Abstract
Aims:
The harms arising from psychoactive drug use are complex, and harm reduction strategies should be informed by a detailed understanding of the extent and nature of that harm. Drug harm is also context specific, and so any comprehensive assessment of drug harm should be relevant to the characteristics of the population in question. This study aimed to evaluate and rank drug harms within Aotearoa New Zealand using a multi-criteria decision analysis (MCDA) framework, and to separately consider harm within the total population, and among youth.
Methods:
Two facilitated workshops involved the separate ranking of harm for the total population, and then for youth aged 12–17, by two expert panels. In the total population workshop, 23 drugs were scored against 17 harm criteria, and those criteria were then evaluated using a swing weighting process. Scoring and weighting were subsequently updated during the youth-specific workshop. All results were recorded and analysed using specialised MCDA software.
Results:
When considering overall harm, the MCDA modelling results indicated that alcohol, methamphetamine and synthetic cannabinoids were the most harmful to both the overall population and the youth, followed by tobacco in the total population. Alcohol remained the most harmful drug for the total population when separately considering harm to those who use it, and harm to others.
Conclusions:
The results provide detailed and context-specific insight into the harm associated with psychoactive drugs use within Aotearoa New Zealand. The findings also demonstrate the value of separately considering harm for different countries, and for different population subgroups.
Keywords: Aotearoa, drug harm, drug policy, psychoactive drugs, youth
The harms arising from the use of psychoactive drugs, including legal drugs such as alcohol and tobacco, are complex and significant. International drug markets are evolving rapidly, and the emergence of new methods of distribution, in addition to the introduction of novel psychoactive substances, has contributed to the highest global drug supply on record (Bonomo et al., 2019; United Nations Office on Drugs and Crime, 2022). In addition, global alcohol use continues to be a significant source of harm and is estimated to contribute to nearly 3 million deaths globally every year (Griswold et al., 2018). Considering limitations in the ability of supply-side interventions to curb these trends (Cunningham et al., 2018; United Nations Office on Drugs and Crime, 2019), there is a need to consider policy reform approaches that collectively prioritise harm minimisation, and provide a balance of supply, demand and harm reduction interventions. For policies that effectively reduce drug harm, however, it is crucial to first understand the relative harm attributable to different drugs, and the profile and distribution of those harms (Bonomo et al., 2019).
The overall harm arising from use of a drug depends upon intrinsic factors such as its pharmacological and pharmacodynamic properties (MacCoun and Reuter, 2001; Nutt et al., 2007) and extrinsic factors including individual, social, cultural, political and legal factors (Rhodes, 2009). Harms can be categorised as those that impact on individuals who use a drug, and those which impact upon others, such as families, communities or broader society. There is a complex interrelationship between harms; for example, drug-related convictions and other related harms tend to further disadvantage vulnerable individuals and communities, and the illegality of some drugs can add to any harms accruing from merely using the drug (Fergusson et al., 2003; Katikireddi et al., 2017). The relative impact of these harms is likely to vary from one location to another due to variables such as use patterns, legal frameworks and cultural values. Additionally, systematic data on particular drugs or forms of harm are scarce, making it difficult to consistently measure markers of harm (Crossin et al., 2022).
One way to manage this complexity is through the use of a multi-criteria decision analysis (MCDA) approach (Phillips, 2017) applied in a Decision Conferencing setting (Phillips and Bana e Costa, 2007). This group decision-making technique, when applied to drug harm, utilises diverse panels of experts, who collaborate to scale and weight predetermined harm criteria. This method has also been used to assess drug policy options (Wilkins et al., 2022). A previously developed MCDA drug harm framework provides a robust method of comparing harms from different drugs (Nutt et al., 2007) and considers harms to both individuals and others. To date, MCDA has been used to rank drug harms within the United Kingdom (Nutt et al., 2010), Australia (Bonomo et al., 2019) and Europe (van Amsterdam et al., 2015b). All these studies consistently ranked alcohol as the most harmful drug, although also yielded somewhat different results for other drugs, highlighting the importance of country- and region-specific drug harm evaluations. These differing results are influenced by a wide range of contextual factors, including drug availability, drug prices, drug purity, use levels, differences in legal status and the composition of the expert panels.
In Aotearoa New Zealand, legislation has been implemented to control the availability and use of drugs, including by the Misuse of Drugs Act 1975, and to regulate access to alcohol by the Sale and Supply of Alcohol Act 2012. Despite these measures, drugs continue to cause significant harm across Aotearoa New Zealand (McFadden Consultancy, 2016; McFadden et al., 2022). This harm is not evenly distributed across the population and affects particular groups more than others. Māori are the indigenous population of Aotearoa New Zealand, making up approximately 17% of the overall population, and have a notably younger age demographic than the overall population (Statistics New Zealand, 2021). Māori tend to be overrepresented in drug harm incidents, including adverse events associated with synthetic cannabinoids (Robson et al., 2021), higher rates of cannabis and methamphetamine use (Marie et al., 2008), an elevated likelihood of arrest and conviction for cannabis-related offences (Fergusson et al., 2003) and disproportionate alcohol-related harm (Alcohol Healthwatch, 2023; Winter et al., 2019). These outcomes reflect cumulative disadvantage for this group, arising as a result of colonisation, and relating to inequities within the health and mental health systems, discrimination, and poorer socio-economic outcomes (New Zealand Ministry of Health, 2020; New Zealand Ministry of Justice, 2021). The profile of drug harm is also likely to differ for adolescents due to factors such as potential interference with education and employment, social norms relating to drug use, and typical traits such as curiosity and sensation seeking (Ball et al., 2022a; Brumback et al., 2021; Gubbels et al., 2019; Nodora et al., 2014; Stautz and Cooper, 2013). In Aotearoa New Zealand, adolescent use of alcohol, tobacco and cannabis appears to have stabilised following a long period of decline; however, binge drinking in adolescents remains high by international standards and this is associated with increased self-reported harm (Ball et al., 2022a; Ball et al., 2022b). The lack of accounting for these differences across population subgroups is a limitation of previous MCDA drug harms ranking studies. Taking a whole population approach averages harms across key subgroups, which, in turn, prevents a more nuanced understanding of harms in a given population, hindering the development of tailored and effective harm-minimisation policies. Finally, while drug harm MCDA studies have previously employed the same criteria, it is important to consider whether it is appropriate to use the same criteria cross-nationally.
This study used an MCDA method to consider drug harm in the Aotearoa New Zealand context, with a modified set of criteria. The study included two new harm criteria, and slightly revised some of the existing criteria to better incorporate worldviews and values that are relevant to Māori, and to the Aotearoa New Zealand sociocultural context as a whole. In addition to a whole-population ranking, a separate ranking process was used to specifically evaluate harm arising from drug use by adolescents in Aotearoa New Zealand. This study aimed to quantify the relative harms of drugs that are commonly used in Aotearoa New Zealand, identify the profile of harms for these drugs, for both the whole population and for adolescents, and identify areas where intervention or policy change should be focused.
Methods
Ethics
This study was approved by the University of Otago human ethics committee (D20/425).
Study design
The study involved a MCDA method with a swing weighting approach (Supplemental Material 1) used in a Decision Conferencing setting (Phillips and Bana e Costa, 2007). This involved a panel of experts from across Aotearoa New Zealand collaborating to rank and weight the relative harms of different drugs. The rankings were completed using a specific set of harm criteria, which were based on the original 16 criteria developed and used by Nutt and colleagues in their ranking of drug harms in the United Kingdom (UK) (Nutt et al., 2010), with these criteria either relating to harm experienced by individuals who use a given drug, or by others. A scale extending from 0 to 100 points of ‘relative harm’ was created for each criterion, enabling each of the drug categories to be scored against each criterion relative to one another. The drug category expected to provide the largest value (most harm) on a given criteria is assigned the highest preference score (usually 100) while the one providing the smallest value is assigned the lowest preference score (for this study, a ‘no drugs’ baseline was assigned the lowest score of 0 for each of the criteria). A weighting process was also used to produce a relative scale for each criterion and meant that the value difference between 0 and 100 could differ for each scale, in a similar way that a Celsius unit differs from a Fahrenheit unit. The ranking process is described in the Workshops section, while a detailed explanation of MCDA is provided in Supplement Material 1.
