Abstract
Objective
Due to the implementation of vaccinations and the development of therapeutic agents, the coronavirus disease 2019 (COVID-19) pandemic that started at the end of 2019 has entered a new phase. As a result, neurosurgeons should reconsider the way they treat their patients. As the COVID-19 situation prolongs, the change in neurosurgical emergency patients according to the number of confirmed cases is no longer clear. Outpatient treatment by telephone was permitted according to government policy. In addition, visits to caregivers in the intensive care unit were limited.
Methods
The electronic medical records of patients who had been treated over the phone for a month (during April 2020, while the hospital was closing) were reviewed. Meanwhile, according to the limited visits to the intensive care unit, a video meeting was held with the caregivers. After the video meeting, satisfaction was evaluated using a questionnaire.
Results
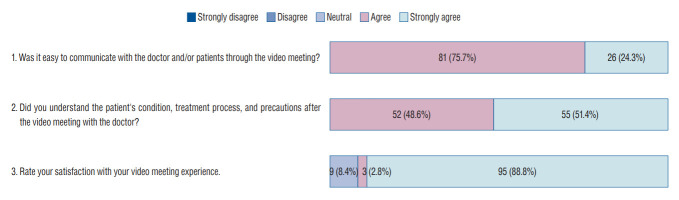
During April 2020, 1021 patients received non-face-to-face care over the telephone. Among the patients, no critical medical problem occurred due to non-face-to-face care. From July 2021 to December 2021, 321 patients were admitted to the neurosurgical intensive care unit and 107 patients (33.3%) including their caregivers agreed to video visits. Twice a week, advance notice was given that access would be made through a mobile device and the nurse explained to caregivers how to use the mobile device. The time for the video meeting was approximately 20 minutes per patient. Based on the questionnaire, 81 respondents (75.7%) answered that they agreed, and 26 respondents (24.3%) answered that they strongly agreed that was easy to communicate through video meetings. Fifty-two (48.6%) agreed and 55 (51.4%) strongly agreed that they were easy to understand the doctor’s explanation. For overall satisfaction with this video meeting, three respondents (2.8%) gave 4/5 points and 95 respondents (88.8%) gave 5/5 points, and nine (8.4%) gave 3/5 points. Their reason was that there was not enough time.
Conclusion
In situations where patient visits are limited, video meetings through a mobile device can provide sufficient satisfaction to caregivers. Telemedicine will likely become common in the near future. Health care professionals should prepare and respond to these needs and changes. Therefore, establishing a system with institutional support is necessary.
Keywords: Neurosurgery, COVID-19, Telemedicine, Outpatients, Intensive care units
INTRODUCTION
Due to the implementation of vaccinations and the development of therapeutic agents, the coronavirus disease 2019 (COVID-19) pandemic that started at the end of 2019 has entered a new phase. However, new variants are continuously emerging; thus, this virus will likely remain a public concern.
In a previous study, the authors confirmed the number of neurosurgical emergency patients decreased due to COVID-19 [12]. In the present study, what type of changes occurred during the ongoing pandemic and how to proceed in the future were investigated.
Due to the increased number of COVID-19 patients in hospitals, remote treatment was subsequently implemented using the phone. Based on the data to date, the effectiveness and risk of non-face-to-face care were examined in the present study. In addition, according to government policy, visits to the intensive care unit (ICU) became difficult, patients and their caregivers could not see each other, and the process for obtaining information from medical staff became longer. Therefore, in the present study, video patient meetings were conducted using a mobile device (tablet). The satisfaction of patients and caregivers using this approach was evaluated and their experiences were shared.
This study was divided into three main sessions. The first is the changing trend of neurosurgical emergency patients in the COVID-19 situation, which was conducted as a follow-up study of the previous study. Second, we summarized the results of non-face-to-face management in the neurosurgical outpatient department, during the COVID-19 situation. Third, a video patient meeting was held for patients in the neurosurgical ICU in a situation where it was not possible to visit the hospital due to the worsening of COVID-19.
MATERIALS AND METHODS
COVID-19 outbreak and changes in neurosurgical emergency patients
The Institutional Review Board (IRB) waived the informed consents for this retrospective study. As a follow-up to the previous study [12], changes of trends in neurosurgical emergency patients were analyzed as the COVID-19 pandemic continued. The overall trend was analyzed from January 2021 to December 2021. Similar to the previous study, confirmed COVID-19 patients in the northern Gyeonggi Province (Uijeongbu, Guri, Pocheon, Namyangju, Dongducheon, Yangju, and Yeoncheon) were identified using data released by the government. In addition, the proportion of the population who received a second dose of COVID-19 vaccination in the region was determined based on the number reported daily on the website (www.gg.go.kr/).
