures, compared with those of the conventional cannulated screw, indicating that the magnesium-titanium hybrid cannulated screw has great potential as a new fixation strategy in future clinical applications.
The translational potential of this article: This study highlights an innovative design of the magnesium-titanium hybrid cannulated screw for the treatment of vertical femoral neck fractures. The novel magnesium-titanium hybrid cannulated screw not only to provide sufficient mechanical strength and fixation stability but also to contribute to the promotion of fracture healing, which could provide a better treatment for the vertical femoral neck fractures, beneficially reducing the incidence of nonunion and reoperation rates.
Keywords: Biomechanics, Cannulated screws, Finite element analysis, Musculoskeletal multibody model, Vertical femoral neck fractures
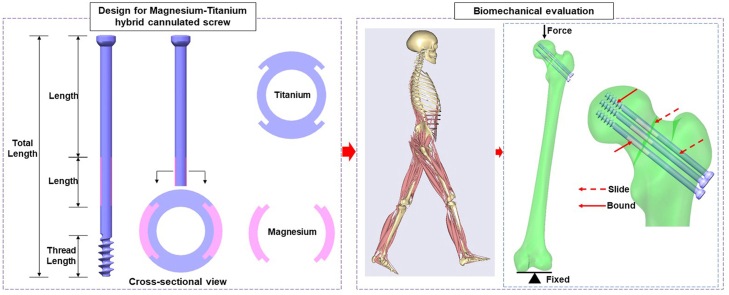
Graphical abstract
1. Introduction
Vertical femoral neck fractures (Pauwels type III) in young patients usually result from high-energy trauma and involve fracture lines with an angle exceeding 70° [[1], [2], [3]]. High shear forces make this type of fracture challenging to treat, requiring a more stable fixation and a more robust construct design for fracture healing [4]. The use of three parallel cannulated screws, placed in an inverted triangular configuration to fix the intermediate fragments, is a typical internal fixation approach for the treatment of vertical femoral neck fractures [[5], [6], [7]]. However, the treatment of vertical femoral neck fractures is associated with substantially high incidence of complications, including fixation failure, malunion or nonunion, and avascular necrosis due to the high shear forces and fixation instability [1,4,8,9]. Liporace et al. conducted a multicenter study with a follow-up of twenty-four months and found a nonunion rate of 19% (n = 61) for patients with high shear angle (>70°) femoral neck fractures fixed with cannulated screws [8]. Similarly, Campenfeldt et al. found that patients with displaced fractures (n = 120) had 23% nonunion and 15% avascular necrosis with a 28% reoperation rate; patients with non-displaced fractures (n = 50) had 12% radiographic avascular necrosis and 8% required reoperation [7]. These complications will result in poor functional outcomes and a high risk of reoperation and lifelong morbidity [1,10].
The majority of conventional cannulated screws are made of non-biodegradable stainless steel or titanium (Ti). The rigidity and biological inertness of these metal implants make it difficult to promote fracture healing and subsequent bone remodeling. Internal fixation implants consisting of magnesium (Mg) and its alloys are currently considered a new generation of degradable metallic biomaterials due to reports that they exhibit adequate mechanical characteristics, excellent biocompatibility and biodegradability, and osteopromotive effects during degradation [[11], [12], [13], [14], [15], [16]]. The Mg-based implants that are now being investigated for clinical use in skeletal sites that are not heavily loaded [14,15,17]. However, a significant barrier to their widespread clinical use continues to be the inadequate mechanical support for stable fracture fixation at the load-bearing sites as a result of the rapid degradation of pure Mg in the early post-implantation period.
Recently, Tian et al. developed an innovative Mg/Ti hybrid fixation system for fixation of long bone fractures in rabbits, which means that Ti plate/screw provides mechanical strength for fracture fixation while Mg screw shares the load and promotes fracture healing, found that the hybrid fixation system not only showed sufficient mechanical strength, but also improved fracture healing by up-regulating the local secretion of calcitonin gene-related peptide (CGRP) [18]. In addition, Luo et al. proposed the Mg-containing hybrid interference screw for anterior cruciate ligament (ACL) reconstruction, which means that the Ti-based interference screw with holes in the screw body allows the Mg rod to release the Mg ions through these holes to the surrounding bone tissue, thus exerting favorable biological effects while overcoming the concerns associated with insufficient mechanical strength [19]. These findings of the current proof-of-concept study implies that the innovative Mg–Ti hybrid system may help reduce delayed fracture healing and non-union rates for future clinical applications. However, very little has been reported in the literature as to whether there is an innovative Mg–Ti hybrid system that can accelerate fracture healing and non-union rates as well as provide sufficient mechanical strength for the femoral neck fractures.
Finite element analysis (FEA) has been used in most previous computational studies to investigate the biomechanical effects of internal fixation methods for femoral neck fractures using an estimated load input (2–3 times body weight (BW)) [2,5,20,21]. However, the estimated load does not accurately represent the body's maximum hip joint forces during normal walking gait. The magnitude of the load has a significant impact on the mechanical strength that the implants can bear, which further influences the design of the implants. Musculoskeletal multibody dynamics models, which delineate the body as an interconnected mechanical system of multiple rigid segments articulated by joints and actuated by muscles, constitute a robust platform for investigating the loading and kinematics [[22], [23], [24]]. In contrast to finite element models, musculoskeletal multibody dynamic models are capable of predicting joint forces and kinematics concurrently and accurately under various physiological activities [[25], [26], [27]]. The predicted joint loads and kinematics in an in vivo musculoskeletal physiological environment can be employed as boundary conditions for finite element models of femoral neck fractures.
Therefore, the objectives of the present study were to: 1) propose the innovative design of the Mg–Ti hybrid cannulated screws for the treatment of vertical femoral neck fractures, capable of providing sufficient mechanical strength while promoting fracture healing; 2) evaluate the impact of biomechanical performance between the Mg–Ti hybrid cannulated screws and the conventional cannulated screws by integrating the musculoskeletal multi-body dynamics and finite element methods.
2. Materials and methods
Experimental data collected from a healthy male adult volunteer (height: 179 cm, weight: 78.15 kg) with written informed consent were used in this study to develop the musculoskeletal multibody dynamics model and the finite element model. The ethics approval was approved by Hong Hui Hospital. The volunteer's computed tomography (CT) images of the entire lower extremity and gait data based on optical motion capture were collected. The three-dimensional model of the femur was created using the MIMICS image processing software (version 16.0; Materialise Mimics, Leuven, Belgium) and Geomagic Studio (version 2013; Geomagic, Research Triangle Park, NC). Gait trails, including one static standing trial and five normal walking trials, were measured using a 10-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA), and ground reaction forces and moments were measured using three force plates (AMTI Corporation, Watertown, MA).
