Abstract
Aims
Impact of skin mottling has been poorly studied in patients admitted for cardiogenic shock. This study aimed to address this issue and identify determinants of 30-day and 1-year mortality in a large cardiogenic shock cohort of all etiologies.
Methods and results
FRENSHOCK is a prospective multicenter observational registry conducted in French critical care units between April and October, 2016. Among the 772 enrolled patients (mean age 65.7 ± 14.9 years; 71.5% male), 660 had skin mottling assessed at admission (85.5%) with almost 39% of patients in cardiogenic shock presenting mottling. The need for invasive respiratory support was significantly higher in patients with mottling (50.2% vs. 30.1%, p < 0.001) and likewise for the need for renal replacement therapy (19.9% vs. 12.4%, p = 0.09). However, the need for mechanical circulatory support was similar in both groups. Patients with mottling at admission presented a higher length of stay (19 vs. 16 days, p = 0.033), a higher 30-day mortality rate (31% vs. 23.3%, p = 0.031), and also showed significantly higher mortality at 1-year (54% vs. 42%, p = 0.003). The subgroup of patients in whom mottling appeared during the first 24 h after admission had the worst prognosis at 30 days.
Conclusion
Skin mottling at admission in patients with cardiogenic shock was statistically associated with prolonged length of stay and poor outcomes. As a perfusion-targeted resuscitation parameter, mottling is a simple, clinical-based approach and may thus help to improve and guide immediate goal-directed therapy to improve cardiogenic shock patients’ outcomes.
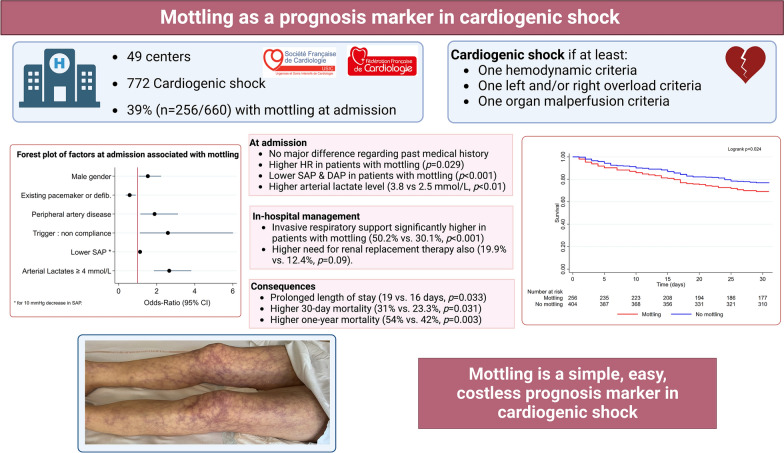
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13613-023-01175-0.
Keywords: Cardiogenic shock, Acute heart failure, Perfusion, Microcirculation
Introduction
To date, even if there is no precise uniform definition of cardiogenic shock (CS), it is generally considered as a primary cardiac dysfunction with low cardiac output leading to critical end-organ hypoperfusion [1, 2] with a high mortality rate (40%) [3]. This inadequate end-organ perfusion associated with microcirculatory dysfunction and multiple organ failure is mentioned in all current definitions of CS as “signs of poor peripheral tissue perfusion” such as cold extremities, mottling, elevated capillary refill time (CRT), altered mental status, oliguria or elevated arterial lactate levels [4]. However, even if the classification of acute heart failure (AHF) and CS patients using perfusion/congestion profiles for treatment approaches related to each category are suggested by the latest European Society of Cardiology guidelines [5] and considered as class I recommendation by the American College of Cardiology/American Heart Association Joint Committee latest guidelines [6], the level of evidence is low (C) due to limited data [6]. Indeed, only recently have studies attempted to better characterize the hypoperfusion and microcirculatory dysfunction in CS [7–9].
Numerous investigations have provided evidence that CS affects not only the macrocirculation, as evidenced by alterations in blood pressure (BP), left ventricular ejection fraction (LVEF), and cardiac index (CI) [10–13], but also has significant perfusion abnormalities of the systemic microcirculation [14, 15]. This intricate network of microvessels, arterioles, capillaries, and venules, which constitutes the terminal vascular network of the systemic circulation, plays a crucial role in the delivery of oxygen and nutrients to organs, as well as the removal of carbon dioxide [16].
The visualization of microcirculation can be achieved using handheld microscopes, including Sidestream Dark-Field (SDF), Incident Dark-Field (IDF) imaging techniques, and tissue laser Doppler imaging [17]. However, these devices have several limitations, such as the need for trained operators, limited availability due to the expensive cost of these devices, difficulty evaluating the sublingual area in non-intubated patients, and limited representation of microcirculatory impairment in other tissues [18]. Interestingly, traditional markers of peripheral tissue perfusion, including skin mottling and CRT, are strongly associated with altered microcirculatory blood flow during septic shock [19–21]. Mottling refers to patchy discoloration of the skin, usually starting around the knees, while CRT measures the time required to recolor the tip of a finger [22].
Even if mottling is easy to assess, costless, and widely described and taught in medical school as a sign of shock or hypoperfusion for centuries, they have been poorly studied in CS to date [7]. Indeed, only one small study has rigorously investigated them in CS [9].
The main objective of this study based on the largest European prospective cohort of CS to date was to assess characteristics and outcomes of CS according to the presence of mottling at admission. The secondary objectives were to assess morbidity and mortality parameters, and also the time course of mottling contribution to CS outcomes among the subgroup of patients who survived the first 24 h.
Methods
Patient population
FRENSHOCK is a prospective multicenter observational registry conducted in metropolitan France during 6 months between April and October 2016 in intensive care units (ICU) and intensive cardiac care units (ICCU) (NCT02703038). The methods used for this registry have been previously described [23]. Briefly, the primary objective was to evaluate the characteristics, management, and outcomes of CS patients, with a new modified definition of CS as seen in routine clinical practice, on a nationwide scale.
All adult patients (≥ 18 years old) with CS were prospectively included in this registry if they met at least one criterion of each of the following three components: (i) hemodynamic criteria, defined as low systolic arterial pressure (SAP) < 90 mmHg and/or the need for maintenance with vasopressors/inotropes and/or a low CI < 2.2 L/min/m2; (ii) left and/or right heart overload, defined by clinical signs, radiology, blood tests, echocardiography, or invasive hemodynamics’ signs; and (iii) signs of organ malperfusion, which could be clinical and/or biological. Patients admitted after cardiopulmonary resuscitation were included if they fulfilled previously defined CS criteria. Patients could be included regardless of CS etiology, and whether CS was primary or secondary. Exclusion criteria were refusal or the inability to consent. A diagnosis of CS was refuted in favor of alternative diagnoses, such as septic shock, refractory cardiac arrest, and post-cardiotomy CS [23].
All institutions were invited to participate in the study, including university teaching hospitals, general and regional hospitals, as well as public and private hospitals that manage CS patients (ICCUs, surgical ICUs, medical ICUs, and general ICUs).
The study was conducted in accordance with the guidelines for good clinical practice and French law. Written consent was obtained for all the patients. The data recorded and their handling and storage were reviewed and approved by the CCTIRS (French Health Research Data Processing Advisory Committee) (n° 15.897) and the CNIL (French Data Protection Agency) (n° DR-2016-109).