During this period, patients who visited the emergency department with head trauma or stroke were identified. Data of all patients initially diagnosed with codes S00–S09 (injuries to the head) or I60–I68 (cerebrovascular diseases, excluding sequelae of cerebrovascular disease) based on the International Classification of Disease-10 were extracted from electronic medical records. In the head trauma cases, a Glasgow coma scale (GCS) score ≤9 and neurotrauma-related surgery (regardless of GCS score) were defined as major trauma cases. In stroke cases, a National Institutes of Health Stroke Scale score ≥10 and requirement for endovascular intervention and surgical treatment were considered major stroke cases. In the trauma and stroke cases, patients that did not survive after treatment as well as those who needed but refused surgical treatment were also included as major cases. In addition, patients who died during hospitalization were identified and defined as mortality cases.
Trauma patients were classified into patients involved and not involved in traffic accidents which included cars, motorcycles, and personal mobility vehicles as well as drivers, passengers, and pedestrians. Stroke patients were classified into ischemic stroke and hemorrhagic stroke groups based on the disease code.
Non-face-to-face outpatient care services for neurosurgical patients Formal consent was not required for this study and the IRB waived the need for informed consent. The authors’ institute was temporarily closed due to COVID-19. In the meantime, faculty conducted non-face-to-face care services over the phone for follow-up patients. Unlike other previous studies, forced non-face-to-face consultation was performed due to a hospital closure, thus, selection bias was excluded. All patients who received non-face-to-face care service were enrolled in the study. Before treatment, the nurse explained the method and limitations of non-face-to-face treatment to the patient or guardian and any measures to be taken if unexpected situations occur later. After in-hospital treatment resumed, face-to-face consultation was performed, and the medical records were reviewed. The types of prescriptions and side effects (e.g., delayed treatment, or detection of deterioration) due to non-face-to-face treatment were recorded.
A video patient meeting in the neurosurgical ICU
The IRB reviewed and approved the study protocol. Written informed consent was obtained from all study participants (patients and/or caregivers). The participants and any identifiable individuals consented to the publication of his/her image.
Due to COVID-19, visits to patients in the ICU were restricted according to government policy. Consequently, patients and their caregivers could not visit in person for an extended period; therefore, measures were taken to ensure patients and their caregivers could meet using a mobile device (tablet).
When first admitted to the ICU, patients and their caregivers were asked whether or not they wanted to participate in this video meeting in advance and informed consent was obtained. Patients who consented to a video meeting were prospectively enrolled in this study. Twice a week at 1 PM, advance notice was given that access would be made through a mobile device and the nurse in charge explained to caregivers outside the hospital how to use the mobile device. On the other days of the week, the patient’s condition was updated daily via text message. At the appointed time for the video meeting, the doctor in charge of the ICU explained the patient’s current condition and treatment status as well as presented any computed tomography (CT) or magnetic resonance imaging (MRI) images to the guardian via the mobile device (Fig. 1). If the patient was conscious, he/she would be able to chat with their family using the screen of the mobile device. The time allowed for the video meeting was approximately 20 minutes per patient. After the video meeting, satisfaction was evaluated using a questionnaire administered by a research team independent of this study. The available responses were reported on a Likert scale ranging from “strongly disagree” to “strongly agree.”
Fig. 1.
Demonstration of a video patient meeting in the neurosurgical intensive care unit (ICU) A : Patient and caregiver talking to each other through the screen. B : Explaining the patient’s condition to the caregiver.
