Abstract
Liver transplantation is the treatment of choice in majority of the patients with end stage liver disease. Vascular complication following liver transplantation is seen in around 7–13% of the patients and is associated with graft dysfunction and high morbidity and mortality. Early diagnosis and prompt treatment are crucial in management of these patients. Advances in interventional radiology have significantly improved the management of vascular complications using minimally invasive percutaneous approach. Endovascular management is preferred in patients with late hepatic artery thrombosis, or stenosis, whereas retransplantation, surgical revision, or endovascular management can be considered in patients with early hepatic artery thrombosis or stenosis. Hepatic artery pseudoaneurysm, arterioportal fistula, and splenic artery steal syndrome are often treated by endovascular means. Endovascular management is also preferred in patients with symptomatic portal vein stenosis, early portal vein thrombosis, and symptomatic late portal vein thrombosis, whereas surgical revision or retransplantation is preferred in patients with perioperative portal vein thrombosis occurring within 3 days of transplantation. Venoplasty with or without stent placement can be considered in patients with hepatic venous outflow tract or inferior vena cava obstruction. Transjugular intrahepatic portosystemic shunt (TIPS) may be required in transplant recipients who develop cirrhosis, often, secondary to disease recurrence, or chronic rejection. Indications for TIPS remain same in the transplant patients; however, major difference is altered vascular anatomy, for which adjunct techniques may be required to create TIPS.
Keywords: liver transplantation, vascular complications, imaging, interventional radiology, TIPS
Graphical abstract
Highlights
-
•
Vascular complication following liver transplantation is seen in around 7–13% of the patients, and early diagnosis and prompt treatment are crucial in management of these patients.
-
•
Endovascular management is the preferred in patients with late hepatic artery thrombosis or stenosis, whereas retransplantation, surgical revision, or endovascular management can be considered in patients with early hepatic artery thrombosis or stenosis.
-
•
Hepatic artery pseudoaneurysm, arterioportal fistula, splenic artery steal syndrome, and hepatic venous/inferior vena cava complications are often treated by endovascular means.
-
•
Endovascular management is also preferred in symptomatic portal vein stenosis, early portal vein thrombosis, and symptomatic late portal vein thrombosis, whereas, surgical revision or retransplantation is preferred in perioperative portal vein thrombosis occurring within 3 days of transplantation.
-
•
Indications for transjugular intrahepatic portosystemic shunt (TIPS) remain same in the transplant patients; however, major difference is altered vascular anatomy, for which adjunct techniques may be required to create TIPS.
Liver transplantation (LT) is the treatment of choice in patients with end stage liver disease and is the second most transplanted organ in the United States, after kidney.1,2 In recent times, living donor LT has been on the rise, considering reduced wait time compared to deceased donor, and also reduced cold ischemic period of transplanted liver. Vascular complications following LT are not uncommon, with incidence of around 7% for deceased donor LT, and 13% for liver donor LT, and are associated with high incidence of graft loss and mortality.1 Transplant-related complications are classified into early (<1 month) and late (>1 month) complications depending on the interval between LT and occurrence of complication. Majority of the vascular complications occur within 3 months of transplant and often present with nonspecific derangement of liver function. Thus, imaging at immediate postoperative period and at follow-up plays an important role in the diagnosis and management of vascular complications.3 Recent improvement in surgical techniques and perioperative medical management have reduced the morbidity and mortality of the transplant patients, with 1-year survival ranging between 86.9% and 93.8%, and 3-year survival between 78.2% and 90.4%.2,4 Hand in hand, in the recent past, there have been advances in interventional radiology that has significantly improved the management of posttransplant complications, using minimal invasive percutaneous approach, obviating the need for repeat surgery and associated morbidity.5 In this review, we will discuss common vascular complications following LT (Table 1), their diagnosis, and role of interventional radiology in their management.
Table 1.
Vascular Complications Following Liver Transplantation.
| Vascular complications |
|---|
| Hepatic artery complications |
| Hepatic artery thrombosis |
| Stenosis |
| Pseudoaneurysm |
| Hepatic artery rupture |
| Portal vein complications |
| Portal vein thrombosis |
| Portal vein stenosis |
| Portal vein steal syndrome |
| Arterial portal fistula |
| Inferior vena cava or hepatic vein thrombosis or stenosis |
| Splenic steal syndrome or portal hyper perfusion syndrome |
Diagnosis of Vascular Complications
Doppler ultrasonography (DUS) is widely used for routine postoperative screening following LT and also to diagnose vascular complications. On table, DUS is performed immediately after anastomosis to confirm adequate hepatic perfusion. Follow-up ultrasonography is performed with in 24 h of transplant to rule out vascular complications. DUS is often performed once or twice daily, in posttransplant patients till 5th postoperative day and in patients with clinical suspicion of vascular complications.6 Common posttransplant findings include periportal edema, edema along the resection margin, perihepatic hematoma, ascites, and right pleural effusion. These usually resolve within first few weeks. Careful assessment of hepatic artery, portal vein, hepatic vein/inferior vena cava (IVC), and biliary anastomoses should be performed.1 Common doppler parameters measured include peak systolic velocity (PSV), systolic upstroke, acceleration time, and resistivity index. Hepatic artery should be evaluated at proper hepatic artery, and right and left intrahepatic segments. Visualization of anastomoses is desired but can be obscured by air shadows during immediate postoperative period. Normal hepatic artery shows variable PSV in immediate postoperative period, steep systolic upstroke, and resistivity index between 0.55 and 0.8. Splenic artery should be evaluated at the hilum, as an internal control to assess hepatic artery, for velocities and resistivity index can be altered with altered systemic hemodynamics, or celiac artery disease. Portal assessment should include main portal vein, and right and left intrahepatic branches. Increased portal vein PSV can be seen in immediate posttransplant period, which gradually normalizes over time. Hepatic veins can show mono-, bi-, or triphasic flow in immediate posttransplant period, which gradually normalizes to triphasic pattern.2,6, 7, 8 Contrast-enhanced computed tomography (CECT) should be performed when vascular abnormality is suspected on DUS or when there is impairment of liver function, and ultrasonography is inconclusive. Magnetic resonance imaging (MRI) is performed if there are contraindications to CECT.1,9
Hepatic Artery Complications
Hepatic artery complications can occur in 4–16% of transplant patients and are associated with high morbidity and mortality.9 Unlike normal liver, transplanted liver has no arterial collateral supply, and hepatic artery is the only arterial supply to biliary system and liver. Therefore, impaired hepatic arterial flow can lead to biliary complications, liver abscess, and graft dysfunction.2,6 Hepatic artery complications are classified into early and late complications depending on the interval between LT and occurrence of complication. Early complications occur within 1 month of transplant and are associated with high incidence of graft dysfunction and mortality. Late complications occur after 1 month of transplant and are often associated with biliary complications.1,6
1. Hepatic artery thrombosis (HAT)
Hepatic artery thrombosis is the most common vascular complication and can be seen in 3–9% of patients following adult LT, and 11–26% patients following pediatric LT.4,6 The incidence of HAT has declined progressively over the past, with current incidence of around 2–3%. HAT is associated with very high morbidity and mortality, with mortality rate ranging between 27% and 58%, and graft loss rate of 50–60%.4, 5, 6,10
Risk factors for HAT include surgical technique (iatrogenic), small donor hepatic artery, donor age >60 years, aortic jump graft, hepatic artery stenosis, rejection, ischemic reperfusion injury, coagulation abnormalities, ABO incompatible transfusion, and prior transarterial chemoembolization.3,5
DUS is the first-line investigation in the diagnosis of HAT. Parameters to be measures include hepatic artery diameter, PSV, and resistivity index. HAT is associated with absence of flow in hepatic artery, with increased resistivity index proximal to thrombosed segment. In patients with suspected HAT on DUS, CECT is performed to confirm the same (Figure 1).1,4
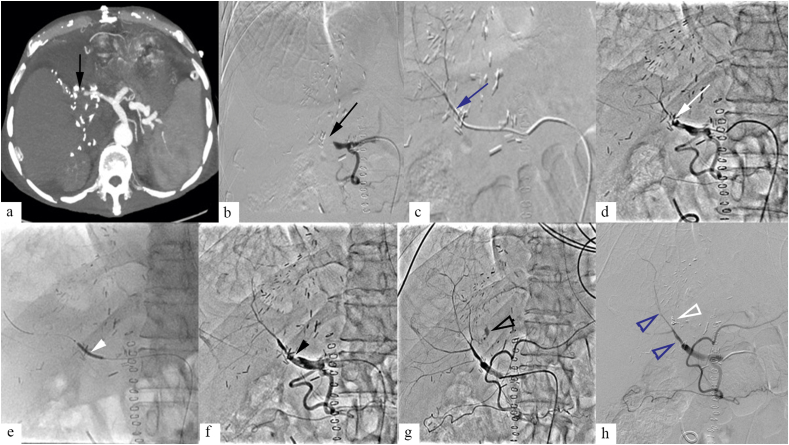
Figure 1.
