Abstract
Background/objective
Some refugee and migrant populations globally showed lower uptake of COVID-19 vaccines and are also considered to be an under-immunized group for routine vaccinations. These communities may experience a range of barriers to vaccination systems, yet there is a need to better explore drivers of under-immunization and vaccine hesitancy in these mobile groups.
Methods
We did a global rapid review to explore drivers of under-immunization and vaccine hesitancy to define strategies to strengthen both COVID-19 and routine vaccination uptake, searching MEDLINE, Embase, Global Health PsycINFO and grey literature. Qualitative data were analysed thematically to identify drivers of under-immunization and vaccine hesitancy, and then categorized using the ‘Increasing Vaccination Model’.
Results
Sixty-three papers were included, reporting data on diverse population groups, including refugees, asylum seekers, labour migrants and undocumented migrants in 22 countries. Drivers of under-immunization and vaccine hesitancy pertaining to a wide range of vaccines were covered, including COVID-19 (n = 27), human papillomavirus (13), measles or Measles-mumps-rubella (MMR) (3), influenza (3), tetanus (1) and vaccination in general. We found a range of factors driving under-immunization and hesitancy in refugee and migrant groups, including unique awareness and access factors that need to be better considered in policy and service delivery. Acceptability of vaccination was often deeply rooted in social and historical context and influenced by personal risk perception.
Conclusions
These findings hold direct relevance to current efforts to ensure high levels of global coverage for a range of vaccines and to ensure that marginalized refugee and migrant populations are included in the national vaccination plans of low-, middle- and high-income countries. We found a stark lack of research from low- and middle-income and humanitarian contexts on vaccination in mobile groups. This needs to be urgently rectified if we are to design and deliver effective programmes that ensure high coverage for COVID-19 and routine vaccinations.
Keywords: vaccination, migrants, COVID-19 vaccines, vaccine hesitancy, refugees, vaccine uptake
Introduction
There are an estimated 1 billion people on the move globally (1 in 7 of the global population), with refugee and migrant populations known to have been disproportionately impacted clinically and socially by the COVID-19 pandemic.1–4 However, despite their increased risk from infection and potentially adverse outcomes, refugees and migrants have shown lower COVID-19 vaccination uptake in the few countries where this has been measured.5–10 For example, in a recent study of 465 470 migrants in the UK, uptake of the first dose was reported to be slower across all age groups for migrants compared with the general population, with this population more likely to not have received their second or third dose.11 Large country and regional differences in COVID-19 vaccine acceptance rates have been reported among all population groups.12 These data sets are a brief snapshot in time in what is a rapidly evolving field; however, they suggest that innovative strategies are likely needed to improve vaccination access and uptake in these populations in the immediate term as COVID-19 vaccines become more widely available globally (including through the COVAX Facility and the COVAX Humanitarian Buffer), alongside ongoing work to strengthen routine vaccination uptake in refugees and migrants in the longer term.13–15
In recent years, debates around vaccination acceptance and intent have become increasingly complex. The term ‘vaccine hesitancy’ has been defined by the WHO Strategic Advisory Group of Experts on Immunization (SAGE) Working Group on Vaccine Hesitancy as ‘the delay in acceptance or refusal of vaccination despite availability of vaccination services’16; it was in 2019 considered among the top 10 threats to global public health.17 Vaccine hesitancy is complex and highly variable in different contexts and over time,16,18,19 yet little focus to date has been placed on determinants of vaccine hesitancy in refugee and migrant populations. The ‘3Cs’ model describes vaccine hesitancy as being driven by the ‘3 Cs’: confidence (importance, safety, and efficacy of vaccines), convenience (access issues, dependent on the context, time and specific vaccines being offered) and complacency (perception of low risk and low disease severity).18,20 Researchers, however, have stressed the need to find better terms to clearly distinguish between vaccine hesitancy (focused around personal/psychological influences) and the other determinants of uptake, such as logistical problems and physical barriers to accessing vaccines, factors that will be particularly pertinent in refugee and migrant populations.21 The Increasing Vaccination Model, recently adapted by the WHO expert working group to measure behavioural and social drivers of vaccination (BeSD) to support more comprehensive planning and evaluation around vaccine uptake, brings together various models and frameworks into a working model to conceptualize drivers of under-immunization. It measures three domains that influence vaccine uptake: what people think and feel about vaccines; social processes that drive or inhibit vaccination (which both combine to influence individual motivations, or hesitancy, to seek vaccination); practical factors involved in seeking and receiving vaccination.22–24 The WHO expert working group has now begun the development of globally standardized tools for health policy makers and planners to measure and monitor reasons for under-immunization in real time, including for COVID-19.22,24
Refugees and migrants may face a range of unique personal, social and physical barriers to accessing health and vaccination services, which may influence vaccine motivation, and evidence shows that they are an under-immunized group for routine vaccinations.6,13,25,26 This may be particularly so among refugees and migrants who are new to the host country, those with precarious immigration status and those residing in camps and detention facilities who may be excluded from mainstream health and vaccination systems.2,13 Drivers of under-immunization and hesitancy may include difficulty understanding the local healthcare system, language barriers, discrimination or racism, and real, restricted or perceived lack of entitlement to free vaccinations, low trust in health systems, cultural barriers and/or being unable to afford direct or indirect costs.6,14,27–33 One systematic review exploring the role of refugees and migrants in outbreaks of vaccine-preventable diseases in Europe reported a high number of outbreaks among adult and child migrants in temporary refugee and migrant camps, linked to lack of access to mainstream vaccination systems.26 Some refugee and migrant populations will face specific barriers to public health messaging that will impact on vaccine motivation,33–37 with a subsequent impact on vaccination uptake in some communities.35 Data on uptake and drivers of under-immunization are often lacking in these populations, and there may be important differences between refugees and migrants residing in high-income, compared to low- and middle-income settings or in specific humanitarian contexts (including closed camp settings or detention centres), for example, that are yet to be fully elucidated. This suggests that that more research is urgently needed to explore and assess drivers of under-immunization and vaccine hesitancy in diverse refugee and migrant populations globally to define evidence-based solutions to support COVID-19 vaccine roll-out.
Methods
We did a rapid review of published and grey literature pertaining to refugee and migrant communities globally. Where relevant, we drew on guidelines developed by the Joanna Briggs Institute for scoping reviews,38 as well as the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist,39 due to a lack of formalized guidelines for rapid reviews, as well as the Interim Guidance from the Cochrane Rapid Reviews Methods Group.40
Inclusion and exclusion criteria
We collected global published literature pertaining to drivers of under-immunization and vaccine hesitancy in refugees and migrants for all vaccines including low-skilled labour migrants, asylum seekers, undocumented migrants, migrant healthcare workers and others, residing in all low-, middle- and high-income countries, and including humanitarian settings.
We defined vaccine hesitancy as ‘the delay in acceptance or refusal of vaccination despite availability of vaccination services’16,41 Refugees are defined in the Convention and Protocol Relating to the Status of Refugees as ‘persons outside their countries of origin who are in need of international protection because of feared persecution, or a serious threat to their life, physical integrity or freedom in their country of origin as a result of persecution, armed conflict, violence or serious public disorder’ (see https://www.unhcr.org/3b66c2aa10 and https://www.unhcr.org/master-glossary.html). We defined a migrant as an individual born outside of their current country of residence (see https://publications.iom.int/system/files/pdf/iml_34_glossary.pdf); however, where this information was not available in the literature, first language, nationality or the paper’s own definition of a migrant were used as a proxy, to avoid excluding relevant literature. Articles published between 1 January 2010 and 5 April 2022 were eligible for inclusion, with no restrictions on language. Articles focusing on drivers of under-immunization and vaccine hesitancy in the wider population with results not disaggregated by legal status were excluded. Papers were not excluded based on study type, and opinion pieces, commentaries, guidelines, policy briefs and review articles were eligible for inclusion where they met our inclusion criteria.
Search strategy
We searched MEDLINE, Embase, Global Health PsycINFO and WHO’s Global research on COVID-19 database (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov) for literature pertaining to drivers of under-immunization and vaccine hesitancy in migrant populations globally. The search strategy used keywords relating to migrant populations, vaccine hesitancy and barriers to vaccination (Supplementary material 1). Subsequently, grey literature sources were searched for, including through the following websites: World Health Organization (WHO), International Organization for Migration (IOM), European Centre for Disease Prevention and Control, Doctors of the World, Médecins sans Frontières (MSF), a variety of humanitarian and wider resources and websites (including the British Red Cross Community Engagement Hub, International Federation of the Red Cross (IFRC), International Organization for Migration (IOM), Reliefweb.org, UNICEF), as well as Google and Google Scholar. Experts from key countries and relevant organizations, such as UN institutions, non-governmental organizations (NGOs) and academics in the migrant health or vaccination fields were engaged through email, with a request for links to relevant documents, to gather further literature.
Data extraction, synthesis and analysis
Data were extracted by A.D., with S.H. duplicating data extraction in 50% of included papers. Qualitative content of included papers was analysed thematically to identify drivers of under-immunization and vaccine hesitancy, then categorized using WHO’s Increasing Vaccination Model, which describes the behavioural and social drivers of vaccination.23,24 This framework consists of three main pillars; ‘thinking and feeling’, described as personal confidence in vaccination, ‘social processes’, which refers to the social norms and factors that may influence motivation as well as ‘practical factors’, which describes physical barriers to access.22,24 Using Microsoft Excel, a standardized form was developed to extract data on the following: author and year of publication of study, study setting and location, study design, vaccine(s) studied (if concerned with a specific vaccine), number of participants (where relevant), refugee and migrant demographics (country of origin, legal status), age group (e.g. children, adolescents, adults), gender, drivers of vaccine hesitancy, and recommended strategies, solutions and best practices to strengthen uptake of vaccines.
Results
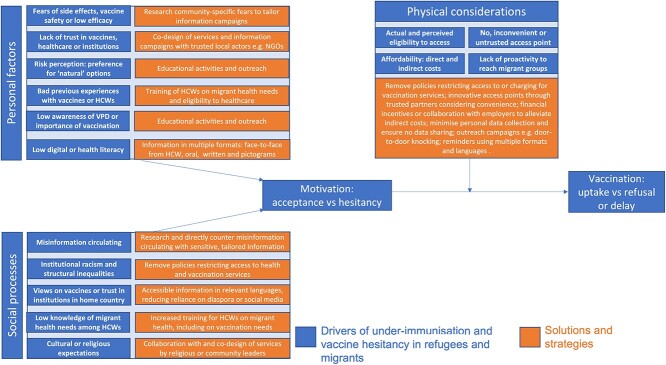
Our searches identified 737 records, of which 631 were identified as unique. After title, abstract and full-text screening, 63 papers were identified and included in this review (see Figure 1).