2.1. Design of the Mg–Ti hybrid cannulated screw
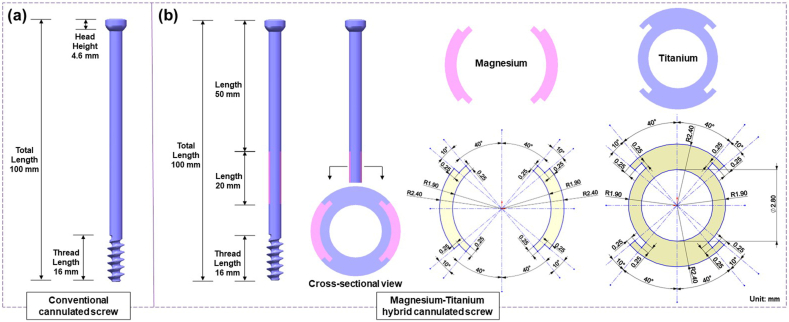
A novel Mg–Ti hybrid cannulated screw was designed, and the conventional cannulated screw was created using SolidWorks software (Dassault Systems SolidWorks Corp., Waltham MA) (Fig. 1). In the novel Mg–Ti hybrid cannulated screw, two 20 mm long Mg plates with a bilaterally symmetrical fan-shaped cross-section were embedded in the middle position of the Ti cannulated screw shaft, where the femoral neck fracture is located. The detailed design parameters were showed in Fig. 1.
Fig. 1.
Schematic diagram of the detailed design parameters for the Magnesium–Titanium hybrid cannulated screws and the conventional cannulated screws.
2.2. Biomechanical simulation of vertical femoral neck fractures
The three-dimensional models of vertical femoral neck fractures with a Pauwels angle of 70° (Pauwels type III) were created using SolidWorks software. The three-dimensional models of vertical femoral neck fractures were separately assembled with the Mg–Ti hybrid cannulated screws and the conventional annulated screws under the guidance of the surgical technique and the experienced surgeon [2,5,8,28]. The finite element models of vertical femoral neck fractures with the Mg–Ti hybrid cannulated screws and the conventional annulated screws were developed in Abaqus software (Abaqus 6.14; SIMULIA, Providence, RI, USA), respectively.
The femur, the Mg–Ti hybrid cannulated screw and the conventional cannulated screw were meshed using the four-node tetrahedral elements (C3D4) [5]. The mesh size of all components was determined by convergence studies and the quality of all components was further checked [29,30]. A change of under 5% was utilized as the convergence criterion [29,30]. A mesh size of 0.5 mm for the femur and a mesh size of was 0.2 mm for both the Mg–Ti hybrid cannulated screw and the conventional cannulated screw were considered to provide sufficiently accurate results. The femur, the Mg–Ti hybrid cannulated screw and the conventional cannulated screw had 12341561, 2121231, 1686946 elements, respectively.
The conventional cannulated screw was assigned a Young's modulus of 110 GPa and Poisson's ratio of 0.3 to represent Ti alloy [5,11]. The Mg–Ti hybrid cannulated screw was assigned a Young's modulus of 110 GPa and Poisson's ratio of 0.3 to represent the Ti alloy, and a Young's modulus of 44.8 GPa and Poisson's ratio of 0.35 to represent the high purity Mg, respectively [17,19]. Detailed data are listed in Table 1. The femur was assigned a Poisson's ratio of 0.3, while Young's modulus of each element in the finite element model was determined based on the average CT greyscale value (in Hounsfield Units, HU) of all voxels contained within the element volume using equations derived from previous studies [[31], [32], [33]], as described by the empirical equations below:
where ρ is the apparent dry density of the bone area of interest and HU is the radiographic greyscale of this area in HU [[32], [33], [34]].
where E is the Young's modulus assigned to the element and ρ is the dry apparent density of bone volume contained within the element [33,35,36].
Table 1.
Material properties for components in finite element models.
| Component | Material | Young's modulus (GPa) | Poisson's ratio |
|---|---|---|---|
| Femur | Bone | Based on CT greyscale value | 0.3 |
| Conventional cannulated screws | Titanium alloy | 110 | 0.3 |
| Titanium-magesium hybrid cannulated screws | Titanium alloy | 110 | 0.3 |
| High purity magnesium | 44.8 | 0.35 |
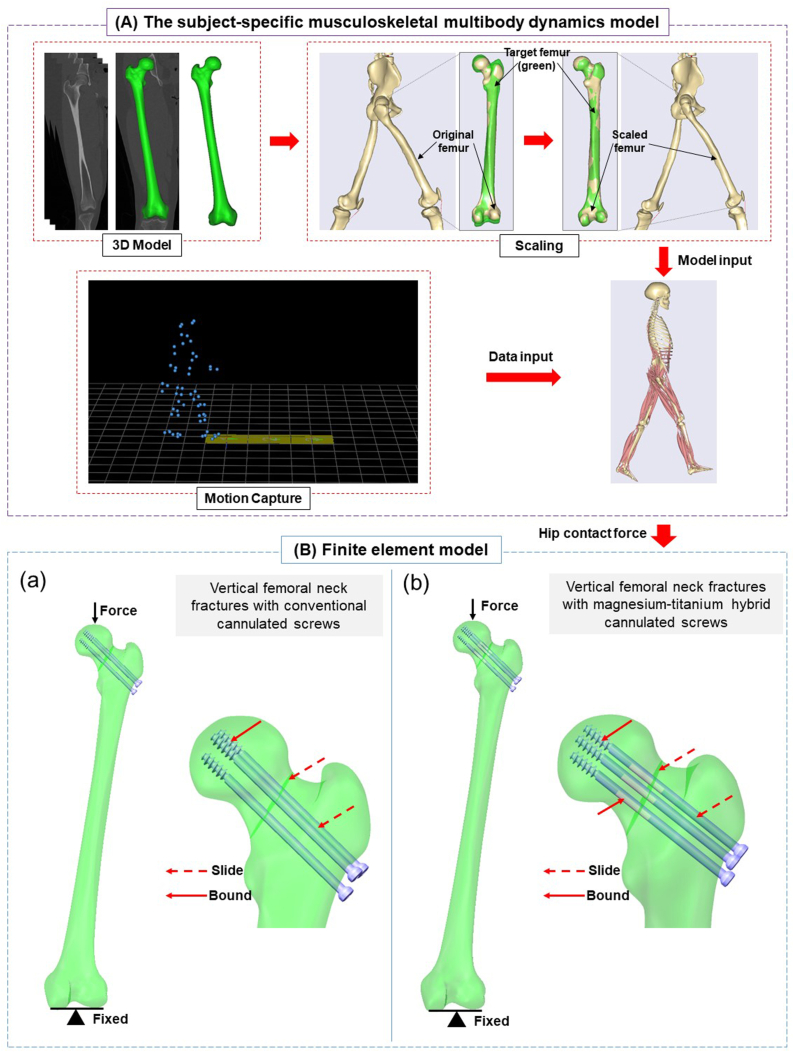
The coefficient of friction at the interface between the screw shaft and the femur was defined as 0.3, and the interface between two fracture surfaces of the femur was defined as a sliding contact with a coefficient of friction of 0.46 [2,5,37]. The screw thread was bonded to the femur [2,5]. Similarly, the Mg component and Ti component were bonded in the Mg–Ti hybrid cannulated screw (Fig. 2(B)). In addition, the six degrees of freedom of the distal femur were restricted [2]. The actual hip joint force (388 %BW), calculated from the subject-specific musculoskeletal multibody dynamics model (Fig. 2(A)), was applied uniformly along the mechanical axis of the femur to the weight-bearing area of the femoral head (Fig. 2 (B)).
