Abstract
Objectives
To determine the baseline risk factors for elective ophthalmic surgery cancellations and characterise the reasons for cancellation.
Methods
This is a retrospective, non-randomised study performed at a large tertiary ophthalmic centre. It included a consecutive sample of patients above the age of 18 who had an ophthalmic surgery scheduled at Cole Eye Institute, Cleveland Clinic, OH between January 2012 and December 2019. An automated search pull identified 75,908 scheduled surgeries (63,987 completed and 11,921 cancelled surgeries). Statistical analysis was performed using R (version 3.5.1). Main outcome measures were baseline factors that impact risk for surgery cancellation and reasons for surgery cancellation.
Results
Analysis was performed on 69,963 scheduled surgeries (57.37% Female, 42.63% Male; Mean age of 62.72 years; 59,959 completed and 10,004 cancelled surgeries). Of the 2384 cancelled surgeries with reasons provided, the most common causes of cancellation were patient refusal (38.42%), patient health condition (18.79%), and rescheduling of surgery (15.27%). Female sex, black race, patient age less than 50 years, non-cataract surgeries, regional mean household income greater than $82,900, Medicare insurance, and geographical distance of less than 10 miles from home to the surgery site were each associated with a significantly increased risk of surgery cancellation (p < 0.01).
Conclusions
This study successfully identified several baseline factors predicting elective ophthalmic surgery cancellation. The clinical insights gained from these lines of enquiry may be used to construct models that not only identify patients at greater risk for cancellation but also highlight which interventions have greatest efficacy in preventing ophthalmic surgery cancellations.
Subject terms: Epidemiology, Health care economics
Introduction
Ophthalmic surgery cancellations affect patient satisfaction and ocular health [1–3]. There is often a delay between diagnosis of a medical condition and its surgical treatment, and the ensuing increased wait time associated with surgery cancellation allows for clinical deterioration, which can increase psychological stress and dependence on others for daily living activities [4]. Within the ophthalmic field, prior literature has noted that preventing cancellation of cataract surgeries could potentially prevent vision loss and improve patient outcomes [3]. Additionally, surgery cancellations decrease the efficiency of healthcare systems and increase the cost of care. The average cost per ocular surgery cancellation has previously been estimated at around $379 [5].
Surgical cancellation can be due to either administrative or patient-related causes. Some of the administrative causes reported involve scarcity of resources, such as unavailable operating room (OR) time, hospital beds, personnel, as well as prioritisation of more emergent cases [2, 6, 7]. Patient-related causes include lack of transportation, financial or insurance concerns, and medical reasons, such as abnormal lab tests or failure to get cleared for surgery [2, 6, 8]. Researchers who have investigated medical causes for elective ophthalmic surgery cancellation suggested that vascular concerns, pulmonary concerns, and uncontrolled diabetes are among conditions that prevented proper pre-surgery clearance [7, 9]. In addition to patient comorbidities, a large number of surgery cancellations for patient-related causes were due to apprehension about undergoing surgery [7, 10].
According to Henderson et al., 41% of ophthalmic surgical cancellations are preventable, especially those due to administrative causes [1]. However, there is no consensus about the most common causes of ophthalmic surgery cancellations, and few studies examine predictive factors of ophthalmic surgery cancellation [1, 10]. Understanding these factors can help guide interventions to minimise cancellations and ultimately improve patients’ visual outcomes. This study aims to identify baseline factors that impact the risk for elective ophthalmic surgery cancellation and characterise the different reasons for cancellation.
Materials/subjects and methods
The study was performed after receiving approval from the Cleveland Clinic Foundation Institutional Review Board. The need for informed consent was waived due to its retrospective nature. The study was compliant with FDA regulations, the Health Insurance Portability and Accountability Act and the Declaration of Helsinki. To determine which baseline factors impact a patient’s risk for ophthalmic surgery cancellation, a retrospective, comparative, non-randomised study was performed both on patients who had experienced surgery cancellations as well as those who had completed their surgeries as scheduled.
