Abstract
Objectives
The aim of this study was to clarify and compare the socioeconomic backgrounds of medical students with those of other health professions and non-health faculty students in an era of increasing inequity in Japanese society.
Design
This was a quantitative nationwide study. Data were collected by a cross-sectional web-based anonymous questionnaire.
Setting
Data from years 3 and 4 medical, health professions and non-health faculty students across Japan were collected in 2021.
Participants
Participants were 1991 students from medical schools, 224 from dental, 419 from pharmacy, 326 from nursing, 144 from other health professions and 207 from non-health faculties.
Results
The proportion of high-income families (>18 million yen: ca. US$140 000) among medical students was 25.6%, higher than that of pharmacy (8.7%) and nursing students (4.1%) (p<0.01). One-third of medical students had a physician parent, more common than in non-medical students (p<0.01). Students who only applied to public medical schools and a regional quota ‘Chiiki-waku’ students with scholarship had lower family income and physician parents compared with those who applied to private medical schools (p<0.01), but they still had higher physician parents compared with non-medical students (p<0.01). Logistic regression revealed that having a physician parent (p<0.01), aspiring to the present profession during elementary school (p<0.01) and private upper secondary school graduation (p<0.01) predicted the likelihood of studying medicine. There were regional differences of backgrounds among medical students, and 80% of medical students with urban backgrounds intended to work in urban localities after graduation.
Conclusions
This study provides evidence that medical students in Japan hail from urban and higher income classes and physicians’ families. This finding has implications for the health workforce maldistribution in Japan. Widening the diversity of medical students is essential for solving physician workforce issues and meeting broad healthcare needs.
Keywords: MEDICAL EDUCATION & TRAINING, SOCIAL MEDICINE, Human resource management
STRENGTHS AND LIMITATIONS OF THIS STUDY
Our study presents a comparative analysis of the socioeconomic backgrounds of Japanese medical and other health professions students, and students in non-health faculties via a voluntary-based anonymous self-report web survey.
Statistical analyses including logistic regression analysis of medical and non-medical students enabled us to examine the diversity of the healthcare workforce and factors related to medical school enrolment from a broader perspective.
Comparison of various subgroups of medical students including Chiiki-waku, a regional quota to nurture physicians in local communities, comparison of application patterns to medical schools and regional differences provide further information on the skewed socioeconomic backgrounds of medical students.
Our study is of students in one country and hence our findings may not be generalisable to other countries and cultural contexts.
Introduction
The purpose of medical student selection is to identify potential doctors, not based on socioeconomic status, gender or ethnicity, but rather on the applicant’s capabilities and attributes.1 However, many studies show that students from certain groups, mostly those from lower socioeconomic backgrounds, are under-represented in medical schools in many countries, including the UK,2 the USA,3 Canada4 and the Netherlands.5 In the UK, for example, applicants from less affluent backgrounds (eg, living in economically deprived areas with parents from lower socioeconomic classes), and those attending public secondary schools were less likely to be admitted to medical school.2 Here, as in many countries, the profession of medicine does not ‘reflect the society from which it is drawn and seeks to serve’.6–8 Similar issues are seen in the USA, where the small number of medical students from lower socioeconomic classes and the under-representation of Hispanic, African American and Native American doctors have been of concern since the 1960s.3 9–11 As per the UK and the USA, the Canadian Medical Students’ Association officially stated that ‘medical schools must improve admission policies to increasingly admit students with low socioeconomic status’ to meet the various needs of citizens.12
Most of the research on this topic comes from only a few countries. Indeed, most of the papers in Patterson et al’s1 review of medical school selection originated from the USA, the UK, Canada and Australia. In fact, only 9/194 studies were from countries outside Europe, North America or Oceania (5 from Asia and 3 from the Middle East). In other words, there is a clear gap in understanding as to the medical school selection processes and outcomes in most countries, and particularly in ‘non-western’ cultural spheres.
We focus on examining this gap in knowledge in Japan. There is a general perception of Japanese people and the medical community that medical students in Japan come from higher socioeconomic backgrounds and are not reflective of Japanese society as a whole. However, this premise is based on historical data. The precise situation has not been investigated since the 1970s when a report on parental occupation and secondary education identified that 33.7% of medical students were children of physicians, and private medical schools were more likely to accept children of physicians.13
Our driver for the study reported in this paper is linked to societal change: social disparity in Japan has increased in the last several decades, with the relative poverty rate being the seventh worst among the Organisation for Economic Co-operation and Development countries, indicating widening socioeconomic disparities in Japan today.14 Internationally, here is a strong pattern of medical students from more affluent backgrounds preferring to work in urban areas2–5 and there is a continued healthcare workforce shortage in rural areas in Japan in spite of various policies.15 Given this, we tentatively propose that today’s Japanese medical students will be even more socioeconomically privileged and homogeneous than previous generations.
Thus, the aim of this study was to identify the relationship between socioeconomic backgrounds (financial status and family education/occupation background) and course of study (primary and secondary education, application, admission, and intended future workplace) in Japanese medical and non-medical students. We also compared the socioeconomic backgrounds of ‘mainstream’ Japanese medical students and those admitted to medical school under the ‘Chiiki-waku’ regional quota scheme (see the Context section for further explanation). Our study is also unique in that we compared the backgrounds of medical students with those of various health professions students and non-health faculty students.
