Abstract
Background and Aims
Alcohol use disorder (AUD) is associated with increased risk of non-fatal suicide attempt. We aimed to measure the strength and mechanistic nature of the association between AUD and increased suicide attempt and determine any causal pathways and/or shared risk factors.
Design
We used Cox proportional hazards models in population-level and co-relative analyses to evaluate the risk of first non-fatal suicide attempt as a function of previous AUD.
Setting and Participants
We used continuously updated longitudinal nationwide Swedish registry data on native Swedes born from 1950 to 1970 (n = 2 229 619) and followed from age 15 until 2012.
Measurements
AUD and suicide attempt were identified using International Classification of Diseases (ICD)-8, ICD-9, and ICD-10 codes. AUD was also identified using pharmacy and criminal records. Genetic and family environmental risks were derived based on relatedness via the Multi-Generation Register and shared residency via the Population and Housing Census and the Total Population Register.
Findings
AUD was robustly associated with suicide attempt in crude models (hazard ratio [HR] = 15.24 [95% CI: 14.92, 15.56]). In models adjusted for sociodemographic factors and psychiatric comorbidity, the association was attenuated: for women, HRs declined gradually across time, ranging from 5.55 (3.72, 8.29) during the observation period that ranged from age 15 to 19 years to 1.77 (1.65, 1.90) at age 40 or older. For men, the corresponding figures were 6.12 (4.07, 9.19) and 1.83 (1.72, 1.94); in contrast to women, risk of suicide attempt among men increased from age 15 to 29 before declining. In co-relative models, a residual association remained, consistent with a causal path from AUD to suicide attempt.
Conclusions
In Sweden, alcohol use disorder appears to be an important predictor of suicide attempt even in the context of other psychiatric disorders. The observed association is likely the result of features that jointly impact risk of alcohol use disorder and suicide attempts (genetic liability, psychiatric illness, and childhood stressors) and a potentially causal pathway, acting independently or in conjunction with one another.
Keywords: Alcohol use disorder, cohort study, comorbidity, correlative model, registry data, suicide attempt
INTRODUCTION
Non-fatal suicide attempts are a persistent public health concern, with a predicted worldwide lifetime prevalence of 2.7% [1]. Suicide attempt is a prominent predictor of later death by suicide [2–5], with nearly 4% of individuals who seek medical attention for self-harm dying by suicide within the subsequent 5 years [6]. However, prior studies have noted differences between fatal and non-fatal suicidal behavior [7–13], including across age and gender (attempts are more common among young people and women, whereas deaths are more common among adults and men), and with respect to the strength of associations with psychiatric illnesses (e.g. anxiety disorders are more strongly associated with attempts than death, whereas non-affective psychosis is more strongly associated with death). To improve efforts at risk prediction, prevention, and intervention, efforts to clarify the specific predictors behind both suicide attempt and suicide death are needed.
Substance use disorders, including alcohol use disorder (AUD), have been identified as among the strongest predictors of suicidal ideation, attempts, and death [9,12,14–19]. Many prior studies of AUD and suicidal behavior have been limited by one or more of the following features: (i) the use of selected/non-representative samples (e.g., psychiatric patients); (ii) small samples with insufficient statistical power; (iii) the inability to jointly account for other potential risk factors, such as psychiatric comorbidity; or (iv)a focus on the association without efforts to determine its source(s). Therefore, although the association between AUD and suicidal behavior has strong support from previous studies, the strength and mechanistic nature of the AUD-suicide attempt association within the general population remain unclear.
We previously reported a strong relationship between AUD and suicide death [20]. That association remained prominent even after accounting for psychiatric comorbidity and was attributable to both shared familial liability—latent genetic and/or familial environmental factors that jointly influence risk for both outcomes—and to a potentially causal pathway in which AUD increased one’s risk of suicide. Whether AUD is similarly related to non-fatal suicide attempt has not yet been explored in a similarly sized sample. Improving our understanding of this relationship is critical: attempts are up to 30 times more common than suicide death [21] and present significant societal costs in the form of economic and psychological burdens [22–24]. Clarification of the AUD-attempt relationship may reveal new opportunities for prevention that would impact a potentially large group of people.
Here, we explore the association between AUD and non-fatal suicide attempt in the Swedish population born in 1950 to 1970 to clarify how the strength of the association is impacted by controlling for, and compares to the effect of, psychiatric comorbidity; whether and how this association changes across the life course and as a function of AUD age of onset; and potential mechanisms underlying the association. These mechanisms might include a causal pathway; latent familial confounding factors that jointly contribute to both outcomes, including genetic influences and shared environmental exposures; or both.
METHODS
Sample
Native Swedish citizensborn between 1950and 1970who had not died or emigrated by age 15 were eligible for inclusion (n = 2 232 747). Observations began at age 15 and ended at suicide attempt, death, emigration from Sweden, or in 2012. Individuals who had attempted suicide (n = 860) or had an AUD registration (n = 2111) before age 15 were censored. Individuals with a suicide attempt registration on the same day as a suicide death were excluded (n = 157). Those with other psychiatric diagnoses before age 15 were retained in the model; for the purposes of time-dependent covariates, these were coded as occurring at age 15. These exclusions resulted in a total sample size of n = 2 229 619 for the current analyses. The study was approved by the Regional Ethical Review Board in Lund. Patient consent was waived because of the secondary nature of the data.
Swedish population registers with national coverage were used to identify suicide attempts, diagnostic status for psychiatric predictors and covariates/confounders, and sociodemographic covariates (parental education and birth year). The availability and content of these registers have been described previously [25,26]. Registers are available for: primary and secondary inpatient and outpatient diagnoses; criminal and suspicion records; prescription records; the Multi-Generation Register; and the National Census Registry and Total Population Registry. Records are linked using unique personal identification numbers, which are replaced by pseudonymized serial numbers to maintain confidentiality. Additional details are available in the Supporting information.
Outcome and predictor variables
The outcome of interest was an individual’s first observed suicide attempt during the observation period. The predictor of primary interest was AUD. Adjusted models included other psychiatric diagnoses as potential confounders. The Supporting information provides International Classification of Diseases (ICD) codes used to identify suicide attempts (e.g. E950-E959, X60-X84), diagnostic status for AUD (e.g. 291,F10[excludingF10.0]),and status for other psychiatric covariates, consistent with prior studies [27,28].
