NEUROONCOLOGY
S02‐NO‐A1
Pineal region high grade neuroepithelial tumors with NTRK fusions belonging to the novel methylation class “diffuse high grade glioma, IDH‐wildtype, subtype E” (HGG_E)—A distinct clinicopathological and molecular presentation
F. D'Almeida Costa 1,2, J. V. Alves de Castro1, L. Domenici Kulikowski3, B. Wolff3, L. J. Gregianin4, C. Scapulatempo Neto2, C. Kotidis5, O. Al Dalahmah5, P. Canoll5, J. Bruce6, K. Aldape7, Z. Abdullaev7, M. Nasrallah8, G. Zanazzi5
1A.C. Camargo Cancer Center, Department of Anatomic Pathology, São Paulo, Brazil; 2DASA—Diagnósticos da América, Division of Pathology and Genomics, São Paulo, Brazil; 3Faculdade de Medicina da Universidade de São Paulo, Laboratório de Citogenômica, São Paulo, Brazil; 4Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil; 5Columbia University, Department of Pathology and Laboratory Medicine, New York, NY, United States; 6Columbia University, Neurosurgery, New York, NY, United States; 7National Cancer Institute, Laboratory of Pathology, Bethesda, MD, United States; 8Hospital of the University of Pennsylvania, Department of Pathology, Philadelphia, PA, United States
Introduction: Pineal region tumors are rare, with germ cell tumors and pineal parenchymal tumors being more frequent than other neuroepithelial tumors. NTRK fusions are also rare in brain tumors, being more common in some entities, such as infant‐type hemispheric glioma, extraventricular neurocytoma, and in new tumor types described as glioneuronal tumor with kinase fusion type A (GNT_A) and glioneuronal tumor with ATRX alteration, kinase fusion and anaplastic features (GTAKA), new tumor classes initially identified by methylation profiling, a powerful tool for diagnosis and discoveries in neuropathology. Diffuse high grade glioma, IDH‐wildtype, subtype E is a new methylation class, with limited information published about its clinicopathological and molecular features.
Objective: To present the clinicopathological features of three pineal region high grade neuroepithelial tumors with NTRK fusions that belong to the same methylation class (HGG_E).
Patients and Methods: Specimens obtained from resections from pineal region tumors from three patients were submitted to histopathological evaluation, RNA sequencing and methylation profiling.
Results: The patients’ ages were 3, 47 and 71. All patients were male. Histologically, the lesions were composed by ovoid cells with occasional formation of multinucleated giant cells. Mitotic activity and necrotic focus were present in all cases. By immunohistochemistry, there was expression of glial markers (GFAP, Olig2) and more variable positivity for neuronal markers (synaptophysin and Neu N). RNA sequencing demonstrated NTRK fusions in all cases (ZBTB10::NTRK3, ETV6::NTRK3 and LHFPL3::NTRK2). Methylation profiling classified all tumors as HGG_E.
Conclusion: Pineal region tumors with NTRK fusions may constitute one of the presentations of the molecular class HGG_E. While this opens opportunities for targeted therapies, further studies are needed in order to better understand the full spectrum of this novel methylation class.
S06‐NO‐A2
Parent‐of‐origin‐dependent somatic evolution of GNAS‐associated medulloblastoma
S. Mottl 1,2,3, M. Sill4, P. Northcott5, N. Jäger4, S. M. Pfister4, S. M. Waszak1,6,7
1Centre For Molecular Medicine Norway (NCMM), Faculty of Medicine, Oslo, Norway; 2Technical University of Munich, Faculty of Medicine, Munich, Germany; 3University of Heidelberg, Faculty of Medicine, Heidelberg, Germany; 4German Cancer Research Center (DKFZ), Division of Pediatric Neurooncology, Heidelberg, Germany; 5St. Jude Children's Research Hospital, Department of Developmental Neurobiology, Memphis, TN, United States; 6University of California, San Francisco, Department of Neurology, San Francisco, CA, United States; 7École Polytechnique Fédérale de Lausanne (EPFL), Swiss Institute for Experimental Cancer Research (ISREC), Lausanne, Switzerland
Germline variants in the GNAS locus can cause several diseases, including Albright hereditary osteodystrophy, McCune‐Albright syndrome, and fibrous dysplasia. Recently, patients with pathogenic germline GNAS variants and medulloblastoma have been reported, but the molecular landscape of GNAS‐associated medulloblastoma is unknown and guidelines for screening of GNAS deficiency in pediatric neuro‐oncology are missing. In this study, we analyzed GNAS‐associated malignancies in a pan‐cancer cohort of 2000 children, adolescents, and young adults. We identified nine patients with pathogenic somatic and germline variants who exclusively developed Sonic hedgehog‐activated medulloblastoma (SHH‐MB). Germline loss‐of‐function (LoF) variants were observed in infant patients (all <5 years at diagnosis) and with SHH‐beta MB, while somatic missense mutations were only seen in AYA patients (all ≥15 years at diagnosis) and with SHH‐delta MB. Analysis of GNAS‐associated SHH‐MB genomes revealed biallelic hits at the GNAS locus via secondary somatic mutations (AYA) and 20q copy‐neutral LOH (infants and AYA). Analysis of 20q copy‐neutral LOH events in an extended cohort of SHH‐MBs revealed that it is a hallmark event of GNAS‐associated medulloblastoma. Absence of classical SHH‐MB drivers supports GNAS deficiency as the primary mechanism of SHH pathway activation. Phasing of somatic 20q copy‐neutral LOH events using DNA methylation arrays and GNAS imprinting regions revealed a novel parent‐of‐origin‐dependent mechanism of somatic evolution in medulloblastoma. Rare germline LoF variants on the paternal GNAS haplotype predispose to SHH‐beta MB during infancy. In contrast, somatic missense mutations on the maternal GNAS haplotype predispose to SHH‐delta MB in adolescents and young adults. Finally, we demonstrate that DNA methylation‐based tumor subtyping and joint inference of GNAS imprinting patterns allows for routine and rapid screening of GNAS deficiency in medulloblastoma patients.
S06‐NO‐A3
Retinoblastoma in Saudi Arabia—Genomic characterization of 172 cases at King Khaled Eye Specialist Hospital
S. AlMesfer1, A. Maktabi1, E. Deepak1, Y. Liu2, R. Hoehndorf2, M. Abedalthagafi 3
1King Khalid Eye Specialist Hospital, Riyadh, Saudi Arabia; 2King Abdullah University for Science and Technology, Thuwal, Saudi Arabia; 3Emory University, Pathology‐Neuropathology, Atlanta, GA, United States
Retinoblastoma is a rare childhood cancer initiated by RB1 mutation or MYCN amplification, while additional alterations may be required for tumor development. To better understand oncogenesis, we determined the genomic landscape of retinoblastoma. We performed exome sequencing of tumor tissue from 172 retinoblastomas and matched blood DNA. Clinical data were available for 133 out of 172 patients. Majority of patients were females (54.9%) with an average age of 22 months. Eighty‐four patients were diagnosed with unilateral retinoblastoma. Thirty‐seven patients developed bilateral retinoblastoma. Trilateral retinoblastoma was only identified in two patients. Next, we determined the presence of single nucleotide variants, and copy number alterations. For the RB1 gene, 168 out of 172 patients carried 735 mutations, either germline or somatic. Three patients were found to harbor MYCN duplication. Four rare germline variants were identified in more than 10 patients: rs779799724 (49 individuals, MUC3A), rs749107413 (48 individuals, MUC3A), rs754548877 (47 individuals, MUC3A) and rs767343984 (11 individuals, PABPC1 gene). Given the high consanguinity rate in this population, we analyzed the cohort mismatch repair genes (PMS2, MSH6, MLH1, MSH2), of which mutations have shown to be potentially leading to retinoblastoma. Only four individuals (2.3%) carried compound heterozygous variants on these genes. We compared the mutation burden between the patients that carried compound heterozygous variants and the others. It shows that there is a significant difference between them (two‐side T test, p value = 0.00125), illustrating that with mismatch repair genes mutated, patients will accumulate more mutations. We present one of the largest genomic cohort of retinoblastoma to date. Comprehensive molecular analysis has significant implications for translational research to understand the genomics beyond RB1 and MYCN and to test the efficacy of novel therapies for this devastating childhood cancer.
S06‐NO‐A4
A highly atypical embryonal tumor with multilayered rosettes (ETMR) versus a new entity—A series of 6 cases
E. Guney1, K. Mirchia1, R. Lu1, A. Putnam2, M. Alashari2, H. Zhou2, N. Whipple2, P. Chan2, S. Cheshier2, D. Samuel3, S. Ferris4, E. Pinarbasi4, M. Terry1, M. Pekmezci1, A. Bollen1, T. Tihan1, K. Aldape5, A. Perry 6
1UCSF, Pathology, San Francisco, CA, United States; 2Primary Children's Hospital, Salt Lake City, UT, United States; 3Valley Children's Hospital, Madera, CA, United States; 4University of Michigan, Ann Arbor, MI, United States; 5National Institute of Health, National Cancer Center, Bethesda, MD, United States; 6UCSF, Pathology and Neurological Surgery, San Francisco, CA, United States
Introduction: Embryonal tumor with multilayered rosettes (ETMR) is a distinct neoplasm with variable histologic features previously described under the rubric of “ependymoblastoma,” “embryonal tumor with abundant neuropil and true rosettes,” and “medulloepithelioma.” It became a recognized WHO entity in 2016 based on unifying features, including strong diffuse LIN28A immunoreactivity and a signature C19MC alteration. A new DICER1‐altered ETMR subtype was added in the 2021 WHO scheme.
Objectives: (1) Increase awareness of a potentially new and diagnostically challenging pediatric brain tumor. (2) Review the clinicopathologic and molecular data from six cases.
Materials and Methods: Clinicopathologic assessment, targeted next‐generation DNA sequencing (NGS), and DNA methylation profiling (DNAMP) was performed on tumor that clustered with ETMR by DNAMP, but showed no evidence of either C19MC or DICER1 alterations.
Results: The patient cohort consists of two male and four female infants ranging from 9 days to 15 months of age (median 8 months). Most tumors were centered in the posterior fossa (N = 5), with one involving midbrain, thalamus, and pineal. Although all featured primitive cells, multilayered rosettes were absent in 5 (83%) and LIN28A was absent to minimally positive in 5 of 6 cases (83%). A missense TP53 mutation was identified in one, but NGS showed no pathogenic alterations in the others. Three patients died 5, 7 and 20 months after surgery, while two are still alive at 8 and 12 months post‐surgery. One showed complete glioneuronal maturation (i.e., no residual primitive component) on three resection specimens following chemotherapy.
Conclusions: Herein, we report six primitive CNS tumors of infancy with unusual histopathologic and molecular features. Currently, it is unclear if these cases represent a new CNS embryonal tumor type or a previously unreported ETMR subtype with atypical features. Further studies are needed to further characterize this novel tumor.

FIGURE 1.

FIGURE 2.
S06‐NO‐A5
Defects of mismatch repair proteins in pediatric high grade gliomas
C. Haberler 1, P. Muller1, L. Müllauer2, A. Azizi3, J. Gojo3, T. Czech4, C. Dorfer4, I. Slavc3, K. Wimmer5
1Medical University of Vienna, Neurology, Division of Neuropathology and Neurochemistry, Vienna, Austria; 2Medical University of Vienna, Clinical Institute of Pathology, Vienna, Austria; 3Medical University of Vienna, Department of Pediatrics and Adolescent Medicine, Vienna, Austria; 4Medical University of Vienna, Department of Neurosurgery, Vienna, Austria; 5Medical University of Innsbruck, Division of Human Genetics, Innsbruck, Austria
Introduction: Hetero‐ and homozygous germline mutations of the mismatch repair genes MLH1, PMS2, MSH2 and MSH6 cause Lynch and constitutional mismatch repair (CMMRD) cancer predisposition syndrome, respectively. Affected CMMRD individuals are at risk to develop a variety of neoplasms including CNS tumors, particularly high grade gliomas (HGG).
Objective: Currently, few data exist on the prevalence of mismatch repair defects in children with pediatric HGG.
Patients and Methods: Fifty HGGs of patients aged between 1.3 and 18 years at diagnosis were analyzed. Immunohistochemistry with antibodies against the mismatch repair (MMR) proteins MLH1, PMS2, MSH2 and MSH6 was performed. Five patients with known CMMRD were included. The evaluation of the slides was made blinded to the CMMRD status. NGS was performed in patients with loss of MMRs.
Results: We found PMS2 or combined MSH2/MSH6 loss in five patients with genetically confirmed CMMRD and diffuse pediatric‐type high‐grade glioma, H3 wildtype and IDH‐wildtype. Additionally, we detected eight patients with loss of MSH2/MSH6 staining in tumor cells, but retained staining in preexisting cells, indicating a pattern like in Lynch syndrome. NGS sequencing of these tumor tissues revealed MSH2 or MSH6 mutations in three patients with diffuse paediatric‐type HGG, H3‐WT and IDH‐WT, whereas in five patients with other HGG types no mutations in the MMR genes were detectable.
Conclusions: We found a low prevalence of CMMRD among HGGs, but identified three patients with probable Lynch syndrome. A combined approach using immunohistochemistry and molecular analyses increases the detection of CMMRD and Lynch patients and should be performed in all diffuse paediatric‐type high‐grade gliomas, H3‐wildtype and IDH‐wildtype.
S06‐NO‐A6
SWI/SNF ATPases as therapeutic targets in H3K27M diffuse midline gliomas
S. Venneti 1, M. Mota1, S. Sweha1, M. Punn1, S. K. Natarajan1, C. Chung1, D. Hawes2, F. Yang2, A. Judkins2, S. Samajdar3, X. Cao1, L. Xiao1, A. Parolia1, A. Chinnaiyan1
1University of Michigan, Ann Arbor, MI, United States; 2Children's Hospital Los Angeles, Los Angeles, CA, United States; 3Aurigene Discovery Technologies, Bengaluru, India
Diffuse midline gliomas (DMGs) including diffuse intrinsic pontine gliomas (DIPGs) are fatal pediatric brain cancers without effective treatments. They bear H3 lysine27‐to‐methionine mutations (H3K27M) that cause global decrease in the transcriptional repressive mark H3K27me3. This is accompanied by an increase in the transcriptional activation mark H3K27ac that is enriched at enhancers resulting in enhancer addiction. We hypothesized that H3K27M mutations could reprogram the epigenome in addition to altering histone H3 modifications. We focused on the chromatin remodeling SWI/SNF master complex that has been implicated in both brain development and cancers in general. The SWI/SNF complex bears obligate subunits termed SMARCA4 and SMARCA2 that are ATP dependent. We used a panel of patient‐derived cell lines and tumor tissues to show that H3K27M increases protein levels of SMARCA4. Conversely, knockdown of mutant H3K27M lowered SMARCA4 protein levels. We took advantage of a proteolysis targeting chimera (PROTAC) tool compound called AU‐15330 that targets both SMARCA4 and SMARCA2 for degradation. AU‐15330 selectively killed H33K27M but not H3 wild‐type, or H3G34V cells. Mechanistically, AU‐15330 lowered global H3K27ac levels, and reduced chromatin accessibility at genomic regions corresponding to enhancers. We used gene‐expression, proteomics, and ATAC‐seq assays to demonstrate that AU‐15330 reduced expression of of FOXO1, a key member of the forkhead family of transcription factors. FOXO1 in turn regulated levels of the RHOB GTPase, and genetic or pharmacologic suppression of FOXO1 resulted in cytotoxicity. Overall, our results suggest that H3K27M reprograms chromatin by modifying the SWI/SNF complex in addition to driving aberrant histone modifications. This creates an epigenetic dependency that can be suppressed by combined targeting of SWI/SNF ATPases. This approach serves as a potent therapeutic strategy for these uniformly fatal pediatric brain tumors.
S12‐NO‐A7
Patterns and evolution of structural complexity in 323 GBM whole genomes
A. Hamdan 1,2,3, S. Aitken2, A. Meynert2, S. Pollard1,3, C. Semple2
1Edinburgh Cancer Research Centre, Edinburgh, United Kingdom; 2Institute of Genetics and Cancer, Edinburgh, United Kingdom; 3Centre for Regenerative Medicine, University of Edinburgh, Edinburgh, United Kingdom
The impact of complex structural variants (SVs) on the evolution of isocitrate dehydrogenase (IDH) wild‐type glioblastoma (GBM) has been underexplored due to the lack of whole genome sequencing (WGS) data. Here we perform a harmonised analysis of 323 publicly available GBM samples with short‐read WGS data, with the aim to provide the most comprehensive landscape of complex SVs in GBM to date. Using a Gamma–Poisson model correcting for covariates known to influence SV formation, we detect SV hotspots in 116 regions within chromosomes 1, 4, 7, 9, 10 and 12 (q < 0.1, l = 1.06). Intergenic SVs within hotpots are enriched with regulatory elements (permutation test; p = 1.1–7) and overlap with regions harbouring chromothripsis (p = 2.2–12), and extrachromosomal DNA (ecDNA) (p = 1.2–14), suggesting positive selection. 59.1% of samples contain at least one chromothriptic event. Intriguingly, we observe no association between p53 alterations or polyploidy with the presence of chromothripsis (chi‐squared tests; p = 0.49, p = 0.35, respectively), suggesting that chromothripsis may occur in genomes without genetic p53 alterations. Over 70% of chromothriptic events disrupt oncogenes/tumour suppressor genes (TSGs), with CDKN2A (17.2% of chromothriptic samples) and EGFR (16.2%) being among the most disrupted GBM genes. We observe events spanning multiple chromosomes in 29.1% of chromothriptic samples; in seven samples, we detect simultaneous alterations of GBM oncogenes and TSGs on separate chromosomes. Comparison of primary‐recurrent samples (N = 30) reveal that chromothripsis is rarely acquired or lost at recurrence, with rates of event acquisition or loss at recurrence of 3% and 3%, respectively. In conclusion, using the largest cohort of GBM whole genomes to date, we highlight the presence of punctuated evolution in most GBM genomes, and discuss the substantial contribution of chromothripsis to genomic instability and tumourigenesis in GBM.
S12‐NO‐A8
Clinical and molecular characterization of extracranial metastases from glioblastomas
J. Jacobsen 1,2, C. O'Rourke3, A. Locallo3,4, J. F. Carlsen5,6, J. D. Ewald7,8, D. Scheie6,9, K. Grunnet10, A. Y. Schmidt11, L. C. Melchior9, J. L. Weischenfeldt3,4, V. A. Larsen5, J. B. Andersen3, H. S. Poulsen10, H. Broholm9, S. R. Michaelsen1,2,10, B. W. Kristensen1,2,10
1Rigshospitalet, Copenhagen University Hospital, Department of Pathology, The Bartholin Institute, Copenhagen, Denmark; 2University of Copenhagen, Department of Clinical Medicine and Biotech Research and Innovation Center (BRIC), Copenhagen, Denmark; 3University of Copenhagen, Biotech Research and Innovation Centre (BRIC), Department of Health and Medical Sciences, Copenhagen, Denmark; 4Rigshospitalet, Copenhagen University Hospital, The Finsen Laboratory, Copenhagen, Denmark; 5Rigshospitalet, Copenhagen University Hospital, Department of Radiology, Copenhagen, Denmark; 6University of Copenhagen, Department of Clinical Medicine, Copenhagen, Denmark; 7Odense University Hospital, Department of Pathology, Odense, Denmark; 8University of Southern Denmark, Department of Clinical Research, Odense, Denmark; 9Rigshospitalet, Copenhagen University Hospital, Department of Pathology, Copenhagen, Denmark; 10Rigshospitalet, Copenhagen University Hospital, The DCCC Brain Tumor Center, Department of Oncology, Copenhagen, Denmark; 11Rigshospitalet, Copenhagen University Hospital, Center for Genomic Medicine, Copenhagen, Denmark
Introduction: Glioblastoma (GBM) is the most common and malignant primary brain tumor in adults, but in contrast to many other malignancies, they rarely metastasize. Metastasizing GBMs cause diagnostic and therapeutic challenges and are poorly investigated.
Objectives: To characterize these tumors clinically and molecularly.
Materials and Methods: We collected the largest cohort to date of tissue from 16 glioma patients (14 GBMs and 2 lower‐grade gliomas) with extracranial metastases to scalp (7) lymph nodes (5), bone (2), liver (1), and upper neck (1). MRI scans were examined and paired primary tumors, recurrences and metastases were investigated by NGS, genome‐wide 850 K methylation profiling and immunohistochemistry (IHC) followed by quantitation of markers of stemness and immune cells in the tumor microenvironment (TME).
Results: Clinically, the patients were comparable to other GBM patients (gender, age, treatment, and survival). 12/16 patients developed one or more intracranial recurrence(s) and 6/7 scalp lesions were extracranial extensions of the brain tumors. MRI scans revealed proximity of the brain tumors to dura, large vessels, and ventricles in many patients. NGS showed that the metastases were clonally derived from the primary tumors and methylation‐ and copy number analysis revealed a patient‐specific signature across paired samples in most patients. We observed methylation subclass switch during tumor progression and an increased number of differentially methylated regions in the olfactory transduction pathway. Levels of tumor stemness and the composition of immune cells did not change, as shown by methylation‐based cell‐type deconvolution, stemness index and IHC.
Conclusion: Extracranial metastases occurred as early events and preserved the tumor‐ and TME characteristics of the primary brain tumors. Parameters such as tumor location, surgery and epigenetic regulation of genes associated with olfactory transduction could be involved in this process.
S12‐NO‐A9
A rationale to screen mismatch repair deficiency among adult patients with glioma—An analysis of 1225 cases
P. Benusiglio1, F. Elder1, M. Touat2, A. Perrier1, M. Sanson2, C. Colas3, L. Guerrini‐Rousseau4, D. T. Tran5, N. Trabelsi6, C. Carpentier6, Y. Marie6, C. Adam7, M. Bernier8, D. Cazals‐Hatem9, K. Mokhtari5, S. Tran5, B. Mathon10, L. Capelle10, M. Dhooge11, A. Idbaih2, A. Alentorn2, C. Houillier2, C. Dehais2, K. Hoang‐Xuan2, S. Cuzzubbo12, A. F. Carpentier12, A. Duval13, F. Coulet1, F. Bielle 5
1Sorbonne Université, Génétique Médicale, Paris, France; 2Sorbonne Université, Neurology, Paris, France; 3Institut Curie, Génétique, Paris, France; 4Institut Gustave Roussy, Cancérologie de l'Enfant et de l'Adolescent, Villejuif, France; 5Sorbonne Université, Neuropathology, Paris, France; 6Paris brain Institute, Paris, France; 7CHU de Bicêtre, AP‐HP, Anatomopathologie, Paris, France; 8Hôpital Foch, Anatomie et Cytologie Pathologiques, Suresnes, France; 9Hôpital Beaujon, AP‐HP, Anatomie Pathologique, Clichy, France; 10Sorbonne Université, Neurosurgery, Paris, France; 11Hôpital Cochin, AP‐HP, Gastroentérologie et Oncologie Digestive, Paris, France; 12Hôpital Saint‐Louis, AP‐HP, Neurology, Paris, France; 13Sorbonne Université, Equipe Instabilité des Microsatellites et Can, Paris, France
Introduction: The prevalence of mismatch repair‐deficiency (MMRd) in de novo adult gliomas is poorly documented. MMRd testing is not required to classify gliomas according to WHO 2021 while MMRd have major clinical implications. It can be the hallmark of Lynch syndrome (LS) and it makes tumor resistant to temozolomide and candidate for immunotherapy.
Objectives: Screening of a large series of unselected gliomas for MMRd and LS, and characterization of their main genomic and clinical features.
Patient and Methods: A consecutive series (2017–2022) of 1225 treatment‐naïve adult gliomas was analysed by targeted next generation sequencing including mismatch repair (MMR) genes MSH2, MSH6, MLH1, and PMS2. Immunostaining (IHC) of corresponding MMR proteins was done for tumors with ≥1 MMR pathogenic variant (PV). Gliomas with ≥1 PV and protein expression loss were considered MMRd. Patients with de novo MMRd tumors had germline testing. An additional cohort of glioblastoma IDH‐wildtype diagnosed over the 2007–2021 period and enriched in young adults was studied by IHC and complementary sequencing (for abnormal IHC results).
Results: Nine gliomas out of 1225 were MMRd (0.73%): 8 glioblastomas, IDH‐wt, and one astrocytoma, IDH‐mutant. ATRX (56%) and TP53 (89%) mutations were frequent in contrast to TERT promoter mutation or EGFR amplification that were absent. Four cases with age <50 had a LS diagnosis because of the glioma, with germline PV in MSH2 (n = 3) and MLH1 (n = 1). One case with age >50 had a LS diagnosis preceding the occurrence of the glioma. One 19‐year‐old patient had PMS2‐associated CMMRD. Three MSH6‐deficient tumors with negative germline testing corresponded to sporadic MMRd gliomas. In the second series of glioblastomas, IDH‐wt, MMRd prevalence was 12.5% in the <40‐year age group, 2.6% in the 40–49 year group, and 1.6% the ≥50 year group.
Conclusion: Our results advocate for a systematic screening for MMRd and LS in glioblastomas, IDH‐wt diagnosed under the age of 50.
S12‐NO‐A10
The clinicopathological, molecular characteristics and prognosis of adult epithelioid glioblastomas—A report of 39 cases
S. Xi 1, S. Jiang1, J. Zeng1
1Sun Yat‐sen Universtiy Cancer Center, Pathology, Guangzhou, China
Question: Epithelioid glioblastoma (eGBM) is a rare subtype of GBM and is reported more often in children and young adults. Since the pediatric‐type and adult‐type gliomas are separated, how about the molecular characteristics and prognosis of adult eGBM?
Methods: We retrospectively reviewed 39 adult eGBM for clinicopathologic information. Molecular profiling using next‐generation sequencing was performed in 10 cases. Survival was analyzed by Kaplan–Meier curves.
Results: EGBM accounted for 11.1% (39/350) of the GBM with IDH and H3 wildtype, with a median age of 53. Male to female ratio was 0.44:1. EGBM mostly occurred in the temporal lobe (16/39, 41%). Microscopically, the tumors mainly or completely consist of epithelioid cells with focal poor cohesive. Zonal necrosis was commonly observed (38/39, 97.4%). Perivascular infiltration (10/39, 25.6%) and leptomeningeal dissemination (7/39, 17.9%) were not uncommon. Fifteen cases showed pleomorphism morphological features. All the cases were diffuse or partially immunopositive for GFAP and Olig‐2. BRAF V600E is positive in the 9 (9/22, 40.9%) cases. According to sequencing, CDKN2A/B homogeneous deletion was the most frequently mutated gene (80%, 8/10), followed by TERT promoter mutation (70%, 7/10) and BRAF V600E mutation (50%, 5/10). The concurrent of three gene alterations was observed in 4 cases (4/10, 40%). Half of the cases (5/10, 50%) possessed EGFR gene alteration. The 2‐year overall survival of adult eGBM was 7%. Adult eGBM carried a dismal prognosis compared to adult GBM with H3 and IDH wildtype (OS: 13.7 vs. 24.1 months; p = 0.003).
Conclusion: Adult's eGBM harbored a high frequency of gene alteration in the MAPK pathway and cyline related genes. Adult eGBM carries a significantly poor prognosis. This rare adult eGBM we collected here would further promote the investigation of dedicated therapeutic strategies.

FIGURE 1 Histopathologic features of adult eGBM.

FIGURE 2 The molecular alterations and survival of adult eGBM.
S12‐NO‐A11
Concurrent RB1 and P53 pathway alterations predispose to the development of primitive neuronal component in glioblastoma through the upregulation of EBF3
F. Pagani1, M. Gryzik1, E. Somenza1, F. Orzan2, F. De Bacco2, G. Crisafulli3, S. Lago4, A. Zippo4, C. Boccaccio2, P. L. Poliani 5
1University of Brescia, Molecular and Translational Medicine, Brescia, Italy; 2Candiolo Cancer Institute—FPO, IRCCS, Laboratory of Cancer Stem Cell Research, Candiolo, Italy; 3Candiolo Cancer Institute—FPO, IRCCS, Bio Informatic Group (BIG) & Laboratory of Molecular Oncology, Candiolo, Italy; 4University of Trento, Laboratory of Chromatin Biology & Epigenetics, Trento, Italy; 5Vita‐Salute San Raffaele University, Pathology, Milan, Italy
Introduction: Glioblastoma with primitive neuronal component (GBM‐PNC) is a rare and poorly recognized GBM variant characterized by nodules containing cells with primitive neuronal differentiation and PNET‐like features along with conventional GBM areas. This entity represents an unique model to investigate the relationships between genetic alterations, tumour biology and their phenotypic manifestations.
Objectives: It was recently reported that GBM‐PNCs frequently show alterations in the RB1 pathway, suggesting that inactivation of RB1 may be a driving mechanism for the development of GBM‐PNC. Hereby, we investigated the molecular mechanisms by which RB1 alterations may predispose to the development of GBM‐PNC.
Materials and Methods: We extensively characterized a cohort of GBM‐PNCs (n = 24) by means of immunophenotypic and high‐throughput molecular analyses, including NGS, RNAseq, ChIP. In vitro studies were performed on both EBF3 knockout glioma stem cells (GSCs) obtained by mean of CRISPR/Cas9‐mediated genome editing and EBF3 overexpressing GSCs obtained by Lentiviral vector transduction.
Results: In GBM‐PNC both components are highly enriched in genetic alterations directly causing cell cycle deregulation (RB1 inactivation or CDK4 amplification) and p53 pathway inactivation (TP53 mutation or MDM2/4 amplification). However, the PNC component displays further upregulation of transcriptional pathways associated with proliferative activity, including overexpression of MYC target genes. In addition, we showed that the PNC phenotype relies on the expression of EBF3, an early neurogenic transcription factor, which is directly controlled by MYC transcription factors in accessible chromatin sites.
Conclusion: The concomitant presence of genetic alterations, impinging on both cell cycle and p53 pathway control, strongly predispose GBM to develop a concomitant poorly differentiated primitive phenotype depending on MYC‐driven EBF3 transcription in a GBM cell subset.
S12‐NO‐A12
DNA hypomethylator phenotype remodels oncogenic glutamate metabolism in glioblastoma
K. Masui 1, M. Harachi2, P. Mischel3, A. Kurata1, N. Shibata1
1Tokyo Women's Medical University, Department of Pathology, Tokyo, Japan; 2RIKEN Center for Integrative Medical Sciences, Laboratory for Developmental Genetics, Yokohama, Japan; 3Stanford University, Department of Pathology, Stanford, CA, United States
Introduction: Epigenetic status including DNA methylation determines chromatin structure to control gene expression, and aberrant DNA methylation pattern is closely associated with oncogenesis. Specifically, a subtype of brain tumors (glioblastoma: GBM) was reportedly associated with DNA demethylation and poor outcome in contrast to a relatively fair isocitrate dehydrogenase gene (IDH)‐mutant glioma subtype with a CpG island methylator phenotype (G‐CIMP), suggesting a close link of DNA hypomethylation with aggressive cancer biology. However, the mechanisms to induce cancer‐specific “hypomethylator phenotype” remain largely unclear.
Methods: To uncover the regulatory mechanism and functional consequences of tumor‐promoting DNA hypomethylation, we interrogated cell lines, mouse tumor models, and clinical samples of GBM, the highly lethal brain cancer in human.
Results: We herein demonstrate that in the highly malignant GBM, IDH‐wildtype with receptor tyrosine kinase (RTK) gene mutation, mechanistic target of rapamycin complex 2 (mTORC2), a critical component of epidermal growth factor receptor (EGFR) signaling, suppresses the transcription of de novo DNA methyltransferase (DNMT3A) to induce genome‐wide DNA hypomethylation. Integrated analyses with comprehensive methylation array and histopathological evaluation of mouse and human GBM samples reveal that mTORC2‐dependent DNA hypomethylation consistently remodels a glutamate metabolism network, eventually affecting neuron‐glioma interaction and glioma cell invasion to sustain tumor cell survival.
Conclusions: The findings nominate mTORC2 as a novel and critical regulator of DNA hypomethylator phenotype in cancer as well as an exploitable target to interfere with cancer‐promoting epigenetic aberration.
S24‐NO‐A13
Investigating regional heterogeneity and progression‐associated markers in oligodendrogliomas
T. Millner 1,2, H. Mikaeili3, A. Shabbir3, A. Lowe3, S. Brandner1,3,2
1Queen Mary University of London, Blizard Institute, London, United Kingdom; 2Division of Neuropathology, UCLH, London, United Kingdom; 3UCL Queen Square Institute of Neurology, Department of Neurodegenerative Disease, London, United Kingdom
Question: Oligodendrogliomas are defined by IDH‐mutation and 1p/19q‐codeletion. Molecular stratification of oligodendrogliomas has proved difficult, despite recent progress in other brain tumours. Loss of H3K27 trimethylation (H3K27me3) is seen in many, but not all oligodendrogliomas, and we have observed H3K27me3 loss predominantly in low‐grade oligodendrogliomas, and more often retention in high‐grade tumours. Our aims are to establish the downstream effects of H3K27me3 regulation in oligodendrogliomas to identify progression‐associated biomarkers.
Methods: Seventy‐eight oligodendrogliomas (CNS WHO grade 2: n = 38, grade 3: n = 40) were tested for H3K27me3 expression. These tumours showed either down‐regulation (H3K27me3−), retention of expression (H3K27me3+) or intratumoural heterogeneity (H3K27me3Het). Sixty‐five regions across these three types were micro‐dissected for DNA methylation profiling and RNA sequencing.
Results: Of the H3K27me3− tumours 85% (35/41) were grade 2, of the H3K27me3+ tumours 100%(10/10) were grade 3, and of the H3K27me3Het tumours 87% (20/23) were grade 3. With DNA methylation arrays and derived copy number data we have shown a different breakpoint of chr 1p in H3K27me3+ areas, and in 15 paired samples, 6 gains and 12 losses in H3K27me3+ regions, and overall 24 copy number differences between H3K27me3+ and me3− areas within the same tumours. RNA sequencing suggests distinct expression profiles between H3K27me3+ and H3K27me3− areas.
Conclusions: We have shown a close correlation between areas with high‐grade features and H3K27me3 expression both between and within tumours. We have shown that H3K27me3+ and me3− areas within the same tumours show copy number changes and have differential gene expression. Using pathway analysis we have identified pathways and genes involved in tumour progression and mediation of histone modification. We are currently using these targets for functional studies and protein level validation with the overall aim of developing IHC biomarkers.
S24‐NO‐A14
CDKN2A/B deletion in IDH‐mutant astrocytomas
M. Ranade 1, A. Sahay1, T. Gupta2, A. Moiyadi3, P. Shetty3, O. Shetty1, S. Kannan4, E. Sridhar1
1Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Pathology, Mumbai, India; 2Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Radiation Oncology, Mumbai, India; 3Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Neurosurgery, Mumbai, India; 4Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Biostatistics, Mumbai, India
Introduction: CDKN2A/B homozygous‐deletion in IDH‐mutant astrocytic tumours is one of the defining features for grade 4.
Objective: To evaluate CDKN2A/B‐deletion in IDH‐mutant astrocytic tumours and correlate with clinico‐pathological parameters.
Methods: CDKN2A/B‐deletion was evaluated by FISH and interpreted by Ambros et al. (method‐1) and Marker et al. (method‐2) methods.
Results: (Table 1): 83 (histological grade 2 = 3, grade 3 = 46, grade 4 = 34) of 94 IDH‐mutant astrocytic tumours were interpretable. By method‐1, 56 showed true‐deletion (of these 54 showed homozygous‐deletion by method‐2), 13 showed imbalance (8 of these showed homozygous‐deletion by method‐2). Fourteen showed no deletion (all showed no deletion by method‐2). Both methods showed good agreement; more on combining true‐deletion and imbalance (Kappa = 0.75). Concordant CDKN2A/B‐deletion was observed in 71% (27/38) of lower‐grade tumours (n = 49) and 89.7% (26/29) of histological grade 4 tumours. Concordant CDKN2A/B‐deletion showed correlation for higher grade (p = 0.02) and inverse correlation for <10% MIB‐1 labeling index (p = 0.01). No significant correlation was observed for any of the clinico‐pathological parameters. Progression/recurrence was in 18 patients, 12 (66.7%) were histologically grade 4. All showed homozygous‐deletion by method‐2; while by method‐1, 10 showed true‐deletion and 2 showed imbalance. Rest 6 (33.3%) were histologically grade 3; 4 cases showed concordant results of deletion in 2 cases, no deletion in 2 cases while 2 cases showed discordant results (no deletion by method‐1; deletion by method‐2). No significant impact CDKN2A/B‐deletion on overall‐survival was observed (Table 1).
Conclusion: CDKN2A/B‐deletion was observed across all histological grades of IDH‐mutant astrocytic tumours, expectedly more in higher grade. Ambros et al. and Marker et al. methods of interpretation for CDKN2A/B deletion showed good agreement, however no significant survival correlation was observed.

S24‐NO‐A15
Heterochromatin dysfunction impacting genomic topology and superenhancer landscapes underlies ATRX‐deficient gliomagenesis
P. B. Malgulwar1, A. K. Saw1, A. Singh1, C. Danussi2, K. Rai1, J. Huse 1
1University of Texas MD Anderson Cancer Center, Pathology and Translational Molecular Pathology, Houston, TX, United States; 2Sanofi, Research and Development, Cambridge, MA, United States
Introduction: Mutational inactivation of the SWI/SNF chromatin regulator ATRX occurs frequently in diffuse gliomas. Whether and how ATRX deficiency promotes oncogenesis remains unclear, despite its implication across a broad array of physiological processes.
Objectives: We sought to delineate the molecular mechanisms by which global epigenomic dysfunction promotes oncogenic phenotypes in ATRX‐deficient glioma models.
Materials and Methods: Building on earlier work implicating chromatin accessibility and transcriptional shifts, we employed integrated epigenomic profiling in Atrx‐intact and ‐deficient murine neuroepithelial progenitor cells (mNPCs), validating findings will functional approaches in human glioma stem cells (GSCs) of appropriate genotype.
Results: We found that ATRX deficiency dramatically impacted the integrity of large heterochromatin domains genome‐wide, with tangible effects on underlying gene expression. This process fundamentally altered chromatin topology, as assessed by Hi‐C analysis, and associated superenhancer landscapes, influencing key developmental gene sets like the HOXA cluster. Pharmacological inhibition of HOXA signaling in GSCs selectively reduced proliferation, increased apoptosis, and impaired in vivo growth in the ATRX‐deficient context. Finally, our results pointed to derepression of LINE1 endogenous retroviral elements as key mediators of ATRX‐deficient heterochromatin dysfunction.
Conclusion: Our work implicates novel and targetable molecular mechanisms involving complex epigenomic rewiring and chromatin topology in ATRX‐deficient oncogenesis. In doing so, we advance the understanding of a deadly brain tumor along with broader conceptions of epigenetic mechanisms as fundamental drivers in cancer.
S24‐NO‐A16
Analysis of the implementation of DNA methylation assay for routine CNS tumors diagnosis
M. Mezmezian 1, N. Arakaki1, G. Sevlever1, H. Martinetto1
1Fleni, Department of Neuropathology and Molecular Biology, Buenos Aires, Argentina
Introduction: In the last years, DNA methylation array emerged as a new tool for CNS tumor diagnosis.
Objectives: To analyze the value of methylation assay for routine CNS tumor diagnosis.
Patients and Methods: We performed methylation array in 182 CNS tumors (100 gliomas (GL), 27 medulloblastomas (MDB), 20 ependymomas (EP), 17 neuronal/glioneuronal tumors (N/GNT), 5 meningiomas, 7 embryonal tumors (ET), and 6 sarcomas) from 2019 for subtyping GL, EP, MDB, meningiomas, and sarcomas, defining the diagnosis in cases without precise histological features or confirming the histological diagnosis.
Results: Scores were >0.75 in 147 cases (81%). The histological diagnosis was maintained and allowed subtyping in 127 cases (70%) (77 GL, 27 MDB, 12 EP, etc.), defined differential diagnoses in 16 cases (9%) (3 sarcomas, 5 ET, 3 EP, etc.), and changed the diagnosis in 4 cases (2%). Scores were ≤0.75 in 35 cases (19%), however, in 7/14 adult diffuse GL, CNV analysis (EGFR amplification, and Chr.10q and CDKN2A/B deletions) led to the diagnosis of the cases as IDH‐wt glioblastomas based on the WHO classification. In 8/35 cases displaying scores ≤0.75, RNA and/or DNA sequencing was performed and led to the diagnosis of 4 tumors (1 sarcoma, 2 DMG H3K27‐altered, and 1 pilocytic astrocytoma). Thus, in 24 cases (13%) diagnosis could not be achieved; among these cases, 10 were N/GNT.
Conclusion: The methylation array is a valuable tool to diagnose most CNS tumors because a single technique offers both the diagnosis and molecular data, mainly for adult diffuse GL, MDB, and EP. Nowadays, the main limitations of the method are the high amount of DNA necessary for performing the study, economic issues for developing countries, and the absence in the classifier of uncommon tumors, such as low‐grade N/GNT, and some of the new tumors of the 2021 WHO classification. The growth of the case base will improve the identification skills of the system, probably perfecting its diagnostic capabilities.
S24‐NO‐A17
A novel type of IDH‐wildtype glioma characterized by highly diffuse growth pattern, distinct epigenetic profile and relatively favorable prognosis
A. Münch 1, D. Teichmann2, D. Spille3, P. Kuzman4, E. Pérez2, S. A. May5, W. C. Mueller4, T. Kombos6, S. Nazari‐Dehkordi6, J. Onken7, P. Vajkoczy7, G. Ntoulias8, C. Bettencourt9, A. von Deimling10, W. Paulus11, F. L. Heppner2,12,13,14, A. Koch2,12, D. Capper2,12, D. Kaul15, C. Thomas11, L. Schweizer1,2,12,16,17
1Universitätsklinikum Frankfurt, Neurologisches Institut (Edinger Institut), Frankfurt a. M., Germany; 2Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neuropathology, Berlin, Germany; 3University Hospital Munster, Department of Neurosurgery, Muenster, Germany; 4University Hospital Leipzig, Institute of Neuropathology, Leipzig, Germany; 5Klinikum Chemnitz, Department of Neurosurgery, Chemnitz, Germany; 6Schlosspark‐Klinik Charlottenburg, Abteilung für Neurochirurgie, Berlin, Germany; 7Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neurosurgery, Berlin, Germany; 8Vivantes Klinikum Neukölln, Department of Neurosurgery, Berlin, Germany; 9University College London, UCL Queen Square Institute of Neurology, London, United Kingdom; 10University Hospital Heidelberg, Department of Neuropathology, Heidelberg, Germany; 11University Hospital Munster, Department of Neuropathology, Muenster, Germany; 12German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Berlin, Berlin, Germany; 13NeuroCure, Cluster of Excellence, Berlin, Germany; 14German Center for Neurodegenerative Diseases (DZNE), Berlin, Germany; 15Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Radiation Oncology and Radiotherapy, Berlin, Germany; 16German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Frankfurt, Frankfurt a. M., Germany; 17Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany
Background: Diffuse gliomas in adults encompass a heterogeneous group of CNS neoplasms. In recent years, extensive (epi‐)genomic profiling has identified several glioma subgroups characterized by distinct molecular characteristics, most importantly IDH1/2 and histone H3 mutations.
Objective: HGG‐F is a novel methylation class of the DKFZ v12.5 Brain Tumor Classifier. We aim to characterize this class morphologically and molecularly.
Methods: A cohort of 16 diffuse gliomas classified as “adult‐type diffuse high grade glioma, IDH‐wildtype, subtype F (HGG‐F)” was identified by the Brain Tumor Classifier. Histopathological characterization, exome sequencing and review of clinical data was performed in all cases.
Results: Based on unsupervised t‐SNE and clustering analysis of genome‐wide DNA methylation data, HGG‐F shows distinct epigenetic profiles separate from established CNS tumors. Exome sequencing demonstrated frequent TERT promoter (12/15 cases), PIK3R1 (11/16) and TP53 mutations (5/16). Radiological characteristics were reminiscent of gliomatosis cerebri in 9/14 cases (64%). Histopathologically, most cases were classified as diffuse gliomas (7/16, 44%) or were suspicious for the infiltration zone of a diffuse glioma (5/16, 31%). None of the cases exhibited microvascular proliferation or necrosis. Outcome of 14 patients with follow‐up data was better compared to IDH‐wildtype glioblastomas with median progression‐free survival of 58 months and overall survival of 74 months (both p < 0.0001).
Conclusion: Our series represents a novel type of adult‐type diffuse glioma with distinct molecular and clinical features. Importantly, we provide evidence that TERT promoter mutations in diffuse gliomas without further morphological or molecular signs of high‐grade glioma should be interpreted in the context of the clinico‐radiological presentation as well as epigenetic profile and may not be suitable as standalone marker for glioblastoma, IDH wildtype.
S24‐NO‐A18
Molecular profiling of ependymomas in Indian cohort
M. C. Sharma 1, A. Sharma1, R. Mallick1, V. Suri1, A. Jagdevan1, M. Singh1, A. Garg1
1All India Institute of Medical Sciences, Neuropathology, Delhi, India
Background: Ependymomas are relatively rare glial tumours which supposedly arise from the radial glial cells and show ependymal differentiation. Similar grade tumours behave differently at different anatomical locations and show different molecular signatures. Molecular profiling is important for risk stratification and prognostication.
Aims and Objective: To study the molecular profiling of ependymomas in different anatomical locations in the Indian cohort of patients.
Material and Methods: Studied 180 cases of ependymomas located in ST (76 cases), PF (30 cases) and spinal cord (76 cases). Immunostaining for LICAM, p65, H3k27me3, H3K27M, EZH2, EZHIP and NMyc was done. FISH for RELA break apart, ZFTA fusion, YAP break apart and NMYC amplification was done.
Results: Seventy‐six cases were located in ST location, of which 56 (76.68%) showed RELA fusion, YAP1 fusion in 2 cases (2.63%) and 18 cases (23.68%) could not be characterized. Thirty cases were in PF, of which 20 showed H3k27me3 loss comprising of PFA 66.6% and PFB 33.3%. Seventy‐six cases were located in the spinal cord comprising of 33 myxopapillary ependymoma, 37 grade 2 ependymoma and 3 were grade 3 and showed NMYC amplification. None of the myxopapillary and grade 2 ependymoma showed NMYC amplification and all three showed Nmyc immunopositivity. Two of NMYC amplified ependymoma recurred within 6 months of surgery and recurrent tumours were also immunopositive for NMyc and NMYC amplified.
Conclusions: The majority of ST ependymomas show RELA fusion and YAP1 fusion is very rare. Nearly 25% of the cases cannot be molecularly characterised and needs further molecular work up. 2/3rd of PF tumours are PFA and have bad prognosis. NMYC amplified spinal ependymomas are rare and immunostaining is good modality for screening of these patients in resource constraint countries before FISH studies as they are expensive, laborious and not available in all laboratories. There, molecular profiling is important for risk stratification in different anatomical locations.
S24‐NO‐A19
Transcriptomic and epigenetic dissection of spinal ependymomas (SP‐EPN) identifies clinically relevant subtypes enriched for tumors with and without NF2 mutation
S. Neyazi1,2, E. Yamazawa3, K. Hack 1,2, G. Nagae4, C. Kresbach1,2,5,6, T. Umeda4, A. Eckhardt1,2,7, K. Tatsuno4, L. Pohl1,2, T. Hana3, M. Bockmayr1,2,6, P. Kim8, M. M. Dorostkar9,10, T. Takami11, D. Obrecht2, K. Takai12, A. K. Suwala13,14, T. Komori15, S. Godbole16, R. Otani17, A. K. Wefers5,6, F. Higuchi18, J. E. Neumann5,16, Y. Nakanishi19, L. Schweizer20, H. Takami3, C. M. Monoranu21, M. Nomura3,22, L. Engertsberger23, K. Yamada3, V. C. Ruf24, A. Mukasa25, T. Mohme26, S. Takayanag3, J. Herms24, K. Ishii3, M. Mynarek2, H. Imai27, K. Lamszus26, K. Ichimura28, L. Kluwe29, T. Koike3, A. von Deimling13,14, R. Matsuura3, M. Benesch23, Y. Kushihara3, M. Snuderl30, S. Nambu3, S. Frank31, T. Omura3, C. Hagel5, K. Kugasawa3, V. F. Mautner32, S. Rutkowski2, S. Tanaka3, H. Aburatani4, N. Saito3, U. Schüller1,2,5
1Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 2University Medical Center Hamburg‐Eppendorf, Department of Pediatric Hematology and Oncology, Hamburg, Germany; 3The University of Tokyo, Department of Neurosurgery, Tokyo, Japan; 4The University of Tokyo, Genome Science and Medicine Laboratory, Tokyo, Japan; 5University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 6University Medical Center Hamburg‐Eppendorf, Mildred Scheel Cancer Career Center HaTriCS4, Hamburg, Germany; 7University Medical Center Hamburg‐Eppendorf, Laboratory for Radiobiology & Experimental Radiation Oncology, Hamburg, Germany; 8Dokkyo Medical University, Department of Neurosurgery, Mibu, Japan; 9Ludwig‐Maximilians‐University, Center for Neuropathology, Munich, Germany; 10German Center for Neurodegenerative Diseases (DZNE), Munich, Germany; 11Osaka Medical and Pharmaceutical University, Department of Neurosurgery, Takatsuki, Japan; 12Tokyo Metropolitan Neurological Hospital, Department of Neurosurgery, Fuchu, Japan; 13University of Heidelberg, Department of Neuropathology, Heidelberg, Germany; 14German Cancer Research Center (DKFZ), Clinical Cooperation Unit Neuropathology, Heidelberg, Germany; 15Tokyo Metropolitan Neurological Hospital, Department of Laboratory Medicine and Pathology, Fuchu, Japan; 16University Medical Center Hamburg‐Eppendorf, Center for Molecular Neurobiology Hamburg, Hamburg, Germany; 17Tokyo Metropolitan Komagome Hospital, Department of Neurosurgery, Tokyo, Japan; 18Teikyo University School of Medicine, Department of Neurosurgery, Tokyo, Japan; 19Osaka City University Graduate School of Medicine, Department of Neurosurgery, Osaka, Japan; 20Charité—Universitätsmedizin Berlin, Institute for Neuropathology, Berlin, Germany; 21University of Würzburg, Department of Neuropathology, Wuerzburg, Germany; 22Harvard Medical School, Massachusetts General Hospital, Boston, MA, United States; 23Medical University of Graz, Division of Pediatric Hematology and Oncology, Graz, Austria; 24LMU Munich, Center for Neuropathology and Prion Research, Munich, Germany; 25Graduate School of Medical Sciences Kumamoto University, Department of Neurosurgery, Kumamoto, Japan; 26University Medical Center Hamburg‐Eppendorf, Department of Neurosurgery, Hamburg, Germany; 27Japan Community Health care Organization Tokyo Shinjuku Medical Center, Department of Neurosurgery, Tokyo, Japan; 28Juntendo University Graduate School of Medicine, Department of Brain Disease Translational Research, Tokyo, Japan; 29University Medical Center Hamburg‐Eppendorf, Department of Oral and Maxillofacial Surgery, Hamburg, Germany; 30NYU Langone Health, Department of Pathology, New York, NY, United States; 31University Hospital Basel, Division of Neuropathology, Basel, Switzerland; 32University Medical Center Hamburg‐Eppendorf, Department of Neurology, Hamburg, Germany
Introduction: Molecularly defined spinal ependymomas (SP‐EPN) are the most common intramedullary tumors in children and adults and are well distinguishable from myxopapillary or MYCN‐amplified ependymoma. Although loss of chromosome arm 22q and mutations in the NF2 gene have been identified as recurrent genetic alterations, additional drivers as well as intertumoral heterogeneity regarding molecular features and clinical outcome remain unclear.
Objectives: We aimed for an integrative analysis of SP‐EPN at the epigenetic, genetic and transcriptomic level and correlated respective findings with clinical follow‐up.
Patients and Methods: We assembled a multi‐institutional cohort of 234 SP‐EPN and integrated clinical data with epigenetic (n = 234), genomic (n = 140), and transcriptomic (n = 76) analyses.
Results: We found that SP‐EPN occur at all ages, are mostly located in the cervical spinal cord, and harbor NF2 mutations in almost 50% of the cases, with at least 16% in the context of Neurofibromatosis type 2. We identified two distinct molecular subtypes of SP‐EPN by consensus clustering of bulk transcriptomic data and confirmed them at the epigenetic level by integrated analysis of an extended cohort. Subtype 1 comprised mostly cases with NF2 wild type sequences and contained significantly more copy number alterations. In contrast, subtype 2 predominantly included cases with germline or somatic NF2 mutations. Also, patients with tumors of subtype 2 showed a significantly worse progression‐free survival and included all cases with disease progression, although they more often underwent post‐operative radiation therapy.
Conclusion: Our study provides a characterization of SP‐EPN in a large cohort and identifies two molecular subtypes. The higher rate of tumor progression in subtype 2 indicates a more aggressive clinical behavior of these tumors and implies clinical relevance.
S24‐NO‐A20
Epigenetically defined angiocentric gliomas may lack angiocentric growth and instead show a variety of growth patterns
L. Stegat1,2, J. L. Rohwer1,2, D. Stichel3,4, D. Schrimpf3,4, R. Coras5, M. Pagès6,7,8, A. Tauziède‐Espariat6, P. Varlet6, V. H. Hans9,10, J. Meyer3,4, J. Schittenhelm11, O. Staszewski12, E. Cheesman13, M. Glatzel1, S. Schmid14,15, P. Wesseling16,17, A. Korshunov3,4, A. Sexton‐Oates18,19, U. Schüller1,2, L. T. Kõrgvee20,21, S. Mueller22,23, A. Olar24, M. Snuderl25, L. Schweizer14,15,26,27,28, E. Aronica29,30, F. Sahm3,4,31, A. von Deimling3,4, I. Blümcke5, D. T. W. Jones31,32, D. Capper14,15, A. K. Wefers 1,33
1Institute of Neuropathology, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 2Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 3University Hospital Heidelberg, Department of Neuropathology, Institute of Pathology, Heidelberg, Germany; 4Clinical Cooperation Unit Neuropathology, German Cancer Consortium (DKTK), German Cancer Research Center (DKFZ), Heidelberg, Germany; 5University Hospital Erlangen, Department of Neuropathology, Erlangen, Germany; 6Department of Neuropathology, Sainte‐Anne Hospital, Descartes University, Paris, France; 7Department of Genetics, Institut Curie, Paris, France; 8SIREDO Paediatric Cancer Center, Institut Curie, Paris, France; 9Dietrich‐Bonhoeffer‐Klinikum, Abteilung Neuropathologie, Institut für klinische Pathologie, Neubrandenburg, Germany; 10Institut für Neuropathologie, Evangelisches Klinikum Bethel gGmbH, Bielefeld, Germany; 11University Hospital of Tübingen, Department of Neuropathology, Institute of Pathology and Neuropathology, Tuebingen, Germany; 12University of Freiburg, Institute of Neuropathology, Faculty of Medicine, Freiburg i. Br., Germany; 13Royal Manchester Children's Hospital Manchester, Department of Paediatric Histopathology, Manchester, United Kingdom; 14Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Berlin, Germany; 15German Cancer Consortium (DKTK), Partner Site Berlin, German Cancer Research Center (DKFZ), Heidelberg, Germany; 16Princess Máxima Center for Pediatric Oncology, Utrecht, Netherlands; 17Amsterdam University Medical Centers/VUmc, Department of Pathology, Amsterdam, Netherlands; 18Cancer and Disease Epigenetics, Murdoch Children's Research Institute, Melbourne, Australia; 19Rare Cancers Genomics Team (RCG), Genomic Epidemiology Branch (GEM), International Agency for Research on Cancer/World Health Organisation (IARC/WHO), Lyon, France; 20Department of Pharmacology, Institute of Biomedicine and Translational Medicine, University of Tartu, Tartu, Estonia; 21Haematology and Oncology Clinic, Tartu University Hospital, Tartu, Estonia; 22Department of Oncology and Children's Research Center, University Children's Hospital of Zurich, Zurich, Switzerland; 23University of California, Department of Neurology, Neurosurgery and Pediatrics, San Francisco, CA, United States; 24NOMIX Laboratories, Denver, CO, United States; 25New York University, Langone Health, Department of Pathology, New York, NY, United States; 26German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Frankfurt a. M., Germany; 27Edinger Institute, Institute of Neurology, University of Frankfurt am Main, Frankfurt a. M., Germany; 28Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 29Amsterdam UMC, University of Amsterdam, Amsterdam Neuroscience, Department of (Neuro) Pathology, Amsterdam, Netherlands; 30Stichting Epilepsie Instellingen Nederland, Heemstede, Netherlands; 31Hopp Children's Cancer Center Heidelberg (KiTZ), Heidelberg, Germany; 32Pediatric Glioma Research Group, German Cancer Research Center (DKFZ), Heidelberg, Germany; 33Mildred Scheel Cancer Career Center HaTriCS4, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany
Introduction: Angiocentric glioma (AG) mainly occurs in children and is associated with a good prognosis. Molecularly, most AG have a MYB‐QKI fusion. Histologically, AG are defined by an angiocentric growth of the tumor cells. However, we noticed that epigenetically defined AG often get different histological diagnoses as they may lack this angiocentric growth pattern.
Objectives: (1) Analyze gene fusions in epigenetically defined AG to confirm the molecular diagnosis. (2) Analyze how reliable epigenetically defined AG are histologically diagnosed based on the WHO criteria.
Materials and Methods: We collected 48 epigenetically defined AG (37 supra‐, 11 infratentorial; 46 patients) for histological and molecular analyses (DNA methylation; RNA‐Seq). AG were classified using cluster analyses and the brain tumor classifier (molecularneuropathology.org).
Results: AG were epigenetically distinct from other gliomas including the diffuse astrocytomas, MYB(L1)‐altered. A MYB‐QKI fusion was detected in 69% (n = 18/26) of AG, confirming the diagnosis. Others had fusions of MYB with intergenic sites, mainly close to QKI (19%; n = 5/26), and MYBL1‐QKI (8%; n = 2/26). Histologically, 75% showed an angiocentric growth, however, often not very pronounced. Many AG displayed an unspecific growth pattern or resembled pilocytic astrocytoma or ependymoma. Hence, about 59% of AG were initially misdiagnosed without molecular analyses (supratentorial 50%, infratentorial 100%). We got similar results expanding the cohort with further epigenetically defined AG (total 68 AG, 65 patients; 50 supra‐, 12 infratentorial, 6 NA; no tissue for a histological re‐evaluation available). In the expanded cohort, 54% of cases were initially misdiagnosed (supratentorial 45%, infratentorial 100%).
Conclusion: AG often lack the typical angiocentric growth pattern, resulting in different diagnoses in >50% of the cases without molecular analyses. Thus, DNA methylation analyses are needed for a reliable diagnosis.
S24‐NO‐A21
High‐grade gliomas occurring in teenagers and young adult patients comprise novel molecular subgroups
M. Clarke 1, R. Pereira1, A. Mackay1, Y. Grabovska1, A. Clarke2, J. Nicoll2, J. Procter3, A. Moore4, J. Schagen4, L. Walker5, F. Roncaroli5, O. Ogunbigi6, T. Jacques6, L. Marshall7, F. Carceller7, Z. Reisz8, S. Al‐Sarraj8, M. Vinci9, K. Kurian10, H. K. Ng11, S. Brandner12, C. Jones1
1Institute of Cancer Research, London, United Kingdom; 2BRAIN UK, Southampton, United Kingdom; 3Royal Preston Hospital, Preston, United Kingdom; 4Queensland Children's Tumour Bank, Brisbane, Australia; 5Northern Care Alliance NHS Foundation Trust, Manchester, United Kingdom; 6Great Ormond Street Hospital for Children NHS Foundation Trust, London, United Kingdom; 7The Royal Marsden NHS Foundation Trust, London, United Kingdom; 8King's College Hospital NHS Foundation Trust, London, United Kingdom; 9Ospedale Pediatrico Bambino Gesù, Rome, Italy; 10Southmead Hospital, North Bristol NHS Trust, Bristol, United Kingdom; 11The Chinese University of Hong Kong, Ma Liu Shui, Hong Kong; 12University College London Hospitals NHS Foundation Trust, Neuropathology, London, United Kingdom
Question: High‐grade gliomas (HGG) in teenagers and young adults (TYA) are understudied; this project aimed to characterise these tumours and identify potential therapeutic targets.
Methods: HGG samples (n = 195, FFPE/FF, 13–30 years) underwent DNA methylation profiling (Illumina EPIC BeadArrays, brain tumour classifier (MNP v12.5 R package), n = 195), classifying cases against a reference cohort. Calibrated scores guided workflows (ArcherDx fusion panel (n = 112), whole exome sequencing (n = 84), histological review). Well‐characterised entities (n = 50, IDH‐mutant (n = 18), PXA (n = 12)) were excluded.
Results: Of cases scoring >0.6, 64% classified as paediatric‐type subgroups (pedHGG_RTK1A/B/C (30%), pedHGG_MYCN (10%), pedHGG_A/B (7%), pedHGG_RTK2A (6%)). 29% classified as subgroups frequently seen in adults (GBM_MES (12%), GBM_RTK1/2 (3%)). 54% classified with a score <0.6. 38% cases were assigned to novel, recently identified subgroups with distinct methylation profiles/molecular features (HGG_B, HGG_E, ANTCON, GBM_CBM). Frequency comparisons to publicly available methylation data showed GBM_MES_ATYP are TYA age‐specific, in contrast to adult age‐specific GBM_MES_TYP. Copy number profiling identified frequent changes (chromosomal gains (chr1q (54%), chr2 (22%), chr7 (41%)) and losses (chr10 (40%), chr13 (64%))). Focal amplifications included PDGFRA (12%), CDK4 (7%), MYCN/ID2 (3%), MYC (2%) and EGFR (0.7%). Most common focal deletion was CDKN2A/p16 (12%). Most frequent glioma‐associated somatic variants included TP53, PDGFRA, EGFR, NF1. BCOR alterations were enriched compared to adult and paediatric reference cohorts. Ten percent cases showed a hypermutator phenotype, enriched in HGG‐E. CDK4 amplifications were recurrent in GBM_RTK1 and GBM_CBM. Histology showed variable cytological/architectural features within novel subgroups.
Conclusion: TYA HGG comprise novel subgroups with distinct methylation profiles and molecular characteristics, representing opportunities to refine treatment.
S18‐NO‐A22
Which meningiomas benefit most from methylation profiling?
F. Ruiz 1, A. Lowe2, L. D'Antona3, M. Dutt1, P. Mariathasan1, A. Merve1, Z. Jaunmuktane1,4, F. Sahm5,6, S. Brandner1,2
1University College London. Institute of Neurology, Neuropathology, London, United Kingdom; 2University College London. Institute of Neurology, Neurodegenerative Disease, London, United Kingdom; 3National Hospital for Neurology and Neurosurgery. University College Hospitals. NHS Foundation Trust, Neurosurgery, London, United Kingdom; 4University College London. Institute of Neurology, Clinical and Movement Neurosciences, London, United Kingdom; 5Institute of Pathology, University Hospital Heidelberg, Neuropathology, Heidelberg, Germany; 6Clinical Cooperation Unit Neuropathology, German Cancer Consortium (DKTK), German Cancer Research Center (DKFZ), Heidelberg, Germany
Introduction: Methylation profiling combined with copy number assay provide a better prognostication than WHO grade alone. Profiling all meningiomas is financially unsustainable in most centres, therefore pathologists and clinicians ask for guidance which meningiomas to analyse.
Objectives: To analyse how the WHO grade resolves into methylation classes and risk strata, to provide guidance which meningiomas to profile.
Methods: From 2018 to 2023 a subset of meningiomas diagnosed within our institution, and all referred meningiomas underwent methylation profiling with copy number assay. Using the classifier 12.6 we determined how the 3 CNS WHO grades (in short G1, G2, G3), resolve into the methylation classes (MC) benign, intermediate, or malignant, or the risk strata low, intermediate, and high [PMID 36377252, 34618539].
Results: Of 1408 locally diagnosed meningiomas, 309 (22%) underwent profiling and 393 meningiomas were referred. Of these 702 meningiomas, 545 had a calibrated score of >0.90. Of 253 G1 meningiomas 231 (91%) allocated to MC benign, and 22 (9%) into MC intermediate. Instead, of the 214 G2 meningiomas, 124 (58%) allocated to MC benign, 77 (36%) to MC intermediate and 13 (6%) into MC malignant. The 17 G3 meningiomas distributed approximately equally into the 3 MC's. Similarly, when analysing the allocation to integrated risk scores, of the 214 G2 meningiomas, 71 (33%) were low, 106 (50%) intermediate, and 37 (17%) high risk. None of the 16 G3 meningiomas had a low risk score, while 5 had an intermediate, and 11 a high risk score. When stratifying G2 meningiomas by grading criterium (brain invasion, mitotic count, histological type) there was a similar risk score distribution across the three criteria.
Conclusion: G2 meningiomas show the most notable discrepancy between grade and methylation class or risk score, and thus should preferentially undergo methylation profiling. Instead, most G1 meningiomas have a low, and most G3 meningiomas a high risk score.
S18‐NO‐A23
Assessment of molecular biomarkers for prognostication in meningiomas
J. Singh 1, V. Suri1, M. C. Sharma1, A. Suri2
1All India Institute of Medical Sciences, Neuropathology, New Delhi, India; 2All India Institute of Medical Sciences, Neurosurgery, New Delhi, India
Introduction: Meningioma is the most common primary neoplasm of the central nervous system in adults. Although majority are WHO grade 1 with indolent behaviour but 10%–15% of low grade meningiomas behave aggressively and recur. WHO CNS5 classification has introduced prognostic biomarkers pTERT mutation and CDKN2A/B homozygous deletion as independent biomarkers for anaplastic meningiomas. Loss of H3K27me3 expression has shown to be associated with poor prognosis. p16 is considered as a surrogate marker for CDKN2A/B deletion.
Objective: To assess the frequency and clinical utility of pTERT mutation, CDKN2A Homozygous deletion, H3K27me3 and p16 expression in meningiomas.
Material and Methods: 208 (97 males and 111 females) cases of grade 1 (n = 109), 2 (n = 83), and 3 (n = 16) meningiomas were included in this study (2012–2022). All cases were assessed for pTERT mutation (C228T/C250T) using sanger sequencing, CDKN2A homozygous deletion by FISH, loss of H3K27me3 and p16 expression by IHC.
Results: This was an ambispective study comprising 199 adult and 9 paediatric cases (Mean age 44.5 years). Majority of the meningiomas were basal (53%), followed by convexity (42%) and other locations (5%). pTERT C228T mutation was observed in 4.8%(10/208) and CDKN2A deletion in 2.4%(5/208) meningiomas. On histology, all pTERT mutant cases were grade 2 while 80% CDKN2A deleted cases were grade 3. There was no correlation of p16 loss with CDKN2A deletion. Substantial proportion of cases in all three grades showed loss of H3K27me3 expression. Overall survival (OS) was poor in patients harbouring these molecular alterations. However, mean OS in pTERT mutant cases was significantly poor compared to wild type (31 vs. 56 months, p < 0.005).
Conclusion: Integrated diagnostic approach provides improved accuracy in predicting outcome and recurrence in grade 2 meningiomas. pTERT mutation is the most significant and economical marker for risk stratification in meningiomas in resource constrained setting.

FIGURE 1.
S18‐NO‐A24
Mitotic count and tumor grading conundrum
M. Haeri 1, H. Gu2, I. Al‐Kharouf1, X. Chen2, N. Lakis1, N. Zarrin‐Khameh3, C. Williams4, S. Magaki4, X. Zhang5, N. Khanlou4, I. Cobos6, H. Vinters4
1University of Kansas Medical Center, Pathology and Laboratory Medicine, Kansas City, MO, United States; 2University of California, Los Angeles, Electrical and Computer Engineering, Los Angeles, CA, United States; 3Baylor College of Medicine, Pathology and Immunology, Houston, TX, United States; 4UCLA David Geffen School of Medicine, Pathology and Laboratory Medicine, Los Angeles, CA, United States; 5McGovern Medical School, Pathology and Laboratory Medicine, Houston, TX, United States; 6Stanford University, Pathology, Stanford, CA, United States
Mitotic count is a key criterion in grading many brain tumors such as meningioma, IDH‐mutant astrocytoma, oligodendroglioma, solitary fibrous tumor and ependymoma among others. Accurate mitosis detection and quantification is time‐consuming, requires training and can be challenging in large and heterogeneous specimens with few highly proliferative foci that can be missed easily. Additionally, mitotic counts can assist with ruling in/out some tumors. For instance, a subependymoma with few mitoses may prompt more careful examination for the possibility of an ependymoma–subependymoma. As a starting point, we employed an artificial intelligence (AI) model (EfficientNet‐b3) to detect mitotic figures in meningiomas by analyzing histologic images. We compared AI sensitivity and precision in mitosis detection with humans by performing a survey with participation of 40 neuropathologists, pathologists, and trainees. The participants labeled mitoses in 48 high‐power‐field images selected from H&E‐stained meningothelial meningiomas. Each image contained 0–6 mitoses. The mitotic figures were verified by immunostaining (PHH3) and confirmed by a neuropathologist. Interestingly, we found that F1 score (i.e., the harmonic mean of the sensitivity and precision) of AI is comparable to those of top participants in mitosis detection and can outperform the majority in sensitivity. The higher F1 score was achieved by the AI model since it maintained a high precision and sensitivity simultaneously, while human participants could not usually achieve both. Based on this result, we hypothesize that an AI‐pathologist collaboration can achieve a higher sensitivity and precision than that of either AI or human alone. In this approach, the AI detects mitoses with the highest sensitivity, followed by pathologists overseeing AI recommendations to achieve the highest precision. Such a collaborative approach can also potentially improve pathologists' consistency and is beneficial in borderline cases.
S18‐NO‐A25
Meningeal solitary fibrous tumor—A genome‐wide DNA methylation study
K. Eschbacher 1, Q. Tran2, S. Jenkins3, K. Fritchie4, E. Moskalev5, R. Stoehr5, A. Caron3, P. Brown3, A. Guajardo6, D. Brat7, A. Wu8, S. Santagata9, D. Louis10, P. Brastianos10, A. Kaplan10, B. Alexander11, S. Rossi12, F. Ferrarese12, D. Raleigh8, M. Nguyen8, J. Gross6, J. Velazquez Vega13, F. Rodriguez14, A. Perry8, M. Martinez‐Lage10, B. Orr2, F. Haller5, C. Giannini3
1University of Iowa Hospitals and Clinics, Pathology, Iowa City, IA, United States; 2St. Jude Children's Research Hospital, Memphis, TN, United States; 3Mayo Clinic, Rochester, MN, United States; 4Cleveland Clinic, Cleveland, OH, United States; 5University Hospital Erlangen, Institute of Pathology, Erlangen, Germany; 6Johns Hopkins University School of Medicine, Baltimore, MD, United States; 7Northwestern University Feinberg School of Medicine, Chicago, IL, United States; 8University of California San Francisco, San Francisco, CA, United States; 9Brigham and Women's Hospital, Boston, MA, United States; 10Massachusetts General Hospital, Boston, MA, United States; 11Dana‐Farber Cancer Institute, Boston, MA, United States; 12Ospedale Ca'Foncello, Treviso, Italy; 13Children's Healthcare of Atlanta, Atlanta, GA, United States; 14University of California, Los Angeles, CA, United States
Introduction: Meningeal solitary fibrous tumor (SFT), characterized by the presence of NAB2::STAT6 fusion, is a rare tumor occurring in adults associated with frequent recurrence and risk of metastasis. In a cohort of 126 SFT patients we recently found that 2021 CNS WHO grade was significantly associated with risk of metastasis (p = 0.005), whereas NAB2::STAT6 fusion type (n = 101), was associated with disease specific survival (p = 0.014). TERT promoter mutation was present in 11 (of 99; 11.2%) patients.
Objectives: To further characterize the subgroups of our meningeal solitary fibrous tumor cohort utilizing genome‐wide DNA methylation screening.
Patients and Methods: Genomic DNA (Illumina Infinium MethylationEPIC v1.0/Illumina USA) was successfully performed in 80 cases (37 F, 43 M; mean age 53.2 years).
Results: Three distinct clusters were identified: cluster 1 (n = 38), cluster 2 (n = 22), and cluster 3 (n = 20). Methylation clusters were significantly associated with fusion type (p < 0.001), with cluster 2 having ex4::ex2‐3 fusion in 16 (of 20; 80.0%), nearly all TERT promoter mutations (7 of 8; 87.5%), and showing predominantly an “SFT” histologic phenotype (15 of 22; 68.2%). Clusters 1 and 3 were less distinct, both dominated by tumors having ex5‐7::ex16‐17 fusion (respectively 25 of 33; 75.8%, and 12 of 18; 66.7%) and with variable histological phenotypes, respectively “SFT” (n = 7, 18.4%; n = 9; 45.0%), “HPC‐like” (n = 12, 31.6%; n = 4, 20.0%), or intermediate (n = 19, 50.0%; n = 7, 35.0%). Methylation clusters were significantly associated with metastasis‐free survival (10‐year estimates: 67.0%, 94.7%, 25.0% for clusters 1, 2, and 3, respectively; p = 0.0134), but not overall survival, recurrence‐free survival, or progression‐free survival.
Conclusion: Meningeal SFT encompasses three distinct methylation clusters, which are significantly associated with fusion type, TERT promoter mutation status, histologic phenotype, and metastasis‐free survival.
S18‐NO‐A26
Intracranial mesenchymal tumor with FET‐CREB fusion—A rare entity
M. H. Phom 1, M. C. Sharma1, S. Das1, V. Suri1, S. Borkar1, A. Garg1
1All India Institute of Medical Sciences, Pathology, New Delhi, India
Introduction: Intracranial mesenchymal tumor with FET‐CREB fusion is a heterogeneous group of low grade sarcoma with variable histomorphology and fusion of FET gene (EWSR1, FUS) with CREB family of transcription factor genes (CREB1, ATF1 or CREM). Mostly located in the supratentorial extra‐axial location attached to meninges and dura. Previously named as angiomatoid fibrous histiocytoma/intracranial myxoid mesenchymal tumor.
Objectives: To describe some morphological, immunohistochemical and molecular features.
Patients and Methods: Four cases were diagnosed based on morphology, IHCs and molecular studies.
Results: Age: 17–35 years with equal M:F ratio.Tumors were located in frontal region, infratemporal fossa, sphenoid and nasal cavity. Morphologically all cases had myxoid or collagenized stroma with spindle to ovoid cells and showed variable immunopositive for EMA, CD99, S100 and desmin. MIB1 labelling index was low. FISH in all the cases showed EWSR1 break‐apart signals. Differential diagnoses considered were fibrous meningioma, SFT or metastasis. A combination of immunoposoitivity for EMA, CD99 and desmin along with FISH is very helpful in the diagnosis.
Conclusion: Myxoid tumours with EWSR1 rearrangement in intracranial location are either angiomatoid fibrous histiocytoma (myxoid variant) or Intracranial myxoid mesenchymal tumour with FET‐CREB fusion. Whether they represent same entity with various fusion partners or different clinicopathological entities is not entirely known. Morphologically they pose diagnostic challenges with variable IHC expression. Targeted sequencing is helpful to reveal the fusion genes. Further studies on large number of cases need to be done to characterize these lesions.
S18‐NO‐A27
Central nervous metastasis—Frequency, location and the role of immunohistochemistry in identifying primary sites
C. Bonacossa da Rocha Neves 1, N. Henriques Silva Canedo1,2, J. M. Gomes da Silva Batista1,2,3
1Federal University of Rio de Janeiro, Pathology, Rio de Janeiro, Brazil; 2Instituto Estadual do Cérebro Paulo Niemeyer—IECPN, Pathology, Rio de Janeiro, Brazil; 3Data Science Academy, Rio de Janeiro, Brazil
Introduction: Brain metastatic disease is one of the greatest causes of morbidity and mortality in cancer patients. This study aims to map their most common primary sites, preferred neuroanatomical locations and the most utilized immunomarkers in two institutions from Rio de Janeiro, Brazil.
Methods: One hundred and eighty‐one patient files with metastatic brain cancer diagnosis were analyzed. Age, sex, location of lesions within the central nervous system, multiplicity of lesions, immunomarkers used to reach their diagnosis and, finally, primary site of disease were documented.
Results: Patient's age varied between 32 and 82 years, the fifth and sixth decades being the most affected within this population. The female:male ratio was 1.91:1; 65.75% (n = 119) of cases being women and 34.25% men (n = 62). The most common primary sites were the lung (35.36%; n = 64), followed by breast (17.68%; n = 32) and skin—melanoma (4.97%; n = 9). In 9.94% of cases primary site remained unknown and a further 14.37% were only diagnosed according to their cell lineage. The most common initial immunohistochemical panel included CK7, CK20 and TTF‐1, which were followed by other organ‐specific markers for breast, gastrointestinal and genitourinary tract. Supratentorial locations concentrated 55.91% of all lesions, both intra and extra‐axial, which were equally distributed between the frontal and parietal lobes. This reflects the regions' high blood‐flow and their relative weight within the nervous system.
Conclusion: The fraction of identified primary sites in relation to those which remained unknown was within expected, lying well within the 25%–30% stated by literature that was reviewed for this study. We were also able to confirm the locations with highest frequency for brain metastatic lesions. Aided by morphological analysis, our immunohistochemical panels, although sometimes limited by institutional conditions, allowed the diagnosis in the majority of cases.
S18‐NO‐A28
Brain metastasis is associated with disturbance of cerebral blood microcirculation and consecutive hypoxic‐ischemic pre‐metastatic niches
J. Roesler1, D. Spitzer1, X. Jia1, S. Aasen2, K. Sommer1, B. Roller1, N. Olshausen3, N. Hebach3, M. T. Forster4, J. P. Steinbach5, L. Sevenich6, K. Devraj1, F. Thorsen2, M. A. Karreman3, K. H. Plate1, Y. Reiss1, P. N. Harter 7
1Edinger Institute, Frankfurt a. M., Germany; 2University Bergen, Bergen, Norway; 3German Cancer Research Center (DKFZ), Clinical Cooperation Unit Neurooncology, Heidelberg, Germany; 4Goethe University Hospital, Neurosurgery, Frankfurt a. M., Germany; 5Goethe University Hospital, Neurooncology, Frankfurt a. M., Germany; 6Institute for Tumor Biology and Experimental Therapy, Georg‐Speyer‐Haus, Frankfurt a. M., Germany; 7LMU Munich, Center for Neuropathology, Munich, Germany
Brain metastasis (BM) poses an ever‐increasing challenge in oncology. BM occurs via extravasation of circulating tumor cells across the blood–brain barrier, followed by seeding and colonization of the perivascular niche. Here we propose a seeding‐and‐colonization process which might be inhibited by therapeutic inhibition of hypoxia‐inducible Ang‐2 and VEGF. Xenograft models of BM were established by intracardiac inoculation of melanoma or breast cancer cells. The effect of intravascular arrest of tumor cells on cerebral blood circulation was measured using intravital 2‐photon cranial window microscopy. BM formation was monitored using cranial magnetic resonance imaging and post‐mortem autopsy of immunodeficient mice. BM formation was targeted with anti‐Ang‐2 and anti‐VEGF strategies. Furthermore, angiogenic factors and clinical outcome were analyzed using tissue microarrays of 191 BM patients. We observed blood vessel occlusions by cancer cells, which were accompanied by significant disturbance of cerebral blood microcirculation and histological signs of hypoxia and ischemia in the early pre‐metastatic niche. Blood vessels showed an increase of Ang‐2 expression in BM mice. Ang‐2 expression in brain microvessels within the metastatic niche was observed in humans and in murine BM models. Combined anti‐Ang‐2/anti‐VEGF therapy led to decrease of total number of brain metastases and metastatic tumor volumes. Ang‐2 expression in tumor vessels of established human brain metastasis negatively correlated with patient survival. Cancer cell vessel occlusion followed by disturbance of cerebral blood microcirculation and early signs of hypoxia and ischemia in the pre‐metastatic niche might facilitate BM seeding by upregulation of vascular permeability factors Ang‐2 and VEGF. Combined inhibition of microenvironmental effects of hypoxia‐inducible Ang‐2 and VEGF in a hypoxic and ischemic perivascular metastatic niche may prevent the outgrowth of macrometastases in the brain.
S26‐NO‐A29
Ultra‐fast deep‐learned pediatric CNS tumor classification during surgery
B. Tops 1, C. Vermeuelen2, M. Pages‐Gallego2, L. Kester1, M. Kranendonk1, P. Wesseling1, J. Van der Lugt1, K. Van Baarsen1, E. Hoving1, J. De Ridder2
1Princess Máxima Center for Pediatric Oncology, Utrecht, Netherlands; 2University Medical Center Utrecht, Utrecht, Netherlands
The primary treatment of CNS tumors starts with a neurosurgical resection in order to obtain tumor tissue for diagnosis and to reduce tumor load and mass effect. The neurosurgeon has to decide between radical resection versus a more conservative strategy to prevent surgical morbidity. The prognostic impact of a radical resection varies between tumor types, however due to a lack of pre‐operative tissue‐based diagnostics, limited knowledge of the precise tumor type is available at the time of surgery. Current standard practice includes preoperative imaging and intraoperative histological analysis, but these are not always conclusive. After surgery, histopathological and molecular tests are performed to diagnose the precise tumor type. The results may indicate that an additional surgery is needed or that the initial surgery could have been less radical. Using rapid nanopore sequencing, a sparse methylation profile can be directly obtained during surgery, making it ideally suited to enable intraoperative diagnostics. We developed a state‐of‐the‐art neural‐network approach called Sturgeon, to deliver trained models that are lightweight and universally applicable across patients and sequencing depths. We demonstrate our method to be accurate and fast enough to provide a correct diagnosis with as little as 20–40 min of sequencing data in 42 out of 48 pediatric samples. In four prospective cases we achieved a turnaround time of 60–90 min from sample biopsy to result; well in time to impact surgical decision making. We conclude that machine‐learned diagnosis based on intraoperative sequencing can assist neurosurgical decision making, allowing neurological comorbidity to be avoided or preventing additional surgeries.
S26‐NO‐A30
In vivo confocal laser endomicroscopy of brain tumors—A new era in intraoperative digital diagnostics
A. Wagner 1, M. C. Brielmaier2,1, N. Pensel2, K. Aftahy1, L. Baumgart1, M. Barz1, J. Höhne3, M. Lautenschlager3, K. M. Schebesch3, S. Brehmer4, M. Ratliff4, F. Enders4, F. Liesche‐Starnecker2, B. Meyer1, J. Gempt1,5, J. Schlegel2
1Klinikum rechts der Isar, Technical University Munich, Department of Neurosurgery, Munich, Germany; 2Institute of Pathology, Technical University Munich, Department of Neuropathology, Munich, Germany; 3University Hospital Regensburg, Department of Neurosurgery, Regensburg, Germany; 4University Hospital Mannheim, Department of Neurosurgery, Mannheim, Germany; 5University Hospital Hamburg‐Eppendorf, Department of Neurosurgery, Hamburg, Germany
Confocal laser endomicroscopy (CLE) has been used for many years in other surgical specialities; however, it has only recently been applied to neurosurgical procedures. The confocal technology enables for a cellular level examination of tumor tissue in real time. CLE is the first technology to ever enable an artifact‐free visualization of tumor tissue by imaging tissue in situ. In order to evaluate the efficacy of the diagnostic approach and its value for intraoperative diagnostics, results of in vivo CLE were compared to traditional frozen section diagnostics. The intraoperative recordings were analysed for impairments and image quality. More than 4000 images were obtained with CLE in vivo. During surgery, the staining agent sodium‐fluorescein was applied as a bolus of 3–5 mg/kg bodyweight at the beginning of the surgical procedure. After opening of the meninges, CLE was performed in situ on the surface of the tumor. From the same location, a tissue sample was taken for conventional frozen sections. The intraoperative diagnoses from CLE and frozen sections were later aligned with the final histological diagnosis. The intraoperative CLE recordings showed specific fluorescein distribution depending on the architecture of the tumor entity. Thus, the diagnoses obtained with CLE showed a high accuracy with the final histological diagnoses, similar to the accuracy of the conventional frozen sections. However, the imaging duration for CLE was significantly shorter. In vivo imaging shows a high number of movement artefacts which, however, do not impair the diagnostic possibilities. The specific distribution of SF allows for a reliable discrimination between the different neoplastic entities. The high diagnostic accuracy and the short imaging duration makes confocal laser endomicroscopy a reliable diagnostic instrument with a promising future in the neurosurgical OR. Being less manipulated by artefacts it opens up wide opportunities for neurooncological research.
S26‐NO‐A31
Classification of brain tumors by nanopore sequencing of cell‐free DNA from cerebrospinal fluid
M. Schoof 1,2, A. K. Afflerbach1,2, C. Rohrandt3, B. Brändl4, M. Sönksen2, J. Hench5, S. Frank5, D. Börningen6, M. Alawi6, M. Mynarek2, B. Winkler2, F. Ricklefs7, M. Synowitz8, L. Dührsen7, S. Rutkowski2, A. K. Wefers9,10, F. J. Müller4,11, U. Schüller1,2,9
1Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 2University Medical Center Hamburg‐Eppendorf, Department of Pediatric Hematology and Oncology, Hamburg, Germany; 3University of Applied Sciences Kiel, 3Institute for Communications Technologies and Embedded Systems, Kiel, Germany; 4University Hospital Schleswig‐Holstein, Center for Integrative Psychiatry, Kiel, Germany; 5University Hospital Basel, Department of Pathology, Basel, Switzerland; 6University Medical Center Hamburg‐Eppendorf, Bioinformatics Core, Hamburg, Germany; 7University Medical Center Hamburg‐Eppendorf, Department of Neurosurgery, Hamburg, Germany; 8University Hospital Schleswig‐Holstein, Department of Neurosurgery, Kiel, Germany; 9University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 10University Medical Center Hamburg‐Eppendorf, Mildred Scheel Cancer Career Center HaTriCS4, Hamburg, Germany; 11Max Planck Institute for Molecular Genetics Berlin, Department of Genome Regulation, Berlin, Germany
Introduction: CNS tumors are very heterogeneous and over 100 different entities are known today. For treatment, the exact diagnosis of type and subtype of the tumor is key. The diagnosis relies on histological characteristics as well as molecular features of the tumor and is dependent on the analysis of tissue from the tumor. Tissue collection implies several risks associated with anesthesia and neurosurgery, especially for lesions in the brain stem or other difficult‐to‐reach anatomical sites or in case of small lesions, for example, at relapse. Moreover, molecular confirmation of relapse in suspicious imaging, and the possible detection of specific “druggable” genetic alterations today requires a biopsy.
Objectives: Here, we employ a novel method to identify CNS tumors by nanopore sequencing of cell‐free DNA (cfDNA) from cerebrospinal fluid (CSF) to overcome challenges associated with the need of biopsy material.
Patients and Methods: We employed nanopore sequencing on 129 CSF samples from a cohort of 23 entities, including malignant and benign tumors from 99 patients and analyzed copy number variation (CNV) plots and global DNA methylation, using a published random forest classifier (NanoDx). Results from sequencing analysis were compared to clinical diagnosis and methylation analysis of tumor tissue, if available.
Results: We unambiguously classified 50/129 analyzed samples (38.8%). CNV plots showed diagnostic and prognostic alterations, such as C19MC amplifications in ETMR or Chr.1q gains and Chr.6q losses in PF‐A ependymoma, respectively. Methylation analysis also correctly classified tumors without CNVs. cfDNA originating from the tumor was detected in samples taken from patients with progressive disease, but also in patients without known residual disease.
Conclusions: Our results suggest that nanopore sequencing data of cfDNA from CSF samples may be a promising approach for initial brain tumor diagnostics and an important tool for disease monitoring.
S15‐NO‐A32
Integrated multiomic analyses of medulloblastoma using bulk proteome and DNA‐methylome data reveals subtype‐specific targetable alterations
S. Godbole 1, H. Voß2, S. Schlumbohm3, Y. Schumann3, B. Peng2, M. Mynarek4,5, S. Rutkowski4, M. Dottermusch1,6, M. M. Dorostkar7,8, A. Korshunov9,10, T. Mair2, S. M. Pfister11,12,13, P. Neumann3, C. Hartmann14, J. Weis15, F. L. Starnecker16, Y. Guan2, H. Schlüter2, U. Schüller6,17,5, C. Krisp2, J. E. Neumann1,17
1Center for Molecular Neurobiology (ZMNH), Eppendorf, Hamburg, Germany; 2Section of Mass Spectrometric Proteomics, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 3Chair for High Performance Computing, Helmut Schmidt University, Hamburg, Germany; 4Mildred Scheel Cancer Career Center HaTriCS4, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 5University Medical Center Hamburg‐Eppendorf, Department of Pediatric Hematoloy and Oncology, Hamburg, Germany; 6Institute of Neuropathology, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 7Ludwig‐Maximilians‐University, Center for Neuropathology, Munich, Germany; 8German Center for Neurodegenerative Diseases (DZNE), Munich, Germany; 9University Hospital Heidelberg, Department of Neuropathology, Heidelberg, Germany; 10Clinical Cooperation Unit Neuropathology, German Cancer Consortium (DKTK), German Cancer Research Center (DKFZ), Heidelberg, Germany; 11Heidelberg University Hospital, Department of Pediatric Hematology and Oncology, Heidelberg, Germany; 12Hopp Children's Cancer Center Heidelberg (KiTZ), Heidelberg, Germany; 13Division of Pediatric Neurooncology, German Cancer Consortium (DKTK), German Cancer Research Center (DKFZ), Heidelberg, Germany; 14Hannover Medical School (MHH), Department of Neuropathology, Hannover, Germany; 15RWTH Aachen University Hospital, Institute of Neuropathology, Aachen, Germany; 16Institute of Pathology and Molecular Diagnostics, University Medical Center Augsburg, Augsburg, Germany; 17Research Institute Children's Cancer Center Hamburg, Hamburg, Germany
Introduction: Medulloblastomas (MBs) are heterogeneous malignant pediatric brain tumors. Epigenomic and transcriptomic analyses have advanced the understanding of these tumors and defined four main molecular subgroups‐comprising of several subtypes‐namely, WNT‐activated, Sonic hedgehog (SHH)‐activated, Group3 and Group4 MBs.
Objective: Despite several advances, the pathogenesis of MB is poorly understood for many subtypes and there is a lack of targeted therapies. Contrary to nucleic acids, proteins (and their modifications) closely reflect the phenotype and hold the potential to uncover functional alterations and new therapy targets.
Materials and Methods: Isobaric label (TMT) based protein quantification of FFPE MB tumors was performed using mass spectrometry. Data were harmonized with published MB proteome datasets to establish a cohort of 167 samples. Eighteen samples were subjected to N‐glycan profiling. Epigenetic data was obtained with the Infinium BeadChip array (EPIC). Data modalities and clinical parameters were integrated.
Results and Conclusion: We found six proteome MB subtypes‐also reflected at the N‐glycan level, which were assigned to two main molecular signatures: transcriptional/translational or synaptic/immunological profile. Integration of proteome and DNA methylome data revealed that WNT MBs showed the highest correlation between the two omic‐data among MB subtypes, indicating a higher conservation of biological processes compared to other proteome subtypes. We further identified a proteomic subtype with MYC signature(pG3myc) that showed poor survival and accumulation of high‐risk features like anaplastic histology, epigenetic subtype II, and MYC amplification. pG3myc showed different protein abundancies of the vincristine resistance associated TriC/CCT complex, and we identified palmdelphin (PALMD) as a suitable biomarker. Our results shed light on new targetable alterations in MB and set foundation for potential immunotherapies targeting glycan structures.