Fig. 2.
The workflow of the subject-specific musculoskeletal multibody dynamics model and the finite element models for the Magnesium-Titanium hybrid cannulated screw system and the conventional cannulated screw system. A. The subject-specific musculoskeletal multibody dynamics model. B(a). The finite element models for the conventional cannulated screw system. B(b). The finite element models for the Magnesium-Titanium hybrid cannulated screw system.
A subject-specific musculoskeletal multibody dynamics model of lower extremity was developed using an advanced bone morphing method based on the CT scan of the subject in Anybody software (version 6.0; AnyBody Technology, Aalborg, Denmark) (Fig. 2(A)) [38,39]. The segments of entire musculoskeletal model and isometric strength of each muscle model were scaled to the subject's weight, height and gait data using the Length-Mass-Fat scaling method. An inverse kinematics method [40] was performed to calculate the pelvic motion, hip angles, and foot locations based on the walking gait data, the scaled musculoskeletal model, and the optimized marker locations [26,41]. These kinematics and ground reaction forces were then entered into the inverse dynamics analysis [26,41,42] to calculate the hip joint contact forces, which were further employed as loads and boundary conditions in the finite element models. The hip joint contact forces for the subject were presented as the mean ± standard deviation for five walking trials. Further details on the development and validation of the subject-specific musculoskeletal multibody dynamics model were available in our previous studies [22,23,26].
The stress/displacement distribution and the maximum stress/displacement of the cannulated screws and the femur as well as the micromotion of the fracture surfaces of the femoral neck were then calculated and analyzed using finite element models. Additionally, the overall stiffness (load divided by displacement, representing the overall stability) was calculated for both models [5].
3. Results
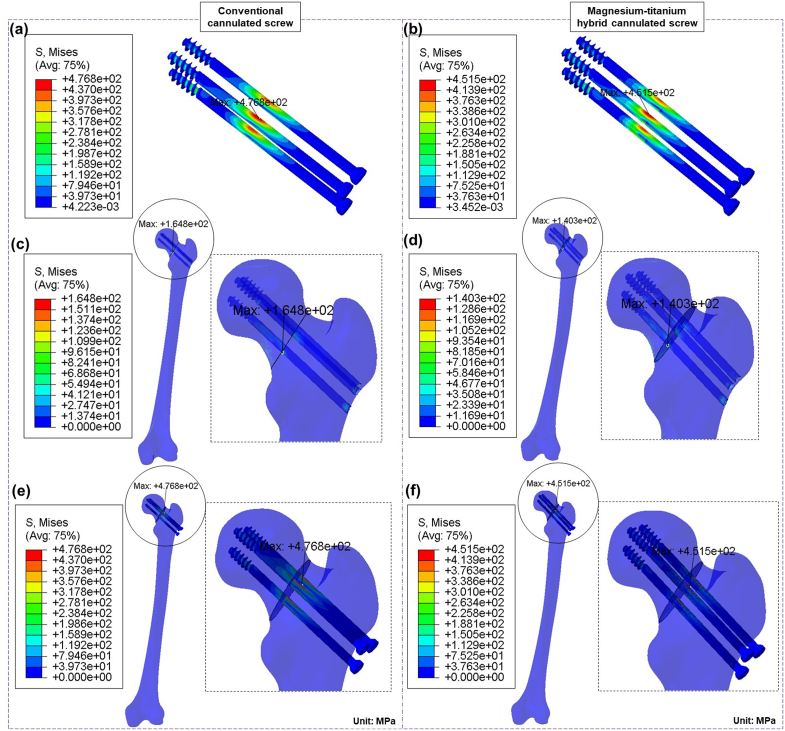
3.1. Stress and displacement
The Mg–Ti hybrid cannulated screws and the conventional cannulated screws both had similar stress distributions, as shown in Fig. 3. Compared to the conventional cannulated screws and the femur, which had maximum stresses of 476.8 MPa and 164.8 MPa, respectively, the Mg–Ti hybrid cannulated screws and the femur had maximum stresses of 451.5 MPa and 140.3 MPa, respectively (Fig. 3). In addition, the Mg plates of the Mg–Ti hybrid cannulated screws had a maximum stress of 154.6 MPa (Fig. 4(a)).
Fig. 3.
Stress distribution for the Magnesium-Titanium hybrid cannulated screw system and the conventional cannulated screw system. (a). Stress distribution for the conventional cannulated screws. (b). Stress distribution for the Magnesium-Titanium hybrid cannulated screws. (c). Stress distribution for the femur of the conventional cannulated screw system. (d). Stress distribution for the femur of the Magnesium-Titanium hybrid cannulated screw system. (e). Stress distribution for the femur and the conventional cannulated screws. (f). Stress distribution for the femur and the Magnesium-Titanium hybrid cannulated screws.
