Abstract
Introduction:
Complementary and alternative medicine or therapies (CAM) are frequently used by skin cancers patients. Patient’s self-administration of CAM in melanoma can reach up to 40–50%. CAMs such as botanical agents, phytochemicals, herbal formulas (“black salve”) and cannabinoids, among others, have been described in skin cancer patients.
Objective:
To acknowledge the different CAM for skin cancers through the current evidence, focusing on biologically active CAM rather than mind-body approaches.
Methods:
We searched MEDLINE database for articles published through July 2022, regardless of study design.
Results:
Of all CAMs, phytochemicals have the best in vitro evidence supporting efficacy against skin cancer including melanoma; however, to date, none have proved efficacy on human patients. Of the phytochemicals, Curcumin is the most widely studied. Several findings support Curcumin efficacy in vitro through various molecular pathways, although most studies are in the preliminary phase. In addition, the use of alternative therapies is not exempt of risks: physicians should be aware of their adverse effects, interactions with standard treatments, and possible complications arising from CAM usage.
Conclusion:
There is emerging evidence for CAM use in skin cancer, but no human clinical trials support the effectiveness of any CAM in the treatment of skin cancer to date. Nevertheless, patients worldwide frequently use CAM, and physicians should educate themselves on currently available CAMs.
Keywords: skin cancer, melanoma, non-melanoma skin cancer, complementary therapy, complementary and alternative medicine
Introduction:
Skin cancer is the most frequent malignancy in humans. Both melanoma and non-melanoma skin cancer (NSMC) have a growing incidence and relatively stable mortality. Dermatology patients are referring a growing interest in complementary and alternative medicine (CAM) therapies.1 The National Institute of Health (NIH): National Center for Complementary and Integrative Health defines CAM as “a group of diverse medical and health care practices and products that are not presently considered to be part of conventional medicine”.1 The use of CAM is a growing phenomenon, and even some (like ‘Kampo medicines’) are covered by health insurances. A survey of 400 directors of private clinics of Japan reported that dermatology was the third medical specialty that prescribed ‘Kampo medicines’ more frequently.2 Dietary supplements (other than vitamins and minerals) are the most commonly used CAM, followed by mind-body approaches (e.g., deep-breathing exercises and acupuncture, among others).1,3 It has been reported that up to 85% of dermatology patients use CAM at some point, more commonly older women.1 CAM data use in skin cancer patients is scarce with most information coming from melanoma patients. It has been reported that ~20% of NMSC patients4 and 40–50% of melanoma patients have used CAM at some point, especially on those with advanced disease.5
Trust in conventional medicine and compliance to physician’s suggestions showed no difference between CAM users and non-users; however, the feeling of less emotional support from the medical team was significantly higher in the conventional medicine group.5 In a study, the largest source of information reported by CAM users was print media, family and friends, physicians, and the internet.3 However, there are reliable resources for finding information regarding complementary health approaches that could be useful to clinicians (Table 1). Herein we performed a literature review on different CAMs for skin cancer. We focused solely on biologically active CAM rather than mind-body approaches. Our objective was to create a resource for dermatologists on different CAMs reported on skin cancer patients.
Table 1:
Recommended Internet resources for integrative oncology. Modified from Lopez, et al.50
| Memorial Sloan Kettering Cancer Center | https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine |
| University of Texas MD Anderson Center, Integrative Medicine Program | https://www.mdanderson.org/patients-family/diagnosis-treatment/care-centers-clinics/integrative-medicine-center.html |
| Natural Medicines Comprehensive Database | https://naturalmedicines.therapeuticresearch.com |
| National Center for Complementary and Integrative Health | www.nccih.nih.gov |
| National Cancer Institute: Office of Cancer Complementary and Alternative Medicine | https://cam.cancer.gov |
| American Institute for Cancer Research | www.aicr.org |
| Society for Integrative Oncology | www.integrativeonc.org |
Methods:
We searched MEDLINE database for articles published through July 2022, using the keywords: (“melanoma” or “nonmelanoma” or “non-melanoma” or “basal cell carcinoma” or “squamous cell carcinoma”) AND (“cutaneous” or “skin” or “skin cancer” AND “complementary therapy” or “complementary medicine” or “alternative therapy” or “alternative medicine” or “non-traditional medicine” or “non-classical medicine”). References within retrieved articles were also reviewed to identify potentially missed studies. We included all studies published to date, in English and/or Spanish, regardless of study design. Exclusion criteria were languages other than English or Spanish and unavailability of the full article. Duplicates were reviewed and excluded.
Results:
I. Complementary and alternative therapies in non-melanoma skin cancer:
Despite 18% of patients with NMSC reported any CAM use, only 1% used it as a primary treatment (alternative use).4 Herein we discuss those with reported outcomes or clinical relevance. No studies on CAM use on systemic/metastatic NMSC were found. Table 2 summarizes the findings.
Table 2:
Summary of complementary and alternative therapies evaluated for non-melanoma skin cancer with most available evidence.