Methods
Context
Japan’s education system is as follows: compulsory elementary and lower secondary education for pupils aged 6–15 years (6 years of elementary school+3 years of lower secondary school), upper secondary education for students aged 15–18 years and higher education.16 17 Two-thirds of upper secondary (high) schools are public and almost tuition free, while the remaining schools are private with very high annual fees up to 1 million yen (ca. US$7700: US$1 in March 2023 is 130 yen). One-third of private secondary schools, that is, about 10% of total upper secondary school, have a 6-year integrated course (lower and upper secondary education) for students aged 12–18 years. This 6-year course provides special preparatory education for university entrance examinations. Private tutoring, also known as ‘cram schools’, is popular among school students and graduates seeking to improve their academic performance and pass university admission tests.18
Higher education health professions programmes include 6-year courses for medicine and dentistry, 6-year or 4-year courses for pharmacy, and 4-year or 3-year courses for nursing and occupational/physical therapy.19 Currently, there are 51 public and 31 private medical schools in Japan, with efforts being made to expand the number of schools and students and to reform medical education.15 20 Public medical schools conduct three annual admission tests on a common schedule, whereas private medical schools provide multiple opportunities of admission tests on their own dates. Tuition for public medical schools is about 500 000 yen (ca. US$3800) annually, whereas for private medical schools it is about 3–7 million yen (US$23 000–US$54 000) annually. Academic performance tests are heavily weighted in the medical school admission process, although the additional use of interviews and essay writing have now been partly introduced by many medical schools.
Japan has a well-documented and long-standing shortage of doctors in remote and rural communities and so ‘Chiiki-waku’, a regional quota, was introduced in 2008, mainly in public medical schools.21 Any applicants who have the intention to serve local communities can apply to this regional quota system, and Chiiki-waku students receive scholarships covering 6 years of tuition and living expenses. On completing their studies, their debt can be waived should they work in their designated regions/areas for approximately 10 years.
The national average and median of family income in Japan are 5.5 million (ca. US$42 000) and 4.4 million yen, respectively. The average income of families with child(ren) and hospital physicians is 7.5 million and 15 million yen, respectively. The percentage of family income over 18 million yen (ca. US$140 000) and 10–18 million yen are 1.7% and 10.4%, respectively. Average household size is 2.4 and over 80% of Japanese families are single or nuclear families consisting of parents and their children.22
Japan is usually divided into six regions from north to south: Hokkaido/Tohoku, Kanto/Tokyo, Chubu, Kansai/Osaka, Chugoku/Shikoku and Kyushu/Okinawa. Of those, Kanto/Tokyo and Kansai/Osaka are metropolitan areas. We used this geographical system in our study.
Data instrument
Data were collected in 2021 via a web-based anonymous questionnaire survey (SurveyMonkey by Momentive, San Mateo, California, USA) developed and administered by YS, YT and KT. The survey was designed via discussions with experts in medicine, education and survey methodology, checked with reference to the wider literature including the CHERRIES checklist.23 Its aim was to collect and collate self-reported data on student sociodemographics, educational experiences and future career aspirations. The questionnaire included items such as age, sex, family residence, degree programme, primary and secondary education, tutoring school experience, estimated annual family income, parental occupation/academic background, application to public/private universities and preferred future workplace (see online supplemental table).
bmjopen-2023-073559supp001.pdf (66.4KB, pdf)
Participants
We targeted third-year and fourth-year students across Japan’s various universities to obtain more responses on their accurate backgrounds and clearer future career intentions, considering maturation of students and closer relationship between these students and faculty members during the COVID-19 pandemic. Forty out of 82 medical schools (20 public and 20 private, total number of 3rd-year and 4th-year year students equals 9300), 8 of 17 dental schools (4 public and 4 private, 945 students), 5 of 29 pharmacy schools (2 public and 3 private, 2014 students), 22 of 75 nursing schools (16 public and 6 private, 3790 students), 5 other health professions schools including occupational/physical therapy, and 21 non-health faculties including education, liberal arts, science and technologies agreed to participate in this study. Most of these health professions schools and non-health faculties belong to the same university as medical school. These groups were selected to allow for comparison across programmes, from health professions students (medicine, dentistry, pharmacy, nursing, other health professions) and from non-health faculty students.
Data collection
In 2021, all the university faculties listed above were sent an invitation letter explaining the study’s purpose and details of ethical approval for data collection and analysis. Faculty members explained or emailed their student cohorts about the study and encouraged the students to participate voluntarily in the web questionnaire. When students opened the survey link, they were immediately presented with the information sheet including ethical considerations, and could decide whether to proceed or not after reading it. Informed consent was implied by checking a box on the questionnaire and questionnaire completion.
Data analysis
Annual family income distribution was analysed by Kruskal-Wallis test. Physician parent ratio, private upper secondary and elementary school graduation, aspiration to the present profession during elementary schools, and first-in-family (FiF) students whose parents did not have a degree of higher education24 were compared among medical and health professions students using χ2 test with Bonferroni correction. Logistic regression analysis was performed with the dependent variable ‘admission to medical school’ and explanatory variables including annual family income over 18 million yen, physician parent, private upper secondary school, aspiration to the present profession during elementary school and family residency in an area with a population size over 1 million. When we compared and analysed differences within the medical student population, we separated Chiiki-waku students from other subgroups such as private and public medical students. SPSS V.23.0 Japan for Windows (SPSS) was used to perform statistical test. Two-tailed p values of <0.05 were considered significant.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination of this research. Thus, patient consent for publication was not required.
Results
Respondents
Valid responses were obtained from 3311students out of 3598 respondents (92.0%): 1991 medical students (1022 public, 753 private and 216 Chiiki-waku; overall response rate 21.4%), 224 dental students (146 public and 78 private; response rate 23.7%), 419 pharmaceutical students (81 public and 338 private; response rate 20.8%), 326 nursing students (218 public and 108 private; response rate 8.6%), 144 other health professions students (78 public and 66 private, response rate 76.6%) and 207 students from education, liberal arts, sciences and technologies (201 public and 6 private, response rate 2.1%) (table 1).
Table 1.
