Abstract
Background:
We aim to explore the factors related to job satisfaction among pain physicians and identify the reasons why individuals minimize or stop practicing outpatient pain medicine.
Objectives/Study Design:
This is a survey-based study with the primary goal to identify factors determining job satisfaction and dissatisfaction among pain medicine fellowship graduates who continue to practice and those who are no longer practicing interventional pain. A secondary goal is to elucidate reasons for anesthesiologists trained in pain medicine to leave pain medicine, despite an additional year of training, and to work as general anesthesiologists.
Methods:
In this study, all 114 pain program directors listed on the Accreditation Council for Graduate Medical Education (ACGME) website, or their administrative assistants were directly contacted via email. All email addresses were obtained from the ACGME website. The survey opened in September 2021, with reminder emails sent before the closing of the survey in December 2021. A final reminder email was sent 4 weeks prior to the closing of the survey.
Results:
Of all the respondents, 79 (89.77%) were currently practicing pain medicine, and 9 (10.23%) were no longer practicing pain medicine.
Limitations:
Our study has a major limitation as we are unable to determine the response rate and are limited in the data points gathered.
Conclusion:
We hope this study will allow for pain medicine fellowship program directors to improve recruitment and retention of pain fellows in the field while addressing the pros and cons of future career aspirations with anesthesiology residents prior to fellowship selection. A larger, more thorough study with an exact response rate can compare the various outcomes based upon different types of settings, such as private practice, partnership, and academia, as well as geographical locations.
Keywords: Burnout, pain medicine, fellowship selection, job satisfaction, retention
Physician career longevity and happiness appear to be a complex combination of multiple variables. Job satisfaction has been defined as a multidimensional construct and a product of the global evaluation of one’s workplace and context (1). Romito and colleagues described burnout as a result of chronic, unmanaged workplace stress with physiological dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis. Burnout can tie into mental health disorders, substance abuse, and other disease processes leading to long-term health consequences (2). Additionally, burnout may potentially be associated with higher levels of pro-inflammatory biomarkers (3).
It is reasonable to consider job satisfaction in pain medicine to be of equal importance to pain physicians as it is for practitioners of other medical specialties. The number of pain physicians who leave pain practice is on the rise, and the rate of exit could potentially be higher in physicians with a core specialty training in anesthesiology as opposed to other fields. In a study by Kroll et al (4), 207 pain physicians were surveyed, with 60.4% reporting high emotional exhaustion, 35.7% reporting high depersonalization, and 19.3% reporting low personal accomplishment. This alarming tendency highlights a need to identify the factors that play a role in job retention among pain medicine fellowship graduates and serves as the basis for our questionnaire study. We aim to explore the factors related to job satisfaction among pain physicians and identify the reasons why individuals minimize or stop practicing outpatient pain medicine.
In academic medical centers, many anesthesiologists who are trained in pain medicine may begin their careers with a hybrid practice and then transition to practice more general anesthesiology. Hyman et al (5) analyzed data from 1,303 subspecialty-trained anesthesiologists and found that chronic pain physicians had greater burnout metrics compared to pediatric or cardiac anesthesiology; critical care anesthesiologists report burnout rates close to 55% (5,6). Additionally, a recent Medscape survey of 13,000 physicians across 29 specialties demonstrated an 8% increase in anesthesiologists’ salaries over the past year, with 86% of surveyed anesthesiologists stating they would choose the same specialty again. Paperwork and administrative time in anesthesiology were the lowest of all specialties included (7). Academic anesthesiologists may have a higher degree of job satisfaction in comparison to colleagues in other practice environments (8). We believe that the main reason physicians leave pain practices is a combination of financial pressure coupled with decreasing reimbursements, challenging patient interactions, and increased documentation demands from electronic medical records. We contend that it is not a lack of interest in the medical side of the field but rather external pressures that may lead people to gravitate toward anesthesiology.
The primary objective of this study is to identify factors determining job satisfaction and dissatisfaction among pain medicine fellowship graduates who continue to practice and those who are no longer practicing interventional pain. A secondary goal is to elucidate reasons for anesthesiologists trained in pain medicine to leave pain medicine and work as general anesthesiologists. We hope this will allow for pain medicine fellowship program directors to improve recruitment and retention of pain fellows in the field while addressing the pros and cons of future career aspirations with anesthesiology residents prior to fellowship selection.
