Abstract
Payment for dental services is one of the key determinants of treatment options, access to health care, and treatment decisions. The ability to pay for services directly affects the quality of life of an individual and also their accessibility to oral health services. The aim of the present study was to identify the different methods of payment used to obtain oral health care in Yaoundé, Cameroon This was a cross-sectional descriptive study carried out in selected dental clinics in Yaoundé using convenient sampling between January 2021 and June 2021. Data was collected using a structured questionnaire. A total of 377 patients aged 8 to 83 years made up of 194 (51.46%) females and 183 (48.54%) males participated in the study. There is no government-assisted package for oral health care in Cameroon and more than two-thirds (66.84%) made direct payments or paid out of pocket without a refund from any insurance company. More than half 147 (58.33%) of the study population did not complete the planned dental care due to insufficient funds. Direct payments covered treatments such as scaling, restorations, root canal therapy, and dental extractions while prostheses (dentures, crowns, bridges, and implants) were only afforded by very few patients. The reasons for the inability to pay for dental services included financial difficulties 107 (72.97%) and lack of time 36 (24.49%). Only half 36 (50%) of the participants employed in the formal sector had access to health insurance and treatments like scaling, dental prosthesis, orthodontics, and dental implants were rarely provided by an insurance company. These procedures were considered to be very expensive with fluctuating prices and were viewed as being for aesthetic purposes. The majority 67 (93.06%) of payments through insurance reported being reimbursed aftercare. Two-thirds of 48 (71.64%) of the insured participants said it was difficult to get reimbursed due to the administrative bottlenecks and as such some preferred to pay out of pocket despite being insured. Late consultations encountered led to caries complications with 105 (52.24%) pulpitis. In general, financial difficulty was reported by 97 (48.26%) as the main reason for not being able to afford dental care. Oral diseases present a huge burden for children and adults due to the high cost of treatment limiting their accessibility and treatment options. There is a need to create compulsory health insurance to enhance greater access to oral health services to encourage the population to seek dental care timeously.
Key words: methods of payment, insurance, oral health care, direct payment, Yaoundé
Introduction
Orofacial diseases are rampant globally as it affects a huge proportion of the world’s population. The importance of oral health cannot be overstated as it impacts physical, emotional, psychological, and socioeconomic well-being, not only at the individual level but also at interpersonal (e.g., family, friends), community, and societal levels.1
One of the major problems of access to oral health care is disparities associated with individual or communal financing of oral health services. Inadequate financing makes it difficult for a health system to achieve its objectives such as the ease of citizens to access health care services, the provision of cost-effective healthcare as well as to meet certain established standards of quality of care.
New and expensive state-of-the-art technology accounts for some of the reasons oral health care is expensive. Financing health is an important aspect of development in a community because healthy populations tend to be more productive and help in the development of the community.2 Though oral health services operate at their maximum in some developed countries, people are more likely to have poor oral health if they are low-income, uninsured, and/or members of racial/ethnic minority, immigrant, or rural populations who have suboptimal access to quality oral health care.1,3 As a result, poor oral health serves as the national symbol of social inequality.2
Irrespective of the high burden of oral health diseases, oral health services are inadequate and unevenly distributed in many developing countries, particularly those in sub-Saharan Africa.3 Rural areas in these countries and poorer sections of the population in urban areas often do not have access to oral health services mainly because of a significant shortage of dentists and the high costs of care.3
Oral diseases affect 3.9 billion people worldwide, impacting almost half of the world’s population, and the fourth most expensive to treat.4,5 The oral health service demands are beyond the capacities of the many health systems in low-middle-income countries. This results in a high proportion of oral diseases being untreated and leads to significant unmet patient needs.2,4 Moreover, even in high-income settings dental treatment is costly, averaging 5% of total health expenditure.5 The increased cost of health is due to the public’s increasing demand for health services, ever-growing technology of health care, lack of incentives in health care, higher quality of health care, and general inflation.