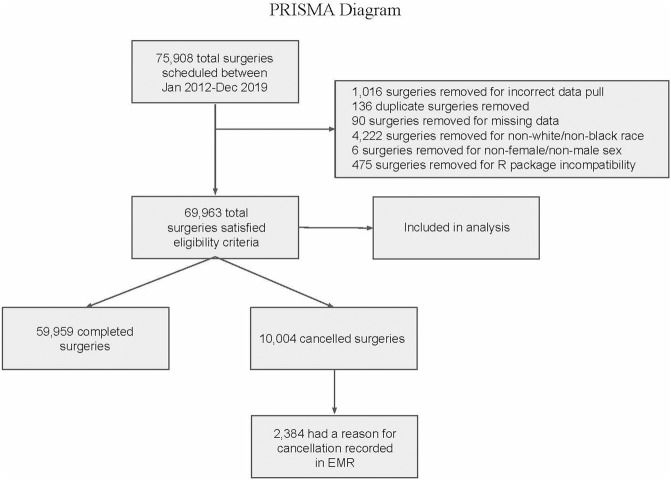
An automated search pull identified 75,908 scheduled surgeries (63,987 completed and 11,921 cancelled surgeries). Patients who were above the age of 18 and had ophthalmic surgery scheduled at Cole Eye Institute, Cleveland Clinic, OH between January 2012 and December 2019 were included in the study. Due to paucity of data available, patients who identified with a sex other than male or female, and race other than black or white were excluded from the analysis. A PRISMA diagram describing the sample selection process is shown in Fig. 1. Variables collected in electronic medical records (EMR) included patient demographic data (age, sex, race, ethnicity), residential zip code, surgery scheduled, scheduled date of surgery, cancelled surgery, date of cancellation, and reason for cancellation.
Fig. 1. PRISMA diagram.
Description of the sample selection process.
Quantitative variables were converted to categorical variables. Patients were categorised based on sample age distribution into groups of younger than 50 years, between 50 and 70 years, and older than 70 years. Residential zip code was used to query median household income using the R package ‘zipcodeR’ [11]. The categories for income were based on Ohio income brackets (<$43,450, $43,450 to $82,900, >$82,900) [12]. The distance from Cole Eye Institute was used to categorise patients as living less than 10 miles away, between 10 and 25 miles away, and greater than 25 miles away. These cutoff values were determined by the distribution of the data. Finally, the time difference between the cancellation date and the surgery date was categorised into less than 7 days and greater than 7 days.
Reasons for ophthalmic surgery cancellation that were recorded in patient charts were categorised into the following groups: transportation, pregnancy, patient refusal, rescheduling of surgery, patient non-adherence, no show, financial reasons, patient health condition, patient improvement, anaesthesiologist scheduling, surgeon scheduling, scheduling error, provider clearance, facility emergency, equipment availability, consent incorrect, and completed previously. These categorisations were based on descriptions provided within the EMR when patients’ cancellations were initially recorded. The charts of patients who cancelled their surgery with verbal commitment to reschedule were reviewed to determine if the surgery was ever rescheduled. If the surgery was found to be rescheduled, they were classified as ‘Rescheduling of Surgery’, otherwise they were classified as ‘Patient Refusal’. Supplementarry Table 1 lists the meanings and gives examples of each reason for cancellation.
To construct a classification learning model, the dataset was randomly split 3:1 into a training dataset and testing dataset. The model was trained with the training dataset and then tested with the testing dataset to assess its predictive capacity in classifying patients at increased risk of surgery cancellation. Testing this model yielded numerous metrics of model performance including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), a receiver operating characteristic (ROC) curve and a precision-recall (PR) curve.
Statistical analysis was performed using R (version 3.5.1). The functions ‘glm’ and ‘multinom’ from the packages ‘stat’ and ‘nnet’ respectively were used for modelling purposes. The packages ‘zipcodeR’ and ‘geosphere’ were used to look up zip code-based median household income data and calculate distance from Cole Eye Institute, respectively. The statistical significance accepted in this study was p < 0.05.
