Abstract
Background
In the Studies of Left Ventricular Dysfunction (SOLVD) Treatment trial, similar clinical benefits were observed between starting doses of enalapril and the target dose achieved by post-randomization up-titration. In our current analysis, protecting the randomization, we examined the early effects of starting doses of enalapril.
Methods
2569 patients with mild-to-moderate chronic heart failure with reduced ejection fraction (HFrEF; ejection fraction ≤35%) were randomized to receive starting doses (5–10 mg/day) of placebo (n=1284) or enalapril (n=1285). At day 14, both study drugs were blindly up-titrated to the target dose (20 mg/day). Overall, 89% (2284/2569) of the patients returned for dose up-titration, which was achieved in 56% (1444/2248), 48% (696/1444) of whom were in the enalapril group. Hazard ratios (HRs) and 95% confidence intervals (CIs) for outcomes in the enalapril group were estimated.
Results
HRs (95% CIs) for all-cause mortality, heart failure hospitalization, and the combined endpoint of heart failure hospitalization or all-cause mortality at 14 days after randomization were 0.80 (0.32–2.03), 0.63 (0.35–1.12), and 0.65 (0.39–1.06) 0.82, respectively. Corresponding HRs (95% CIs) at 30 days were (0.41–1.67), 0.43 (0.27–0.68), and 0.43 (0.27–0.68). The magnitude of these early effects of starting doses of enalapril is similar to its previously reported long-term effects at the target dose.
Conclusion
These data suggest that in stable ambulatory patients with heart failure with reduced ejection fraction, the magnitude of the early effect of starting doses of enalapril is similar to that observed during longer-term therapy with the target doses of the drug.
Keywords: Angiotensin-converting enzyme inhibitors, starting dose, enalapril, heart failure
Introduction
Angiotensin-converting enzyme inhibitors significantly improve clinical outcomes in patients with heart failure with reduced ejection fraction (HFrEF).1,2 These drugs are recommended for patients with HFrEF unless contraindicated and clinicians are encouraged to initiate angiotensin-converting enzyme inhibitors at a low starting dose and up-titrate them to higher target doses used in major randomized controlled trials.3,4 The predetermined daily target dose of enalapril in the Studies of Left Ventricular Dysfunction (SOLVD) Treatment trials was 20 mg/day, divided into equal twice daily doses.2 In the SOVLD Treatment trial, patients were randomized to receive either placebo or enalapril at the starting doses of 5–10 mg/day, with the intent of a blinded up-titration to the target dose of 20 mg/day at 14 days after randomization.2 Findings from a post hoc analysis of data from the SOLVD Treatment trial suggest similar clinical benefits from starting and target doses of enalapril.5 However, a key limitation of that post hoc analysis was that the up-titration to target dose was a post-randomization event.6 In the current analysis, we preserved the protection of randomization and examined the effects of enalapril on short-term outcomes in patients receiving starting doses of the drug.