Methods
Study Design
The attached survey attempts to identify reasons for an anesthesiologist to choose to pursue pain medicine fellowship training yet eventually limit their time spent in that area. The survey is broken down into 4 main sections, with the first section collecting demographics, the second addressing practice background, the third identifying the motivations and expectations of pursuing a pain medicine fellowship, and the fourth gathering reasons for either continuing to practice pain medicine or to leave pain medicine. The last 2 sections are further divided into 3 subgroups— patient-physician, medical, or financial/lifestyle. In addition, a percentile range is used to gather responses from numerous questions in the survey pertaining to practice patterns.
In this study, all 114 pain program directors listed on the Accreditation Council for Graduate Medical Education (ACGME) website, or their administrative assistants were directly contacted via email. All email addresses were obtained from the ACGME website. The survey opened in September 2021, with reminder emails sent before the closing of the survey in December 2021. A final reminder email was sent 4 weeks prior to the closing of the survey.
The survey primarily targeted anesthesiologists currently practicing pain medicine and those who have practiced pain medicine in the past and transitioned to primarily or only general anesthesiology. An electronic link for the survey posted on survey monkey was emailed to the program directors, who were then asked to forward this email to all pain medicine fellowship alumni. The surveys contained a disclaimer on the first page stating that the survey was completely voluntary and anonymous. In addition to that, the survey clearly informed participants that survey submission grants the authors permission to analyze and publish any data provided by the respondent.
Sample Size Calculation
This survey attempted to collect data from all the pain medicine ACGME institutions in the United States. Based on our own and other program statistics, pain doctors comprise around 20% of the attending physician population among anesthesiologists. Our goal was to gather information from around 150 potential survey responders with an anticipated 80% response rate. Analysis of missing data methods was decided after identifying the pattern of the missing data. Surveys with important missing data or incomplete surveys were excluded from the data analysis.
Statistical Methods
Analysis of this data is descriptive. Categorical variables are summarized using count and percentage and compared between practitioner groups using Fisher’s exact test. Continuous variables are summarized using median and interquartile range (IQR) and compared between practitioner groups using the Wilcoxon rank sum test. Current practitioners and practitioners that stopped practicing had a separate set of questions, and these are described separately. We have identified characteristics that differentiate currently practicing pain physicians from those who minimize practicing pain.
Results
Demographics
The survey was sent to 114 ACGME pain program directors via email, and a total of 95 physicians participated in the survey. The response rate is unknown as it cannot be determined how many physicians received the survey from the 114 program directors, but this was a lower response than expected. The mean survey time was 2 minutes and 51 seconds. The survey was first distributed on August 24, 2021. Two follow-up reminder emails were sent in October 2021 and November 2021. We received 45 responses (47%) between August 2021 and October 2021 after the initial email, 30 responses (32%) between October 2021 and November 2021 after the first reminder email, and 20 responses (21%) between November 2021 and January 2022 after the second and final reminder email. The survey was officially closed on December 31, 2021.
Participant characteristics for the 88 pain physicians met the inclusion criteria for analysis are presented in Table 1. Physicians who did not complete accredited fellowship training in pain medicine (n = 3) and pain physicians who did not report whether they are currently practicing pain medicine (n = 4) were excluded. All 88 respondents had completed accredited fellowship training in pain medicine, and 78 (88.64%) had obtained American Board of Anesthesiology (ABA) subspecialty certification in pain medicine. The majority of physicians were between the ages of 36 to 45 (54.5%), followed by physicians aged 25 to 35 (29.5%), 46 to 55 (10.23%), 56 to 65 (4.5%), and > 65 (1.1%). Of the respondents, 50 (56.82%) were men, and 38 (43.18%) were women. Responders most commonly completed fellowship 3 to 5 years ago (35.2%), less than 3 (25%), 6 to 8 (15.9%), 12 to 20 (14.8%), and 9 to 11 (9.1%). Of all the respondents, 79 (89.77%) were currently practicing pain medicine, and 9 (10.23%) were no longer practicing pain medicine.
Table 1.
Participant characteristics.