Results
A total of 69,963 outpatient ophthalmic scheduled surgeries (59,959 completed and 10,004 cancelled surgeries) satisfied eligibility criteria and were included in the analysis. Of the 10,004 cancelled surgeries, 2384 had a reason for cancellation recorded in EMR (Fig. 1).
The study population had an overall mean age of 62.72 years and was predominantly white patients (78.71%). The most common types of insurance held within the study population were Medicare (57.79%) and Private (35.20%) insurances. Cataract surgery was the most common surgery scheduled, accounting for 56.32% of scheduled surgeries. Table 1 provides a summary of the study population’s characteristics. The data that support the findings of this study are available on request from the corresponding author KET. The data are not publicly available due to them containing information that could compromise patient privacy/consent.
Table 1.
Summary of Study Population.
| Overall (n = 69,963) | Completed Surgeries (n = 59,959) | All Cancelled Surgeries (n = 10,004) | Cancelled Surgeries With Documented Reasons (n = 2384) | |
|---|---|---|---|---|
| Surgery status, No. (%) | ||||
| Completed | 59,959 (85.70) | |||
| Cancelled | 10,004 (14.30) | |||
| Sex, No. (%) | ||||
| Female | 40,137 (57.37) | 34,180 (57.01) | 5957 (59.55) | 1452 (60.91) |
| Male | 29,826 (42.63) | 25,779 (42.99) | 4047 (40.45) | 932 (39.09) |
| Age, No. (%) | ||||
| <50 | 9611 (13.74) | 7726 (12.89) | 1885 (18.84) | 140 (5.87) |
| 50–70 | 37,067 (52.98) | 31,559 (52.63) | 5508 (55.06) | 701 (29.40) |
| >70 | 23,285 (33.28) | 20,674 (34.48) | 2611 (26.10) | 1543 (64.72) |
| Race, No. (%) | ||||
| White | 55,070 (78.71) | 47,643 (79.46) | 7427 (74.24) | 1859 (77.98) |
| Black | 14,893 (21.29) | 12,316 (20.54) | 2577 (25.76) | 525 (22.02) |
| Income, No. (%) | ||||
| <43,450 | 21,164 (30.25) | 17,871 (29.81) | 3293 (32.92) | 654 (27.43) |
| $43,450–$82,900 | 42,704 (61.04) | 31,559 (52.63) | 5818 (58.16) | 1467 (61.54) |
| >82,900 | 6095 (8.71) | 7726 (12.89) | 893 (8.93) | 263 (11.03) |
| Insurance, No. (%) | ||||
| Medicaid | 3814 (5.45) | 3264 (5.44) | 550 (5.50) | 99 (4.15) |
| Medicare | 40,435 (57.79) | 33,313 (55.56) | 7122 (71.19) | 1689 (70.85) |
| Private/other | 24,624 (35.20) | 22,421 (37.39) | 2203 (22.02) | 569 (23.87) |
| Self-Pay | 1090 (1.56) | 961 (1.60) | 129 (1.29) | 27 (1.13) |
| Distance, No. (%) | ||||
| <10 miles | 25,655 (36.67) | 21,558 (35.95) | 4097 (40.95) | 963 (40.39) |
| 10–25 miles | 26,199 (37.45) | 22,672 (37.81) | 3527 (35.26) | 916 (38.42) |
| >25 miles | 18,109 (25.88) | 15,729 (26.23) | 2380 (23.79) | 505 (21.18) |
| Surgery type, No. (%) | ||||
| Cataract surgery | 39,403 (56.32) | 34,126 (56.92) | 5277 (52.75) | 1446 (60.65) |
| Other | 30,560 (43.68) | 25,833 (43.08) | 4,727 (47.25) | 938 (39.35) |
| Time Difference, No. (%) | ||||
| <7 days | 999 (41.90) | |||
| >7 days | 1385 (58.10) | |||
Analysis of baseline factors predicting surgery cancellation