A 44-year-old male patient, presenting with graft dysfunction at postoperative day 8 of liver transplantation. Contrast enhanced CT (a), and digital subtraction angiogram (DSA) (b) showed hepatic artery thrombosis (HAT) (black arrow). Catheter directed thrombolysis (CDT) was done for HAT (c). DSA at 24 h of thrombolysis (d) showed hepatic artery stenosis (HAS) at the anastomotic site, for which balloon angioplasty was done (e, white arrowhead). Postangioplasty DSA (f) showed residual HAT (black arrowhead). CDT was continued for 12 h, following which DSA was done which showed resolution of HAT, and improved hepatic artery flow (h, blue open arrowhead). However, arterial extravasation was noted along the hepatic cut surface (g, black open arrowhead), for which selective coil embolization was done (h, white open arrowhead).
Retransplantation is the treatment of choice for early HAT, however, is limited due to scarcity of donor liver. Surgical revascularization procedures can be done; however, it is difficult to treat extensive intrahepatic thrombosis. Surgical revision is preferred in early HAT occurring within 5 days of transplant, unless comorbidities preclude surgery, when endovascular treatment can be done. Endovascular treatment of HAT in 1st week following transplant carries risk of hepatic artery rupture. Endovascular revascularization is often the first line of treatment in HAT occurring after 1 week of transplant (Figure 1).6,11, 12, 13 In patients with late onset HAT, when onset of HAT is gradual, collaterals can develop, perfusing the intrahepatic branches of hepatic artery. These patients may not require endovascular intervention.13
Endovascular treatment for HAT includes intraarterial thrombolysis, with or without balloon angioplasty, and stenting. In comparison with systemic anticoagulation, intraarterial thrombolysis has the advantage of high local thrombolytic concentration, lower thrombolytic dose required, and minimal systemic side effects or hemorrhage risk.11,14,15
For endovascular procedure, femoral artery access is commonly achieved using 5F or 6F sheath. Guide catheter or sheath is placed in celiac artery or at the origin of common femoral artery, through which microcatheter and guidewire is coaxially introduced to selectively catheterize hepatic artery; 0.014 or 0.018 system is used to reduce the risk of vasospasm and arterial injury. Additionally, intra-arterial nitroglycerin through the guide catheter reduces the risk of vasospasm. Angiogram is taken to confirm the diagnosis. After crossing the occlusion, multiple side hole catheter is then placed across the thrombosed segment for continuous infusion of thrombolytic agent, either recombinant tissue plasminogen activator (0.5–1 U/hour, maximum dose of 24 U/day) or urokinase. If occlusion cannot be crossed, single end hole catheter can be placed just proximal to thrombosis, for thrombolytic infusion. Heparin can be simultaneously infused (1000 U/hour) through the vascular access sheath. Angiography is repeated after 24 h to look for resolution of thrombosis. Decision for continuation of thrombolytic therapy is taken based on the angiographic findings. In case of persistent thrombosis or narrowing, angioplasty and/or stenting can be considered.6,13,16
2. Hepatic artery stenosis (HAS)
Hepatic artery stenosis is seen in 4–11% of the transplant patients, and is more common at the site of anastomoses.1,4,6
Risk factors for HAS include artery size mismatch, clamp injury, interrupted vasa vasorum during transplantation, extrinsic compression, graft rejection, ischemic injury during cold preservation, and prior transarterial chemoembolization.4
DUS is the first line of investigation in diagnosis of HAS. DUS findings in HAS include.
-
a.
Prestenotic hepatic artery shows resistivity index of >0.80. However, one should remember that resistivity index >0.80 can be seen in normal patients during immediate posttransplant period for first 3 days, which then gradually normalizes.
-
b.
At the site of narrowing, hepatic artery PSV measures >200 cm/s and shows turbulent flow. Hepatic artery PSV >400 cm/s can be seen in patients with >70% narrowing.
-
c.
Poststenotic hepatic artery shows reduced resistivity index (<0.50) and parvus-tardus waveform.1,4,6,17
HAS suspected on DUS is confirmed with CT angiography (Figure 1), which is the technique of choice. CT angiography allows better quantification of stenosis and also allows evaluation of hepatic artery when DUS is not possible due to improper window.1
Early HAS can be treated with surgical revision or endovascular management; however, endovascular management carries some risk of hepatic artery injury and rupture in early postoperative period.13 Endovascular management is the first line of management for late onset HAS. Endovascular management options include angioplasty (Figure 1) with or without stenting and primary stenting alone. Both techniques are equally efficacious, with similar complication rates.6,17 A 2012 meta-analysis by Rostambeigi et al. showed that both angioplasty and stent placement were equally efficacious, with comparable patency rate.18 A more recent comparative study by Magand et al. showed higher 1 year patency rate with stent (93.8%) than with angioplasty alone (73.5%).19 PTA alone for significant HAS carries risk of dissection and hepatic artery rupture in 7% of patients. Hepatic artery rupture or extravasation can be managed with covered stent placement.20 Use of coronary stent for hepatic artery stenosis is considered as an off-label indication. Following stenting, 75 mg clopidogrel is administered daily for 6 months and 81 mg aspirin daily, indefinitely.13 Surgical revascularization is considered for patients where endovascular treatment is unsuccessful. Retransplantation is treatment of choice, however, is limited by scarcity of liver graft and is reserved for patients where revascularization procedures fail.6
3. Hepatic artery pseudoaneurysm (HAP)
Hepatic artery pseudoaneurysm is a contained leak from the hepatic artery, which commonly occurs secondary to iatrogenic injury during transplantation. Incidence of HAP ranges between 0.27 and 3%.1,6 HAP more commonly occurs within 1 month of transplant, and associated mortality is high ranging between 69% and 100%.6,21
HAP can be extrahepatic or intrahepatic. Extrahepatic pseudoaneurysm often occurs at anastomotic site. Risk factors for extrahepatic pseudoaneurysm include technical difficulties during transplantation, treatment of HAS, and peritoneal infection. Intrahepatic pseudoaneurysm commonly occurs after liver biopsy, where HAP can be seen in ∼50% of patients undergoing biopsy in 1st week, and incidence drops to 10% in patients undergoing biopsy after a month. Intrahepatic pseudoaneurysm can also be associated with bile duct infections.1,8,22