Data collection
Data on baseline characteristics, including demographics (age, gender, body mass index, social status), risk factors (hypertension, diabetes, current smoking, hypercholesterolemia, family history of coronary artery disease), and medical history [cardiomyopathy, myocardial infarction, stroke, peripheral artery disease, chronic kidney disease, active cancer, chronic obstructive lung disease], were collected as previously mentioned. Clinical, biological, and echocardiographic data were collected at admission and 24 h after admission. Skin mottling, define as patchy skin discoloration starting around the knees was assessed at admission and 24 h after admission by a senior physician as requested in the case report form. Therefore, patients with mottling (of any extent) were considered in the group called “Mottling” and those without mottling in the "No mottling" group. Up to three CS triggers were determined for each patient by the local investigator, that is, ischemic (Type 1 or Type 2 acute myocardial infarction according to European guidelines); ventricular and supraventricular arrhythmia; conduction disorder; infectious disease; non-compliance (poor compliance with medical treatment or hygiene and diet rules, for example, stopping or skipping an angiotensin-converting enzyme inhibitor or beta-blocker treatment, deviation from a low sodium diet, etc.); or iatrogenesis. Investigators could also note other existing factors or etiologies. Such triggering factors were indicated as ‘other’. Information regarding the use of cardiac procedures, that is, coronary angiography and/or percutaneous coronary intervention (PCI); right heart catheterization; the need for medications (inotropes, vasopressors, diuretics, and fibrinolysis) and organ replacement therapies such as mechanical ventilation (invasive or non-invasive); temporary mechanical circulatory support [intra-aortic balloon pump (IABP); venoarterial-extracorporeal membrane oxygenation (VA-ECMO) or Impella® (Abiomed, Danvers, MA, USA)]; and renal replacement therapy (RRT) were collected. In-hospital complications were noted, such as stroke, bleeding and transfusions, hemolysis, thrombocytopenia, nosocomial infections, vascular complications, and death. Information on mortality was obtained directly by the local investigators (cause and date) through a 30-day and 1-year follow-up.
Statistical analysis
Continuous variables were reported as means (standard deviation, SD) or medians and interquartile ranges when appropriate. Discrete variables were described in numbers and percentages. The two groups (presence or absence of mottling at admission) were compared using student’s t tests or Mann and Whitney non-parametric tests for continuous variables and using χ2 or Fisher’s exact tests for categorical variables. Factors independently associated with mottling were studied using multiple logistic regression. Survival analyses were conducted using the Kaplan–Meier method and factors associated with 30 days and 1-year mortality were identified using a Cox Proportional Hazards Model, with a stepwise backward method for covariates elimination. Odds ratios (ORs) and hazard ratios (HRs) were presented with their 95% confidence intervals (CIs). Statistical analyses were performed using Stata (Stata Statistical Software SE/17.0. StataCorp LLC. College Station. TX. USA.). For all analyses, two-sided p values < 0.05 were considered significant.
Results
Study population
A total of 772 CS patients were included in 49 centers, in whom mottling was assessed in 660 patients at inclusion (85.5%). Among these CS patients, clinical characteristics between patients with and without mottling are presented in Table 1. The mean age (66 ± 14 years) was similar in the two groups, but men were significantly predominant in mottling patients (76% vs. 68%, p = 0.02). In patients with mottling, a medical history of cardiac disease was reported in 53.9% (30.9% coronary artery disease), previous PCI in 21.9%, previous ischemic stroke in 9.8%, and peripheral artery disease in 15.2% with no significant difference between groups. There was also no difference in terms of cardiovascular risk factors, or medical history except for a higher rate of already implanted pacemakers or defibrillators among patients with mottling (p = 0.042 and p = 0.041, respectively). Peripheral artery disease was numerically more frequent among patients with mottling (15.2% vs. 10.2%).
Table 1.
Baseline characteristics of cardiogenic shock patients included
| Overall (n = 660) | No mottling (n = 404) | Mottling (n = 256) | p | ||||
|---|---|---|---|---|---|---|---|
| Male gender | 469 | 71.1 | 275 | 68.1 | 194 | 75.8 | 0.020 |
| Age (years), mean ± SD | 66.0 | ± 14.0 | 65.9 | ± 15.7 | 66.0 | ± 14.0 | 0.963 |
| BMI (kg/m2), mean ± SD | 25.8 | ± 5.6 | 25.8 | ± 5.9 | 25.7 | ± 4.9 | 0.977 |
| n | 644 | 394 | 250 | ||||
| Risk factors, n (%) | |||||||
| Current smoker | 182/634 | 28.7 | 107/387 | 27.7 | 75/247 | 30.4 | 0.461 |
| Diabetes mellitus | 183/659 | 27.8 | 115/403 | 28.5 | 68/256 | 0.6 | 0.581 |
| Arterial hypertension | 320 | 48.5 | 190 | 47.0 | 130 | 50.8 | 0.347 |
| Dyslipidaemia | 236 | 35.8 | 137 | 33.9 | 99 | 38.7 | 0.214 |
| Medical history, n (%) | |||||||
| History of cardiac disease | 368 | 55.8 | 230 | 56.9 | 138 | 53.9 | 0.446 |
| Ischaemic | 197 | 29.9 | 118 | 29.2 | 79 | 30.9 | 0.651 |
| Hypertrophic | 10 | 1.5 | 7 | 1.7 | 3 | 1.2 | 0.748 |
| Idiopathic | 65 | 9.9 | 47 | 11.6 | 18 | 7.0 | 0.053 |
| Toxic | 26 | 3.9 | 12 | 3.0 | 14 | 5.5 | 0.108 |
| Multisite pacing | 51 | 7.7 | 38 | 9.4 | 13 | 5.1 | 0.042 |
| Defibrillator | 104 | 15.8 | 73 | 18.1 | 31 | 12.1 | 0.041 |
| CABG | 54 | 8.2 | 36 | 8.9 | 18 | 7.0 | 0.391 |
| PCI | 145 | 22.0 | 89 | 22.0 | 56 | 21.9 | 0.963 |
| Peripheral artery disease | 80 | 12.1 | 41 | 10.2 | 39 | 15.2 | 0.051 |
| Ischaemic stroke | 56 | 8.5 | 31 | 7.7 | 25 | 9.8 | 0.34.7 |
| Chronic renal failure | 139 | 21.1 | 88 | 21.8 | 51 | 19.9 | 0.568 |
| COPD | 45 | 6.8 | 28 | 6.9 | 17 | 6.6 | 0.885 |
| Active neoplasy | 43 | 6.5 | 22 | 5.5 | 21 | 8.2 | 0.162 |
| Previous medications, n (%) | |||||||
| Aspirin | 250/659 | 37.9 | 157/404 | 38.9 | 93/255 | 36.5 | 0.538 |
| P2Y12 inhibitor | 119/659 | 18.1 | 77/404 | 19.1 | 42/255 | 16.5 | 0.400 |
| Statins | 243/659 | 36.9 | 154/404 | 38.1 | 89/255 | 34.9 | 0.404 |
| Beta-blockers | 273/659 | 41.4 | 177/404 | 43.8 | 96/255 | 41.4 | 0.118 |
| Vitamin K antagonist | 144/659 | 21.9 | 93/404 | 23.0 | 51/255 | 20.0 | 0.361 |
| Direct oral anticoagulant | 50/659 | 7.6 | 29/404 | 7.2 | 21/255 | 8.2 | 0.618 |
| ACE inhibitors or ARB | 248/659 | 37.6 | 154/404 | 38.1 | 94/255 | 36.9 | 0.746 |
| Sacubitril/valsartan | 15/659 | 2.4 | 9/404 | 2.3 | 6/255 | 2.5 | 1.000 |
| Furosemide | 325/659 | 49.3 | 210/404 | 52.0 | 115/255 | 45.1 | 0.085 |
| Aldosterone antagonist | 94/659 | 14.3 | 67/404 | 16.6 | 27/255 | 10.6 | 0.032 |
| Amiodarone | 119/643 | 18.5 | 66/391 | 16.9 | 53/252 | 21.0 | 0.186 |
| Proton pump inhibitor | 236/650 | 36.3 | 152/397 | 38.3 | 84/253 | 33.2 | 0.189 |
| Triggers | |||||||
| Ischaemic | 255 | 38.6 | 151 | 37.4 | 104 | 40.6 | 0.404 |
| Mechanical | 17 | 2.6 | 8 | 2.0 | 9 | 3.5 | 0.225 |
| Ventricular arrhythmia | 83 | 12.6 | 45 | 11.1 | 38 | 14.8 | 0.162 |
| Atrial arrhythmia | 95 | 14.4 | 56 | 13.9 | 39 | 15.2 | 0.624 |
| Conductive disorders | 17 | 2.6 | 10 | 2.5 | 7 | 2.7 | 0.838 |
| Infectious | 80 | 12.1 | 45 | 11.1 | 35 | 13.7 | 0.331 |
| Non-compliance | 26 | 3.9 | 10 | 2.5 | 16 | 6.3 | 0.015 |
| Iatrogenic | 49 | 7.4 | 29 | 7.2 | 20 | 7.8 | 0.762 |
| Other | 88 | 13.3 | 57 | 14.1 | 31 | 12.1 | 0.462 |
| None/undefined | 92 | 13.9 | 67 | 16.6 | 25 | 9.8 | 0.783 |
Values in italics indicate the number of patients included in the statistical analysis
ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blocker; BMI, body mass index; CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; PCI, percutaneous coronary intervention; SD, standard deviation
There was no significant difference in previous cardiac treatments except more aldosterone antagonists being prescribed in non-mottling patients (p = 0.032). Besides cardiovascular diseases, there was also no difference in medical history of chronic obstructive pulmonary disease or chronic kidney disease.