As the cost of dental care continues to rise, the majority of people are not able to afford dental treatment. Preventive measures are not given much importance for various reasons including high costs. This places a large burden on households, especially the poor and indigent.3 Taking into account all the above, many developed countries have guaranteed the accessibility of health through universal health coverage, where oral health care systems are financed through general taxation or social insurance, and the role of private services is significant.2
In developing countries oral health still remains an issue. Oral health services are inadequate in many developing countries, particularly those in Sub-Saharan Africa.2 Access to oral health services is limited, treatment is limited to pain and sepsis and teeth are often untreated or are extracted because of pain or discomfort.2,3 The few available dentists are located in urban areas, leaving most people with very limited access to affordable oral health care.
In Cameroon, there are no national oral health prevention programs. Oral health care is not a priority and a few oral health education programs are organized by Non-Governmental Organization (NGO) or the religious community.6 The minimum monthly wage of an average Cameroonian is US$63 which is one of the lowest in the Central Africa sub-region.7 The lack of universal health coverage, low wages, and poor oral health education motivated the present study whose aim was to determine the methods of payment for oral health care in Yaounde town.
Materials and Methods
This was a cross-sectional descriptive study carried out in selected dental clinics in Yaounde, the political capital of Cameroon between February and June 2020.
Yaounde is an urban city hosting more than half of the dental clinics in Cameroon. It has 48 dental clinics (private, public, and private confessional) registered with the national order of dental surgeons. The study population was made up of all patients who consulted at the selected dental clinics and accepted to participate in our study using a consecutive sampling technique. Clinics were selected randomly and classified into public, confessional, and private clinics.
Data was collected using a questionnaire (Supplementary material). The questionnaire was used to collect information on socio-demography (age, gender), the different types of planned dental treatment, types of treatment that could not be done as a result of lack of finance, the methods of payment of treatments, and the consequences of not receiving dental treatment. Data analysis was carried out with Epi-info 7.
Ethical clearance was obtained from the Research Committee and the Institutional Ethical Committee of Université des Montagnes, Cameroon, and the Ethical Committee of the Yaoundé General Hospital Research authorization from the Institutional Ethics Committee of Université des Montagnes. Research authorization to carry out the study was also obtained from the regional delegate of public health of the center region and from different directors of hospitals, the head doctors, and dentists in different cabinets.
Results
Socio-demographic profile
A total of 377 individuals aged between 8 to 83 years (mean age 34.11±14.2 s.d years and a median age of 32 years) participated. Just over half (51%) were females. More than half 175 (60.1%) were employed, 75(19.8%) were housewives, 70 (18.57%) were students, 38 (10.1%) were retired and 19 (3.0%) were unemployed (Table 1). The most represented age groups were 20-30 years and 30-40 years with 108 (28.7%) people in each group respectively.
Methods of payment for oral health care
More than a third 154 (40.8%) preferred public hospitals as compared to other health facilities. More than two-thirds 252 (66.8%) used direct payment or out-of-pocket method for their dental needs, 72 (19.1%) through insurance and 53 (14.1%) used both insurance and direct payment (co-insurance) (Figure 1).
Sources of finances
Individual payments for dental services account for 62.1% of all payments which constitute 52 (40.3%) direct payments from individuals and 50 (13.1%) from individual insurance. Parents 97 (25.7%) and spouses 31 (8.2%) respectively constituted a significant source of payments (Table 2).
Planned dental care
A third 269 (30%) of all dental treatment planned in the clinic was scaling and polishing, 226 (25%) obturations or fillings, 172 (19%) endodontic treatment, 159 (18%) extractions, 59 (6%) dental prostheses, 10 (1%) minor oral surgery, orthodontic treatment 7 (1%) and dental implants 6 (1%).
Realization of care
More than half 147 (58.33%) using the direct method of payment affirmed to not have completed the planned dental care.
Dental care is not covered by most insurance
We also noticed that not all dental treatments were covered by insurance. Dental treatments like scaling, prosthetics, orthodontics, and dental implants were rarely or not covered by insurance.
Unrealized dental care in the direct method of payment
Scaling 82 (55.78%) was the highest dental care patients requested, followed by root canal therapy and filling (Table 1). Financial difficulty was the most common reason given for abandoning dental treatment (72.79%) (Table 3).
Professional affiliations of the insured
Half 36 (50%) of the insured were employees of the formal sector, 19(26%) were employees of the informal sector, 9(13%) were students, 8(11%) were retirees (Figure 2).