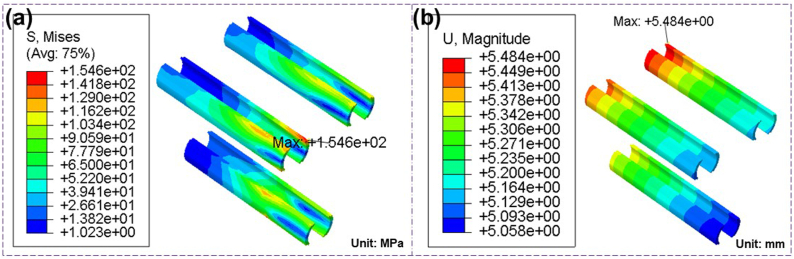
Fig. 4.
Stress and displacement distribution for the Mg plate of the Magnesium-Titanium hybrid cannulated screws. (a). Stress distribution for the Mg plate of the Magnesium-Titanium hybrid cannulated screws. (b). Displacement distribution for the Mg plate of the Magnesium-Titanium hybrid cannulated screws.
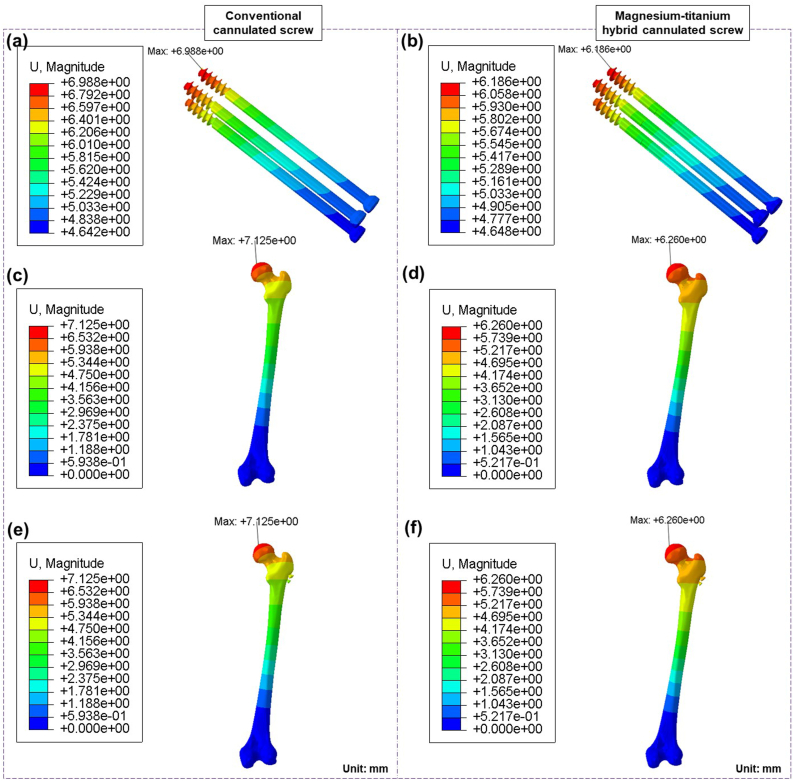
Similarly, the Mg–Ti hybrid cannulated screws and the conventional cannulated screws both had similar displacement distributions, as shown in Fig. 5. Compared to the conventional cannulated screws and the femur, which had maximum displacements of 6.988 mm and 7.125 mm, respectively, the Mg–Ti hybrid cannulated screws and the femur had maximum displacements of 6.186 mm and 6.260 mm, respectively (Fig. 5). In addition, the Mg plates of the Mg–Ti hybrid cannulated screws had a maximum displacement of 5.484 mm (Fig. 4(b)).
Fig. 5.
Displacement distribution for the Magnesium-Titanium hybrid cannulated screw system and the conventional cannulated screw system. (a). Displacement distribution for the conventional cannulated screws. (b). Displacement distribution for the Magnesium-Titanium hybrid cannulated screws. (c). Displacement distribution for the femur of the conventional cannulated screw system. (d). Displacement distribution for the femur of the Magnesium-Titanium hybrid cannulated screw system. (e). Displacement distribution for the femur and the conventional cannulated screws. (f). Displacement distribution for the femur and the Magnesium-Titanium hybrid cannulated screws.
3.2. Stiffness
The overall stiffness of the Mg–Ti hybrid cannulated screw system was 490.17 N/mm, while that of the conventional cannulated screw system was 433.92 N/mm (Table 2).
Table 2.
Comparison of biomechanical results between conventional cannulated screws and titanium-magnesium hybrid cannulated screws.
| Results | Model for conventional cannulated screws | Model for titanium-magnesium hybrid cannulated screws |
|---|---|---|
| The maximal Von mises stresses of screws (MPa) | 476.8 | 451.5 |
| The maximal Von mises stresses of femur (MPa) | 164.8 | 140.3 |
| The maximal shear stress of fracture (MPa) | 7.6 | 7.2 |
| The maximal displacement of screws (mm) | 6.988 | 6.186 |
| The maximal displacement of femur (mm) | 7.125 | 6.260 |
| Overall stiffness of cannulated screw system (N/mm) | 433.92 | 490.17 |
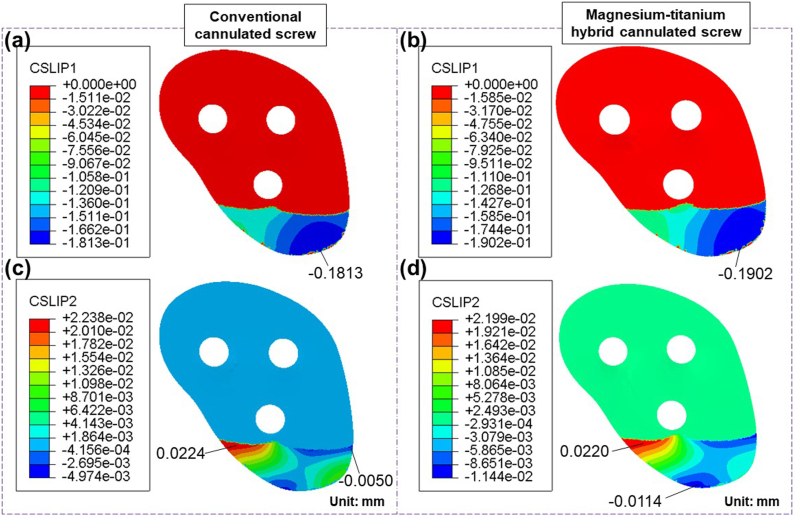
3.3. Micromotion
CSLIP1 and CSLIP2, which represent the tangential micromotions to the contact surfaces in the two orthogonal directions, are used to characterize the tangential micromotions of the fracture surfaces of the femoral neck [29]. Compared to the fracture surface of the femoral neck for the conventional cannulated screws, which was 0.1813 mm, the CSLIP1 in the fracture surface of the femoral neck for the Mg–Ti hybrid cannulated screws was 0.1902 mm (Fig. 6 (a) (b)). Similarly, compared to the fracture surface of the femoral neck for the conventional cannulated screws, which was 0.0224 mm, the CSLIP2 in the fracture surface of the femoral neck for the Mg–Ti hybrid cannulated screws was 0.0220 mm (Fig. 6 (c) (d)).