FIGURE 1.

FIGURE 2.
S15‐NO‐A33
Spatial multiome mapping of therapy‐induced, pathological changes in glioblastoma at single‐cell resolution
M. Vanmechelen1,2, P. Nazari1,2, J. Beckervordersandforth3, A. Antoranz1,2, W. Moors3, D. Leunissen3, M. Verduin4, L. Hoosemans3, J. Messiaen1,2, E. Geens3, D. B. P. Eekers4, A. Claeys1,2, M. Derweduwe1,2, A. Zur Hausen3, F. Bosisio2,5, F. Weyns6, T. Daenekindt6, P. Van Eycken7, M. Govers8, K. Hovinga2, S. De Vleeschouwer9, P. Clement10, M. P. G. Broen11, M. A. G. Vooijs4, R. Sciot5, J. Pey12, A. Hoeben13, E. J. M. Speel3,13, F. De Smet 1,2
P. Nazari, J. Beckervordersandforth, J. Pey, A. Hoeben, and F. De Smet contributed equally to this study.
1KU Leuven, The laboratory for precision cancer medicine, Translational Cell and Tissue Research Unit, Department of imaging and pathology, Leuven, Belgium; 2KU Leuven, The Leuven Institute for Single‐cell Omics (LISCO), Leuven, Belgium; 3Maastricht University Medical Center, Department of Pathology, Maastricht, Netherlands; 4Maastricht University Medical Center, Department of Radiation Oncology (Maastro), GROW School for Oncology and Reproduction, Maastricht, Netherlands; 5KU Leuven, Translational Cell and Tissue Research Unit, Department of imaging and pathology, Leuven, Belgium; 6Ziekenhuizen Oost Limburg (ZOL), Department of Neurosurgery, Genk, Belgium; 7Ziekenhuizen Oost Limburg (ZOL), Department of Pathology, Genk, Belgium; 8Ziekenhuizen Oost Limburg (ZOL), Department of Oncology, Genk, Belgium; 9University Hospitals Leuven, Department of Neurosurgery, Leuven, Belgium; 10University Hospitals Leuven, Department of Oncology, Leuven, Belgium; 11Maastricht University Medical Center, Department of Neurology, Maastricht, Netherlands; 12Intelligent Biodata, San Sebastián, Spain; 13Maastricht University Medical Center, Department of Medical Oncology, GROW School for Oncology and Reproduction, Maastricht, Netherlands
Glioblastoma (GBM) remains a highly malignant, intrinsically resistant and inevitably recurring brain tumor with dismal prognosis. The aggressiveness and lack of effective GBM treatments can be attributed to the highly heterogeneous and plastic nature of GBM tumor cells, which easily confer resistance to standard‐of‐care (SOC) therapy. While tumor progression has also been attributed to interactions with the tumor microenvironment, quantitative data describing these interactions are still largely missing. Here, we used an multiome approach combining high‐dimensional, multiplexed immunohistochemistry and spatial transcriptomics to map evolutions in the spatial, single‐cell tissue architecture of 100 paired adult GBM tumor samples derived from 50 patients at diagnosis (ND) and upon recurrence (REC) following SOC treatment. We mapped the spatial distribution of a multitude of GBM tumoral subtypes across this multicentric cohort, through which we identified a high level of heterogeneity defined by specific tumoral niches within and across patients and which evolved when subjected to SOC therapy. In addition, we describe the relationship of the various tumoral niches with their local immune‐infiltrates, highlighting an even more immunosuppressive environment following SOC resistance. Finally, by aligning these findings to the observed genomic aberrations and the clinical data of the patients, we are now able to more precisely describe the heterogeneous landscape of glioblastoma and how it evolves under SOC treatment at spatial, single‐cell resolution.
S15‐NO‐A34
Diffuse glioma multiomics—Epigenetic and proteomic analyses for tumor characterization and biomarker detection
K. J. Weber 1,2,3,4, J. Enßle5, I. Divé2,3,4,6, T. I. Hartung1, A. Di Fonzo5, B. Häupl2,3,5, M. Ronellenfitsch2,3,4,6, K. Wenger7, M. Czabanka8, K. H. Plate1,2,3,4, J. P. Steinbach2,3,6, F. Buettner2,3,9, T. Oellerich2,3,5, P. N. Harter1,2,10,11
1University Hospital Frankfurt, Neurological Institute (Edinger Institute), Frankfurt a. M., Germany; 2German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Heidelberg, Germany; 3Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 4University Cancer Center (UCT), Frankfurt a. M., Germany; 5University Hospital Frankfurt, Department of Medicine II, Hematology/Oncology, Frankfurt a. M., Germany; 6Goethe University Frankfurt, Dr. Senckenberg Institute of Neurooncology, Frankfurt a. M., Germany; 7University Hospital Frankfurt, Institute of Neuroradiology, Frankfurt a. M., Germany; 8University Hospital Frankfurt, Department of Neurosurgery, Frankfurt a. M., Germany; 9University Hospital Frankfurt, Department of Medicine, Frankfurt a. M., Germany; 10Ludwig‐Maximilians‐University, Center for Neuropathology, Munich, Germany; 11German Cancer Consortium (DKTK), Partner Site Munich, German Cancer Research Center (DKFZ), Heidelberg, Germany
Introduction: Diffuse gliomas are the most frequent primary malignant brain tumors in adults and are reliably classified by DNA methylation profiling. DNA methylation‐based tumor deconvolution in non‐CNS cancer was further shown to predict therapy response. While proteome analyses contributed greatly to the understanding of tumor biology including metabolism and malignant progression, their translation into clinical actionable targets and biomarkers for disease course and prognosis remains challenging.
Objective: We set out to combine DNA methylation patterns with proteome data for an advanced characterization of diffuse glioma subtypes and biomarker detection.
Patients and Methods: We deployed reference‐free and ‐based tumor deconvolution techniques to large scale DNA methylation data of 450 diffuse gliomas. One hundred and thirty matched samples were subjected to proteome analysis. Latent factors were called separately as well as integratively for the data sets.
Results: We discovered cluster allocation of samples according to prognosis with clues of epigenetic molecular heterogeneity, cellular composition of the tumor microenvironment and copy number alterations to drive this sample clustering in a subtype of diffuse glioma. The proteome served as biological interpreter of cluster formation.
Conclusion: This integrative multiomics strategy aims towards a dissection of diffuse glioma subtypes for prognostic biomarker detection and transfer from proteomic insights of tumor biology into the epigenetic tumor classification.
S08‐NO‐A35
The landscape of tumor cell states and spatial organization in H3‐K27M mutant diffuse midline glioma across age and location
I. Liu 1,2, L. Jiang2, E. Samuelsson3, S. Marco Salas3, A. Beck4, O. Hack2, D. Jeong2, M. Shaw2, B. Englinger2, J. LaBelle2, H. Mire2, S. Madlener5, L. Mayr5, M. Quezada6, M. Trissal2, E. Panditharatna2, K. Ernst7, J. Vogelzang2, T. Gatesman8, M. Halbert8, H. Palova9, P. Pokorna9, J. Sterba9, O. Slaby9, R. Geyeregger5, A. Diaz10, I. Findlay11, M. Dun11, A. Resnick12, M. Suva13, D. T. W. Jones7, S. Agnihotri8, J. Svedlund3, C. Koschmann14, C. Haberler5, T. Czech5, I. Slavc5, J. Cotter15, K. Ligon2, S. Alexandrescu2, W. K. A. Yung16, I. Arrillaga‐Romany13, J. Gojo5, M. Monje6, M. Nilsson3, M. Filbin2
1Charité—Universitätsmedizin Berlin, Berlin, Germany; 2Dana‐Farber Cancer Institute, Boston, MA, United States; 3Stockholm University, Stockholm, Sweden; 4LMU Munich, Munich, Germany; 5Medical University of Vienna, Vienna, Austria; 6Stanford University, Stanford, CA, United States; 7DKFZ, Heidelberg, Germany; 8University of Pittsburgh, Pittsburgh, PA, United States; 9Masaryk University, Brno, Czech Republic; 10UCSF, San Francisco, CA, United States; 11University of Newcastle, Callaghan, Australia; 12Children's Hospital of Philadelphia, Philadelphia, PA, United States; 13MGH, Boston, MA, United States; 14University of Michigan, Ann Arbor, MI, United States; 15CHLA, Los Angeles, CA, United States; 16MD Anderson Cancer Center, Houston, TX, United States
Introduction: Histone 3 lysine27‐to‐methionine mutations (H3‐K27M) frequently occur in childhood diffuse midline gliomas (DMGs) of the pons, thalamus and spinal cord, presumed to be driven by the specific spatiotemporal context of these midline locations during postnatal development. While most common in the pons and at mid‐childhood ages, the same oncohistone mutation is recurrently detected in adult DMGs and throughout different midline regions. The potential heterogeneity of tumors at different ages and in different anatomical locations of the midline is vastly understudied.
Objectives: Here, we investigated the question how age‐ and location‐dependent contexts shape glioma cell‐intrinsic and ‐extrinsic features in light of the shared driver oncohistone mutation.
Materials and Methods: We dissected the transcriptomic, epigenomic and spatial architectures of a comprehensive cohort of n = 50 patient H3‐K27M DMGs—spanning an age range from 2 to 68 years and locations from spinal cord to thalamus—at single cell resolution.
Results: We identify that oligodendrocyte precursor (OPC)‐like cells constitute the stem‐like compartment in H3‐K27M DMGs across all clinico‐anatomical groups, however, depending on location, display varying levels of maturity resembling less differentiated pre‐OPCs or more mature OPCs further differentiated along the oligodendroglial lineage. We further demonstrate increased mesenchymal cell states in adult tumors, which we link to age‐related differences in glioma‐associated immune cell compartments. We for the first time resolve the spatial organization of H3‐K27M DMG cell types in intact patient tissues, identifying a local niche of the oligodendroglial lineage.
Conclusion: Our study provides a powerful resource for rational modeling and therapeutic frameworks taking into account determinants of age and location in this lethal glioma group.
S14‐NO‐A36
Mean global DNA methylation serves as independent prognostic marker in glioblastoma, IDH wildtype
A. Eckhardt 1,2,3, R. Drexler4, M. Schoof2,5, N. Struve1,6, D. Capper7, C. Jelgersma8, J. Onken8,9, P. N. Harter10,11,12,13, K. J. Weber10,11,12, I. Divé14,15, K. Rothkamm1, K. Hoffer1, S. Huber16, K. Ganser16, C. Petersen1, F. Ricklefs4, M. Kriegs1, U. Schüller2,3,5
1Hubertus Wald Tumor Center—University Cancer Center Hamburg, University Medical Center Hamburg‐Eppendorf, Department of Radiotherapy & Radiation Oncology, Hamburg, Germany; 2Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 3University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 4University Medical Center Hamburg‐Eppendorf, Department of Neurosurgery, Hamburg, Germany; 5University Medical Center Hamburg‐Eppendorf, Department of Pediatric Hematology and Oncology, Hamburg, Germany; 6Mildred Scheel Cancer Career Center HaTriCS4, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 7Charité—University Medicine Berlin, Department of Neuropathology, Berlin, Germany; 8Charité University Medicine Berlin, Department of Neurosurgery, Berlin, Germany; 9German Cancer Consortium (DKTK), Partner Site Berlin, German Cancer Research Center (DKFZ), Heidelberg, Germany; 10Neurological Institute (Edinger Institute), University Hospital, Frankfurt a. M., Germany; 11German Cancer Consortium (DKTK), Heidelberg, Germany and German Cancer Research Center (DKFZ), Heidelberg, Germany; 12Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 13Ludwig‐Maximilians‐University, Center for Neuropathology, Munich, Germany; 14Dr. Senckenberg Institute of Neurooncology, Goethe University Frankfurt, Frankfurt a. M., Germany; 15University Cancer Center Frankfurt (UCT), Goethe University Frankfurt, Frankfurt a. M., Germany; 16University of Tübingen, Department of Radiation Oncology, Tuebingen, Germany
Introduction: Glioblastoma (GBM), IDH wildtype patients have an overall poor prognosis. However, the survival of patients can range from a few weeks up to 5 years.
Objectives: The aim of this project was to analyze the prognostic value of the epigenome in more detail.
Methods: The mean global DNA methylation of 645 primaries and 31 relapsed GBM was analyzed by the Illumina array system and compared to patients’ survival. Of these, 492 patients received combination therapy, and 148 patients received radiation only. Moreover, the mean global DNA methylation of 23 independent GBM cell lines was profiled and correlated to their cellular radiosensitivity as measured by colony formation assay.
Results: Patients with primary GBM, IDH wildtype and standard therapy (surgery [incl. biopsy], radiotherapy, chemotherapy) did not show any differences in survival depending on the DNA methylation subgroup. However, dichotomizing the cohort, we observed a significant correlation of a high mean global DNA methylation with an improved overall survival that was independent from age, MGMT promoter methylation, and extent of resection (median OS: 18.0 months vs. 13.0 months; HR: 1.50 (1.11–2.04); p = 0.009). The analysis of cellular radiosensitivity revealed a significantly higher mean global DNA methylation for radiosensitive cell lines compared to radioresistant cell lines (p = 0.007). Moreover, improved survival of GBM patients treated with radiotherapy only was associated with higher DNA methylation as well (p = 0.029), whereas relapsed GBM samples revealed a significantly lower global DNA methylation compared to the matching primary tumor samples (p = 0.041).
Conclusion: Our results indicate that global DNA methylation is independently associated with outcome in GBM, IDH wildtype. The data also indicate that a higher DNA methylation is associated with higher radiosensitivity and a lower relapse risk, both of which presumably contribute to the observed correlation with survival.
S14‐NO‐A37
Exploring myeloid‐lymphoid interactions in glioblastomas—NK cells as rheostats in the immune microenvironment
R. Sankowski 1, A. Dalmau Gasull1, A. Khavaran1, J. Cahueau1, G. Monaco1, M. Prinz1
1University of Freiburg Medical Center, Institute of Neuropathology, Freiburg i. Br., Germany
Glioblastomas, characterized by their aggressive nature and composition of up to 60% myeloid cells, present significant challenges due to complex molecular dynamics within their immune microenvironment. We have conducted a detailed exploration of these dynamics during glioblastoma progression, leveraging the power of single‐cell RNA‐sequencing datasets from GL261 syngeneic glioma models. Our analysis revealed an unexpected accumulation of NK cells over time. Intriguingly, these cells seem to transition gradually into a dysfunctional phenotype, marked by a downregulation of interferon genes, upregulation of apoptosis genes, and enhanced lymphotoxin signaling. Specifically, there is a distinct upregulation of the lymphotoxin‐beta (LTB) gene, a member of the TNF superfamily pivotal in the development of adaptive immunity and inflammation. This pattern was also observed in human single‐cell RNA‐sequencing datasets, with LTB expression spatially correlated with the NK cell exhaustion marker KLRG1 and MES‐like glioblastomas. Further, our cell‐cell interaction analysis identified myeloid cells, including resident microglia and infiltrating monocytes, as primary recipients of LTB. This suggests an intricate crosstalk between lymphoid, tumor, and myeloid cells within a glioblastoma, positioning NK cells as rheostats in this environment. In vitro fucntional studies confirmed the attenuated immune effector functions of tumor‐derived NK cells. These findings highlight LTB as a potential marker for “immune de‐differentiation” and a promising therapeutic target. Targeting the LTB pathway may halt these de‐differentiation processes and enhance the efficacy of immune therapies leading to new avenues for subtype‐specific glioblastoma treatments. By accounting for its granularity and intricate interactions our approach dissects the immune microenvironment of glioblastoma and paves the way for improved therapeutic strategies.
S14‐NO‐A38
Newly designed fish MYCN/ID2 is useful to identify paediatric‐type diffuse high‐grade glioma, IDH‐ and H3‐wildtype, MYCN‐subtype
A. Tauziède‐Espariat 1, A. Métais1, E. Uro‐Coste2, Y. Nicaise2, F. Chretien1, P. Varlet1
1Sainte‐Anne Hospital GHU Paris Psychiatry and Neurosciences, Neuropathology, Paris, France; 2Toulouse University Hospital, Toulouse, France, Toulouse, France
Introduction: Diffuse paediatric‐type high‐grade glioma (pHGG), IDH‐ and H3‐wildtype are currently subidvided into three epigenetic subgroups: RTK (receptor tyrosine kinase) 1, RTK2, and MYCN. They present recurrent gene amplifications such as PDGFRA (RTK1), EGFR (RTK2) and MYCN (MYCN), but these alterations are not specific of these subgroups. Although recurrent histopathological and genetic features (TP53 mutations, particularly in a context of Li–Fraumeni syndrome) have been identified in pHGG‐MYCN, this diagnosis remains today based only on DNA‐methylation profiling.
Objectives: Because a subset of pHGG‐MYCN may present ID2 and/or MYCN amplifications, we hypothesize that a FISH (fluorescence in situ hybridization) technique targeting both loci would improve this diagnosis.
Materials and Methods: We have shaped a FISH MYCN/ID2 technique and performed it on a series of pHGG, IDH‐ and H3‐wildtype of the three subgroups.
Results: The current series included cases with a calibrated score (>0.9) for pHGG‐RTK1 (n = 3), pHGG‐RTK2 (n = 9), and pHGG‐MYCN (n = 8). All pHGG‐MYCN harbored an amplification of MYCN, and four of them an ID2 amplification. A MYCN amplification was also observed in 17% (2/12) of other subgroups (all RTK2) but no ID2 amplification was evidenced.
Conclusion: The current work is the first to evaluate the diagnostic value of MYCN/ID2 FISH analysis in pHGG subtyping. This technique may improve the diagnosis of pHGG‐MYCN, particularly when DNA‐methylation profiling is not available or when the material is limited. Because MYCN amplification alone is not specific of this subgroup and because not all pHGG‐MYCN harbored this alteration, the presence of the coamplification MYCN/ID2 may constitute an alternative hallmark for this diagnosis. MYCN/ID2 FISH analyses may also present a diagnostic help in the exceptional case of pHGG‐MYCN with an amplification of ID2 without MYCN amplification.
S14‐NO‐A39
Fatal outcome of a case of central neurocytoma—A rare and challenging diagnosis
A. C. Medina 1
1Rizal Medical Center, Department of Pathology and Laboratory Medicine, Angono, Philippines
Introduction: Central neurocytoma (CN) is a rare type of brain tumor that primarily affects young adults and can be challenging to diagnose due to its histological similarity to other clear cell neoplasms in the central nervous system (CNS).
Case summary: A 27‐year‐old male presented with left extremity seizures and was diagnosed with a large mass lesion in the right ventricle with severe hydrocephalus, initially suspected to be a malignant glioma. However, intraoperatively, the tumor was grayish, pink, friable, and highly vascular.
Methodology: Histopathologic examination revealed monotonous cells with ample clear to eosinophilic cytoplasm, consistent with CN or clear cell ependymoma. Immunohistochemistry showed cytoplasmic staining with synaptophysin and absence of GFAP and EMA, confirming the diagnosis of CN.
Discussion: Recent studies have emphasized the significance of GFAP, EMA, and synaptophysin in diagnosing CN, and the importance of molecular profiling and DNA methylation profiling for accurate diagnosis and potential therapeutic targets. A recent meta‐analysis suggests gross total resection as the first‐line treatment for CN, while partial resection or biopsy increases recurrence rates. Radiotherapy and chemotherapy can be used in cases of incomplete resection or recurrence.
Conclusion: CN is a rare brain tumor that primarily affects young adults and is challenging to diagnose. Immunohistochemistry and molecular profiling are essential for accurate diagnosis and potential therapeutic targets. Gross total resection is the preferred treatment, prioritizing surgical intervention for better outcomes and lower recurrence rates.
Keywords: Brain tumors, central neurocytoma, GFAP, immunohistochemistry, synaptophysin.

S14‐NO‐A40
DICER‐1 mutant primary intracranial sarcoma—A call for extensive molecular profiling in CNS tumours with spindle morphology
L. I. Weng 1, W. Jian1
1Fudan University Shanghai Cancer Center, Pathology, Shanghai, China
DICER‐1 mutant primary intracranial sarcoma is rare. Their high‐grade sarcomatous features with partial myogenic differentiation encompass a wide range of differential diagnoses that pose a challenge for pathologists who are unfamiliar with this unique tumour type. We hereby report two cases of DICER‐1 mutant primary intracranial sarcoma by which diagnosis is made through the application of both DNA and RNA next‐generation sequencing. The first patient is an 11‐year‐old boy with a complaint of headache with vomiting. CT scan suggests a left frontal lobe subdural hematoma associated with thickened cerebral surface vascularity. At low power, the dura‐based lesion was composed of spindle cells arranged in fascicles. At higher magnification, the neoplastic cells had basophilic cytoplasm with an ovoid to pleomorphic smudgy nuclei harbouring indistinct nucleoli. Mitotic figures were easily encountered. The second patient is an 18‐year‐old man with a similar clinical presentation as the first patient but displayed a different histomorphology. The short spindled to pleomorphic tumour cells were haphazardly arranged, and in part, dipped into the brain parenchyma hence mimicking a gliosarcoma. Immunohistochemically, the neoplastic cells in both cases showed only focal staining of desmin with a high Ki‐67 index, while patchy staining of CD34 was observed in the first case. Subsequent DNA sequencing confirmed the mutation of DICER‐1 in both cases and additionally identified a PARP6::SMAD3 fusion by RNA next‐generation sequencing in the second case, a fusion that has not been described thus far. Our cases and review of the literature suggest that taxonomizing primary sarcomatous CNS tumours are arduous. Hence, the diverse morphology and inconsistent immunophenotypes of DICER‐1 mutant primary intracranial sarcoma, would hinder and even lead to misdiagnosis without supplementary molecular studies. Thus, multi‐platform testing may reduce underreporting of cases.


PS2‐NO‐A41
Utility of DNA‐methylation profiling and integrated molecular‐morphologic meningioma classification as a prognostic biomarker in CNS WHO grade 2 meningiomas—A retrospective feasibility study in a patient cohort with resected meningiomas in New Zealand
F. Ziad 1, T. Slatter2, G. Jones3, A. Saraiva2, Z. Thotathil4, M. Maharaj5, B. Bhat3, P. Gan5, N. Hung2, M. Jameson6
1Waikato Hospital, Pathology, Hamilton, New Zealand; 2Dunedin School of Medicine, Pathology, Dunedin, New Zealand; 3Dunedin School of Medicine, Surgical Sciences, Dunedin, New Zealand; 4Waikato Hospital, Radiation Oncology, Hamilton, New Zealand; 5Waikato Hospital, Neurosurgery, Hamilton, New Zealand; 6Waikato Hospital, Medical Oncology, Hamilton, New Zealand
Introduction: Molecular biomarkers such as DNA methylation profiling and copy number variations (CNV) have proven to be a powerful tool in predicting risk of recurrence, superior to the WHO grading in meningiomas. An integrated and validated grading approach incorporating histology, CNVs, and the methylation classes (MCs) showed a more reliable stratification of patients with CNS WHO Grade 2 meningiomas to guide treatment.
Objectives: To determine the discordance between WHO grade and DNA methylation classes/integrated classification in resected Grade 2 meningiomas. Secondary objectives include determining the feasibility of performing DNA methylation profiling for meningioma in NZ, the correlation of methylation groups and integrated classification with clinical outcomes.
Methods: DNA methylation profiling and copy number data were obtained from formalin fixed paraffin embedded samples of 72 patients with resected WHO Grade 2 meningioma at Waikato Hospital, New Zealand. Integrated score was derived using the scheme published by Mass et al. [1].
Results: DNA methylation profiling segregated 38 out of 72(52%) WHO Grade 2 meningiomas into the benign MC, while integrated classification stratified 27 out of 72(37%) as low risk. DNA methylation‐based subgrouping and integrated scoring better separated out those with recurrence (Figures 1 and 2, benign vs. IntA/IntB/Mal and low risk vs. Int/high risk combined, both p = 0.0014, log rank test). Both DNA methylation‐based subgrouping and integrated classification had high positive predictive values (>80%), and integrated scoring showed high specificity (82%) for predicting recurrence. However, both methods had relatively poor sensitivity (<65%).
Conclusion: Integrated approach to classify meningiomas is a more reliable tool when compared to WHO grading to stratify meningiomas according to risk of recurrence and guide further treatment.
Reference: [1] Maas SLN, et al. J Clin Oncol. 2021 39(34):3839–52.


PS2‐NO‐A42
Clinical implications of DNA methylation‐based integrated classification of histologically defined grade 2 meningiomas
F. Ehret 1, E. Pérez2, D. Teichmann2, S. Meier2, C. Zeus2, D. Kaul1, D. Capper2
1Charité—Universitätsmedizin Berlin, Radiation Oncology, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany
Introduction: The integration of DNA‐methylation analysis with the addition of histopathological characteristics and genetic markers such as copy number variations enables a more precise risk stratification and integrated classification of meningiomas. However, the clinical implications of such classification for patients suffering from grade 2 meningiomas are poorly understood.
Objectives: Correlate the clinical outcomes of histopathologically confirmed grade 2 meningioma with an integrated risk stratification and determine its clinical implications.
Patients and Methods: Grade 2 meningioma patients treated at our institution were re‐classified and subject to DNA‐methylation and TERT promoter analyses as well as integrated risk stratification as previously described (Maas et al., JCO, 2021).
Results: Grade 2 meningioma treated between 2007 and 2021 (n = 123) were retrospectively analyzed. The median clinical and radiographic follow‐up periods were 56.3 and 51.4 months. Integrated molecular‐morphologic risk groups were as follows: 43 benign (35%), 62 intermediate (50%), 18 high‐risk (15%) (Figure 1). In the multivariable Cox regression analysis, grouping was significantly associated with the local recurrence risk (hazard ratio [HR] intermediate: 5.8, HR high‐risk: 6.0, both p < 0.01; vs. benign) (Figure 2). Resection status was not formally associated (HR gross total resection: 0.46, p = 0.07; vs. subtotal resection). Only one TERT promoter mutation and one homozygous deletion of CDKN2A/B were identified.
Conclusion: In our institutional retrospective series, we were able to stratify histologically defined grade 2 meningiomas into clinically meaningful groups. Integrated molecular risk stratification is crucial to guide the clinical management of patients and should be routinely applied to avoid over‐ and undertreatment.

FIGURE 1 Alluvial plot showing the risk group distribution.

FIGURE 2 Kaplan–Meier estimates for local recurrence stratified by risk groups.
PS2‐NO‐A43
Using molecular and immunohistochemical features to predict outcomes in grade 3 meningiomas
K. Chornenka Martin 1, K. Tosefsky2, A. D. Rebchuk2, J. Z. Wang3,4,5, G. Zadeh3,4,5, S. Makarenko2, S. Yip1
1University of British Columbia, Department of Pathology & Laboratory Medicine, Faculty of Medicine, Vancouver, Canada; 2University of British Columbia, Division of Neurosurgery, Vancouver, Canada; 3University of Toronto, Division of Neurosurgery, Toronto, Canada; 4University Health Network and University of Toronto, MacFeeters Hamilton Neuro‐Oncology Program, Princess Margaret Cancer Centre, Toronto, Canada; 5University Health Network, Princess Margaret Cancer Centre, Toronto, Canada
Objective: Although meningiomas have traditionally been graded using morphologic features, a subset of meningiomas demonstrates behaviour that is discordant with their histologic grade. The WHO 2021 classification introduces molecular alterations in meningiomas that are associated with increased risk of recurrence, shorter time to progression, and/or shorter overall survival, and these include TERT promoter (TERTp) mutations, CDKN2A/B homozygous deletion, loss of H3 K27me3, and BAP1 loss. With the precise prognostic implications of these molecular markers pending further characterization, we explored these molecular alterations and associated clinical outcomes in a single‐center cohort of grade 3 intracranial meningiomas. Furthermore, we examined whether p16 and MTAP immunohistochemistry may be used as surrogate markers to predict CDKN2A/B homozygous deletion.
Methods: Demographic, clinical and histopathological information were obtained from the electronic medical records of all grade 3 meningioma cases surgically treated at a tertiary center between 2007 and 2020. Tissue blocks were reviewed by a neuropathologist and molecular testing for TERTp mutations and CDKN2A/B copy number profiles were performed. Immunohistochemistry for H3 K27me3, BAP1, p16, and MTAP were performed on all cases. Expression of p16 and MTAP was independently scored by two blinded neuropathologists and correlated with CDKN2A/B status. Predictors of survival were identified by Cox regression.
Results: Fifteen patients (8 female, 7 male) with a median age of 64 (IQR: 48, 73.5) years were included. Eight (53%) tumors were classified as anaplastic, 6 (40%) as rhabdoid and 1 (6.7%) as papillary. One (7%) rhabdoid tumor exhibited BAP1 loss, while four (27%) tumors harbored TERTp mutations and 3 (20%) demonstrated homozygous CDKN2A/B homozygous deletion. TERTp mutations and CDKN2A status were associated with significant reductions in OS (HR = 8.72, 95% CI [1.87, 40.6] and HR = 6.18, 95% CI [1.30, 29.4], respectively). The association between reduced OS and TERTp mutations (p=0.002) and CDKN2A/B copy number status (p = 0.02) held independent of Simpson resection grade. All three cases that demonstrated CDKN2A/B homozygous deletion showed loss of p16 and MTAP immunoreactivity.
Conclusion: In grade 3 meningiomas, TERTp mutations and CDKN2A/B homozygous deletion are significantly associated with reduced overall survival independent of resection extent. Our findings support using these molecular markers for prognostication in these tumors.
PS2‐NO‐A44
Intracranial myxoid mesenchymal tumor with EWSR1‐CREM gene fusion—2 cases report and literature review
X. Ba 1, K. Sun1, B. Wang1
1The First Affiliated Hospital, Zhejiang University School of Medicine, Department of Pathology, Hang Zhou, China
Introduction: “Intracranial mesenchymal tumor with FET‐CREB fusion” occurs primarily in children or young adults. These masses are more commonly located in supratentorial sites than in infratentorial sites, and most are extraaxial attached to the meninges or dura. These entities appear with variable histomorphology and has previously been termed intracranial angiomatoid fibrous histiocytoma or intracranial myxoid mesenchymal tumor. These tumors harboring EWSR1 fusion with CREB transcriptional factor gene families were recently described in several case reports, especially EWSR1 fusion with CREB1/ATF1.
Patients and Methods: We herein describe two cases of intracranial mesenchymal myxoid tumours arising differently in spinal cord and cerebellum of middle‐aged man.
Results: The first case presents spindle cells with sheet‐like growth or reticular cord‐like structures and contains myxoid stroma, prominent haemangioma‐like collections of dilated thin‐walled vessels. At the tumour periphery shows dense lymphoplasmacytic cuffing. The second is composed of cords of monotonous atypical round cells with eosinophilic cytoplasms and contains collagenous or myxoid stroma partly. However, lymphoplaxmacytic cuffing is not common and ossification is visible. The mitotic activity of these two tumours are low (<2 mitoses/mm2) and proliferation are focally 5%–6%. They showed immunoreactivities for CD99 and EMA, were negative foe S100, GFAP, Desmin, PR, CD34, SSTR2A. EWSR1 and CREM gene fusion were identified using FISH assay. No other treatments were used in either case. No recurrence or metastasis has occurred in the two cases since follow‐up (case 1, 36 months and case 2, 19 months after surgical operation).
Conclusion: The full spectrum of clinical behavior is not yet known well. More cases and epidemiological evidence studies are needed to figure out the problem.

FIGURE 1.

FIGURE 2.
PS2‐NO‐A45
Transcription factor expression profile in immunonegative pituitary adenomas
G. Chacko 1, A. Ravichandran1, R. Jayachandran1, A. H. S.1, N. Thomas1, A. Chacko1, V. Rajshekhar1, G. Mahasampath1, P. Mannam1, V. Joseph1
1Christian Medical College Vellore, Neuropathology, Department of Pathology, Vellore, India
Objective: To identify true null cell adenomas among the immunonegative pituitary adenomas using the transcription factors Steroidogenic factor‐1 (SF‐1), T‐Pit and Pit‐1, and to ascertain if their clinical behaviour is truly aggressive.
Methods: This study included a prospective and retrospective cohort between 2009 and 2021. Slides of each biopsy were reviewed. The hormonally immunonegative cases were subjected to immunohistochemical staining for SF‐1, T‐Pit and Pit‐1. Statistical analysis was done with continuous variables and presented with mean (SD)/median (IQR). Categorical data were expressed as a frequency (%). The risk for invasion, recurrence and MIB‐1 were analysed with logistic regression analysis and presented as an odds ratio (95% CI).
Results: There were 994 cases of pituitary adenomas of which 92 (9.25%) were hormonally immunonegative. Among the latter, 48 were positive for SF‐1, 9 were positive for T‐pit and 3 were positive for Pit‐1. Following the application of transcription factors, the proportion of null cell adenomas dropped to 3.21% from the earlier prevalence of 9.25%. Null cell adenomas had a significantly higher prevalence of invasion (84.38%) as well as recurrence (54.84%) when compared with most other subtypes. Among the “high‐risk” aggressive adenomas, the sparsely granulated somatotroph adenomas and silent corticotroph adenomas had a significantly higher prevalence of invasion as compared to the other subtypes. Silent corticotroph adenomas had significantly higher recurrence rates as compared to the functional corticotroph adenomas. The prevalence of invasion in lactotroph adenomas was higher in males (90%) than in females (37.50%).
Conclusion: The use of transcription factors, better defines subtypes of pituitary adenomas. This is of extreme clinical significance as one is then able to identify patients with “high‐risk” adenomas which can be followed up more closely and provided with adjuvant therapy in addition to surgical resection.
PS2‐NO‐A46
Lineage‐dependent expression of Islet‐1 in pituitary neuroendocrine tumors
E. Hewer 1, T. Maragou2, S. Berezowska1, M. Wartenberg2
1Lausanne University Hospital and University of Lausanne, Institute of Pathology, Lausanne, Switzerland; 2University of Bern, Bern, Switzerland
The clinical and biological heterogeneity of pituitary neuroendocrine tumors (PitNET) mirrors distinct histogenetic lineages. Lineage‐specific transcription factors are the backbone of the classification of PitNETs and can furthermore distinguish PitNETs from mimics. Islet‐1 (ISL1) which is diagnostically used as a marker of pancreatic neuroendocrine tumors is also involved in pituitary development, but its expression in adult pituitary or PitNET has not been systematically studied. We assessed ISL1 expression in PitNET by tissue microarrays and full histological slides. Gonadotroph, lactotroph and TSH‐positive (uni‐ or plurihormonal) PitNETs frequently expressed ISL1. Specifically, all thyrotroph adenomas (3/3; 100%), four of five null cell adenomas (45; 80%), the majority of gonadotroph adenomas (91/96; 95%), one third of the lactotroph adenomas (5/15; 33%) and five of 12 plurihormonal adenomas (5/12; 42%) expressed ISL1. Corticotroph and somatotroph PitNEts did not express ISL1 (0/16 and 0/29, respectively). Non‐neoplastic anterior pituitary tissue present in surgical specimens displayed a heterogeneous staining pattern, consistent with that of LH/FSH‐producing cells. In conclusion, ISL1 is frequently expressed in both gonadotropic PitNETs as well as TSH‐positive tumors (uni‐ or plurihormonal). Since expression is usually strong and diffuse, it may contribute favorably to a diagnostic panel for classification of PitNET. Awareness of this immunophenotype may help to correctly identify a pituitary origin in case of locally extensive or metastatic disease.
PS2‐NO‐A47
Expression of transcription factors is associated with higher recurrence in craniopharyngiomas
J. Cienfuegos Meza 1, M. L. Tena Suck1
1National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Neuropathology, Mexico City, Mexico
Background: Craniopharyngioma is a benign tumor of the sellar region with high recurrence rate, associated with high morbidity. Transcription factors have been identified originally as key components of cytokine signaling pathways in these tumours. Differential expression in recurrent versus non‐recurrent tumours has not been investigated.
Methods: FFPE tissue blocks from patients with adamantinomatous craniopharyngiomas (AdaCP) were retrieved for immunohistochemical and immunofluorescence analysis with β‐catenin, STAT2, STAT3, STAT4, STAT6, HDAC1, HADC2, PDGR, β‐FGF, and TNFα. Coexpression of these markers was analyzed by confocal microscopy.
Results: We included 40 cases, 20 were recurrent tumours. This group of recurrent cases showed more expression of STAT3, STAT6, HDCA, β‐catenin, and TNFα. Coexpression of β‐Catenin with STAT2 and STAT3, and of STAT6 with TNFα was higher in recurrent cases.
Conclusion: Inflammation, cell proliferation, and chromatin regulation markers are upregulated in recurrent craniopharyngiomas. These factors are not only essential for tumor development, but also play a role in tumor progression, invasion and recurrence.
PS2‐NO‐A48
Expression of apolipoproteins in adamantinomatous craniopharyngiomas correlates with tumor recurrence and survival
J. Cienfuegos Meza 1, M. L. Tena Suck1, A. Ortiz Plata2
1National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Neuropathology, Mexico City, Mexico; 2National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Experimental neuropathology, Mexico City, Mexico
Purpose: The cystic component of craniopharyngiomas has been studied for its potential to induce inflammation and tumor progression. We studied inflammatory, cell adhesion, and extracellular matrix molecules as biomarkers for prognosis in Craniopharyngiomas.
Methods: Immunohistochemistry was performed in 36 adamantinomatous craniopharyngiomas for apolipoproteins (APOA‐I, APOA‐II, APOB, APOC and perilipin), β‐catenin, lectin 1, TNFα, IL‐6, collagen IV, smooth muscle actin, metalloproteinases 1, 2, and 9, connectin, osteoconectin, laminin and vimentin. We use correlations of the clinic‐pathological features with immunohistochemical and proteomic results.
Results: All cases showed common expression of APO‐AI by proteomic analysis in the cystic content. By immunohistochemistry, we found APO‐AI and APO‐C positive expression in ghost cells and wet keratin, fibroblasts, and endothelial cells. APO‐II, APO‐B, and Perilipins were negative. Lectin‐1 was positive in neoplastic epithelial cells, and together with a high Ki‐67 proliferation index and β‐catenin loss, correlation was found with recurrence rate and survival.
Conclusions: Craniopharyngioma is a histologically benign and heterogeneous tumor. Expression of apolipoproteins in both cystic fluid and neoplastic cells could be a biological marker for tumor recurrence.
PS1‐NO‐A49
The correlation between pleomorphic xanthoastrocytoma methylation class and the integrated pathological diagnosis
M. Alturkustani 1,2
1King Abdulaziz University, Department of Pathology, Jeddah, Saudi Arabia; 2Western University, Department of Pathology and Laboratory Medicine, London, Ontario, Canada
Introduction: The methylation class (MC) for pleomorphic xanthoastrocytoma (PXA) includes cases with a histological diagnosis of high‐grade gliomas, astroblastomas, and gangliogliomas. Some cases with histological features of PXA are under different MCs.
Objectives: This study aims to interpret the MC in cases diagnosed with PXA based on either methylation profiling or the integrated pathological diagnosis (IPD).
Materials and Methods: The Children's Brain Tumor Network online database searched for cases diagnosed with PXA. The MCs of these cases, an additional 324 cases, and the CDKN2A/B status were obtained from the Heidelberg methylation brain tumor classifier (v12.5). The clinical information, histological features, and next‐generation sequencing data were used to formulate the IPD. The results were divided into three groups: Group 1 when both IPD and MC matched the PXA diagnosis (7 cases), Group 2 when the PXA diagnosis was only by IPD (7 cases), and Group 3 when the PXA was by MC only (5 cases).
Results: All seven cases in the first group showed classic morphological features and BRAF V600E and CDKN2A/B homozygous deletion. Reassessment of the second group supported the change of PXA diagnosis in five cases, while the possibility of PXA could not be excluded in two cases. All cases in the third group showed different morphological features than the classic PXA. The prognosis in two cases supported the possibility of different entities, while the possibility of an expanded morphological spectrum of PXA can not be excluded in the remaining three cases.
Conclusion: The MC of PXA in cases with classic morphological features is diagnostic of PXA. Cases with morphological suggestions of PXA but MC other than PXA require reassessment for a high possibility of an alternative diagnosis. Cases with non‐classic histological features may represent an expansion of the morphological spectrum or false classification.
PS1‐NO‐A50
Insights into molecular biology of pleomorphic xanthoastrocytoma
V. Suri 1, J. Singh1, I. Dandapath1, M. C. Sharma1
1AIIMS—New Delhi, Neuropathology, New Delhi, India
Introduction: Pleomorphic xanthoastrocytomas (PXAs) are rare, accounting for less than 1% of astrocytomas, and commonly occur in young patients. Majority are WHO grade 2. A fraction of tumors that present or recur with malignant change are classified as grade 3. A fraction of tumors that present or recur with malignant change are classified as grade 3. Limited data are available on their molecular characteristics.
Objectives: To evaluate a gene expression‐based histology independent classifier and check whether this tool is predictive of survival and develop a minimal robust gene signature panel for prognostication and designing effective therapeutic strategies.
Methods: Genome‐wide expression profiling of 14 PXA and 6 APXAs was performed by microarray. Among differentially expressed genes (DEGs), Cyclin‐Dependent Kinase 14 (CDK14) and Mitochondrial Fission Process 1 (MTFP1) were validated by qRT PCR.
Results: Unsupervised hierarchical clustering revealed two distinct molecular clusters (Cluster 1: 10 PXA, 3 APXA and Cluster 2: 4 PXA, 3 APXA) with grade 2 and 3 tumors distributed in both highlighting molecular heterogeneity within the same grade. There was an insignificant difference in age, sex, immunohistochemical profile, frequency of BRAF mutation, or CDKN2A deletion among the two clusters. Significantly, worse PFS was observed in cluster 2 (p = 0.003). mRNA profiling‐based prediction of recurrence was superior to and independent of histological grade, BRAF mutation, or CDKN2A deletion status. A total of 10 upregulated and 418 downregulated genes were identified between the PXA clusters. qRT‐PCR validation of CDK14 (upregulated in cluster 2) and MTFP1 (upregulated in cluster 1) showed strong concordance with expression array data.
Conclusion: This is the first comprehensive study highlighting distinct molecular subgroups of PXA. The differentially expressed genes between two clusters may potentially be used for developing histology independent classification schemes, prognostication and may serve as prospective therapeutic targets for PXA patients.
PS1‐NO‐A51
Polymorphous low‐grade neuroepithelial tumor of the young—A short series from a tertiary care centre in South India
D. Narasimhaiah 1, G. Vilanilam1, R. Menon1, A. Cherian1, B. Thomas1, C. Kesavadas1, R. Poyuran1
1Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Pathology, Thiruvananthapuram, India
Question: To describe the clinico‐pathological features of polymorphous low‐grade neuroepithelial tumor of the young (PLNTY) diagnosed at our Institute.
Methods: Cases of PLNTY diagnosed between 2018 and 2022 were included in the study. Haematoxylin and eosin stain and immunohistochemistry were performed on all cases.
Results: Six cases of PLNTY were diagnosed during the study period, 4 paediatric and 2 adults. The patients ranged in age from 10 to 31 years (median: 14 years, mean: 18.3 years) with a male:female ratio of 2:1. The tumors were equally distributed between temporal lobe, mesial temporal structures and insula. The patients presented with refractory epilepsy with the duration ranging from 5 months to 11 years. All patients were treated with surgery. On histopathological examination, the tumors showed a diffuse pattern and were composed of oligo‐like cells with perinuclear halos. Pleomorphism ranged from mild to moderate and there was no evidence of mitotic activity. Four cases showed calcification. Immunohistochemistry for CD34 stained the tumor cells, as well as stellate cells in the adjoining cortex. The tumor cells were positive for OLIG2, negative for R132H‐mutant IDH1 with retained ATRX expression. The MIB‐1 proliferation index was between 2% and 4%. The tumors could not be tested for BRAF p.V600E mutation or FGFR2/FGFR3 gene fusions. There was no associated focal cortical dysplasia or hippocampal sclerosis. All tumors were diagnosed as polymorphous low‐grade neuroepithelial tumor of the young, not otherwise specified (NOS), CNS WHO grade 1. The post‐surgical follow‐up ranged from 1 to 39 months, with residual tumor present in one case.
Conclusions: Among the diagnosed cases of PLNTY, two patients were older than 18 years of age with a male predominance and mainly temporal localization. Calcification was lacking in two tumors. The tumors showed the typical morphological and immunohistochemical features. All patients with gross total resection were free of seizures.
PS1‐NO‐A52
Diffuse gliomas with low‐grade histopathological features and FGFR3‐TACC3 fusion—A diagnostic dilemma
V. Barresi 1, E. Miele2, L. Pedace2, G. Pinna3, A. Scarpa1
1University of Verona, Diagnostics and Public Health, Verona, Italy; 2Ospedale Pediatrico Bambino Gesù, Rome, Italy; 3University and Hospital Trust of Verona, Verona, Italy
Introduction: FGFR3‐TACC3 fusion has been found in glioblastomas (GBM) with a better prognosis and has been reported in approximately 30 cases of histologically diffuse low‐grade gliomas. Due to the unclear genetic and clinical features of the latter, optimal postsurgical management remains to be defined.
Objective: This study aimed to clarify the clinical, genetic, and epigenetic features of histologically low‐grade diffuse gliomas with FGFR3‐TACC3 fusion.
Patients and Methods: Two tumors with hemispheric location and inhomogeneous contrast enhancement were resected from two female patients, aged 53 and 68 years, after a history of seizures for 12 and 5 months, respectively, during which they remained unchanged in size. In one patient, a second lesion, radiologically consistent with GBM, was observed in the corpus callosum one month before surgery. We assessed the histological and genetic features of both cases and the DNA methylation profile of one case.
Results: Both tumors showed oligodendroglial‐like cells, extensive calcifications, vague perivascular pseudorosettes, strong CD34 immunostaining, and FGFR3‐TACC3 fusion, and lacked mitosis, microvascular proliferation, or necrosis, thus fulfilling the WHO criteria for polymorphous neuroepithelial tumor of the young. No recurrence was seen 3 and 2 months after surgery, despite the lack of adjuvant treatments. However, both cases also featured chromosome 7+/chromosome 10− and pTERT mutations, consistent with the WHO criteria for GBM. In the case analyzed, the top score of the DNA methylation profile was mesenchymal GBM using version 11. b6 of the classifier and ganglioglioma in version 12.5.
Conclusion: The relatively long clinical history, along with the onset of a second lesion, molecular stigmata of GBM, and DNA methylation profile, suggest that diffuse gliomas with FGFR3‐TACC3 fusion and histologically low‐grade may represent precursors of a distinct variant of GBM with more favorable clinical outcomes.
PS1‐NO‐A53
VGLL‐altered CNS schwannoma is a new tumor entity with distinct DNA‐methylation profile and recurrent gene fusions of either VGLL3 or VGLL1
S. Schmid 1, K. Mirchia2, M. Snuderl3,4,5, J. Schittenhelm6,7, C. Hartmann8, A. Korshunov9, S. Brandner10,11, S. Paine12, M. Hasselblatt13, R. Coras14, C. Stadelmann15, S. Zechel15, S. Epari16, A. Tietze17, A. Koch1, P. Hernáiz Driever18, M. Simon18, F. Sahm9, A. Perry2, D. T. W. Jones19,20, D. Capper1,21
1Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Neuropathology, Berlin, Germany; 2University of California, Pathology, San Francisco, CA, United States; 3NYU Langone Health, Neuropathology, New York, NY, United States; 4NYU Langone Health, Laura and Isaac Perlmutter Cancer Center, New York, NY, United States; 5NYU Langone Health, Division of Molecular Pathology and Diagnostics, New York, NY, United States; 6University Hospital Tübingen, Neuropathology, Tuebingen, Germany; 7University Hospital Tübingen, Center for Neuro‐Oncology, Comprehensive Cancer Center Tübingen‐Stuttgart, Tuebingen, Germany; 8Hannover Medical School, Neuropathology, Hannover, Germany; 9Heidelberg University Hospital, Neuropathology, Heidelberg, Germany; 10University College London Hospitals, Neuropathology, London, United Kingdom; 11UCL Queen Square Institute of Neurology, Neurodegenerative Disease, London, United Kingdom; 12Nottingham University Hospitals NHS Trust, Neuropathology Laboratory, Nottingham, United Kingdom; 13University Hospital Munster, Neuropathology, Muenster, Germany; 14Universitätsklinikum Erlangen, Neuropathology, Erlangen, Germany; 15University Medical Center Gottingen, Neuropathology, Goettingen, Germany; 16Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Pathology, Mumbai, India; 17Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Radiologie, Berlin, Germany; 18Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Pediatric Oncology and Hematology, Berlin, Germany; 19Hopp Children's Cancer Center Heidelberg (KiTZ), Heidelberg, Germany; 20University of Birmingham, NIHR Birmingham Biomedical Research Centre, Birmingham, United Kingdom; 21German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Berlin, Heidelberg, Germany
Introduction: Gliofibroma/intracerebral schwannoma are rare CNS tumors with unresolved histopathologic criteria, molecular features and classification. The launch of the 12.5 version of the DNA methylation‐based brain tumor classifier introduced the new class “CNS schwannoma, VGLL‐fused.”
Objectives: We aim to further characterize the clinicopathologic and genetic features of these rare CNS tumors.
Materials and Methods: The tumor cohort consists of 20 tumors with DNA methylation profile “CNS schwannoma, VGLL‐fused” with 11 cases with available clinicoradiological data. The histopathology was reviewed and a standard immunohistochemical panel was applied. 450k/850k Illumina Beadchip arrays and targeted RNA‐Next‐Generation‐Sequencing were performed.
Results: Patient age ranged from 7 to 75 (median 13.5) years, with a slight male predominance (1:1.2). All tumors were located within CNS parenchyma, either supratentorial (n = 14), infratentorial (n = 4), or spinal (n = 1), without any obvious peripheral nerve contact. All cases showed highly similar DNA‐methylation profiles and formed a distinct cluster in tSNE analysis. In RNA Seq (n = 16), 15 cases showed gene fusions of either the VGLL3 or the VGLL1 gene, the most common fusion being CHD7::VGLL3 (n = 9). The tumors showed classic pathologic features of schwannoma and often a lobule‐like growth pattern surrounded by reactive CNS tissue. Others had prominent Rosenthal fibers, although it was hard to reliably distinguish intratumoral from peritumoural localization. The median clinical follow‐up was 3.1 years (range, 3.3 months to 7.7 years). No relapses occurred during follow‐up (n = 7). One patient died of unknown reason 7 months after surgery.
Conclusion: We describe a new low‐grade CNS tumor class, characterized by schwannoma‐like features, specific DNA‐methylation profile and recurrent VGLL3 or VGLL1 fusions. Our data suggests a benign biology.
PS1‐NO‐A54
Chordoid glioma—A case report of an intracranial mass in a forty‐four‐year‐old female
S. A. Salih 1, M. A. Ang1,2, E. Muñoz2
1University of the Philippines Manila, Laboratories, Manila, Philippines; 2University of the Philippines Manila, Pathology, Manila, Philippines
Introduction: Chordoid gliomas are rare neoplasms first described in 1998. It was included as a separate entity in the WHO 2007 classification and assigned grade II. It usually occurs in adults with a mean age of 46, in females (M:F ratio of 1:2) with location commonly being the anterior third ventricle and presenting with headache, visual changes, and memory deficits.
Objectives: To investigate the case of an intracranial mass, centered in the Foramen of Monro, with a clinical diagnosis of craniopharyngioma.
Patients and Methods: A forty‐four‐year‐old female presented with 1‐year history of behavioral, gait, and memory recall changes. Imaging revealed a soft tissue mass at the Foramen of Monro. Excision of the mass was done and sent for routine examination.
Results: Gross examination of the specimen revealed multiple cream‐white to cream‐tan, irregularly shaped, firm tissue fragments with cream‐white to tan‐brown cut surfaces. Histomorphologic evaluation showed papillary and gland formation, lymphoplasmacytic stroma, and basophilic myxoid areas. The tumor cells showed round to ovoid nuclei with an abundant eosinophilic cytoplasm. The immunohistochemistry panel requested revealed immunoreactivity to GFAP, Cam5.2, TTF‐1, CD34, patchy staining with CK7, and absence of staining for Synaptophysin, S100, EMA, and Brachyury. The differential diagnoses included papillary glioneuronal tumor (PGNT), metastatic carcinomas, and choroid plexus neoplasms. Given the absence of staining with brachyury, and staining with TTF‐1 and CD34 at the myxoid areas, the diagnosis of a Chordoid Glioma was finally reached. Some journals noted TTF‐1 staining in tumors of the third ventricle region, highlighting its use in this case. Other patterns include solid, fusiform, and fibrosing patterns.
Conclusion: In patients with masses at the Foramen of Monro, thorough evaluation and a comprehensive panel to rule out mimickers assists in the pathologic diagnosis of these neoplasms.

FIGURE 1.

FIGURE 2.
PS1‐NO‐A55
Characterisation of gene fusions in MYB(L1)‐altered gliomas
J. L. Rohwer 1,2, D. Stichel3,4, D. Schrimpf3,4, R. Coras5, M. Pagès6,7,8, A. Tauziède‐Espariat6, P. Varlet6, V. H. Hans9,10, J. Meyer3,4, J. Schittenhelm11,12, O. Staszewski13, E. Cheesman14, M. Glatzel1, S. Schmid15,16, A. Korshunov3,4, A. Sexton‐Oates17,18, L. T. Kõrgvee19,20, S. Mueller21,22, A. Olar23, W. N. M. Dinjens24, J. M. Kros24, B. Kusters25, S. Brandner26,27, M. Thom28, M. Snuderl29, L. Schweizer15,16,30,31,32, F. Sahm3,4,33, P. Wesseling34,35, E. Aronica36,37, U. Schüller1,2, A. von Deimling3,4, I. Blümcke5, D. Capper15,16, D. T. W. Jones33,38, A. K. Wefers1,39
1Institute of Neuropathology, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany; 2Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 3University Hospital Heidelberg, Department of Neuropathology, Institute of Pathology, Heidelberg, Germany; 4Clinical Cooperation Unit Neuropathology, German Cancer Consortium (DKTK), German Cancer Research Center (DKFZ), Heidelberg, Germany; 5University Hospital Erlangen, Department of Neuropathology, Erlangen, Germany; 6Department of Neuropathology, Sainte‐Anne Hospital, Descartes University, Paris, France; 7Department of Genetics, Institut Curie, Paris, France; 8SIREDO Paediatric Cancer Center, Institut Curie, Paris, France; 9Dietrich‐Bonhoeffer‐Klinikum, Abteilung Neuropathologie, Institut für klinische Pathologie, Neubrandenburg, Germany; 10Institut für Neuropathologie, Evangelisches Klinikum Bethel gGmbH, Bielefeld, Germany; 11University Hospital of Tübingen, Department of Neuropathology, Institute of Pathology and Neuropathology, Tuebingen, Germany; 12University Hospital of Tübingen, Center for CNS Tumours, Comprehensive Cancer Center Tübingen‐Stuttgart, Tuebingen, Germany; 13University of Freiburg, Institute of Neuropathology, Faculty of Medicine, Freiburg i. Br., Germany; 14Royal Manchester Children's Hospital, Department of Paediatric Histopathology, Manchester, United Kingdom; 15Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Berlin, Germany; 16German Cancer Consortium (DKTK), Partner Site Berlin, German Cancer Research Center (DKFZ), Heidelberg, Germany; 17Cancer and Disease Epigenetics, Murdoch Children's Research Institute, Melbourne, Australia; 18Rare Cancers Genomics Team (RCG), Genomic Epidemiology Branch (GEM), International Agency for Research on Cancer/World Health Organisation (IARC/WHO), Lyon, France; 19Department of Pharmacology, Institute of Biomedicine and Translational Medicine, University of Tartu, Tartu, Estonia; 20Haematology and Oncology Clinic, Tartu University Hospital, Tartu, Estonia; 21Department of Oncology and Children's Research Center, University Children's Hospital of Zurich, Zurich, Switzerland; 22University of California, Department of Neurology, Neurosurgery and Pediatrics, San Francisco, CA, United States; 23NOMIX Laboratories, Denver, CO, United States; 24Erasmus MC Cancer Institute, Department of Pathology, Rotterdam, Netherlands; 25Radboud University Medical Center, Department of Pathology, Nijmegen, Netherlands; 26University College London, Department of Neurodegeneration, Institute of Neurology, London, United Kingdom; 27University College London Hospitals NHS Foundation Trust, Division of Neuropathology, The National Hospital for Neurology and Neurosurgery, London, United Kingdom; 28UCL Queen Square Institute of Neurology, Department of Clinical and Experimental Epilepsy, London, United Kingdom; 29New York University, Langone Health, Department of Pathology, New York, NY, United States; 30German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Heidelberg, Germany; 31Edinger Institute, Institute of Neurology, University of Frankfurt am Main, Frankfurt a. M., Germany; 32Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 33Hopp Children's Cancer Center Heidelberg (KiTZ), Heidelberg, Germany; 34Princess Máxima Center for Pediatric Oncology, Utrecht, Netherlands; 35Amsterdam University Medical Centers/VUmc, Department of Pathology, Amsterdam, Netherlands; 36Amsterdam UMC, University of Amsterdam, Amsterdam Neuroscience, Department of (Neuro) Pathology, Amsterdam, Netherlands; 37Stichting Epilepsie Instellingen Nederland, Heemstede, Netherlands; 38Pediatric Glioma Research Group, German Cancer Research Center (DKFZ), Heidelberg, Germany; 39Mildred Scheel Cancer Career Center HaTriCS4, University Medical Center Hamburg‐Eppendorf, Hamburg, Germany
Introduction: “MYB(L1)‐altered gliomas” comprise two related entities: “angiocentric gliomas” (AG) and “diffuse astrocytomas, MYB‐ or MYBL1‐altered” (DA‐MYB(L1)). Both subgroups have gene fusions of the proto‐oncogenes MYB or MYBL1 and are graded as CNS WHO grade 1. However, since MYB(L1)‐altered gliomas are rare, little is known about the biology of these gliomas.
Objectives First, to molecularly define subgroups of MYB(L1)‐altered gliomas. Second, to characterise gene fusions in these tumours.
Materials and Methods: 176 MYB(L1)‐altered gliomas with sufficient tissue (FFPE) for DNA methylation analyses (cluster and copy number analyses) and RNA‐Seq (74/176; gene fusion analyses), were classified with v11b4 and v12 of the “brain tumor classifier” (Capper et al., Nature 2018).
Results: Unsupervised hierarchical cluster analysis identifies four molecular subgroups: AG divide into supra‐ and infratentorial tumours and DA‐MYB(L1) divide into two groups: “isomorphic diffuse gliomas” (IDG) and “MYB(L1)‐altered gliomas, other” (MYB(L1) other). The median age of patients at diagnosis differed: AG 9 years (2–45 years), MYB(L1) other 4 years (1–36) versus IDG 31 years (6–50). In 59/74 (80%), we detected a MYB or MYBL1 fusion. The most common fusion in AG was MYB‐QKI (66%, 19/29). In both groups of DA‐MYB(L1), we detected more MYBL1 fusions (56%, 25/45) than MYB fusions (16%, 7/45), each with different fusion partners (most frequent: 6/45 MYB‐PCDHGA1, 5/45 MYBL1‐KHDRBS3, 4/45 MYBL1‐MMP16). Although not all copy number alterations (CNA) detected were specific for a distinct fusion, a CNA of the MYB or MYBL1 locus supports the diagnosis of a MYB(L1)‐altered glioma.
Conclusion: MYB(L1)‐altered gliomas divide into four molecular subgroups that we added to v12 of the brain tumor classifier. AG and DA‐MYB(L1) have different gene fusions. To further investigate the biological role of different gene fusions, in vitro studies, as well as histological, molecular, and clinical analyses are ongoing.
PS1‐NO‐A56
Molecular characteristics and prognostic biomarkers of central neurocytoma
M. Krech 1, A. Münch2, D. Teichmann1, P. Kuzman3, M. Müther4, K. J. Weber2,5, K. Wenger‐Alakmeh6, J. Onken7, P. Vajkoczy7, F. Behling8, S. A. May9, G. Ntoulias10, J. K. Krauss11, O. Atallah11, M. Esmaeilzadeh11, W. C. Mueller3, F. L. Heppner1,12, H. Radbruch1, W. Stenzel1, A. Koch1,12, D. Capper1,12, D. Kaul13, W. Paulus14, K. H. Plate2,5, R. Beschorner15, J. E. Neumann16,17, C. Hartmann18, C. Thomas14, L. Schweizer2,5
1Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neuropathology, Berlin, Germany; 2University of Frankfurt am Main, Edinger Institute, Institute of Neurology, Frankfurt a. M., Germany; 3University of Leipzig, Paul‐Flechsig‐Institute for Neuropathology, Leipzig, Germany; 4University Hospital Munster, Department of Neurosurgery, Muenster, Germany; 5German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Frankfurt a. M., Germany; 6University Hospital Frankfurt, Institute of Neuroradiology, Frankfurt a. M., Germany; 7Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neurosurgery, Berlin, Germany; 8Universitätsklinikum Tübingen, Department of Neurosurgery, Tuebingen, Germany; 9Klinikum Chemnitz, Department of Neurosurgery, Chemnitz, Germany; 10Vivantes Klinikum Neukölln, Department of Neurosurgery, Berlin, Germany; 11Hannover Medical School, Department of Neurosurgery, Hannover, Germany; 12German Cancer Consortium (DKTK), Partner Site Berlin, German Cancer Research Center (DKFZ), Heidelberg, Germany; 13Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Radiation Oncology and Radiotherapy, Berlin, Germany; 14University Hospital Munster, Institute of Neuropathology, Muenster, Germany; 15Universitätsklinikum Tübingen, Department of Neuropathology, Tuebingen, Germany; 16University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 17University Medical Center Hamburg‐Eppendorf, Center for Molecular Neurobiology Hamburg, Hamburg, Germany; 18Medizinische Hochschule Hannover, Institute for Pathology, Hannover, Germany
Introduction: Central neurocytomas (CN) are intraventricular brain tumors occurring in young adults. In the majority of patients, long‐term prognosis is favorable. However, tumor progression occurs in a considerable fraction of patients. Progression risk is currently assessed based on cellular atypia and/or an elevated Ki67 proliferation index (>3%).
Objectives: We aimed to identify prognostic markers in a series of epigenetically defined CN.
Methods: We analyzed a retrospective cohort of 108 histologically diagnosed CNs by DNA methylation profiling. Follow‐up information was available for 45 patients.
Results: The vast majority of cases were assigned to the methylation class “central neurocytoma” (96/108 cases; 89%), whereas 12/108 cases (11%) were assigned to other methylation classes based on the v12.5 Brain Tumor Classifier. Histologically, cases were previously classified as classical CN (71/96), CN with increased proliferation (10/96) and atypical CN (15/96). In 50/77 cases (65%, NA = 19), a Ki67 >3% was reported. A diagnosis of classical CN was made despite an elevated Ki67 in 25 cases. Interrater reliability between four raters for Ki67 estimation in 10 cases was poor (intraclass correlation coefficient < 0.5). Copy number alterations were observed in 9/96 cases (9%). Median progression‐free survival (PFS) was 72 months, none of the patients died (observation time: 3–141 months). Outcome between classical and atypical CNs (n = 45; median PFS 73 vs. 26 months, p‐value = 0.067) and between ≤3% and >3% Ki67 (n = 45; median PFS NA vs. 72 months, p‐value = 0.44) was not significantly different.
Conclusion: Preliminary data indicate that interrater reliability of Ki67 estimation was poor and diagnostic criteria were inconsistently applied. Histological classification and Ki67 proliferation rate were not associated with PFS in neurocytomas. Further research is necessary to identify novel markers to predict recurrence risk and benefit from adjuvant therapies.
PS6‐NO‐A57
A novel definition of low‐grade astrocytoma IDH‐mutant to inform observational follow‐up and the upcoming era of IDH mutant inhibitors
S. Tran1, A. Thomas2, I. Alouat3, M. Touat4, C. Karachi3, F. Lozano4, K. Mokhtari1, C. Dehais4, L. Feuvret2, C. Carpentier5, M. Giry5, H. Doukani6, J. Lerond5, Y. Marie5, M. Sanson4, A. Idbaih4, A. Carpentier3, K. Hoang‐Xuan4, L. Capelle3, F. Bielle 1
1Sorbonne Université, Neuropathology, Paris, France; 2Sorbonne Université, Radiotherapy, Paris, France; 3Sorbonne Université, Neurosurgery, Paris, France; 4Sorbonne Université, Neurology, Paris, France; 5Paris brain Institute, Paris, France; 6Sorbonne Université, P3S, Paris, France
Intoduction: In resected astrocytoma IDH‐mutant, the distinction between WHO grade 2 and 3 is instrumental to choose between observational follow‐up or adjuvant treatment. Grade 2 is also a criteria for upcoming treatment by IDH‐mutant inhibitors. However, criteria of grade 2 versus 3 have not been updated since the WHO 2007 classification.
Objectives: We measured mitotic activity on a series of resected astrocytoma IDH‐mutant and assessed its prognostic impact.
Patients and Methods: Maximal mitotic activity on consecutive high power fields corresponding to 3 mm2 (MMA) was examined in 118 astrocytoma IDH‐mutant without necrosis nor microvascular proliferation. Impact of MMA on time‐to‐treatment (TTT) and overall survival (OS) and of other candidate prognostic factors (including postsurgical residual tumor volume) were analysed in tumors (i) with ATRX loss, and (ii) without CDKN2A homozygous deletion (HD) nor lesional enhancement. A validation cohort of 81 tumors had the same criteria.
Results: Distribution of MMA among tumors identified a main population of tumors with <6 mitoses while tumors with CDKN2A HD constantly had ≥6 mitoses. The MMA, the post‐surgical residual volume and the plurilobar involvement were independent prognostic factors of TTT (p < 0.0001) among the 75 tumors with post‐surgery observational follow‐up. The threshold of MMA <6 mitoses was identified as the most relevant to predict TTT and OS: median TTT was 55 months for patients with “grade 2” tumors versus 19 months for “grade 3” (p = 0.0057) and median OS was 102 months versus 73 months respectively (p = 0.001). Residual volume <1 cm3 was associated with longer OS (113 months vs. 88 months, p = 0.0021).
Conclusions: A MMA <6 mitoses/3 mm2 identified a main population of low‐grade tumors among astrocytoma IDH‐mutant. The combination of this low‐grade definition and a residual post surgical volume <1 cm3 identifies the best candidates for observational follow‐up with longer TTT and OS.
PS6‐NO‐A58
Beyond IDH1 R132H mutation—Clinicopathological characteristics of non‐canonical IDH mutant gliomas
E. Martinez‐Saez 1, A. Hernández Lain2, N. Vidal3, J. Gama4, E. Rivas5, R. Taipa6, C. Carrato7, J. Pimentel8, J. Ferrer‐Lozano9, M. Varela3, J. Hernandez‐Losa1, J. Camacho‐Soriano1, M. Pinto6, O. Rebelo4, R. Roque8, S. Ramón y Cajal1, O. Toldos‐Gonzalez2
1Vall d'Hebron University Hospital, Pathology, Barcelona, Spain; 212 de Octubre University Hospital, Pathology, Madrid, Spain; 3Bellvitge University Hospital, Pathology, Barcelona, Spain; 4Centro Hospitalar e Universitário Coimbra, Coimbra, Portugal; 5Virgen del Rocío University Hospital, Pathology, Seville, Spain; 6Centro Hospitalar Universitário de Santo António, Porto, Portugal; 7Germans Trias i Pujol University Hospital, Pathology, Badalona, Spain; 8Centro Hospitalar Universitario Lisboa Norte, Lisbon, Portugal; 9La Fe University Hospital, Pathology, Valencia, Spain
Introduction: Isocitrate‐dehydrogenase (IDH) mutations are one of the most important molecular alteration in adult‐type diffuse gliomas (atDG), leading to the 2021 WHO classification into “IDH‐mutant” and “IDH‐wt” entities. The IDH1 p.R132H mutation is the most frequent change, but about 10% of IDH mutations are “non‐canonical” (ncIDHmut) and recent studies suggest their association with a better prognosis, infratentorial location and familial history of cancer. The aim of this study is to describe the clinico‐pathological characteristics of these non‐canonical mutations in our reference population.
Methods: A retrospective multicentric study was performed, involving nine large hospitals in Spain and Portugal. NcIDHmut‐gliomas and classic IDH‐mutant ones (cIDHmut) were identified and clinico‐pathological data were collected.
Results: Ninety‐one gliomas with non‐canonical IDH mutations were found, corresponding to 45 low‐grade (29 astrocytomas‐A, 16 oligodendrogliomas‐O) and 46 high‐grade gliomas (22 A3, 14 A4 and 10 O3). No significant differences in patients’ age, gender, tumor location or survival were found between ncIDH1 and IDH2. Ninety‐one cIDHmut cases were collected, with a similar distribution regarding grade and histology. ncIDHmut patients were significantly younger than cIDHmut ones (p = 0.01). The prognosis of ncIDHmut patients was significantly better than cIDHmut ones (172 vs. 152 months, p = 0.011), only in grade 2 tumors after multivariate analysis. No significant differences regarding infratentorial location or family history of cancer were found.
Conclusions: Our results extend the knowledge about these infrequent tumors, and confirm ncIDHmut as an independent prognostic factor in grade 2 atDG. However, we could not reproduce the predominant infratentorial location or familial history of cancer reported by previous works.
PS6‐NO‐A59
Sirtuin 2 inhibition modulates chromatin landscapes genome‐wide to induce senescence in ATRX‐deficient malignant glioma
P. B. Malgulwar1, C. Danussi2, S. Dharmaiah1, W. Johnson1, A. Rao3, J. Huse 1
1University of Texas MD Anderson Cancer Center, Pathology and Translational Molecular Pathology, Houston, TX, United States; 2Sanofi, Research and Development, Cambridge, MA, United States; 3University of Michigan, Biostatistics, Ann Arbor, MI, United States
Introduction: Inactivating mutations in ATRX characterize large subgroups of malignant gliomas in adults and children. ATRX deficiency in glioma induces widespread chromatin remodeling, driving transcriptional shifts and oncogenic phenotypes. Effective strategies to therapeutically target these broad epigenomic sequelae remain undeveloped.
Materials and Methods: We utilized integrated mulit‐omics and the Broad Institute Connectivity Map (CMAP) to identify drug candidates that could potentially revert ATRX‐deficient transcriptional changes. We then employed disease‐relevant experimental models to evaluate functional phenotypes, coupling these studies with epigenomic profiling to elucidate molecular mechanism(s).
Results: CMAP analysis and transcriptional/epigenomic profiling implicated the Class III HDAC Sirtuin2 (SIRT2) as a central mediator of ATRX‐deficient cellular phenotypes and a driver of unfavorable prognosis in ATRX‐deficient glioma. SIRT2 inhibitors reverted Atrx‐deficient transcriptional signatures in murine neuroprogenitor cells (mNPCs), impaired cell migration in Atrx/ATRX‐deficient mNPCs and human glioma stem cells (GSCs), and increased expression of senescence markers in glioma models. Moreover, SIRT2 inhibition impaired growth and increased senescence in ATRX‐deficient GSCs in vivo. These phenotypic effects were accompanied by genome‐wide shifts in enhancer‐associated H3K27ac and H4K16ac marks, with the latter in particular demonstrating compelling transcriptional links to SIRT2‐dependent phenotypic reversals. Motif analysis of these data identified the transcription factor KLF16 as a mediator of phenotype reversal in Atrx‐deficient cells upon SIRT2 inhibition.
Conclusions: Our findings indicate that SIRT2 inhibition selectively targets ATRX‐deficient gliomas for senescence through global chromatin remodeling, while demonstrating more broadly a viable approach to combat complex epigenetic rewiring in cancer.
PS6‐NO‐A60
Comprehensive genomic profiling of ATRX‐deficient IDH‐wildtype adult high‐grade gliomas reveals clinically relevant genetic patterns
G. Bedics1,2, P. Szőke1, B. Bátai1,2, T. Nagy1,2, G. Papp1, N. Kránitz3, H. Rajnai1, L. Reiniger1, C. Bödör1,2, B. Scheich 1
1Semmelweis University, Department of Pathology and Experimental Cancer Research, Budapest, Hungary; 2Semmelweis University, HCEMM‐SE Molecular Oncohematology Research Group, Department of Pathology and Experimental Cancer Research, Budapest, Hungary; 3County Hospital Győr, Petz Aladár Hospital, County Hospital Győr, Petz Aladár Hospital, Győr, Hungary
Introduction: Glioblastoma, the most common IDH‐wildtype adult high‐grade glioma, frequently harbors mutations in the promoter region of the TERT gene (pTERT) and utilizes the subsequent telomerase‐dependent telomere length maintenance. Rare cases show loss of ATRX protein and is characterized by the related alternative lengthening of telomeres.
Objectives: Genetic patterns of ATRX‐deficient IDH‐wildtype adult high‐grade gliomas are poorly characterized. Thus, we performed the comprehensive genomic profiling (CGP) of a cohort of these tumors in comparison with ATRX‐intact glioblastomas.
Patients and Methods: CGP of 12 ATRX‐deficient and 13 ATRX‐intact IDH‐wildtype adult high‐grade gliomas was performed using the Illumina TruSight Oncology 500 targeted next‐generation sequencing panel.
Results: Mutations in ATRX and pTERT were mutually exclusive in our cohort. Variants of DNMT3A gene were detected exclusively in ATRX‐deficient tumors, while PTEN mutations were confined to the ATRX‐intact glioblastomas. EGFR amplification was more characteristic in the ATRX‐intact, while variants of the RAS‐MAPK pathway including NF1 and BRAF alterations accumulated in the ATRX‐deficient group. High tumor mutational burden accompanied by mismatch repair deficiency was detected in two ATRX‐deficient glioblastomas. One of these showed a peculiar association of oligodendroglioma‐like morphology, mutations of POLE, previously unreported fusions involving the NTRK2 and LRRFIP2 genes and therapy‐induced MLH1 and PMS2 loss. The other case showed loss of MSH2 and MSH6 proteins without genetic alterations in the encoding genes.
Conclusion: To the best of our knowledge, this is the first complex genetic characterization of ATRX‐deficient IDH‐wildtype adult high‐grade gliomas. CGP revealed significant differences in the patterns of affected genes compared to ATRX‐intact glioblastomas. The results suggest that the subgroup of our interest is a promising target of certain future targeted therapies.
PS6‐NO‐A61
Gliomas with immunohistochemical loss of MMR proteins—Clinico‐pathological evaluation, a tertiary care cancer institute experience
S. Epari 1, R. Kaur1, M. Ranade1, A. Chatterji1, A. Sahay1, A. Sahu1, A. Dasgupta1, M. Prasad1, G. Chinnaswamy1, V. Singh1, P. Shetty1, A. Moiyadi1, T. Gupta1
1Tata Memorial Hospital and ACTREC, Tata Memorial Centre, Homi Bhabha National Institute, Mumbai, Pathology, Mumbai, India
Background: Mismatch repair genes altered, Lynch syndrome and Constitutional mismatch repair deficiency syndrome (CMMRD), characterized by mono‐allelic loss and bi‐allelic loss of function of MMR genes, respectively.
Objectives: To evaluate clinico‐pathological features of gliomas with loss of MMR proteins.
Material and Methods: Thirty cases that showed immunohistochemical loss of one/more MMR proteins (MLH1, PMS2, MSH2, MSH6) evaluated for clinico‐pathological features.
Results: Pattern 1 (complete loss of MMR proteins in both tumour and native cells; n = 20): Age‐range: 3–19 years (median: 8; >18 years: 2). Male:female = 1:1. Cerebrum (n = 19) was the commonest location. Café au lait macules (CALM; n = 15), history of consanguinity (h/o CS; n = 9), family history of malignancy (FHM; n = 9) and other malignancies (n = 3) were observed. All showed high grade astrocytic histology morphology with bizarre giant cells (n = 16) and relative undifferentiated morphology (n = 9). Most were positive for p53 immunohistochemistry (n = 18) and 11 showed ATRX loss. Combined MLH1 and PMS2 loss (n = 8), isolated PMS2 loss (n = 8); combined MSH2 and MSH6 loss (n = 1) and isolated MSH2 loss (n = 1) was observed. Pattern 2 (loss in tumour cells only; n = 10): Age‐range: 1–44 years (median: 11; >18 years:4). Male:female = 1.5:1. Cerebrum (n = 9) was the commonest location. CALM (n = 5), h/o CS (n = 2), FHM (n = 3) and other malignancies (n = 1) were noted. All showed high grade astrocytic histology with bizarre giant cells (n = 3) and relative undifferentiated morphology (n = 1). Most were p53 positive (n = 10) and showed retained ATRX expression (n = 9). Isolated MSH6 loss (n = 4); combined MSH2 and MSH6 loss (n = 3); combined MLH1 and PMS2 loss (n = 2), and isolated MLH1 loss (n = 1) was observed.
Conclusion: MMR protein deficient tumors are commonly high grade glial with presence of giant cells, affecting children and young adults. Loss of PMS2 is commonest in CMMRD phenotype, while MSH6 in Lynch phenotype.
PS6‐NO‐A62
Proteome signatures are closely associated with histomorphology in embryonal tumors with multilayered rosettes (ETMR)
M. Dottermusch 1,2, A. Biabani3, H. Voß3, D. Obrecht4, S. Frank5, M. M. Dorostkar6, U. Schüller2,4,7, J. E. Neumann1,2
1University Medical Center Hamburg‐Eppendorf, Center for Molecular Neurobiology (ZMNH), Hamburg, Germany; 2University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 3University Medical Center Hamburg‐Eppendorf, Section of Mass Spectrometric Proteomics, Hamburg, Germany; 4University Medical Center Hamburg‐Eppendorf, Department of Pediatric Hematology and Oncology, Hamburg, Germany; 5University Hospital Basel, Division of Neuropathology, Basel, Switzerland; 6Ludwig‐Maximilians‐University, Center for Neuropathology and Prion Research, Munich, Germany; 7Children's Cancer Research Center Hamburg, Hamburg, Germany
Introduction: Embryonal tumors with multilayered rosettes (ETMR) are rare malignant brain tumors, which mainly occur in infants. Three histomorphological ETMR variants have been described, all of which harbor a devastating prognosis for the young patients: embryonal tumor with abundant neuropil and true rosettes (ETANTR), ependymoblastoma (EBL), and medulloepithelioma (MEPL). Comprehension of ETMR molecular biology is currently restricted to only few previous molecular studies, which—as of today—have lacked proteome investigations. In this study, we aimed to explore the proteome landscape of ETMR.
Methods: We compiled formalin‐fixed paraffin‐embedded tumor tissue from a case series of 16 molecularly confirmed ETMR. Liquid chromatography coupled with tandem mass spectrometry (LC‐MS/MS) was applied for protein quantification of representative tumor samples. Additionally, proteome data were acquired from microdissected, morphologically distinct tumor areas in three ETMR with prominent intratumoral morphological heterogeneity.
Results: Unsupervised cluster analysis of proteome data grouped ETMR samples according to histomorphology, separating neuropil‐rich tumors (ETANTR) from tumors with primitive and undifferentiated morphology (MEPL and EBL). Differential protein analyses confirmed a neuronal‐like proteome signature in the neuropil‐rich tumors. Conversely, an abundance of proteins involved in DNA metabolism and chromosome organization was found in the undifferentiated tumors. Microdissection analyses attested high concordance of inter‐ and intratumoral morphology‐associated proteome heterogeneity. Moreover, the impact of tumor morphology overpowered the impact of tumor identity on the proteome signature.
Conclusions: Histomorphology and proteome signatures are closely related in ETMR. Ongoing investigations aim to identify the clinical impact of morphology‐associated ETMR proteomics and uncover novel therapeutic vulnerabilities in these deadly tumors.
PS6‐NO‐A63
Adult medulloblastoma—Clinico‐molecular spectrum, an institutional experience
V. Adhvaryu 1, M. Gurav2, G. Deshpande1, R. Rumde2, O. Shetty2, A. Sahay1, A. Dasgupta3, A. Chatterji3, T. Gupta3, P. Shetty4, A. Moiyadi4, S. Epari1
1Tata Memorial Centre, Pathology, Mumbai, India; 2Tata Memorial Centre, Molecular Pathology, Mumbai, India; 3Tata Memorial Centre, Radiation Oncology, Mumbai, India; 4Tata Memorial Centre, Neurosurgery, Mumbai, India
Introduction: Medulloblastoma (MB) is uncommon and molecularly lesser known in adults than their pediatric counterparts.
Objectives: To study the histomorphology and molecular grouping of adult MB and correlate with various clinical features.
Methodology: One hundred and thirteen cases of MB in >18 years were included. Molecular grouping (WNT‐activated, SHH‐activated, non‐WNT/non‐SHH, gp 3 and non‐WNT/non‐SHH, gp 4) was done by gene expression.
Results: Age‐range was 19–59 years; 60.3% (64/106) were lateralized. 58 (51.3%) were classic, 27 desmoplastic (D/N; 23.9%), 8 paucinodular (7.1%), 7 large cell/anaplastic (LCA; 6.1%), and 13 unclassified (11.5%). 64.8% (59/91) were SHH‐activated; 14.3% (13/91) and 9.9% (9/91) were WNT and gp 4 respectively, 3 were of gp 3 and 6 were unclassifiable. All D/N cases were SHH; while LCA had SHH, WNT and gp3 (see Figure 1). p53‐mutant pattern of immunopositivity was observed in 7/113 (6.2%; 3—SHH; 1—WNT; 1—gp3; 2—not known). Of the three lateralised LCA, two were SHH‐activated TP53‐mutant and one WNT‐activated. Within the SHH group, p53 mutant pattern was noted in five and one was MYCN‐amplified. SHH group had a 2‐year survival rate of 95.2% followed by WNT (71.1%) and gp 4 (66.7%). Twenty‐four of SHH had progression—14 local, 8 spinal, 2 intracranial, and 2 extracranial (skeletal and nodal). The mean disease‐free survival for SHH‐activated TP53‐mutant and MYCN‐amplified cases was 21 months against 43.3 months for other SHH cases and 16.8 months for gp 3. In WNT, both monosomy 6 and CTNNB1 mutation were seen in five cases and one case each had an isolated alteration. Anaplastic histology and TP53 mutation did not affect survival of WNT.
Conclusion: SHH‐activated is the most common adult MB molecular group; p53 diffuse immunopositivity and MYCN amplification showed worser biology. LCA and p53 positivity did not affect survival in WNT‐activated group. Gp 3 is very rare but not non‐existent in adults.