Methods
Data Source and Study Population
The SOLVD Treatment trial was sponsored by the National Heart, Lung and Blood Institute and public-use copies of SOLVD data used for the current analysis were obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center.5 The details of the design, methods and results of the SOLVD trial have been reported previously.2 In brief, SOLVD Treatment was a double-blind placebo-controlled randomized controlled trial of 2569 ambulatory patients with mild to moderate chronic heart failure with ejection fraction ≤35%.2
Randomization and Dose Titration after Randomization
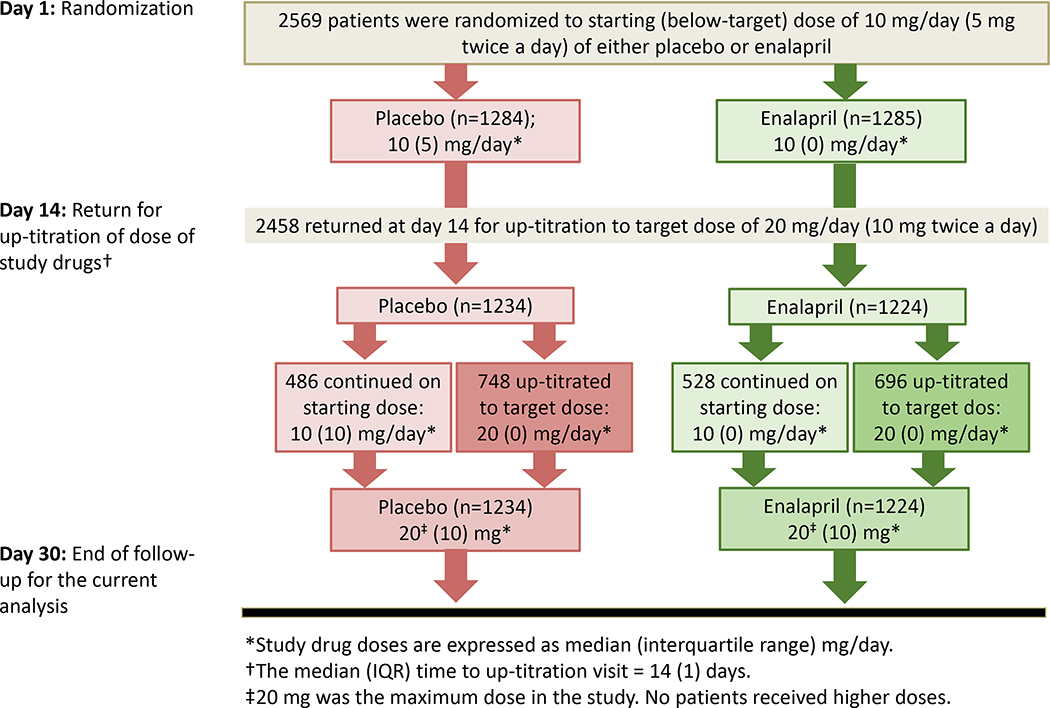
Patients who tolerated a pre-randomization stabilization phase with single-blinded enalapril of 5 mg/day for a week were randomized to receive either placebo (n=1284) or enalapril (n=1285) in starting doses of 5–10 mg/day, taken as equal twice daily doses. Patients were instructed to return 14 days after randomization for a protocol-driven blinded up-titration of both study drugs to the higher target dose of 20 mg/day. Overall, 2532 (99%) patients returned for dose up-titration and 1444 (56%) received the target dose, of whom 748 belonged to the placebo group and 696 to the enalapril group (Figure 1).
Figure 1.
Flow chart displaying the dose up-titration process in patients with heart failure with reduced ejection fraction randomized to receive enalapril or placebo in the SOLVD Treatment trial
Outcomes
The primary outcomes of interest for the current analysis were all-cause mortality, heart failure hospitalizations, and the combined endpoint of heart failure hospitalization or all-cause mortality at 14 days post-randomization when all patients were receiving starting doses (5–10 mg/day) of the study drugs. We also examined these outcomes at 30 days when over half of the patients were receiving the target (20 mg/day) dose of enalapril during days 15 to 30.
Statistical Analyses
We conducted Kaplan Meier survival analysis to plot the combined endpoint at 30 days by the two treatment groups. Using Cox proportional hazard models, we then estimated hazard ratios (HR) and 95% confidence intervals (CI) for outcomes associated with enalapril use for all patients using an intent-to-treat approach. To determine whether the early effects of enalapril were homogenous across clinically relevant subgroups of patients, we conducted subgroup analyses for the combined endpoint of heart failure hospitalization or all-cause mortality at 30 days. We repeated the subgroup analyses for the combined endpoint at the study end of 4.6 (median, 2.9) years. All statistical tests were two-tailed with 95% confidence levels were considered significant. IBM SPSS Statistics for Windows, Version 25.0 (Armonk, NY: IBM Corp.) was used for all data analysis.
Results
Baseline Characteristics
As reported previously, patients in the placebo and enalapril groups had similar baseline characteristics (Table 1).2,5 The median (interquartile range) starting doses of placebo and enalapril were 10 (5) and 10 (0) mg/day. Respective target doses were 20 (10) and 20 (10) mg/day. The median time to up-titration visit was 14 days (interquartile range, 1 day).