Profiles of participants
| Medicine | Dentistry | Pharmacy | Nursing | Other health professions* | Non-health faculties† | |
| No of participants | 1991 | 224 | 419 | 326 | 144 | 207 |
| Age (mean) | 24.1 | 22.8 | 21.7 | 22.8 | 21.5 | 22.5 |
| Women (%) | 45 | 60.4 | 77.3 | 96.9 | 70.8 | 55.6 |
| Public university (%) | 55.7 | 65 | 19.3 | 66.9 | 54.2 | 97.1 |
| Family residency (%) | ||||||
| Hokkaido/Tohoku (10.9% of total population) | 6.8 | 4.4 | 3.3 | 14.7 | 33.3 | 13.5 |
| Kanto/Tokyo (34.6) | 31.5 | 28.9 | 56.3 | 20.9 | 45.1 | 25.6 |
| Chubu (18.2) | 18.5 | 19.6 | 23.1 | 14.4 | 3.5 | 36.2 |
| Kansai/Osaka (16.3) | 21.2 | 11.6 | 3.3 | 16.3 | 0.7 | 10.6 |
| Chugoku/Shikoku (8.7) | 10.2 | 12 | 5.3 | 11 | 6.3 | 11.1 |
| Kyushu/Okinawa (11.3) | 11.6 | 22.2 | 8.4 | 22.7 | 11.1 | 2 |
| Family residency >1 million population (%) | 27 | 20 | 32.2 | 12.3 | 20.8 | 12.1 |
| Annual family income | ||||||
| >18 million yen‡ (%) | 25.6 | 32.5 | 8.7 | 4.1 | 1.4 | 1.3 |
| >10 million yen | 56.5 | 68.8 | 37.2 | 23.9 | 12.5 | 24.8 |
| <3.5 million yen | 6.4 | 1.9 | 6.5 | 15.8 | 11.8 | 15.7 |
| First-in-family students (%) | 5.9 | 4.6 | 10 | 17.1 | 9.7 | 21.7 |
| Physician parent (%) | 33.2 | 13.8 | 8.8 | 4.3 | 4.2 | 2.4 |
| Dentist parent (%) | 2.7 | 39.7 | 1.7 | 0.9 | 0.7 | 1 |
| Private upper secondary (high) school (%) | 55.1 | 60.1 | 52.2 | 24.9 | 27.8 | 17.8 |
| 6-year integrated secondary (high) school (%) | 52 | 56.5 | 39.8 | 19.3 | 16 | 9.3 |
| Private elementary school (%) | 14.3 | 15.3 | 8.6 | 1 | 3.5 | 2.6 |
| Aspiration to the present profession during elementary school (%) | 16.8 | 5.8 | 7.6 | 5.8 | 0.7 | 0.5 |
| Tutoring school >3 days/week during elementary school (%) | 48.2 | 48.1 | 37.7 | 20.3 | 14.6 | 15.5 |
| Failure of university admission test (%)§ | 56.1 | 46.5 | 20 | 11.1 | 6.9 | 15.5 |
| Private tutoring programme for medical school admission (%)¶ | 50.5 | 46.2 | 21.1 | 15.6 | 10 | 3.4 |
*School of occupational/physical therapy and others.
†Schools for education, liberal arts, sciences and technologies.
‡ca. US$140 000.
§On graduation of secondary school.
¶For those who failed admission examination on graduation of secondary school, including dental and pharmacy school admission.
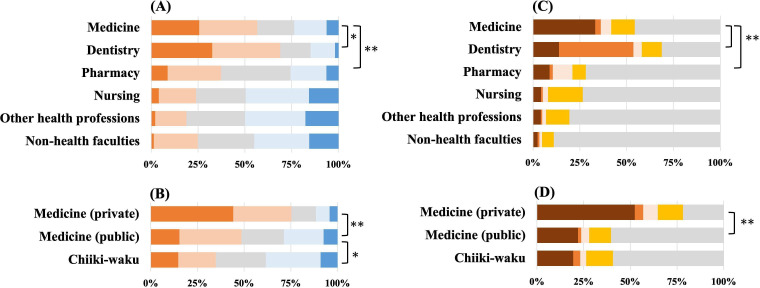
Family background of medical and health professions students
Figure 1A displays estimated annual family income of health professions students. Approximately 20% of students answered ‘do not know’ for this item and were therefore excluded. A χ2 test revealed that dental students had the highest percentage of annual family income over 18 million yen (ca. US$140 000), followed by medical, pharmacy and nursing students (figure 1A). Kruskal-Wallis test revealed that medical and dental students come from families with higher annual family income than pharmacy and nursing students (p<0.01). Among medical students, those in private medical schools came from the families with higher income, followed by public students, and then Chiiki-waku students (figure 1B).
Figure 1.
Family background of medical and health professions students. (A) Annual family income of medical and health professions students. (B) Annual family income of private, public and Chiiki-waku medical students.  ≧18 million yen (Ca. US$140 000)
≧18 million yen (Ca. US$140 000)  ≧10 million
≧10 million  ≧7 million
≧7 million  ≧3.5 million
≧3.5 million  <3.5 million. (C) Parent occupation (any one of or both) of medical and health professions students. (D) Parent occupation of private, public and Chiiki-waku medical students.
<3.5 million. (C) Parent occupation (any one of or both) of medical and health professions students. (D) Parent occupation of private, public and Chiiki-waku medical students.  Physician
Physician  dentist
dentist  pharmacist
pharmacist  nurse
nurse  others. *p<0.05 **p<0.01.
others. *p<0.05 **p<0.01.
Figure 1C displays parental occupations. Having a physician parent was most common in medical students (33.2%) as compared with dental, pharmacy, nursing and non-health faculty students (p<0.01). Forty per cent of dental, 11% of pharmacy and 19% of nursing students chose the same profession as their parents, which was a higher percentage as compared with other health professions students (p<0.01). More than half of private medical students had a physician parent, while 20% of public and Chiiki-waku students had a physician parent (p<0.01) (figure 1D). The percentage of physician parents in Chiiki-waku students was not different to that of public medical students, but higher than those of health professions and non-health faculty students (p<0.01).