FIGURE 1.
PS6‐NO‐A64
DNA methylation profiling of adult spinal glial tumours—Results from a large single centre study
M. Clarke 1,2, R. Pereira1, A. Mackay1, Y. Grabovska1, R. Cruickshank2, M. Dutt2, P. Mariathasan2, A. Kumar3, A. Casey2, A. Merve2,3, Z. Jaunmuktane2, C. Jones1, S. Brandner2
1Institute of Cancer Research, London, United Kingdom; 2University College London Hospitals NHS Foundation Trust, Neuropathology, London, United Kingdom; 3Great Ormond Street Hospital for Children NHS Foundation Trust, London, United Kingdom
Question: Glial tumours can occur in any central nervous system location, including the spinal cord. Although rare, spinal gliomas can represent a significant diagnostic challenge and are recognised as separate tumour types in the WHO classification. This study used DNA methylation profiling to characterise adult spinal glial tumours from a large neurosurgical centre, exploring relative frequencies, and the value of this technique in diagnostic workflows.
Methods: A search in our laboratory information management system (2006–2021) identified 116 tumours, from patients aged 17.2–79.2 years. Diagnoses included ependymomas (all grades/subtypes) and other high‐ or low‐grade gliomas (HGG/LGG). Extrinsic tumours (metastases, meningiomas, schwannomas) were excluded. DNA underwent methylation profiling (Illumina EPIC BeadArrays, n = 116). iDat files were processed using the brain tumour classifier (MNP v12.5 R package), classifying cases against a reference cohort (n = 2800). Longitudinal (n = 8) and poor QC cases (n = 3) were excluded.
Results: 83% (n = 87) classified as an ependymoma (myxopapillary ependymoma [EPN_MPE, n = 44], spinal ependymoma [n = 43], spinal subependymoma [n = 1]). We identified HGGs that were not diagnosed histologically (diffuse midline glioma, H3 K27‐altered [n = 2], high‐grade astrocytoma with piloid features [n = 1]) and 41% of cases (n = 18/44) diagnosed histologically as an ependymoma, CNS WHO grade 2, classified as EPN_MPE. LGGs were less frequent (pilocytic astrocytoma [n = 3], pleomorphic xanthoastrocytoma [n = 1], rosette‐forming glioneuronal tumour [n = 1]). Nine per cent (n = 9) did not classify with existing methylation classes. Copy number analysis revealed subtype‐specific changes, including prognostic alterations.
Conclusion: In conclusion, this single‐centre study highlights the crucial role of DNA methylation profiling as part of diagnostic workflows for spinal glial tumours.
PS7‐NO‐A65
Leveraging attention‐based convolutional neural networks for meningioma classification in computational histopathology
J. Sehring 1, H. Dohmen1, C. Selignow1, K. Schmid1, S. Grau1, M. Stein1, E. Uhl1, A. Mukhopadhyay2, A. Nemeth1, D. Amsel1, T. Acker1
1Justus‐Liebig‐University Giessen, Neuropathologie, Giessen, Germany; 2Technische Universität Darmstadt, Informatik, Darmstadt, Germany
Introduction: Convolutional neural networks (CNNs) have emerged as powerful tools in computational histopathology, enabling precision medicine through image analysis. Accurate grading and classification of meningiomas, the most common primary intracranial tumors, are critical for informed clinical decision‐making. DNA methylation‐based molecular classification has shown superior predictive accuracy for meningioma recurrence; however, it is expensive and not widely accessible. Thus, a digital histology‐based method for predicting DNA methylation classes would be advantageous, complementing molecular classification.
Objectives: Our objective was to develop and evaluate an attention‐based multiple‐instance deep neural network for predicting meningioma methylation classes.
Materials and Methods: We utilized tumor methylome data from 142 (+51) patients and corresponding hematoxylin‐eosin‐stained histological sections. Pairwise analysis of sample cohorts across three meningioma methylation classes was performed, followed by performance validation using an independent dataset of 51 meningioma patient samples.
Results: Pairwise analysis yielded high accuracy in two combinations of meningioma methylation classes. Attention map visualization revealed that the algorithm primarily focuses on tumor regions considered significant by neuropathologists, providing insight into the CNN's decision‐making process.
Conclusion: Our study demonstrates the potential of CNNs to effectively extract phenotypic information from histological sections using computerized images, thereby advancing precision medicine. The proposed AI framework holds considerable promise for supporting, enhancing, and expediting meningioma classification in the future.
PS7‐NO‐A66
Morphology‐based molecular classification of spinal cord ependymomas using deep neural networks
Y. Schumann 1, M. Dottermusch2,3, L. Schweizer4, M. Krech5, U. Schüller2,6, J. E. Neumann2,3, P. Neumann1
1Helmut‐Schmidt University, Chair for High Performance Computing, Hamburg, Germany; 2University Medical Center Hamburg‐Eppendorf, Institute for Neuropathology, Hamburg, Germany; 3University Medical Center Hamburg‐Eppendorf, Center for Molecular Neurobiology, Hamburg, Germany; 4University Medical Center Frankfurt, Neuroscience Center, Frankfurt a. M., Germany; 5Charité—Universitätsmedizin Berlin, Institute for Neuropathology, Berlin, Germany; 6University Medical Center Hamburg‐Eppendorf, Forschungsinstitut Kinderkrebs‐Zentrum, Hamburg, Germany
Introduction: Ependymomas (EPNs) are neuroepithelial neoplasms of the central nervous system and are broadly distinguished into 10 main molecular types based on methylation profiles. Current standards in diagnostics often combine molecular analyses with histological characterization, for example, using hematoxylin‐ and eosin‐staining (HE). However, recent studies have hinted towards frequent mismatch between the assigned methylation classes and histological EPN diagnoses.
Objective: Focusing on two molecularly defined EPN types of the spinal cord “myxopapillary (SP‐MPE)” and “spinal (SP‐EPN),” we aimed to resolve the relation of morphological and DNA‐methylation patterns by employing deep‐learning techniques to predict the molecular type from HE‐stained whole‐slide images (WSIs).
Materials and Methods: We collected a cohort of HE‐stained WSIs from 139 patients who were diagnosed with either SP‐MPE or SP‐EPN using methylation profiling. For classification, we combined siamese representation learning and attention‐based multiple instance learning.
Results: Our approach yielded reliable predictions of the molecular type (up to 98% accuracy), thereby improving over the accuracy of histomorphological assessment by human pathologists. Using dedicated encoders instead of transfer learning proved to be a key aspect for enhanced classification performance. We applied our approach to various magnifications of the WSIs and utilize attention scores to provide a comprehensive explanation of histologic features which are relevant for assigning the correct molecular subtype.
Conclusions: In summary, we established an interpretable method to reliably predict molecular types of spinal cord EPNs from whole‐slide images. As HE‐stained WSIs are increasingly available in the era of digital pathology, our approach provides a fast and inexpensive way for first assessment of molecular EPN classification and may prospectively enable rapid decisions on patient‐specific treatment.
PS7‐NO‐A67
A deep learning‐approach to infer somatic alterations in glioma using digital tissue slides
B. Kriener 1,2, S. Mueller3, S. M. Waszak3,4,1,2
1Oslo University Hospital, Oslo, Norway; 2Center for Molecular Medicine Norway, University of Oslo, Oslo, Norway; 3University of California, San Francisco, Department of Neurology, San Francisco, CA, United States; 4École Polytechnique Fédérale de Lausanne (EPFL), Swiss Institute for Experimental Cancer Research (ISREC), Lausanne, Switzerland
Introduction: Precision medicine in neuro‐oncology requires deep understanding of molecular changes present in tumor cells due to the large variety of brain tumor types. Optimal diagnostic workflows combine classical histopathology and deep molecular profiling. However, many patients currently do not benefit from modern therapies due to lack of sufficient tissue, but also costs and access to deep molecular tumor profiling. In recent years computer vision and deep learning methods showed it is feasible to predict molecular data directly from digitized tumor tissue slides for several cancer types.
Objective: To develop a deep learning‐based digital neuro‐pathology workflow that enables prediction of molecular phenotypes from digital tissue slides and to aid treatment decisions for patients with little amount of tumor tissue.
Materials and Methods: Diagnostic tissue slides stained with hematoxylin and eosin (H&E) and patient‐matched DNA sequencing‐derived genomic profiles were obtained from 41 hospitals and 800 patients with adult‐type diffuse glioma. We addressed challenges arising from data domain shifts using new augmentation strategies and how to transfer predictive models to novel sites.
Results: WHO2021‐defined adult‐type diffuse gliomas (n = 3), somatic alterations in glioma driver genes (n = 16), and chromosomal alterations (n = 17) can be learned from diagnostic tissue slides. Good to high predictive performance (AUC > 0.75) was obtained to distinguish adult‐type diffuse gliomas (AUC 0.85–0.95), somatic driver alterations in IDH1, IDH2, EGFR, CDKN2A, TP53, and CIC, and somatic copy number alterations on chromosomes 1, 7, 10, and 19.
Conclusion: We demonstrate that clinically relevant genomic biomarkers can be learned from routine diagnostic tissue slides for patients with adult‐type diffuse glioma, thus potentially enabling access to targeted therapies for a larger patient population.
PS7‐NO‐A68
brAIn App—A versatile smartphone app to annotate histopathological images for enhanced AI training and medical education
M. Dudde1, F. Dörmer1, J. Sehring1, K. Schmid1, N. Heller2, K. Sohrabi2, H. Dohmen1, T. Acker1, D. Amsel 1
1Justus‐Liebig‐University Giessen, Neuropathologie, Giessen, Germany; 2Technische Hochschule Mittelhessen, Medizininformatik, Giessen, Germany
Introduction: Digital pathology and whole slide images are increasingly used in histopathological analysis. While existing software can classify tissues as tumor or non‐tumor and count mitosis, the efficacy of artificial intelligence algorithms relies heavily on the quality of their training data. Recognizing morphological changes and patterns also poses a significant challenge for medical students.
Objectives: Here, we present a novel method for training AI algorithms using a smartphone app, which enables the generation of potentially infinite crowd‐sourced annotations. Simultaneously, the app provides medical students access to real‐world diagnostic data for educational purposes, as opposed to polished textbook images.
Materials and Methods: The brAIn app was developed using Flutter, ensuring compatibility with both iPhone and Android systems. Training modules for specific histological features can be easily created by depositing images in a predefined folder structure within an accessible file system. Users confirm the presence or absence of specific morphological characteristics through binary decisions using a swipe function.
Results: The brAIn app facilitates learning and crowdsourcing for binary classification of images. The annotation mode generates a well‐characterized dataset for developing AI algorithms, while simultaneously enabling medical student to deepen their understanding of histopathology.
Conclusion: We demonstrate the dual advantage of crowd sourcing in generating valuable annotated data for AI algorithm training and enhancing the learning experience of medical students. This innovative approach holds significant potential for improving AI‐driven histopathological analysis and medical education.
PS7‐NO‐A69
Crowd powered neuropathology annotations for machine learning algorithms—A citizen science pilot study focused on the Hispanic community
P. Michelucci1, L. Gusman1, M. Lane1, R. Dussaruth1, G. Vaičaitytė1, J. Lou2, S. Magaki3, L. Minaud4, M. Keiser4, B. Dugger 5
1Human Computation Institute, Ithaca, NY, United States; 2University of California, Irvine, Pathology and Laboratory Medicine, Irvine, CA, United States; 3University of California, Los Angeles, Pathology and Laboratory Medicine, Los Angeles, CA, United States; 4University of California, San Francisco, San Francisco, CA, United States; 5University of California, Davis, Pathology and Laboratory Medicine, Sacramento, CA, United States
Introduction: There is a need to provide more objective finer grained pathological evaluations in a scalable manner as well as increase community outreach and education especially within the Hispanic community.
Objective: To fill these gaps, we piloted a citizen science project involving new human computation methods to engage public volunteers in the histopathological analysis of whole slide images (WSI) of human brain.
Materials and Methods: Our study developed a pipeline to break down histopathological analysis into a step‐wise series of manageable online tasks to be accomplished by non‐expert members of the general public. We incorporated “wisdom of crowd” methods for each step of the analysis combining individual answers into a single expert‐like answer. This pilot compared the two‐stage crowd‐based analysis to gold standard data generated by experts for two major pathology categories: cored plaques and cerebral amyloid angiopathy.
Results: Through methodological development, including testing of annotation interfaces and consensus methods (Figure 1), we found with sufficient aggregation of non‐expert answers, it is possible to consistently achieve a level of agreement with gold standard data equivalent to interrater agreement among expert annotators (Figure 2).
Conclusions: These approaches support the rapid production of high‐volume datasets for use in machine learning algorithm development to provide deeper phenotyping of neurodegenerative diseases. These pilot results support the plausibility of moving forward with an openly available online platform, which will be used to execute the first ever de novo analysis of Alzheimer's histopathology imagery by a crowd of volunteers (geared towards those of Hispanic heritage). The platform will engage Hispanic communities directly impacted by this research, while providing a culturally responsive outreach and inclusion program for these communities to represent themselves in discussions with researchers.


PS7‐NO‐A71
Outsourcing of molecular testing for CNS tumors in the era of integrated molecular diagnosis—An experience from King Hussein Cancer Center
M. Al‐Hussaini 1, R. Alabweh1, N. Hasasna1, S. Alyazjeen1
1King Hussein Cancer Center, Pathology and Laboratory Medicine, Amman, Jordan
The diagnosis of CNS tumors in adults and children is becoming complex and requires a correlation between clinical, radiological, histopathology, immunohistochemistry, and more recently molecular findings, which might be challenging in the setting of countries with limited resources. This is a retrospective study of cases outsourced for molecular testing in patients diagnosed with CNS tumors. Eight‐three patients are included over 2021–2023, with a mean age of 10 years. The largest group was medulloblastoma (n = 36, 43.4%), followed by low‐grade glioma/glioneuronal tumors (n = 24, 28.9%), and high‐grade glioma (n = 13, 15.7%). Tests required were medulloblastoma subgrouping, low‐grade fusion gene analysis (inc BRAF fusion) for low‐grade glioma, and Trusight pan‐cancer RNAseq panel clinical test for high‐grade glioma. The turnaround time from shipping the samples to receiving the results was 74.5 calendar days, with a total cost of 133,000 US$ (122,000 Euro). Out of all the samples sent, there were 2 cash patients who refused to pay due to the unaffordable cost of the test, 3 samples were lost during shipping, and 11 were resent due to inadequate tissue or poor quality. There was one major change in diagnosis in an embryonal tumor from BCOR sarcoma to an undifferentiated solitary fibrous tumor (NAB2::STAT6 fusion). For the low‐grade glioma there were 7 KIAA1549(ex16)::BRAF(ex09) fusion, 2 BRAFp.V600E, 1 BRAFp.G469.A SNV, 1 BRAFp.K601E SNVs, 2 FGFR, 2 NF‐1, 1 MYB::PCDHGA1 fusion, for which most patients received compassionate targeted treatment. For the medulloblastoma, there were 5 WNT, 12 SHH (including 7 p53mutant), 5 group3, 6 group‐4, 2 None3‐none4, 1 failed, and 3 without available results. Outsourcing molecular testing is an option for better assessment and management of CNS tumors. Challenges encountered include cost, long TAT, and potential loss of specimens. Providing targeted treatment for low‐grade glioma is the most notable advantage for our patients.
PS7‐NO‐A72
Comparing p16 and MTAP loss of expression in detecting CDKN2A homozygous deletion in pleomorphic xanthoastrocytoma
M. A. Vizcaino 1, C. Zepeda Mendoza1, R. Vaubel1, A. T. Nguyen1, J. A. Trejo‐Lopez1, A. Raghunathan1, S. Jenkins2, R. Jenkins1, C. Giannini1
1Mayo Clinic, Department of Laboratory Medicine and Pathology, Rochester, MN, United States; 2Mayo Clinic, Department of Research Services, Rochester, MN, United States
Introduction: Pleomorphic xanthoastrocytoma (PXA) is a rare, circumscribed glioma characterized by frequent CDKN2A homozygous deletion (HD) (>90%) resulting in loss of p16 expression. Loss of MTAP expression has been proposed as a surrogate marker for CDKN2A HD, since deletions of MTAP, located on chromosome 9p21 ~100 kb telomeric to CDKN2A, frequently co‐occur with CDKN2A HD. This raises the question of whether MTAP loss may be used by itself and/or in conjunction with p16 to predict CDKN2A status in PXA by immunohistochemistry (IHC).
Objectives: To compare p16 and MTAP loss by IHC in a PXA cohort in detecting CDKN2A HD and to determine if IHC can be used as a surrogate marker for CDKN2A HD.
Methods: Thirty‐seven PXA cases (23 WHO grade 2, 14 grade 3) with available chromosomal microarray data from previous studies and our clinical practice (ThermoFisher, OncoScan™ CNV Assay with 50–100 kb copy number resolution in ~900 cancer genes, including detection of CDKN2A/B homozygous/hemizygous deletions) were evaluated for p16 (clone E6H4, Ventana) and MTAP (clone 2G4, Abnova) by IHC. CDKN2A/B and MTAP deletion status by microarray and expression of p16 and MTAP (present/absent) by IHC were blindly assessed by independent reviewers.
Results: CDKN2A HD was present in 37 cases (100%), CDKN2B HD in 36 (97.3%) and MTAP HD in 23 (62.2%). MTAP HD was absent in 5 cases and uncertain in 9. P16 expression was lost in 34 (of 37) cases, equivocal in 1 and failed in 2, while MTAP expression was lost in 27 (of 37) cases, retained in 9 and equivocal in 1 resulting in a sensitivity of p16 and MTAP IHC in detecting CDKN2A HD respectively of 91.9 and 73.0%. Positive predictive value was 100% for both. MTAP expression was lost in the 2 cases in which p16 IHC failed with a combined (p16 and/or MTAP loss of expression) sensitivity of 97.3%.
Conclusions: Combined p16 and MTAP IHC accurately detected CDKN2A HD, but MTAP IHC alone showed a low sensitivity in detecting CDKN2A HD.
eP‐NO‐A73
Glioma diagnosis in the genomic era—Gene panel NGS as a key tool
L. R. S. Lam 1, R. C. M. Shek1, Y. H. Lui1
1Pamela Youde Nethersole Eastern Hospital, Department of Clinical Pathology, Hong Kong, Hong Kong
Background and Objectives: The 5th edition of the WHO Classification of Tumors of the Central Nervous System (CNS) emphasizes the crucial role of molecular diagnostics in classification of gliomas. We report on the establishment and validation of gene panel next generation sequencing (NGS) for the molecular diagnostics of diffuse gliomas.
Method: A cohort of formalin‐fixed paraffin‐embedded tissue samples of diffuse glioma cases was analyzed by NGS using a targeted assay (Oncomine Comprehensive Assay Plus, on Ion GeneStudio S5 Prime System [Thermo Fisher Scientific]) that provides comprehensive genomic profiling covering more than 500 genes. A custom filter was designed to facilitate the identification of genetic aberrations relevant to glioma. Single‐nucleotide variants (SNVs), short insertions and deletions (indels) and copy number variations (CNVs) detected by NGS were validated by single gene analyses.
Result: NGS data obtained from the analysis of 22 samples of diffuse glioma allowed for their molecular classification into distinct biological groups, including (i) isocitrate dehydrogenase gene (IDH) 1 or 2 mutant astrocytoma with frequent α‐thalassemia/mental retardation syndrome X‐linked (ATRX) and tumor protein p53 (TP53) gene mutations, (ii) oligodendroglioma, IDH‐mutant and 1p/19q‐codeleted, with frequent telomerase reverse transcriptase (TERT) promoter mutation, (iii) glioblastomas, IDH‐wildtype, with or without epidermal growth factor receptor (EGFR) amplification or TERT promoter mutation, as well as (iv) diffuse midline glioma, H3 K27‐altered.
Conclusion: Our findings proved gene panel NGS as a promising technique which allows a single assay solution for molecular characterization required for integrated glioma diagnosis. The results support its use in routine diagnostic service. Further optimization and validation of diagnostic relevant copy number variations are in progress.
eP‐NO‐A74
Clinical, pathological and genomic features of infratentorial IDH‐mutant gliomas
L. Wang 1
1Xuanwu Hospital, Pathology, Beijing, China
Isocitrate dehydrogenase (IDH) 1/2 mutations are rare in infratentorial gliomas, which of clinico‐molecular characteristics of infratentorial IDH‐mutant gliomas have not been well characterized. In the current study, a series of 12 cases of infratentorial IDH‐mutant gliomas were described for clinical, pathological, and genomic characteristics. The median age of this cohort at diagnosis was 41‐year‐old (range: 10–67). Nine tumors were located in posterior fossa, including 5 (41.7%) were only in the brainstem and 4 (33.3%) were present in both brainstem and cerebellum, and 3 (25%) in spinal cord. Histopathologic diagnosis of twelve cases is all diffuse astrocytoma. Eight cases were low‐grade astrocytoma (WHO grade 2) including one with concomitant KIAA1549‐BRAF fusion and IDH mutation in pediatric spinal cord astrocytoma, and four high‐grade astrocytoma (WHO grade 3). Comprehensive genomic profiling revealed that non‐canonical IDH (50%, 6/12) and TP53 (75%, 9/12) mutations were more frequent in infratentorial IDH‐mutant astrocytomas than supratentorial cases. While ATRX mutation (33.3%, 4/12) and MGMT promoter methylation (41.7%, 5/12) were less frequent (p < 0.005). No mutations of H3.1, H3.3, TERT, homozygous deletion of CDKN2A/B, or co‐deletion of 1p/19q were detected. Our data revealed infratentorial IDH‐mutant gliomas have distinct clinical, pathological, molecular, and prognostic characteristics, differed from supratentorial cases.
eP‐NO‐A75
Clinicopathological characters of lymphomatosis cerebri
Y. J. Fu 1, Z. L. Zhao1, B. Cui1, D. H. Lu1, Y. S. Piao1
1Xuanwu Hospital, Pathology, Beijing, China
Objective: Lymphomatosis cerebri is a special type of primary central nervous system lymphoma, which involves the central nervous system diffusely, especially white matter, and the differential diagnosis is complex and diverse. This article summarizes and analyzes the clinicopathological characteristics of 11 cases of lymphomatosis cerebri, in order to provide ideas for clinical diagnosis and treatment.
Methods: The clinical, radiological and pathological data of 11 patients with lymphomatosis cerebri diagnosed in our hospital from January 2020 to April 2023 were retrospectively analyzed.
Results: Among the 11 patients, 4 were males and 7 were females, aged 29–68 years, and the median age was 61 years. Clinical symptoms include progressive cognitive dysfunction, behavioral changes, and gait abnormalities. On radiology, all 11 cases showed diffuse and multiple lesions of the brain, mainly white matter involvement, low density on CT, iso‐ or hypo‐intense signal on T1WI, hyperintense signal on T2WI and FLAIR, and the enhancement area was significantly limited. Ten cases were stereotactic needle biopsy specimens, and one case was a craniotomy excision specimen. The histological diagnosis was diffuse large B‐cell lymphoma, combined with clinical and radiological findings, consistent with primary central nervous system lymphoma and lymphomatosis cerebri.
Conclusion: Lymphomatosis cerebri is a diffuse lesion involving the central nervous system, mainly white matter involvement, subacute or rapidly progressive cognitive dysfunction as its prominent clinical feature, involving complex and diverse differential diagnosis, stereotactic needle biopsy provides the possibility for obtaining a definitive diagnosis, and early identification of pathological diagnosis is the key to ensure accurate clinical treatment.
eP‐NO‐A76
Uncovering a novel population of proliferative cells defined by the expression of BCAS1 in glioblastoma
R. Morales‐Gallel 1, M. J. Ulloa‐Navas2, R. Prat‐Acín3, G. Reynés‐Muntaner3, V. Capilla‐González4, J. Ferrer‐Lozano3, J. M. García‐Verdugo1
1Institute Cavanilles of Biodiversity and Evolutionary Biology, University of Valencia, Paterna, Spain; 2Mayo Clinic, Department of Neuroscience, Jacksonville, FL, United States; 3Hospital Universitari i Politècnic La Fe, Valencia, Spain; 4Andalusian Center for Molecular Biology and Regenerative Medicine (CABIMER), Seville, Spain
Question: Glioblastoma (GB) is the most common and aggressive malignant primary brain tumor in adults with no satisfactory treatment available. Therefore, identifying novel markers and targets is critical to develop more direct and specific treatments. Brain Enriched Myelin Associated Protein 1 (BCAS1) defines an immature oligodendrocyte population in healthy human brain and has emerged as a novel marker of tumorigenesis in non‐central nervous system. However, the role of BCAS1 in brain tumors is still uncertain. In this study, we investigated whether BCAS1 is expressed in patient‐derived GB samples and contributed to uncover the identity and proliferative state of BCAS1+ cells.
Methods: We analyzed BCAS1 expression in tumor tissue from patients with GB (n = 60), from the edge and core region. We characterized this cell population by immunohistochemistry and immunofluorescence, co‐staining BCAS1 with markers of oligodendroglial cells (Olig2, SOX10), stemness (PDGFRa, EGFR), invasion (Vimentin, CXCR4), and proliferation (Ki67). Additionally, we performed immunoelectron microscopy to determine the ultrastructure of BCAS1+ cells and BCAS1 subcellular localization.
Results: Our results show that BCAS1+ cells constitute a heterogeneously distributed oligodendrocyte‐like population in GB with stellate or spherical morphology. Stellate cells are proliferative cells located in the tumor core that form large groups of cells close to blood vessels. In contrast, spherical cells appear isolated or forming small groups of 2–5 cells in the tumor edge, which is characterized by presenting an abundant network of BCAS1+ filaments. Importantly, both BCAS1+ cell morphologies found in GB differ from the morphology described in BCAS1+ cells in the healthy human tissue.
Conclusions: Our results suggest that BCAS1 is a key marker that defines a proliferative cell population within the tumor core. Further investigations will help to elucidate the role of BCAS1+ cells in GB progression.
eP‐NO‐A77
Eight cases of Lynch syndrome‐associated glioblastomas
Z. Yao 1,2, W. J. Wen3, Y. J. Xue1, Z. M. Zheng4, Y. C. Nie1, M. Q. Zhao5, Z. Wang1, G. H. Zhang6, D. Z. Wang7,8
1Shandong Provincial Hospital Affiliated to Shandong First Medical University, Pathology, Jinan, China; 2Shandong Provincial Hospital, Cheeloo College of Medicine, Shandong University, Pathology, Jinan, China; 3Liaocheng People's Hospital, Pathology, Liaocheng, China; 4Shandong Provincial Hospital Affiliated to Shandong First Medical University, Neurosurgery, Jinan, China; 5Shandong Cancer Hospital and Institute, Shandong First Medical University and Shandong Academy of Medical Sciences, Pathology, Jinan, China; 6The First Affiliated Hospital of Shandong First Medical University and Shandong Provincial Qianfoshan Hospital, Pathology, Jinan, China; 7Taihe Hospital, Hubei University of Medicine, Pathology, Shiyan, China; 8Taihe Hospital, Hubei University of Medicine, Taihe Clinical Molecular Diagnostic Center, Shiyan, China
Question: Lynch syndrome (LS) is an inherited disorder that increases the risk of many types of cancer. Identifying LS‐associated glioblastoma (GBM) is crucial for early diagnoses and cancer surveillance of at‐risk family members.
Methods: We assessed mismatch repair (MMR) status using immunohistochemistry (IHC) staining. MGMT promoter (MGMTp) methylation was determined by pyrosequencing. TERTp mutations (C228/C250) were detected by Sanger sequencing. EGFR, 1p/19q, and CDKN2A were detected via FISH. Germline mutations were analyzed using NGS and Sanger sequencing.
Results: We identified eight cases of LS‐associated GBM, including six women and two men with an average age of 55 years. The most common clinical symptoms were headaches and cognitive impairment. Tumors were predominantly located in the temporal and frontal lobes, ranging in size from 3.0 to 8.7 cm. Morphologically, seven cases showed bizarre giant cells and/or (wreath‐shaped) multinucleated cells (Figure 1). Recurrent GBM in Case 2 (2R) displayed spindle cells arranged in a fascicular pattern (Figure 1C). IHC staining revealed combined MSH2/MSH6 loss in six cases, MLH1/PMS2/MSH6 loss in one case, and isolated PMS2 loss in one case (Table 1). TP53 mutation was detected in seven cases. Variable MGMTp methylation and CDKN2A homozygous deletion were observed, but TERTp mutation, 1p/19q co‐deletion, and IDH mutation were not detected in any of the eight cases. All eight cases had personal and/or family histories of cancers, fulfilling the revised Bethesda criteria. Germline MMR gene testing revealed pathogenic variants in four cases.
Conclusion: The presence of abundant bizarre giant and/or multinucleated cells in GBM should remind pathologists to perform IHC staining to evaluate MMR status and determine the necessity of further germline testing and genetic counseling.

FIGURE 1. HE stainings of GBMs. Bar = 50 μm.

TABLE 1. Genetic alterations in GBMs.
eP‐NO‐A78
Machine learning‐based assessment of intratumor heterogeneity in glioblastoma
D. Hieber 1,2,3, G. Prokop4, M. Karthan2,3, B. Märkl1, J. Schlegel4, R. Pryss3, G. Grambow5, J. Schobel2, F. Liesche‐Starnecker1
1University of Augsburg, Pathology, Medical Faculty, Augsburg, Germany; 2Neu‐Ulm University of Applied Sciences, Institute DigiHealth, Neu‐Ulm, Germany; 3University of Würzburg, Institute of Clinical Epidemiology and Biometry, Wuerzburg, Germany; 4Technical University of Munich, Department of Neuropathology, Munich, Germany; 5Aalen University of Applied Sciences, Aalen, Germany
Introduction: Currently, there exist no standardized approaches to objectively and reproducibly determine the intratumor heterogeneity of glioblastoma (GBM). Instead, neuropathologists manually analyze GBM in a time‐consuming and error‐prone process with no guarantee of exact reproducibility.
Objectives: To objectively determine the heterogeneity of GBM, a machine learning (ML) model is trained based on whole slide images (WSI) of hematoxylin and eosin (HE) stained slides. The model shall be able to reproducibly determine the heterogeneity of GBM without any additional input.
Material and Methods: Based on 103 GBM HE‐stained WSI from 56 patients, a classification ML model was developed and trained to assess the degree of heterogeneity. Out of these 103 images, 38 were selected as basis for the trained model. Using a newly implemented image analysis algorithm, each WSI was converted into a smaller image showing only four representative regions of the tumor tissue, distributed throughout the original image. Using nested cross‐validation, an optimal ML model with hyperparameters was selected to perform the classification task.
Results: Based on the available 38 input images, a heterogeneity classification accuracy of approx. 67% was achieved. While this may not seem like a huge success, values above 60% are generally considered a working classification. Given the small sample size (i.e., only 38 images), this can be seen as a strong validation of the feasibility and a very promising approach. Including preprocessing of the WSI, the complete analysis can be processed in less than 3 min per image.
Conclusions: Based on 38 HE stained WSI, an ML model was trained for the classification of intratumor heterogeneity in GBM. Considering the small amount of available data, the achieved accuracy of 67% can be considered a great success and strongly validates the feasibility of further research.
eP‐NO‐A79
A rare case of a primary intracranial sarcoma associated with a DICER1 mutation with focal cartilaginous differentiation
L. Robinson 1, D. Cannon2, J. Mendez3, S. Menacho4, M. Kohler1, Q. Mao1
1University of Utah, Pathology, Salt Lake City, UT, United States; 2University of Utah, Radiation Oncology, Salt Lake City, UT, United States; 3University of Utah, Neuro‐oncology, Salt Lake City, UT, United States; 4University of Utah, Neurosurgery, Salt Lake City, UT, United States
Introduction: A 22‐year‐old male, with no previous extracranial history of malignancy, presented with altered mental status and speech difficulties. Brain MRI demonstrated an enhancing extra‐axial mass in the left frontal lobe with associated hemorrhage. The patient underwent a left frontal craniotomy for resection of the mass.
Objectives: To describe a case of primary intracranial sarcoma harboring a DICER1 mutation with focal cartilaginous differentiation and negative immunopositivity for sarcoma markers.
Materials and Methods: Histological assessment of the tumor sections with special and immunohistochemical stain interpretation. Molecular ancillary testing and DNA methylation profiling.
Results: Hematoxylin and eosin sections demonstrated a hypercellular, spindle neoplasm arranged in fascicles. Multifocal areas showed primitive appearing dedifferentiated small round blue cells with focal cartilaginous morphology. The Mitotic index was up to 20/10 high‐power fields. No definitive necrosis or microvascular proliferation was identified. Immunohistochemical profiling showed the tumor cells were positive for CD99 and negative for GFAP, Desmin, Myogenin, S100, OCT3/4, and SOX10. Synaptophysin and Chromogranin‐A staining highlighted a potential neuronal component and entrapped, intervening axons. Sections of tumor were referred to the National Institute of Health for DNA methylation profiling for further tumor classification. The methylation‐based tumor profiling results showed a primary intracranial sarcoma, DICER1‐mutant.
Conclusions: Primary intracranial sarcomas with DICER1 mutations are challenging to diagnose on morphology and immunohistochemical assessment alone due to their heterogeneous morphological features and immunohistochemical profiles that overlap with other tumors. This case further highlights the importance of tumor methylation profiling in classifying these enigmatic entities.

FIGURE 1.

FIGURE 2.
eP‐NO‐A80
Study of inherited mismatch repair deficiency in pediatric and adult gliomas
K. Kaur 1, K. Srivastava1, S. Singh1, S. Das1, A. Suri1,2, M. C. Sharma1, A. Garg2, V. Suri1
1All India Institute of Medical Sciences, Pathology, New Delhi, India; 2All India Institute of Medical Sciences, New Delhi, India
Introduction: Constitutional mismatch repair deficiency (CMMRD) is a highly penetrant devastating tumor predisposition syndrome with early childhood brain tumors being the most commonly reported. It is pertinent to detect this syndrome as the patients possess high risk to develop multiple cancers, which show resistance chemotherapy. Hence, early detection can lead to genetic counselling, timely surveillance, and these ultramutant tumors have shown response to immunotherapy.
Objectives: To study the prevalence of MMRD in pediatric and adult gliomas, and to correlate with histopathological features, and clinical findings.
Materials and Methods: FFPE tumor samples of pediatric and adult high grade gliomas will be collected. Clinical parameters and histopathology features will be reviewed. IHC will be performed for MMR proteins: MLH1, MSH2, PMS2, MSH6.
Results: Eighty cases have been analyzed: Among 40 pediatric cases, 8 cases showed loss of one or more MMR protein expression: 7 cases revealed loss of PMS2: age 3–15 years, all grade4 gliomas, 1 case showed combined loss of MLH1 and PMS2: 2‐years‐old female with grade4 glioma. All were IDH1 wildtype, and were negative for histone alterations; 50% showed p53 positivity. Four cases had follow up data: 2 developed recurrences and one died of disease, all within a year of diagnosis. Isolated PMS2 loss was also identified in young adults(19–30 years); 2 were grade3, and 2 grade4 astrocytomas. One tumor in a 24‐year‐old male showed combined MSH2 and MSH6 loss. IDH1R32H was positive in 2 tumors: grade2, and 3 astrocytomas; p53was positive in all. Whole exome sequencing is being performed.
Conclusion: There was complete loss of expression of one of MMR proteins in 20% of pediatric and 12.5% of young adult high grade astrocytic tumors. Almost all cases revealed more nuclear anaplasia and tumor giant cells. p53 positivity was noted in all adult and 50% pediatric tumors. A correlation was noted with consanguinity and café au‐lait spots.
eP‐NO‐A81
High‐grade neuroepithelial tumor; EWSR1‐PATZ1 fusion—A case report
L. Wang 1, M. Tian1, L. Teng1
1Xuanwu Hospital, Pathology, Beijing, China
PATZ1 fusion positive was provisionally accepted as a type in the most recent 5th edition of the World Health Organization (WHO) Classification of Tumours of the Central Nervous System. We reported a rare case of a 4‐year‐old boy who was diagnosed as a high‐grade neuroepithelial tumor with EWSR1‐PATZ1 fusion. Cranial MRI showed a round mass measuring 29 × 27 × 20 mm located in the pineal region. Histopathological examination of the tumor revealed typical findings of high‐grade neuroepithelial tumor. Next‐generation sequencing revealed a EWSR1‐PATZ1 fusion (EWSR1:exon8~PATZ1:exon1) using GeneseeqOneTM 494 gene panel associated with central nervous system tumors, which was confirmed by FISH (EWSR1‐PATZ1 fusion probes).

FIGURE 1.
eP‐NO‐A82
Implementation of the fifth edition of the WHO classification of tumors of the central nervous system and its implications in a Belgian cohort
M. Ahmed 1, A. Sieben1, B. Verbraeken1, T. Menovsky1, M. Rasschaert1, P. Meijnders1, P. Cras1, L. C. van Kempen1, M. Lammens1
1Antwerp University Hospital, Pathological Anatomy, Edegem, Belgium
Introduction: The implementation of the 2021 WHO CNS tumor classification has introduced molecular analyses as an ancillary diagnostic test.
Objective: The objective of this study was to investigate how the new edition of the WHO CNS tumors changed the clinicopathological assessment of IDH1/2‐wild type diffuse glioma.
Patients and Methods: All cases with a diagnosis of IDH1/2‐wild type diffuse glioma were included (n = 148). The time span for inclusion was limited to the period between November 2021 until March 2023. Molecular testing on DNA and RNA levels was a requirement for inclusion.
Results: A TERT promotor mutation was observed in 117/148 cases (79%), a rate comparable with the literature. An isolated pTERT mutation was observed in 12/148 (8%) of the cases. Morphological diffuse glioma grade 2 or 3 was upgraded to glioblastoma based on molecular alterations alone in 17/148 cases (i.e., molecular GBM, 11%). Sixteen of these 17 cases showed a TERT promotor mutation, 7 cases showed an EGFR amplification. At the RNA level, different gene fusion transcripts were detected: EGFR, FGFR3, PTRRZ, MET and ROS1. Only one case of IDH1/2‐wild type low‐grade diffuse glioma did not contain a molecular alterations. The methylation profile was compatible with glioblastoma, IDH‐wild type.
Conclusion: Implementation of molecular diagnostics for CNS tumors according the current WHO guideline resulted in the upgrading of IDH‐wild type diffuse glioma, (grade 2 or 3) to an IDH‐wild glioblastoma, (grade 4) in 11% of cases based on the molecular results only. This has a considerable impact on the treatment trajectory for these patients. Ninety‐four per cent of the upgrading was due to a TERT promotor mutation. An isolated TERT promotor mutation was seen in 8% of all cases, which may have prognostic consequences according to the literature. Furthermore, molecular results pointed towards options for targeted therapy.
eP‐NO‐A83
Molecular characterization of precursor lesions of high grade astrocytoma with piloid features (HGAP)
E. Pérez 1,2, A. Reinhardt3, D. Teichmann2, S. Schmidt2, L. Schweizer2,4,5,6,7, H. Boldt8, B. W. Kristensen9,10,11,12, P. French13, S. Brandner14, P. Wesseling15,16, B. Kusters17, B. Ulhøi18, R. Sigaud19,20,21, D. T. W. Jones19,22, D. Capper4,2
1Berlin School of Integrative Oncology (BSIO), Berlin, Germany; 2Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt‐Universität zu Berlin, Department of Neuropathology, Berlin, Germany; 3Center for Human Genetics Tuebingen, Tuebingen, Germany; 4German Cancer Consortium (DKTK), Partner Site Berlin, German Cancer Research Center (DKFZ), Heidelberg, Germany; 5Edinger Institute, Institute of Neurology, University of Frankfurt am Main, Frankfurt a. M., Germany; 6German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Frankfurt a. M., Germany; 7Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 8Department of Pathology, University Medical Centre Utrecht, Utrecht University, Utrecht, Netherlands; 9Department of Pathology, Odense University Hospital, Odense, Denmark; 10Research Unit of Pathology, Department of Clinical Research, University of Southern Denmark, Odense, Denmark; 11Department of Pathology, The Bartholin Institute, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark; 12Department of Clinical Medicine and Biotech Research and Innovation Center (BRIC), University of Copenhagen, Copenhagen, Denmark; 13Erasmus MC Cancer Institute, Brain Tumor Center, Department of Neurology, Rotterdam, Netherlands; 14Universitätsklinikum Erlangen, FAU Erlangen‐Nürnberg, Department of Neurosurgery, EpiCARE Partner, Erlangen, Germany; 15Department of Pathology, Amsterdam University Medical Centers/VUmc, Amsterdam, Netherlands; 16Laboratory for Childhood Cancer Pathology, Princess Máxima Center for Pediatric Oncology, Utrecht, Netherlands; 17Donders Institute for Brain, Cognition and Behaviour, Radboud University Medical Center, Department of Pathology, Nijmegen, Netherlands; 18Department of Pathology, Aarhus University Hospital, Aarhus, Denmark; 19Hopp Children's Cancer Center Heidelberg (KiTZ), Heidelberg, Germany; 20Clinical Cooperation Unit Pediatric Oncology, German Cancer Research Center (DKFZ), Heidelberg, Germany; 21National Center for Tumor Diseases (NCT), Heidelberg, Germany; 22German Cancer Research Center (DKFZ) and German Cancer Consortium (DKTK), Division of Pediatric Glioma Research, Heidelberg, Germany
Introduction: High grade astrocytoma with piloid features (HGAP) is a recently recognised brain tumour type defined by a specific DNA methylation profile and a poor outcome. A large proportion of HGAP patients have a history of a low‐grade glioma, often occurring several decades prior. Currently it is unclear if the low‐grade gliomas represent precursors of HGAP.
Objectives: (1) Clarify if there is a clonal relation between the low‐grade gliomas occurring earlier in life and HGAP, (2) analyse molecular and histopathological alterations associated with progression, and (3) characterise the low‐grade gliomas to identify markers that may indicate potential for malignant transformation.
Materials and Methods: A cohort of cases diagnosed as HGAP which had a histologically diagnosed pilocytic astrocytoma earlier in life were identified via the MNP brain tumour classification website and FFPE tissue was collected. For each case DNA methylation‐based profiling by EPIC array and NGS TSO500 gene panel sequencing were performed for at least two time‐points.
Results: Obtaining tissue pairs for this study was challenging, as the time between manifestations may span decades. For some cases, only an intermediate time point could be obtained, as the initial tumour was not retrievable. In total, we retrieved eight tissue pairs for molecular analyses. Early data of single cases indicates a clonal relation between the pilocytic astrocytomas and HGAPs. Further molecular analysis shows changes in the DNA methylation and mutation profiles of the tumours over time, including switching of DNA methylation class and accumulation of mutations and copy number changes.
Conclusion: At least some HGAPs develop from low‐grade precursors. A substantial accumulation of mutations and chromosomal changes is observed and accompanied by a switching of DNA methylation class. Currently we are further profiling the initial tumours to identify potential features of early malignant transformation.
eP‐NO‐A84
Quantitative characterization of the cell composition in recurrent glioblastoma and its impact on survival
M. Rinke 1, A. M. Wurzer2, F. Schmidt‐Graf2, B. Wiestler3, J. Schlegel1, B. Märkl4, F. Liesche‐Starnecker4
1Technical University of Munich, Institute of Pathology, Munich, Germany; 2Technical University of Munich, Department of Neurology, Munich, Germany; 3Technical University of Munich, Department of Neuroradiology, Munich, Germany; 4University of Augsburg, Institute of Pathology, Augsburg, Germany
Introduction: The prognostic impact of histopathologic features in surgically resected recurrent glioblastoma (GBM) specimens remains unclear.
Objectives: The aim of this study was to quantify immunohistopathologic characteristics in recurrent GBM after radio‐chemotherapy and their association with survival.
Methods: Using immunohistochemical analysis, we measured the cell composition in 39 recurrent IDH‐wildtype GBM for the following parameters: Ki67 (proliferation‐index), area of GFAP‐positive cells, amount of Iba1‐positive microglial cells, amount of CD3‐positive T‐lymphocytes and area of CD34‐positive vascularization. After slide digitalization with an Aperio AT2 scanner, image analysis was performed with specially trained pixel classifiers for each parameter in QPath.
Results: Tumor samples from 39 patients with recurrent GBM were assessed. The median overall survival was 23 months (95% CI 12.9–33.1). The median survival after the first recurrence was 9 months (95% CI 7.6–10.5). A shorter time interval from the initial diagnosis to the first recurrence was associated with a reduced overall survival. In a Cox proportional‐hazards model, high values of Iba1‐positive cells were associated with a worse survival rate (HR 1.18, 95% CI 1.03–1.31, p‐value = 0.024). On the other hand, high GFAP values indicated a longer survival (HR 0.98, 95% CI 0.97–0.99, p‐value = 0.008).
Conclusions: In patients with recurrent GBM, GFAP and Iba1 are prognostic markers. A high amount of Iba1‐positive microglial cells in the recurrent GBM and a short time to recurrence are associated with reduced survival. High GFAP is associated with a longer survival. Histopathologic quantification of the cell composition should be considered as a prognostic assessment of survival after GBM recurrence in routine diagnostics.
eP‐NO‐A85
Distribution and tumor cell proximity of immune cells in the tumor core, transition zone and periphery of glioblastomas
V. Pedersen1,2, A. Møldrup Knudsen3,4, S. Regner Michaelsen1,2, B. Winther Kristensen 1,2
1Bartholin Institute, Department of Pathology, Rigshospitalet, Copenhagen, Denmark; 2University of Copenhagen, Department of Clinical Medicine and Biotech Research & Innovation Centre (BRIC), Copenhagen, Denmark; 3Odense University Hospital, Department of Pathology, Odense, Denmark; 4University of Southern Denmark, Department of Clinical Research, Odense, Denmark
Introduction: Glioblastoma is the most frequent and malignant brain tumor. Immune therapies have had limited effect but not much is known about the frequency and type of immune cells in the transition zone and periphery of the tumors. In these areas, tumor cells migrate into the brain parenchyma and prevent total tumor resection thereby leading to recurrence.
Objectives: This study aims to quantify the type and distribution of immune cells in glioblastomas.
Materials and Methods: A cohort of 67 glioblastomas with strong P53 immunoreactivity in the tumor cells was established. Slides contained tissue from central tumor and/or transition zone and/or tumor periphery. A chromogenic multiplex was established, where tissue sections were stained with P53 (tumor cells), FOXP3 (FOXP3+ regulatory T cells), CD8 (CD8+ cytotoxic T cells) and IBA1 (microglia/macrophages). Cells were counted in tumor core, transition zone and periphery using Visiopharm software. The number of tumor cells with immune cells in proximity (30 μm) was quantified, and the distance from a reference cell to another cell type within 30 μm was calculated.
Results: The densities of CD8+, FOXP3+ and IBA1+ cells were significantly higher in the core than in the periphery (p < 0.001), and in the transition zone than in the periphery (p < 0.001). The CD8+, FOXP3+ and IBA1+ cell/tumor cell ratio increased from core to transition zone and the CD8+ and IBA1+ cell/tumor cell ratio increased again to periphery (p < 0.001). The highest density of tumor cells with CD8+ cells in proximity was in the tumor core (p < 0.001), whereas the highest density of tumor cells with IBA1+ cells and FOXP3+ cells in proximity was in the transition zone (p < 0.001).
Conclusion: Although levels of immune cells are highest in the tumor core—the higher proximity and ratio of immune cells to tumor cells in the transition zone/periphery suggest immune‐suppressive mechanisms.
eP‐NO‐A86
Nucleation of LDHA promotes the catabolism of BCAAs to sustain GBM cell proliferation through the TxN antioxidant pathway
J. Xiong1, Z. Du1, F. Tang1, Y. Wang1, Y. Liu 2
1Huashan Hospital, Shanghai Medical College, Fudan University, Department of Pathology, Shanghai, China; 2School of Basic Medical Sciences, Fudan University, Department of Pathology, Shanghai, China
Glutamate has excitatory neuron toxicity. The import of glutamine or glutamate from the blood into the brain is limited. Therefore, branched‐chain amino acids (BCAAs) catabolism replenishes glutamate in brain cells. Branched‐chain amino acid transaminase 1 (BCAT1) activity silenced by epigenetic methylation in IDH mutant gliomas. However, glioblastomas (GBMs) are IDH wild type. Here, we investigated how oxidative stress promotes BCAAs metabolism to maintain intracellular redox balance and involves the rapid progress of GBMs. We found that ROS accumulation promoted LDHA nuclear translocation that triggered DOT1L (disruptor of telomeric silencing 1‐like)‐mediated histone H3K79 hypermethylation and elevated BCAA catabolism in GBM cells. Glutamate derived from BCAAs catabolism participates in antioxidant thioredoxin (TxN) production. Inhibition of BCAT1 decreased the tumorigenicity of GBM cells in orthotopic transplanted nude mice and prolonged their survival time. In GBM samples, BCAT1 expression negatively correlated with the patients’ overall survival time (OS). These findings highlight the role of the non‐canonical enzyme activity of LDHA on BCAT1 expression, which links the two major metabolic pathways in GBMs. Glutamate produced by the catabolism of BCAAs is involved in complementary antioxidant TxN synthesis to balance the redox state in tumor cells and promote the progression of GBMs.
eP‐NO‐A87
Rosette‐forming glioneuronal tumors may exhibit H3 K28me3 loss along with H3 K27M mutation
E. Marastoni 1, S. Ammendola1, S. Rossi2, I. Giovannoni2, A. Feletti1, A. Scarpa1, V. Barresi1
1University of Verona, Verona, Italy; 2Ospedale Pediatrico Bambino Gesù, Rome, Italy
Introduction: Immunohistochemical loss of histone H3 trimethylated at lysine 28 (H3 p. K28me3) is a criterion, along with midline location and H3 K27M mutation, or EZHIP overexpression, or EGFR amplification/mutation, for the diagnosis of diffuse midline glioma H3 K27‐altered. Owing to its poor prognosis, the latter is classified as a CNS WHO grade 4. However, H3 p. K28me3 loss, along with the H3 K27M mutation, has rarely been reported in circumscribed gliomas (including pilocytic astrocytomas, gangliogliomas, or glioneuronal tumors not otherwise specified) arising from midline anatomical structures. Rosette‐forming glioneuronal tumor (RGNT) is a rare CNS WHO grade 1 neoplasia located in the midline and composed of neurocytes, forming rosettes and/or perivascular pseudorosettes, and piloid and oligodendroglial‐like cells. H3 K27M mutations have not been reported in this tumor.
Objectives: This study aimed to evaluate the immunohistochemical expression of H3 K28me3 and the presence of H3 K27M mutation in RGNTs.
Patients and Methods: The immunohistochemical expression of H3 K28me3 was analyzed in five RGNTs from four female and one male patient, age range 22–42 years. H3 mutations and EZHIP immunoexpression were then tested in cases with H3 K28me3 loss.
Results: Two of the five RGNTs exhibited H3 K28me3 loss. This was associated with the H3 K27M mutation in one case and with the immunoexpression of H3 p.K28M in another (pending gene mutation analysis). These two patients had unremarkable follow‐up at 18 and 134 months after diagnosis, despite incomplete surgical resection in the former case.
Conclusion: We demonstrated that loss of H3 K28me3, along with the H3 K27M mutation, can also be found in RGNTs. This could lead to misdiagnosis as a diffuse midline glioma in cases of partial resection of the sole glial component of RGNTs.
eP‐NO‐A88
Epigenetic and genetic characterization of T‐cell lymphomas
C. Siewert 1,2, A. Saksena3, B. Englert4, D. Teichmann1, S. Schmid1, E. Pérez1, J. Richter5, R. Turakulov3, M. Raffeld3, S. Pittaluga3, E. Jaffe3, Z. Abdullaev3, D. Pratt3, J. Hench6, S. Frank6, A. Tzankov6, W. Klapper5, I. Anagnostopoulos7, A. Rosenwald7, C. Kreßler8, K. Ou8, J. K. Polansky8, M. Wobser9, F. Fend10, L. Quintanilla‐Martinez10, G. Ferrer11, M. Esteller11, A. von Deimling12, M. Hummel13, K. Aldape3, D. Capper1,2
1Charité—Universitätsmedizin Berlin, Department of Neuropathology, Berlin, Germany; 2German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Berlin, Heidelberg, Germany; 3National Institutes of Health, Laboratory of Pathology, Center for Cancer Research, National Cancer Institute, Bethesda, MD, United States; 4Ludwig‐Maximilians‐University, Institute of Neuropathology, Munich, Germany; 5Christian‐Albrechts‐University of Kiel, University‐Hospital Schleswig‐Holstein (UKSH), Department of Pathology, Hematopathology Section and Lymph Node Registry, Kiel, Germany; 6University Hospital Basel, Institute for Pathology, Basel, Switzerland; 7University of Würzburg, Institute of Pathology, Wuerzburg, Germany; 8Berlin Institute of Health at Charité—Universitätsmedizin Berlin, BIH Center for Regenerative Therapies, Berlin, Germany; 9University Hospital Würzburg, Department of Dermatology, Venereology and Allergology, Wuerzburg, Germany; 10Eberhard Karls University of Tübingen and Comprehensive Cancer Center, University Hospital Tübingen, Institute of Pathology and Neuropathology, Tuebingen, Germany; 11Josep Carreras Leukaemia Research Institute (IJC), Barcelona, Spain; 12University Hospital of Heidelberg, Institute of Pathology, Department of Neuropathology, Heidelberg, Germany; 13Charité—Universitätsmedizin Berlin, Institute of Pathology, Molecular Diagnostics, Berlin, Germany
Introduction: T‐cell lymphomas (TCL) present a biologically diverse diseases that accounts for up to 12% of all lymphomas and include both indolent and aggressive forms that occur at multiple anatomic sites, including blood and bone marrow (leukemic TCL), lymph nodes, and extranodal sites such as the gastrointestinal tract, spleen, skin, and CNS.
Objectives: Here we investigate whether DNA methylation patterns can be used to separate BCL from TCL and subgroup TCL and if this subgrouping correlates with histopathological tumor classes and mutational patterns.
Materials and Methods: FFPE material or DNA was acquired from archival cases and analyzed using Illumina Infinium EPIC arrays and studied together with publicly available cases (TCL: n = 353, BCL: n = 139). In addition, a selection of tumors was sequenced using the TruSight Oncology 500 assay (n = 94 of TCL). Data were quality checked and further processed by R scripts and packages.
Results: Unsupervised t‐SNE clustering demonstrates the separation of TCL from BCL as well as from reference samples such as sorted blood cells (e.g., T and NK cells). In addition, several subtypes of TCL form distinct clusters in accordance with their diagnostic assignment (e.g., monomorphic epitheliotropic intestinal TCL, extranodal NK/TCL, nasal type, T‐follicular helper (TFH) cell lymphoma, Sezary syndrome). In contrast, others do not form distinct groups (e.g., peripheral TCL, NOS). Additional molecular data is currently being analyzed.
Conclusion: Several subtypes of TCL form distinct methylation groups and methylation profiling may be helpful for the diagnosis of such lesion. Expected considering their known molecular heterogeneity, peripheral TCL, NOS do not form a distinct methylation class but rather intermix with other classes. Additional studies are required to further define the best classification in such instances.
eP‐NO‐A89
Atypical teratoid/rhabdoid tumour (AT/RT) in an adolescent
T. Bierling 1,2, O. Adeyi 3, R. R. Reimann1, N. Krayenbühl4, A. S. Guerreiro Stücklin5, T. Hortobágyi1
1University Hospital Zurich, Institute of Neuropathology, Zurich, Switzerland; 2Ludwig‐Maximilians‐University, Medical School, Munich, Germany; 3University of Exeter, Medical School, Exeter, United Kingdom; 4University Hospital Zurich, Department of Neurosurgery, Zurich, Switzerland; 5University Children's Hospital Zurich, Department of Oncology, Zurich, Switzerland
Introduction: Atypical teratoid/rhabdoid tumour (AT/RT) is a rare CNS WHO grade 4 malignant embryonal neoplasia. The mean age at presentation is below two years and the usual localization is in the posterior fossa. Biallelic inactivation of SMARCB1 or INI1 is the genetic hallmark, which can be reliably detected by immunohistochemistry.
Objectives: Presentation of an adolescent AT/RT patient with unusual clinical features and up‐to‐date neuropathological work‐up.
Patient and Methods: A 16‐year‐old boy with headache and epileptic fits. Imaging revealed an intraparenchymal hemispheric tumour. Partial tumour resection. Postoperatively, brief asystolic episodes. Routine neuropathological workup with immunohistochemistry was followed by genetic analysis (copy number variations [CNV], Heidelberg Methylation Classifier v12.5, Basel EpiDip Methylome and CNV). Literature review via PubMed and Google. Cell expansion and drug response profiling are in progress.
Results: Histology revealed a cellular tumour with rhabdoid cells, frequent mitotic figures, vague rosettes. Immunohistochemistry: tumour cells negative with INI1 (SMARCB1/INI1 loss). Some positivity for SMA, GFAP, CD34, CA‐125 (MUC‐6), ERG, EMA, ATRX; negative for Olig‐2, pan‐CK, IDH‐1R132H, and synaptophysin. p53 wild‐type pattern. Ki67 index: 20% (focally up to 50%). Other INI‐negative tumours in particular epitheloid sarcoma were considered and excluded. Methylation class: AT/RT (score: 0.91958/1.0), MYC‐subtype (score: 0.83045). Unmethylated MGMT promoter. Epidip Basel: it clustered with AT/RT‐MYC. According to the literature in adolescents AT/RT occurs extremely rarely and, like our case, is usually supratentorial and of MYC molecular subtype.
Conclusion: AT/RT remains a differential diagnostic possibility in adolescents with intrinsic brain tumours. Molecular profiling and subtyping aids in diagnosis and may have therapeutic implications.
eP‐NO‐A90
The epigenetic effect of dexamethasone on glioblastoma cell line
A. M. Barciszewska 1,2, A. Belter3, M. Giel‐Pietraszuk3, I. Gawrońska3, M. Z. Naskręt‐Barciszewska3
1Poznan University of Medical Sciences, Neurosurgery and Neurotraumatology, Poznań, Poland; 2University Clinical Hospital, Neurosurgery and Neurotraumatology, Poznań, Poland; 3Institute of Bioorganic Chemistry of the Polish Academy of Sciences, Poznań, Poland
Dexamethasone (DEX) is a first‐line antiedematic drug for glioblastoma (GBM) patients. There is also some evidence it inhibits GBM cell proliferation and migration, impacting patient outcomes. However, other studies show that the use of DEX is associated with poor treatment outcomes in GBM patients. The exact mechanism of DEX action is unclear, and no definitive conclusion has yet been reached on its benefits in neurooncological treatment. Temozolomide (TMZ) is a first‐line chemotherapeutic in GBM.
Epigenetics offers a connection between genetic and environmental factors that influence the development of the disease. The best‐characterized epigenetic mark is 5‐methylcytosine (m5C) in DNA. The aim of that project is to show the effects of DEX administration on the total DNA methylation level. Using the nucleotide post‐labeling method, we analyzed the total amount of m5C in DNA of GBM (T98G, U118, U138), cancer (HeLa) and normal (HaCaT) cell lines treated with DEX, and a combination of DEX and with TMZ. We adjusted the DEX doses to the ones achieved in the central nervous system during treatment. We observed a dose‐dependent increase in total DNA methylation in all cell lines. However, the exposition of GBM cells to the combination of DEX and TMZ caused an adverse synergistic effect resulting in DNA demethylation in high doses of both drugs. In lower concentrations of both drugs, DEX kept the increased DNA methylation and attenuated the demethylating effect of TMZ. Total DNA methylation changes in glioma cell lines under DEX treatment suggest the new mechanism of that drug action and promote clinical implications for adjusting DEX and TMZ therapy in GBM patients. Our results show the potential and possible obstacles of the combined therapy of TMZ with DEX. Our experiments show that combined therapy with both drugs leads to total DNA hypomethylation in high doses of both drugs. Therefore the conclusion would be to adjust DEX administration during TMZ chemotherapy.
eP‐NO‐A91
Sarcoidosis lymphoma syndrome presenting as primary central nervous system lymphoma developed during long‐term immunosuppressive treatment—A case report
M. Watanabe 1, Y. Sugita2, K. Ohashi3, Y. Eishi3, T. Maeda4, K. Shibagaki5, S. Ohue5, H. Miki6, R. Ueda7, A. Shiraoka1, I. Kyoraku1, K. Okamoto1
1Ehime Prefectural Central Hospital, Neurology, Ehime, Japan; 2St. Mary's Hospital, Neuropathology, Fukuoka, Japan; 3Tokyo Medical and Dental University, Human Pathology, Tokyo, Japan; 4Ehime Prefectural Central Hospital, Pathology, Ehime, Japan; 5Ehime Prefectural Central Hospital, Neurosurgery, Ehime, Japan; 6Ehime Prefectural Central Hospital, Radiology, Ehime, Japan; 7Ehime Prefectural Central Hospital, Hematology, Ehime, Japan
Introduction: Patients with sarcoidosis have a significantly high risk of developing cancer, especially lymphoma, called sarcoidosis‐lymphoma syndrome. Primary central nervous system lymphoma (PCNSL) accounts for 1%–5% of all brain tumors. However, there are only three case reports of developing PCNSL with sarcoidosis.
Objectives: We aim to report the clinical characteristics of an extremely rare case of sarcoidosis‐lymphoma syndrome presenting as PCNSL.
Patients and Methods: Not applicable.
Results: A 64‐year‐old woman with sarcoidosis, involved in lymph nodes, lung, and cervical cord, and diagnosed by lymph node biopsy thirteen years ago, developed recurrent simple partial seizure in the left face with conjugate gaze to the left side. Contrast brain MRI showed an enhanced mass lesion with heterogeneous granular spots within an edematous area in the right precentral gyrus, accompanied by enhanced linear lesions in cerebral sulci and perivascular spaces. FDG‐PET CT represented increased uptake consistent with the enhanced lesion of MRI and no uptake lesion in other organs. We performed a biopsy of the brain lesion exacerbated contrast enhancement despite treatment with intravenous methylprednisolone. Hematoxylin and eosin staining showed marked diffuse infiltration of atypical large lymphocytes with no noncaseating granuloma. Immunohistochemistry for lymphocytic markers showed CD20‐ and MUM1‐positive B cells with no CD3‐ and CD10‐positive cells. In addition, EBER‐ISH was positive and immunohistochemistry using anti‐Propionibacterium acnes monoclonal antibody showed no positive lesion, corresponding to EBV‐positive diffuse large B cell lymphoma. Chemotherapy of only 2 cycles has kept a partial response for a year.
Conclusion: Early brain biopsy should be considered when new enhanced brain lesions appear in patients of sarcoidosis receiving long‐term immunosuppressive treatment. In particular, we should pay attention to the lesions poorly responsive to the treatment.
eP‐NO‐A92
DNA methylation‐based classification of pituitary carcinomas
S. Schmid 1, A. Thieme2, C. Siewert1, D. Teichmann1, A. Koch1, E. G. Hain1, J. Schittenhelm3,4, B. Englert5, A. Kratz6, L. Reiniger7, A. Pagenstecher8,9, J. Hench10, M. Brodhun11, R. Buslei12, W. Saeger13, C. Giannini14,15, M. B. Lopes16, D. Capper1,2
1Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Neuropathology, Berlin, Germany; 2German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Berlin, Heidelberg, Germany; 3University Hospital Tübingen, Neuropathology, Tuebingen, Germany; 4University Hospital Tübingen, Center for Neuro‐Oncology, Comprehensive Cancer Center Tübingen‐Stuttgart, Tuebingen, Germany; 5Ludwig‐Maximilians‐University, Center for Neuropathology and Prion Research, Munich, Germany; 6Center for Human Genetics Tuebingen, Tuebingen, Germany; 7Semmelweis University, Laboratory of Nanochemistry, Department of Biophysics and Radiation Biology, Budapest, Hungary; 8University Hospital Marburg, 1st Department of Pathology and Experimental Cancer Research, Marburg, Germany; 9University Hospital Marburg, Neuropathology, Marburg, Germany; 10University and University Hospital of Basel, Pathology, Institute of Medical Genetics and Pathology, Basel, Switzerland; 11Helios Klinikum, Pathology, Erfurt, Germany; 12Sozialstiftung Bamberg, Klinikum Bamberg, Pathology, Bamberg, Germany; 13University Hospital Hamburg‐Eppendorf, Neuropathology, Hamburg, Germany; 14Mayo Clinic, Anatomic Pathology, Department of Laboratory Medicine & Pathology, Rochester, MN, United States; 15University of Bologna, Biomedical and Neuromotor Sciences (DIBINEM), Bologna, Italy; 16University of Virginia Health System, Pathology‐Neuropathology, Charlottesville, VA, United States
Introduction: Pituitary adenomas (also known as pituitary neuroendocrine tumors) are typically benign but can be aggressive and invasive to adjacent structures. Tumors that metastasize are exceedingly rare and are referred to as pituitary carcinomas. We previously showed that pituitary adenomas cluster by their DNA methylation patterns into seven distinct methylation classes. However, data regarding the methylation profiling of pituitary carcinomas is unknown.
Objectives: Our aim is to retrospectively analyze if pituitary carcinomas form a distinct DNA methylation cluster and if molecular features associated with disease progression can be identified.
Materials and Methods: The DNA methylation profiles of 13 pituitary carcinomas were compared to a reference cohort of methylation profiles of 269 pituitary tumors, comprising seven adenoma reference groups. For 4/13 carcinomas material of multiple lesion was available for comparative analysis. NGS panel analysis and copy number variation analysis of the cases is currently ongoing.
Results: Descriptive analysis of the methylation data using t‐distributed stochastic neighbor embedding (tSNE) indicate that pituitary carcinomas do not form a separate cluster but distribute to the main pituitary adenoma methylation classes. The carcinoma samples were classified into ACTH (n = 6), PRL (n = 1) and densely granulated STH (subgroup A; n = 1) methylation class. One case showed low scores for FSH/LH methylation class. Two cases were reclassified as non‐pituitary neoplasms (methylation classes Ewing sarcoma and AT/RT) and two other cases could not be classified by DNA‐methylation analysis.
Conclusion: Pituitary carcinomas do not form a separate DNA methylation cluster but tumors rather fall into the different pituitary adenoma methylation reference groups. Tumors of the ACTH class are clearly overrepresented. Further mutational and copy number analyses are currently ongoing.
eP‐NO‐A93
The epigenetic therapeutic effect of Juglone on glioblastoma
A. M. Barciszewska 1,2, A. Belter3, I. Gawrońska3, M. Giel‐Pietraszuk3, M. Z. Naskręt‐Barciszewska3
1Poznan University of Medical Sciences, Neurosurgery and Neurotraumatology, Poznań, Poland; 2University Clinical Hospital, Neurosurgery and Neurotraumatology, Poznań, Poland; 3Institute of Bioorganic Chemistry of the Polish Academy of Sciences, Poznań, Poland
Glioblastoma (GBM) is the most common and aggressive primary brain tumor with the highest mortality. Standard approaches for GBM, including, gross total resection, radiotherapy, and chemotherapy, are not fully effective and the prognosis for GBM remains poor. Therefore new therapeutic strategies are needed. Juglone (J), which exhibits cytotoxic, anti‐proliferative, and anti‐invasive effects on various cells could be a promising agent for GBM therapy. We analyzed the effects of juglone alone and in combination with temozolomide (TMZ) on glioblastoma cell lines. We estimated the total DNA methylation in T98G, U138, U118, and HaCaT lines after treatment with different J and J/TMZ concentrations and incubation time using TLC separation of radioactively labeled nucleotides. The combination treatment with J and TMZ was evaluated with total DNA methylation analysis and 8‐oxo‐dG (oxidative stress marker) estimation using EC detection. We observed concentration and time‐dependent changes in total DNA methylation. The highest increase was present in the T98G cell line after 24 h. Normal cell line (HaCaT) did not present significant changes. TMZ alone induced a lowering of DNA methylation, but juglone diminished that effect. J induces minute oxidative stress in low concentrations, but is quite high and rapid at concentrations over 50 μM, paralelly with none/slight decrease in DNA methylation. The combination of J/TMZ in increasing concentrations diminished the oxidative stress effect. Our research show that a combination of juglone and temozolomide can be applied for better GBM treatment. At specific incubation times and concentrations, juglone increases DNA methylation, which is a positive therapeutic effect in oncogenesis. Small doses of J keep a low level of 8‐oxo‐dG with an increase in DNA methylation. The combination of J/TMZ in high concentrations of both drugs decreases the oxidative stress effect of chemotherapy.
eP‐NO‐A94
Clinicopathological features of rosette‐forming glioneuronal tumour—Single centre experience
I. Bodi 1, Z. Reisz1, R. Laxton1, L. Bhaw1, B. Clark1, B. Zebian1, C. Chandler1, C. Bleil2, R. S. Bhangoo1, A. King1, S. Al‐Sarraj1
1King's College Hospital NHS Foundation Trust, Clinical Neuropathology, London, United Kingdom; 2King's College Hospital NHS Foundation Trust, Neurosurgery, London, United Kingdom
Introduction: Rosette‐forming glioneuronal tumour (RFGNT) is a rare CNS neoplasm primarily affecting young adults and typically arises in the midline (WHO grade 1). RFGNT is characterized by a biphasic histologic architecture consisting of well‐differentiated neurocytic rosettes and a glial component resembling pilocytic astrocytoma. It is also characterised by a distinct DNA methylation profile, and FGFR1 hotspot mutations are typical, with co‐occurrence of PIK3CA mutations in the majority of cases.
Patients: After reviewing the departmental records from 2007 we found 11 patients with diagnosis of RFGNT(M:F = 6:5). Apart from one patient aged 68, most patients were young adults (10–37 years). One patient had NF1 and another one had Noonan syndrome (PTPN11 deletion) confirmed by genetics.
Results: Apart from arising from the fourth ventricle (6/11), some cases presented in the midbrain (2), the lateral ventricle, the cerebellar hemisphere and the thalamus. In 9/11 cases the histological features were typical, allowing confident diagnosis. One case had necrosis and a mitotic figure in a small biopsy. The other case arose from the midbrain dominated by cavernoma‐like appearances with presence of hyalinised capillaries surrounded by a few pleomorphic astrocytes. In both cases the diagnosis was confirmed by methylation array and presence of FGFR1 mutation by NGS. Two patient had multiple surgeries due to recurrence, one of them is clear of tumour. Two patients received radiochemotherapy. Two cases had recurrent nodules on scans and another patient had craniospinal dissemination.
Conclusion: In small or non‐representative histological samples, the diagnosis of RFGNT is aided by DNA methylation profiling and demonstrating FGFR1 mutations by NGS. The clinical course is favourable in terms of survival but rare recurrences and even craniospinal dissemination may occur.
eP‐NO‐A95
Microglia and macrophages in human glioblastomas and relations to tumour growth
H. Araste 1, M. Kvisten1, B. Ytterhus1, Ø. Salvesen2, H. S. Pettersen1,3, A. J. Skjulsvik1,3, S. H. Torp1,3
1Norwegian University of Science and Technology (NTNU), Department of Clinical and Molecular Medicine, Trondheim, Norway; 2Norwegian University of Science and Technology (NTNU), MH Faculty Administration, Trondheim, Norway; 3St. Olavs Hospital, Trondheim University Hospital, Department of Pathology, Trondheim, Norway
Introduction: Glioblastomas (GBMs) are the most common primary malignant brain tumour. The prognosis is still poor despite considerable progress in molecular genetics, tumour biology and treatment options. In addition to neoplastic astrocytes, the glioblastoma tissue contains a high number of microglia and macrophages, commonly denoted tumour‐associated macrophages (TAMs). Their role in GBMs may be either tumour‐suppressive or ‐supportive.
Objectives: The aim of this study was to investigate the influence of TAMs on the growth of these tumours.
Materials and Methods: In a series of 92 human GBMs tumour growth was estimated by means of tumour volume segmentation from two MRIs taken as diagnostic and preoperative scans resulting in groups of slow‐ and fast‐growing tumours. Standard immunohistochemistry was used for visualization of TAMs using CD206 for macrophages, TMEM119 for microglia and Iba1 for all TAMs. Digital pathology was used to assess and compute immunoreactivity.
Results: We estimated the quantity of TAMs immunoreactive for CD206, TMEM119, and Iba1, and we found no significant correlation between these groups of TAMs and tumour growth.
Conclusion: In our series of GBMs we found that TAMs did not have any influence on tumour growth.
eP‐NO‐A96
POST (preview of spinal tumours) study
A. Juneja 1, S. Epari1, A. Sahay1, A. Shah1, O. Shetty1, A. Chatterji1, A. Dasgupta1, A. Sahu1, G. Chinnaswamy1, M. Prasad1, V. Patil1, A. Moiyadi1, T. Gupta1, P. Shetty1, V. Singh1
1Tata Memorial Hospital, Mumbai, Pathology, Mumbai, India
Intra‐spinal lesions comprise non‐tumourous spinal lesions and intra‐spinal tumours. This study evaluates the spectrum of intra‐spinal lesions diagnosed in the institute from 1st January 2003 to 31st July 2021. Total 377 cases (28, non‐tumourous intra‐spinal lesions and 349 intra‐spinal tumours). Age was subgrouped into 0–6 (n = 34, 9%), 7–18 (n = 63, 16.7%), 19–39 (n = 142, 37.7%), 40–59 (n = 101, 26.8%) and >60 years (n = 37, 9.8%). M:F ratio—1.2:1. Intramedullary location (57.3%) and thoracic region (43.5%) were more common. Glial, glioneuronal tumours, and neuronal tumours (57%) included ependymomas (54.8%) and gliomas (45.2%). Ependymomas were divided into spinal ependymoma (grade 2; n = 59 and grade 3; n = 14, total n = 68, 62.4%), myxopapillary ependymoma (grade 2, n = 31, 28.4%), subependymoma (grade 1, n = 4, 3.7%) and spinal ependymoma, MYCN amplified (grade 3, n = 1, 0.9%). Glial tumours comprised high‐grade diffuse gliomas, NOS (n = 45, 50.6%; including diffuse midline glioma, H3K27‐altered) circumscribed astrocytic gliomas (n = 27, 30.3), low‐grade glial tumours, NOS (n = 14,15.7%) and high‐grade neuroepithelial tumour (n = 4, 4.4%). Nerve sheath tumours (18.6%) consisted of Schwannoma (n = 44, 68.7%), MPNST (n = 8, 12.5%), MMNST (n = 7, 10.7%), Neurofibroma (n = 1, 1.5%) and Paraganglioma (n = 5, 7.8%). Meningioma (n = 40, 11.5%),others including mesenchymal tumours [n = 12; lipomas (41.7%), hemangioblastomas (20%) and Ewing's sarcoma (16.7%)], embryonal tumours (n = 9), hematolymphoid tumours (n = 4), melanocytic tumours (n = 1), mature cystic teratoma (n = 3), choroid plexus tumour (n = 1) and metastases (n = 14). Ependymal tumours were overall the most common tumours. Nerve sheath tumours were common in the older age groups, and gliomas in lower age groups(statistically significant correlation, p value = 0.00). Nerve sheath tumours were more common at cervical and lumbar spinal levels while meningiomas at the thoracic spinal level(statistically significant correlation, p‐value = 0.00).
Keywords: Ependymoma, intra‐spinal, nerve sheath tumours.
eP‐NO‐A97
Can we predict glioblastoma, IDH wild type with FGFR3::TACC3 fusion morphologically?
T. Soylemez‐Akkurt 1, F. Kusku‐Cabuk1, A. Ersen‐Danyeli2
1Basaksehir Cam and Sakura City Hospital, Pathology, Istanbul, Turkey; 2Acibadem MAA University, School of Medicine, Pathology, Istanbul, Turkey
Question: We present seven cases of gliomas with FGFR3::TACC3 fusion and highlight the histological, immunohistochemical and molecular characteristics that are frequently present in this entity.
Methods: This study included seven patients with diffuse gliomas containing the FGFR3::TACC3 fusion. The clinicopathological and immunohistochemical (IDH1 R132H, ATRX, MIB1, P53, OLIG2 and CD34) findings were retrospectively evaluated and retrieved from clinical and pathological data. The mutational status of the IDH1 and IDH2 genes, and of the TERT promoter as well as MGMT promoter methylation status was analyzed.
Results: Three females and four males were included. The median age at diagnosis was 54 years (range, 37–75). Among the seven cases reviewed, two patients presented histopathological features of grade 4 diffuse glioma. All tumors demonstrated a diffuse growth pattern. Endocrinoid vascular network and monomorphous ovoid nuclei were recorded in all cases and 5/7 cases, respectively. Calcifications were observed in 5/7 cases. The immunohistochemical features of the series were: negative IDH1 R132H, retained ATRX expression, negative p53 and expression of Olig2 in all cases. CD34 immunolabeling highlighted the dense branched vascular network vessels in all cases while extravascular CD34 expression was observed in 2/7 cases. The mean Ki67 proliferation index was 14%. TERT promoter mutation was recorded in all cases. IDH1/IDH2 mutation and methylation of the MGMT were not detected.
Conclusions: The FGFR3::TACC3 fusion is relatively uncommon in human glioblastoma, with a prevalence of 3%–4%. The neuropathologists should be aware that the presence of monomorphous ovoid nuclei, endocrinoid network of thin capillaries, and calcification may reliably predict a distinct molecular profile of glioblastoma, IDHwt and perform additional molecular test for FGFR3::TACC3 fusion. FGFR3::TACC3 fusion might be a novel option for personalized targeted therapy in this patients.
eP‐NO‐A98
Cribriform neuroepithelial tumor with intracytoplasmic eosinophilic hyaline droplets in an infant
S. Al‐Dandan 1,2, M. Murad3, F. Al‐Otaibi4, Z. AlNaqib5, W. AlShakweer1
1King Fahad Medical City, Anatomic Pathology Department. Pathology and Clinical Laboratory Medicine Administration, Riyadh, Saudi Arabia; 2King Fahad Medical City, Anatomic Pathology Section. Department of Laboratory and Blood Bank, Al‐Ahsa, Saudi Arabia; 3King Fahd Armed Forces Hospital, Anatomic Pathology Department, Jeddah, Saudi Arabia; 4King Fahad Medical City, Pediatric Neurosurgery Department. National Neurologic Institute, Riyadh, Saudi Arabia; 5King Fahad Medical City, Department of Pediatric Hematology & Oncology. Comprehensive Cancer Center, Riyadh, Saudi Arabia
Introduction: Cribriform neuroepithelial tumors (CRINET) are rare non‐rhabdoid SMARCB1 (INI1)‐deficient neuroectodermal neoplasms. Eosinophilic hyaline droplets (EHD) occur at variable proportions in different brain neoplasms, especially gliomas, but are almost unheard of in the scarcely reported cases of CRINETs.
Objectives: We aimed to characterize the morphological and ultrastructural features of EHDs in a molecularly defined CRINET.
Patients and Methods: A 7‐month‐old male infant with a family history of renal malignant rhabdoid tumor in a sibling presented to the emergency department with a two‐week history of left‐sided weakness and bulged anterior fontanelle. MRI imaging showed a sizeable intraventricular tumor associated with midline shift and active hydrocephalus. The patient underwent right‐sided craniotomy and tumor resection.
Results: Histopathological examination of the tumor revealed cribriform ribbons, trabeculae, and papillae. Tumor cells were cuboidal to columnar and displayed eosinophilic to clear cytoplasm and oval‐to‐round pleomorphic nuclei. Intracytoplasmic eosinophilic hyaline refractile droplets were scattered in multiple areas and were PAS‐positive and diastase‐resistant. Immunohistochemistry showed loss of nuclear INI1 expression and luminal reactivity for EMA stain. Ultrastructurally, there were numerous electron‐dense deposits of different sizes and zipper‐like junctional complexes near the luminal surfaces. Next‐generation sequencing demonstrated loss of chromosome 22 (inclusive of SMARCB1) and no pathogenic genomic mutations or fusions.
Conclusion: We described a CRINET with PAS‐positive EHDs, which may suggest a secretory function of the tumor cells. Similar droplets have been described in choroid plexus neoplasms. Our findings shed light on the similarities between CRINETs and choroid plexus neoplasms regarding younger age at presentation, ventricular localization, papillary morphology, and cytoplasmic secretory changes.

FIGURE 1.

FIGURE 2.
eP‐NO‐A99
Papillary tumors of the skull base—Are they all corticotroph adenomas?
N. Lakis 1, M. Haeri1
1The University of Kansas Health System, Pathology, Kansas City, MO, United States
Introduction: Adenohypophyseal tumors were recently renamed pituitary neuroendocrine tumors (PitNET). These are mostly benign but may be clinically “aggressive.” It is a recommended practice to classify them into lineages: lactotroph, somatotroph and thyrotroph (PIT1), corticotroph (TPIT), gonadotroph (SF1), null cell or immunonegative tumor and plurihormonal tumors. Some tumors require extra workup for appropriate diagnostic classification, especially to identify more aggressive subtypes.
Methods: Three cases received at the University of Kansas Health System were evaluated. All three were within the “skull base,” “sellar/suprasellar/sphenoid sinus” regions. All underwent a standard immunohistochemical and special stain panel: Reticulin, FSH, LH, hGH, TSH, Prolactin, CAM5.2, ACTH, TPIT, Pit1 and SF1. Other immunostains including synaptophysin, olig2, GFAP, and so forth were also performed on selected cases. All cases were sent to the NIH/NCI for methylation profiling.
Results: Case 1: “low grade papillary neuroendocrine tumor, favor pituitary adenoma,” with no expression of hormones, PIT1, SF1 and very focal cells positive for TPIT. Methylation profiling reported consensus class of “pituitary adenoma, ACTH.” Case 2: “papillary neoplasm, with neuroendocrine and glial expression,” with no expression of hormones, PIT1, SF1, very focal TPIT positivity, and GFAP positivity. Methylation profiling reported: “corticotroph PitNET/adenoma.” Case 3: “most consistent with TPIT positive corticotroph adenoma, silent type,” with focal expression of ACTH and positivity for T‐PIT. Methylation profiling confirmed a “corticotroph adenoma.”
Conclusion: Additional workup and methylation profiling may be helpful in subtyping of papillary neuroendocrine tumors/lesions of the skull base. This is especially warranted when the immunostaining is equivocal, suggestive of a non‐functioning adenoma, and/or an aggressive subtype, such as the “silent corticotroph.”
eP‐NO‐A100
A rare case of light chain deposition disease in brain—Diagnosis and management in a 34‐year‐old female
F. Al Sufiani 1, A. AlAssiri1, D. Pinilla Arias2
1Ministry of National Guard Health Affairs (MNGHA), Pathology and Laboratory Medicine, Riyadh, Saudi Arabia; 2Ministry of National Guard Health Affairs (MNGHA), Neurosurgery, Riyadh, Saudi Arabia
Background: Light chain deposition disease (LCDD) is a rare condition characterized by the deposition of monoclonal immunoglobulin light chains in various organs, typically affecting the kidneys. Involvement of the central nervous system (CNS) is exceedingly rare. We present a unique case of a 34‐year‐old female with isolated LCDD in the brain.
Case presentation: The patient presented with a 1‐month history of slurred speech, without accompanying nausea, vomiting, seizure, headache, weakness, or weight loss. MRI brain revealed a well‐circumscribed right parietal lobe subcortical lesion displaying low T1 and heterogeneously high T2 signal, central linear high T1 signal with T2 blooming, and heterogeneous avid enhancement. T2‐FLAIR mismatch within the solid component favored astrocytoma over oligodendroglioma. Following craniotomy and gross total resection, histopathological examination identified the lesion as LCDD, characterized by amorphous nonamyloidogenic material deposition surrounded by dense lambda‐restricted lymphoplasmacytic aggregates. Adjacent brain parenchyma was gliotic. The patient underwent a comprehensive multiple myeloma workup, which returned negative results. She was subsequently treated with triple intrathecal therapy (methotrexate, hydrocortisone, cytarabine) and discharged in good condition.
Conclusion: This case report highlights the diagnostic challenge posed by isolated CNS LCDD in the absence of systemic manifestations. Accurate diagnosis is crucial for appropriate management and prognosis. This case contributes to the limited literature on LCDD in the brain and underscores the importance of considering LCDD in the differential diagnosis of CNS lesions.
References: [1] https://doi.org/10.1177/1066896917717338. [2] https://doi.org/10.1016/j.humpath.2006.07.010.

FIGURE 1. Amorphous nonamyloidogenic material deposition surrounded by dense lambda‐restricted lymphoplasmacytic aggregates. (A) low‐magnification, (B) high mag, (C) PAS, (D) H&E, (E) Kappa, (F) Lambda.

FIGURE 2.
eP‐NO‐A101
Brain metastasis from scalp pleomorphic dermal sarcoma—A rare case report
A. G. Shivane 1, D. A. Hilton1, A. Oriolowo1, K. Pearce2, E. Lim3, P. Fewings4
1University Hospitals Plymouth NHS Trust, Department of Cellular and Anatomical Pathology, Plymouth, United Kingdom; 2University Hospitals Plymouth NHS Trust, Department of Radiology, Plymouth, United Kingdom; 3University Hospitals Plymouth NHS Trust, Department of Oncology, Plymouth, United Kingdom; 4University Hospitals Plymouth NHS Trust, Department of Neurosurgery, Plymouth, United Kingdom
Clinical History: A 69‐year‐old man presented to our hospital with recent history of collapse and seizure. On clinical examination he had right hand weakness and expressive dysphasia. He had previous excision of left sided scalp lesion in 2021 which confirmed a pleomorphic dermal sarcoma. He also had surgery for right temple lesion which was a squamous cell carcinoma. MRI head showed a left frontal lesion. There was no direct invasion through skull at the site of previously operated scalp lesion. A CT scan of thorax, abdomen and pelvis did not show any significant lesion. He underwent operation to biopsy the left frontal rapidly growing lesion.
Histology: The core biopsies from left frontal lesion showed a cellular tumour composed of pleomorphic rounded/epithelioid and occasional spindle cells with round to oval nuclei arranged in diffuse sheets and around blood vessels. There were small areas of necrosis, but vascular endothelial proliferation was not prominent. Histology from the previous scalp lesion was reviewed and the appearances were in keeping with pleomorphic dermal sarcoma. Immunohistochemistry of the brain lesion showed strong expression of CD10 (similar to the scalp sarcoma), but only occasional cells stained with EMA and P53 antibodies. The GFAP, IDH1 (R132H), cytokeratins (MNF116, Cam5.2), synaptophysin, S100, Melan A, CD3, CD20 and SMA stains were negative in the tumour cells. Tissue was further analysed using DNA methylation profiling (sarcoma classifier v12.2) which confirmed an atypical fibroxanthoma/pleomorphic dermal sarcoma with a confidence score of 0.75. Follow‐up MRI showed two additional lesions. He is now undergoing radiotherapy to the lesions.
Conclusion: Brain metastases from a pleomorphic dermal sarcoma is extremely rare and there is only one previously reported case in the medical literature. This will be the second case of cerebral metastasis from a scalp pleomorphic dermal sarcoma.

FIGURE 1.

FIGURE 2.
eP‐NO‐A102
A rare case of a metastatic hepatocellular carcinoma to the pituitary gland
L. Robinson 1, S. Barnes1, W. Couldwell2, J. Alt3, Q. Mao1, R. Rennert2, M. Kohler1
1University of Utah, Pathology, Salt Lake City, UT, United States; 2University of Utah, Neurosurgery, Salt Lake City, UT, United States; 3University of Utah, Head and Neck Surgery, Salt Lake City, UT, United States
Introduction: A 52‐year‐old female, with no previous history of malignancy, presented with persistent right orbital headaches, diplopia, and epistaxis. Magnetic resonance imaging of the brain demonstrated a large centrally necrotic cystic/solid mass centered in the region of the sella. Endocrine testing was within normal limits. The patient underwent transsphenoidal resection of the pituitary mass. Intraoperative consultation revealed a solid tumor composed of epithelioid cells with ample eosinophilic cytoplasm and high‐grade nuclear atypia.
Objectives: Most sellar‐based tumors are pituitary adenomas often accompanied by endocrine abnormalities or focal neurologic deficits correlating with the patients’ initial clinical presentation. Metastases to the pituitary gland are very rare and account for approximately 1% of all pituitary tumors in the sellar region with a vast majority of them being comprised of carcinomas from the lung, breast, and colon.
Materials and Methods: Histological assessment of the tumor sections with special and immunohistochemical stain interpretation.
Results: Hematoxylin and eosin sections showed a malignant epithelioid neoplasm with tumor cells arranged in cohesive clusters, sheets, and trabeculae with tumor cells having abundant eosinophilic cytoplasm, pleomorphic nuclei, and prominent nucleoli. Endothelial wrapping was present around clusters of tumor cells, which is suggestive of hepatocytic differentiation. Tumor cells were positive for hepatocyte specific antigen (HSA), arginase, and CAM5.2 while simultaneously staining negative for CK7 and CK20. The final rendered diagnosis was metastatic carcinoma, consistent with hepatocellular carcinoma.
Conclusions: Metastatic hepatocellular carcinoma to the pituitary gland is an exceedingly rare entity with only 15 cases being reported in the medical literature. This case emphasizes the importance for consideration of rare metastatic carcinomas of unknown primary to the pituitary gland.

FIGURE 1.

