Abstract
Introduction
There is uncertainty about the advantages and disadvantages of laparoscopic hysterectomy compared with abdominal hysterectomy, particularly the relative rate of complications of the two procedures. While uptake of laparoscopic hysterectomy has been slow, the situation is changing with greater familiarity, better training, better equipment and increased proficiency in the technique. Thus, a large, robust, multicentre randomised controlled trial (RCT) is needed to compare contemporary laparoscopic hysterectomy with abdominal hysterectomy to determine the safest and most cost-effective technique.
Methods and analysis
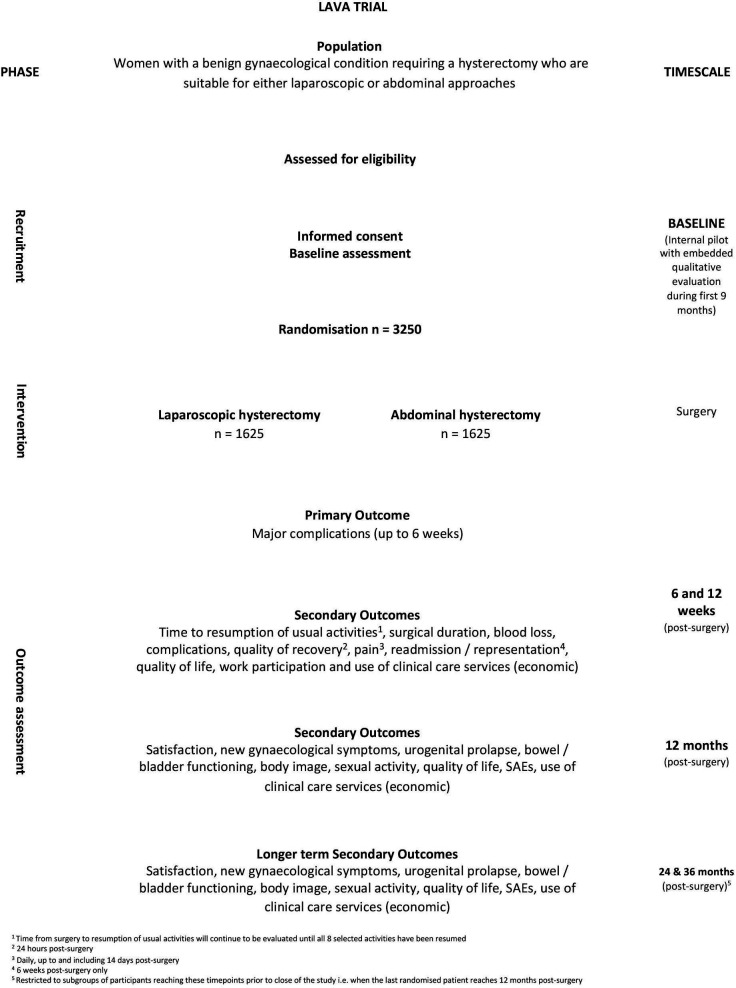
A parallel, open, non-inferiority, multicentre, randomised controlled, expertise-based surgery trial with integrated health economic evaluation and an internal pilot with an embedded qualitative process evaluation. A within trial-based economic evaluation will explore the cost-effectiveness of laparoscopic hysterectomy compared with open abdominal hysterectomy. We will aim to recruit 3250 women requiring a hysterectomy for a benign gynaecological condition and who were suitable for either laparoscopic or open techniques. The primary outcome is major complications up to six completed weeks postsurgery and the key secondary outcome is time from surgery to resumption of usual activities using the personalised Patient-Reported Outcomes Measurement Information System Physical Function questionnaire. The principal outcome for the economic evaluation is to be cost per QALY at 12 months’ postsurgery. A secondary analysis is to be undertaken to generate costs per major surgical complication avoided and costs per return to normal activities.
Ethics and dissemination
The study was approved by the West Midlands-Edgbaston Research Ethics Committee, 18 February 2021 (Ethics ref: 21/WM/0019). REC approval for the protocol version 2.0 dated 2 February 2021 was issued on 18 February 2021.
We will present the findings in national and international conferences. We will also aim to publish the findings in high impact peer-reviewed journals. We will disseminate the completed paper to the Department of Health, the Scientific Advisory Committees of the RCOG, the Royal College of Nurses (RCN) and the BSGE.
Trial registration number
ISRCTN14566195.
Keywords: minimally invasive surgery, gynaecology, health economics
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The LAparoscopic Versus Abdominal (LAVA) trial is larger than all the previous 25 randomised controlled trials evaluating laparoscopic and open hysterectomy and of higher quality, addressing the methodological deficiencies of previous trials; namely their power to show a meaningful difference, accounting for surgical expertise bias and the ensuring the validity of outcomes assessments, especially the key secondary outcome of personalised recovery.
In the LAVA trial a novel, validated, personalised recovery tool is used via SMS and an expertise-based design to mitigate against surgical expertise bias employed.
Third part randomisation is to be performed balancing important prognostic variables.
Due to the differing natures of the intervention, it is impossible to blind either the care providers, investigators or participants to their allocated group.
Introduction
Hysterectomy is common, with 1 in 10 women undergoing the procedure in their lifetime, mostly for benign conditions.1–3 A total of 30 000 women undergo a hysterectomy every year in the UK for benign indications such as abnormal uterine bleeding and pelvic pain.1–3
The procedure is associated with high rates of patient satisfaction and improvement in quality of life (QoL) but serious complications can arise.4 5 The morbidity arising from hysterectomy imposes a burden on women and the ubiquity of the procedure uses a substantial amount of scarce healthcare resources.6–9 Currently, most hysterectomies are performed by laparotomy, through a vertical or transverse incision because this traditional method is thought to minimise intraoperative complications but the increased trauma of an abdominal incision can prolong recovery.5 This may be especially true in overweight and obese women, where morbidity is greater from mobility restrictions and wound infection.10
Several randomised controlled trial (RCTs), mostly small and of low or moderate quality, have compared the surgical approach to hysterectomy for benign disease. The 2015 Cochrane review identified 25 trials (2983 women) comparing laparoscopic and abdominal hysterectomy.5 Laparoscopic hysterectomy was found to have significantly more urinary tract injuries (bladder or ureter) but the available evidence was of low quality. The largest RCT included in this review was conducted over 15 years ago, when laparoscopic hysterectomy was in its infancy.11 Smaller, but more recent trials of laparoscopic hysterectomy, have shown a trend towards a lower major complication rate.12–15 The Cochrane review5 identified no differences in the costs or outcomes apart from return to normal activities, which was shorter in the laparoscopic hysterectomy group by 14 days on average.