Figure 1.
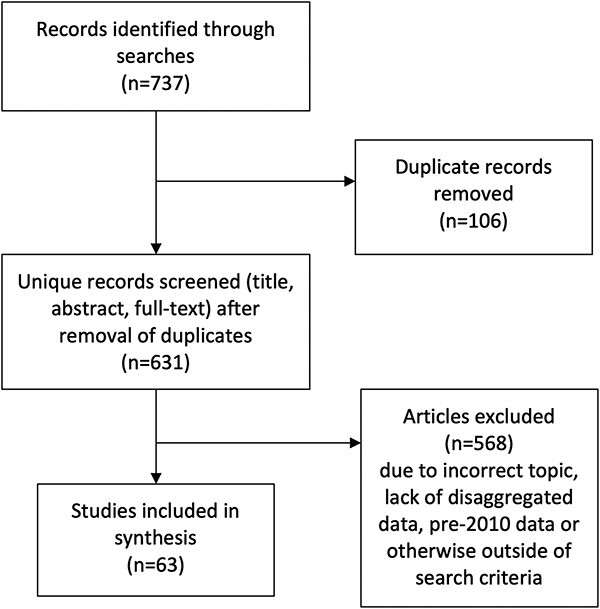
PRISMA diagram of included and excluded studies.
Included papers summarized in Table 1 reported data on migrants and refugees from 20 countries (Australia, Bangladesh, Canada, Denmark, France, Greece, Hungary, Italy, Japan, Lebanon, Netherlands, Norway, Poland, Qatar, South Korea, Sweden, Switzerland, UAE, USA, UK), with six papers reporting on a regional or global scale (Europe, Africa). Papers covered a wide range of specific vaccines, including COVID-19 vaccines (n = 27), human papillomavirus (HPV) vaccines (13), measles or MMR vaccines (3), influenza vaccines (3) and tetanus vaccines (1), with other papers focusing on vaccination in general and/or childhood vaccines. Multiple migrant types, different nationality groups and contexts were covered in the included literature, including data pertaining to refugees, asylum seekers, labour migrants and undocumented migrants, in both community (urban and rural) and humanitarian settings.
Table 1.
Characteristics of included literature (n = 63)
| Year | Disease/vaccine | Study type | Country/region | Population | n | Context | Urban/rural/humanitarian | |
|---|---|---|---|---|---|---|---|---|
| Abba-aji | 2022 | COVID-19 | Systematic review | Global | Migrants generally | N/A | All | Mixed |
| Andrade | 2022 | COVID-19 | Questionnaire | UAE | Migrants generally | 426 | Community | Mixed |
| Aragones | 2016 | HPV | Qualitative: focus groups | USA | Latino immigrants | 36 | Community | Urban |
| Armocida | 2021 | COVID-19 | Opinion | Europe | All | N/A | Policy level | N/A |
| Artiga | 2021 | COVID-19 | Opinion | USA | Migrants generally | N/A | All | Mixed |
| Bentivegna | 2022 | COVID-19 | Community-based research | Italy | Migrants in informal settlements | 660–750 | Informal settlements | Humanitarian |
| Berardi | 2022 | COVID-19 | Policy analysis | Australia, Canada, Japan, South Korea, USA | Migrants generally | N/A | Policy level | Mixed |
| Campeau | 2019 | Measles | Qualitative: interviews | USA | Somali immigrants | N/A | Community | N/A |
| Chauhan | 2019 | Childhood vaccines | Evaluation of intervention | UK | Asylum-seeking children | 14 | Primary care | Urban |
| Clark | 2021 | COVID-19 | Opinion | USA | Migrants generally | N/A | Policy level | N/A |
| Crawshaw | 2021 | COVID-19 | Opinion | UK | Migrants generally | N/A | Policy level | N/A |
| Dailey | 2017 | HPV | Qualitative: interviews | USA | Somali parents | 20 | Community | Urban |
| Deal | 2021 | COVID-19 | Qualitative: interviews | UK | Refugees, asylum seekers, undocumented migrants | 32 | Community | Mixed |
| Diaz | 2021 | COVID-19 | Opinion | USA | Latinx | N/A | General | Mixed |
| El Salibi | 2021 | COVID-19 | Questionnaire | Lebanon | Syrian refugees | 1037 | Not stated | Humanitarian |
| Ganczak | 2021 | Childhood vaccines | Qualitative: focus groups | Poland | Ukrainian | 22 | Community | Urban |
| Gehlbach | 2021 | COVID-19 | Qualitative: focus groups | USA | Latinx | 55 | Community | Rural |
| Riccardo | 2012 | Childhood/all | Survey data | 22 Mediterranean countries | All | 22 countries | Country level | N/A |
| Godoy-Ramirez | 2019 | Childhood vaccines | Qualitative: interviews | Sweden | Undocumented migrants | 7 | Community | Urban |
| Gonzalez | 2021 | COVID-19 | Survey data | USA | Immigrant families | 550 | Community | Mixed |
| Gorman | 2020 | Influenza | Survey data | Scotland, UK | Polish migrants | 365 | Community | Mixed |
| Gorman | 2019 | HPV | Qualitative: focus groups | Scotland, UK | Polish migrants | 13 | Community | Urban |
| Grandahl | 2012 | HPV | Qualitative: focus groups | Sweden | Immigrant women | 50 | Community | Urban |
| Harmsen | 2015 | Childhood vaccines | Qualitative: focus groups | Netherlands | Immigrant parents | 33 | Community | Urban |
| Jalloh | 2018 | Childhood vaccines | Qualitative: focus groups | Bangladesh | Rohingya refugees | 25 | Refugee camp (Cox’s bazaar) | Humanitarian |
| Kim | 2015 | HPV | Qualitative: focus groups | USA | Korean migrants | 26 | Community | Urban |
| Kobetz | 2011 | HPV | Community-based participatory research, focus groups | USA | Haitian migrants | 41 | Community | Urban |
| Lin | 2022 | COVID-19 | Survey data | Canada | Migrants generally | 3522 | Community | Mixed |
| Louka | 2019 | Childhood/all | Questionnaire | Greece, Netherlands | Asylum seekers and refugees | 61 | Community and refugee camps | Humanitarian |
| Marek | 2018 | Childhood/all | Questionnaire | Hungary | Asylum seekers and refugees | 123 | Refugee reception centre | Humanitarian |
| McGeown | 2019 | Childhood/all | Evaluation of intervention | UK | Immunization commissioners | 262 GP practices | Primary care | Urban |
| Mellou | 2018 | Childhood vaccines | Evaluation of intervention | Greece | Refugee children | 3786 | Refugee camps | Humanitarian |
| Miller | 2020 | COVID-19 | Evaluation of intervention | USA | Migrant farm workers | 48 | Community | Rural |
| Netfa | 2020 | HPV | Systematic review | Global | Immigrant parents | 2206 | Mix | Mixed |
| Page | 2022 | COVID-19 | Questionnaire | France, Italy, Switzerland, USA | Undocumented migrants | 812 | Mix | Urban |
| Perry | 2019 | Childhood | Registry data | Wales, UK | Asylum-seeking children | 388 | Not stated | N/A |
| Ricco | 2016 | Tetanus | Questionnaire | Italy | Immigrant construction workers | 554 | Community | N/A |
| Rubens-Augustson | 2019 | HPV | Qualitative: interviews | Canada | HCWs | 10 | Primary care | Urban |
| Sim | 2011 | Influenza | Qualitative: interviews | Scotland, UK | Polish and Scottish pregnant women | 10 | Community | N/A |
| Tankwanchi | 2021 | All vaccines | Systematic Review | Global | Migrants generally | N/A | All | Mixed |
| Thomas | 2021 | COVID-19 | Opinion | USA | Migrants generally | N/A | All | Mixed |
| Tomlinson | 2013 | Childhood | Qualitative: interviews | UK | Somali women | 23 | Community | Urban |
| Truman | 2020 | Childhood | Survey | USA | Karen refugees | 120 | Community | Urban |
| Vita | 2019 | Childhood | Descriptive cross-sectional | Italy | Asylum seekers | 3941 | Asylum centres | N/A |
| Walker | 2021 | COVID-19 | Opinion | Africa | Migrants generally | N/A | All | Mixed |
| Wang | 2021 | COVID-19 | Literature review | Canada | Asian migrants | N/A | Community | N/A |
| Zehireva | 2021 | COVID-19 | Policy brief | USA | Migrants generally | N/A | Policy level | N/A |
| Jama | 2018 | MMR | Qualitative: interviews | Sweden | Somali mothers | 13 | Community | Urban |
| Jenness | 2021 | Measles | Registry data | Norway | Somali immigrants | 11 600 | Community | Mixed |
| Khodadadi | 2020 | HPV | Survey data | USA | Latina mothers | 317 | Community | Mixed |
| Pratt | 2020 | HPV | Qualitative: focus groups | USA | Somali adolescents | 34 | Community | Urban |
| Lockyer | 2021 | COVID-19 | Qualitative: interviews | UK | Range of nationalities | 20 | Community | Urban |
| Mupandawana | 2016 | HPV | Qualitative: interviews | UK | African parents | 10 | Community | Urban |
| Chadenier | 2011 | HPV | Questionnaire surveys | Italy | Foreign born mothers | N/A | Community | Urban |
| Bell | 2020 | Measles | Qualitative interviews | UK | Romanian women and key providers | 9 Romanian women; 33 providers | Community | Urban |
| Bell | 2019 | All, influenza | Qualitative interviews | UK | Romanian and Polish and HCWs | 30 migrants; 20 HCWs | All | |
| Suppli | 2018 | HPV, MMR | Nationwide register-based survey | Denmark | Girls of non-western mothers | N/A | All | All |
| Hellenic Red Cross | 2021 | COVID-19 | Questionnaire survey | Greece | Refugees, migrants from deprived areas | 569 refugees and migrants | Deprived areas | Humanitarian |
| RCCE Collective Service | 2021 | COVID-19 | Interim guidance | All | Refugees, Internally displaced people (IDPs), asylum seekers, stateless people, migrants, returnees | N/A | N/A | N/A |
| Khaled SM | 2021 | COVID-19 | Survey | Qatar | Migrants | 1038 migrants and non-migrants | N/A | N/A |
| Alabdulla M | 2021 | COVID-19 | Survey | Qatar | Migrants | 7821 migrants and non-migrants | N/A | N/A |
| WHO | 2021 | COVID-19 | Interim guidance | All | Refugees and migrants | N/A | N/A | N/A |
N/A = data not available.