At admission, in patients with mottling, the mean heart rate was 99 (± 35.2) bpm (47.3% with sinus rhythm), SAP was 97 (± 27) mmHg, and DAP was 60 (± 18) mmHg. Heart rate was statistically higher in CS patients with mottling while blood pressure parameters were statistically lower compared to CS patients without mottling (p = 0.029, p < 0.01, and p < 0.01, respectively) (Table 2). No significant difference was found between patients with and patients without mottling regarding clinical signs of left (75% vs. 68%, respectively, p = 0.18) and right (53% vs. 47%, p = 0.13) heart failure.
Table 2.
Clinical, echographic, and biological characteristics of cardiogenic shock patients included
| Overall (n = 660) | No mottling (n = 404) | Mottling (n = 256) | p | ||||
|---|---|---|---|---|---|---|---|
| Admission unit, n (%) | 0.007 | ||||||
| CICU | 356 | 69.1 | 235 | 73.4 | 121 | 62.1 | |
| Reanimation | 159 | 30.9 | 85 | 26.6 | 74 | 37.9 | |
| Clinical presentation at admission | |||||||
| Heart rate (bpm), mean ± SD | 95.8 | ± 30.0 | 93.8 | ± 26.0 | 99 | ± 35.2 | 0.029 |
| n | 659 | 403 | 256 | ||||
| SAP (mmHg), mean ± SD | 101 | ± 25 | 103 | ± 23 | 97 | ± 27 | < 0.001 |
| n | 660 | 404 | 256 | ||||
| DAP (mmHg), mean ± SD | 63 | ± 18 | 65 | ± 17 | 60 | ± 18 | < 0.001 |
| n | 659 | 403 | 256 | ||||
| Sinus rhythm, n (%) | 336/659 | 51.0 | 215/403 | 53.4 | 121/256 | 47.3 | 0.128 |
| Cardiac arrest, n (%) | 73 | 11.1 | 38 | 9.4 | 35 | 13.7 | 0.089 |
| Blood tests at admission | |||||||
| Sodium (mmol/L), mean ± SD | 135 | ± 6 | 135 | ± 6 | 135 | ± 6 | 0.608 |
| n | 652 | 399 | 253 | ||||
| eGFR (mL/min/1.73 m2), mean ± SD | 49.5 | ± 26.2 | 50.8 | ± 27.6 | 47.4 | ± 23.8 | 0.112 |
| n | 644 | 396 | 248 | ||||
| Bilirubin (mg/L), median (IQR) | 16 (9–28) | 16 (9–27) | 17 (10–32) | 0.159 | |||
| n | 461 | 281 | 180 | ||||
| Hamoglobin (g/dL), mean ± SD | 12.5 | ± 2.5 | 12.5 | ± 2.3 | 12.5 | ± 2.5 | 0.808 |
| n | 649 | 398 | 251 | ||||
| Arterial blood lactates (mmol/L), median (IQR) | 3.0 (2.0–5.0) | 2.5 (2.0–4.0) | 3.8 (2.0–6.0) | < 0.001 | |||
| n | 595 | 357 | 238 | ||||
| ASAT (IU/L), median (IQR) | 91 (38–304) | 83 (37–270) | 118 (42–388) | 0.077 | |||
| n | 458 | 288 | 170 | ||||
| ALAT (IU/L), median (IQR) | 59 (26–184) | 57 (25–179) | 69 (31–236) | 0.074 | |||
| n | 468 | 292 | 176 | ||||
| Nt proBNP (pg/mL), median (IQR) | 8938 (3894–24,363) | 8388 (3466–20,333) | 9277 (4411–30,000) | 0.399 | |||
| n | 185 | 111 | 74 | ||||
| BNP (pg/mL), median (IQR) | 1211 (484–2852) | 1437 (509–2997) | 1099 (484–2262) | 0.236 | |||
| n | 234 | 153 | 81 | ||||
| CRP (mg/L), median (IQR) | 28 (10–64) | 26 (9–56) | 32 (10–95) | 0.111 | |||
| n | 352 | 225 | 127 | ||||
| Baseline echography | |||||||
| LVEF (%), mean ± SD | 26.2 | ± 13.2 | 26.8 | ± 12.6 | 25.3 | ± 14.1 | 0.160 |
| n | 653 | 400 | 253 | ||||
| TAPSE (mm), mean ± SD | 13.5 | ± 5.1 | 13.9 | ± 5.1 | 12.9 | ± 5.2 | 0.132 |
| n | 235 | 148 | 87 | ||||
| PSVtdi (cm/s), median (IQR) | 8 (6–11) | 8 (6–11) | 9 (6–11) | 0.443 | |||
| n | 191 | 121 | 70 | ||||
| Severe mitral regurgitation, n (%) | 94/631 | 14.9 | 64/388 | 16.5 | 30/243 | 12.4 | 0.154 |
| Severe aortic stenosis, n (%) | 32/650 | 4.9 | 14/399 | 3.5 | 18/251 | 7.2 | 0.036 |
| Severe aortic regurgitation, n (%) | 9/647 | 1.4 | 4/398 | 1.0 | 5/249 | 2.0 | 0.316 |
Values in italics indicate the number of patients included in the statistical analysis
ALAT, alanine aminotransferase; ASAT, aspartate aminotransferase; CICU, cardiologic intensive care unit; CRP, C-reactive protein; DAP, diastolic arterial pressure; IQR, interquartile range; LVEF, left ventricular ejection fraction; PSVtdi, peak systolic velocity tissue Doppler imaging; SAP, systolic arterial pressure; SD, standard deviation; TAPSE, tricuspid annular plane systolic excursion
The main triggers of CS (not mutually exclusive) in patients with mottling were ischemic (40.6%), atrial arrhythmia (15.2%), and ventricular arrhythmia (14.8%) (Table 1). Non-compliance to cardiovascular medications was significantly more frequent in patients with mottling (6.3% vs. 2.5%, p = 0.015) compared to patients without mottling. Most patients in both groups had multiple organ failures as evidenced by kidney dysfunction, hepatic cytolysis and cholestasis, and lactate elevation (Table 2). Notably, lactate level at admission was significantly increased in patients with mottling compared to patients without (3.8 vs. 2.5 mmol/L, p < 0.01).
At baseline echocardiography, patients with mottling showed a mean left ventricular ejection fraction (LVEF) of 25.3% (± 14.1) which was not different from patients without mottling. Severe aortic stenosis appeared to be almost twice more frequent in patients with mottling (7.2% vs. 3.5%, p = 0.036).
Factors associated with mottling
A multivariate analysis identified four independent factors at admission associated with mottling: male gender (OR: 1.5; p = 0.025), peripheral artery disease (OR: 1.9; p = 0.013), non-compliance as a trigger (OR: 2.6; p = 0.027), and lactates > 4 mmol/L (OR: 2.7; p < 0.001) (Table 3).
Table 3.
Baseline characteristics associated with mottling
| Odds-ratio | 95% CI | p | |
|---|---|---|---|
| Male gender | 1.53 | 1.05–2.23 | 0.025 |
| Existing pacemaker of defibrillator | 0.58 | 0.37–0.90 | 0.015 |
| Peripheral artery disease | 1.89 | 1.14–3.12 | 0.013 |
| Trigger: non-compliance | 2.59 | 1.11–6.01 | 0.027 |
| SAP (mmHg) | 0.89 | 0.83–0.95 | 0.001 |
| Lactates (mmol/L) | |||
| < 4 | 1.00 | Ref. | |
| 4 + | 2.66 | 1.85–3.82 | < 0.001 |
| Unknown | 0.94 | 0.52–1.72 | 0.848 |
Hosmer and Lemeshow goodness of fit p = 0.573
CI, confidence interval; SAP, systolic arterial pressure
In-hospital management
In-hospital management is reported in Table 4. Approximately 70% of the CS patients were directly referred to ICCU while 30% were directly referred to ICU.