Comparison of medical students with physician parent (n=661) and those with non-physician parent (n=1330) revealed that former group showed higher percentages of private medical school enrolment (63.5 vs 34.7%), annual family income over 18 million yen (42.4 vs 6.8%), graduation of the private upper secondary school (68.8 vs 46.4%) and elementary school (22.2 vs 9.0%), and private tutoring school over 3 days/week during elementary school (59.8 vs 37.7%) (p<0.01).
Primary and secondary education
Over 50% of the medical and dental students graduated from private secondary schools with a 6-year integrated course for ages 12–18 (table 1), that is, higher than in nursing students (p<0.01). About 80% of nursing and non-health faculty students graduated from public secondary schools with a regular 3-year course for ages 15–18. Medical and dental students also graduated from private elementary schools more frequently (p<0.01) (table 1). Furthermore, many medical and dental students attended private tutoring schools in the evening or on weekends since elementary school ages (table 1).
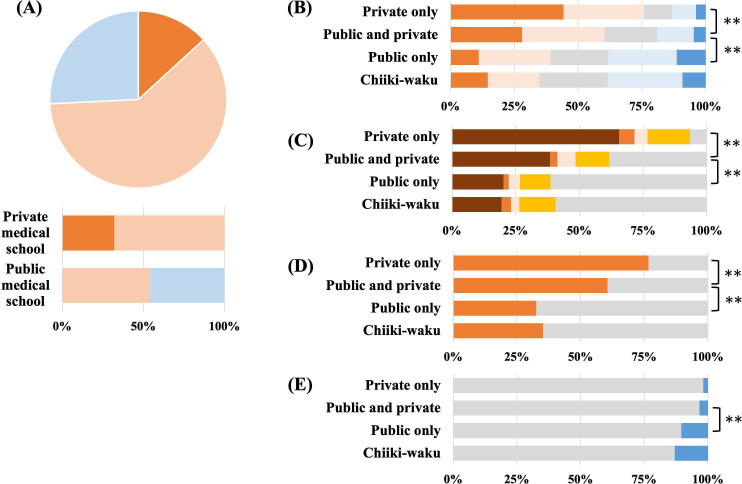
Application to medical schools
Among medical students, 25.8% of students applied only to public medical schools, 61.0% applied to both public and private schools, and 13.2% applied only to private schools (figure 2A). Overall, 74.2% of medical students applied to private medical schools. There were clear differences in family income, physician parent and type of secondary school among these subgroups. Students who applied only to public medical schools were from families with lower family income (p<0.01) (figure 2B), had non-physician parent (p<0.01) (figure 2C) and graduated from public upper secondary schools (p<0.01) (figure 2D) compared with the subgroups who applied to private or both private and public medical schools. Chiiki-waku students had similar socioeconomic backgrounds to those of students who applied only to public medical schools. FiF students24 were fewer in the group that applied to both private and public medical schools (p<0.01) (figure 2E). Thus, the backgrounds of students applying only to public medical schools and Chiiki-waku students were broader than those of students applying to private or both private and public medical schools, but still of a higher socioeconomic level than those of other health professions (except dental) and non-health faculty students: annual family income over 18 million yen (p<0.05) and proportion of physician parent (p<0.01).
Figure 2.
Application to medical schools and Chiiki-waku. (A) Application to medical school  private medical school only
private medical school only  private and public medical school
private and public medical school  public medical school only. (B) Annual family income of medical students who applied private medical school only, both public and private school, public medical school only, and Chiiki-waku.
public medical school only. (B) Annual family income of medical students who applied private medical school only, both public and private school, public medical school only, and Chiiki-waku.  ≥18 million yen (Ca. US$140 000)
≥18 million yen (Ca. US$140 000)  ≥10 million
≥10 million  ≥7 million
≥7 million  ≧3.5 million
≧3.5 million  <3.5 million. (C) Occupation of parent
<3.5 million. (C) Occupation of parent  physician
physician  dentist
dentist  pharmacist
pharmacist  nurse
nurse  others. (D) Upper secondary school
others. (D) Upper secondary school  private school
private school  public school. (E) Academic background of parents
public school. (E) Academic background of parents  higher education
higher education  secondary education (first-in-family). **p<0.01.
secondary education (first-in-family). **p<0.01.
Admission to health professions schools
A larger proportion of medical and dental students were rejected on graduation of upper secondary school than were nursing and non-health faculty students (table 1). Approximately half of medical and dental students who failed admission tests for their respective schools took a specialised and expensive private tutoring programme for admission into medical and dental schools (table 1).
Logistic regression analysis
Table 2 shows the results of logistic regression of variables that predict the likelihood of entering medical school, with the comparison of 1991 medical students and 1320 non-medical students. Students who were enrolled into medical school showed the following characteristics and significant p values: physician parent (p<0.01), private upper secondary school graduation (p<0.01) and aspiration to the present profession during elementary school (p<0.01). Annual family income over 18 million yen did not show significant difference (p=0.055), however, when we exclude dental students from the non-medical student group, the difference in annual family income of medical and other students was significant (p<0.01). Family residency in an area with a population size over 1 million was not significant.
Table 2.
Logistic regression analysis predicting the enrolment into medical school (forced entry method)
| Variables | β | SE | P value | OR | 95% CI |
| Annual family income >18 million yen* | 0.276 | 0.144 | 0.055 | 1.32 | 0.99 to 1.75 |
| Physician parent | 1.663 | 0.125 | <0.01 | 5.27 | 4.13 to 6.74 |
| Private upper secondary school | 0.376 | 0.084 | <0.01 | 1.46 | 1.24 to 1.72 |
| Aspiration to the present profession during elementary school | 1.247 | 0.146 | <0.01 | 3.48 | 2.61 to 4.64 |
| Family residency >1 million population | 0.136 | 0.097 | 0.163 | 1.15 | 0.95 to 1.39 |
*ca. US$140 000.