| Agent | Mechanism of action | Effect in vitro / animal models | Effect in human participants | Potential for harm/toxicity | Level of evidence* |
|---|---|---|---|---|---|
| Botanical agents | |||||
| Goldenseal (Hydrastis canadensis) | • Inhibits glucose uptake inhibiting skin carcinogenesis | In vitro / Mice | No | • Potentially hinder glucose control in people with type 2 diabetes taking metformin (reduces 25% level) • May be safe taken alone, but there are not reliable studies that evaluate its safety. |
5 |
| Pond apple (Annona glabra) | • Down-regulates Bcl-2 gene • Up-regulates Bax gene • Antiproliferative effect |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Bitter melon (Momordica charantia) | • Molecular pathway not available • Inhibits carcinogenesis |
Mice | No | • Not reliable studies that evaluate its safety. | 5 |
| Ginger (Zingiber officinale) | • Molecular pathway not available • Inhibits skin tumor initiation and promotion |
Mice | No | • Used safely on dietary supplement and topical use. • Abdominal discomfort, heartburn, diarrhea, and mouth and throat irritation, especially if taken in large doses. |
5 |
| Willow tree bark (Salix caprea) | • Inhibits oxidative stress and ornithine decarboxylase activity with anti-carcinogenesis effects | Mice | No | • Not reliable studies that evaluate its safety. | 5 |
| Frankincense (Boswellia serrata) | • Activates caspase-8 pathway and inhibits phosphorylation of the ERK 1/2 with antiproliferative effect | In vitro / Mice | Case reports | • When added in escharotic agents: subclinical extension of tumor. • Scarring and tissue damage, which could lead to disfiguring. |
5 |
| Sodom apple plant (Solanum sodomaeum) | • Not available. | In vitro / Mice | Case reports: cream formulation has shown efficacy on BCC, SCC, keratoacanthomas, and actinic keratosis at least 3 years after cessation of therapy | • Not reliable studies that evaluate its safety. | 5 |
| Plants of the genus Gelsemium | • Increases production of PCNA with antiproliferative and propaoptotic effect | In vitro / Mice | No | • Not reliable studies that evaluate its safety. | 5 |
| Polypodium leucotomos | • Decreases cyclobutane pyrimidine dimers • Decreases epidermal cells and dermal mast cell infiltration • Photoprotective effects against UVR. |
In vitro / Mice | Case reports: Increases the efficacy of photodynamic therapy in actinic keratosis | • Not reliable studies that evaluate its safety. | 5 |
| Phytochemicals | |||||
| Resveratrol | • Inhibits MMP-2 and MMP-9 secretion with antiproliferative effects on SCC models | In vitro | No | • May increase concentrations of pimozide (by CYP3A4 inhibition) | 5 |
| Cryptolepine | • Increases phosphorylation of • ATM/ATR, BRCA1, Chk1/Chk2 and γH2AX. • Activates of p53 signaling pathway • Downregulates of cyclin-dependent kinases, cyclin D1, cyclin A, cyclin E and proteins involved in cell division • Antiproliferative and propaoptotic effects |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Apigenin | • Propapoptotic effect through TNFR- and Bcl-2-mediated pathway | In vitro: Enhances susceptibility of head and neck SCC to 5-fluorouracil and cisplatin | No | • Not reliable studies that evaluate its safety. | 5 |
| Curcumin | • Inhibits NF-κB signaling pathway, Akt, ERK1/2, STAT3 with antiproliferative and propaoptotic effects • Up-regulates miR-9 expression • Supresses Wnt/β-catenin signaling pathway • Decreases cyclin D1 level • Inhibits mTOR signaling pathway • Antiproliferative effects on oral SCC |
In vitro / Mice | Case reports and case series: chemoprevention of cancer, including arsenic Bowen’s disease and oral leukoplakia | • No treatment-related toxicity up to 8,000 mg/day | 4 |
| Curcuminoids | • Inhibites proliferation of HNO97 cell lines (Human oral squamous cell carcinoma). • Morphological changes of HNO97 cell lines: appearance of apoptosis. • Induces apoptosis of HNO97 cell lines in a time-dependent manner. • Alters the cell cycle distribution of HNO97 cell lines • DNA damage in HNO97 cell lines. • Supresses the colony-forming ability of HNO97 cell lines in a time-dependent manner. |
In vitro | Case reports | • Safely when taken orally or applied to the skin (turmeric) but lacks bioavailability. | 5 |
| Silymarin/Silibinin | • Protects against UVB-induced thymine dimer formation. • Promotes DNA repair. Apoptosis in damaged cells via an increase in p53 levels. • Target aberrant signaling pathways • Induction of anti-inflammatory responses (TNFα, IL-1α and COX-2 pathway). |
In vitro | No | • Milk thistle (contains silymarin) may lower blood sugar levels in people with type 2 diabetes | 5 |
| Herbal formulas | |||||
| “Black salve” | • Inhibits NF-κB with proapoptotic effect | In vitro | Case reports: complete BCC remission cases and residual infiltrating BCC. | • When added in escharotic agents: subclinical extension of tumor • Scarring and tissue damage, which could lead to disfiguring. |
5 |
| Cannabinoids | |||||
| Exogenous cannabinoids | • CB1 and CB2 activation shows antitumor effect in skin papillomas and NMSC in mice • Prevented growth and vascularization of malignant epidermal tumor cells |
In vitro / Mice | No | • Cannabis: risk of motor vehicle crashes, lower birth weight when consumed on pregnancy, orthostatic hypotension, severe mental illnesses (in predisposed). | 5 |
| Anandamide | • Elevated in skin tumor cells, leading to cell apoptosis | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
Level of evidence based on www.ebmconsult.com/articles/levels-of-evidence-and-recommendations
1. Botanical agents (herbs):
Botanical agents or “herbs” is used to refer to the whole plant without extraction of the active substances. The active substances of botanical agents are named “Phytochemicals”. The biologic effect of a botanical agent mainly comes from its “phytochemicals”, but it is not limited to it as other components might have relevant effects. Botanical agents have some biological activity in NSMC, mostly in murine models. Botanical agents with proven biological effect on skin tumors include: Goldenseal (Hydrastis canadensis),6 pond apple (Annona glabra),7 bitter melon (Momordica charantia),8 ginger (Zingiber officinale),6 frankincense (Boswellia serrata),9 and willow-tree bark (Salix caprea).6 The glycoalkaloids from Sodom apple plant (Solanum sodomaeum) have shown efficacy on basal cell carcinoma (BCC), squamous cell carcinoma (SCC), keratoacanthomas, and actinic keratoses when used topically (cream) in humans.6 Plants of the genus Gelsemium showed growth reduction of topical carcinogens induced papilloma and skin cancer in mice.10 Polypodium leucotomos has been shown to increase the efficacy of photodynamic therapy in the treatment of actinic keratosis in humans.11 Some botanical agents showed photoprotective effects against ultraviolet radiation (UVR), such as red clover flowers (Trifolium pretense),6 flower of Orpheus (Haberlea rhodopensis), grape seed extract,12 green tea,12 golden polypody (Polypodium leucotomos),11 and ground pine (Lycopodium clavatum).13
1.1. Phytochemicals:
Phytochemicals can modulate multiple biochemical pathways involved in carcinogenesis and can protect cells from damage from free radicals and ultraviolet radiation (UVR). The most relevant type of phytochemicals with anticancer activity are polyphenols, particularly flavonoids, mainly from parsley and celery.
Those with activity in skin tumors and NMSC are resveratrol,14 cryptolepine, apigenin,13 and curcumin (Diferuloylmethane).15 Curcumin was particularly evaluated for SCC. A phase I trial in humans demonstrated that 8000 mg/day curcumin were non-toxic when taken orally for 3 months, and suggested biologic effect in premalignant lesions, including arsenical Bowen’s disease and oral leukoplakia.16 Phytochemicals with photoprotective activity include silibinin12 and curcumin.