| Currently Practicing Pain Medicine | ||||
|---|---|---|---|---|
| No (n = 9) |
Yes (n = 79) |
Total (n = 88) |
P value |
|
| Accredited Pain Medicine Fellowship | ||||
| Yes | 9 (100.00%) | 79 (100.00%) | 88 (100.00%) | |
| Missing | 0 | 0 | 0 | |
| Age | ||||
| 25 to 35 | 2 (22.22%) | 24 (30.38%) | 26 (29.55%) | 0.211 |
| 36 to 45 | 6 (66.67%) | 42 (53.16%) | 48 (54.55%) | |
| 46 to 55 | 0 (0.00%) | 9 (11.39%) | 9 (10.23%) | |
| 56 to 65 | 0 (0.00%) | 4 (5.06%) | 4 (4.55%) | |
| >65 | 1 (11.11%) | 0 (0.00%) | 1 (1.14%) | |
| Missing | 0 | 0 | 0 | |
| Gender | ||||
| Man | 5 (55.56%) | 45 (56.96%) | 50 (56.82%) | 1.000 |
| Woman | 4 (44.44%) | 34 (43.04%) | 38 (43.18%) | |
| Missing | 0 | 0 | 0 | |
| Years Since Completed Fellowship | ||||
| 12 to 20 | 2 (22.22%) | 11 (13.92%) | 13 (14.77%) | 0.126 |
| 3 to 5 | 6 (66.67%) | 25 (31.65%) | 31 (35.23%) | |
| 6 to 8 | 1 (11.11%) | 13 (16.46%) | 14 (15.91%) | |
| 9 to 11 | 0 (0.00%) | 8 (10.13%) | 8 (9.09%) | |
| Less than 3 | 0 (0.00%) | 22 (27.85%) | 22 (25.00%) | |
| Missing | 0 | 0 | 0 | |
| ABA Subspecialty Certification | ||||
| No | 1 (11.11%) | 9 (11.39%) | 10 (11.36%) | 1.000 |
| Yes | 8 (88.89%) | 70 (88.61%) | 78 (88.64%) | |
| Missing | 0 | 0 | 0 | |
| When Decided to Pursue Pain Medicine | ||||
| After residency | 2 (25.00%) | 6 (8.00%) | 8 (9.64%) | 0.288 |
| Before residency | 2 (25.00%) | 21 (28.00%) | 23 (27.71%) | |
| During residency | 4 (50.00%) | 48 (64.00%) | 52 (62.65%) | |
| Missing | 1 | 4 | 5 | |
| Setting Envisioned: Academic Organization | ||||
| No | 3 (33.33%) | 35 (44.30%) | 38 (43.18%) | 0.726 |
| Yes | 6 (66.67%) | 44 (55.70%) | 50 (56.82%) | |
| Missing | 0 | 0 | 0 | |
| Setting Envisioned: Private Group Practice | ||||
| No | 5 (55.56%) | 44 (55.70%) | 49 (55.68%) | 1.000 |
| Yes | 04 (44.44%) | 35 (44.30%) | 39 (44.32%) | |
| Missing | 0 | 0 | 0 | |
| Setting Envisioned: Single Specialty Practice | ||||
| No | 8 (88.89%) | 69 (87.34%) | 77 (87.50%) | 1.000 |
| Yes | 1 (11.11%) | 10 (12.66%) | 11 (12.50%) | |
| Missing | 0 | 0 | 0 | |
| Setting Envisioned: Multi-Specialty Practice | ||||
| No | 6 (66.67%) | 55 (69.62%) | 61 (69.32%) | 1.000 |
| Yes | 3 (33.33%) | 24 (30.38%) | 27 (30.68%) | |
| Missing | 0 | 0 | 0 | |
| Setting Envisioned: Solo Practice | ||||
| No | 9 (100.00%) | 73 (92.41%) | 82 (93.18%) | 1.000 |
| Yes | 0 (0.00%) | 6 (7.59%) | 6 (6.82%) | |
| Missing | 0 | 0 | 0 | |
| Percent of Time Envisioned: Inpatient | ||||
| Median (IQRa) | 15.5 (2.0 – 30.0) | 10.0 (0.0 – 25.0) | 10.0 (0.0 – 25.0) | 0.515 |
| Range | 0.00 – 50.00 | 0.00 – 100.00 | 0.00 – 100.00 | |
| Percent of Time Envisioned: Outpatient | ||||
| Median (IQR) | 80.5 (50.0 – 98.0) | 80.0 (51.0 – 100.0) | 80.0 (50.0 – 100.0) | 0.722 |
| Range | 35.00 – 100.00 | 20.00 – 100.00 | 20.00 – 100.00 | |
| Percent of Time Envisioned: Anesthesia | ||||
| Median (IQR) | 5.5 (0.0 – 50.0) | 10.0 (0.0 – 29.0) | 10.0 (0.0 – 30.0) | 0.780 |
| Range | 0.00 – 50.00 | 0.00 – 63.00 | 0.00 – 63.00 | |
Interquartile Range
Demographic variables were not statistically different between participants currently practicing pain medicine and those who no longer practice pain medicine based upon age (P = 0.211), gender (P = 1.000), years since fellowship (P = 0.126), ABA subspecialty certification (P = 1.000), when participants decided to pursue a career in pain (P = 0.288), or work setting envisioned (academic, private group practice, single specialty, multi-specialty, solo practice). There was no statistically significant difference between the participants currently practicing pain medicine and those who no longer practice pain medicine based upon envisioned time allocation in inpatient (P = 0.515), outpatient (0.722), or anesthesia settings (0.780).