FIGURE 2.
eP‐NO‐A103
Imaging‐pathological findings of lesions in the sillar region in a tertiary care center in Mexico
M. T. Espinosa Romero 1, L. G. Chávez Macías1, E. Gómez Apo1, A. Escobar España1, L. A. Téllez Manríquez1, W. R. Toscano‐Rengifo1, D. Villa Sepúlveda2
1Hospital General de México, Neuropathology, Mexico City, Mexico; 2Hospital General de México, Pathology, Mexico City, Mexico
The sellar region is a complex area and is related to other structures in which lesions of diverse etiology can originate, including developmental anomalies, inflammatory processes, metastases, and primary neoplasms, mainly pituitary adenoma/PitNET. Contrast‐enhanced magnetic resonance is the imaging study of choice to evaluate this region; however, despite the great precision it offers, the need for a histopathological diagnosis is essential to determine the treatment and prognosis of the patient. The present study is carried out to determine the epidemiology of lesions in the sellar region at Mexico General Hospital “Dr. Eduardo Liceaga” (HGMEL) and to evaluate the concordance of the findings in imaging studies with the histopathological result. The Neuropathology Unit database was used, including incisional and excisional biopsies, from 2011 to 2021 with imaging studies present in the Comprehensive Hospital Administration System‐HGMEL PACS System. A sample of 645 cases of lesions in the sellar region was used. The most frequent lesions were in the age group of 40 to 59 years (305 cases, 47.3%), female gender (339 cases, 52.9%) and size greater than 1.0 cm (428 cases, 66.4%). Pituitary adenoma/PitNET is the most frequent lesion (85.4%), followed by adamantinomatous craniopharyngioma (30%) and meningioma in third place (13%). The concordance between the histopathological‐imaging diagnosis is 87.7%. Conclusion: In the HGMEL, lesions in the sellar region are diagnosed more frequently in women and in the age group of 40–59 years by means of imaging studies, however, although they have very good diagnostic accuracy, since the variety of lesions in said location is so wide and of different etiology, it is essential to carry out a histopathological study to integrate an accurate diagnosis.
Reference: [1] Chaudhary S, Prakash A, Gupta P. Role of MRI in evaluation of sellar, parasellar and suprasellarlesion with histopathological correlation. IJCR. 2019;11(8):6084–93.
eP‐NO‐A104
Transcriptomic analysis of ZFTA‐fusion positive and negative ependymoma reveals significant differential dysregulation of genes related to important signalling pathways—Report from a tertiary care centre in North India
K. Gupta 1, A. Saraswati1, P. Bhatia1, A. Verma1, P. Salunke1, B. Radotra1, N. Kumar1
1Postgraduate Institute of Medical Education and Research, Histopathology, Chandigarh, India
Question: Ependymoma (EPN) are classified according to the anatomic site and molecular signature in the 2016 WHO classification of CNS tumors. ZFTA negative EPN form a minor elusive subset at supratentorial (ST) location. We hypothesized that differential gene expression among these fusion positive and negative tumors could be due to their underlying epigenetic differences.
Methods: Forty fusion positive and negative EPN were selected based on immunoreactivity for NF‐kβ effector proteins and sequencing for known fusion transcripts, followed by transcriptomic analysis on 14 fusion negative and 5 fusion positive EPN. Gene Ontology (GO) and KEGG pathway analysis were performed for functional and pathway enrichment. Methylation pattern of 5 top up‐regulated and down‐regulated genes was evaluated using methylation specific PCR. Survival differences were sought in these subgroups.
Results: Transcriptomic analysis showed dysregulation of genes related to NF‐kβ and TNF‐β pathway (NFKBIL1, NFKB2, IL1B, PTGS, TNFRSF1B) in fusion positive EPN while fusion negative tumors demonstrated dysregulation of genes (FOXJ1, PARD6B, FGF19) related to Hippo and Notch pathway. The dysregulated gene difference in both the subgroups was noted to be epigenetically controlled based on concordant methylation status of these genes. Follow‐up ranged from 12 days to 65 months (median = 65 days). Survival analysis performed for fusion negative and positive tumors, and for methylated and unmethylated subgroups did not reveal any statistically significant difference in the outcome.
Conclusion: Our data reveals distinct dysregulation of NF‐kβ and TNF‐β pathway genes in fusion positive EPN in comparison to Hippo and Notch pathways genes in fusion negative EPN. Although, our sample size was limited, we did not identify any survival differences across these subgroups.
eP‐NO‐A105
Anaplastic evolution of pilocytic astrocytomas—A case report and review of the literature
L. Lebrun 1, H. B. Pouleau2, C. Van Campenhout1, S. Rorive3, C. A. Maurage4, F. Escande5, I. Salmon1
1Erasme Hospital, Department of Pathology, Brussels, Belgium; 2Centre Hospitalier Universitaire (CHU) TIVOLI, Department of Neurosurgery, La Louvière, Belgium; 3Centre Universitaire inter Régional d'expertise en Anatomie Pathologique Hospitalière (CurePath, CHIREC, CHU Tivoli, ULB), Department of Pathology, Jumet, Belgium; 4CHU Lille, Department of Pathology, Lille, France; 5CHU Lille, Service de Biochimie et biologie moléculaire, Lille, France
Introduction: Pilocytic astrocytomas (PA) represent the most common and indolent CNS tumor in the pediatric population. These grade 1 tumors can harbor anaplastic features leading to the terms of “pilocytic astrocytoma with histological anaplasia” according to the 2021 WHO classification. Scare data are available regarding their molecular profiles and clinical evolution. The objectives here are to provide clinico‐pathological, molecular and epigenetics features of a case diagnosed as “pilocytic astrocytoma with histological anaplasia” with an extensive review of the literature.
Methods: Molecular analyses were performed by NGS (14‐genes and KIAA1549‐BRAF fusions panels), CDKN2A FISH and DNA‐methylation profiling. A literature review regarding “Pilocytic astrocytoma with histological features of anaplasia” was conducted.
Case report: A 15‐year girl case harbored in 2019 a cerebellar cystic lesion for which complete surgical resection was performed. Microscopic examination revealed typical PA morphology. Mitotic figures and necrosis were not seen. Molecular analyses reported BRAF T599dup mutation. In 2022, follow‐up MRI suggested a tumoral recurrence. We observed highly cellular tumoral lesion with geographical necrosis and numerous mitosis leading to the diagnosis of “pilocytic astrocytoma with anaplastic features.” BRAF T599dup mutation and no CDKN2A deletion were reported. DNA‐methylation brain classifier v12.5 classified the case as LG glial/glioneuronal/neuroepithelial tumours, MC infratentorial PA (cs = 0.84). CNV profile suggested gain of whole chromosomes 6, 7, 10 and 12. No adjuvant treatment was provided and for now, no recurrences were observed.
Conclusion: The clinical evolution, molecular and epigenetics profiles of “pilocytic astrocytoma with histological anaplasia” seem to be different than those observed in PA and anaplastic astrocytoma with piloïd features. Further investigation could precise the prognosis and the evolution for these patients.
eP‐NO‐A106
High‐risk neuroblastoma with recurrence 28 years after initial diagnosis—A case report
M. Kritselis 1, M. Punsoni1, H. Mistry1, J. Boxerman1
1Rhode Island Hospital, Neuropathology, Providence, RI, United States
Introduction: Neuroblastoma (NB) is the most common neoplasm during the first year of life, and the most common extracranial solid tumor in the first two years of life. Patients with NB are classified into risk‐groups based on a combination of predictive factors, with variable patterns of event‐free survival. In particular, high‐risk neuroblastoma (HR‐NB) accounts for approximately half of all patients diagnosed with NB.
Materials and Methods: We present the first reported case of an individual with high‐risk neuroblastoma initially diagnosed at two years of age, who presented with spinal cord compression secondary to an extradural neuroblastoma, 28 years following initial diagnosis. In addition, we review the current literature for reports of recurrence in patients with neuroblastoma.
Results: High‐risk neuroblastoma was originally associated with a <50% 5‐year event‐free survival. While these odds have improved over time due to advances in treatment, 50%–60% of children with HR‐NB experience relapse or fail to respond to neoadjuvant therapy, with a median progression‐free survival of 6.4 months, overall 4‐year progression‐free survival, and survival rates of 6% and 20%. While the median time from diagnosis to first relapse/progression ranges from 18.7 to 22 months, there are rare cases of late recurrence. Very rarely patients have been reported to develop late recurrence of NB up to 20 years after the initial diagnoses.
Discussion: This novel report reinforces that close monitoring is important in patients with HR‐NB, as well as suggests that extreme outliers exist, and additional investigation of these individuals may contribute to our understanding of this common and deadly disease.
eP‐NO‐A107
An unusual spinal tumour with meningeal and histiocytic features—A case report
A. G. Shivane 1, D. A. Hilton1, R. Sivakumaran2, S. Brandner3
1University Hospitals Plymouth NHS Trust, Department of Cellular and Anatomical Pathology, Plymouth, United Kingdom; 2University Hospitals Plymouth NHS Trust, Department of Neurosurgery, Plymouth, United Kingdom; 3The National Hospital for Neurology and Neurosurgery, Department of Neuropathology, London, United Kingdom
Clinical History: A 58‐year‐old man presented to our hospital with progressive weakness and back pain. MRI head showed a well circumscribed intradural extramedullary cervico‐thoracic lesion with no clear dural attachment. He had no significant past medical history. He underwent operation to resect the growing spinal lesion.
Histology: The resection specimen showed a cellular tumour composed of fascicles of bland‐appearing spindle cells with admixed foamy histiocytes, prominent Touton giant cells and focal sparse small lymphocytic infiltrates. There were occasional perivascular whorl‐like structures, but no psammomatous calcification, increased mitoses or necrosis was identified. Immunohistochemistry showed strong expression of EMA and weak focal SSTR2 staining in the spindle cell component and positivity for macrophage markers (CD68, CD163) within the histiocytes and Touton giant cells. The S100 and CD1a stains were negative in the tumour. Tissue was further analysed using DNA methylation profiling, the earlier Heidelberg brain tumour classifier (v11b4) classified this tumour as meningioma, however, the new brain tumour (v12b6) and sarcoma classifier (v12.6) failed to classify this tumour.
Conclusion: This is a highly unusual benign‐appearing tumour, although has some features raising the possibility of a meningioma, the presence of histiocytes and multinucleated Touton giant cells are unusual. The differential diagnoses and challenges to make a definitive diagnosis are discussed.

FIGURE 1.

FIGURE 2.
eP‐NO‐A108
Comparison of clinicopathological differences between the RICH lesions of the brain according to the type of radiation treatment and preceding lesions
S. H. Kim 1
1Yonsei University, College of Medicine, Pathology, Seoul, South Korea
Introduction: Radiation‐induced organizing hematoma (RIOH) is a sporadic form of cavernous hemangioma and a late complication of cerebral radiation. RIOH lesions are histologically distinct from de novo cavernous hemangioma; however, detailed research on this subject is lacking.
Objective: We aimed to evaluate the clinical and histological features of RIOHs according to causative lesions.
Patients and Methods: Thirty‐seven RIOHs confirmed by surgical excision from January 2009 to May 2020 in Yonsei Severance Hospital were included in the analysis. Clinical data, including age, sex, tumor site, multiplicity, and latency (time taken to diagnose RIOH after the last radiation), were obtained. We also compared the size and wall thickness of the original tumors and RIOHs. All cases were divided into subgroups based on the type of radiation treatment (gamma knife surgery [GKS; N = 24] vs. conventional radiation therapy [RT; N = 13]) and the pathology of the original lesion (arteriovenous malformation [N = 14]; glioma [N = 12]; metastasis [N = 4]; other tumors [N = 7]). The clinicopathological results were compared between the groups.
Results: The GKS group showed longer latency (5.85 ± 4.06 years vs. 11.15 ± 8.27 years, p = 0.046) and thicker tumor wall (693.7 ± 565.7 μm vs. 406.9 ± 519.7 μm, p = 0.049) than the RT group. No significant difference was found according to the pathology of the original lesion.
Conclusions: We suggest that RIOH is more likely to occur earlier with thick tumor wall in cases that underwent GKS rather than those that underwent conventional RT.

FIGURE 1.
eP‐NO‐A109
Application of CXorf67 and H3K27me3 protein in pathological diagnosis of germinoma of central nervous system
J. Xiong 1, Z. Du1, Y. Wang1, F. Tang1
1Huashan Hospital Fudan University, Pathology, Shanghai, China
Introduction: To investigate immunohistochemical expression of CXorf67 and H3K27me3 in central nervous system germ cell tumors (CNS GCTs) and to assess value of both in diagnosis and differential diagnosis.
Methods: Three hundred and seventy cases of central nervous system germ cell tumors were collected from 2013 to 2020 at Department of pathology of Fudan University Affiliated Huashan Hospital. To analyses the expression of CXorf67, H3K27me3 and common indexes OCT4, PLAP, CD117, D2‐40, CD30 by immunohistochemistry (EnVision) in different subtypes of CNS GCTs. The sensitivity and specificity of each index were compared by contingency table and area under ROC curve.
Results: Cxorf67 was specifically highly positive in the nuclei of germinoma and normal germ cell, but not in other subtypes; H3K27me3 was negative in germinoma, but positive in nuclei of GCTs without germinoma and surrounding normal tissue. In 283 GCTs with germinoma components, the positive expression rates of CXorf67 were 90.5% (256/283), but all cases were not expressed H3K27me3. There was a significant negative correlation between them (r 2 = −0.8309, p = 0.00); In 63 MGCTs with germinoma components, the positive expression rates of CXorf67 were 84.10% (53/63), but all cases were not expressed H3K27me3. The area ranking under the ROC curve of each index was H3K27me3, CXorf67, D2‐40, OCT4, PLAP, CD117 respectively (p < 0.05).
Conclusion: CXorf67 and H3K27me3 have strong sensitivity and high specificity in the differential diagnosis of germinoma. There is significant negative correlation between them. Both of them can be used as new specific immunohistochemical indexes in the diagnosis of germinoma.

FIGURE 1.
eP‐NO‐A110
MGMT gene promoter methylation in diffuse midline glioma, H3K27‐mutant
P. Shah 1, M. Gurav1, P. Bapat1, S. Hatkar1, A. Sahay1, G. Chinnaswamy1, P. Shetty1, A. Moiyadi1, O. Shetty1, S. Epari1
1Tata Memorial Hospital, Mumbai, Pathology, Mumbai, India
Introduction: Diffuse midline glioma, H3 K27‐altered (DMG) are biologically hypomethylated. However, the literature is deficient on O6‐methyl‐guanine‐DNA methyltransferase (MGMT) promoter methylation status on this entity.
Objective: Evaluation for MGMT‐promoter methylation in DMG.
Materials and Methods: Forty‐three cases of DMGs were evaluated for MGMT‐promoter methylation by methylation‐specific PCR using primers for both methylated and unmethylated sequences of MGMT gene‐promoter, and correlated with various clinicopathological parameters.
Results: (Table 1). Age ranged from 6 to 56 years (Median: 30; 0–6 years: 1; 7–18 years: 9; 19–25 years: 6; 26–39 years: 16; ≥40 years: 11); 26 (60.5%) were males and 17 (39.5%) were females. Twenty‐seven cases (62.8%) were supratentorial in location (including thalami, pineal and third ventricular), 11 (25.6%) were in the posterior fossa (pons, cerebellum, midbrain and medulla oblongata) and 5 (11.6%) in the spinal cord. Five cases (11.6%; age‐ranged 30–40 years) showed MGMT gene‐promoter methylation—4 were supratentorial (all of thalamic region, 2 of them were extending into temporal cortex) and one of posterior fossa (parapontine region). Histologically, 42 were high grade and the other case was of low‐grade morphology (45‐year female, pineal location). All 25 sequenced cases showed H3F3A mutation. Median follow up period was 7 months (0–79 months) for 23 cases. Cases with methylated MGMT promoter showed 66.7% 1‐year overall survival, whereas the unmethylated group showed 46.6% (p = 0.267).
Conclusion: MGMT‐promoter methylation in DMGs is uncommon; it is not seen in <25 years age‐group but is uncommon in younger adults. No significant correlation for the location observed, though methylation was more common in supratentorial location.

FIGURE 1.

eP‐NO‐A111
Cervical extramedullar intradural intermediate grade melanocytic neoplasm—An aggressive evolution
L. G. Chávez Macías 1, E. Gómez Apo1, G. Aristi Urista1, J. Garduño Becerra1, M. Madrazo Moya1
1Hospital General de México, Pathology, Mexico City, Mexico
Introduction: Melanocytomas are infrequent tumours, account for 1 case per 10 million population. They occur at any age, most frequently in the fifth decade with a slight female predominance. Most arise in the extramedullary, intradural compartment of cervical and thoracic spine, dural‐based or nerve associated. They can arise from the leptomeninges and in the trigeminal cave and associate with naevus of Ota.
Objectives: Since melanocytoma is an infrequent tumour that lacks anaplastic features, it is very difficult to predict recurrence, invasion of CNS or malignant transformation, so it is useful to share this case.
Patient and Methods: A woman, 30‐year‐old, presented with long term neck pain. She had a well circumscribed, intradural tumour located in C2‐C3 cervical spine, hyperintense on T1 MRI. It was fully excised. The tumour measured 2.5 × 2.0 cm with a tiny pedicle, dark brown, soft (Figure 1). The tumour cells were forming nests, oval shaped with heavily pigmented cytoplasm (Figure 2) and bland nuclei with some small nucleoli, very scant mitotic figures and a Ki67 index of 1%. Immunohistochemistry demonstrated HMB45 and MelanA positivity. One year later she went back to surgery with a very similar nodule, in the same location, during pregnancy. The tumour was operated and looked identical. Two years after first surgery the tumour has grown to reach ventral aspect of the pons. She died a few days after third surgery. This time the neoplasm invaded pons, and the only histological differences were more prominent nucleoli and mitotic index of 4%.
Results: First and second specimens were diagnosed as melanocytoma. Third was as intermediate grade melanocytic neoplasm.
Conclusion: In our institutions there is very limited access to molecular diagnosis, it was not possible to determine mutations of GNAQ, GNA11, losses of chromosome 3 or 6, TERT, BRAF and KIT, or even changes in DNA methylation patterns, that can be characteristic or predictor of malignant behaviour in melanotic neoplasms.

FIGURE 1.

FIGURE 2.
eP‐NO‐A112
Primary CNS lymphoma presenting as hemichorea hemiballismus
N. Sharma 1
1PGIMER, Neurology, Chandigarh, India
Sixty‐one‐year‐old female presented with three weeks history of acute onset abnormal involuntary movements of right half of body. These movements were irregular, non‐rhythmic, purposeless with intermittent flinging of right arm. There was no history of headache, seizures and vision loss. She had a significant past history of sensorineural hearing loss which recovered with short course of oral steroids 18 months prior to the presentation. For current symptoms she received iv methylprednisolone pulse for 5 days and she started to recover over 1 month. Examination showed increased tone on right upper and lower limb with normal sensory examination. She was started on tetrabenazine titrations gradually maximum up to 75 mg/day. Her hemichorea and hemiballismus responded to treatment but subsequently during admission she developed right hemiparesis with right upper motor neurone facial palsy. Lab investigations showed normal hemogram and biochemistry. CSF showed 170 cells, 170 mg/dL protien and 54 mg/dL sugar. MRI brain showed T2 FLAIR hyperintensity and heterogenous contrast enhancing lesion in left gangliocapsular region extending up to subthalamus. FDG PET done showed increased FDG uptake in left globes palladium, internal capsule and thalamus. Stereotactic brain biopsy was done and was suggestive of lymphoma as histopathology examination showed atypical lymphoid cells with perivascular accentuation and CD20 diffuse membranous positivity consistent with diffuse large B cell lymphoma.
eP‐NO‐A113
Multiple abnormalities of neurofibromatosis type 2 (meningiomatosis, vestibular schwannomas, at the cervicomedullary junction with syringomyelia‐syringobulbia and cortical hamartia) in a previously undiagnosed man—Autopsy case report
D. Villa Sepúlveda 1, L. A. Camacho‐Rodríguez1, C. A. Durán López2, L. A. Téllez Manríquez2, W. R. Toscano‐Rengifo2, M. T. Espinosa Romero2, V. González‐Flores1, L. G. Chávez Macías2, A. Escobar España2, E. Gómez Apo2
1Hospital General de México, Anatomical Pathology, Mexico City, Mexico; 2Hospital General de México, Neuropathology, Mexico City, Mexico
Background: NF 2 is an autosomal dominant genetic syndrome, characterized by the formation of multiple CNS tumors, the most frequent being bilateral vestibular schwannomas, accompanied by tinnitus, sensorineural hearing loss, and balance disturbance, in addition to skin manifestations. This is the autopsy report of a case of NF2 with a fatal outcome secondary to intracranial hypertension associated with multiple central nervous system tumors.
Autopsy Case Report: A 34‐year‐old man, the final condition began with two convulsive crises the day before death, he was received in the emergency department with no audible heart rate, and no response to stimuli, advanced management of the airway was required, and he died. His relatives mentioned that he suffered from headaches, hearing loss, vision disturbances, seizures, and intracranial hypertension that required placement of a ventricular peritoneal shunt after a month of evolution.
Results: The autopsy findings were: On the exterior habitus, there are some “café au lait” spots with distribution on the thorax and legs; also, with few skin schwannomas. In CNS, there are bilateral vestibular schwannoma, hydrocephalus, meningiomatosis (including intraventricular and intrasellar meningioma), ependymoma at the cervicomedullary junction with syringomyelia‐syringobulbia. Microscopically, with abundant hamartia with diffuse distribution in the brain. Upon opening the thoracic and abdominal cavities, pulmonary thromboembolism was identified with pulmonary infarctions, and concentric left ventricular hypertrophy. Also, a microscopic meningioma was observed in the pulmonary parenchyma.
Conclusions: The morphological characteristics of the multiple lesions in this case allow us to reach the diagnosis of type 2 neurofibromatosis, it is the first case diagnosed in the family. It would be ideal to have genetic and molecular biology studies to carry out an integrated diagnosis that allows confirming the syndrome.
eP‐NO‐A114
Ganglioneurocytoma of septum pellucidum with prominent dystrophic axonal spheroids
S. Al‐Dandan 1,2, G. Al‐Zahrani3, W. AlShakweer1
1King Fahad Medical City, Anatomic Pathology Department. Pathology and Clinical Laboratory Medicine Administration, Riyadh, Saudi Arabia; 2King Fahad Medical City, Anatomic Pathology Section. Department of Laboratory and Blood Bank, Al‐Ahsa, Saudi Arabia; 3King Fahad Medical City, Department of Adult Neurosurgery. National Neurologic Institute, Riyadh, Saudi Arabia
Introduction: Ganglionic differentiation is common in extra‐ventricular neurocytomas but rare in central locations (septum pellucidum). The presence of dystrophic axonal spheroids (DAS) is a distinctive finding in neurocytomas, with only two reported cases in the English literature.
Objectives: We aimed to describe the morphologic features of ganglioneurocytoma with DASs.
Patients and Methods: A 50‐year‐old female presented to the emergency department with a 2‐month history of bifrontal headaches and episodic blurred vision. Brain MRI revealed a septum pellucidum lesion near the foramen of Monro associated with a cystic component, faint enhancement, calcification, and mild hydrocephalus. The patient underwent a right craniotomy and tumor resection under neuronavigation.
Results: Microscopic examination demonstrated a neuroepithelial tumor composed of sheets of uniform round cells with monotonous nuclei and finely speckled chromatin. There were few neurocytomatous rosettes and frequent ganglion and ganglioid cells. DASs were round to oval and were faintly to densely eosinophilic. Some spheroids had a dense core, pale halo, and narrow peripheral clefting. The spheroids were PAS‐positive and reacted positively to synaptophysin, chromogranin, and neurofilament immunostains. Next‐Generation Sequencing detected no reportable pathogenic mutations or fusions.
Conclusion: Diagnostic challenges surfaced when distinguishing DASs from eosinophilic globular bodies, ballooned cells, and various aggresomes of neurodegeneration (dystrophic axons, Lafora bodies, Lewy bodies, and corpora amylacea). The overall pattern of reactivity of the spheroids to histochemical and immunohistochemical stains indicated neuronal‐axonal derivation. DASs may occur in the central and peripheral nervous system under many circumstances, both physiological and pathological. The presence of DASs in ganglioneurocytoma is a unique finding and has been exceptionally reported in the literature.

FIGURE 1.

FIGURE 2.
eP‐NO‐A115
Primary central nervous system lymphoma accompanied with amyloid angiopathy—An autopsy case report
C. Mao 1, J. Gao1, Y. Guo1
1Peking Union Medical College Hospital, Neurology, Beijing, China
A 47‐year‐old female was admitted to PUMCH with progressive memory loss, cognitive impairment and incontinence for 1 month. The patient was found unable to work and could not find washroom at home 1 month ago. She also had episodic headache without vomiting. A clonic tonic seizure was occurred. She progressively had neuropsychiatric symptoms including screaming and irritability. She suffered from right occipital and temporal lobe hemorrhage respectively 10 and 2 years ago. No hypertension or DM history was presented. After admission, head MRI showed widespread white matter lesions in posterior temporal, occipital and parietal lobe. MRA showed stenosis in right ICA, MCA and PCA. LP: pressure >350 mm H2O, WBC 10/mm3; GLU 77 mg/dL, PRO 192 mg/dL, CL 119 mg/dL, OB(+). CSF cytology revealed no malignant cells. Although active treatment was given, the patient progressed to left hemiplegia and coma. She died of respiratory and renal failure. On autopsy, the brain weighted 1450 g. Macroscopically, bilateral cerebellar tonsillar herniation was seen. Vascular malformation was found on circle of Willis. Necrosis and lesions were found in cerebral white matter, basal ganglia, corpus callosum on coronal sections. Microscopically, wide spread tumors cells were found invading temporal lobe, occipital lobe, hippocampus, basal ganglia, corpus callosum and brain stem. Tumor cells were small round, with large nuclear and atypia. Tumor cells were angiocentric and invading via Virchow‐Robin space. The tumor cells were CD20 positive B cells which supporting large B cell lymphoma. Besides, old softening lesions with hemosiderin deposition was found in temporal and occipital lobe. Amyloid deposition was detected in small vessels in occipital lobe and subarachnoid space. Structure malformation was found in circle of Willis without arthrosclerosis. It was a rare case presented with both primary central nervous system large B cell lymphoma and cerebral amyloid angiopathy.

FIGURE 1.
eP‐NO‐A116
Sellar high‐grade astrocytoma with piloid features—Case report with literature review
Y. Yousfi 1
1SAAD Dehlab University, Medecine, Blida, Algeria
Introduction: High‐grade astrocytoma with piloid features (HGAP) is a recently described brain tumor entity showing high grade piloid and/or glioblastoma‐like histological features and a distinct DNA methylation profile. It has been integrated in the World Health Organization classifcation of central nervous system tumours in 2021.
Materials and Methods: One case has been identified: A 53‐year‐old woman presented with headaches and rapid deterioration in visual acuity over a period of 6 month with symptoms of diabetes insipidus.
Results: Brain MRI demonstrated a large ovoid shaped lesion measuring (4.1 × 3.3 × 3.2) cm, involving the intra‐sellar and the suprasellar region. The margins of the lesion were not well defined. The lesion was relatively homogenous with isointense T1 and hyperintense T2 signals. Following intravenous Gd‐DTPA injection, the lesion showed significant heterogenous enhancement: it had enveloped the internal carotid arteries on both sides and had infiltrated the bilateral cavernous sinuses, the floor of the third ventricle and the hypothalamus region. Microscopic examination shows pituitary parenchyma massively infiltrated by glial‐like cell proliferation arranged in microcystic masses of high cellularity, associated with a component of giant and pleomorphic cells. The vascularization is abundant, focally proliferative. No evidence of necrosis. Positivity of Olig2, loss of nuclear ATRX expression, IDHR132H and BRAF negativity, no EGFR amplification in the tumour cells have been reported in immunohistochemistry study. the correlation between the morphological aspects and the immunohistochemical profile pleads for the diagnosis of high‐grade astrocytoma with piloid features.
Conclusion: High‐grade astrocytoma with piloid features is a recently described glial tumour with variable histological features requiring DNA methylation profiling to establish the diagnosis. Here, we contribute by reporting this case original by its sellar localisation.
eP‐NO‐A117
Immunohistochemical expression of H3K27me3 protein in IDH‐mutant gliomas
V. Raje 1, E. Sridhar1, A. Sahay1, A. Shah1, T. Gupta2, A. Moiyadi3, P. Shetty3
1Tata Memorial Centre, Pathology, Mumbai, India; 2Tata Memorial Centre, Radiation oncology, Mumbai, India; 3Tata Memorial Centre, Neurosurgery, Mumbai, India
Introduction: Immunohistochemical expression of H3K27me3 protein in IDH‐mutant gliomas is one of the emerging markers of diagnostic relevance.
Objective: To study the pattern of immunohistochemical expression of H3K27me3 protein in IDH‐mutant gliomas.
Materials and Methods: One hundred and twenty‐six cases of IDH‐mutant gliomas (64 cases with oligodendroglial morphology and 62 cases of astrocytomas) comprised the study cohort. The patterns of H3K27me3 protein expression were noted and also correlated with 1p19q co‐deletion status wherever the data was available.
Results: Sixty‐one of 64 cases of oligodendroglial morphology were IDH1R132H‐mutant and others were IDH2R172K‐mutant. Thirty‐nine out of these 64 cases were canonical oligodendroglioma with 1p19q co‐deletion; of which 31 (79.50%) showed underexpression (weak or loss of expression) of H3K27me3 protein; 6 (15.40%) showed retained expression and in 2 cases, IHC was non‐contributory. 1p19q co‐deletion status was either not available or uninterpretable in 25 cases, which were classified as oligodendroglioma, NOS based on histomorphology and retained ATRX protein expression; of which 19 (76%) showed underexpression (weak or loss of expression) of H3K27me3 protein, 4 (16%) showed retained expression and in 2 cases, IHC was non‐contributory. Of the 62 IDH‐mutant astrocytomas, 20 (32.26%) showed retained expression of H3K27me3 protein, 19 (30.65%) showed loss, 17 (27.40%) showed mosaic pattern and in 6 cases, IHC was non‐contributory.
Conclusion: Differential staining pattern of H3K27me3 protein was observed in IDH‐mutant astrocytic and oligodendroglial tumours but not mutually exclusive. Underexpression of H3K27me3 protein showed significant correlation for 1p19q co‐deletion, however is not exclusive of 1p19q co‐deletion, thus is not a good surrogate for 1p19q co‐deletion.
eP‐NO‐A118
Clinicopathological and molecular study of embryonal tumour with multilayered rosettes
L. Wang 1
1Xuanwu Hospital, Pathology, Beijing, China
Objective: To analyze clinicopathological and molecular features of embryonal tumour with multilayered rosettes (ETMRs).
Methods: A total of 14 cases of ETMRs in Xuanwu Hospital were retrospectively summarized. The clinical and imaging characteristics, pathological and molecular characteristics were analyzed.
Results: All 14 patients (6 males and 8 females) aged from 9 months old to 3 years old (mean 2 years) mainly had a history of headache or/and vomiting. Twelve tumors were supratentorial and two infratentorial, seven of which occurred in the frontal lobe. The enhanced MRI showed abnormal enhancement signals. Pathological finding showed that 14 cases had displaying the morphological characteristics of ETMR, including 13 displaying the morphological characteristics of embryonal tumour with abundant neuropil and true rosettes, and one displaying ependymoblastoma. The distribution of tumor cells is sparse and uneven, and some cells arrange in multiple layers and grow around blood vessels, forming rosettes structure. Mitotic figures are commonly observed. IHC showed Syn and Lin28a were immunopositive in all 14 cases (14/14). GFAP and Olig‐2 were partially immunopositive in 3 cases (3/14). EMA was dot‐and/or‐ring immunopositive in 2 cases (90%, 2/14). At the same time, there was a case immunopositive for H3K27M, with the loss of H3K27me3. Twelve ETMRs were available to detect C19MC and Dicer1 gene mutation. Eleven in 12 (91.7%) were found to have C19MC amplification, and one have Dicer1 mutation as well as H3K27M mutation. Among the 14 patients after surgery, all 10 patients received adjuvant radiotherapy/chemotherapy. Progression‐free survival was 6.2 months, and overall survival was 11 months.
Conclusion: ETMRs have relatively distinguishing clinical and histopathological features. C19MC alteration and Dicer1 gene mutation, can be considered as useful biomarkers for the diagnosis and differential diagnosis, and provide a direction for targeted therapy in the future.

FIGURE 1.

FIGURE 2.
eP‐NO‐A119
Central nervous tissue in ovarian mature teratoma—A histopathological and immunohistochemical study of its neuropathological alterations
M. Shintaku 1
1Kansai Medical University, Pathology, Hirakata, Japan
Introduction: Ovarian mature teratoma frequently contains central nervous system (CNS) tissue that often exhibits a variety of intriguing neuropathological alterations.
Objectives: Our aim is to elucidate the full spectrum of neuropathological alterations seen in CNS tissue of ovarian mature teratoma.
Materials and Methods: These changes in CNS tissue were systematically examined in a series of 251 cases of resected ovarian mature teratoma.
Results: A total of 101 (40.2%) cases of teratoma contained CNS tissue in varying amounts. Neuropil consisting mainly of neuronal and astrocytic processes formed the chief component of the CNS tissue, and ependymal cells and the choroid plexus were found at various rates. In five cases, well‐organized cerebral and/or cerebellar cortical tissues had formed, and a disruption of the glia limitans associated with spillage of cortical tissue into the “subarachnoid” space was observed. Other notable findings included Rosenthal fibers, anemic infarct‐like lesions, hamartoma‐like hyperplasia of arachnoid cells, tubular transformation of the choroid plexus, and various degenerative changes seen in the dendrites of Purkinje cells.
Conclusions: Some of these observations will facilitate a deeper understanding of the pathogenesis of various lesions seen in the human brain.
eP‐NO‐A120
Next generation sequencing (NGS) in glial tumor diagnosis—Single center experience
K. E. Akar 1, M. Sakar2, B. M. Atasoy3, A. Dağçınar2, İ. Ziyal2, S. Uyar Bozkurt1
1Marmara University, Department of Pathology, Istanbul, Turkey; 2Marmara University, Department of Neurosurgery, Istanbul, Turkey; 3Marmara University, Department of Internal Medicine, Istanbul, Turkey
Introduction: Next generation sequencing (NGS) is a term that describe a technology for determining the sequence of DNA or RNA to study genetic variation associated with diseases.
Objectives: Our aim was to demonstrate the role of genetic sequencing in the diagnosis of glial tumors and its association with clinicopathological parameters.
Materials and Methods: Sixty‐eight cases diagnosed with glial tumor between 2021 and 2022 at Marmara University were reviewed for histomorphological and clinical parameters. They also genetically analyzed with targeted NGS method.
Results: The study included 39 males (57.4%) and 29 females (42.6%). The mean age was 44 (range, 4–80) years. Of 68 cases; 23 (34.8%) were located in the frontal lobe, 3 (4.5%) in the occipital lobe, 9 (13.6%) in the midline structures, 11 (16.7%) in the parietal lobe, 4 (6.1%) in the posterior fossa, 16 (24.2%) in the temporal lobe. Microvascular proliferation was seen in 34 (50.7%) cases and necrosis was seen in 33 (48.5%) cases. The mean and standard deviation for mitotic rate was 9.09 ± 13.6 mitoses/10 HPF. When histopathological and molecular findings are compared; TERT promoter mutation was more frequent in cases with >5 mitosis/10 HPF (Fisher's test, p:0.012). Tert promoter mutations were more common in cases with necrosis, but IDH1 mutations were mostly detected in cases without necrosis (Fisher's test, p:0.023). Variables of age, gender, tumor localization, microvascular proliferation and genetic changes were not statistically related. With the NGS method; 11 IDH‐wild type cases with TERT‐promoter mutation and 1 IDH‐wild type case with EGFR mutation were diagnosed as “molecularly‐defined glioblastoma, grade 4.” There were no high‐grade histological features in these 12 cases.
Conclusion: According to the recommendations of WHO classification of tumors of the CNS (2021), molecular changes such as EGFR and TERT mutation are associated with poor prognosis, and their detection in IDH‐wild type glial tumors is diagnostic.

eP‐NO‐A121
Unusual case of ganglioglioma grade 1 transforming into a IDH mutant high grade astrocytoma to glioblastoma (IDH wild type) over 10 years
S. Ahlawat 1, G. Khanna1, F. Ahmad2, A. Pais2, R. Miglani2, R. Patir2, R. K. Gupta3, R. Gogi4
1SRL‐Fortis Memorial Research Institute, Department Histopathology, Noida, India; 2Fortis Memorial Research Institute, Department of Neurosurgery, Noida, India; 3Fortis Memorial Research Institute, Department of Radiodiagnosis, Noida, India; 4SRL‐Fortis Memorial Research Institute, Department of Medical‐Oncologist, Noida
Case Report: Presenting a case of 21‐year‐old young man having a tumour near third ventricle, operated in 2013 and diagnosed as ganglioglioma grade 1. No chemotherapy or radiotherapy was given as it was a near total resection. The tumour recurred in 2017 and this time agin operated and found to have an IDH mutant grade 4 astrocytoma. This is a rare transformation, very few such cases are reported. We are presenting the case with review of literature.
eP‐NO‐A122
Wunderlich syndrome in a woman with tuberous sclerosis complex—Autopsy case report
D. Villa Sepúlveda 1, M. López‐Estrada1, L. A. Téllez Manríquez2, W. R. Toscano‐Rengifo2, M. T. Espinosa Romero2, L. G. Chávez Macías2, A. Escobar España2, E. Gómez Apo2
1Hospital General de México, Anatomical Pathology, Mexico City, Mexico; 2Hospital General de México, Neuropathology, Mexico City, Mexico
Background: Tuberous sclerosis complex is a multisystem autosomal dominant genetic disorder characterized by hamartomas formation, neurological disorders including epilepsy, and intellectual disability. It is generally diagnosed in childhood, unlike our current case. Report an autopsy case of tuberous sclerosis complex, with fatal outcome due to perirenal hematoma associated with rupture of left renal angiomyolipoma (Wunderlich syndrome).
Case Report: A 33‐year‐old woman, the final condition began with sudden abdominal pain of moderate intensity, she went to different hospital units where she was not treated due to lack of physical space during SARS‐Cov2 pandemic. She was received in the emergency unit without vital signs. Her relatives denied any previously diagnosed illnesses.
Results: The autopsy study was performed with the following findings. In the exterior habitus, there are multiple nodules on the face, thorax, and legs, and nail fibromas on the feet. At the opening of the thoracic and abdominal cavities, there is a massive left perirenal hematoma and hemothorax secondary to left renal angiomyolipoma; other findings include angiomyolipoma in the right kidney, and diffuse bilateral pulmonary lymphangioleiomyomatosis. In the brain, there are cortical tubers, paraventricular hamartomas, and a subependymal giant cell astrocytoma. After the autopsy, an interrogation was carried out directed at the next of kin; any familial tumor syndrome was denied; and we were told that the patient has a son with facial nodules, limited cognition, and epilepsy. We do not have genetic studies, although the patient has criteria for tuberous sclerosis. She is probably the first case in her family and surely her son inherited this syndrome.
Conclusions: Wunderlich syndrome refers to spontaneous renal or perirenal hemorrhage that occurs in the absence of known trauma.
eP‐NO‐A123
Frequent co‐occurrence of Alzheimer‐type neurodegeneration in glioblastoma‐adjacent cortex
L. Greutter 1,2, Y. Miller‐Michlits2, S. Klotz2, E. Krause2, P. Stepper3, K. H. Nenning4, B. Baumann1, A. Wöhrer2
1Medical University of Vienna, Center for Medical Physics and Biomedical Engineering, Vienna, Austria; 2Medical University of Vienna, Department of Neurology, Division of Neuropathology and Neurochemistry, Vienna, Austria; 3The Research Center for Molecular Medicine, CEMM, Vienna, Austria; 4The Nathan S. Kline Institute for Psychiatric Research, Center for Biomedical Imaging & Neuromodulation, New York, NY, United States
Introduction: With aging societies, the incidence of both brain cancer and neurodegenerative diseases are increasing. Despite being distinct, biologic associations have been suggested between glioblastoma and Alzheimer's disease (AD), which share a propensity for the aging brain.
Objectives: We here aimed to establish the co‐occurrence of AD‐type pathology in a large cohort of patients with glioblastoma using histological screening of tumor‐adjacent cortex and volumetric hippocampal volumes as relevant biomarkers.
Methods: The cohort comprised 205 patients with glioblastoma (37% females, aged 27–92 years) with tumor tissues for histological screening. Among them 48 patients had MRI images at diagnosis and follow‐up (280 volumes). We systematically quantified cortical tumor cell infiltration, A‐beta and tau‐AT8 load using custom Matlab scripts and QuPath. Tumor‐contralateral hippocampal volumes were segmented upon T1‐weighted MR images using FMRIB's Automated Segmentation Tool, and compared against existing age‐matched cohorts, for example, UK biobank.
Results: A total of 107 patients (52%) showed A‐beta and/or tau pathology in tumor‐adjacent cortex. AD‐type changes correlated significantly with patient age (p < 0.001) and varied spatially with the most frequent A‐beta deposits in the occipital (50%, n = 10/20) and tau deposits in the temporal cortex (56%, n = 44/79). Median cell density in tumor‐infiltrated cortex was 1895/mm2, where a higher density correlated with loss of neurons (p < 0.001) and decreased AD pathology. Among patients with atrophic hippocampus at time of surgery 10/12 (83%) showed AD pathology.
Conclusion: Our preliminary data suggest frequent co‐occurrence of glioblastoma and AD‐like pathology in the same individual. Within the tumor‐adjacent cortex, increased tumor cell infiltration parallels neuronal and AD‐type pathology loss. The findings encourage further investigation of common pathogenic mechanisms and synergistic effects on cognitive decline.
eP‐NO‐A124
Different expression and clinical implications of cancer‐associated fibroblast (CAF) markers in brain metastases
R. Akanda1,2, E. J. Ahn1, Y. J. Kim3, S. M. A. Salam1, M. G. Noh1, S. S. Kim4, T. Y. Jung3, I. Y. Kim3, C. H. Kim5, K. S. Moon3, K. H. Lee 4,1
1Chonnam National University Hwasun Hospital, Pathology, Hwasun‐gun, South Korea; 2Sylhet Agricultural University, Pharmacology and Toxicology, Sylhet, Bangladesh; 3Chonnam National University Hwasun Hospital, Neurosurgery, Hwasun‐gun, South Korea; 4Chonnam National University Medical School, Pathology, Hwasun‐gun, South Korea; 5Chonnam National University Hwasun Hospital, Surgery, Hwasun‐gun, South Korea
Question: This study assessed the expression and clinical relevance of cancer‐associated fibroblast (CAF)‐related biomarkers in brain metastasis (BM). Moreover, molecular characterization of patient‐derived primary CAFs and normal fibroblasts (NFs) was performed.
Methods: Sixty‐eight patients with BM from various primary cancer types were selected. Immunohistochemistry (IHC) and immunofluorescence (IF) staining were performed to evaluate the expression of various CAF‐related biomarkers. CAFs and NFs were isolated from fresh tissues.
Results: Various CAF‐related biomarkers were expressed in CAFs in BMs of different primary cancers. However, only PDGFR‐β, α‐SMA, and collagen type I were associated with BM size. PDGFR‐β and α‐SMA were associated with BM recurrence after resection. PDGFR‐β was associated with recurrence‐free survival (RFS). Interestingly, high expression of PDGFR‐β and α‐SMA was found in the patients with previous chemotherapy or radiotherapy for primary cancer. In primary cell culture, PDGFR‐β and α‐SMA were expressed at higher levels in patient‐derived CAFs than in NFs or cancer cells. The origins of CAF in BM were presumed to be pericytes of blood vessels, circulating endothelial progenitor cells, or transformed astrocytes of the peritumoral glial stroma.
Conclusions: Our results suggest that high expression of CAF‐related biomarkers, particularly PDGFR‐β and α‐SMA, is associated with poor prognosis and recurrence in patients with BM. With the elucidation of the role and origins of CAF in the tumor microenvironment, CAF can be a new imperative target for BM immunotherapy.

FIGURE 1.
eP‐NO‐A125
p16 immunohistochemistry as a screening tool for the detection of homozygous CDKN2A deletions in glial tumors and meningiomas
V. Zschernack 1, F. Andreiuolo2, E. Doerner1, A. Wiedey3, S. Jünger4, L. Friker1, R. Maruccia1, T. Pietsch1
1University of Bonn Medical Center, Department of Neuropathology, Bonn, Germany; 2Instituto Estadual do Cérebro Paulo Niemeyer and the IDOR Institute, Rio de Janeiro, Brazil; 3University of Bonn Medical Center, Department of Neurology, Bonn, Germany; 4University of Cologne Medical Center, Department of Neurosurgery, Cologne, Germany
Question: The 2021 WHO classification of tumors of the central nervous system emphasizes the significance of molecular parameters for an integrated diagnosis. Homozygous deletion of CDKN2A has been associated with an adverse prognosis in IDH‐mutant gliomas, supratentorial ependymomas, meningiomas, and MPNST. In this study, we examined the value of p16 protein immunohistochemistry as a screening tool for predicting a homozygous CDKN2A deletion.
Methods: Genetic analyses for CDKN2A deletion in 30 pleomorphic xanthoastrocytomas, 32 IDH‐wildtype high‐grade gliomas and 40 supratentorial ependymomas with ZFTA‐RELA gene fusion, 10 IDH‐mutant astrocytomas, and 10 meningiomas were performed either by a molecular inversion probe assay (MIP), a high‐resolution, quantitative technology for the accurate, genome‐wide assessment of chromosomal copy number alterations, or by 850k methylation profile‐deduced copy number analysis or multiplex ligation‐dependent probe amplification analysis.
Results: In pleomorphic xanthoastrocytomas and IDH‐wildtype high‐grade gliomas, p16 immunohistochemistry showed high specificity (100% both), moderate sensitivity (76% and 56%), and a high positive predictive value (PPV; 100% both) for the presence of a homozygous CDKN2A deletion. In supratentorial ependymoma with ZFTA‐RELA gene fusion, immunohistochemistry for p16 protein was highly sensitive and specific (90% and 97%) for a homozygous CDKN2A deletion and exhibited a high PPV and NPV (90% and 97%, respectively). For lower‐grade meningioma, no correlation between the p16 immunohistochemical status and the CDKN2A deletion status was possible.
Conclusions: Therefore, p16 protein expression detected by immunohistochemistry is a useful prescreening tool for detecting a homozygous CDKN2A deletion in glial tumors.


eP‐NO‐A126
Evaluation of 1p deletion by fluorescence in situ hybridization in meningiomas—A simple easy to implement prognostic stratifier
A. Shah 1, J. Saha1, N. Goyal1, M. Ankolkar2, O. Shetty2, A. Sahay1, A. Chatterji3, A. Dasgupta3, T. Gupta3, V. Singh4, P. Shetty4, A. Moiyadi4, S. Epari1
1Tata Memorial Centre, Pathology, Mumbai, India; 2Tata Memorial Centre, Molecular Pathology, Mumbai, India; 3Tata Memorial Centre, Radiation Oncology, Mumbai, India; 4Tata Memorial Centre, Neurosurgical division of Surgical Oncology, Mumbai, India
Introduction: Chromosome 1p deletion has now been shown as one of the independent prognostic markers in meningiomas. Integrated histomolecular algorithms incorporating 1p deletion has shown good stratification, especially in histologically grade 1 and 2 meningiomas.
Objectives: (1) Evaluation of 1p deletion by fluorescence in situ hybridization (FISH) in meningiomas. (2) Determining the frequency of 1p deletion and recurrence rate across meningioma grades.
Materials and Methods: Seventy‐seven meningiomas were evaluated for 1p deletion by FISH using Zytolight SPEC 1p36/1q25 Dual Colour Probe set which formed the study cohort. 1p deletion was considered if >50% nuclei contained 1 signal of 1p probe with ≥2 signals of 1q probe and 1p/1q ratio ≤0.8 ratio.
Results: The 77 patients comprised of 33 males and 44 females with a median age of 52 years. Median follow‐up time was 8.3 months which was available for 65 cases. 22 of 77 (28.57%) meningiomas showed 1p deletion. Four of 33 grade 1 (12.90%), 16 of 41 grade 2 (39.02%) and 2 of 3 grade 3 (66.67%) meningiomas showed 1p deletion. Among the 16 cases with follow‐up data categorized as “1p deleted,” the recurrence rate was 31.25%, and interestingly, all five cases that recurred were classified as grade 2. In the non‐deleted category, 4 grade 1 (9.09%) and 6 grade 2 (13.64%) showed recurrence. Additionally, there was one equivocal case of grade 2 meningioma which showed recurrence.
Conclusion: Grade 2 meningiomas with 1p deletion showed higher recurrence compared to meningiomas without 1p deletion. Incorporation of FISH‐based detection of 1p deletion with appropriate cut‐off criteria into routine clinical practice can be particularly useful for making treatment decisions in patients with Grade 1/2 tumors.
eP‐NO‐A127
Chordoid Glioma—A rare tumor of diagnostic dilemma
A. Wadekar 1, M. C. Sharma1, V. Suri1
1AIIMS—New Delhi, Pathology, New Delhi, India
Background: Chordoid gliomas are extremely uncommon CNS World Health Organisation (WHO) grade 2 glial tumors which are well circumscribed and mostly located in the anterior third ventricle with characteristic morphology, arranged in cords of epitheloid cells. They show defining molecular signatures characterised by PRKCAAp.D463H mutations. They pose a diagnostic dilemma when they occur in odd locations and show varied morphology.
Materials and Methods: During a period of 25 years, we encountered four cases of chordoid gliomas, two of which were published earlier. All the cases were reviewed and immunohistochemistry was done.
Results: Age ranged from 7 to 55 years (7, 55, 39, 30) with equal distribution of male to female ratio. In pediatric patient, tumor was located in juxtraventricular region of occipital horn of lateral ventricle, one was in sellar and suprasellar region, two had classical location in anterior third ventricle. Gross total resection was achieved in all the cases but tumor in the sellar/suprasellar region recurred within a year. Three cases had classical chordoid morphology in a myxoid background with interspersed inflammatory cells, at places forming lymphoid follicles. One case showed bipolar spindle cells in a myxoid background and were immunonegative for GFAP (glial fibrillary acidic protein). Rest all were immunopositive for GFAP, CD34, Pan CK and TTF‐1. Ultrasturctural examination was done in all the cases showed ependymal differentiation.
Conclusion: Chordoid glioma is a rare glioma mostly located in the anterior third ventricle. This entity should be distinguished from other chordoid mimics. Pathologist should be aware of this entity especially when location and morphology is unusual and molecular analysis is not possible in resource constraint countries.
eP‐NO‐A128
The role of neutrophil to lymphocyte ratio (NLR) in predicting survival outcome in glioblastoma
M. Al‐Hussaini 1, A. Amer Abu‐Shanab1, Y. Halaseh1
1King Hussein Cancer Center, Pathology and Laboratory Medicine, Amman, Jordan
Question: Neutrophil to lymphocyte ratio (NLR) is of value in predicting the survival outcome in various solid tumors. We investigated whether NLR can predict the outcome of glioblastoma.
Methods: A retrospective review of 117 GBM at King Hussein Cancer Center (2010–2020). Data collected included age, biological sex, interventions (surgery, chemotherapy, radiotherapy), performance status, IDH1 immunostain, last contact, and vital status. Baseline CBC with differential counts was collected, including WBC count, absolute neutrophil (ANC), and absolute lymphocyte (ALC) count, then NLR was calculated. Kaplan–Meier curves were used for calculating the overall survival (OS) around the mean and median.
Results: The mean and median age was 50 years, with a predominance of males (65%). Gross total resection (GTR) was achieved in 32.5%, chemotherapy was administered to 87.9%, and radiotherapy in 91.4%. 59.0% were alive with a median survival of 20.98 months. Variables significantly associated with better survival include younger age (OS of patients with WBC above the mean (8980/μL), and median (9100/μL) was significantly lower than below the mean (14.07 vs. 34.89 months; p = 0.015), and median (12.90 vs. 38.46 months; p = 0.001)). Also, the OS was significantly lower for patients with ANC above the mean (>6098.7/μL), (14.07 vs. 34.89 months, p = 0.016), and median (5881.3/μL), (14.33 vs. 34.89, p = 0.029). Patients with baseline NLR above the mean (>6.13/μL) were more likely to live shorter (14.07 vs. 26.43 months; p = 0.0349).
Conclusions: Younger patients, and patients with lower WBC count, ANC, and NLR fared better than their comparators. A simple blood test might help delineate patients with better survival, which might affect the counseling of patients and families.

FIGURE 1.

FIGURE 2.
eP‐NO‐A129
Meningioma‐to‐malignant peripheral nerve sheath tumor transdifferentiation by a single genetic event
A. Bakaric1, A. R. Kurzbuch2, V. Soubeyran3, D. Merkler1,4, I. Letovanec5, K. Egervari 1,4
1Geneva University Hospitals, Department of Diagnostics/Clinical Pathology, Geneva, Switzerland; 2Valais Hospital, Service of Neurosurgery, Sion, Switzerland; 3Valais Hospital, Service of Nuclear Medicine, Sion, Switzerland; 4University of Geneva, Department of Pathology and Immunology, Geneva, Switzerland; 5Valais Hospital, Histocytopathology, Sion, Switzerland
Introduction: Meningiomas originate from arachnoid cells and malignant peripheral nerve sheath tumors (MPNST) from peripheral nerves. Rare cases of intracranial MPNSTs not associated with cranial nerves have been described; however, their origin remains undefined.
Objectives: Here we describe a case of meningioma with sarcomatous transformation showing morphological, genetic and epigenetic features consistent with an MPNST.
Patients and Methods: Seventy‐two‐year‐old female presented a fronto‐parietal, extra‐ and intra‐cranial, osteolytic lesion with two components and disseminated bone metastases. We performed histopathological characterization and methylation profiling with copy number variation (CNV) predictions of both components.
Results: We found a dense, necrotic and mitotically active (>20 mitoses/10 HPF) tumor with atypical, epithelioid cells, immunopositive for epithelial membrane antigen (EMA), negative for cytokeratin (CK) 5/6 and smooth muscle actin (SMA), compatible with an anaplastic meningioma. We saw transition to a second component: a spindle cell tumor with mitoses and EMA‐negative, CK 5/6‐ and SMA‐positive tumor cells. Methylation profiling and classification (Brain Classifier v12.5, DKFZ, Heidelberg) of the first component gave a match with the family of meningiomas with highest calibrated scores (0.75) for intermediate meningiomas. The sarcomatous part was a match (0.94) with the class of MPNSTs. Near identical CNVs proved the common clonal origin of the two. In addition, the sarcomatous part showed a focal loss of EED, a gene frequently altered in MPNSTs. Consistently, we found loss of H3K27me3 in the sarcomatous component.
Conclusion: We describe a neoplastic transdifferentiation of meningioma into MPNST most probably due to a single genetic event of EED deletion, leading to H3K27me3 loss and epigenetic reprogramming. Our case raises the hypothesis that intracranial MPNSTs may develop from a meningothelial precursor away from peripheral nerves.
eP‐NO‐A130
Giant cell enriched IDH wildtype glioblastoma differs in metabolic phenotype, tumor microenvironment composition and DNA methylation age acceleration
P. Cakmak1,2, P. Jurmeister3,4, I. Divé2,5,6,7, J. P. Steinbach2,5,7, K. H. Plate1,2,5,6, M. Czabanka8, P. N. Harter3,9, K. J. Weber 1,2,5,6
1University Hospital Frankfurt, Neurological Institute (Edinger Institute), Frankfurt a. M., Germany; 2Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 3German Cancer Consortium (DKTK), Partner Site Munich, German Cancer Research Center (DKFZ), Heidelberg, Germany; 4Ludwig‐Maximilians‐University, Institute of Pathology, Munich, Germany; 5German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Heidelberg, Germany; 6University Cancer Center (UCT), Frankfurt a. M., Germany; 7Goethe University Frankfurt, Dr. Senckenberg Institute of Neurooncology, Frankfurt a. M., Germany; 8University Hospital Frankfurt, Department of Neurosurgery, Frankfurt a. M., Germany; 9Ludwig‐Maximilians‐University, Center for Neuropathology, Munich, Germany
Introduction: Besides their usage for CNS tumor classification, DNA methylation profiles can be exploited for tumor deconvolution to infer the cellular composition of the tumor microenvironment (TME). Furthermore, properties of the energy metabolism in glioma are deducible from epigenetic changes of metabolic genes. By use of epigenetic clocks DNA methylation data was recently evaluated also for its capability to serve as biomarker linked to tumor‐induced age acceleration.
Objectives: We therefore set out to analyse giant cell enriched glioblastoma, IDH wildtype (gcGBM) as this histologic variant is supposed to differ with regard to the TME and rather harbours p53 mutations, which lead to accumulation of DNA double‐strand breaks, potentially fueling epigenetic defects.
Patients and Methods: Three hundred and ten epigenetically classified GBM were analysed including 26 gcGBM. We collected large‐scale DNA methylation data and subjected it to tumor deconvolution and analyses of genome‐wide and focused differential methylation of metabolic and mitotic genes. The cohorts were immunohistochemically characterized for expression of p53, glycolytic and mitochondrial proteins. Methylation‐based age prediction was conducted via elastic net regression.
Results: gcGBM patients were significantly younger than patients from the comparison cohort. While glioblastoma without GC showed a mean DNA methylation age acceleration (MethAgeAcc) of 12 years, GC‐enriched tumors were characterized by a balanced chronological and epigenetic age. gcGBM showed lower proportions of intratumoral neurons and infiltrating CD4+ T cells. Expression scores of the anti‐mitochondrial antibody MTC02 were higher in gcGBM.
Conclusion: Gc might contribute to an altered TME with lower infiltrating T helper cells as well as promote oxidative phosphorylation. The observed differences in MethAgeAcc between glioblastoma with and without gc questions their association with DNA damage and sequel for prediction of patient survival.
eP‐NO‐A131
Application of spatial biology to assess prognostic and predictive biomarkers in the tumor microenvironment
K. H. Plate 1, Y. Reiss1, P. Cakmak1, J. H. Lun1, J. Schupp1, T. Tonn2, M. Burger3, W. Wels4, J. P. Steinbach3
1University Hospital, Goethe University, Edinger Institute, Frankfurt a. M., Germany; 2DRK‐Blutspendedienst Nord‐Ost, Dresden, Germany; 3University Hospital, Goethe University, Senckenberg Institute for Neurooncology, Frankfurt a. M., Germany; 4Georg‐Speyer‐Haus, Institute for Tumor Biology, Frankfurt a. M., Germany
Introduction: The resistance to therapy in glioblastoma is mainly attributed to the tumor microenvironment, characterized by low numbers of CD8 lymphocytes and an abundance of immunosuppressive cells.
Objectives: The CAR2BRAIN phase I first‐in‐human clinical trial was designed to determine feasibility and safety of local injection of HER2‐specific NK‐92/5.28.z CAR‐NK cells in patients with recurrent GBM, and to interrogate the tumor immune landscape by spatial biology for biomarkers predictive of efficacy. In addition, DNA‐derived biomarkers such as tumor mutational burden (TMB) and microsatelite instability (MSI) were tested by whole exome sequencing.
Methods: FFPE‐sections of primary and recurrent glioblastoma from 12 patients were stained using the Opal Polaris 7 color kit based on the tyramide signal amplification immunostaining technique. 7‐plex stainings targeting human CD3, CD8α, von Willebrand Factor, CD163, Iba‐1 and CD47, and/or human CD3, CD8α, CD4, PD‐1, FoxP3 and Ki‐67 were performed on a LabSat™ Research Automated Staining Instrument. Multiplex stainings were acquired on a Vectra Polaris instrument Whole slide multispectral image analysis was performed.
Results: Intratumoral CD8+ T cells in the recurrent but not the primary tumor tissue correlated with PFS and OS. Receiver‐operating characteristic (ROC) analysis indicated 1.60% of total cells in the recurrent tumor samples being CD8+ T cells as a cut‐off value to distinguish two patient groups with different probability of survival, with a median PFS of 4 weeks (5 patients; range, 2–7 weeks) for the group with <1.60% CD8+ T cells (range, 0.15–1.50%) and 26.5 weeks (4 patients; range, 11–37 weeks) for the group with >1.60% CD8+ T cells (range, 1.63%–6.40%) (p = 0.0051, Log‐rank test). Neither TMB nor MSI correlated with PFS or OS.
Conclusion: These findings suggest that tissue based analyses of the intratumoral immune landscape facilitates biomarker identification in immune‐oncology trials in glioblastoma.
eP‐NO‐A132
Molecular and clinical characterization of atypical neurofibromas
C. Kresbach 1,2,3,4, M. Dottermusch1, A. Eckhardt2,3,5, I. Ristow6, P. Paplomatas2,3, L. Altendorf2,3, A. K. Wefers1,4, M. Bockmayr2,3,4, S. Belakhoua7, I. Tran7, L. Pohl2,3, S. Neyazi2,3, H. Bode2,3, S. Farschtschi8, L. Well6, R. Friedrich9, D. Reuss10, M. Snuderl7, C. Hagel1, V. F. Mautner8, U. Schüller1,2,3
1University Hospital Hamburg‐Eppendorf, Department of Neuropathology, Hamburg, Germany; 2University Hospital Hamburg‐Eppendorf, Department of Pediatric Hematology and Oncology, Hamburg, Germany; 3Research Institute Children's Cancer Center Hamburg, Hamburg, Germany; 4University Hospital Hamburg‐Eppendorf, Mildred Scheel Cancer Career Center HaTriCS4, Hamburg, Germany; 5University Hospital Hamburg‐Eppendorf, Lab of Radiobiology & Experimental Radiation Oncology, Hubertus Wald Tumorzentrum, Hamburg, Germany; 6University Hospital Hamburg‐Eppendorf, Department of Diagnostic and Interventional Radiology and Nuclear Medicine, Hamburg, Germany; 7NYU Langone Health, Department of Pathology, New York, NY, United States; 8University Hospital Hamburg‐Eppendorf, Department of Neurology, Hamburg, Germany; 9University Hospital Hamburg‐Eppendorf, Department of Oral and Maxillofacial Surgery, Hamburg, Germany; 10University of Heidelberg, Department of Neuropathology, Heidelberg, Germany
Introduction: Neurofibromatosis type 1 (NF1) is a tumor predisposition syndrome that causes a broad spectrum of benign and malignant tumors. Most frequently, patients develop a multitude of benign neurofibromas (NF). Evidence supports that NF can progress to risk lesions called atypical neurofibromas (ANF), that can further undergo malignant transformation to highly aggressive malignant peripheral nerve sheath tumors (MPNST). MPNST have a dismal prognosis and are considered incurable upon occurrence of metastasis. However, while identification of ANF is of great importance for NF1 patients, histomorphological diagnosis remains challenging to date.
Objectives: We aimed to identify molecular and microenvironmental features that distinguish ANF from other peripheral nerve sheath tumors (PNST).
Materials and Methods: We performed global DNA methylation analysis in a series of 40 histologically defined ANF and compared their epigenetic profile to other PNST including MPNST, low grade MPNST, NF, and schwannomas. Molecular data were then integrated with clinical features of ANF.
Results: We found that the majority of histologically defined ANF formed a distinct methylation cluster in proximity to the benign PNST entities. ANF from this cluster had frequent loss of CDKN2A/B and significantly more lymphocyte infiltration than MPNST, schwannomas, and NF. ANF often received misleading high scores for the brain tumor methylation class schwannoma and remained unclassifiable with the sarcoma classifier. Currently, we are conducting investigations of tumor heterogeneity within PNST that show areas of both ANF and MPNST. By analysing epigenetic, mutational, and transcriptional features of the different tumor morphologies, we hope to better understand the mechanisms of malignant progression from ANF to MPNST.
Conclusion: Our data suggest that ANF reveal varying morphology, but show distinct epigenetic similarities and cluster in proximity to benign PNST entities.
eP‐NO‐A133
Rhythmic expression of BMAL in normal human Schwann cells and disturbance of clock gene expression in malignant NF1 associated tumor cells
S. Leisz1, A. Pellegrino2, S. Fritzsche1, M. Wiegers1, T. Simon3, C. Rothgaenger‐Strube4, O. Storozhuk3, C. Scheller1, C. Strauss1, E. Ehrentreich‐Förster2, F. Dehghani4, E. Maronde5, A. Harder 6
1Martin Luther University Halle‐Wittenberg, Department of Neurosurgery, Medical Faculty, Halle‐Wittenberg, Germany; 2Fraunhofer Institute for Cell Therapy and Immunology, Branch Bioanalytics and Bioprocesses IZI‐BB, Potsdam, Germany; 3Martin Luther University Halle‐Wittenberg, CURE‐NF Research Group, Medical Faculty, Halle‐Wittenberg, Germany; 4Martin Luther University Halle‐Wittenberg, Institute of Anatomy and Cell Biology, Medical Faculty, Halle‐Wittenberg, Germany; 5Goethe University Frankfurt, Institute for Anatomy II, Faculty of Medicine, Frankfurt a. M., Germany; 6University Medical Center Johannes Gutenberg University (UMC) Mainz, Institue of Neuropathology, Mainz, Germany
Introduction: Neurofibromatosis type 1 (NF1) is an autosomal dominant tumor syndrome caused by NF1 gene variants. Sleep disturbances are among other symptoms being recapitulated in animal models. Studies of the circadian clock unraveled a role of NF1 in Drosophila and mammalian astrocytes. Core clock genes maintain 24 h rhythms and regulate fundamental body functions. Impaired rhythms can drive tumorigenesis. In NF1 neurofibromas arise from peripheral Schwann cells (SCs). For its malignant change, NF1−/− SCs underlie further genetic alterations. Studies on rhythmic gene expression in NF1 associated tumors do not exist so far. It is unknown if normal (NF1+/+) SCs or NF1‐associated SCs (NF1+/−) show a rhythmic gene expression.
Objectives: NF1 exerts a role to regulate circadian rhythms in astrocytes. We hypothesize that (1) also normal SCs maintain a circadian rhythm, and show a disturbance in NF1. We also hypothesize that (2) NF1 derived tumors fail to show a rhythmic clock gene expression.
Materials and Methods: NF1 associated malignant SC (MPNST) were investigated for rhythmicity. Expression was analysed by a custom panel (Illumina) and evaluated by Cosinor analysis.
Results: (1) Normal human SCs showed a rhythmic expression of the core clock gene BMAL1. Expression was also inducible for BMAL1, CRY2, CLOCK, TIMELESS, CSNK1E, CCND1, CREM, and MYC and was spontaneous for BMAL, CRY1, CRY2, CLOCK, TIMELESS, CSNK1E, CCND1, CREM, DBP, NR1D1 and MYC. (2) Expression of clock genes was disturbed in MPNST. BMAL1 expression was not rhythmic.
Conclusions: Rhythmic BMAL1 expression is crucial to maintain circadian rhythms in central cells. For the first time we show rhythmic expression of BMAL1 in peripheral glia (SCs). As BMAL1 knockdown leads to circadian rhythm related disorders, we speculate that disturbances can also lead to tumor development of SC. NF1 associated tumors showed an altered expression of important clock and associated genes which might be important for tumor growth in NF1.
eP‐NO‐A134
Quantifying heterogeneity in WSI using ecological diversity indices is a prognostic marker in glioblastoma
G. Prokop 1, J. Schlegel1, B. Märkl2, F. Liesche‐Starnecker1,2
1Institute of Pathology, Technical University Munich, Department of Neuropathology, Munich, Germany; 2Institute of Pathology, University of Augsburg, Augsburg, Germany
Introduction: Intratumor heterogeneity is linked to therapy resistance, tumor recurrence and poor overall survival, especially in Glioblastoma (GBM). However, no clinically applicable method for quantification is currently available.
Objectives: This study examines whether the Simpson index, an index derived from ecology to measure biological diversity, can quantify tumor heterogeneity on the basis of pixel intensities in whole slide images (WSI) of hematoxylin and eosin (HE) stained GBM slides. Additionally, it is evaluated to what extent this heterogeneity assessment can predict tumor prognosis more accurately.
Materials and Methods: We included 359 WSI of 132 patients with therapy‐naïve GBMs, IDH‐wt. Seventy‐seven patients were derived from two local study cohorts and served as an exploration data set. Fifty‐five patients from the TCGA database served as validation dataset. Pictorial heterogeneity was assessed as the diversity of pixel intensities within the WSI. Depending on the number and size of the WSI per tumor, five or more representative sample images of the tumor core were analyzed using custom Python scripts. Quantification of intratumor heterogeneity was achieved by determining the standard deviation of the measured Simpson‐Index across all images of a tumor.
Results: The GBM WSI displayed great diversity in their pixel intensities. By using the median as cut‐off, a survival benefit for the heterogenous group could be observed in the exploration data set (10.3 vs. 16.4 months, p = 0.0048). The results are currently validated by analyzing the TCGA dataset.
Conclusion: Analysis of pixel diversity revealed extensive intratumor heterogeneity with a strong impact on patient survival. It is a robust method across different datasets.
eP‐NO‐A135
Comprehensive molecular and clinical characterization of glioblatomas with long‐term survival
A. M. Wurzer 1, C. Delbridge2, S. Baur2, S. Dintner3, T. Schaller3, B. Märkl3, F. Schmidt‐Graf1, F. Liesche‐Starnecker3
1Department of Neurology, Munich, Germany; 2Institute of Neuropathology, Munich, Germany; 3Institute of Neuropathology, Augsburg, Germany
Introduction: Despite the overall poor prognosis of glioblastomas (GBM) with a median survival of 15 months, 10% of the patients are long‐term survivors (LTS, ≥2 years). But there is no certain explanation of clinical and molecular differences between LTS and short‐term survivors (STS, <2 years), yet.
Objectives: The purpose of this study is to compare LTS and STS regarding their clinical and molecular characteristics. 850k Methylation Array (850k) and Next Generation Sequencing (NGS) are performed in a group of extra‐LTS (≥4 years) to characterize LTS tumors more precisely and compare them to STS tumors.
Patients and Methods: Adult patients with histologically confirmed primary diagnosis of GBM (IDH‐wildtype, CNS WHO grade 4) with recorded date of death were included in this study. Depending on their survival, patients were divided into STS and LTS. For further analyses, a subgroup of extra‐LTS (≥4 years) was formed. For 16 cases, consisting of 8 extra‐LTS and 8 STS cases, 850k and NGS were performed.
Results: As expected, LTS (n = 66) were more likely to be younger (median age 59 vs. 70 years, p < 0.001) and had less multifocal tumors at first diagnosis (13.6% vs. 32,6%, p = 0.006) compared to STS (n = 92). The tumors of LTS patients were smaller in axial diameter (median axial diameter 3.4 vs. 4.2 cm, p = 0.003) and more likely to show MGMT promotor methylation (60% vs. 42,2%, p = 0.044). Preliminary data show no significant differences of the methylation profiles between extra‐LTS and STS, but some analyses are still pending.
Conclusions: In conclusion, LTS are statistically significant younger, have smaller and more unifocal tumors that rather show MGMT promotor methylation. In combination with the results of 850k and NGS, these data may assist in predicting LTS at diagnosis and in understanding the clinical journey of GBM patients better.
eP‐NO‐A137
Scaffold‐based (Matrigel™) 3D culture technique of glioblastoma recovers a patient‐like immunosuppressive phenotype
F. K. Braun1, T. Rothhammer‐Hampl1, J. Lorenz1, S. Pohl1, A. N. Menevse2, A. Vollmann‐Zwerenz3, E. Bumes3, M. Büttner4, S. Zoubaa1, M. Proescholdt5, N. O. Schmidt5, P. Hau3, P. Beckhove2,6, B. Winner7,8, M. J. Riemenschneider 1
1Regensburg University Hospital, Department of Neuropathology, Regensburg, Germany; 2Leibniz Institute for Immunotherapy, Divison of Interventional Immunology, Regensburg, Germany; 3Regensburg University Hospital, Department of Neurology and Wilhelm Sander‐NeuroOncology Unit, Regensburg, Germany; 4Helmholtz Center Munich, Insitute of Computational Biology, Munich, Germany; 5Regensburg University Hospital, Department of Neurosurgery, Regensburg, Germany; 6Regensburg University Hospital, Department of Internal Medicine III, Regensburg, Germany; 7Friedrich Alexander University (FAU) Erlangen‐Nürnberg, Department of Stem Cell Biology, Erlangen, Germany; 8Friedrich Alexander University (FAU) Erlangen‐Nürnberg, IZKF Junior Research Group 3 and BMBF Researc Group Neuroscience, Interdisciplinary Center for Clinical Research, Erlangen, Germany
3D (organoid) models in cancer research are considered the novel gold standard for in vitro experiments. Nevertheless, a variety of different protocols exits and the models are often used uncritically in lack of further validation. In this study, we aimed to characterize a scaffold‐based (Matrigel™) 3D glioma cell culture approach. We compared the 3D technique to conventional 2D culturing in its efficacy of generating models and in respect to its exact modeling properties. Models were generated from 62 patients with CNS tumors, most of them with glioblastomas, IDH‐wildtype (GBM, n = 43). Pairs of 11 GBM models (2D and 3D) together with corresponding patient material were further characterized using bulk and single‐cell RNA sequencing as well as 850k methylation analysis. Functional aspects of 3D tumor organoids were analyzed using a coculture system (Incucyte® SX5 live cell imager) with tumor infiltrating lymphocytes. Compared to conventional 2D culture the Matrigel™‐based 3D protocol was not superior in terms of the successful generation of in vitro models. However, NGS‐based bulk and single‐cell sequencing of matched pairs of 2D and 3D models showed an altered transcription of key immune regulatory genes in the 3D models, indicating the reoccurrence of an immunosuppressive phenotype. Changes included the presentation of different HLA surface molecules as well as cellular stressors. In the coculturing approach, lymphocyte mediated cell killing appeared less effective in clearing 3D models than their 2D counterparts. IFN‐γ release as well as live cell staining and proliferation analysis pointed towards an elevated resistance of 3D models. In conclusion, we found that the scaffold‐based (Matrigel™) 3D culture technique depicts clinically highly important aspects of tumor‐immune cell interactions, with the potential to explore immunotherapeutic approaches in an easily accessible in vitro system.
eP‐NO‐A138
The role of p16 immunohistochemistry as a prognostic biomarker in meningiomas
J. Schittenhelm 1, C. Fodi2,3, E. M. Di Francesco2,3, E. Hoffmann3,4, J. Honegger2,3, G. Tabatabai3,5, M. Tatagiba2,3, F. Behling2,3
1University Clinic Tuebingen, Neuropathology Tübingen, Tuebingen, Germany; 2University Hospital Tübingen, Department of Neurosurgery, Tuebingen, Germany; 3Comprehensive Cancer Center Tübingen‐Stuttgart, Center for Neuro‐Oncology, Tuebingen, Germany; 4University Hospital Tübingen, Department of Radiation Oncology, Tuebingen, Germany; 5University Hospital Tübingen, Department of Neurology and Interdisciplinary Neuro‐Oncology, Tuebingen, Germany
Introduction: Despite best clinical management many patients suffering from meningiomas experience tumor recurrence. Homozygous loss of CDKN2A and increased CDKN2A mRNA expression identify a subset of biologically aggressive meningiomas. Therefore, p16 immunohistochemistry is frequently requested in tumor boards as a potential surrogate marker.
Objectives: In many tumors, loss of p16 is associated with tumor progression. Evaluation of p16 staining in a large cohort to identify recurring meningiomas is of clinical and therapeutic interest.
Patients and Methods: In this retrospective single‐institutional study the immunohistochemical staining for p16 was analyzed in 647 CNS WHO grade 1, 139 grade 2 and 5 grade 3 paraffin‐embedded meningioma tissue microarray samples. The distribution and association with tumor grading, clinical data and progression‐free survival via radiographic tumor recurrence were statistically assessed.
Results: Of 791 meningioma samples of 69 tumors were immunopositive for p16 (13%). Significantly higher rates of p16 frequency was observed in meningiomas with higher WHO CNS‐grade (p < 0.0001), in recurrent tumors (p < 0.0001), brain invasion (p = 0.0055), higher MIB1 proliferation (p < 0.0001) and male patients (p = 0.0175) but not with resection status and patient age. Univariate analysis revealed a higher rate of tumor recurrence in meningiomas with p16 immunopositivity (p = 0.0071) and an unfavorable progression‐free survival in the Kaplan–Meier analysis (p = 0.0054). However, p16 remained non‐significant in the multivariate analysis, where CNS WHO grade, tumor recurrence, resection status and adjuvant RT were significant independent factors.
Conclusion: The prognostic impact of p16 is mostly attributed to the confounding clinical factors WHO CNS tumor grade, recurrent tumor status and adjuvant RT. Immunohistochemistry of p16 in meningioma samples without further molecular data does not allow for tumor risk stratification.
eP‐NO‐A139
Mapping the tumor microenvironment in primary and recurrent glioblastoma by multiplex immunofluorescence, methylation and AI‐based approaches
P. Cakmak 1,2, M. Köhler1,2, J. H. Lun1,2, J. Macas1,2, T. Starzetz1,2, Y. Reiss1,2,3, K. H. Plate1,2,3,4, K. J. Weber1,2,3,4
1University Hospital Frankfurt, Neurological Institute (Edinger Institute), Frankfurt a. M., Germany; 2Frankfurt Cancer Institute (FCI), Frankfurt a. M., Germany; 3German Cancer Consortium (DKTK), Partner Site Frankfurt, German Cancer Research Center (DKFZ), Heidelberg, Germany; 4University Cancer Center (UCT), Frankfurt a. M., Germany
Introduction: IDH‐wildtype glioblastoma (GBM), an aggressive brain tumor with a high recurrence rate, is known to have a complex tumor microenvironment (TME) that can impact on the effectiveness of immune‐based therapies. Furthermore, a remodelling of the TME, rather than the diversification of the genetic landscape, has been shown to complicate the management of progressive disease. Thus, the composition of immunosuppressive or ‐stimulatory cell types within the TME are critical factors in glioma biology.
Objectives: To further understand glioma tumour progression and evolution, we identified and quantified the lymphocyte and monocyte/microglia subtypes within the TME of matched epigenetically classified primary and recurrent GBM samples using various methods.
Patients and Methods: The study included 36 matched samples. The methods used to for analysis of the TME comprised of (i) a conventional estimation of relative cell counts in immunohistochemical stainings (cIHC), (ii) an AI‐based cell segmentation pipeline (AI‐pipe), (iii) multiplex immunofluorescence stainings (mIF), and (iv) a reference‐based cellular deconvolution from DNA methylomes (MethDecon).
Results: Overall, an increase of CD8+ T cells was observed in recurrent GBM with our approaches except for MethDecon. The estimated cell populations by cIHC were similar to those identified with mIF for CD3+ T cells, CD20+ B cells and subsets of macrophages, as well as with estimates from AI‐pipe for CD4+ subsets, CD20+ B cells and Iba1+ cells. The number of CD3+ T cells and CD163+ macrophages scored significantly higher with AI‐pipe, whereas MethDecon computed significantly higher proportions of CD4+ subsets and CD20+ B cells.
Conclusion: This study provides insights into the accuracy and reproducibility of different methodologies for TME analysis, which could aid in the development of better diagnostic and treatment strategies in GBM. It highlights and critically elucidates the potential of in silico and multiplex assays.
NEURODEGENERATION
S04‐ND‐A140
LATE‐NC exacerbates tau pathology and seeding potential in Alzheimer's disease
S. Tomé 1, G. Tsaka1,2, A. Ronisz1, S. Ospitalieri1, K. Gawor1, M. Otto3, C. A. F. von Arnim3,4, P. Van Damme5, L. Van Den Bosch5, R. Vandenberghe5,6, J. Schymkowitz2, F. Rousseau2, D. R. Thal1,7
1KU Leuven, Imaging and Pathology, Leuven, Belgium; 2KU Leuven, Department of Cellular and Molecular Medicine, Leuven, Belgium; 3Ulm University, Department of Neurology, Ulm, Germany; 4University Medical Center Gottingen, Goettingen, Germany; 5KU Leuven, Department of Neuroscience, Leuven, Belgium; 6UZ Leuven, Department of Neurology, Leuven, Belgium; 7UZ Leuven, Department of Pathology, Leuven, Belgium
Introduction: TDP‐43 is known to co‐accumulate in the brains of most Alzheimer's disease (AD) cases, and it has been recently defined as limbic‐predominant age‐related TDP‐43 encephalopathy (LATE‐NC). LATE‐NC is thought to worsen cognitive decline and neurodegeneration, but it is not yet fully understood how TDP‐43 aggravates AD pathogenesis.
Objectives: We aimed at investigating the impact of TDP‐43 on AD pathogenesis, specifically tau pathology.
Materials and Methods: We performed a histological evaluation of 89 human cases including controls, symptomatic AD cases with (AD/LATE‐NC) and without (pure AD) LATE‐NC using paraffin‐embedded post‐mortem tissue, in which we assessed p‐tau load. We also measured brain levels of p‐tau181 through ELISA using fresh frozen tissue. Moreover, we tested the seeding potential of AD/LATE‐NC and pure AD seeds in vivo, using a TDP‐43A315T transgenic mouse model as well as in vitro, using a tau biosensor cell line.
Results: We observed that AD/LATE‐NC cases presented increased hippocampal (CA1) and cortical tau pathology compared to pure AD (CA1, p = 0.0034, frontal cortex, p = 0.0072) and controls (p < 0.0001). Moreover, the AD/LATE‐NC group showed increased levels of p‐tau181 in frontal and entorhinal cortex compared to pure AD. TDP‐43A315T mice injected with AD/LATE‐NC seeds exhibited significantly increased p‐tau seeding compared to AD (p = 0.0163) and control‐injected animals (p = 0.0007). In line with these findings, AD/LATE‐NC seeds also triggered increased p‐tau cell seeding in tau biosensor cells compared to AD seeds (p = 0.0048).
Conclusion: These results highlight the synergy between TDP‐43 and tau proteins in the context of AD pathogenesis. Specifically, our data suggest that the presence of comorbid LATE‐NC in AD aggravates tau pathology, increasing its aggregation and seeding. We highlight the importance of considering comorbid co‐pathologies in the context of clinical diagnosis and patient stratification.
S04‐ND‐A141
Propagation of pathologic alpha‐synuclein from kidney to brain
L. Chen 1, X. Yuan2, S. Nie2, Z. Zhang2
1University of Minnesota Medical School, Laboratory Medicine and Pathology, Minneapolis, MN, United States; 2Wuhan University, Wuhan, China
The aggregation and prion‐like spreading of alpha‐synuclein (alpha‐Syn) are pivotal events in the pathogenesis ofLewy body disease (LBD). Converging evidence suggests that alpha‐Syn aggregation can originate in peripheral organs and progress to the brain. The incidence of PD is increased in patients with chronic renal failure. However, the molecular mechanisms linking renal failure and PD remain unknown. Here we show that α‐Syn deposits in the kidney of LBD patients. Strikingly, pathologic alpha‐Syn was found in the kidney, brainstem, and amygdala of end‐stage renal disease patients without clinical documentation of LBD. We found that kidney physiologically removes alpha‐Syn from the blood. Renal failure interferes with the clearance of circulating α‐Syn in mouse models of α‐synucleinopathies, resulting in the deposition of pathologic alpha‐Syn in the kidney and subsequent spreading into the brain. Intra‐renal injection of alpha‐Syn fibrils induces the propagation of α‐Syn pathology from the kidney to the brain, which was blocked by renal denervation. Furthermore, deletion of alpha‐Syn in the blood cells by transplantation of bone marrow from the Snca knockout mice alleviates alpha‐Syn pathology in α‐Syn A53T transgenic mice. Our findings provide the first evidence that the kidney may act as a peripheral organ of initiation site for pathogenic alpha‐Syn to spread. Thus, compromised renal function may represent a novel mechanism for the onset of alpha‐Syn pathology in LBD.
S04‐ND‐A142
The role of karyopherin abnormalities in the onset and progression of synucleinopathies
D. Sharipov 1, E. Bereczki2, R. Killick3, T. Hortobágyi3, C. Troakes1, D. Aarsland3, F. Hirth1
1King's College Hospital NHS Foundation Trust, Basic & Clinical Neuroscience, London, United Kingdom; 2Karolinska Institutet, Neurogeriatrics, Stockholm, Sweden; 3King's College Hospital NHS Foundation Trust, Old Age Psychiatry, London, United Kingdom
Parkinson's disease (PD), dementia with Lewy bodies (DLB), and Parkinson's disease dementia (PDD) are synucleinopathies characterised by the aggregation of alpha‐synuclein (aSyn). aSyn is a disordered protein prone to accumulation via phase separation (PS). Previous studies showed that PS is associated with karyopherins (KPN), mediating nucleocytoplasmic cargo transport and acting as disaggregases against misfolding proteins. Furthermore, KPN abnormalities have been implicated in synucleinopathy, but their role in disease formation remains enigmatic. Using a multi‐disciplinary approach, we characterised levels and localisation of KPN and aSyn in the prefrontal cortex (BA9) of human post‐mortem brain tissue of controls, Alzheimer's disease (AD), PD, DLB and PDD. We also used human SH‐SY5Y cells and Drosophila to accumulate either wildtype or mutant (A30P) aSyn and established its effect on KPNs. Our analyses identified altered KPN expression levels in BA9 that were not detected in AD or controls. We found aSyn accumulated and aggregatedin the cytoplasm and nucleus, with an altered nucleocytoplasmic ratio in BA9 of the investigated cases versus controls. Moreover, KPN was depleted from the cytoplasm and accumulated in the nucleus in PD, PDD and DLB, with abnormal nuclear co‐localisation with aSyn. New Drosophila models of synucleinopathy demonstrated that accumulating aSyn caused alterations in levels and localisation of KPN and progressive motor impairment that were exacerbated by aSyn‐A30P. Human cell experiments revealed that accumulating aSyn‐A30P formed spontaneous intracellular aggregates that sequestered and mislocalised KPN, a pathogenic process accelerated in the presence of prefibrillar aSyn. Overall, our findings demonstrate the pathological accumulation of nuclear aSyn and KPN alterations in PD, PDD and DLB, suggesting a vicious cycle of protein alterations that propagate the pathological aggregation of aSyn in neurodegenerative synucleinopathies.
S10‐ND‐A143
The CurePSP brain bank at Mayo Clinic Florida and its contributions to research on neurodegenerative tauopathies
D. Dickson 1
1Mayo Clinic, Neuroscience, Jacksonville, FL, United States
Introduction: The CurePSP brain bank has 1780 cases of PSP and 364 cases of CBD, 49 cases of globular glial tauopathy (GGT) and 54 cases of frontotemporal lobar degeneration (FTLD‐tau) with mutations in the tau gene (MAPT).
Objectives: Describe the contributions of the CurePSP brain bank to the neuropathology and genetics of 4R tauopathies.
Materials and Methods: Brain bank donations are from all 50 States. One half is fixed in formalin and one half is frozen and shipped by commercial couriers. Cases receive diagnostic evaluation before sharing with researchers. A standardized neuropathologic assessment uses thioflavin S fluorescent microscopy and tau immunohistochemistry. Quantitative data on tau and Alzheimer type pathologies are recorded in a relational database and linked to genetic information and sample sharing.
Results: Frozen tissue samples from over 1500 cases has been shared with research investigators. Over 120 peer‐reviewed publications on PSP, 73 on CBD, 6 on GGT and 13 on FTDP‐17 have used resources of the brain bank. International consensus criteria for the diagnosis of PSP were formulated in 2022 (PMCID: PMC9468104). Notable studies from the brain bank are on genetics of PSP, including genome wide association studies, whole genome and whole exome sequencing. In addition to MAPT, other genetic loci have been implicated in PSP, including loci near EIF2AK3 and MOBP and STX6. Variants in the MAPT gene (H1 haplotype) are a risk for sporadic PSP, and mutations in MAPT cause autosomal dominant PSP. Given the rarity of the other 4R tauopathies (CBD and GGT), much less is known about their genetics, but MAPT variants are also a risk factor for CBD.
Conclusion: The CurePSP brain bank has been instrumental in refining neuropathologic criteria for PSP and documenting heterogeneity of 4R tauopathies. It is valuable resource for genetic studies on 4R tauopathies.

FIGURE 1.