Table 1.
Characteristics of patients with heart failure with reduced ejection fraction in the SOLVD Treatment trial, by randomization to enalapril versus placebo
| Placebo (n=1284) | Enalapril (n=1285) | P value | |
|---|---|---|---|
| Age (years) | 61 (10) | 60 (10) | 0.414 |
| Women | 259 (20%) | 245 (19%) | 0.481 |
| African American | 187 (15%) | 209 (16%) | 0.233 |
| Prior myocardial infarction | 835 (50%) | 852 (51%) | 0.497 |
| Hypertension | 534 (42%) | 551 (43%) | 0.508 |
| NYHA class III-IV | 403 (31%) | 423 (33%) | 0.406 |
| Ejection fraction (%) | 25 (7) | 25 (7) | 0.656 |
| Systolic blood pressure (mm Hg) | 125 (18) | 125 (18) | 0.926 |
| Serum creatinine (mg/dL) | 1.2 (0.3) | 1.2 (0.3) | 0.323 |
| Starting dose (mg/day) | 8.7 (2.5) | 8.9 (2.5) | 0.138 |
| Starting dose duration (days) | 15.4 (4.4) | 15.3 (3.7) | 0.693 |
| Target dose (mg/day) | 15.3 (5.8) | 14.8 (5.8) | 0.048 |
Effect of Starting Dose of Enalapril on Early Outcomes
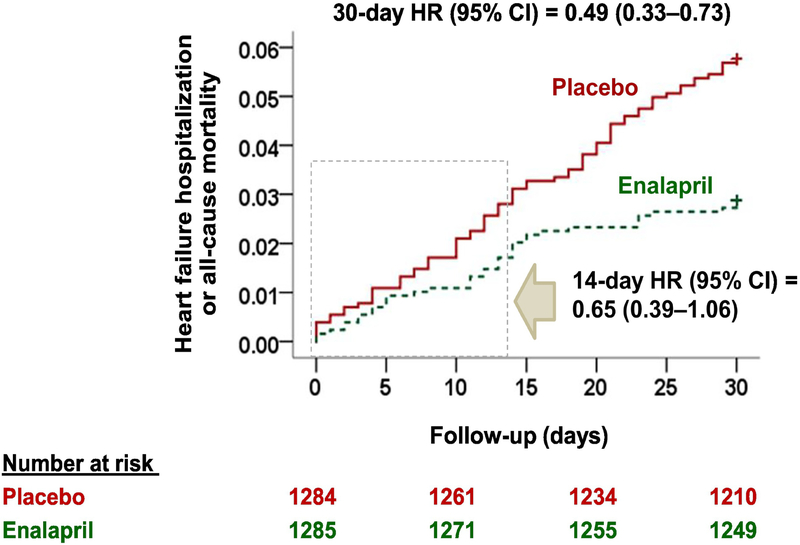
During 14 days after randomization when all patients were receiving starting doses (5–10 mg/day) of the study drugs, HRs (95% CIs) for all-cause mortality, heart failure hospitalization, and the combined endpoint of heart failure hospitalization or all-cause mortality, when enalapril was compared with placebo, were 0.80 (0.32–2.03), 0.63 (0.35–1.12), and 0.65 (0.39–1.06), respectively (Table 2 and Figure 2). Corresponding HRs (95% CIs) at 30 days after randomization were (0.41–1.67), 0.43 (0.27–0.68), and 0.43 (0.27–0.68), respectively (Table 2 and Figure 2).
Table 2.