Expert panel
A panel of experts was selected to reflect a broad and diverse range of knowledge and experience. To build this panel, a core advisory group (RC, JB, LC, TP, SA, CW and MR) prepared an initial list of possible panel members. Prospective panel members were approached and invited to participate, and those who agreed were sent an information sheet and consent form to sign. In some cases, snowball recruitment was used to fill remaining expertise gaps. A total of 23 panel members attended the workshops. The expertise of this panel included emergency medicine, law enforcement, addiction research, addiction treatment, pharmacology, toxicology, Māori health and advocacy, Pacific health, youth justice, harm reduction, clinical psychology, peer support, criminology, drug markets and drug policy. A number of panel members have lived experience of drug harm and use, and all decisions about disclosure of this were left to the individual panel members. From within this panel, a youth-specific panel was also established and comprised eight individuals with specific knowledge pertaining to drug harm among adolescents, encompassing areas such as youth health and development, research, juvenile justice, drug policy and youth mental health. The full panel and their expertise are detailed in Table 1.
Table 1.
Expert panel members and areas of expertise.
| Name | Sector/speciality | Youth panel |
|---|---|---|
| Adam Pomerleau | Emergency medicine, toxicology | |
| Amanda Jones | Research, public health | |
| Blair MacDonald | Law enforcement, police | |
| Chris Wilkins | Research | |
| Dwaine Faletanoai | Pacific, youth health | Yes |
| Fiona Hutton | Criminology | |
| Geoffrey Noller | Harm reduction | |
| Ian Lambie | Clinical psychology, youth justice | Yes |
| Jane Sheridan | Research | Yes |
| Jason George | Harm reduction | |
| Joseph Boden | Research | Yes |
| Jude Ball | Youth substance use | Yes |
| Kali Mercier | Policy, harm reduction, advocacy | |
| Lana Cleland | Research, youth support | Yes |
| Marta Rychert | Research | Yes |
| Nicki Jackson | Policy, advocacy | |
| Patricia Walsh | Social work, drug harm to Māori | |
| Rhys Ponton | Pharmacy, harm reduction research | |
| Rose Crossin | Policy, research | |
| Simon Adamson | Clinical psychology, addiction | |
| Susan Bagshaw | Medicine, youth mental health | Yes |
| Suresh Muthukumaraswamy | Psychopharmacology | |
| Tracey McIntosh | Criminology, drug harm to Māori |
Additional criteria development
A key alteration for the Aotearoa New Zealand workshops included the addition of two new harm criteria to the existing criteria used by previous drug harm MCDA studies (Bonomo et al., 2019; Nutt et al., 2010), which were developed to incorporate a Māori worldview. The development of these new criteria began with an online survey promoted during an online conference for Māori working in the drug sector. The opportunity to complete the survey was offered to volunteers who attended the conference, and to a targeted group of Māori experts. The survey asked respondents to evaluate each of the existing criteria (Nutt et al., 2010) and their relevance to Māori, in addition to any changes that should be made to the criteria, and gaps in terms of drug harm from a Māori worldview perspective. The responses from this survey were then collated and anonymised (RC and LC) before being assessed by a Māori consultant (K Maynard) who used the feedback to review the criteria and develop two new criteria: intergenerational harm and non-physical/spiritual harm. These criteria (detailed in Table 2) were further assessed and agreed upon by Māori expert panel members, and the wording was then checked by a facilitator (PS) to ensure that they fit within the MCDA model. Although it is acknowledged that the drug harms criteria initially developed in the UK are based on a Western worldview, it was a priority to include criteria that were broadly relevant to Māori while still enabling comparisons with drug harm MCDA work done in other countries.
Table 2.
Harm criteria against which the drugs were ranked, separated by harm to those who use the drug, and harm to others.
| Drug harm criteria | Definition |
|---|---|
| Harms to person who uses the drug | |
| Drug-specific mortality | Intrinsic lethality of the drug expressed as ratio of lethal dose and standard dose (for adults). Does not include consideration of how difficult it might be to measure the dose. |
| Drug-related mortality | The extent to which life is shortened by the use of the drug (excludes drug-specific mortality) – for example, road traffic accidents, lung cancers, HIV, suicide. |
| Drug-specific damage | Drug-specific damage to physical health – for example, cirrhosis, seizures, strokes, cardiomyopathy, stomach ulcers (taking into account differences in help-seeking behaviour and existing health inequalities). Includes the impacts from withdrawal. |
| Drug-related damage | Drug-related damage to physical health, including consequences of, for example, unwanted sexual activities and self-harm/self-injury, blood-borne viruses, and emphysema. |
| Dependence | The extent to which a drug creates a propensity to continue to use despite adverse consequences (ICD 10 or DSM 5). Includes consideration of how quick it is to become dependent compared to how difficult it is to stop once dependent. |
| Drug-specific and drug-related impairment of mental functioning | Drug-specific and drug-related impairment of mental functioning, for example, amphetamine-induced psychosis, ketamine intoxication. Including mood disorders, depression, anxiety. Not including the intended intoxicating effect of the drug. |
| Loss of tangibles | Extent of loss of tangible things (e.g. income, housing, job or employment position, educational achievements or training opportunities, criminal record, imprisonment). |
| Loss of relationships | Extent of loss of relationship or connections with family/whānau, friends, social or community groups. |
| Non-physical/spiritual damage | Extent to which the use of a drug negatively impacts on mana, 1 wehi, 1 tapu, 1 ihi, 1 mauri, 1 wairua, 1 ahua/aura; lowers ihi rangaranga (energetic vibration) and increases vulnerability to wairua poke (negative entities/demons). Also includes impacts on reputation, identity, potential (e.g. through imprisonment or criminal conviction, reduced ability to fulfil cultural obligations). |
| Harms to others (harms arising per person using the drug) | |
| Injury | Extent to which the use of a drug increases the chance of injuries to others both directly and indirectly–for examp violence (including family violence), traffic accident, foetal harm, drug waste, secondary transmission of blood-borne viruses, injury associated with criminal activity related to supply. The ‘proximal’ harm. |
| Crime | Extent to which the use of a drug involves or leads to an increase in volume of crime (beyond the use-of-drug act) or organised criminal activity directly or indirectly (at the population level, not the individual level). This excludes violence in general (covered under ‘Injury’) but does include sexual violence and exploitation. |
| Family adversities | Extent to which the use of a drug negatively impacts on family/whānau well-being – for example, family/whānau 2 breakdown, economic well-being, emotional or spiritual wellbeing, future prospects of children, child neglect or maltreatment. |
| Intergenerational | Extent to which the use of a drug directly or indirectly impacts on future generations (e.g. mana of the family/whānau, transmission of addictive behaviours, loss of knowledge and connection to whakapapa (genealogy), tikanga (customs/way of doing things) and culture. |
| (Total harms to Aotearoa New Zealand and from drug use within Aotearoa New Zealand) | |
| Community | Extent to which the use of a drug creates decline in social cohesion, decline in the productiveness and well-being of the community, and decline in the reputation of the community, increases associated stigma and whakamā (state of shame or embarrassment), or distorts the tikanga (customs/way of doing things) and/or narratives of hapū (kinship group/subtribe)/iwi (large social units/tribe) or marae. 3 |
| Environmental damage | Extent to which the use and production of a drug causes environmental damage locally and disregard for kaitiakitanga (guardianship of the environment)–for example, toxic waste from amphetamine factories, discarded needles. |
| International damage | Extent to which the use of a drug in Aotearoa New Zealand contributes to damage internationally, for example, deforestation, destabilisation of countries, international crime, new markets. |
| Economic cost | Extent to which the use of a drug causes direct costs to Aotearoa New Zealand (e.g. health care, police, prisons, social services, customs, insurance, crime) and indirect costs (e.g. loss of productivity, absenteeism). |
These Māori concepts are aspects of the non-physical/spiritual dimension of a human being. A further explanation of these concepts can be found in the online Māori dictionary (Moorfield, 2023b).
Whanau (loosely translated as family) refers to immediate, extended and/or even distant kin relationships and is also used, sometimes, to capture close non-kin relationships (Moorfield, 2023a).
’The marae is a symbol of tribal identity and solidarity’ (Barlow, 1991: p. 73) and a significant ‘focal point of any Māori community’ (Pohatu, 2007: p. 6).
