Abstract
Background and purpose
The Brace Questionnaire (BrQ) is a disease-specific health-related quality of life (HRQOL) instrument for measuring perceived health status of scoliosis patients undergoing brace treatment. The purpose of this study is to evaluate the validity and reliability of a translated and culturally adapted Dutch version of the BrQ.
Patients and methods
The original Greek BrQ was translated into Dutch and a cross-cultural adaptation and validation processes were conducted. Subsequently, 80 adolescent idiopathic scoliosis (AIS) patients undergoing active brace treatment were included from 4 scoliosis centers to evaluate the validity and reliability of the Dutch version of the BrQ. The questionnaire’s floor and ceiling effects, internal consistency, and test–retest reliability were assessed. Concurrent validity was evaluated by comparing the BrQ with the revised Scoliosis Research Society 22-item questionnaire (SRS-22r) scores.
Results
The mean total BrQ score was 75.9 (standard deviation [SD] 11.3) and the mean domain scores varied between 3.4 (SD 0.9) and 4.2 (SD 0.7) for the domains “vitality” and “bodily pain,” respectively. There were no floor and ceiling effects for the total BrQ score. The BrQ showed satisfactory internal consistency in most subdomains with a Cronbach’s α ranging between 0.35 for the domain “general health perception” and 0.89 for the domain “self-esteem and aesthetics.” Excellent test–retest reproducibility was observed for the total BrQ score (ICC 0.91), and the BrQ was successfully validated against the SRS-22r.
Conclusion
The translated and culturally adapted Dutch version of the BrQ is a valid and reliable HRQOL instrument for AIS patients undergoing brace treatment.
Bracing of adolescent idiopathic scoliosis (AIS) is effective to decrease the progression risk and subsequent need for surgical treatment [1]. The success rate of bracing is mainly associated with compliance, as significant positive association between hours of brace wear and rate of treatment success has been observed [1-3]. Generally, studies have reported low compliance. Many factors contribute to this low compliance, including comfort, social issues, and self-image [3,4]. Disease-specific health-related quality of life (HRQOL) measurement could provide better insights into the impact of brace wear on different health domains, to improve compliance and subsequently long-term treatment success [5].
The revised Scoliosis Research Society 22-item questionnaire (SRS-22r) assesses the overall HRQOL of AIS patients but does not contain a specific item on the influence of brace therapy on HRQOL [6]. Therefore, the Brace Questionnaire (BrQ) was developed as a new instrument for measuring HRQOL of scoliosis patients undergoing brace treatment [7]. The original Greek BrQ has previously been translated into different languages and validated but has not yet been translated into the Dutch language [8-15]. Therefore, this study will evaluate the validity and reliability of a translated and culturally adapted Dutch version of the BrQ.
Patients and methods
Translation and cross-cultural adaption process
The translation and cross-cultural adaptation process were conducted in accordance with previously described guidelines [16]. First, 2 independent native Greek speakers, of whom 1 has a medical background, translated the original Greek BrQ into Dutch. These translations were merged into 1 Dutch version by both translators and a recording observer (CP) who guided the translation and adaptation process. All discrepancies were solved by consensus. Subsequently, a blinded backtranslation from Dutch into Greek was performed by 2 other independent native Greek speakers of whom 1 has a medical background. Finally, all translations were reviewed and a prefinal Dutch version was created during an expert committee meeting. 4 translators, including 2 language professionals, 2 orthopedic spine surgeons (DK and CF), and the recording observer attended the meeting. At this meeting the semantic, idiomatic, experiential, and conceptual equivalences between the original Greek BrQ and prefinal Dutch version were also examined. For the pretest 32 AIS patients, aged between 11 and 16 years old (23% male), completed the prefinal Dutch version of the BrQ and were asked for any difficulties in interpretation of the questions and answers. Since no difficulties in interpretation were experienced and only 2 words (“with scoliosis”) were added to Question 13 for better understanding, a second consultation of the expert committee was unnecessary. The final version of the Dutch BrQ after cross-cultural testing is shown in Supplementary data 1.