The uptake of laparoscopic hysterectomy is increasing with greater familiarity and increased proficiency in the technique aided by improved training and better surgical equipment.16–18 Patient’s values and preferences, especially around speed of recovery may also be driving this trend.
A systematic review of cost-effectiveness studies of hysterectomy, found laparoscopic hysterectomy to be the least cost-effective but the authors felt that conclusions were difficult to draw due to variation in study design, follow-up times and the QoL measurement used.19 20 Thus, we designed a large RCT to determine the clinical and cost-effectiveness of laparoscopic hysterectomy compared with open abdominal hysterectomy for women with a benign gynaecological condition.
Aims and objectives
Main clinical objective
To compare laparoscopic hysterectomy with open abdominal hysterectomy in terms of major intraoperative and postoperative surgical complications (up to 6 weeks). Postoperative recovery will also be evaluated by measuring the time from surgery to resumption of usual activities.
Economic objectives
To compare the relative cost-effectiveness of laparoscopic hysterectomy with open abdominal hysterectomy in terms of cost per quality-adjusted life-year. Additional cost-effectiveness analyses will explore cost per major surgical complication avoided and cost per return to normal activities.
Study design and setting
Trial design
The study is designed as a parallel, open, non-inferiority, multicentre, randomised controlled, expertise-based surgery trial with integrated health economic evaluation and an internal pilot with an embedded qualitative process evaluation to assess the ability of the study to recruit and randomise.
Trial setting
Recruitment to the LAparoscopic Versus Abdominal (LAVA) study will take place in gynaecology departments (general and relevant specialist clinics including menstrual disorders and pelvic pain clinics, hysteroscopy and colposcopy services) in up to 50 National Health Service (NHS) Hospitals within the UK.
Identification of participants
Eligible women will be identified by a member of the clinical team responsible for the direct care of the potential participant in outpatient gynaecology clinics and preoperative assessment clinics in each recruiting centre. The LAVA study will be introduced by a member of the clinical or research team, with full counselling about the trial (including provision of information about the qualitative process evaluation).
Substudies
Qualitative evaluation
A qualitative process evaluation will be undertaken in parallel to the pilot phase. The primary aim of the qualitative study is to explore the feasibility, acceptability and appropriateness of the trial and intervention for women and healthcare professionals (HCPs). The results will inform decision-making around progression to a full trial, including study design and processes.
Health economic evaluation
An economic evaluation alongside the RCT will explore the cost-effectiveness of laparoscopic hysterectomy compared with open abdominal hysterectomy based on a primary outcome of quality-adjusted life-years and secondary outcomes such as major surgical complications avoided. The analysis will adopt the perspective of the health service. All resource use will be collected prospectively and unit costs attached. Deterministic and probabilistic sensitivity analysis will be carried out.
Patient and public involvement
Our research has been developed with involvement of members of the Royal College of Obstetricians and Gynaecologists (RCOG) Women’s Voices group, the Hysterectomy Association and the Birmingham Women’s Hospital Hysterectomy Focus Group. A total of 945 women responded to our patient and public involvement (PPI) survey. Major complications were ranked as the most important outcome for the trial to assess, with return to usual activities considered the second most important outcome (ranked in the top three most important outcomes in the BSGE survey). A measure of the speed and quality of recovery (QoR) was also considered one of the most important outcomes to measure after major complications and improvement in QoL in the PPI survey.
Two focus groups felt the burden placed on women from administering outcome questionnaires at 24 hours’ postsurgery and the frequency of dissemination postoperatively proposed was acceptable. Indeed, the consensus view was that measuring recovery against preset targets was a good thing (with tools already available on the internet). This frequency of contact was also supported by the PPI survey; 6 weeks 485/945 (51%) and 12 months 514/945 (54%) were the most popular time points.
Overall, almost 50% (462/945) of PPI survey respondents were willing to consider taking part in the proposed trial. Excluding the 483 women declining to participate because they had already undergone a hysterectomy revealed that 63% (292/462) of respondents were willing to take part, with the remainder being ‘not sure’.
Results of the study will be shared with study participants, staff members at research sites and investigators of other studies related to hysterectomy and benign gynaecological surgery. A formal notification to the ethics committee, Department of Health, key partners and sponsors will be made. Outreach to other key stakeholders (trial networks, health advocates) involved in related trials is planned. The trial team has key individuals to optimise the dissemination of results. With our PPI coapplicants and contacts we will produce effective, contemporary formats for dissemination, for example, the use of video podcasts and social media outlets.
Participants
Women are eligible for recruitment to the LAVA trial if they meet the following inclusion criteria and do not have any of the exclusion criteria set out below:
Inclusion criteria
Aged between 18 and 55 years of age and able to give informed consent to participate.
Have a benign gynaecological condition that is being treated with a hysterectomy.
This hysterectomy can be undertaken by either a laparoscopic or open abdominal routes. The feasibility and appropriateness of both routes of hysterectomy for women were to be decided pragmatically, the operating surgeon deciding where their equipoise was taking into consideration factors such as the size of the uterus, likelihood of pelvic adhesions and anticipated surgical complexity for either approach.
Exclusion criteria
Women with suspected malignant disease of the genital tract.
Women who require concomitant gynaecological surgery for bladder or other pelvic support.
Women who require concomitant gynaecological surgery for excision of deep endometriosis that requires dissection of the pararectal space.
Choice of intervention
The LAVA trial will compare laparoscopic with conventional abdominal hysterectomy. Vaginal hysterectomy has been shown to be beneficial in terms of complications and recovery but this technique is largely confined to women with prolapse and where the uterus is not enlarged.16 While the uptake of laparoscopic hysterectomy has been slow,17 the situation is changing with greater familiarity, better training, better equipment and increased proficiency in the technique, such that nearly as many hysterectomies for benign disease are now being done laparoscopically as abdominally.18 19
Contemporary gynaecological practice has developed rapidly in response to technological advances facilitating less invasive surgical techniques for common operations aligned with innovations in preoperative, perioperative and postoperative care designed to ‘enhance’ recovery.20 The results of this trial will have a significant impact on day-to-day clinical practice in women’s healthcare.
Consent
It will be the responsibility of the Investigator to obtain informed consent (paper or electronic) for each participant prior to performing any trial related procedure (online supplemental file 1). A research nurse, research midwife or clinician is able to take consent providing that local practice allows this and responsibility has been delegated by the principal investigator (PI) as captured on the Site Signature and Delegation Log.
bmjopen-2022-070218supp001.pdf (42.6KB, pdf)
Recruitment, enrolment and randomisation
Recruitment
Potential participants will be identified and approached by medical staff who are responsible for the direct care of the potential participant in participating centres after having received appropriate training relating to the trial and who are delegated this task on the site delegation log. Recruitment will take place in gynaecology clinics in gynaecologist lead centres located across the UK. Research ethics committee (REC) approved posters making potential participants aware of the study may be displayed in areas that will be accessed by them, such as waiting areas, clinics and consulting rooms
Enrolment
Women with benign gynaecological conditions requiring a hysterectomy and who are suitable for either surgical technique are eligible for inclusion in the LAVA trial.