Curcuminoids:
Curcuminoids are a spice with a yellow color extracted from the roots of the Curcuma longa herb (Turmeric), which belongs to the ginger family. Curcumin is also known as ‘Golden spice’ because of its yellow color found in curry powder.15 Curcuminoids consist of diferuloylmethane (curcumin), desmethoxycurcumin, and bisdemethoxycurcumin.15 A study in human oral squamous cell carcinoma (HNO97 cell line) showed inhibition in proliferation, morphological changes (apoptosis-like), alterations in cell cycle distribution, and DNA damage.15 Also investigators found apoptosis induction and suppression of colony-forming ability in a time-dependent manner.15
Silymarin/Silibinin
Silymarin is isolated from the seed of milk thistle (Silybum marianum, Astteraceae family), which is an annual or biennial Mediterranean native herb.12 Silibinin is a constituent of silymarin. Investigators found protective effect of silbinin against UVB induced-photocarcinogenesis. Silbinin accelerated the removal of UVB-induced DNA damage products and reduction of tumor number, multiplicity, and volume in p53+/+ mice.12 They also reported a silbinin effect against UVB-induced genomic instability; inhibitory effect against skin SCC/BCC growth and proliferation; induction of apoptotic cell death of skin epidermal cells after UVB exposure; inhibitory effect on molecular expression and activation of inflammatory molecules and oxidative pathways (essential in tumorigenesis); and a inhibitory effect against drug-resistant BCC cells (via targetin EGFR/AKT and Hedghog pathway).12
Cannabinoids:
Cannabinoid receptors are expressed in both NMSC and melanoma.17 Studies have shown in vivo and in vitro effects on NMSC.17 In mice, local administration of cannabinoids prevented growth and vascularization of malignant epidermal tumor cells.17 Anandamide, an endocannabinoid, may be elevated in skin tumor cells, leading to endocannabinoid-induced apoptosis and tumor cells death.17 No study has been performed in humans, yet. Furthermore, cannabinoids may have immunosuppressive potential and tumor promoting effects.18
2. Herbal formulas:
Most of the preparations found on the internet are herbal ‘formulas’ of mixed compounds, including zinc chloride, urea, apricot pits, bloodroot and goldenseal.6 Of these, escharotic agents are the most notorious, with corrosive properties that produce eschars and scarring. The most frequently used escharotic agent is “black salve”.19
2.1. “Black salve”:
“Black salve” paste has been widely promoted for its supposed ability to eradicate BCC through topical application on social media and online forums.19 The composition of “black salve” varies, but it usually includes zinc chloride, and powdered bloodroot from Sanguinaria canadensis. Bloodroot probably inhibits nuclear factor-kappa B (NF-kB), inducing selective apoptosis of cancer cells in in vitro.19 Histopathological analysis showed scarring, granulomatous responses, extensive necrosis, and suppurative inflammation.20 “Black salve” treatment efficacy for BCC varies, from complete remission with no residual tumor on biopsy to residual infiltrating BCC.20 The latter is found more frequently, and moreover, the resulting ulcer from escharotics can last up to 6 months.20 As escharotics appear to work on the base of direct tissue destruction, the efficacy of “black salve” depends on the extent of the tumor relative to the amount applied.
II. Complementary and alternative therapies in melanoma:
The most frequent CAM reported among melanoma patients are dietary supplements.3 Reported satisfaction is less than 50% in melanoma patients; mind-body alternatives have shown higher satisfaction rates.3 Interestingly, some research has evaluated its potential role on systemic/metastatic disease. Table 3 summarizes the findings.
Table 3:
Summary of complementary and alternative therapies evaluated for melanoma skin cancer with most available evidence.
| Agent | Mechanism of action | Effect in vitro / animal models | Effect in human participants | Potential for harm/toxicity | Level of evidence* |
|---|---|---|---|---|---|
| Botanical agents | |||||
| Tea tree oil (Melaleuca alternifolia) | • Activates caspase-dependant apoptosis | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Slippery elm (Ulmus rubra) | • Oligonucleosomal fragmentation • Activates caspase-3 signaling pathway • Decreases expression of Bcl-2 gene and Bcl-XL gene • Increases expression of Bax gene • Propapototic effect |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Chapparel (Larrea tridentata) | • Molecular pathway not described • Tumor growth inhibition |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Alpinia galanga | • Inhibits MAPK signaling pathway • Inhibits p44/42 signaling pathway • Inhibits NF-κB signaling pathway • Antiproliferative and cytotoxic effects |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Flower buds of Lawsonia inermis (Henna) | • Inhibits TYR, TRP-1 and TRP-2 and mRNA expression • Antimelanogenesis effect |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Young green barley (Hordeum vulgare L.) | • Molecular pathway not described • Inhibits activity in melanoma cells |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| The desert plant Anastatica hierochuntica | • Inhibits phosphorylation of ERK1/2 • mRNA expression of tyrosinase and TRP-1 and −2 is contradictory • Inhibits melanogenesis |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Homeopathic mother tincture (Phytolacca decandra) | • Generates oxidative damage • Down-regulates of Akt and Bcl-2 gene • Up-regulates of Bax gene, p53, and caspase 3 signaling pathway • Antiproliferative and proapoptotic effects |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Gurmar or woody climber tree (Gymnema sylvestre) | • Causes DNA fragmentation • Increases level of mRNA expression of apoptotic signal related genes |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Hibiscus rosa-sinensis flower extract | • Induces caspases cleavages, Bcl-2 family proteins regulation, and Fas/FasL activation • Antiproliferative effects and induces autophagy |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Lingzhi (Ganoderma lucidum) | • Inhibits release of IL-8, IL-6, MMP-2, and MMP-9 • Decreases viability of melanoma cells |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Yellow jessamine (Gelsemium sempervirens) | • Down-regulates cyclin-D1, PCNA, survivin, and STAT-3 • Up-regulates of p53 and caspase-3 signaling pathway • Proapoptotic effect |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Solanum nigrum | • Decreases MMP-9, Akt activity and PKCα, Ras, and NF-κB protein expressions • Cytostatic and cytotoxic effect against human and mouse melanoma cells |
In Vitro / Mice | No | • Not reliable studies that evaluate its safety. | 5 |
| Hedyotis diffusa | • Activates caspase-3, caspase-8, and caspase-9 • Antiproliferative effect |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Panax ginseng | • Increases the production of TNF-alpha, NO and IL-6. • Regulates the C-jun N-terminal kinase phosphorylation, and p38. • Activates Akt, MAPKs, and NF-κB • Induces cell death in vitro • Reduces melanoma cell viability |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Phytochemicals | |||||
| Capsaicin | • Depletion of substance P • Inhibits PI3K, Akt, mTOR and NF-κB • Antiangioneogenisis, and proapototic effects |
In vitro | No | • Topical: Application site burning, erythema, pain, pruritus, edema, blister, scar. | 5 |
| Genistein | • Inhibits Akt, MAPK, P38 and JNK signaling pathway • Anti-angionegenisis, antiproliferative and proapototic effects |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Indole-3-carbinol | • Inhibits Akt and MITF with antiproliferative and propapoptotic effects | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Proanthocyanidins | • Inhibits NF-κB and ERK1/2 with antiproliferative effect | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Resveratrol | • Increases Connexin 43 gap junction communications • Decreases expression of cyclin B, cyclin D, CDK-2 and CDK-4 • Decreases expression FLIP gene, Bcl-2, and survivin • Inhibits ERK1/2 • Increases tumor suppressor protein 53 and matrix protein TSP1 • Antiproliferative effects |