Outcomes with use of enalapril in patients with heart failure with reduced ejection fraction in the SOLVD Treatment trial
| Placebo (n=1284) | Enalapril (n=1285) | Hazard ratio (95% confidence interval) | |
|---|---|---|---|
| All-cause mortality | |||
| 14 days | 10 (0.8%) | 8 (0.6%) | 0.80 (0.32–2.03) |
| 30 days | 17 (1.3%) | 14 (1.1%) | 0.82 (0.41–1.67) |
| 4.6 years (overall) | 510 (39.7%) | 451 (35.1%) | 0.84 (0.74–0.96) |
| Heart failure hospitalization | |||
| 14 days | 30 (2.3%) | 19 (1.5%) | 0.63 (0.35–1.12) |
| 30 days | 58 (4.5%) | 25 (1.9%) | 0.43 (0.27–0.68) |
| 4.6 years (overall) | 469 (36.5%) | 337 (26.2%) | 0.65 (0.55–0.73) |
| Heart failure hospitalization or all-cause mortality | |||
| 14 days | 40 (3.1%) | 26 (2.0%) | 0.65 (0.39–1.06) |
| 30 days | 74 (5.8%) | 37 (2.9%) | 0.49 (0.33–0.73) |
| 4.6 years (overall) | 736 (57.3%) | 614 (47.8%) | 0.74 (0.66–0.82) |
Figure 2.
Kaplan-Meier survival plots for the combined endpoint of heart failure hospitalization or all-cause mortality at 30 days by enalapril versus placebo in the Studies of Left Ventricular Dysfunction (SOLVD) Treatment trial (HR = hazard ratio; CI = confidence interval)
Similarities Between Early and Long-Term Effects
As previously reported,2 during 4.6 (median, 2.9) years of follow-up, HRs (95% CIs) for all-cause mortality, heart failure hospitalization, and the combined endpoint of heart failure hospitalization or all-cause mortality, when enalapril was compared with placebo, were 0.84 (0.74–0.96), 0.65 (0.55–0.73), and 0.74 (0.66–0.82), respectively (Table 2). The magnitude of these benefits are similar to those observed at 14 and 30 days after randomization (Table 2).
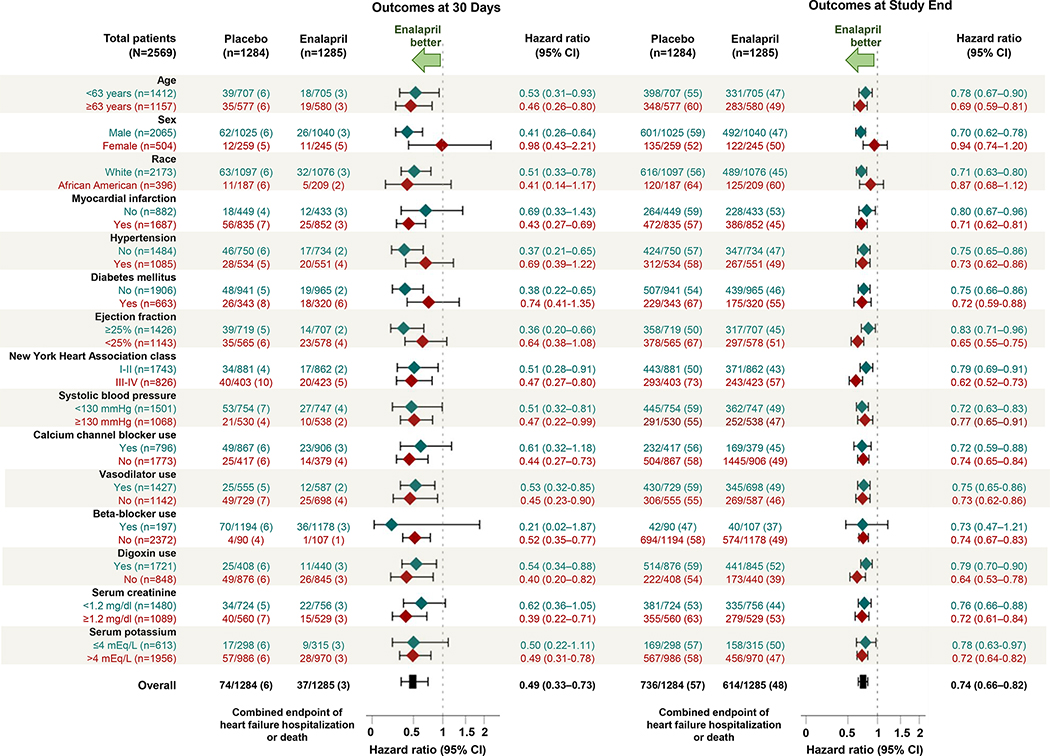
Effect of Starting Dose of Enalapril in Subgroups
The effects of the starting dose of enalapril on the combined endpoint of heart failure hospitalization or all-cause mortality at 30 days were generally similar across most clinically relevant subgroups of patients (Figure 3). These subgroup effects were similar during the entire follow-up of 4.6 years (median, 2.9 years) of the SOLVD trial (Figure 3).