Fig. 6.
Tangential micromotion at the contact surfaces in the two orthogonal directions for the Magnesium-Titanium hybrid cannulated screw system and the conventional cannulated screw system. (a). Tangential micromotion at the contact surfaces for the conventional cannulated screw system. (b). Tangential micromotion at the contact surfaces for the Magnesium-Titanium hybrid cannulated screw system. (c). Tangential micromotion at the contact surfaces for the conventional cannulated screw system. (d). Tangential micromotion at the contact surfaces for the Magnesium-Titanium hybrid cannulated screw system.
4. Discussion
The most significant findings of the present study were that the biomechanical performance of the Mg–Ti hybrid cannulated screw designed for the treatment of vertical femoral neck fracture was validated. The maximum stress and the maximum displacement of the Mg–Ti hybrid cannulated screw system were lower than those of the conventional cannulated screw system. The overall stiffness of the Mg–Ti hybrid cannulated screw system was higher than that of the conventional cannulated screw system. In addition, the tangential micromotion at the contact surfaces in the two orthogonal directions was comparable between the Mg–Ti hybrid cannulated screw system and the conventional cannulated screw system.
To validate the finite element models of vertical femoral neck fractures, the same loading (1188.5 N) and boundary conditions were applied according to the previous study [5]. The results were in agreement with the results of the previous study (Table 3) [5], which can be a validation of the proposed finite element method in this study.
Table 3.
Finite element model validation.
| Finite element model | Maximum stress | Stiffness |
|---|---|---|
| The previous study [5] | 196.8 MPa | 428.15 N/mm |
| Intact model in this study | 188.9 MPa | 428.44 N/mm |
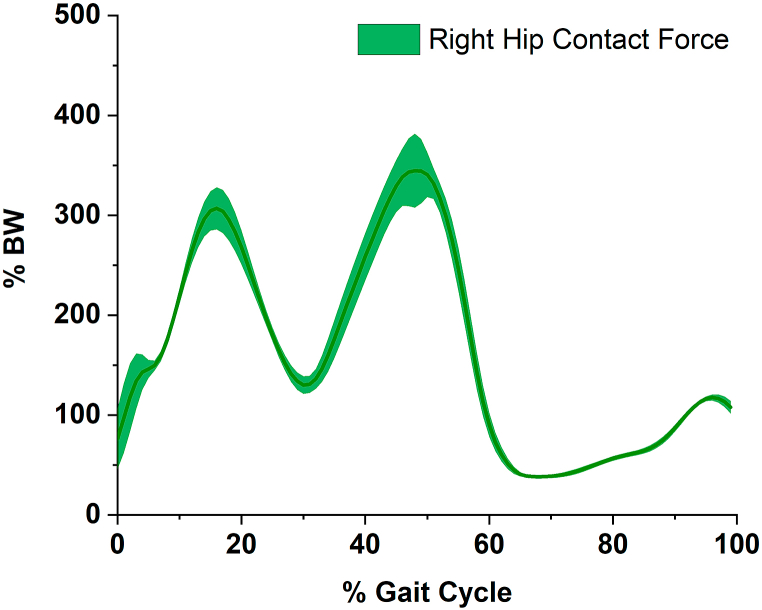
In the present study, the maximum hip joint force was 388% of BW at 50% of the walking gait cycle (Fig. 7), which was consistent with those found in our previous studies [43], and comparable to the studies of Hurwitz et al. [44]. and Lewis et al. [45]. Nevertheless, the estimated load (2–3 times body weight or 2100 N) used for the load input in the FEA method in the previous computational studies [2,5,20,46], which was lower than the result calculated by the musculoskeletal multibody dynamics model based on the subject's experimental data. Therefore, considering the higher hip joint force employed as the load input in the FEA method in the present study, the maximum stresses/displacements in the hybrid/conventional cannulated screw system were higher than those in the previous computational studies [2,5,12].
Fig. 7.
Right hip joint contact force during the walking gait cycle (the bold solid line represents the mean value, and the surrounding envelope represents the standard deviation value).
Similar stress and displacement distributions were found between the Mg–Ti hybrid cannulated screws and the conventional cannulated screws in the present study, as shown in Fig. 3, Fig. 5. However, the maximum stress and maximum displacement of the Mg–Ti hybrid cannulated screws were 451.5 MPa and 6.186 mm, respectively, lower than those of the conventional cannulated screws, which were 476.8 MPa and 6.988 mm, respectively. A possible explanation was that the structural modification in the Ti portion of the hybrid cannulated screw shaft would have a substantial impact on the stress and displacement distribution compared to the conventional cannulated screw. Furthermore, the Young's modulus of Mg plates was low, the difference of Young's modulus between the Mg plates of the hybrid cannulated screws and the femoral bone was small, and the stress concentration and the maximum stress in the hybrid cannulated screw system could be partially reduced in terms of the low Young's modulus of Mg plates and structural modification compared to the conventional Ti cannulated screws [12]. As a result, the hybrid cannulated screws improved the stress distribution of the fixation model, which further influenced the displacement distribution of the fixation model and reduced the maximum displacement. These findings indicated that the mechanical strength of the Mg–Ti hybrid cannulated screws was even superior to that of the conventional cannulated screws in terms of the stress and displacement distributions.
Similarly, the maximum stress and maximum displacement of the femur with the Mg–Ti hybrid cannulated screws were 140.3 MPa and 6.260 mm, respectively, lower than those of the femur with the conventional cannulated screws, which were 164.8 MPa and 7.125 mm, respectively. As discussed in the previous paragraph, the reason may be explained by the fact that the structural modification in the Ti portion and the low Young's modulus of the Mg plates in the hybrid cannulated screws significantly affected the stress and displacement of the cannulated screws, which in turn would further have an impact on the stress and displacement distribution of the surrounding bone. Therefore, the hybrid cannulated screw system could reduce the stress shielding of the fixation model and decrease the stress concentration at the interface between the cannulated screws and the surrounding bone in terms of the structural modification of the Ti portion and the low Young's modulus of the Mg plates compared to the conventional Ti cannulated screw system, which further influenced the displacement distribution of the femur and reduced the maximum displacement of the femur. These findings suggested that the femur with the Mg–Ti hybrid cannulated screws had lower stress and lower displacement (Fig. 3, Fig. 5) for the same hip joint force compared to the femur with the conventional cannulated screws, potentially reducing the incidence of the fixation failure and further lowering the reoperation rate.