In vitro | No | • May increase concentrations of pimozide (by CYP3A4 inhibition) | 5 |
| Apigenin | • ncreases ROS • Activates caspase-3 signaling pathway • Decreases phosphorylation of ERK1/2 proteins, Akt and mTOR • Antiproliferative and proapoptotic effects |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Quercetin | • Up-regulates CDK inhibitors p27(KIP1) and p21(CIP1) • Antioxidant, cell cycle arrest and proapoptotic activity |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Silymarin and silybin | • Decreases phosphorylation of ERK1/2 and RSK2, • Decreases activation of NF-κB, AP-1, and STAT3 • Increases casein kinase 1α and glycogen synthase kinase-3β • Decreases nuclear β-catenin • Inhibits of MMP-2 and MMP-9 • Antiproliferative, cell cycle arrest and proapoptotic effect |
In vitro | No | • Milk thistle (contains silymarin) may lower blood sugar levels in people with type 2 diabetes | 5 |
| Epigallocatechin-3-gallate | • Inhibits cell growth, EMT and invasion • Inhibits NF-κB signaling pathway • Decreases IL-1β secretion. inhibited iNOS, COX-2, MMPs, IL-6, IL-8, IL-12 and TNFα • Down-regulates the inflammasome • Decreases NLRP1 • Reduces caspase-1 activation Induces cell cycle arrest and apoptosis |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Chrysin | • Stimulates IL-2, IL-10 expression in mice melanoma cells | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Paradise tree extract | • Apoptosis in melanoma cells from the A375 and G361 cell lines in-vitro | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Berberine | • Increases melanoma cell levels of ROS and produces AMPK activation • Downregulation of ERK and p38 MAPK • Reduction in COX-2, PGE2 and PGE2 receptors |
In vitro / Mice | No | • Golden seal (contains berberine): potentially hinder glucose control in people with type 2 diabetes taking metformin (reduces 25% level) • May be safe taken alone, but there are not reliable studies that evaluate its safety. |
5 |
| Pancratistatin | • Targets mitochondrial vulverabilities • Apoptosis in melanoma cells (A375) • In combination with tamoxifen is more effective than either agent standalone (in-vitro) |
In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Curcumin | • Anti-inflammatory and anti-oxidative pathways which allow it to selectively target melanoma cells. • Up-regulates of miRNA, p53, p21(Cip1), p27(Kip1) and checkpoint kinase 2 • Down-regulates of anti-apoptotic Bcl-2, PCNA, iNOS, DNA-PKcs expression, PRL-3, anti-apoptotic Mcl-1 protein • Activates caspase-3, caspase 8, MST1 gene • Inhibits of NF-κB, PDE 1 to 5 • Inhibits phosphorylation of STAT1 and STAT3, MMP-2, mTOR activity • Increases levels of IFN-γ secretion and production of granzyme b or IFN-γ. • Reduces level of IL-12. • Akt phosphorylation has shown contradictory results. Induces MPTP opening • Multiple antioxidative, antiproliferative, proapoptotic effects on melanoma cells in vitro and murine models. • Poor bioavailability when tested in-vivo mouse models. |
In vitro / Mice | No | • Safely when taken orally but lacks bioavailability. | 5 |
| Curcuminoids | |||||
| EF24 | • Inhibits the NF-κB | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| DM-1 | • Modulates iNOS and COX-2 gene expression | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| D6 | • Induces overexpression of HSP and induces melanoma cells apoptosis | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| Herbal formulas | |||||
| “Black salve” | • Induces caspase signaling pathway and oxidative stress. | In vitro | Case reports: escharotic effect. | • When added in escharotic agents: subclinical extension of tumor • Scarring and tissue damage, which could lead to disfiguring. • In melanoma has been associated with ulcer, local recurrence, and metastatic disease |
5 |
| Cannabinoids | |||||
| CB1 | • Tumor-promoting signal in human cutaneous melanoma | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| CB1 and CB2 | • Alters Akt protein and pRb phosphorylation decreasing angiogenesis, proliferation, and metastasis of melanoma | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| PEA | • PEA in combination with URB597 (inhibitor of fatty acid amide hydrolase) decreases melanoma progression associated with increased PEA levels | In vitro | No | • Not reliable studies that evaluate its safety. | 5 |
| THC | • Inhibits tumor growth of transplanted melanoma, inhibiting tumor growth in mice | In vitro | No | • Cannabis: risk of motor vehicle crashes, lower birth weight when consumed on pregnancy, orthostatic hypotension, severe mental illnesses (in predisposed). | 5 |
| Vitamin C | |||||
| Vitamin C | • Decreases the phosphorylated form of BRAF gene (dose dependent) • Increases the phosphorylation of ERK • Increased the phosphorylated form of AKT which mediates cell survival and growth. |
In vitro | No | • Oral: hyperoxaluria (with large doses), hemolysis (in patients with glucose-6-phosphate dehydrogenase deficiency). | 5 |
Level of evidence based on www.ebmconsult.com/articles/levels-of-evidence-and-recommendations
1. Botanical agents (herbs):
Melanoma models have shown anticancer effect of multiple botanical agents through diverse molecular pathways: Tea tree oil (Melaleuca alternifolia),6 slippery elm (Ulmus pumila), chaparral (Larrea tridentata),21 Alpinia galanga,22 flower buds of Henna (Lawsonia inermis),23 young green barley (Hordeum vulgare L.),24 the desert plant Anastatica hierochuntica,25 homeopathic mother tincture (Phytolacca decandra),26 gurmar or woody climber tree (Gymnema sylvestre),27 Hibiscus rosa-sinensis flower extract,28 Lingzhi (Ganoderma lucidum),29 and yellow jessamine (Gelsemium sempervirens).10 Ferula species mixed with derivatives of curcumin showed no cytotoxic effect on SK-MEL-28 melanoma cells.30 Finally, the water extracts of Solanum nigrum, a herb in traditional Chinese medicine, has cytotoxic effect against human melanoma cell lines and inhibited the metastasis of mouse melanoma cells.31
1.1. Phytochemicals:
Phytochemicals with proven in vitro activity in melanoma models are: Capsaicin, found in chili peppers;32 genistein, found in soybeans;33 indole-3-carbinol, found in vegetables including broccoli, cauliflower, and brussels sprouts;34 proanthocyanidins, found in cocoa, grapes, apple, tea and red wine;35 resveratrol, found in grapes, peanuts, mulberries, cranberries, and eucalyptus;14 fisetin, found in strawberries; mangoes, kiwis, apples, grapes, persimmons, cucumbers and onions;36 luteolin found in carrots, peppers, celery, olives, peppermint, thyme, rosemary, and oregano;37 apigenin, found in as parsley, celery, artichokes and chamomile;13 betulinic acid, found in the birch bark;38 quercetin, found in apples, berries, and onions; Berberine, found in roots of plants from the genus Berberis;39 Pancratistatin, obtained from the beach spider lily (Hymencallis littoralis);39 Paradise tree extract, isolated from the Lakshmi Taru (Simarouba glauca);39 and silymarin (Silybum marianum).12 Some of the propolis compounds have shown biological activity, such as chrysin, which has been shown to stimulate IL-2 and IL-10 expression in murine melanoma cells, and galangin, which downregulates ERK 1/2 and activates p38 MAP kinases in human melanoma cells. Chitosan nanoparticles containing limonene and limonene-rich essential oils (Citrus sinensis and Citrus limon) showed viability reduction on melanoma cell line A375, but the mechanism is unknown.40
Of note, some phytochemicals have shown potential benefit on metastatic disease. For instance, catechins (present in green tea extract) have been shown to modulate cancer cell growth, metastasis, angiogenesis, and other aspects of cancer progression by affecting different mechanisms.41 Epidemiological studies suggest that regular consumption of green tea and ginseng attenuates the risk of many cancers. The main catechin with anticancer activity in green tea is epigallocatechin-3-gallate, with evidence showing promising effects in melanoma models.41
Curcumin:
Curcumin anti-neoplastic and anti-angiogenic effects have been reported widely. Multiple studies have used curcumin or its analogues,42 because of its known potent anti-angiogenic, antiproliferative and proapoptotic effects in melanoma cells.43 In contrast to NMSC, no human studies on melanoma patients have been reported to date.