Prior to clinical consultations, the medical records of potential participants may be screened for eligibility by clinic doctors, nurses and research nurses, after having received appropriate training relating to the trial.
Potential participants will be provided with an REC approved study participant information sheet (PIS) and given time to consider their involvement. Clinic doctors will confirm eligibility for the trial. After participant eligibility is confirmed and informed consent received, the baseline questionnaires are to be completed and then the participant randomised into the trial. Baseline data collected include demographic and medical data (age ethnicity, body mass index (BMI) (≤29.9, 30–34.9, ≥35 kg/m2), previous caesarean section (yes/no), uterine size ≤12 weeks, >12 weeks, planned retention of cervix yes/no); Patient-Reported Outcomes Measurement Information System Physical Function (PROMIS-PF) item bank V.1.219 (see ‘key secondary outcome’); QoL, symptom and physical functioning questionnaires, EuroQoL-5 Dimensions-3 Level (EQ-5D-5L) and EQ Visual Analogue Scale (VAS),15 Urogenital Distress Inventory (UDI),21 Pelvic Organ Prolapse Symptom Score (POP-SS),21 Defecatory Distress Inventory (DDI),22 Sexual Activity Questionnaire (SAQ).23
Participants should be aware at the beginning that they can freely withdraw (discontinue participation) from the trial (or part of) at any time. LAVA has adopted an analysis based on a modified intention to treat principle, that is, all participants will be followed up and analysed in the treatment group to which they were randomised provided a hysterectomy (of any type) was undertaken unless they withdraw from the study.
Randomisation
Randomisation is provided by a secure online randomisation system at the Birmingham Clinical Trials Unit (BCTU) (available at http://www.trials.bham.ac.uk/lava). Participants will be randomised at the level of the individual in a 1:1 ratio to undergo their hysterectomy by either a laparoscopic or open abdominal route. A minimisation algorithm will be used within the online randomisation system to ensure balance in the treatment allocation over the following variables:
Previous caesarean section (yes/no).
BMI (≤29.9, 30–34.9, ≥35 kg/m2).
Uterine Size (≤12 weeks, >12 weeks).
Planned retention of cervix (yes/no).
Recruiting centre.
Blinding
Due to the differing natures of the intervention, it is impossible to blind either the care providers, investigators or participants to their allocated group.
Interventions and expertise-based surgery
Hysterectomy is undertaken by either a laparoscopic or an open abdominal route, by a surgeon who had self-declared as having expertise in laparoscopic hysterectomy, abdominal hysterectomy or both approaches to hysterectomy.
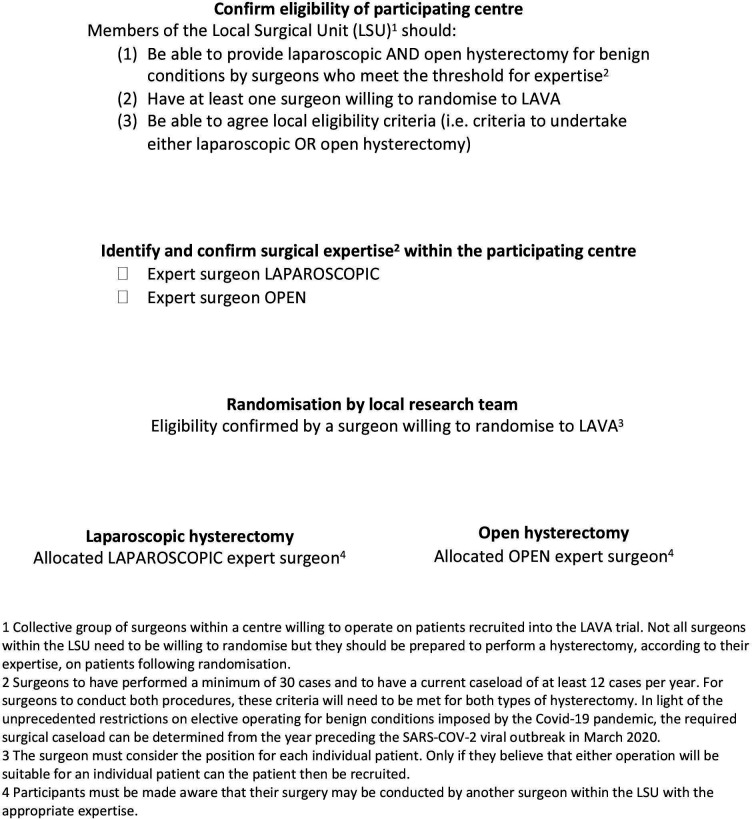
The decision to remove or retain cervix (total or subtotal) or remove and retain ovaries was left to the discretion of the participant in consultation with her gynaecologist. The expertise design process for eligible centres is depicted in figure 1.
Figure 1.
The expertise design process for eligible centres. LAVA, LAparoscopic Versus Abdominal.
Satisfactory experience requires surgeons to have performed a minimum of 30 cases24 and to have a current caseload of at least 12 cases per year.25–27 For surgeons to conduct both procedures, these criteria will need to be met for both procedures. These thresholds are evidence based. In a series of over 10 000 laparoscopic hysterectomies, surgeons who had performed more than 30 laparoscopic hysterectomies had a significantly lower incidence of ureteric and bladder injuries (0.5% and 0.8%, respectively) compared with those performing 30 operations or fewer (2.2% and 2.0%, respectively).24
The importance of surgical experience as a predictor of successful surgical outcome has been shown in other studies.25 Surgical volume is well recognised to correlate with safety in hysterectomy.26 A systematic review and meta-analysis of studies including 741 760 patients reported complication rates according to surgical volume. High volume surgeons were defined as performing at least one of a particular type of hysterectomy per month on average (ie, a minimum of 12 per year). Low volume surgeons performed fewer than 12 hysterectomies per year and had higher major complication rates (total complications (OR 1.3, 95% CI 1.2 to 1.5%), intraoperative complications (OR 1.6, 95% CI 1.2% to 2.1%) and postoperative complications (OR 1.4, 95% CI 1.3% to 1.4%).27
Outcome measures
Women who give consent in a face-to-face setting will subsequently complete their baselines questionnaires and then proceed to randomisation. The baseline questionnaires are self-explanatory but help to complete them will be provided by the local or central medical research teams on request using remote means (telephone/VOIP/video consultation) where feasible. Participants will be made aware of this resource by the local research teams. It is anticipated that some participants may need help to select their 8 personalised recovery targets from 29 options PROMIS-PF item bank V.1.2.19 21–23 Local research teams will offer remote (telephone, VOIP or video) contact, or exceptionally face to face appointments, to provide explanation.