Personal factors: what people think and feel about vaccines
Personal confidence in vaccines such as concerns about safety and side effects are often cited as key drivers of vaccine hesitancy among refugees and migrants,42–48 for example, a study of 1037 Syrian refugees in Lebanon found that COVID-19 vaccine refusal was significantly associated with negative perceptions about vaccine safety.45 A Canadian study showed that among those who were vaccine hesitant, a significantly higher percentage of migrants reported concerns about vaccine safety (71.3 vs 49.5% Canadian-born), side effects (66.4 vs 47.3%) and mistrust in vaccinations (12.5 vs 6.6%) as reasons for vaccine refusal.48 Risk perception has been shown to be important among migrant communities when making vaccination decisions,49 with the perceived dangers of vaccination weighed against complacency around either the need for vaccination50 or perceptions of danger relating to the specific vaccine-preventable disease.51 In some communities, preferences exist for ‘more natural’ or traditional options such as herbal remedies, avoiding human contact and reliance on our immune system.43,47 A study looking at influenza vaccine attitudes among Polish migrants in the UK found that participant complacency about flu risk was often weighed against trust in the healthcare system and trust in the vaccine (in terms of side effects) when making vaccination decisions.51 One study among refugees and migrants in deprived areas in Greece found that many (111 of 447) did not know whether the vaccine was effective in ending the pandemic, and 91 of 447 respondents did not think it was,52 and despite having various concerns about the COVID-19 vaccine specifically (side effects, low perception of risk etc.), they were generally supportive of vaccination more widely (314 of 447 believed vaccines were important for disease prevention).
Trust is a major factor in opinions on vaccination (both trust in vaccination itself, and the wider governance and healthcare system of the host country).33,46,51,53–55 In one UK study among Romanian women around measles vaccines, the active decline in vaccination was linked to distrust in healthcare services, which were partly rooted in negative experiences of healthcare in Romania and the UK.56 Research suggests that low trust among some refugee and migrant populations towards vaccination itself or vaccination systems could be solved by engagement49,57–60 with community/religious leaders, relevant NGOs and community groups.61 In-depth research should be done in advance to identify and engage with relevant actors, who should be chosen dependent on context.13
Data also suggest that an individual’s awareness and access to information, which are often dependent on their health and digital literacy, are important factors in vaccine hesitancy. For example, a systematic review on attitudes towards HPV vaccination in migrants found that attitudes often changed for the better once information was given,62 and low awareness about a vaccine or vaccine-preventable disease has been shown to be a key barrier to vaccination.63 Some refugee and migrant populations face specific barriers to information access, such as digital literacy or lack of technology,43,64 language barriers,13,34,42,43,50,54,64–67 poor doctor–patient communication,44,63,67,68 or a lack of information in an accessible and acceptable format,47,50,63,64,67 leading to low awareness. The evidence suggests that prior to a vaccination campaign, research should be done on what information is felt to be important among different groups.44,45,50,64,66,69 For example, many groups consider safety and efficacy data essential.43,70 Multiple formats should always be used to increase reach, and these should depend on the context.43 For example, a UK study reported that health visitors felt translated leaflets were not sufficient, as many refugees and migrants struggle with literacy.71 Kim et al. noted that, contrary to other studies of vaccination knowledge among US-based immigrants, Korean immigrants in the USA often did not receive or understand information disseminated through traditional media such as TV advertisements or radio.72 This shows the importance of information formats, distribution and languages being culturally appropriate and tailored to the target group53,69 based on local evidence and informed/co-designed by collaborations with local actors.13,43,44,47,50,59,61,63 Language barriers are often a problem among refugee and migrant groups, despite increased efforts in some health systems to combat this. In five countries (Australia, Canada, Japan, South Korea, USA), which all ran translated campaigns on COVID-19 vaccination, a lack of details in translated campaigns, inadequacy in the diversity of languages covered and delays in producing translated campaigns were consistently criticized as major hurdles in vaccinating refugees and migrants.73 Multiple languages should be used to disseminate vaccination information, both in written and other formats, e.g. interpreters present either virtually or in person to answer questions.13,53,66,67,73,74 Six included papers suggest that education programmes should be created for refugee and migrant communities in collaboration with trusted, relevant actors to ensure cultural acceptability and reach.60,67,72,74,75
Table 2 summarizes the factors contributing to low acceptability of vaccination and some proposed solutions arising from the research.
Table 2.
Factors contributing to low acceptability of vaccination, and proposed solutions
| Vaccine | Population | Factors contributing to low acceptability | Solutions, strategies, best practices proposed | |
|---|---|---|---|---|
| Andrade, UAE | COVID-19 | Migrants generally | Alienation from society, perceived ethnic discrimination, education levels | Educational campaigns, vaccine mandates, increased social integration |
| Aragones, USA | HPV | Latino immigrants | Lack of provider recommendation, fear of side effects | Need for tailored information, preferably from HCWs |
| Artiga, USA | COVID-19 | Migrants generally | Fear of side effects; language barriers to information; fear of links to immigration services | Tailored outreach and education; culturally appropriate information in range of languages; pop-up services to counter lack of trust |
| Berardi, multiple countries | COVID-19 | Migrants generally | Lack of details and language diversity in translated campaigns, requirement for undocumented migrants to register, exclusion from healthcare/welfare systems, stigmatization | effective community engagement for bidirectional communication and dialogue |
| Campeau, USA | Measles | Somali parents | Migration history and structural marginalization (which make it hard to trust medical providers) during resettlement, concerns about non-inclusive clinical research, beliefs in immunity as flexible and personalized (developed through encounters with germs, not through vaccination) influence vaccination decisions | Collective social and institutional change and resource redistribution |
| Crawshaw, UK | COVID-19 | Migrants generally | Doctor–patient relationships; language barriers; religious and cultural beliefs; structural inequities; susceptibility to misinformation; conflicting recommendations from country of origin; lack of inclusiveness in vaccination programmes | Participatory approaches, engagement and co-design of vaccination programmes/interventions; provide platforms for concerns to be shared without judgement; build trust through transparency |
| Dailey, USA | HPV | Somali parents | Fears of side effects, cultural beliefs, complacency about need for vaccine, lack of information on efficacy | Tailored, culturally appropriate communication needed with stress on health benefits of vaccination, oral information given by a GP/HCW important |
| Deal, UK | COVID-19 | Refugees, asylum seekers, undocumented migrants | Fears of side effects, misinformation circulating, lack of trust in authorities, fears over immigration checks, preference for ‘natural’ solutions, structural inequity, religious beliefs | Campaigns to increase trust in primary care and educate HCWs about migrant health needs; walk-in/pop-up vaccination centres in trusted places; tailored information in range of languages; avoid stigmatization; collaboration with community/religious groups or non-governmental organizations |
| El Salibi, Lebanon | COVID-19 | Syrian refugees | Fears of side effects or low vaccine safety, newness of vaccine, COVID-19 vaccine not essential, newness of vaccine, lack of confidence in vaccine efficacy, preference for ‘natural’ prevention methods (e.g. social distancing), lack of trust in the system | Information campaigns to counter misinformation, collaboration with community leaders, organizations and other key influencers to re-establish trust |
| Ganczak, Poland | Childhood | Ukrainian | Difficulty finding trusted information on vaccines, low trust in the system and vaccines in home country, misinformation circulating, fears around vaccine safety | Information on vaccination importance and safety to be given by HCWs, training needed to allow HCWs to do this accurately, translated information/material required |
| Gehlbach, USA | COVID-19 | Latinx farm workers | Distrust in the system and medicine, misinformation circulating, financial and social insecurity and inequality, lack of access to internet or other information sources, language barriers | Education in digital literacy; normalization of vaccination; engage community in decision making around service delivery and outreach; tailored information campaigns |
| Riccardo, EU | Childhood/all | Migrants generally | Lack of trust in authorities, cultural acceptability and fear of immunization | Advocate for decreasing inequalities in healthcare, involve and empower community health leaders; use cultural mediators; guidelines training and tools should be created for migrant sensitive advocacy and communication |
| Godoy-Ramirez, Sweden | Childhood | Undocumented migrants | Low trust in system; fear of side effects; instability meaning vaccination becomes a lower priority; previous bad experiences of host healthcare system | Education for HCWs on migrant health needs, efforts to restore trust in health system; greater focus on tailoring appropriate strategies to specific groups; interventions should be multi-component and dialogue based |
| Gonzalez, USA | COVID-19 | Immigrant families | Fears of side effects, unsure about vaccine efficacy or feel vaccination is not needed | Immigrants more likely than non-immigrants to trust local public health officials; use elected officials and religious leaders for vaccine information; culturally appropriate, tailored information of vaccine safety, efficacy and access points needed |
| Gorman, UK | Influenza | Polish migrants | Fear of side effects, influence of diaspora/home media; complacency around rare disease; distrust in new vaccines | Promote vaccination on social media through community-specific influencers; recruit HCWs from specific community |
| Gorman, UK | HPV | Polish migrants | Influence of distrust in home healthcare system; difficulty understanding UK health and vaccination system; communication and language barriers | Educate parents and HCWs, tailor information and ensure it is accessible and understandable; collaboration with community members |
| Jalloh, Bangladesh | Childhood | Rohingya refugees | Fear of side effects, preference for traditional treatments; religious beliefs; past experiences of vaccination in the camp; fears that ‘white’ humanitarian workers had ulterior motives behind vaccination | Information campaigns in religious or community meetings; collaboration with community and religious leaders; increased awareness and accommodation of religious or cultural barriers among HCWs |
| Kim, USA | HPV | Korean migrants | Worries about vaccine safety, peer opinions on vaccination | Recommendation by HCW or other authority (e.g. school) important, school-based education recommended or education in any other existing, familiar environment (e.g. church) |
| Kobetz, USA | HPV | Haitian migrants | Scepticism about vaccine efficacy; fear of side effects and safety; ambivalence; fears about newness of vaccine | Recommendation by doctor important; information and education about side effects and efficacy delivered through trusted sources e.g. community HCW |
| Lin, Canada | COVID-19 | Migrants generally | Fear of side effects, vaccine safety and mistrust in vaccination generally | Pro-active health communication, pop-up COVID-19 vaccine clinics via community- and faith-based organizations |
| Louka, Greece, Netherlands | Childhood/all | Asylum seekers | Vaccination not always considered important, particularly in country of resettlement (i.e. Netherlands) compared with transit countries (i.e. Greece) | Point of entry to Europe considered best timing for vaccination by asylum seekers; public healthcare system preferred as access point over NGOs; promotional work on vaccination important |