RESULTS
COVID-19 outbreak and changes in neurosurgical emergency patients
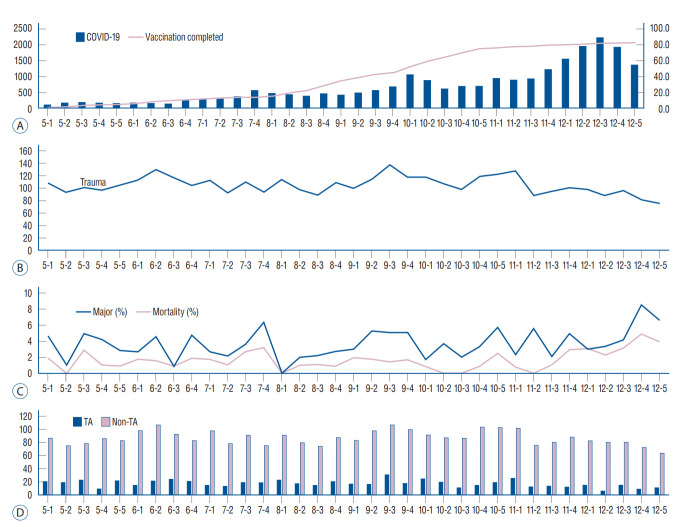
The number of COVID-19 confirmed cases remained below 500 per week in the northern Gyeonggi Province, but after a surge in October, it gradually increased, exploding to 2000 per week due to the occurrence of the Omicron variant in December. Vaccination completed cases gradually increased with the 2nd vaccination that started in May, but the increase in vaccination did not have effective enough to reduce the number of confirmed cases. A median of 104 trauma patients visited the emergency room per week. The median of major trauma cases was 3.4% and the median mortality rate was 1.6%. Among the patients, the number of traffic accident-related cases was 615, accounting for 16.8% of all trauma patients. In a previous study, the number of trauma patients reportedly decreased as the number of COVID-19 cases increased; however, that pattern was not observed in the present study. Although the number of confirmed cases surged due to the spread of the Omicron variant at the end of 2021, the number of trauma patients did not significantly decrease. At the end of 2021, as the social distancing policy was lifted, an increase in major trauma cases was observed. A higher mortality rate has been observed with the increased number of confirmed cases. It could not be confirmed that this result was due to a lack of medical resources, after medical resources were focused on management of COVID-19 patients. (Fig. 2 and Table 1).
Fig. 2.
Association between coronavirus disease 2019 (COVID-19) outbreak and head trauma patients in 2021. A : Weekly number of COVID-19 patients (blue bar) and proportion of the population who received a second dose of COVID-19 vaccination (red line) in northern Gyeonggi Province. B : Weekly number of head trauma patients in 2021. C : Proportion of major trauma and mortality cases in head trauma patients. D : Comparison of head trauma incidence in patients involved in traffic-related accidents (blue bar) and non-traffic-related accidents (red bar). TA : traffic accidents.
Table 1.
Demographics of trauma injury patients and stroke patients during the COVID-19 pandemic (January 2021 to December 2021)
| Trauma case | Stroke case | |
|---|---|---|
| Total number of patients | 3670 | 928 |
| Age (years) | 28 (1–99) | 73 (26–98) |
| Sex, male | 2429 (66.2) | 511 (55.1) |
| Major cases | 133 (3.4) | 123 (11.1) |
| Mortality cases | 59 (1.6) | 54 (4.3) |
| Traffic accident cases | 615 (16.8) | |
| Non-traffic accident cases | 3055 (83.2) | |
| Ischemic stroke cases | 745 (80.2) | |
| Hemorrhagic stroke cases | 183 (19.8) |
Values are presented as median (range) or number (%). COVID-19 : coronavirus disease 2019
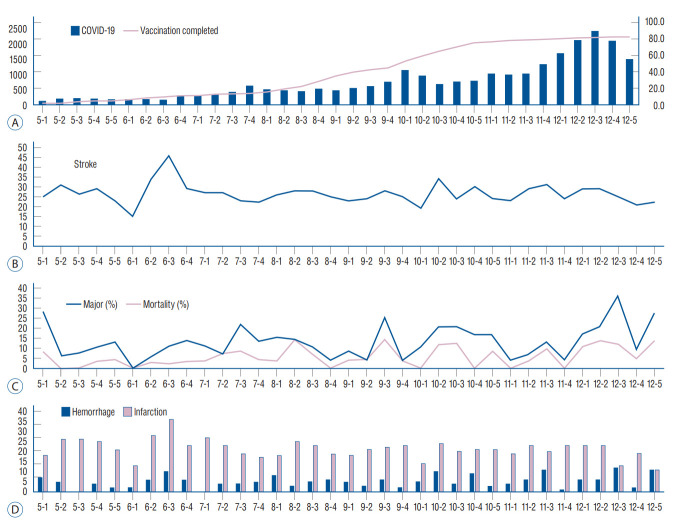
A median of 73 stroke patients visited the emergency room per week. The median of major stroke cases was 11.1% and the median mortality rate was 4.3%. The number of hemorrhagic stroke cases was 183, accounting for 19.8% of all stroke patients. Similar to the trauma cases mentioned above, a significant pattern associated with an increased number of COVID-19 cases was not observed. In addition, the proportion of major stroke cases and mortality cases increased with the surge of the Omicron variant at the end of the year (Fig. 3 and Table 1).