While some of the patients can be asymptomatic, majority of the patients present with massive hemorrhage, gastrointestinal bleed, hemorrhagic shock, or nonspecific symptoms of fever and abdominal pain.21
On DUS, HAP is seen as anechoic or hypoechoic outpouching with turbulent flow within giving yin-yang appearance on color doppler. On CT angiography, HAP is seen as contrast-filled outpouching, whose density matches that of the adjacent hepatic artery.1
Endovascular management is the preferred treatment in HAP, and surgery is considered in patients where endovascular treatment isn't successful. Stent graft is preferred treatment for extrahepatic HAP where HAP is excluded while preserving hepatic arterial supply. Other less preferred endovascular methods include intra-aneurysmal thrombin injection or coil placement.6,13 Intrahepatic HAP can be embolized with coils (Figure 1) or liquid embolizing agents or by US-guided thrombin injection.13
Hepatic Artery Rupture (HAR)
Hepatic artery rupture is characterized by active extravasation from the hepatic artery, which can occur spontaneously or as a complication of HAP. HAR is uncommon, with the incidence of 0.64%.23 It is associated with high chances of graft dysfunction and mortality. Anastomotic site infection is an important predisposing factor for HAP or HAR.6
Patients can present with hemoperitoneum, hematoma, gastrointestinal bleed, or hemorrhagic shock. CT angiography can be useful to confirm the diagnosis; however, HAR being life-threatening emergency, patient is often directly taken up for endovascular management, or surgery, when HAR is suspected. Endovascular management includes embolization and/or covered stent placement to cover the site of extravasation.6,23
Portal vein complications
Portal vein complications are uncommon, seen in less than 2% of population.24 Portal vein complications are more common in pediatric or living donor LT, and split liver graft. Surgical anastomosis is the most common site involved. Portal vein complications following LT include portal vein thrombosis, and portal vein stenosis.1,6,25
Portal vein thrombosis (PVT)
Portal vein thrombosis is an uncommon complication, with incidence of 0.3–2.6%.26
Risk factors for PVT include small caliber or hypoplastic portal vein, redundant portal vein, prior PVT requiring thrombectomy, prior portal vein intervention, redundant portal vein, portal vein stenosis or kinking, and large portosystemic collaterals.6
Early PVT can present with acute graft dysfunction and can have poor prognosis, whereas late PVT often presents with features of portal hypertension such as variceal bleed, ascites, and severity of which depends on extent of portosystemic collaterals.6,13
DUS is often the first line of investigation in patients suspected to have PVT. On DUS, PVT is seen as echogenic intraluminal thrombus, with absent flow in portal vein. PVT is seen as intraluminal filling defect on contrast-enhanced CT and MRI (Figure 2).1,4,6
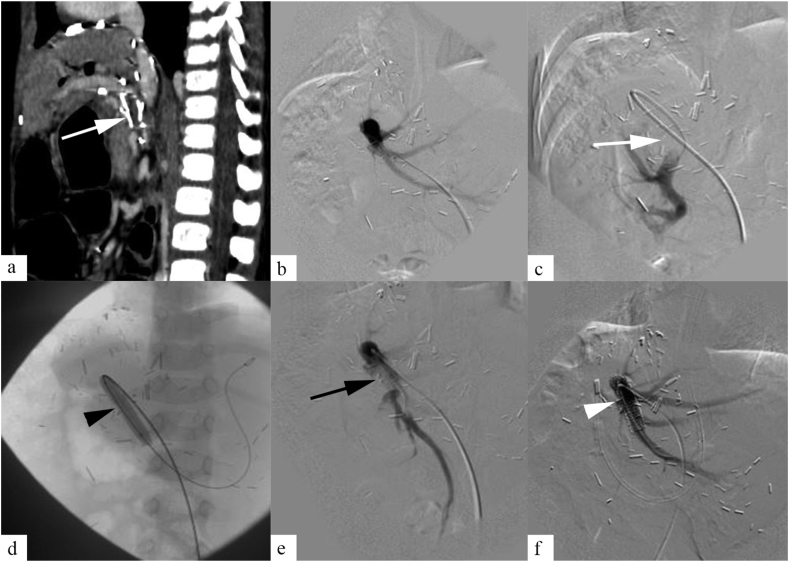
Figure 2.
A 34-month-old male child presenting with variceal bleeding, 3 months following liver transplantation. Contrast enhanced CT abdomen (a), and DSA (b, c) showed chronic thrombosis of portal vein graft (white arrow). Percutaneous transhepatic access was achieved, and balloon angioplasty was done for portal vein thrombosis (d, black arrowhead). DSA following angioplasty (e) showed residual portal vein thrombosis (black arrow). Stenting was done across the portal vein graft (f, white arrowhead), and final angiogram showed good flow across the stent.
Surgical revision is preferred in patients with early PVT occurring within 3 days of transplant. Retransplantation is considered in patients where surgical revision fails.13 In patients who are not suitable for surgery due to comorbidities, catheter-directed thrombolysis can be considered. Endovascular management is preferred in patients with PVT presenting between 3 days and 30 days posttransplant. Endovascular management includes catheter-directed thrombolysis, angioplasty, and/or stenting. In patients presenting after 30 days, management depends on clinical features. Asymptomatic patients with normal liver function are managed conservatively. Symptomatic patients can be managed with systemic anticoagulation and/or endovascular treatment (Figure 2).6
For endovascular management, either direct or indirect approach can be used. In direct approach, access into portal vein is achieved through one of the following routes:
-
a.
Transjugular intrahepatic portosystemic shunt (TIPS) route is preferred in patients with coagulopathy and ascites. It has the advantage of lower bleeding risk, treatment of associated features of portal hypertension such as ascites, and variceal bleeding, and resolution of PVT due to improved flow through portal vein. TIPS access can be difficult if patients has portal vein thrombosis and is time-consuming.
-
b.
Transhepatic route (Figure 2) is relatively easy procedure, with short procedure time. However, it is associated with high bleeding risk especially in patients with ascites, coagulopathy, or patients requiring longer duration of catheter-directed thrombolysis.
-
c.
Transileocolic venous route requires surgical access and is used when altered anatomy and/or ascites precludes TIPS or transhepatic access.
-
d.
Transsplenic route is used only when other direct approach, medical and surgical management, has failed. It is associated with high risk of bleeding.
In indirect approach, SMA is cannulated commonly through transfemoral access. It is only suitable for catheter-directed thrombolysis. Mechanical thrombectomy, angioplasty, and stent aren't possible through this route.
For catheter-directed thrombolysis, multiple side hole catheter or single end hole microcatheter is placed within the thrombus for continuous thrombolytic infusion (recombinant tissue plasminogen activator, 0.5–1 U/hour, maximum dose of 24 U/day). Heparin infusion (1000 U/hour) is given through access sheath. Thrombolysis can be continued for 3–10 days, depending on the extent of thrombosis, during which thrombin time is maintained between 1.5 and 2.5, and activated partial thromboplastin time is maintained between 2 and 2.5.4,6 Once the thrombolysis is complete, vascular access is removed. In case of transhepatic or trans splenic access, access tract is embolized using coil or glue. Patients is then shifted to systemic anticoagulation, when international normalized ratio (INR) is maintained between 2 and 3.4,6 Technical success rate for endovascular treatment ranges between 68%, and 100%, with procedure related morbidity and mortality of ∼11% and 0% respectively.27 Data on long-term patency are limited.
Portal Vein Stenosis (PVS)
Portal vein stenosis is an uncommon complication seen in 1–2% of transplant patients.25,28,29 They more commonly occur after 6 months of posttransplant and usually occur at anastomotic site.