Study procedure
Patients from 4 scoliosis centers were prospectively included in this multicenter study from April 2022 to January 2023, according to the following inclusion criteria: (i) they were diagnosed with AIS, (ii) aged between 12 and 18 years, (iii) Dutch-speaking, and (iv) undergoing active brace treatment for at least 3 months. Patients with non-idiopathic scoliosis or previous spinal surgery were excluded. Eligible patients were asked for participation at the outpatient clinic or by telephone. After obtaining informed consent, included patients received a link to 2 questionnaires by email: (1) the final adapted Dutch version of the BrQ, and (2) the Dutch version of the SRS-22r for comparison and concurrent validity [6]. The SRS-22r questionnaire has previously been successfully translated into Dutch and validated and was used in previous BrQ validation studies in other languages as a scoliosis-specific quality-of-life questionnaire [8,10,12,13,15]. Both questionnaires were sent twice to investigate the test–retest reliability. After completing the first questionnaires, patients received a second link by email after an interval of 10–14 days. The patient could only complete the electronic questionnaire if all questions were answered.
The BrQ consists of 34 Likert-scale brace-related items, which are grouped into 8 domains (general health perception, physical functioning, emotional functioning, self-esteem and aesthetics, vitality, school activity, bodily pain, and social functioning) [7]. The scoring of the questions and domains of the Dutch version of the BrQ and SRS-22r was performed according to the corresponding scoring guidelines [6,7,17]. Both questionnaire scores range from 1 (minimum score) to 5 (maximum score). For the BrQ items 4, 5, 6, 12, 14, 15, 16, and 17, the answer “always” received a score of 5, and “never” a score of 1, because the answer “always” to these questions indicates better HRQOL. For the other 26 BrQ items, the answer “always” received a score of 1, and “never” a score of 5, because the answer “never” indicates better HRQOL for these specific questions. Subsequently, each item score is multiplied by 20 and the total score is divided by 34, resulting in a total minimum score of 20 and maximum score of 100. A higher score indicates better HRQOL [7]. Regarding the SRS-22r scoring system, total scores range between 5 and 25 for the domains function, pain, self-image, and mental health, and between 2 and 10 for satisfaction/dissatisfaction with management [6]. The average scores per domain and the total SRS-22r score vary between 1 and 5, where a higher score indicates better HRQOL.
Statistics
For both the BrQ and SRS-22r, the mean, standard deviation (SD), range, floor, and ceiling effects were determined per domain. Floor and ceiling effects were assessed by calculating the frequency of lowest and highest possible domain scores. The lowest possible domain score for each domain was 1 (in case all questions of the domain received a score of 1), and the highest possible domain score was 5 (in case all questions of the domain received a score of 5).
The reliability of the BrQ was assessed and compared with the SRS-22r by determining the internal consistency and reproducibility, respectively. Cronbach’s α was used to evaluate the internal consistency of each unidimensional scale (domain). A Cronbach’s α of 0.70–0.80 represents acceptable internal consistency, and > 0.80 represents good or excellent internal consistency [18]. Reproducibility was evaluated by a test–retest reliability analysis for the total score and per domain of the first and second measurement, using an intraclass correlation coefficient (ICC) (one-way random, single measures). An ICC larger than 0.90 is considered to indicate excellent reliability, and a value of 0.75–0.90 indicates good reliability [19].
Concurrent validity was assessed by comparing the mean scores of four BrQ domains (physical functioning, emotional functioning, self-esteem and aesthetics, and bodily pain) with 4 comparable domains of the SRS-22r (function, mental health, self-image, pain) using Pearson’s correlation coefficient [10,13]. A Pearson’s rho of > 0.75 is considered to represent good-to-excellent concurrent validity, a rho of 0.50–0.75 represents moderate-to-good validity, and 0.25–0.50 represents poor validity [20]. IBM SPSS Statistics for Windows, version 23.0 (IBM Corp, Armonk, NY, USA) was used for all statistical analysis. A P value < 0.05 was considered as statistically significant (2-tailed).