Workshops
The workshops took place in Wellington, Aotearoa New Zealand in April 2022, with all experts meeting over two consecutive days to rank overall drug harms in Aotearoa New Zealand. The youth-specific panel, which involved eight experts from the overall panel, then met for a third day to rank harms arising from drug use by youth in Aotearoa New Zealand. The workshops were facilitated by two decision conferencing specialists (PG and EP) with extensive knowledge and expertise in facilitating MCDA workshops, including those examining drug harms.
The group engaged in open and collaborative discussions to reach a consensus on each of the ranking decisions. All drugs (Table 3) were ranked against a given criterion before moving on to the next. The process for ranking each of the criteria replicates steps taken within the previous drug harm MCDA studies (Bonomo et al., 2019; Nutt et al., 2010) – the group first discussed and agreed a rank order against the criterion, then agreed on a ‘score’ between 0 (‘no harm’) and 100 points (the highest ranked/most harmful drug). Scores and weights were captured live using an MCDA software tool which then displayed the results. Full details of this ranking process are provided in Supplemental Material 2.
Table 3.
Drugs evaluated by the expert panel, adjusted from previous MCDA studies for relevance to the Aotearoa New Zealand context.
| Drug name | Definition and other names |
|---|---|
| Alcohol | All ethanol for drinking including commercially prepared and ‘homebrew’ products. |
| ENDs/vapes | Electronic Nicotine Delivery Systems (e-cigarettes containing nicotine). |
| Kava | Preparation of sedative Piper methysticum. |
| Tobacco products | Includes cigarettes and other products containing tobacco. |
| Amphetamine-type substances | Amphetamine (excluding crystalline methamphetamine, including tablets, powder, base/paste, liquid and amphetamine sulphate). |
| Benzodiazepines | Use of prescription benzodiazepines (positive allosteric modulators – GABA-A receptor, benzodiazepine site), including diazepam or lorazepam, without a prescription or outside of prescribed use. |
| Cannabis | Limited to psychoactive forms (i.e. not purified CBD products). Includes illegal cannabis consumed for medicinal reasons, but excludes prescribed medicinal cannabis. |
| Cocaine | Cocaine hydrochloride used by insufflation or injection. Excludes crack cocaine (use of this is very limited in Aotearoa New Zealand). |
| GHB and GBL | Gamma hydroxybutyrate and gamma butyrolactone (in New Zealand, GHB and related substances may also be known as ‘Fantasy’). |
| Hallucinogens | Lysergic acid diethylamide (LSD) and natural psychedelic products (including salvia, mushrooms, cactus, etc.). |
| Illegal fentanyls (high potency opioids) | Fentanyl-based and fentanyl analogue opioids including fentanyl, carfentanil, acetyl fentanyl, furanyl fentanyl (that are obtained illegally i.e. not by prescription). |
| Ketamine | Ketamine used without a prescription or outside of prescribed use. |
| MDMA (Ecstasy) | Methylenedioxymethamphetamine. |
| Methamphetamine | Crystalline methamphetamine. |
| Nitrite-based inhalants | Inhaled nitrite-based drugs including amyl nitrite, isobutyl nitrite, isopentyl nitrite. |
| Nitrous oxide | Inhaled nitrous oxide. |
| Non-prescription opioids | Opioids that are not obtained by prescription including heroin, morphine, ‘homebake’ morphine (Bedford et al., 1987). |
| Opioid substitution products | Opioids used in opioid substitution therapies (including methadone or buprenorphine) without a prescription or outside of prescribed use. |
| PIEDs | Performance and Image Enhancing Drugs (including anabolic steroids and growth hormones). |
| Prescription opioids | Prescription opioids including morphine, oxycodone and codeine without a prescription or outside of prescribed use. |
| Solvents and fuels | Fuel and solvent inhalation. |
| Synthetic cannabinoids | Synthetic cannabinoid receptor agonists e.g. spice, AMB-FUBINACA. |
| Synthetic cathinones | Including mephedrone. |
| No drugs | Baseline measure. |
The process was also informed by several assumptions, which were outlined and discussed by the full panel beforehand. These assumptions are listed below:
a) Harm to those who use the drug: refers to the effect of use of a single person who typically uses that drug, and in what was considered to be a typical way, and did not take prevalence of use into account (this is in contrast to the Australian drug harms ranking study, which subsequently adjusted results by prevalence of use) (Bonomo et al., 2019).
b) Harm to others: refers to the effect of use of that drug on people other than an individual who uses the drug, focusing on groups such as families and wider communities. Half of these criteria (injury, crime, family adversities and intergenerational harm) considered only the harm from a single, average person who uses the drug. The other half (community, environmental damage, international damage and economic cost) considered the total harm to others from the use of the drug in Aotearoa New Zealand.
c) Use of any drug has the potential to cause harm, but not all drug use results in harm.
d) Harm may be acute or chronic and may affect the individual or others.
-
e) The panel considered a ‘realistic middle ground’ with harms that were most relevant for the majority of those using a drug in Aotearoa New Zealand. This meant considering a scenario that was:
1. Not the worst case – every unfavourable context
2. Not the best case – no harm despite unfavourable context
-
f) Harms were considered specifically for the drug under consideration, that is,
1. Irrespective of any cutting agents, that is assuming that many drugs will be ‘cut’ or diluted with different substances, as these could not be systematically accounted for in any reasonable manner.
2. Assuming the drug was actually the specified drug, as opposed to another substance sold as a particular drug despite being something different in reality.
g) Harm was considered within the context of the most common method/route of administration within Aotearoa New Zealand.
h) Harms associated with drug use were assessed without balancing that harm against perceived benefits or motivation for use.
i) Harms were assessed at the time of the workshops, and in the policy context that was current at the time.
After the ranking and weighting process was complete for all the drugs against the harm criteria, preliminary results were shown to the panel. This step served to ensure that the final rankings demonstrated face validity based on the discussions that took place during the workshops, and to encourage discussions surrounding whether any sensitivity analyses were required. If consensus could not be reached on a final score or rank, multiple results were recorded, and sensitivity testing was undertaken to determine the impacts of the difference.
On day 3, the youth expert panel met for the youth-specific workshop. The results for the total population were used as the starting point, with all scores and weightings reviewed and discussed. Scores and weights were changed ‘by exception’ to account for a youth-specific context. ‘Youth’ was defined as 12–17 years of age, to reflect a higher-risk neurodevelopmental and behavioural period, and an age where an individual cannot legally purchase any of the listed (legal) drugs. It was assumed that progressive harms from drug use that continued into adulthood, such as drug-related damage to physical health experienced from continued use after the age of 17, would be excluded from consideration as those would have already been captured in the general/overall population MCDA results. All other assumptions were the same as for the total population, including that scoring and weighting was based on what would be realistic or expected for the majority of youth using that drug.