Risk factors for PVS include donor–recipient portal vein mismatch, donor portal vei–graft mismatch, complex anastomosis, technical difficulties in anastomosis, and neoadjuvant adjuvant chemotherapy prior to transplant. PVS is more common in patients with pediatric or adult split liver graft. Early PVS is often due to surgical cause, and late PVS occurs due to intimal hyperplasia and fibrosis.4,6,30
PVS can present with symptoms of portal hypertension such as ascites, variceal bleeding, and splenomegaly, liver function abnormality, and sometimes lead to PVT. Many patients with PVS are asymptomatic.4, 5, 6
DUS is often the first line of investigation in diagnosis of PVS. In patients with significant PVS (characterized by >50% narrowing of portal vein), PSV at the site of stenosis is often >125 cm/s. However, PSV measurement can be affected by varied anatomy and angle of insinuation. Therefore, ratio of PSV in stenotic segment versus prestenotic segment >3 is preferred criteria in diagnosis of PVS. Turbulent flow can be seen at the site of stenosis; however, it could be normal finding in immediate posttransplant period. CT angiography can confirm the diagnosis and quantify the extent of the disease (Figures 3 and 4).1
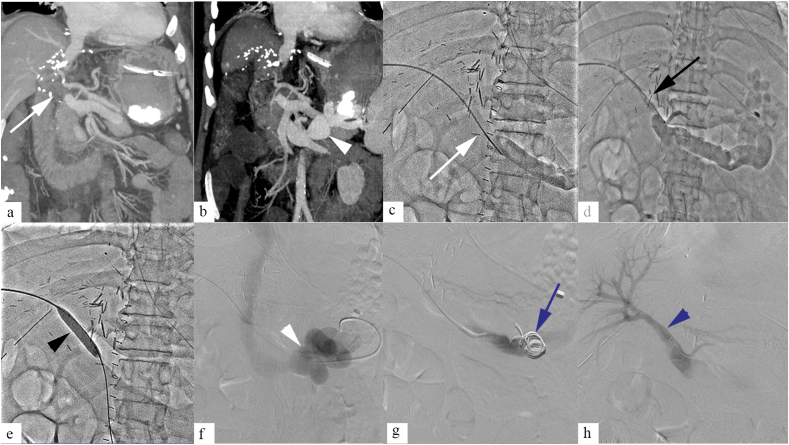
Figure 3.
A 33-month-old male child presenting with liver function abnormality, a year after liver transplantation. Contrast enhanced CT (a), and DSA (b, c) showed portal vein stenosis (PVS) (white arrow) at the site of anastomosis. Balloon angioplasty was done for PVS (d, e, black arrow). Postprocedure angiogram showed good flow across the anastomotic site (f, white arrowhead).
Figure 4.
A 46-year-old female patients presenting with variceal bleeding, 8 months following liver transplantation. Contrast enhanced CT abdomen (a), and venogram (b) showed portal vein stenosis at the site of anastomosis (white arrow). Primary stenting was done (c, black arrow), following which good flow was noted with in the portal vein across the anastomosis (d, back arrowhead).
Asymptomatic patients with normal LFT can be managed conservatively. Endovascular management is treatment of choice in symptomatic patients with PVS, with high success rate, and low complication risk.4,6 Transstenotic pressure gradient of >3–5 mmHg is considered significant.31,32 Angioplasty is often the first line of management (Figure 3). Both transjugular or transhepatic approach are commonly used. Size of the balloon depends on size of the normal portal vein segment. End point of angioplasty is when there is no significant residual stenosis and significant reduction of transstenotic gradient. A study by Saad et al. reported 82% 5 year patency rate in angioplasty group, and 100% in the stent group.33 While primary stenting is associated with high patency rate (Figure 4), stenting is often reserved for patients with incomplete response to angioplasty or restenosis, as stent within portal vein can hinder retransplantation if required, and progressive stenosis can be seen in pediatric patients with increase in age.4,6 Self-expandable stent of size same as or ∼10–20% greater than prestenotic segment is commonly used. In pediatric patients, short length balloon expandable stent of size >7–8 mm is often preferred because they can be accurately positioned.34 Though there is no consensus regarding periprocedural anticoagulation, systemic anticoagulation is generally recommended following angioplasty. INR is maintained between 2 and 3. In our practice, unfractionated heparin is initially used for anticoagulation with close monitoring of coagulation parameters. This is followed by low molecular weight heparin. Subsequently, depending upon the patency, portal flow, and. platelet count, the maintenance anticoagulation is prescribed. DUS is performed every 1–3 months posttransplant. CT angiography is done when abnormality is suspected on DUS. Surgical revision or retransplantation for PVS is rarely required.4,6
Portal Vein Steal Syndrome
Persistent portosystemic shunt causing impaired portal venous flow is referred as portal steal syndrome.35 Portal steal syndrome is a rare occurrence after LT, seen in ∼0.2% of liver transplant recipient.36 In patients with adequately sized well-functioning liver graft, more so in deceased donor liver graft, normalization of portal pressure usually causes spontaneous regression of portosystemic shunts. Persistent high intrahepatic resistance to portal blood flow in patients with small for size graft, hepatic congestion, volume overload, and acute rejection can lead to persistence or increase in portosystemic shunt following transplantation. In patient with liver donor LT with split liver graft and small hepatic vascular bed, decompression of portal pressure may be suboptimal. In addition, rapid regeneration in living donor LT may further increase intrahepatic resistance to portal blood flow, resulting in persistence of portosystemic shunt.35,36 Persistent large portosystemic shunt may further decrease antegrade flow in portal vein, causing portal vein thrombosis (Figure 5), graft dysfunction, or hepatic encephalopathy.37, 38, 39
Figure 5.
A 52-year-old male patient presenting with graft dysfunction, 20 days following liver transplantation. Contrast enhanced CT images showed portal vein thrombosis (a, white arrow), and large splenorenal shunt (b, white arrowhead) diverting the portal blood flow to the left renal vein and IVC. Portal venogram (c) showed thrombosed main portal vein (white arrow). Portal venogram after a bolus of catheter directed thrombolysis (d) showed recanalization of portal vein with small residual thrombus load (black arrow), and persistent large splenorenal shunt diverting the portal blood flow. Balloon maceration of thrombus was done (e, black arrowhead). In view of large shunt size, and persistent hepatofugal flow, decision to occlude the shunt was taken to reduce the risk of recurrent portal vein thrombosis. Selective catheterization of the splenorenal shunt was done, and venogram (f) showed opacification of tortuous collaterals draining into left renal vein through splenorenal shunt (white arrowhead). Coil embolization of the splenorenal shunt was done (g, blue arrow). Postembolization portal venogram (h) showed completely recanalized portal vein with antegrade hepatopetal flow (black arrow).
On DUS, main portal vein following transplantation shows hepatopetal flow, continuous waveform with phasicity, and mean PSV of >30 cm/s. In patients with portal steal syndrome, portal blood flow is reduced below 20 cm/s or shows flow reversal. CT is required to evaluate location, size, and extent of the portosystemic shunt and is useful in planning therapeutic intervention.35,36
There is no universally accepted consensus regarding management of portosystemic shunt, before, during, or after LT. Intraoperative ligation of portosystemic shunt during transplantation is preferred in large portosystemic shunt (>10 mm), and in small (<10 mm) shunts, if portal venous flow or pressure is reduced, or if it is associated with portal venous stenosis in preoperative CT.40, 41, 42, 43 Small portosystemic shunts may be left untreated due to innocuous appearance or inaccessible location. Some of these may eventually increase in size and cause hemodynamically significant alteration of portal blood flow and portal steal syndrome. In addition, iatrogenic portosystemic shunt, created in patients with small for size graft to reduce harmful effect of portal hyper perfusion on small graft,36 may eventually lead to portal steal syndrome. Endovascular management is preferred in patients with large portosystemic shunt presenting with portal vein steal syndrome in posttransplant period. Endovascular management include percutaneous embolization of shunt, balloon occluded retrograde obliteration of portosystemic shunt (BRTO), and its modifications (plug assisted technique (PARTO), and coil-assisted technique (CARTO), percutaneous transhepatic, or transjugular obliteration of shunt (Figure 5), and transvenous obliteration of portocaval shunt using covered stent. Embolizing agents used include coils, vascular plugs, glue, sclerosing agents, and geofoam, alone or in combination. Data on results after portosystemic shunt embolization in the setting of LT are limited. Surgical ligation is reserved for patients where endovascular approach is not feasible or has failed.36,37
Arterioportal Fistula (APF)
Hepatic arterioportal fistula is rare complication following LT, seen in 5.4% of patients13 and commonly occurs following liver biopsy or percutaneous cholangiogram.4,6
Most patients with small APF are asymptomatic and are incidentally detected on imaging. Patients with large APF may present with graft ischemia, graft dysfunction, and hemobilia.