Ethics, funding, and disclosures
This study was approved by the Medical Ethical Review Board from University Medical Center Groningen (RR-number:202100536). No funding was received for conducting this study. The authors have no conflicts of interest to declare that are relevant to the content of this articles. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18492
Results
Patient characteristics
80 AIS patients undergoing active brace treatment gave their informed consent and were included in this multicenter validation and reliability study of the Dutch version of the BrQ (Table 1). The number of inclusions per center varied between 13 and 31. The response rate was 72% and varied per center (39% to 94%). 57 included patients (71%) completed both sets of questionnaires (Figure). The mean age at study inclusion was 14 years (SD 1.4), and 60 patients (75%) were female. A Boston brace was used in 99% of the included patients; 1 patient wore a Cheneau brace. The mean pre-brace major-curve Cobb angle was 38° (SD 12), and the self-reported mean number of hours of brace wear per day during the past month was estimated at 15.5 hours (SD 6.5).
Table 1.
Patient characteristics (80 patients)
| Criterion | missing, n | |
|---|---|---|
| Female sex | – | 60 |
| Postmenarchal at study inclusion | – | 44/60 |
| Age at brace initiation in years, mean (SD) | – | 12.7 (1.7) |
| Age at study inclusion in years, mean (SD) | – | 14.3 (1.4) |
| Body mass index at study inclusion, mean (SD) | – | 18.0 (2.9) |
| Risser stage a at study inclusion | – | |
| stage 0 | – | 18 |
| stage I | 7 | |
| stage II | 10 | |
| stage III | 15 | |
| stage IV | 29 | |
| stage V | 1 | |
| Pre-brace Cobb angle, mean (SD) | 2 | 38 (12) |
| Initial in-brace correction in %, mean (SD) | 10 | 29 (17) |
| Cobb angle at study inclusion, mean (SD) a | – | 36 (14) |
| Lenke classification before surgery | – | |
| type 1 | 50 | |
| type 5 | 19 | |
| type 2, 3, 4, or 6 | 11 | |
| Daily hours of brace wear, mean (SD) b | – | 15.5 (6.5) |
Measured on the last in-brace or out-of-brace radiograph before study inclusion.
Patients were asked to estimate their average number of hours of brace wear per day during the past month of brace treatment.
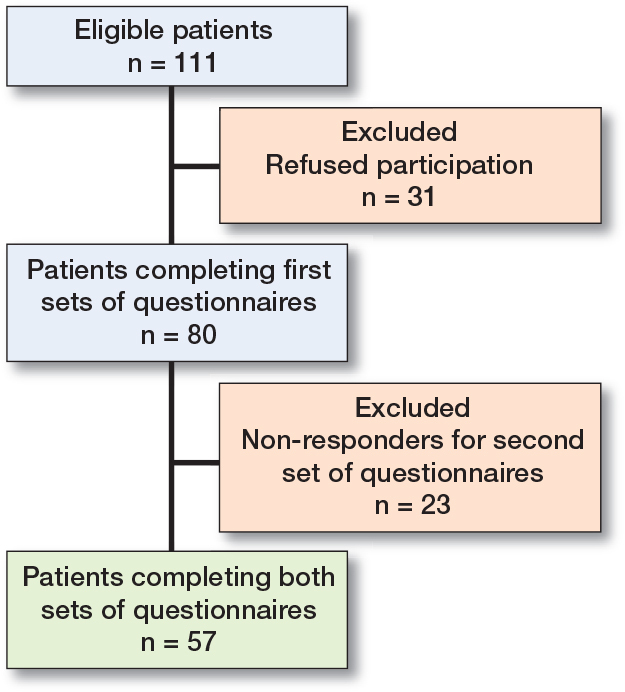
Patient inclusions and exclusions.
Total and domain scores
The mean total BrQ score for this Dutch study population was 75.9 (SD 11.3) and the mean domain scores of the 8 different BrQ domains varied between 3.4 (SD 0.9) for the domain “vitality” and 4.2 (SD 0.7) for the domain “bodily pain” (Table 2). There were no floor and ceiling effects for the total BrQ score. Also, no floor effects were observed for the BrQ domains, but ceiling effects between 1.3% and 15% were observed for all BrQ domains.
Table 2.