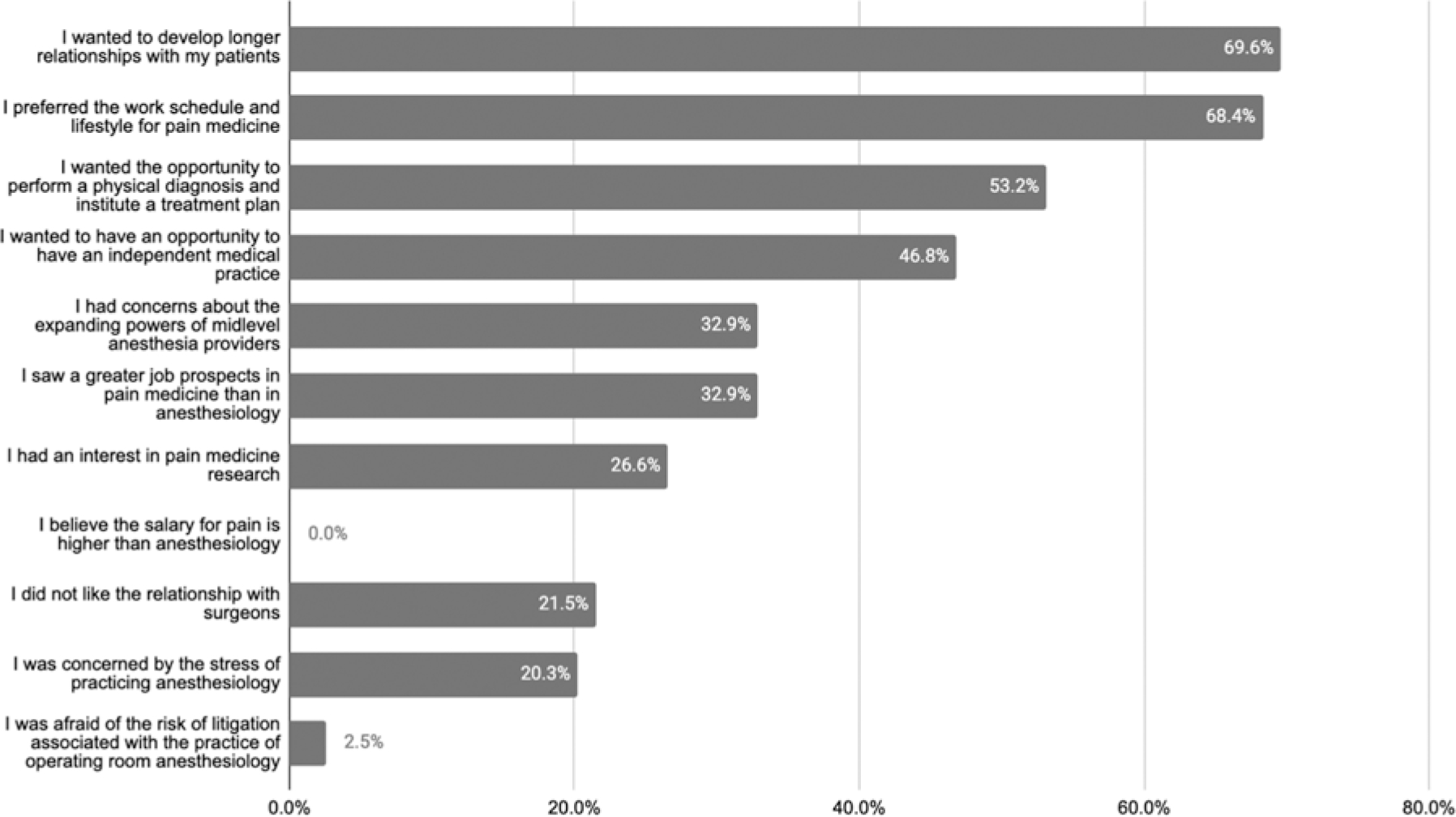
Respondents Currently Practicing Pain Medicine
Characteristics of respondents currently practicing pain are presented in Table 2. The majority of respondents currently practice pain work in a hybrid inpatient and outpatient role (51.90%), followed by outpatient alone (41.77%), and inpatient alone (5%). The majority of the respondents reported that they currently practice in an academic setting (52%), followed by private practice (42.67%), and 4 respondents (5.33%) identified as having worked in both academic and private practice. While the majority of respondents still practicing pain have been practicing for 5 years or less (60.52%), 12 participants (15.79%) have been practicing for 6–8 years, 7 participants (9.21%) have been practicing for 9–11 years, and 11 participants (14.47%) have been practicing for 12–20 years. Compared to the respondents’ prediction of time allocation between inpatient 5 participants (6.33%), outpatient 33 respondents (41.77%), or both inpatient and outpatient 41 respondents (51.90%). The majority of respondents reported similar time breakdowns while practicing pain medicine, with less than 21% of their time in anesthesiology, less than 21% of their time in inpatient pain, and 81–100% of their time in outpatient pain. Respondents’ reported reasons for continuing to practice pain medicine are presented in Fig. 1. The most common reasons include the desire to develop longer-term patient relationships (69.62%), preference for the work schedule and lifestyle within pain medicine (68.35%), and desire to perform a physical diagnosis and institute a treatment plan (53.16%). No participant reported higher pay in pain medicine compared to anesthesiology as a reason to continue practicing pain medicine. Regarding job satisfaction, 38 (76.32%) reported that they were either satisfied or very satisfied, 7 (9.21%) were neither satisfied nor dissatisfied, and 11 (14.48%) were either dissatisfied or very dissatisfied.