Statistical analyses
Primary analyses
We used Cox proportional hazards models with robust standard errors to test the AUD-suicide attempt association. AUD and other registrations derived from ICD codes were included as time-varying covariates at the level of the month. From age 15 until the first AUD-related registration, an individual was considered to not have AUD; beyond the first AUD registration, the individual was considered to have AUD. Mean parental education and birth year were included as covariates to account for socioeconomic status and potential cohort effects. Hazard ratios (HRs) and 95% CI are reported for all variables. All analyses were conducted in SAS 9.4 (2002–2012 SAS Institute).
Age of AUD onset
We conducted a modified version of the primary model to estimate AUD-based HRs for suicide attempt as a function of AUD age of onset. Additional details are presented in the Supporting information.
Co-relative analyses
We identified sets of same-sex cousins, half-siblings, and full siblings born within 10 years of one another for inclusion in co-relative analyses, which controlled for shared familial factors that may confound the AUD-suicide attempt association by testing for effects within family strata. Sets of relatives who are discordant in exposure to the putative risk factor (here, AUD) at some point in time are informative. Individuals who were members of more than one relative pair meeting our criteria (same sex and born within 10 years) were included in multiple datasets. These analyses included the following numbers of informative sets: cousins, 67 489; half-siblings, 17 451; and full siblings, 40 215. A supplementary co-relative analysis was conducted that extrapolated results to discordant monozygotic twin pairs, which we otherwise lacked sufficient statistical power to test, particularly in women.
These analyses were not pre-registered and should be considered exploratory.
RESULTS
Descriptive statistics
The cohort consisted of n = 2 229 619 individuals (48.6% women). Table 1 provides descriptive statistics for the sample. The overall prevalence of AUD and non-fatal suicide attempt were 5.1% and 3.6%, respectively. AUD was more common among men, whereas suicide attempt was slightly more common among women. Among those with a lifetime AUD registration, 26.7% (n = 30 655) had a suicide attempt, with a mean (SD) time to suicide attempt (from age 15) of 19.3 (11.1) years and a median of 18.4; 2.3% (n = 48933) of those with no AUD registration had a lifetime suicide attempt, with a mean time to suicide attempt of 21.2 (11.8) years and a median of 21.8. The first AUD registration preceded the first suicide attempt for n = 12 297 (40.1%) individuals, with a mean latency between AUD registration and suicide attempt of 7.3 (SD = 7.4) years and a median of 4.8 years. In a crude logistic regression, a lifetime AUD registration was associated with lifetime suicide attempt (OR = 15.41 [95% CI = 15.16, 15.65]).
Table 1.
Descriptive statistics for sample.
| Total n = 2 229 619 | Women n = 1 084 033 | Men n = 1 145 586 | |
|---|---|---|---|
|
| |||
| Lifetime alcohol use disorder n (%) | 114 674 (5.1) | 32730 (3.0) | 81944 (7.2) |
| Lifetime non-fatal suicide attempt n (%) | 79588 (3.6) | 39650 (3.7) | 39938 (3.5) |
| Age at first AUD registration Mean (SD) |
39.6 (11.5) | 40.0 (11.7) | 39.4 (11.5) |
| n (%) at age 15–24 | 16735 (0.75) | 4854 (0.45) | 11881 (1.04) |
| n (%) at age 25–34 | 22645 (1.02) | 5526 (0.51) | 17119 (1.49) |
| n (%) at age 35–44 | 33390 (1.50) | 9656 (0.89) | 23734 (2.07) |
| n (%) at age 45–54 | 32366 (1.45) | 9864 (0.91) | 22502 (1.96) |
| n (%) at age 55–62b | 9538 (0.43) | 2830 (0.26) | 6708 (0.59) |
| Age at first suicide attempt Mean (SD) |
35.5 (11.5) | 34.5 (11.8) | 36.4 (11.2) |
| n (%) at age 15–24 | 19.217 (0.86) | 11.017 (1.02) | 8200 (0.72) |
| n (%) at age 25–34 | 19535 (0.88) | 9432 (0.87) | 10103 (0.88) |
| n (%) at age 35–44 | 22031 (0.99) | 10448 (0.96) | 11583 (1.01) |
| n (%) at age 45–54 | 15273 (0.69) | 7119 (0.66) | 8154 (0.71) |
| n (%) at age 55–62b | 3532 (0.16) | 1634 (0.15) | 1898 (0.17) |
| Mid-parent educationa | |||
| 1 | 833 528 (38.9) | 404 410 (38.8) | 429 118 (39.0) |
| 1.5 | 465 605 (21.8) | 226 922 (21.8) | 238 683 (21.7) |
| 2 | 502 861 (23.5) | 245 427 (23.6) | 257 434 (23.4) |
| 2.5 | 171 808 (8.0) | 83165 (8.0) | 88643 (8.1) |
| 3 | 166909 (7.8) | 81177 (7.8) | 85732 (7.8) |
Data was available through December 2012, at which point the oldest members of the cohort were 62.
Parental education was coded as follows: 1 = 9 or fewer years; 2 = 10–11 years; 3 = 12 years or more. Mid-parental education considers both parents’ educational attainment. AUD = alcohol use disorder.
Survival models
In a crude survival model where AUD was included as a time-varying predictor of suicide attempt, the resulting HR was 15.24 (14.92, 15.56). We tested for an interaction between AUD and sex. The resulting HR (HR = 1.19 [1.14, 1.25]) indicated that the association was stronger among women; we, therefore, stratified subsequent analyses by sex.
We assessed whether the data were consistent with the proportionality assumption of the Cox model by examining the Kaplan–Meier curves and testing whether the interaction between the time-dependent AUD predictor and the log of time was significant. Non-parallel curves and significant proportionality tests (P < 0.05) indicated a deviation from proportionality across time. For the primary models, we, therefore, estimated HRs separately for 5-year age of observation increments (ages 15–19, 20–24, 25–29, 30– 34, 35–39, and 40+). For the observation period of age 15 to 19, the HR for AUD is a function of individuals whose AUD registrations occurred during this time period compared to controls. For the observation period from age 20 to 24, the HR for AUD still includes those with AUD onset between ages 15 to 19, but now also includes those with AUD onset from 20to24. That is, as the observation period progresses, the number of AUD cases increases (as cases accumulate over time) and the number of controls decreases (because those who did not have an AUD registration earlier in life get one later in life).