The reimbursement procedure
The majority 67 (93.06%) were reimbursed aftercare but 48 (71.64%) said the reimbursement procedure was not easy.
Consequences due to non-payment for oral care
The main reasons why people consulted the dental clinic were because of caries and periodontal (gum) diseases. Notwithstanding they only came when it was at an advanced stage which led to complications.
Consequence of not paying for dental care
Pulpitis 105 (52%), periapical pathologies 54 (27%) and pulp necrosis 32 (16%) were the complications associated with dental caries due to late payment of treatment (Figure 3).
Reasons mentioned
Cost of treatment 97 (48%), negligence 72 (36%), fear of the dentist 29 (14%), and 3 (1%) location of the clinic were the reasons for late presentation to the clinic (Figure 4).
Table 1.
Utilization of health facility and socio-demographic profile.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| Health sector | ||
| Public | 154 | 40.85 |
| Private | 136 | 36.07 |
| Confessional | 87 | 23.08 |
| Gender | ||
| Female | 194 | 51.5 |
| Male | 183 | 48.5 |
| Age range (years) | ||
| <10 | 3 | 0.8 |
| 10-20 | 50 | 13.3 |
| 20-30 | 108 | 28.7 |
| 30-40 | 108 | 28.7 |
| 40-50 | 47 | 12.7 |
| 50-60 | 61 | 16.1 |
| 60-70 | 7.4 | |
| 70 | 0.8 | |
| Professional profile | ||
| Employed | 175 | 60.1 |
| House wives | 75 | 19.8 |
| Students/ pupils | 70 | 18.6 |
| Retired | 38 | 10.1 |
| Unemployed | 19 | 3.0 |
| Total | 377 | 100.00 |
Figure 1.

Unrealized dental care.
Table 2.
Sources of finance and methods of payment for oral care.
| Origin | Direct (%) | Insurance (%) | Mixed (%) | Total |
|---|---|---|---|---|
| Individua | 152 (40.3) | 50 (13.1) | 32 (8.4) | 234 (62.1) |
| Parent | 71 (18.8) | 13 (3.4) | 13 (3.4) | 97 (25.7) |
| Spouse | 19 (5.0) | 7 (2.17) | 5 (1.3) | 31 (8.2) |
| Others | 10 (2.6) | 2 (0.5) | 3 (0.8) | 15 (3.9) |
| Total | 252 (66.7) | 72 (18.9) | 53 (13.9) | 377 (100.00) |
Table 3.
Reasons evoked for renouncing dental care.
| Reasons | Frequency | Percentages (%) |
|---|---|---|
| Financial difficulties | 107 | 72.79 |
| Lack of time | 36 | 24.49 |
| Other reasons | 4 | 2.72 |
| Total | 147 | 100.00 |
Figure 2.

Insured population according to professional affiliation.
Discussion
The present study revealed that more than half of the participants used direct methods of payment for dental services, those who were insured for dental services were from the formal sector, and dental treatments like scaling, prostheses, orthodontics, and dental implants were rarely or not covered by insurance. The study also revealed that the high cost of treatment is responsible for poor access to oral care as well as limiting treatment options.
Just over half of the study participants were females. Shaffer et al. (2015) in the United States of America and Hamasha et al. (2018) in Saudi Arabia reported that women are at a higher risk of dental pathologies and experience more carious lesions than men, and why they frequent dental clinics than men.8,9 Generally, women have a more positive oral health-seeking behavior than men. The present study found that middle-aged adults constituted the majority of the population who utilized dental services. Since this group constitutes the active workforce and independent group, it is unusual that they tended to go to the hospital when they are able to finance their treatments and were financially capable of handling payment for medical services themselves.
Figure 3.

Caries complications and consequences.
Figure 4.
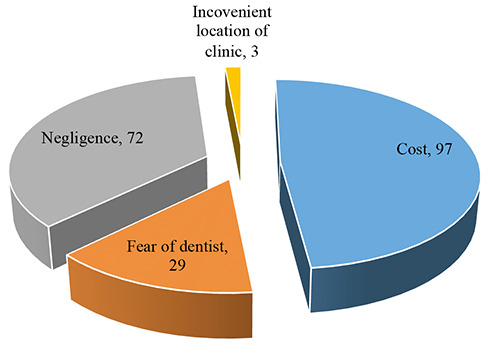
Different reasons mentioned.