Trial outcomes
Primary outcome
Major surgical complications: These will be objectively ascribed and largely in accordance with the validated and widely used Clavien-Dindo classification of surgical complications.28 They will be defined as any of the following up to and including 6 full weeks’ postsurgery: (1) all Clavien-Dindo grades III–V complications, (2) Clavien-Dindo grade II complications of pulmonary embolus or blood transfusion or (3) haemorrhage ≥1 L or; iv) major adverse anaesthetic event. The specific type of major complication will be presented in addition to the Clavien-Dindo grades III–V classification.
However, other less common major surgical or anaesthetic complications may arise and these will be ascribed in accordance with the appropriate Clavien-Dindo classification shown in table 1.
Table 1.
Definition of major surgical complications in the LAVA trial
| Major haemorrhage | Haemorrhage ≥1 L |
| Clavien-Dindo grade II | Pulmonary embolus, blood transfusion |
| Clavien-Dindo grade III | Complication requiring surgical, endoscopic or radiological intervention |
| Clavien-Dindo grade IV | Life-threatening complication requiring management on a high-dependency unit (HDU)/intensive therapy unit* |
| Clavien-Dindo grade V | Death |
| Major anaesthetic event | Anaphylaxis, awareness, nerve injury (including epidural/spinal anaesthesia), hypoxic brain injury, malignant hyperthermia, iatrogenic complication (eg, pneumothorax from central line, limb ischaemia from arterial line) |
*Non-life-threatening elective or precautionary admission to an HDU (eg, because of medical comorbidities) postoperatively will not be considered a grade IV complication.
LAVA, LAparoscopic Versus Abdominal.
Complication data occurring during and up to 6 weeks following hysterectomy will be collected from the relevant case report forms (CRF) completed by the local research team:
-
Day of surgery CRF.
Detailing the type of major perioperative complications.
-
Postoperative inpatient CRF.
Detailing the type and timing of major surgical complications occurring during inpatient stay up until hospital discharge).
-
Six-week postsurgery complication and representation CRF.
Detailing the type and timing of major postoperative complications, as well as any reattendance and/or readmissions to hospital up to 6 weeks postsurgery, will be recorded. The data will be acquired by the local research team from scrutiny of the hospital case notes and/or follow-up consultation (if conducted routinely at approximately 6 weeks posthysterectomy).
Key secondary outcome
Time from surgery to resumption of usual activities. To increase accuracy and to minimise recall bias, the validated, personalised PROMIS-PF item bank V.1.2 will be used.19 Twenty-nine items covering relevant activities for our study population will be used from the entire 121 item bank.21 Every item contains five response categories.
At baseline, participants were asked to select 8 activities from this list of 29 that, in their view, would most reflect their day-to-day activities. In this way, participants created their personalised physical function short form. Participants will record when each activity is resumed, with full recovery being achieved once all eight personalised activities have been resumed. Until all personalised activities have resumed participants will be asked to complete this weekly for the first 12 weeks, then fortnightly from week 13 to week 26 after which requests will cease.
Other secondary outcomes
-
Surgical outcomes:
Duration of operation, (minutes).
Estimated blood loss (mL).
-
In hospital stay:
In hospital postoperative pain using a Numerical Rating Scale (NRS) (with 0 indicating no pain to 10 indicating maximum pain)*, measured daily.
Total analgesia use.*
Overall QoR score taken from the QoR 15 (QoR-15) questionnaire25 (with 0 indicating worst recovery and 10 indicating best recovery), measured at approximately 24 hours postoperation.*
Time from operation to discharge in days.
-
Up to 14 days after surgery:
Postoperative pain using an NRS (with 0 indicating no pain to 10 indicating maximum pain), measured daily.
Total analgesia use.
Overall QoR score taken from the QoR-15 questionnaire25 (with 0 indicating worst recovery and 10 indicating best recovery), measured at approximately 24 hours postoperation.*
Time from operation to discharge in days.
-
Up to 6 weeks postsurgery:
Minor complications (haemorrhage 500 mL to ≤1 L; fever (presumed infection) requiring antibiotics; pain uncontrolled with usual analgesic management; urinary retention requiring recatheterisation; catheterisation for longer than 72 hours; pelvic haematoma not requiring radiological or surgical intervention; pelvic abscess not requiring radiological or surgical intervention; wound infections/complications managed at the bedside or on the ward).
Representation to hospital.
Readmission to hospital.
Use of health services.
Time away from normal activities.
-
Six weeks postsurgery:
QoL score using EQ-5D-5L questionnaire29 (with −0.285 indicating worst possible value and 1.0 as best possible value).
QoL score using EQ-5D-5L VAS (with 0 indicating worst possible score and 100 as best possible score).
-
Twelve weeks postsurgery:
QoL score using EQ-5D-5L questionnaire29 (with −0.285 indicating worst possible value and 1.0 as best possible value).
QoL score using EQ-5D-5L VAS.
Time from surgery to work (if working) in days.
Work productivity and activity impairment scores using Work Productivity and Activity Impairment Questionnaire: General Health (WPAI-GH)30 (absenteeism score, presenteeism score, work productivity loss score, activity impairment score—all scored 0 good to 100 bad) at 12 weeks only.
-
12/24/36 months postsurgery:**
Satisfaction with hysterectomy.
Symptoms of urogenital prolapse using the POP-SS questionnaire.21 31
Bladder function using UDI22 32 questionnaire.
Bowel function using DDI23 questionnaire.
Sexual function using the SAQ.33
QoL score using EQ-5D-5L questionnaire.
QoL score using EQ-5D-5L VAS.
Body image using the Body Image Scale questionnaire.34
New gynaecological symptoms (abdominal pain (cyclical, non-cyclical and dyspareunia) and vaginal bleeding; yes/no).
Contact with Community Social and Clinical Care Services, that is, outpatients or emergency visits, and hospital services, for example, representations, readmissions, outpatient appointments and further medical treatment, time away from normal activities.
Throughout: serious adverse events (SAEs)
*Questionnaire may be completed at home if patient discharged on the same day as surgery.
**The latter two time points will only be collected for participants who reach these times prior to the study closes after all patients have been followed up for 12 months.
A summary of the schedule of assessments is shown in online supplemental table 1 and the trial flow diagram shown is figure 2.
Figure 2.
Trial schema. LAVA, LAparoscopic Versus Abdominal.