In crude models, uncorrected for covariates but stratified by sex, AUD was strongly associated with suicide attempt from age 15 to 19 for women (HR = 22.58 [18.10, 28.16]) and men (HR = 26.10 [21.08, 32.31]) and remained elevated across ages (Supporting information Table S1 and Supporting information Fig. S1). Adjusting for birth year and parental education did not substantively impact results (Supporting information Table S1).
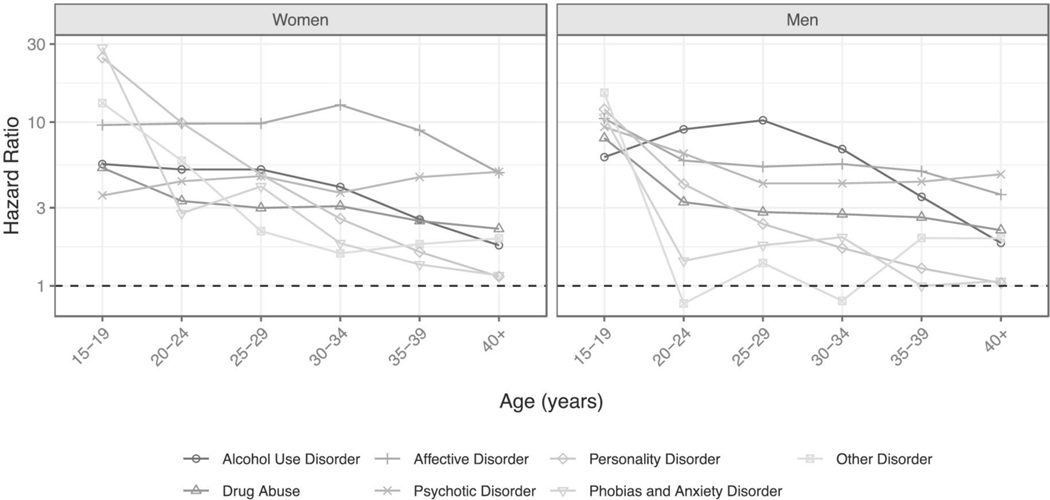
We next adjusted for psychiatric comorbidity. Results are depicted in Fig. 1, with complete estimates provided in Supporting information Table S2. HRs were comparable across sex for ages 15 to 19 (HRwomen = 5.55, HRmen = 6.12), but diverged as time elapsed. For women, risk remained stable through age 29 before declining gradually. For men, HRs increased through age 29 to a maximum of 10.26 before declining. By age 40 and later, risk of suicide attempt remained modestly elevated for both sexes (HRwomen = 1.77, HRmen = 1.83).
Figure 1.
Hazard ratios (HR) for alcohol use disorder and psychiatric covariates from survival models estimating their association with first suicide attempt, adjusted for sociodemographic covariates. The y-axis is on the log scale. The horizontal dashed black line represents the null (HR = 1). CIs are excluded because of their breadth and are presented in Supporting information Table S2
Age of AUD onset
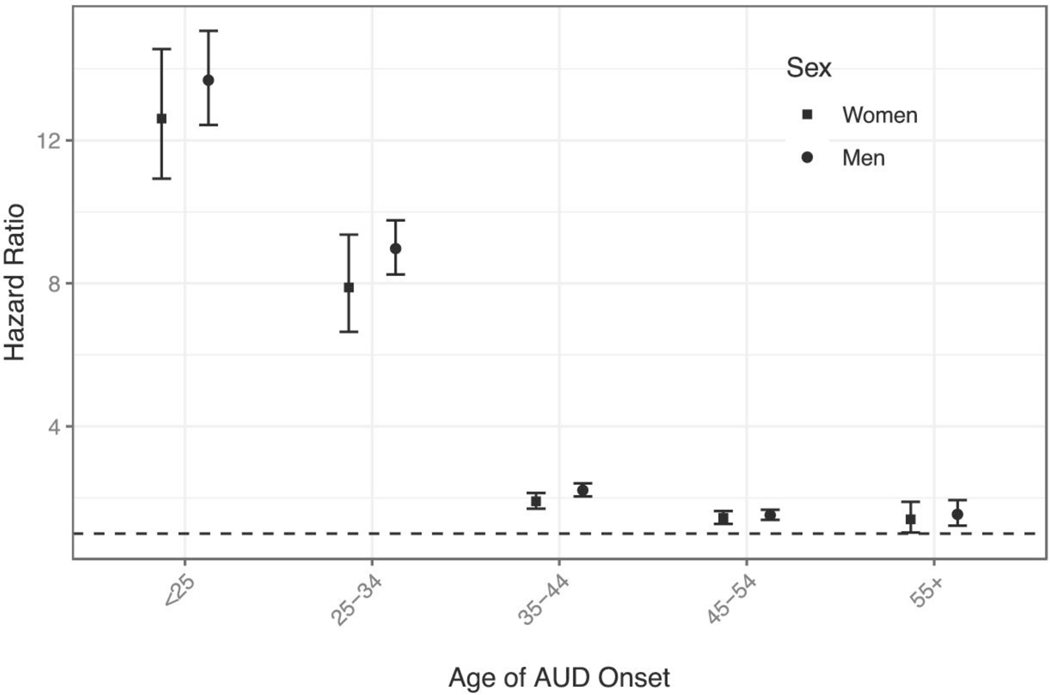
Early onset of AUD is frequently considered an indicator of severity and of propensity toward externalizing behavior. We therefore evaluated whether the association between AUD and attempt varied as a function of AUD age of onset (binned into the following ranges: <25 years of age, 25–34, 35–44, 45–54, 55+). Suicide attempts were more common among those with an earlier AUD onset: 45.5% (n = 7614) of thosewhosefirst AUD registration was before age 25had a lifetime suicide attempt, and this rate declined across age bins to 9.6% (n = 919) among the latest AUD onset group. We next tested this association in the context of a Cox model, where the HR for psychiatric covariates was averaged across time because of estimation difficulties. For both sexes, risk of suicide attempt was lower among those with later AUD onset relative to onset by age 25. Figure 2 depicts the AUD-based HR for suicide attempt for the first relevant observation period (i.e. before age 25 for those with AUD onset before age 25; age 25–34 for those with AUD onset during that time; etc.) See Supporting information Table S4 for results across observation periods.