FIGURE 2.
S10‐ND‐A144
Structures of α‐synuclein filaments from human brains
Y. Yang 1, Y. Shi1, M. Schweighauser1, A. Kotecha2, A. Murzin1, H. Garringer3, P. Cullinane4, Y. Saito5, T. Foroud3, T. Warner4, K. Hasegawa6, R. Vidal3, S. Murayama7, T. Revesz4, B. Ghetti3, M. Hasegawa8, T. Lashley4, S. Scheres1, M. Goedert1
1Medical Research Council Laboratory of Molecular Biology, Cambridge, United Kingdom; 2Thermo Fisher Scientific, Eindhoven, Netherlands; 3Indiana University School of Medicine, Department of Pathology and Laboratory Medicine, Indianapolis, IN, United States; 4University College Queen Square Institute of Neurology, Department of Neurodegenerative Disease and Queen Square Brain Bank for Neurological Disorders, London, United Kingdom; 5Department of Neuropathology, Metropolitan Institute of Gerontology, Tokyo, Japan; 6Division of Neurology, Sagamihara National Hospital, Sagamihara, Japan; 7Molecular Research Centre for Children's Mental Development, United School of Child Development, University of Osaka, Osaka, Japan; 8Department of Brain and Neurosciences, Metropolitan Institute of Medical Science, Tokyo, Japan
Parkinson's disease (PD) is the most common movement disorder, with resting tremor, rigidity, bradykinesia and postural instability being major symptoms. Neuropathologically, it is characterised by the presence of abundant filamentous inclusions of α‐synuclein in the form of Lewy bodies and Lewy neurites in some brain cells, including dopaminergic nerve cells of the substantia nigra. PD is increasingly recognised as a multisystem disorder, with cognitive decline being one of its most common non‐motor symptoms. Many patients with PD develop dementia more than 10 years after diagnosis. PD dementia (PDD) is clinically and neuropathologically similar to dementia with Lewy bodies (DLB), which is diagnosed when cognitive impairment either precedes parkinsonian motor signs or begins within one year from their onset. In PDD, cognitive impairment develops in the setting of well‐established PD. Besides PD and DLB, multiple system atrophy (MSA) is the other major synucleinopathy. It is characterised by the presence of abundant filamentous α‐synuclein inclusions in brain cells, especially oligodendrocytes (Papp‐Lantos bodies). We previously reported the electron cryo‐microscopy (cryo‐EM) structures of two types of α‐synuclein filaments extracted from the brains of individuals with MSA. Each filament type is made of two different protofilaments. Here we report that the cryo‐EM structures of α‐synuclein filaments from the brains of individuals with PD, PDD and DLB are made of a single protofilament (Lewy fold) that is markedly different from the protofilaments of MSA. These findings establish the existence of distinct molecular conformers of assembled α‐synuclein in neurodegenerative disease.
S10‐ND‐A145
Distribution of Lewy‐related pathology in the brain, spinal cord, and periphery in the population‐based Vantaa 85+ study—Evidence for two distinct LRP types
L. Myllykangas 1, A. Raunio1, V. Kivistö1, M. Kero1, J. Tuimala1, S. Savola1, M. Oinas1, E. Kok1, K. Colangelo1, A. Paetau1, T. Polvikoski1, P. J. Tienari1, H. Puttonen1
1University of Helsinki, Department of Pathology, Helsinki, Finland
Introduction: Evidence has supported the existence of two anatomically distinct Lewy‐related pathology (LRP) types. Investigation of spinal cord and peripheral LRP can elucidate mechanisms for Lewy body disorders and the origins of synuclein accumulation. Very few unselected studies have focused on LRP in these regions.
Objectives: To analyse LRP in spinal cord, dorsal root ganglion, and adrenal gland in the population‐based Vantaa 85+ study, including every ≥85 year old citizen living in the city of Vantaa in 1991 (n = 601).
Materials and Methods: Samples from spinal cord (C6‐7, TH3‐4, L3‐4, S1‐2) were available from 303, lumbar dorsal root ganglion from 219, and adrenal gland from 164 subjects. Semiquantitative scores of LRP were determined from immunohistochemically stained sections (5G4). LRP in the ventral and dorsal horns, thoracic intermediolateral column, spinal ganglion and adrenal gland were compared with brain LRP, previously determined according to DLB Consortium criteria and by caudo‐rostral versus amygdala‐based LRP classification.
Results: Spinal LRP was found in 28% of the total population and in 61% of those who had LRP in the brain. Spinal cord LRP was found only in those subjects with LRP in the brain, and the quantity of spinal cord LRP was associated with the severity of brain LRP (p < 0.001). K‐means analysis identified two cluster types of spinal and brain LRP corresponding to caudo‐rostral and amygdala‐based LRP types. The caudo‐rostral LRP type was associated with more frequent and severe pathology in spinal cord, dorsal root ganglion and adrenal gland than the amygdala‐based LRP type. Thoracic intermediolateral column and sacral dorsal horn were the most frequently affected spinal cord regions in both LRP types.
Conclusion: This population‐based study provides support for the concept of at least two distinct LRP types.
References: [1] Raunio et al. Acta Neuropathol Commun. 2022;10(1):178. [2] Raunio et al. Acta Neuropathol. 2019;138(5):771–82.
S19‐ND‐A146
Cryo‐EM—Neuropathology's gateway toward an understanding of the atomic structures of amyloids in neurodegenerative diseases
B. Ghetti 1, W. Jiang2, R. Vidal1
1Indiana University, Pathology and Laboratory Medicine, Indianapolis, IN, United States; 2Purdue University, Biological Sciences, West Lafayette, IN, United States
Introduction: Neuropathology has revealed the morphology of intracellular and extracellular amyloids filaments and linked the amyloid filaments to specific proteins. Electron cryogenic microscopy (cryo‐EM) has made possible to determine the atomic structure of amyloids associated with neurodegenerative dementias.
Objectives: We focused on the amyloids of two genetically determined prion protein (PrP) amyloidoses, Gerstmann–Sträussler–Scheinker (GSS) disease and prion protein cerebral amyloid angiopathy (PrP‐CAA), and the MAPT tauopathy, multiple systems tauopathy with presenile dementia (MSTD) to determine the structure of PrP and tau filaments.
Materials and Methods: We used neurohistology, immunohistochemistry, electron microscopy, biochemistry, and molecular genetics to study post‐mortem brain tissue from GSS, PrP‐CAA, and MSTD patients. Amyloid filaments were analyzed by Cryo‐EM.
Results: In PrP‐CAA (Q160X), tau filaments are made of both paired helical filaments (PHFs) and straight filaments (SFs), while in GSS (F198S), only PHFs are found. In MSTD (intron 10 +3), tau filaments in gray and white matter have the same fold as in argyrophilic grain disease (AGD) with a four‐layered ordered structure accommodating amino acids 279–381 of tau, packing two protofilaments with C2 symmetry. In GSS (F198S), APrP filaments are composed of dimeric, trimeric and tetrameric left‐handed protofilaments with their protomers sharing a common protein fold. Each protomer comprises nine short β‐strands and span from glycine 80 to phenylalanine 141, adopting a previously unseen spiral fold.
Conclusions: Cryo‐EM analysis reveals that the atomic models of the Tau filaments obtained from PrP‐CAA (Q160X) and GSS (F198S) are identical to those of the Tau filaments from AD. In MSTD, tau filaments from gray and white matter have identical folds. Work in progress will show whether PrP filaments in GSS differ from those in PrP‐CAA.
S19‐ND‐A147
Neurodegenerative proteinopathy‐specific dysregulation of iron homeostasis in the human brain
S. Lee 1, I. Martinez‐Valbuena1, G. G. Kovacs1,2
1University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada; 2University Health Network, Toronto, Canada
Question: Progressive supranuclear palsy (PSP) and multiple system atrophy (MSA) are neurodegenerative diseases involving distinct protein pathology but are commonly characterized by pronounced iron deposition in early affected brain regions. Association of neurotoxic iron burden with regions of protein pathology is greatly evidenced, but function of iron in the pathogenesis of PSP and MSA remains unknown. We hypothesized that differences in cellular iron homeostasis could correlate with protein cytopathology and disease progression.
Methods: We performed the first cellular characterization of iron deposition in early affected regions of human post‐mortem PSP and MSA brains using a combination method of iron staining and immunohistochemistry developed in‐house. Iron burden was evaluated in four different tau and synuclein‐affected and unaffected cell types. To examine underlying mechanisms, we evaluated mRNA expression changes of relevant homeostatic genes in the same brain regions.
Results: In PSP brains, we found astrocytes to selectively accumulate iron species in all examined regions, highly associated with the cellular deposition of tau pathology. In contrast, iron deposition was dominantly observed in microglia and oligodendrocytes in MSA brains and was scarcely associated with synuclein cytopathology. In both diseases, neuronal population showed lowest iron burden. We found key iron‐related genes in PSP and oxygen homeostatic genes in MSA brains to be differentially expressed compared to that of age‐matched controls.
Conclusions: Our study reveals distinct cellular vulnerability patterns of iron deposition in MSA and PSP, especially in relation to protein cytopathologies. Despite common observations of elevated iron levels in neurodegenerative brains, our findings suggest proteinopathy‐specific mechanisms of iron dyshomeostasis in disease pathways. Our findings inform efforts in iron chelation therapies at the disease and cellular‐specific levels.
S19‐ND‐A148
Altered cortical expression of long non‐coding RNAs associates with specific Alzheimer's disease—Related phenotypes in epidemiologic studies
I. Delalle 1, J. Blusztajn2, T. Stein2,3, G. Jun2,4, A. Fischer5
1Brown University, Pathology and Laboratory Medicine, Providence, RI, United States; 2Boston University Chobanian & Avedisian School of Medicine, Boston, MA, United States; 3Boston University Alzheimer's Disease Research Center, Boston, MA, United States; 4Boston University School of Public Health, Boston, MA, United States; 5Deutsches Zentrum für Neurodegenerative Erkrankungen e. V. (DZNE), Goettingen, Germany
Effective causative therapies for Alzheimer's disease (AD) remain elusive as the development of diagnostic tools and therapies continues to focus on the part of the genome that encodes proteins. However, 97% of the genome consists of non‐coding RNAs (ncRNAs), increasingly recognized as pivotal regulators of cellular processes. ncRNAs have emerged as key regulators of brain functions derailed in AD and those longer than 200 nucleotides are known as long‐noncoding RNAs (lncRNAs). We hypothesize that the lncRNAs in cortical cells become deregulated in AD and might serve as specific pathology‐associated biomarkers. We performed a transcriptome‐wide expression profiling by RNAseq in 176 postmortem samples of the dorsolateral prefrontal cortex (DLPFC) in Framingham heart study (FHS) to investigate gene expression associations with two categories of AD‐related phenotypes. The first category included clinical dementia rating (CDR) score, the duration of cognitive impairment, the diagnosis of AD by NIA Reagan criteria, Braak & Braak (BB) stage, and CERAD‐C neuritic plaque (NP) score. The second category included quantitative pathology measures within the DLPFC, including phospho‐Tau immunostaining, the levels of amyloid β peptides 40 and 42, the levels of a presynaptic neuronal protein αSynuclein and of the postsynaptic density protein 95, and the cellular density of IBA1+ microglia. We found significantly differentially expressed genes (DEG) most prominently in inflammatory and apoptotic pathways. Among the DEGs, there were 9 annotated lncRNAs associated with IBA1 signal and 27 lncRNAs associated with CDR score. We compared our results to those made available by Religious Orders Study and Rush Memory and Aging Project (ROSMAP). Ten of FHS top noncoding DEGs appeared also in ROSMAP data and were, in addition to IBA1 signal and CDR score, associated also with BB stage and NP score. These data justify further investigations into deregulation of cortical lncRNAs in AD.
S19‐ND‐A149
Blood–brain barrier leakiness is associated with CSF evidence of increased TIE2 cleavage and ANGPT2 release in Alzheimer's disease
S. Ince 1, S. Miners1, H. Zetterberg2, K. Blennow3, S. Love1
1University of Bristol, Translational Health Sciences, Bristol, United Kingdom; 2University of Gothenburg, Psychiatry and Neurochemistry, Gothenburg, Sweden; 3University of Gothenburg, Psychiatry and Neurochemistry, Mölndal, Sweden
Introduction: Blood–brain barrier (BBB) leakiness is one of the early manifestations of neurovascular dysfunction in Alzheimer's disease (AD). In AD patients, we previously reported that elevated CSF albumin, a marker of BBB leakage, is associated with a rise in soluble platelet‐derived growth factor‐β (sPDGFRB), a marker of pericyte damage. Cerebral blood vessels are stabilised through activation of endothelial TIE2 receptors by angiopoietin‐1 (ANGPT1), released by pericytes. In response to injury, endothelial cells release ANGPT2, which acts as a weak agonist or an antagonist of TIE2 and promotes angiogenesis and BBB leakiness. TIE2 activity can also be inhibited by TIE2 shedding. This may be induced by vascular endothelial growth factor, which we showed to be upregulated in association with reduced cerebral perfusion in AD.
Objectives: To assess CSF alterations in ANGPT‐TIE signal proteins in relation to pathological markers (t‐tau, p‐tau and Aβ42) and BBB leakiness markers (albumin, fibrinogen, IgG and sPDGFRB) in AD.
Materials and Methods: CSF samples from AD patients and controls (Table 1), and matched CSF/serum samples from neurologically normal individuals (Table 2), were received from University of Gothenburg, Sweden. CSF ANGPT2, sTIE2 and sTIE1 were measured by ELISA (Quantikine and DuoSet kits, R&D Systems).
Results: CSF ANGPT2 and sTIE2 were elevated in AD (p < 0.05 and p < 0.01, respectively). CSF sTIE1 was unchanged. CSF sTIE2 correlated strongly with p‐tau (r = 0.49, p < 0.0001), t‐tau (r = 0.47, p < 0.001), albumin (r = 0.27, p < 0.05), fibrinogen (r = 0.26, p < 0.05) and sPDGFRB (r = 0.56, p < 0.0001). CSF sTIE2 level correlated with CSF/serum albumin ratio (r = 0.72, p < 0.01) in CSF/serum matched cohort.
Conclusions: These data suggest that BBB breakdown in AD is associated with increased TIE2 cleavage and elevated ANGPT2 release. Measurement of sTIE2 and ANGPT2 in CSF may allow early detection and monitoring of BBB breakdown in AD.

S19‐ND‐A150
Neuropathology based biomarker discovery for vascular pathologies co‐existing with Alzheimer's disease neuropathologic change
M. Flanagan 1, K. Ajroud1, C. Spencer2, T. J. Montine3, S. A. Bukhari3, C. H. Kawas4, M. M. Corrada4, E. Pladies5, L. Pan5, J. F. Tranovich6, R. R. Reichard6, H. Zhang2, Q. Mao7, M. M. Mielke8, R. C. Petersen6, D. Dickson6, M. E. Murray6, M. M. Mesulam2, T. Gefen2, X. Liu9, S. Seshadri1
1University of Texas Health San Antonio, Pathology and Bigg's Institute, San Antonio, TX, United States; 2Northwestern University, Chicago, IL, United States; 3Stanford University, Stanford, CA, United States; 4University of California, Irvine, Irvine, CA, United States; 5NanoString, Seattle, WA, United States; 6Mayo Clinic, Jacksonville, FL, United States; 7University of Utah, Salt Lake City, UT, United States; 8Wake Forest University School of Medicine, Winston‐Salem, NC, United States; 9University of New Orleans, New Orleans, LA, United States
Introduction: Dementia is characterized by the progressive loss of intellectual functioning. Alzheimer's disease (AD), characterized by plaques and Tau tangles, is the most common form of dementia followed by vascular dementia. Notably, co‐existing Tau tangles and vascular dementia pathologies (e.g., chronic microinfarcts) are the norm and not the exception in human disease. Increased pathological Tau burden has also been described in the setting of co‐existing vascular pathologies.
Question: Are there cell‐specific Tau alterations in the development of dementia that are associated with the presence of co‐existing chronic microinfarcts?
Methods: Immunofluorescence staining and whole transcriptome atlas digital spatial profiling were performed on human autopsy brain samples (n = 16) with matched AD pathology and increasing co‐existing chronic microinfarct counts, in addition to increasing memory impairment. Basal ganglia and middle frontal cortex were examined. Other co‐existing lesions (e.g., TDP43) were excluded. The following groups were assessed: 0 microinfarcts/cognitively intact (0), 1 microinfarct/cognitively intact (1), 2 microinfarcts/cognitively impaired (2), and 3 microinfarcts/demented (3). Cell‐type specific markers were applied as “masks.” Principal Component Analysis and hierarchical clustering were performed.
Results: Decreasing astrocytic PTBP1 with increasing chronic microinfarcts was most prominent in preclinical disease. In amnestic mild cognitive impairment, PSD95/pTau214 colocalization was increased in the presence of co‐existing vascular pathologies when compared to controls (p = 0.005) but not between amnestic mild cognitive impairment cases lacking co‐existing vascular pathologies versus controls.
Conclusion: Increased synaptic pTau214 in the presence of co‐existing vascular pathologies may result from altered regulation of Tau exon 10 splicing due to reduced expression of astrocytic PTBP1. Results highlight PTBP1's potential role as a preclinical biomarker.

FIGURE 1.

FIGURE 2.
S19‐ND‐A151
Investigating the effect of mixed pathologies on neuropathological spread in dementia with Lewy bodies
L. Walker 1, K. McAleese1, J. Attems1
1Newcastle University, Translational and Clinical Research Institute, Newcastle upon Tyne, United Kingdom
Objective: Dementia with Lewy bodies (DLB) is neuropathologically defined by inclusions of α‐synuclein (α‐syn). However, concomitant Alzheimer's disease (AD) pathologies, hyperphosphorylated tau (HP‐T) and β amyloid, are observed frequently at post‐mortem examination, with 50%–70% of DLB cases found to have medium to high‐level of AD neuropathologic change. Mixed pathologies are associated with an accelerated cognitive decline, which can make diagnosis challenging. An increased burden of all three pathologies in end‐stage dementia suggests a potential synergistic interaction between these proteins and is supported by studies that demonstrate α‐syn and HP‐T are co‐localised. Proteins can undergo numerous alterations, which can affect their structure and enhance toxicity, however little is known regarding which post‐translational modifications (PTMs) of α‐syn and tau are co‐localised, and are associated with specific clinical symptoms.
Methods: Using tissue microarray (TMA) slides that incorporate 15 anatomically distinct brain regions we investigated if a number of PTMs of α‐syn and tau (i.e., asyn phosphorylated at serine 129, MC1, CP13, Alz 50 and PHF‐)1 are frequently co‐localised and are predictors of neuropathological spread and clinical disease progression in DLB by using human post‐mortem brain tissue.
Results: Co‐localisations between a‐syn pS129 and all tau markers were observed in multiple brain regions, in particular the amygdala and topographical distributions differed between DLB cases with low and high levels of concomitant AD related neuropathology.
Conclusions: It seems paramount that we understand the interplay between these two pathological proteins, as presently there are no combination therapies to target both pathologies in clinical trials.
S22‐ND‐A152
Extracellular vesicles in blood—Potential biomarkers for Alzheimer's disease and differential diagnosis based on synaptic function and brain‐region related proteins
C. Tian 1, Z. Guo1, J. Zhang1
1Zhejiang University School of Medicine the First Affiliated Hospital, Pathology, Hangzhou, China
Question: Alzheimer's disease (AD) currently lacks convenient and rapid diagnostic method, as well as precision biomarkers. The effective treatment of AD relies heavily on accurate and sensitive diagnosis.
Methods: The pathogenesis of AD is closely related to synaptic function, and the onset of AD is strongly associated with specific brain regions. We searched for blood‐based extracellular vesicles (EVs) markers and identified NMDAR2A, a protein related to synaptic function, as a novel marker of CNS‐derived plasma EVs. We also identified GABRD and GPR162 as brain‐region (cortical and hippocampal regions) related biomarkers. We developed a flow cytometry‐based assay for detecting these plasma EVs, which was tested in a cross‐sectional study to distinguish AD from healthy controls (HCs). The assay was further validated using an independent cohort collected from multiple centers, including non‐AD dementia (NAD) cohorts for differential diagnosis.
Results: The study found that CNS‐derived EVs (NMDAR2A+) in plasma, were significantly reduced in AD compared to HCs. Integrating NMDAR2A‐EVs with Aβ and pTau, improved the accuracy of diagnosis, with an AUC of 0.915 in the discovery cohort (32 HCs, 45 AD) and 0.810 in the validation cohort (82 HCs, 66 AD). We also identified GABRD‐ and GPR162‐carrying pTau217 EVs in plasma, which were greatly reduced in AD compared to HCs. Moreover, the size distribution of these EVs differed significantly between AD and NAD. Integrating the number of GABRD‐ or GPR162‐carrying pTau217 EVs and their size distribution accurately discriminated AD from HCs, with an AUC of 0.96 in discovery cohort (85 HCs, 132 AD) and 0.93 in validation cohort (70 HCs, 99 AD), and effectively distinguished AD from NAD, with an AUC of 0.91 in discovery cohort (132 AD, 93 NAD) and 0.90 in validation cohort (99 AD, 44 NAD).
Conclusion: We first identified EV markers related to synaptic function and specific brain regions, which provide novel biomarkers for AD diagnosis and differential diagnosis. In addition, we developed a fast and stable flow cytometry‐based EV detection system, which can provide a new technology for future clinical translation.

FIGURE 1.
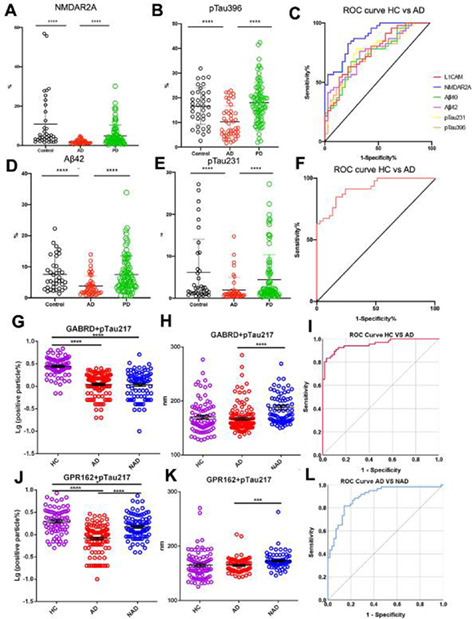
FIGURE 2.
S22‐ND‐A153
Treatment with necroptosis‐inhibitors reduces accumulation of necroptosis‐related proteins and neuronal loss in APP23xTAU58 mice
M. Koper1,2,3, S. Moonen1,2,3, A. Ronisz1, S. Ospitalieri1, S. Rabe4, M. Staufenbiel4,5, B. De Strooper2,3, S. Balusu2,3, D. R. Thal 1,6
1KU Leuven, Imaging and Pathology, Leuven, Belgium; 2VIB, Center for Brain & Disease Research, Leuven, Belgium; 3KU Leuven, Neuroscience, Leuven, Belgium; 4Novartis Institutes for Biomedical Research, Basel, Switzerland; 5Hertie Institute for Clinical Brain Research, Cellular Neurology, Tuebingen, Germany; 6UZ Leuven, Pathology, Leuven, Belgium
Introduction: Neuronal death is the result of the neurodegenerative process in Alzheimer's disease (AD). To model AD‐like neuronal death, mouse models for AD pathology can be used. Recently, the necroptotic cell death pathway was found to be activated in the AD brain with the activated necrosome being found in granulovacuolar degeneration (GVD) lesions in neurons.
Objectives: To inhibit necroptosis pathway activation and to reduce neuron loss.
Materials and Methods: We analyzed APP23xTAU58 transgenic mice for the presence of the activated necrosome in GVD lesions. APP23xTAU58 mice at 2, 6, and 12 months of age were studied (n = 5–10 animals/group). Neuronal densities in the subiculum and the amygdala were compared with those of wildtype littermates. To clarify whether necroptosis inhibitors can interfere with neuron death, we treated APP23xTAU58 mice from 2 to 6 months either with dabrafenib or ponatinib (n = 5 animals/group) and compared neuronal densities with that of vehicle‐treated mice. Neuronal densities and the percentage of necroptosis markers‐exhibiting neurons in the subiculum was assessed.
Results: Six‐ and 12‐month‐old APP23xTAU58 mice showed decreased neuronal densities in the subiculum and amygdala compared to wildtype mice (p < 0.005), as well as an increased number of neurons exhibiting the necroptosis executor pMLKL in GVD lesions (p < 0.0001). Treatment with the necroptosis inhibitors ponatinib and dabrafenib reduced neuronal loss in the subiculum compared to vehicle treatment (p ≤ 0.0002).
Conclusion: These results show that neuron loss in the APP23xTAU58 model is associated with the accumulation of necroptosis‐related proteins. This neuron loss and the expression of necrosome components can be reduced by ponatinib or dabrafenib. Thus, it is tempting to speculate that necroptosis inhibition could be a promising strategy to prolong neuronal survival and, by doing so, to slow down cognitive decline in AD patients.
Funding: FWO.
S22‐ND‐A154
Detection of alpha‐synuclein in biopsies and surgical resections of peripheral organs in patients with isolated REM sleep behavior disorder
I. Aldecoa 1,2, G. Maya3, N. Vidal‐Robau1, C. Gaig3, J. Santamaria3, M. Serradell3, L. Molina‐Porcel2,3, E. Gelpi4, À. Iranzo3
1Hospital Clinic Barcelona, Pathology, Barcelona, Spain; 2FCRB‐IDIBAPS, Neurological Tissue Bank of the Biobank, Barcelona, Spain; 3Hospital Clinic Barcelona, Neurology, Barcelona, Spain; 4Medical University of Vienna, Neurology, Vienna, Austria
Introduction: REM sleep behavior disorder (RBD) is a parasomnia with high risk of developing an alpha‐synuclein (ASyn) pathology, mainly Lewy body disease (LBD). There is evidence of ASyn inclusions in the peripheral autonomic nervous system (PNS) of RBD and LBD patients, but with conflicting results.
Objectives: To assess the presence of phosphorylated ASyn (pASyn) and/or oligomeric ASyn (oASyn) in gastrointestinal, skin, and/or urological biopsies of RBD patients and matched controls.
Patients and Methods: One hundred and seventy samples from 46 polysomnogram (PSG) confirmed RBD patients were retrospectively collected from the Pathology Department archives. One hundred and seventy samples from 134 neurological controls were matched by age and biopsy location. pASyn pSyn64, Wako and oASyn 5G4, Roboscreen, antibodies were used. A biopsy was positive when coarse, delicate or punctate aggregates were clearly identified in neural structures (neurons or neurites). Compatible images in the context of moderate or severe background were identified as suggestive.
Results: Preliminarly analyses of PASyn in 117 RBD samples (36 patients) and 139 control samples (116 controls) revealed a positive result in 9/117 RBD samples (7.7%) and 1/139 (0.7%) controls. Of the 9 positive RBD samples, 1 was obtained in the presymptomatic stage, 2 prior to RBD diagnosis and 6 after PSG confirmation of RBD, without parkinsonism or dementia. Regarding location, 8 were prostatic samples, 1 colon and 1 gallbladder. There were 25/117 (21.4%) RBD samples and 12/139 (8.6%) control samples that were either positive or suggestive. At least 49.2% of the samples had moderate to severe staining background.
Conclusion: pASyn deposits in the PNS may occur very early in disease, even prior to the clinical diagnosis of RBD. pASyn assessment can be difficult in retrospective samples with multiple processing protocols, and sensitivity and specificity can vary greatly depending on the strictness of the positivity criteria.
S28‐ND‐A155
Treatment with the autophagy activator spermidine reduced amyloid beta pathology and neuroinflammation in an Alzheimer's disease mouse model
M. Jendrach 1, K. Freitag1, N. Sterczyk1, S. Wendlinger1, B. Obermayer2, J. Schulz1, V. Farztdinov3, M. Mülleder3, M. Ralser4, J. Houtman1, L. Fleck1, C. Braeuning5, R. Sansevrino6, C. Hoffmann6, D. Milovanovic6, S. J. Sigrist7, T. Conrad5, D. Beule2, F. L. Heppner1
1Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 2Berlin Institute of Health at Charité—Universitätsmedizin Berlin, Core Unit Bioinformatics, Berlin, Germany; 3Charité—Universitätsmedizin Berlin, Core Facility—High‐Throughput Mass Spectrometry, Berlin, Germany; 4Charité—Universitätsmedizin Berlin, Biochemistry, Berlin, Germany; 5MDC, Genomics Technology Platform, Berlin, Germany; 6DZNE, Laboratory of Molecular Neuroscience, Berlin, Germany; 7FU Berlin, Institute for Biology and Genetics, Berlin, Germany
Introduction: Alzheimer's disease (AD) and dementia are among the top 10 leading causes of death according to the WHO (Global Health Estimates, 2019). Main hallmarks of AD are extracellular amyloid plaques (main component amyloid‐beta (Aβ) peptide), neurofibrillary tangles (main component hyperphosphorylated MAP tau) and neuroinflammation. Despite intensive and lengthy research a cure is still elusive. Therefore, we concentrated on possible interventions to slow disease progression.
Objectives: A growing body of evidence shows that modulation of autophagy can influence neuroinflammation and AD pathology. Therefore, we investigated possible health benefits of autophagy activation.
Materials and Methods: The AD‐like mouse model APPPS1 was treated with 3 mM of the autophagy activator and nutritional supplement spermidine via their drinking water, starting prior to disease onset. AD pathology was analyzed at an earlier (120 d) and late (290 d) disease state.
Results: Spermidine treatment significantly reduced soluble Aβ levels, and at 290 d also neuroinflammation. Single nuclei RNA sequencing showed that microglia were the main CNS cell type affected by spermidine. Accordingly, treatment of isolated microglia with spermidine increased migration and Aβ phagocytosis and blunted the release of cytokines in response to various stimuli. In correlation, proteome analysis of isolated microglia from spermidine‐treated APPPS1 mice showed activation of autophagy and downregulation of inflammatory pathways.
Conclusion: In mice, spermidine mediates amelioration of AD pathology. Therefore, the extension of spermidine supplementation from individuals with subjective cognitive decline to clinical trials aimed at testing spermidine in AD patients appears to be reasonable.
S28‐ND‐A156
Amyloid‐β deposits distinctively correlate with tangles and glial activation in Alzheimer's disease subtypes
B. D. C. Boon 1, N. Kouri1, S. A. Labuzan1, Z. Peng2, J. F. Tranovich1, I. Frankenhauser3, C. Lachner4,5, N. Ertekin‐Taner1,4, R. Duara6, N. R. Graff‐Radford4, D. Dickson1, M. E. Murray1
1Mayo Clinic, Neuroscience, Jacksonville, FL, United States; 2Mayo Clinic, Quantitative Health Sciences, Jacksonville, FL, United States; 3Paracelsus Medical University, Salzburg, Austria; 4Mayo Clinic, Neurology, Jacksonville, FL, United States; 5Mayo Clinic, Psychiatry and Psychology, Jacksonville, FL, United States; 6Mount Sinai Medical Center, Miami Beach, FL, United States
Question: Amyloid‐β (Aβ) deposits are required for Alzheimer's disease (AD) diagnosis. However, Aβ does not correlate well with the other AD neuropathological hallmark; tangles. Different types of Aβ deposits are recognized, and we previously characterized the new coarse‐grained plaque. The current study questions how distinct Aβ deposits correlate with neuropathologic change and glial activation in AD subtypes.
Methods: The association cortices of 60 AD cases (hippocampal sparing, typical, and limbic predominant) were scored for Aβ deposits (classic cored plaques, coarse‐grained plaques, cerebral amyloid angiopathy [CAA]‐Type 1, CAA‐Type 2) (Figure 1). These scores were correlated to clinicopathologic characteristics, neuropathologic stages, AD neuropathologic change (Aβ, [phospho‐] tau, tangles) and glial activation (CD68 and GFAP).
Results: In the frontal cortex of hippocampal sparing AD, higher scores of classic cored plaques correlated with older age at onset and death, non‐APOE ε4 carriership, and less CAA‐Type 1 and Type 2 (Figure 2). On the contrary, the severity of coarse‐grained plaques correlated with a younger age at onset and death, APOE ε4 carriership, higher scores for CAA‐Type 1, CAA‐Type 2, and increased burden of Aβ, GFAP, and CD68. Classic cored plaques correlated negatively with phospho‐tau and tau, whereas coarse‐grained plaques correlated positively with phospho‐tau, tau, and tangles. The two Aβ deposits were negatively correlated with each other. CAA‐Types showed correlations resembling those observed for the coarse‐grained plaques, but weaker. In the other AD subtypes (Figure 2) and regions, Aβ deposit correlations were weaker but showed similar trends.
Conclusions: The observed inverse correlations for the classic cored and the coarse‐grained plaque on AD neuropathologic change suggest that the Aβ deposit‐associated pathophysiology may be protective in certain deposits but detrimental in others, which is relevant for therapies targeting Aβ.


S08‐ND‐A157
Single nuclei RNA‐sequencing across different brain regions in multiple system atrophy
V. C. Ruf 1, N. Briel1,2, F. L. Struebing1,2, J. Mielke1, S. Roeber1, T. Arzberger1,2,3, O. Windl1, J. Herms1,2,4
1Ludwig‐Maximilians‐University, Center for Neuropthology and Prion Reserach, Munich, Germany; 2German Center for Neurodegenerative Diseases (DZNE), Munich, Germany; 3Ludwig‐Maximilians‐University, Department of Psychiatry and Psychotherapy, Munich, Germany; 4Munich Cluster for Systems Neurology, Munich, Germany
Introduction: Multiple system atrophy (MSA) is a devastating rapidly progressive neurodegenerative disease for which no potent symptomatic nor causal treatment is available to date. Histologically, MSA is characterized by severe neuronal loss and gliosis in distinct brain regions accompanied by glial cytoplasmic inclusions (GCIs) of alpha‐synuclein in oligodendrocytes. How the different cell types in the brain contribute to and interact in disease pathogenesis is so far only poorly understood.
Objectives: The aim of this study is to characterize the transcriptomic profile of various cell types in differentially affected brain regions of MSA patients and healthy controls in order to improve our understanding of the underlying cellular and molecular pathomechanisms.
Materials and Methods: Single nuclei RNA‐sequencing and subsequent bioinformatic analysis was performed on approximately 250,000 nuclei isolated of the frontal cortex, frontal white matter and occipital white matter of 10 MSA patients and 5 healthy controls.
Results: After appropriate preprocessing, distinct clusters were formed and annotated. We were able to detect various differentially expressed genes across different cell populations, suggesting different extents of involvement of the cell types in the disease pathogenesis.
Conclusion: Our study presents a large and powerful dataset helping to unravel underlying molecular mechanisms and processes in MSA and providing potential links for molecular targets for diagnostic and/or therapeutic intervention.
S08‐ND‐A158
Studying selective vulnerability in Parkinson's disease using spatial transcriptomics—Technical appraisal and optimisation
A. K. L. Liu 1, A. Z. Zhao1, J. M. Sandoval2, J. Morgan2, M. Rokicki2, C. Webber2, L. Parkkinen1
1University of Oxford, Nuffield Department of Clinical Neurosciences, Oxford, United Kingdom; 2Cardiff University, Dementia Research Institute, School of Medicine, Cardiff, United Kingdom
Introduction: Transcriptomics techniques, such as bulk and single‐cell RNA sequencing, have enabled the study of selective vulnerability in Parkinson's disease (PD) through the analysis of gene expression profiles in specific cell type within a tissue. However, spatial organisation of cells is lost using these techniques. Recent advancement in spatial transcriptomics technology means that gene expression can be precisely mapped to individual cell populations within an anatomical region.
Objectives: We aim to assess the feasibility of spatial transcriptomics on archival formalin‐fixed paraffin‐embedded (FFPE) human brain tissues using the novel Visium Spatial Gene Expression technology.
Materials and Methods: FFPE blocks containing the substantia nigra and entorhinal cortex from three PD and three aged‐controls were obtained from the Oxford Brain Bank. Degree of RNA fragmentation of the tissue was assessed using the DV200 metric. Tissue sections were mounted on spatially barcoded slides from the Visium Spatial Gene Expression kit and stained with H&E. Following library construction and sequencing, gene expression data was visualised and analysed using the Loupe Browser.
Results: Following sequencing, an average of approximately 337 unique genes were detected per barcoded spot (range, 11–1047). Expression‐based clustering analysis revealed up to eight clusters which maps well to distinct anatomical regions. Spearman correlation identified the median number of unique genes per spot significantly correlates with time in fixation (Rho = −0.78, p = 0.0016), but not DV200 (Rho = 0.17, p = 0.5573) or post‐mortem interval (Rho = 0.24, p = 0.4132).
Conclusion: This study demonstrates it is feasible to use archival FFPE brain tissues for spatial transcriptomics despite high degree of RNA fragmentation as measured by DV200. Future work should aim to use samples with a post‐mortem formalin fixation time of less than 3–4 weeks.
S14‐ND‐A159
Consistent and distinct involvement of the cranial and spinal nerves in PSP and other tauopathies
H. Tanaka 1, I. Martinez‐Valbuena1, B. Couto2, N. G. Reyes2, S. Lee1, J. Li1, A. M. Karakani1, A. E. Lang2, G. G. Kovacs1,3,4
1University of Toronto, Department of Laboratory Medicine and Pathobiology, Toronto, Canada; 2Toronto Western Hospital, Toronto, Canada; 3Toronto Western Hospital, Krembil Research Institute, Toronto, Canada; 4University Health Network, Laboratory Medicine Program, Toronto, Canada
Introduction: In neurodegenerative diseases, the aggregation of pathological proteins in peripheral nerves is well‐recognized in α‐synucleinopathies, but the status in tauopathies is uncertain.
Objectives: To clarify the involvement of tau pathology in the peripheral nervous system (PNS) in tauopathies.
Materials and Methods: We investigated the tau pathology in PNS (PNS‐tau) in 45 cases of tauopathies (progressive supranuclear palsy: PSP, n = 16; Alzheimer's disease: AD, n = 18; corticobasal degeneration: CBD, n = 6; chronic traumatic encephalopathy: CTE, n = 5) using immunohistochemistry, biochemistry, and tau seeding assays.
Results: Most PSP cases revealed tau aggregates (4‐repeat tau) in the PNS, (number of tau‐positive cases/available cases) cranial nerves III: 8/9 (89%), IX/X: 10/11 (91%), XII: 6/6 (100%); anterior spinal roots: 10/10 (100%). The tau‐positive inclusions in PSP often showed large structures with fibrillary (neurofibrillary tangle‐like) morphology in the axon that were recognized with Gallyas staining also. Some of the nerve fibers were filled with the large tau inclusions. In contrast, tau pathology in the PNS was not evident in AD and CTE cases. CBD cases rarely showed a few fine granular tau deposits. The severity of tau lesions in the PNS and the corresponding brainstem nuclei was compared in PSP. Occasionally, tau aggregates were present in the PNS but not in the related brainstem nuclei. For the first time, we demonstrated using seed amplification assays that tau aggregates found in the PNS also have seeding capacity.
Conclusion: The involvement of PNS is most prominent in PSP. The morphological differences of PNS‐tau between PSP and CBD suggest that the tau pathology in PNS could reflect that in the CNS. The high frequency and early presence of tau lesions in PSP suggest that PNS‐tau may have clinical and biomarker relevance.
S14‐ND‐A160
DNA methylation differences in Alzheimer's disease neuropathology in old age—A comprehensive brain region survey
A. L. Lang 1, T. Eulalio2, E. Fox3, K. Yakabi3, S. A. Bukhari3, C. H. Kawas4,5, M. M. Corrada4,6, S. B. Montgomery2,3,7, F. L. Heppner1,8,9, D. Capper1, D. Nachun7, T. J. Montine3
1Charité—Universitätsmedizin Berlin, Department of Neuropathology, Berlin, Germany; 2Stanford University, Department of Biomedical Data Science, Stanford, CA, United States; 3Stanford University, Department of Pathology, Stanford, CA, United States; 4University of California, Irvine, Department of Neurology, Irvine, CA, United States; 5University of California, Irvine, Department of Neurobiology and Behavior, Irvine, CA, United States; 6University of California, Irvine, Department of Epidemiology, Irvine, CA, United States; 7Stanford University, Department of Genetics, Stanford, CA, United States; 8German Center for Neurodegenerative Diseases (DZNE), Berlin, Germany; 9Cluster of Excellence, NeuroCure, Berlin, Germany
Introduction: Alzheimer's disease (AD) is the most prevalent cause of dementia, with advancing age as its primary risk factor. AD neuropathologic change (ADNC) has been associated with various DNA methylation (DNAm) changes in the human brain, but epigenetic studies of ADNC have so far neglected the oldest old (>90 years) population.
Objectives: We aimed to investigate ADNC‐related DNAm changes in old age and provide a comprehensive DNAm survey of the aging human brain.
Materials and Methods: The study included 47 participants aged over 90 years from The 90+Study at UCI Irvine. Using the Illumina 850k BeadChip, we analyzed DNAm from bulk samples in eight brain regions: middle frontal gyrus, cingulate gyrus, entorhinal cortex, dentate gyrus, CA1, substantia nigra, locus coeruleus and cerebellar cortex. We used computational methods to deconvolve bulk data into cell type‐specific (CTS) signals and examined CTS‐DNAm differences across multiple levels of ADNC.
Results: The dentate gyrus and cingulate gyrus showed the highest amount of ADNC‐related DNAm differences (Figure 1). In neurons of the dentate gyrus, DNAm significantly differed with increased burden of Aβ plaques at 5897 promoter regions of protein coding genes. Increased Aβ plaque burden was thereby associated with promoter hypomethylation of two important genes of the γ‐secretase complex (PEN‐2, NCSTN), a complex that is responsible in part for the endoproteolytic cleavage of amyloid precursor protein into Aβ peptides (Figure 2).
Conclusion: We shed light on ADNC‐related DNAm changes in old age. Computational deconvolution of bulk data enabled the recovery of CTS signals without the need for cell sorting. The dentate gyrus and cingulate gyrus, with the highest ADNC‐associated DNAm differences, have prior been underrepresented in multi‐omic studies. Our open‐sourced dataset can serve as a brain region reference panel for future studies and help advance research in aging and neurodegeneration.

FIGURE 1.

FIGURE 2.
S14‐ND‐A161
Blood CNS regionally enriched extracellular vesicles carrying pTau217 for Alzheimer's disease diagnosis and differential diagnosis
Z. Guo 1, C. Tian1, J. Zhang1
1The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
Introduction: To treat Alzheimer's disease (AD) effectively depends heavily on precise early diagnosis and differential diagnosis among various dementias. Recently, the strategy of enriching central nervous system (CNS)‐specific biomarkers from the blood by targeting extracellular vesicles (EVs) has been explored, with promising results for AD diagnosis; but differential diagnosis from other dementias remains challenging.
Objectives: To identify novel blood‐borne neuronal EVs that are more enriched in the brain regions vulnerable to AD, and to evaluate their ability to differentiating AD from non‐AD dementia (NAD) in addition from healthy control (HC).
Patients and Methods: This study included 523 participants, with dementing subjects classified as AD or NAD based on levels of Aβ40, Aβ42, t‐tau in cerebrospinal fluid and/or Centiloid scale of PIB‐PET. Participants without clinical dementia were considered as HC. The performance of newly identified brain regionally enriched EVs markers, GABRD and GPR162, in conjunction with the known AD molecule pTau217, was tested using an optimized nanoflow cytometry‐based technology.
Results: The results demonstrated that GABRD+‐ or GPR162+‐carrying pTau217‐EVs in plasma were significantly reduced in AD compared with HC. Additionally, the size distributions of GABRD+‐ and GPR162+‐carrying pTau217‐EVs were significantly different between AD and NAD. An integrative model, combining the number and the corresponding size of the distribution mode of GABRD+‐ or GPR162+‐carrying pTau217 EVs as well as age, accurately discriminated AD from HC (AUC: 0.96, discovery cohort; 0.93, validation cohort) and effectively differentiated AD from NAD (AUC: 0.91, discovery cohort; 0.90, validation cohort).
Conclusion: Plasma brain regionally enriched EVs carrying pTau217 have the potential to be a minimally invasive diagnostic and differential diagnostic tool for AD, which is critical in both clinical practice and trials.
S14‐ND‐A162
Investigating ALS pathogenesis caused by distinct SOD1 strains in transgenic mouse models
T. Brännström 1, I. Sigfridsson1
1Umeå University, Department of Medical Biosciences, Umeå, Sweden
Abnormal proteins are central in neurodegenerative diseases such as Alzheimer's, Parkinson's, Huntington's and amyotrophic lateral sclerosis (ALS). In these diseases, evolving evidence show the capability of the misfolded proteins to assemble into different strains and propagate in a prion‐like manner. The presence of aggregates formed by misfolded superoxide dismutase‐1 (SOD1) proteins is hallmarks of ALS caused by mutations in the SOD1 gene. In our laboratory, two structurally distinct strains of human (h) SOD1 aggregates (denoted A and B) have previously been identified in transgenic (Tg) hSOD1 mice. Intra‐spinal inoculations of these strains into adult mice have shown their capability to induce strain‐specific aggregation through templating and cause premature fatal motor neuron disease, supporting that ALS caused by SOD1 mutations is a prion‐like disease. Additionally, it was shown that strain A and B affect the progression of the disease differently, suggesting a difference in pathogenesis provoked by the distinct strains. Whether this difference could be explained by unique cellular or subcellular localizations in the central nervous system (CNS) has previously not been examined. In this study, we optimized protocols to detect strain A and B aggregates at a cellular and subcellular level in order to investigate their localization in the CNS. Antibodies targeting strain specific sequences were used to label hSOD1 aggregates in spinal cords of hSOD1G85R and hSOD1D90A Tg mice. The aggregates were visualized using confocal imaging and electron microscopy. Our results show successfully developed protocols for histological visualization of strain A and B and for studying localization of hSOD1 aggregate species in the CNS of ALS Tg mouse models. These findings form the basis to further investigate the difference in disease progression provoked by strain A and B hSOD1 aggregates and will be of great importance for the development of therapeutic strategies.
S14‐ND‐A163
Alterations of neuroprotective ER‐co‐chaperone SIL1—Disruption of autophagy and RNA binding protein homeostasis and selective neuronal vulnerability in amyotrophic lateral sclerosis (ALS)
H. Guo 1, A. Yamoah1,2,3, P. Tripathi1,2,3, I. Katona1, E. Aronica4, M. Naumann5, A. Hermann5,6, H. Steinbusch2,3, A. Roos7,8, J. Weis1, A. Goswami1,9,10
1RWTH Aachen University Hospital, Institute of Neuropathology, Aachen, Germany; 2School for Mental Health and Neuroscience, Maastricht University, Department of Psychiatry and Neuropsychology, Maastricht, Netherlands; 3EURON—European Graduate School of Neuroscience, Maastricht University, Maastricht, Netherlands; 4Academic Medical Centre, Division of Neuropathology, Department of Pathology, Amsterdam, Netherlands; 5Translational Neurodegeneration Section “Albrecht‐Kossel,” Department of Neurology and Center for Transdisciplinary Neurosciences Rostock (CTNR), University Medical Center Rostock, University of Rostock, Rostock, Germany; 6German Center for Neurodegenerative Diseases (DZNE), Rostock, Germany; 7University Hospital Bergmannsheil, Ruhr University Bochum, Department of Neurology, Heimer Institute for Muscle Research, Bochum, Germany; 8University Duisburg‐Essen, Department of Neuropediatrics and Neuromuscular Centre for Children and Adolescents, Center for Translational Neuro‐ and Behavioural Sciences, Essen, Germany; 9Columbia University, Department of Neurology, Center for Motor Neuron Biology and Disease, New York, NY, United States; 10Eleanor and Lou Gehrig ALS Center, Columbia University, Department of Neurology, New York, NY, United States
Amyotrophic lateral sclerosis (ALS) is a devastating disease characterized by progressive loss of upper and lower motor neurons (MNs). Recent studies showed that selectively viable neurons are often equipped with several protective factors, while vulnerable neurons lack them. Among others, ER co‐chaperone SIL1 warrants such selective MN viability. However, the precise molecular mechanism(s) of such neuroprotection as well as its role in maintaining neuronal proteostasis is largely unclear. We aimed to validate the concept of selective neuronal vulnerability in human ALS together with investigating the neuroprotective role of SIL1 associated with the protein quality control (PQC) mechanism. We used ALS postmortem autopsy materials and compared them with human iPSC‐derived motor neurons as well as cells expressing ALS‐causing mutant proteins. Our results confirmed that in the human lumbar spinal cord SIL1 protein levels were specifically elevated in slow fatigue‐resistant motor neurons (ERRβ2‐positive sMNs) compared to the fast‐fatigable MNs (CHODL‐positive fMNs) in sporadic ALS (sALS). CHODL‐positive fMNs appeared to be selectively vulnerable as they often harbored pathogenic pTDP‐43 aggregates, while ERRβ2‐positive sMNs were mostly devoid of such aggregates. Interestingly both in sALS as well as in fALS, α‐MNs showing increased levels of SIL1 were mostly lacking toxic aggregates. Of note, SIL1 was found to be sequestered with various forms of pTDP‐43 and other aggregates in ALS MNs, human IPSc‐derived fALS MNs as well as cells expressing ALS‐causing mutant proteins. Furthermore, overexpression of SIL1 facilitates the clearance of the above‐mentioned pathogenic aggregates via induction of autophagy which was further confirmed by loss of function approaches. In summary, our results suggest that SIL1 is crucial for neuronal PQC mechanism and survival. Pathogenic SIL1 modification such as SIL1 depletion and aggregation could be detrimental to the neurons.
PS3‐ND‐A165
Pathologic subtyping of Alzheimer's disease brain tissue reveals disease heterogeneity
T. Lam1, S. Leskinen1, B. Ciener1, S. Sivakumar1, H. Xiao1, D. Flaherty1, A. Ropri1, J. P. Vonsattel1, A. Teich 1
1Columbia University, New York, NY, United States
Introduction: In recent years, multiple groups have shown that what is currently thought of as “Alzheimer's disease” (AD) may in fact be usefully viewed as several related disease subtypes. Biologically relevant subtyping has been shown using a variety of metrics, including pathologic information, RNA‐seq data, and integration of multi‐omic data.
Objectives: Over the past 20 years, brains at Columbia University have been signed out with up to 196 pathologic variables recorded on each brain. Our goal was to use this data to help further inform efforts to understand AD disease subtyping using a well‐characterized dataset.
Materials and Methods: We assembled all of the recorded pathologic data on a cohort of 1439 brains that pass a threshold of having at least 80% of the 196 variables recorded and performed K‐medoids clustering to identify pathologic clusters within the data. We also performed bulk RNA‐seq on 513 pre‐frontal cortex samples (Brodmann area 8/9) and examined how this data segregates by pathologic cluster.
Results: Pathologic clustering revealed 14 pathologic clusters across all 1439 brains. This clustering reproduced known diagnostic groups as well as suggested subtyping within diseases, with notable subtyping within cases with a primary diagnosis of AD. Clustering of the 666 AD cases separately revealed 8 pathologic subtypes that are differentiated by varying levels of tau and non‐tau pathology. RNA‐seq of pre‐frontal cortex also revealed clustering that segregates differently across AD subtypes, providing orthogonal biological validation of our disease subtyping.
Conclusions: Neurodegenerative disease heterogeneity can be usefully approached with an unbiased clustering approach which can both reproduce established diagnostic categories as well as suggest subdivisions within disease categories that may be useful for future investigation.
PS3‐ND‐A166
Understanding the role of extracellular vesicles in the pathophysiology of Alzheimer's disease
M. Shafiq 1, A. Matamoros‐Angles1, L. Amin2, B. Mohammadi1, E. Karadjuzovic1, S. Da Vela3, I. Egger1, A. Zafar1, C. Seuring4, B. Siebels5, H. Voß5, H. Schlüter5, I. Ferrer6, M. Schweizer7, H. C. Altmeppen1, D. Svergun3, D. A. Harris2, M. Glatzel1
1University Medical Center Hamburg‐Eppendorf, Institute of Neuropathology, Hamburg, Germany; 2Boston University School of Medicine, Department of Biochemistry, Boston, MA, United States; 3European Molecular Biology Laboratory, Hamburg, Germany; 4Centre for Structural Systems Biology, Multi‐User CryoEM facility, Hamburg, Germany; 5University Medical Center Hamburg‐Eppendorf, Institute of Clinical Chemistry and Laboratory Medicine, Hamburg, Germany; 6Bellvitge University Hospital, Barcelona, Spain; 7University Medical Center Hamburg‐Eppendorf, Core Facility of Electron Microscopy, Center for Molecular Neurobiology, Hamburg, Germany
Introduction: Extracellular vesicles (EVs) are excellent cargo vehicles for cell‐to‐cell communication and are involved in crucial brain functions, such as myelin maintenance and neurotransmission. EVs have a high abundance of cellular prion protein (PrPC) on their surface. PrPC is a GPI‐anchored protein with highest expression in the nervous tissues; and in Alzheimer's disease (AD), EV‐PrPC along with other extracellular PrPC fragments is suggested to sequesters Aβ oligomers (Aβo) and reduces Aβo neurotoxicity; however, formal evidence and structural insights into the aggregation process are still lacking. Here, we aim to study the role of PrPC expressing EVs in Aβ fibrillation and to highlight physiological alterations associated with EV in AD.
Materials and Methods: PrPC‐expressing (WT) and ‐deficient (KO) EVs were obtained from WT and PrPC‐KO Neuro‐2a cells and also from WT and PrPC‐KO mice brain. Human brain‐derived EVs were isolated from frontal cortices of AD and age‐matched controls. EVs were characterized using Nanoparticle tracking analysis (NTA), immunoblotting, and negative stain TEM. To further the study objectives, small angle x‐ray scattering (SAXS), super‐resolution microscopy (SRM), Cryo‐EM, proteomic profiling, and associative biochemical and biophysical methods were employed.
Results: SAXS, EM, SRM and aggregation assays highlighted potent Aβo‐sequestering activity of the WT‐EVs. Lipidomic and proteomic profiling of N2a‐derived EVs pointed towards marked differences, however no variations were found for the Aβ binding proteins between WT‐ and KO‐EVs. EV isolated from AD brain tissues show alterations in PrPC expression compared to those of controls. Omics data from human EVs also highlight compositional differences specific to AD.
Conclusions: Our data suggest crucial role of EVs in AD by their involvement in Aβ aggregation, a related potential rescue mechanism against Aβo toxicity, and AD‐specific EV‐mediated intercellular communication.
PS3‐ND‐A167
The role of CD22 in Alzheimer's disease pathology in APPPS1 mice
V. Tschui 1, T. Pugeda1, M. Jendrach1, F. L. Heppner1
1Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany
CD22, a canonical B‐cell receptor, is involved in regulating B‐cell receptor signalling and cell adhesion, migration, proliferation, and survival. In the brain, CD22 is only expressed by myeloid cells. Functionally, CD22 showed a negative regulation of microglial phagocytosis of Amyloid‐β (Aβ) [1,2]. During aging and in the Alzheimer's disease (AD)‐like mouse model APPPS1, CD22 expression was upregulated in microglia surrounding Amyloid‐β (Aβ) plaques. Based on the hypothesis that in the course of AD CD22 upregulation leads to decreased phagocytosis and reduces Aβ uptake and degradation, we assessed whether a lack of CD22 impacts neuroinflammation and AD pathology in vitro and in vivo by means of in situ hybridisation, immunohistochemical stainings and biochemical approaches, as well as by employing in vitro assays to study phagocytosis of aged microglia. This way we analysed the Aβ burden in 4 (beginning of pathology) and 12‐month‐old (established pathology) APPPS1 mice, the amount of pro‐inflammatory cytokines, microglial activation as well as the phagocytic activity of microglia lacking CD22. Our data uncover the role of CD22 in microglia and the effect of CD22 deletion on AD pathology in this AD‐like mouse model.
References: [1] Pluvinage JV, et al. CD22 blockade restores homeostatic microglial phagocytosis in ageing brains. Nature. 2019;568(7751):187–92. [2] Aires V, et al. CD22 blockage restores age‐related impairments of microglia surveillance capacity. Front Immunol. 2021;12:684430.
PS3‐ND‐A168
Interleukin‐12‐driven crosstalk in Alzheimer's disease affecting oligodendrocyte survival and myelination
M. Geesdorf 1, S. Schneeberger1, E. Friebel1, E. Pérez1, A. Haake1, N. Gimber2, J. Schmoranzer2, J. Edgar3, F. L. Heppner1
1Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, AMBIO—Advanced Medical Bioimaging Core Facility, Berlin, Germany; 3University of Glasgow, Infection, Immunity and Inflammation, Gasgow, United Kingdom
Neuroinflammation is regarded as one of the pathological hallmarks of Alzheimer's disease (AD). The microglia‐derived interleukin (IL)‐12 herein presents an important player in the inflammatory processes promoting disease progression in APPPS1 mice, a mouse model with severe amyloid beta (Aβ) deposition, followed by neuroinflammation and a malformation of axon‐ensheathing myelin. Using single nuclei RNA‐sequencing we found that the receptors for IL‐12 are expressed on oligodendrocytes and subgroups of neurons. In the present study, we now investigated the underlying molecular mechanisms of the IL‐12 signaling pathway in oligodendrocytes and neurons in the AD context and its effect on myelination. The blockage of IL‐12 receptor signaling by deleting Il12b, encoding p40—the common subunit of IL‐12 and IL‐23, leads to significant changes in AD pathology in APPPS1.Il12b−/− mice and also to the rescue of myelin deficits such as myelin sheath thickness. We further assessed the effect of IL‐12 signaling on mature oligodendrocytes and myelin integrity by various in vitro methods, which includes primary murine as well as human neuronal stem cell‐derived oligodendrocytes. Our data supports the increasing interest in neuroinflammation‐driven microglia‐oligodendrocyte crosstalk and validates the potential of IL‐12‐driven novel interventional approaches to tackle AD.
PS3‐ND‐A169
Extra densities in cryo‐EM maps of fibrils from Alzheimer's disease and other neurodegenerations
L. Bridges 1
1St George's Hospital, Neuropathology, Cellular Pathology, London, United Kingdom
Introduction: In the last 5 years, electron cryo‐microscopy (cryo‐EM) maps of fibrils from a wide range of neurodegenerative diseases have been published and deposited by various authors in the electron microscopy data bank (EMDB), a public repository.
Objectives: To identify the constituent molecule(s) of extra densities (EDs) present in these maps.
Materials and Methods: Cryo‐EM maps of neurodegenerative fibrils from the EMDB were examined in silico, primarily using the molecular visualisation software UCSF ChimeraX.
Results: EDs are a common feature of fibrils involving alpha‐synuclein, tau, PrP and other proteins from Alzheimer's disease, argyrophilic grain disease, multiple system atrophy, Parkinson's disease, scrapie and other neurodegenerations. Typically, they are continuous and at right angles to protein rungs, and within hydrogen‐bonding distance of lysines and other basic residues, suggestive of a polyanion.
Conclusion: In addition to protein, a second component is present in fibrils from Alzheimer's disease and other neurodegenerations. This would appear to be a polyanionic substance for which ribonucleic acid (RNA) is a feasible candidate. The significance of this is discussed.
PS3‐ND‐A170
The neuropathological landscape of Hispanic and non‐Hispanic White decedents with Alzheimer's disease
R. Scalco 1, N. Saito2, L. Beckett2, M. L. Nguyen1, E. Huie1, H. P. Wang1, S. Leskinen3, D. Flaherty3, L. Honig3, C. DeCarli4, R. Rissman5, A. Teich3, L. W. Jin1, B. Dugger1
1University of California Davis, Pathology and Laboratory Medicine, Sacramento, CA, United States; 2University of California Davis, Department of Public Health Sciences, Division of Biostatistics, Davis, CA, United States; 3Columbia University, Taub Institute for Research on Alzheimer's Disease and Aging Brain, New York, NY, United States; 4University of California Davis, Department of Neurology, Sacramento, CA, United States; 5University of California San Diego, Department of Neuroscience, San Diego, CA, United States
Older persons within the United States are demographically diverse, leading to diversity among those with Alzheimer's disease (AD). Most autopsy‐based studies, however, have focused on cohorts of non‐Hispanic White decedents (NHWD), with few studies including Hispanic decedents (HD). We aimed to characterize the neuropathologic landscape of AD in NHWD (n = 185) and HD (n = 92) evaluated across three Alzheimer's Disease Research Centers: University of California San Diego, University of California Davis, and Columbia University. Only demented persons with a neuropathologic diagnosis of intermediate/high AD determined by NIA Reagan criteria were included. A frequency‐balanced random sample without replacement was drawn from the NHWD group using a 2:1 age and sex matching scheme with HD. Four brain areas were evaluated: posterior hippocampus, frontal, temporal, and parietal cortices. Sections were stained with antibodies against Aβ (4G8) and phosphorylated tau (AT8). We compared the distribution and semi‐quantitative densities for neurofibrillary tangles, neuropil threads, core, diffuse, and neuritic plaques. Evaluations were conducted by an expert blinded to demographics and group status. Wilcoxon's two‐sample test revealed higher levels of neuritic plaques in the frontal cortex (p = 0.02) and neuropil threads (p = 0.02) in HD. Although the median was similar for both groups in the temporal cortex, the density of cored plaques was statistically greater in NHWD (p = 0.02). Results from ordinal logistic regression controlling for age, sex, and site of origin were similar. In other evaluated brain regions, semi‐quantitative scores of plaques, tangles, and threads showed no statistical differences between groups. Our results indicate HD may be disproportionately burdened by AD‐related pathologies in select anatomic regions, particularly tau deposits. Further research is needed to understand the heterogeneous pathological presentations and their relation to underlying factors.

FIGURE 1.
PS3‐ND‐A171
The interaction between kallikrein‐8 and its inhibitory network affects Alzheimer's disease
P. Pereira de Almeida 1, K. Groll1, A. Herring1, M. Knoll1, N. Macha1, K. Keyvani1
1University Hospital Essen, Institue of Neuropathology, Essen, Germany
Introduction: Previous work in our lab has identified kallikrein‐8 (KLK8) as a potential upstream mover in the pathogenesis of Alzheimer's disease (AD) and as a possible therapeutic target. Proper KLK8 function depends on a tightly regulated but yet unknown inhibitory network. Serpin A3, serpin B6, alpha‐2 macroglobulin (α2M) and the acetylcholine (ACh) producing PEBP1 are considered as main protagonists.
Objectives: To determine the interaction pattern of KLK8 with its putative inhibitors, and to assess the functional consequences of this interaction on AD.
Methods: First, we examined the inhibitory effect of serpin A3/B6, PEBP1 and α2M on the enzymatic activity of KLK8 in an in vitro assay. Co‐Immunoprecipitation and western blotting were used to verify the complexation, and to quantify the levels of free and complexed molecules, respectively in the hippocampi of patients and TgCRND8 mice with or without KLK8 knockdown. Given that excess of KLK8 diminishes Aβ phagocytosis in primary glia, we tested whether serpin A3/B6, PEBP1 or α2M can inhibit KLK8 and reverse this effect. Last, we examined whether KLK8‐PEBP1 complexation can suppress ACh production in SH‐SY5Y cells.
Results: Serpin A3, Serpin B6 and α2M, but not PEBP1 inhibited the activity of KLK8. While the levels of these four inhibitors did not change in human hippocampi, complexation of KLK8 with Serpin A3 and α2M reduced, and with PEBP1 increased over the course of disease. Contrary to humans, mice showed no complexation alterations, but a depletion in Serpin A3 and PEBP1 levels in early stage disease, which could be reversed by KLK8 knockdown. Co‐incubation with serpin A3, B6 or α2M abrogated KLK8‐mediated impairment of glial phagocytosis, and KLK8 presence reduced PEBP1‐based ACh production.
Conclusion: Decreased serpin A3/B6/α2M+KLK8 complexation could be a reason for pathologically elevated KLK8 levels, and increased KLK8+PEBP1 complex formation a reason for ACh decline in AD brain.
PS8‐ND‐A173
MAPT mutation ΔK281 causes genetically determined pick disease
K. Newell 1, M. Schweighauser2, M. Masada‐Suzukake3, T. Klingstedt4, H. Garringer1, R. Vidal1, B. Ghetti1, S. Scheres2, M. Goedert2
1Indiana University, Pathology and Laboratory Medicine, Indianapolis, IN, United States; 2MRC Laboratory of Molecular Biology, Cambridge, United Kingdom; 3Tokyo Metropolitan Institute of Medical Science, Tokyo, Japan; 4Linkoping University, Linkoping, Sweden
Introduction: In sporadic Pick disease (PiD), the inclusions forming the Pick bodies are made of three repeat (3R) tau. By cryogenic electron microscopy (cryo‐EM), the structures of tau filaments from PiD are characterized. They consist of residues K254‐F378 of 3R tau, which are folded differently when compared to tau in Alzheimer disease filaments. PiD associated with a MAPT ΔK280 mutation has been reported. This variant is predicted to lead to the deletion of one of two tandem lysine residues at positions 280 and 281. Current nomenclature convention now refers to this variant as ΔK281.
Objectives: We study two siblings who were diagnosed neuropathologically as having PiD.
Patients and Methods: Two siblings developed dementia in their late 40s and the ΔK281 MAPT mutation was found in both. We used neuropathologic, biochemical, and molecular genetic methods to study post‐mortem brain tissue from the two patients. Tau filaments have been being analyzed by Cryo‐EM.
Results: Severe atrophy of the frontal and temporal lobes, caudate nucleus, and substantia nigra is associated with severe neuronal loss and gliosis. Pick bodies are numerous in frontal and temporal cortices. Using silver methods, they are stained by Bodian and negative by Gallyas. By immunohistochemistry, Pick bodies are immunoreactive for 3R tau, AT8, and PHF‐1 antibodies and negative with 12E8 antibody. Sarkosyl‐insoluble tau consists of 3R only tau. Tau inclusions in astrocytes and oligodendroglia are positive for 3R tau. Cryo‐EM studies show that the tau filament structures are identical to those of the Pick fold found in sporadic Pick disease.
Conclusion: We have established that the MAPT ΔK281 mutation causes PiD and that the neuronal and glial inclusions are composed of 3R tau, including the oligodendroglia of the subcortical white matter. Cryo‐EM studies of the frontal cortex and white matter will firmly establish the structure of tau filaments from these two anatomical areas.
PS8‐ND‐A174
The LifeAfter90 study—2023 report on the neuropathology of an ethnically diverse cohort study of oldest‐old in the United States
B. Dugger 1, L. W. Jin1, K. Ortega1, C. DeCarli2, P. Gilsanz3, D. Mungas2, C. H. Kawas4, M. M. Corrada4, R. Whitmer2,3
1University of California, Davis, Pathology and Laboratory Medicine, Sacramento, CA, United States; 2University of California, Davis, Neurology, Sacramento, CA, United States; 3Kaiser Permanente, Northern California Division of Research, Oakland, CA, United States; 4University of California, Irvine, Neurology, Irvine, CA, United States
Introduction: There is a dearth of studies on neuropathology of ethnoracial diversity oldest‐old decedents; most studies include exclusively non‐Hispanic White decedents.
Objective: Our goal is to characterize neuropathology in a cohort of racially and ethnically diverse oldest‐old decedents.
Methods: The LifeAfter90 study is an ongoing study in the United States on Kaiser Permanente Northern California members, aged 90+ with targeted recruitment across different racial/ethnic groups of persons with no prior dementia diagnosis. Research assessments occur approximately every 6 months with brain donation available to all interested consenting participants. The National Alzheimer's Coordinating Center Neuropathology form v.10 is used to assess neuropathology.
Results: As of January 2023, 304 (40%) were enrolled in autopsy (20% Asian, 18% African American, 17% Latino, 9% multiracial/other, and 36% White participants). Of these, 59 died and neuropathology evaluations were completed. The median age of death was 93 years (range, 90–105), 56% were female. The cohort consisted of 8 Asian, 5 Black, 10 Latino, 31 White, and 5 multiracial/other decedents. At final assessment, 17 participants had dementia (29%), 25 questionable/mild cognitive impairment (42%), and 16 were cognitively normal (27%). Twenty two percent did not have Alzheimer disease (AD), one had no evidence of neurofibrillary tangles (NFT); 27% had Lewy bodies, and 18% had TDP‐43 deposits. High likelihood of AD was infrequent (N = 2). For vascular pathologies, 98% had some level of arteriolosclerosis, 97% had atherosclerosis, 70% had cerebral amyloid angiopathy, and 26% had at least one old microinfarct. The proportion of demented persons tended to increase with increasing pathology severity especially for AD.
Conclusions: This diverse cohort of oldest‐old individuals reveal numerous brain pathologies are present with advanced age. Future analyses will investigate their role with cognitive impairment.
PS8‐ND‐A175
Inconsistent cytopathological distinction between astrocytic plaques and tuft‐shaped astrocytes along their morphological spectrum—A neuropathology based inter‐rater study
T. Uchihara 1,2,3, E. Yasuda3, S. Toru1, G. G. Kovacs4, C. Duyckaerts5, A. Rosemuller6, E. Gelpi7, S. Forrest4, K. Hirokawa1, T. Yokota3
1Nitobe Memorial Nakano General Hospital, Tokyo, Japan; 2Tokyo Metropolitan Institute of Medical Science, Tokyo, Japan; 3Tokyo Medical and Dental University, Neurology and Neurological Science, Tokyo, Japan; 4Toronto University, Laboratory Medicine and Pathobiology, Toronto, Canada; 5Hôpital de La Salpêtrière, Laboratoire de Neuropathologie Escourolle, Paris, France; 6Amsterdam UMC, Pathology, Amsterdam, Netherlands; 7Klinischen Institut für Neurologie der Medizinischen Universität Wien, Klin. Abt. für Neuropathologie und Neurochemie, Wien, Austria
Clinical distinction between corticobasal degeneration (CBD) and progressive supranuclear palsy (PSP) is sometimes difficult. However, their pathological distinction has been considered to be always possible based mainly on the distinct morphology of astrocytes: tuft‐shaped astrocytes (TAs) for PSP and astrocytic plaques (APs) for CBD. Current diagnostic framework is based on the assumption that TAs and APs are consistently distinguishable and never coexist in the same brain. However, it is not clear how TAs and APs are distinguished by different neuropathologists. Independent 200 images of Gallyas‐positive astrocytes from the motor cortex of four cases of PSP/CBD were presented for possible distinction to five authority neuropathologists, blinded to clinical and pathological diagnoses. Each image was independently rated into +2:TA; +1:TA‐like; 0:unclassifiable; −1:AP‐like; −2:AP. Typical TAs rated as +2 or typical APs rated as −2, as agreed by five neuropathologists, were limited. Surprisingly, some images were rated as +2:TA by some and rated −2:AP by others. Such instability in cytopathological recognition may be related to the Gestalt nature of image recognition, differently black‐boxed in each neuropathologist. Even though, k‐means method enabled to sort these data into three clusters: TA, AP and mixed clusters, each containing unclassifiable images. In a case with clinical diagnosis of PSP/CBD with TA or TA‐like lesions, two out of the five neuropathologists recognized AP or AP‐like lesions as well, which may complicate the case diagnosis in the current framework. Although the target images were stable and objective, their recognition and interpretation were unstable and could be subjectively influenced by internal Gestalt, black‐boxed inside the examiner. An operational protocol, not influenced by the internal Gestalt, is necessary to reach an objective consensus to distinguish TA/AP and PSP/CBD.
PS8‐ND‐A176
Autopsy case of corticobasal degeneration with 3‐repeat tau accumulation in the precentral gyrus, basal ganglia, substantia nigra and locus coeruleus
H. Shintaku 1
1Tokyo Medical and Dental University, Pathology, Bunkyo‐ku, Tokyo, Japan
Background: Corticobasal degeneration (CBD) is characterized by the accumulation of 4‐repeat tau (4R tau). We report an atypical case diagnosed pathologically as CBD with accumulation of 3‐repeat tau (3R tau) in the precentral gyrus, basal ganglia, and brainstem.
Case: The patient became aware of difficulty in lifting the left leg at the age of 58, and subsequently developed myoclonus‐like involuntary movements in the left toe. The symptoms progressed to involve the entire left lower limb, and at the age of 60, spasticity was observed in both the left upper and lower limbs. MRI of the head revealed atrophy with asymmetry in the frontal lobe. Based on the findings of decreased cortical blood flow in the right dominant parietal lobe on SPECT, a diagnosis of corticobasal syndrome was made. At the age of 62, the patient experienced rigidity in the left upper limb. By the age of 63, the patient became bed rest. At the age of 64, the patient started experiencing hallucinations. The patient experienced recurrent aspiration pneumonia, and ultimately passed away at the age of 67.
Pathological findings: Ballooned neurons and astrocytic plaques were observed in the precentral gyrus of the cerebral cortex. Neuronal loss was noted in the putamen, pallidum, and subthalamic nucleus. Depigmentation was observed in the cerebellar substantia nigra. Accumulation of 4R tau was observed in degenerated areas. Accumulation of 3R tau was observed in the precentral gyrus and basal ganglia of cerebral cortex, substantia nigra, and locus coeruleus. The pathology of Alzheimer's disease (AD) was mild, and there was little accumulation of 3R tau in the hippocampus.
Discussion: Accumulation of 3R tau in CBD has been reported in cases where there is coexistence with the pathology of AD. In this case, the pathology of AD was mild, and the prominent accumulation of 3R tau in the precentral gyrus may be based on mechanisms distinct from the pathology of AD, suggesting a unique case.
PS8‐ND‐A177
Tau pathology in limbic predominant neuronal inclusion body disease—A new 4R tauopathy
B. Ghetti 1, Y. Shi2, W. Zhang2, Y. Yang2, A. Murzin2, H. Garringer1, R. Vidal1, M. Goedert2, S. Scheres2
1Indiana University, Pathology and Laboratory Medicine, Indianapolis, IN, United States; 2MRC, LMB, Cambridge, United Kingdom
Introduction: 4R tauopathies are forms of lobar degeneration (FTLD) characterized by the presence of tau inclusions in neurons and glia. Progressive supranuclear palsy (PSP) is the most frequently diagnosed 4R tauopathy; atypical forms of PSP have unusual clinical and neuropathologic features.
Objectives: Analysis of the clinical and neuropathologic phenotypes associated with a novel tau filament structure of an atypical case of PSP.
Patients and Methods: A 66‐year‐old woman was diagnosed as having FTD with a predominant frontal presentation and parkinsonism. We used neuropathologic, biochemical, and molecular genetic methods to study the patients post‐mortem brain tissue. Tau filaments were analyzed by Cryo‐EM. We determined structures, with resolutions of up to 2.7 Å, of tau filaments from the temporal cortex.
Results: In limbic areas and other brain regions, abundant spherical neuronal inclusions are stained using the Gallyas silver method, basophilic by hematoxylin and eosin and are 4R tau immunopositive using RD4 antibody. Globular glial tau inclusions are occasionally seen. By immunoblot analysis, hyperphosphorylated full‐length tau (64 and 68 kDa) and C‐terminal fragments (33 and 37 kDa) are detected in sarkosyl‐insoluble fractions from the frontal cortex using the antibody T46. By cryo‐EM, a novel tau fold is seen, which has similarities to the folds found in PSP and glial globular tauopathies (GGT) and is identified as GGT‐PSP‐Tau (GPT) fold. Two types of GPT filaments are present: type 1 filaments comprise a single protofilament; type 2 filaments pack two protofilaments.
Conclusion: This case is clinically different from PSP. Pathologically, the relevant differences from PSP are the abundant spherical, 4R tau‐immunoreactive, basophilic neuronal inclusions in limbic and other brain regions. We therefore name this disease Limbic Predominant Neuronal Inclusion Body 4R Tauopathy (LNT). Additional cases of LNT remain to be identified.
PS8‐ND‐A178
Cell‐specific MAPT gene expression is preserved in neuronal and glial tau cytopathologies in progressive supranuclear palsy
S. Forrest 1, S. Lee1, I. Martinez‐Valbuena1, V. Sackmann1, J. Li1, L. Ittner2, A. E. Lang1, G. G. Kovacs1
1University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada; 2Macquarie University, Dementia Research Centre, Sydney, Australia
Introduction: Tau, a microtubule‐associated protein encoded by the MAPT gene, has well‐known neuronal functions. In tau‐related neurodegenerative diseases, there is active debate whether there is uptake and internalisation of tau by glial cells, or whether glia produce and fibrillize tau independently, without an external source. Furthermore, there is a paucity of data on whether fibrillar tau in neurons compromise MAPT transcription.
Objectives: To map and quantify MAPT expression across different cell types and brain regions, and evaluate whether tau cytopathology affects MAPT expression in progressive supranuclear palsy (PSP).
Materials and Methods: Using RNAscope combined with immunofluorescence (AT8) and single‐nuclear RNAseq, this study systematically mapped and quantified MAPT expression across different cell types and brain regions in controls (n = 3), and evaluated whether tau cytopathology affects MAPT expression in PSP (n = 3). This was complemented with spatial transcriptomics in the motor cortex of a single PSP case to evaluate tissue distribution of MAPT transcripts.
Results: MAPT transcripts were the highest in neurons followed by oligodendroglia and astrocytes. MAPT transcripts varied between brain regions and within each cell type, likely reflecting biological variability between neuronal and glial subpopulations. In PSP, the presence of MAPT transcripts were preserved in cells that contained phosphorylated‐tau inclusions, including neurofibrillary tangles, oligodendroglial coiled bodies, and tufted astrocytes.
Conclusion: Rather than tau being solely taken up from neurons, this study supports the notion that glial cells express MAPT, serving as a cellular pool for local protein production that can potentially be phosphorylated and fibrillized into pathological inclusions. This study emphasises that tau cytopathology does not compromise MAPT gene expression in PSP and argues against a complete loss of tau protein expression as a pathogenic component.
PS8‐ND‐A179
TDP‐43 forms amyloid filaments with a distinct fold in the brains of GRN mutation carriers
B. Ghetti 1, D. Arseni2, R. Chen2, A. Murzin2, S. Peak‐Chew2, H. Garringer1, K. Newell1, F. Kametani3, A. Robinson4, R. Vidal1, L. Cracco1, M. Hasegawa3, B. Ryskeldi‐Falcon2
1Indiana University, Pathology and Laboratory Medicine, Indianapolis, IN, United States; 2MRC, LMB, Cambridge, United Kingdom; 3Tokyo Metropolitan Institute of Medical Science, Department of Brain and Neurosciences, Tokyo, Japan; 4School of Biological Sciences, Division of Neuroscience, Manchester, United Kingdom
Introduction: A causal role for transactive response DNA binding protein 43 kDa (TDP‐43) assembly in neurodegeneration is evidenced by dominantly inherited missense mutations in TARDBP, the gene encoding TDP‐43. In patients with Granulin (GRN) mutations, frontotemporal lobar degeneration (FTLD) is associated with TDP‐43 pathology.
Objectives: To determine the disease‐associated post‐translational modifications and assembly structures of TDP‐43 in patients with GRN mutations.
Patients and Methods: Tissue from the frontal cortex of three GRN mutation carriers was studied. The patients presented with non‐fluent variant primary progressive aphasia. All individuals had normal C9orf72 hexanucleotide repeat numbers. Post‐mortem brain tissue from these patients was used for neuropathology, biochemistry, genetic sequencing, mass spectrometry and cryogenic electron microscopy (cryo‐EM).
Results: Neuropathology revealed that the TDP‐43 inclusions corresponded to FTLD‐TDP Type A. TDP‐43 filaments were observed by immuno‐electron microscopy. Mass spectrometry revealed disease‐associated post‐translational modifications of TDP‐43, including phosphorylation and N‐terminal acetylation, as well as two new modifications, citrullination and mono‐methylation of arginine 293. Cryo‐EM showed that the TDP‐43 filaments have a new fold resembling a chevron badge, that was the same in all individuals, suggesting that this fold characterizes GRN mutation carriers and FTLD‐TDP Type A.
Conclusion: The structures and post‐translational modifications of assembled TDP‐43 in FTLD caused by GRN mutations are reported for the first time. The amyloid filament structures differ from those found in individuals affected by ALS and FTLD‐TDP Type B, establishing that distinct filament folds of TDP‐43 characterize different neurodegenerative conditions.
PS9‐ND‐A180
NOTCH2NLC GGC repeat expansion causes retinal pathology of NIID patients
J. Sone 1,2,3, S. Ueno4, A. Akagi1, H. Miyahara1, C. Tamai1, Y. Riku1, H. Yabata1, R. Koizumi1, Y. Hashizume5, G. Sobue6, M. Yoshida1, Y. Iwasaki1
1Aichi Medical University, Institute for Medical Science of Aging, Nagakute, Japan; 2National Hospital Organization Suzuka National Hospital, Neurology, Suzuka, Japan; 3Nagoya City University Graduate School of Medical Sciences, Neurology, Nagoya, Japan; 4Hirosaki University, Ophthalmology, Hirosaki, Japan; 5Fukushimura Hospital, Choju Medical Institute, Toyohashi, Japan; 6Aichi Medical University, Nagakute, Japan
Neuronal intranuclear inclusion disease (NIID) is a progressive neurodegenerative disease that is characterized by eosinophilic hyaline intranuclear inclusions in neuronal and somatic cells.A wide range of clinical manifestations of NIID have been reported, and they are said to be mainly associated with dementia. in 2019, expanded GGC repeats in the NOTCH2NLC gene were reported as the cause of both the sporadic and familial NIID. The retinal pathology of genetically confirmed neuronal intranuclear inclusion disease (NIID) is yet unknown. We report the ocular findings of NIID patients with NOTCH2NLC GGC repeat expansion to investigate the pathology of retinopathy. All NIID patients were diagnosed by skin biopsy and NOTCH2NLC GGC repeat analysis. The histopathology of the retina was studied on autopsy samples with immunohistochemistry. All patients had the GGC repeat expansion in the NOTCH2NLC gene. Two patients were legally blind and had been diagnosed with retinitis pigmentosa prior to the diagnosis of NIID, and assessed with whole exome sequencing to rule out comorbidity with other retinal diseases. The histopathology of autopsy samples showed diffusely scattered intranuclear inclusions throughout the retina from the retinal pigment epithelium to the ganglion cell layer, and optic nerve glial cells. And severe gliosis was observed in retina and optic nerve. The NOTCH2NLC GGC repeat expansion causes numerous intranuclear inclusions in the retina and optic nerve cells and gliosis. Visual dysfunction could be the first sign of NIID. We should consider NIID as one of the causes of retinal dystrophy and investigate the GGC repeat expansion in NOTCH2NLC.

FIGURE 1.

FIGURE 2.
PS9‐ND‐A181
Alpha‐Synuclein pathology in the enteric nervous system is a potential biomarker for Parkinson's disease
A. Emmi 1, M. Sandre1, F. P. Russo2, S. Edoardo2, G. Tombesi3, F. Garrì1, M. Campagnolo1, M. Carecchio1, R. Biundo1, G. Cosco1, A. Tushevski1, V. Macchi1, A. Porzionato1, R. De Caro1, L. Bubacco3, P. Piero4, G. G. Kovacs5, A. Antonini1
1University of Padova, Department of Neuroscience, Padova, Italy; 2University of Padova, Department of Surgery, Oncology and Gastroenterology, Padova, Italy; 3University of Padova, Department of Biology, Padova, Italy; 4University of Bologna, Department of Biomedical and Neuromotor Sciences, Bologna, Italy; 5University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada
Background: The role of the gut‐brain axis has been recently highlighted as a major contributor to Parkinson's disease (PD) physiopathology, with numerous studies investigating bidirectional transmission of pathological protein aggregates, such as α‐synuclein (αSyn). However, the extent and the characteristics of pathology in the enteric nervous system (ENS) have not been fully investigated.
Objectives: We characterized αSyn pathology, glial responses and immune‐cell populations in duodenum biopsies of PD patients by employing topography‐specific sampling and conformation‐specific αSyn antibodies.
Methods: We examined 18 patients with advanced PD who underwent Duodopa Percutaneous Endoscopic Gastrostomy and Jejunal Tube (PEG‐J) procedure, 10 untreated patients with early PD (disease duration <5 years), as well as 18 age‐ and sex‐matched healthy control subjects undergoing routine diagnostic endoscopy. A mean of 4 duodenal wall biopsies were sampled from each patient. Immunohistochemistry was performed for anti‐aggregated αSyn (5G4), enteric glial markers (GFAP, S100B, SOX10) and immune‐population markers followed by morphometrical‐semi‐quantitative analysis.
Results: Immunoreactivity for aggregated αSyn was identified in all PD patients (early and advanced) and colocalized with neuronal marker β‐III‐tubulin. Evaluation of enteric glia cells revealed an increased size and density when compared with controls, suggesting reactive gliosis. Similarly, increased T and B lymphocyte densities, as well as higher expression of HLA‐DR, was detected in the gut of PD patients.
Conclusions: We found evidence of synuclein pathology and gliosis in the duodenum of PD patients including early de novo cases. Future studies are required to evaluate how early in the disease process duodenal pathology occurs and its possible contribution to levodopa effect in chronic patients.
PS9‐ND‐A182
Relation between clinical findings and progression of cerebral cortical pathology in sporadic Creutzfeldt–Jakob disease
Y. Iwasaki 1, A. Akagi1, Y. Riku1, J. Sone1, H. Miyahara1, M. Yoshida1
1Institute for Medical Science of Aging, Aichi Medical University, Department of Neuropathology, Nagakute, Japan
In our pathologic observation of the cerebral cortex including the neocortex, hippocampus, and limbic cortex in 43 Japanese patients with MM1‐type sporadic Creutzfeldt–Jakob disease, the earliest pathologic finding was spongiform change and next was gliosis. Subsequently, neuropil rarefaction appeared, followed by neuron loss. On the basis of these observations, we propose the following cortical pathologic staging: Stage I, spongiform change; Stage II, hypertrophic astrocytosis; Stage III, neuropil rarefaction; Stage IV, neuron loss; Stage V, status spongiosus; and Stage VI, large cavity formation. We also suggest a more simple staging classification: Stage I and II, mild; Stage III and IV, moderate; and Stage V and VI, severe involvement. Based on statistical analysis of the cases, strong correlation coefficients were obtained between the neocortical and limbic pathologic stage and both total disease duration and brain weight. We estimated that the first observation times of cortical hyperintensity on diffusion‐weighted images of magnetic resonance imaging, myoclonus, and periodic sharp wave complexes on the electroencephalogram approximately correspond to the early phase of Stage II of the neocortex. The time to reach the akinetic mutism state approximately corresponds to the middle phase of Stage II of the neocortex. Therefore, we think that approximate clinical manifestations at death, total disease duration, and brain weight can be estimated according to the pathologic stage of the neocortex or limbic cortex. Panencephalopathic‐type pathology appeared approximately 12 months after disease onset, and this time approximately corresponds to the middle phase of Stage III of the neocortex.