Table 4.
In-hospital management and prognosis of cardiogenic shock patients according to the presence of mottling at admission
| Overall (n = 660) | No mottling (n = 404) | Mottling (n = 256) | p | ||||
|---|---|---|---|---|---|---|---|
| Medications used, n (%) | |||||||
| Diuretics | 532/657 | 81.0 | 332/402 | 82.6 | 200/255 | 78.4 | 0.186 |
| Volume expander | 281/656 | 42.8 | 153/401 | 38.2 | 128/255 | 50.2 | 0.002 |
| Dobutamine | 540/657 | 82.2 | 329/402 | 81.8 | 211/255 | 82.8 | 0.768 |
| If yes, maximum dose (mg/kg/min) | 0.007 | ||||||
| 5–10 | 340 | 62.6 | 225 | 68.0 | 115 | 54.2 | |
| 10–15 | 121 | 22.3 | 59 | 17.8 | 62 | 29.2 | |
| > 15 | 44 | 8.1 | 26 | 7.9 | 18 | 8.5 | |
| Unknown | 38 | 7.0 | 21 | 6.3 | 17 | 8.0 | |
| Norepinephrine | 344/657 | 52.4 | 194/402 | 48.3 | 150/255 | 58.8 | 0.008 |
| If yes, maximum dose (mg/h) | 0.128 | ||||||
| < 1 | 67 | 19.3 | 44 | 22.4 | 23 | 15.2 | |
| 1–5 | 177 | 51.0 | 99 | 50.5 | 78 | 51.7 | |
| > 5 | 71 | 20.5 | 33 | 16.8 | 38 | 25.2 | |
| Unknown | 32 | 9.2 | 20 | 10.2 | 12 | 7.9 | |
| Epinephrine | 86/657 | 13.1 | 39/402 | 9.7 | 47/255 | 18.4 | 0.001 |
| If yes, maximum dose (mg/h) | 0.395 | ||||||
| < 1 | 32 | 36.0 | 18 | 43.9 | 14 | 29.2 | |
| 1–5 | 34 | 38.2 | 12 | 29.3 | 22 | 45.8 | |
| > 5 | 13 | 14.6 | 6 | 14.6 | 7 | 14.6 | |
| Unknown | 10 | 11.2 | 5 | 12.2 | 5 | 10.4 | |
| Norepinephrine + dobutamine combination | 299/657 | 45.5 | 165/402 | 41.0 | 134/255 | 52.6 | 0.004 |
| Levosimendan | 47/657 | 7.2 | 34/402 | 8.5 | 13/255 | 5.1 | 0.576 |
| Dopamine | 1/657 | 0.2 | 0/402 | 0.0 | 1/255 | 0.4 | 1.000 |
| Isoprenaline | 30/657 | 4.6 | 15/402 | 3.7 | 15/255 | 5.9 | 0.198 |
| Antiarrhythmic | 261/657 | 39.7 | 154/402 | 38.3 | 107/255 | 42.0 | 0.351 |
| Transfusion | 115/656 | 17.5 | 60/401 | 15.0 | 55/255 | 21.6 | 0.030 |
| Fibrinolysis | 11/656 | 1.7 | 5/401 | 1.3 | 6/255 | 2.4 | 0.353 |
| Organ replacement therapies, n (%) | |||||||
| Respiratory support | |||||||
| Invasive | 249/657 | 37.9 | 121/402 | 30.1 | 128/255 | 50.2 | < 0.001 |
| Non-invasive | 183/657 | 27.9 | 103/402 | 25.6 | 80/255 | 31.4 | 0.109 |
| Mechanical circulatory support | 122/658 | 18.5 | 66/402 | 16.4 | 56/256 | 21.9 | 0.079 |
| If yes | |||||||
| IABP | 43/121 | 35.5 | 23/66 | 34.9 | 20/55 | 36.4 | 0.862 |
| Impella | 22/121 | 18.2 | 11/66 | 16.7 | 11/55 | 20.0 | 0.636 |
| ECLS | 72/121 | 59.5 | 37/66 | 56.1 | 35/55 | 63.6 | 0.398 |
| Renal replacement therapy | 101/659 | 15.3 | 50/403 | 12.4 | 51/256 | 19.9 | 0.009 |
| Invasive cardiology, n (%) | |||||||
| CAG | 346 | 52.4 | 219 | 54.2 | 127 | 49.6 | 0.249 |
| If yes | |||||||
| CAG result | 0.205 | ||||||
| Normal | 61 | 17.6 | 39 | 17.8 | 22 | 17.3 | |
| 1—Mono | 71 | 20.5 | 51 | 23.3 | 20 | 15.7 | |
| 2—Bi | 80 | 23.1 | 49 | 22.4 | 31 | 24.4 | |
| 3—Tri | 76 | 22.0 | 50 | 22.8 | 26 | 20.5 | |
| Unknown | 58 | 16.8 | 30 | 13.7 | 28 | 22.0 | |
| Culprit lesion | 225/281 | 80.1 | 143/178 | 80.3 | 82/103 | 79.6 | 0.883 |
| Any PCI | 192 | 29.1 | 121 | 30.0 | 71 | 27.7 | 0.541 |
| Right heart catheterisation | 107/657 | 16.3 | 70/402 | 17.4 | 37/255 | 14.5 | 0.326 |
| Pace-maker implantation | 28/625 | 4.5 | 16/388 | 4.1 | 12/237 | 5.1 | 0.582 |
| Defibrillator implantation | 31/625 | 5.0 | 18/388 | 4.6 | 13/237 | 5.5 | 0.636 |
| Radiofrequency ablation | 15/625 | 2.4 | 13/388 | 3.4 | 2/237 | 0.8 | 0.047 |
| Discharge | |||||||
| LVEF (%), mean ± SD | 34.8 | ± 14.2 | 34.2 | ± 13.7 | 36 | ± 14.9 | 0.221 |
| n | 375 | 240 | 135 | ||||
| LVEF variation*, mean ± SD | 8.2 | ± 14.0 | 7.4 | ± 13.7 | 9.5 | ± 14.5 | 0.172 |
| n | 372 | 238 | 134 | ||||
| Length of stay in ICU/ICCU (days), median (IQR) | 12 (7–21) | 11 (7–20) | 13 (8–25) | 0.061 | |||
| n | 380 | 232 | 148 | ||||
| Length of stay in hospital (days), median (IQR) | 16 (11–27) | 16 (11–25) | 19 (12–31) | 0.033 | |||
| n | 367 | 238 | 129 | ||||
| Discharge mode | 0.074 | ||||||
| Home | 141 | 25.4 | 96 | 28.3 | 45 | 20.8 | |
| Rehabilitation | 38 | 6.8 | 23 | 6.8 | 15 | 6.9 | |
| Transferred (other center/other department) | 183 | 33.0 | 116 | 34.2 | 67 | 31.0 | |
| Death | 190 | 34.2 | 103 | 30.4 | 87 | 40.3 | |
| Other | 3 | 0.5 | 1 | 0.3 | 2 | 0.9 | |
| Registration on transplant waiting list | 33/552 | 6.0 | 21/333 | 6.3 | 12/219 | 5.5 | 0.689 |
| Mortality | |||||||
| 30-day mortality | 173 | 26.2 | 94 | 23.3 | 79 | 30.9 | 0.031 |
| 1-year mortality** | 308 | 46.7 | 170 | 42.1 | 138 | 53.9 | 0.003 |
Values in italics indicate the number of patients included in the statistical analysis
CAG, coronary arteriography; ECLS, extracorporeal membrane oxygenation; IABP, intra-aortic balloon pump; ICCU, intensive cardiac care unit; ICU, intensive care unit; IQR, interquartile range; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention; SD, standard deviation
*At discharge compared with admission
**2.5% of patients lost to follow-up at 1-year
Medical management was relatively different between patients with mottling and patients without. Patients with mottling had significantly more volume expansion (p = 0.002), more maximum dose of dobutamine above 10 µg/kg/min (p = 0.007), more often norepinephrine (p = 0.008), or epinephrine (p = 0.001). Indeed, norepinephrine was used in 59% of patients with mottling vs. 48% in patients without (p = 0.008). Epinephrine was used twice more often in patients with mottling compared to patients without mottling (18.4% vs. 9.7%, p = 0.001).