Domain scores of the BrQ and SRS-22r (80 patients)
| Domain (n) a | Mean (SD) | Range | Floor effect b | Ceiling effect b |
|---|---|---|---|---|
| BrQ | ||||
| General health perception (2) | 3.7 (0.8) | 2.0–5.0 | 0 | 6.3 |
| Physical functioning (7) | 3.6 (0.7) | 1.7–5.0 | 0 | 1.3 |
| Emotional functioning (5) | 3.6 (0.9) | 1.6–5.0 | 0 | 5.0 |
| Self-esteem and aesthetics (2) | 3.5 (0.9) | 1.5–5.0 | 0 | 10 |
| Vitality (2) | 3.4 (0.9) | 1.0–5.0 | 1.3 | 5.0 |
| School activity (3) | 3.9 (0.8) | 1.7–5.0 | 0 | 14 |
| Bodily pain (6) | 4.2 (0.7) | 2.3–5.0 | 0 | 15 |
| Social functioning (7) | 4.0 (0.8) | 1.6–5.0 | 0 | 6.3 |
| Total BrQ score | 75.9 (11.3) | 52.9–95.3 | 0 | 0 |
| SRS-22r | ||||
| Function (5) | 4.4 (0.5) | 3.0–5.0 | 0 | 16 |
| Pain (5) | 4.1 (0.7) | 1.4–5.0 | 0 | 8.8 |
| Self-image (5) | 3.5 (0.8) | 1.6–5.0 | 0 | 2.5 |
| Mental health (5) | 3.6 (0.8) | 1.0–5.0 | 1.3 | 2.5 |
| Satisfaction/dissatisfaction with management (2) | 3.8 (0.7) | 2.0–5.0 | 0 | 8.8 |
| Total SRS-22r score | 3.9 (0.6) | 2.2–4.8 | 0 | 0 |
BrQ = Brace Questionnaire.
SRS-22r = revised Scoliosis Research Society 22-item questionnaire
n = number of questions per domain.
Floor and ceiling effects are the percentage of patients who scored the lowest or highest possible domain score, respectively.
Regarding the SRS-22r, the mean total score was 3.9 (SD 0.6) and the domain scores varied between 3.5 (SD 0.8) for the domain “self-image” and 4.4 (SD 0.5) for the domain “function.” There were also no floor and ceiling effects for the total SRS-22r score. Ceiling effects between 2.5% and 16.3% were observed for all SRS-22r domains.
Internal consistency and reproducibility
The Cronbach’s α of the 8 different BrQ domains ranged between 0.35 (95% confidence interval [CI] –0.02 to 0.58) for the domain “general health perception” and 0.89 (CI 0.82–0.93) for the domain “self-esteem and aesthetics” (Table 3). The Cronbach’s α of the 5 SRS-22r domains varied between 0.57 and 0.85. The test–retest reproducibility was excellent for the BrQ (ICC 0.91, CI 0.85–0.94) and good for the SRS-22r (ICC 0.87, CI 0.79–0.92). The ICCs of the BrQ domains varied between 0.62 (CI 0.43–0.76) for the domain “self-esteem and aesthetics” and 0.86 (CI 0.78–0.92) for the domain “bodily pain,” and the ICCs of the SRS-22r domains varied between 0.64 and 0.85 (Table 3). The average time between the first and second measurement was 28 days (SD 17).
Table 3.