| Netfa, Global | HPV | Immigrant parents | Side effect and vaccine safety concerns; religious and cultural norms; feeling vaccination is not important or needed; distrust in medical provider/pharmaceutical companies | Negative attitudes often changed when information given; information in multiple languages; personal counselling in clinics; educational programmes |
| Page, multiple countries | COVID-19 | Undocumented migrants | Use of social media or community networks as vaccination information source | Community engagement and messaging in multiple languages |
| Perry, UK | Childhood | Asylum-seeking children | Lack of trust; language barriers with HCWs | None given |
| Ricco, Italy | Tetanus | Immigrant construction? Workers | Foreign-born more likely to see recommendation by local public health services as a reason to get vaccinated; more likely to state religious/personal belief as a reason to not | Foreign-born workers mostly received doses through occupational health teams |
| Sim, UK | Influenza | Polish pregnant women | Complacency about seriousness of vaccine-preventable diseases; fears around vaccine safety; concerns about being used as ‘guinea pigs’ | Provide translated, accessible information for range of literacy skills, assistance accessing face-to-face advice |
| Thomas, USA | COVID-19 | Migrants generally | Lack of investment in community partnerships | Integrate community groups and individuals into vaccination processes; including at leadership and decision-making levels |
| Tomlinson, UK | Childhood | Somali women | Risk perception: disease vs vaccine safety, fears of side effects, misinformation, peer opinions, religious concerns especially worry around gelatine content | Oral information from a Somali speaker; develop closer relationships between health providers and community; work with religious leaders |
| Truman, USA | Childhood/all | Karen refugees | Longer time spent in USA associated with more reluctance to vaccinate | Culturally fit interventions and education programmes recommended |
| Walker, Africa | COVID-19 | Migrants generally | Fears around hidden agendas of ‘the west’, misinformation, different policies about vaccination across countries (e.g. Tanzania, Madagascar) | Inclusion of community groups, religious leaders etc; sharing information online in migrant languages |
| Wang, Canada | COVID-19 | Asian migrants | Misinformation on social media; language and literacy barriers; mistrust in healthcare services; hesitancy among HCWs; systematic racism and mistrust | Incorporate cultural competency in healthcare; tailored information for preferred languages; directly address specific concerns; HCWs from migrant communities can aid communication |
| Jama, Sweden | MMR | Somali mothers | Fear of side effects (autism); bad previous experiences with HCWs; misinformation from word-of-mouth; stigmatization and feeling their views are not listened to by HCWs; peer opinions on vaccination | Interventions that focus on communication mechanisms; particularly through nurses |
| Jenness, Norway | Measles | Somali immigrants | More time in host country and urban location associated with lower uptake | Tailored strategies for community; social network analysis needed to identify influencers in communities to collaborate with; improved communication |
| Khodadadi, USA | HPV | Latina mothers | Low perceived risk of HPV associated with reluctance to vaccinate | Education and improvement of health literacy to increase risk awareness |
| Pratt, USA | HPV | Somali adolescents | Scepticism or fear about vaccines in general; religious and cultural norms; feelings of stigmatization | |
| Lockyer, UK | COVID-19 | Mix | Fear of side effects and vaccine safety; structural inequality and precarity, confusion and distrust in authorities and traditional media; conflicting or negative information from home country or social media, existing distrust in institutions | Systematic monitoring of misinformation on social media and responding sensitively; inform HCWs about circulating misinformation; harnessing connections with trusted community network; providing information in multiple languages |
| Grandahl, Sweden | HPV | Immigrant women | Communication barriers; cultural health norms, fears of side effects of low efficacy | Ensure availability of interpreter; more information required; translated invitation letters |
| Mupandawana, UK | HPV | African parents | Cultural and religious norms, complacency about VPD risk; risk perception, preferring natural prevention methods (abstinence); side effects, misinformation; distrust of ‘the West’ | Tailored information that addresses cultural and religious concerns; create smaller subgroups for targeted communication; video/story-based educational material, collaboration with religious or other leaders |
| Rubens- Augustson, Canada | HPV | HCWs | Language barriers; lack of appropriate information resources; cultural and religious factors; limited HCW time | Targeted health promotion e.g. in schools, ensuring access to appropriate personnel, culturally sensitive risk communication |
| Tankwanchi, Global | All | Migrants generally | Fears and misinformation about safety; limited knowledge of VPDs and vaccines; distrust of host health systems; language barriers; religious beliefs | Tailored, community-based immunization service delivery with migrant-friendly health systems and policies that affirm and protect human rights and dignity |
| Harmsen, Netherlands | All | Immigrant parents | Lack of time/information given to patients by HCWs; fear of side effects; language barriers; newness of vaccines | Information in own language; more oral information from HCWs or in specific educative meetings |
| Bell, UK | All | Polish and Romanian migrants | Expectations largely built on knowledge and experience from Poland and Romania; greater refusal of influenza vaccine due to perceptions around lack of efficacy | HCWs to explain how the health system works and clarify expectations; outreach to those facing barriers to healthcare; translated information; use pictograms or pictures; improve access to interpreting and translation services; use views and expectations of service users to shape services |
| Bell, UK | Measles | Romanian women and key providers | Concerns around vaccine safety; distrust in healthcare services, which were partly rooted in negative experiences of healthcare in Romania and the UK | Tackle cultural and linguistic barriers; strengthen provider–service user relationships; establish trust providers must find ways to connect with and develop a greater understanding of the communities they serve |
| Hellenic Red Cross | COVID-19 | Refugees and migrants in deprived areas | Do not think vaccines are effective in ending the pandemic; did not consider themselves at risk; side effects; not adequately informed about the vaccine; did not believe COVID-19 existed | Creation of information material with Q&A type information in all spoken languages; because respondents sourced information from the internet, provide robust sources of internet information; use a combination of information approaches—printed material, posters, community meetings; establish a COVID-19 handbook for all involved in vaccine delivery |
HCW = healthcare worker; GP = general practitioner.
Social processes: drivers or inhibitors of individual motivation to seek vaccination
Included research strongly suggests that the perceived acceptability of vaccines among refugee and migrant groups is highly dependent on context and social processes, including historical, economic, religious or political factors in different countries or regions.33 In some cases, migrant expectations may be built on knowledge and experience from their home countries.34 For example, a lack of trust in vaccines in a refugee and migrant’s country of origin, or the influence of factors from the home country or diaspora media can be an important factor in vaccine confidence in some groups.36,42,50,76 However, distrust of vaccination can also originate or worsen after arrival in the host country; for example, a study in the USA showed that among Karen refugees, a longer time spent in USA was associated with lower levels of perception that vaccinations were safe.75 Another study from Norway found that children born to mothers residing in Norway for >6 years had lower measles coverage compared to those residing <2 years prior to their birth, with coverage overall declining between 2000 and 2016.77 This could be due to social exclusion or alienation after arrival33,78 or precarity in resettlement,79 which have both been shown to negatively affect vaccine confidence in included papers. A study in the UK found that the more confused, distressed and mistrusting the participants felt during the COVID-19 pandemic, the more likely they were to be hesitant about uptake of the COVID-19 vaccine.42
Political and economic processes can also be important factors affecting motivation to vaccinate, as shown in two studies from Qatar, which found that migrant status was associated with lower levels of vaccine hesitancy and reluctance to accept a vaccine compared with Qatari nationals. The authors noted that migrants’ residency status in Qatar is tied to employment contracts, suggesting they will be more accepting of government or employer policy.80,81 Historical and structural racism in the host country can also influence motivation to vaccinate in migrant communities,42,61,64,79 for example, fears that certain ethnic groups or communities may be used as ‘guinea pigs’ in the COVID-19 vaccine roll-out,42,43,51,64 often originating from historical events (e.g. the Tuskegee study). In Africa, fears that there are hidden agendas of ‘the West’ behind vaccination campaigns are reported to be circulating, including among refugee and migrant groups.61 Interestingly, the same concerns around vaccines based on distrust in ‘the West’ were brought up by African refugees and migrants living in the UK,82 supporting the theory that home country context and diaspora media remain important factors in the perceived acceptability of vaccination.
Misinformation on vaccines can spread rapidly through social media or word of mouth and may have a strong influence on individual and community vaccine confidence, particularly in communities, such as many refugee and migrant communities, where distrust already exists and/or who have more limited access to robust public health information.42,43,64,83 Questionnaires of undocumented migrants in Paris, Rome, Baltimore and Milan have suggested that using social media or community networks as the preferred source of vaccination information was negatively associated with demand.84 A study in Bradford, UK, showed that rapid local and targeted responses to specific misinformation can be a solution and cited an example of a video produced by Bradford city council in Urdu and Punjabi that debunked a specific conspiracy story spreading in these local communities, which was reported to be effective.42
Religious norms or expectations are another key social process that may influence migrants’ motivation to vaccinate and have been previously shown affect perceived acceptability of vaccines.44,47,85 A study in Italy found immigrant workers more likely than non-immigration workers to state religious belief as a reason to not vaccinate85; another study of Lebanese immigrants in Australia found that religious values around health played a major part in vaccination decision making69 and a lack of female vaccinators (with male HCWs vaccinating females seen as unacceptable due to Islamic principle of purdah) was seen as a barrier to vaccination among Rohingya refugees in camps in Bangladesh.47 Collaboration with religious and cultural leaders is important,47 and education, outreach activities and tailored information campaigns should draw on specific religious values where appropriate for the target community.69 For example, Muslim communities may have concerns about whether vaccinations contain pork,49 which is a crucial factor to be addressed in communications.
Low knowledge of refugees and migrant health needs or of eligibility to healthcare among healthcare workers (HCWs) is another social process that may drive migrant motivation to vaccinate. HCWs were often considered the main expected source of information among refugees and migrants HCWs are often considered the main expected source of information among refugees,43,67,86,87 yet Rubens-Augustson showed in a qualitative interview study in Canada that HCWs working with migrants often feel that communication barriers and inability to address cultural or religious concerns restricted them in informing refugee and migrant patients about HPV vaccines.67 Education programmes for HCWs on working with refugee and migrant populations59,88 and on refugee and migrant entitlement to healthcare and vaccination43,67,86,87 were widely recommended in the literature, with one study showing increased uptake of catch-up vaccination in a centre for unaccompanied asylum-seeking children with increased awareness of migrant vaccination needs among HCWs.88
Table 3 describes a set of case studies showing the use of different strategies to overcome vaccine hesitancy in humanitarian settings.
Table 3.