Another major difference was the use of red blood cell transfusion, which was much more frequent in patients with mottling (21.6 vs. 15%, p = 0.03) despite equal levels of hemoglobin in both groups at admission. Regarding organ support, the need for invasive respiratory support was significantly higher in patients with mottling (50.2% vs. 30.1%, p < 0.001) and likewise for the need for RRT (19.9% vs. 12.4%, p = 0.09). However, the need for mechanical circulatory support (MCS) was similar in both groups.
Interventions such as radiofrequency ablation during hospitalization were less frequent in patients with mottling than patients without (0.8% vs. 3.4%, p = 0.047).
Thirty-day and 1-year outcomes and correlates
The median length of stay in hospital was significantly higher in patients exhibiting mottling, with 19 vs. 16 days (p = 0.033). There was no difference between groups regarding discharge mode after hospitalization.
The mortality rate at 30 days and 1 year were significantly increased in patients with mottling compared to patients without (31% vs. 23%, p = 0.031 and 54% vs. 42%, p = 0.003, respectively) (Fig. 1 and Additional file 1: Fig. S1).
Fig. 1.
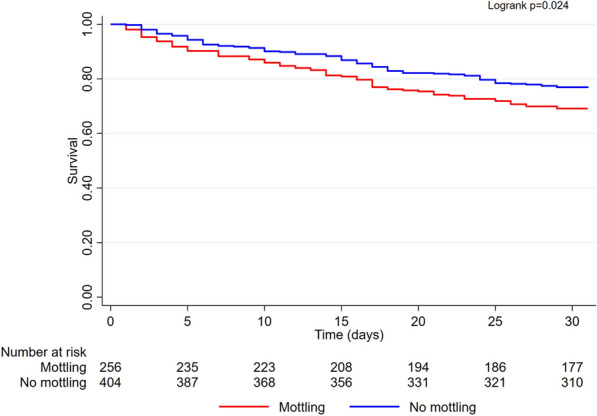
Kaplan–Meier curve showing early and long-term mortality in cardiogenic shock according to the presence of mottling at admission
Multivariate analyses identified as factors associated with 30-day mortality in patients with mottling: low LVEF (HR: 1.03; p = 0.05), low glomerular filtration rate (HR: 1.14; p = 0.036), low hemoglobin (HR: 1.15; p = 0.009), older age (for 1 year) (HR: 1.3; p = 0.03), current smoking (HR: 2.8; p < 0.01), history of ischemic stroke (HR: 2.92; p = 0.01), a mechanical trigger of CS (HR: 3.35; p = 0.022) (Fig. 2). A history of cardiac disease was associated with better outcomes (HR: 0.41; p = 0.001).
Fig. 2.
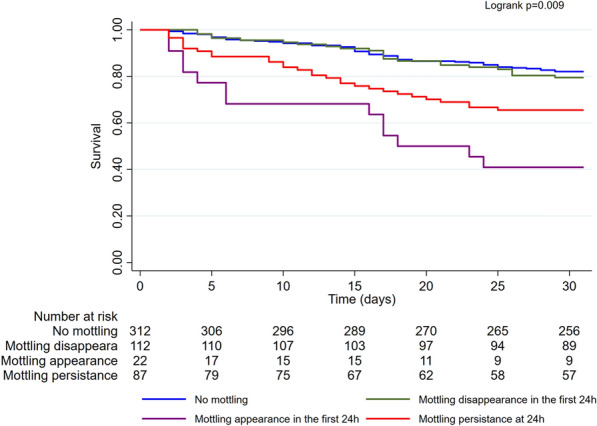
Kaplan–Meier curve showing early and long-term mortality in cardiogenic shock in the subgroup of patients who were still alive after 24 h, according to the presence of mottling at admission and its evolution at 24 h. Survival in the subgroup of patients who were still alive after 24 h according to the presence of mottling at admission and its evolution at 24 h. The “No mottling” group corresponds to patients without mottling at admission or at 24 h. The “mottling disappearance” corresponds to patients with mottling at admission that disappears at 24 h. The “mottling appearance” group corresponds to patients without mottling at admission in which mottling appears at 24 h. The “mottling persistence” group corresponds to patients with mottling at admission and mottling persistence at 24 h
In the subgroup of patients who were still alive after 24 h (Fig. 3), the prognosis of patients whose mottling had regressed was comparable to that of patients who never had mottling (HR = 1.15 [0.71–1.86], p = 0.58 compared with patients who never had mottling). Conversely, the appearance or the persistence of mottling at 24 h was a poor prognostic factor (respectively, HR = 4.68 [2.56–8.57]; p < 0.001, and HR = 2.22 [1.42–3.46]; p < 0.001).
Fig. 3.
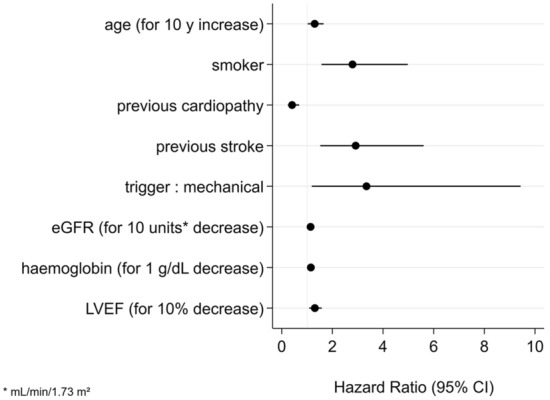
Forest plot of factors at admission associated with 30-day mortality in patients with mottling—multivariate analysis 30-day mortality
Additional file 2: Fig. S2 illustrates the respective weight of mottling and arterial lactate level at admission on mortality: patients without mottling and with arterial lactate < 4 mmol/L had a significantly higher probability of survival as compared with other groups of patients (HR = 0.59 [0.43–0.81], p = 0.001). No difference was found regarding the probabilities of 30-day survival between the three other groups of patients, i.e., patients without mottling and arterial lactate ≥ 4 mmol/L, patients with mottling and with arterial lactate < 4 mmol/L, and patients with mottling and with arterial lactate ≥ 4 mmol/L.
Additional files 3 and 4: Figs. S3 and S4 illustrate the composite endpoint of 30-day mortality or the need for acute mechanical circulatory support as endpoints. Additional file 5: Fig. S5 shows the integration of lactate level and mottling, in a sub-population, in which these parameters can be assessed at admission and 24 h.
Discussion
To date, this analysis of the FRENSHOCK registry is the first analysis of mottling in CS based on a post hoc analysis of a large prospective register of unselected CS. Findings from this validation cohort confirm preliminary results from a previous smaller cohort of patients in cardiogenic shock [9].
Foreseeing the survival of patients with CS at the time of admission is challenging, requiring collection, integration, and analysis of complex clinical manifestations and biomarkers while managing the precarious hemodynamic status. In this pragmatic prospective observational study of patients with CS, we examined the effects of skin mottling assessment during a simple physical examination on survival and other relevant outcomes. The main results are that mottling was present at admission in almost 39% of patients in CS, patients admitted with mottling presented a significantly higher length of stay (19 vs. 16 days, p = 0.033), a higher 30-day mortality rate (31% vs. 23.3%, p = 0.031), and significantly higher mortality at 1-year (54% vs. 42%, p = 0.003). These results were consistent with previous studies based on Forrester's perfusion/congestion profiles, clinically adapted by Nohria et al. [24], showing that CS's main clinical presentations are mostly wet-cold (∼65%) and dry-cold (∼30%) (“cold” meaning hypoperfusion) [8, 25]. Of note, however, mottling as a clinical sign of end-organ hypoperfusion was not part of the parameters initially described by Nohria et al. [24].