Results
Overall population rankings
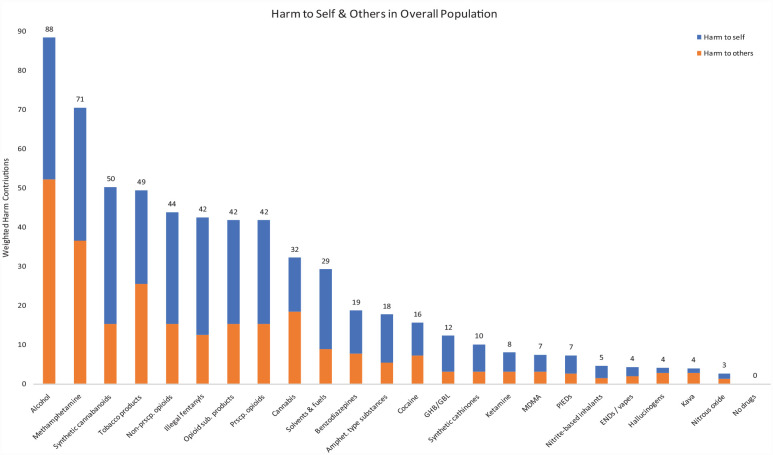
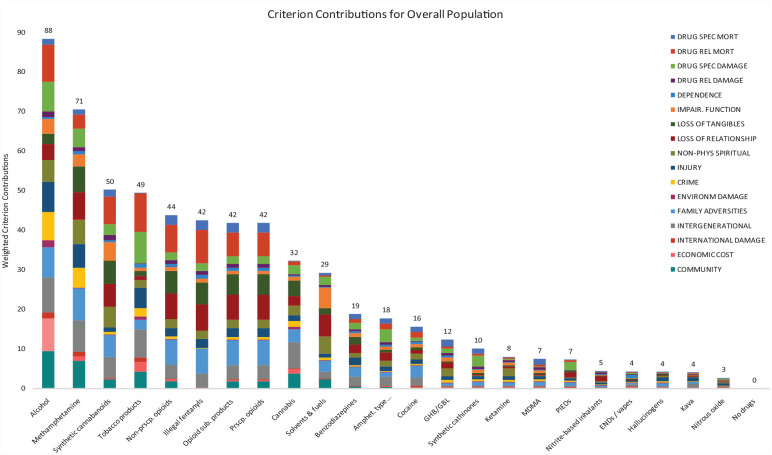
Results from the total population drug harm MCDA are shown in Figure 1. The contributions of individual criteria after weighting are shown in Figure 2. Alcohol was ranked as the most harmful drug overall (weighted preference value of 88 points) and remained the most harmful when separately considering harm to those who use it, and to others. High scores on many different criteria were observed for alcohol, with high rankings across half of the harm criteria (the two highest contributing criteria were drug-related mortality and community damage). Methamphetamine was ranked as the second most harmful drug overall (71 points), ranking third most harmful when only considering harm to those who use it, and second most harmful when considering only harms to others. Some of the highest contributions to this score were from ratings for family adversities, in addition to community damage. Synthetic cannabinoids were ranked as third most harmful overall (50 points); however, when considering only harm to those who use synthetic cannabinoids, drugs in this category were ranked much higher (second most harmful) than they were for harm to others (fifth most harmful). Tobacco was ranked as fourth most harmful overall (49 points) and featured high ratings in both harm to self and harm to others categories. In particular, drug-related mortality was the highest-ranked criterion in the harm to self category for tobacco, while intergenerational harm was the highest-ranked criterion in the harm to others- category. All of the opioid categories were clustered together in the overall rankings, and this remained consistent when separately considering each of the two broad harm categories (i.e. harm to self and harm to others). Overall weighted preference value numbers also indicated no difference, or minimal differences, between the opioid groups in terms of overall harm and harm within the two broad harm categories (harm to self and harm to others). Opioids were followed by cannabis which was ranked ninth and evaluated as causing more harm to others than to oneself, with intergenerational harm and community harm being the two highest ranked criteria for this drug. Nitrous oxide was consistently ranked as the least harmful overall and within the two broad harm categories. Additionally, kava, ENDs/vapes, hallucinogens and nitrite inhalants tended to cluster at the lower end of overall rankings.
Figure 1.
Drugs in order of their overall harm scores for the Aotearoa New Zealand population, showing contributions from harms experienced by those who use the drug and harm experienced by others. The cumulative weighted preference values (sum of all weighted scores for all the criteria of harm to those who use the drugs, and all the criteria of harm to others) for each drug are shown above each bar. Previous drug harm MCDA studies did not present drugs in order of decreasing overall harm.
MCDA: multi-criteria decision analysis.
Figure 2.
Drugs in order of their overall harm scores for the Aotearoa New Zealand population, showing individual criterion contributions after weighting. The cumulative preference values (sum of weighted contribution for each criterion) for each drug are shown above each bar. Previous drug harm MCDA studies did not present drugs in order of decreasing overall harm.
MCDA: multi-criteria decision analysis.
During the scoring process for the drug-related damage criterion, the panel discussed whether the initial decision to score cocaine at 15 was too low. It was agreed that a higher score of 45 would be tested; however, this ultimately made no discernible difference to the overall ranking. This also indicated that the scoring results were robust to such changes. Following the weighting process for all drugs, some members of the panel reflected that the assessment of tobacco for drug-related mortality was too low at 100, comparative to other drugs, and suggested an alternative score of 140. It was agreed to sensitivity test this result as consensus could not be reached at the time. This change moved tobacco from fourth to third in the ranking. The impact of this sensitivity analysis upon the overall results is depicted in Supplemental Material 3.
Youth-specific rankings
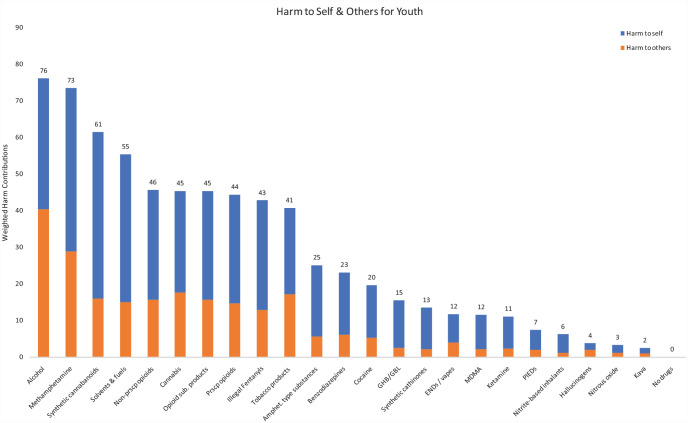
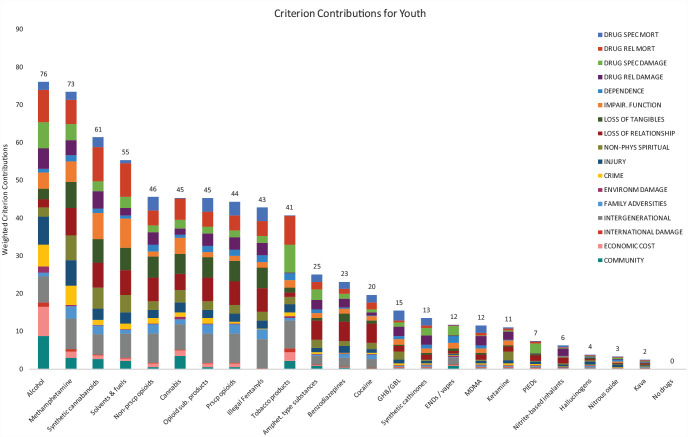
The results from the youth-specific rankings are included in Figure 3, broken down by harm to youth who use the drugs, and to others. Figure 4 also shows the full, weighted breakdown of the youth harm scores across each of the harm categories. As with rankings for the overall population, alcohol was again ranked highest for overall harm in the youth category (76 points), with more of the attributable harm being experienced by others. In contrast, alcohol was ranked fourth most harmful when considering only harm to youth who used it (harm to self). For overall harm in this group, alcohol was followed by methamphetamine (73 points), which also ranked second when considering each of the broad harm categories. Synthetic cannabinoids were rated third most harmful to youth overall (61 points) and as more harmful to oneself than to others; when considering only harms to youth who use these drugs, synthetic cannabinoids were evaluated as most harmful. Solvents and fuels were ranked as fourth most harmful overall for youth (55 points) and also ranked as more harmful to those that used them, compared with harm to others. Cannabis was rated as sixth most harmful overall for youth and was evaluated as more harmful to oneself than to others, which is in contrast to the total population ratings. Within the broader harm to self-criterion for cannabis, drug-related mortality (e.g. cannabis-related road deaths) was rated as most harmful. Nitrous oxide, hallucinogens and kava were ranked as the three least harmful drugs overall, and this was consistent when considering harm to youth who used these drugs, and to others.
Figure 3.
Drugs in order of their overall harm scores for Aotearoa New Zealand youth, showing contributions from harms experienced by those who use the drug and harm experienced by others. The cumulative weighted preference values (sum of all weighted scores for all the criteria of harm to users, and all the criteria of harm to others) for each drug are shown above each bar. Previous drug harm MCDA studies did not present drugs in order of decreasing overall harm.
MCDA: multi-criteria decision analysis.
Figure 4.
Drugs in order of their overall harm scores for Aotearoa New Zealand youth, showing individual criterion contributions after weighting. The cumulative preference values (sum of weighted contribution for each criterion) for each drug are shown above each bar. Previous drug harm MCDA studies did not present drugs in order of decreasing overall harm.
MCDA: multi-criteria decision analysis.