FIGURE 1.
PS9‐ND‐A183
Regional variability of α‐synuclein inclusion size in multiple system atrophy
A. Kim 1,2, G. G. Kovacs1,2,3,4,5, S. Forrest2,3
1Laboratory Medicine & Pathobiology, University of Toronto, Toronto, Canada; 2Tanz Centre for Research in Neurodegenerative Diseases, University of Toronto, Toronto, Canada; 3Krembil Brain Institute, University Health Network, Toronto, Canada; 4Edmond J. Safra Program in Parkinson's Disease and the Morton and Gloria Shulman Movement Disorders Clinic, Toronto Western Hospital, Toronto, Canada; 5Laboratory Medicine Program, University Health Network, Toronto, Canada
Introduction: Multiple system atrophy (MSA) patients show variable duration of illness and distinct constellations of clinical symptoms and pathological phenotypes, suggestive of different pathological α‐synuclein (αSyn) strains. Neuropathologically, MSA is characterized by accumulation of αSyn in oligodendrocytes, termed glial cytoplasmic inclusions (GCI). GCIs are found in region‐specific brain regions and their size varies between brain regions and patients.
Objective: This study quantified the size of GCIs in MSA patients and correlated regional inclusion size with clinicopathological phenotypes.
Materials and Methods: The putamen and cerebellar white matter from 16 MSA cases were immuno‐stained with the disease‐specific αSyn (clone 5G4) antibody. Sections were scanned using Huron TissueScope™ and images pre‐processed using Photoshop. Oligodendrocytes with 5G4‐immunoreactive inclusions were optically dissected and inclusion size was evaluated using novel computer‐based algorithms developed using Image J.
Results: The size of GCIs significantly varied between cases (n = 16; p < 0.0001) and brain regions (p < 0.0001). Comparing brain regions in each case, GCIs were larger in the cerebellar white matter than GCIs in the putamen in 12 cases. In two cases, the inclusion size was larger in the putamen than GCIs in the cerebellum. Similar GCI size was found in the putamen and the cerebellum in two cases.
Conclusion: We developed a novel computer‐based method to measure the size of αSyn inclusions in MSA that is easily accessible and reproducible. Our observations on the variability of GCI size between brain regions and cases, support the notion of distinct MSA subtypes. Our study provides a first step to developing AI‐based inclusion size evaluation strategies for large scale comparative studies.
PS9‐ND‐A184
Impaired synaptic gene expression networks in patients with alpha‐synuclein and tau co‐pathology
F. L. Struebing 1,2, J. Widmann1, T. De Vecchi1, V. C. Ruf1, O. Windl1, J. Herms1,2,3
1University of Munich, Center for Neuropathology and Prion Research, Munich, Germany; 2German Center for Neurodegenerative Diseases (DZNE), Munich, Germany; 3Munich Cluster for Systems Neurology, Munich, Germany
Introduction: The most commonly occurring co‐pathology among all neurodegenerative diseases upon autopsy are concomitant deposits of misfolded alpha‐synuclein (SNCA) and tau (MAPT) aggregates. While studies have demonstrated adverse interactions of SNCA and MAPT on the protein level, little is known about the genomic networks leading up to this phenomenon.
Objectives: We hypothesize that MAPT and SNCA act synergistically on gene expression networks specifically related to synaptic pathology.
Materials and Methods: Gene expression assays and immunohistochemistry were performed on human iPSC cultures differentiated to neurons and organoids with a cortical phenotype. Post‐mortem human brains from patients with “pure” MAPT and MAPT+SNCA pathology clinically diagnosed with dementia (Braak&Braak Stage 6, APOE3/4 heterozygotes) underwent single‐nucleus transcriptome sequencing.
Results: In human neurons and organoids, SNCA overexpression led to increased MAPT transcript levels and differences in synaptic gene and protein expression. Single‐nucleus transcriptome sequencing revealed a differentially expressed cluster whose ontological annotation showed striking similarities to dopaminergic neurons and where differentially expressed transcripts localized to the synapse. Functional annotation of this cluster demonstrated suppressed synaptic translation in MAPT+SNCA patients, reminiscent of what we and others have found in brains of mice and synucleinopathy patients prior to the occurrence of clinical symptoms. Bioinformatic analysis suggested a network of small RNAs to be involved in this process, which were also found to be differentially expressed in human neurons and organoids upon SNCA overexpression.
Conclusion: Our results suggest that SNCA and MAPT are part of a genetic network where the overexpression of SNCA drives the development of synaptic deficits by increasing MAPT transcript levels, which is mediated in part by regulatory RNAs.
PS9‐ND‐A185
Original histological phenotype after the experimental transmission to primate of an unusual human prionopathy (VPSPr)
J. Mikol 1, J. Delmotte1, W. Zou2,3, J. P. Deslys1, E. Comoy1
1Commissariat à l'energie Atomique, Institut François Jacob/Prion research Group, Fontenay‐aux‐Roses, France; 2Case Western Reserve University School of Medicine, Department of Pathology, Cleveland, OH, United States; 3Institute of Neurology, Nanchang, China
VPSPr, a novel rare human prion disease described in 2010 is characterized by the accumulation of abnormal PrPd with a limited resistance to proteolysis. It showed uncertain infectivity in transgenic mouse models. Recent publications report VPSPr cases with different unevocative clinical pictures, leading the authors to consider that VPSPr might be underestimated. One of our macaques intracerebrally inoculated with a brain sample derived from a VPSPr patient (Met/Val at codon 129) exhibited after 8.5 years of silent incubation several episodes of self‐aggression first focused on his left leg, which extended to the whole hindquarters, and abnormalities of both hind limbs sensitive conduction. We performed euthanasia 4 months later for humane reasons and examined brain tissues with histological techniques. Pathological examination revealed a spongiform change decreasing from the frontal to the occipital cortex, also present in the thalamus, the basal ganglia, the hippocampus, mild brainstem and spinal cord, accompanied with a massive neuronal vacuolation and reactive astrocytosis. Purkinje cells were rarefied and vacuolated. Abnormal PrPd deposition was present as synaptic deposits mixed with some mini‐aggregates of PrPd diffused in the tissue or packed in small fussy unlimited area of variable intensity, appearing as pre‐plaques. These lesions, never previously observed in primates exposed to other prion strains, were mainly observed in the insula and the frontal cortex but were absent in the thalamus, the basal ganglia and the hippocampus. Furthermore, we observed massive Ab deposits, but not in the hippocampus except the subiculum, not co‐localized with PrPd. In contrast, a two‐times older animal had three‐times less deposits. The original disease phenotype observed in this primate will be discussed and compared to the expressions of VPSPr in humans, and other prion diseases in the macaque model.
PS9‐ND‐A186
Dynamic change of synuclein transcription during Lewy body formation
T. Kon 1,2, S. Forrest3, S. Lee3, I. Martinez‐Valbuena3, J. Li3, A. E. Lang3, G. G. Kovacs1,4
1University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada; 2Hirosaki University, Neurology, Hirosaki, Japan; 3University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada; 4University Health Network, Laboratory Medicine Program, Toronto, Canada
Introduction: Lewy body disease (LBD) is characterized by the accumulation of α‐synuclein (α‐syn) encoded by SNCA. α‐Syn is conformationally changed to a misfolded form that recruits the monomeric form of α‐syn as the seed in the diseased state. Point mutations and multiplication of SNCA lead to familial Parkinson's syndrome and a gene‐dosage effect has been hypothesized. It is unclear whether SNCA transcripts are preserved or lost during Lewy body (LB) formation.
Objectives: To investigate SNCA transcription during LB formation.
Materials and Methods: We measured the volume density of SNCA RNA transcripts in the substantia nigra and amygdala in LBD (n = 5) using a novel in‐situ hybridization technique, RNAscope combined with immunofluorescence for disease‐associated α‐syn protein. In addition, we immunostained cases of LBD and controls (n = 5, each group) using antibodies detecting the pan‐α‐syn and/or disease‐associated α‐syn.
Results: The volume density of SNCA RNA transcripts is preserved in neurons with α‐syn protein pre‐aggregates as compared to neurons without α‐syn inclusions. However, we detected a gradual and significant decrease in neurons with compact α‐syn protein inclusions followed by those with classical Lewy bodies. Immunostaining for pan α‐syn showed similar patterns in controls and LBD cases while only pathological α‐syn was found in LBD cases. Low levels of SNCA transcription were found in astrocytes with or without α‐syn protein.
Conclusion: We have shown that SNCA transcription is preserved in neurons with disease‐associated α‐syn protein deposits. When Lewy bodies are formed, SNCA transcription decreases supporting the notion that these cells have disrupted neuronal function. This study provides important insights into the pathogenesis of the development and progression of LBD.
PS9‐ND‐A187
Qualitative and quantitative alterations of synaptotagmin 13 in synucleinopathies
Y. Miki 1, M. Tanaka1, S. Shimoyama1, A. Nakahara1, A. Kakita1, K. Wakabayashi1
1Hirosaki University, Department of Neuropathology, Hirosaki, Japan
Introduction and Objectives: Endocytosis and exocytosis may be a key mechanism for the spread of pathogenic α‐synuclein in the brains of patients with synucleinopathies (Parkinson's disease [PD], dementia with Lewy bodies [DLB] and multiple system atrophy [MSA]). Synaptotagmins are a family of 17 membrane trafficking proteins involved in the regulation of neurotransmitter release and exocytosis. However, little is known about the involvement of synaptotagmin 13 (SYT13) in the pathogenesis of synucleinopathies. In the present study, we aimed to investigate the qualitative and quantitative alterations of SYT13 in synucleinopathies.
Materials and Methods: We performed immunohistochemistry, proximity ligation assay, RNA scope and immunoblotting using the brains of patients with PD (N = 11), DLB (N = 16) and MSA (N = 14) and controls (N = 23).
Results: Immunohistochemistry showed incorporation of SYT13 into Lewy bodies and glial cytoplasmic inclusions, the pathological hallmarks of PD and DLB, and MSA, respectively. Proximity ligation assays also revealed protein‐protein interactions of SYT13 with not only endogenous, but also phosphorylated α‐synuclein in Lewy bodies and glial cytoplasmic inclusions. SYT13 mRNA levels were significantly reduced in the substantia nigra and pons of PD and MSA compared with controls. However, immunoblotting confirmed higher protein levels of SYT13 in the temporal lobes of DLB and MSA than in controls. In addition, the smear band of SYT13 was found in the insoluble fraction, corresponding to that of phosphorylated α‐synuclein.
Conclusion: Mislocalisation and accumulation of SYT13 may be common features in the pathogenesis of synucleinopathies. The results of the present study support the propagation of pathogenic α‐synuclein via endocytosis and exocytosis. Further study is necessary to clarify how pathogenic α‐synuclein can be spread via SYT13.
eP‐ND‐A188
Kallikrein‐8 cleaves APOE4, but not APOE2 and thereby affects Alzheimer's pathology
K. Groll 1, P. Pereira de Almeida1, C. Bandowski1, M. Farhat1, N. Macha1, M. Knoll1, A. Herring1, K. Keyvani1
1University Hospital Essen, Institute of Neuropathology, Essen, Germany
Introduction: Apolipoprotein E (APOE) is the most prominent risk gene for Alzheimer's disease (AD). APOE2 isoform protects against and APOE4 increases the risk for AD. The reason for this blatant functional difference remains unknown. Previous work in our lab identified kallikrein‐8 (KLK8) as a potential upstream mover in the pathogenesis of AD and as a possible therapeutic target. Here we investigate the interaction between KLK8 and APOE isoforms.
Objectives: To determine the capacity of KLK8 in degrading APOE2, 3, 4, and to assess the functional consequences of this interaction on APOE+Aβ complexation and Aβ metabolism.
Materials and Methods: Interaction of KLK8 and APOE and its effect on APOE+Aβ complexation were investigated in cell free in vitro assays, in hippocampus and serum of AD patients with different APOE genotypes and in TgCRND8 mice with or without mKlk8 knockdown in different disease stages by Western blot. The effect on Aβ metabolism was determined in primary murine glia.
Results: KLK8 cleaved rapidly both recombinant and native brain and blood APOE4, while fragmentation of APOE3 and APOE2 was minor or completely absent. Similarly, APOE fragmentation (APOEΔ) in brain and blood of patients was highest in APOE4 carriers. Moreover, APOEΔ rose in late stage disease. Comparable results regarding APOE were obtained in mice. Intriguingly, APOEΔ was lowered to control levels following mKlk8 knockdown. APOE+Aβ complexation was decreased in brain of AD patients in late stage disease, especially in APOE4‐associated genotypes. Aβ metabolism in primary glia was not altered by addition of APOE2 or E4 alone, but was markedly disturbed when co‐incubated with APOE4+KLK8.
Conclusion: The higher affinity of KLK8 to degrade APOE4 and its inability to breakdown APOE2 might explain why the first one is a risk for and the latter protective against AD. It seems that the interaction between KLK8 and APOE4 but not APOE4 per se is responsible for the destructive effects in AD.
eP‐ND‐A189
Dysregulation of the kallikrein‐kinin‐system in Alzheimer's disease is mediated by kallikrein‐8
K. Groll 1, P. Pereira de Almeida1, I. Farid1, N. Macha1, M. Knoll1, A. Herring1, K. Keyvani1
1University Hospital Essen, Institute of Neuropathology, Essen, Germany
Introduction: Dysregulation of the kallikrein‐kinin‐system (KKS) boosts inflammation and worsens Alzheimer's disease (AD) pathology. Our lab was the first to show elevated levels of the serine protease Kallikrein‐8 (KLK8) in blood of AD and MCI due to AD patients. Whether this pathological alteration contributes to dysregulation of the KKS, and if so with which after‐effects is yet unknown.
Objectives: To determine the level of bradykinin (BK), bradykinin receptor B1 and B2 (B1R/B2R) in vivo and to assess the capability of KLK8 to increase BK levels in human plasma.
Materials and Methods: ELISA and Western blotting were used to quantify the expression of BK, B1R and B2R. Analysis was conducted in hippocampus and plasma in different disease stages in AD patients or in TgCRND8 mice with or without mKlk8 knockdown. The effect of KLK8 on BK synthesis in human plasma was measured by ELISA.
Results: BK and B1R levels were increased in brain and blood of AD patients and TgCRND8 mice in late stage disease. No significant changes were observable for B2R expression. Increased BK and B1R levels were lowered back to control levels in TgCRND8 mice following mKlk8 knockdown, while addition of recombinant KLK8 to human plasma elevated BK levels.
Conclusion: Pathologically increased KLK8 levels in blood and brain might be a reason for KKS dysregulation in AD.
eP‐ND‐A190
Heterogeneity of medullary pathology in multiple system atrophy
C. Rowe 1, M. Wojewska1, S. Gentleman1
1Imperial College London, Department of Brain Sciences, London, United Kingdom
Introduction: Multiple system atrophy (MSA) is a rare neurodegenerative disease characterised by the presence of widespread glial cytoplasmic inclusions of α‐synuclein (α‐syn). Based on the predominant motor symptoms, there are two clinical subtypes, MSA‐P (parkinsonian‐type) and MSA‐C (cerebellar‐type). Autonomic symptoms, such as orthostatic hypotension (OH) and cardiovascular dysfunction, are also commonly seen. The precise pathology underlying these symptoms remains unclear but the inferior olivary nucleus and ventrolateral medulla (VLM) have been implicated.
Objectives: To investigate whether the extent and localisation of α‐syn pathology and neuronal loss in the medulla correlates with motor subtypes and presence of autonomic symptoms.
Materials and Methods: Immunostaining was conducted on sections of medulla from 30 cases selected from Parkinson's UK Brain Bank (10 MSA‐C, 10 MSA‐P, 10 PD) using antibodies against α‐syn, tyrosine hydroxylase (TH), tryptophan hydroxylase (TpH) and choline acetyl transferase (ChAT). QuPath (v0.3.2) software was used to quantify stained pathology.
Results: Significantly more α‐syn pathology was seen in the inferior olive in MSA‐C than in MSA‐P. No significant difference was seen in the amount of α‐syn pathology in the VLM in cases with and without OH. However, significantly fewer catecholaminergic and serotonergic neurons were seen in the VLM of MSA cases when compared to PD.
Conclusions: Differences in the distribution and severity of pathology in the medulla correlate with clinical phenotypes in MSA and PD.
eP‐ND‐A191
Microglial LRRK2‐mediated NFATc1 attenuates α‐synuclein immunotoxicity in association with CX3CR1‐induced migration and the lysosome‐initiated degradation
L. Feng 1, J. Zheng1, Y. Yan1, X. Pan1
1Fujian Medical University Union Hospital, Department of Neurology, Center for Cognitive Neurology, Fuzhou, China
Question: Synucleinopathies refer to a range of neurodegenerative diseases caused by abnormal α‐synuclein (α‐Syn) deposition, including Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). Their pathogenesis is strongly linked to microglial dysfunction and neuroinflammation, which involves the leucine‐rich‐repeat kinase 2 (LRRK2)‐regulated nuclear factor of activated T‐cells (NFAT). Of the NFAT family, NFATc1 has been found to be increasingly translocated into the nucleus in α‐syn stimulation. However, the specific role of NFATc1‐mediated intracellular signaling in PD remains elusive in regulating microglial functions.
Methods: In the current study, we crossbred LRRK2 or NFATc1 conditional knockout mice with Lyz2Cre mice to generate mice with microglia‐specific deletion of LRRK2 or NFATc1, and by stereotactic injection of fibrillary α‐Syn, we generated PD models in these mice.
Results: We found that LRRK2 deficiency enhanced microglial phagocytosis in the mice after α‐Syn exposure and that genetic inhibition of NFATc1 markedly diminished phagocytosis and α‐Syn elimination. We further demonstrated that LRRK2 negatively regulated NFATc1 in α‐Syn‐treated microglia, in which microglial LRRK2‐deficiency facilitated NFATc1 nuclear translocation, CX3CR1 upregulation, and microglia migration. Additionally, NFATc1 translocation upregulated the expression of Rab7 and promoted the formation of late lysosomes, resulting in α‐Syn degradation. In contrast, the microglial NFATc1 deficiency impaired CX3CR1 upregulation and the formation of Rab7‐mediated late lysosomes.
Conclusions: These findings highlight the critical role of NFATc1 in modulating microglial migration and phagocytosis, in which the LRRK2‐NFATc1 signaling pathway regulates the expression of microglial CX3CR1 and endocytic degradative Rab7 to attenuate α‐synuclein immunotoxicity.

FIGURE 1.

FIGURE 2.
eP‐ND‐A192
N‐ and O‐linked sialylation in Alzheimer's disease postmortem brain tissue
C. Fastenau1,2, M. Keating1, S. Hopp2, K. Bieniek 1
1UT Health San Antonio, Pathology and Laboratory Medicine, San Antonio, TX, United States; 2UT Health San Antonio, Pharmacology, San Antonio, TX, United States
Question: We recently observed increase expression of the post‐translational modification sialylation (specifically the α‐2,6 bond) on plaque‐associated microglia of an Alzheimer's disease (AD) mouse model. Based on this observation, we sought to answer the question “what patterns of different N‐ and O‐linked sialylation are observed in human postmortem brain tissue and how could this modification impact the physiology of microglia in AD and related dementias?”
Methods: N‐linked sialylation was assessed through biotinylated sambucus nigra lectin staining. O‐linked sialylation was evaluated using several different histologic stains, namely Alcian blue (AB), periodic acid Schiff (PAS), and high iron diamine (HID), to label carboxylated, neutral, and sulfonated sialic acid residues, respectively. Immunohistochemistry with tau, β‐amyloid, and IBA1 antibodies was performed to visualize AD pathology and microglia. Whole slide images were generated using an Aperio AT2 slide scanner and images were analyzed using ImageScope color deconvolution digital pathology algorithms.
Results: We observed a significant correlation between N‐linked sialylatation and microglia in AD (r = 0.70), but not α‐2,6 sialylation and tau pathology (r = 0.04). O‐linked sialylation stains highlighted plaques labeled with PAS and HID, but not AB, whereas plaque‐associate microglia were reactive for AB and PAS, but not HID.
Conclusions: N‐ and O‐linked sialic acid modification impacts β‐amyloid aggregates and microglia in AD, but not tau pathologic aggregates. AD plaques appear to have O‐linked neutral and sulfinated sialoproteins whereas microglia surrounding aggregates exhibit neutral and acidic sialoproteins. These differences may account for dynamic cell‐cell and cell‐pathology interactions within the plaque microenvironment. Future assessment of O‐acyl sialic acid modifications as well as experimental manipulation of sialic acid residues to measure microglial activity is an area of interest.
eP‐ND‐A193
Progressive supranuclear palsy subtypes in a neuropathology cohort
A. Sieben 1, B. Verbraeken1, M. Ahmed1, V. Capiau2, D. Crosiers3, P. Cras3, M. Lammens1
1Antwerp University Hospital, Pathology, Antwerp, Belgium; 2Leuven University Hospital, Pathology, Leuven, Belgium; 3Antwerp University Hospital, Neurology, Antwerp, Belgium
Introduction: Progressive supranuclear palsy (PSP) is a neurodegenerative disorder, characterized by 4R tau aggregates in subcortical neurons, astrocytes and oligodendroglia. The clinical picture is heterogeneous, varying from the classic Richardson phenotype (PSP‐RS), over atypical parkinsonism (PSP‐P), corticobasal syndrome (PSP‐CBS), progressive gait freezing (PSP‐PGF), cerebellar symptomatology (PSP‐C) to predominant frontal syndromes (PSP‐F) and speech disorders (PSP‐SL). In 2020, Kovacs et al. published a neuropathological staging system distinguishing PSP subtypes based on the spatial and cellular distribution of the tau‐aggregates (Acta Neuropathologica, 2020).
Objectives: The neurobiobank of the Born Bunge Institute (IBB, NBB‐IBB, FA190113) is a neurodegenerative brain biobank with more than 6000 brains. In our study, 48 PSP cases are reassessed based on the findings of Kovacs et al. Next to PSP pathology, other proteinopathies and cerebrovascular pathology are included.
Materials and Methods: The clinical files were reviewed. The brains were reassessed and additional immunohistochemical stainings with antibodies against 3R and 4Rtau, Amyloid β, TDP‐43 and α‐synuclein were performed. Semiquantitative scoring of 4R tau pathology in neurons, astrocytes and oligodendroglia and scoring of cerebrovascular pathology were performed.
Results: Our cohort includes 50% females (n = 24). Mean age of death was 73.0 years. The clinical presentation was 56% PSP‐RS (n = 27), 17% PSP‐P (n = 8), 10% PSP‐F (n = 5), 6% PSP‐CBS (n = 3), 6% PSP‐SL (n = 3), 4% PSP‐C (n = 2). Co‐occurring proteinopathies occurred in 44% of cases (n = 21) including Alzheimer's disease, primary age‐related tauopathy (PART), Lewy body disease, cerebrovascular disease and cerebral amyloid angiopathy.
Conclusion: We present the data of the tau pathology, related to the stages of the PSP tauopathy and to the clinical phenotype. These data are compared with the prementioned study of Kovacs et al.
eP‐ND‐A194
Clinicopathological features of progressive supranuclear palsy with asymmetrical atrophy of the superior cerebellar peduncle
R. Koizumi 1,2, A. Akagi1, Y. Riku1, J. Sone1, H. Miyahara1, F. Tanaka2, M. Yoshida1, Y. Iwasaki1
1Aichi Medical University, Department of Neuropathology, Institute for Medical Science of Aging, Nagakute, Japan; 2Yokohama City University, Department of Neurology and Stroke Medicine, Graduate School of Medicine, Yokohama, Japan
Introduction: It is known that patients with progressive supranuclear palsy (PSP) present with atrophy in the superior cerebellar peduncle (SCP). There have been reports of PSP cases with asymmetrically atrophic SCPs and degeneration of the Guillain–Mollaret triangle.
Objectives: We aimed to identify PSP cases with asymmetrical atrophic SCPs and degeneration of the Guillain–Mollaret triangle from consecutive autopsy cases in the brain bank.
Materials and Methods: We analyzed 48 cases with neuropathologically diagnosed PSP to investigate the clinicopathological asymmetry of brain lesions involving the SCPs. We defined the larger SCP as the side with a larger average width, and we defined the smaller SCP as the side with a smaller average width. The SCP was deemed asymmetrically atrophic if the ratio of the width between the larger and smaller SCP was two or more; a symmetrical SCP had a ratio less than two. The degree of neuronal loss, atrophy/myelination, and tau pathology were evaluated semi‐quantitatively on a 3‐point scale and compared between the two groups.
Results: Among the 48 autopsied patients whose data were included, seven (14.6%) had an asymmetrically atrophic SCP. The width of the smaller SCP was different between the asymmetrical and symmetrical groups (0.5 mm vs. 0.9 mm, p = 0.0146). In the asymmetrically atrophic SCP group, SCP atrophy and neuropathology of the dentate nucleus were worse on the same side. In contrast, the degeneration sides of the red nucleus, central tegmental tract, and inferior olivary nucleus were predominantly opposite to the SCP sides that exhibited increased atrophy.
Conclusion: This study identified cases with an asymmetrically atrophic SCP in a PSP autopsy series. The PSP pathology may spread asymmetrically, consistent with the neuroanatomy of the Guillain–Mollaret triangle.
eP‐ND‐A195
Novel quantitative digital pathology pipeline to map regional misfolded protein pathology in Parkinson's disease
H. R. Nelvagal 1,2, T. Curless1,2, A. Rockliffe1,2, R. Real1, J. Hardy3, H. Morris1, Y. M. Lim3, S. Brandner3, Z. Jaunmuktane1,2
1University College London, Department of Clinical and Movement Neurosciences, London, United Kingdom; 2University College London, Queen Square Brain Bank for Neurological Disorders, London, United Kingdom; 3University College London, Department of Neurodegenerative Diseases, London, United Kingdom
Introduction: The characteristic α‐synuclein inclusions in Parkinson's disease (PD) are variably accompanied with concomitant amyloid‐β plaques and tau neurofibrillary tangles which may influence the rate of dementia progression in PD. However, the extent of misfolded protein pathologies across the brain in PD is not fully described. Current semi‐quantitative assessment schemes are subjective and prone to bias. There is therefore a need to establish novel pipelines for consistent, rapid and scalable quantification of regional misfolded protein pathology.
Objectives: To use machine learning‐based tools for quantitative image analysis on digital whole slide images across multiple brain regions to generate automatically quantified data for further downstream integration with clinical phenotypes, genetic profiles and regional transcriptomic signatures to identify disease subtypes.
Materials and Methods: Digitally scanned regional brain sections stained for alpha‐synuclein, amyloid‐beta and hyperphosphorylated tau from PD and control cases were segmented into regions of interest to quantify the pathology in specific anatomical regions. Using open‐source pathology image analysis software (QuPath), algorithms have been developed for large‐scale high‐throughput quantification of misfolded protein pathology.
Results: We have quantified misfolded protein load across multiple brain regions in over 300 cases. Comparative analyses of these pathologies within the same region and between regions have identified distinct patterns of pathology between different presentations of PD, based on clinical and genetic data.
Conclusion: We report a novel digital pathology pipeline that is reproducible and robust for quantification of misfolded protein pathology in PD. Such an approach can now be further developed to include other pathological markers and established for other disease profiles. Studies to further elucidate the underlying mechanisms with spatial transcriptomic data are ongoing.

FIGURE 1.
eP‐ND‐A196
Intranasal administration of trehalose reduces α‐synuclein oligomers by accelerating aggregate formation in a mouse model of multiple system atrophy
M. Tanaka 1, Y. Miki1, F. Mori1, T. Furukawa2, S. Shimoyama2, Y. Tatara3, K. Wakabayashi1
1Hirosaki University, Neuropathology, Hirosaki, Japan; 2Hirosaki University, Neurophysiology, Hirosaki, Japan; 3Hirosaki University, Stress response science, Hirosaki, Japan
Introduction and Objectives: Abnormal α‐synuclein (Syn) accumulates in the brains of patients with multiple system atrophy (MSA). Because the blood–brain barrier blocks the access of drugs to the brain, neuroprotective drugs have not been developed for the treatment of MSA. Oral administration of trehalose activates the major degradation pathway (autophagy). However, our previous study showed that clearance of abnormal human Syn in the brains of mice expressing A53T Syn was suboptimal when trehalose was administered orally. In the present study, using human Syn‐inducible MSA model mice, we investigated how intranasal administration of trehalose can affect the accumulation of abnormal Syn.
Materials and Methods: We administered trehalose and/or maltose (control) intranasally and orally to the MSA model mice (N = 44, 22–26 weeks old) after human Syn induction. Using these mice, we performed behavioural tests, physiological analyses, immunohistochemistry, proximity ligation assay, immunoblotting and filter trap assay. In addition, we performed an in vitro kinetic assay to investigate the effect of intranasal trehalose treatment on human Syn aggregation.
Results: The MSA model treated with intranasal trehalose reversed memory impairment compared with MSA mice treated with maltose. Contrary to our expectation, immunohistochemistry and Western‐blot analysis showed increased levels of phosphorylated Syn in the brains of trehalose‐treated mice. In addition, an in vitro kinetic assay confirmed that trehalose promoted the formation of Syn aggregates. Notably, proximity ligation assay and filter trap assay revealed that intranasal trehalose treatment decreased soluble Syn oligomers.
Conclusion: Intranasal trehalose treatment may reduce the toxicity of Syn oligomers by accelerating Syn aggregates.
eP‐ND‐A197
Clinical and pathologic spectrum of neurodegeneration with TDP‐43(+) inclusions—ALS, PLS and semantic variant of primary progressive aphasia
S. Bannykh 1, A. Oren1, K. Bannykh1
1Cedars‐Sinai Medical Center, Pathology and Laboratory Medicine, Los Angeles, CA, United States
Introduction: Amyotrophic lateral sclerosis (ALS) and fronto‐temporal dementia (FTD) affected are unified by the presence of altered function and pathologic inclusions containing TAR DNA‐binding protein 43 (TDP‐43). Recently there has been a steady progress in understanding of the molecular role of TDP‐43 in the nuclear processing of RNA, raising hopes for novel therapies.
Objectives: Comparative analysis of distribution of TDP‐43(+) inclusions in patients with progressive lateral sclerosis (PLS), semantic variant of primary progressive aphasia (PPA‐SV) and ALS. Clinical, gross and histopathologic review of cases of PLS and PPA‐SV.
Patients and Methods: Clinical and autopsy findings of 21 cases of ALS, and 1 case of PLS and PPA‐SV each were evaluated for expression of phospho‐TDP‐43. Clone 11‐9 by Cosmo Bio USA was used for IHC analysis followed by morphometric evaluation of a fraction of pTDP‐43‐bearing neurons. The clinical, gross and microscopic presentation of PLS and PPA‐SV cases were illustrated.
Results: Among the cases of ALS all showed pTDP‐43(+) inclusions in the motor neurons of the spinal cord and degeneration of corticospinal tracts. Only one of the ALS cases showed neurofibrillary tangles in motor cortex with no pTDP‐43(+) cortical inclusions. None of the cases showed significant beta amyloid (Aβ) deposits. The case of PLS showed extensive pTDP‐43(+) inclusions in the motor cortex with no concomitant tau staining. The case of PPA‐SV showed striking pTDP‐43(+) inclusions in the neocortices but no tau or Aβ(+) deposits.
Conclusion: Our data confirm that among the TDP‐43(+) diseases the ALS is the predominant. Only 1 of 21 ALS cases showed coexisting tauopathy. In contrast to orderly and progressive expansion of Aβ and tau deposits in Alzheimer's disease, the sites of TDP‐43(+) inclusions retain clinical syndrome‐specific distribution.
eP‐ND‐A198
Clinicopathological characterization and concomitant proteinopathies in ALS patients
E. Stenvall 1, Z. Rohan1, K. Forsberg2, T. Brännström1
1Umeå University, Medical Biosciences, Umeå, Sweden; 2Umeå University, Clinical Sciences, Umeå, Sweden
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative syndrome characterized by progressive loss of motor neurons in the cortex, brainstem and spinal cord. It is estimated that up to 50% of ALS patients show cognitive impairment upon neuropsychological testing, and about 15% fulfill the criteria for frontotemporal lobe dementia (FTD). Recent studies indicate that in many cases of neurodegenerative diseases CNS tissue contain inclusions of several disease‐linked proteins. In this study we investigate if ALS patients have multiple proteinopathies (inclusions of various sort, including SOD1, pTDP‐43, Tau, beta‐amyloid, alfa‐synuclein, FUS, p62 and inclusions containing repeat expansion motifs, primarily dipeptide expansions). In addition, we want to know if a correlation between pathology and phenotype or genotype can be found and to what extent these patients have a correct clinical diagnose. We have a comprehensive collection of autopsy samples where tissue from ALS patients has been collected since 1993. Both sporadic and familial variants with mutations in C9orf72, SOD1, FUS, KIF5A and TBK1 are included. Each patient is clinically and genetically well documented and standardized neuropathological assessment with immunohistochemistry has been performed. In this ongoing work, we found that Alzheimer's disease (AD) in different stages was seen in 56% and α‐synuclein was seen in 12% of all patients. SOD1 inclusions were found in patients with different phenotype or genotype, not just in familial SOD1 patients. One patient revealed to be high grade AD with tau inclusions in spinal motor neurons, mimicking ALS. To conclude, our preliminary results suggest that multiple proteinopathies are common in ALS patients and that neuropathological investigations are important tools for correcting and calibrating clinical diagnoses.
eP‐ND‐A199
ROS attenuates TET2‐dependent ZO‐1 epigenetic expression in cerebral vascular endothelial cells
Y. Liu 1, J. Xiong2, Y. Wang2
1School of Basic Medical Sciences, Fudan University, Department of Pathology, Shanghai, China; 2Huashan Hospital, Shanghai Medical College, Fudan University, Department of Pathology, Shanghai, China
Aims: To investigate whether DNA active demethylase TET regulates the expression of tight junction proteins in endothelial cells of the blood–brain barrier (BBB).
Methods: Correlations between TET2 activity (indicated by its catalytic product 5hmC) and the expression of BBB tight junction proteins were examined in Tet2 knockout mice and post‐mortem human brain tissues. In cultured endothelial cells, the impact of changes of TET activity on the expression of tight junction protein, ZO‐1, was studied. BBB permeability assays were performed in Tet2 knockout mice.
Results: It was found that the level of 5hmC decreased in brain microvascular endothelial cells of aging mice. In Tet2 knockout mice, the level of 5hmC in endothelial cells was weaker and significantly correlated with the reduced expression of tight junction protein ZO‐1. In cultured endothelial cells, H2O2 significantly decreased the expression of 5hmC and ZO‐1. Tet2 knock‐down using siRNA significantly downregulated the expression of ZO‐1 in endothelial cells. hMeChip‐PCR showed that H2O2 decreased the level of 5hmC in the ZO‐1 promoter region, which was rescued by N‐acetyl cysteine (NAC). Consistently, Tet2 knock‐down using siRNA significantly downregulated the level of 5hmC in the ZO‐1 promoter region. It was also found that the level of 5hmC decreased in endothelial cells of aging human brains compared with that of adult brains, and the level of ZO‐1 was positively correlated with that of 5hmC in microvascular endothelial cells.
Conclusions: These findings suggest that TET activity is essential in regulating ZO‐1 expression of BBB. It might be a potential target for neuroprotection during aging and in diverse neurological conditions.
eP‐ND‐A200
Validation of spatial transcriptomics approaches on post‐mortem brain tissue from patients with Lewy body disorders
T. Curless 1, H. R. Nelvagal1, J. Hardy2, H. Morris2, R. Real2, M. Ryten2, M. Blunskyte2, D. Gavriouchkina2, Z. Jaunmuktane2
1UCL, Clinical and Movement Neurosciences, London, United Kingdom; 2UCL, London, United Kingdom
Introduction: The underlying mechanisms of Lewy pathology progression in patients with Parkinson's disease (PD), and factors which drive the development of dementia in patients with PD (PDD) are not understood. More specifically, it is not currently known how the transcriptomic profile of patients with PD and PDD differs, and to what extent it is influenced by APOE status. Numerous spatial transcriptomics platforms have been developed, providing morphological and spatial context for gene transcription characterisation, in a cellular context, however their applicability for use on human FFPE post‐mortem brain tissue is yet to be validated.
Objective: To use spatial transcriptomic approaches to identify transcriptional differences in cortical regions of patients with PD and PDD. Additionally, we seek to identify transcriptional differences between APOE4 carriers and non‐carriers.
Materials and Methods: Two different spatial transcriptomic platforms were used. One platform was used to assess transcriptomic profiles of GFAP positive astrocytes across cortical and white matter regions in 42 cases, comprised of PD, PDD and controls, stratified by APOE genotype. The other platform was used to provide non‐cell type specific transcriptomic profiles of a subset of the cases.
Results: We have explored the use of antibody based and image based spatial transcriptomic platforms. We demonstrate a greater depth of transcript data on the antibody‐based platform, while the image‐based platform provides greater breadth across a smaller subset of genes.
Conclusion: We demonstrate the validity of spatial transcriptomics platforms for use on human post‐mortem FFPE brain tissue, and highlight transcriptional differences between disease groups, anatomical regions and APOE genotypes. Further analysis to provide greater insight into these transcriptional differences is ongoing.
eP‐ND‐A201
Salivary alpha‐synuclein as a potential diagnostic marker of Parkinson's disease
D. Hrabos 1, M. Kaiserova2, M. Kavalkova1, M. Levkova1, K. Mensikova2
1University Hospital Olomouc, Department of Clinical and Molecular Pathology, Olomouc, Czech Republic; 2University Hospital Olomouc, Department of Neurology, Olomouc, Czech Republic
Introduction: The neuropathological hallmark of Parkinson's disease is an accumulation of alpha‐synuclein in the form of oligomers, Lewy bodies and Lewy neurites in the brain. However, there is growing evidence that both monomeric and oligomeric alpha‐synuclein could be found in body fluids of the patient, for example, cerebrospinal fluid, saliva or tears. Our study aimed to analyse protein levels of alpha‐synuclein in saliva of patients with Parkinson's disease and correlate these with the progression of the disease and patients' age.
Methods: We have established a protocol for routine collection and analysis of saliva. In the study, we have analysed total protein concentration and total alpha‐synuclein concentration (ELISA) in saliva from 41 symptomatic Parkinson's disease patients and 16 healthy controls. The mean age of the patients was 67.9 ± 6.1 and the mean disease duration was 9.2 ± 5.2.
Results: Our analysis of saliva did not show a significant difference in total protein concentration between Parkinson's disease patients and healthy controls (p = 0.1263). Further, there was no significant difference in total alpha‐synuclein levels between the groups (p = 0.1883). Similarly, there was no significant results after analysing total alpha‐synuclein level to total protein level ratios. No significant correlation was observed between total alpha‐synuclein levels and disease duration or the age of the patients.
Conclusion: The result of the study reflects a growing consensus that salivary alpha‐synuclein is indeed an unreliable marker of Parkinson's disease and its progression. Moreover, using commercially available ELISA kits, we have not been able to successfully detect oligomeric alpha‐synuclein. Next step would be to analyse saliva for alpha‐synuclein using seeding amplification assay.
eP‐ND‐A202
Clinicopathological spectrum of globular glial tauopathies (GGT)
M. Yoshida 1, A. Akagi1, Y. Riku1, J. Sone1, H. Miyahara1, Y. Iwasaki1
1Aichi Medical University, Department of Neuropathology, Institute for Medical Science of Aging, Nagakute, Japan
Introduction: Globular glial tauopathies (GGT) is a 4‐repeat (4R) tauopathy characterized by globular glial inclusions (GGIs). The wide range of clinicopathological features make clinical diagnosis challenging.
Objectives: To elucidate characteristic features of GGT, we investigated whole neuropathological pictures and extract core findings.
Patients and Methods: The study included eight pathologically proven cases with GTT among 6400 autopsied cases in Aichi Medical University Brain Resource Center. Signed informed consent for autopsy, the archiving of tissue for research purposes, and genetic analysis were obtained from the family members of all cases in compliance with the Ethical Committee for Medical Researches of Aichi Medical University. The cerebral hemispheres, brainstem, cerebellum and spinal cord were fixed in 20% neutral‐buffered formalin, and paraffin embedded sections were stained using haematoxylin‐eosin, Klüver–Barrera, Gallyas–Braak silver staining and distribution and severity of tau pathology was evaluated, using for anti‐hyperphosphorylated tau, anti‐3R‐tau and anti‐4R‐tau immunohistochemistry.
Results: The cases include five females and three males, age at death was 76 ± 8.5 (average ± standard deviation), age at onset was 71 ± 8.6, disease duration was 5.9 ± 3.1(3–12)years. All cases showed 4R‐tau positive GGIs, predominantly in white matter. Frontal cortex including precentral gyrus was involved in 88%, corticospinal tract degeneration in 75%, severe temporal lesion in 25%, and laterality of cortical lesions were found in 75%. Degeneration of the substantia nigra, pallidum, and subthalamic nucleus was found in 88%, although neuronal loss of the pallidum, and subthalamic nucleus was relatively mild compared to that of PSP‐Richardson syndrome.
Conclusion: Vulnerable regions of GGT included precentral gyrus and corticospinal tract. These pathological areas may reflect clinical features of motor symptoms and clinical diagnosis of ALS, or PLS.
eP‐ND‐A203
Investigation of HDL and LDL levels and screen for de novo mutation in MCU gene in Alzheimer's disease patients
B. Vellingiri 1, A. Venugopal2, H. W. Suresh Babu1, A. Elangovan1
1Central University of Punjab, Zoology, Bathinda, India; 2Bharathiar University, Human Genetics and Molecular Biology, Coimbatore, India
Background: The most prevalent form of dementia, Alzheimer's disease (AD) is a chronic illness that is on the rise among the geriatric population. Even though research into its biochemical, and gene mutations has advanced, its aetiology is still unclear and complex.
Aim: In this study, we aim to screen for alterations in biochemical parameters such as LDL and HDL levels among AD subjects. Further we also aim to understand the role of MCU gene mutations in the progression of AD.
Methodology: Twenty‐eight (28) participants diagnosed with AD were recruited for the study where the biochemical parameters as well as genetic mutations were analysed from India.
Result: The present study revealed that the biochemical parameters revealed no statistical significance in the study though a pattern could be observed in the serum levels of HDL and LDL levels for cholesterol among AD subjects. Further de novo mutations were observed in the MCU gene of mitochondrial calcium uniporter among the late‐onset subjects of AD.
Conclusion: All these findings reveal the need for a larger cohort study to gain a better and more detailed understanding of the aetiology of AD.
eP‐ND‐A204
A new case of mitochondrial membrane protein associated neurodegeneration (MPAN)
J. Bonnin 1, K. Newell1, B. Ghetti1
1Indiana University, Pathology and Laboratory Medicine, Indianapolis, IN, United States
Introduction: Mitochondrial membrane protein associated neurodegeneration (MPAN) is characterized by gait changes followed by progressive spastic paresis, progress dystonia and cognitive decline. The neuropathology of MPAN is characterized by the presence of numerous axonal spheroids and cortical Lewy bodies.
Objectives: We are studying in detail the neuropathology using coronal brain sections of the cerebrum and cerebellum of a male carrying two mutations, one in each of his C19orf12 genes.
Patients and Methods: We used neuropathologic methods to study post‐mortem brain tissue from a 39‐year‐old male.
Results: A 19‐year‐old adult male developed a progressive neurogenic disorder and presented with motor deficits and atrophy of hands muscles. At age 33, optic nerve atrophy and impaired eye motility were documented. The clinical diagnosis was MPAN. He expired at age 39 years. There was no family history of a neurological disorder. Severe brain atrophy was present. Histologically, marked neuronal loss and gliosis throughout the cerebrum, cerebellum, and brainstem. Axonal swelling and Lewy neurites are present in the neocortex and globus pallidus. Severe tau pathology using AT8 was seen in the putamen, hippocampus including the end plate, parahippocampal cortex and entorhinal cortex. Iron deposits are present in the putamen, globus pallidus and substantia nigra.
Conclusions: There is evidence supporting an autosomal recessive pattern in most cases of MPAN; however, in some instances a single mutation has been reported consistent with dominant inheritance. Current neuropathologic and genetic studies in the present case will provide additional insights on the biology of this condition.
eP‐ND‐A205
Mesenchymal stem cells therapy exerts neuroprotection in an animal model of Parkinson's disease
S. Bagheri‐Mohammadi 1
1Shahid Beheshti University of Medical Sciences, Department of Physiology and Neurophysiology Research Center, School of Medicine, Tehran, Iran
Background: Parkinson's disease (PD) is the second most common neurodegenerative disorder after Alzheimer's disease and is expected to impose an increasing social and economic burden on societies as populations’ age. The ground‐breaking developments in stem cell research in the last decade have revived interest in intracerebral cell transplantation as a therapeutic approach for PD. The experimental research with intranasal administration of stem cells in a PD mouse model can work and in some cases induce major, long‐lasting improvement. This research was done for evaluating the effect of intranasal delivery of HEDSCs in a mouse model of PD.
Methods: In this research, the intranasal route was used for the administration of human endometrium‐derived stem cells (HEDSCs)‐GFP labeled in a mouse model of PD (intrastriatal injection of 6‐OHDA) in three doses (10,000, 50,000, and 100,000 cells μL−1). During four months after stem cell application, behavioral tests including rotational behavior test, Rotarod test, and open field test were examined. In addition, immunohistochemistry (IHC) was used to assay the GFP, human neural Nestin, and tyrosine hydroxylase (TH) markers in the fixed brain tissue at the substantia nigra pars compacta (SNpc) area.
Results: The result demonstrated that the administration of HEDSCs enhanced behavioral parameters compared with the control group significantly. The data from IHC analysis revealed that the GFP marker (Figure 1) and also Nestin (as a differential neuronal biomarker, Figure 2) were expressed in the SNpc area. Also, TH as a dopaminergic neuron marker significantly increased after cellular therapy in an optimized dose of 500,000 cells μL−1.
Conclusions: Our investigation revealed that cellular therapy with HEDSCs (intranasal method) improved the PD symptoms in a mouse model of PD as an effective method.
Keywords: Cell therapy, dopaminergic neurons, intranasal method, mesenchymal stem cells, Parkinson's disease.
eP‐ND‐A206
Honey and black seed synergistically promote regeneration of oligodendrocytes in cuprizone intoxicated quail brain
M. Z. K. Raimi 1, A. Shabbir1,2
1Univeristy of Abomey Calavi, Biosciences, Abomey Calavi, Benin; 2Comsats University, Biosciences, Islamabad, Pakistan
Multiple sclerosis (MS) is a complex disorder, characterized by demyelination and loss of axonal parts of neurons in the central nervous system involving multiple genetic and environmental factors. Currently, three different approaches are being utilized to treat MS, where synthetic drugs are the most frequently used but they do not cure the disease. Second, the stem cell therapy but this too has limited success in treating MS in humans. The thirds technique involving administering hormones has been found to be most effective method but this too have some significant side effects. Alternatively, natural products can potentially serve as an affordable and effective substitute for the treatment of MS with minimum or no side effects. Blackseeds (Nigella sativa) and honey possessing potent neuroprotective, antioxidant, and anti‐inflammatory properties with no reported side effects can be a prospective candidate for an alternate remedial treatment of MS in animal model as well as in humans. In this study we established a new animal model (quail), to assess the synergistic efficacy of honey and black seed against demyelination within brain. A total of 35 male quails were used, among 10 were non treated and 25 were treated with 200 mg/kg/day cuprizone (CPZ) demyelination for six months to induce demyelination. After that they were divided into seven groups of five animals each where three CPZ treated groups received either honey, black seed oil or mixture of both for 6 weeks after demyelination. Behavioral tests were performed at the end of treatment. Afterwards, oligodendrocyte population was estimated in cerebellar white matter after histology. It was found that all three treatments efficiently induce remyelination. Interestingly, the mixture of honey and black seed was significantly more efficient than honey and black seed alone. Our data support the need of clinical trials for administration of N. sativa and honey in MS patients.

FIGURE 1.

FIGURE 2.
eP‐ND‐A207
Severe argyrophilic grain disease in a centenarian with severe dementia who did not show the “sloping shoulders sign”
T. Iwase 1, M. Yoshida2, Y. Iwasaki2, K. Sakurai3, Y. Hashizume4, D. Kaneda4, K. Adachi1, K. Ojika1, N. Matsukawa5
1Nagoya City University Mirai Kousei Hospital, Department of Neurology, Nagoya, Aichi, Japan; 2Aichi Medical University, Institute for Medical Science of Aging, Nagakute, Aichi, Japan; 3National Center for Geriatrics and Gerontology, Department of Radiology, Obu, Aichi, Japan; 4Fukushimura Hospital, Institute for Neuropathology, Toyohashi, Japan; 5Nagoya City University Graduate School of Medical Sciences, Department of Neurology and Neuroscience, Nagoya, Aichi, Japan
Introduction: The “sloping shoulders sign” is seen in moderate to severe Alzheimer's disease (AD). It is characterized by the hippocampus on both sides smoothly descending outward in axial CT/MRI.
Objectives: The aim of this study was to investigate the neuropathological changes in a centenarian with severe dementia who did not show the “sloping shoulders sign.”
Patients and Methods: The patients dementia progressed from around the age of 93. At age 102, there were episodes of playing with food, and getting naked everywhere. At age 104, she had difficulty in communication, and passed away peacefully. The CT/MR images of the brain did not show the “sloping shoulders sign.” Brain and spinal cord were neuropathologically investigated. The formalin‐fixed paraffin‐embedded sections stained with hematoxylin and eosin (HE), Klüver–Barrera (KB), Gallyas–Braak and immunostainings for amyloid‐β (Aβ), phosphorylated tau (p‐tau), α‐synuclein, and phosphorylated transactivation response DNA‐binding protein of 43 kDa (p‐TDP‐43) were used.
Results: Numerous argyrophilic grains were found under the microscope. The distribution of argyrophilic grains corresponded to Saito's stage III, and the density of argyrophilic grains was very high. Spongiform changes were observed in the superficial cortical layer in areas rich in argyrophilic grains. Despite the relatively large amount of Aβ accumulation, the distribution of neurofibrillary tangles (NFTs) was limited to the medial temporal lobe, corresponding to Braak stage III and Braak AT8 immunohistochemistry stage III. The level of AD‐related neuropathologic change was intermediate.
Conclusion: Argyrophilic grain disease (AGD) is a relatively frequent slowly progressive dementia with late onset. This study led to the discovery that argyrophilic grain disease does not show the “sloping shoulders sign.” The “sloping shoulders sign” is useful to differentiate AGD from AD.
eP‐ND‐A208
α‐Synuclein in blood CNS‐originating extracellular vesicles—An inconclusive diagnostic quest for Parkinsonian disorders
H. B. Taha 1, S. S. Ati1
1University of California, Los Angeles, Integrative Biology & Physiology, Los Angeles, CA, United States
Parkinsonian disorders, including Parkinson's disease (PD), multiple system atrophy (MSA), dementia with Lewy bodies (DLB), progressive supranuclear palsy (PSP), and corticobasal syndrome (CBS), present shared early motor symptoms but differing cellular and regional pathophysiology. Accurate premortem diagnosis remains challenging. Extracellular vesicles (EVs) contain cell‐state‐specific biomolecules and can cross the blood–brain barrier to the peripheral circulation, providing a unique central nervous system (CNS) insight. Measuring biomarkers in blood CNS‐originating EVs have become a promising avenue for minimally invasive diagnostics. This study evaluated the potential levels of blood‐isolated neuronal and oligodendroglial EVs (nEVs and oEVs) α‐synuclein (α‐syn) proteoforms in Parkinsonian disorders. We searched PUBMED, EMBASE, google scholar and recent reviews of the literature to include studies that have measured mean ± SD of α‐syn in putative nEVs and oEVs in patients with PD and at least one other Parkinsonian disorder or healthy controls (HCs). Thirteen studies were included in the final meta‐analysis and demographic and clinical variables were collected for meta‐regressions. We quantified the effect size (SMD) using an inverse‐variance random‐effects model. The studies included 1565 patients with PD, 206 with MSA, 21 with DLB, 172 with PSP, 152 with CBS and 967 HCs. Findings suggest that a combination of nEVs and oEVs α‐syn concentrations are higher in patients with PD vs. HCs (k = 14, SMD = 0.21; p = 0.021; Figure 1), while nEVs α‐syn is lower in patients with PSP and CBS versus PD (k = 6, SMD = −1.04; p = 0.0017) or HCs (k = 4, SMD = −0.41, p < 0.001). Additionally, α‐syn levels in oEVs did not effectively differ among PD, MSA, or HCs (Figure 2), contradicting the literature. Meta‐regressions showed demographic/clinical were not significant predictors of nEVs or oEVs α‐syn concentrations. These findings highlight the need for more accurate biomarkers.

FIGURE 1.

FIGURE 2.
eP‐ND‐A209
Demyelination triggers divergent neuropathological consequences in APPSWE and APPSWE/PSEN1dE9 transgenic mouse models of Alzheimer's disease
G. W. Cheng1, I. W. Ma1, J. Huang2, S. H. Yeung1, P. Ho1, Z. Chen3, H. K. F. Mak2, K. Herrup4, K. W. Y. Chan3,5, K. H. Tse 1
1The Hong Kong Polytechnic University, Department of Health Technology and Informatics, Hung Hom, Kowloon, Hong Kong; 2University of Hong Kong, Department of Diagnostic Radiology, LKS Faculty of Medicine, Hong Kong, Hong Kong; 3City University of Hong Kong, Department of Biomedical Engineering, Kowloon, Hong Kong; 4University of Pittsburgh School of Medicine, Department of Neurobiology, Pittsburgh, Hong Kong; 5Johns Hopkins University School of Medicine, Russell H. Morgan Department of Radiology and Radiological Science, Baltimore, MD, United States
Introduction: Neuroimaging identified myelin degradation as one of the early structural changes in aging and sporadic Alzheimer's disease (AD) brain, but it remains elusive whether early myelin loss accelerates AD progression.
Objectives: We aim to examine the effects of cuprizone‐mediated demyelination on young mouse models carrying APPSWE and APPSWE/PSEN1dE9 transgenes, respectively. We asked if increasing burden of amyloidosis confers a higher vulnerability to cuprizone, and if demyelination exacerbates premature amyloid aggregation these models.
Materials and Methods: Magnetic resonance imaging (MRI) at 3T with magnetization transfer ratio (MTR), diffusion tensor imaging (DTI) and MR spectroscopy (MRS) sequences was applied on wildtype(n = 16), R1.40(APPSWE n = 6) and APP/PS1(APPSWE/PSEN1dE9 n = 14) with or without cuprizone (0.2% in diet, 4 weeks). A radio‐pathological investigation was conducted on the scanned brains with region‐specific immunohistochemistry, biochemistry and targeted‐RNA‐seq.
Results: MRI detected distinct demyelination responses in R1.40 and APP/PS1, where they showed an opposing change of myelin tract diffusivity in both gray and white matter in DTI. Cuprizone led to an abnormally high level of axonal damage in R1.40 with a significant reduction of N‐acetylaspartate (NAA) signal in MRS. Yet demyelination resulted in a significant build‐up of intraneuronal amyloid deposition only in APP/PS1, which has a strong correlation with a higher diffusivity. Frontal lobe in APP/PS1 was found particularly vulnerable to demyelination where a significant DNA double strand breaks(53BP1+) formation was found in oligodendrocytes with a truncated DNA damage response identified by targeted RNA‐seq. Despite these damages, cuprizone‐treated mice showed no cognitive impairment or hippocampal pathology.
Conclusion: We show that demyelination may exacerbate neuropathology in AD mouse models and shed light on the causal relationship between early myelin loss and AD progression.
eP‐ND‐A210
Progressive supranuclear palsy presenting with late onset chorea plus ataxia syndrome—A rare phenotype with severe oligodendrocytic involvement and globular morphologies
R. Taipa 1,2, M. Pinto1, I. Reis1, M. Rodrigues3
1Centro Hospitalar Universitário de Santo António, Portuguese Brain Bank, Neuropathology Unit, Department of Neurosciences, Porto, Portugal; 2University of Porto, Biomedical Sciences Institute Abel Salazar, Porto, Portugal; 3Hospital de Braga, Department of Neurology, Braga, Portugal
Introduction: Progressive supranuclear palsy (PSP) is 4‐repeat tauopathy associated with various clinical phenotypes. The clinical heterogeneity can be related to different patterns of cellular tau pathology. Additionally, some overlap with distinct tau morphologies, namely globular glial tauopathies (GGT), has been described.
Objectives: To describe a rare clinical phenotype associated to PSP pathology. Characterize tau pathology morphologies and distribution.
Patients and Methods: Clinical, neuroimage and pathological description.
Results: A 57‐year‐old male started progressive cerebellar ataxia associated with generalized chorea. Three years later, he was only able to walk with a walker. The neurological examination by the age of 62 revealed slow ocular saccades, but no limitation of gaze, generalized chorea, bilateral limb dysmetria and widened base gait. The patient progressed with worsening of the cerebellar symptoms, disappearing of the chorea and emerging of an asymmetrical parkinsonism that never responded to levodopa. Two years before death he developed cervical dystonia and blepharospasm, but his ocular movements, despite slow were complete. MRI showed midbrain and cerebellar atrophy. Multiple genetic testing, including Huntington disease, SCAs and recessive ataxias were negative. The patient died at 68. The neuropathology study showed severe atrophy and neuron loss in the globus pallidus, subthalamic nucleus, midbrain (including substantia nigra, tegmentum and tectum), pons and cerebellar dentate nucleus. The immunohistochemistry showed a 4‐Repeat tauopathy consistent with PSP with severe oligodendrocytic involvement, including globular morphologies. There was striking cerebellar white matter involvement.
Conclusion: Chorea has been very rarely described in PSP, particularly has a present symptom. The neuropathology study showed characteristics beyond typical PSP pathology, with some features of GGT with particular anatomical distribution.

FIGURE 1.

FIGURE 2.
eP‐ND‐A211
CCP1, a regulator of tubulin post‐translational modifications, potentially plays an essential role in cerebellar development
A. Araki 1,2, B. Pang1, L. Zhou3, H. Takebayashi4, T. Harada1, K. Kadota1,2
1Shimane University Hospital, Department of Organ Pathology, Izumo, Japan; 2Shimane University Hospital, Pathology Division, Izumo, Japan; 3Niigata University, Department of Cellular Neurobiology, Brain Research Institute, Niigata, Japan; 4Niigata University, Division of Neurobiology and Anatomy, Graduate School of Medical and Dental Sciences, Niigata, Japan
Introduction: The cytosolic carboxypeptidase (CCP) 1, alias Nna1, protein, encoded by CCP1, is expressed in cerebellar Purkinje cells (PCs). In model mouse studies, the dysfunction of CCP1 protein and the loss of CCP1 protein all lead to the degeneration of cerebellar PCs by shortening the length of microtubule glutamate side chains and disturbing microtubule transport, thereby leads to cerebellar ataxia. Recently, the CCP1 dysfunction has been revealed the disease cause of infantile‐onset neurodegeneration, mainly affected the cerebellum.
Objectives: By comparing with the cerebellar CCP1 distribution in wild‐type (WT) and Ccp1 mutant mice on postnatal days (P) 7–28 to investigate the differential effects of CCP1 protein deficiency and disorder on cerebellar development.
Materials and Methods: Two Ccp1 mutants (i.e., AMS mice and Nna1 knockout (KO) mice) are used as disease models in which the distribution of CCP1 was observed by immunohistochemistry (IHC) and immunofluorescence (IF), and the expression of CCP1 protein was detected by Western blotting (WB), as well as the ultrastructural changes of Purkinje cells were observed by transmission electron microscope (TEM).
Results: IHC and IF studies revealed significant differences in the cerebellar CCP1 expression in WT and mutant mice of P7 and P15, but no significant difference between AMS and Nna1 KO mice. WB results showed that the expression of CCP1 in AMS mice was decreased in four ages, and the expression of CCP1 protein was not detected in the cerebellum of Nna1 KO mice. TEM showed slight abnormality in the nuclear membrane structure of PCs in the AMS and Nna1 KO mice at P15 and significant abnormality with depolymerization and fragmentation of microtubule structure at P21.
Conclusion: We revealed the morphological changes of PCs in two Ccp1 mutants at postnatal stages and indicated that CCP1 played an important role in cerebellar development, most likely via polyglutamylation.
eP‐ND‐A212
Evaluation of disease‐specific α‐synuclein seeding in formaldehyde‐fixed paraffin‐embedded human brain archived long‐term
A. Kim 1,2, I. Martinez‐Valbuena2,3, J. Li2, A. E. Lang2,3,4, G. G. Kovacs1,2,3,4,5
1Laboratory Medicine & Pathobiology, University of Toronto, Toronto, Canada; 2Tanz Centre for Research in Neurodegenerative Diseases, University of Toronto, Toronto, Canada; 3Krembil Brain Institute, University Health Network, Toronto, Canada; 4Edmond J. Safra Program in Parkinson's Disease and the Morton and Gloria Shulman Movement Disorders Clinic, Toronto Western Hospital, Toronto, Canada; 5Laboratory Medicine Program, University Health Network, Toronto, Canada
Introduction: Recent studies have been able to detect α‐synuclein (αSyn) seeding in formalin‐fixed paraffin‐embedded (FFPE) tissue from patients with synucleinopathies using seed amplification assays (SAAs), but with relatively low sensitivity due to limited protein extraction efficiency.
Objective: This study developed a novel, streamlined protein extraction protocol for evaluating disease‐specific seeding in FFPE human brain tissue.
Materials and Methods: We evaluated the protein extraction efficiency of different tissue preparations, deparaffinizations, and protein extraction buffers using formalin‐fixed and FFPE tissue from a patient with Lewy body disease (LBD). Heat‐induced antigen‐retrieval and dissociation using a commercially available kit was also incorporated.
Results: Our novel protein extraction protocol allows a high‐yield extraction of protein from 10 sections of 4.5‐μm‐thickness or 2‐mm‐diameter micro‐punch of FFPE tissue, which can then be used to seed SAAs. We demonstrate that extracted proteins from FFPE still preserve seeding potential and further show disease‐specific seeding in LBD and multiple system atrophy.
Conclusion: Our findings open new perspectives in re‐evaluating archived human brain tissue and provide an alternate option to frozen tissue. This is the first study to recapitulate disease‐specific αSyn seeding behavior in FFPE human brain, with ultra‐structural validation using electron microscopy. Our study allows the expansion of disease‐specific seeding assays to larger cohorts to facilitate molecular subtyping of synucleinopathies.
eP‐ND‐A213
Multi‐centric plaques in kuru
B. Sikorska 1, P. P. Liberski1
1Medical University of Lodz, Department of Molecular Pathology and Neuropathology, Lodz, Poland
Introduction: Kuru, discovered by Gajdusek and Zigas, was transmissible human prion disease, spread by ritual endocannibalism among the Fore group of Papua New Guinea. Kuru was fatal cerebellar ataxia syndrome, microscopically characterized by numerous amyloid plaques.
Objectives: We present a detailed study of amyloid plaques in a kuru case, using electron and confocal laser microscopy.
Materials and Methods: We re‐evaluated archival formalin‐fixed, paraffin‐embedded brain specimens, including cerebellum, several cortical areas, hippocampus, and basal ganglia, of a 16‐year‐old male who died of kuru. Electron, laser confocal microscopy and 3D image analysis software with volume rendering was used to study the structure of the amyloid plaques, their spatial organization and association with cells.
Results: The typical kuru plaques were numerous in the cerebellar cortex but were also present in the striatum and hippocampal formation. Apart from these classic changes, we observed a few florid plaques similar to those described in vCJD and most interestingly, multi‐centric plaques unique to GSS. These plaques, reconstructed into 3D‐structural images, using confocal laser microscopy, showed several neurites crossing the amyloid plaques. The 3D images confirmed structural similarity of the multicentric plaques of kuru to those observed in GSS.
Conclusions: The multi‐centric neuritic plaques found in this kuru brain are typical only of GSS, and to our knowledge have never been reported in any other disease. Taking into consideration that iatrogenic cases of prion disease and vCJD cases transmitted by blood transfusion showed that prion transmission from human to human does not significantly change the neuropathological and biochemical phenotype and that the unique type of plaques was observed only in GSS and kuru, it may be hypothesized that kuru originated from a GSS case cannibalized incidentally, resulting in subsequent epidemics.
eP‐ND‐A214
Coats Plus syndrome—A case report
C. Pontinha 1, D. Forte2, M. Correia2, A. Sagarribay2, C. Conceição3, M. Mafra1, M. Matos2
1Central Lisbon University Hospital Center, Anatomical Pathology, Lisbon, Portugal; 2Central Lisbon University Hospital Center, Neurosurgery, Lisbon, Portugal; 3Central Lisbon University Hospital Center, Department of Neuroradiology, Lisbon, Portugal
Introduction: Coats Plus syndrome or cerebroretinal microangiopathy with calcifications and cysts (CRMCC) is a rare disease with an autosomal recessive pattern caused by a mutation in the CTC1 gene. This gene is located on chromosome 17p13.1 and plays an important role in telomere replication. It is a multisystem disorder characterized by retinal telangiectasia and subretinal exudate, intracranial calcification, leukodystrophy, prenatal and postnatal growth retardation, parenchymal brain cysts, osteopenia with predisposition to fractures, bleeding in gastrointestinal tract and portal hypertension. CT features are extensive calcifications involving bilateral basal ganglia, bilateral deep cerebellar nuclei and brain stem. MRI demonstrates abnormal white matter hyperintensity suggesting leukodystrophy.
Methods: The authors describe a case of an adolescent diagnosed with CRMCC that underwent surgical cyst removal.
Results: The authors show a surgical case of Coats Plus syndrome in a 14 years old patient with multiple cyst and calcifications in supratentorial and posterior fossa regions and a progressive asymmetric spastic tetraparesis. A pontine cyst was described some years before surgery and it grew in the last two so we decided to remove it in order to relieve signs and symptoms of tetraparesis. The postoperative period was uneventful and was discharged without complications. He gained some autonomy in positioning and transferring. The revision of literature show less than 100 cases described and few of them underwent brain surgery, so histopathological examination is very rare in Coats Plus syndrome.
Conclusion: Coats Plus syndrome or CRMCC is a rare degenerative disease that may be included in the differential diagnosis of cerebral calcification and cysts and may need neurosurgical intervention.

FIGURE 1.
eP‐ND‐A215
Multiple system atrophy with abundant nigral neuronal cytoplasmic inclusions presenting slowly progressive levodopa‐responsive parkinsonism
T. Ikeda 1,2, T. Fujioka1, N. Matsukawa1, K. Ueda3, T. Ando2,4, A. Akagi2, Y. Riku2,4, H. Miyahara2, J. Sone2, H. Inagaki3, Y. Iwasaki2, M. Yoshida2
1Nagoya City University Graduate School of Medical Sciences, Department of Neurology and Neuroscience, Nagoya, Japan; 2Aichi Medical University, Department of Neuropathology, Institute for Medical Science of Aging, Nagakute, Japan; 3Nagoya City University Graduate School of Medical Sciences, Department of Pathology and Molecular Diagnostics, Nagoya, Japan; 4Nagoya City University Graduate School of Medical Sciences, Department of Neurology, Nagoya, Japan
Introduction: Although some pathological confirmed multiple system atrophy (MSA) cases who had been clinically diagnosed with Parkinson disease (PD) were reported, the neuropathological differences between typical MSA and PD mimicking MSA were unclear.
Clinical Summary: A Japanese man developed resting tremor on his right leg at age 54. At age 58, he developed gait disturbance and clumsiness on his right hand. Neurologic examination revealed cogwheel rigidity on his right limbs and mild bradykinesia. Because of the good response to carbidopa‐levodopa treatment and normal brain MRI, he was diagnosed with PD. At age 67, his gait disturbance became worse and he developed slurred speech. Truncal and bilateral limb ataxia and severe orthostatic hypotension were observed. Brain MRI revealed progressive atrophy of pontine basis and putamen. The patient died of aspiration pneumonia at the age of 68.
Pathological Findings: Macroscopically, severe atrophy of the putamen and pontine basis was observed. Depigmentation was severer in the substantia nigra than the locus coeruleus. Microscopically, severe neuron loss with gliosis and abundant GCIs were observed in the putamen. Severe neuron loss with gliosis was also observed in the substantia nigra. Most of the exiting neurons in the substantia nigra had sickly eosinophilic rounded inclusions in their cytoplasm dense. These neuronal inclusions were positive by Gallyas–Braak silver staining and anti α‐synuclein immunohistochemistry and visibly different from Lewy body. Electron microscopy revealed that the nigral NCIs were composed of randomly orientated granule‐coated filaments. The distribution and extent of these neuropathological changes were corresponding to SND grade III and OPCA grade II according to the MSA grading scales proposed by Jellinger et al. Lewy body and Lewy neurites were not observed.
Conclusion: The abundant nigral NCIs might be a supportive neuropathological feature corresponding to PD mimicking MSA.
eP‐ND‐A216
Significant contralaterality of temporal‐predominant neuro‐astroglial tau pathologies and FTLD‐TDP type C presenting with the right temporal variant FTD
H. Tanaka 1, M. A. Hird2, D. F. Tang‐Wai2,3,4, G. G. Kovacs1,3,5
1University of Toronto, Department of Laboratory Medicine and Pathobiology, Toronto, Canada; 2University of Toronto, Department of Medicine, Division of Neurology, Toronto, Canada; 3Toronto Western Hospital, Krembil Research Institute, Toronto, Canada; 4Toronto Western Hospital, University Health Network, Toronto, Canada; 5University Health Network, Laboratory Medicine Program, Toronto, Canada
Introduction: A peculiar form of temporal‐predominant neuro‐astroglial tau pathology (TATP) associated with TDP‐43 proteinopathy and TMEM106B rs1990622 A/A genotype has been recently described.
Objectives: To clarify the clinicopathologic characteristics of TATP through a detailed examination of an autopsy case, with special reference to contralaterality.
Patient and Methods: The clinical features were recorded and autopsied tissue was examined histologically.
Results: A right‐handed man without a history of familial neurodegenerative diseases noticed progressive word‐finding difficulty at age 72, followed by phonagnosia, decline in personal hygiene, perseverative behavior, and prosopagnosia. He died at age 81. MRI showed progressive right temporal lobe atrophy. The diagnosis was right temporal variant frontotemporal dementia (rtvFTD). Autopsy revealed frontotemporal brain atrophy (brain weight 1044 g) with right predominance, severe neuronal loss and gliosis in regions including the temporal pole, fusiform gyrus, and inferior/middle temporal gyrus. TDP‐43 pathology was predominant on the right side with p‐TDP‐43‐positive dystrophic neurites and occasional neuronal cytoplasmic inclusions (NCIs). Meanwhile, tau pathology (4‐repeat tau) was predominant on the left side, featuring diffuse granular immunopositivity in astrocytes and neurons. Double‐label immunofluorescence revealed co‐localization of p‐TDP‐43 and p‐tau in NCIs and neurites.
Conclusions: This study demonstrates the co‐existence of the rare TATP and FTLD‐TDP type C, are present with marked contralaterality. Both proteins accumulate in some lesions, with p‐tau and p‐TDP‐43 co‐localizing in NCIs and neurites, indicating potential interaction. This study suggests that two pathological proteins might occur by common pathogenesis and/or interactions, and then, develop independently.
eP‐ND‐A217
A study on the expression profile of genes coding for secretory proteins using in vitro model of Alzheimer's disease
R. Singh 1, A. Sunkaria1
1Guru Nanak Dev University, Amritsar, Amritsar, India
Introduction: Age‐related neurological illness like Alzheimer's disease (AD) is steadily becoming more prevalent among the aged population. Cognitive deficits are caused by a progressive loss of normal brain functions. Increased production of amyloid (Aβ) and the development of neurofibrillary tangles are the two most significant pathogenic events that occur during AD progression. Until today, many attempts have been made towards discovering novel targets which are more precise and could identify the progression of the disease at very early stage.
Objective: To identify novel early‐stage secretory biomarkers of AD.
Methodology: In the present study, the Human Protein Atlas (HPA) database was used to filter out total human secretome. Using single cell type proteome of the HPA database, neuronal proteins were compared with total human secretome to discover overlapping proteins and their respective genes. Further, AD associated genes were extracted using DisGeNet database and ranked according to their Gene‐Disease Association (GDA) score. Further, different proteoforms of Aβ were used to treat neuronal cells in vitro to mimic early stages of AD like pathology. The expression of secretory protein genes from in vitro model system has been analysed.
Results: Out of 1678 genes, 30 neuronal genes were identified that were coding for secretory proteins. These genes were further categorized according to their proteins function. Specific primers for the top five genes were designed and expression analyses were conducted. Analyses revealed modulation in the expression of APOE, MAPT, NPY, NGF, and RELN genes.
Conclusion: The aim of this study was to discover early‐stage biomarkers for AD. In the present study, we have tried to identify modulation in the genes coding for secretory proteins which might be reflected at protein levels also. Currently, we are working on to fully understand the modulation of AD secretome which would enable us to identify AD specific early stage biomarkers.
eP‐ND‐A218
Mixed brain pathology in neurodegenerative parkinsonism and dementia
K. Mensikova 1, L. Tuckova1, D. Hrabos1, J. Bouchal1, J. Ehrmann1, P. Kanovsky1
1Faculty of Medicine and Dentistry, Palacky University, University Hospital Olomouc, Olomouc, Czech Republic
Introduction: There is increasing evidence that high number of cases diagnosed clinically with phenotype, which corresponds to one of neurodegenerative proteinopathies (alpha‐synucleinopathy, tauopathy, Alzheimer's disease [AD] related proteinopathy, etc.) suffered actually from two or more neurodegenerative pathological processes.
Objective: To assess the presence of mixed neurodegenerative pathology and its proportion in the prospective cohort of patients treated for any phenotype of neurodegenerative parkinsonism, in whom the diagnosis was done according to the validated clinical diagnostic criteria.
Patients and Methods: A total of 49 brains of patients who were diagnosed with neurodegenerative parkinsonism or dementia and who consented to join the donor programme were autopsied; neuropathological examinations were performed according to the standard protocol.
Results: There were 25 patients, in whom the pathological examination confirmed the presence of single pathology: 13 patients suffered from alfa‐synucleinopathy, 5 patients suffered from tauopathy, 1 patient suffered from TDP‐34‐pathology and 6 suffered from AD—related proteinopathy. In 21 patients has examination revealed the presence of double pathology (4 syn/tau, 7 syn/AD, 6 tau/AD, 4 AD/TDP‐43), and in 3 patients has examination revealed the presence of triple pathology (syn/tau/AD). The correct clinical diagnosis was confirmed in 26 cases, and the incorrect clinical diagnosis was done in 23 cases; 13 of these cases suffered from the mixed brain pathology.
Conclusion: The mixed brain pathology is relatively common finding at brain autopsy in patients who suffered from neurodegenerative parkinsonism, even when the recent and validated clinical diagnostic criteria were used during the diagnostic process. This fact should serve as a basis for the further discussion about their usefulness.
Supported by: MH CZ‐DRO (FNOl, 00098892) and IGA LF 2023‐015.
eP‐ND‐A219
Altered iron content in superficial and deep white matter in Alzheimer's disease
A. M. Birkl‐Toeglhofer 1,2, J. Haybaeck1,2, R. Höftberger3, A. Rauscher4, C. Birkl5,6
1Medical University of Innsbruck, Institute of Pathology, Neuropathology and Molecular Pathology, Innsbruck, Austria; 2Medical University of Graz, Diagnostic and Research Institute of Pathology, Graz, Austria; 3Medical University of Vienna, Department of Neurology, Vienna, Austria; 4University of British Columbia, UBC MRI Research Centre, Vancouver, Canada; 5Medical University of Innsbruck, Department of Neuroradiology, Innsbruck, Austria; 6Medical University of Graz, Department of Neurology, Graz, Austria
Question: Iron is essential for physiological brain functioning impacting a wide range of cellular processes and accumulates during aging. Several diseases are linked with altered iron content in various brain regions including Alzheimer's disease (AD). Imaging and histological studies have demonstrated elevated iron content in the superficial white matter (SWM), located between the gray matter of the cortex and the deeper white matter (DWM), in health and disease. This region contains short U‐fibers which facilitate intracortical connections. The precise function of iron in the SWM in the context of AD is poorly understood. Our study focused on investigating the iron content in the SWM in AD.
Methods: To detect iron, post mortem brain tissue from three individuals with neuropathologically confirmed AD and one control case (HC) were examined using magnetic resonance imaging (MRI) and histological analyses. For quantitative MRI, a gradient echo sequence was used to map the R2* relaxation rate. For histological visualization, diaminobenzidine‐enhanced Turnbull blue staining was used.
Results: The histological analysis showed a pronounced iron staining in the U‐fibers and only sparse iron staining in the DWM of the HC. In the AD cases, the iron staining did not allow a clear distinction between SWM and DWM. The MRI showed higher SWM R2* values indicating higher iron content than in the DWM of the HC. The AD subjects had lower SWM R2* values indicating less iron content than in the DWM. The R2* values for the AD subjects in the SWM were lower than in the HC.
Conclusions: The study findings suggest an iron distribution shift in the SWM and DWM in AD. In subjects with high Braak and Braak stage, the iron content is more dispersed between the SWM and the DWM. The altered iron content in the SWM may be due to an iron shift from the U‐fibers to the DWM. Further research is necessary to determine the significance of SWM iron content in the human brain and its role in AD.
eP‐ND‐A220
Astrocytic permeability disorder in spheroid leukoencephalopathy with CSF1R mutation
T. Dot Gómara 1, S. Leclère2,3, I. Plu2,3,4, S. Boluda Casas2,3,4, D. Seilhean2,3,4
1Hospital Universitario de Navarra, Pathology, Pamplona, Spain; 2NeuroCEB Brainbank, Paris, France; 3CNRS UMR7225, INSERM U1127 Paris Brain Institute Sorbonne University, Paris, France; 4Pitié‐Salpêtrière University Hospital, Department of Neuropathology, Paris, France
Adult‐onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP) is a rare, progressive neurological disease associated with mutations in CSF1R (colony‐stimulating factor‐1 receptor) gene, known to control the production, differentiation and function of macrophages. We analyzed a series of seven cases of ALSP with regards to microglial, astrocytic and axonal markers. We observed a progressive loss of microglia associated with a change in the shape and size of remaining cells. The distribution of astrocytic aquaporin‐4 (AQP4) was significantly different in ALSP compared to controls. In the relatively spared subcortical regions, an abundance of ramified IBA1+ microglia was noticed as well as a strong expression of astrocytic AQP4. In contrast, in the most severely affected regions these markers were extinguished. These arguments provide evidence for the toxic role of microglia and disorders of water flow between cells as factors in the progression of lesions in the disease.
eP‐ND‐A221
Histological methods to study spinal receptor expression after degeneration of descending tracts
A. Simonovska Serra 1, P. Jauk1, A. Lotz1, A. Hainfellner2, F. Assen3, A. Adilovic1, N. Fehringer1, C. Haider4, U. Hofstötter1, W. J. Weninger2, R. Höftberger4, K. Minassian1
1Medical University of Vienna, Center for Medical Physics and Biomedical Engineering, Vienna, Austria; 2Medical University of Vienna, Center for Anatomy and Cell Biology, Vienna, Austria; 3Medical University of Vienna, Department of Dermatology, Vienna, Austria; 4Medical University of Vienna, Division of Neuropathology and Neurochemistry, Department of Neurology, Vienna, Austria
Introduction: Spinal cord injury (SCI) leads to a degeneration of descending monoaminergic pathways resulting in profound adaptations in the distal spinal cord circuits. Consequence is spinal spasticity and permanent paralysis. Recent studies demonstrated that neuromodulation of the altered spinal circuits by means of epidural electrical stimulation can improve spasticity and restore walking ability. A new therapeutic perspective is pharmacological neuromodulation of the respective receptors expressed by the circuits.
Objectives: These developments have motivated us to study in detail monoaminergic receptor expression of the human lumbar spinal cord and their alterations following SCI.
Materials and Methods: We targeted different monoaminergic receptors by immunohistochemistry and multiplex immunofluorescence on FFPE human spinal cord autopsy tissue as well as by western blotting on frozen spinal cord tissue. Tissue samples were derived from human subjects who had an intact CNS as well as those who had sustained a SCI.
Results: We established a broad spectrum of antibodies using immunohistochemistry and western blotting on positive control and spinal cord tissue. Several immunolabeled targets were identified in the human spinal cord for the first time, some of which had not been demonstrated in non‐human primates. We found that alpha motoneurons in the ventral horn co‐express receptors that mediate both inhibitory and excitatory actions. SCI not only upregulated receptor expression, but changed the distribution pattern throughout the Rexed laminae.
Conclusion: Our preliminary results may explain why previous pharmacological studies using precursor drugs or broad agonists failed to improve locomotor function in patients with SCI and rather had anti‐spasticity effects. They may further inform on future, more potent and targeted neuromodulation strategy.
eP‐ND‐A222
Discover the role of APOE gene and oxidative stress for the progression of late‐onset Alzheimer's disease (LOAD) from Coimbatore population, India
M. Balachandar 1, A. Venugopal2, B. Vellingiri3
1Karpagam Academy of Higher Education, Department of Biotechnology, Coimbatore, India; 2Bharathiar University, Department of Human Genetics and Molecular Biology, Coimbatore, India; 3Central University of Punjab, Department of Zoology, Bathinda, India
Background: Cognitive decline is a hallmark of Alzheimer's disease (AD), a progressive neurodegenerative disorder. The ε4 allele of apolipoprotein E (APOE) is the major genetic risk factor for Alzheimer's disease. Although strong genetic and biochemical evidence suggests that an increase in total A production, an increase in the ratio of Aβ42 to Aβ40, or generation of a mutant form of Aβ with greater amyloidogenic propensity are the main mechanisms for AD.
Aim: In the current study, we aim to understand the gene expression levels of APOE gene and oxidative stress as a major factor for progression of the disease condition among LOAD patients from Coimbatore, Tamil Nadu, India.
Methodology: Blood samples were collected from 18 participants diagnosed with LOAD. The levels of SOD and CAT for oxidative stress among ASD subjects were analysed by using HPLC. Further the gene expression of the APOE gene was analysed by conducting mutational analysis.
Result: We found that LOAD patients plasma had lower superoxide dismutase (SOD) and higher catalase (CAT) activity, resulting in lower SOD/CAT ratio. Further our studies revealed increased expression levels of APOE subunit in late‐onset AD participants when compared to controls.
Conclusion: To fully comprehend the significance of APOE in AD, more advanced research on the function of this gene and its association in causing oxidative stress needs to be conducted with a bigger cohort size.
eP‐ND‐A223
Molecular subtyping of progressive supranuclear palsy—A proof of concept
I. Martinez‐Valbuena 1, S. Lee1, E. Santamaria2, J. Fernandez‐Irigoyen2, B. Couto1, N. G. Reyes1, H. Tanaka1, S. Forrest1, A. Kim1, H. Qamar1, J. Li1, A. M. Karakani1, K. Senkevich1, E. Rogaeva1, N. Visanji1, A. E. Lang1, G. G. Kovacs1
1University of Toronto, Tanz Centre for Research in Neurodegenerative Diseases, Toronto, Canada; 2Navarrabiomed, Pamplona, Spain
Hypothesis: PSP is a 4R‐tauopathy characterised by subcortical pathology in neurons, astrocytes and oligodendroglia associated with a broad range of clinical phenotypes. We hypothesized that heterogeneity in PSP is a consequence of the molecular diversity of tau between different patients and among different brain regions.
Methods: We performed an extensive biochemical characterisation of the soluble, oligomeric tau species in 20 different brain regions from a cohort of 21 deeply phenotyped patients with PSP. This was complemented by detailed clinical, neuropathological and genetic data together with tau seeding amplification assays proteomics and spatial transcriptomics.
Results: Our study has exposed a striking patient‐to‐patient heterogeneity in the soluble oligomeric tau species across the 20 brain regions examined. Tau seeding in motor cortex from all subjects revealed a strong correlation between the amount of soluble oligomeric tau species and the tau seeding capacity, strongly implicating these species in driving the seeding activity of tau in PSP. We also quantified the amount of phosphorylated tau and evaluated the physical properties of tau using a protease‐sensitivity digestion assay that differentiates protein conformations. Finally, we have performed the first proteomic‐wide profiling of the motor cortex in PSP and uncovered several mechanistic pathways that differentiate patients with high seeding activity and low and low seeding activity.
Conclusions: Our observations strongly suggest that distinct molecular populations of tau contribute to the observed phenotypic differences in PSP. These data support the concept that individuals with PSP may have multiple molecular drivers of an otherwise common phenotype and emphasize the need for a novel molecular classification of PSP that will underpin the future development of personalized therapeutic approaches to curtail symptom progression.
eP‐ND‐A224
Alpha‐synuclein inclusions in the dentate gyrus are associated with cognitive impairment in multiple system atrophy
M. Wojewska 1, D. Petrova Quayle2, M. Otero Jimenez1, J. Alegre‐Abarrategui1, L. T. Middleton2, S. Gentleman1
1Imperial College London, Brain Sciences, London, United Kingdom; 2Imperial College London, Neuroepidemiology and Ageing Research Unit, School of Public Health, London, United Kingdom
Introduction: Cognitive impairment is considered a non‐supporting feature for a diagnosis of multiple system atrophy (MSA). However, recent evidence demonstrates it may affect up to 30% of patients living with MSA although the pathophysiological mechanism underlying these changes remains elusive.
Objectives: Cognitive impairment may reflect hippocampal pathology therefore we compared the hippocampus and parahippocampal gyrus in MSA cases with and without cognitive impairment.
Materials and Methods: Hippocampal sections from a large cohort of 64 MSA cases and 13 additional cases with both MSA and Parkinson's disease (PD) pathology from the Parkinson's UK tissue bank were included. They were immunostained for alpha‐synuclein (α‐syn) and tau.
Results: Semi‐quantitative analysis of α‐syn inclusions revealed that 33 of 64 MSA patients (52%) had at least one ring‐shaped neuronal perinuclear inclusion in the dentate granule cells. None of the cases with predominantly PD pathology exhibited this type of inclusion. All but one MSA case with documented cognitive impairment (10/11) had inclusions in the dentate gyrus and cornu ammonis sectors. Therefore, MSA cases with cognitive impairment were significantly more likely to display these pathological structures. None of these ring‐shaped inclusions seen in the dentate gyrus were immunoreactive for tau.
Conclusion: Our observations suggest pathological α‐syn involvement of hippocampal neurons likely represents a clinicopathological correlate of cognitive impairment in MSA.
eP‐ND‐A225
Beta‐amyloid is only seen in the extracellular compartment in diagnostic brain biopsies from idiopathic normal pressure hydrocephalus patients
S. Libard 1,2, M. Hodik1,3, K. G. Cesarini4, A. Dragomir1,2, I. Alafuzoff2
1Uppsala University, Immunology, Genetics and Pathology, Uppsala, Sweden; 2Uppsala University Hospital, Surgical Pathology, Uppsala, Sweden; 3Uppsala University, Bio Vis Platform, Uppsala, Sweden; 4Uppsala University Hospital, Neurosurgery, Uppsala, Sweden
Introduction: Beta‐amyloid (Aβ), one of the hallmark lesions of Alzheimer's disease, aggregates within the extracellular (EC) compartment of the grey matter of the brain. During the disease progress Aβ undergoes biochemical changes, producing toxic variants. Some of the Aβ variants are proposed to be detected in the intracellular (IC) compartment.
Objectives: To study cellular compartmentalisation of Aβ in diagnostic brain biopsies from idiopathic normal pressure hydrocephalus (iNPH) subjects using light microscopy (LM) and electron microscopy (EM).
Patients and Methods: During 2018–2019, brain biopsies for both LM and EM were obtained from 12 iNPH patients. Three of the subjects displayed representative grey matter in both the LM and EM samples. The tissue samples from these three iNPH patients were immunohistochemically (IHC) stained both for LM and EM with various Aβ antibodies (Ab) and an amyloid precursor protein (APP) Ab and assessed in regard to compartmentalisation.
Results: Aβ was detected in five biopsies. The three subjects with representative EM material were in this cohort. In LM, high level of EC Aβ aggregates was visualized in all subjects with 4G8, 6F/3D, unmodified (um) Aβ (7H3D6) and in two subjects with pyroglutamylated (py) Aβ (N3pE). The py Aβ was moderate in one biopsy. The phosphorylated (p) Aβ (1E4E11) was expressed at low level in one subject and at moderate level in two biopsies. The APP was expressed in all samples. Using the EM‐IHC the Aβ 4G8, 6F/3D and py Aβ was detected in all samples whereas the um and p variants were absent. The Aβ staining was located extracellularly with no specific signal within the IC compartment. The APP was seen both IC and EC.
Conclusion: All Aβ markers displayed EC localisation in both LM and EM, reflecting the pathological EC accumulation of Aβ in the human brain. No IC Aβ pathology was detected. The APP was visualized both IC and EC which corresponds to the localisation of the protein in membranes of cells and organelles.
NEUROIMMUNOLOGY
S05‐NI‐A226
Myelin insulation as a risk factor for axonal degeneration in autoimmune demyelinating disease
E. Schäffner1,2, M. Bosch Queralt 1, J. M. Edgar3, M. Lehning1, J. Strauß4, N. Fleischer1, T. Kungl5, P. Wieghofer5,6, S. A. Berghoff2,7, T. Reinert1,8, M. Krueger5, M. Morawski9, W. Möbius2, A. Barrantes‐Freer1, J. Stieler9, T. Sun2, G. Saher2, M. H. Schwab1, C. Wrede10, M. Frosch11, M. Prinz11,12,13, D. S. Reich14, A. Flügel4, C. Stadelmann15, R. Fledrich2,5, K. A. Nave2, R. M. Stassart1,2
1Paul‐Flechsig Institute of Neuropathology, Leipzig, Germany; 2Max‐Planck‐Institute of Experimental Medicine, Department of Neurogenetics, Goettingen, Germany; 3Institute of Infection, Immunity and Inflammation, College of Medical Veterinary and Life Sciences, University of Glasgow, Glasgow, United Kingdom; 4Institute of Neuroimmunology, University Medical Center Göttingen, Goettingen, Germany; 5Institute of Anatomy, Leipzig University, Leipzig, Germany; 6University of Augsburg, Cellular Neuroanatomy, Institute of Theoretical Medicine, Medical Faculty, Augsburg, Germany; 7German Center for Neurodegenerative Diseases (DZNE), Munich, Germany; 8Max‐Planck‐Institute for Human Cognitive and Brain Sciences, Department of Neurophysics, Leipzig, Germany; 9Paul‐Flechsig‐Institute of Brain Research, Leipzig University, Leipzig, Germany; 10Institute of Functional and Applied Anatomy, Research Core Unit Electron Microscopy, Hannover Medical School, Hannover, Germany; 11University of Freiburg, Institute of Neuropathology, Medical Faculty, Freiburg i. Br., Germany; 12Centre for NeuroModulation (NeuroModBasics), University of Freiburg, Freiburg i. Br., Germany; 13Signalling Research Centres BIOSS and CIBSS, University of Freiburg, Freiburg i. Br., Germany; 14Translational Neuroradiology Section, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, Bethesda, MD, United States; 15University Medical Center Göttingen, Institute of Neuropathology, Goettingen, Germany
Axonal degeneration determines the clinical outcome of multiple sclerosis (MS), and is thought to result from autoimmune‐mediated demyelination and exposure of denuded axons to inflammatory damage. Myelin is hence widely considered a protective structure for axons in MS. However, axonal pathology is visible already in early stages of autoimmune demyelination, prior to the overt loss of myelin. We here therefore challenged the view of myelin as an exclusive axon protectant and examined axonal pathology as a function of myelin insulation in human MS and its mouse models. Together with a genetic manipulation of myelination in murine autoimmune encephalomyelitis, we show that myelin ensheathment itself increases the risk of axons to degenerate under inflammatory conditions. We propose a model in which for axons in an autoimmune environment, not the absence but persistence of myelination by dysfunctional oligodendrocytes turns fatal for axonal survival.
S05‐NI‐A227
Neuroprotective effect of a ganglioside‐containing drug on allergic autoimmune encephalomyelitis
H. Zanginyan 1, G. Ghazaryan1, L. Hovsepyan1
1Institute of Molecular biology NAS of Armenia, Experimental Biology, Yerevan, Armenia
Aims: Experimental autoimmune encephalomyelitis (EAE) in rats is an experimental model of human multiple sclerosis. The aim of the work was to study the effect of ganglioside‐containing drugs on the development of free radical lipid oxidation, protein oxidative modification in the brain and spinal cord in rats with experimentally induced allergic encephalitis. As a therapeutic agent, we used the drug Cronassial, the structure of which includes mono‐di‐tri‐sialgangliosides.
Methods: The experiments were conducted using 30 inbred white rats weighing 180–200 g. EAE was induced by immunization homogenate of bovine spinal cord+ Freund's adjuvant, Complete according to the immunization protocol. Lipid peroxidation activity was assessed by the content of hydroperoxides and Malone dialdehyde. The content of diene and triene conjugates, Schiff bases were registered by Deryugina methodology. The level of oxidative modifications of the proteins in the homogenate of brain was evaluated by the content of carbonyl derivatives of amino acids in proteins.
Results: Cronassial administration resulted in partial normalization of oxidative processes of proteins. Myelin destruction is considered as a universal mechanism of reaction to damage. In case of progression of demyelination and in case of damage of 40%–60% of all myelin sheath different neurological syndromes are developed, which are generally called demyelinating diseases. We suppose that one of the most probable reasons of myelin damage may be increased formation of the products of oxidative stress—peroxides, hydroperoxides, oxidized proteins. This leads to mitochondrial disfunction, lack of energy necessary for the normal conduction of cellular processes.
Conclusions: Therefore, the obtained data indicates of neuroprotector and antioxidant effects of Cronassial upon its administration to the animals with autoimmune encephalomyelitis.
S05‐NI‐A228
Multimodal non‐invasive longitudinal retinal imaging reveals optic neuritis precedes retinal pathology in experimental autoimmune encephalomyelitis
R. Raspe 1,2, R. Günther3, R. Uecker1,2, F. Paul4,5, R. Niesner3, H. Radbruch1, A. E. Hauser2,6
1Charité—Universitätsmedizin Berlin, Institute of Neuropathology, Berlin, Germany; 2German Rheumatism Research Center, Immunodynamics, Berlin, Germany; 3German Rheumatism Research Center, Biophysics, Berlin, Germany; 4Charité—Universitätsmedizin Berlin, NeuroCure Clinical Research Center, Berlin, Germany; 5Charité—Universitätsmedizin Berlin, Department of Neurology, Berlin, Germany; 6Charité—Universitätsmedizin Berlin, Department of Rheumatology, Berlin, Germany
Introduction: As the only part of the central nervous system accessible to optical imaging, the retina can serve as a “window to the brain,” providing unique insight into the pathology of neuroinflammatory diseases.
Objectives: Combining an imaging modality already established in clinical diagnostics with pre‐clinical intravital microscopy, our goal was to harness the optical accessibility of the retina to gather insight into the interplay of structural and functional retinal pathology in the course of neuroinflammation.
Materials and Methods: Mice with fluorescent microglia and myeloid cells as well as mice carrying a reporter construct indicating Ca2+ levels in neurons in addition to red fluorescence in myeloid cells were immunized using MOG35–55 peptide to induce experimental autoimmune encephalomyelitis. Combined in vivo retinal two‐photon microscopy (2PM) and optical coherence tomography (OCT) was performed longitudinally over the course of one month of disease. Retinae and optic nerves of imaged mice were histologically analyzed at different stages of disease.
Results: In vivo, migration of CX3CR1+ cells towards the optic nerve head was observed at an early stage of disease (7 days post immunization = dpi). Over the course of OCT measurements, healthy adolescent control mice displayed residual thickening of the inner retinal layers which was absent in EAE mice. As confirmed in higher‐resolution post‐mortem imaging, activation of resident retinal mononuclear cells as well as neuronal stress could be detected only after clinical peak of disease (21 and 28 dpi). Notably, signs of optic neuritis and upstream retinal pathology appeared even in the absence of motor symptoms.
Conclusion: Using a unique combination of retinal 2PM and OCT in the same beam path, we could show that retinal pathology in EAE is preceded by in vivo observable and in vitro confirmed recruitment of immune cells towards the optic nerve head, independent of clinical signs of disease.
S05‐NI‐A229
Progressive multifocal leukoencephalopathy (PML), diagnostic approach in a country with a developing economy—A case report
B. Diaz‐Gomez1, S. L. Rojas‐Soto 2
1Centro de Tratamiento e Investigación sobre Cáncer Luis Carlos Sarmiento Angulo (CTIC)/Clìnica Colsanitas, Bogotá‐Colombia, Cundinamarca, Bogotá, Colombia; 2Laboratorio Clínico Hematológico LTDA., Pathology, Medellín, Colombia
Introduction: Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of the central nervous system and diffuse swelling, a severe condition due to the presence of JC polyomavirus (JCV), affecting oligodendrocytes, and derived from innate or acquired cellular immunity deficiency.
Objectives: Make a pathology diagnosis in a limited resource setting of this rare entity. Highlight the importance of proper diagnosis requires radiologic and clinical correlation in patients with progressive multifocal leukoencephalopathy in our practice.
Patients and Methods: A 44‐year‐old man stage C3 HIV positive with recent initiation of antiretroviral therapy (ART), latent syphilis, and behavioural disturbance with rhombencephalitis, a magnetic resonance imaging (MRI) scan was performed with a hyperintensity of the cerebellar hemisphere and right middle cerebellar peduncle, a resection was made.
Results: Microscopic examination revealed a cerebellar parenchyma, with the presence in white matter, areas with cytomegalic cells, hyperchromatic cells and atypical glial cells with accumulations of histiocytes. Immunohistochemistry enhances reactive gliosis with PFGA, CD68 enhances scattered histiocytes, Olig2 and p53 are positive in cells of interest (atypical cytomegalic). Negativity for toxoplasma, and Ki67 of 8%. Histochemistry stains show slight axonal decrease with neurofilament and decreased myelination with Luxol fast blue. Methenamine silver and Ziehl Neelsen, confirms the absence of fungi and acid‐fast bacilli, respectively.
Conclusion: The diagnosis of multifocal progressive multifocal leukoencephalopathy (PML) is supported, and a proper histopathological evaluation with an adequate neuroimaging findings if JCV DNA test is not available (polymerase chain reactions or in situ hybridization), is considered of great importance and being aware of these unusual diseases, allows an adequate and early treatment.
S07‐NI‐A230
Progressive encephalomyelitis with rigidity and myoclonus with glycine receptor and GAD65 autoantibodies—Clinico‐pathological correlates and potential pathomechanisms of a rare disease
M. Winklehner 1,2, J. Wickel3, E. Gelpi2, D. Brämer3, V. Rauschenberger4, A. Günther3, J. Bauer5, G. Ricken2, C. Villmann4, R. Höftberger2, C. Geis3
1Kepler University Hospital, Department of Neurology, Linz, Austria; 2Medical University of Vienna, Division of Neuropathology and Neurochemistry, Department of Neurology, Vienna, Austria; 3Jena University Hospital, Section of Translational Neuroimmunology, Department of Neurology, Jena, Germany; 4Julius‐Maximilians‐University of Würzburg, Institute of Clinical Neurobiology, University Hospital, Wuerzburg, Germany; 5Medical University of Vienna, Department of Neuroimmunology, Center for Brain Research, Vienna, Austria
Introduction: Progressive encephalomyelitis with rigidity and myoclonus (PERM) is a severe form of stiff‐person spectrum disorder that can be associated with antibodies against surface antigens (glycine receptor [GlyR] or dipeptidyl‐peptidase‐like protein 6), and antibodies against intracellular antigens (glutamic acid decarboxylase [GAD65] or amphiphysin).
Objectives: To report a clinical case and postmortem neuropathological findings of a patient with PERM with GlyR and GAD65 antibodies.
Patients and Methods: A 74‐year‐old man presented with myoclonus and pain of the lower extremities. Despite therapy he developed severe motor symptoms, hyperekplexia, a pronounced startle reflex, hallucinations, and dysautonomia. Immunotherapy comprised corticosteroids, IVIG, plasma exchange, immunoadsorption, cyclophosphamide, and bortezomib. Intensive care treatment and permanent isoflurane sedation was required for more than 20 weeks. He died 10 months after onset. No tumor was detected. We performed neuropathology and immunohistochemistry on formalin‐fixed and paraffin‐embedded brain tissue of the case and controls.
Results: Inflammation and tissue damage predominantly affected GlyR rich expression sites, representing a pallido‐nigro‐dentato‐bulbar‐spinal degeneration pattern. Neuropathology revealed a diffuse neuronal loss and massive astro‐ and HLA‐DR+ microgliosis. Neurons showed pSTAT1, MHC‐I and GRP78 upregulation. Inflammation was moderate and characterized by parenchymal and perivascular CD8+ T cells and single CD20+/CD79a+ B/plasma cells mainly within the meninges. Focal tau‐positive thread‐like deposits were detected in highly gliotic areas involving the dorsal vagal and solitary nuclei. In the spinal cord, GlyR and glycine transporter 2 expression were strongly reduced.
Conclusion: Clinico‐pathological correlates in this rare PERM case show both antibody‐ and T cell‐mediated pathomechanisms possibly leading to irreversible neuronal damage and therapeutic limitations.
S07‐NI‐A231
Microglial engulfment of GABAergic interneurons in stiff‐person syndrome
T. Ikeda 1,2,3, H. Yabata2,4, Y. Riku2,5, H. Miyahara2, M. Tada3, G. Yamada3, K. Yamada3, K. Kamimoto3, R. Nakamura4, S. Sugiyama4, I. Yamakawa4, A. Akagi2, J. Sone2, Y. Hashizume6, Y. Iwasaki2, M. Urushitani4, N. Matsukawa1, M. Yoshida2
1Nagoya City University Graduate School of Medical Sciences, Department of Neurology and Neuroscience, Nagoya, Japan; 2Aichi Medical University, Department of Neuropathology, Institute for Medical Science of Aging, Nagakute, Japan; 3Nagoya City University East Medical Center, Department of Neurology, Nagoya, Japan; 4Shiga University of Medical Science, Department of Neurology, Otsu, Japan; 5Nagoya City University Graduate School of Medical Sciences, Department of Neurology, Nagoya, Japan; 6Fukushimura Hospital, Choju Medical Institute, Toyohashi, Japan
Introduction: Stiff‐person syndrome (SPS) is a rare chronic disorder characterised by progressive rigidity and muscle spasms affecting the axial and limb muscles. Autoimmune mechanism against inhibitory pathways mediated by γ‐amino butyric acid (GABA) was suspected, but the pathological proof of the involvement of GABAergic interneurons has not been established.
Objectives: This study aims to evaluate the involvement of GABAergic interneurons in the autopsied cases with SPS.
Materials and Methods: We performed immunohistochemical observations of glutamic acid decarboxylase (GAD) and parvalbumin (PV)‐positive neurons in the brains and spinal cords of the two SPS cases and the four controls.
Results: Anti‐GAD immunohistochemistry recognized the cytoplasm and axon terminals of the PV‐positive GABAergic interneurons. Density of the GAD‐positive neurons and terminals were spared in the SPS cases as in the controls. In the precentral gyrus of the SPS cases, microglial processes often engulfed GAD and PV‐positive neurons (Figure 1). The microglial reaction in SPS was found to be more specific to GAD/PV‐positive neurons than GAD/PV‐negative neurons; the finding was not observed in the controls. The quantitative assessment revealed that GAD/PV‐positive neurons were more frequently encircled by Iba1‐positive microglial process than GAD/PV‐negative neurons in the SPS cases. The controls showed no significant differences for it.
Conclusion: The microglial reaction against GABAergic interneurons of the precentral gyrus suggests impairment of GABAergic inhibitory pathways in SPS as a possible therapeutic target.