Baseline factors identified as being significant predictors of surgery cancellation include patient age, sex, race, type of procedure scheduled, mean household income, insurance type, and geographical distance from home to surgery site. Relative to patients above 70 years of age, patients between the age of 50 and 70 were less likely (RR = 0.552 [0.524, 0.581], p < 0.001) to experience a surgical cancellation while patients below 50 years of age were more likely (RR = 1.91 [1.79, 2.03], p < 0.001). Relative to patients who identified as female, patients who identified as male were less likely (RR = 0.930 [0.890, 0.972], p = 0.00132) to have their surgery cancelled. Relative to patients who identified as white, patients who identified as black were more likely (RR = 1.18 [1.11, 1.26], p < 0.001) to have their surgery cancelled. Relative to patients scheduled for non-cataract procedures, patients scheduled for cataract surgeries were less likely (RR = 0.827 [0.790, 0.867], p < 0.001) to have their surgery cancelled. Relative to patients living in an area with a median household income greater than $82,900, patients living in an area with a median household income between $43,450 and $82,900 were less likely (RR = 0.847 [0.782, 0.918], p < 0.001) to have their surgery cancelled. Patients living in an area with a median household income less than $43,450 were also less likely (RR = 0.835 [0.760, 0.917], p < 0.001) to have their surgery cancelled. Relative to patients with Medicare insurance coverage, patients holding private/other insurance were less likely (RR = 0.335 [0.317, 0.354], p < 0.001) to have their surgery cancelled. Similarly, patients holding Medicaid insurance were less likely (RR = 0.427 [0.386, 0.473], p < 0.001) to have their surgery cancelled. Relative to patients living less than 10 miles from the surgery site, patients living between 10 and 25 miles away were less likely (RR = 0.863 [0.812, 0.917], p < 0.001) to have their surgery cancelled. Patients living greater than 25 miles away from the surgery site were also less likely (RR = 0.793 [0.744, 0.844], p < 0.001) to have their surgery cancelled. This data are summarised in Table 2.
Table 2.
Baseline factors predicting surgery cancellation.
| Reference | Factor | Relative Risk [95% CI] | P Value |
|---|---|---|---|
| Income > $82,900 | Income: <$43,450 | 0.835 [0.760, 0.917] | <0.001 |
| Income $43,450–$82,900 | 0.847 [0.782, 0.918] | <0.001 | |
| Non-Cataract Surgery | Cataract Surgery | 0.827 [0.790, 0.867] | <0.001 |
| Sex: Female | Sex: Male | 0.930 [0.890, 0.972] | 0.001 |
| Patient Race: White | Patient Race: Black | 1.183 [1.113, 1.259] | <0.001 |
| Age > 70 | Age <50 | 1.905 [1.785, 2.033] | <0.001 |
| Age >50 and <70 | 0.552 [0.524, 0.581] | <0.001 | |
| Insurance: Medicare | Insurance: Medicaid | 0.427 [0.386, 0.473] | <0.001 |
| Insurance: Private/Other | 0.335 [0.317, 0.354] | <0.001 | |
| Insurance: Self-Pay | 0.402 [0.333, 0.486] | <0.001 | |
| Distance <10 miles | Distance >10 miles and <25 miles | 0.863 [0.812, 0.917] | <0.001 |
| Distance >25 miles | 0.793 [0.744, 0.844] | <0.001 |
Analysis of reasons for surgery cancellation
Of the 2384 cancelled surgeries with reasons provided, the most common causes of cancellation were Patient Refusal (38.42%), Patient Health Condition (18.79%), and Rescheduling of Surgery (15.27%). Other causes of cancellation included Financial Reasons (6.96%), Scheduling Error (5.96%), Provider Clearance (5.79%), Transportation (3.90%), and No Show (1.55%). The least common causes were Surgeon Scheduling (1.17%), Patient Improvement (1.01%), Patient Non-Adherence (0.71%), and Completed Previously (0.46%).