Figure 3.
Forest plots displaying hazard ratios and 95% confidence intervals (CI) for the combined endpoint of heart failure hospitalization or all-cause mortality at 30 days and during the overall follow-up of 4.6 years, between enalapril versus placebo, in subgroups of patients enrolled in the Studies of Left Ventricular Dysfunction (SOLVD) Treatment trial
Discussion
Findings from this post hoc analysis of the SOLVD Treatment trial demonstrate that the magnitudes of early benefit of the starting doses of enalapril (5 mg twice daily) were similar to the long-term benefit of target dose (10 mg twice daily) of the drug observed during the entire follow-up of the trial. We also observed that these early effects were rather homogenous across several clinically relevant subgroups of patients, and these effects in subgroups were similar to those seen during longer-term follow-up. Although most of the early effects were not significant due to lack of adequate power due to the sparse number of events, similarities in the directions and magnitudes of their effect suggest that the clinical benefit of enalapril occurs early when most patients were on a 10 mg daily dose. Although previous studies have reported early benefits of starting doses of other heart failure drugs,7–9 to the best of our knowledge, this is the first report of an early benefit of starting doses of an angiotensin-converting enzyme inhibitor in patients with heart failure.
The early clinical benefit in the enalapril group may in part be explained by the early neurohormonal suppression that occurs after initiation of therapy with angiotensin-converting enzyme inhibitors.10,11 In patients with acute myocardial infarction, angiotensin-converting enzyme inhibitors have been shown to decrease left ventricular diastolic and systolic volume and prevent infarct expansion.12–15 These early effects of angiotensin-converting enzyme inhibitors on left ventricular remodeling, however, were observed in studies that used target doses similar to those used in the SOLVD trial.2 Findings from our analyses suggest that enalapril, when started at a 5 mg twice daily dose, may also improve clinical outcomes. Clinical effectiveness of angiotensin-converting enzyme inhibitors in lowering the risk of 30-day mortality and heart failure readmission in observational studies 16 may also be attributed to below-target doses as most patients with HFrEF in the real world often do not receive target dose of the drug.17–19 Findings from our prior post hoc analysis of the SOLVD Treatment trial suggest that the long-term clinical benefit of enalapril was similar among patients who were continued on the starting dose of 5 mg twice daily as well as whose dose could be up-titrated the target dose of 10 mg twice daily.5 Taken together, these findings suggest efficacy and clinical effectiveness of angiotensin-converting enzyme inhibitors at a daily dose of 10 mg/day (5 mg twice daily), which is below the target dose used in randomized controlled trials and recommended by national heart failure guidelines.