How curcumin exerts its antitumoral effects in cutaneous melanoma is yet to be completely elucidated, but it involves anti-inflammatory and anti-oxidative pathways which allow it to selectively target melanoma cells.39 It has been described to interact with NF-kB,44 caspases, miRNA, Bcl-2 protein expression,44 inducible nitric oxide synthase inhibition,45 downregulation of DNA-dependent protein kinase catalytic subunit; and upregulation of p53, p21, p27, checkpoint kinase 2.45 Also by activation of mammalian sterile 20-like kinase 1, downregulation of phosphatase of regenerating liver-3 expression, lowering levels of STAT3 and JAK-2 protein phosphorylation,44 pore opening of mitochondrial permeability transition with activation of cell death pathway, inhibition of matrixmetalloproteinase-2 activity, and downregulation of AKT/mTOR, among other effects.43 Non-selective inhibition of cyclic nucleotide phosphodiesterase 1–5 has also been described.43 Curcuminoids have also shown anti-cancer activity, such as EF24, which inhibits the NF- kB; DM-1, modulating iNOS and COX-2 gene expression; and D6, inducing overexpression of heat shock proteins, among others.42
Because of the limited oral bioavailability of curcumin, different mechanisms have been tested to improve delivery: micelles; transdermal presentations; chitosan-coated nanoparticles; among others. When cooked, curcumin decomposition products include deketene curcumin, with proven toxicity on melanoma cells. Visible light and combined red and blue light irradiation could synergize with curcumin enhancing apoptosis in human melanoma cells.42 However, stimulation of natural killer cells with curcumin reduced the level of IL-12- induced IFN-γ secretion and production of granzyme-B or IFN-γ.42 These latter immunologic effects imply that curcumin might also adversely affect the responsiveness of immune effector cells to clinically relevant cytokines that possess anti-tumor properties. When evaluating effects on metastatic disease, oral administration of curcumin alone or through chitosan-coated nanoparticles in melanoma-tumor-bearing mice, inhibits the lung metastasis of melanoma by as much as 80%, increasing survival by 144%.42
Berberine:
Berberine is a natural isoquinolone alkaloid which can be extracted through the roots of plants from the genus Berberis.39 It increases melanoma cell levels of reactive oxygen species (ROS) which causes AMP-activated protein kinase (AMPK) activation, altering the activity of several signaling pathways.39 Signaling molecules such as ERK and p38 MAPK are downregulated preventing invasive effects on cancer cells. A reduction in COX-2, PGE2 and PGE2 receptors prevents cancer cell migration, decreasing metastatic potential for melanoma cells.39 Berberine has been tested on the B16F10 melanoma cell lines through in vitro and in vivo tests in combination with doxorubicin. Berberine and doxorubicin combination caused tumor volume (85%) decrease and weight (78%) loss when compared to control mice.39
Pancratistatin:
Pancratistatin is obtained from the beach spider lily (Hemanocallis littoralis). It is thought that targets mitochondrial vulnerabilities which are unique to cancer cells. It induces apoptosis in melanoma cells in vitro. 39 When combined with tamoxifen, it was more effective that either agent alone both in the A375 and G361 human melanoma cell lines.39
Cannabinoids:
Although endocannabinoid system apparently does not influence melanoma growth and progression, a study showed that cannabinoid type 1 receptor might serve as a tumor-promoting signal in human melanoma cells.18 Moreover, activation of cannabinoid receptors in melanoma cells showed a decrease in angiogenesis, proliferation, and metastasis, by altering Akt protein and pRb phosphorylation.17 Anandamide, 2- arachidonoylglycerol, and palmitoylethanolamide have proven anti-melanoma effects in murine models. Additionally, mice treated with Tetrahydrocannabinol have shown inhibition of tumor growth and decreased melanoma viability and proliferation.17
2. Herbal formulas:
“Black salve” (Sanguinaria canadensis) has shown to induce melanoma-cells death through caspase signaling pathway and oxidative stress. We found 2 cases of melanoma treated with topical “black salve” by patient’s initiative. In both cases, the site of the application presented ulceration and evolved with local recurrence and metastatic disease.20 Furthermore, eschars formed by this formulation can mimic melanoma and obscure clinical evaluation.
3. Vitamin C:
At millimolar concentrations vitamin C reduced cell viability, invasiveness, and induced apoptosis in vitro. At micromolar concentrations promoted cell growth, migration, and cell cycle progression, and protected against mitochondrial stress, with higher tumor volume in mice compared to control group. Furthermore, vitamin C displayed synergistic cytotoxicity with Vemurafenib.46
Discussion:
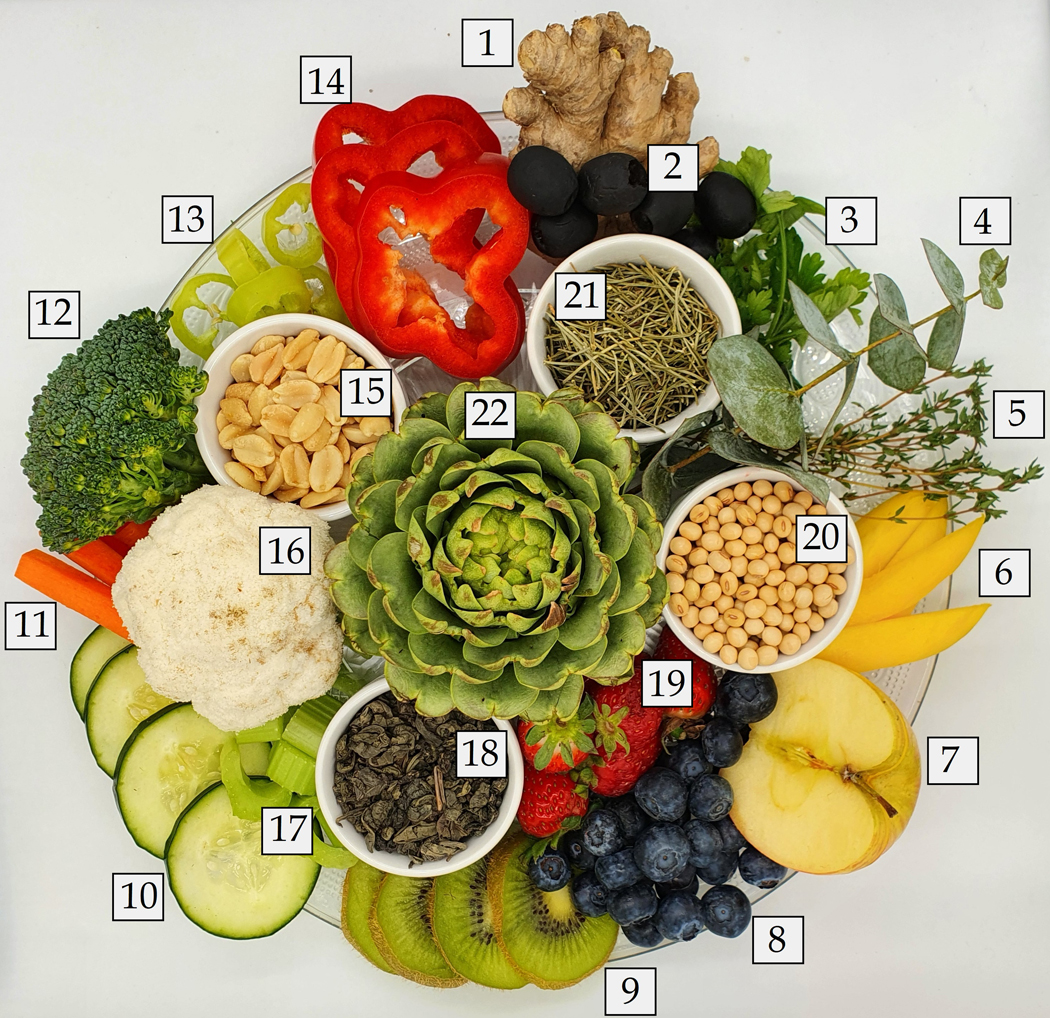
In this article, we have reviewed the published data on CAM on skin cancers. It is undeniable that many patients look for and use CAM therapies, so clinicians must be informed regarding the different compounds (Figure 1). The attitude and perception of CAM is improving among physicians, as show in an Italian study where 42% believed that CAM could have an integrative role.47 It is important to highlight that many ‘conventional’ dermatologic treatments widely used nowadays, have derived from ‘natural’ compounds (e.g., tacrolimus, 8-methoxypsoralen, podophyllin, and salicylates, among others).1 We believe that a comprehensive knowledge of the role of CAM (Table 1) can strengthen the patient-physician relationship, potentially improving patient care.1
Figure 1:
Examples of herbs with compounds studied on skin cancer.
Figure 1A: celery (red arrow), grape seeds (green arrow), ground turmeric (curcuma, on orange arrow), and parsley (blue arrow). Photographs by Karina Carrasco and Leonel Hidalgo.
There are several CAM therapies used on patients with skin cancer, and while most studies are in an experimental phase and have never been formally tested in humans, some have proven biological plausibility with potential clinical utility in the future. Clinicians should keep in mind that patient satisfaction from CAM ranges from 20% to 86% and specifically ask their patients about concurrent or past CAM use.48 Asking patients regarding CAM use is important given there are inherent risks associated to CAM usage, including (1) avoidance and/or delay of assessment of conventional treatments, (2) potential side effects as a direct result of the CAM itself or from the (3) interaction with concurrent or future conventional therapies. For instance, turmeric has been found to decrease CYP450 activity and to inhibit cyclophosphamide-induced apoptosis and tumor regression. For specific side effects and interactions with specific agents see weblinks in Table 1. Of CAM users, 37% have found to be at risk of interaction with their conventional therapies; and for Chinese herbs, this can reach up to 88%.49 This has special relevance when treating patients with comorbidities that use anticoagulants/antiplatelets or nonsteroidal anti-inflammatory drugs, where the risk of interaction is as high as 50%. Other drugs that may harm in combination with CAM are statins and hypoglycemic drugs.49 Particular consequences should be considered when treating metastatic disease with systemic drugs, where the risk of interaction is even greater. In patients with systemic melanoma who receive systemic therapy (including interferon, chemotherapy, BRAF-inhibitors, and ipilimumab) and concurrent CAM use, the risk of interaction was as high as 85%.49 Clinicians should also consider that CAMs have the potential of severe medical side effects (e.g. Ginkgo leaf extract has been linked to intracerebral hemorrhage) and not overlook these compounds. Furthermore, use of alternative therapies instead of conventional therapies was associated with worse survival rates for cancer patients.47
Conclusion:
Even though there is growing evidence for a role of CAM in skin cancer, most therapies currently used by patients have no formal medical indications and bear possible severe complications. Physicians should educate themselves on CAMs to further educate their patients and lower the risk of interactions or the risk of omission of traditional, evidence-based therapies. We encourage clinicians to specifically ask patients for CAM use, to evaluate and avoid potential side effects. Despite emerging studies on animals, to date, there is no evidence from human clinical trials supporting the effectiveness of any CAM in the treatment of skin cancer, and future research must be done to elucidate their role in this field.
Figure 1B:
1. Ginger; 2. Olives; 3. Parsley; 4. Eucalyptus; 5. Thyme; 6. Mangoes; 7. Apple; 8. Blueberries (one of the many kinds of berries); 9. Kiwis; 10. Cucumbers; 11. Carrots; 12. Broccoli; 13. Chili peppers; 14. Pepper; 15. Peanuts; 16. Cauliflower; 17. Celery; 18. Green tea; 19. Strawberries; 20. Soybeans; 21. Rosemary; 22. Artichokes. Photographs by Karina Carrasco and Leonel Hidalgo.
Founding source:
This research is funded in part by grant from the National Cancer Institute / National Institutes of Health (P30-CA008748) made to the Memorial Sloan Kettering Cancer Center.