The skin, as a conveniently accessible organ, offers the opportunity for easy assessment of local microcirculatory perfusion through observable changes in skin color, i.e., mottling [19]. The pathophysiological underpinnings of hypoperfusion in skin mottling remain incompletely understood [21, 26]. However, studies suggest that the foremost causative mechanism behind diminished blood perfusion is local vasoconstriction caused by sympathetic neuro-activation [27]. Further contributors to impaired microcirculatory flow may include local endothelial dysfunction [28], leukocyte adhesion, platelet activation, and fibrin deposition [19].
Although mottling has been known by physicians for decades [29], it was only in 2011 that Ait-Oufella et al., developed an original clinical score of skin mottling, based on the extension of mottling around the knee (ranging from 0 to 5), allowing a more reliable assessment [30]. The reproducibility of this score was excellent with very good agreement between observers [30]. Based on this scoring system, studies found that mottling score measured 6 h after initial resuscitation in ICU, is a strong predictor of mortality in patients with septic shock [30, 31] but also among all critically ill patients admitted in ICU [32]. A decrease in mottling score during the first 6 h of resuscitation has also been significantly associated with better outcomes in septic shock [33]. Therefore, in 2014, an expert task force of the European Society of Intensive Care Medicine (ESICM) recommended assessing abnormal skin perfusion in their consensus on circulatory shock and hemodynamic monitoring [34].
The primary aim in the management of CS is to restore macrocirculation parameters such as SAP, mean arterial pressure (MAP), and CI. However, some studies have highlighted that up to 45% of patients who die of CS have a restored CI, explaining why optimization of macrocirculatory parameters alone may not be sufficient [35]. This observation may be partly due to organ perfusion disorders that extend beyond the macrocirculation and subsequently lead to multiple organ failures [36]. The state in which the main macrocirculation parameters such as SAP, MAP, and CI are restored, while microcirculation parameters remain impaired, is referred to as "loss of hemodynamic coherence" [37].
Here, past medical history was similar between groups independently of skin mottling (except for a higher rate of already implanted pacemakers or defibrillators in patients without skin mottling). However, in the multivariate analysis, a history of cardiac disease was associated with lower mortality at day 30 in patients with mottling at admission. One hypothesis that might explain this unexpected result, would be because of a vascular adaptation in patients with chronic heart failure [38]. Moreover, a lower prescription of aldosterone antagonists in medical history was also found in patients with mottling. Although there are limited data to date, these results might be explained by the deleterious effect of aldosterone on macro and microcirculation, which have been shown both in pre-clinical animal models [39, 40] and in humans [41, 42].
Clinical presentation and baseline echocardiography were significantly different whether the patient with CS had mottling or not, with higher non-compliance as a trigger of CS, higher heart rate, lower SAP and diastolic arterial pressure, and more severe aortic stenosis among patients with mottling at admission.
In-hospital management significantly differs since catecholamines, inotropes, volume expansion, transfusion, and organ support (invasive ventilation and RRT) were more often used in patients with mottling than in patients without. This was probably due to greater severity, with more mixed circulatory shocks combining a vasoplegic component with the pre-existing cardiogenic one, and also with greater end-organ hypoperfusion requiring more organ support.
Some may attribute these findings to the higher doses of vasopressors in the most severe patients’ group, however, a recent study has shown that mottling remains an independent high prognostic marker regardless of the dose of vasopressors in septic shock [33].
In the subgroup of patients who were still alive after 24 h, the prognosis of patients whose mottling had regressed at 24 h was comparable to that of patients who never had mottling. Whereas, in this subgroup, the appearance or persistence of mottling at 24 h was a poor prognostic factor. However, this subgroup analysis carries the inherent risk of immortal time bias [43].
Simple signs of peripheral tissue perfusion, such as mottling or CRT, could be of interest to guide hemodynamic management in CS. A recent large, randomized control clinical trial, the ANDROMEDA-SHOCK trial, suggested that CRT can be used to guide early resuscitation in septic shock, performing as well as lactate levels [44]. A Bayesian reanalysis of this study even showed that peripheral perfusion-targeted resuscitation may result in lower mortality and faster resolution of organ dysfunction when compared with a lactate-targeted resuscitation strategy [45].
Thus, the main finding of this study is that a simple clinical parameter such as mottling may markedly predict 30-day mortality in CS. As suggested by Additional file 2: Fig. S2, patients presenting mottling at admission have almost the same mortality as patients with an arterial lactate level ≥ 4 mmol/L. Thus, mottling may also be integrated with other variables to develop practical tools for risk assessment of short-term mortality for patients with CS, such as the Cardiogenic Shock Score [46] or the CardShock score [47], to help clinicians in their decision-making processes for MCS indications [48]. Thus, further prospective research is warranted to confirm how using mottling could be integrated in cardiogenic shock management.
As in any observational study, our analysis has limitations. Data from patients who died before informed consent was obtained were not collected and recorded in the database because of administrative regulations. Thus, it cannot be excluded that the most severe patients i.e., with several comorbidities, frailty, or multiple end-stage organ failure could not have been admitted to ICU/ICCU for futility or have been deceased before inclusion. This could be a source of bias resulting in an underestimation of mortality. A confounding bias cannot be eliminated; indeed we cannot exclude that therapeutic management was not guided by peripheral tissue hypoperfusion. The mottling data collected in FRENSHOCK consisted only of the presence or absence of mottling assessed by a senior physician once per day, without information on the intensity and extent of mottling, i.e., the mottling score. It would have been interesting in our study to evaluate this score more closely to better assess the impact of the intensity and modulations of this mottling score on the outcomes. Dark skin patients were not included only because accurate clinical evaluation of mottling is difficult to assess in this population. Another limitation to mention is that SCAI SHOCK Stage Classification was not used for the CS severity classification given that this score was not yet available at the time of the study, since it was published recently in 2019 [49] and updated in 2022 [50]. Finally, mottling cannot be generalized to all patients because dark skin severely limits the ability to properly assess this clinical sign [30].
Conclusion
In this prospective multicenter observational study of critically ill patients with cardiogenic shock, our data confirm that skin mottling at admission in patients with cardiogenic shock was statistically associated with prolonged length of stay, and higher 30-day and 1-year mortalities.
Mottling is a simple non-invasive, priceless tool allowing a real-time assessment of microcirculation at bedside, which seems to be strongly associated with the outcome. Our results suggest that the presence of skin mottling and its evolution should be closely monitored while managing patients with cardiogenic shock. Further prospective research is, however, warranted to define the most effective way to integrate it into the early management of cardiogenic shock.
Supplementary Information
Additional file 1: Fig. S1. Kaplan–Meier curve showing long-term mortality in cardiogenic shock according to the presence of mottling at admission.
Additional file 2: Fig. S2. Survival according to mottling and arterial lactate level at admission.
Additional file 3: Fig. S3. Kaplan–Meier curve showing 30-day mortality or the need for acute mechanical circulatory support in cardiogenic shock according to the presence of mottling at admission.
Additional file 4: Fig. S4. Kaplan–Meier curve showing 30-day mortality or the need for acute mechanical circulatory support in cardiogenic shock in the subgroup of patients who were still alive after 24 h, according to the presence of mottling at admission and its evolution at 24 h.
Additional file 5: Fig. S5. Kaplan–Meier curve showing 30-day mortality, according to the lactate level and the presence of mottling at admission and their evolutions at 24 h (n = 270).
Acknowledgements
FRENSHOCK is a registry of the French Society of Cardiology, managed by its Emergency and Acute Cardiovascular Care Working Group. Our thanks go out to all the devoted personnel of Société Française de Cardiologie who participated in the upkeep of the registry. The authors are deeply indebted to all the physicians who took care of the patients at the participating institutions.