Overall population and youth-specific harm comparisons
When considering the contribution of individual harm criteria to overall harm scores, differences were observed between the total population and youth. For instance, family adversities had a higher contribution to harm for the total population, and drug-related damage tended to account for more harm in youth (e.g. unwanted sexual activity, accidents to the person using the drug). Cannabis was evaluated as more harmful to youth, ranking sixth for youth, compared with ninth for the overall population. Youth ratings for cannabis were higher in the broader harms to self-category, with larger contributions from criteria such as impairment in function and drug-related mortality (e.g. due to the outcomes of cannabis-related motor vehicle accidents where impairment is a contributing or causal factor, and higher weighting of youth drug-related mortality). In contrast, tobacco was rated lower for youth, when compared with its ranking in the whole population, largely because the youth panel did not consider harms accrued over the lifetime. Solvents and fuels were also ranked much higher in the youth MCDA, and this ranking was particularly high when considering harm only to the youth that use these substances. Similar to the overall population harm rankings, the opioid groups mostly clustered together in the youth-specific rankings. However, though many substance categories had a similar position in rankings for youth and for the overall population, for youth there were much smaller differences in the number of points between the drug ranked as most harmful (alcohol) and the following eight most harmful drugs. Lastly, while rankings for ENDs and vapes were still relatively low in the youth workshops, they were ranked as higher in this population due to patterns of heavy use by individuals and the impact of high nicotine exposure.
Discussion
This study involved the ranking and weighting of harms from a wide range of drugs used in Aotearoa New Zealand, with an expert panel employing an established MCDA methodology. In addition to ranking drug harms for the overall population, we also undertook a separate process focused specifically on drug harm among Aotearoa New Zealand youth aged 12–17 years. This is, to the best of our knowledge, the first drug harms ranking study specific to youth. The study also modified existing criteria and included two new harm criteria to more closely reflect an Aotearoa New Zealand cultural view.
Consistent with drug harm MCDA findings for the United Kingdom (UK), European Union (EU) and Australia (Bonomo et al., 2019; Nutt et al., 2010; van Amsterdam et al., 2015b), alcohol was ranked as the most harmful drug in the overall population workshops, and in the youth-specific workshop in Aotearoa New Zealand. The issue of alcohol misuse in New Zealand is widespread, where an estimated 19% of adults, and 33% of Māori adults, drink to hazardous levels (New Zealand Ministry of Health, 2022). Many experts argue that current alcohol policy and regulations in Aotearoa New Zealand are insufficient to curb these harms and their inequitable distribution, with the annual cost of alcohol harm estimated as $7 billion (Nana, 2018). When only considering harms to self, alcohol was ranked lower in the youth MCDA, with the panel discussion focussing on an ‘average user’ of alcohol in youth, and reflecting on current consumption patterns (Fleming et al., 2020). Despite this ‘average user’ approach, it is also important to note that binge drinking among this group remains high when compared with other countries, reflecting the relative ease at which youth can access alcohol (Fleming et al., 2020). To meaningfully reduce alcohol-related harm in New Zealand, it is important to consider the major recommendations made by the New Zealand Law Commission in 2010, which are well supported by international evidence: increasing the price of alcohol via excise tax; eliminating alcohol advertising and sponsorship; reducing the density and opening hours of alcohol outlets; and increasing the age of purchase from 18 to 20 (New Zealand Law Commission, 2010). A minimum unit pricing scheme is also recommended, with this strategy having demonstrated efficacy in several countries (Franco, 2015; Hydes et al., 2019). Furthermore, with regard to inequity of harm, alcohol law and policies must also address the ongoing impacts of colonisation and the broader social determinants of health, as well as enable Māori to lead and define the way forward for them in the alcohol space.
Methamphetamine was ranked as second most harmful in the overall population and youth workshops, which reflected its significant adverse impacts upon those who use it and their communities. This high ranking was at odds with findings from the EU and UK rankings, but consistent with those of the Australian drug harms ranking study. As with Australia, Aotearoa New Zealand has a comparatively high prevalence of methamphetamine use by international standards, with use being overrepresented in areas of socio-economic deprivation, among males, and among Māori (Bax, 2021; Price et al., 2021). In contrast, Europe has lower rates of methamphetamine use, with use being largely limited to specific countries and regions (Bonomo et al., 2019). However, one key difference between the Australian and Aotearoa New Zealand MCDA findings was that the harm to others arising from methamphetamine use was significantly higher in Aotearoa New Zealand. In the overall population ranking, methamphetamine received high scores on harm to others criteria including family adversities, intergenerational harm and community harm. Factors that contributed to the high ranking of methamphetamine included its deleterious effects upon physical and mental health, high potency and associated risk of dependence, impacts on cognitive function, contribution to acquisitive and violent crime, stigmatisation, and impact upon communities (Barr et al., 2006; Boden et al., 2023; Darke et al., 2008; Deen et al., 2021; Foulds et al., 2020; McKetin et al., 2020; Potvin et al., 2018). Taken together, these findings indicate that methamphetamine use is a significant social and community issue in Aotearoa New Zealand. Several approaches have recently been recommended to address this harm, including the expansion of an existing social well-being intervention, health-harm reduction measures, and increased treatment and support for those who use methamphetamine (Yasbek et al., 2022).
For both the total population and youth, synthetic cannabinoids were rated as third most harmful overall, and as more harmful than cannabis. While improved drug checking and surveillance systems will assist in mitigating the harms associated with the rapidly evolving supply of high potency synthetic cannabinoids (Peacock et al., 2019), these drugs are likely to have ongoing appeal due to their low price, high strength and ability to avoid detection in drug tests. Thus, ongoing review of synthetic cannabinoid harm reduction measures and policy settings will be necessary. In Aotearoa New Zealand, the Psychoactive Substances Act was put in place to regulate and to assess and potentially approve new psychoactive substances including synthetic cannabinoids for legal sales (Rychert and Wilkins, 2018a; Rychert and Wilkins, 2018b); however, no psychoactive products have been approved under this framework. When considering only harms to the individual, synthetic cannabinoids and methamphetamine were ranked almost equally as being most harmful to youth who use these drugs, due to factors such as impacts on education, death from overdoses, and the impact of losing close relationships and support systems as an adolescent. It is also notable that cannabis was rated as being significantly more harmful to youth who use these drugs, relative to other drugs, than to the overall population. This difference reflects issues such as the negative psychosocial impact of early onset cannabis use in particular (Fergusson et al., 2002).
The harm scores for opioid drugs were lower than those seen in Australia, with the opioid drug groups ranking fifth or lower for the overall Aotearoa New Zealand population, compared to heroin and fentanyls in Australia that ranked third and fourth, respectively. Fentanyl was first detected as a contaminant in the Aotearoa New Zealand illicit drug market in February 2018 (Know Your Stuff, 2018); however, it is important to note that our workshops occurred prior to further detections of local use of powdered fentanyl (Heikell, 2022). Although prevalence was not considered in these workshops, the previous lack of use meant that expert knowledge on local fentanyl-related harms was limited. While the mortality risks of fentanyl were widely understood by the panel members, very limited local data may have meant that some local fentanyl-related harms, such as community damage, were less salient for our expert panel. It is essential to be prepared for these high-potency opioids increasing in the local drug market, and therefore, investment in harm reduction needs to be proactive (Ponton and George, 2020). This should include overdose prevention measures such as supervised injecting facilities and take-home naloxone programmes, both of which have extensive evidence of efficacy in reducing harm (Monds et al., 2022; Levengood et al., 2021; Tse et al., 2022). Given that Aotearoa New Zealand’s drug market may change, integrated and responsive systems for rapid surveillance, and engagement with affected communities is vital.
When comparing rankings from the youth and overall population MCDA results, several differences were apparent. The family adversity criterion was evaluated as being less significant in the youth panel than the population panel. Although drug use by young people can result in significant family adversity, including worry and conflict between family members, there were several additional features of this criterion which were more relevant to the wider population. For instance, drug use by adolescents was identified as less likely to result in issues such as child maltreatment, loss of family income due to job loss or drug purchase, or separation of families due to drug-related imprisonment. Another key difference was seen for drug-related damage, which tended to make up a higher proportion of overall harm scores in the youth workshops, relative to the overall workshops. For youth, ratings for this criterion were elevated at times due to issues such as associations between the use of some drugs and self-harm (Bresin and Mekawi, 2022), and the higher risk of self-harm among young people (Klonsky, 2007). In terms of the rankings for specific drugs, a large difference was observed for solvents and fuels, which were ranked fourth most harmful for youth, compared with tenth for the overall population. In addition to potentially causing pronounced and lasting cognitive impairment following chronic use (Dingwall and Cairney, 2011; Manikandan and Balasubramanian, 2020), solvents and fuels are more commonly used by youth who are already vulnerable, including those from lower socio-economic backgrounds and more troubled families (Dinwiddie, 1994; Kurtzman et al., 2001). For these individuals, impacts on neurological and physiological functioning may further limit opportunities such as educational attainment and associated career pathways (Real et al., 2021; Manikandan and Balasubramanian, 2020). Given these unique findings for youth, and their ability to inform specific drug harm strategies for this group, future drug harm studies should also consider the value of separately ranking harm for younger individuals.