Abbreviations used:
- Bcl-2
B-cell lymphoma 2
- ERK 1/2
Extracelular signal regulated kinase 1 and 2
- SCC
squamous cell carcinoma
- PCNA
Proliferating Cell Nuclear Antigen
- MMP-2
matrixmetalloproteinase-2
- MMP-9
matrixmetalloproteinase-9
- ATM
Ataxia-telangiectasia-mutated
- ATR
Ataxia telangiectasia and Rad3-related
- BRCA1
breast cancer 1
- Chk1
Checkpoint kinase 1
- Chk2
Checkpoint kinase 2
- TNFR
Tumor necrosis factor receptor
- NF-κB
nuclear factor kappa-light-chain-enhancer of activated B cells
- STAT3
Signal transducer and activator of transcription 3
- mTOR
mammalian Target of Rapamycin
- CB1
Cannabinod receptor type 1
- CB2
Cannabinod receptor type 2
- NMSC
Non-melanoma skin cancer
- Bcl-XL
B-cell lymphoma-extra large
- MAPK
Mitogen-activated protein kinase
- TYR
Tyrosinase
- TRP-1
Tyrosinase related protein 1
- TRP-2
Tyrosinase related protein 2
- mRNA
Messenger RNA
- FasL
Fas ligand
- IL-8
Interleukin 8
- PKCα
Protein kinase C alpha
- NO
Nitric oxide
- IL-6
Interleukin 6
- PI3K
phosphatidylinositide 3-kinases
- MAPK
mitogen-activated protein kinase
- JNK
c-Jun N-terminal kinases
- MITF
Microphthalmia-associated transcription factor
- CDK2
Cyclin- dependent kinase 2
- CDK4
Cyclin- dependent kinase 4
- TSP1
thrombospondin-1
- AP-1
Activator protein 1
- α-MSH
α-Melanocyte-stimulating hormone
- ROS
reactive oxygen species
- IL-1β
Interleukin 1 beta
- iNOS
Inducible nitric oxide synthase
- COX-2
Cyclooxygenase-2
- MMPs
matrixmetalloproteinases
- IL-12
Interleukin 12
- TNFα
Tumor necrosis factor alpha
- NLRP1
Nuclear localization leucine-rich-repeat protein 1
- IL-2
Interleukin 2
- IL-10
Interleukin 10
- DNA-PKcs
DNA-dependent protein kinase catalytic subunit expression
- PRL-3
Phosphatase of regenerating liver-3
- MST1
Mammalian Sterile 20-like kinase 1
- PDE
Cyclic nucleotide phosphodiesterases
- STAT1
Signal transducer and activator of transcription 1
- IFN-γ
Interferon gamma
- MPTP
Mitochondrial permeability transition pore opening
- HSP
Heat shock proteins
- CB1
Cannabinoid receptoy type 1
- CB2
Cannabinoid receptoy type 2
- PEA
Palmitoylethanolamide
- THC
Tetrahydrocannabinol
Footnotes
Conflict of interest: The authors have not conflict of interest to declare.
Consent for publication: The authors consent the publication of this submission (manuscript and figures).
Prior presentation: none.
IRB status: N/A.
References:
- 1.Pourang A, Hendricks AJ, Shi VY. Managing dermatology patients who prefer “all natural” treatments. Clin Dermatol 2020;38:348–53. [DOI] [PubMed] [Google Scholar]
- 2.Motoo Y, Yukawa K, Hisamura K, Tsutani K, Arai I. Internet survey on the provision of complementary and alternative medicine in Japanese private clinics: a cross-sectional study. J Integr Med 2019;17:8–13. [DOI] [PubMed] [Google Scholar]
- 3.Loquai C, Dechent D, Garzarolli M, et al. Use of complementary and alternative medicine: A multicenter cross-sectional study in 1089 melanoma patients. Eur J Cancer 2017;71:70–9. [DOI] [PubMed] [Google Scholar]
- 4.Dinehart SM, Alstadt K. Use of alternative therapies by patients undergoing surgery for nonmelanoma skin cancer. Dermatol Surg 2002;28:443–6. [DOI] [PubMed] [Google Scholar]
- 5.Söllner W, Zingg-Schir M, Rumpold G, Fritsch P. Attitude toward alternative therapy, compliance with standard treatment, and need for emotional support in patients with melanoma. Arch Dermatol 1997;133:316–21. [DOI] [PubMed] [Google Scholar]
- 6.Jellinek N, Maloney ME. Escharotic and other botanical agents for the treatment of skin cancer: a review. J Am Acad Dermatol 2005;53:487–95. [DOI] [PubMed] [Google Scholar]
- 7.Zhang YH, Peng HY, Xia GH, Wang MY, Han Y. Anticancer effect of two diterpenoid compounds isolated from Annona glabra Linn. Acta Pharmacol Sin 2004;25:937–42. [PubMed] [Google Scholar]
- 8.Takasaki M, Konoshima T, Murata Y, et al. Anticarcinogenic activity of natural sweeteners, cucurbitane glycosides, from Momordica grosvenori. Cancer Lett 2003;198:37–42. [DOI] [PubMed] [Google Scholar]
- 9.Hostanska K, Daum G, Saller R. Cytostatic and apoptosis-inducing activity of boswellic acids toward malignant cell lines in vitro. Anticancer Res 2002;22:2853–62. [PubMed] [Google Scholar]
- 10.Khuda-Bukhsh AR, Bhattacharyya SS, Paul S, Boujedaini N. Polymeric nanoparticle encapsulation of a naturally occurring plant scopoletin and its effects on human melanoma cell A375. Zhong Xi Yi Jie He Xue Bao 2010;8:853–62. [DOI] [PubMed] [Google Scholar]
- 11.Auriemma M, Di Nicola M, Gonzalez S, Piaserico S, Capo A, Amerio P. Polypodium leucotomos supplementation in the treatment of scalp actinic keratosis: could it improve the efficacy of photodynamic therapy? Dermatol Surg 2015;41:898–902. [DOI] [PubMed] [Google Scholar]
- 12.Prasad RR, Paudel S, Raina K, Agarwal R. Silibinin and non-melanoma skin cancers. J Tradit Complement Med 2020;10:236–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao G, Han X, Cheng W, et al. Apigenin inhibits proliferation and invasion, and induces apoptosis and cell cycle arrest in human melanoma cells. Oncol Rep 2017;37:2277–85. [DOI] [PubMed] [Google Scholar]
- 14.Carletto B, Berton J, Ferreira TN, et al. Resveratrol-loaded nanocapsules inhibit murine melanoma tumor growth. Colloids Surf B Biointerfaces 2016;144:65–72. [DOI] [PubMed] [Google Scholar]
- 15.Almalki Z, Algregri M, Alhosin M, Alkhaled M, Damiati S, Zamzami MA. In vitro cytotoxicity of curcuminoids against head and neck cancer HNO97 cell line. Braz J Biol 2021;83:e248708. [DOI] [PubMed] [Google Scholar]
- 16.Cheng AL, Hsu CH, Lin JK, et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res 2001;21:2895–900. [PubMed] [Google Scholar]
- 17.Ladin DA, Soliman E, Griffin L, Van Dross R. Preclinical and Clinical Assessment of Cannabinoids as Anti-Cancer Agents. Front Pharmacol 2016;7:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carpi S, Fogli S, Polini B, et al. Tumor-promoting effects of cannabinoid receptor type 1 in human melanoma cells. Toxicol In Vitro 2017;40:272–9. [DOI] [PubMed] [Google Scholar]
- 19.Lim A Black salve treatment of skin cancer: a review. J Dermatolog Treat 2018;29:388–92. [DOI] [PubMed] [Google Scholar]
- 20.Leecy TN, Beer TW, Harvey NT, et al. Histopathological features associated with application of black salve to cutaneous lesions: a series of 16 cases and review of the literature. Pathology 2013;45:670–4. [DOI] [PubMed] [Google Scholar]
- 21.Lambert JD, Sang S, Dougherty A, et al. Cytotoxic lignans from Larrea tridentata. Phytochemistry 2005;66:811–5. [DOI] [PubMed] [Google Scholar]