Abbreviations
- CI
Cardiac index
- CRT
Capillary refill time
- CS
Cardiogenic shock
- ESICM
European Society of Intensive Care Medicine
- IABP
Intra-aortic balloon pump
- ICCU
Intensive cardiac care unit
- ICU
Intensive care unit
- IDF
Incident Dark-Field
- LVEF
Left ventricular ejection fraction
- MAP
Mean arterial pressure
- MCS
Mechanical circulatory support
- PCI
Percutaneous coronary intervention
- RRT
Renal replacement therapy
- SAP
Systolic arterial pressure
- SDF
Sidestream Dark-Field
- TAPSE
Tricuspid annular plane systolic excursion
- VA-ECMO
Venoarterial-extracorporeal membrane oxygenation
Author contributions
Coordination and supervision of the FRENSHOCK registry: CD. Funding acquisition: FR, ME, and EB. Project administration: FR, ME, EB, and CD. Investigations: all authors. Conceptualization, HM, FM, and CD. Statistical analysis: VB. Writing—original draft: HM, FM, and CD. Writing—review and editing: AC, LB, FR, CG and VB. Validation: all authors approved the final manuscript.
Funding
The study was sponsored by the Fédération Française de Cardiologie and was funded by unrestricted grants from Daiichi-Sankyo and Maquet SAS.
Availability of data and materials
All summarized data are available upon request.
Declarations
Ethics approval and consent to participate
The data recorded and their handling and storage were reviewed and approved by the CCTIRS (French Health Research Data Processing Advisory Committee) (n° 15.897) and the CNIL (French Data Protection Agency) (n° DR-2016-109).
Consent for publication
All authors hereby consent to the publication.
Competing interests
The authors declare no competing interests.
Footnotes
At a Glance: This work provides new insights into the significance of mottling, a simple and costless clinical parameter, in cardiogenic shock. Mottling at admission is associated with an early prediction of 30-day mortality and long-term mortality at 1 year. The time course of mottling during hospitalization also allows the prediction of the outcome of cardiogenic shock.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reyentovich A, Barghash MH, Hochman JS. Management of refractory cardiogenic shock. Nat Rev Cardiol. 2016;13(8):481–492. doi: 10.1038/nrcardio.2016.96. [DOI] [PubMed] [Google Scholar]
- 2.Tehrani BN, Truesdell AG, Psotka MA, Rosner C, Singh R, Sinha SS, et al. A standardized and comprehensive approach to the management of cardiogenic shock. JACC Heart Fail. 2020;8(11):879–891. doi: 10.1016/j.jchf.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arrigo M, Jessup M, Mullens W, Reza N, Shah AM, Sliwa K, et al. Acute heart failure. Nat Rev Dis Primers. 2020;6(1):16. doi: 10.1038/s41572-020-0151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones TL, Nakamura K, McCabe JM. Cardiogenic shock: evolving definitions and future directions in management. Open Heart. 2019;6(1):e000960. doi: 10.1136/openhrt-2018-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 6.Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032. doi: 10.1161/CIR.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 7.Jung C. Assessment of microcirculation in cardiogenic shock. Curr Opin Crit Care. 2019;25(4):410–416. doi: 10.1097/MCC.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 8.Chioncel O, Mebazaa A, Maggioni AP, Harjola VP, Rosano G, Laroche C, et al. Acute heart failure congestion and perfusion status—impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA Heart Failure Long-Term Registry. Eur J Heart Fail. 2019;21(11):1338–1352. doi: 10.1002/ejhf.1492. [DOI] [PubMed] [Google Scholar]
- 9.Merdji H, Curtiaud A, Aheto A, Studer A, Harjola VP, Monnier A, et al. Performance of early capillary refill time measurement on outcomes in cardiogenic shock: an observational, prospective multicentric study. Am J Respir Crit Care Med. 2022;1:1. doi: 10.1164/rccm.202204-0687OC. [DOI] [PubMed] [Google Scholar]
- 10.De Backer D, Ortiz JA, Salgado D. Coupling microcirculation to systemic hemodynamics. Curr Opin Crit Care. 2010;16(3):250–254. doi: 10.1097/MCC.0b013e3283383621. [DOI] [PubMed] [Google Scholar]
- 11.den Uil CA, Lagrand WK, van der Ent M, Jewbali LS, Cheng JM, Spronk PE, et al. Impaired microcirculation predicts poor outcome of patients with acute myocardial infarction complicated by cardiogenic shock. Eur Heart J. 2010;31(24):3032–3039. doi: 10.1093/eurheartj/ehq324. [DOI] [PubMed] [Google Scholar]
- 12.Jung C, Fuernau G, de Waha S, Eitel I, Desch S, Schuler G, et al. Intraaortic balloon counterpulsation and microcirculation in cardiogenic shock complicating myocardial infarction: an IABP-SHOCK II substudy. Clin Res Cardiol. 2015;104(8):679–687. doi: 10.1007/s00392-015-0833-4. [DOI] [PubMed] [Google Scholar]
- 13.Wijntjens GW, Fengler K, Fuernau G, Jung C, den Uil C, Akin S, et al. Prognostic implications of microcirculatory perfusion versus macrocirculatory perfusion in cardiogenic shock: a CULPRIT-SHOCK substudy. Eur Heart J Acute Cardiovasc Care. 2020;9(2):108–119. doi: 10.1177/2048872619870035. [DOI] [PubMed] [Google Scholar]
- 14.De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL. Microvascular alterations in patients with acute severe heart failure and cardiogenic shock. Am Heart J. 2004;147(1):91–99. doi: 10.1016/j.ahj.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 15.Jung C, Ferrari M, Rodiger C, Fritzenwanger M, Goebel B, Lauten A, et al. Evaluation of the sublingual microcirculation in cardiogenic shock. Clin Hemorheol Microcirc. 2009;42(2):141–148. doi: 10.3233/CH-2009-1194. [DOI] [PubMed] [Google Scholar]
- 16.Guven G, Hilty MP, Ince C. Microcirculation: physiology, pathophysiology, and clinical application. Blood Purif. 2020;49(1–2):143–150. doi: 10.1159/000503775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mongkolpun W, Orbegozo D, Cordeiro CPR, Franco C, Vincent JL, Creteur J. Alterations in skin blood flow at the fingertip are related to mortality in patients with circulatory shock. Crit Care Med. 2020;48(4):443–450. doi: 10.1097/CCM.0000000000004177. [DOI] [PubMed] [Google Scholar]
- 18.De Backer D. Is microcirculatory assessment ready for regular use in clinical practice? Curr Opin Crit Care. 2019;25(3):280–284. doi: 10.1097/MCC.0000000000000605. [DOI] [PubMed] [Google Scholar]
- 19.Hariri G, Joffre J, Leblanc G, Bonsey M, Lavillegrand JR, Urbina T, et al. Narrative review: clinical assessment of peripheral tissue perfusion in septic shock. Ann Intensive Care. 2019;9(1):37. doi: 10.1186/s13613-019-0511-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ait-Oufella H, Bakker J. Understanding clinical signs of poor tissue perfusion during septic shock. Intens Care Med. 2016;42(12):2070–2072. doi: 10.1007/s00134-016-4250-6. [DOI] [PubMed] [Google Scholar]
- 21.Kazune S, Caica A, Volceka K, Suba O, Rubins U, Grabovskis A. Relationship of mottling score, skin microcirculatory perfusion indices and biomarkers of endothelial dysfunction in patients with septic shock: an observational study. Crit Care. 2019;23(1):311. doi: 10.1186/s13054-019-2589-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ospina-Tascon GA, Umana M, Bermudez WF, Bautista-Rincon DF, Valencia JD, Madrinan HJ, et al. Can venous-to-arterial carbon dioxide differences reflect microcirculatory alterations in patients with septic shock? Intens Care Med. 2016;42(2):211–221. doi: 10.1007/s00134-015-4133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Delmas C, Puymirat E, Leurent G, Elbaz M, Manzo-Silberman S, Bonello L, et al. Design and preliminary results of FRENSHOCK 2016: a prospective nationwide multicentre registry on cardiogenic shock. Arch Cardiovasc Dis. 2019;112(5):343–353. doi: 10.1016/j.acvd.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Nohria A, Tsang SW, Fang JC, Lewis EF, Jarcho JA, Mudge GH, et al. Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. J Am Coll Cardiol. 2003;41(10):1797–1804. doi: 10.1016/s0735-1097(03)00309-7. [DOI] [PubMed] [Google Scholar]