Internal consistency and test-retest reproducibility of the BrQ and SRS-22r domains (57 patients)
| Domain (n) | Internal consistency Cronbach’s α (CI) | Test-retest reproducibility ICC (CI) |
|---|---|---|
| BrQ total | 0.91 (0.85–0.94) | |
| General health perception (2) | 0.35 (–0.02–0.58) | 0.67 (0.50–0.79) |
| Physical functioning (7) | 0.55 (0.38–0.69) | 0.82 (0.71–0.89) |
| Emotional functioning (5) | 0.80 (0.72–0.86) | 0.79 (0.67–0.87) |
| Self-esteem and aesthetics (2) | 0.89 (0.82–0.93) | 0.62 (0.43–0.76) |
| Vitality (2) | 0.70 (0.53–0.81) | 0.79 (0.67–0.87) |
| School activity (3) | 0.59 (0.40–0.72) | 0.72 (0.57–0.82) |
| Bodily pain (6) | 0.78 (0.69–0.85) | 0.86 (0.78–0.92) |
| Social functioning (7) | 0.78 (0.69–0.84) | 0.80 (0.69–0.88) |
| SRS-22r total | 0.87 (0.79–0.92) | |
| Function (5) | 0.64 (0.50–0.75) | 0.74 (0.60–0.84) |
| Pain (5) | 0.80 (0.73–0.86) | 0.77 (0.64–0.86) |
| Self-image (5) | 0.79 (0.70–0.85) | 0.85 (0.75–0.91) |
| Mental health (5) | 0.85 (0.80–0.90) | 0.77 (0.64–0.86) |
| Satisfaction/dissatisfaction with management (2) | 0.57 (0.33–0.72) | 0.64 (0.45–0.77) |
For abbreviations, see Table 2.
ICC = interclass correlation coefficient; CI = 95% confidence interval
Concurrent validity
Statistically significant concurrent validity was established for the total BrQ and total SRS-22r scores (Table 4). Also, the BrQ domains “physical functioning,” “emotional functioning,” “self-esteem and aesthetics,” and “bodily pain” correlated significantly with the comparable domains of the SRS-22r (function, mental health, self-image, pain). The Pearson’s rho correlation coefficient varied between 0.41 (CI 0.21–0.58) for the BrQ domain “physical functioning” and 0.64 (CI 0.49–0.75) for the BrQ domain “bodily pain.”
Table 4.
Concurrent validity of the BrQ domains in relation to comparable SRS-22r domains
| BrQ domains | SRS-22r domains | Pearson’s rho (CI) | P value |
|---|---|---|---|
| Physical functioning | Function | 0.41 (0.21–0.58) | < 0.001 |
| Emotional functioning | Mental health | 0.63 (0.47–0.75) | < 0.001 |
| Self-esteem and aesthetics | Self-image | 0.51 (0.32–0.65) | < 0.001 |
| Bodily pain | Pain | 0.64 (0.49–0.75) | < 0.001 |
| Total score | Total score | 0.79 (0.69–0.86) |
Discussion
The aim of this study was to translate and culturally adapt the original Greek BrQ into the Dutch language and to evaluate the validity and reliability of this Dutch version. The BrQ was successfully translated and adapted, and the Dutch version of the BrQ showed no floor and ceiling effects for the total BrQ score, excellent test–retest reproducibility, and satisfactory internal consistency in most subdomains. Also, moderate-to-good concurrent validity was found for the BrQ domains “emotional functioning,” “self-esteem and aesthetics,” and “bodily pain.” The mean total BrQ score for this Dutch study population was 75.9 (SD 11.3), which is comparable to population groups in other countries [8,11,14].
Generally, a minimum Cronbach’s α of 0.70 is recommended for satisfactory internal consistency of a scale [7,18]. Some researchers also compute the Cronbach’s α for the total scale (items of all domains), but as this scale will not be unidimensional, this approach is less informative (the Cronbach’s α for the total BrQ in this study was 0.91 [CI 0.88–0.94]). The Cronbach’s α scores of the 8 subdomains in the present study varied (0.35–0.89) and were slightly lower than in most other BrQ validation studies [7,11-13]. The Cronbach’s α is impacted by the number of items. Therefore, a lower α coefficient may be expected with only 3 or fewer items, which could explain the relatively low Cronbach’s α of 0.35 (CI –0.02 to 0.58) for the domain “general health perception,” which consists of 2 questions, and the Cronbach’s α of 0.59 (CI 0.40–0.72) for the domain “school activity,” which consists of 3 questions. The relatively low Cronbach’s α of 0.55 (CI 0.38–0.69) for the domain “physical functioning” was more remarkable as the domain consists of 7 questions. Using the “Cronbach’s α if item deleted” procedure, the exclusion of item 5 (“you managed to wear the brace without any help”) improved the Cronbach α to 0.67. Age seemed to influence the score for this item as the mean score of item 5 was 3.9 (SD 1.6) for patients aged 15 or older, and 3.3 (SD 1.8) for patients aged 14 years or younger, but the difference was not significant (P 0.06, one-sided). Besides age, brace type and length of brace wear are also factors that could influence the score of item 5, and could be possible explanations for the improvement in internal consistency if this item were deleted. Further sub-analyses concerning this matter fell outside the scope of this study and were therefore not conducted.