- 22.Lo CY, Liu PL, Lin LC, et al. Antimelanoma and antityrosinase from Alpinia galangal constituents. ScientificWorldJournal 2013;2013:186505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakashima S, Oda Y, Nakamura S, et al. Inhibitors of melanogenesis in B16 melanoma 4A5 cells from flower buds of Lawsonia inermis (Henna). Bioorg Med Chem Lett 2015;25:2702–6. [DOI] [PubMed] [Google Scholar]
- 24.Meng TX, Irino N, Kondo R. Melanin biosynthesis inhibitory activity of a compound isolated from young green barley (Hordeum vulgare L.) in B16 melanoma cells. J Nat Med 2015;69:427–31. [DOI] [PubMed] [Google Scholar]
- 25.Nakashima S, Matsuda H, Oda Y, Nakamura S, Xu F, Yoshikawa M. Melanogenesis inhibitors from the desert plant Anastatica hierochuntica in B16 melanoma cells. Bioorg Med Chem 2010;18:2337–45. [DOI] [PubMed] [Google Scholar]
- 26.Ghosh S, Bishayee K, Paul A, et al. Homeopathic mother tincture of Phytolacca decandra induces apoptosis in skin melanoma cells by activating caspase-mediated signaling via reactive oxygen species elevation. J Integr Med 2013;11:116–24. [DOI] [PubMed] [Google Scholar]
- 27.Chakraborty D, Ghosh S, Bishayee K, Mukherjee A, Sikdar S, Khuda-Bukhsh AR. Antihyperglycemic drug Gymnema sylvestre also shows anticancer potentials in human melanoma A375 cells via reactive oxygen species generation and mitochondria-dependent caspase pathway. Integr Cancer Ther 2013;12:433–41. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg KH, Yin AC, Mupparapu A, Retzbach EP, Goldberg GS, Yang CF. Components in aqueous Hibiscus rosa-sinensis flower extract inhibit in vitro melanoma cell growth. J Tradit Complement Med 2017;7:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barbieri A, Quagliariello V, Del Vecchio V, et al. Anticancer and Anti-Inflammatory Properties of Ganoderma lucidum Extract Effects on Melanoma and Triple-Negative Breast Cancer Treatment. Nutrients 2017;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valiahdi SM, Iranshahi M, Sahebkar A. Cytotoxic activities of phytochemicals from Ferula species. Daru 2013;21:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ling B, Michel D, Sakharkar MK, Yang J. Evaluating the cytotoxic effects of the water extracts of four anticancer herbs against human malignant melanoma cells. Drug Des Devel Ther 2016;10:3563–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shin DH, Kim OH, Jun HS, Kang MK. Inhibitory effect of capsaicin on B16-F10 melanoma cell migration via the phosphatidylinositol 3-kinase/Akt/Rac1 signal pathway. Exp Mol Med 2008;40:486–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Danciu C, Borcan F, Bojin F, Zupko I, Dehelean C. Effect of the isoflavone genistein on tumor size, metastasis potential and melanization in a B16 mouse model of murine melanoma. Nat Prod Commun 2013;8:343–6. [PubMed] [Google Scholar]
- 34.Aronchik I, Kundu A, Quirit JG, Firestone GL. The antiproliferative response of indole-3-carbinol in human melanoma cells is triggered by an interaction with NEDD4–1 and disruption of wild-type PTEN degradation. Mol Cancer Res 2014;12:1621–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaid M, Singh T, Prasad R, Katiyar SK. Bioactive proanthocyanidins inhibit growth and induce apoptosis in human melanoma cells by decreasing the accumulation of β-catenin. Int J Oncol 2016;48:624–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pal HC, Baxter RD, Hunt KM, et al. Fisetin, a phytochemical, potentiates sorafenib-induced apoptosis and abrogates tumor growth in athymic nude mice implanted with BRAF-mutated melanoma cells. Oncotarget 2015;6:28296–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwak JY, Seok JK, Suh HJ, et al. Antimelanogenic effects of luteolin 7-sulfate isolated from Phyllospadix iwatensis Makino. Br J Dermatol 2016;175:501–11. [DOI] [PubMed] [Google Scholar]
- 38.Ju EM, Lee SE, Hwang HJ, Kim JH. Antioxidant and anticancer activity of extract from Betula platyphylla var. japonica. Life Sci 2004;74:1013–26. [DOI] [PubMed] [Google Scholar]
- 39.Sood S, Jayachandiran R, Pandey S. Current Advancements and Novel Strategies in the Treatment of Metastatic Melanoma. Integr Cancer Ther 2021;20:1534735421990078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alipanah H, Farjam M, Zarenezhad E, Roozitalab G, Osanloo M. Chitosan nanoparticles containing limonene and limonene-rich essential oils: potential phytotherapy agents for the treatment of melanoma and breast cancers. BMC Complement Med Ther 2021;21:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, Lei Z, Huang Z, et al. Epigallocatechin-3-gallate(EGCG) suppresses melanoma cell growth and metastasis by targeting TRAF6 activity. Oncotarget 2016;7:79557–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mirzaei H, Naseri G, Rezaee R, et al. Curcumin: A new candidate for melanoma therapy? Int J Cancer 2016;139:1683–95. [DOI] [PubMed] [Google Scholar]
- 43.Zhao G, Han X, Zheng S, et al. Curcumin induces autophagy, inhibits proliferation and invasion by downregulating AKT/mTOR signaling pathway in human melanoma cells. Oncol Rep 2016;35:1065–74. [DOI] [PubMed] [Google Scholar]
- 44.Zhang YP, Li YQ, Lv YT, Wang JM. Effect of curcumin on the proliferation, apoptosis, migration, and invasion of human melanoma A375 cells. Genet Mol Res 2015;14:1056–67. [DOI] [PubMed] [Google Scholar]
- 45.Zheng M, Ekmekcioglu S, Walch ET, Tang CH, Grimm EA. Inhibition of nuclear factor-kappaB and nitric oxide by curcumin induces G2/M cell cycle arrest and apoptosis in human melanoma cells. Melanoma Res 2004;14:165–71. [DOI] [PubMed] [Google Scholar]
- 46.Yang G, Yan Y, Ma Y, Yang Y. Vitamin C at high concentrations induces cytotoxicity in malignant melanoma but promotes tumor growth at low concentrations. Mol Carcinog 2017;56:1965–76. [DOI] [PubMed] [Google Scholar]
- 47.Berretta M, Rinaldi L, Taibi R, et al. Physician Attitudes and Perceptions of Complementary and Alternative Medicine (CAM): A Multicentre Italian Study. Front Oncol 2020;10:594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vapiwala N, Mick R, Hampshire MK, Metz JM, DeNittis AS. Patient initiation of complementary and alternative medical therapies (CAM) following cancer diagnosis. Cancer J 2006;12:467–74. [DOI] [PubMed] [Google Scholar]
- 49.Loquai C, Schmidtmann I, Garzarolli M, et al. Interactions from complementary and alternative medicine in patients with melanoma. Melanoma Res 2017;27:238–42. [DOI] [PubMed] [Google Scholar]
- 50.Lopez G, Mao JJ, Cohen L. Integrative Oncology. Med Clin North Am 2017;101:977–85. [DOI] [PubMed] [Google Scholar]