The impact upon families and communities was pronounced for many of the drugs, including alcohol, methamphetamine, tobacco, synthetic cannabinoids and different opioid drugs. These harms encompass issues such as child abuse and neglect, problems with emotional development for children, intimate partner violence and foetal alcohol spectrum disorder (Kelley et al., 2010; Wells, 2009). In many cases, the continued purchase of drugs can result in debt, unemployment and risks to housing, while imprisonment due to drug-related crimes can lead to separation of families and loss of employment opportunities. Issues such as these may perpetuate a cycle of intergenerational harm, whether through increased likelihood of drug misuse among younger generations, loss of connection to family/whānau, or through associated adverse psychosocial outcomes. Higher rates of drug use can also lead to stigmatisation of particular communities in which drug use occurs, while internalised stigma may lead to further harm within these groups (Can and Tanrıverdi, 2015). The findings also highlighted the relevance of the two new criteria of intergenerational harm (harm to others) and non-physical/spiritual harm (harm to self) in capturing drug-related harm in Aotearoa New Zealand. For many drugs, these two criteria made up a large portion of the overall harm from a given drug. For instance, in both the youth and overall results, intergenerational harm represented one of the highest criterion contributions for several drugs, including alcohol, methamphetamine, cannabis, and tobacco. Findings from these two new criteria highlighted additional ways that many drugs can harm others and perpetuate existing difficulties arising from drug use. Considering their utility in measuring additional forms of harm, future drug harms MCDA studies may similarly choose to include these criteria in their decision matrices.
For many drugs, current policy responses contributed to higher ratings on specific criteria, with one example being criminalisation due to drug possession and use. Therefore, for drugs such as cannabis, the higher harm scores are largely a function of current drug policy settings. For those affected by drug misuse, prosecution for possession acts as an additional stressor while reducing future opportunities. Māori are disproportionally affected by criminalisation of people who use drugs; although Māori make up 17% of the population of Aotearoa New Zealand, 48% of those convicted of drug possession are Māori, demonstrating clearly that drug laws are being enforced in a racially biased manner (New Zealand Drug Foundation, 2022; Statistics New Zealand, 2021). Our recommendation is that a review of Aotearoa New Zealand’s drug policy is needed, which considers a health-based approach to managing drug use and structural determinants of drug harm, including any negative effects of the current prohibition-based drug policy. Drug-related harms and existing strategies to prevent drug availability and use also tend to impact the most vulnerable populations. Therefore, implementing evidence-based harm reduction measures, in addition to focusing on population-level risk factors, such as socio-economic deprivation, may be a more effective way of reducing drug-related harm (Holland et al., 2022).
These findings should be considered with a number of limitations in mind, some of which have been previously described in relation to the MCDA method used to rank drug harms (Nutt et al., 2010; van Amsterdam et al., 2015a; van Amsterdam et al., 2015b). Firstly, experts can only draw on available knowledge and resources, which are incomplete and limited for some drug types. For instance, for some drugs that are novel or have a lower prevalence of use within Aotearoa New Zealand, there may be incomplete data on some kinds of harm (e.g. social harms). It is possible that higher-profile harms or more prevalent drugs had more salience for the expert panel; the process relies on best-available knowledge at a given point in time. For instance, as data on ENDs/vapes are currently limited, it is possible that the ratings for this category may differ markedly in a future drug harms ranking for Aotearoa New Zealand. The process was also conducted under time pressure, meaning that decisions had to be made fairly quickly and relied heavily upon the knowledge of panel members at the time. Group decisions are inherently susceptible to social biases, and it is possible that these sources of bias influenced the evaluations, although these were perhaps limited by the facilitation process. Another potential source of bias involved the use of the overall population data as a starting point for the youth MCDA, as opposed to starting the process anew. However, this was the most practical option at the time and was also beneficial in that most youth panel members gained valuable insights during the overall population workshop. We aimed to include a wide range of expertise, but it is also likely there remained knowledge gaps that may have influenced the outcomes of the ranking exercise. For example, had there been more panel members working in areas such as opioid substitution therapy services and pain clinics, scores for the opioid categories may have been higher. Similarly, the inclusion of more first responders, such as ambulance personnel, could have increased the diversity of expertise within the panel. We did not adjust our harm to user scores by prevalence of use, which was a decision made in part because of incomplete prevalence data. Although the concept of an ‘average’ individual who uses a drug was difficult to apply at times, the investigators believed that this was the best way of avoiding a ‘worst case’ evaluation of drug harm, or only considering the harms in terms of rare outcomes that are not experienced by the majority of individuals who use them. Additionally, while a set of assumptions was established for the ranking process, discussion at times strayed away from those assumptions; nonetheless, the panel and facilitators were usually quick to reiterate those assumptions and steer the discussion accordingly.
Our findings highlight the importance of separately considering harms to young people but also have two relevant limitations. First, expert panel members needed to be at least 18 years of age due to the ethical approval for this study, meaning the workshops could not directly include the perspectives of anyone aged 12–17 years. Second, an adult construct of harm was used for these workshops, in part to facilitate comparison of results, but it is likely that drug harm is conceptualised and experienced differently by young people. Due to this, young people may place more weight on different criteria, or may identify types of harm which are not well described in the current criteria. Understanding this will be the focus of a future research project as the perspectives of young people are particularly important in guiding prevention and early intervention policy and strategies. Lastly, we note that we have not yet undertaken this process for Māori, who, as noted previously, are disproportionately subject to drug policy harms (arrest/conviction). A further step in this research will be for a Māori expert panel, which has been established, to later meet and specifically examine drug harms for Māori. The outcomes from this component of the research will be presented separately.
A broad range of harms are associated with psychoactive drug use, though the extent and nature of those harms is difficult to quantify. This study is the first local drug harms ranking study using an MCDA approach to evaluate and rank the harm arising from drugs used within Aotearoa New Zealand. It should be acknowledged that not all people who use drugs experience harm (NZ Drug Foundation; United Nations Office on Drugs and Crime, 2022). However, drugs are nonetheless associated with considerable harm for many people, and an understanding of that harm should be used to prevent or otherwise minimise the impact upon those individuals. These local results can be used to inform drug policy, funding decisions, treatment and education, and, ultimately, to reduce harm and associated inequities.
Supplemental Material
Supplemental material, sj-docx-1-jop-10.1177_02698811231182012 for The New Zealand drug harms ranking study: A multi-criteria decision analysis by Rose Crossin, Lana Cleland, Chris Wilkins, Marta Rychert, Simon Adamson, Tuari Potiki, Adam C Pomerleau, Blair MacDonald, Dwaine Faletanoai, Fiona Hutton, Geoff Noller, Ian Lambie, Jane L Sheridan, Jason George, Kali Mercier, Kristen Maynard, Louise Leonard, Patricia Walsh, Rhys Ponton, Sue Bagshaw, Suresh Muthukumaraswamy, Tracey McIntosh, Edward Poot, Paul Gordon, Patrick Sharry, David Nutt and Joseph Boden in Journal of Psychopharmacology
Acknowledgments
The authors acknowledge the contributions of Amanda Jones, Jude Ball and Nicki Jackson as expert panel members for this study.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The project was funded by the Health Research Council of NZ (Grant 21-638) awarded to authors RC, JB, TP and CW, as well as a University of Otago Research Grant (2021) awarded to authors RC and JB.
ORCID iDs: Rose Crossin  https://orcid.org/0000-0003-1814-1330
https://orcid.org/0000-0003-1814-1330
Rhys Ponton  https://orcid.org/0000-0002-4833-2333
https://orcid.org/0000-0002-4833-2333
Supplemental material: Supplemental material for this article is available online.