Figure 2.
Hazard ratios (HR) (95% CI) for suicide attempt as a function of age of alcohol use disorder onset. Estimates for the first possible period of observation are presented; see Supporting information Table S4 for results across all periods of observation. Y-axis is on the log scale. The dashed horizontal black line represents a HR of 1 (no increased risk of suicide attempt)
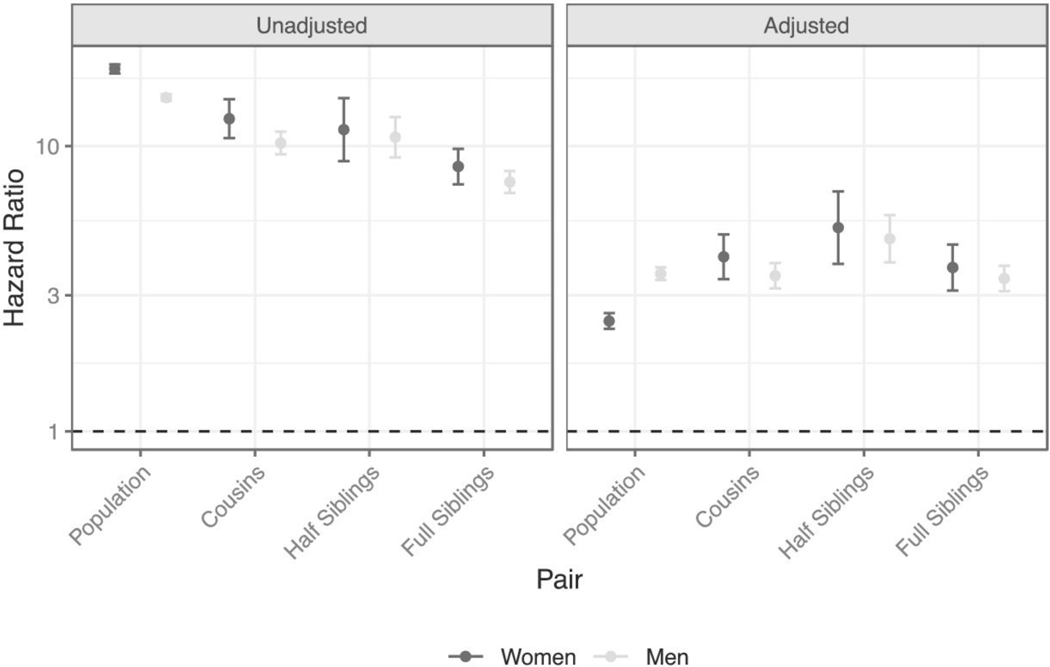
Co-relative model
We conducted co-relative models without stratification into 5-year observation bins because of insufficient sample sizes within co-relative groups. In models unadjusted for psychiatric comorbidity, we observed a decline in HRs from the population level to full siblings as increasing familial confounding was accounted for in both women and men, although half-siblings deviated somewhat from this trend (Fig. 3, left panel). In models adjusted for psychiatric comorbidity, HRs were attenuated (Fig. 3, right panel), consistent with the primary results. Although AUD-based risk was somewhat elevated among half-sibling pairs, which have often experienced familial disruption, HRs were quite consistent across cousins and full-siblings despite the discrepancy in genetic relatedness. Furthermore, HRs exceeded 1, where a HR of 1 would indicate no increased risk of attempt as a function of AUD status. This pattern is generally consistent with a causal pathway from AUD to suicide attempt.
Figure 3.
Hazard ratios (HR) and 95% CI between alcohol use disorder and suicide attempt for co-relative pairs discordant for exposure to or timing of AUD. The HR for the overall population is provided for comparison. Estimates unadjusted and adjusted for psychiatric comorbidity are presented in the left and right panels, respectively. The y-axis is on the log scale. Horizontal black dashed line represents the null (HR = 1)
We were underpowered for estimating HRs among monozygotic twin pairs, which, when feasible, act as a powerful group for inferring causality. We, therefore, applied a previously developed method of extrapolating estimates for this group [29]. In these models, the AUD-suicide attempt association for female monozygotic twins was HR = 3.75 (2.89, 4.87), and for male monozygotic twins was HR = 3.63 (3.08, 4.28) (see Supporting information Table S5 for full results), closely paralleling estimates for cousins and full-siblings.
DISCUSSION
The current results demonstrate that alcohol use disorder is a prominent risk factor for suicide attempts, and suggest that this association is attributable to both shared familial liability and a causal influence of AUD. We observed differences across sex with respect to the overall strength of the association, which was higher for men in models adjusted for sociodemographic and psychiatric covariates, and temporal changes in risk. Other key findings are that accounting for psychiatric comorbidity attenuates the association between AUD and suicide attempt but does not eliminate it, and that individuals with earlier AUD onset are at highest risk of suicide attempt.
Comparison to other psychiatric predictors
Although affective disorders are frequently considered important predictors of suicidal behavior [30]—indeed, suicidal thoughts or behaviors are a symptom of major depression—AUD has received less attention as an indicator of risk. In the current study, the strength of the association between AUD and suicide attempt relative to other psychiatric predictors varied as a function of age (Fig. 1 and Supporting information TableS2). Among women age 15 to 19, phobia/anxiety and personality disorders were the most prominent predictors with HRs of ~25 to 28, whereas the corresponding HR for AUD was 5.55. However, during later observation periods, AUD’s association with suicide attempt exceeded or closely matched those disorders’ effects. Although the HRs for most predictors diminished across time, the reduction of AUD’s impact was more gradual. Ultimately, affective and psychotic disorders emerged as stronger/more consistent predictors of risk relative to AUD, particularly among older women.