Case studies for increasing vaccine acceptance in humanitarian settings
|
Case Study 1: A qualitative study44 with residents of Cox’s Bazaar refugee camp in Bangladesh found that a lack of sensitivity to cultural gender norms in the vaccination procedures (specifically, a lack of female HCWs to vaccinate women and girls), as well as fears that vaccines were being used by ‘white humanitarian workers’ to convert the local population to Christianity, were major barriers in a measles and diphtheria vaccination campaign. Engagement with local, particularly religious, leaders and faith-based messaging were suggested and subsequently used by the researchers. Case study 2: In Kenya, vaccine hesitancy within the government and national population, as well as misinformation about COVID-19 spread through social media and word of mouth in refugee camps, including rumours that international aid agencies are creating the virus to make money, have had a strong effect on populations living in refugee camps.58 In Dadaab camp, a radio host from the camp, known locally as the ‘Corona Guy’, has used his radio station with success to directly combat misinformation circulating in the camp and to create a dialogue with other camp residents. Case study 3: In Turkey, the government and partners conducted a mass vaccination campaign to provide missing doses of MMR and polio to 400 000 refugee and migrant children. Vaccines were delivered door-to-door in homes, communities and health centres by trained Syrian refugee doctors and nurses to bridge the language gaps and help build trust. Additional communication channels were used concurrently, including live radio broadcasts, mosques and local health centres.86 |
Physical considerations: the ability of individuals to be reached by, reach or afford recommended vaccines
Included papers described the accessibility of vaccination as potential driver of vaccine hesitancy among refugee and migrant populations, with migrant entitlement to health and vaccination systems in the host country a critical factor.57 In the context of the COVID-19 vaccine roll-out, it is as yet unclear in several countries the extent to which refugees and migrants will have access to vaccines based on migrant status, with a wide range in terms of the extent to which migrant entitlement is specifically mentioned in national vaccination policies globally. Particular concerns include undocumented migrants in several European countries where coverage is otherwise relatively high,6 as well as in humanitarian or low-income contexts, where there may be a lack of clear policy, structural vaccine shortages or specified lack of entitlement for migrants.89
Evidence suggests groups such as undocumented migrants residing in high-income countries may have fears about data sharing, immigration checks, lack of eligibility and other immigration-related concerns, highlighting that it is essential going forward for personal data collection associated with vaccination campaigns to be kept minimal and for undocumented migrants and for these groups to be offered access points where they feel safe from immigration enforcement.43,46,58,64,90 A study among migrants living in informal settlements in Italy showed that irregular migrants had the lowest COVID-19 vaccine coverage (15.7%) of all migrant groups (asylum seekers 28.9%, other residence permit 38.5%).55 A need to create awareness among migrant population, as well as HCWs, about their entitlement was reported43,46,59; perceived ineligibility for vaccination and/or free healthcare in the host country can contribute to hesitancy.43 Papers highlight several examples of good practice specifically around undocumented migrants and addressing barriers to vaccination: for example, some governments have removed healthcare entitlement barriers to testing and vaccination for COVID-19 or stated that vaccines will be available irrespective of residence status, and can be acquired anonymously with no links to immigration enforcement and the Colombian government has provided a 10-year temporary protection status to Venezuelan migrants, which will allow them to register for vaccination.6,13,91
Convenience of access points is often a key factor in vaccination decision-making among refugees and migrants, particularly those for whom losing a day of work to visit a distant vaccination centre may entail significant financial loss. Specific access points should be created, advised by and in collaboration with local actors58; for example, a US-based policy brief has recommended that legislation is passed to allow pharmacists to administer vaccines in underserved communities including migrant communities.92 Interventions that ‘take vaccination to migrants’ rather than expect migrants to present themselves for vaccines have historically had success: in Italy, migrant construction workers mostly received tetanus and diphtheria vaccines through occupational health as opposed to community-based primary care85 and a door-to-door vaccination programme for refugees in Greece in collaboration with local NGOs saw >20 000 childhood vaccination doses delivered.93 Good vaccine uptake was noted during an intervention offering on-farm COVID-19 vaccine to migrant farmworkers in the USA,94 and vaccination uptake was observed to be much higher in a migrant reception centre in Italy when doctors came to centre and gave vaccines when migrants arrived.95 In a paper by Chauhan et al., proactive contacting of migrants for their vaccinations was suggested to maximize uptake88 and Thomas et al. suggest proactivity in bringing vaccination to migrants rather than expecting them to present at vaccination services improved uptake.53 One of six recommendations suggested in one paper to increase uptake in migrants was to create a reminder system for specific vaccines in primary care, so that patients can be reminded of and offered their missing vaccinations when presenting for other reasons.67 One study from Denmark found that migrant girls were more likely than Danish-born girls to have HPV after receiving a reminder96; on the other hand, a study around measles vaccination in Romanian migrants in the UK found that the blanket approach of sending text message reminders appeared to be not that effective due to language and literacy barriers.56 The mobility of some migrant populations may need to be considered especially when multiple doses of vaccines are required,46,97 which may be an important issue in COVID-19 vaccine roll-out with most vaccines requiring two doses. A study among migrants living in informal settlements in Italy found that those who were in transit had significantly lower COVID-19 vaccine coverage.55 Population mobility in Greek refugee camps was overcome by door-to-door visits by staff from NGOs to actively record vaccination status within 2 weeks of each vaccination intervention.93
Several papers suggest that economic barriers and affordability of vaccines are also important in decision making for some refugees and migrants.43,50,55,56,60,65,67,70,98 This can include direct costs; for example, Louka et al. found that asylum seekers in Greece and the Netherlands became less likely to accept vaccination as the cost increased.60 In another report, discussing HPV vaccination in Canada, healthcare providers recommended publicly funding vaccination as a key facilitator to maximize uptake among refugees and migrants67; in a qualitative study in the USA, the majority of refugees and migrants interviewed responded positively when asked about HPV vaccine intent provided the vaccine be affordable. In Italy, foreign-born mothers were reported to be less likely to be willing or able to pay 100 Euros for their daughters to be vaccinated.65 In addition, a lack of clarity about charges for vaccination and/or healthcare may put migrants off seeking vaccination.56 Costs and other factors may influence where migrants choose to get vaccinated, with one UK study reporting Polish migrants returning home for cheaper vaccines (chicken pox) and/or after the birth of a child for routine vaccines, with numerous implications at a service provider level.34 Indirect costs, such as travel costs, and wages lost from time off work are also an important factor, particularly for groups with precarious status or working in low-skilled jobs. One paper on vaccination among Latinx immigrants in the USA suggested that workers from this group may not be given permission or time off to attend a COVID-19 vaccination appointment, and be unable to pay for transportation to distant vaccination sites, recommending that vaccination campaigns should educate employers to give employees time off for vaccination as well as ensuring that vaccination sites are easily accessible to underserved communities.90
Figure 2 summarizes key behavioural and social drivers of vaccination, and solutions and strategies to tackling it in the context of COVID-19 roll-out, compiled from the included literature in this review.
Figure 2.
Solutions and strategies for increasing COVID-19 vaccination uptake in refugee and migrant populations, based on the Increasing Vaccination Model22–24
Discussion
This review has compiled a wide range of literature pertaining to drivers of under-immunization and vaccine hesitancy in refugee and migrant populations, and solutions and strategies to addressing it. We found a stark lack of research from low- and middle-income countries and humanitarian contexts, a situation that needs to be urgently rectified as COVID-19 vaccine roll-out gathers pace beyond high-income countries. We found that there are a range of factors driving under-immunization and hesitancy in some refugee and migrant groups, with the acceptability of vaccination often deeply rooted in social and historical context and influenced by personal risk perception. Unique issues relating to awareness and access to vaccination for some refugee and migrant populations also influence vaccine motivation and need to be better considered in research, policy making and service delivery in the context of COVID-19 vaccination. There is an urgent need for more robust research on the influence of circulating misinformation on social media platforms, and the impact of information from other sources (e.g. diaspora media) on COVID-19 vaccine uptake in refugees and migrants. Lessons learned to date suggest that there are relatively simple solutions and strategies to improve COVID-19 vaccine uptake in refugees and migrants that will be context dependent, with a focus needed on meaningful community engagement, patient/provider interactions and building trust, strong risk communications, designing and delivering tailored information that is context and audience specific, and identifying innovative migrant-friendly access points.
Drivers of under-immunization and vaccine hesitancy in refugee and migrant populations are complex, multi-factorial and highly context dependent. Important contextual factors include economics and politics in the host country, particularly related to healthcare access, the precarity of specific migrant groups, cultural and religious norms around healthcare and vaccination, historical factors or structural racism in the host country as well as misinformation or vaccination norms from migrants’ home countries. WHO’s Tailoring Immunization Programmes framework99 and more recent Data for Action survey tools for COVID-1924 aim to support countries to assess and monitor vaccine hesitancy and low uptake in susceptible populations, recognizing that behaviours are complex, populations are diverse and that a ‘one size fits all’ approach will not work. These approaches stress the importance of doing robust research prior to any vaccination campaigns to identify key behavioural and social drivers of vaccination to vaccination and innovative strategies. Working to better understand how drivers of under-immunization and vaccine hesitancy in refugees and migrants impacts on vaccine uptake, as well as working more closely with affected communities, will ensure effective solutions are developed and delivered. Practical approaches to strengthening demand and uptake in refugees and migrants for COVID-19 vaccines have been outlined in a recent WHO Operational Guide (https://www.who.int/publications/i/item/WHO-2019-nCoV-immunization-demand_planning-refugees_and_migrants-2022.1). A summary of guidance documents suggesting policy actions for strengthening delivery and uptake of vaccination in refugees and migrants is available in Table 4.
Table 4.