DUS may be useful in detection of large symptomatic APF, which are characterized by reduced hepatic arterial resistivity index (<0.5), and arterialized and increased portal venous flow. DUS is not useful in small APF. Diagnostic hepatic artery angiogram can demonstrate sometimes small APF.
Small asymptomatic APF are usually left untreated, considering the risk of hepatic artery dissection or thrombosis associated with endovascular manipulation. These patients are to be carefully monitored so that prompt embolization can be performed before APF becomes hemodynamically significant or involve large caliber hepatic artery. Endovascular coil embolization is treatment of choice in patients with large or symptomatic APF.4,6
IVC and Hepatic Vein Complications
IVC and hepatic vein complications are uncommon and are seen in less than 2% of transplant patients.25,44
Early complications can be due to donor and recipient vein size mismatch, kinking, and technical difficulty or error during transplantation. Late complications are often due to intimal hyperplasia, or fibrosis, and can also be secondary to extrinsic compression by growing split liver graft, hematoma, collection, or abscess.1,4,6
Hepatic vein stenosis or thrombosis can have varied presentation. Some patients may be asymptomatic with normal liver function, while others present with Budd Chiari syndrome, impaired liver function, portal hypertension, and cirrhosis. Symptoms in IVC stenosis or thrombosis depend on level of obstruction. Patients with suprahepatic IVC obstruction often present similar to hepatic vein obstruction, and patients with IVC obstruction below the level of hepatic veins can present with lower limb edema, ascites, and engorged abdominal wall veins.4
On DUS, diagnosis of hepatic vein or IVC stenosis is made by reduced flow in hepatic veins and/or IVC, with loss of bi- or tri-phasic pattern, and turbulent flow at the site of stenosis. IVC or hepatic vein thrombosis is seen as intraluminal echogenic contents with absent flow. CECT can help confirm the diagnosis.4
Endovascular management is preferred treatment option in patients with hepatic vein or IVC complications. Transjugular or transfemoral approach is commonly used to access hepatic veins or IVC.6 In patients with piggy back anastomosis, transjugular approach allows easy access into hepatic veins, and in patients with caval interposition, either transjugular or transfemoral approach can be used.5 Venogram is obtained to confirm the diagnosis, and pressure gradient across the stenosis is measured. Gradient of >3 mmHg is considered pathological, and gradient of >10 mmHg is often considered to be hemodynamically significant.3,4 Balloon angioplasty (Figure 6) is associated with high technical success rate approaching 100%, and low complication rate.4 Metallic stenting is often reserved for patients with recurrent or residual stenosis. Considering that many patients often require repeated balloon angioplasty and high patency rate associated with metallic stenting, some authors suggest primary stenting (Figure 7) as the viable option.3, 4, 5 Surgical revision can be considered when endovascular treatment is unsuccessful, particularly in patients with early complications where stenosis can be due to kinking, or torsion, at the site of anastomosis.13 In patients with severe graft dysfunction, retransplantation can be considered.6
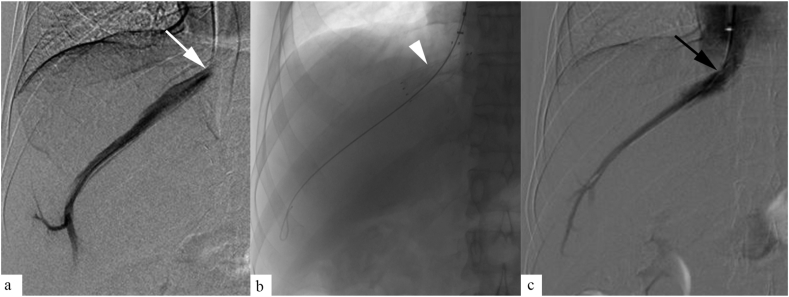
Figure 6.
A 40-year-old male patients presenting with refilling ascites at 18 months following liver transplantation. Venogram (a) showed tight stenosis at suprahepatic segment (white arrow) with trans-stenotic pressure gradient of 11 mmHg. Balloon angioplasty was done using 20 mm balloon catheter (b, black arrowhead). Postprocedure venogram (c) revealed improved flow through the IVC (black arrow), with reduction in trans-stenotic gradient to 3 mmHg.
Figure 7.
A 38-year-old male patient, presenting with refilling ascites, 1 year following liver transplantation. Venogram (a) revealed tight stenosis at the hepatic vein ostium (white arrow). Primary stenting was done across the stenosis (b, white arrowhead). Postprocedure venogram revealed good flow through the stent (c, black arrow).
Splenic Steal Syndrome (Nonocclusive Hepatic Artery Hypoperfusion; Portal Hyper Perfusion Syndrome)
Splenic steal can be seen in ∼4% of patients following LT and is an important cause of graft ischemia.4,17,45
Initially thought to be due to stealing of blood by hypertrophied splenic artery, secondary to prior portal hypertension and splenomegaly. However, recently it is believed to be secondary to increase portal venous blood flow, reducing hepatic arterial flow by compression of hepatic artery at sinusoids, and by triggering hepatic artery buffer mechanism (mediated by adenosine).4,13,34
Patients often present with graft dysfunction. Some of the patients may develop frank features of portal hypertension such as ascites and varices, often refractory to medical therapy. Prolonged arterial steal can lead biliary strictures and reperfusion injury.4
On DUS, splenic steal or portal hyperperfusion syndrome is associated with increased resistivity index (>0.8), with absent or reversed diastolic flow. Other cause of increased resistivity index such as graft edema, and graft rejection should be ruled out before diagnosis of splenic steal syndrome is considered. Increased flow can be seen in portal vein. On angiogram, there is reduced flow through otherwise patent hepatic artery, with increased splenic arterial flow. Findings are subjective, and diagnosis is considered in corroboration with clinical features, DUS, and after excluding other possible causes.4,13
Endovascular management is preferred in treatment of splenic steal syndrome. Proximal splenic artery embolization (Figure 8) with coils or vascular plug is performed which reduce portal blood flow by reducing splenic artery flow. Subsequently hepatic arterial flow increases, mediated by hepatic artery buffer mechanism. Proximal splenic artery embolization is relatively safe, with low risk of splenic infarction and abscess formation which are seen with distal embolization. Surgical procedures such as splenectomy, splenic artery ligation, or mesocaval shunt can be performed to reduce the portal blood flow.4,6,13
Figure 8.
A 37-year-old male patient, presenting with liver function abnormality on 17th postoperative day of liver transplantation. Celiac artery angiogram (a) showed non-visualization of hepatic artery (white arrow), and prominent gastroduodenal and splenic artery (white arrowheads). Selective hepatic artery angiogram (b) revealed small caliber hepatic artery with non-visualization of intrahepatic branches (black arrow). Coil embolization of GDA, and splenic artery was done (blue arrowhead). Postembolization angiogram (c) showed improved flow through hepatic artery with opacification of intrahepatic branches (black arrowhead). Postprocedure improvement in liver function test was noted.