Table 2.
Characteristics of physicians currently practicing pain
| Total (n = 79) | |
|---|---|
| Setting Practicing Pain Medicine | |
| Both Inpatient and Outpatient | 41 (51.90%) |
| Inpatient | 5 (6.33%) |
| Outpatient | 33 (41.77%) |
| Missing | 0 |
| Years Practicing Pain Medicine | |
| 12 to 20 | 11 (14.47%) |
| 3 to 5 | 23 (30.26%) |
| 6 to 8 | 12 (15.79%) |
| 9 to 11 | 7 (9.21%) |
| Less than 3 | 23 (30.26%) |
| Missing | 3 |
| Percent of Time Practicing Anesthesia | |
| 21 to 40 | 8 (10.53%) |
| 41 to 60 | 6 (7.89%) |
| 61 to 80 | 7 (9.21%) |
| 81 to 100 | 3 (3.95%) |
| Less than 21 | 52 (68.42%) |
| Missing | 3 |
| Percent of Time Practicing Pain Medicine | |
| 21 to 40 | 12 (15.79%) |
| 41 to 60 | 7 (9.21%) |
| 61 to 80 | 9 (11.84%) |
| 81 to 100 | 41 (53.95%) |
| Less than 21 | 7 (9.21%) |
| Missing | 3 |
| Percent of Time Non-Clinical | |
| 21 to 40 | 9 (11.84%) |
| 41 to 60 | 1 (1.32%) |
| 61 to 80 | 4 (5.26%) |
| Less than 21 | 62 (81.58%) |
| Missing | 3 |
| Environment Practicing Pain Medicine | |
| Academic | 39 (52.00%) |
| Both Academic and Priv Pract | 4 (5.33%) |
| Private Practice | 32 (42.67%) |
| Missing | 4 (5.06%) |
| Job Satisfaction | |
| Dissatisfied | 10 (13.16%) |
| Neither | 9 (11.84%) |
| Satisfied | 28 (36.84%) |
| Very dissatisfied | 1 (1.32%) |
| Very satisfied | 28 (36.84%) |
| Missing | 3 |
Fig. 1. Reasons participants continue to practice pain medicine.