Summary of policy actions to support strategies for COVID-19 vaccine roll out in refugees and migrants (adapted from91,102,106)
| √ Advocate for countries that are getting vaccines from COVAX and other sources, to explicitly include marginalized populations. Include refugees and migrants in all national, provincial and local contingency, prevention and response plans and interventions. √ Advocate for information systems to capture vaccination coverage data for refugees and migrants, while ensuring data protection. √ Advocate for inclusion and non-discriminatory access of refugees and migrants to public health services. √ Firewalls should be put in place to shield migrants in irregular situations from the possible transfer of their personal data to immigration authorities and the risk of facing immigration enforcement measures when they attempt to access healthcare services, including COVID-19 immunization. √ Research and plan appropriate communication on access to vaccinations in collaboration with communities themselves or local actors. Multiple communication strategies will be needed to address the different motivations and social and cultural practices behind vaccine acceptance and preferred communication channels. Diversify communication tools and format, and simplify messages; ensuring to test messages with target group. √ Strengthen the capacity of healthcare providers to identify opportunities to promote vaccination among refugees and migrants. Advocate for mobile vaccination points, expanded hours for vaccination services, increased mobilization of volunteer steward/vaccinator support services. √ Given the importance of primary healthcare services for refugee and migrant populations, consider advocating for primary health centres (PHCs) to be used as accredited vaccination centres, provided access would not lead to deportation. √ Ensure refugees and migrants receive precise information on vaccine side effects, due to their limited access to health providers for follow-up questions and services. √ Educate healthcare and frontline workers on how refugees and migrants can be stigmatized and encourage community action to prevent or mitigate stigma, particularly within vaccination points and health centres. √ Improve training and awareness of healthcare workers and other frontline works on the needs and cultural, religious and social perspectives of refugees and migrants. Involve the host community to defuse any potential conflict (vaccine nationalism discourse). √ Mobilize refugees and migrant-led organizations, and networks to have a meaningful role in COVID-19 response and vaccination rollout plans from their inception. If national healthcare workers are prioritized as part of vaccination rollout plans, advocate for refugee, migrant and IDP healthcare workers to also be prioritized to support rollout plans. √ Partner with these groups to identify barriers, enablers and behavioural factors, preferred and trusted communication channels, preferred languages, misinformation and questions about vaccination uptake. √ Practise bottom-up approaches in developing community engagement strategies to emphasize the participation of the local community in developing initiatives and to ensure community ownership, commitment and accountability. Engage existing volunteer groups to use their creativity to raise awareness. √ National vaccination policies need to adopt innovative measures for hard-to-reach populations living in conflict or in secured areas, and where centralized vaccination policies and implementation strategies may face additional barriers to building trust. √ In humanitarian settings, it is important to enter systematically into new partnerships with humanitarian actors who are already active in missed or under-vaccinated communities and have experience implementing vaccination campaigns. √ The demand for vaccines for refugees and migrants needs to be carefully synchronized with supply availability to ensure that doses are not wasted. Demand should not outstrip a country’s ability to administer/deliver the doses it receives and allocates to avoid eroding public trust. |
Our work has highlighted the importance of social processes and physical considerations in influencing vaccination motivation in some refugee and migrant populations, and that these processes are often unique to refugee and migrant populations—for example, a lack of entitlement to access the health and vaccination system in the host country, or lack of trust in institutions and institutional racism and other structural barriers. We have found that although concerns around vaccination or misinformation may travel with refugees and migrants from their home countries, or circulate in diaspora media or social groups, studies have also shown that refugees and migrants residing in the host country for longer are more likely to be hesitant towards vaccination, suggesting their hesitancy originates after migration due to precarity, structural inequalities or social exclusion in the host country. Cultural or religious norms were often also cited in included literature as important drivers of under-immunization and vaccine hesitancy in refugee and migrant populations, especially where these norms are not shared by the host country or host country health system. Key to tackling this is for countries to explore innovative refugee- and migrant-friendly access points for distribution of COVID-19 vaccines and ensure that HCWs and vaccine deliverers are trained about the unique needs of refugees and migrants.100
We have shown that personal factors affecting an individuals’ motivation to vaccinate often revolve around risk perception in refugee and migrant groups, with the perceived safety of the vaccine in question and trust in institutions and healthcare services, which is often based on previous experience. This is much in line with drivers of hesitancy in most populations, with risk perception based on concerns around vaccine safety and side effects usually stated as key factors in COVID-19 vaccine hesitancy generally.101 An individuals’ awareness of the vaccine, the risk associated with the specific vaccine-preventable disease and the importance of vaccination generally are also key factors affecting motivation, with low knowledge of any of these often associated with hesitancy. Multiple solutions were proposed in the included literature, often revolving around educational activities with specific community groups, co-design, and outreach and tailored information campaigns in a range of formats and languages. It is also important to acknowledge the role of the Western medical approach and the significance of recognizing the value of traditional medicine for patients and establishing a transdisciplinary approach to appropriately convey vaccine offerings. A recent Collective Service for Risk Communication and Community Engagement interim-guidance report on risk communication and community engagement for COVID-19 vaccines in marginalized groups stresses that advanced planning takes place to identify barriers to COVID-19 vaccines (considering gender and intersectoral needs, among others) and that it is essential that all new initiatives place community engagement at each point of the process because perceptions and information will change, and that preferred and trusted communication channels that meet a range of different communication needs are found and used.102
Greater consideration too must be given to new and rapidly evolving drivers of vaccine hesitancy globally, including the influence of social media-based communication as a major source of vaccine misinformation.103 One COVID-19 survey among refugees and migrants in Greece found that 275 of 447 respondents said their main source of information about COVID-19 disease was through social media.52 WHO has drawn attention to the challenge of the ‘infodemic’ or misinformation and disinformation pandemic in the context of COVID-19, calling for universal access to credible health information and efforts to tackle these important new challenges. Specific misinformation should be directly addressed in communities where it is known to be circulating, using sympathetic and transparent messaging in a range of formats and languages. The IFRC has recently developed a series of resources to tackle rumours and misinformation circulating in communities, an information pack on effectively listening and responding to communities around COVID-19 and ensuring feedback mechanisms are in place, including a survey to gain specific data at a community level on individual’s perceptions of COVID-19 vaccination and barriers to access.104
These findings hold direct relevance to efforts to ensure high levels of global vaccine coverage for COVID-19 and routine vaccination and highlight the urgent need for a concerted international effort to understand, analyse and overcome vaccine hesitancy. The limitations of this research include that, as a rapid review, quality assessments were not done for included literature; therefore, the quality of the available evidence is not certain. It is also important to note that the scope of the results presented is limited by the availability and quality of published literature, in which we have identified major gaps, such as the availability of published data on vaccine hesitancy in migrants from LMICs. Based on the evidence we have, it was not possible to explore in-depth the similarities and differences between diverse settings and regions of the world, and solutions and strategies are also not necessarily generalizable between countries, regions or migrant groups and only a few of them are ever robustly tested to explore their effectiveness on actually increasing vaccine uptake.
Further research is warranted that places greater emphasis on better understanding vaccination motivation and barriers to vaccination in refugees and migrants, and robustly tests strategies and solutions to better understand their effectiveness in increasing uptake (Table 5). Renewed efforts and investment must be placed on supporting countries to collect, analyse and source disaggregated data pertaining to vaccination and migration. The near complete absence of vaccine uptake data for COVID-19 vaccination in most high-income countries, with which to inform real-time evidence-based service delivery, is a stark reminder of how just how invisible refugee and migrant populations still are, a situation that now needs to be urgently rectified if we are to improve health outcomes in these groups and meet the regional and global goals of WHO’s new Immunisation Agenda 2030.105 Of key importance now is to ensure marginalized refugee and migrant populations are specifically included in national vaccine-delivery plans of low-, middle- and high-income countries, through initiatives including the COVAX Facility and the COVAX Humanitarian Buffer as a last resort, as we advocate for more rapid roll-out of COVID-19 vaccines in low- and middle-income countries and humanitarian settings and promote global vaccine equity.
Table 5.
Recommendations for further research into vaccine confidence and uptake among migrant groups
| √ Generate evidence to more fully understand drivers of under-immunization and vaccine hesitancy in diverse migrant populations in low- and middle-income countries and in humanitarian contexts globally (including closed settings such as migrant camps and detention centres). √ Explore and assess the influence of social media-based communication as a new and major source of vaccine misinformation in marginalized populations with less access to robust public health messaging, including the extent to which certain nationalities and marginalized groups are being specifically targeted. √ Better understand the role of diaspora media, and a migrant’s links to their country of origin, and how this may specifically influence their views around a specific vaccine or vaccine-preventable disease. Factor this into the development of specific strategies to improve vaccine uptake. √ Address the major gap in research to measure the impact of refugees’ and migrants’ attitudes and knowledge around vaccination and various social process and physical barriers on subsequent uptake of vaccines, and the extent to which initiatives are effective in increasing uptake of a specific vaccination. √ Better define the role of healthcare workers and employers, and appropriate communication strategies that could be adopted, to drive vaccine uptake for COVID-19. √ Renewed efforts and investment must be placed on supporting countries to collect, analyse and source refugee- and migrant-disaggregated, gender-disaggregated and local-level data pertaining to vaccine hesitancy and its impact on vaccination uptake/coverage in refugee and migrant populations. |
Funding
This research was funded by the Department of Foreign Affairs, Trade and Development (DFATD), Canada. A.D. is funded by the Medical Research Council (MRC/N013638/1). S.H. is funded by the National Institute for Health Research (NIHR300072, NIHR134801), Research England, the Academy of Medical Sciences (SBF005\1111) and the La Caixa Foundation, and acknowledges funding from the MRC and WHO.
Author contributions
Anna Deal (Data curation [equal], Formal analysis [lead], Writing—original draft [equal]), Alison Crawshaw (Formal analysis [supporting], Writing—review & editing [equal]), Jessica Carter (Writing—review & editing [equal]), Felicity Knights (Writing—review & editing [equal]), Michiyo Iwami (Writing—review & editing [equal)], Mohammad Darwish (Formal analysis [supporting], Writing—review & editing [equal]), Rifat Hossain (Writing—review & editing [equal]), Palmira Immordino (Conceptualization [equal], Writing—review & editing), Kanokporn Kaojaroen (Conceptualization [equal], Writing—review & editing [equal]), Santino Severoni (Conceptualization [equal], Writing—review & editing [equal]), and Sally Hargreaves (Conceptualization [equal], Writing—review & editing [equal]).
Conflict of interest: None declared.
Data availability
Primary data from this study is available from authors on reasonable request.
Supplementary Material
Contributor Information
Anna Deal, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK; Department of Public Health and Policy, London School of Hygiene and Tropical Medicine, London, UK.
Alison F Crawshaw, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK.
Jessica Carter, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK.
Felicity Knights, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK.
Michiyo Iwami, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK.
Mohammad Darwish, The Health and Migration Programme, World Health Organization, Geneva, Switzerland.
Rifat Hossain, The Health and Migration Programme, World Health Organization, Geneva, Switzerland.
Palmira Immordino, The Health and Migration Programme, World Health Organization, Geneva, Switzerland.
Kanokporn Kaojaroen, The Health and Migration Programme, World Health Organization, Geneva, Switzerland.
Santino Severoni, The Health and Migration Programme, World Health Organization, Geneva, Switzerland.
Sally Hargreaves, The Migrant Health Research Group, Institute for Infection and Immunity, St George’s, University of London, London, UK.
References
- 1. Hayward SE, Deal A, Cheng C et al. Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: a systematic review. J Migration and Health 2021;3:100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Red Cross Red Crescent Global Migration Lab . Locked down and left out? Why access to basic services for migrants is critical to our COVID-19 response and recovery. Melbourne: Red Cross Red Crescent Global Migration Lab, 2021. https://www.redcross.org.au/getmedia/3c066b6d-a71f-46b8-af16-2342ff304291/EN-RCRC-Global-Migration-Lab-Locked-down-left-out-COVID19.pdf.aspx.