Factors identified as significant predictors of reasons for surgery cancellation were patient race and time of surgery cancellation. Relative to patients who identified as white, patients who identified as black were more likely to have their surgery cancelled with a listed reason of ‘No Show’ (RR = 7.875 [1.199, 51.705], p = 0.032). Relative to surgeries cancelled less than 7 days before their scheduled surgery date, surgeries cancelled more than 7 days before their scheduled surgery date were more likely to be cancelled with a listed reason of ‘Rescheduling of Surgery’ (RR = 4.418 [1.298, 15.034], p = 0.017). This data is summarised in Table 3. Supplementary Table 2 details the full results of the analysis of reasons for cancellation.
Table 3.
Factors predicting reasons for cancellation.
| Reference | Factor | Variable | Financial Reasons | No Show | Patient Health Condition | Patient Improvement | Patient Non-Adherence | Patient Refusal | Provider Clearance | Rescheduling of Surgery | Scheduling Error | Surgeon Scheduling | Transportation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Difference <7 Days | Time Difference >7 Days | Relative Risk [95% CI] | 2.785 [0.801, 9.687] | 0.198 [0.040, 0.991] | 0.796 [0.237, 2.671] | 1.136 [0.266, 4.853] | 0.084 [0.008, 0.883] | 2.191 [0.657, 7.312] | 0.826 [0.238, 2.865] | 4.418 [1.298, 15.034] | 1.709 [0.493, 5.925] | 3.310 [0.757, 14.468] | 0.615 [0.172, 2.193] |
| P Value | 0.11 | 0.05 | 0.71 | 0.86 | 0.04 | 0.2 | 0.76 | 0.02 | 0.4 | 0.11 | 0.45 | ||
| Patient Race: White | Patient Race: Black | Relative Risk [95% CI] | 0.869 [0.172, 4.382] | 7.954 [1.203, 52.595] | 1.107 [0.237, 5.166] | 0.281 [0.020, 3.963] | 0.512 [0.060, 4.367] | 0.897 [0.193, 4.159] | 2.625 [0.540, 12.747] | 0.657 [0.138, 3.120] | 1.033 [0.210, 5.071] | 1.115 [0.160, 7.745] | 0.759 [0.147, 3.912] |
| P Value | 0.87 | 0.03 | 0.9 | 0.35 | 0.54 | 0.89 | 0.23 | 0.6 | 0.97 | 0.91 | 0.74 |
Significant values (p < 0.05) are highlighted.
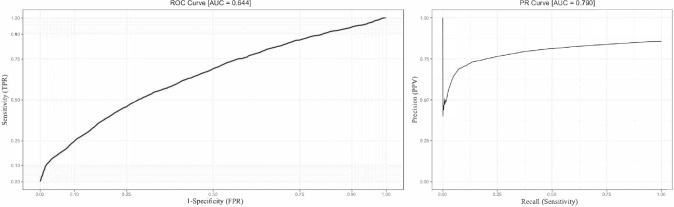
Surgery cancellation prediction model
Using a machine learning algorithm, a classification model was constructed that achieved a sensitivity of 50.14%, specificity of 71.57%, PPV of 22.73%, and NPV of 89.59% when predicting surgery cancellation on a test dataset. The ROC curve and PR curve for this model are shown in Fig. 2. The ROC area under curve (AUC) and the PR AUC were 0.644 and 0.790, respectively.
Fig. 2. ROC and PR curves for the classification model.
AUC is calculated and reported for each curve.
Discussion
This study founds that female sex, black race, younger patient age, non-cataract surgeries, high mean household income, Medicare insurance, and shorter geographical distance from home to surgery site were associated with a significantly increased risk of elective ocular surgery cancellation. Among patients with a documented reason for surgery cancellation, black race and greater lead time to the surgical date were significant predictors of no show cancellations and rescheduled surgeries respectively. The most common reasons for cancellation in this analysis were patient refusal, patient health condition, and rescheduling of surgery. These results support and build on prior literature findings that health conditions and patient refusal are leading causes of surgical cancellation and thus give a potential target for interventions aimed at decreasing cancellations.