Fig. 3.
Association between coronavirus disease 2019 (COVID-19) outbreak and stroke patients in 2021. A : Weekly number of COVID-19 patients (blue bar) and proportion of the population who received a second dose of COVID-19 vaccination (red line) in northern Gyeonggi Province. B : Weekly number of stroke patients in 2021. C : Proportion of major stroke and mortality cases in stroke patients. D : Comparison of hemorrhagic stroke (blue bar) and ischemic stroke (red bar) in stroke patients.
Non-face-to-face outpatient care services for neurosurgical patients
During April 2020, 1021 patients received non-face-to-face care service over the telephone. Five hundred ninety-nine patients were male, and 422 patients were female. The median age was 52 years old (range, 13 to 97). Seven hundred nine patients were interviewed by the patients themselves, but the other 312 patients were interviewed by their caregivers. The causes were cognitive impairment, consciousness disorder, and being a minor. Five hundred seventy-four were vascular patients (ischemic or hemorrhagic), 70 were trauma patients, 51 patients were brain tumor patients, 245 patients had spine disorders, 59 patients had functional diseases, and 22 patients had miscellaneous problems. Because the patients could not meet in person, information was provided only through conversations over the phone with patients or caregivers and the patient’s condition was determined. If there were no specific problems, the previously prescribed medication was repeated.
After reviewing the medical records, critical medical problems did not occur during non-face-to-face consultations, such as delayed treatment, or detection of deterioration. However, due to the hospital closure, CT, MR), and digital subtraction angiography tests were delayed for eight patients. In spite of this, critical problems, such as tumor progression or recurrence, did not occur as a result of the delay in the examination. In addition, coil embolization for unruptured aneurysms was planned but delayed for six patients; however, additional problems such as hemorrhage due to early rupture did not occur due to the delay. Due to the hospital closure caused, we had no choice but to provide non-face-to-face treatment, even though accordingly delays in certain procedures, the patients did not experience any additional problems. Elderly patients (over 60 years old) were compared with the other patients, but there were very few cases where problems occurred, so statistically significant results were not shown.
A video patient meeting in the neurosurgical ICU
From July 2021 to December 2021, 321 patients were admitted to the neurosurgical ICU and 107 patients (33.3%) including their caregivers agreed to video visits. Twenty-one patients (6.5%) who refused video meetings and requested only text messages were excluded from this study. Other patients did not consent to the study or had no related guardians who can obtain consent. During the video meeting, the doctor explained the patient’s current condition, and future treatment directions, and recently performed images such as CT and MRI to the guardian. Afterward, showing the patient’s current state (whether conscious or not), it provided emotional stability to the caregiver, and in the case of a conscious patient, an opportunity to have a private conversation with the caregiver for the rest of the meeting time. A questionnaire was conducted with the caregivers of enrolled patients. Based on the questionnaire, 1. Was it easy to communicate with the doctor and/or patient through the video meeting? To this question, 81 respondents (75.7%) answered that they agreed, and 26 respondents (24.3%) answered that they strongly agreed. This might have been due to the nurse explaining enough before the meeting. 2. Did you understand the patient’s condition, treatment process, and precautions after the video meeting with the doctor? To the question, 52 (48.6%) agreed and 55 (51.4%) strongly agreed. For overall satisfaction with this video meeting, three respondents (2.8%) gave 4/5 points and 95 respondents (88.8%) gave 5/5 points, but nine (8.4%) gave 3/5 points. Their reason was that there was not enough time (Fig. 4).
Fig. 4.
The questionnaire and its results.
DISCUSSION
In a previous study [12], the number of neurosurgery emergency patients significantly decreased due to the COVID-19 pandemic. As a consequence of social distancing, the number of trauma patients declined, particularly the number of non-traffic accident patients. Because the COVID-19 pandemic has been prolonged, the government policy assures a way to maintain daily life by switching to “Living with COVID-19” instead of continuing social distancing. Previously, physicians and patients were limited in using telemedicine due to several reasons such as the lack of need, limited reimbursements, and concerns regarding reliability. However, the situation has currently changed and the use of telemedicine has become a necessity [10].