The present study also found that the overall stiffness of the Mg–Ti hybrid cannulated screw system was 490.17 N/mm, higher than the conventional cannulated screw system, which was 433.92 N/mm (Table 2). Because the overall stiffness was inversely proportional to the displacement, the maximum displacement of the Mg–Ti hybrid cannulated screw system was lower than that of the conventional cannulated screw system. Therefore, the hybrid cannulated screw system exhibited higher overall stiffness compared to the conventional cannulated screw system. In addition, the tangential micromotions in two orthogonal directions at the fracture surfaces of the femoral neck for the Mg–Ti hybrid cannulated screws were 0.1902 mm and 0.0220 mm, respectively, comparable to those of the conventional cannulated screws, which were 0.1813 mm and 0.0224 mm (Fig. 6). This might be explained by the possibility that the interaction between the shear force of the fracture surfaces and the stress distribution of the cannulated screw system contributed to the comparable tangential micromotions in both cannulated screw systems. These findings revealed that the Mg–Ti hybrid cannulated screws could provide sufficient mechanical stability in femoral neck fractures to prevent secondary femoral neck fractures in terms of overall stiffness and micromotions.
Furthermore, the Ti portion of the Mg–Ti hybrid cannulated screws already offered sufficient mechanical strength and fixation stability for the treatment of vertical femoral neck fractures, thus the Mg plates do not require to provide mechanical support. More importantly, the primary purpose of the Mg–Ti hybrid cannulated screws treated for vertical femoral neck fractures was to promote bone healing through the Mg plates as opposed to the conventional cannulated screws, which solely provided mechanical fixation. Increasing evidence had revealed that Mg could promote fracture healing by inducing larger callus formation, enhancing endochondral ossification, accelerating the mineralization process, and bone remodeling [11,[17], [18], [19],47]. It was further confirmed that this unique Mg-induced osteogenic effect regulated by CGRP through the periosteum. The innovative design of the Mg–Ti hybrid cannulated screws in the present study fundamentally addressed the weaknesses of the conventional cannulated screws and pure Mg cannulated screws. In particular, the conventional cannulated screws have a relatively high incidence of nonunion and reoperation rates without the ability to promote fracture healing while having strong mechanical strength. On the contrary, pure Mg cannulated screws alone were unable to offer sufficient mechanical support for stable fracture fixation at load bearing sites due to its quick degradation in the early stages of implantation. Therefore, the innovative Mg–Ti hybrid cannulated screws provided a better treatment for the vertical femoral neck fractures, beneficially reducing the incidence of nonunion and reoperation rates.
Several limitations of this study should be discussed. First, the present work developed models to reflect the bone condition of young people using the subject's femoral CT data. Since the Mg–Ti hybrid cannulated screws were able to provide strong mechanical strength as well as promote fracture healing and bone remodeling, the biomechanical evaluation for the elderly patients and osteoporotic patients would be performed in the future study. Second, the most commonly used internal fixation method for the treatment of vertical femoral neck fractures was used to evaluate the biomechanical performance of the Mg–Ti hybrid cannulated screw during the normal walking gait. Different internal fixation strategies for the treatment of vertical femoral neck fractures under different types of gaits should also be evaluated in the future study. Third, the present study focused on initial mechanical stability rather than the entire bone healing process. Nevertheless, the initial stability of vertical femoral neck fractures had a significant impact on the fracture healing [48]. Fourth, the FEA method in the present study neglected the muscles attached to the femur, applying force solely along the mechanical axis of the femur. However, the FEA model used in this study was validated, and the results were consistent with those of a prior study [5]. The simultaneous acquisition of accurate measurements pertaining to the magnitude and location of muscles, ligaments, and contact forces in the human body or a patient presents a significant obstacle. Fifth, the biomechanical effect of screw axial orientation should be evaluated in future work. Finally, clinical studies of the Mg–Ti hybrid cannulated screw needed to be conducted and clinical outcomes should be evaluated in the future studies. Notwithstanding these limitations, the present study clearly indicated that the innovative Mg–Ti hybrid cannulated screw offered superior treatment for vertical femoral neck fractures.
5. Conclusion
This study designed and validated the biomechanical performance of the novel Mg–Ti hybrid cannulated screws for the treatment of vertical femoral neck fractures. The maximum stress and maximum displacement in the Mg–Ti hybrid cannulated screw system were lower than those of in the conventional cannulated screw system. The overall stiffness of the Mg–Ti hybrid cannulated screw system was higher than that of the conventional cannulated screw system. The tangential micromotion at the contact surfaces in the two orthogonal directions was comparable between the Mg–Ti hybrid cannulated screw system and the conventional cannulated screw system. These findings indicated that the innovative Mg–Ti hybrid cannulated screw for the treatment of vertical femoral neck fractures not only provide adequate mechanical strength and fixation stability, but also contribute to the promotion of fracture healing and the reduction of the nonunion rate. The innovative Mg–Ti hybrid cannulated screw has great potential as a new fixation strategy for future clinical applications.
Authorship
Category 1: Conception and design of study: Qida Zhang, Zhenxian Chen, Zhongmin Jin, Ling Qin; acquisition of data: Qida Zhang, Yinghu Peng, Zhenxian Chen; analysis and/or interpretation of data: Qida Zhang.
Category 2: Drafting the manuscript: Qida Zhang; revising the manuscript critically for important intellectual content: Zhenxian Chen, Zhongmin Jin, Ling Qin.
Category 3: Approval of the version of the manuscript to be published (the names of all authors must be listed): Qida Zhang, Yinghu Peng, Zhenxian Chen, Zhongmin Jin, Ling Qin.
Declaration of competing interest
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgments
This study was supported by “National Natural Science Foundation of China” [Grants number: 11902048, 52035012], and the Areas of Excellence Scheme (AoE/M402/20) under the Research Grant Council of Hong Kong.
Contributor Information
Qida Zhang, Email: zhangqida621@163.com.
Ling Qin, Email: lingqin@cuhk.edu.hk.