Regional differences of background in medical students
Regional differences in the backgrounds of medical students were analysed in relation to four indicators: annual family income over 10 million yen (ca. US$77 000), private upper secondary school graduation, applications only to public medical schools and local student ratio in public medical schools. As shown in figure 3A, the percentage of medical students from families with over 10 million yen annually in the metropolitan areas such as Kansai/Osaka (68.6%) and Kanto/Tokyo (61.7%) was higher than in the remote areas such as Kyushu/Okinawa (41.4%) and Hokkaido/Tohoku (44.3%) (p<0.01). The percentage of medical students who graduated from private secondary schools in Kansai/Osaka (82.6%) and Kanto/Tokyo (67.0%) was also higher (p<0.01) and lowest in Hokkaido/Tohoku (14.2%) (figure 3B). The percentage of medical students who applied only to public medical schools showed the opposite: lower (p<0.01) in Kanto/Tokyo (12.7%) and Kansai/Osaka (17.3%) (figure 3C). The percentage of local students in public medical schools in Hokkaido/Tohoku (41.0%) was lower than any of other areas (p<0.01) (figure 3D), and students from Kanto/Tokyo accounted for 46.7% of public medical school students in Hokkaido/Tohoku.
Figure 3.
Regional differences of medical students. (A) Annual family income >10 million yen (Ca. US$77 000). (B) Private upper secondary school graduation. (C) Application only to public medical school. (D) Local student ratio in public medical schools.  ≧60%
≧60%  ≧45%
≧45%  ≧30%
≧30%  <30%. 1: Hokkaido/Tohoku, 2: Kanto/Tokyo, 3: Chubu, 4: Kansai/Osaka, 5: Chugoku/Shikoku, 6: Kyushu/Okinawa.
<30%. 1: Hokkaido/Tohoku, 2: Kanto/Tokyo, 3: Chubu, 4: Kansai/Osaka, 5: Chugoku/Shikoku, 6: Kyushu/Okinawa.
Finally, the desired future workplaces of medical students were investigated in relation to the population size of the locality/conurbation in which they had been raised (family location) (see online supplemental figure). The distribution of medical students raised within areas with more than 1 million people; 200 000–1 million; 50 000–200 000; and less than 50 000 were 28.0%, 36.8%, 26.2% and 9.0%, respectively, whereas distribution of Chiiki-waku students from these regions was 17.0%, 34.4%, 32.1% and 16.5% respectively. In short, Chiki-waku students were more likely to come from less densely populated areas. Eighty per cent of medical students from cities with over 200 000 population expressed a preference for working in cities with over 200 000 residents in the future. On the other hand, students from areas with populations less than 50 000 and Chiiki-waku students seemed open to working in various areas, however, relatively few students wanted to work in areas with a population size of less than 50 000 (online supplemental figure, green).
bmjopen-2023-073559supp002.pdf (386.4KB, pdf)
Discussion
Main findings
This study, in collaboration with many health professions schools and non-health faculties nationwidely, examined the socioeconomic backgrounds of medical students in Japan, and compared them with dental, pharmacy, nursing, other health professions and non-health faculty students. We found that medical and dental students come from higher socioeconomic groups (figure 1, table 1). For example, the annual family income of medical and dental students was significantly higher than that of other health and non-health faculty students, and indeed higher than the national average and distribution of family income.22 Furthermore, one-third of medical students were physicians’ children and had clear educational advantages over non-physician children (eg, private education, tutoring) before applying for medical school. Logistic regression analysis revealed that having a physician parent, aspiration to the present profession as early as elementary school, and private upper secondary school education were predictors for admission to medical school (table 2).
Our focus from here on is medical students. The medical students who applied only to public medical schools and Chiiki-waku medical students had broader socioeconomic backgrounds in respect of annual family income, physician parent, secondary education and parental academic background compared with those who applied only to private medical schools and those who applied to both private and public schools (figure 2). However, Chiiki-waku students still had higher socioeconomic backgrounds than those of other health professions (except dental) and non-health faculty students, suggesting they were still from a privileged group. Clear preferences for location of work after graduation were also observed. Many medical students from metropolitan areas migrate to public medical schools outside their home areas but they intend to return home, that is, metropolitan areas, after graduation (figure 3 and online supplemental figure). Our results are relevant to an international audience—there is much interest in understanding the socioeconomic backgrounds of medical students globally because of the associations between backgrounds and later career choices.
Strengths and weaknesses of this study
Our study analysed the socioeconomic backgrounds of Japanese medical and other health professions students by using a web survey. These comparisons clearly elucidated the differences of backgrounds of medical and non-medical health professions students, and subgroups of medical students (those who enrolled in private, public and Chiiki-waku schools). Logistic regression analysis clarified strong explanatory variables for admission to medical school, thus providing further insights on the socioeconomic backgrounds of medical students.
Our study has several limitations. First, the number of participants and the response rate was relatively low in non-medical students. Although an anonymous survey was found to be suitable to the aim of our study, the questions primarily focused on medical students and may have been less relevant to non-medical students and faculty members. Our study is of students in one country and hence our findings may not be generalisable to other countries and cultural contexts.
Comparison with previous literature
Reflecting patterns seen in other global regions (eg, North America3 4 and Europe1 2 5), the current study demonstrates that medical students in Japan also tend to come from higher socioeconomic groups. While Chiiki-waku students generally have broader backgrounds than other medical students, they are still from higher socioeconomic backgrounds, that is, higher family income and higher physician parent ratio, compared with other health professions and non-health faculty students. Again, reflecting the patterns seen in other countries,25 the majority of Japanese medical students wish to return to work in urban areas—in other words, going back to where they are from.