The ceiling effect percentages per domain in the present study were slightly higher compared with most other BrQ validating studies in literature, but did not exceed 15% [7,9,11,12,14]. For the overall BrQ score, no floor or ceiling effects were observed. Although the average time between the first and second measurement was relatively long (28 days, SD 17), the test–retest reproducibility was excellent for the overall BrQ score (ICC 0.91), which was also comparable with the literature [10,12-14].
Clinical implications
As the generally low compliance rates during brace treatment of AIS remain a challenge for healthcare professionals, further knowledge regarding the impact of brace wear and the effect of new brace modifications or brace-related interventions on different HRQOL domains could lead to new insights for better brace compliance. The SRS-22r assesses the overall HRQOL of AIS patients but does not contain a specific item on the influence of brace therapy on HRQOL. The results of this study prove that the BrQ can be used reliably in the Dutch population group. Overall, the BrQ and SRS-22r questionnaires showed comparable floor and ceiling effects, internal consistency, and reproducibility between the 2 questionnaires. However, the BrQ contains specific items on the influence of the brace treatment on HRQOL. This might help to provide better insight into the impact of bracing during clinical monitoring of patients.
It is important to identify those patients undergoing active brace treatment who are scoring below the norm, in order to provide additional brace adjustments, extra monitoring, and proper support of the physician, the parents, and/or a psychologist in the form of individual sessions or group sessions [21].
Limitations
First, the number of patients included in this study (80 patients) was considered large enough for the validity and reliability assessment, as in previous studies [8-15], but not large enough to test the discriminative ability of the BrQ. To explore the discriminative ability, it might be better to use the BrQ at biannual time intervals during the whole bracing period in multi-center, long-term longitudinal follow-up studies, instead of adding more patients, as the impact of brace wear for the individual AIS patient can change over time. Second, 99% of the patients wore a Boston brace. Different types of braces could have a different effect on HRQOL scores. Third, the questionnaire is limited in that a significant number of the BrQ questions relate to daytime brace wear. This questionnaire might therefore be less useful for patients wearing nighttime braces.
Conclusion
The translated and culturally adapted Dutch version of the BrQ proved to be a valid and reliable HRQOL measuring instrument for AIS patients undergoing brace treatment. Therefore, this instrument is considered useful as a clinical evaluation tool for both clinical and research purposes for the Dutch AIS group during brace treatment.
Supplementary data
The Dutch Brace Questionnaire is available as Supplementary data on the article page, doi: 10.2340/17453674.2023.18492
Supplementary Material
All authors have made direct contributions to the intellectual content of the paper and have approved the final version of the paper.
The authors would like to thank the 4 Greek translators (G F Giannakópoulos, E Massali, I Agathou, and M de Haas) for their help during the Brace Questionnaire translation process.
Handling co-editors: Ilkka Helenius and Philippe Wagner
Acta thanks Thomas Andersen, Ivar Rossvoll, and Hans Tropp for help with peer review of this manuscript.