We observed a different pattern among men, for whom, at ages 15 to 19, AUD had the lowest HR among predictors. However, during the observation period spanning ages 20 to 34, AUD was the most prominent predictor of suicide attempt. As with women, affective and psychotic disorders were stronger predictors than AUD in later adulthood. These findings are consistent with serious mental illness being a critical risk factor for suicide attempts [9,31], while underscoring the clinical relevance of AUD even after accounting for psychiatric comorbidity. Our results highlight the need to account for life stage with respect to risk evaluation: AUD may be an especially useful indicator of suicide attempt risk in early/mid-adulthood, whereas other psychiatric predictors might be more informative in adolescence or later adulthood.
Age of AUD onset
Our finding that early-onset AUD was more strongly associated with suicide attempt is consistent with evidence that early onset is an indicator of AUD severity [32–35]. In classic typologies of AUD, early onset is more strongly related to impulsivity/externalizing and psychiatric comorbidity [36,37]. Our findings provide support for a joint role of AUD and other psychiatric conditions on risk of suicide attempt, although we did not directly test whether the effect of early onset AUD was especially strongly mediated by other psychiatric conditions. Prior studies indicate that early initiation of alcohol use is associated with greater risk of subsequent AUD [38] and suicidal behavior [39–41]; this group may be an important target for intervention/prevention. Family-based and communitywide efforts have shown promise in this area [42–44], although parental rules regarding alcohol use are not always effective [45].
Co-relative models
The pattern of decreasing HRs across pairs of increasing relatedness in unadjusted models (Fig. 3, left panel) suggests that the association between AUD and suicide attempt was confounded at least in part by genetic and familial environmental factors that jointly influence both outcomes. Co-relative models do not require specification of individual risk factors, but molecular genetic studies provide support for shared genetic liability across alcohol misuse and suicidality [46], and family environmental exposures such as parental divorce [47,48] and harsh parenting [49,50] have been associated with both outcomes.
In models adjusted for psychiatric comorbidity (Fig. 3, right panel), HRs across relative pairs were more consistent, particularly among men, and remained considerably above one. This, in conjunction with findings from the supplementary analysis in which extrapolated HRs for discordant monozygotic twins were 3.63–3.75 (Supporting information Table S4), provides evidence consistent with a causal pathway from AUD to suicide attempt. Overall, these results suggest two contributions to the AUD-suicide attempt association, which may act independently or in conjunction with one another: (i) shared familial factors—in particular, those that predispose to psychiatric illness in general; and (ii) a causal pathway from AUD to non-fatal suicide attempt.
The causal role of AUD in suicidality may take many forms. One straightforward possibility is that acute intoxication may facilitate suicidality [51–53], potentially by its impact on impulsivity and behavioral disinhibition [54,55]. Alcohol-induced depressive episodes may also play an important role in suicide attempt risk [56,57]. With respect to less direct explanations, one study found that individuals with AUD were more likely than controls to attempt suicide on the same day as experiencing a stressful life event, suggesting that these individuals may be more sensitive to such events [58]. Other work suggests that the nature of stressors experienced by individuals in the weeks preceding suicide death differs across those with alcohol or substance use disorders versus mood disorders; specifically, the former experience more arguments and attachment disruptions (e.g. divorce) [59]. Although our use of registry data precludes direct testing of some of these possibilities, others should be the focus of future analyses.
Comparison to suicide death
Comparison of the current results from adjusted models to our previous report of the association between AUD and suicide death reveals potentially important differences alongside some similarities. First, the HRs for suicide attempt (1.77–10.26) are lower than those for suicide death (HR = 2.44–128.0) [20]. This is inconsistent with results of a meta-analysis of the association between AUD and suicide attempt versus death, which reported a slightly higher OR for attempt than death, although with overlapping CI [60]. However, few prior studies have assessed both relationships within the same sample. An exception is a study of Swedish conscripts born 1950 to 1951 [61], who are included in the current study; in that report, AUD was identified using only inpatient records, and was more strongly associated with attempt than suicide death.
Second, we observe different patterns of risk across sexes for suicide attempt versus death. For attempts, the magnitude of AUD-based risk differed much less across sexes than for death: for example, the HRs for ages 15 to 19 were HRwomen = 5.55 (3.72, 8.29) and HRmen = 6.12 (4.07, 9.19) for attempts, compared to HRwomen = 128.0 (76.1, 215.1) and HRmen = 28.0 (17.7, 44.3) for deaths [20]. This could reflect the hypothesis that women who manifest AUD (or other substance use disorders) may have a higher underlying liability than do men with the same disorder, given social constraints on, and stigma against, women’s substance use [62,63]. Under this model, women whose biological and/or environmental liability to AUD meets/exceeds the threshold required to manifest alcohol problems have a higher propensity for more severe negative outcomes, such as suicide death. Finally, although for suicide death, AUD-based risk declined—precipitously at first, then gradually—across observation time for both sexes, a different pattern emerged for suicide attempt. Namely, risk declined gradually for women across observation time/age, whereas for men, AUD-based risk increased from age 15 to 29, then declined.
We also observed similarities between suicide attempt and death. First, early onset AUD was more strongly associated with both suicide attempt and death than onset after age 25. Second, accounting for psychiatric comorbidity strongly attenuated the association between AUD and both outcomes. Therefore, for both suicide attempt and suicide death, psychiatric problems capture a non-trivial component of familial and other confounding factors that underlie the AUD-suicidal behavior association. Finally, the HRs from our analysis that extrapolated to monozygotic twin pairs were strikingly similar across outcomes, ranging from HR = 3.63–3.75. Although estimates were averaged across observation time because of limited sample sizes for co-relative models, these findings support a causal role for AUD in both suicidal behavior outcomes.