Statistical consideration
Sample size
To enable 90% power to test the non-inferiority hypothesis at a one-sided 2.5% significance level (two-sided 5% level) assuming a 3% margin of non-inferiority and a major surgical complication rate of 6% in the abdominal (control) group requires 2634 participants. The estimate of 6% is taken from a similar previous comparative study.11 A 3% margin is justifiable because of the trade-off of potentially swifter recovery with laparoscopic surgery; a view shared by our patient focus group and is substantially less than the 5% difference observed in the previous major trial11 which led to the continued use of open abdominal hysterectomy.
An extra consideration is the potential for clustering by surgeon due to the expertise based design19 22 Under the assumption that each of the 50 centres will use 6 surgeons (operating on approximately 9 patients on average during the study), along with an intracluster correlation (ICC) estimate of 0.02, the sample size has been increased by 16% to 3055. This ICC estimate used—in the absence of precise estimates—is considered conservative given the outcome is clinical and of low prevalence, both of which are factors associated with low ICC.23 33 However, even varying these factors up to an ICC of 0.07 or average cluster size of 29, shows we will have at least 80% power to establish non-inferiority in these situations. A final inflation of 6% to account for loss to follow-up brings the final sample size total to 3250 participants. This size of sample would give the ability to detect meaningful differences between groups in our key secondary outcome of time from surgery to resumption of usual activities. Assuming the median recovery time in the abdominal group is between 6 and 9 weeks,34 we will have high levels of power (>90%) to detect reductions of 1 week in all cases.
Analysis of outcome measures
A separate statistical analysis plan will be produced and will provide a more comprehensive description of the planned statistical analyses. For the primary outcome, given the nature of the non-inferiority design, supportive per-protocol and CACE analyses35 will be considered alongside the intention-to-treat population. All outcomes will be adjusted for the minimisation variables where possible.
For all major outcome measures, summary statistics and differences between groups, for example, relative risks, will be presented with 95% CIs. For the primary outcome, this is equivalent to a one-sided 97.5% CI and hence conservative in terms of the non-inferiority margin. For the trial to declare non-inferiority of the laparoscopic approach, the upper margin of the absolute risk difference CI must not exceed 3%.
For the key secondary outcome of time from surgery to resumption of usual activities, we will incorporate a conditional hierarchical approach to interpretation of the 95% CI to ensure we appropriately control for the overall rate of type I error.36
Primary outcome measure
We will use a mixed effect binomial regression model to estimate the absolute risk difference and 95% CI (primary method). Relative risks will be calculated in a similar fashion. Parameters for treatment group as well as the minimisation variables will be included in the model as fixed effects. We will explore methods to most appropriate account for both centre and surgeon variation; these elements will also be included in the model as random effect.
Secondary outcome measures
The key secondary outcome of time from surgery to resumption of normal activities will be analysed using a mixed effects (‘frailty’) Cox proportional hazard model,37 allowing the same minimisation variables and incorporating parameters for both centre and surgeon.
Linear regression models will be used to analyse response from continuous outcome measures such as, for example, participant-reported questionnaires, duration of surgery and pain via NRS; mean differences and 95% CIs will be produced. Other binary and time-to-event analyses will be considered in the same fashion as the primary and key secondary outcomes. Satisfaction responses will be analysed using ordinal logistic regression. SAEs will be summarised and analysed using a χ2 test. Analgesia use will be summarised but not formally analysed.
We will capture recovery more fully with the other included validated outcome measures (eg, PROMIS-PF item bank V.1.2),19 21–23 QoR-15 questionnaire,25 NRSs. The variation in analgesia type and use (secondary outcome) over the 14-day postoperative diary will presented descriptively because meaningful quantitative analysis is compromised due to the variation in type of analgesia and how to aggregate such data to allow valid comparison because meaningful quantitative analysis is compromised due to the variation in type of analgesia and how to aggregate such data to allow valid comparison. Appropriate summary statistics split by group will be presented for each outcome (eg, proportions/percentages, mean/SD or median/IQR).
Subgroup analyses
Subgroup analyses will be limited to the same variables used in the minimisation algorithm, and performed on the primary and key secondary outcomes. Given they will have low power to assess non-inferiority on the primary outcome variable they will be treated as exploratory. Tests for statistical heterogeneity (eg, by including the treatment group by subgroup interaction parameter in the regression model) will be undertaken.
Missing data and sensitivity analyses
Every attempt will be made to collect full follow-up data on all study participants; it is thus anticipated that missing data will be minimal. Participants with missing primary outcome data will not be included in the primary analysis in the first instance. This presents a risk of bias, and sensitivity analyses will be undertaken to assess the possible impact of the risk.
Planned interim analysis
Interim analyses of safety and efficacy for presentation to the independent data monitoring committee (DMC) will take place during the study. The committee will meet prior to study commencement to agree the manner and timing of such analyses but this is likely to include the analysis of the primary and key secondary outcome and full assessment of safety (SAEs) at least at annual intervals. Criteria for stopping or modifying the study based on this information will be ratified by the DMC. Details of the agreed plan will be written into the statistical analysis plan.
Planned final analyses
The primary analysis for the study will occur once all participants have completed the assessments at 12 months postsurgery and corresponding outcome data has been entered onto the study database and validated as being ready for analysis. This analysis will include data items up to and including this time point only. The longer term data collected at 24 months and 36 months postsurgery will be restricted to the subgroup of patients who have reached these assessment points prior to study close and reported at a later date (see trial schema, figure 2).
Substudies
Full details of these substudies are available from the authors on request.
Qualitative process evaluation
A qualitative process evaluation was undertaken in parallel to the pilot phase. The primary aim of the qualitative study was to explore the feasibility, acceptability and appropriateness of the trial and intervention for women and HCPs. The results were to inform decision-making around progression to a full trial, including study design and processes.
Health economic evaluation
An economic evaluation was designed to assess the cost-effectiveness of laparoscopic hysterectomy compared with open abdominal hysterectomy in the management of benign gynaecological conditions. A within trial-based economic evaluation was to explore the cost-effectiveness of laparoscopic hysterectomy compared with open abdominal hysterectomy. The principal outcomes for the economic evaluation was cost per QALY at 12 months postsurgery. A secondary analyses was planned to generate costs per major surgical complication avoided and costs per return to normal activities.
Data collection
In the first instance, participants will be invited to participate in an interview via telephone/video conference (eg, Zoom, Skype or WhatsApp). To ensure inclusivity, where participants are unable to participate virtually, we may consider face-to-face interviews in the clinic where they were treated/work, at the University of Birmingham (if local to Birmingham), in the participant’s home or in an appropriate public space.