- 3. Greenaway C, Hargreaves S, Barkati S et al. COVID-19: exposing and addressing health disparities among ethnic minorities and migrants. J Travel Med 2020;27:taaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Passos-Castilho AM, Labbé A-C, Barkati S et al. Outcomes of hospitalized COVID-19 patients in Canada: impact of ethnicity, migration status and country of birth. J Travel Med 2022;29:taac041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bell S, Clarke R, Mounier-Jack S et al. Parents and guardians; views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine 2020;38:7789–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. ECDC . Reducing COVID-19 Transmission and Strengthening Vaccine Uptake Among Migrant Populations in the EU/EEA. Stockholm: ECDC, June 3, 2021.
- 7. Paul E, Steptoe A, Fancourt D. Anti-vaccine attitudes and risk factors for not agreeing to vaccination against COVID-19 amongst 32,361 UK adults: implications for public health communications. MedRxiv, pp. 2020–10. [Google Scholar]
- 8. Robertson E, Reeve KS, Niedzwiedz CL et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun 2021;94:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Razai MS, Osama T, McKechnie DGJ et al. Covid-19 vaccine hesitancy among ethnic minority groups. BMJ 2021;372:n513. [DOI] [PubMed] [Google Scholar]
- 10. Office of National Statistics . Coronavirus (COVID-19) Latest Insights. London: UK Government, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19/latestinsights#vaccinations.
- 11. Burns R, Campos-Matos I, Harron K et al. COVID-19 vaccination uptake for half a million non-EU migrants and refugees in England: a linked retrospective population-based cohort study. The Lancet 2022;400:S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. RCCE Collective service . DataSsynthesis: Public Perceptions of the COVID-19 Vaccination. RCCE Collective service, June 2021. https://communityengagementhub.org/wp-content/uploads/sites/2/2021/07/Public-Perceptions-of-the-COVID-19-Vaccinations-June-2021-Data-synthesis-Report-1.pdf.
- 13. Crawshaw AF, Deal A, Rustage K et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J Travel Med 2021;28:taab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hargreaves S, Nellums LB, Ravensbergen SJ et al. Divergent approaches in the vaccination of recently arrived migrants to Europe: a survey of national experts from 32 EU/EEA countries. Euro Surveill 2018;23:1700772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. WHO . Delivery of Immunisation Services for Refugees and Migrants: Technical Guidance. Copenhagen: WHO Regional Office for Europe, 2019. [Google Scholar]
- 16. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33:4161–4. [DOI] [PubMed] [Google Scholar]
- 17. World Health Organization (WHO) . Ten Threats to Global Health in 2019. Geneva: WHO, 2019. [Google Scholar]
- 18. Larson HJ, Jarrett C, Eckersberger E et al. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 2014;32:2150–9. [DOI] [PubMed] [Google Scholar]
- 19. De Figueiredo A, Simas C, Karafillakis E et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. The Lancet 2020;396:898–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Larson HJ, Jarrett C, Schulz WS et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine 2015;33:4165–75. [DOI] [PubMed] [Google Scholar]
- 21. Bedford H, Attwell K, Danchin M et al. Vaccine hesitancy, refusal, and access barriers: the need for clarity in terminology. Vaccine 2018;36:6556–8. [DOI] [PubMed] [Google Scholar]
- 22. WHO . Development of Tools to Measure Behavioural and Social Drivers (BeSD) of Vaccination: PROGRESS REPORT. Switzerland/Geneva: WHO, 2020 [Google Scholar]
- 23. Brewer NT. What works to increase vaccination uptake. Acad Pediatr 2021;21:S9–16. [DOI] [PubMed] [Google Scholar]
- 24. WHO, UNICEF .Data for Action: Achieving High Uptake of COVID-19 Vaccines. Interim Guidance. 1 April 2021. Geneva: WHO, 2021. (https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccination-demand-planning-2021.1). [Google Scholar]
- 25. Kasstan B. Vaccines and vitriol: an anthropological commentary on vaccine hesitancy, decision-making and interventionism among religious minorities. Anthropol Med 2020;28:411–19. [DOI] [PubMed] [Google Scholar]
- 26. Deal A, Halliday R, Crawshaw AF et al. Migration and outbreaks of vaccine-preventable disease in Europe: a systematic review. Lancet Infect Dis 2021;21:e387–98. [DOI] [PubMed] [Google Scholar]
- 27. Kang C, Tomkow L, Farrington R. Access to primary health care for asylum seekers and refugees: a qualitative study of service user experiences in the UK. Br J GenPract 2019;69:e537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nellums L, R. K., Hargreaves S, Friedland J, Miller A. Access to Healthcare for People Seeking and Refused Asylum in Great Britain: A Review of Evidence. London: Equality and Human Rights Commission, 2018. [Google Scholar]
- 29. Rafighi E, Poduval S, Legido-Quigley H et al. National Health Service Principles as experienced by vulnerable London migrants in “austerity Britain”: a qualitative study of rights, entitlements, and civil-society advocacy. Int J Health Policy Manag 2016;5:589–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Van Loenen T, Van Den Muijsenbergh M, Hofmeester M et al. Primary care for refugees and newly arrived migrants in Europe: a qualitative study on health needs, barriers and wishes. Eur J Public Health 2018;28:82–7. [DOI] [PubMed] [Google Scholar]
- 31. De Vito E, De Waure C, Specchia ML et al. Are undocumented migrants’ entitlements and barriers to healthcare a public health challenge for the European Union? Public Health Rev 2016;37:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Seedat F, Hargreaves S, Friedland JS. Engaging new migrants in infectious disease screening: a qualitative semi-structured interview study of UK migrant community health-care leads. PLoS One 2014;9:e108261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tankwanchi AS, Bowman B, Garrison M et al. Vaccine hesitancy in migrant communities: a rapid review of latest evidence. Curr Opin Immunol 2021;71:62–8. [DOI] [PubMed] [Google Scholar]
- 34. Bell S, Edelstein M, Zatonski M, Ramsay M et al. “I don’t think anybody explained to me how it works”: qualitative study exploring vaccination and primary health service access and uptake amongst polish and Romanian communities in England. BMJ Open 2019;9:e028228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gahr P, DeVries AS, Wallace G et al. An outbreak of measles in an undervaccinated community. Pediatrics 2014;134:e220–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gorman D, Bielecki K, Willocks L et al. A qualitative study of vaccination behaviour amongst female polish migrants in Edinburgh, Scotland. Vaccine 2019;37:2741–7. [DOI] [PubMed] [Google Scholar]
- 37. Letley L, Rew V, Ahmed R et al. Tailoring immunisation programmes: using behavioural insights to identify barriers and enablers to childhood immunisations in a Jewish community in London, UK. Vaccine 2018;36:4687–92. [DOI] [PubMed] [Google Scholar]
- 38. Peters MD, Godfrey CM, Khalil H et al. Guidance for conducting systematic scoping reviews. JBI Evid Implement 2015;13:141–6. [DOI] [PubMed] [Google Scholar]
- 39. Tricco AC, Lillie E, Zarin W et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. [DOI] [PubMed] [Google Scholar]
- 40. Garrity C, Gartlehner G, Kamel C et al. Interim guidance from the Cochrane rapid reviews methods group. Cochrane Rapid Rev 2020. http://methods.cochrane.org/sites/methods.cochrane.org.rapidreviews/files/uploads/cochrane_rr_-_guidance-23mar2020-final.pdf. [Google Scholar]
- 41. Tankwanchi AS, Jaca A, Larson HJ et al. Taking stock of vaccine hesitancy among migrants: a scoping review protocol. BMJ Open 2020;10:e035225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lockyer B, Islam S, Rahman A et al. Understanding COVID-19 misinformation and vaccine hesitancy in context: findings from a qualitative study involving citizens in Bradford, UK. Health Expect 2021;24:1158–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Deal A, Hayward SE, Huda M et al. Strategies and action points to ensure equitable uptake of COVID-19 vaccinations: a national qualitative interview study to explore the views of undocumented migrants, asylum seekers, and refugees. J Migr Health 2021;4:100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dailey PM, Krieger JL. Communication and US-Somali immigrant human papillomavirus (HPV) vaccine decision-making. J Cancer Educ 2017;32:516–21. [DOI] [PubMed] [Google Scholar]
- 45. El Salibi N, Abdulrahim S, El Haddad M et al. COVID-19 vaccine acceptance in older Syrian refugees: preliminary findings from an ongoing study. Prev Med Rev 2021;24:101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Godoy-Ramirez K, Byström E, Lindstrand A et al. Exploring childhood immunization among undocumented migrants in Sweden-following qualitative study and the World Health Organization’s guide to tailoring immunization programmes (TIP). Public Health 2019;171:97–105. [DOI] [PubMed] [Google Scholar]
- 47. Jalloh MF, Bennett SD, Alam D et al. Rapid behavioral assessment of barriers and opportunities to improve vaccination coverage among displaced Rohingyas in Bangladesh, January 2018. Vaccine 2019;37:833–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lin S. COVID-19 pandemic and Im/migrants’ elevated health concerns in Canada: vaccine hesitancy, anticipated stigma, and risk perception of accessing care. J Immigr Minor Health 2022;24:896–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tomlinson N, Redwood S. Health beliefs about preschool immunisations: an exploration of the views of Somali women resident in the UK. Divers Health Care 2013;10:101–13. [Google Scholar]
- 50. Ganczak M, Bielecki K, Drozd-Dąbrowska M et al. Vaccination concerns, beliefs and practices among Ukrainian migrants in Poland: a qualitative study. BMC Public Health 2021;21:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sim J, Ulanika A, Katikireddi S et al. ‘Out of two bad choices, I took the slightly better one’: vaccination dilemmas for Scottish and polish migrant women during the H1N1 influenza pandemic. Public Health 2011;125:505–11. [DOI] [PubMed] [Google Scholar]
- 52. Cross HR, Community E, Accountability. Survey on the Beliefs of the Vulnerable Population Regarding the COVID-19 Vaccine. A Case Study of the Heelenic Red Cross. Athens: Hellenic Red Cross, 2021. [Google Scholar]
- 53. Thomas CM, Osterholm MT, Stauffer WM. Critical considerations for COVID-19 vaccination of refugees, immigrants, and migrants. Am J Trop Med Hyg 2021;104:433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Abba-Aji M, Stuckler D, Galea S et al. Ethnic/racial minorities’ and migrants’ access to COVID-19 vaccines: a systematic review of barriers and facilitators. J Migr Health 2022;5:100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bentivegna E, Di Meo S, Carriero A et al. Access to COVID-19 vaccination during the pandemic in the informal settlements of Rome. Int J Environ Res Public Health 2022;19:719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bell S, Saliba V, Ramsay M, Mounier-Jack S. What have we learnt from measles outbreaks in 3 English cities? A qualitative exploration of factors influencing vaccination uptake in Romanian and Roma Romanian communities. BMC Public Health 2020;20:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Armocida B, Formenti B, Missoni E et al. Challenges in the equitable access to COVID-19 vaccines for migrant populations in Europe. Lancet Region Health 2021;6:100147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Artiga S, Ndugga N, Pham O. Immigrant Access to COVID-19 Vaccines: Key Issues to Consider. San Francisco: Henry J. Kaiser Family Foundation, 2021. [Google Scholar]
- 59. Marek E, D’Cruz G, Katz Z et al. Improving asylum seekers’ health awareness in a Hungarian refugee reception centre. Health Promot Int 2019;34:e36–46. [DOI] [PubMed] [Google Scholar]
- 60. Louka C, Chandler E, Ranchor AV et al. Asylum seekers’ perspectives on vaccination and screening policies after their arrival in Greece and the Netherlands. PLoS One 2019;14:e0226948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Walker R, Maple N, Vearey J. Migrants & the Covid-19 vaccine roll-out in Africa. Johannesburg: Migration and Coronavirus in Southern Africa Coordination Group, 2021.