References
- 1.Shen M., Wang C., Chen H., Rui Y-f, Zhao S. An update on the Pauwels classification. J Orthop Surg Res. 2016;11(1):161. doi: 10.1186/s13018-016-0498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xia Y., Zhang W., Hu H., Yan L., Zhan S., Wang J. Biomechanical study of two alternative methods for the treatment of vertical femoral neck fractures - a finite element analysis. Comput Methods Progr Biomed. 2021;211 doi: 10.1016/j.cmpb.2021.106409. [DOI] [PubMed] [Google Scholar]
- 3.Bartonícek J. Pauwels' classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma. 2001;15(5):358–360. doi: 10.1097/00005131-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Ly T.V., Swiontkowski M.F. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am. 2008;90(10):2254–2266. [PubMed] [Google Scholar]
- 5.Jiang D., Zhan S., Wang L., Shi L.L., Ling M., Hu H., et al. Biomechanical comparison of five cannulated screw fixation strategies for young vertical femoral neck fractures. J Orthop Res. 2021;39(8):1669–1680. doi: 10.1002/jor.24881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhan S., Jiang D., Ling M., Ding J., Yang K., Duan L., et al. Fixation effects of different types of cannulated screws on vertical femoral neck fracture: a finite element analysis and experimental study. Med Eng Phys. 2021;97:32–39. doi: 10.1016/j.medengphy.2021.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Campenfeldt P., Hedström M., Ekström W., Al-Ani A.N. Good functional outcome but not regained health related quality of life in the majority of 20-69 years old patients with femoral neck fracture treated with internal fixation: a prospective 2-year follow-up study of 182 patients. Injury. 2017;48(12):2744–2753. doi: 10.1016/j.injury.2017.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Liporace F., Gaines R., Collinge C., Haidukewych G.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90(8):1654–1659. doi: 10.2106/JBJS.G.01353. [DOI] [PubMed] [Google Scholar]
- 9.Enocson A., Lapidus L.J. The vertical hip fracture - a treatment challenge. A cohort study with an up to 9 year follow-up of 137 consecutive hips treated with sliding hip screw and antirotation screw. BMC Muscoskel Disord. 2012;13:171. doi: 10.1186/1471-2474-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sterling R.S. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469(7):1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tian L., Tang N., Ngai T., Wu C., Ruan Y., Huang L., et al. Hybrid fracture fixation systems developed for orthopaedic applications: a general review. J Orthop Translat. 2018;16:1–13. doi: 10.1016/j.jot.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ding K., Yang W., Zhu J., Cheng X., Wang H., Hao D., et al. Titanium alloy cannulated screws and biodegradable magnesium alloy bionic cannulated screws for treatment of femoral neck fractures: a finite element analysis. J Orthop Surg Res. 2021;16(1):511. doi: 10.1186/s13018-021-02665-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao D., Huang S., Lu F., Wang B., Yang L., Qin L., et al. Vascularized bone grafting fixed by biodegradable magnesium screw for treating osteonecrosis of the femoral head. Biomaterials. 2016;81:84–92. doi: 10.1016/j.biomaterials.2015.11.038. [DOI] [PubMed] [Google Scholar]
- 14.Lee J.W., Han H.S., Han K.J., Park J., Jeon H., Ok M.R., et al. Long-term clinical study and multiscale analysis of in vivo biodegradation mechanism of Mg alloy. Proc Natl Acad Sci U S A. 2016;113(3):716–721. doi: 10.1073/pnas.1518238113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Windhagen H., Radtke K., Weizbauer A., Diekmann J., Noll Y., Kreimeyer U., et al. Biodegradable magnesium-based screw clinically equivalent to titanium screw in hallux valgus surgery: short term results of the first prospective, randomized, controlled clinical pilot study. Biomed Eng Online. 2013;12:62. doi: 10.1186/1475-925X-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y., Xu J., Ruan Y.C., Yu M.K., O'Laughlin M., Wise H., et al. Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat Med. 2016;22(10):1160–1169. doi: 10.1038/nm.4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J., Wu Y., Li H., Liu Y., Bai X., Chau W., et al. Magnesium alloy based interference screw developed for ACL reconstruction attenuates peri-tunnel bone loss in rabbits. Biomaterials. 2018;157:86–97. doi: 10.1016/j.biomaterials.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Tian L., Sheng Y., Huang L., Chow D.H., Chau W.H., Tang N., et al. An innovative Mg/Ti hybrid fixation system developed for fracture fixation and healing enhancement at load-bearing skeletal site. Biomaterials. 2018;180:173–183. doi: 10.1016/j.biomaterials.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Luo Y., Zhang C., Wang J., Liu F., Chau K.W., Qin L., et al. Clinical translation and challenges of biodegradable magnesium-based interference screws in ACL reconstruction. Bioact Mater. 2021;6(10):3231–3243. doi: 10.1016/j.bioactmat.2021.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J., Yin P., Zhang L., Chen H., Tang P. Medial anatomical buttress plate in treating displaced femoral neck fracture a finite element analysis. Injury. 2019;50(11):1895–1900. doi: 10.1016/j.injury.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Wang F., Liu Y., Huo Y., Wang Z., Zhang J., Xu M., et al. Biomechanical study of internal fixation methods for femoral neck fractures based on Pauwels angle. Front Bioeng Biotechnol. 2023;11 doi: 10.3389/fbioe.2023.1143575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Q., Chen Z., Zhang Z., Jin Z., Muratoglu O.K., Varadarajan K.M. Leveraging subject-specific musculoskeletal modeling to assess effect of anterior cruciate ligament retaining total knee arthroplasty during walking gait. Proc Inst Mech Eng H. 2020;234:1445–1456. doi: 10.1177/0954411920947204. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Q., Chen Z., Zhang J., Hu J., Peng Y., Fan X., et al. Insert conformity variation affects kinematics and wear performance of total knee replacements. Clin Biomech. 2019;65:19–25. doi: 10.1016/j.clinbiomech.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 24.Fischer M.C.M., Eschweiler J., Schick F., Asseln M., Damm P., Radermacher K. Patient-specific musculoskeletal modeling of the hip joint for preoperative planning of total hip arthroplasty: a validation study based on in vivo measurements. PLoS One. 2018;13(4) doi: 10.1371/journal.pone.0195376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu J., Chen Z., Xin H., Zhang Q., Jin Z. Musculoskeletal multibody dynamics simulation of the contact mechanics and kinematics of a natural knee joint during a walking cycle. Proc Inst Mech Eng H. 2018;232(5):508–519. doi: 10.1177/0954411918767695. [DOI] [PubMed] [Google Scholar]