For women, we will aim to conduct interviews within 4–6 weeks of them being approached to participate (decliners) or being randomised (women who consent to randomisation). This will, however, remain flexible to accommodate the needs of the women.
Management of risk
If a participant raises issues about their care that the qualitative research team deem as potentially harmful to them (or others) then the researcher will advise them to contact their local Patient Advice and Liaison Service (or equivalent) whose contact details are provided in the PIS. The lead for the qualitative substudy will also inform the CI. The CI, where appropriate, will ensure that the local unit PI is aware of the woman and potential concerns so that follow-up can be arranged if required. Should a participant have questions about their clinical care then the qualitative research team will advise the woman to contact her clinical team and/or her general practitioner.
Data management
Data Protection Registration: The University of Birmingham has Data Protection Registration to cover the purposes of analysis and for the classes of data requested. The University’s Data Protection Registration number is Z6195856.
Coding and validation will be agreed between the trial’s coordinator, statistician and programmer and the trial database will be signed off once the implementation of these has been assured.
Data can be entered onto the bespoke trial database by staff at BCTU, delegated staff at site or, in the case of participant completed questionnaires, the participant themselves if an on-line option is available.
Data source can be found in table 2.
Table 2.
Data source
| Data | Source |
| Participant- reported outcomes | The original participant-completed CRF is the source and will be kept with the participant’s trial record at site, while copies will be provided to the Trials Office |
| Lab results | The original lab report (which may be electronic) is the source data and will be kept and maintained in line with normal local practice. Information will be transcribed onto CRFs |
| Imaging | The source is the original imaging usually as an electronic file. Data may be supplied to the Trials Office as a password-protected, anonymised, copy of the electronic file or as an interpretation of the imaging provided on a CRF. This will be transferred via fax or secure email, and stored on a secure computer server at the University of Birmingham. Where data are interpreted, the CRF onto which it is transcribed becomes the source. A copy of the CRF should be provided to the Trials Office. |
| Clinical event data | The original clinical annotation is the source data. This may be found on clinical correspondence, or electronic or paper participant records. Clinical events reported by the participant, either in or out of clinic (eg, phone calls), must be documented in the source data. |
| Health economics data | Often obtained by interview directly with the participant for transcription onto the CRF. |
| Recruitment | The original record of the randomisation is the source. It is held on University of Birmingham servers as part of the randomisation and data entry system. |
CRF, case report form.
Discussion
The LAVA trial protocol was designed in 2019 and amended during 2020 before funding and ethical approval was granted. The trial commenced recruitment in September 2021 but failed to meet its RAG (‘red; amber; green) criteria for site set up and recruitment rate and so for this reason and the recognition by the funder (The NIHR HTA Programme) of insufficient NHS clinical and Research and Development (R&D) capacity post the COVID-19 pandemic, the trial was closed. The research question remains relevant, given that almost 30 000 hysterectomies are undertaken per year7 18 and especially now that the laparoscopic approach to hysterectomy is being facilitated further by advances in instrumentation including robotic surgery.37 38 Our research group plans to analyse qualitative and quantitative data acquired from the commencement of the trial to inform future surgical trials and aid future researchers wishing to undertake comparative trials in hysterectomy. We believe that our carefully considered protocol will be of value to future researchers working in the field of optimising clinical outcomes for women undergoing hysterectomy.
Strengths and limitations
The LAVA trial was larger than all the previous 25 RCTs evaluating laparoscopic and open hysterectomy and of higher quality, addressing the methodological deficiencies of previous trials; namely their power to show a meaningful difference, the validity of outcomes assessment, especially the key outcome of recovery and a failure to account for surgical expertise. In the LAVA trial, we used a novel, validated, personalised recovery tool16 21 22 and employed an expertise-based design to mitigate against surgical expertise bias.18 22 Third part randomisation was performed balancing important prognostic variables. Due to the differing natures of the intervention it is impossible to blind either the care providers, investigators or participants to their allocated group.
Potential impact and implications
Hysterectomy is common, with 1 in 10 women undergoing the procedure in their lifetime, mostly for benign conditions.12–14 The operation imposes substantial morbidity on women, disrupts families and impacts on wider society through utilisation of scarce healthcare resources and lost productivity.3–6 15 These burdens could potentially be reduced with safe, less invasive surgery allowing quicker recovery. Currently, most hysterectomies are performed abdominally because this traditional method is thought to minimise intraoperative complications but the increased trauma of an abdominal incision can prolong recovery.2 This may be especially true in overweight and obese women, where morbidity is greater from mobility restrictions and wound infection.16
Laparoscopic hysterectomy avoids the need for a large surgical incision speeding recovery for most women but has been associated with serious complications and specialist surgical skills. However, scientific advances in imaging and equipment, has made laparoscopic surgery easier as well as more accessible to general gynaecologists.11 16 17 Furthermore, laparoscopic surgery forms an integral part of modern packages of nursing, anaesthetic and surgical care designed to enhance recovery and allow 24-hour hospital discharge.20
The wider adoption of contemporary laparoscopic hysterectomy has the potential to minimise morbidity, expedite recovery and improve clinical outcomes for women in the short term and longer term. Furthermore, enhanced recovery has the potential to be economically advantageous to the NHS through resource efficiencies and wider society via increased productivity.
Ethics and dissemination
The study was approved by the West Midlands-Edgbaston Research Ethics Committee. REC approval for the protocol was issued on 18 February 2021. All participants gave informed consent before participation. The trial was being conducted in accordance with the Research Governance Framework for Health and Social Care, the applicable UK Statutory Instruments, (which include the Data Protection Act 1998) and the Principles of GCP.
The findings will be presented and disseminated via the BSGE, RCOG and other national and international conferences. We will also aim to publish the findings in high-impact peer-reviewed journals. We will disseminate the completed paper to the Department of Health, the Scientific Advisory Committees of the RCOG, the Royal College of Nurses (RCN) and the BSGE.
Confidentiality
Personal data recorded on all documents will be regarded as strictly confidential and will be handled and stored in accordance with the Data Protection Act 1998.
Participants will always be identified using their unique trial identification number and partial date of birth (month/year) on the CRF and correspondence between BCTU and local centres.
The investigator must maintain documents not for submission to BCTU (eg, participant identification logs) in strict confidence.
BCTU will maintain the confidentiality of all participant’s data and will not disclose information by which participants may be identified to any third party other than those directly involved in the treatment of the participant and organisations for which the participant has given explicit consent for data transfer (eg, laboratory staff, competent authority, sponsor).
Trial organisational structure
Sponsor
University of Birmingham.
Contact Details: Research Governance, University of Birmingham, Edgbaston, Birmingham, B15 2TT. Email: researchgovernance@contacts.bham.ac.uk
Coordinating centre
The trial coordinating centre (Trial Office) is Birmingham Clinical Trials Unit, based at the University of Birmingham.