CONCLUSIONS
These observations have clinical implications. First, individuals with AUD are at greater risk for more severe suicidality, including attempts that warrant medical attention, and should be monitored accordingly, potentially by enhanced clinical screening for suicidality risk on AUD diagnosis and/or referral to mental health care providers. Where possible, the affected individual and their family members should be educated about risks of suicidality and potential warning signs. Second, this increased risk applies to both sexes, although it differs in magnitude depending on outcome (attempt versus death). Therefore, although suicide attempts are more common among women, the introduction of AUD as a risk factor complicates assumptions about risk of suicidal behavior. Third, the shifts across the life course with respect to AUD-based risk of suicide attempt underscore the need for continuous monitoring. Women with AUD are at highest risk in late adolescence and their male counterparts’ risk peaks at around age 30. Therefore, health care providers should be aware that individuals with AUD may defy expectations about when risk of suicidal behavior is of greatest concern.
The current findings should be interpreted in the context of several limitations. First, our use of Swedish national registries to identify AUD and psychiatric predictors limits us to conditions that came to the attention of a health care professional or the criminal justice system and likely represent more severe manifestations of these disorders. Some individuals with AUD will escape the notice of their health care providers; these individuals are false negatives in the registry data, and may contribute to higher risk estimates for suicide attempt than would be observed if a spectrum of AUD severity were well-represented among our identified cases. Similarly, suicide attempts that did not warrant medical attention or were not reported to a health care provider are also false-negatives in our data. Conversely, our inclusion of psychiatric conditions might result in over-correction of true AUD-based effects. Our findings should be considered alongside those from studies that involve self-reported alcohol misuse and suicide attempts, which may capture lower-severity manifestations of these outcomes. Second, we did not pursue all possible mechanistic models that might explain the association between AUD and suicide attempt. For example, future research might directly interrogate the role of mood disorders, which might increase risk for AUD and suicide attempts. Third, Sweden does not collect nationwide data on race/ ethnicity, so we are unable to address whether different patterns of risk exist across these groups. Fourth, although co-relative models account for confounders shared by family members—including both genetic and environmental factors—they do not account for environmental exposures that are not shared by family members (e.g. those experienced after one has left the family home, such as divorce). Therefore, the HRs estimated from these models are potentially inflated. Finally, our analyses do not account for the potential role of AUD treatment and potential remission on suicide attempt risk; this should be explored using datasets where such information is available, because it would further clarify the causal role of AUD.
In summary, we provide evidence from a well-powered, representative, national Swedish cohort that AUD is a prominent marker of risk for suicide attempts, even after accounting for psychiatric comorbidity. The observed association is likely the result of features that jointly impact risk of AUD and suicide attempts (e.g. genetic liability, psychiatric illness, and childhood stressors) and a potentially causal pathway, acting independently or in conjunction with one another. Health care providers should be aware that risk is dynamic across the life course, and that individuals with early onset AUD may be particularly vulnerable. Alongside our previous report on the association between AUD and suicide death [20], these findings underscore the impact of AUD on suicidal behavior above and beyond that of other psychiatric illness.
Supplementary Material
Figure S1 Hazard ratios (95% CI) from crude survival models estimating the association between first alcohol use disorder registration and first non-fatal suicide attempt, stratified by sex. Y-axis is on the log scale. Results from the fully adjusted model are presented in the main text (Fig. 1).
Table S1 Hazard ratios (HR) and 95% CI for crude and intermediate models of the association between first alcohol use disorder registration and first non-fatal suicide attempt. Results are stratified by sex. The intermediate model is adjusted for birth year and parental education.
Table S2 Hazard ratios (HR) and 95% CI for fully adjusted models of the association between first alcohol use disorder registration and first non-fatal suicide attempt. Results are stratified by sex.
Table S3 Hazard ratios (HR) and 95% CI from a sensitivity analysis in which individuals who died by suicide after a non-fatal suicide attempt were excluded.
Table S4 Hazard ratios (HR) (95% CI) from models estimating the association between AUD and risk of suicide attempt, grouped by AUD age of onset and observation period.
Table S5 Hazard ratios (HR) (95% CI) for unadjusted co-relative models in which estimates are extrapolated based on degree of relatedness, as described in the Supplemental Methods section. Because of limited sample size of informative sets, HRs are averaged across observation time.
Acknowledgements
The current study was supported by National Institutes of Health (AA027522, AA023534, and DA030005) and by Swedish Research Council and ALF funding from Region Skåne, Sweden.
Footnotes
Declaration of interests
None.
Supporting Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
References
- 1.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 2008; 192: 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geulayov G, Casey D, Bale L, Brand F, Clements C, Farooq B, et al. Suicide following presentation to hospital for nonfatal self-harm in the multicentre study of self-harm: a long-term follow-up study. Lancet Psychiatry 2019; 6: 1021–30. [DOI] [PubMed] [Google Scholar]
- 3.Foster T, Gillespie K, McClelland R Mental disorders and suicide in Northern Ireland. Br J Psychiatry 1997; 170: 447–52. [DOI] [PubMed] [Google Scholar]
- 4.Gairin I, House A, Owens D Attendance at the accident and emergency department in the year before suicide: retrospective study. Br J Psychiatry 2003; 183: 28–33. [DOI] [PubMed] [Google Scholar]
- 5.Runeson B, Haglund A, Lichtenstein P, Tidemalm D Suicide risk after nonfatal self-harm: a national cohort study, 2000–2008. J Clin Psychiatry 2016; 77: 240–6. [DOI] [PubMed] [Google Scholar]