Just under half (40.85%) preferred the public hospitals, 136 (36.07%) the private sector, and 87 (23.08%) used the mission hospital. These findings corroborate the study carried out by Shu (2010) on service quality and patient choice of hospitals in Cameroon where 115 (47.1%) participants preferred the public health and private health facilities.11 This could be due to the fact that the public sector has more structured technical support, higher budget allocations, an increasing number of doctors and implement relatively low charges, which are affordable health care services and medications. Due to these advantages, people preferred the public sector, although the private sector is well known for its sophisticated, up-to-date equipment and less waiting time for patients, due to its high cost, it is not accessible to everyone.
In the present study, more than two-thirds of the participants paid for their dental treatment through direct payment or out-ofpocket payment, corroborating the recent World Health Organisation’s finding that 66.3% of the Cameroonian population pays for their health needs through direct payment.12 Direct payment for health care is still high in Cameroon because of the small formal sector of the economy and the universal health care system of the country is grossly underdeveloped. In the present study, this method of payment is very high because the study was carried out in an urban area where the purchasing power of urban dwellers is high. The primary oral health care sector of Cameroon is grossly underdeveloped and insurance cover in rural areas is almost absent.
In the present study, a quarter of the participants paid for oral health care by insurance. This contrasts with reports from the Bureau International du Travail for Central Africa (2016) that estimated that only 2% of the population in Cameroon is insured.12 This could be due to the fact that half of the participants with insurance policies were employees who receive health insurance through their employment. Younoussa (2017) reported that less than 25% of Cameroonians have health insurance due to a lack of constant sources of income and that insurance was affordable only to a particular group of people.14 Scaling, prosthetics, orthodontics and dental implants were rarely or not covered by insurance. Scaling was judged to be an aesthetic care and as a result, should not be included in the insurance coverage; dental prostheses, orthodontics, and dental implants were considered to be very costly with fluctuating prices.
Another hindrance to access to oral care among those that were insured was administrative paperwork. Two-thirds of the participants reported that it was difficult to recover the money from their insurance company after payment. The reimbursement process was long, difficult, and time-consuming, and hence, despite being insured some preferred to pay for dental care out of pocket. Inadequate feedback from the insurance companies and throughput bottlenecks have led to high dropout of the insured and overall low population coverage.15 Insurance companies need to collaborate with clinics or hospitals to completely cover the costs of the clients or inform their clients of clinics that they can be reimbursed after treatment, in so doing, this will reduce reimbursement and waiting time and this will encourage the utilization of dental services and reduce default. While scaling and fillings were the most needed dental care, most insurance companies did not cover dental prophylaxis in the form of scaling and polishing. Basic and routine professional teeth cleaning should be covered by insurance as a preventive measure that will help remove plaque, the main risk factor for dental caries and periodontal diseases. More than half reported that they did not complete their treatment for financial reasons. The treatments not covered were scaling, root canal therapy, and fillings. Vujicic et al. (2016) found that a perceived high cost of dental treatment was the main reason for not accessing needed dental care irrespective of age, income level, and type of insurance. They also observed that many people reported financial barriers to receive dental care than they did for any other type of health care.16 In Cameroon, oral healthcare-seeking behavior is motivated by symptomatic presentations like a toothache; people do not see the importance of scaling, considering it as unnecessary especially when their symptoms are relieved.
Many sought treatment when their oral disease was already at an advanced stage. Late consultation counted for more than 70% of the people and led to the dental caries complications, such as pulpitis. Other complications included pulp necrosis, peri-apical lesions, cellulitis, and abscess. The main reason for seeking care at such a late stage was financial difficulty. Agbor et al. (2018) reported that in Cameroon, self-medication in the management of toothache remains the main reason for late consultations, followed by a lack of awareness and financial difficulties.17 In the present study, negligence, fear of the dentist, and the awkward location of clinics were some of the reasons for the late presentation.