Trial management group
The trial management group will take responsibility for the day-to-day management of the trial and will include (but is not limited to) the CI, coapplicants, statistician, team leader and trial manager. The role of the group is to monitor all aspects of the conduct and progress of the trial, ensure that the protocol is adhered to and take appropriate action to safeguard participants and the quality of the trial itself.
Trial steering committee
The role of the trial steering committee (TSC) is to provide the overall supervision of the trial. Ideally, the TSC should include members who are independent of the investigators, their employing organisations, funders and sponsors. The TSC should monitor trial progress and conduct and advise on scientific credibility. The TSC will consider and act, as appropriate, on the recommendations of the DMC or equivalent and ultimately carries the responsibility for deciding whether a trial needs to be stopped on grounds of safety or efficacy.
Data monitoring committee
Data analyses will be supplied in confidence to an independent DMC, which will be asked to give advice on whether the accumulated data from the trial, together with the results from other relevant research, justifies the continuing recruitment of further participants. The DMC will operate in accordance with a trial specific charter based on the template created by the Damocles Group. The DMC will meet at regular intervals that will allow them to effectively monitor the trial unless there is a specific reason (eg, safety phase) to amend the schedule.
Amendments
As sponsor, The University of Birmingham will be responsible for deciding whether an amendment is substantial or nonsubstantial. Substantive changes will be submitted to REC for approval. Once this has been received, R&D departments will be notified of the amendment and requested to provide their approval. If no response is received within 35 days, an assumption will be made that the site has no objection to the amendment and it will be implemented at the site.
Access to the final trial dataset
During the period of the study only the trial steering group will have access to the full trial dataset. Following publication of the findings, the final trial dataset will be made available to external researchers on approval from the trial management group and the BCTU data sharing committee in line with standard data sharing practices for clinical trial data sets.
Post-trial care
All patients will continue to receive standard medical care following participation in the clinical trial. There are no interventions that participant’s will be prevented from accessing after their participation in the trial has been completed.
Publication policy
Authors must acknowledge that the trial was performed with the support of the University of Birmingham and Birmingham Clinical Trials Unit. Intellectual property rights will be addressed in the Clinical Study Site Agreement between sponsor and site.
Results of the study will be shared with study participants, staff members at research sites and investigators of other studies related to hysterectomy and benign gynaecological surgery.
Auditing
The investigator will permit trial-related monitoring, audits, ethical review and regulatory inspection(s) at their site, providing direct access to source data/documents.
bmjopen-2022-070218supp002.pdf (128.2KB, pdf)
Supplementary Material
Acknowledgments
The authors thank Dr Zeyah Sairally, and Dr Lynsey Matthews for their help in the LAVA trial.
Footnotes
Twitter: @drlauraljones, @tracyrobertsbham, @TJustinC
Contributors: TJC, LM, PB, JF, MM, KC, ES, LJ, PS, TR, WM, SB and RW were involved in conception and trial design. TJC and LA and were involved in drafting of the article. TJC reviewed and critiqued the article for intellectual content. All the authors were involved in final approval of the article.
Funding: Funding for the LAVA trial is provided by an award from the National Institute of Health Research Health Technology Assessment program. Ref: NIHR128991.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Ruiz de Azua Unzurrunzaga G, Brewster DH, Wild SH, et al. Declining hysterectomy prevalence and the estimated impact on uterine cancer incidence in Scotland. Cancer Epidemiol 2019;59:227–31. 10.1016/j.canep.2019.02.008 [DOI] [PubMed] [Google Scholar]
- 2.ACOG committee opinion No.444: choosing the route of hysterectomy for benign disease. Obstet Gynecol 2009;114:1156–8. 10.1097/AOG.0b013e3181c33c72 Available: 10.1097/AOG.0b013e3181c33c72 [DOI] [PubMed] [Google Scholar]
- 3.Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2009;10:CD003677. 10.1002/14651858.CD003677.pub4 Available: [DOI] [PubMed] [Google Scholar]
- 4.Middleton LJ, Champaneria R, Daniels JP, et al. Hysterectomy, endometrial destruction, and levonorgestrel releasing Intrauterine system (Mirena) for heavy Menstrual bleeding: systematic review and meta-analysis of data from individual patients. BMJ 2010;341:c3929. 10.1136/bmj.c3929 Available: 10.1136/bmj.c3929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aarts JWM, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2015;2015:CD003677. 10.1002/14651858.CD003677.pub5 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Royal College of Obstetricians and Gynaecologists LSoHTM, Ipsos MORI . National Heavy Menstrual Bleeding Audit: Final report. London, UK: RCOG Press, 2014. Available: https://www.rcog.org.uk/globalassets/documents/guidelines/research--audit/national_hmb_audit_final_report_july_2014.pdf [Google Scholar]
- 7.Royal College of Obstetricians and Gynaecologists LU . Patterns of benign Gynaecology care in English NHS hospital trusts 2015/16. 2018. Available: https://www.rcog.org.uk/en/guidelines-research-services/audit-quality-improvement/clinical-indicators-programme/benign-gynaecological-care/benign-gynaecology-report-2015-16/
- 8.Liu Z, Doan QV, Blumenthal P, et al. A systematic review evaluating health-related quality of life, work impairment, and health-care costs and utilization in abnormal uterine bleeding. Value in Health 2007;10:183–94. 10.1111/j.1524-4733.2007.00168.x Available: [DOI] [PubMed] [Google Scholar]