These findings have implications for policy and practice. There is evidence from other countries that medical students from remote and rural regions are more likely to return to these regions after graduation, and the likelihood of them returning is increased if they have rural intention at the point of admissions and rural exposure when in medical school.26 27 Many reports have indicated the enrolment of local students is the strongest factor in the settlement of the healthcare workforce.28 A report from Australia clarified that medical students from rural areas are eight times more likely to practice in remote areas after graduation, whereas students with high academic scores are less likely to do so.29 If Japan wishes to staff its remote and rural regions, more ways must be found to attract and select more students from these regions into medicine.
Socioeconomic differences are apparent from early education onwards in Japan. Many students in our survey graduated from private secondary schools with a special 6-year course to prepare them for admission to medical schools and prestigious universities. Such private schools often cost up to 1 million yen (ca. US$7700) annually.30 Increasing numbers of Japanese parents think it is natural or inevitable that a family’s income dictate access to education.31 Moreover, those who are from higher socioeconomic groups and educated privately may receive more encouragement from others, including teachers, to apply for high prestige courses, such as medical school.32 33 On the contrary, students from low socioeconomic classes not only feel financial hardship, but also experienced discouragement from surrounding people and teachers,33 thus perpetuating the status quo.
According to a Japanese nationwide survey conducted in 1974,13 physicians’ children represented 37.7% of all medical students (1679 of 4452 students per year), and there was a huge difference of percentages between public medical schools (12.9%, 278 of 2148 students) and private medical schools (60.8%, 1401 of 2304 students). This study clarified that not much has changed over all: 33.2% of medical students are physicians’ children and the difference between public and private medical schools are 21.7% and 47.6%, respectively. Estimated number of physicians’ children in public, private and total medical schools, based on our results, are 1270 of 5852 public students (21.7%), 1706 of 3653 private students (47.6%) and 2976 of 9505 total medical students (33.2%), indicating 4.6-fold increase in public and 1.2-fold increase in private, and totally 1.8-fold increase. While possibly at least in part associated with an increase in doctors in Japan,34 this trend is concerning—it is clear that the background of medical students is not widening, or diversifying, in Japan. The heavy reliance on private hospitals and clinics in Japan35 and contribution of the private education system at the level of secondary and higher education in Japan16 17 may affect who is selected into medicine and thus who enters the medical workforce (and hence ultimately will also predict the distribution of physicians). However, this observation may not be linked solely to socioeconomics and prior education. A survey in Sweden, a country with public education and healthcare systems, revealed an increase in physicians’ children among medical students, from 6% in the 1950s birth cohort to 20% in the 1980s cohort.36 It would be beneficial to investigate whether this trend is worldwide and to examine the possibly influencing factors in more depth.
Finally, we identified clear differences in socioeconomic backgrounds among students from various health professions similar to those seen in the USA37 and France.38 Interestingly, around 40% of dental students in our study applied also to medical schools. Whether dentistry is ‘second best’ to medicine or vice-versa merits further investigation. It was clear from the data that students studying medicine and dentistry are different in terms of socioeconomic backgrounds to those studying nursing or other subjects, while pharmacy students seem to be ‘in-between’ medicine/dentistry and nursing/other in terms of background. We do not know if this pattern is seen in other countries. Longitudinal and multicohort studies are needed to examine if the patterns observed are consistent or fade over time.
Implications
Policies and methods to increase diversity among medical students and applicants differ according to country history and culture. The UK mainly adopts soft actions, including 6-year gateway courses for under-represented students,39 40 and outreach initiatives for students from low socioeconomic classes in secondary schools by providing career education and encouraging application to medical schools,41–43 whereas the USA,10 Canada4 and Australia29 have quota systems. The quota system, a hard affirmative action, has a long history of political controversy in the USA.44 Despite these initiatives, changes to the diversity of medical students, and hence the medical profession, have been slow.45 46 This is perhaps not surprising: selection and widening access to medicine has been labelled a ‘wicked problem’, that is, complex in nature, have innumerable causes associated with multiple social environments and actors with unpredictable behaviour and outcomes, and are difficult to define or even resolve.47 A country’s position on the broad issues of social mobility and justice are highly influential on the prioritisation, or not, of widening access to medical school. For example, meritocracy and academic excellence continue to be emphasised in the UK and Canada48 49 whereas Australia’s focus on social accountability in achieving equity and workforce diversity enables them to prioritise affirmative action.50 Japan seems to have adopted a position of meritocracy and academic excellence since 20th century. Given the discourses surrounding widening access and selection into medical school can act as barriers to applicants and thus to change,48 49 51 we respectfully suggest that a careful but proactive discussion on healthcare human resource development policies, including selecting to meet the healthcare needs of society, would be timely in Japan.
Conclusion
This study provides evidence that medical students in Japan hail from urban and higher income classes and physicians’ families. Even those medical students on a remote and rural workforce stream, Chiiki-Waku, are mostly from higher socioeconomic groups. If the associations between backgrounds and medical career preferences in Japan reflect those seen in other countries, physician maldistribution will continue into the future. We propose that widening the diversity of medical students in Japan is the key to solving physician workforce issues and meeting broad healthcare needs.
Supplementary Material
Acknowledgments
The authors thank Professor Junji Otaki, Tokyo Medical University and Professor Sohei Aramaki, Osaka University, for their helpful discussions and comments on this research project.