There is an incomplete understanding in the current literature on the impact of sex and age on ophthalmic surgery cancellation. Dey et al., which examined the causes of ocular surgery cancellation, found no significant association between patient sex and surgery cancellations; however, they analysed only 5407 ocular surgical procedures (with a cancellation rate of 9.6%) and their results reflect a single institution’s experience that might be specific for the UK population [10]. Studies outside ophthalmology, however, have found an association. Cho et al. examined surgery cancellation across all disciplines in a university hospital in Korea and found that female patients had a lower risk of cancellation [13]. In contrast, this study found that identifying as male was associated with a lower risk of surgery cancellation. These discrepancies indicate that regional or hospital-specific factors could be at play. With regards to patient age, Henderson et al. found that rates of ocular surgery cancellation decreased with increasing patient age [1]. This study found that patients between the ages of 50 and 70 were associated with lower risk of having their surgery cancelled relative to patients above 70 years in age, and patients below the age of 50 were associated with increased risk of experiencing a surgery cancellation. These results argue against the simple inversely proportional relationship between age and rates of ocular surgery cancellation described in Henderson et al.
Like Dey et al., this study also found that non-cataract surgeries were associated with a higher risk of cancellation compared to other ophthalmic surgeries [10]. Given that cataract surgeries are highly efficacious and cost-effective, patients may be less likely to cancel or defer these surgeries [14].
Patient race was another significant predictor of risk for surgery cancellation. Black patients were more likely to have an ophthalmic surgery cancellation and more likely to cancel due to no show relative to white patients. The findings are in concordance with established evidence that black communities are disproportionately affected by socioeconomic hurdles and experience limited access to quality healthcare [15, 16]. Patients who may lack the financial or physical means to transport themselves to their surgery site would be at greater risk of no show cancellations. Interestingly, this study found that patients living in areas with a higher average household income had a higher risk for surgery cancellation than those who live in less wealthy areas, regardless of race. Wealthier patients with reliable access to healthcare and more of a discretionary budget may be more able to cancel or defer an elective surgery. In contrast, Sommer et al. analysed data from the Canadian Community Health Survey over a period of 10 years and found no significant difference in rates of elective surgery cancellation across household income groups [4]. The variance in results speaks to the complex interplay between race, income, healthcare access, and surgery cancellation risk. This analysis is limited by the fact that this research only studied black and white patients and excluded non-black and non-white patients due to the small numbers of patients in other patient populations.”
Regarding insurance status, having Medicare insurance was associated with higher risk for cancellation compared to all other forms of insurance. Medicare and private insurance predominate in the study population, accounting for 92.99% of patients when combined. Therefore, patients who self-paid or held Medicaid insurance may have been insufficiently represented in this study to draw accurate conclusions about these insurance groups.
Another noteworthy finding was that living farther away from their surgery site was associated with a lower risk for cancellation. Although counterintuitive, this may be because patients who live further away need to plan out logistics like transportation in advance, while patients who live closer to their surgery site may be more willing to reschedule or cancel since such logistics do not require as much planning.
Previous studies have examined the relationship between surgery cancellation date and the scheduled surgery date with conflicting results. Henderson et al. found that only 5.3% of ophthalmic surgeries were cancelled within 24 h of the planned surgery time, while Mehran et al. found this to be 56.9% [1, 6]. The majority of surgery cancellations in this study (58.1%) occurred at least a week before the scheduled date of surgery. Patients cancelling at least a week before the scheduled date of surgery were more likely to reschedule their surgery. This is likely because patients with known scheduling conflicts have a greater opportunity to call ahead and reschedule compared to cancellations closer to the scheduled date, where patients may be unable to reschedule due to an urgent change in plans.