Telemedicine has been defined as the use of medical information that is exchanged from one site to another through electronic communication to improve a patient’s health [19]. This is a concept that includes a simple phone call or video call using a tablet, as in the present study. The efficacy of telemedicine has been investigated in several previous studies. In medical conditions such as hypertension, diabetes, and inflammatory bowel disease, the utility of telemedicine has been investigated in numerous studies [3,6,17]. Telemedicine was reportedly safer and reduced outpatient visits and hospitalizations compared with standard care. In addition, various mobile telemedicine devices have been developed in the medical field that can replace or support the doctor’s in-person physical examination [1,2,16,20]. Furthermore, several tele-rehabilitation devices are currently being developed for stroke patients [4,18]. However, because neurological deficit may cause various symptoms, more research is needed to apply telemedicine devices in the field of neurosurgery. Although difficult, these attempts are still being made in the field of neurosurgery [7,13,14].
Telemedicine has the advantage of 1) removing geographic and socioeconomic barriers to patient care and saves time and cost from coming to the hospital. In addition, if telemedicine becomes common, access to medical care will become more convenient and patients in remote areas can see a doctor more easily. Similarly, people with financial difficulties can receive treatment. Telemedicine is also considered effective for minor issues (e.g., simple headache, low back pain) or chronic disease management for which the same medication is always prescribed. In addition, telemedicine can prevent exposure to other infectious conditions such as COVID-19 when traveling to a hospital. Providing a video meeting for ICU patients can useful in cases where physically seeing the patient is difficult, even if not a COVID-19 case. For a conscious patient, maintaining a relationship with a caregiver provides the patient emotional stability and can be a motivation to recover. Even in the case of an unconscious patient, telemedicine can help maintain a good doctor-patient relationship by letting the caregiver know the patient is continuously being cared for and treated.
However, telemedicine has several disadvantages. Most importantly, 1) the potential for leakage of personal information. If a security system is not in existence, personal information could be hacked and misused. Furthermore, 2) sufficient evidence has not yet been established. In addition, performing a physical examination directly is not possible and 3) the risk of misdiagnosis remains because of the limitations on testing.
Obstacles need to be overcome to establish telemedicine as common practice. Based on the medical evidence mentioned above, 1) appropriate indications should be defined. 2) Selecting a suitable platform is also required. A system should be built to ensure some basic and fundamental information can be provided through a standardized platform. In addition, through 3) amendment of the insurance system, unnecessary expenses should be reduced and institutional support provided for proper profit creation. Furthermore, all these considerations and implementations should be accepted through 4) social consensus (Table 2).
Table 2.
Considerations for telemedicine
| Advantages | Saves time and cost for transport |
| Improved access to medical care | |
| Convenience of minor issues or chronic disease management | |
| Obstacles | Personal information leakage |
| Lack of evidence | |
| Potential for misdiagnosis | |
| Requirements | Define appropriate indications |
| Selecting the suitable platform | |
| Amendment of insurance system | |
| Social consensus |
Social distancing cannot be maintained forever and restrictions cannot be lifted. Video patient meetings using a mobile device were introduced in response to the COVID-19 pandemic. Although generalization is difficult due to the limited amount of data, the results of the study provide an opportunity to understand the potential benefits of telemedicine.
Although whether the COVID-19 pandemic will end is unknown, the possibility exists that face-to-face visits may not proceed due to factors such as the environment, medical staff, and caregivers. Therefore, efforts such as insurance support are needed to resolve these problems. During video patient meetings, several problems were encountered. First, the tablet had to be prepared and then the appropriate platform selected. The doctor, guardian, and patient all needed to keep appointments and start on time. Another issue was the sound of the ICU monitoring devices from other patient beds nearby. The use of the video for many patients was complicated due to these difficulties. Despite these efforts, however, the hospital cannot obtain economic benefits from these efforts because the appropriate insurance support has not yet been determined. The government temporarily permitted non-face-toface treatment for this COVID-19 situation, and provided a guideline accordingly, but this is only a temporary measure. Recently, some research groups have attempted to present guidelines for telemedicine [8,9,11]. However, no detailed guideline or tool for quantitative analysis of telemedicine has yet been presented. In these guidelines, the importance of objective evaluation was pointed out. In the field of pediatrics, four measurement domains 1) health outcomes; 2) health delivery (quality and cost); 3) experience, and 4) program implementation and key performance indicators, were suggested to evaluate the telemedicine [5,15]. It is necessary to establish a guideline for appropriate telemedicine for neurosurgery patients by benchmarking the previously published guidelines.