Footnotes
Contributors: The study was designed by YS, YT, KT, TS and mutually developed with JC from the international perspectives. YS obtained the ethical permission for this study. YS, YT and KT developed and administered web questionnaire. KT and YS carried out data collection and analysis. YS wrote the first draft of the paper. YT and TS discussed and edited it extensively, and JC carefully commented and edited from her position as a someone enmeshed in Western medical education and selection practices who has little understanding of Japan’s educational traditions, norms and culture, but has experiences as a visiting professor of the authors’ institution in Japan. All authors contributed to the later versions of the paper and approved the final version. The guarantor of this study was YS.
Funding: This study was supported by a Grant-in-Aid for Scientific Research (B) (Number 20H03909) from the Japan Society for the Promotion of Science.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and this study was approved by the Institutional Review Board of Gifu University (approval no. 2020-165). Participants gave informed consent to participate in the study before taking part.
References
- 1.Patterson F, Knight A, Dowell J, et al. How effective are selection methods in medical education? A systematic review. Med Educ 2016;50:36–60. 10.1111/medu.12817 [DOI] [PubMed] [Google Scholar]
- 2.Steven K, Dowell J, Jackson C, et al. Fair access to medicine? retrospective analysis of UK medical schools application data 2009–2012 using three measures of socioeconomic status. BMC Med Educ 2016;16:11. 10.1186/s12909-016-0536-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Youngclaus J, Roskovensky L. An updated look at the economic diversity of U.S. medical students. Analysis in Brief, AAMC 2018;18. Available: https://www.aamc.org/media/9596/download [Google Scholar]
- 4.Pitre T, Thomas A, Evans K, et al. The influence of income on medical school admissions in Canada: a retrospective cohort study. BMC Med Educ 2020;20:209. 10.1186/s12909-020-02126-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mulder L, Wouters A, Twisk JWR, et al. Selection for health professions education leads to increased inequality of opportunity and decreased student diversity in the Netherlands, but lottery is no solution: A retrospective multi-cohort study. Med Teach 2022;44:790–9. 10.1080/0142159X.2022.2041189 [DOI] [PubMed] [Google Scholar]
- 6.The expansion of medical student numbers in the United Kingdom. In: Medical School Council Position Paper. October 2021. Available: https://www.medschools.ac.uk/media/2899/the-expansion-of-medical-student-numbers-in-the-united-kingdom-msc-position-paper-october-2021.pdf [Google Scholar]
- 7.British Medical Association . The right mix: how the medical profession is diversifying its workforce. 2015. Available: https://questionnaires.bma.org.uk/news/therightmix/index.html
- 8.Medical School Council . Selecting for excellence final report. 2012. Available: https://www.medschools.ac.uk/media/1203/selecting-for-excellence-final-report.pdf
- 9.Rosinsky EF. Social class of medical students: A look at an untapped pool of possible medical school applicants. JAMA 1965;193:95–8. 10.1001/jama.1965.03090020009002 [DOI] [PubMed] [Google Scholar]
- 10.Association of American Medical Colleges. In: Diversity in medical education: Facts & Figures. 2012. Available: https://www.aamc.org/media/9951/download [Google Scholar]
- 11.Blake V. Affirmative action and medical school admissions. AMA J Ethics 2012;14:1003–7. 10.1001/virtualmentor.2012.14.12.hlaw1-1212 [DOI] [PubMed] [Google Scholar]
- 12.Khan R, Leung R, Lew B, et al. Socioeconomic status as a determinant of medical school admissions. In: Ontario Medical Student Association (OMSA) Position Paper. March 2016. Available: https://omsa.ca/en/position-papers/socioeconomic-status-determinant-medical-school-admissions [Google Scholar]
- 13.Tanaka T, Suzuki J, Konishi E, et al. On background and condition of living of medical students in Japan. Med Educ (Japan) 1974;5:381–400. [Google Scholar]
- 14.OECD data. poverty rate. Available: https://data.oecd.org/inequality/poverty-rate.htm
- 15.Suzuki Y, Gibbs T, Fujisaki K. Medical education in Japan: a challenge to the healthcare system. Med Teach 2008;30:846–50. 10.1080/01421590802298207 [DOI] [PubMed] [Google Scholar]
- 16.National information center for academic recognition Japan. In: The Japanese Education system. Available: https://www.nicjp.niad.ac.jp/en/japanese-system/about.html [Google Scholar]
- 17.National Institute for educational policy research. Education in Japan. Available: https://www.nier.go.jp/English/educationjapan/index.html [Google Scholar]
- 18.Allen D. Japanese cram schools and exam washback. Asian J App Linguist 2016;3:54–67. [Google Scholar]
- 19.Health professions education systems. White paper on medical education, 2022: 287–374. [Google Scholar]
- 20.Hirakata M. Student selection. In: White paper on medical education. Japan Society for Medical Education, 2022: 7–11. [Google Scholar]
- 21.Matsumoto M, Takeuchi K, Owaki T, et al. Results of physician licence examination and scholarship contract compliance by the graduates of regional quotas in Japanese medical schools: a nationwide cross-sectional survey. BMJ Open 2017;7:e019418. 10.1136/bmjopen-2017-019418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Summary report of comprehensive survey of living conditions 2019. In: Ministry of Health, Labour and Welfare of Japan. Available: https://www.mhlw.go.jp/english/database/db-hss/dl/report_gaikyo_2019.pdf [Google Scholar]
- 23.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet E-surveys (CHERRIES). J Med Internet Res 2004;6:e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bassett AM, Brosnan C, Southgate E, et al. Transitional journeys into, and through medical education for first-in-family (Fif) students: a qualitative interview study. BMC Med Educ 2018;18:102. 10.1186/s12909-018-1217-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myhre DL, Bajaj S, Jackson W. Determinants of an urban origin student choosing rural practice: a scoping review. Rural Remote Health 2015;15:3483. [PubMed] [Google Scholar]