Early clinical benefit at starting doses of a drug in patients with heart failure is not unique to angiotensin-converting enzyme inhibitors. In the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) study, patients with heart failure and ejection fraction <25% were randomized to receive either carvedilol or placebo at daily starting doses of 6.25 mg for 2 weeks, 12.5 mg for 4 weeks, 25 mg for 6 weeks, and finally at the target dose of 50 mg – all given in two equally divided doses.20 In that study, patients in the carvedilol group had a significant 35% lower risk of death during nearly 2 years of follow-up. Findings from a post hoc analysis of the COPERNICUS trial demonstrated that the early effect of the starting below-target doses of carvedilol was similar to its long-term effect on target dose.7 Similarly, in the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) trial, patients with acute myocardial infarction, heart failure and ejection fraction ≤40% were randomized to receive either eplerenone or placebo, starting at 25 mg daily for 4 weeks and increasing to a target dose of 50 mg daily.21 In that trial, patients in the eplerenone group had a significant 15% lower risk of death during nearly 3 years of follow-up. Findings from a post hoc analysis of the EPHESUS trial demonstrated that the early effect of below-target dose of eplerenone was similar to its long-term effect on target dose.8
The benefit of a lower dose of heart failure drug is also observed when the dose is reduced from an initial high dose. In the Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial, patients were randomized to high starting doses of the study drugs, which could be lowered during follow-up if patients could not tolerate the high doses.22 In that trial, patients with heart failure and ejection fraction ≤40% were randomly assigned to receive high starting doses of either enalapril (10 mg twice daily) or sacubitril/valsartan (200 mg twice daily; 160 mg as valsartan), an angiotensin receptor neprilysin inhibitor. Patients in the angiotensin receptor neprilysin inhibitor group had a significant 20% lower risk of the primary composite outcome of heart failure hospitalization or cardiovascular death during nearly 3.5 years of follow-up. Findings from a post hoc analysis of the PARADIGM-HF trial demonstrated that the dose reduction occurred in 43% and 42% of the patients in the enalapril and ARNI groups, respectively, and that the treatment benefit of angiotensin receptor neprilysin inhibitor in these patients (a 20% reduction) was similar to those who continued the high dose (a 21% reduction).23
Findings of our study have important clinical implications. If the clinical benefits of enalapril are seen within 14 days when all patients were receiving the starting dose (5 mg twice daily) or within 30 days when half of the patients were receiving the target dose (10 mg twice daily) during the last 2 weeks as demonstrated in the current study, and if the clinical benefit of enalapril is similar at both 5 and 10 mg twice daily doses,2,5 is it necessary to titrate angiotensin-converting enzyme inhibitors or angiotensin receptor blockers to target doses? The effects of high vs. low doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers on outcomes in heart failure have been examined in two major prospective randomized clinical trials: the Assessment of Treatment with Lisinopril and Survival (ATLAS) and the Heart Failure Endpoint Evaluation of Angiotensin II Antagonist Losartan (HEAAL) trials.24,25 In the ATLAS trial, 3164 patients with HFrEF (ejection fraction ≤30%) were randomly assigned to low-dose (2 to 5 mg daily) vs. high-dose (32.5 to 35 mg daily) lisinopril, an angiotensin-converting enzyme inhibitor, and were followed for over 4 years. High-dose lisinopril reduced the risk of the combined endpoint of heart failure hospitalization or all-cause mortality (HR, 0.85; 95% CI, 0.78–0.93; p<0.001), but had no effect on the primary endpoint of all-cause mortality (HR, 0.92; 95% CI, 0.82–1.03; p=0.128).24 In the HEAAL trial, 3846 patients with HFrEF (ejection fraction ≤40%) and intolerance to angiotensin-converting enzyme inhibitors were randomly assigned to low-dose (50 mg daily) vs. high-dose (150 mg daily) losartan, an angiotensin receptor blocker, and were followed for over 5 years. High-dose losartan reduced the risk of the primary endpoint of heart failure hospitalization or all-cause mortality (HR, 0.90; 95% CI, 0.82–0.99; p=0.027).25 This was driven by a modest reduction in the risk of heart failure hospitalizations, which occurred in 26% and 23% of patients in the low-dose and high-dose groups, respectively – a 3% absolute risk reduction over 5 years (HR, 0.87; 95% CI, 0.76–0.98; p=0.025).25 As in the ATLAS trial, high doses of losartan in the HEAAL trial had no effect on mortality (HR, 0.94; 95% CI, 0.84–1.04; p=0.124).25 Furthermore, the exceptionally high doses used in these trials are seldom used in clinical practice.
Cumulative evidence now indicate that in trials where patients were typically receiving sub-target doses of inhibitors of the renin-angiotensin system at the time of enrollment, the addition of beta-blockers and mineralocorticoid receptor antagonists and replacement of an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker with an angiotensin receptor neprilysin inhibitor provided a more meaningful survival benefit than up-titration of an inhibitor of the renin-angiotensin system.26,27 Patients with HFrEF are more likely to tolerate angiotensin-converting enzyme inhibitors or angiotensin receptor blockers at below-target doses,24,25 and the current analysis suggests that these doses provide meaningful clinical benefits. Therefore, the implementation of a strategy of broad-based neurohormonal antagonism should not be delayed because of efforts to first achieve target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.