References
- Alcohol Healthwatch (2023) Harm to Māori. Available at: http://www.ahw.org.nz/Issues-Resources/Harm-to-Māori (accessed 21 February 2023).
- Ball J, Crossin R, Boden J, et al. (2022. a) Long-term trends in adolescent alcohol, tobacco and cannabis use and emerging substance use issues in Aotearoa New Zealand. J R Soc N Z 52: 450–471. [Google Scholar]
- Ball J, Zhang J, Kim A, et al. (2022. b) Addressing Alcohol Harm in Adolescents. Technical Report 1: Methods and Overview of Findings. Wellington: University of Otago. [Google Scholar]
- Barlow C. (1991) Tikanga Whakaaro: Key Concepts in Māori Culture. Australia: Oxford University Press. [Google Scholar]
- Barr AM, Panenka WJ, MacEwan GW, et al. (2006) The need for speed: An update on methamphetamine addiction. J Psychiatry Neurosci 31: 301–313. [PMC free article] [PubMed] [Google Scholar]
- Bax T. (2021) The life-course of methamphetamine users in Aotearoa/New Zealand: School, friendship and work. J Criminol 54: 425–447. [Google Scholar]
- Bedford KR, Nolan SL, Onrust R, et al. (1987) The illicit preparation of morphine and heroin from pharmaceutical products containing codeine: ‘Homebake’ laboratories in New Zealand. Forensic Sci Int 34: 197–204. [DOI] [PubMed] [Google Scholar]
- Boden JM, Foulds JA, Newton-Howes G, et al. (2023) Methamphetamine use and psychotic symptoms: Findings from a New Zealand longitudinal birth cohort. Psychol Med 53: 987–994. [DOI] [PubMed] [Google Scholar]
- Bonomo Y, Norman A, Biondo S, et al. (2019) The Australian drug harms ranking study. J Psychopharmacol 33: 759–768. [DOI] [PubMed] [Google Scholar]
- Bresin K, Mekawi Y. (2022) Different ways to drown out the pain: A meta-analysis of the association between nonsuicidal self-injury and alcohol use. Arch Suicide Res 26: 348–369. [DOI] [PubMed] [Google Scholar]
- Brumback T, Thompson W, Cummins K, et al. (2021) Psychosocial predictors of substance use in adolescents and young adults: Longitudinal risk and protective factors. Addict Behav 121: 106985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Can G, Tanrıverdi D. (2015) Social functioning and internalized stigma in individuals diagnosed with substance use disorder. Arch Psychiatr Nurs 29: 441–446. [DOI] [PubMed] [Google Scholar]
- Crossin R, Cleland L, Rychert M, et al. (2022) Measuring drug harm in New Zealand: A stocktake of current data sources. N Z Med J 135: 93–104. [PubMed] [Google Scholar]
- Cunningham R, Kvalsvig A, Peterson D, et al. (2018) Stocktake Report for the Mental Health and Addiction Inquiry. Wellington, New Zealand: University of Otago. [Google Scholar]
- Darke S, Kaye S, McKetin R, et al. (2008) Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev 27: 253–262. [DOI] [PubMed] [Google Scholar]
- Deen H, Kershaw S, Newton N, et al. (2021) Stigma, discrimination and crystal methamphetamine (‘ice’): Current attitudes in Australia. Int J Drug Policy 87: 102982. [DOI] [PubMed] [Google Scholar]
- Dingwall KM, Cairney S. (2011) Recovery from central nervous system changes following volatile substance misuse. Subst Use Misuse 46: 73–83. [DOI] [PubMed] [Google Scholar]
- Dinwiddie SH. (1994) Abuse of inhalants: A review. Addiction 89: 925–939. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Swain-Campbell N. (2002) Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction 97: 1123–1135. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Swain-Campbell NR, Horwood LJ. (2003) Arrests and convictions for cannabis related offences in a New Zealand birth cohort. Drug Alcohol Depend 70: 53–63. [DOI] [PubMed] [Google Scholar]
- Fleming T, Ball J, Peiris-John R, et al. (2020) Youth19 Rangatahi Smart Survey Initial Findings: Substance Use. Available at: https://www.fmhs.auckland.ac.nz/assets/fmhs/faculty/ahrg/docs/2020/Youth19-Initial-Findings-Intro-and-Method.pdf (accessed 23 February 2023).
- Foulds JA, Boden JM, McKetin R, et al. (2020) Methamphetamine use and violence: Findings from a longitudinal birth cohort. Drug Alcohol Depend 207: 107826. [DOI] [PubMed] [Google Scholar]
- Griswold MG, Fullman N, Hawley C, et al. (2018) Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 392: 1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubbels J, van der Put CE, Assink M. (2019) Risk factors for school absenteeism and dropout: A meta-analytic review. J Youth Adolesc 48: 1637–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikell L. (2022) Urgent warning after powdered fentanyl found in New Zealand for first time, 11 hospitalised. Newshub. Available at: https://www.newshub.co.nz/home/new-zealand/2022/06/urgent-warning-after-powdered-fentanyl-found-in-new-zealand-for-first-time-11-hospitalised.html (accessed 27 November 2022).
- Holland A, Stevens A, Harris M, et al. (2022) Analysis of the UK government’s 10-year drugs strategy—a resource for practitioners and policymakers. J Public Health. Epub ahead of print 29 October 2022. DOI: 10.1093/pubmed/fdac114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hydes T, Gilmore W, Sheron N, et al. (2019) Treating alcohol-related liver disease from a public health perspective. J Hepatol 70: 223–236. [DOI] [PubMed] [Google Scholar]
- Katikireddi SV, Whitley E, Lewsey J, et al. (2017) Socioeconomic status as an effect modifier of alcohol consumption and harm: Analysis of linked cohort data. Lancet Public Health 2: e267–e276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley ML, Klostermann K, Doane AN, et al. (2010) The case for examining and treating the combined effects of parental drug use and interparental violence on children in their homes. Aggress Violent Behav 15: 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED. (2007) Non-suicidal self-injury: An introduction. J Clin Psychol 63: 1039–1043. [DOI] [PubMed] [Google Scholar]
- Know Your Stuff (2018) Fentanyl found at New Zealand festival. Available at: https://knowyourstuff.nz/2018/03/20/fentanyl-found-at-new-zealand-festival/ (accessed 27 November 2022).
- Kurtzman TL, Otsuka KN, Wahl RA. (2001) Inhalant abuse by adolescents. J Adolesc Health 28: 170–180. [DOI] [PubMed] [Google Scholar]
- Levengood TW, Yoon GH, Davoust MJ, et al. (2021) Supervised injection facilities as harm reduction: A systematic review. Am J Prev Med 61: 738–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoun RJ, Reuter P. (2001) Drug War Heresies: Learning From Other Vices, Times, and Places. Cambridge: Cambridge University Press. [Google Scholar]
- Manikandan K, Balasubramanian S. (2020) An uprising health concern of inhalant abuse among adolescents: A mini review. J Pharm Sci Res 12: 151–155. [Google Scholar]
- Marie D, Fergusson DM, Boden JM. (2008) Links between ethnic identification, cannabis use and dependence, and life outcomes in a New Zealand birth cohort. Aust N Z J Psychiatry 42: 780–788. [DOI] [PubMed] [Google Scholar]
- McFadden Consultancy (2016) The New Zealand Drug Harm Index 2016. Wellington: Ministry of Health. [Google Scholar]
- McFadden M, Bellamore L, MacDonald B. (2022) The New Zealand Illicit Drug Harm Index 2020. Wellington: Ministry of Health. [Google Scholar]
- McKetin R, Boden JM, Foulds JA, et al. (2020) The contribution of methamphetamine use to crime: Evidence from Australian longitudinal data. Drug Alcohol Depend 216: 108262. [DOI] [PubMed] [Google Scholar]
- Monds LA, Bravo M, Mills L, et al. (2022) The Overdose Response with Take Home Naloxone (ORTHN) project: Evaluation of health worker training, attitudes and perceptions. Drug Alcohol Rev 41: 1085–1094. [DOI] [PubMed] [Google Scholar]
- Moorfield JC. (2023. a) Te Aka Māori Dictionary. Available at: https://maoridictionary.co.nz/search?&keywords=whanau (accessed 1 May 2023).