- 26.O’Sullivan BG, McGrail MR, Russell D, et al. A review of characteristics and outcomes of Australia’s undergraduate medical education rural immersion programs. Hum Resour Health 2018;16:8. 10.1186/s12960-018-0271-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Budhathoki SS, Zwanikken PAC, Pokharel PK, et al. Factors influencing medical students' motivation to practise in rural areas in low-income and middle-income countries: a systematic review. BMJ Open 2017;7:e013501. 10.1136/bmjopen-2016-013501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization . WHO guideline on health workforce development, attraction, recruitment and retention in rural and remote areas. 2021. Available: https://www.ncbi.nlm.nih.gov/books/NBK570763/pdf/Bookshelf_NBK570763.pdf [PubMed]
- 29.Puddey IB, Mercer A, Playford DE, et al. Medical student selection criteria as predictors of intended rural practice following graduation. BMC Med Educ 2014;14:218. 10.1186/1472-6920-14-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Annual learning expenses in 2021 . Ministry of Education, Culture, Sports, Science and Technology. Available: https://www.mext.go.jp/content/20221220-mxt_chousa01-000026656_1a.pdf
- 31.Tachibanaki T. Increasing indifference to Japan’s education inequality [Nippon.com]. 2021. Available: https://www.nippon.com/en/in-depth/d00659/
- 32.Otaki J, Taketomi K, Shibahara M, et al. Factors that hinder medical career aspirations: A nationwide questionnaire survey of teachers in charge of career guidance in Japanese high schools. PLoS ONE 2022;17:e0270477. 10.1371/journal.pone.0270477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grace MK. Subjective social status and premedical students' attitudes towards medical school. Soc Sci Med 2017;184:84–98. 10.1016/j.socscimed.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 34.Statistics of Physicians, Dentists and Pharmacists 2018 . Ministry of Health, Labour and Welfare of Japan. Available: https://www.mhlw.go.jp/english/database/db-hss/dl/spdp_2018.pdf
- 35.Survey of medical institutions 2017 . Ministry of Health, Labour and Welfare of Japan. Available: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/m18/dl/is1802_01.pdf
- 36.Polyakova M, Persson P, Hofmann K, et al. Does medicine run in the family -Evidence from three generations of physicians in Sweden: retrospective observational study. BMJ 2020;371:m4453. 10.1136/bmj.m4453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gallagher JE, Niven V, Donaldson N, et al. Widening access? characteristics of applicants to medical and dental schools, compared with UCAS. Br Dent J 2009;207:433–45. 10.1038/sj.bdj.2009.963 [DOI] [PubMed] [Google Scholar]
- 38.Hennequin M, Tubert S, Devillers A, et al. Socio-economic and schooling status of dental undergraduates from six French universities. Eur J Dent Educ 2002;6:95–103. 10.1034/j.1600-0579.2002.60301.x [DOI] [PubMed] [Google Scholar]
- 39.Curtis S, Smith D. A comparison of undergraduate outcomes for students from gateway courses and standard entry medicine courses. BMC Med Educ 2020;20:4. 10.1186/s12909-019-1918-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gibson Smith K, Alexander K, Cleland J. Opening up the black box of a gateway to medicine programme: a realist evaluation. BMJ Open 2021;11:e049993. 10.1136/bmjopen-2021-049993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Azmy J, Nimmons D. Reflections on a widening participation teaching role. Clin Teach 2017;14:139–40. 10.1111/tct.12574 [DOI] [PubMed] [Google Scholar]
- 42.Rees E, Woolf K. Selection in context: the importance of clarity, transparency and evidence in achieving widening participation goals. Med Educ 2020;54:8–10. 10.1111/medu.14023 [DOI] [PubMed] [Google Scholar]
- 43.Bhalla G, Dominic C, Kumar P. A successful widening participation model for medical admissions. Med Educ 2021;55:655. 10.1111/medu.14513 [DOI] [PubMed] [Google Scholar]
- 44.Urofsky MI. The affirmative action puzzle. A living history from reconstruction today. Pantheon Books, 2020. [Google Scholar]
- 45.Apampa A, Kubacki A, Ojha U, et al. Challenges in widening participation outreach: is enough being done to tackle the under-representation of low-income students in medicine Adv Med Educ Pract 2019;10:917–23. 10.2147/AMEP.S211895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White C. Shut out: the medical profession’s intractable class problem. BMJ 2019;367:l6433. 10.1136/bmj.l6433 [DOI] [PubMed] [Google Scholar]
- 47.Cleland JA, Patterson F, Hanson MD. Thinking of selection and widening access as complex and wicked problems. Med Educ 2018;52:1228–39. 10.1111/medu.13670 [DOI] [PubMed] [Google Scholar]
- 48.Alexander K, Fahey Palma T, Nicholson S, et al. Why not you?’ discourses of widening access on UK medical school websites. Med Educ 2017;51:598–611. 10.1111/medu.13264 [DOI] [PubMed] [Google Scholar]
- 49.Razack S, Maguire M, Hodges B, et al. What might we be saying to potential applicants to medical school? discourses of excellence, equity, and diversity on the web sites of Canada’s 17 medical schools. Acad Med 2012;87:1323–9. 10.1097/ACM.0b013e318267663a [DOI] [PubMed] [Google Scholar]
- 50.Coyle M, Sandover S, Poobalan A, et al. Meritocratic and fair? The discourse of UK and Australia’s widening participation policies. Med Educ 2021;55:825–39. 10.1111/medu.14442 [DOI] [PubMed] [Google Scholar]
- 51.Cleland J, Razack S. When I say … privilege. Med Educ 2021;55:1347–9. 10.1111/medu.14599 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-073559supp001.pdf (66.4KB, pdf)
bmjopen-2023-073559supp002.pdf (386.4KB, pdf)
Data Availability Statement
No data are available.