- 25.Menon V, White H, LeJemtel T, Webb JG, Sleeper LA, Hochman JS. The clinical profile of patients with suspected cardiogenic shock due to predominant left ventricular failure: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries in cardiogenic shocK? J Am Coll Cardiol. 2000;36(3 Suppl A):1071–1076. doi: 10.1016/s0735-1097(00)00874-3. [DOI] [PubMed] [Google Scholar]
- 26.Ait-Oufella H, Bourcier S, Alves M, Galbois A, Baudel JL, Margetis D, et al. Alteration of skin perfusion in mottling area during septic shock. Ann Intensive Care. 2013;3(1):31. doi: 10.1186/2110-5820-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lima A, Bakker J. Noninvasive monitoring of peripheral perfusion. Intens Care Med. 2005;31(10):1316–1326. doi: 10.1007/s00134-005-2790-2. [DOI] [PubMed] [Google Scholar]
- 28.Bourcier S, Joffre J, Dubee V, Preda G, Baudel JL, Bige N, et al. Marked regional endothelial dysfunction in mottled skin area in patients with severe infections. Crit Care. 2017;21(1):155. doi: 10.1186/s13054-017-1742-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.La D-B. gangrène gazeuse pendant la Première Guerre mondiale (Front occidental) Annales de démographie historique. 2002;103(1):51–70. [PubMed] [Google Scholar]
- 30.Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, et al. Mottling score predicts survival in septic shock. Intens Care Med. 2011;37(5):801–807. doi: 10.1007/s00134-011-2163-y. [DOI] [PubMed] [Google Scholar]
- 31.de Moura EB, Amorim FF, da Cruz Santana AN, Kanhouche G, de Souza Godoy LG, de Jesus AL, et al. Skin mottling score as a predictor of 28-day mortality in patients with septic shock. Intens Care Med. 2016;42(3):479–480. doi: 10.1007/s00134-015-4184-4. [DOI] [PubMed] [Google Scholar]
- 32.Coudroy R, Jamet A, Frat JP, Veinstein A, Chatellier D, Goudet V, et al. Incidence and impact of skin mottling over the knee and its duration on outcome in critically ill patients. Intens Care Med. 2015;41(3):452–459. doi: 10.1007/s00134-014-3600-5. [DOI] [PubMed] [Google Scholar]
- 33.Dumas G, Lavillegrand JR, Joffre J, Bige N, de Moura EB, Baudel JL, et al. Mottling score is a strong predictor of 14-day mortality in septic patients whatever vasopressor doses and other tissue perfusion parameters. Crit Care. 2019;23(1):211. doi: 10.1186/s13054-019-2496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intens Care Med. 2014;40(12):1795–1815. doi: 10.1007/s00134-014-3525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim N, Dubois MJ, De Backer D, Vincent JL. Do all nonsurvivors of cardiogenic shock die with a low cardiac index? Chest. 2003;124(5):1885–1891. doi: 10.1378/chest.124.5.1885. [DOI] [PubMed] [Google Scholar]
- 36.Merdji H, Levy B, Jung C, Ince C, Siegemund M, Meziani F. Microcirculatory dysfunction in cardiogenic shock. Ann Intens Care. 2023;13(1):38. doi: 10.1186/s13613-023-01130-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19(Suppl 3):S8. doi: 10.1186/cc14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Drexler H, Munzel T, Riede U, Just H. Adaptive changes in the periphery and their therapeutic consequences. Am J Cardiol. 1991;67(12):29C–34C. doi: 10.1016/0002-9149(91)90073-t. [DOI] [PubMed] [Google Scholar]
- 39.Arima S, Kohagura K, Xu HL, Sugawara A, Abe T, Satoh F, et al. Nongenomic vascular action of aldosterone in the glomerular microcirculation. J Am Soc Nephrol. 2003;14(9):2255–2263. doi: 10.1097/01.asn.0000083982.74108.54. [DOI] [PubMed] [Google Scholar]
- 40.Lapi D, Emdin M, Mastantuono T, Sapio D, Santillo M, Colantuoni A. Microvascular responses to aldosterone in hamster cheek pouch microcirculation. Clin Hemorheol Microcirc. 2013;53(4):303–315. doi: 10.3233/CH-2012-1552. [DOI] [PubMed] [Google Scholar]
- 41.Gkaliagkousi E, Anyfanti P, Triantafyllou A, Gavriilaki E, Nikolaidou B, Lazaridis A, et al. Aldosterone as a mediator of microvascular and macrovascular damage in a population of normotensive to early-stage hypertensive individuals. J Am Soc Hypertens. 2018;12(1):50–57. doi: 10.1016/j.jash.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 42.Buffolo F, Tetti M, Mulatero P, Monticone S. Aldosterone as a mediator of cardiovascular damage. Hypertension. 2022;79(9):1899–1911. doi: 10.1161/HYPERTENSIONAHA.122.17964. [DOI] [PubMed] [Google Scholar]
- 43.Yadav K, Lewis RJ. Immortal time bias in observational studies. JAMA. 2021;325(7):686–687. doi: 10.1001/jama.2020.9151. [DOI] [PubMed] [Google Scholar]
- 44.Hernandez G, Ospina-Tascon GA, Damiani LP, Estenssoro E, Dubin A, Hurtado J, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs. serum lactate levels on 28-day mortality among patients with septic shock: the ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA. 2019;321(7):654–664. doi: 10.1001/jama.2019.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zampieri FG, Damiani LP, Bakker J, Ospina-Tascon GA, Castro R, Cavalcanti AB, et al. Effects of a resuscitation strategy targeting peripheral perfusion status versus serum lactate levels among patients with septic shock. A Bayesian reanalysis of the ANDROMEDA-SHOCK Trial. Am J Respir Crit Care Med. 2020;201(4):423–429. doi: 10.1164/rccm.201905-0968OC. [DOI] [PubMed] [Google Scholar]
- 46.Beer BN, Jentzer JC, Weimann J, Dabboura S, Yan I, Sundermeyer J, et al. Early risk stratification in patients with cardiogenic shock irrespective of the underlying cause—the Cardiogenic Shock Score. Eur J Heart Fail. 2022;24(4):657–667. doi: 10.1002/ejhf.2449. [DOI] [PubMed] [Google Scholar]
- 47.Harjola VP, Lassus J, Sionis A, Kober L, Tarvasmaki T, Spinar J, et al. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail. 2015;17(5):501–509. doi: 10.1002/ejhf.260. [DOI] [PubMed] [Google Scholar]
- 48.Bernhardt AM, Copeland H, Deswal A, Gluck J, Givertz MM. The international society for heart and lung transplantation/heart failure society of America guideline on acute mechanical circulatory support. J Heart Lung Transpl. 2023;1:1. doi: 10.1016/j.healun.2022.10.028. [DOI] [PubMed] [Google Scholar]
- 49.Baran DA, Grines CL, Bailey S, Burkhoff D, Hall SA, Henry TD, et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock: this document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter Cardiovasc Interv. 2019;94(1):29–37. doi: 10.1002/ccd.28329. [DOI] [PubMed] [Google Scholar]
- 50.Naidu SS, Baran DA, Jentzer JC, Hollenberg SM, van Diepen S, Basir MB, et al. SCAI SHOCK Stage Classification Expert Consensus Update: A Review and Incorporation of Validation Studies: This statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC), International Society for Heart and Lung Transplantation (ISHLT), Society of Critical Care Medicine (SCCM), and Society of Thoracic Surgeons (STS) in December 2021. J Am Coll Cardiol. 2022;79(9):933–946. doi: 10.1016/j.jacc.2022.01.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. S1. Kaplan–Meier curve showing long-term mortality in cardiogenic shock according to the presence of mottling at admission.
Additional file 2: Fig. S2. Survival according to mottling and arterial lactate level at admission.
Additional file 3: Fig. S3. Kaplan–Meier curve showing 30-day mortality or the need for acute mechanical circulatory support in cardiogenic shock according to the presence of mottling at admission.
Additional file 4: Fig. S4. Kaplan–Meier curve showing 30-day mortality or the need for acute mechanical circulatory support in cardiogenic shock in the subgroup of patients who were still alive after 24 h, according to the presence of mottling at admission and its evolution at 24 h.
Additional file 5: Fig. S5. Kaplan–Meier curve showing 30-day mortality, according to the lactate level and the presence of mottling at admission and their evolutions at 24 h (n = 270).
Data Availability Statement
All summarized data are available upon request.