Conclusions
The universal healthcare system of Cameroon is grossly inadequate to take care of the oral health needs of the population. The majority of Cameroonians use direct payment, few have insurance coverage for dental care, and half of the individuals are from the formal sector. Insurance coverage is not complete and restricts the treatment options and accessibilities of patients. Lack of finance, lack of time, and distance to dental services are the reasons for poor access to oral health, because of inadequate financing, patients presented with complications of dental caries such as pulpitis, pulp necrosis, and periapical lesions.
Recommendation
The formal and informal sectors of the economy should make efforts to procure health insurance policies. The Ministry of Public Health put in place an effective health insurance policy that will benefit all Cameroonians irrespective of their affiliation or income. The Ministry of Public Health should invest in preventive dentistry in order to reduce the burden of oral diseases in the country by instituting free oral health outreach programs targeting vulnerable groups like children 3-16 years old and adults above 60 years of age. The ministry should also ensure the even distribution of dentists both in rural and urban areas for the availability and accessibility of oral health services. A review of the prices should be carried out by oral healthcare givers and the Ministry of Health.
References
- 1.Northridge ME, Kumar A, Kaur R. Disparities in Access to Oral Health Care. Annu Rev Pub Health 2020;41:513-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mach EP. The financing of health systems in developing countries: discussion paper. Soc Sci Med 1978;12:7-11. [PubMed] [Google Scholar]
- 3.Achembong LN, Ashu AM, Hagopian A, et al. Cameroon midlevel providers offer a promising public health dentistry model. Hum Resour Health. 2012;10:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin LJ, Lamster IB, Greenspan JS, et al. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis 2016;22:609-19. [DOI] [PubMed] [Google Scholar]
- 5.Heilmann A, Tsakos G, Watt RG. Oral health over the life course. In a life course perspective on health trajectories and transitions. Springer cham; 2015:39-59. [Google Scholar]
- 6.Agbor AM, Azodo CC, Naidoo S. The Oral Health workforce in Cameroon; the past, the present and the future. Afr J Oral Health 2018;7:1-9. [Google Scholar]
- 7.Minimum wage of Cameroon. Available from: https://www.minimum-wage.org/international/cameroon#:~:text=Cameroon's%20Minimum%20Wage%20is%20the,all%20employees%20in%20all%20sectors. (Accessed on 06/02/2022). [Google Scholar]
- 8.Shaffer JR, Leslie EJ, Feingold E, et al. Caries experience differs between females and males across age groups in Northern Appalachia. Int J Dent 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamasha AA, Alshehri A, Alshubaiki A, et al. Gender-specific oral health beliefs and behaviors among adult patients attending king Abdulaziz Medical City in Riyadh. Saudi Dent J 2018;30:226-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shu CA. Public and private hospitals in Cameroon: service quality and patients’ choice of hospitals. Eastern Mediterranean University (EMU), 2010. [Google Scholar]
- 11.Bertrand NA. Analysis of determinants of public hospitals efficiency in Cameroon. African Economic Research Consortium; 2012. [Google Scholar]
- 12.World Health Organization. Primary health care systems. A case study from Cameroon. Available from: https://www.who.int/alliance-hpsr/projects/alliancehpsr_cameroon_abridgedprimasys2018.pdf. (Accessed on 26/02/2022). [Google Scholar]
- 13.L’équipe d’appui technique du Bureau Internationale du Travail (BIT) pour l’Afrique Centrale. Cameroun-sécurité sociale: Lancement d’un système de couverture universelle en santé au Cameroun. 2016. [Google Scholar]
- 14.Younoussa BM. L’assurance maladie. Cameroun; complication, l’assurance maladie, une affaire d’elite. 2017. [Google Scholar]
- 15.Gurung GB, Panza A. Implementation bottlenecks of the National Health Insurance program in Nepal: Paving the path towards Universal Health Coverage: A qualitative study. Int J Health Plann Manage 2022;37:171-88. [DOI] [PubMed] [Google Scholar]
- 16.Vujicic M, Buchmueller T, Klein R. Dental Care presents the highest level of financial barriers, Compared to other types of Health Care Services. Health Affairs 2016;35:2176-82. [DOI] [PubMed] [Google Scholar]
- 17.Agbor MA., Dematou F, Azodo CC. Reasons for Late Dental Consultations at the Central Hospital of Yaoundé. Cameroon”. EC Dental Science 2018;4:360-7. [Google Scholar]