Vascular Complications in Living Donor Liver Transplantation
Radiological interventions for vascular complications are more challenging in living donor LT or partial liver transplants. The surgical details of graft implantation, pretransplant recipient imaging, and donor vascular anatomy help in decision-making and tailoring the intervention in individual patients. Compared to whole liver grafts, in living donor LT, the arterial anastomosis is closer to the graft, usually right or left hepatic artery instead of CHA is used for anastomosis. The graft arteries have shorter length, narrow caliber, and there might be immediate branching after the anastomosis. Recipient arterial anatomy, need for re-do arterial anastomosis, any kink of the arteries, anatomical versus nonanatomical reconstruction, and preservation of gastroduodenal artery are some important aspects those may impact decision making.
Portal vein reconstruction techniques are different in living donor LT or partial grafts than whole liver grafts. Short stump of graft portal vein, shorter diameter, branching pattern of right or left portal vein, any venoplasty performed during implantation or presence of interposition graft, and so on, make it challenging for the intervention. Hepatic vein reconstruction is technically different in living donor LT as the recipient IVC is almost always preserved. Single versus dual outflow reconstruction, anterior sector venous outflow reconstruction (PTFE versus venous graft), size of the anastomosis may influence the intervention. The unique phenomenon in living donor LT is the regeneration of the liver graft, which may change the orientation or alignment of the venous anastomosis as the grafts grow in size. Particularly patients presenting with late venous complications and revisiting the immediate posttransplant imaging may be helpful to evaluate changes due to graft regeneration.46,47
Vascular Complications in Pediatric Liver Transplantation
In India, around 1500 to 2000 LT are done every year, with 10% of them being pediatric LT.48 Pediatric patients are treated with either cadaveric whole liver, reduced size liver, or split LT or living donor LT.49 Auxiliary LT is type of partial LT, where graft is placed without fully removing native liver. It is indicated in patients with acute liver failure and metabolic diseases without cirrhosis, as it allows immunosuppression free survival if native liver regenerates.48 However, auxiliary LT is more challenging with higher rate of complications. Partial graft transplantation is common in pediatric patients, which increases complexity of both donation and transplantation. Donor recipient mismatch can be associated with significant morbidity related to discrepancies in transplanted tissue volume.50 Small for size graft syndrome is characterized by small transplanted tissue volume, with relative high portal blood flow. These patients can present with portal hypertension, gastrointestinal bleed, ascites, and progressive cholangiopathy or cholestasis. Large for size graft syndrome is characterized by large transplanted tissue volume, with relatively poor portal blood flow. Large for size graft is associated with increased warm ischemic period, and ischemic reperfusion injury, which can result in graft dysfunction and massive hepatic necrosis.50 Incidence of vascular complications in pediatric population varies between 2 and 30% and is more common than in adult LT.49 Hepatic artery thrombosis or stenosis, a dreaded complication of LT, is more common in pediatric LT (5–18%) than in adult LT, possibly related to larger number of partial liver graft, underweight recipients (<2 years of age), and large for size graft syndrome.50,51 Left hepatic vein stenosis at its anastomosis with inferior vena cava is a typical complication of pediatric left lateral segment LT, which can lead to Budd Chiari syndrome, and graft dysfunction. With increasing use of triangulation technique for anastomosis, incidence of this complication has reduced. Portal vein thrombosis is seen in 5–10% of pediatric LT. It is more common in patients treated for biliary atresia because of common occurrence of hypoplastic portal vein in these patients, which may require replacement of entire portal vein up to splenoportal confluence to avoid thrombosis from reduced portal flow.51 Management of vascular complications in pediatric population is similar to adult patients, with special challenges related altered vascular anatomy in partial liver graft.
Table 2 summarizes treatment options in various vascular complications following LT. Figure 9 shows suggested algorithm for management of vascular complications following LT.
Table 2.
Management of Vascular Complications of Liver Transplantation.
| Vascular complications | Treatment options |
|---|---|
| Hepatic artery thrombosis (HAT) | Early (within 7 days) HAT – retransplantation/surgical revascularisation > endovascular management. Early (after 7 days), and Late symptomatic HAT – Endovascular management is preferred. |
| Hepatic artery stenosis (HAS) | Early HAS - surgical revascularisation > endovascular management. Late HAS - Endovascular management is preferred. |
| Hepatic artery pseudoaneurysm | Endovascular management is preferred |
| Hepatic artery rupture | Endovascular management/surgery |
| Portal vein thrombosis (PVT) | Early PVT (within 3 days) – surgical revision/retransplantation > endovascular management. Early PVT (after 3 days), and Late symptomatic PVT - endovascular management is preferred. |
| Portal vein stenosis (PVS) | Asymptomatic PVS – managed conservatively with or without systemic anticoagulation. Symptomatic or tight PVS - endovascular management is preferred. |
| Portal vein steal syndrome | Prevention - In patients with large portosystemic shunt, or small shunt with reduced portal blood flow/pressure or portal vein stenosis in preoperative CT – shunt ligation during surgery is preferred to prevent portal vein steal syndrome. Management – Endovascular or percutaneous obliteration of shunt is preferred. |
| Hepatic vein, and IVC obstruction | Endovascular management is preferred. |
| Splenic steal syndrome or portal hyper perfusion syndrome | Endovascular management is preferred. |
CT, computed tomography; HAS, Hepatic artery stenosis; HAT, Hepatic artery thrombosis; IVC, inferior vena cava; PVT, Portal vein thrombosis; PVS, Portal vein stenosis
Figure 9.
Algorithm for management of vascular complications following liver transplantation. Abbreviations: HAT, Hepatic artery thrombosis; HAS, Hepatic artery stenosis; HAP, Hepatic artery pseudoaneurysm; HAR, Hepatic artery rupture; PVT, Portal vein thrombosis; PVS, Portal vein stenosis; PSS, Portal steal syndrome; SSS, Splenic steal syndrome.
Transjugular Intrahepatic Portosystemic Shunt (TIPS) in Liver Transplant Patients
TIPS is commonly used to reduce portal pressure in patients with refractory ascites and variceal bleeding. Indications for TIPS remain same in transplant patients (Figure 10); however, main difference is the altered vascular anatomy. Portal hypertension can develop in transplant patients secondary to recurrence of underlying liver disease, organ size mismatch, vascular complications, chronic rejection, or other factors.5,13 Around 2% of transplant recipients develop portal hypertension and may require TIPS.52
Figure 10.
A 53-year-old male transplant recipient with chronic liver disease and refractory ascites. Contrast enhanced CT (a, b) showed ascites, splenomegaly, and partial thrombosis of main portal vein, and thrombosis of right and left portal vein (white arrow). Transjugular intrahepatic portosystemic shunt (TIPS) (c) was done in view of refractory ascites. Resolution of ascites was noted following TIPS.
Standard TIPS technique may be difficult in transplant patients due to altered vascular anatomy. Direct transhepatic hepatic venous access, direct portal vein access with “gun-sight” technique, or use of intravascular US may be required in difficult cases. Technical success is similar to nontransplant patients. One year TIPS patency rate in transplant patient is reported to be 80%. Clinical success of TIPS in transplant patients depends on model for end stage liver disease (MELD) score, where patients with score <15 do better compared to those with score >15. In general, clinical success is lower in transplant patient than in nontransplant patients; 50–80% of transplant patients with ascites, and 20% patients with variceal bleeding, show complete resolution, or significant symptomatic improvement following TIPS. Procedure-related mortality is reported around 2%. Major complications following TIPS include hepatic encephalopathy, and post-TIPS liver failure. If needed, TIPS reduction or occlusion can be considered in these patients.5,13
LT is the treatment of choice in majority of the patients with end stage liver disease. Vascular complication following LT is seen in around 7–13% of the patients and is associated with graft dysfunction and high morbidity and mortality. Early diagnosis and prompt treatment are crucial in management of these patients. In recent past, advances in interventional radiology has allowed safe and effective management of vascular complications following LT, with associated low complication risk compared to open surgery. Therefore, both diagnostic and interventional radiology forms an integral part of liver transplant management team.