The performance of the classification model constructed using a machine learning algorithm can be analysed using ROC and PR curves. The ROC AUC and the PR AUC were 0.644 and 0.7896, respectively. AUC values closer to 1 represent stronger performing classification models. PR curves are more informative than ROC curves when working with binary classification models and datasets with imbalanced class distribution [17]. Given the relatively infrequent occurrence of surgery cancellations compared to completed surgeries, this dataset has an imbalanced class distribution, arguing in favour of using the PR metric. The model yielded a high NPV of 89.59% and specificity of 71.57%, which demonstrates that it was effective at deciding which patients were at low risk of surgery cancellation, but less accurately selected which patients were at higher risk, as evidenced by the low PPV of 22.73% and sensitivity of 50.14%.
There are several limitations of this study. Firstly, categorisation of patients’ reasons for cancellation relied upon the authors’ judgement, which is a possible source of bias. Additionally, the study excluded a large proportion of the population by looking at only black and white patients, which may limit generalisability. Similarly, the model that was constructed uses a binomial distribution and thus, data were converted to categorical variables, which may limit a more nuanced analysis of some of the variables studied in this research.” Another limitation is the methodology used to analyse mean household income, since this data was extracted from patients’ residential zip codes and is dependent on the reliability of the census-based database provided in the R package ‘zipcodeR’. Lastly, the models and results shown in this study are based on datasets of patients seen at one surgery site and therefore, these results may not be fully generalisable across different geographical regions.
However, this study successfully identified several baseline factors predicting elective ophthalmic surgery cancellation and characterised reasons for cancellation. The depth of analysis in this study was extensive, incorporating a large sample of scheduled surgeries across 8 years. Female sex, black race, patient age less than 50 years, non-cataract surgeries, regional mean household income greater than $82,900, Medicare insurance, and geographical distance of less than 10 miles from home to the surgery site were all associated with increased risk of surgery cancellation. Current suggestions for the prevention of surgical cancellation include general preoperative clinics that assess a patient’s readiness and health status in preparation for elective ophthalmic surgery [7]. This general approach could certainly reduce surgery cancellation rates, but more targeted interventions would likely have greater efficacy. Given that there is no definitive consensus on interventions that may reduce ophthalmic surgery cancellation, this remains an avenue of future exploration by which patient health outcomes and healthcare efficiency can be markedly improved. The data gathered from such lines of enquiry could be used to construct models that not only identify patients at greater risk for cancellation but also highlight which interventions would have greatest efficacy in preventing a surgery cancellation.
Summary table
What was known before
Ophthalmic surgery cancellations negatively affect patient satisfaction and ocular health. Additionally, surgery cancellations decrease the efficiency of healthcare systems and increase the cost of care. Prior literature has noted that preventing cancellation of cataract surgeries could potentially prevent vision loss and improve patient outcomes. There is no consensus about the most common causes for ophthalmic surgery cancellations, and few studies examine predictive factors of ophthalmic surgery cancellation.
What this study adds
This study found that female sex, black race, younger patient age, non-cataract surgeries, high mean household income, Medicare insurance, and shorter geographical distance from home to surgery site were all associated with a significantly increased risk of elective ocular surgery cancellation.
Among patients with a documented reason for surgery cancellation, black race and greater lead time to the surgical date were significant predictors of no show cancellations and rescheduled surgeries respectively. The most common reasons for cancellation in this analysis were patient refusal, patient health condition, and rescheduling of surgery.
The clinical insights gained may be used to construct models that not only identify patients at greater risk for cancellation but also highlight which interventions would have greatest efficacy in preventing ophthalmic surgery cancellations.
Supplementary information
Acknowledgements
RPS reports personal fees from Genentech/Roche, personal fees from Alcon/Novartis, grants from Apellis and Graybug, personal fees from Zeiss, personal fees from Bausch + Lomb, personal fees from Regeneron Pharmaceuticals, Inc and personal fees from Gyroscope and Asceplix. KET reports personal fees from Genentech/Roche, research fees from Zeiss and research grants from Regenxbio. All other authors report no disclosures. The authors report no funding sources related to this research. This work has not been presented at any meetings.