There are several limitations to our study. This is a post-hoc analysis and was not powered to identify significant treatment effect during early follow-up. Thus, instead of significance of short-term effects, we focused on the similarities in the magnitude of short- and long-term effects. The effect of enalapril on 30-day outcomes may not be totally attributed to the starting doses (5 mg twice daily) as over half of the patients were receiving target doses (10 mg twice daily). However, most patients were receiving below-target doses during the first 30 days as nearly half of the patients were on below-target dose for the entire 30 days and half were on below-target dose for the first 14 days. Furthermore, the magnitude of the risk reduction during the first 30 days was generally similar to that observed during the first 14 days. The treatment of HFrEF has evolved substantially since the publication of the SOLVD Treatment trial data. Less than 10% of SOLVD participants were receiving beta-blockers and data on the use mineralocorticoid receptor antagonists were not collected.2 However, data from the SOLVD Treatment trial still serves as the primary evidence supporting a benefit of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with chronic heart failure.
Conclusions
Findings of our post hoc analyses of the SOLVD Treatment trial demonstrate that in stable ambulatory patients with HFrEF, the early clinical benefits of below-target dose enalapril is comparable to its long-term clinical benefits at target dose.
Clinical Significance.
In stable ambulatory patients with heart failure with reduced ejection fraction, the magnitude of the early effect of starting doses of enalapril is similar to that observed during longer-term therapy with the target doses of the drug.
Therefore, the implementation of a strategy of broad-based neurohormonal antagonism should not be delayed because of efforts to first achieve target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.
Acknowledgements and Disclaimer
The Studies of Left Ventricular Dysfunction (SOLVD) trial was conducted and supported by the NHLBI in collaboration with the CHS Investigators. This manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the SOLVD or the NHLBI. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Veterans Health Administration. The authors wish to thank Gauravpal S. Gill, MD for his help in the preparation of part of Figure 2.
Funding: Dr. Ali Ahmed was in part supported by the National Institutes of Health through grants (R01-HL085561, R01-HL085561-S and R01-HL097047) from the National Heart, Lung, and Blood Institute.
Footnotes
Conflict of interest and Disclosures: Dr. Fonarow reports consulting with Abbott, Amgen, Bayer, Janssen, Novartis, and Medtronic. He serves as an Associate Editor of JAMA Cardiology. None of the other authors report any conflicts of interest related to this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987;316(23):1429–1435. [DOI] [PubMed] [Google Scholar]
- 2.The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293–302. [DOI] [PubMed] [Google Scholar]
- 3.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776–803. [DOI] [PubMed] [Google Scholar]
- 4.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. [DOI] [PubMed] [Google Scholar]
- 5.Lam PH, Dooley DJ, Fonarow GC, et al. Similar clinical benefits from below-target and target dose enalapril in patients with heart failure in the SOLVD Treatment trial. Eur J Heart Fail. 2018;20(2):359–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Packer M Inferential characterization of the dose-response relationships of neurohormonal antagonists in chronic heart failure: A novel approach based on large-scale trials with active comparators. Int J Cardiol. 2018;261:130–133. [DOI] [PubMed] [Google Scholar]
- 7.Krum H, Roecker EB, Mohacsi P, et al. Effects of initiating carvedilol in patients with severe chronic heart failure: results from the COPERNICUS Study. JAMA. 2003;289(6):712–718. [DOI] [PubMed] [Google Scholar]