Credit authorship contribution statement
All the authors have significantly contributed to literature review, data collection, manuscript writing, and proof reading.
Conflicts of interest
The authors have none to declare.
Acknowledgement
None.
Funding
No funding was received for the conduct of this study. No financial disclosure to be done.
References
- 1.Delgado-Moraleda J.J., Ballester-Vallés C., Marti-Bonmati L. Role of imaging in the evaluation of vascular complications after liver transplantation. Insights Imag. 2019 Dec;10:78. doi: 10.1186/s13244-019-0759-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horrow M.M., Huynh M.H.L., Callaghan M.M., Rodgers S.K. Complications after liver transplant related to preexisting conditions: diagnosis, treatment, and prevention. Radiographics. 2020 May;40:895–909. doi: 10.1148/rg.2019190120. [DOI] [PubMed] [Google Scholar]
- 3.Miraglia R., Maruzzelli L., Caruso S., et al. Interventional radiology procedures in adult patients who underwent liver transplantation. World J Gastroenterol. 2009;15:684. doi: 10.3748/wjg.15.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thornburg B., Katariya N., Riaz A., et al. Interventional radiology in the management of the liver transplant patient: thornburg et al. Liver Transpl. 2017 Oct;23:1328–1341. doi: 10.1002/lt.24828. [DOI] [PubMed] [Google Scholar]
- 5.Mehrzad H., Mangat K. The role of interventional radiology in treating complications following liver transplantation. ISRN Hepatol. 2013 Dec 3;2013:1–6. doi: 10.1155/2013/696794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta A., Narkhede A., Yadav A.K. In: Basics of Hepatobiliary Interventions [Internet] Mukund A., editor. Springer Singapore; Singapore: 2021. Vascular complications after hepatic transplantation: role of interventional radiology in management; pp. 217–233.http://link.springer.com/10.1007/978-981-15-6856-5_17 [cited 2022 Oct 6] Available from: [Google Scholar]
- 7.Dodd G.D., Memel D.S., Zajko A.B., Baron R.L., Santaguida L.A. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. Radiology. 1994 Sep;192:657–661. doi: 10.1148/radiology.192.3.8058930. [DOI] [PubMed] [Google Scholar]
- 8.Crossin J.D., Muradali D., Wilson S.R. US of liver transplants: normal and abnormal. Radiographics. 2003 Sep;23:1093–1114. doi: 10.1148/rg.235035031. [DOI] [PubMed] [Google Scholar]
- 9.Cheng Y.F. Interventional radiology in living donor liver transplant. World J Gastroenterol. 2014;20:6221. doi: 10.3748/wjg.v20.i20.6221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantrell J. The role of interventional radiology in complications after paediatric liver transplantation. S Afr Med J. 2014 Oct 24;104:825. doi: 10.7196/samj.8619. [DOI] [PubMed] [Google Scholar]
- 11.Saad W.E.A., Davies M.G., Saad N.E.A., et al. Catheter thrombolysis of thrombosed hepatic arteries in liver transplant recipients: predictors of success and role of thrombolysis. Vasc Endovasc Surg. 2007 Feb;41:19–26. doi: 10.1177/1538574406296210. [DOI] [PubMed] [Google Scholar]
- 12.Figueras J., Busquets J., Dominguez J., et al. Intra-arterial thrombolysis in the treatment of acute hepatic artery thrombosis after liver transplantation. Transplantation. 1995 May 15;59:1356–1357. [PubMed] [Google Scholar]
- 13.Naidu S.G., Alzubaidi S.J., Patel I.J., et al. Interventional radiology management of adult liver transplant complications. Radiographics. 2022 Oct;42:1705–1723. doi: 10.1148/rg.220011. [DOI] [PubMed] [Google Scholar]
- 14.Singhal A., Stokes K., Sebastian A., Wright H.I., Kohli V. Endovascular treatment of hepatic artery thrombosis following liver transplantation. Transplant International. 2010 Mar;23:245–256. doi: 10.1111/j.1432-2277.2009.01037.x. [DOI] [PubMed] [Google Scholar]
- 15.Abdelaziz O., Hosny K., Amin A., Emadeldin S., Uemoto S., Mostafa M. Endovascular management of early hepatic artery thrombosis after living donor liver transplantation: endovascular management of early hepatic artery thrombosis after LDLT. Transpl Int. 2012 Aug;25:847–856. doi: 10.1111/j.1432-2277.2012.01509.x. [DOI] [PubMed] [Google Scholar]
- 16.Škegro D. Percutaneous endovascular treatment for hepatic artery stenosis after liver transplantation: the role of percutaneous endovascular treatment. Pol J Radiol. 2015;80:309–316. doi: 10.12659/PJR.893831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimura Y., Tapia Sosa R., Soto-Trujillo D., Kimura Sandoval Y., Casian C. Liver transplant complications radiologist can’t miss. Cureus. 2020 Jun 5;12(6) doi: 10.7759/cureus.8465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rostambeigi N., Hunter D., Duval S., Chinnakotla S., Golzarian J. Stent placement versus angioplasty for hepatic artery stenosis after liver transplant: a meta-analysis of case series. Eur Radiol. 2013 May;23:1323–1334. doi: 10.1007/s00330-012-2730-9. [DOI] [PubMed] [Google Scholar]
- 19.Magand N., Coronado J.L., Drevon H., et al. Primary angioplasty or stenting for hepatic artery stenosis treatment after liver transplantation. Clin Transplant. 2019 Dec;33 doi: 10.1111/ctr.13729. [DOI] [PubMed] [Google Scholar]
- 20.Boyvat F., Aytekin C., Harman A., Sevmis S., Karakayali H., Haberal M. Endovascular stent placement in patients with hepatic artery stenoses or thromboses after liver transplant. Transplant Proc. 2008 Jan;40:22–26. doi: 10.1016/j.transproceed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 21.Sommacale D. Preservation of the arterial vascularisation after hepatic artery pseudoaneurysm following orthotopic liver transplantation: long-term results. Ann Transplant. 2014;19:346–352. doi: 10.12659/AOT.890473. [DOI] [PubMed] [Google Scholar]
- 22.Quiroga S., Sebastià M.C., Margarit C., Castells L., Boyé R., Alvarez-Castells A. Complications of orthotopic liver transplantation: spectrum of findings with helical CT. Radiographics. 2001 Sep;21:1085–1102. doi: 10.1148/radiographics.21.5.g01se061085. [DOI] [PubMed] [Google Scholar]
- 23.Boleslawski E., Bouras A.F., Truant S., et al. Hepatic artery ligation for arterial rupture following liver transplantation: a reasonable option: arterial raupture after liver transplantation. Am J Transplant. 2013 Apr;13:1055–1062. doi: 10.1111/ajt.12135. [DOI] [PubMed] [Google Scholar]
- 24.Pérez-Saborido B., Pacheco-Sánchez D., Barrera-Rebollo A., et al. Incidence, management, and results of vascular complications after liver transplantation. Transplant Proc. 2011 Apr;43:749–750. doi: 10.1016/j.transproceed.2011.01.104. [DOI] [PubMed] [Google Scholar]
- 25.Buell J.F., Funaki B., Cronin D.C., et al. Long-term venous complications after full-size and segmental pediatric liver transplantation. Ann Surg. 2002 Nov;236:658–666. doi: 10.1097/00000658-200211000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sánchez-Bueno F., Hernández Q., Ramírez P., et al. Vascular complications in a series of 300 orthotopic liver transplants. Transplant Proc. 1999 Sep;31:2409–2410. doi: 10.1016/s0041-1345(99)00406-6. [DOI] [PubMed] [Google Scholar]