CONCLUSION
The COVID-19 pandemic is expected to continue for some time; however, physicians cannot stop treating patients. Attention needs to be given to patients and their caregivers through non-face-to-face care services and patient experiences managed. Furthermore, telemedicine will likely become common in the near future. Health care professionals should prepare and respond to these needs and changes. Therefore, establishing a system with institutional support is necessary.
Footnotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : MHL, TKL; Data curation : SRJ; Formal analysis : MHL; Methodology : TKL; Visualization : MHL, SRJ; Writing - original draft : MHL, SRJ; Writing - review & editing : MHL, SRJ, TKL
Data sharing
None
Preprint
None
References
- 1.Alessa T, Hawley MS, Hock ES, de Witte L. Smartphone apps to support self-management of hypertension: review and content analysis. JMIR Mhealth Uhealth. 2019;7:e13645. doi: 10.2196/13645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashrafzadeh S, Hamdy O. Patient-driven diabetes care of the future in the technology era. Cell Metab. 2019;29:564–575. doi: 10.1016/j.cmet.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019–2082. doi: 10.1016/S0140-6736(20)32374-6. [DOI] [PubMed] [Google Scholar]
- 4.Chen J, Sun D, Zhang S, Shi Y, Qiao F, Zhou Y, et al. Effects of home-based telerehabilitation in patients with stroke: a randomized controlled trial. Neurology. 2020;95:e2318–e2330. doi: 10.1212/WNL.0000000000010821. [DOI] [PubMed] [Google Scholar]
- 5.Chuo J, Macy ML, Lorch SA. Strategies for evaluating telehealth. Pediatrics. 2020;146:e20201781. doi: 10.1542/peds.2020-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, Cilissen M, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390:959–968. doi: 10.1016/S0140-6736(17)31327-2. [DOI] [PubMed] [Google Scholar]
- 7.Eichberg DG, Basil GW, Di L, Shah AH, Luther EM, Lu VM, et al. Telemedicine in neurosurgery: lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 2020;88:E1–e12. doi: 10.1093/neuros/nyaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang S, Kim D, Yi E, Choi G, Song M, Lee EK. Telemedicine and the use of Korean medicine for patients with COVID-19 in South Korea: observational study. JMIR Public Health Surveill. 2021;7:e20236. doi: 10.2196/20236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung EY, Kang HW, Park IH, Park DK. Proposal on the establishment of telemedicine guidelines for Korea. Healthc Inform Res. 2015;21:255–264. doi: 10.4258/hir.2015.21.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahn EN, La Marca F, Mazzola CA. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 11.Kim HS. Towards telemedicine adoption in Korea: 10 practical recommendations for physicians. J Korean Med Sci. 2021;36:e103. doi: 10.3346/jkms.2021.36.e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee MH, Jang SR, Lee TK. Comparative analysis of COVID-19 outbreak and changes in neurosurgical emergency patients. J Korean Neurosurg Soc. 2022;65:130–137. doi: 10.3340/jkns.2021.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Majmundar N, Ducruet AF, Wilkinson DA, Catapano JS, Patel J, Baranoski JF, et al. Telemedicine for endovascular neurosurgery consultation during the COVID-19 era: patient satisfaction survey. World Neurosurg. 2021;158:e577–582. doi: 10.1016/j.wneu.2021.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mouchtouris N, Lavergne P, Montenegro TS, Gonzalez G, Baldassari M, Sharan A, et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olson CA, McSwain SD, Curfman AL, Chuo J. The current pediatric telehealth landscape. Pediatrics. 2018;141:e20172334. doi: 10.1542/peds.2017-2334. [DOI] [PubMed] [Google Scholar]
- 16.Omboni S, Caserini M, Coronetti C. Telemedicine and M-health in hypertension management: technologies, applications and clinical evidence. High Blood Press Cardiovasc Prev. 2016;23:187–196. doi: 10.1007/s40292-016-0143-6. [DOI] [PubMed] [Google Scholar]
- 17.Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. 2020;76:1368–1383. doi: 10.1161/HYPERTENSIONAHA.120.15873. [DOI] [PubMed] [Google Scholar]
- 18.Tchero H, Tabue Teguo M, Lannuzel A, Rusch E. Telerehabilitation for stroke survivors: systematic review and meta-analysis. J Med Internet Res. 2018;20:e10867. doi: 10.2196/10867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377:1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Xue H, Huang Y, Huang L, Zhang D. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr. 2017;8:449–462. doi: 10.3945/an.116.014100. [DOI] [PMC free article] [PubMed] [Google Scholar]