- 8.Pitt B, White H, Nicolau J, et al. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46(3):425–431. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Lukas MA, Robertson M, Colucci WS, Dargie HJ. Effects of carvedilol early after myocardial infarction: analysis of the first 30 days in Carvedilol Post-Infarct Survival Control in Left Ventricular Dysfunction (CAPRICORN). Am Heart J. 2007;154(4):637–644. [DOI] [PubMed] [Google Scholar]
- 10.Reams GP, Lal SM, Whalen JJ, Bauer JH. Enalaprilat: an intravenous substitute for oral enalapril therapy. Humoral and pharmacokinetic effects. J Clin Hypertens. 1986;2(3):245–253. [PubMed] [Google Scholar]
- 11.Remme WJ. Effect of ACE inhibition on neurohormones. Eur Heart J. 1998;19 Suppl J:J16–23. [PubMed] [Google Scholar]
- 12.Sigurdsson A, Held P, Swedberg K, Wall B. Neurohormonal effects of early treatment with enalapril after acute myocardial infarction and the impact on left ventricular remodelling. Eur Heart J. 1993;14(8):1110–1117. [DOI] [PubMed] [Google Scholar]
- 13.Schulman SP, Weiss JL, Becker LC, et al. Effect of early enalapril therapy on left ventricular function and structure in acute myocardial infarction. Am J Cardiol. 1995;76(11):764–770. [DOI] [PubMed] [Google Scholar]
- 14.Foster RE, Johnson DB, Barilla F, et al. Changes in left ventricular mass and volumes in patients receiving angiotensin-converting enzyme inhibitor therapy for left ventricular dysfunction after Q-wave myocardial infarction. Am Heart J. 1998;136(2):269–275. [DOI] [PubMed] [Google Scholar]
- 15.Bazzino O, Navarro Estrada JL, Sosa Liprandi A, et al. Early treatment with low-dose enalapril after acute myocardial infarction: an equilibrium radionuclide angiographic study. Enalapril despues del Infarto (EDI) Trial Investigators. J Nucl Cardiol. 1997;4(2 Pt 1):133–139. [DOI] [PubMed] [Google Scholar]
- 16.Sanam K, Bhatia V, Bajaj NS, et al. Renin-Angiotensin System Inhibition and Lower 30-Day All-Cause Readmission in Medicare Beneficiaries with Heart Failure. Am J Med. 2016;129(10):1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gheorghiade M, Albert NM, Curtis AB, et al. Medication dosing in outpatients with heart failure after implementation of a practice-based performance improvement intervention: findings from IMPROVE HF. Congest Heart Fail. 2012;18(1):9–17. [DOI] [PubMed] [Google Scholar]
- 18.Barywani SB, Ergatoudes C, Schaufelberger M, Petzold M, Fu ML. Does the target dose of neurohormonal blockade matter for outcome in Systolic heart failure in octogenarians? Int J Cardiol. 2015;187:666–672. [DOI] [PubMed] [Google Scholar]
- 19.de Groote P, Isnard R, Assyag P, et al. Is the gap between guidelines and clinical practice in heart failure treatment being filled? Insights from the IMPACT RECO survey. Eur J Heart Fail. 2007;9(12):1205–1211. [DOI] [PubMed] [Google Scholar]
- 20.Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344(22):1651–1658. [DOI] [PubMed] [Google Scholar]
- 21.Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348(14):1309–1321. [DOI] [PubMed] [Google Scholar]
- 22.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004. [DOI] [PubMed] [Google Scholar]
- 23.Vardeny O, Claggett B, Packer M, et al. Efficacy of sacubitril/valsartan vs. enalapril at lower than target doses in heart failure with reduced ejection fraction: the PARADIGM-HF trial. Eur J Heart Fail. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Packer M, Poole-Wilson PA, Armstrong PW, et al. Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation. 1999;100(23):2312–2318. [DOI] [PubMed] [Google Scholar]
- 25.Konstam MA, Neaton JD, Dickstein K, et al. Effects of high-dose versus low-dose losartan on clinical outcomes in patients with heart failure (HEAAL study): a randomised, double-blind trial. Lancet. 2009;374(9704):1840–1848. [DOI] [PubMed] [Google Scholar]
- 26.Packer M Love of Angiotensin-Converting Enzyme Inhibitors in the Time of Cholera. JACC Heart Fail. 2016;4(5):403–408. [DOI] [PubMed] [Google Scholar]
- 27.Packer M Kicking the tyres of a heart failure trial: physician response to the approval of sacubitril/valsartan in the USA. Eur J Heart Fail. 2016;18(10):1211–1219. [DOI] [PubMed] [Google Scholar]