- 6.Carroll R, Metcalfe C, Gunnell D Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS One 2014; 9: e89944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull 2017; 143: 187–232. [DOI] [PubMed] [Google Scholar]
- 8.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S Suicide and suicidal behavior. Epidemiol Rev 2008; 30: 133–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barak-Corren Y, Castro VM, Javitt S, Hoffnagle AG, Dai Y, Perlis RH, et al. Predicting suicidal behavior from longitudinal electronic health records. Am J Psychiatry 2017; 174: 154–62. [DOI] [PubMed] [Google Scholar]
- 10.Beautrais AL Suicides and serious suicide attempts: two populations or one? Psychol Med 2001; 31: 837–45. [DOI] [PubMed] [Google Scholar]
- 11.Simon GE, Hunkeler E, Fireman B, Lee JY, Savarino J Risk of suicide attempt and suicide death in patients treated for bipolar disorder. Bipolar Disord 2007; 9: 526–30. [DOI] [PubMed] [Google Scholar]
- 12.Conner KR, Beautrais AL, Conwell Y Risk factors for suicide and medically serious suicide attempts among alcoholics: analyses of Canterbury suicide project data. J Stud Alcohol 2003; 64: 551–4. [DOI] [PubMed] [Google Scholar]
- 13.Kendler KS, Ohlsson H, Sundquist J, Sundquist K, Edwards AC The sources of parent-child transmission of risk for suicide attempt and deaths by suicide in Swedish National Samples. Am J Psychiatry 2020; 177: 928–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Borges G, Walters EE Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry 1999; 56: 617–26. [DOI] [PubMed] [Google Scholar]
- 15.Lynch FL, Peterson EL, Lu CY, Hu Y, Rossom RC, Waitzfelder BE, et al. Substance use disorders and risk of suicide in a general US population: a case control study. Addict Sci Clin Pract 2020; 15: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agrawal A, Tillman R, Grucza RA, Nelson EC, McCutcheon VV, Few L, et al. Reciprocal relationships between substance use and disorders and suicidal ideation and suicide attempts in the collaborative study of the genetics of alcoholism. J Affect Disord 2017; 213: 96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J,et al. Association of Cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiat 2019; 76: 426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilcox HC, Conner KR, Caine ED Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend 2004; 76: S11–S19. [DOI] [PubMed] [Google Scholar]
- 19.Conner KR, Bridge JA, Davidson DJ, Pilcher C, Brent DA Metaanalysis of mood and substance use disorders in proximal risk for suicide deaths. Suicide Life Threat Behav 2019; 49: 278–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards AC, Ohlsson H,SundquistJ., SundquistK.,KendlerK. S. Alcohol use disorder and risk of suicide in a Swedish population-based cohort. Am J Psychiatry 2020; 177: 627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bachmann S Epidemiologyof suicide and the psychiatric perspective. Int J Env Res Public Health 2018; 15: 1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kinchin I, Doran CM The economic cost of suicide and non-fatal suicide behavior in the Australian workforce and the potential impact of a workplace suicide prevention strategy. Int J Env Res Public Health 2017; 14: 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shepard DS, Gurewich D, Lwin AK, Reed GA Jr., Silverman MM Suicide and suicidal attempts in the United States: costs and policy implications. Suicide Life Threat Behav 2016; 46: 352–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pien FC, Chang YC, Feng HP, Hung PW, Huang SY,Tzeng WC Changes in quality of life after a suicide attempt. West J Nurs Res 2016; 38: 721–37. [DOI] [PubMed] [Google Scholar]
- 25.Kendler KS, Ji J, Edwards AC, Ohlsson H, Sundquist J, Sundquist K An extended Swedish national adoption study of alcohol use disorder. JAMA Psychiat 2015; 72: 211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kendler KS, Ohlsson H, Sundquist J, Sundquist K Alcohol use disorder and mortality across the lifespan: a longitudinal cohort and co-relative analysis. JAMA Psychiat 2016; 73: 575–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez de la Cruz L, Rydell M, Runeson B, D’Onofrio BM, Brander G, Ruck C, et al. Suicide in obsessive-compulsive disorder: a population-based study of 36 788 Swedish patients. Mol Psychiatry 2017; 22: 1626–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kendler KS, Ohlsson H, Edwards AC, Karriker-Jaffe KJ,Sundquist J, Sundquist K Clinical features of registryascertainedalcoholusedisordersthatreflectfamilialrisk.Drug Alcohol Depend 2016; 164: 135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kendler KS, Lonn SL, Sundquist J, Sundquist K Smoking and schizophrenia in population cohorts of Swedish women and men: a prospective co-relative control study. Am J Psychiatry 2015; 172: 1092–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hawton K, Casanas ICC, Haw C, Saunders K Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord 2013; 147: 17–28. [DOI] [PubMed] [Google Scholar]
- 31.Simon GE, Johnson E, Lawrence JM, Rossom RC, Ahmedani B, Lynch FL, et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic healthrecords. AmJPsychiatry2018appiajp201817101167; 175: 951–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on alcohol and related conditions III. JAMA Psychiat 2015; 72: 757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson PR, Banu S, Ashok MV Severity of alcoholism in Indian males: correlation with age of onset and family history of alcoholism. Indian J Psychiatry 2010; 52: 243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Connor JP, Weier M, Hall WD The Age of Onset of Alcohol Use Disorders. In: Girolamo G, McGorry PD, Sartorius N, editors. Age of Onset of Mental Disorders: Etiopathogenetic and Treatment Implications. Cham: Springer International Publishing; 2019, pp. 169–82. [Google Scholar]
- 35.Hingson RW, Heeren T, Winter MR Age of alcohol-dependence onset: associations with severity of dependence and seeking treatment. Pediatrics 2006; 118: e755–e763. [DOI] [PubMed] [Google Scholar]
- 36.Babor TF., Hofmann M., DelBoca FK., Hesselbrock V., Meyer RE., Dolinsky ZS., et al. Types of alcoholics, I. evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry 1992; 49: 599–608. [DOI] [PubMed] [Google Scholar]
- 37.Del Boca FK, Hesselbrock MN Gender and alcoholic subtypes. Alcohol Health Res World 1996; 20: 56–62. [PMC free article] [PubMed] [Google Scholar]
- 38.Sartor CE, Jackson KM, McCutcheon VV, Duncan AE, Grant JD, Werner KB, et al. Progression from first drink, first intoxication, and regular drinking to alcohol use disorder: a comparison of African American and European American youth. Alcohol Clin Exp Res 2016; 40: 1515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bossarte RM, Swahn MH The associations between early alcohol use and suicide attempts among adolescents with a history of major depression. Addict Behav 2011; 36: 532–5. [DOI] [PubMed] [Google Scholar]