- Moorfield JC. (2023. b) Te Aka Māori Dictionary. Available at: https://maoridictionary.co.nz/dictionary-info (accessed 9 February 2023).
- Nana G. (2018) Alcohol costs-but, who pays. In: Alcohol Action NZ Conference, Wellington, New Zealand. [Google Scholar]
- New Zealand Drug Foundation (2022) Drugs snapshot shows system grossly failing Māori across the board. Available at: https://www.drugfoundation.org.nz/news-media-and-events/drugs-snapshot-shows-system-grossly-failing-maori-across-the-board/ (accessed 1 May 2023).
- New Zealand Law Commission (2010) Alcohol in our lives: Curbing the harm. Available at: https://www.lawcom.govt.nz/sites/default/files/projectAvailableFormats/NZLC%20R114.pdf (accessed 20 April 2023).
- New Zealand Ministry of Health (2020) Waitangi tribunal health services and outcomes inquiry (Wai 2575). Available at: https://www.health.govt.nz/our-work/populations/maori-health/wai-2575-health-services-and-outcomes-kaupapa-inquiry (accessed 24 April 2023).
- New Zealand Ministry of Health (2022) Annual update of key results 2021/22: New Zealand health survey. Available at: https://www.health.govt.nz/publication/annual-update-key-results-2021-22-new-zealand-health-survey. (accessed 20 April 2023)
- New Zealand Ministry of Justice (2021) Te Rau o te Tika: The justice system kaupapa inquiry (Wai 3060). Available at: https://www.justice.govt.nz/justice-sector-policy/justice-system-kaupapa-inquiry/#te-rau-o-te-tika (accessed 24 April 2023).
- Nodora J, Hartman SJ, Strong DR, et al. (2014) Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav 39: 1695–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt D, King LA, Phillips L. (2010) Drug harms in the UK: A multicriteria decision analysis. Lancet 376: 1558–1565. [DOI] [PubMed] [Google Scholar]
- Nutt D, King LA, Saulsbury W, et al. (2007) Development of a rational scale to assess the harm of drugs of potential misuse. Lancet 369: 1047–1053. [DOI] [PubMed] [Google Scholar]
- NZ Drug Foundation (nd). Drugs in NZ – an overview. Available at: https://www.drugfoundation.org.nz/policy-and-advocacy/drugs-in-nz-an-overview/ (accessed 20 January 2023).
- Peacock A, Bruno R, Gisev N, et al. (2019) New psychoactive substances: Challenges for drug surveillance, control, and public health responses. Lancet 394: 1668–1684. [DOI] [PubMed] [Google Scholar]
- Phillips LD. (2017) Best practice for MCDA in healthcare. In: Marsh K, Goetghebeur M, Thokala P, et al. (eds) Multi-Criteria Decision Analysis to Support Healthcare Decisions. Cham: Springer, pp. 311–329. [Google Scholar]
- Phillips LD, Bana e, Costa CA. (2007) Transparent prioritisation, budgeting and resource allocation with multi-criteria decision analysis and decision conferencing. Ann Oper Res 154: 51–68. [Google Scholar]
- Pohatu W. (2007) The Marae: Nau Mai Haere Mai Ki Te Marae. Welcome to Our Marae, Welcome to Our Culture. Auckland: Reed Publishing (NZ) Ltd. [Google Scholar]
- Ponton R, George J. (2020) Pharmaceutical opioid changes risk overdose increase in New Zealand. N Z Med J 133: 95–96. [PubMed] [Google Scholar]
- Potvin S, Pelletier J, Grot S, et al. (2018) Cognitive deficits in individuals with methamphetamine use disorder: A meta-analysis. Addict Behav 80: 154–160. [DOI] [PubMed] [Google Scholar]
- Price M, Wilkins C, Tscharke BJ, et al. (2021) Spatial, temporal and socioeconomic patterns of illicit drug use in New Zealand assessed using wastewater-based epidemiology timed to coincide with the census. N Z Med J 134: 11–26. [PubMed] [Google Scholar]
- Real T, Cruz SL, Medina-Mora ME, et al. (2021) Inhalant addiction. In: el-Guebaly N, Carrà G, Galanter M, et al. (eds) Textbook of Addiction Treatment. Cham: Springer, pp. 281–306. [Google Scholar]
- Rhodes T. (2009) Risk environments and drug harms: A social science for harm reduction approach. Int J Drug Policy 20: 193–201. [DOI] [PubMed] [Google Scholar]
- Robson H, Braund R, Glass M, et al. (2021) Synthetic cannabis: Adverse events reported to the New Zealand Pharmacovigilance Centre. Clin Toxicol (Phila) 59: 472–479. [DOI] [PubMed] [Google Scholar]
- Rychert M, Wilkins C. (2018. a) A critical analysis of the implementation of a legal regulated market for new psychoactive substances (“legal highs”) in New Zealand. Int J Drug Policy 55: 88–94. [DOI] [PubMed] [Google Scholar]
- Rychert M, Wilkins C. (2018. b) Understanding the development of a regulated market approach to new psychoactive substances (NPS) in New Zealand using Punctuated Equilibrium Theory. Addiction 113: 2132–2139. [DOI] [PubMed] [Google Scholar]
- Sassi F. (2015) Tackling Harmful Alcohol Use Economics and Public Health Policy: Economics and Public Health Policy. Paris: OECD publishing. [Google Scholar]
- Statistics New Zealand (2021) Māori Population Estimates: At 30 June 2021. Available at: https://www.stats.govt.nz/information-releases/maori-population-estimates-at-30-june-2021/ (accessed 30 April 2023).
- Stautz K, Cooper A. (2013) Impulsivity-related personality traits and adolescent alcohol use: A meta-analytic review. Clin Psychol Rev 33: 574–592. [DOI] [PubMed] [Google Scholar]
- Tse WC, Djordjevic F, Borja V, et al. (2022) Does naloxone provision lead to increased substance use? A systematic review to assess if there is evidence of a ‘moral hazard’ associated with naloxone supply. Int J Drug Policy 100: 103513. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (2019) World Drug Report 2019. Vienna: United Nations Publication. [Google Scholar]
- United Nations Office on Drugs and Crime (2022) World Drug Report 2022. Vienna: United Nations Publication. [Google Scholar]
- van Amsterdam J, Brunt T, van den Brink W. (2015. a) The adverse health effects of synthetic cannabinoids with emphasis on psychosis-like effects. J Psychopharmacol 29: 254–263. [DOI] [PubMed] [Google Scholar]
- van Amsterdam J, Nutt D, Phillips L, et al. (2015. b) European rating of drug harms. J Psychopharmacol 29: 655–660. [DOI] [PubMed] [Google Scholar]
- Wells K. (2009) Substance abuse and child maltreatment. Pediatr Clin North Am 56: 345–362. [DOI] [PubMed] [Google Scholar]
- Wilkins C, Rychert M, Queirolo R, et al. (2022) Assessing options for cannabis law reform: A Multi-Criteria Decision Analysis (MCDA) with stakeholders in New Zealand. Int J Drug Policy 105: 103712. [DOI] [PubMed] [Google Scholar]
- Winter T, Riordan BC, Surace A, et al. (2019) Association between experience of racial discrimination and hazardous alcohol use among Māori in Aotearoa New Zealand. Addiction 114: 2241–2246. [DOI] [PubMed] [Google Scholar]
- Yasbek P, Mercier K, Elder H, et al. (2022) Minimising the Harms From Methamphetamine. Available at: https://www.drugfoundation.org.nz/assets/uploads//NZDF-and-HCF-Minimising-the-harms-from-methamphetamine-report-for-web.pdf (accessed 20 April 2023).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jop-10.1177_02698811231182012 for The New Zealand drug harms ranking study: A multi-criteria decision analysis by Rose Crossin, Lana Cleland, Chris Wilkins, Marta Rychert, Simon Adamson, Tuari Potiki, Adam C Pomerleau, Blair MacDonald, Dwaine Faletanoai, Fiona Hutton, Geoff Noller, Ian Lambie, Jane L Sheridan, Jason George, Kali Mercier, Kristen Maynard, Louise Leonard, Patricia Walsh, Rhys Ponton, Sue Bagshaw, Suresh Muthukumaraswamy, Tracey McIntosh, Edward Poot, Paul Gordon, Patrick Sharry, David Nutt and Joseph Boden in Journal of Psychopharmacology