- 27.Cavallari A., Vivarelli M., Bellusci R., Jovine E., Mazziotti A., Rossi C. Treatment of vascular complications following liver transplantation: multidisciplinary approach. Hepato-Gastroenterology. 2001 Feb;48:179–183. [PubMed] [Google Scholar]
- 28.Khalaf H. Vascular complications after deceased and living donor liver transplantation: a single-center experience. Transplant Proc. 2010 Apr;42:865–870. doi: 10.1016/j.transproceed.2010.02.037. [DOI] [PubMed] [Google Scholar]
- 29.Schneider N., Scanga A., Stokes L., Perri R. Portal vein stenosis: a rare yet clinically important cause of delayed-onset ascites after adult deceased donor liver transplantation: two case reports. Transplant Proc. 2011 Dec;43:3829–3834. doi: 10.1016/j.transproceed.2011.09.068. [DOI] [PubMed] [Google Scholar]
- 30.Wei B.J., Zhai R.Y., Wang J.F., Dai D.K., Yu P. Percutaneous portal venoplasty and stenting for anastomotic stenosis after liver transplantation. World J Gastroenterol. 2009 Apr 21;15:1880–1885. doi: 10.3748/wjg.15.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Funaki B., Rosenblum J.D., Leef J.A., et al. Percutaneous treatment of portal venous stenosis in children and adolescents with segmental hepatic transplants: long-term results. Radiology. 2000 Apr;215:147–151. doi: 10.1148/radiology.215.1.r00ap38147. [DOI] [PubMed] [Google Scholar]
- 32.Shibata T., Itoh K., Kubo T., et al. Percutaneous transhepatic balloon dilation of portal venous stenosis in patients with living donor liver transplantation. Radiology. 2005 Jun;235:1078–1083. doi: 10.1148/radiol.2353040489. [DOI] [PubMed] [Google Scholar]
- 33.Saad W. Portal interventions in liver transplant recipients. Semin Intervent Radiol. 2012 Jun;29:99–104. doi: 10.1055/s-0032-1312570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ko G.Y., Sung K.B., Gwon D.I. The application of interventional radiology in living-donor liver transplantation. Korean J Radiol. 2021;22:1110. doi: 10.3348/kjr.2020.0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim B., Kim K.W., Song G.W., Lee S.G. Portal flow steal after liver transplantation. Clin Mol Hepatol. 2015;21:314. doi: 10.3350/cmh.2015.21.3.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jajodia S., Khandelwal A.H., Khandelwal R., Kapoor A.K., Baijal S.S. Endovascular management of portal steal syndrome due to portosystemic shunts after living donor liver transplantation. JGH Open. 2021 May;5:599–606. doi: 10.1002/jgh3.12540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centonze L., Di Sandro S., Cereda M., et al. Endovascular treatment of acute posttransplant portal vein thrombosis due to portal steal from mesocaval and coronary portosystemic shunts. Exp Clin Transplant. 2020 Oct;18:653–656. doi: 10.6002/ect.2019.0273. [DOI] [PubMed] [Google Scholar]
- 38.Lee M., Kim S.K., Chung Y.E., et al. Portal venous perfusion steal causing graft dysfunction after orthotopic liver transplantation: serial imaging findings in a successfully treated patient. Ultrasonography. 2016 Jan 1;35:78–82. doi: 10.14366/usg.15012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barritt A.S., Fried M.W., Hayashi P.H. Persistent portosystemic shunts after liver transplantation causing episodic hepatic encephalopathy. Dig Dis Sci. 2010 Jun;55:1794–1798. doi: 10.1007/s10620-009-0901-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elshobary M., Shehta A., Salah T., et al. Ligation of huge spontaneous porto-systemic collaterals to avoid portal inflow steal in adult living donor liver transplantation: a case-report. Int J Surg Case Rep. 2017;31:214–217. doi: 10.1016/j.ijscr.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ikegami T., Shirabe K., Nakagawara H., et al. Obstructing spontaneous major shunt vessels is mandatory to keep adequate portal inflow in living-donor liver transplantation. Transplantation. 2013 May 27;95:1270–1277. doi: 10.1097/TP.0b013e318288cadc. [DOI] [PubMed] [Google Scholar]
- 42.Reddy M.S., Rela M. Portosystemic collaterals in living donor liver transplantation: what is all the fuss about? Liver Transpl. 2017 Apr;23:537–544. doi: 10.1002/lt.24719. [DOI] [PubMed] [Google Scholar]
- 43.Moon D.B., Lee S.G., Kim K.H., et al. The significance of complete interruption of large spontaneous portosystemic collaterals in adult living donor liver transplantation as a graft salvage procedure. Transpl Int. 2008 Jul;21:698–700. doi: 10.1111/j.1432-2277.2008.00639.x. [DOI] [PubMed] [Google Scholar]
- 44.Ko G.Y., Sung K.B., Yoon H.K., Lee S. Early posttransplantation portal vein stenosis following living donor liver transplantation: percutaneous transhepatic primary stent placement. Liver Transpl. 2007 Apr;13:530–536. doi: 10.1002/lt.21068. [DOI] [PubMed] [Google Scholar]
- 45.Saad W.E.A. Nonocclusive hepatic artery hypoperfusion syndrome (splenic steal syndrome) in liver transplant recipients. Semin Intervent Radiol. 2012 Jun;29:140–146. doi: 10.1055/s-0032-1312576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Samstein B., Smith A.R., Freise C.E., et al. Complications and their resolution in recipients of deceased and living donor liver transplants: findings from the A2ALL cohort study: complications in LDLT and DDLT. Am J Transplant. 2016 Feb;16:594–602. doi: 10.1111/ajt.13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barbetta A., Butler C., Barhouma S., et al. Living donor versus deceased donor pediatric liver transplantation: a systematic review and meta-analysis. Transplant Direct. 2021 Sep 20;7:e767. doi: 10.1097/TXD.0000000000001219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malhotra S., Sibal A., Goyal N. Pediatric liver transplantation in India: 22 Years and counting. Indian Pediatr. 2020 Dec 15;57:1110–1113. [PubMed] [Google Scholar]
- 49.Emre S., Gondolesi G.E., Muñoz-Abraham A.S., Emre G., Rodriguez-Davalos M.I. Pediatric liver transplantation: a surgical perspective and new concepts. Curr Transplant Rep. 2014 Dec;1:224–231. [Google Scholar]
- 50.Ibáñez Pradas V., Cortés Cerisuelo M., Montalvá Orón E. Pediatric liver transplantation. Cir Pediatr. 2022 Jan 10;35:1–9. doi: 10.54847/cp.2022.01.11. [DOI] [PubMed] [Google Scholar]
- 51.Spada M., Riva S., Maggiore G., Cintorino D., Gridelli B. Pediatric liver transplantation. World J Gastroenterol. 2009 Feb 14;15:648–674. doi: 10.3748/wjg.15.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saad W.E.A., Darwish W.M., Davies M.G., et al. Transjugular intrahepatic portosystemic shunts in liver transplant recipients: technical analysis and clinical outcome. Am J Roentgenol. 2013 Jan;200:210–218. doi: 10.2214/AJR.11.7653. [DOI] [PubMed] [Google Scholar]