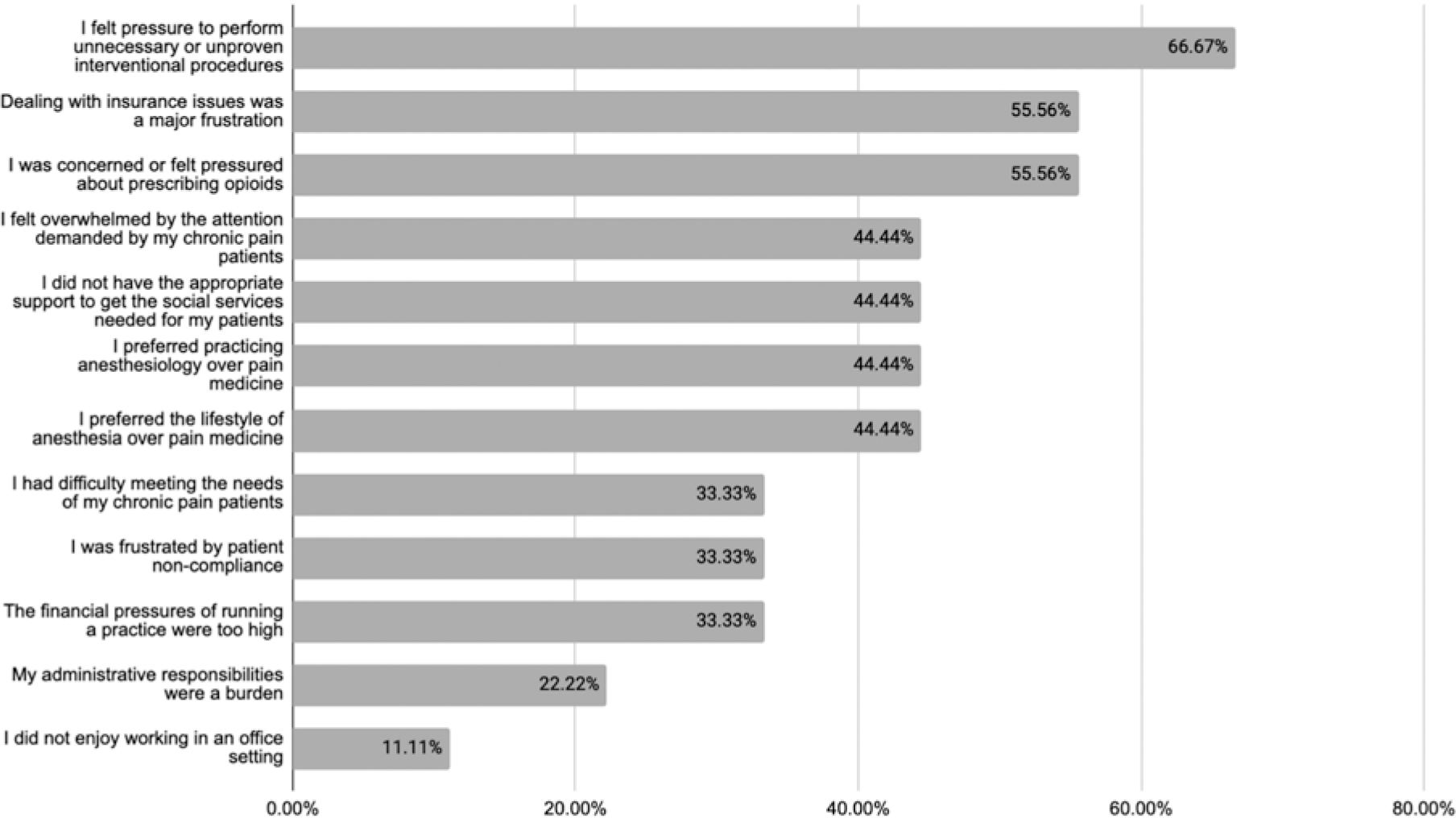
Respondents No Longer Practicing Pain Medicine
Additional characteristics of respondents no longer practicing pain medicine are presented in Table 3. The majority of respondents no longer practicing pain medicine worked in the pain medicine setting for less than 3 years (50.00%), followed by 3–5 years (37.50%) and 6–8 years (12.50%). Respondents’ reported reasons for leaving pain medicine are presented in Fig. 2. The most common reasons for leaving pain medicine included pressure to perform unnecessary or unproven interventional procedures (66.67%), pressure to prescribe opioids (55.56%), and frustration with insurance issues (55.56%). Of the respondents who left pain medicine, no participant reported a plan to return to pain medicine.
Table 3.
Characteristics of physicians no longer practicing pain medicine.
| Total (n = 9) | |
|---|---|
| Years Practiced Pain Medicine | |
| 3 to 5 | 3 (37.50%) |
| 6 to 8 | 1 (12.50%) |
| Less than 3 | 4 (50.00%) |
| Missing | 1 |
| Years Since Practicing Pain | |
| 3 to 5 | 4 (50.00%) |
| Less than 3 | 4 (50.00%) |
| Missing | 1 |
| Plan to Return to Pain | |
| No | 9 (100.00%) |
| Missing | 0 |
Fig. 2. Reasons participants left pain medicine.