References
- 1.Weinstein S L, Dolan L A, Wright J G, Dobbs M B. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013; 369: 1512-21. doi: 10.1056/NEJMoa1307337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katz D E, Herring J A, Browne R H, Kelly D M, Birch J G. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 2010; 92: 1343-52. doi: 10.2106/JBJS.I.01142. [DOI] [PubMed] [Google Scholar]
- 3.Karol L A, Virostek D, Felton K, Wheeler L. Effect of compliance counseling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg 2016; Am 98: 9-14. doi: 10.2106/JBJS.O.00359. [DOI] [PubMed] [Google Scholar]
- 4.Sanders J O, Newton P O, Browne R H, Katz D E, Birch J G, Herring J A. Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am 2014; 96: 649-53. doi: 10.2106/JBJS.M.00290. [DOI] [PubMed] [Google Scholar]
- 5.Wang H, Tetteroo D, Arts J J C, Markopoulos P, Ito K. Quality of life of adolescent idiopathic scoliosis patients under brace treatment: a brief communication of literature review. Qual Life Res 2021; 30: 703-11. doi: 10.1007/s11136-020-02671-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schlosser T P, Stadhouder A, Schimmel J J, Lehr A M, van der Heijden G J, Castelein R M. Reliability and validity of the adapted Dutch version of the revised Scoliosis Research Society 22-item questionnaire. Spine J 2014; 14 :1663-72. doi: 10.1016/j.spinee.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 7.Vasiliadis E, Grivas T B, Gkoltsiou K. Development and preliminary validation of Brace Questionnaire (BrQ): a new instrument for measuring quality of life of brace treated scoliotics. Scoliosis 2006; 1: 7. doi: 10.1186/1748-7161-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aulisa A G, Guzzanti V, Galli M, Erra C, Scudieri G, Padua L. Validation of Italian version of Brace Questionnaire (BrQ). Scoliosis 2013; 8: 13. doi: 10.1186/1748-7161-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deceuninck J, Tirat-Herbert A, Rodriguez Martinez N, Bernard J C. French validation of the Brace Questionnaire (BrQ). Scoliosis Spinal Disord 2017; 12: 18. doi: 10.1186/s13013-017-0126-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gur G, Yakut Y, Grivas T. The Turkish version of the Brace Questionnaire in brace-treated adolescents with idiopathic scoliosis. Prosthet Orthot Int 2018; 42: 129-35. doi: 10.1177/0309364617690393. [DOI] [PubMed] [Google Scholar]
- 11.Kinel E, Kotwicki T, Podolska A, Bialek M, Stryla W. Polish validation of Brace Questionnaire. Eur Spine J 2012; 21:1603-1608. doi: 10.1007/s00586-012-2188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim J M, Goh T S, Shin J K, Kim D S, Lee C S, Lee J S. Validation of the Korean version of the Brace Questionnaire. Br J Neurosurg 2018; 32: 678-81. doi: 10.1080/02688697.2018.1501464. [DOI] [PubMed] [Google Scholar]
- 13.Rezaee S, Jalali M, Babaee T, Kamali M. Reliability and concurrent validity of a culturally adapted Persian version of the Brace Questionnaire in adolescents with idiopathic scoliosis. Spine Deform 2019; 7: 553-8. doi: 10.1016/j.jspd.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Yi H, Chen H, Wang X, Xia H. Cross-cultural adaptation and validation of the Chinese version of the Brace Questionnaire. Front Pediatr 2021; 9: 763811. doi: 10.3389/fped.2021.763811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu S, Zhou G, Xu N, Mai S, Wang Q, Zeng L, et al. Translation and validation of the Chinese version of Brace Questionnaire (BrQ). Transl Pediatr 2021; 10: 598-603. doi: 10.21037/tp-20-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaton D E, Bombardier C, Guillemin F, Ferraz M B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000; 25: 3186-91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 17.Scoliosis Research Society outcomes ; 2013. Available from: http://www.srs.org/professionals/SRS_outcomes/
- 18.Bland J M, Altman D G. Cronbach’s alpha. BMJ 1997; 314: 572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koo T K, Li M Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016; 15: 155-63. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Portney L G, Watkins M P, editors. Statistical measures of reliability. In: Foundations of clinical research: applications to practice, 3rd ed. London: Pearson Education; 2009. Ch. 26. [Google Scholar]
- 21.Rivett L, Rothberg A, Stewart A, Berkowitz R. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathic scoliosis: a comparative study. BMC Musculoskelet Disord 2009; 10: 5. doi: 10.1186/1471-2474-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Risser J C. The iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop 1958; 11: 111-19. [PubMed] [Google Scholar]
- 23.Lenke L G, Betz R R, Harms J, Bridwell K H, Clements D H, Lowe T G, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001; 83: 1169-81. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