FIGURE 1.
S07‐NI‐A232
Role of immunoassays in the detection of onconeuronal antibodies—A retrospective study from an Australian laboratory
S. Ali 1,2, A. Cecchin2, B. Rebecca2, J. Ravindran3, D. Field3, J. King2,4, P. Pucar1,2, T. Banovic1,2
1Royal Adelaide Hospital, Clinical Immunology and Allergy, Adelaide, Australia; 2SA Pathology, Immunology, Adelaide, Australia; 3Royal Adelaide Hospital, Neurology, Adelaide, Australia; 4Womens' and Childrens' Hospital, Clinical Immunology and Allergy, Adelaide, Australia
Background: Onconeural antibodies are implicated in heterogenous clinical presentations. Commercial assays include indirect immunofluorescence (IIF) and line immunoblot (LIB). While LIB is sensitive, high rates of false positives are common. Routine confirmatory assays are currently not available in diagnostic laboratories.
Objectives: To determine frequency of positive LIB on serum and/or cerebrospinal fluid (CSF) and establish concordance with IIF and clinical presentation.
Methods: A retrospective analysis of all LIB performed over a 4‐year period on patient serum and CSF samples. Healthy control serum samples were also analysed with IIF and LIB.
Results: Of the 2097 LIBs performed, 209 (10.0%) were positive from 164 patients: 90 females (54.9%) and 74 males (45.1%) with mean age of 60 years. Amphiphysin (n = 33, 15.8%), Yo (n = 32, 15.3%), GAD65 (n = 23, 11%) and SOX‐1 (n = 17, 8.1%) were most frequent. Of the positive LIBs, 170 (81.3%) had concurrent IIF and 8 samples (4.7%) had a typical IIF pattern. Clinical relevance of a positive LIB, irrespective of IIF, was seen in 12 patients (7.3%): amphiphysin (n = 2), GAD65 (n = 3), Yo (n = 2), SOX1 (n = 2), Tr (n = 1), Hu (n = 1) and CV2 (n = 1). There were 71 healthy controls run, all with negative IIF. Eight (11.3%) had positive LIB, with three in very weak band range. The remaining five (7.0%) had a medium band (n = 4, amphiphysin, CV2, SOX1 and Yo) or strong band (n = 1, Yo). A higher average signal intensity 27 (strong band) was seen in those with clinical relevance, compared to those without (signal intensity 11/medium band) and healthy controls (signal intensity 2/negative band) (p < 0.001).
Conclusions: Positive LIB can be useful in diagnostic work up, when accompanied by ancillary tests and a high clinical suspicion. False positives are common in LIB and recognition of these is important. Commercial IIF kits as screening methods still require accompanying LIB.


S07‐NI‐A233
Viral metagenomics from formalin‐fixed paraffin‐embedded specimens
A. Albers1, E. Chteinberg1, R. Siebert1, L. Schweizer1, C. Thomas 1
1Institute of Neuropathology Münster, Muenster, Germany
Introduction: Diagnosis of viral diseases affecting the central nervous system is challenging. Using routine immunohistochemical methods, viral pathogens can often not be identified.
Objectives: To evaluate the feasibility of a next‐generation sequencing (NGS) panel with pan‐viral enrichment for unbiased viral pathogen detection from formalin‐fixed paraffin‐embedded (FFPE) specimens.
Materials and Methods: DNA and RNA from three FFPE specimens with known viral infections (HIV, tick‐borne encephalitis, and JC polyomavirus) and DNA from two controls (EBV‐positive lymphoma cell lines) were extracted. After library preparation and target enrichment with the Comprehensive Viral Research Panel (Twist Bioscience), samples were sequenced on a NextSeq device. In addition, two FFPE specimens (tick‐borne encephalitis and JC polyomavirus) were also sequenced without viral enrichment. Data analysis was performed with Kraken2 using the standard database and subsequent alignment to viral reference genomes.
Results: Samples were sequenced with a median read depth of 15 million read pairs per sample. The average fraction of viral reads was 52% (range, 0.5%–99.6%) and the vast majority of remaining reads were assigned as host reads (Homo sapiens). In all five samples, the associated viral pathogens were detected with a median viral coverage of 99.7% and an average read depth of 13,894X. For comparison, two FFPE samples were also sequenced without target enrichment (shotgun sequencing) and showed considerably lower fraction of viral reads: 5.3% versus 99.6% (tick‐borne encephalitis virus) and 0.0042% versus 27.9% (JC polyomavirus).
Conclusion: Target enrichment with a pan‐viral NGS panel may represent a valuable method for unbiased viral pathogen detection and viral whole‐genome sequencing from FFPE specimens.
S21‐NI‐A234
Detection of SARS‐CoV‐2 viral proteins and genomic sequences in the human brainstem
A. Emmi 1, S. Rizzo2, L. Barzon3, M. Sandre1, E. Carturan2, A. Sinigaglia3, G. Cosco1, S. Riccetti3, M. Della Barbera2, A. Tushevski1, V. Macchi1, A. Antonini1, M. De Gasperi2, C. Basso2, R. De Caro1, A. Porzionato1
1University of Padova, Department of Neuroscience, Padova, Italy; 2University of Padova, Department of Cardio‐Thoracic‐Vascular Sciences & Public Health, Padova, Italy; 3University of Padova, Department of Molecular Medicine, Padova, Italy
Question: Since its initial outbreak in 2019, the COVID‐19 pandemic has raised the question whether frequently‐reported neurological manifestations are caused by direct viral invasion of the central nervous system (CNS) by the disease's causative agent, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), or if other mechanisms, such as systemic inflammation, represent the main mediators of neurological impairment.
Methods: We assess the neuropathological alterations in 24 COVID‐19 patients and 18 matched controls who died due to pneumonia/respiratory failure.
Results: Aside from a wide spectrum of neuropathological alterations, mostly including hypoxic‐ischemic injury and small vessel thromboses, SARS‐CoV‐2‐immunoreactive neurons were detected in the medulla and in the substantia nigra of 5 COVID‐19 subjects. Viral RNA was also detected by RT‐PCR. Inflammatory perturbations, lympho‐monocytic infiltrates, M2 perivascular macrophages and reactive microglia with a pro‐inflammatory phenotype were detected. Topographic quantification of reactive microglia revealed an anatomically segregated pattern of inflammation within affected brainstem regions, and was higher when compared to controls.
Conclusions: The findings of our study suggest the possibility that, although not frequently, SARS‐CoV‐2 may gain access to specific regions of the CNS [1]. Yet, neuropathology encountered in COVID‐19 subjects is mostly determined by hypoxic‐ischemic injury and inflammation. Future studies are required to determine whether or not SARS‐CoV‐2 neurotropism is present in COVID‐19 survivors suffering from the long‐term effects of infection, and its role in long‐term neurological sequelae.
Reference: [1] Emmi A, et al. Detection of SARS‐CoV‐2 viral proteins and genomic sequences in human brainstem nuclei. npj Parkinsons Dis. 2023;9:25.

FIGURE 1 SARS‐CoV‐2 N protein immunofluorescence in the midbrain.
S21‐NI‐A235
Persistence of SARS‐CoV‐2 in the brain—Truth or myth?
J. Radke 1, J. Meinhardt2, T. Aschman2, L. Chua3, V. Farztdinov4, E. Friebel2, J. Franz5, K. Peters1, C. Thomas5, S. Streit2, R. v. Manitius2, A. Osterloh6, W. Stenzel2, C. Stadelmann‐Nessler5, F. L. Heppner2, M. Mülleder4, C. Conrad3, H. Radbruch2
1Universitätsmedizin Greifswald, Pathology, Greifswald, Germany; 2Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 3Berlin Institute of Health at Charité—Universitätsmedizin Berlin, Berlin, Germany; 4Charité—Universitätsmedizin Berlin, Berlin, Germany; 5University Medical Center Gottingen, Neuropathology, Goettingen, Germany; 6Universitatsklinikum Ulm, Pathology, Ulm, Germany
Introduction: In COVID‐19 neurological alterations are noticed during the systemic viral infection. Various pathophysiological mechanisms on the central nervous system (CNS) have been suggested in the past years, including the viral neurotropism hypothesis and a viral persistence in the brain.
Objective: To investigate long‐term changes and cytotoxic effects in the CNS due to the systemic inflammation.
Materials and Methods: We profile single‐nucleus transcriptomes and proteomes of brainstem tissue from N = 21 deceased COVID‐19 patients and N = 9 controls who underwent rapid autopsy. Patients were divided into two groups, namely “acute” (n = 10) and “late” (n = 11) depending on whether death occurred within 14 days from the beginning of symptoms or more than 14 days, respectively.
Results: We detect a disease phase‐dependent inflammatory type‐I interferon response in acute COVID‐19 which levels off in late COVID‐19 cases. Integrating single‐nucleus RNA sequencing and spatial transcriptomics, we could localize two transcriptomic patterns of reaction to severe systemic inflammation. One neuronal pattern with direct focus on cranial nerve nuclei and one pattern diffusely affecting the whole brainstem rather reflecting a bystander effect mediated via the vascular unit.
Conclusion: Our results indicate that even without neurotropism of SARS‐CoV‐2, the CNS tissue activates highly protective mechanisms, which also cause functional disturbances that may explain the neurological symptoms of COVID‐19, triggered by strong systemic type‐I IFN signatures in the periphery. We could not find any direct or indirect signs of viral persistence in the CNS. The late disease phase shows a resolution of the inflammatory imprint detected during acute infection.
S21‐NI‐A236
Multifactorial white matter damage in the acute phase and pre‐existing conditions may drive cognitive dysfunction after SARS‐CoV‐2 infection—Neuropathology‐based evidence
E. Gelpi 1, S. Kotz1, M. Beyerle2, S. Wischnewski3, V. Harter4, H. Kirschner4, K. Stolz5, C. Reisinger5, E. Lindeck‐Pozza6, A. Zoufaly7, M. Leoni8, G. Gorkiewicz8, M. Zacharias8, C. Haberler1, J. Hainfellner1, A. Wöhrer1, S. Hametner1, T. Rötzer1, T. Voigtländer1, G. Ricken1, V. Endmayr1, C. Haider1, S. Lang9, I. Simonitsch‐Klupp9, C. Kornauth9, M. Nackenhorst9, J. Kläger9, R. Kain9, A. Chott10, R. Wasicki10, R. Krause11, G. Weiss12, J. Löffler‐Rag12, T. Berger1, P. Moser13, A. Soleimann13, M. Asslaber8, R. Sedivy4, N. Klupp5, M. Klimpfinger4,9, D. Risser5, H. Budka1, L. Schirmer3, A. K. Pröbstel2, R. Höftberger1
1Division of Neuropathology and Neurochemistry, Department of Neurology, Medical University of Vienna, Vienna, Austria; 2University Hospital and University of Basel, Basel, Switzerland; 3Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany; 4Klinik Favoriten, Department of Pathology, Vienna, Austria; 5Medical University of Vienna, Department of Forensic Medicine, Vienna, Austria; 6Klinik Favoriten, Department of Neurology, Vienna, Austria; 7Klinik Favoriten, Intensive care unit, Vienna, Austria; 8Medical University of Graz, Institute of Pathology, Graz, Austria; 9Medical University of Vienna, Department of Pathology, Vienna, Austria; 10Klinik Ottakring, Department of Pathology, Vienna, Austria; 11Medical University of Graz, Div Infectious Diseases, Graz, Austria; 12Medical University Innsbruck, Internal Medicine, Innsbruck, Austria; 13Medical University Innsbruck, Department of Pathology, Innsbruck, Austria
Introduction: There is an urgent need to better understand the mechanisms underlying acute and long‐term neurological symptoms after COVID‐19.
Objective: Neuropathological studies can contribute to a better understanding of some of these mechanisms.
Materials and Methods: Detailed postmortem neuropathological analysis of 32 patients who died due to COVID‐19 during 2020 and 2021 in Austria.
Results: All cases showed diffuse white matter damage with a diffuse microglial activation of variable severity, including one hemorrhagic leukoencephalopathy. Some cases revealed mild inflammatory changes, including olfactory neuritis (25%), nodular brainstem encephalitis (31%), and cranial nerve neuritis (6%), which were similar to those observed in non‐COVID‐19, severely ill patients. One previously immunosuppressed patient developed acute herpes simplex encephalitis. Acute vascular pathologies (acute infarcts 22%, vascular thrombosis 12%, diffuse hypoxic–ischemic brain damage 40%) and pre‐existing small vessel diseases (34%) were frequent findings. Moreover, silent neurodegenerative pathologies in elderly persons were common (AD neuropathologic changes 32%, age‐related neuronal and glial tau pathologies 22%, Lewy bodies 9%, argyrophilic grain disease 12.5%, TDP43 pathology 6%).
Conclusion: Our results support some previous neuropathological findings of apparently multifactorial and most likely indirect brain damage in the context of SARS‐CoV‐2 infection rather than virus‐specific damage, and they are in line with the recent experimental data on SARS‐CoV‐2‐related diffuse white matter damage, microglial activation, and cytokine release.

FIGURE 1.
S21‐NI‐A237
Cerebral intussusceptive angiogenesis—Distinct small vessel pathology associated with COVID‐19
V. Umathum 1,2, R. Dettmeyer3, C. Mawrin4, T. Acker1, A. Schänzer1
1Justus‐Liebig‐University Giessen, Institute of Neuropathology, Giessen, Germany; 2Bundeswehrkrankenhaus Ulm, Institute of Pathology and Molecular Pathology, Ulm, Germany; 3Justus‐Liebig‐University Giessen, Institute of Forensic Medicine, Giessen, Germany; 4Otto‐von‐Guericke‐University Magdeburg, Institute of Neuropathology, Magdeburg, Germany
Introduction: COVID‐19 patients have been reported to display cerebral small vessels pathology, including microthrombi and vasculitis/endotheliasis. Intussusceptive angiogenesis (IA) is defined as the splitting of a pre‐existing blood vessel. The exact mechanism is not yet fully understood, but it is discussed that pericytes invaginate from the outside and form a pillar that promotes the splitting. IA is a striking pathology observed in lungs of COVID‐19 patients. In our study, we investigated whether IA is present in COVID‐19 brains and might contribute to CNS pathology.
Patients and Methods: Morphometric analyses were performed on brain tissue from patients who died of COVID‐19 between 03/2020 and 06/2021 (C19: n = 26). Three sex‐ and age‐matched groups of patients with sepsis (Ctr1: n = 13), with chronic lung disease (Ctr2: n = 5) and patients without chronic cardio‐pulmonary disease (Ctr3: n = 12) served as controls. We analysed IA, defined as at least 2 adjacent vessels, on HE‐stained sections and by immunohistochemistry with alpha smooth muscle actin (αSMA) from cortex (CX) and oblongate medulla (MO). Sections were digitalised and IA/mm2 were evaluated by NDP.view 2.
Results: IA were present with occasional microthrombosis in all C19 brains (Figure 1; mean: CX = 0.24 IA/mm2; MO = 0.19 IA/mm2;) which was significantly higher compared to all control groups (ANOVA CX: p < 0.0001; MO: p = 0.0023; Ctr1 mean: CX = 0.06 IA/mm2; MO = 0.05 IA/mm2, Ctr2 mean: CX = 0.08 IA/mm2; MO = 0.04 IA/mm2, Ctr3 mean: CX = 0.04 IA/mm2; MO = 0.02 IA/mm2). IA in the neocortex was only seen in the grey matter.
Discussion: The presence of IA in COVID‐19 brains is consistent with studies reporting IA in COVID‐19 lungs, suggesting a similar pathomechanism. Therefore, cerebral IA may contribute to the neurological symptoms observed in some COVID‐19 patients, expanding our understanding of COVID‐19 CNS pathology beyond microthrombosis and highlighting the need for further investigation into the mechanisms of IA.

FIGURE 1.
S21‐NI‐A238
Post‐COVID syndrome is associated with capillary alterations, macrophage infiltration and distinct transcriptomic signatures in skeletal muscles
T. Aschman 1, E. Wyler2, O. Baum3, A. Hentschel2, F. Legler3, A. Roos4, F. L. Heppner1, H. Radbruch1, F. Paul3, C. Scheibenbogen3, W. Stenzel1, N. Dengler3
1Charité—Universitätsmedizin Berlin, Institute of Neuropathology, Berlin, Germany; 2MDC, Berlin, Germany; 3Charité—Universitätsmedizin Berlin, Berlin, Germany; 4University Children's Hospital, Department of Pediatric Neurology, Duisburg‐Essen, Germany
Introduction: The SARS‐CoV‐2 pandemic not only resulted in millions of acute infections worldwide, but also caused innumerable cases of post‐infectious syndromes, referred to as “long COVID” or “post‐COVID syndrome.” Due to the heterogeneous nature of symptoms and scarcity of available tissue samples, little is known about the underlying mechanisms.
Objectives: The objective of our study was to find out whether patients with post‐COVID‐syndrome showed morphological and molecular correlates on the tissue‐level of the skeletal musculature.
Patients and Methods: Eleven patients suffering from enduring fatigue and post‐exertional malaise that first occurred after an infection with SARS‐CoV‐2 and that could not be explained by alternative diagnoses were included, and Musculus vastus lateralis biopsies were obtained in average one year after initial infection. Two different groups of age‐matched samples from the same muscle region obtained prior to 2019 served as controls, the first one consisting of patients with clinical symptoms affecting the musculature but for whom no histological abnormalities could be observed, and the second consisting of samples in which a selective atrophy of type‐2b‐fibers was present, an unspecific finding associated with muscle disuse and deconditioning.
Results: Compared to two independent historical control cohorts, patients with post‐COVID exertion intolerance had fewer capillaries, thicker capillary basement membranes and increased numbers of CD169+ macrophages. SARS‐CoV‐2 RNA could not be detected in the muscle tissues, but transcriptomic analysis revealed distinct gene signatures compared to the two control cohorts, indicating immune dysregulations and altered metabolic pathways.
Conclusion: We conclude that the initial viral infection may have caused immune‐mediated structural changes of the microvasculature, potentially explaining the exercise‐dependent fatigue and muscle pain.


FIGURE 2.
S21‐NI‐A239
Berlin autopsy study on cause of death upon vaccinations against SARS‐CoV‐2
T. Kock 1, M. Windgassen1, A. Osterloh2, S. Streit2, E. Friebel2, R. von Manitius2, J. Meinhardt2, J. Melchert3, V. Corman3, H. Radbruch2, M. Tsokos1, F. L. Heppner2
1Charité—Universitätsmedizin Berlin, Legal Medicine, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 3Charité—Universitätsmedizin Berlin, Virology, Berlin, Germany
Introduction: Forensic autopsies are the standard procedure to determine the cause of death in uncertain deaths upon medical interventions. Autopsy studies linking death to possible side‐effects of vaccinations against SARS‐CoV‐2 are rare and often reported as case studies with a small N. To rule out other reasons of death upon SARS‐CoV‐2 vaccination, such as infections, intoxications or death by natural cause, and to get insight into severe co‐morbidities possibly being the cause of death, an autopsy study with a high N is required.
Objectives: Systemic analysis of autopsy cases upon vaccination against SARS‐CoV‐2 by the Berlin‐based institutes of forensic pathology (Germany).
Patients and Methods: We analyzed autopsies with a suspected link to SARS‐CoV‐2 vaccination by the prosecutor office between 01/2021 and 12/2022 performed by the two institutions for forensic pathology in Berlin. We included information regarding age, sex, co‐morbidities, cause of death upon autopsy, vaccinations status, and potential intoxications.
Results: Seventy‐six post SARS‐CoV‐2 vaccination cases could be included comprising 30 male and 36 female subjects, with an age range from 19 to 92 years (mean 68). Duration between vaccination and death ranged from 1 to 114 days with a mean of 6 days. The cohort included SARS‐CoV‐2 vaccinations of all sorts approved by the European Medicines Agency (EMA), with a majority of mRNA vaccinations (58 cases). Main cause of death based on the autopsy findings were: cardiovascular diseases n = 38, pulmonary or cerebral thromboembolic events n = 9, breakthrough infections (Covid‐19) n = 5, cerebro‐vascular diseases n = 7, pulmonal diseases n = 6, multi organ failure n = 4, renal failure n = 2, hyperglycemia n = 1. Four cases remained unclear.
Conclusion: Lethal complications of SARS‐CoV‐2 vaccinations do occur, but are rare. In the assessed Berlin, yet rather small cohort, 33 cases had a defined cause of death, which appeared not to be directly related to SARS‐CoV‐2 vaccination while in 43 cases there a competing influences next to SARS‐CoV‐2 vaccination. Only in four cases, SARS‐CoV‐2 vaccination appeared to have a conditional causality.
PS5‐NI‐A241
CD8 T cell‐mediated enteric ganglionitis may induce severe gastrointestinal dysmotility
A. Brunn 1, M. Sanchez‐Ruiz2, M. Montesinos‐Rongen2, C. Rudroff3, G. Pfitzer4, M. Deckert1
1University Hospital Düsseldorf and Medical Faculty, Heinrich Heine University Düsseldorf, Institute of Neuropathology, Duesseldorf, Germany; 2Faculty of Medicine and University Hospital of Cologne, Department of Neuropathology, Cologne, Germany; 3Evangelisches Krankenhaus Köln Weyertal, Department of General and Visceral Surgery, Cologne, Germany; 4Faculty of Medicine and University Hospital of Cologne, Institute of Vegetative Physiology, Cologne, Germany
Introduction: Enteric nervous system (ENS) disturbance is a frequent complication in patients with a variety of inflammatory bowel diseases. The prominent loss of myenteric neurons in experimental colitis raises the question which mechanisms link inflammation and neuronal damage.
Objective: We addressed the topic whether an autoimmune reaction is causative for the severe neuronal loss in patients with gastrointestinal (GI) dysmotility.
Patients and Methods: Full‐thickness colonic specimens of 30 patients with GI dysmotility of unknown origin were investigated after exclusion of well‐known reasons for GI dysmotility by thoroughly clinical investigation.
Results: In all patients, inflammation targeted the ENS with two stages of disease depending on the course of clinical symptoms. CD8 T cell‐dominated inflammation was active in patients with a clinical history of less than six years. CD8 T cells were closely attached to vital neurons of the submucosal and myenteric plexus which had upregulated MHC class I antigen. In contrast, only single CD4 T cells and CD68 macrophages were scattered throughout the intestinal wall but not preferentially associated with enteric neurons. Beyond six years, there was no evidence for inflammation; remarkably, 74.8% of enteric neurons of the submucosal and myenteric plexus had vanished. Remaining neurons were mostly apoptotic. These clinical data were mimicked by murine experimental enteric ganglionitis.
Conclusion: The study points to a high vulnerability of ENS neurons to an autoimmune CD8 T‐cell attack which, ultimately, destroyed enteric neurons, clinically manifesting as GI dysmotility. It will be important to identify potential candidate neuronal autoantigens recognized by CD8 T cells and to identify patients in the active inflammatory phase to therapeutically prevent irreversible neuronal loss.
PS5‐NI‐A242
Bornavirus encephalitis serves as model disease for neurotropic virus infections
F. Liesche‐Starnecker 1, N. Jungbäck1, Y. Vollmuth2, E. Sipos1, T. Mögele1, J. Schlegel2, B. Märkl1, D. Tappe3
1University of Augsburg, Pathology, Augsburg, Germany; 2Technical University of Munich, Institute of Pathology, Munich, Germany; 3Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany
Question: The Borna disease virus 1 (BoDV‐1) and the variegated squirrel bornavirus 1 (VSBV‐1) were recently shown to cause mostly fatal encephalitis in humans. Although both forms of human bornavirus encephalitis (BVE) are extremely rare and BoDV‐1 infection occurs only in a defined endemic area, the importance for detailed knowledge about their pathogenesis lies in its model character for neurotropic virus infections. The aim of our studies is to provide a comprehensive characterization of the neuropathology and (immuno‐)pathogenesis of human BVE, including a comparison between BoDV‐1 and VSBV‐1 infection.
Method: Multiple brain autopsy specimens of nine patients with BoDV‐1 encephalitis and of three patients with VSBV‐1 infection were included. Besides standard hematoxylin/eosin stain, RNA in‐situ hybridization for BoDV‐1/VSBV‐1 and immunohistochemistry for bornaviruses, as well as cellular markers including GFAP, Iba1 and CD45 were performed for a comparative characterization of virus/reaction distribution. Furthermore, profiling of the involved neuroimmunopathological pathways was performed using the RNA‐based nCounter‐technology (Nanostring). For a detailed disaggregation of the infected neuronal and glial subpopulation, spatial transcriptomic analyses with GeoMx technology (Nanostring) were performed.
Results: BoDV‐1 and VSVB‐1 encephalitis show similar distribution patterns and neuropathological characteristics, summarized as sclerosing lymphocytic panencephalitis with formation of microglial nodules. In infections with VSBV‐1, necrotic or hemorrhagic changes are more often present compared to BoDV‐1 infection. The results of immunological profiling are pending.
Conclusion: BoDV‐1 and VSBV‐1 show similar neuropathological changes with a high recognition value. A detailed characterization of the (neuro‐)immunological processes has high importance, as it can help to understand the pathogenesis of infections with neurotropic viruses in general.
PS5‐NI‐A243
Rasmussen encephalitis in a case with mild malformation of cortical development with oligodendroglial hyperplasia and epilepsy (MOGHE) with SLC35A2 brain mosaicism
N. Fransen 1, E. Aronica2, J. H. Lee3, W. Van Hecke1, K. P. J. Braun4, A. Mühlebner1
1Utrecht University Medical Centre, Pathology, Utrecht, Netherlands; 2Amsterdam University Medical Centre, Pathology, Amsterdam, Netherlands; 3Korea Advanced Institute of Science and Technology (KAIST), Translational Neurogenetics Laboratory, Daejeon, South Korea; 4Utrecht University Medical Centre, Neurology, Utrecht, Netherlands
Rasmussen encephalitis (RE) is a severe immune mediated brain disorder leading to unilateral hemispheric atrophy, progressive neurological dysfunction and refractory epilepsy. Pathology resembles a viral or auto‐immune encephalitis; however, the etiology remains unknown. Co‐occurrence of the destructive pathology of RE in cases with mild malformation of cortical development and oligodendroglial hyperplasia and epilepsy (MOGHE) has not been described. This could have implications for understanding the pathophysiology of RE. Here we report a case with refractory epilepsy that underwent neurosurgical treatment with the pathology of both RE and mild malformation of cortical development with oligodendroglial hyperplasia and epilepsy (MOGHE). There was a SLC35A2 mosaicism with a pathogenic stop‐gain mutation (c.502C>T: p.Gln168*; somatic VAF 3.64%). Furthermore, sequencing of 6 classical RE cases for SLC35A2 brain mosaicism was performed. Histological characteristics of MOGHE were examined using both LuxolPAS as well as Olig2 and NeuN immunohistochemical stainings. One classical RE case showed a non‐pathogenic nonsense mutation in SLC35A2 (in exon 4, c.753G>A, p.W251*, in 22% of the reads). In 3/5 cases histological characteristics of MOGHE were identified (ectopic neurons in 3/5; oligodendroglial hyperplasia in 4/6; focal hypomyelination in 1/6). This case report and analysis of 6 RE cases suggest that histological and molecular characteristics of MOGHE can be identified in RE encephalitis. The occurrence of this dual pathology may have implications for the pathophysiology in RE.
PS5‐NI‐A244
Cerebral actinomycosis as a mimic lymphoma in an HIV‐infected patient—Diagnosis by stereotactic biopsy analysis
M. T. Espinosa Romero 1, B. M. Jesús Quetzalcóatl2, D. P. Duarte Mora2, L. A. Téllez Manríquez1, W. R. Toscano‐Rengifo1, D. Villa Sepúlveda3, L. A. Quintero Arias4, L. G. Chávez Macías1, T. C. Ramos Santillán4, A. Escobar España1, J. A. Bonifaz Trujillo1,5, E. Gómez Apo1
1Hospital General de México, Neuropathology, Mexico City, Mexico; 2Hospital General de México, Neurosurgery, Mexico City, Mexico; 3Hospital General de México, Pathology, Mexico City, Mexico; 4Hospital General de México, Cytopathology, Mexico City, Mexico; 5Hospital General de México, Mycology, Mexico City, Mexico
Actinomycosis is a polymicrobial infection caused by filamentous Gram‐positive bacteria. N. brasiliensis has been isolated in 87%. Skin involvement is the most common form, while CNS infection is rare. To report a case of actinomycosis in the CNS that was approached as a neoplastic lesion. A 36‐year‐old man was diagnosed with HIV infection (December 2022) with AIDS criteria. The current condition began in March 2023 with right‐sided paresthesias that progressed to hemiparesis, limiting his daily activities. On physical examination, there was central facial palsy, hypoesthesia, and limited gait. MRI revealed two intra‐axial lesions located in the left thalamus and internal capsule, with partially defined borders; T1‐hypointense and intense ring enhancement with administration of contrast medium. Spectroscopy showed increased lactate suggestive of necrosis. Due to these characteristics; the initial diagnosis of lymphoma was considered. A brain biopsy for stereotaxy was performed. In the lesion smears, a fibrillar background and abundant gemistocytes were observed, as well as the presence of inflammatory cells. In the histological sections, fragments of nervous tissue with reactive gliosis were observed, as well as scant structures with central necrotic material, thin filamentous bacterial structures with an eosinophilic border (Splendore–Hoeppli phenomenon) and highlighted by PAS stain.
Actinomycosis is considered a tropical disease of slow progression, whose etiology is polymicrobial. The opportune diagnosis has an important impact on the therapeutic and prognosis of patients, for which the pathological examination is imperative in all cases since the culture does not always allow the growth or identification of the causative agents.
Reference: [1] Ravindra N, et al. Central nervous system actinomycosis—a clinicoradiologic and histopathologic analysis. World Neurosurg. 2018;116:e362–70.
PS5‐NI‐A245
Neonatal brain aspergillosis—A case report and literature review
P. Franco del Toro1, M. A. Gonzalez Adame 1, A. Cordero Zamora1, J. C. Lona Reyes1, E. F. Acosta Gómez1
1Hospital Civil de Guadalajara “Dr. Juan I. Menchaca,” Guadalajara, Mexico
Introduction: Aspergillus is an ascomicete ubiquitous in the environment surviving under variable temperature, pH, water and nutrient conditions in soil and moist materials. Epidemiologic data is limited in children. Risk factors include primary or secondary immunodeficiencies, chronic granulomatous disease, premature newborns, among others.
Objectives: Present a case of invasive infection of brain aspergillosis in a patient without immunodeficiencies.
Clinical Summary: A 51‐day‐old infant who born at home with an uncertified midwife, with an anti‐vaccination mother who consumed cannabis and ayahuasca during pregnancy, was taken by her mother to a temazcal at her 20 day post birth, 15 days later she presented status epilepticus and then projectile vomiting, for this reason her mother brought her to the hospital. The first MRI and CT reveals parasagital necrosis and right frontal porencephalus cyst, a month later another imaging study was performed determining multiloculated hydrocephalus and periventricular calcifications. A neuronavigation was performed reporting classifying lesions and cotton like patches in left temporal region and septum pellucidum.
Results: Liquid samples were taken with histopathologic report of non‐pigmented, septated hyphae with acute angle branching. Grocott methenamine silver stain and periodic acid‐Schiff reactives on fungal structures most compatible with aspergillus sp. Primary and secondary immunodeficiencies were ruled out. She was treated with voriconazole and then switched to amphotericine B liposomal, however, her mother requested to discontinue it and change back to voriconazole. The patient died at home 15 days after her hospital released.
Conclusion: Pediatric invasive infections of aspergillus in patients without immunodeficiencies are rare. Exposure to soil, humidity and moisty spaces such as a temazcal at short ages should be avoided.
PS5‐NI‐A246
Iron handling in progressive MS
C. J. Riedl 1, D. Bormann2, G. Testa1, A. Steinmaurer3, M. Mildner4, R. Höftberger1, S. Hametner1
1Medical University of Vienna, Division of Neuropathology and Neurochemistry, Department of Neurology, Vienna, Austria; 2Medical University of Vienna, Department of Thoracic Surgery, Laboratory for Cardiac and Thoracic Diagnosis and Regeneration, Vienna, Austria; 3Medical University of Vienna, Department of Neurology, Vienna, Austria; 4Medical University of Vienna, Department of Dermatology, Vienna, Austria
Question: Disease progression in MS is difficult to measure using standard MRI or laboratory testing. This reflects a lack in our understanding of the pathomechanisms underlying relapse‐independent disease progression in MS. Chronic active lesions show an accumulation of iron‐laden myeloid cells at the rim. Conversely, the loss of iron‐sensitive MRI signal in the thalamus and other brain regions of MS patients and its correlation with disability progression have been shown by multiple groups. Histological examinations revealed that oligodendrocytes are experiencing the most pronounced loss of iron. To understand the mechanisms behind the efflux of iron from oligodendrocytes, we are studying iron transport mechanisms under inflammatory conditions in an autopsy sample, and in cell culture experiments.
Methods: Our autopsy sample comprises MS cases and controls from our tissue bank. We performed immunohistochemistry. For cell culture experiments we used primary rodent cells of the oligodendrocyte lineage and microglia. After stimulation, qPCR and immunocytochemistry were performed.
Results: Tim‐1, the receptor responsible for ferritin uptake in oligodendrocytes, was located on myelin sheaths and showed a correlation with brain iron concentration. Tim‐1 and LRP1, a scavenging receptor also involved in iron‐heme‐hemopexin uptake, were upregulated in myeloid cells at the rims of chronic active lesions. In our cell culture experiments, we found an upregulation of LRP1 in myeloid cells upon IFN‐γ exposure, while oligodendrocyte precursor cells downregulated LRP1. Tim‐2, the rodent homologue to Tim‐1 in humans, was induced by Toll‐like receptor 4 signaling in microglia.
Conclusions: Changes in the expression pattern of these receptors potentially explain the shift of iron from oligodendroglia to the myeloid cell compartment in MS, leading to iron‐depleted oligodendrocytes and iron‐laden pro‐inflammatory microglia.
PS5‐NI‐A247
Histopathological infectious brain lesions presented as ring enhancing lesions on imaging—Case series
A. Malango 1, A. Mwakimonga1, F. Fezeu2, J. Mtei3, M. Saleh4, C. Ngimba5, M. Mbezi1
1Muhimbili National Hospital, Anatomical Pathology, Dar Es Salaam, United Republic of Tanzania; 2Brainglobal, Neurology and Neurological Surgery, Salisbury, MD, United States; 3Muhimbili Orthopedic Institute, Neurosurgery, Dar Es Salaam, United Republic of Tanzania; 4Muhimbili University of Health and Allied Sciences, Radiology, Dar Es Salaam, United Republic of Tanzania; 5Agakhan Hospital, Pathology, Dar Es Salaam, United Republic of Tanzania
Introduction: Brain infections also known as encephalitis have been recognized as among most devastating diseases. These infections can be caused by bacterial, viral, fungal or parasites. Radiologically may present as ring enhancing lesions which can be a differential diagnosis of range of diseases including inflammatory, neoplastic and vascular diseases.
Methodology: Three cases submitted to Anatomical Pathology Department at Muhimbili National Hospital within a period of one year were evaluated. All cases were received from Neurosurgery Department, Muhimbili Orthopedic Institute.
Results: All patients were adults with average age of 43 years. Two of these patients were male and one female. All patients shared the similar presentation of convulsions and altered level of consciousness. Other symptoms were hemiparesis and headache. On magnetic resonance imaging (MRI), two of the three cases each had single ring enhancing brain lesion. One was located in the right frontal region and other one was on the left parietal region. The other case had multiple ring enhancing lesions on the right parietal and frontal region. All cases were associated with edema and midline shift. Histology results revealed cerebral tuberculosis for the two cases with single ring enhancing lesion and fungal meningoencephalitis for the case with multiple ring enhancing lesions on MRI.
Conclusion: Ring enhancing lesions of the brain can range from infectious to malignant conditions, distinguishing these lesions is very important so as to avoid unwarranted neurosurgery, harmful brain irradiation and toxic chemotherapy. Advanced imaging techniques may help to distinguish these lesions, however histological diagnosis is usually needed to confirm the diagnosis.
eP‐NI‐A248
Neuroimmunological profile and virus detection in human Borna virus encephalitis
N. Jungbäck 1, E. Sipos1, Y. Vollmuth2, T. Mögele1, B. Märkl1, D. Tappe3, F. Liesche‐Starnecker1
1Pathology, Medical Faculty, University of Augsburg, Augsburg, Germany; 2Institute of Pathology, School of Medicine, Technical University of Munich, Munich, Germany; 3Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany
Introduction: The highly neurotropic Borna disease virus 1 (BoDV‐1) was just recently shown to cause predominantly fatal encephalitis in humans. As newly proven zoonotic virus, only little is known about the pathogenesis and distribution pattern in the human disease.
Objectives: Aim of the study is to characterize the immunological profile in human Borna virus encephalitis in respect to the spatial distribution of viral loads.
Material and Methods: The neuroimmunological profile, viral load and morphological breakdown were based on the analysis of a complete coronary cross‐section of an autoptic retrieved brain of a patient with Borna virus encephalitis. The section was divided into 34 formalin‐fixed, paraffin‐embedded blocks, which were all stained for hematoxylin/eosin, as well immunohistochemically for GFAP, Iba‐1, CD3, CD20 and the nucleoprotein of BoDV‐1 (antibody Bo18). In addition, RNA in‐situ hybridization was performed, and quantitative PCR was used to determine viral loads. By using the Neuroimmunology Panel for the nCounter Nanostring technology, around 700 genes, involved in neuroimmunological processes, were separately analyzed in all blocks of one hemisphere plus the midline (18 blocks) to compare the immunological profile of regions with low, medium and high viral loads.
Results: By PCR, immunohistochemistry and RNA in‐situ hybridization, it can be shown that high viral loads are mainly found in the hypothalamus, thalamus, basal nuclei and brainstem. Furthermore, quantitative assessment of virus detection yielded highest sensitivity for PCR, followed by RNA in‐situ hybridization and lastly, Bo18 immunohistochemistry. The results of the immunological profiling are pending.
Conclusion: The analysis of a complete frontal brain cross‐section of a deceased with Borna virus encephalitis allows to draw conclusions about infection route and spatial characterization of the immunological pathways in a uniquely comprehensive way.
eP‐NI‐A249
The challenges of diagnosing chronic inflammatory pathologies in the central nervous system—A case report of Erdheim–Chester disease
L. Kawelke 1, M. Buthut2, F. L. Heppner1, H. Prüß2, K. Ruprecht2, H. Radbruch1
1Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neurology, Berlin, Germany
Introduction: Demyelinating diseases of the central nervous system (CNS) typically present with severe clinical signs. While Multiple sclerosis (MS) is by far the most prevalent demyelinating disease, other less frequent pathologies may remain unrecognized in the first place, thus prolonging the diagnostic process. One such rare differential diagnosis for a demyelinating lesion is Erdheim–Chester disease (ECD), which is defined by a non‐Langerhans cell histiocytosis presented by histiocytic antigens expressing foamy cells lacking classical Langerhans cell markers.
Objectives: Description of autopsy findings in an ECD and discussion of histopathological and molecular findings.
Patients and Methods: Histopathological, immunohistological stainings and molecular findings of a case with an unclear MRI‐lesion and an initial clinical diagnosis of MS were analysed.
Results: A 58 year old man showed progressive sensible and motoric impairment as well as a substantially reduced health‐related quality of life. Based on the initial clinical diagnosis of MS by a practitioner, immunotherapy was initiated, which did not result in clinical improvement. Eight months after diagnosis, the patient died suddenly. Neuropathological autopsy was conducted. Based on the histopathological presentation and the clinical work‐up with the Neurology colleagues, ECD was diagnosed and confirmed by a molecular testing of a BRAF‐mutation, while epigenetic profiling did not result in a match using the known methylation classes in the brain tumor classifier (v11.4).
Conclusion: ECD is a rare differential diagnosis of inflammatory and demyelinating CNS lesions and needs to be considered especially in unusual cases, which are difficult to classify diagnostically and/or a failure of initial therapy. While BRAF‐mutation analyses support diagnosis of ECD, methylation‐based analysis needs to be interpreted with caution in the context of histiocytosis.
eP‐NI‐A250
Mouse strain‐dependent effects of host microbiota on microglia during homeostasis and disease
D. Erny 1
1Institut für Neuropathologie, Uniklinik Freiburg, Neurozentrum, Freiburg i. Br., Germany
Introduction: As innate immune cells microglia fulfil tissue homeostasis and immune surveillance in the central nervous system (CNS) across species. However, the microglial phenotype in in a mouse strain‐dependent context is largely unknown.
Objectives: The aims of the study are to (1) characterize the microglial phenotype across various mouse strains and (2) to investigate the contribution of gut microbiota on microglia in C57BL/6, BALB/c and FVB mice under steady‐state and viral infection with LCMV. (3) We investigated the composition of the host microbiota composition in these mouse strains.
Materials and Methods: We characterized the microglial phenotype in different mouse strains by histology, 3D‐reconstructions, bulk‐ and single‐cell RNA‐sequencing. Microbiota was analyzed by shotgun metagenomics and metabolic profiling. Further, we performed microbiota transfer of C57BL/6 mice to germ‐free BALB/c and FVB mice.
Results: We revealed distinct microglial numbers, morphologies and transcriptional signatures in C57BL/6, BALB/c and FVB mice. Further, we determined that the microbiota‐dependent phenotype of microglia is mouse‐strain dependent. The microbiota from C57BL/6 mice was able to overcome the host genetics and modulate microglia properties in BALB/c and FVB mice.
Conclusion: These findings indicate that different mouse strains harbor specific compositions of the gut microbiota driving functions of microglia during health and disease.
eP‐NI‐A251
Viral propagation occurs exclusively by oligodendrocyte lineage cells in early progressive multifocal leukoencephalopathy lesions
A. Kutllovci 1, L. Stork1, M. N. I. Mlynek1, J. Franz1, C. Stadelmann‐Nessler1, I. Metz1
1University Medical Center Gottingen, Institute of Neuropathology, Goettingen, Germany
Progressive multifocal leukoencephalopathy (PML) is a devastating CNS disease caused by the JC virus (JCV) in immunosuppressed individuals. It is known that glial cells promote viral replication, but it remains unclear which cells initially become infected and permit JCV replication, leading to lesion initiation and progression. Recent studies suggested that astrocytes and glial progenitor cells are more susceptible to JCV than oligodendrocytes, but these findings have not yet been confirmed in human PML tissue. We aimed to characterize early PML lesions and identify which cell populations are responsible for lesion development and enlargement. Triple fluorescence immunohistochemical stainings were performed on post‐mortem brain tissue from a 77‐year‐old female PML patient to detect viral proteins in glial cells. The patient had suffered from chronic lymphocytic leukemia that was treated with chemotherapy including rituximab, and had died two months after PML diagnosis. Based on the number of infected/replicating cells, macrophage invasion and demyelination lesions were classified into temporal stages.
Results showed that JCV primarily targets oligodendrocytes, including oligodendrocyte precursor cells, intermediate differentiation stages, and mature oligodendrocytes, but neither infection nor replication occurred in GFAP+ astrocytes (lesion initiation, stage 1). Furthermore, viral propagation was exclusively found in oligodendrocyte subpopulations in early lesion stages (early lesion development, stages 2–4). This was associated with a major reduction in oligodendrocyte populations and a minor decrease in astrocytes. Our findings show that JCV exclusively targets all subpopulations of oligodendrocytes in early lesion stages, which underscores the importance of preventing their infection and viral replication when searching for new PML treatments. Further studies are necessary to determine whether virus‐induced or bystander mechanisms cause glial cell loss.

eP‐NI‐A252
Retrospective case finding of human Borna virus encephalitis on fluid‐ and tissue samples
J. ten Pas 1, D. Rubbenstroth2, M. Flaskamp3,4, C. Delbridge1, Y. Vollmuth1, N. Jungbäck5, B. Hemmer3,4, B. Märkl5, F. Liesche‐Starnecker5
1Technical University of Munich, Neuropathology, Munich, Germany; 2Friedrich‐Loeffler‐Institute, Diagnostic Virology, Greifswald, Germany; 3Technical University of Munich, Neurology, Munich, Germany; 4Munich Cluster for Systems Neurology, Munich, Germany; 5University Hospital Augsburg, Pathology, Augsburg, Germany
Introduction: Borna virus encephalitis in humans, caused by the Borna disease virus 1 (BoDV‐1) was described only recently. It is a rare disease in a closely circumscribed endemic area with an estimated incidence of 5–6 cases per year. Nonetheless, the accurate annual case number remains unclear.
Objective: The aim of this study was to clarify if the disease went undiscovered in past cases and to create a database for etiologically unresolved cases of encephalitis.
Materials and Methods: Serum and cerebrospinal fluid (CSF) samples of 61 patients with encephalitis of unknown etiology admitted from 2009 to 2021 to the Hospital of the Technical University of Munich (TUM) were analyzed for BoDV‐1‐reactive antibodies using indirect immunofluorescence testing. Five CSF samples were additionally tested for BoDV‐1 RNA by RT‐qPCR. The archives of the Institutes of Pathology at the TUM and the University Hospital Augsburg were searched for encephalitis cases of unknown etiology. Sixty‐nine formalin‐fixed paraffin‐embedded brain tissue samples from 31 patients (13 autopsy and 18 biopsy cases) with encephalitis matching this profile were screened immunohistochemically for BoDV‐1 antigen.
Results: All serum and CSF samples were tested negative for BoDV‐1‐reactive antibodies and all CSF samples were negative for virus‐RNA in the RT‐pPCR. In contrast, direct immunohistochemistry screening on tissue samples revealed four positive autopsy cases and one positive biopsy of a male patient surviving BoDV‐1 encephalitis.
Conclusion: In this retrospective study, Borna virus infections are found in a significant number of cases with severe encephalitis of unknown etiology in endemic areas. In rare cases, patients may survive a BoDV‐1 encephalitis. Ongoing studies on this case will investigate the circumstances of infection and survival.
eP‐NI‐A253
Early immunosuppressive therapy of human bornavirus encephalitis shows impact on the immunopathology
Y. Vollmuth 1, J. ten Pas1, N. Jungbäck2, T. Mögele2, S. Wunderlich3, F. Schmidt‐Graf3, J. Schlegel1, T. Schaller2, B. Märkl2, F. Liesche‐Starnecker2
1Technical University of Munich, Department of Neuropathology, Munich, Germany; 2University of Augsburg, Institute of Pathology, Augsburg, Germany; 3Technical University of Munich, Department of Neurology, Munich, Germany
Introduction: Borna disease virus 1 (BoDV‐1) was only recently discovered to cause usually fatal encephalitis in humans. Due to this discovery, an increasing number of human cases are retrospectively detected in Germany. The virus mediates cytotoxicity through CD8‐positive T‐lymphocytes. Initial observations indicate that early immunosuppressive therapy may have an impact on disease progression.
Objectives: The aim of this study was to compare the clinical management and immunosuppressive therapy of patients with BoDV‐1 encephalitis to neuropathological features.
Patients and Methods: Brain autopsy specimens and clinical data of 7 BoDV‐1‐infected individuals were examined. On average, 12 (range, 5–21) samples per individual were analyzed. In addition to hematoxylin/eosin staining, immunohistochemistry for BoDV‐1 (antibody Bo18) and CD45 was used to visualize the topography and extent of infection and inflammation. Sections were digitized and evaluated quantitively using Image‐J. The patients' data were taken from the clinical information system and analyzed in a firmly structured way. Clinical disease progression and treatment of patients was compared with the histological findings.
Results: The comparison of neuropathological and clinical features revealed that three patients who received an early (defined as up to day 13 after symptom onset), high‐dose steroid shot had significantly lower whole‐brain lymphocyte counts compared to those who received late or no immunosuppressive therapy, as can be expected. In addition, the immunosuppressed patients survived longer compared to patients without immunosuppression (33 [26–40] days after symptom onset compared to 27 [22–31] days).
Conclusion: The results suggest that early high‐dose steroid therapy could be a key to positively influencing the clinical course of bornavirus encephalitis. However, early diagnosis is essential for timely therapy, which underlines the importance of high awareness of this disease.
eP‐NI‐A254
Mycobacterium tuberculosis cell wall antigens induce the formation of immune complexes and the development of vasculitis in an experimental murine model
J. Cienfuegos Meza 1, M. L. Tena Suck1, C. Salinas Lara1, C. Sánchez Garibay1, A. L. Calderón Garcidueñas1, J. J. Torres Ruíz2, J. L. Montero Maravilla3, M. Castañón Arreola4, M. E. Hernández Campos5, C. Rodríguez Balderas6
1National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Neuropathology, Mexico City, Mexico; 2National Institute of Medical Ciences and Nutrition Salvador Zubiran, Immunology and Rheumatology, Mexico City, Mexico; 3National Institute of Medical Ciences and Nutrition Salvador Zubiran, Research, Mexico City, Mexico; 4Universidad Nacional Autónoma de México, Genomic sciences, Mexico City, Mexico; 5Instituto Politecnico Nacional, Postgrado, Mexico City, Mexico; 6National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Mexico City, Mexico
Introduction: Tuberculosis (TB) of the central nervous system (CNS) presents high mortality due to brain damage associated with inflammation, vasculitis, and cerebrovascular events. Formation and deposition of immune complexes (ICs) in the brain microvasculature during Mycobacterium tuberculosis (Mtb) infection might be crucial for its pathobiology. However, the relevance of ICs to Mtb antigens in the pathogenesis of CNS‐TB has been poorly explored.
Objective: To establish a murine experimental model of ICs‐mediated brain vasculitis induced by cell wall antigens of Mtb.
Methods: We administered a cell wall extract of the prototype pathogenic Mtb strain H37Rv to male BALB/c mice by the subcutaneous and intravenous route at day zero and 15, respectively. A separate group of mice received saline solution in parallel and served as controls. At given time points after the last cell wall administration, the serum concentration and deposition of ICs onto blood vessels were determined by polyethylene glycol precipitation, ELISA, and immunofluorescence. Histopathological changes in the brain, lung, spleen, liver, and kidney were evaluated by hematoxylin and eosin staining.
Results: Vasculitis developed in the brain, lung, liver, and kidney of treated animals, whereas germinal center reactions were observed at the spleen. High serum levels of ICs and vascular deposition were evident in the brain, lung, and kidneys early after the last cell wall antigen administration.
Conclusions: Cell wall Mtb antigens induce strong type III hypersensitivity reactions and the development of systemic vasculitis with brain vascular changes and meningitis, supporting a role for ICs in the pathogenesis of TB.
eP‐NI‐A255
Concurrent brain toxoplasmosis and nocardiosis—Two case reports
M. Kisiel 1, V. Bass2, C. Fong3, A. Graham1, M. Lannon2, Z. Zodar2, J. Q. Lu1
1McMaster University, Pathology and Molecular Medicine, Hamilton, Canada; 2McMaster University, Surgery/Neurosurgery, Hamilton, Canada; 3McMaster University, Radiology, Hamilton, Canada
Introduction: Both Toxoplasma gondii (TG) and Nocardia are rare causative microorganisms of brain abscesses in immunocompetent individuals, but in immunocompromised patients, toxoplasmosis and nocardiosis are relatively common opportunistic infections. In rare cases, brain abscesses contained multiple pathogens such as TG coexisting with Mycobacterium tuberculosis and Nocardia coexisting with Salmonella. While there were a few case reports in which clinically diagnosed brain toxoplasmosis turned out to be nocardiosis on pathological examination, concurrent brain toxoplasmosis and nocardiosis were not previously reported. Here, we present two cases of brain toxoplasmosis coexisting with nocardiosis.
Methods: Case reports.
Results: Case 1 was a 63‐year‐old previously healthy male who received a booster COVID‐19 vaccine to his left deltoid muscle and developed the muscle/skin Nocardia+ abscess 2–7 weeks later. In the following 4 weeks, he presented with new headache and confusion. Brain MRI revealed a single multilobulated, peripherally enhancing lesion in the left parietal lobe with intraventricular extension. The lesion was surgically excised. Pathological examination showed brain abscess containing TG (positive by immunostaining and polymerase chain reaction) and Nocardia (positive by histologic stains and tissue culture). Case 2 was a 61‐year‐old female who had a liver transplant 18 years ago with immunosuppressive therapy thereafter. Her presentation was described in a Letter to the Editor [Graham et al. 2023; https://pubmed.ncbi.nlm.nih.gov/35067253/]. Brain MRI showed multiple nodular or ring enhancing lesions bilaterally in several regions. Pathologically, the resected frontal lesion exhibited an abscess containing TG and Nocardia species.
Conclusions: Brain abscesses may be caused by concomitant TG and Nocardia; concurrence of brain toxoplasmosis and nocardiosis may occur not only in immunocompromised patients but also in previously healthy individuals.
eP‐NI‐A256
CMV encephalitis with intracranial hemorrhages in newborn/infant
N. Yeldir 1, A. Çakır1, M. S. Doğan1, N. Akalan1
1Medipol Hospital, Pathology, Istanbul, Turkey
Introduction: Viral etiologies are common causes of encephalitis. They can be sporadic or epidemic. The most common cause of sporadic viral encephalitis is the herpes family. Biopsy may be required for diagnosis or to rule out other possible diseases.
Objectives: A 50‐day‐old male patient who presented to the emergency department with fever, symptoms of convulsions and meningitis was presented.
Patients: Anemia was detected in the first examination. Cranial USG showed hemorrhagic lesion containing fluid leveling at/adjacent to the corpus callosum. Multiple nodular hemorrhages centralized to the corpus callosum and subcallosum and intraventricular hemorrhage were observed on MRI. Biopsy was taken from the adjacent corpus callosum to rule out the possibility of an intracranial tumor. In H&E sections, glial tissue around the large hematoma showed parenchymal and perivascular acute chronic inflammation with of lymphocyte/mononuclear cells, which largely effaced the normal glial tissue. Hyperchromatic large‐nucleated cells and viral cytopathic effect were noted in a few areas. Immunohistochemically, cells expressing CMV were detected in the background rich in CD3 positive T‐lymphocytes. Also, extramedullary hematopoiesis was observed.
Results: It was determined that he had CMV encephalitis. CMV was also shown in PCR in the cerebrospinal fluid. Viral encephalitis treatment was started. At the last examination, 3 months after the diagnosis, it was learned that the patient was followed up for immune deficiencies and hyperIgM syndrome.
Conclusion: CMV encephalitis is more common in newborns than adults. Clinical symptoms of hemolytic anemia, thrombocytopenia, and hyperbillurbinemia are seen. Radiologically, periventricular cysts, calcification and hemorrhage are remarkable. CMV can involve the brain and spinal cord. Necrotizing encephalitis, inclusions, microglial nodules, ventriculitis, myeloradiculitis may be seen due to CMV. It should be kept in mind that inclusions or inflammation cannot be seen always, and viral encephalitis should be kept in the differential diagnosis in newborn, elderly and immunosuppressed individuals.
eP‐NI‐A257
Clinical and radiological features of antibody positive neuromyelitis optica spectrum disorder (NMOSD) and myelin oligodendrocyte glycoprotein antibody‐associated disease (MOGAD)
R. Poyuran 1, S. Nair2, D. Narasimhaiah1
1SCTIMST, Pathology, Trivandrum, India; 2SCTIMST, Neurology, Trivandrum, India
Introduction: NMOSD and MOGAD are immune mediated demyelinating diseases. Antibody testing plays a crucial role in their diagnosis.
Objective: To compare clinical and radiological features of antibody positive NMOSD and MOGAD patients.
Methods: Antibody detection was performed using commercially available fixed cell based assay. Seventy‐five out of 652 tested cases were positive. Of which, six cases had alternate diagnosis and antibody positivity was weak and restricted to few cells.
Results: Sixty‐nine cases were included in the study, 21 were AQP4 antibody positive and 48 were MOG antibody positive.
NMOSD: Median age at onset was 18.5 years (age range: 7–55 years) with male to female ratio of 0.3:1. Infective prodrome was evident in 7 (33%) cases, with COVID‐19 infection in one. At disease onset, unilateral optic neuritis was the most common presentation (40%) followed by isolated myelitis and isolated brainstem syndrome (20% each). Relapse was noted in 67% of cases. Mean CSF IgG index was 0.6. Of the three cases tested for CSF oligoclonal bands, one showed type 3 pattern. MOGAD: Median age at onset was 23 years (age range: 4–76 years) with male to female ratio of 0.6:1. Infective prodrome was evident in 11 (23%) with three cases associated with COVID‐19 infection. COVID‐19 vaccination before onset was present in 3 cases. Unilateral optic neuritis was the most common presentation at onset (32%) followed by bilateral optic neuritis (17%) and isolated myelitis (17%). Relapse was noted in 52% of cases. Of the 10 cases tested for CSF oligoclonal bands, two showed type 3 pattern and mean CSF IgG index was 0.68.
Conclusion: Both NMOSD and MOGAD present initially as optic neuritis or myelitis. Involvement of entire cord and conus medullaris was common in MOGAD. Isolated brainstem syndrome was more common in NMOSD and isolated cerebral syndrome in MOGAD at disease onset. Incidence of relapse was more common in NMOSD associated optic neuritis and brainstem syndrome when compared with their MOGAD counterparts.
eP‐NI‐A258
Autoimmune encephalitis manifested as CD8+ T‐lymphocyte encephalitis
S. I. Kim 1, S. D. Lim2, S. H. Park 1
1Seoul National University College of Medicine, Pathology, Seoul, South Korea; 2Konkuk University School of Medicine, Pathology, Seoul, South Korea
Introduction: Autoimmune encephalitis (AIE) is a group of immunoreactive encephalitic disorders characterized by the presence or absence of identifiable neuronal autoantibodies. It is considered the most common form of acute or subacute noninfectious encephalitis. However, confirming AIE through biopsy or autopsy is rare.
Methods: Autopsy and special and immunohistochemical studies were performed with LFB, Bieschowsky, Gallyas, and antibodies to CD3, CD4, CD8, CD20, IBA‐1, beta‐amyloid, pTau(AT8), TDP43, and a‐synuclein.
Case report: In this case report, an 80‐year‐old male with a history of pulmonary tuberculosis presented with decreased appetite and confusion. MRI scans showed chronic infarct in the right cerebellum, hydrocephalus, and medial temporal atrophy. EEG results showed no epileptiform discharge. He was suspected of having the syndrome of inappropriate antidiuretic hormone secretion, and his mental state improved after medication. However, he developed paralytic ileus and died within 6 weeks of hospitalization. The brain autopsy revealed lymphocytic infiltration in the dura, leptomeninges, and gray and white matter, with CD8+ T lymphocytes dominating and several in close proximity to neurons. There was no evidence of viral infection or microglial nodules. Additionally, Alzheimer's disease neuropathologic changes, atherosclerosis and arteriolosclerosis, and aging‐related tau astrogliopathy were observed.
Discussion: This report highlights the potential use of pathological findings in diagnosing AIE when serological autoantibody tests are not available. However, more biopsy or autopsy‐based studies are necessary for a pathological approach to AIE.

FIGURE 1.

FIGURE 2.
eP‐NI‐A259
A viral demyelizing disease diagnosed by vision loss—Progressive multifocal leukoencephalopathy
A. Çakir1, N. Yeldir 1, G. Ertan Akan1, N. Akalan1
1Medipol Hospital, Pathology, Istanbul, Turkey
Introduction: Viruses may show affinity to certain regions and cells in the central nervous system, may cause latent reinfections. Progressive multifocal leukoencephalopathy (PML) is an infectious disease caused by reactivated JCvirus, characterized by demyelination due to its affinity to oligodendrocytes, and is seen in individuals with immunodeficiency, especially AIDS/HIV(+) patients, and monoclonal antibody therapy.
Objectives: A 39‐year‐old male patient had an accident due to visual impairment for 1 month. Left homonymous hemianopsia was detected in his examination. We present his blood analyses, brain MRI and biopsy findings.
Patient: The patient, who was found to be HIV positive in blood tests at the time of admission, showed hypo‐hyperintense lesions in the right parietooccipital white matter, corpus callosum, right lateral ventricle and medial thalamus on MRI. Demyelinating diseases, especially infectious, were included in the differential diagnosis due to hypoperfusion and involvement pattern. When the possibility of tumor was also mentioned, the sample taken from the right parietooccipital area was evaluated intraoperatively and no glial tumor was observed. In the examination of subsequent biopsies, patchy demyelination with axons preserved (shown by Neurofilament staining), predominantly perivascular small T‐lymphocytes, diffuse parenchymal histiocytes were observed. Some large bizarre pleomorphic astrocytes and accumulations suggestive of nuclear viral inclusion were seen. Immunohistochemically, p53 and ki67 expression were detected in SV40 positive, virus‐infected cells.
Results: Radiological and histopathological findings, HIV positivity and immunohistochemical SV40 expression were evaluated together and the case was diagnosed as JC virus encephalopathy/PML. Infection treatment was started.
Conclusion: JCvirus infection should be considered in demyelinating lesions in immunosuppressed individuals, especially HIV, and histopathological, glial tumor should not be misdiagnosed because of atypia and p53, ki67 expression in virus‐infected cells.
eP‐NI‐A260
Actinomycotic abscess in cerebellum—A case report and literature review
P. Franco del Toro 1, E. Gómez Apo2, L. G. Chávez Macías2, J. A. Bonifaz Trujillo2, A. Larrazolo López2, G. D. J. Parra Romero2, R. Frade Flores2, M. Tovar Echavarri3
1Hospital Civil de Guadalajara “Dr. Juan I. Menchaca,” Guadalajara, Mexico; 2Hospital General de México, Mexico City, Mexico; 3Hospital Central Militar, Mexico City, Mexico
Introduction: Actinomycete infection manifests mostly in the cervicofacial area due to dissemination from the oral cavity. However, its presentation in the brain is exceptional and less common in the cerebellum.
Objectives: Describe histopathological findings of a cerebellar actinomycotic abscess.
Clinical Summary: A 50‐year‐old man who started with holocranial pulsatile headache of one month long and fever with one episode of generalized tonic‐clonic seizure, dizziness and lateralization of the gait, for which he was admitted to rule out infection by COVID‐19. Physical examination: conscious, oriented, cooperative, Glasgow Score of 15, dysdiadochokinesia, bilateral dysmetries with right predominance. Computed axial tomography and magnetic resonance imaging were performed: an intraaxial, infratentorial lesion was found in the right cerebellar hemisphere with lobulated edges and dimensions of 3.7 × 2.8 × 2.5 cm. Therefore, he underwent surgery where a puncture was performed on the lesion site, 12 mL of pus was drained and sent for histopathological study.
Results: Microscopic sections shows abundant neutrophils, cellular debris, with scattered filamentous bacterial colonies with occasionally Splendore–Hoeppli phenomenon. The diagnosis of cerebellar abscess was made by filamentous bacteria morphologically compatible with Actinomyces sp.
Conclusion: Cerebellum actinomycotic abscesses can be clinically and radiologically indistinguishable from other infections in the CNS or even neoplasms, due to this, microscopic assessment is extremely important because only 26% can be isolated by culture and its growth may be slow.
eP‐NI‐A261
Progressive multifocal leukoencephalopathy is changing—A case series from the eighties to our days
M. J. López Martínez 1, J. Jiménez Almonacid2, H. Rodrigo Lara3, A. Hernández Lain2, A. Rábano Gutiérrez1
1Banco de Tejidos Neurológicos de la Fundación CIEN, Neuropathology, Madrid, Spain; 2Hospital Universitario 12 de Octubre, Neuropathology, Madrid, Spain; 3Hospital Clínico Universitario Virgen de la Arrixaca, Neuropathology, Murcia, Spain
Introduction: Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease of the central nervous system resulting from JC virus reactivation in the context of impaired cellular immunity. The diagnosis of probable PML requires the presence of a combination of histopathological features, while a definitive diagnosis needs the detection of JC virus in brain tissue by immunohistochemistry, PCR or electron microscopy.
Objectives: Our aim is to analyze the epidemiological, clinical, radiological, and histopathological characteristics of patients with neuropathological diagnosis of PML.
Methods: We study a case series including all PML cases with neuropathological evaluation between 1988 and 2022 in Hospital Universitario 12 de Octubre and the Neurological Tissue Bank of the CIEN Foundation in Madrid, Spain.
Results: Twenty four patients were included, 17 were male and 7 female. Immunosupression was a common factor among all patients, 16 were HIV‐positive and 8 were pharmacologically immunosupressed. Mean age was 48 years (IQR 35–57) in HIV‐positive patients and 65 (IQR 49–73) in HIV‐negative ones. All patients displayed progressive neurological symptoms, being motor deficit the most common initial manifestation; 13 patients had died within the first 6 months of clinical evolution. Nineteen patients were diagnosed from biopsy material and 5 underwent autopsy. The classic histopathological triad linked to this disease, characterized by oligodendroglial inclusions, hypertrophic astrocytes and foci of demyelination, was found in all cases. The existence of JC virus in brain tissue was demonstrated in 11 cases, in 9 of them by immunohistochemical study and in 2 by PCR.
Conclusions: The paradigmatic PML patient profile has changed, due to HIV treatment and the increasing number of iatrogenic cases associated with the use of immunosuppressing drugs. The information provided by case series remains useful for a better understanding of this evolution.
eP‐NI‐A262
Biopsy proven cerebral sparganosis—A case report
C. Mao 1, J. Gao1
1Peking Union Medical College Hospital, Neurology, Beijing, China
Introduction: Cerebral sparganosis is a rare parasite central nervous system infection. The clinical manifestation is heterogeneous and difficult to diagnosis. Sometimes neuroimaging could mimicke brain tumor. Although discovery of Spirometra mansoni during operation is standard for diagnosis, it is not so easy to seen.
Objectives: To discuss the neuroimaging and histology characteristics of cerebral sparganosis for diagnosis.
Methods: We reported a case of cerebral sparganosis with series of neuroimaging and pathology after operation. Histology included H&E and immunohistochemical stains.
Results: A 28‐year‐old female patient presented with weakness and numbness of right hand for 1.5 months. After admission, brain MRI revealed an occupying lesion at left frontal and temporal lobe, with severe surrounding edema and multiple ring‐like enhancements. Brain tumor or inflammatory granuloma was suspected. Serum and CSF examination revealed no definite evidence. Exploratory craniotomy was done and lesion resection was performed. On microscope, necrosis and wide spread of inflammatory cells were seen. There were granulomas formation and eosinophils around. No pathogen was found. The histology indicated parasite infection. Recurrent serum examination showed positive antibody of Spirometra mansoni. After several courses of praziquantel treatment, the patient recovered well.
Conclusion: Diagnosis of rare parasite infection is difficult. Necrosis and granuloma with eosinophils on histology suggested parasite infection, but it is difficult to find pathogen.

FIGURE 1.
MUSCLE AND NERVE
S03‐MN‐A263
Myelin protein zero mutation‐related hereditary neuropathies—Neuropathological insight from a new nerve biopsy cohort
J. Bremer 1, A. Meinhardt1, I. Katona1, J. Senderek2, E. Kämmerer‐Gassler3, A. Roos1, A. Ferbert4, J. M. Schröder1, S. Nikolin1, K. Nolte1, B. Sellhaus1, K. Popzhelyazkova1, F. Tacke5, U. Schara‐Schmidt6, E. Neuen‐Jacob7, C. Ceuterick de Groote8, P. de Jonghe8, V. Timmerman8, J. Baets8, J. Weis1
1Uniklinik Aachen, Institut für Neuropathologie, Aachen, Germany; 2LMU Munich, Friedrich Baur Institute at the Department of Neurology, Munich, Germany; 3Uniklinik Aachen, Institut für Pathologie, Aachen, Germany; 4Klinikum Kassel, Department of Neurology, Kassel, Germany; 5Charité—Universitätsmedizin Berlin, Department of Hepatology and Gastroenterology, Berlin, Germany; 6University of Essen, Department of Neuropaediatrics, Essen, Germany; 7Heinrich‐Heine University Duesseldorf, Department of Neuropathology, Duesseldorf, Germany; 8Institute Born‐Bunge, and Translational Neurosciences, Faculty of Medicine, University of Antwerp, Laboratory of Neuromuscular Pathology, Antwerp, Belgium
Myelin protein zero (MPZ) is a major structural protein of peripheral nerve myelin. Disease‐associated variants in the MPZ gene cause a wide phenotypic spectrum of inherited peripheral neuropathies. Previous nerve biopsy studies showed evidence for subtype‐specific morphological features. Here, we aimed at enhancing the understanding of these subtype‐specific features and pathophysiological aspects of MPZ‐neuropathies. We examined archival material from two Central European centers and determined genetic, clinical and neuropathological features of 21 patients with MPZ mutations compared to 16 controls. Cases were grouped based on nerve conduction data into congenital hypomyelinating neuropathy (CHN), demyelinating Charcot‐Marie‐Tooth (CMT) type 1, intermediate CMTi and axonal CMT2. We detected four MPZ variants not previously described in patients with neuropathy. Light and electron microscopy of nerve biopsies confirmed fewer myelinated fibers, more onion bulbs and reduced regeneration in demyelinating CMT1 compared to CMT2/CMTi. In addition, we observed significantly more denervated Schwann cells, more collagen pockets, fewer unmyelinated axons per Schwann cell unit and a higher density of Schwann cell nuclei in CMT1 compared to CMT2/CMTi. CHN was characterized by basal lamina onion bulb formation, a further increase in Schwann cell density and hypomyelination. In one autopsy case, we observed prominent neuromatous hyperinnervation of the spinal meninges. Muscle biopsies were available in six cases; four of them displayed marked structural mitochondrial abnormalities. These results show that MPZ alterations not only affect myelinated nerve fibers, leading to either primarily demyelinating or axonal changes, but also non‐myelinated nerve fibers. The autopsy case offers insight into spinal nerve root pathology in MPZ neuropathy. Finally, our data suggest a peculiar association of MPZ mutations with mitochondrial alterations in muscle.
S03‐MN‐A264
Repair strategies in the injured peripheral nervous system
R. M. Stassart 1, R. Fledrich2
1University Clinic Leipzig, Paul‐Flechsig‐Institute of Neuropathology, Leipzig, Germany; 2University of Leipzig, Institute of Anatomy, Leipzig, Germany
Introduction: Restoration of injured tissue is a fundamental biological process that has evolved to secure survival. In mammals, the peripheral nervous system is a prime example of a tissue with regenerative potential. Although remarkably efficient under idealized experimental conditions, full functional recovery is rare. Indeed, the clinical outcome of acute nerve injuries and chronic peripheral neuropathies usually remains poor and constitutes a significant clinical and economic burden.
Objectives: Nerve repair is mainly mediated by myelinating glial cells, the Schwann cells, which transdifferentiate into repair cells to orchestrate nerve de‐ and regeneration. The associated catabolic and anabolic cellular processes pose a comprehensive metabolic challenge towards repair Schwann cells but glial metabolic dynamics remain largely unknown.
Materials and Methods: In order to address the role of Schwann cell metabolism for nerve repair, we took advantage of mouse models for peripheral nerve injury combined with light and electron microscopic imaging techniques, state of the art molecular biology and mitochondrial respirometry.
Results: We here demonstrate that acute nerve injury provokes pronounced metabolic adaptations by Schwann cells and identified the leptin/leptin receptor signaling axis as an upstream regulatory module of the glial metabolic repair response. Schwann cell leptin receptor signaling promotes a cascade of pro‐regenerative responses in Schwann cells and ensures successful peripheral nerve repair. When searching for the cellular source of the ligand leptin, we discovered adipocyte‐derived leptin as a metabolic modulator of diseased Schwann cells and found leptin treatment to promote nerve regeneration.
Conclusions: Our findings propose a model according to which acute nerve injury triggers a therapeutically targetable intercellular crosstalk that modulates glial metabolism, which may be relevant for acute and chronic peripheral nerve diseases.
S13‐MN‐A265
Molecular insights in skeletal muscle under physiological condition—Age versus aging
A. Schaiter 1, A. Hentschel2, F. Kleefeld3,4, V. Umathum1,5, C. Nelke6, A. Roth1, A. Hahn7, H. Krämer8, J. Kreutzberg9, P. van der Ven9, T. Ruck6, R. Horvarth3, M. Bartkuhn10,11, A. Roos12,13, A. Schänzer1
1Justus‐Liebig‐University Giessen, Institute of Neuropathology, Giessen, Germany; 2Leibnitz Institut für Analytische Wissenschaften‐ISAS e.V., Dortmund, Germany; 3John Van Geest Centre for Brain Repair, School of Clinical Medicine, University of Cambridge, Department of Clinical Neurosciences, Cambridge, United Kingdom; 4Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neurology, Berlin, Germany; 5Bundeswehrkrankenhaus Ulm, Institute of Pathology and Molecular Pathology, Ulm, Germany; 6University Hospital Düsseldorf, Department of Neurology, Duesseldorf, Germany; 7Justus‐Liebig‐University Giessen, Departemnt of Pediatric Neurology, Giessen, Germany; 8Justus‐Liebig‐University Giessen, Departement of Neurology, Giessen, Germany; 9Institute for Cell Biology, University of Bonn, Department of Molecular Cell Biology, Bonn, Germany; 10Justus‐Liebig‐University Giessen, Biomedical Informatics and Systems Medicine, Giessen, Germany; 11Institute for lung health (ILH), Justus‐Liebig University Giessen, Giessen, Germany; 12Centre for Neuromuscular Disorders, Centre for Translational Neuro‐ and Behavioral Sciences, University Duisburg‐Essen, Department of Pediatric Neurology, Essen, Germany; 13Children's Hospital of Eastern Ontario Research Institute, Ottawa, Canada
Introduction: To further understand skeletal muscle alterations caused by aging and sarcopenia, it is important to identify the underlying mechanisms regulating muscle function under physiological condition. Despite high plasticity in skeletal muscle, molecular studies have mainly focused on adults, leaving limited knowledge of the regulating mechanisms in young human subjects. Therefore, identifying the molecular changes that occur with age and aging in healthy skeletal muscle is crucial to advance our understanding of age‐related changes in muscle.
Objectives: We aim to analyze differences of infant and adult human skeletal muscle through proteomic and transcriptomic analysis.
Methods: Proteomic and transcriptomic analysis of skeletal muscle biopsies from healthy infants (4–22 months) and adults (19–65 years) were conducted. Results were validated by mitochondrial assays and immunofluorescence studies.
Results: Fifty‐six differentially expressed proteins (DEP) were identified in infants compared to adults with 44 down‐regulated and 12 up‐regulated proteins in adult muscle. Identified DEPs were predominantly associated with metabolism, immune response, sarcomere structure and cytoskeleton. Transcriptomic analysis confirmed the role of age dependent processes in immune regulation and structural development. Despite mitochondrial copy number not differing between the age groups, long chain PCR for MTA depletion revealed mitochondrial alterations from 55 years on.
Conclusions: Being the first study including skeletal muscle samples from younger subjects, it highlights the difference of the molecular profile of infant and adult muscle under physiological condition. This data not only provides a deeper understanding of age dependent mechanisms in skeletal muscle, but also indicates that these mechanisms should be considered when performing molecular profiling of neuromuscular disorders in varying age groups.
S13‐MN‐A266
Investigations of the specific interferon‐signature in anti‐synthetase syndrome‐associated myositis
C. Preusse 1,2, L. Gallay3, I. Pinal‐Fernandez4,5, A. Mammen4,5,6, O. Benveniste7, H. H. Goebel1, N. Streichenberger8, A. Roos9,10, T. Ruck11, W. Stenzel1
1Charité—Universitätsmedizin Berlin, Neuropathologie, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neurology, Berlin, Germany; 3Edouard Herriot University Hospital, Clinical immunology, Lyon, France; 4Johns Hopkins University School of Medicine, Neurology, Baltimore, MD, United States; 5National Institute of Arthritis and Musculoskeletal and Skin Diseases, Muscle Disease Unit, Bethesda, MD, United States; 6Johns Hopkins University School of Medicine, Medicine, Baltimore, MD, United States; 7Pitié‐Salpêtrière University Hospital, Internal Medicine and Clinical Immunology, Paris, France; 8Hospices Civils de Lyon, Neuropathology, Lyon, France; 9University Children's Hospital, University of Duisburg‐Essen, Pediatric Neurology, Essen, Germany; 10Leibniz‐Institut für Analytische Wissenschaften—ISAS—e.V., Dortmund, Germany; 11Heinrich‐Heine University Duesseldorf, Neurology, Duesseldorf, Germany
Introduction: Myositis affects skeletal muscles, but may also feature multi‐systemic organ involvement. Patients are classified based on clinical and morphological factors. In recent years, two major achievements have emerged: (1) autoantibodies (AB) have become a key pillar in diagnostics used to classify subtypes of myositis, for example, anti‐synthetase syndrome (ASyS), accounting for ~20% of myositis patients harboring ABs against t‐RNA synthetases. (2) Relevance of interferon (IFN)‐induced gene expression delineated molecular mechanisms in different IIM subgroups. Recently, transcripts induced by type I and II IFNs were studied in more than 100 myositis patients, and it was shown that dermatomyositis (DM) has a type I over type II signature, while ASyS is characterized by a type II over type I signature. However, subgrouping depending on ABs was not reported.
Objectives: We investigated gene expression of type I/II IFN genes in ASyS patients, expanding the previous analyses to other ASyS‐specific AB. We will answer the open question, whether IFN signatures quantitatively or qualitatively differ among subgroups.
Patients and Methods: We included patients with diagnosed ASyS with Jo1+, PL7+ or PL12+ AB, as well as with DM and NDCs. Methods used were gene expression analyses via qPCR, unbiased proteomic profiling and immune histochemistry.
Results: On transcript levels, we demonstrate that our data are in agreement with those by Pinal‐Fernandez. Furthermore, we prove that analysis of all AB subgroups is of importance, since IFN levels do significantly differ among subgroups, with Jo1+ ASyS having the strongest IFN signature of ASyS subgroups, while PL‐12+ ASyS had weaker activation. The findings were confirmed on protein level.
Conclusion: Since multiple interferon‐regulatory treatments exist, a detailed analysis of the entire IFN signature is critical, as ASyS is likely not homogeneous and AB subgroups differ in their IFN signature and subsequent potential treatment response.
S13‐MN‐A267
Neuropathological and transcriptional analysis of PrPC overexpression‐induced necrotizing myopathy
R. R. Reimann 1, S. Sorce1, M. Koderman1, D. Caredio1, A. Armani1, T. Hortobágyi1, M. Nuvolone1, A. Aguzzi1
1Institiute of Neuropathology, Zurich, Switzerland
Introduction: Cellular prion protein (PrPC) accumulates in several human myopathic conditions [1–3], without the formation of the proteinase K resistant isoform of PrPSC (the transmitting agent in prion disease) [2]. Interestingly, a non‐cell autonomous overexpression of PrPC induces a necrotizing myopathy [4]. These observations may point to PrPC‐overexpression associated processes as putative pharmacological targets in muscular disease.
Objectives: In order to investigate the underlying mechanisms we generated an inducible conditional mouse model with selective PrPC overexpression in skeletal muscle and performed neuropathological and genome wide transcriptional analysis.
Materials and Methods: We crossed our CAG‐CAT‐PrP transgenic mouse model [5] with the tamoxifen‐inducible muscle specific cre line ACTA1‐creERt2. In order to characterized the model we analyzed plasma and tissue samples and performed RNA sequencing followed by a gene set enriched analysis (GSEA).
Results: A significant increase of serum creatine kinase was found as early as two weeks later. Histologic analysis depicted a severe myopathy with many necrotic and numerous degenerating/regenerating fibres (Figure 1), and respiratory chain abnormalities. A GSEA analysis of an RNASeq library revealed respiratory chain alterations associated with inflammation and cell death (Figure 2).
Conclusion: Cell autonomous overexpression of PrPC in skeletal muscle in a mouse model causes a fulminant necrotizing myopathy with respiratory chain defects. Further studies are in progress to explore the cascade of events and the possible therapeutic interventions.
References: [1] Askanas V, et al. Neuroreport. 1993. [2] Zanusso G, et al. Brain Path. 2001. [3] Kovacs G, et al. J Path. 2004. [4] Westaway D, et al. Cell. 1994. [5] Lakkaraju A, et al. Brain Path. 2022.

FIGURE 1 Cell autonomous cellular prion protein (PrPC) overexpression induced necrotizing myopathy.