- 9.Frick KD, Clark MA, Steinwachs DM, et al. Financial and quality-of-life burden of dysfunctional uterine bleeding among women agreeing to obtain surgical treatment. Women’s Health Issues 2009;19:70–8. 10.1016/j.whi.2008.07.002 Available: 10.1016/j.whi.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 10.Blikkendaal MD, Schepers EM, van Zwet EW, et al. Hysterectomy in in very obese and Morbidly obese patients: a systematic review with cumulative analysis of comparative studies. Arch Gynecol Obstet 2015;292:723–38. 10.1007/s00404-015-3680-7 Available: 10.1007/s00404-015-3680-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garry R, Fountain J, Mason S, et al. The eVALuate study: two parallel randomised trials, one comparing Laparoscopic with abdominal hysterectomy, the other comparing Laparoscopic with vaginal hysterectomy. BMJ 2004;328:129. 10.1136/bmj.37984.623889.F6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghezzi F, Uccella S, Cromi A, et al. Postoperative pain after Laparoscopic and vaginal hysterectomy for benign gynecologic disease: a randomized trial. Am J Obstet Gynecol 2010;203:118. 10.1016/j.ajog.2010.04.026 Available: 10.1016/j.ajog.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 13.Song T, Cho J, Kim T-J, et al. Cosmetic outcomes of Laparoendoscopic single-site hysterectomy compared with multi-port surgery: randomized controlled trial. J Minim Invasive Gynecol 2013;20:460–7. 10.1016/j.jmig.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 14.Paraiso MFR, Ridgeway B, Park AJ, et al. A randomized trial comparing conventional and Robotically assisted total Laparoscopic hysterectomy. Am J Obstet Gynecol 2013;208:S0002-9378(13)00144-0. 10.1016/j.ajog.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 15.Janssen MF, Bonsel GJ, Luo N. Is EQ-5D-5L better than EQ-5D-3L? A head-to-head comparison of descriptive systems and value SETS from seven countries. Pharmacoeconomics 2018;36:675–97. 10.1007/s40273-018-0623-8 Available: 10.1007/s40273-018-0623-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SH, Oh SR, Cho YJ, et al. Comparison of vaginal hysterectomy and Laparoscopic hysterectomy: a systematic review and meta-analysis. BMC Women’s Health 2019;19:83. 10.1186/s12905-019-0784-4 Available: 10.1186/s12905-019-0784-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madhvani K, Curnow T, Carpenter T. Route of hysterectomy: a retrospective, cohort study in English NHS hospitals from 2011 to 2017. BJOG 2019;126:795–802. 10.1111/1471-0528.15539 Available: 10.1111/1471-0528.15539 [DOI] [PubMed] [Google Scholar]
- 18.Cook JA, Elders A, Boachie C, et al. A systematic review of the use of an expertise-based randomised controlled trial design. Trials 2015;16:241. 10.1186/s13063-015-0739-5 Available: 10.1186/s13063-015-0739-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rose M, Bjorner JB, Gandek B, et al. The PROMIS physical function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. J Clin Epidemiol 2014;67:516–26. 10.1016/j.jclinepi.2013.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barber EL, Van Le L. Enhanced recovery pathways in Gynecology and gynecologic oncology. Obstet Gynecol Surv 2015;70:780–92. 10.1097/OGX.0000000000000259 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagen S, Glazener C, Sinclair L, et al. Psychometric properties of the pelvic organ Prolapse symptom score. BJOG 2009;116:25–31. 10.1111/j.1471-0528.2008.01903.x Available: 10.1111/j.1471-0528.2008.01903.x [DOI] [PubMed] [Google Scholar]
- 22.van Brummen HJ, Bruinse HW, van de Pol G, et al. Defecatory symptoms during and after the first pregnancy: prevalences and associated factors. Int Urogynecol J Pelvic Floor Dysfunct 2006;17:224–30. 10.1007/s00192-005-1351-0 Available: 10.1007/s00192-005-1351-0 [DOI] [PubMed] [Google Scholar]
- 23.Thirlaway K, Fallowfield L, Cuzick J. The sexual activity questionnaire: a measure of women’s sexual functioning. Qual Life Res 1996;5:81–90. 10.1007/BF00435972 Available: 10.1007/BF00435972 [DOI] [PubMed] [Google Scholar]
- 24.Makinen J. Morbidity of 10110 Hysterectomies by type approach. Human Reproduction 2001;16:1473–8. 10.1093/humrep/16.7.1473 [DOI] [PubMed] [Google Scholar]
- 25.Twijnstra AR, Blikkendaal MD, van Zwet EW, et al. Predictors of successful surgical outcome in Laparoscopic hysterectomy. Obstet Gynecol 2012;119:700–8. 10.1097/AOG.0b013e31824b1966 [DOI] [PubMed] [Google Scholar]
- 26.Glaser LM, Brennan L, King LP, et al. Surgeon volume in benign gynecologic surgery: review of outcomes, impact on training, and ethical contexts. J Minim Invasive Gynecol 2019;26:279–87. 10.1016/j.jmig.2018.09.775 [DOI] [PubMed] [Google Scholar]
- 27.Mowat A, Maher C, Ballard E. Surgical outcomes for low-volume vs high-volume Surgeons in Gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol 2016;215:21–33. 10.1016/j.ajog.2016.02.048 [DOI] [PubMed] [Google Scholar]
- 28.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. 10.1097/01.sla.0000133083.54934.ae Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Euroqol--a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. 10.1016/0168-8510(90)90421-9 Available: 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 30.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993;4:353–65. 10.2165/00019053-199304050-00006 Available: 10.2165/00019053-199304050-00006 [DOI] [PubMed] [Google Scholar]
- 31.Groenendijk AG, Birnie E, Roovers J-PW, et al. Contribution of primary pelvic organ Prolapse to micturition and Defecation symptoms. Obstet Gynecol Int 2012;2012:798035. 10.1155/2012/798035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uebersax JS, Wyman JF, Shumaker SA, et al. Short forms to assess life quality and symptom distress for urinary Incontinence in women: the Incontinence impact questionnaire and the Urogenital distress inventory. Neurourol Urodyn 1995;14:131–9. 10.1002/nau.1930140206 Available: 10.1002/nau.1930140206 [DOI] [PubMed] [Google Scholar]
- 33.Hopwood P, Fletcher I, Lee A, et al. A body image scale for use with cancer patients. Eur J Cancer 2001;37:189–97. 10.1016/s0959-8049(00)00353-1 Available: 10.1016/s0959-8049(00)00353-1 [DOI] [PubMed] [Google Scholar]
- 34.Hewitt CE, Torgerson DJ, Miles JNV. Is there another way to take account of noncompliance in randomized controlled trials CMAJ 2006;175:347. 10.1503/cmaj.051625 Available: 10.1503/cmaj.051625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huque MF, Dmitrienko A, D’Agostino R. Multiplicity issues in clinical trials with multiple objectives. Statistics in Biopharmaceutical Research 2013;5:321–37. 10.1080/19466315.2013.807749 [DOI] [Google Scholar]
- 36.Austin PC. A Tutorial on Multilevel survival analysis: methods, models and applications. Int Stat Rev 2017;85:185–203. 10.1111/insr.12214 Available: 10.1111/insr.12214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gitas G, Hanker L, Rody A, et al. Robotic surgery in Gynecology: is the future already here Minimally Invasive Therapy & Allied Technologies 2022;31:815–24. 10.1080/13645706.2021.2010763 [DOI] [PubMed] [Google Scholar]
- 38.Totaro A, Campetella M, Bientinesi R, et al. The new surgical Robotic platform HUGOTM RAS: system description and dOcking settings for robot-assisted radical Prostatectomy. Urologia 2022;89:603–9. 10.1177/03915603221107855 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-070218supp001.pdf (42.6KB, pdf)
bmjopen-2022-070218supp002.pdf (128.2KB, pdf)