Discussion
Despite pain medicine commonly residing under the subspecialty field of anesthesiology, the 2 fields are different in many ways. Anesthesiologists specializing in pain medicine are usually board certified in both anesthesiology and pain medicine, allowing them to practice either specialty or both. There is a lack of published literature to determine the number of anesthesiologists with pain medicine fellowships who practice pain medicine compared to those who practice anesthesiology alone. The goal of this paper is to determine how often anesthesiologists who completed pain medicine fellowship stay in pain medicine and some of the reasons behind their decisions. These findings are important because they can help academic anesthesiology programs determine the quantity of resources to set aside for training physicians in the field of pain medicine. There is an increasing number of pain medicine fellowship programs and positions coupled with a decreasing overall number of applicants that apply for these positions (9). This data may also help inform anesthesiology residents who are ambivalent about pursuing pain medicine understand the trends of where their peers ultimately practice after fellowship.
Prior to the study, we expected higher levels of dissatisfaction with pain medicine given the current climate of lower reimbursements, constant battle with insurance companies for procedures, increased burnout rates, and COVID-19 pandemic pressures. The impact of COVID-19 on patient volume during pain medicine fellowship may contribute to increased anxiety associated with independent practice after training. The reasons for this are multifactorial, but the use of telehealth and reduced exposure to challenging interventional procedures are potential reasons (10–13). However, what we found was that most of the pain medicine physicians continue practicing in a pain medicine setting, whether it is inpatient, outpatient, or a combination of the 2. Further investigation shows that most physicians who continue to practice pain medicine spend most of their time in pain medicine. More importantly, most of the physicians we surveyed who were still doing pain medicine were satisfied with their jobs. Seventy-five percent of respondents in the survey who are currently practicing pain medicine reported satisfaction with their job. This finding is comparable to other surveys of general physician job satisfaction throughout the country (14–16). While this study’s respondents are mostly those in the earlier stages of their careers, 14% have been practicing for over 12 years. The younger surveyed population may not have experienced the long-term frustrations of practicing pain medicine.
Interestingly, the respondents who do not participate in any form of pain medicine left the field almost entirely due to external pressures: pressure to perform unnecessary interventions, pressure to prescribe opioids, or frustrations with insurance issues. This may indicate that the field of treating patients’ pain itself is gratifying, but the external forces are what make the job unsatisfactory.
Although studies on this topic show variable results, burnout rates in anesthesiology were recently found to be nearly 50% (17). This percentage has held true even prior to the COVID-19 pandemic (18). While this rate is lower than the pain medicine burnout rates noted by Kroll et al (4), there are many other factors involved in burnout, such as the number of hours worked per week and perceived support received at work. Jha et al (19) showed that the COVID-19 pandemic affected 98% of pain physicians surveyed negatively, and a majority had a negative perception of the healthcare industry for a variety of reasons, including in-house billing and time spent with the electronic medical record. This is coupled with the psychological and financial stressors of practicing and scheduling elective cases during a pandemic (19,20). Despite this, many anesthesiology-trained pain medicine physicians continued to practice pain with a high percentage of satisfaction.
Limitations
Our study has a significant limitation as we are unable to determine the response rate. Due to the nature of the question and the methods by which it was sent to individuals who completed the study, it is not possible to know the exact number of study recipients. While this is a limitation of this study, the number of responses still provides valuable insight and consideration into this topic, and some conclusions can be statistically validated. Given survey dissemination relied on the academic program directors sharing the survey with previous pain medicine fellows and alumni, the low response number may be due to either lack of participation by program directors or broken lines of communication between program directors and previous fellows in addition to a lower response rate in the no longer practicing group due to lack of involvement in pain medicine. Additionally, a general overall increased email burden and decreased cognitive bandwidth amid the COVID-19 pandemic, along with a condensed timing of email reminders, may serve as a reason. This pilot study may be biased by the program directors who are more active in pain medicine education, thus sending out the surveys resulting in a cohort that is more likely to stay involved in pain medicine. Survey fatigue and burnout could also possibly add to the decreased response rate. If fatigue or burnout caused a lower number of respondents, the results are likely biased towards those who were not burned out and, thus, more satisfied with their current job situation. The results do not take into consideration geographic location or details of fellowship.
Lastly, this study only looked at anesthesiologists practicing pain medicine. There are many other specialties that pursue pain medicine, including, but not limited to, physical medicine and rehabilitation, emergency medicine, neurology, and psychiatry. There are also a significant number of non-accredited or private practice/industry-sponsored pain medicine training programs around the country, for which this survey does not account.
Conclusion
While this pilot study is a small sample, the findings show that pain medicine in anesthesiology is a field that may be satisfying despite the concerns of multiple factors causing decreasing job satisfaction. A larger, more thorough study can compare the various outcomes based on different types of settings, such as private practice, partnership, and academia, as well as geographical locations.
Acknowledgments
Disclaimer: This study was supported by MSK Cancer Support Grant/Core Grant (P30 CA008748).