Author contributions
ARB was responsible for conducting the analysis, extracting and analysing data, interpreting results, writing the report, updating reference lists and creating the data tables. RK was responsible for designing the study protocol, interpreting results, writing the report, and updating reference lists. CCSV was responsible for interpreting results, writing the report, and providing feedback on the report. AK was responsible for designing the study protocol and extracting the data. RPS and KET were responsible for designing the study protocol and providing feedback on the report.
Data availability
The data that support the findings of this study are available on request from the corresponding author KET. The data are not publicly available due to them containing information that could compromise patient privacy/consent.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41433-023-02421-2.
References
- 1.Henderson BA, Naveiras M, Butler N, Hertzmark E, Ferrufino-Ponce Z. Incidence and causes of ocular surgery cancellations in an ambulatory surgical center. J Cataract Refract Surg. 2006;32:95–102. doi: 10.1016/j.jcrs.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 2.al Talalwah N, McIltrot KH. Cancellation of surgeries: integrative review. J PeriAnesthesia Nurs. 2019;34:86–96. doi: 10.1016/j.jopan.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Mayro EL, Pizzi LT, Hark LA, Murchison AP, Wisner D, Koka A, et al. A proposed intervention to decrease resident-performed cataract surgery cancellation in a tertiary eye care center. Am Health Drug Benefits. 2018;11:480–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Sommer JL, Jacobsohn E, El-Gabalawy R. Impacts of elective surgical cancellations and postponements in Canada. Can J Anesthesia. 2021;68:315–23. doi: 10.1007/s12630-020-01824-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maimaiti N, Rahimi A, Aghaie LA. Economic impact of surgery cancellation in a general hospital. Ethiop J Health Dev. 2016;30:94–8.
- 6.Mehran N, Ojalvo I, Myers JS, Razeghinejad R, Lee D, Kolomeyer NN. Surgical cancellations in glaucoma practice. Ophthalmol Glaucoma. 2021;4:427–32. doi: 10.1016/j.ogla.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 7.Maa A, Sullivan BR. Medical reasons for same-day cancellations in ophthalmic surgery at a VA hospital. Federal Pract. Published online 2010;27:17–21.
- 8.Boudreau SA, Gibson MJ. Surgical cancellations: a review of elective surgery cancellations in a tertiary care pediatric institution. J PeriAnesthesia Nurs. 2011;26:315–22. doi: 10.1016/j.jopan.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Bamashmus M, Haider T, Al-Kershy R. Why is cataract surgery canceled? A retrospective evaluation. Eur J Ophthalmol. 2010;20:101–5. doi: 10.1177/112067211002000113. [DOI] [PubMed] [Google Scholar]
- 10.Dey M, Fitter S, Ibrahim J. The incidence and causes of ocular surgery cancellations in a district general hospital unit. Invest. Ophthalmol. Vis. Sci. 2008;49:4993.
- 11.Rozzi GC. zipcodeR: advancing the analysis of spatial data at the ZIP code level in R. Softw Impacts. 2021;9:100099. doi: 10.1016/j.simpa.2021.100099.. [DOI] [Google Scholar]
- 12.Ohio Department of Taxation. Annual Tax Rates. https://tax.ohio.gov/wps/portal/gov/tax/individual/resources/annual-tax-rates.
- 13.Cho HS, Lee Y, Lee S, Kim J, Kim T. Reasons for surgery cancellation in a general hospital: a 10-year study. Int J Environ Res Public Health. 2018;16. 10.3390/ijerph16010007 [DOI] [PMC free article] [PubMed]
- 14.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–8. doi: 10.1016/j.ophtha.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Waidmann TA, Rajan S. Race and ethnic disparities in health care access and utilization: an examination of state variation. Med Care Res Rev. 2000;57:55–84. doi: 10.1177/1077558700057001S04. [DOI] [PubMed] [Google Scholar]
- 16.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57:108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 17.Saito T, Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLOS One. 2015;10:0118432. doi: 10.1371/journal.pone.0118432.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author KET. The data are not publicly available due to them containing information that could compromise patient privacy/consent.