- 40.Cho H, Hallfors DD, Iritani BJ Early initiation of substance use and subsequent risk factors related to suicide among urban high school students. Addict Behav 2007; 32: 1628–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Borges G, Benjet C, Orozco R, Medina-MoraM. E, Menendez D Alcohol, cannabis and other drugs and subsequent suicide ideation and attempt among young Mexicans. J Psychiatr Res 2017; 91: 74–82. [DOI] [PubMed] [Google Scholar]
- 42.Spoth RL, Guyll M, Day SX Universal family-focused interventions in alcohol-use disorder prevention: cost-effectiveness and cost-benefit analyses of two interventions. J Stud Alcohol 2002; 63: 219–28. [DOI] [PubMed] [Google Scholar]
- 43.Dishion TJ, Nelson SE, Kavanagh K The family check-up with high-risk young adolescents: preventing early-onset substance use by parent monitoring. Behav Ther 2003; 34: 553–71. [Google Scholar]
- 44.Perry CL, Williams CL, Veblen-Mortenson S, Toomey TL, Komro KA, Anstine PS, et al. Project northland: outcomes of a communitywide alcohol use prevention program during early adolescence. Am J Public Health 1996; 86: 956–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van der Vorst H, Engels RC, Meeus W, Dekovic M The impact of alcohol-specific rules, parental norms about early drinking and parental alcohol use on adolescents’ drinking behavior. J Child Psychol Psychiatry 2006; 47: 1299–306. [DOI] [PubMed] [Google Scholar]
- 46.Docherty AR, Shabalin AA, DiBlasi E, Monson E, Mullins N, Adkins DE, et al. Genome-wide association study of suicide death and polygenic prediction of clinical antecedents. Am J Psychiatry 2020; 177: 917–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thompson RG, Alonzo D, Hasin DS Parental divorce, maternal-paternal alcohol problems, and adult offspring lifetime alcohol dependence. J Soc Work Pract Addict 2013; 13: 295–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jr Thompson R. G.., Alonzo D, Hu MC, Hasin DS The influences of parental divorce and maternal-versus-paternal alcohol abuse on offspring lifetime suicide attempt. Drug Alcohol Rev 2017; 36: 408–14. [DOI] [PubMed] [Google Scholar]
- 49.Garcia OF, Serra E., Zacares JJ, Calafat A, Garcia F Alcohol use and abuse and motivations for drinking and non-drinking among Spanish adolescents: do we know enough when we know parenting style? Psychol Health 2020; 35: 645–64. [DOI] [PubMed] [Google Scholar]
- 50.Kingsbury M, Sucha E, Manion I, Gilman SE, Colman I Pathways from parenting practices to adolescent suicidality: evidence on the role of emotional and behavioral symptoms from a prospective cohort of Canadian children. Suicide Life Threat Behav 2020; 50: 1149–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Norstrom T, Rossow I Alcohol consumption as a risk factor for suicidal behavior: a systematic review of associations at the individual and at the population level. Arch Suicide Res 2016; 20: 489–506. [DOI] [PubMed] [Google Scholar]
- 52.Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med 2017; 47: 949–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Conner KR, Bagge CL Suicidal behavior: links between alcohol use disorder and acute use of alcohol. Alcohol Research 2019; 40(1): e1–e4. 10.35946/arcr.v40.1.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carballo JJ, Oquendo MA, Giner L, Zalsman G, Roche AM, Sher L Impulsive-aggressive traits and suicidal adolescents and young adults with alcoholism. Int J Adolesc Med Health 2006; 18: 15–9. [DOI] [PubMed] [Google Scholar]
- 55.Pompili M, Serafini G, Innamorati M, Dominici G, Ferracuti S, Kotzalidis GD, et al. Suicidal behavior and alcohol abuse. Int J Env Res Public Health 2010; 7: 1392–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Conner KR, Duberstein PR Predisposing and precipitating factors for suicide among alcoholics: empirical review and conceptual integration. Alcohol Clin Exp Res 2004; 28: 6S–17S. [DOI] [PubMed] [Google Scholar]
- 57.Conner KR, Gamble SA, Bagge CL, He H, Swogger MT, Watts A, et al. Substance-induced depression and independent depression in proximal risk for suicidal behavior. J Stud Alcohol Drugs 2014; 75: 567–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Conner KR, Houston RJ, Swogger MT, Conwell Y,You S, He H, et al. Stressful life events and suicidal behavior in adults with alcohol use disorders: role of event severity, timing, and type. Drug Alcohol Depend 2012; 120: 155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Duberstein PR, Conwell Y, Caine ED Interpersonal stressors, substance abuse, and suicide. J Nerv Ment Dis 1993; 181: 80–5. [DOI] [PubMed] [Google Scholar]
- 60.Darvishi N, Farhadi M, Haghtalab T, Poorolajal J Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS One 2015; 10: e0126870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rossow I, Romelsjo A, Leifman H Alcohol abuse and suicidal behaviour in young and middle aged men: differentiating between attempted and completed suicide. Addiction 1999; 94: 1199–207. [DOI] [PubMed] [Google Scholar]
- 62.Women Tuchman E. and addiction: the importance of gender issues in substance abuse research. J Addict Dis 2010; 29: 127–38. [DOI] [PubMed] [Google Scholar]
- 63.Hecksher D., Hesse M. Women and substance use disorders. Mens Sana Monographs 2009; 7: 50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Hazard ratios (95% CI) from crude survival models estimating the association between first alcohol use disorder registration and first non-fatal suicide attempt, stratified by sex. Y-axis is on the log scale. Results from the fully adjusted model are presented in the main text (Fig. 1).
Table S1 Hazard ratios (HR) and 95% CI for crude and intermediate models of the association between first alcohol use disorder registration and first non-fatal suicide attempt. Results are stratified by sex. The intermediate model is adjusted for birth year and parental education.
Table S2 Hazard ratios (HR) and 95% CI for fully adjusted models of the association between first alcohol use disorder registration and first non-fatal suicide attempt. Results are stratified by sex.
Table S3 Hazard ratios (HR) and 95% CI from a sensitivity analysis in which individuals who died by suicide after a non-fatal suicide attempt were excluded.
Table S4 Hazard ratios (HR) (95% CI) from models estimating the association between AUD and risk of suicide attempt, grouped by AUD age of onset and observation period.
Table S5 Hazard ratios (HR) (95% CI) for unadjusted co-relative models in which estimates are extrapolated based on degree of relatedness, as described in the Supplemental Methods section. Because of limited sample size of informative sets, HRs are averaged across observation time.