Footnotes
Conflict of interest: Each author certifies that he or she, or a member of his or her immediate family, has no commercial association (i.e., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted manuscript.
References
- 1.Krueger P, Brazil K, Lohfeld L, Edward HG, Lewis D, Tjam E Organization specific predictors of job satisfaction: Findings from a Canadian multi-site quality of work life cross-sectional survey. BMC Health Serv Res 2002; 2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romito BT, Okoro EN, Ringqvist JRB, Goff KL. Burnout and wellness: The anesthesiologist’s perspective. Am J Lifestyle Med 2020; 15:118–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Metlaine A, Sauvet F, Gomez-Merino D, et al. Sleep and biological parameters in professional burnout: A psychophysiological characterization. PLoS One 2018; 13:e0190607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroll HR, Macaulay T, Jesse M. A preliminary survey examining predictors of burnout in pain medicine physicians in the United States. Pain Physician 2016; 19:E689–E696. [PubMed] [Google Scholar]
- 5.Hyman SA, Card EB, De Leon-Casasola O, Shotwell MS, Shi Y, Weinger MB. Prevalence of burnout and its relationship to health status and social support in more than 1000 subspecialty anesthesiologists. Reg Anesth Pain Med 2021; 46:381–387. [DOI] [PubMed] [Google Scholar]
- 6.Wong A, Olusanya O. Burnout and resilience in anaesthesia and intensive care medicine. BJA Educ 2017; 17:334–340. [Google Scholar]
- 7.Becker’s ASC Review. www.beckersasc.com/anesthesia/anesthesiologist-pay-jumps-8-5-stats.html#:~:text=Anesthesiologist%20pay%20jumped%20nearly%208,through%20Jan.%2019%2C%202022
- 8.Adams PS, Gordon EKB, Berkeley A, et al. Academic faculty demonstrate higher well-being than residents: Pennsylvania anesthesiology programs’ results of the 2017–2018 ACGME well-being survey. J Clin Anesth 2019; 56:60–64. [DOI] [PubMed] [Google Scholar]
- 9.National Resident Matching Program, Results and Data: Specialties Matching Service 2022 Appointment Year. National Resident Matching Program, Washington, DC. March 2022. [Google Scholar]
- 10.Hagedorn JM, Moeschler S, Furnish T, Sayed D, Durbhakula S. Impact of COVID-19 on pain medicine fellowship training. Reg Anesth Pain Med 2021; 46:188–189. [DOI] [PubMed] [Google Scholar]
- 11.Kassem H, Urits I, Kaye AD, Viswanath O. The role of COVID-19 in shaping the experiences of pain medicine fellowship training. Pain Physician 2020; 23:S463–S464. [PubMed] [Google Scholar]
- 12.Prem A, Anand S, Chandrashekar A. Impact of COVID-19 on an academic pain fellowship program. Pain Physician 2020; 23:S433–S438. [PubMed] [Google Scholar]
- 13.Kohan L, Sobey C, Wahezi S, et al. Maintaining high-quality multidisciplinary pain medicine fellowship programs: Part II: Innovations in clinical care workflow, clinical supervision, job satisfaction, and postgraduation mentorship for pain fellows during the COVID-19 pandemic. Pain Med 2020; 21:1718–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CompHealth Blog. 2019 AAFP/CompHealth Physician Happiness Survey. March 19. 2019. [Google Scholar]
- 15.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc 2019; 94:1681–1694. [DOI] [PubMed] [Google Scholar]
- 16.Simpson AL, Chang Y, Yu L, Campbell EG, Armstrong K, Walensky RP. Assessment of job satisfaction and feeling valued in academic medicine. JAMA Intern Med 2019; 179:992–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afonso AM, Cadwell JB, Staffa SJ, Zurakowski D, Vinson AE. Burnout rate and risk factors among anesthesiologists in the United States. Anesthesiology 2021; 134:683–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rama-Maceiras P, Jokinen J, Kranke P . Stress and burnout in anaesthesia: A real world problem? Curr Opin Anaesthesiol 2015; 28:151–158. [DOI] [PubMed] [Google Scholar]
- 19.Jha SS, Shah S, Calderon MD, Soin A, Manchikanti L. The effect of COVID-19 on interventional pain management practices: A physician burnout survey. Pain Physician 2020; 23:S271–S282. [PubMed] [Google Scholar]
- 20.Manchikanti L, Pampati V, Jha SS, et al. The impact of COVID-19 on interventional pain management practices is significant and long-lasting: An interventional pain management physician survey. Pain Physician 2022; 25:131–144. [PubMed] [Google Scholar]