- 26.Chen Z., Zhang Z., Wang L., Li D., Zhang Y., Jin Z. Evaluation of a subject-specific musculoskeletal modelling framework for load prediction in total knee arthroplasty. Med Eng Phys. 2016;38(8):708–716. doi: 10.1016/j.medengphy.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 27.Tomasi M., Artoni A., Mattei L., Di Puccio F. On the estimation of hip joint loads through musculoskeletal modeling. Biomech Model Mechanobiol. 2023;22(2):379–400. doi: 10.1007/s10237-022-01668-0. [DOI] [PubMed] [Google Scholar]
- 28.Florschutz A.V., Langford J.R., Haidukewych G.J., Koval K.J. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–129. doi: 10.1097/BOT.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y., Chen Z., Zhao D., Yu J., Ma X., Jin Z. Articular geometry can affect joint kinematics, contact mechanics, and implant-bone micromotion in total ankle arthroplasty. J Orthop Res. 2023;41(2):407–417. doi: 10.1002/jor.25381. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Y., Chen Z., Hongmou Z., Zhao D., Zhang X., Ma X., et al. Comparison of joint load, motions and contact stress and bone-implant interface micromotion of three implant designs for total ankle arthroplasty. Comput Methods Progr Biomed. 2022;223 doi: 10.1016/j.cmpb.2022.106976. [DOI] [PubMed] [Google Scholar]
- 31.Sopher R.S., Amis A.A., Calder J.D., Jeffers J.R. Total ankle replacement design and positioning affect implant-bone micromotion and bone strains. Med Eng Phys. 2017;42:80–90. doi: 10.1016/j.medengphy.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McBroom R.J., Hayes W.C., Edwards W.T., Goldberg R.P., White A.A., 3rd Prediction of vertebral body compressive fracture using quantitative computed tomography. J Bone Joint Surg Am. 1985;67(8):1206–1214. [PubMed] [Google Scholar]
- 33.Snyder S.M., Schneider E. Estimation of mechanical properties of cortical bone by computed tomography. J Orthop Res. 1991;9(3):422–431. doi: 10.1002/jor.1100090315. [DOI] [PubMed] [Google Scholar]
- 34.Tuncer M., Hansen U.N., Amis A.A. Prediction of structural failure of tibial bone models under physiological loads: effect of CT density-modulus relationships. Med Eng Phys. 2014;36(8):991–997. doi: 10.1016/j.medengphy.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Keyak J.H., Lee I.Y., Skinner H.B. Correlations between orthogonal mechanical properties and density of trabecular bone: use of different densitometric measures. J Biomed Mater Res. 1994;28(11):1329–1336. doi: 10.1002/jbm.820281111. [DOI] [PubMed] [Google Scholar]
- 36.Morgan E.F., Bayraktar H.H., Keaveny T.M. Trabecular bone modulus-density relationships depend on anatomic site. J Biomech. 2003;36(7):897–904. doi: 10.1016/s0021-9290(03)00071-x. [DOI] [PubMed] [Google Scholar]
- 37.Zeng W., Liu Y., Hou X. Biomechanical evaluation of internal fixation implants for femoral neck fractures: a comparative finite element analysis. Comput Methods Progr Biomed. 2020;196 doi: 10.1016/j.cmpb.2020.105714. [DOI] [PubMed] [Google Scholar]
- 38.Damsgaard M., Rasmussen J., Christensen S.T., Surma E., de Zee M. Analysis of musculoskeletal systems in the AnyBody modeling system. Simulat Model Pract Theor. 2006;14(8):1100–1111. [Google Scholar]
- 39.Pellikaan P., van der Krogt M.M., Carbone V., Fluit R., Vigneron L.M., Van Deun J., et al. Evaluation of a morphing based method to estimate muscle attachment sites of the lower extremity. J Biomech. 2014;47(5):1144–1150. doi: 10.1016/j.jbiomech.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 40.Andersen M.S., Damsgaard M., MacWilliams B., Rasmussen J. A computationally efficient optimisation-based method for parameter identification of kinematically determinate and over-determinate biomechanical systems. Comput Methods Biomech Biomed Eng. 2010;13(2):171–183. doi: 10.1080/10255840903067080. [DOI] [PubMed] [Google Scholar]
- 41.Marra M.A., Vanheule V., Fluit R., Koopman B.H., Rasmussen J., Verdonschot N., et al. A subject-specific musculoskeletal modeling framework to predict in vivo mechanics of total knee arthroplasty. J Biomech Eng. 2015;137(2) doi: 10.1115/1.4029258. [DOI] [PubMed] [Google Scholar]
- 42.Andersen M., Rasmussen J. Proceedings of the international society of biomechanics conference. International Society of Biomechanics, ISB; 2011. Total knee replacement musculoskeletal model using a novel simulation method for non-conforming joints. [Google Scholar]
- 43.Zhang X., Chen Z., Wang L., Yang W., Li D., Jin Z. Prediction of hip joint load and translation using musculoskeletal modelling with force-dependent kinematics and experimental validation. Proc Inst Mech Eng H. 2015;229(7):477–490. doi: 10.1177/0954411915589115. [DOI] [PubMed] [Google Scholar]
- 44.Hurwitz D.E., Foucher K.C., Andriacchi T.P. A new parametric approach for modeling hip forces during gait. J Biomech. 2003;36(1):113–119. doi: 10.1016/s0021-9290(02)00328-7. [DOI] [PubMed] [Google Scholar]
- 45.Lewis C.L., Sahrmann S.A., Moran D.W. Effect of hip angle on anterior hip joint force during gait. Gait Posture. 2010;32(4):603–607. doi: 10.1016/j.gaitpost.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lin S., Shang J., Xing B., Wu B., Peng R., Wang G., et al. Modified F configuration in the treatment of Pauwels type III femoral neck fracture: a finite element analysis. BMC Muscoskel Disord. 2021;22(1):758. doi: 10.1186/s12891-021-04638-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang J.L., Xu J.K., Hopkins C., Chow D.H., Qin L. Biodegradable magnesium-based implants in orthopedics-A general review and perspectives. Adv Sci (Weinh) 2020;7(8) doi: 10.1002/advs.201902443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aminian A., Gao F., Fedoriw W.W., Zhang L.Q., Kalainov D.M., Merk B.R. Vertically oriented femoral neck fractures: mechanical analysis of four fixation techniques. J Orthop Trauma. 2007;21(8):544–548. doi: 10.1097/BOT.0b013e31814b822e. [DOI] [PubMed] [Google Scholar]