- 62. Netfa F, Tashani M, Booy R et al. Knowledge, attitudes and perceptions of immigrant parents towards human papillomavirus (HPV) vaccination: a systematic review. Trop Med Infect Dis 2020;5:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Aragones A, Genoff M, Gonzalez C et al. HPV vaccine and Latino immigrant parents: if they offer it, we will get it. J Immigr Minor Health 2016;18:1060–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gehlbach D, Vázquez E, Ortiz G et al. COVID-19 Testing and Vaccine Hesitancy in Latinx Farm-Working Communities in The Eastern Coachella Valley. Res Sq [Preprint] 2021. 10.21203/rs.3.rs-587686/v1. [DOI]
- 65. Chadenier GMC, Colzani E, Faccini M et al. Assessment of the first HPV vaccination campaign in two northern Italian health districts. Vaccine 2011;29:4405–8. [DOI] [PubMed] [Google Scholar]
- 66. Grandahl M, Tydén T, Gottvall M et al. Immigrant women’s experiences and views on the prevention of cervical cancer: a qualitative study. Health Expect 2015;18:344–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Rubens-Augustson T, Wilson LA, Murphy MS et al. Healthcare provider perspectives on the uptake of the human papillomavirus vaccine among newcomers to Canada: a qualitative study. Hum Vaccin Immunother 2019;15:1697–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jama A, Ali M, Lindstrand A et al. Perspectives on the measles, mumps and rubella vaccination among Somali mothers in Stockholm. Int J Environ Res Public Health 2018;15:2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Brooke D, Omeri A. Beliefs about childhood immunisation among Lebanese Muslim immigrants in Australia. J Transcult Nurs 1999;10:229–36. [DOI] [PubMed] [Google Scholar]
- 70. Kobetz E, Menard J, Hazan G et al. Perceptions of HPV and cervical cancer among Haitian immigrant women: implications for vaccine acceptability. Educ Health (Abingdon) 2011;24:479. [PubMed] [Google Scholar]
- 71. Redsell SA, Bedford H, Siriwardena AN et al. Health visitors’ perception of their role in the universal childhood immunisation programme and their communication strategies with parents. Prim Health Care Res Dev 2010;11:51–60. [Google Scholar]
- 72. Kim K, Kim B, Choi E et al. Knowledge, perceptions, and decision making about human papillomavirus vaccination among Korean American women: a focus group study. Womens Health Issues 2015;25:112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Berardi C, Lee ES, Wechtler H et al. A vicious cycle of health (in)equity: migrant inclusion in light of COVID-19. Health Policy Technol 2022;11:100606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Harmsen IA, Bos H, Ruiter RA et al. Vaccination decision-making of immigrant parents in the Netherlands; a focus group study. BMC Public Health 2015;15:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Truman T, Higham R, Chernenko A et al. Beliefs and experiences about immunization among refugees resettled in the United States from the Thailand-Myanmar (Burma) border. Int J Health Promot Educ 2020;59:226–35. [Google Scholar]
- 76. Gorman D, Bielecki K, Larson H et al. Comparing vaccination hesitancy in Polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine 2020;38:2795–9. [DOI] [PubMed] [Google Scholar]
- 77. Jenness SM, Aavitsland P, White RA et al. Measles vaccine coverage among children born to Somali immigrants in Norway. BMC Public Health 2021;21:668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Andrade G, Bedewy D, Bani I. Motivational factors to receive the COVID-19 vaccine in the United Arab Emirates: a cross-sectional study. J Community Health 2022;47:530–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Campeau KL. Vaccine barriers, vaccine refusals: situated vaccine decision-making in the wake of the 2017 Minnesota measles outbreak. Rhetor Health Med 2019;2:176–207. [Google Scholar]
- 80. Alabdulla M, Reagu SM, Al-Khal A et al. COVID-19 vaccine hesitancy and attitudes in Qatar: a national cross-sectional survey of a migrant-majority population. Influenza Other Respi Viruses 2021;15:361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Khaled SM, Petcu C, Bader L et al. Prevalence and Potential Determinants of COVID-19 Vaccine Hesitancy and Resistance in Qatar: Results from a Nationally Representative Survey of Qatari Nationals and Migrants between December 2020 and January 2021. Vaccines 2021;9:471. 10.3390/vaccines9050471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Mupandawana ET, Cross R. Attitudes towards human papillomavirus vaccination among African parents in a city in the north of England: a qualitative study. Reprod Health 2016;13:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Knights F, Carter J, Deal A et al. Impact of COVID-19 on migrants’ access to primary care and implications for vaccine roll out: a National Qualitative Study. Br J Gen Prac 2021;71:e583–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Page KR, Genovese E, Franchi M et al. COVID-19 vaccine hesitancy among undocumented migrants during the early phase of the vaccination campaign: a multicentric cross-sectional study. BMJ Open 2022;12:e056591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Ricco M, Cattani S, Veronesi L et al. Knowledge, attitudes, beliefs and practices of construction workers towards tetanus vaccine in northern Italy. Ind Health 2016; 2015–0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. McGeown H, Moore J, Heffernan C. Embedding commissioner visits to general practices to improve childhood immunisations. Br J Healthcare Manage 2019;25:16–21. [Google Scholar]
- 87. Wang A. Exploring Gaps in COVID-19 Related Information Dissemination and Vaccine Hesitancy in Asian Communities. Toronto: Ryerson University, 2021.
- 88. Chauhan B. Quality improvement project: understanding and improving health outcomes for unaccompanied asylum seeking children (UASC) in Harrow. Adopt Foster 2019;43:225–30. [Google Scholar]
- 89. Wickramage K, Ito C, Hilali M et al. Migrants in the Middle East and North Africa during the COVID-19 pandemic. J Travel Med 2023;30:taab097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Diaz AA, Celedón JC. COVID-19 vaccination: helping the Latinx community to come forward. EClinicalMedicine 2021;35:100860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. WHO . COVID-19 Immunization in Refugees and Migrants: Principles and Key Considerations. Interim Guidance. Geneva: WHO, 2021. [Google Scholar]
- 92. Zehireva S. IPHA Policy Brief: Immigrants’ Health in Illinois: Medical Distrust–COVID-19 Vaccines. Lisle (IL): Benedictine University, 2021.
- 93. Mellou K, Silvestros C, Saranti-Papasaranti E et al. Increasing childhood vaccination coverage of the refugee and migrant population in Greece through the European programme PHILOS, April 2017 to April 2018. Eurosurveillance 2019;24:1800326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Miller AR. Increasing Influenza Vaccination Access among Migrant Farmworkers on Dairy Farms in Northern Vermont. Family Medicine Clerkship Student Projects 2020;607. https://scholarworks.uvm.edu/fmclerk/607.
- 95. Vita S, Sinopoli MT, Sulekova LF et al. Vaccination campaign strategies in recently arrived migrants: experience of an Italian reception centre. J Infect Dev Ctries 2019;13:1159–64. [DOI] [PubMed] [Google Scholar]
- 96. Suppli CH, Dreier JW, Rasmussen M et al. Sociodemographic predictors are associated with compliance to a vaccination-reminder in 9692 girls age 14, Denmark 2014-2015. Prev Med Rep 2018;10:93–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Perry M, Townson M, Cottrell S et al. Inequalities in vaccination coverage and differences in follow-up procedures for asylum-seeking children arriving in Wales, UK. Eur J Pediatr 2020;179:171–5. [DOI] [PubMed] [Google Scholar]
- 98. Han K, Francis MR, Zhang R et al. Confidence, acceptance and willingness to pay for the COVID-19 vaccine among migrants in shanghai, China: a cross-sectional study. Vaccine 2021;9:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. World Health Organization . Tailoring Immunization Programmes (TIP). Copenhagen: WHO EURO, 2019. [Google Scholar]
- 100. Larson H. Vaccine Hesitancy among Healthcare Workers and Their Patients in Europe: A Qualitative Study. Stockholm: ECDC, 2015. [DOI] [PubMed] [Google Scholar]
- 101. Office for National Statistics . Coronavirus (COVID-19) Latest Insights: Vaccines. London: UK Government, 2021.
- 102. RCCE . Risk Communication and Community Engagement: Guidance on COVID-19 Vaccines for Marginalized Populations, 2021.
- 103. Puri N, Coomes EA, Haghbayan H et al. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother 2020;16:2586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. IFRC . https://communityengagementhub.org/resource/ifrc-covid-19-community-feedback-package/.
- 105. World Health Organization . Immunization Agenda 2030: A Global Strategy to Leave No One Behind. Geneva: WHO; April 1, 2020. [DOI] [PubMed] [Google Scholar]
- 106. UN Women and Translators without Borders, RCCE Working Group on COVID-19/Interagency Standing Committee . COVID-19: How to INCLUDE Marginalized and Vulnerable People in Risk Communication and Community Engagement, 2021. https://interagencystandingcommittee.org/system/files/2020-03/COVID-19%20-%20How%20to%20include%20marginalized%20and%20vulnerable%20people%20in%20risk%20communication%20and%20community%20engagement.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Primary data from this study is available from authors on reasonable request.