FIGURE 2 GSEA over time in skeletal muscle upon PrPC overexpression.
S16‐MN‐A268
Evaluation of clinico‐pathological and genetic spectrum of RYR1 mutations in Indian cohort
M. C. Sharma 1, A. Dhall1, B. Jassal1, V. Suri1, M. Faruq1, U. Shamim1, R. Bhatia1, B. Chakarwarti1, S. Gulati1, V. Venugopalan Y1
1All India Institute of Medical Sciences, Neuropathology, Delhi, India
Background: Congenital myopathies (CM) are characterised by early onset of symptoms and slow or static progression. Central core disease (CDC) is one of the important causes of CM and is characterised by RYR1 mutations. With the introduction of NGS both morphological and phenotypic spectrum of muscle diseases is expanding.
Aims: To evaluate clinical, pathological and genetic spectrum of RYR1 mutations in Indian population.
Methods: One hundred and ninety‐two patients (year 2018–2022) suspected of muscular dystrophy or congenital myopathies from unrelated families underwent phenotypic characterization followed by muscle histopathological analysis. Confirmed cases were subjected to targeted next generation sequencing (NGS) using a customized panel of 88 genes. Sequencing data was annotated using VariMAT pipeline for generating variants.
Results: Ten patients were diagnosed with RYR1 mutations amounting to a frequency estimation of 5.20% of all muscular dystrophies and congenital myopathies in Indian cohort. The age ranged from 15 months to 39 years. CPK levels ranged from 50 to 1600 U/L. Five patients presented with congenital myopathy and five with LGMD phenotype. Histomorphological changes were minimal in five patients, five show features of muscular dystrophy. Ultrastructurally, cores were observed in four cases and myofibrillary disruption in one case. Sequencing results revealed a total of three novel and nine reported exonic mutations (non‐frameshift, nonsense and non‐synonymous SNVs) across RYR1 gene.
Conclusion: In our study, NGS enabled thorough and rapid investigation leading to identification of a considerable proportion of mutations thus broadening the genetic spectrum. Certain variants were found in other Asian (Japanese, Chinese) and European populations. No genotype–phenotype correlation existed, suggesting that clinical phenotype is determined not only by genetic factors but also likely through a complex interplay of environmental, epigenetic, and genetic factors.
S16‐MN‐A269
Anti‐α‐Actinin immunostaining is sensitive but non‐specific as a diagnostic marker for sporadic late‐onset nemaline myopathy
M. Gao 1, D. Yue2, N. Cheng3,4,5, K. Jiao3,4,5, X. Xia3,4,5, N. Wang3,4,5, C. Zhao3,4,5, W. Zhu3,4,5
1Huashan Hospital Fudan University, Department of Pathology, Shanghai, China; 2Jing'an District Center Hospital of Shanghai, Department of Neurology, Shanghai, China; 3Huashan Hospital Fudan University, Department of Neurology, Shanghai, China; 4National Center for Neurological Disorder, Shanghai, China; 5Huashan Hospital, Shanghai Medical College, Fudan University, Huashan Rare Disease Center, Shanghai, China
Introduction: Alpha‐actinin, an important structural protein in muscles, anchors actin filaments and stabilizes myofibrils. Some studies suggest that anti‐α‐actinin antibody may serve as a diagnostic marker for sporadic late‐onset nemaline myopathy (SLONM), but its specificity and sensitivity remain debated.
Objectives: To investigate the utility of anti‐α‐actinin antibody as a diagnostic marker for SLONM and to study its expression in other muscle diseases.
Materials and Methods: Muscle specimens were obtained from 54 cases, including SLONM, neurogenic atrophy, rhabdomyolysis, type II fiber atrophy, dermatomyositis, immune‐mediated necrotizing myopathy, inclusion body myopathy, and normal controls. The samples were stained with anti‐α‐actinin antibody using standard protocols, and two independent observers blinded to the sample groups evaluated the staining results.
Results: The positive expression rate of α‐actinin was highest in SLONM (11/12) but was also present in other muscle diseases. The upregulation of anti‐α‐actinin expression is not specific to SLONM and may occur whenever metabolic abnormalities or functional damage to muscle cells are present.
Conclusion: In clinical practice, the expression level of anti‐α‐actinin alone is insufficient for diagnosing SLONM or other muscle diseases. A comprehensive diagnosis and assessment based on additional clinical and pathological characteristics is necessary.
S25‐MN‐A270
Skeletal muscle expression of immune regulating proteins in myositis subtypes
A. Nishimura1, A. Mensch2, M. Huber3, A. Roth1, E. Neuen‐Jacob4, H. Krämer5, U. Müller‐Ladner3, W. Stenzel6, T. Ruck7, A. Schänzer 1
1Justus‐Liebig‐University Giessen, Institute of Neuropathology, Giessen, Germany; 2Martin Luther University Halle‐Wittenberg, Department of Neurology, Halle‐Wittenberg, Germany; 3Kerckhoff‐Klinik, Justus‐Liebig‐University Giessen, Department of Rheumatology, Giessen, Germany; 4Heinrich Heine University, Institute of Neuropathology, Duesseldorf, Germany; 5Justus‐Liebig‐University Giessen, Department of Neurology, Giessen, Germany; 6Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt‐Universität zu Berlin, Department of Neuropathology, Berlin, Germany; 7University Hospital Düsseldorf, Düsseldorf, Germany, Department of Neurology, Duesseldorf, Germany
Introduction: Idiopathic inflammatory myopathies (IIM) are autoimmune diseases classified as dermatomyositis (DM), immune‐mediated necrotizing myopathy (IMNM), anti‐synthetase syndrome (ASyS) and inclusion body myositis (IBM). IIM subtypes follow different immune regulatory mechanisms necessitating adapted therapeutic strategies.
Objectives: Analyzing immune regulating proteins in skeletal muscle tissues increases the understanding of the underlying pathomechanisms.
Materials and Methods: Skeletal biopsies from adult patients (n = 30) (average age 53.8 years; 58.18% female) with diagnosis of IIM (6 DM; 7 IMNM; 6 ASyS; 11 IBM), neurogenic atrophy (NA; n = 4) and controls (HC; n = 8) were included in our study. Immunofluorescence staining was performed with antibodies against MHC class I, MHC class II, ICAM‐1, spectrin and desmin. Sections were digitalized using a Zeiss Axio Scan.Z1 slide scanner. The coexpression was analyzed on entire sections with Fiji software and quantified by Manders' coefficient.
Results: MHC class I expression was significantly upregulated in ASyS, DM, IBM and IMNM compared to HC. In IMNM the expression was significantly lower compared to other IIMs. Significant upregulations of MHC class II were present in ASyS, DM and IBM compared to HC. ICAM‐1 expression was upregulated in all IIMs compared to HC, while only ASyS and DM showed a significantly stronger expression of ICAM‐1 on endomysial capillaries.
Conclusion: Analysis of digitized whole sections provides accurate data on entire skeletal muscle sections. Differences in expression of immune regulating proteins provide deeper insights in pathogenesis of IIM subtypes and might drive future therapeutic approaches.
S25‐MN‐A271
Longitudinal TDP43‐associated cryptic exon splicing in early and full‐blown inclusion body myositis
F. Kleefeld 1, C. Preusse2, A. Schänzer3, A. Nishimura3, K. Hahn1, S. L. Louis4, O. Benveniste4, Y. Allenbach4, H. H. Goebel2, M. Schülke‐Gerstenfeld5, W. Stenzel2
1Charité—Universitätsmedizin Berlin, Neurology, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany; 3Universitätsklinikum Giessen, Neuropathology, Giessen, Germany; 4Institute of Myology, Pitié‐Salpêtrière Hospital, Paris, France; 5Charité—Universitätsmedizin Berlin, Neuropediatrics, Berlin, Germany
IBM is an inflammatory muscle disease characterized by a distinct clinical picture including finger flexor weakness, and dysphagia in patients >50 years. Apart from inflammation and mitochondrial abnormalities, “degenerative” features are characteristic for IBM. This includes deposition of TDP43, a protein relevant in degenerative diseases such as amyotrophic lateral sclerosis. TDP43 plays an important role in transcriptional regulation by binding to RNA and affecting its splicing, and stability. Accumulation and sequestration of TDP43 in the cytosol may lead to aberrant splicing patterns and mRNA processing. We aimed at identifying alternative splicing targets known to be regulated by TDP43, which may play a role in the pathogenesis of IBM‐SD. We studied in total 40 muscle biopsy samples of patients with IBM‐SD, with 20 patients showing histological features of early IBM‐SD (ex “PM‐Mito”) and 20 samples of full‐blown IBM by immunohistochemistry, electron microscopy, and RNA‐sequencing (RNAseq) and compared patterns of cryptic exon splicing. Five muscle biopsies derived from healthy controls were also included for RNAseq. Cryptic exon splicing was evident in all patients with IBM‐SD and relevant in PPP2R2D and ZPF91 genes, which are related to the biological functions of TDP43 and are strongly expressed in IBM‐SD skeletal muscles. In early IBM‐SD (PM‐Mito) compared to classic IBM the same patterns of cryptic exon splicing were detected, but less abundantly, while we did not detect aberrant splicing patterns in healthy controls. Alternative splicing of PPP2R2D and ZPF91 is present in all disease stages of IBM‐SD, with early cases (PM‐Mito) showing the same patterns, albeit a lower frequency of aberrant splicing events. We hypothesize that this may lead to a loss of function of TDP43, creating a possible link to impaired autophagy and inflammation. These processes are relevant during disease development of IBM‐SD, and may serve as a therapeutic target in the future.
S25‐MN‐A272
Pipestem capillaries in necrotizing myopathy—A pathological and clinical characterization in Chinese patients
M. Gao 1, X. Xia2,3,4, D. Yue5, N. Cheng2,3,4, K. Jiao2,3,4, N. Wang2,3,4, C. Zhao2,3,4, W. Zhu2,3,4
1Huashan Hospital Fudan University, Department of Pathology, Shanghai, China; 2Huashan Hospital Fudan University, Department of Neurology, Shanghai, China; 3National Center for Neurological Disorder, Shanghai, China; 4Huashan Hospital, Shanghai Medical College, Fudan University, Huashan Rare Disease Center, Shanghai, China; 5Jing'an District Center Hospital of Shanghai, Department of Neurology, Shanghai, China
Introduction: Pipestem capillaries were observed in a subgroup of patients with necrotizing myopathy, characterized by thickening of capillary walls and deposition of membrane attack complex (MAC), resulting in muscle fiber necrosis and minimal cellular infiltration.
Objective: This study aims to provide a pathological and clinical characterization of necrotizing myopathy with pipestem capillaries in Chinese patients.
Patients and Methods: Clinical data of six patients fulfilling the pathological criteria were reviewed retrospectively. Open muscle biopsies and transmission electron microscopy (TEM) were performed to examine capillary ultrastructure.
Results: All six patients were female, with a median age of 48 years and disease duration ranging from 1 to 18 months. Symptoms included proximal muscle weakness, elevated CK levels, increased ESR, and positive results for MSAs or MAAs. Pathological studies and electron microscopy showed marked thickening of capillaries with complement deposition. “Pipestem‐like capillaries” were identified as thickening of the basal lamina at the ultrastructural level. Slight mononuclear cell infiltration was observed. MAC deposition was not predominant. Two types of thickened duplication and diffuse thickening basal lamina morphology were observed under electron microscopy.
Conclusion: This study provides a characterization of necrotizing myopathy with pipestem‐like capillaries. Further research on the relationship between microvascular alterations and muscle damage may help to explain the mechanism of necrotizing myopathy.
S08‐MN‐A273
A comparative single nuclei transcriptomics approach to evaluating the terminally differentiated lymphocytes in autoimmune myositis
F. V. De Los Reyes 1, S. Hayashi1, S. Noguchi1, I. Nishino1
1National Institute of Neuroscience, National Center of Neurology and Psychiatry, Department of Neuromuscular Research, Kodaira, Japan
Question: The utilization of genome‐based studies has allowed the expansion of our understanding to encompass the role of transcriptomics in understanding diseases. The main goal of the study is to establish that sNuc RNA‐seq can show the differences in the transcriptome expression of autoimmune myositis with respect to the PD‐1/PD‐L1, KLRG1/E‐cadherin family, and CTLA4/B7 family interaction for anti‐synthetase syndrome (ASS), dermatomyositis (DM), immune‐mediated necrotizing myopathy, and inclusion body myositis (IBM).
Methods: Transcriptomics evaluation using sNuc gene expression in diagnosed samples that fulfilled the immunohistopathologic criteria for the diagnosis alongside muscle specific antibodies (MSA), as applicable, was performed. A comparative analysis of the differential gene expression across disease conditions was done.
Results: Terminally differentiated T cells (TdTc) were the second most abundant non‐myogenic cell type across all samples, following only the main macrophage population, with IBM expressing a relatively larger proportion. A separate TdTc population with an intact capacity for producing cytotoxic granules (cytotoxic TdTc) was also observed. The upregulation of the PD‐1 gene, PDCD1, was observed most prominently in the TdTc of ASS_Jo‐1 and IBM, and in the cytotoxic TdTc group of ASS_Jo‐1 and ASS_OJ. The gene for PD‐L1, CD247, was upregulated in the TdTc and the cytotoxic TdTc, suggesting the role of cell‐cell interaction among the TdTc population to mitigate tissue injury. Among the diseases, the TdTc group of IBM showed that 19% of TdTc have an upregulation of KLRG1. In contrast, CTLA4 expression was limited and ASS_Jo‐1 expressed it only on a few cytotoxic TdTc and B cells.
Conclusion: The behavior of inflammatory cells in autoimmune myositis is a core contributory to the pathomechanism of the disease. The gene signatures may provide a target to addressing the fundamental regulatory mechanism that may mitigate the disease.
S14‐MN‐A274
Megaconial congenital muscular dystrophy associated with ichthyosis due to CHKD mutation
I. Bodi 1, S. O'Sullivan1, C. Deshpande2, J. Mellerio1, E. Wraige1
1King's College Hospital NHS Foundation Trust, Clinical Neuropathology, London, United Kingdom; 2Central Manchester University Hospitals NHS Foundation Trust, Manchester, United Kingdom
Introduction: Megaconial congenital muscular dystrophy (MCMD) is a recently identified rare neuromuscular disorder due to loss of function mutations in the CHKB gene. We describe a retrospectively diagnosed case with remarkable ultrastructural findings in muscle and associated ichthyosis.
Patients and Methods: Three‐year‐old girl presented with proximal weakness, scapular winging, laxity, microcephaly and developmental delay. CK was mildly elevated to 517 IU/L. The muscle showed mild dystrophic changes and many fibres with centrally absent oxidative enzymes, and subsarcolemmally located Gomori trichrome positive structures (Figure 1). Electron microscopy revealed markedly enlarged, in places giant, mitochondria at the periphery of fibres leading to mitochondrial investigations (Figure 2). One year later she presented with a presumed infected eczema and a clinical diagnosis of ichthyosis was made.
Results: Biochemistry revealed complex IV deficiency. Genetics performed 5 years later confirmed compound heterozygote CHDK mutation. She remains restricted in mobility with learning difficulties but no cardiomyopathy to date.
Conclusion: The subsarcolemmal accumulation of structurally abnormal giant mitochondria may mimic mitochondrial myopathy and should raise the suspicion of MCDM if associated with dystrophic changes and ichthyosis. MCDM is characterised by multi‐system involvement including intellectual impairment, ichthyosis‐like skin changes and sometimes dilated cardiomyopathy.

FIGURE 1.

FIGURE 2.
S14‐MN‐A275
Application of serial section electron microscopy for 3D visualization of the neuromuscular junction in a patient with seronegative myasthenia gravis
C. Dittmayer 1, S. Timm2, C. Preusse1,3, J. C. Rückert4, M. Schülke‐Gerstenfeld5, A. Meisel6, W. Stenzel1, S. Hoffmann3
1Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neuropathology, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Core Facility Electron Microscopy, Berlin, Germany; 3Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neurology, Berlin, Germany; 4Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of General, Visceral, Vascular and Thoracic Surgery, Berlin, Germany; 5Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neuropediatrics, Berlin, Germany; 6Charité—Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität zu Berlin, Department of Neurology, Integrated Mysthenia Center, Neuroscience Clinical Research Center, Center for Stroke Research Berlin, Berlin, Germany
Question: Myasthenia gravis (MG) is a rare disease characterized by fatigable muscle and mediated by autoantibodies directed against postsynaptic antigens of the neuromuscular junction (NMJ). Complement‐mediated damage of the NMJ is thought to be the most relevant effector mechanism in acetylcholine receptor antibody‐positive MG. 2D electron microscopy (EM) studies consistently report alteration of the NMJ including a rarefication and plumping of the postsynaptic folds. However, in a series of seronegative MG patients, we found complement deposition at the NMJ but only a fraction of patients showed ultrastructural alterations of the NMJ. 3D EM might detect more subtle ultrastructural changes. To establish a workflow for digitization of the entire volume of NMJ for 3D EM using biopsies that were fixed and embedded according to routine protocols.
Methods: A biopsy of intercostal skeletal muscle tissue was selected based on superior structural preservation. Approximately 1000 ultrathin sections were cut using the automated tape‐colleting ultramicrotome, stabilized by heat and stained. A region of 285 consecutive ultrathin sections, covering an entire NMJ, was digitized using a scanning electron microscope with a backscattered electron detector. 2D Images were processed to a digital volume using TrakEM2 for visualization in IMOD.
Results: We digitized an entire NMJ and thereby provide a dataset for further analysis. We did not observe prominent alterations such as coarsened postsynaptic foldings. However, we found vesicular structures, which showed similar substructure as compared to the “buttons terminal” next to the NMJ and require further analysis.
Conclusions: We established a pipeline for ultrastructural digitization of entire NMJ aiming at in‐depth analysis of NMJ 3D ultrastructure in patients with MG. Digitization of further NMJs from different MG patients and non‐diseased control tissues are required for comparative analysis.
S14‐MN‐A276
Histopathological features and autophagy aspects of Ku+ myositis
C. Preusse 1,2, M. T. Holzer3, U. Schneider4, A. Schänzer5, S. Léonard‐Louis6, O. Benveniste7, J. Weis8, K. Claeys8,9, B. Schoser10, F. Montagnese10, A. Uruha11, M. Huber12, L. Gallay13, N. Streichenberger14, M. Krusche3,14, W. Stenzel1
1Charité—Universitätsmedizin Berlin, Neuropathologie, Berlin, Germany; 2Charité—Universitätsmedizin Berlin, Neurology, Berlin, Germany; 3University Medical Center Hamburg‐Eppendorf, III Medical Department, Division of Rheumatology, Hamburg, Germany; 4Charité—Universitätsmedizin Berlin, Rheumatology, Berlin, Germany; 5Justus‐Liebig‐University Giessen, Neuropathology, Giessen, Germany; 6Pitié‐Salpêtrière University Hospital, Reference Center of Neuromuscular Pathology Paris‐Est, Paris, France; 7Pitié‐Salpêtrière University Hospital, Internal Medicine and Clinical Immunology, Paris, France; 8RWTH Aachen University, Neuropathology, Aachen, Germany; 9University Hospitals Leuven, Neurology, Leuven, Belgium; 10Ludwig‐Maximilians‐University, Neurology, Munich, Germany; 11Tokyo Metropolitan Neurological Hospital, Neurology, Tokyo, Japan; 12Kerckhoff‐Klinik, Justus‐Liebig‐University Giessen, Rheumatology, Bad Nauheim, Germany; 13Hospices Civils de Lyon, Internal Medicine, Lyon, France; 14Hospices Civils de Lyon, NeuroMyogène, Lyon, France
Introduction: Ku+ myositis is a rare form of myositis, with antibodies that are associated with connective tissue disease and the clinical picture of the patients often varies. A few histopathological examinations have shown a broad picture with inflammatory or necrotizing aspects, but a precise description and characterization of Ku+ myositis is still lacking.
Objective: The aim of this study was to perform a detailed histopathological and transcriptional examination of muscle samples from Ku+ patients to uncover possible pathophysiological mechanisms/commonalities.
Methods: Muscle biopsies from 23 patients with Ku antibodies and clinical/morphological signs of myositis were analyzed by immune histochemistry and qPCR. Furthermore, a comparison was made with biopsies from non‐disease controls and immune‐mediated necrotizing myopathy.
Results: We found that 91% of patients were women with an average age of 55 years. There was an overlap with systemic sclerosis in 30% of cases and isolated myositis in 26%. All patients presented myalgia, of which nine patients showed no clinical signs of muscle weakness. CK elevation was present in 91% of cases. Histopathological examinations showed a wide spectrum from mild to very pronounced myositis. MHC‐cl. I showed overexpression with diffuse, focally enhanced expression. In almost all samples (87%), we noted varying degrees of necrosis with concurrent inflammatory aspects. We also noted small vacuoles in 59% of biopsies and p62+ and LC3+ and myotilin aggregates. Immunofluorescence showed co‐localization of p62 and myotilin.
Conclusion: In this study, we identified a histopathological pattern of Ku+ myositis with predominant MHC‐cl. I overexpression, inflammation, necrosis, and small vacuoles, as well as specific p62+, LC3+ aggregation. Co‐localization of p62 and myotilin may indicate protein aggregation and induction of autophagy pathways and is now the subject of continued investigation.
eP‐MN‐A277
Morphological study of prepathologic SMA can help identify rare genetic constellations and pave timely therapy
J. Meinhardt 1, H. H. Goebel1, W. Stenzel1
1Charité—Universitätsmedizin Berlin, Neuropathology, Berlin, Germany
Introduction: SMA is a neuronopathy caused by an autosomal recessive genetic defect of the SMN1 gene (loc.5q13.2). In 96% of cases, the underlying cause is a homozygous deletion of exon 7/8 of the SMN1 gene—this constellation is detected by newborn screening, which has been routinely performed in Germany since October 2021. 4% of cases show a compound heterozygous SMN1 deletion and a pathogenic sequence variant of the SMN1 gene, which is not detected by newborn screening. Therapeutic approaches are available for several years now using gene replacement or synthesis enhancement of SMN protein. Timing of treatment initiation determines clinical efficacy, emphasizing the importance of rapid diagnosis. Here, we show three cases of myopathologic diagnosis of pre‐pathologic SMA and, present the clinic, diagnostic and therapy of one child in detail.
Results: Skeletal muscles showed morphological changes characteristic for a prepathological SMA including immaturity of myofibres and rounded atrophic partially grouped type 2 fibres. One child presenting with generalized muscle weakness showed an unremarkable newborn screening and targeted deletion search in the SMN1 gene. Muscle biopsy showed morphological changes characteristic for a pre‐pathological SMA. At the age of 4 months, a 5q‐SMA was also detected genetically by whole exome analysis showing two pathogenic point mutations in the SMN1 gene in compound heterozygous state.
Discussion: Newborn screening does not detect all genetic constellations leading to SMA. Even an inconspicuous result by MLPA does not completely exclude the presence of a 5q‐SMA since compound heterozygosity for two pathogenic sequence variants of the SMN1 gene may be present. It is therefore advisable to perform a muscle biopsy and sequencing of the SMN1 gene at early stage if the constellation is clinically and morphologically suggestive. Only in this way is it possible to detect rare constellations and to assign affected children to timely therapy.


FIGURE 2.
eP‐MN‐A278
A comparison of neurofilament in peripheral nerve and serum in patients undergoing nerve biopsy
S. Streit 1, N. Gimber2, J. Kestenbach3, J. Schmoranzer2, C. Meisel3, K. Ruprecht4, W. Stenzel1, P. Körtvélyessy3,4,5
1Charité—Universitätsmedizin Berlin, Department of Neuropathology, Berlin, Germany; 2Universitätsmedizin, Advanced Medical BioImaging Core Facility—AMBIO, Berlin, Germany; 3Labor Berlin—Charité Vivantes GmbH, Berlin, Germany; 4Charité—Universitätsmedizin Berlin, Department of Neurology, Berlin, Germany; 5German Center for Neurodegenerative Diseases (DZNE), Magdeburg, Germany
Neurofilament light chain (NfL) is a neuronal intermediate filament protein and biomarker for axonal damage that could aid diagnosis and therapeutic monitoring in a variety of nervous system disorders. Regarding peripheral nerve disease, a correlation with disease activity in patients with polyneuropathy and vasculitic neuropathy has been discussed. However, the exact impact of neuronal damage in peripheral nerves on NfL‐serum levels remains poorly understood, thus limiting evaluation of NfL as a biomarker in clinical practice. To further characterize the relationship between nerve damage and NfL‐serum levels, we retrospectively identified matched nerve biopsy‐ and serum samples from patients treated at Charité university hospital (n = 21). Two neuropathologists (SiSt, WeSt) assessed total loss of neurofilaments in histological sections stained for neurofilament on a semi quantitative scale ranging from “0” (no loss) to “4” (near complete loss of neurofilaments). Neurofilament status assessment was performed on cryosections stained for neurofilament (DAKO M 0762). NfL serum levels were analyzed in two batches using the commercial Simoa® NfL‐assay. Unadjusted data shows no monotonic correlation between total loss of neurofilaments in nerve samples and serum NfL levels in our cohort (Spearman r: 0.15; p: 0.5). Adjustment for age and non‐pathological levels of NfL did not change the results. Pathological elevated NfL level have been shown to correlate with lower nerve conduction velocities as well as with severity of polyneuropathies. In our preliminary assessment, we do not find a similar correlation between neurofilament loss and serum NfL.

FIGURE 1.
eP‐MN‐A279
Characteristic histopathological findings in congenital MYL‐1 myopathy—Type II myofibres atrophy with type I myofibres hipertophy
C. Jou 1, A. Codina1, I. Madrigal2, L. Rodriguez3, R. Lavilla1, G. Arca4, G. Sebastiani4, C. Ortez5, L. Rodriguez2, J. M. Expósito5, B. Estevez6, L. Carrera5, D. Natera de Benito5, A. Nascimento5
1Hospital Sant Joan de Déu, Pathology, Esplugues de LLobregat, Spain; 2Hospital Clínic, Genetics, Barcelona, Spain; 3Hospital Clínic, Pathology, Barcelona, Spain; 4Hospital Clínic, Neonatology, Barcelona, Spain; 5Hospital Sant Joan de Déu, Neurology, Esplugues de LLobregat, Spain; 6Institut de Recerca Sant Joan de Déu, Neurogenetics and molecular medicine, Esplugues de LLobregat, Spain
The increasing accessibility to genetic tests and massive sequencing has enabled genetic diagnosis in congenital myopathies, but despite this, in a significant proportion of cases the genetic cause remains unknown. Congenital myopathies are a heterogeneous group of disorders resulting in hypotonia, muscle weakness, and myopathic features on muscle biopsy. MYL1‐related congenital myopathy is a very rare entity only described in two individuals to date. Here we present a case of a patient with MYL‐1 related myopathy. We analyzed histology in several muscles and in all of them marked myopathic changes involving high variability in fibre size, internalized nuclei, fibrosis, and severe fatty infiltration were observed. Most fibres in all studied muscles were small and co‐expressed fast and fetal myosin, and were surrounded by larger fibres, which expressed only slow myosin. No inclusions were observed with Gomori trichrome staining. NADH and SDH staining in larger myofibrils showed uniform intermyofibrillar pattern, while in some of the smaller myofibrils there was an accumulation of oxidative staining which gave a darker appearance to these fibres. These findings were verified in electronic microscopy studies. Additionally, MYL‐1 quantification was performed in immunoblot, showing a decrease in the protein amount in patient. These findings confirm that bi‐allelic MYL1 variants are associated with a relatively homogeneous clinical and histopathological phenotype that is recognizable. Histopathological characteristics involving type II myofibres atrophy along with type I myofibres hypertrophy could help in diagnosis of MYL‐1 mutations in those patients with a severe congenital myopathy.
eP‐MN‐A280
A case report of amyloidosis of the brachial plexus nerve and review of the literature
C. Sun 1, J. Lin1, Y. Wang1
1Huashan Hospital Fudan University, Neurology, Shanghai, China
Question: To summarize the clinical features of focal peripheral nerve amyloidosis.
Methods: To retrospectively analyze the general data, clinical manifestations, imaging features, laboratory tests and pathological features of a patient with focal brachial plexus amyloidosis, and to retrieve relevant domestic and foreign literature for literature review.
Results: The patient was a female, 34 years old, with a right cervical mass found for 2 years and right upper limb weakness for 2 months. Brachial plexus MRI revealed nerve root and superior trunk tumor‐like changes in the right cervical 5 and cervical 6 nerves (Figure 1). Electromyography revealed injury to the right upper trunk of the brachial plexus nerve. Brachial plexus nerve biopsy revealed positive Congo red staining for amyloid deposits. Tissue mass spectrometry analysis identified the amyloid type as AHL type (G‐λ) (Figure 2). After definitive diagnosis, the patient was treated with a nerve graft. A review of the literature on focal spinal amyloidosis revealed that the mean age of onset of this type of disease was 62.4 years, the radial nerve was the most susceptible site, followed by the lumbosacral plexus, and 50% of the amyloid types were of type AL, for which there is no uniform treatment protocol.
Conclusions: Focal peripheral nerve amyloidosis is a rare amyloidosis that occurs in middle‐aged and elderly people, but also in young people, with focal neurological symptoms predominating, and histopathological testing is the gold standard for diagnosis, and mass spectrometry or immunohistochemistry can be improved to clarify the amyloid type.

FIGURE 1.

FIGURE 2.
eP‐MN‐A281
Evaluation of muscle biopsies in pediatric cases presenting with neuromuscular disease—Analysis of 720 cases from a single center
S. Erdogan 1, O. Herguner1, S. Zorludemir1
1Cukurova University Medical Faculty, Pathology, Adana, Turkey
Question: Muscle biopsy has an important role at the diagnosis of neuromuscular diseases in pediatric cases. The aim of this study is to examine and analyze the diagnoses of neuromuscular diseases in muscle biopsy samples of pediatric patients who referred to our center.
Methods: We evaluated the muscle biopsies of pediatric cases (<18 years old) that performed at Çukurova University Medical Faculty Hospital during the years of 2012–2022. The fresh muscle biopsy samples sent to our muscle laboratory were used to prepare frozen sections, which were then stained with hematoxylin and eosin (H&E) as well as various histological and immunohistochemical stains for specific proteins.
Results: When we look at the distribution by type, it can be seen that muscular dystrophy 276 (38.3%) and myopathy 184 (25.5%) are the most common diagnoses among the 720 patients. Within the muscular dystrophy group, dystrophinopathy (including Duchenne muscular dystrophy) was the most common subtype. Central core myopathy was the most common subtype among the congenital myopathies 19 (2.6%), while mitochondrial myopathy and glycogen storage disease were the most common types in the metabolic myopathy group 26 (3.6%). Neurogenic atrophy 36 (5%), inflammatory myopathy 17 (2.3%) were the other diagnoses. Non‐specific changes were 45 (6.2%). Additionally, there were some cases where biopsies were not appropriately submitted 21 (2.9%) or no pathological findings were observed 96 (13.3%).
Conclusion: After the implementation of genetic diagnostic methods, the preference for muscle biopsy in pediatric patients may have decreased. However, we believe that a muscle biopsy taken under appropriate conditions and subjected to histopathological evaluation is still one of the most reliable methods for evaluating specific protein losses and cellular structure, and for correlating clinical, laboratory, and molecular findings.
eP‐MN‐A282
MxA upregulation in smooth muscle—A case report of gastrointestinal perforation in NXP‐2‐dermatomyositis
M. Gao 1, D. Yue2, N. Cheng3,4,5, K. Jiao3,4,5, X. Xia3,4,5, N. Wang3,4,5, C. Zhao3,4,5, W. Zhu3,4,5
1Huashan Hospital Fudan University, Department of Pathology, Shanghai, China; 2Jing'an District Center Hospital of Shanghai, Department of Neurology, Shanghai, China; 3Huashan Hospital Fudan University, Department of Neurology, Shanghai, China; 4National Center for Neurological Disorder, Shanghai, China; 5Huashan Hospital, Shanghai Medical College, Fudan University, Huashan Rare Disease Center, Shanghai, China
Introduction: NXP‐2 dermatomyositis is a subtype of dermatomyositis. It primarily affects muscles and skin, causing symptoms such as muscle weakness, pain, wasting, and skin rash. Rare complications like gastrointestinal perforation may occur due to chronic inflammation or immunosuppressive medications. MxA, an interferon‐induced protein, was initially identified as a marker for myositis and dermatomyositis with high expression in skeletal muscle. The MxA expression in the smooth muscle of digestive tract is unknown.
Objectives: To investigate MxA expression in gastrointestinal smooth muscle and its correlation with clinicopathological features in patients with NXP‐2 antibody‐positive dermatomyositis.
Patients and Methods: A 33‐year‐old female patient with a history of immunosuppressive therapy was admitted to the hospital with abdominal pain, muscle pain, and weakness. She was found to be NXP‐2 seropositive with high creatine kinase levels, and imaging revealed a perforation in the ascending colon. A right hemicolectomy and colostomy were performed, and pathological examination showed chronic inflammation of the mucosa with upregulated MxA expression in smooth muscle and mTOR signaling expression in vasculitis. The patient died despite aggressive treatment with methylprednisolone and sirolimus.
Results: MxA expression is upregulated in the gastrointestinal smooth muscle of patients with NXP‐2‐positive dermatomyositis, while it is negative in normal controls. The exact etiology of NXP‐2 dermatomyositis is yet to be understood.
Conclusion: The expression of MxA in smooth muscle cells suggests interferon‐induced pathway involvement in gastrointestinal complication of NXP‐2 dermatomyositis.
eP‐MN‐A283
Differential resorption pathways of chitosan and collagen nerve tubes
R. Schober 1, S. Rein2,3, T. Kremer2
1Klinikum St. Georg gGmbH, Pathology and Tumor Diagnostics, Leipzig, Germany; 2Klinikum St. Georg gGmbH, Department of Plastic and Handsurgery, Burn Unit, Leipzig, Germany; 3Martin Luther University Halle‐Wittenberg, Halle‐Wittenberg, Germany
In peripheral nerve surgery following injury, nerve tubes are either used to bridge nerve gaps of up to 3 cm length or to protect nerve coaptations. Biodegradable nerve guides that are currently on the market include Chitosan or collagen‐based ones. Histological aspects of their degradation, highly relevant for the progress of neuronal regeneration, are mainly based on experimental studies so far. We have investigated four clinical cases that underwent secondary hand or arm surgery with removal of non‐degraded nerve tubes. The time between implantation and explanation varied between 6 months and 4 years for the two Chitosan tubes (Reaxon®) and 8 months for the two collagen tubes (Neuragen®). The documentation included both the operative situs and the histology and immunohistochemistry of the tubes and their contents as well of the adjacent tissue. The Chitosan tubes proved to be largely intact in their structure even several years after implantation, just losing small droplets of tube‐identical color to the covering cell layer and adjacent dense collagen respectively scar tissue. These then were apparently resorbed via Podoplanin‐positive lymphatic channels. The collagen tubes, in contrast, were progressively split from the periphery into individual strands with intervening loose matrix and small vessels, followed by macrophage resorption and some further scarification. Foreign body granulomas or significant inflammatory infiltrates were not seen in both tube types, they were restricted to suture granulomas. We conclude that the resorption process of Chitosan and collagen nerve tubes is very different in time and quality, which should be carefully considered in clinical applications. Further studies with different time intervals after implantation of the tubes and also with Chitosan tubes of different grades of acetylation are indicated to further specify the results.
eP‐MN‐A284
Gadolinium contrast agents—Dermal deposits and potential effects on epidermal small nerve fibers
A. Jeibmann 1,2, H. Krämer3, P. Bücker4, H. Richter5, A. Rosenbohm6, J. Jeske3, P. Baka7, C. Geber7,8, U. Karst4, A. Schänzer9, C. van Thriel10
1Institute of Neuropathology Münster, Muenster, Germany; 2University Hospital Munster, Institute of Neuropathology, Muenster, Germany; 3Justus‐Liebig‐University Giessen, Department of Neurology, Giessen, Germany; 4University of Münster, Institute of Inorganic and Analytical Chemistry, Muenster, Germany; 5University of Zurich, Department of Clinical Diagnostics and Services, Zurich, Switzerland; 6University hospital of Ulm, Department of Neurology, Ulm, Germany; 7University Medical Center Mainz, Department of Neurology, Mainz, Germany; 8DRK Pain Center Mainz, Mainz, Germany; 9Justus‐Liebig‐University Giessen, Institute of Neuropathology, Giessen, Germany; 10IfADo‐Leibniz Research Centre for Working Environment and Human Factors, Dortmund, Germany
Small fiber neuropathy (SFN) affects unmyelinated and thinly myelinated nerve fibers causing neuropathic pain with distal distribution and autonomic symptoms. In idiopathic SFN (iSFN), 30% of the cases, the underlying aetiology remains unknown. Gadolinium (Gd)‐based contrast agents (GBCA) are widely used in magnetic resonance imaging (MRI). However, side‐effects including musculoskeletal disorders and burning skin sensations were reported. We investigated if dermal Gd deposits are more prevalent in iSFN patients exposed to GBCAs, and if dermal nerve fiber density and clinical parameters are likewise affected. Twenty‐eight patients (19 females) with confirmed or no GBCA exposure were recruited in three German neuromuscular centers. iSFN was confirmed by clinical, neurophysiological, laboratory and genetic investigations; six volunteers (two females) served as controls. Distal leg skin biopsies were obtained according to European recommendations. In these samples Gd was quantified by elemental bioimaging and intraepidermal nerve fibers (IENF) density via immunofluorescence analysis. Pain phenotyping was performed in all patients, quantitative sensory testing (QST) only in a subset (15 patients; 54%). All patients reported neuropathic pain, described as burning (n = 17), jabbing (n = 16) and hot (n = 11) and five QST scores were significantly altered. Compared to an equal distribution significantly more patients reported GBCA exposures (82%), while 18% confirmed no exposures. Compared to unexposed patients/controls significantly increased Gd deposits and lower z‐scores of the IENF density were confirmed in exposed patients. QST scores and pain characteristics were not affected. This study suggests that GBCA exposure might alter IENF density in iSFN patients. Our results pave the road for further studies investigating the possible role of GBCA in small fiber damage, but more investigations and larger samples are needed to draw firm conclusions.
eP‐MN‐A285
Evaluation of clinicopathological and genetic spectrum of LAMA2 mutations in in an Indian cohort
S. Kanaujia 1, M. C. Sharma1, A. Dhall1, B. Jassal1, V. Suri1, M. Faruq1, U. Shamim1, R. Bhatia1, V. Venugopalan Y1, B. Chakarwarti1, S. Gulati1, S. Dagar1
1All India Institute of Medical Sciences, Pathology, Delhi, India
Background: LAMA2 associated myopathy is a group of recessive disorders resulting from mutations in the LAMA2 gene encoding alpha‐2 chain of laminin‐211. It is characterized by progressive muscular dystrophy and neuropathies resulting in severe congenital muscular dystrophy type 1A (MDC1A) to milder late‐onset milder limb girdle autosomal recessive 23 form (LGMDR23). It is diagnosed in routine practice with clinicopathological findings along with ancillary merosin IHC. With the introduction of NGS, diagnosis of LAMA2‐RDs is increasing along with expansion of morphological and phenotypic spectrum.
Aims: To study the clinical, pathological, and genetic spectrum of LAMA2 mutations in Indian cohort.
Methods: One hundred and ninety‐two patients (year 2018–2022) suspected of muscular dystrophy from unrelated families underwent phenotypic characterization followed by muscle histopathological analysis. These cases were subjected to targeted NGS using a customized panel of 88 genes. The sequencing data was annotated using VariMAT pipeline for generating variants.
Results: Eleven patients were diagnosed with LAMA2 myopathies amounting to a frequency estimation of 5.72% of all muscular dystrophies. Six patients presented with congenital muscular dystrophy type 1A while five were LGMDR23 phenotype. Ages from 5 months to 32 years. CPK levels ranged from 530 to 3018 U/L. Merosin IHC on muscle biopsy showed complete loss in three cases. NGS results revealed a total of 3 novel and 10 reported exonic mutations (frameshift 2), nonsense (4) and missense (7) across LAMA2 gene. One variant was inherited in homozygous state while all others were heterozygous (11).
Conclusion: In our study, targeted NGS enabled identification of a considerable proportion of mutations thus broadening the genetic and diagnostic spectrum of LAMA2‐RDs; and reinforcing that merosin IHC and clinical findings are mere adjuncts to diagnosing this entity, thus necessitating the use of NGS for a definitive diagnosis, specific treatment and family screening.
EPILEPSY
S09‐EP‐A286
Detection of brain somatic mutations in focal cortical dysplasia during epilepsy presurgical workup
S. Baldassari 1, R. Checri1, M. Chipaux2, S. Ferrand‐Sorbets2, E. Raffo2,3, C. Bulteau2,4, S. D. Rosenberg2, M. Doladilhe1, G. Dorfmüller2, H. Adle‐Biassette5, S. Baulac1
1Sorbonne Université, Paris, France; 2Department of Pediatric Neurosurgery, Rothschild Foundation Hospital, Paris, France; 3Université de Lorraine, Vandoeuvre‐lès‐Nancy, France; 4Université de Paris Cité, MC2Lab, Institut de Psychologie, Boulogne‐Billancourt, France; 5Université de Paris Cité, service d'Anatomie Pathologique, APHP, Hôpital Lariboisière, DMU DREAM, UMR 1141, INSERM, Paris, France
Background/objectives: Brain‐restricted somatic variants in genes of the mTOR signaling pathway cause severe focal epilepsies associated with focal cortical dysplasia type II (FCDII). We hypothesized that somatic variants could be identified from trace tissue adherent to explanted stereoelectroencephalography (SEEG) electrodes used in the presurgical epilepsy workup to map the epileptogenic zone.
Methods: We investigated three pediatric patients with drug‐resistant focal epilepsy subjected to neurosurgery, diagnosed with FCDII, and undergoing SEEG for a second presurgical evaluation. We performed deep gene panel sequencing on matched blood–brain DNA samples for variant discovery and ddPCR or deep amplicon sequencing for variant validation in DNA from individual SEEG electrodes.
Results: We identified low‐level mosaic somatic mutations in AKT3 and DEPDC5 genes in the resected brain tissues. From electrodes, we obtained on average 60 ng of DNA and identified 4/33 mutation‐positive samples in contact with the epileptogenic zone or at the border of the dysplasia from two patients.
Conclusions: We provide the proof‐of‐concept that somatic mutations with low levels of mosaicism can be detected from individual SEEG electrodes and support a link between mutation load and epileptic activity. The DNA recovered from SEEG electrodes would be sufficient to perform capture gene panel sequencing in routine diagnostic settings. Our findings emphasize future opportunities for integrating genetic testing from SEEG electrodes into the presurgical evaluation of refractory epilepsy patients to improve the patients diagnostic journey and guide toward precision medicine.
S09‐EP‐A287
Characterizing the hippocampal dentate gyrus involvement in temporal lobe epilepsy
Q. Zhang 1, C. Twible1
1Western University, Pathology, London, Ontario, Canada
Introduction: Hippocampal sclerosis (HS) is the most common pathology finding for drug‐resistant temporal lobe epilepsy (TLE). HS is diagnosed by identifying pyramidal neuronal loss and gliosis in Cornu Ammonis (CA). Dentate gyrus (DG) is the critical entry point to the hippocampus and is the only site with adult neurogenesis. However, changes in DG are not included in the current diagnostic criteria of HS. In this study, we will characterize the morphological and genomic features of the hippocampal DG in TLE patients and investigate the underlying epileptogenic mechanisms.
Methods: Twenty‐one TLE surgical resection cases (14 HS, 7 no‐HS) and 10 control cases were included. QuPath software was used to perform morphometry analysis on the DG, including Delaunay mean, cellular density, nuclear size and circularity. The DG of 18 selected TLE cases were micro dissected and underwent gene expression profiling, using NanoString targeted panels (1400 genes, targeted Neuroinflammation and Glial profiling panels). Histopathological diagnosis and post‐operative outcome were included for clinicopathological correlation.
Results: (1) HS patients show a significant increase in granule cell (GC) spacing and decrease in GC density within the DG compared to no‐HS patients. (2) Regardless of the clinical diagnosis, patients achieved seizure freedom post‐operatively (Engel outcome scale 1) demonstrated an increase in GC spacing and decrease in GC density in comparison to patients without significant seizure reduction (Figure 1). (3) The DG of HS patients demonstrated significant complement system activation, increased gliosis (both A1 and A2 astrocytes) and apoptosis; but decrease in neurogenesis and neuronal populations.
Discussion: Dentate gyrus has distinct morphometric features and gene expression in TLE patients, suggesting an important role in epileptogenesis.

FIGURE 1.
S17‐EP‐A288
DNA methylation classifier of ganglioglioma with adverse clinical outcome
L. Hoffmann 1, R. Coras1, K. Kobow1, I. Blümcke1, S. Jabari1
1Universitätsklinikum Erlangen, Department of Neuropathology, Erlangen, Germany
Question: Ganglioglioma (GG) is a common type of low‐grade brain tumor found in children and young adults with drug‐resistant focal epilepsy. However, diagnosing this type of epilepsy‐associated tumor can be challenging. Its differential diagnosis is controversial to many new entities in the 5th edition of the WHO brain tumor classification scheme. About 20% of patients with GG do not become seizure‐free after surgery, and this adverse postsurgical outcome is not reflected in the current WHO classification scheme.
Methods: To address this issue, we studied 128 low‐grade epilepsy‐associated brain tumors (LEATs) using whole exome sequencing, genotyping, and/or DNA‐methylation analysis. Clinical data were obtained from the European Epilepsy Brain Bank database and histopathology staining was available in all cases.
Results: The study revealed a novel DNA methylation class for GG defined by (1) PTPN11 alterations (a candidate gene in focal epilepsy), (2) copy number variant gains of chromosome 12, and (3) additional CNV gains in NF1, KRAS, FGFR4, and RHEB, as well as (4) BRAFV600E alterations. The histopathology of these tumors showed an unusual subarachnoidal tumor spread and large, pleomorphic, and multinuclear cellular features with a glial‐neuronal phenotype. The study also found that the proportion of patients who were free of disabling seizures two years after surgery was significantly lower (38% had Engel I) in the group of atypical GG tumors compared to the group of GG with only (85% having Engel I) BRAFV600E mutations.
Conclusion: These findings suggest the existence of a subgroup of GG with complex genetic alterations, adverse postsurgical outcomes, and cellular atypia in glial and neuronal cell components. These findings require prospective validation in clinical practice and modifications to the WHO grading system for developmental, glial‐neuronal tumors associated with early‐onset focal epilepsy.
S17‐EP‐A289
BRAF V600E mutation underlies some hippocampal and neocortical epileptogenic non‐expansive lesions
J. Lerond1, B. Mathon2, M. Scopin3, L. Nichelli4, J. Guégan5, C. Bertholle6, B. Izac6, M. Andrieu6, T. Gareau5, F. Donneger3, B. Mohand Oumoussa7, F. Letourneur6, S. Tran8, M. Bertrand5, I. Le Roux1, M. Touat9, S. Dupont10, J. C. Poncer3, V. Navarro11, F. Bielle 8
1Paris brain Institute, Paris, France; 2Sorbonne Université, Neurosurgery, Paris, France; 3Sorbonne Université, Institut du Fer À Moulin, Paris, France; 4Sorbonne Université, Neuroradiology, Paris, France; 5Paris brain Institute, Data Analysis Core, Paris, France; 6Université Paris Cité, Institut Cochin, Paris, France; 7Sorbonne Université, Plateforme Post‐génomiquedela Pitié‐Salpêtrière, Paris, France; 8Sorbonne Université, Neuropathology, Paris, France; 9Sorbonne Université, Neurology, Paris, France; 10Sorbonne Université, Rehabilitation Unit, Paris, France; 11Sorbonne Université, Neurology and EEG Unit, Paris, France
Introduction: The etiology of Mesial Temporal Lobe Epilepsy‐associated Hippocampal Sclerosis (MTLE‐HS) remains poorly understood. We previously identified CD34 positive extravascular stellar cells (CD34+ cells) with BRAF V600E immunopositivity in a subset of MTLE‐HS.
Objectives: We searched for the BRAF V600E mutation in epilepsy surgery specimens without radiological expansive lesion and characterized the CD34+ cells.
Patients and Methods: We screened 53 MTLE‐HS samples and 9 non‐expansive neocortical lesions resected during epilepsy surgery for BRAF V600E mutation by digital droplet polymerase chain reaction. BRAF WT MTLE‐HS, and BRAF V600E mutant non‐expansive lesion of hippocampus and/or neocortex were studied by ex vivo multi‐electrode array recording, immunolabeling, methylation microarray and single nucleus RNAseq.
Results: The BRAF V600E mutation was present in five MTLE‐HS samples with CD34+ cells and in five neocortical samples with CD34+ cells. Single nucleus RNAseq of resected samples identified two unique clusters of abnormal cells (including CD34+ cells) associated with senescence and oligodendrocyte development in both hippocampal and neocortical BRAF V600E mutant samples. Multiplex immunostaining confirmed the co‐expression of the oncogene‐induced senescence marker p16 and, the outer subventricular zone radial glia progenitor marker HOPX, and phosphoERK in CD34+ cells. Pseudotime analysis showed that abnormal clusters mimicked a developmental lineage from progenitors to myelinating oligodendrocytes. Epilepsy surgery achieved seizure freedom in 8 of the 10 patients with BRAF mutant lesions.
Conclusion: A subset of MTLE‐HS and epileptogenic non‐expansive neocortical focal lesions with CD34+ cells involved the BRAF V600E mutation. Our results advocate for CD34 immunostaining of epilepsy surgery samples and detection of the BRAF V600E mutation, which may help diagnosis and opens perspectives of targeted therapies.
S17‐EP‐A290
Mild malformation of cortical development with oligodendroglial hyperplasia in epilepsy (MOGHE)—First case series from Latin‐America
J. Cienfuegos Meza 1,2, M. A. Alonso Vanegas2, I. Tapia del Río2, E. D. J. Quintero López2, E. Brust Mascher2
1National Institute of Neurology and Neurosurgery Manuel Velasco Suárez, Neuropathology, Mexico City, Mexico; 2International Center for Epilepsy Surgery HMG Hospital, Neurosurgery, Mexico City, Mexico
Purpose: Mild malformation of cortical development with oligodendroglial hyperplasia in epilepsy (MOGHE) is an emerging, highly epileptogenic pathological entity in drug‐resistant epilepsy. While defining its clinical features remains an ongoing process, research has demonstrated that patients with MOGHE tend to have lesions primarily impacting the frontal lobe, and knowledge about this entity continues to expand. Consequently, additional clinical aspects are being evaluated for their correlation with MOGHE. This is a case series of five patients from México who underwent epilepsy surgery with MOGHE as the neuropathological diagnosis. Clinicopathological features are described.
Methods: Descriptive analysis of clinical characteristics, EEG patterns, seizure semiology, radiological findings, surgical outcomes, and neuropathology description were conducted in a cohort of five Mexican patients were neuropathologically diagnosed after epilepsy surgery.
Results: Four patients were male, one was female. Seizure semiology correlated with EEG findings and all five patients had localized lesions in frontal lobe (three right, two left). En bloc frontal lobectomy was performed. Neuropathology evaluation showed areas of increased subcortical cellularity by oligodendrocytes (Olig2 positive) with no proliferative activity, and heterotopic neurons in the white matter, without any other lesion. Surgical outcomes at one year follow‐up revealed four patients in Engel IA and one with Engel IB.
Conclusion: MOGHE represents an extensive and complex pathology with white matter lesions. Distinction from focal cortical dysplasia is important, as clinicopathological and molecular features are different.
S17‐EP‐A291
Loss of maturity and homeostatic functions in TSC astrocytes: A potential aggravator of epilepsy and inflammation?
M. Luinenburg 1, M. Scheper1, A. Mühlebner2, E. Aronica1
1Amsterdam UMC, Pathology, Amsterdam, Netherlands; 2UMC, Pathology, Utrecht, Netherlands
Question: What are the biological differences between TSC and control astrocytes in regards to the maturity and homeostatic function such as glutamate buffering and phagocytosis?
Methods: We used single nuclei sequencing (6 control, 11 TSC) in combination with an primary‐isolated in vitro model (4 control, 5 TSC) to interrogate the functional differences. These include maturity, the ability to maintain glutamate homeostasis and the real‐time clearance of pHrodo‐red conjugated crude synaptic fractions. All of the in vitro assays included inflammatory conditions to add a dimension of modulation (IL1‐β, C1q, TNF‐α or IL1‐α, TNF‐α). Seven days prior to the assay, cells were incubated in defined FCS‐free media to better simulate the brain environment.
Results: TSC astrocytes show reduced maturity on RNA and protein level, the inability to clear excess glutamate through the loss of both enzymes and transporters complementary to a complete loss of phagocytic capabilities when compared to control astrocytes.
Conclusions: In this study, we employed a combination of snRNA sequencing together with an primary in vitro model to assess the changes observed in human TSC derived astrocytes on cell maturity and two homeostatic function; glutamate buffering and debris phagocytosis. We can conclude from our collected evidence that these functions are indeed impaired and could aggravate the pathological systems present in TSC patients.
PS4‐EP‐A292
Mild malformations of cortical development with oligodendroglial hyperplasia in epilepsy (MOGHE) and with pathogenic SLC35A2 mutations reveal aberrant protein distribution and myelin loss
E. Cecchini 1, L. Hoffmann1, R. Coras1, S. Jabari1, T. Hartlieb2,3, C. Stadelmann4, K. Kobow1, I. Blümcke1
1Universitätsklinikum Erlangen, Department of Neuropathology, Erlangen, Germany; 2Schoen‐Clinic, Center for Pediatric Neurology, Neurorehabilitation, and Epileptology, Vogtareuth, Rosenheim, Germany; 3Paracelsus Medical University, Research Institute for Rehabilitation, Transition, and Palliation, Salzburg, Austria; 4University Medical Center Gottingen, Institute for Neuropathology, Goettingen, Germany
We aimed to histopathologically characterize MOGHE with gene mutations in the solute carrier family 35 member A2 (SLC35A2), which codes for a galactose transporter involved in sphingolipid glycosylation. Surgical brain tissue from 28 MOGHE patients and controls were analyzed using a new N‐terminal SLC35A2 antibody and electron microscopy. Our preliminary results revealed five interesting observations: (1) A decrease of SLC35A2 protein in MOGHE cases carrying the mutation compared to MOGHE without SLC35A2 mutations and controls. Thereby, variant allelic frequency inversely correlated with SLC35A2 protein abundance. (2) SLC35A2 protein primarily localized to the Golgi apparatus (arrows in Figure 1A). (3) Aberrant SLC35A2 staining appeared at the Golgi outpost close to myelin sheets (Figure 1C,D). (4) However, transmission electron microscopy (TEM) confirmed a dramatic loss of myelination in MOGHE (Figure 2D). (5) Oligodendroglial nuclei within the MOGHE lesion showed a high proportion of heterochromatin compared to controls (Figure 2B). Our results support our previous assumption of a myelination deficiency in MOGHE and the important role of SLC35A2 in myelin maintenance. Further investigations are needed to understand MOGHE disease mechanism, that is, oligodendroglial hyperplasia and epilepsy, but also myelin regeneration observed during the long‐term course of the disease.

FIGURE 1 SLC35A2 immunoreactivity in MOGHE. A control (A) with perinuclear accumulation of SLC35A2 (red, arrows). MOGHE (B and C) with loss of perinuclear and neuropil staining. SLC35A2 protein co‐localized with CNPase (green, arrows in D).

FIGURE 2 There is a significant reduction of myelinated axons in MOGHE (B and D) compared to perilesional tissue of same cases (A and C). Un‐/dysmyelinated axons in D (e.g., asterisks). Lesional oligodendrocyte with heterochromatin enriched nucleus (B, arrow).
PS4‐EP‐A293
Patterns of pTau in focal cortical dysplasia type III and acquired lesions in an epilepsy surgical series
A. Mrzyglod 1, A. Mebrouk1, M. Ryniejska1, M. Thom1
1UCL Queen Square Institute of Neurology, Department of Clinical and Experimental Epilepsy, London, United Kingdom
Introduction: Phosphorylated Tau protein (pTau) has been reported in the context of focal cortical dysplasia (FCD) type II and hippocampal sclerosis in focal epilepsy. Its prevalence in FCD type III (“acquired dysplasias”) is unexplored. Whether pTau in epilepsy is driven by mTOR activation, seizures, or inflammation is unclear. CTE patterns have also been reported and brain trauma due to seizures may be a further factor.
Objectives: To investigate pTau patterns in a broad range of early and late acquired focal brain lesions in an epilepsy surgical series.
Materials and Methods: Cases were selected from the epilepsy tissue bank to include FCD type IIIA, IIIB, IIIC/vascular malformations (Sturge Weber syndrome [SWS], cavernomas), IIID (perinatal brain injury/Rasmussen's encephalitis [RE]), encephaloceles and acute and chronic brain injuries. AT8 immunohistochemistry was carried out and selected cases were further investigated for other pTau epitopes, pS6(240,235)/mTOR activation, neuronal and glial lineage markers.
Results: Findings included pTau accumulation in the gliotic parenchyma adjacent to cavernomas and in association with SWS. In FCDIIID/perinatal infarcts, pTau in the subpial layer, residual neurones in layer II, cytomegalic neurones and periventricular and white matter neuronal heterotopia were noted. In contrast, FCDIIID/RE cases often showed little pTau. pTau was observed in old scars following brain injury and the gliotic cortical surface of encephaloceles. pS6(240,235)/mTOR activation and microglial upregulation were observed with some lesions.
Conclusions: Varied pTau accumulation is noted in association with focal acquired epileptogenic lesions. Patterns in early brain injury are reminiscent of persistent fetal pTau, whereas, in other pathologies, traumatic damage and vascular impairment may be relevant. The significance of pTau for progression and impact on cognitive impairment in focal epilepsies remains unclear.

FIGURE 1.

FIGURE 2.
PS4‐EP‐A294
IGF‐1R expression is associated with memory performance in patient with temporal lobe epilepsy and type 2 hippocampal sclerosis
H. Cruz1, R. C. Scandiuzzi2, T. Velasco2, J. P. Leite2, J. E. Peixoto‐Santos 1
1Unifesp, Neurology and Neurosurgery, São Paulo, Brazil; 2University of Sao Paulo, Neurosciences and Behavioral Sciences, Ribeirao Preto, Brazil
Question: Patients with mesial temporal lobe epilepsy (TLE) and hippocampal sclerosis in the left hemisphere often present with verbal memory deficits. According to recent studies, these deficits are linked to neuronal loss in the hippocampal granular cell layer (GCL), which is seen in patients with hippocampal sclerosis (HS) ILAE types 1 and 3, but not HS type 2. However, some patients with HS type 2 can present memory deficits. Since some studies showed the effects of insulin‐like growth factor (IGF1), we aimed to investigate whether differential expression of IGF1 receptor (IGF‐1R) on the GCL correlated with memory performance in patients with HS type 2.
Methods: We selected patients with left TLE and hippocampal sclerosis type 2 and divided them into two groups: normal memory (NM, n = 10), and memory deficit (MD, n = 11), based on the overall performance in the Logical Memory (LM) test of the Revised Wechsler Memory Scale and in Rey Auditory Verbal Learning Test (RAVLT). Hippocampal sections of these patients were immunostained for NeuN and IGF‐1R and evaluated for neuron density and IGF‐1R integrated optic density, respectively.
Results: There was no difference in GCL neuronal density between NM and MD groups, or any correlation between neuronal density and the scores of RAVLT or ML. Patients with NM had a higher expression of IGF‐1R in the outer layer of the GCL and in the Subiculum compared to those with MD. The expression of IGF‐1R in the GCL correlated positively with RAVLT's learning score (r = 0.664, p = 0.018), late recall score (r = 0.611, p = 0.035), and average score (r = 0.594, p = 0.042).
Conclusion: The expression of IGF‐1R in the GCL correlates positively with verbal memory performance in patients with left TLE and HS type 2.
PS4‐EP‐A295
White matter microvasculature in temporal lobe epilepsy and neurite orientation dispersion and density imaging (NODDI) correlations
M. Thom 1, S. Patodia1, Y. Lim1, J. Liu1, L. Binding1, M. Koepp1
1University College London, Neuropathology, London, United Kingdom
Introduction: Widespread white matter (WM) abnormalities are recognised in temporal lobe epilepsy (TLE) with diffusion weighted imaging (DWI), with differences between superficial and deep WM correlating with cognitive impairment. Microstructural changes are reported on neurite orientation dispersion and density imaging (NODDI). Microangiopathy has been reported which may be relevant to WM pathology.
Objectives: To investigate WM angiopathy in TLE compared to control groups, other WM pathology and correlations with diffusion NODDI imaging.
Materials and Methods: In 45 TLE temporal lobe resections, regions of interest (ROI) in the superficial (gyral core) and deep WM was compared to control groups. NODDI imaging in 26 TLE cases was co‐registered with ROI for comparison. Microvasculature was evaluated using COL41a, SMA and PDGFRb (pericytes) immunohistochemistry and vessel density, size, and pericyte coverage quantified. Cases were further quantified using a broad panel of axonal, myelin, matrix and glial markers, gene‐expression data and compared to clinical and neuropsychology indicators.
Results: Vascular sclerosis was significantly increased in the TLE group and age independent. Regionally increased WM vessel densities were noted in TLE with COL41a/SMA/PDGFRb with increased pericyte coverage and reduced mean vessel diameters. We noted greater differences in vascular measures between core and deep WM compared to controls, paralleled by similar regional differences in NODDI metrics. Vascular pathology also correlated with WM myelin and axonal reduction and glial densities in TLE. Altered WM angiogenesis gene‐expression was noted in TLE.
Conclusions: Altered microvasculature in TLE includes degenerative vascular sclerosis, increased density of small vessels and pericytes with evidence for a gradient between core and deep white matter. These may be critical to other degenerative white matter pathology, observed DWI alterations and neuropsychology impairment.

FIGURE 1.
PS4‐EP‐A296
Epileptogenic lesions with predilection for white matter involvement
D. Metodiev 1, K. Minkin2, P. Dimova2, M. Penkov3, T. Tododrov4, A. Todorova4, D. Parvanov5, M. Russeva5, R. Ganeva5, S. Nachev1
1Neuropathological Laboratory, University Hospital “Saint Ivan Rilski,” 1431 Sofia, Bulgaria, Neuropathology, Sofia, Bulgaria; 2University Hospital “Saint Ivan Rilski,” Epilepsy Surgery Center, Sofia, Bulgaria; 3University Hospital “Saint Ivan Rilski,” Department of Radiology, Sofia, Bulgaria; 4Genetic and medico diagnostic laboratory, Genica, Genetics, Sofia, Bulgaria; 5Nadezhda Women's Health Hospital, Department of Research, Sofia, Bulgaria
The 2022 revised ILAE classification of FCD includes new pathological entities predominantly affecting the white matter. The detection of subcortical heterotopic neurones in the absence of other structural lesion is defined as mild malformation of cortical development (mMCD). The presence of heterotopic neurones, in combination with oligodendroglial hyperplasia and blurring of the grey–white matter boundary are determining features of the recently defined condition—mild malformation of cortical development with oligodendroglial hyperplasia (MOGHE). The purpose of our study is to identify the frequency, the histopathological findings, and the differences in lesions which predominantly affect the white matter and can lead to pharmacoresistant epilepsy. Our study included 13 histopathologycally proven cases with mMCD (9 cases) and MOGHE (4 cases), from 202 consecutive patients operated for drug‐resistant epilepsy. Brain tissue materials were embedded in paraffin using routine histological techniques. Further immunohistochemical examinations were performed. The majority of MOGHE cases were genetically proven (SLC35A2). We examined 13 cases with epileptogenic lesions with predilection for white matter involvement (6.4% of our series). Mild MCD was more commonly diagnosed in adults, and predominantly involved the temporal lobe. The paediatric patient group was predominantly represented by cases with MOGHE, with frontal localisation only. Neuronal heterotopia was present in both lesions, but in mMCD it involved deeper areas of cerebral white matter. The epileptogenic lesions with predilection involvement of white matter are a rare cause for pharmacoresistant epilepsy. MOGHE are found only in the frontal lobe and mMCD have a temporal predilection. The genetic examination may provide further insight into the mechanisms underlying these conditions thereby opening novel therapeutic avenues as has been the case with MOGHE (oral galactose supplementation).
PS4‐EP‐A297
Synapse‐specific changes in Arc and BDNF in rat hippocampus following chronic temporal lobe epilepsy
D. L. Egbenya 1, S. Hussain2, Y. C. Lai3, A. E. Anderson3, S. Davanger2
1University of Cape Coast, Physiology, Cape Coast, Ghana; 2University of Oslo, Division of Anatomy, Department of Molecular Medicine, Oslo, Norway; 3Baylor College of Medicine, Jan and Dan Duncan Neurological Research Institute, Houston, TX, United States
Introduction: Expression of immediate early genes (IEGs) in the brain is important for synaptic plasticity, and probably also in neurodegenerative conditions.
Objective: To understand the cellular mechanisms of the underlying neuropathophysiological processes in epilepsy, we need to pinpoint changes in concentration of synaptic plasticity‐related proteins at subsynaptic levels.
Materials and Methods: In this study, we examined changes in synaptic expression of activity‐regulated cytoskeleton‐associated (Arc) and brain‐derived neurotrophic factor (BDNF) in a rat model of kainate‐induced temporal lobe epilepsy (TLE) using western blotting and electron microscopy.
Results: Western blotting showed reduced concentrations of Arc and increased concentrations of BDNF in hippocampal synaptosomes in chronic TLE rats. Then, using quantitative electron microscopy, we found corresponding changes in subsynaptic regions in the hippocampus. Specifically, we detected significant reductions in the concentrations of Arc in the presynaptic terminal of Schaffer collateral glutamatergic synapses in the stratum radiatum of the CA1 area in TLE, as well as in their adjacent postsynaptic spines. In CA3, there was a significant reduction of Arc only in the presynaptic terminal cytoplasm. Conversely, in CA3, there was a significant increase in the expression of BDNF in the presynaptic terminal, but not in the postsynaptic spine. Significant increase in BDNF concentration in the CA1 postsynaptic density was also obtained.
Conclusion: The observed changes in Arc and BDNF may contribute to both cognitive impairments and increased excitotoxic vulnerability in chronic epilepsy.
PS4‐EP‐A298
Mild malformation of cortical development with oligodendroglial hyperplasia in epilepsy (MOGHE) and a brain lesion histologically identical to MOGHE in a clinically non‐epilepsy patient
H. Miyata 1, N. Oka2, N. Sakamoto3, S. I. Osawa4, Y. Kubota5,6, E. Ishikawa7, H. Suzuki2,8
1Research Institute for Brain and Blood Vessels, Akita Cerebrospinal and Cardiovascular Center, Department of Neuropathology, Akita City, Japan; 2National Hospital Organization, Sendai Medical Center, Department of Pathology and Laboratory Medicine, Sendai, Japan; 3Institute of Medicine, University of Tsukuba, Department of Diagnostic Pathology, Tsukuba, Japan; 4Tohoku University Graduate School of Medicine, Department of Neurosurgery, Sendai, Japan; 5TMG Asaka Medical Center, Epilepsy Center, Asaka City, Japan; 6Adachi Medical Center, Tokyo Women's Medical University, Department of Neurosurgery, Adachi‐ku, Japan; 7Institute of Medicine, University of Tsukuba, Department of Neurosurgery, Tsukuba, Japan; 8South Miyagi Medical Center, Department of Pathology, Ogawara Town, Japan
MOGHE is a recently identified epileptogenic lesion that frequently carries mosaic SLC35A2 variants and mainly affects cerebral white matter (WM). We report two patients with MOGHE and a non‐epilepsy patient with a brain lesion histologically identical to MOGHE. Case 1 is a 32‐year‐old (yo) woman with histories of febrile seizure with status epilepticus at age 1 and MRI non‐lesional focal impaired awareness seizure since age 14. Temporal lobectomy with amygdalohippocampectomy at age 26 was ineffective, with a pathological diagnosis of no lesion. Eventually, the left frontal lobectomy was performed based on EEG findings and blurred cortex (CTX)‐WM junction on MRI (Engel class III). Case 2 is a 23‐yo man with MRI non‐lesional left frontal lobe epilepsy since age 9. Resection of the pars triangularis in the inferior frontal gyrus was performed (Engel class II). Case 3 is a 31‐yo man with a headache and no history of epilepsy. MRI revealed a widespread blurred CTX‐WM junction in the right frontal and temporal lobes, and the latter was partially resected. Histopathological examination of the surgical specimens revealed features consistent with MOGHE in all three cases, including the following common findings: (1) foci of myelin pallor in shallow subcortical WM with excess heterotopic neurons and astrogliosis, (2) excess numbers of olig2‐positive nuclei in WM (>3000/mm2), (3) perineuronal satellitosis in the deeper cerebral cortex, and (4) mildly enlarged oligodendroglial nuclei with weaker olig2 immunoreactivity. Ki‐67 labeling indices were focally higher (2%) in cases 1 and 2 than in case 3 (<0.1%). Genetic analysis by whole exome sequencing using FFPE tissue identified heterozygous SLC35A2 variants in cases 1 and 2 but not in case 3. The lesion in case 3 suggests a molecular basis distinct from SLC35A2 alteration. It may reflect a broader clinicopathological spectrum of mMCD with oligodendroglial hyperplasia, including patients without the clinical manifestation of epilepsy.

FIGURE 1.

FIGURE 2.
PS4‐EP‐A299
Epileptic seizures revealing Sturge Weber's disease in a tropical environment—Study of eight cases
S. M. Diallo 1, M. B. Diallo1, M. L. Toure1
1Hopital National Igance Deen, Service de Neurologie, Conakry, Guinea
Introduction: In sub‐Saharan Africa (SSA), the etiological factors of epilepsy are multiple and phacomatoses, in particular Sturge Weber's disease, are rarely reported due to under medicalization and insufficient multidisciplinary care.
Patients and Methods: We carried out a retrospective study of 216 patients hospitalized for recurrent epileptic seizures between 2015 and 2022 in the neurology and pediatrics department of the University Hospital Center of Conakry, among whom eight patients were identified for Sturge Weber's disease in order to reassess this pathology from a clinical and paraclinical point of view in a tropical environment.
Results: Sturge Weber's disease was retained in eight on the presence of symptomatic partial epileptic seizures (age 6 months to 14 years) with frequency of status epilepticus, homonymous lateral hemiparesis linked to occipital involvement, piriform calcifications on imaging and ocular disorders. The delay in consultation and medical care revealed severe mental deterioration in our patients.
Conclusion: This study shows a stereotyped clinical picture in a context of aggravation of signs related to a delay in multidisciplinary management. These results are important for the diagnostic, therapeutic and prognostic discussion.
Keywords: Conakry‐Guinea, Sturge Weber disease.
eP‐EP‐A300
A deep learning‐based histopathology classifier for focal cortical dysplasia
J. Vorndran 1, I. Blümcke1, S. Jabari1
1University Hospital Erlangen, Neuropathology, Erlangen, Germany
A light microscopy‐based histopathology diagnosis of human brain specimens obtained from epilepsy surgery remains the gold standard to confirm the underlying cause of a patients focal epilepsy and further inform postsurgical patient management. The differential diagnosis of neocortical specimens in the realm of epilepsy surgery remains, however, challenging. We developed an open access, deep learning‐based classifier to histopathologically assess whole slide microscopy images (WSI) and to automatically recognize various subtypes of focal cortical dysplasia (FCD), according to the ILAE consensus classification update of 2022 by training of a convolutional neuronal network (CNN) with fully digitalized WSI of hematoxylin–eosin stainings obtained from 125 patients covering mMCD, MOGHE, FCD1a, FCD2a and FCD2b using 414 archival tissue blocks. An additional series of 198 postmortem tissue blocks from 59 patients without neurological disorders served as control to train the CNN for homotypic frontal, temporal and occipital areas and heterotypic Brodmann Areas 4 and 17, entorhinal cortex and dentate gyrus. Special stains and immunohistochemical reactions were used to comprehensively annotate the region of interest. We then programmed a novel tile extraction pipeline and graphical dashboard to visualize all areas on the WSI recognized by the CNN. Our deep learning‐based classifier is able to compute 1000 × 1000 μm large tiles and recognizes 25 anatomical regions and FCD categories with an accuracy of 98.8%. Microscopic review of regions predicted by the network confirmed these results. This deep learning‐based classifier will serve as blueprint to build a digital histopathology slide suite addressing all major brain diseases encountered in patients with surgically amenable focal epilepsy. Full text published online in “Neural Computation and Application” March 9th 2023 (see https://rdcu.be/c7bWq).

FIGURE 1.

FIGURE 2.
eP‐EP‐A301
The effects of chronic morphine administration on kindling‐induced epileptiform activity in hippocampal CA1 pyramidal neurons of male Wistar rats
M. Abdollahzade 1
1Veterinary Medicine School of Tabriz University, Basic science, Tabriz, Iran
Introduction: The purpose of this study is to examine the effects of simultaneous and chronic use of morphine as measured through electrophysiological means on the alteration of seizure‐like activities caused by PTZ chemical kindling, including changes in number, amplitude, and onset time.
Method: Forty male Wistar rats, with weights ranging from 200 to 250 g, were randomly assigned to four groups of normal saline (negative control, 1 mL/kg), diazepam (positive control, 2 mg/kg), morphine 2 and 10 mg/kg with 10 animals in each group. Animals were administered daily intraperitoneal doses of diazepam, normal saline, or morphine for a period of 10 weeks. Pentylenetetrazole 35 mg/kg was administered every other day for 10 weeks to induce kindling. At the end of 10 weeks, the animals were anesthetized with the ketamine‐xylazine combination (80 + 8 mg/kg, intraperitoneally). A 1.5–2 cm longitudinal incision was made in the head region, with Bregma being identified based on Watson's coordinates. An electrode was then positioned within the CA1 region of the hippocampus, whereupon the brain's basic activity was recorded for 5 min in a baseline state. Subsequently, 80 mg/kg of pentylenetetrazole was administered intraperitoneally to induce seizure activity. Following the induction of activities using the eLab device, field action potentials were collected from the CA1 region of the hippocampus, and diazepam 2 mg/kg was administered to suppress the desired activities.
Result: In a group of animals that received morphine at dose levels of 2 and 10 mg/kg, convulsive activities showed a significant increase in terms of the number of spikes compared to the control group. However, the amplitude of convulsive activities and their onset time does not show a significant difference compared to the control group.
Conclusion: A dose‐dependent increase in seizure activity was observed when chronic morphine use was combined with kindling caused by pentylenetetrazol.

FIGURE 1.

FIGURE 2.
eP‐EP‐A302
Hippocampal T2 relaxation correlates with the levels of functional astroglial proteins in patients with mesial temporal lobe epilepsy
I. L. Arruda1, R. F. Arruda1, H. Carrete Junior1, R. D. S. Centeno1, J. C. Duarte1, M. S. B. Guaranha1, L. M. D. Guilhoto1, E. M. Yacubian1, T. Velasco2, J. P. Leite2, C. E. G. Salmon3, A. C. D. Santos4, J. E. Peixoto‐Santos 1
1Unifesp, Neurology and Neurosurgery, São Paulo, Brazil; 2University of Sao Paulo, Neurosciences and Behavioral Sciences, Ribeirao Preto, Brazil; 3University of Sao Paulo, Physics and Mathematics, Ribeirao Preto, Brazil; 4University of Sao Paulo, Internal Medicine, Ribeirao Preto, Brazil
Question: Mesial temporal lobe epilepsy is the most frequent focal pharmacoresistant epilepsy with surgical indication. Most patients have hippocampal sclerosis, characterized by reduced volume and increased T2 signal on preoperative MRI. Since gliosis is often associated with the increased T2 signal, we aimed to compare whether functional glial markers such as metallothioneins I and II (MT‐I/II) and the glutamate transporter EAAT2 had a stronger correlation with the T2 signal than the expression of the structural astroglial protein GFAP.
Methods: Patients with temporal lobe epilepsy and hippocampal sclerosis (n = 44) who underwent axial multi‐echo T2 MRI scan at a 3 Tesla machine (TEs = 20–100 ms; TR = 3000 ms; voxel = 1 × 1 × 3 mm) were selected. Hippocampal sections were submitted to immunohistochemistry for the detection of EAAT2, MT‐I/II, and GFAP proteins. T2 relaxation time, and immunostaining intensity for selected glial proteins were quantified.
Results: Twenty patients had T2 relaxation within the normal range (107.4 ± 6.9 ms) and 22 had increased hippocampal T2 relaxation (132.6 ± 13.4 ms). Cases with increased T2 relaxation had higher GFAP staining in CA2 (p = 0.03) and a trend towards reduced EAAT2 staining in CA4 and increased MT‐I/II expression in CA2 (p > 0.05). Hippocampal T2 relaxation time correlates positively with the immunostaining for MT‐I/II (r = 0.507, p = 0.005), and GFAP (r = 0.371, p = 0.043) in CA2 and negatively with EAAT2 in CA4 (r = −0.373, p = 0.016). A stepwise linear regression indicated that the combination of MT‐I/II immunostaining in all CA subfields, EAAT2 immunostaining in the granule cell layer, CA4‐CA2, and the subiculum, and GFAP immunostaining in CA4 explain 77% of the hippocampal T2 relaxation (r = 0.88, p < 0.0001).
Conclusions: Our study indicated that the increased T2 relaxation is strongly related to functional rather than structural astroglial proteins.
eP‐EP‐A303
Retrospective cohort study of 2068 patients with drug‐resistant epilepsy—Etiology analysis
J. Li 1
1West China Hospital, Department of Neurology, Chengdu, China
Objective: To investigate the pathological etiolog of patients with drug‐resistant epilepsy in West‐South China.
Methods: In this retrospective study, pathological and clinical data of consecutive cases of intractable epilepsy receiving surgical resection between January 1, 2011, and December 31, 2020 at West China Hospital and Guangdong Sanjiu Brain Hospital were assessed. Clinical data, which included demographic characteristics, seizure classification, imaging data, video electroencephalogram (VEEG) data were collected. Immunohistochemical markers including NeuN, NF, MAP‐2, GFAP, MN, EMA, SMI32, Oligo2, MOG, Mutant IDH1/2 and Ki67 and so forth were used. Logistic regression was used to identify relationships between data variables and etiology of drug‐resistant epilepsy.
Results: We retrospectively reviewed 2099, of which 31 patients were excluded due to incomplete clinical data (lack of age at seizure onset and pathological diagnosis). The onset of seizures occurred before 18 years of age in 66.0% of patients overall, and 69.8% of the patients underwent surgery as adults. The mean duration of epilepsy before surgery was 10.4 years among adults and 4.2 years among children. The temporal lobe was involved in 60.5% of operations. The most common pathological diagnosis was hippocampal sclerosis, found in 26.5% of the patients (83.8% were adults and 16.2% were children.), epilepsy‐associated tumors in 21.3% patients (68.9% of cases were adults, 31.1% of cases were children.), and malformations of cortical development in 17.6% (53.3% of cases were adults, 46.7% were children). 7.6% of patients with drug‐resistant epilepsy had no histopathological abnormal finding.
Conclusions: In patients with drug‐resistant focal epilepsy requiring surgery, hippocampal sclerosis, epilepsy‐associated tumors, cortical dysplasia, vascular malformation and glial scar were the most common causes, which was consistent with previous reports.

FIGURE 1.

FIGURE 2.
eP‐EP‐A304
Hyaline eosinophilic astrocytic inclusions in two children with drug‐resistant epilepsy—Case reports and literature review
M. Mezmezian 1, N. Arakaki1, P. Yañez2, E. Arias‐Cebollada1, V. Muro3, G. Sevlever1
1Fleni, Department of Neuropathology and Molecular Biology, Buenos Aires, Argentina; 2Fleni, Department of Diagnostic Imaging, Buenos Aires, Argentina; 3Hospital Britanico, Department of Neurology, Buenos Aires, Argentina
Introduction: Hyaline eosinophilic astrocytic inclusion (HEAI) is a rare histological finding in cases with drug‐resistant epilepsy (DRE).
Objectives: To describe two cases of DRE with HEAI and review the literature.
Patients and Methods: Case 1: A 5‐year‐old boy with a history of DRE since 5 months of age and global developmental delay, nonverbal (GDD, NV). MRI revealed signs of polymicrogyria, involving the right frontal operculum with an abnormal cortical folding and rotation pattern. The genetic panel showed a variant of uncertain significance in the SCL2A1 gene. Outcome: Engel IV‐B. Case 2: A 5‐year‐old boy with a history of DRE since 4 months of age and GDD, NV. MRI showed abnormal cortical folding and cortical thickening in the right frontal lobe. Genetic testing demonstrated a variant of uncertain significance in the ADAR gene. Outcome: Engel IV‐A. Resection of the lesion was performed in both patients.
Results: Both cases showed brightly eosinophilic structures within the astrocytic cytoplasm in the gray matter and FCD type 2A. The inclusions were negative with PAS and Congo red. By immunohistochemistry, they were positive for S100 and negative for vimentin, and GFAP. We also analyzed the data of all the previously reported cases.
Conclusion: HEAI is a rare entity, with only 53 cases reported, including our cases. Evaluating all the cases, the average age at seizure onset of pediatric patients (n = 48) was 7 months, without sex predilection. Seven patients had Aicardi syndrome, and 23 patients presented GDD. Seizures were observed in 47 patients. Outcome Engel: I in 10 cases, II in 5, III in 9, and IV in 9. Most cases involved the frontal lobe (n = 40). HEAIs were positive for S100 in 21/25 (84%), filamin in 22/25 (88%), GFAP in 3/32 cases (9%), vimentin in 1/16 (6%), and PAS in 3/21 (14%). FCD was observed in 19/50 patients (38%). The significance of HEAI is not clear. Genetic studies of the surgical specimens will probably allow a better comprehension of this entity.
eP‐EP‐A305
Validation of the Georgian version of the stigma‐scale of epilepsy (SSE)
M. Lazariashvili1 , S. Kasradze1,2, N. Gogatishvili1,2
1Institute of Neurology and Neuropsychology, Department of Neurology, Tbilisi, Georgia; 2Caucasus International University, CIU, Tbilisi, Georgia
Background: Common misconceptions and negative attitudes towards epilepsy often cause significant psychosocial problems in patients with epilepsy, which complicate treatment and worsen the course of the disease. Therefore, assessing the components of epilepsy stigma with reliable tools is essential for planning appropriate interventions. Since the international questionnaire has not yet been validated in the Georgian language, studies on the stigmatization of epilepsy in the country have not yet been conducted.
Purpose: Adaptation and validation of the epilepsy stigma scale (ESS) in Georgian.
Methods: The study was carried on the base of INN. SSE—questionnaire was elaborated by the one‐wards‐backwards translations by three independent specialists, checked for gross inconsistencies or conceptual errors between the original source and the back‐translated format, and final Georgian version of SSE was created. Descriptive statistics were used for demographic variables. The Kolmogorov–Smirnov and the Shapiro–Wilk tests were used to assessing the normality of the distribution of continuous variables. Internal consistency of the Georgian versionSSE was assessed with Cronbach's alpha. Statistical analyses were performed using SPSS (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp). A probability <0.05 was considered statistically significant.
Results: 87 adult people were enrolled in the study: 32 (36.8%) with diagnosed epilepsy (EPI), and 55 (63.2%) without epilepsy (WE). Overall mean score of SSE was 19.5 (SD 10.1; min. 2, max. 53). The mean SSE score for WE was 20.7 (SD 8.9; min. 2, max. 53) and for EPI 17.5 (SD 10.4; min. 3, max. 42); the difference was not statistically significant. For the overall sample, Cronbach's alpha was 0.854: for the EPI cohort 0.876 and for individuals WE 0.8237, that showed the Georgian version of SSE has good internal consistency. Kaiser–Meyer–Olkin Measure was 0.705 and the Bartlett's test of sphericity was 926.2 (df 276; p < 0.001) indicating acceptable sample adequacy.
Conclusion: The Georgian version of the SSE is a valid tool for population research on the components of epilepsy stigma.
eP‐EP‐A306
Similar frequency of depression in patients with temporal lobe epilepsy and different types of hippocampal sclerosis
T. F. Batelli1, J. C. Duarte1, M. S. B. Guaranha1, L. M. D. Guilhoto1, H. Carrete Junior1, R. D. S. Centeno1, E. M. Yacubian1, J. E. Peixoto‐Santos 1
1Unifesp, Neurology and Neurosurgery, São Paulo, Brazil
Question: Hippocampal sclerosis (HS) is the most frequent etiology of drug‐resistant temporal lobe epilepsy. Besides seizures, patients with TLE often present psychiatric comorbidities such as depression. While some studies have not shown a link between HS types and psychiatric comorbidities, those often have only a few cases with atypical HS types. We aimed to analyze if patients with type 1 HS have a higher frequency of depression than patients with HS types 2 and 3.
Methods: Patients with drug‐resistant TLE who underwent seizure control surgery were divided into three groups according to ILAE's HS classification in HS1 (n = 23); HS2 (n = 21), and HS3 (n = 9). Clinical data were obtained from medical records and included the clinical history and the psychiatric evaluation. For HS categorization we used NeuN and/or hematoxylin and eosin‐stained hippocampal sections. Data were tested for normality and homoscedasticity, and ANOVA with Bonferroni's post hoc, Kruskal–Wallis with Dunn's post hoc and Fisher's exact tests were applied.
Results: We saw no difference in clinical history between the patients with different HS types. Depression was diagnosed in 52% of the patients with HS1, in 29% of those with HS2, and in 11% of cases presenting with HS3. Fisher test revealed a trend towards a higher frequency of depression in HS1 when compared to the HS3 group.
Conclusions: We reinforced the findings that HS types do not differ in the frequency of depression.
eP‐EP‐A307
Data of misdiagnoses of transient conditions—Study in Georgia
K. Khomeriki 1, T. Jisjkariani2,3
1Clinic New Life, Neurology, Tbilisi, Georgia; 2Institute of Neurology and Neuropsychology, Neurology, Tbilisi, Georgia; 3Institute of Neurology and Neuropsychology, Tbilisi, Georgia
Introduction: Not all convulsive episodes are due to epilepsy. The three most important causes of a transient loss of consciousness (TLOC) are syncope, epilepsy and psychogenic blackouts. Failure to identify these patients delays the provision of adequate therapy while at the same time exposes the individual to the risk of injury or death.
Methods: During 6 month 250 patients were referred to clinic k. Eristavi National Center for experimental and Clinical Surgery Clinic New life in neurology department median age was 40 years and (range, 18–75 years) and 60% of them were women. All persons underwent an extensive multidisciplinary (CT/MRI; EEG, neurologic and epileptic) evaluations.
Results: One hundred and eighty of 250 were found not to have epilepsy. Psychogenic non‐epileptic seizures were found in—65 (36%); Cardiogenic syncope in—30 (16%); Neurogenic syncope in—85 (48%). Thirty patients of 180 (16%) were on antiepileptic drug treatment the median during 3 years.
eP‐EP‐A308
Activation of the Reelin/GSK‐3β/p‐Tau signaling pathway in the hippocampus of patients with temporal lobe epilepsy
Y. S. Piao 1, J. Lin1, Y. J. Fu1, S. Yu1
1Xuanwu Hospital, Pathology, Beijing, China
Question: Temporal lobe epilepsy (TLE) is the most prevalent form of chronic focal epilepsy. In this study, we assessed the expression and significance of proteins in the Reelin/GSK‐3β/p‐Tau signaling pathway in the hippocampus of TLE patients.
Methods: A total of 37 cases of TLE was collected from the Department of Pathology, Xuanwu Hospital, Capital Medical University. All cases had a primary clinical diagnosis of TLE with history of chronic, drug‐refractory disease, while five cases of hippocampal autopsies served as the control group. The 37 cases were divided into two groups according to the presence or absence of HS based on the histological findings. Immunohistochemical staining for Reelin, GSK‐3βand AT8 was performed on paraffin‐embedded sections. We also have selected 10 cases from both groups and 5 controls for the histelide assay with primary antibodies of AT‐8 and GSK‐3β.
Results: Immunohistochemical staining for hyperphosphorylated tau (AT8) revealed punctate and filamentous positive expression in the CA1, CA2 and CA3 regions of the hippocampus, with TLE under the ependyma, distributed in a band‐like pattern. By contrast, the control group did not exhibit any immunopositivity. GSK‐3β was strongly positive in the neuronal bodies, apical dendrites and axons in both groups of TLE, while all controls were negative. The histelide assay indicated that the amounts of AT8 and GSK‐3β were significantly increased in the two TLE groups (p < 0.05). Notably, there was a positive correlation between AT8 and GSK‐3β in TLE without HS (p = 0.038 < 0.05).
Conclusions: The present data indicates that phosphorylated tau protein and GSK‐3β are activated in the hippocampus of patients with TLE. We consider that the regulatory network of tau protein between the two groups may be similar but not identical.
eP‐EP‐A309
Prevalence of seizure disorders in patients with glial tumours—A study from Saudi Arabia
A. Alkhotani 1, A. Alkhotani1
1Umm Al‐Qura University, Pathology, Makkah, Saudi Arabia
Introduction: Glial tumours are a diverse group of primary central nervous system tumours arising from glial cells. They range from low grade tumours to aggressive types of Grade 4 glioblastoma. Their clinical presentations are variable according to site of lesion and the aggressiveness of the tumours.
Objectives: The aim of this study is to assess the prevalence of seizure disorders as an initial presentation of glial tumours in patients from Saudi Arabia.
Patients and Methods: We retrospectively reviewed patients with Glial tumours from the two largest hospitals in city of Makkah between 2016 and 2022.
Results: A total of 34 patients with glial tumours were identified. Fifteen patients out of 35 had a seizure as their initial presentation. With a prevalence of 44%. A total of 21 (61.8%) patients had frontal tumor, 6 (17.6%) had temporal tumor, 4 (11.8%) had parietal tumor, 3 other location. IDH1 was positive among 16 (47.1%) cases. 61.5% of patients with glial tumor aged less than 30 years had seizure disorder versus 9.1% of others aged more than 50 years with recorded statistical significance (p = 0.017). seizure was detected among 81.3% of patients with positive IDH1 compared to 11.1% of others with negative IDH1 (p = 0.001). Likewise, Seizure was detected among all cases with grade 2 tumor compared to 11.1% of others with grade 4 (p = 0.001).
Conclusion: Factors associated with seizure as an initial presentation of glioma are age less than 30, IDH1 mutatn and Grade 2 glioma.
eP‐EP‐A310
Valproate as antioxidant factor in Mexican children
E. Beltran Sarmiento 1,2, N. Cardenas Rodriguez3, E. Floriano Sanchez2
1Instituto Politecnico Nacional, Molecular Biology, Cuauhtémoc, Mexico; 2Escuela Militar de Graduados de Sanidad, Postgrade, Mexico City, Mexico; 3Instituto Nacional de Pediatria, Medicina Experimental, Mexico City, Mexico
Epilepsy is a global disease and the most common chronic neurologic disorder. Approximately 70 million people have epilepsy worldwide, and approximately 90% of them are in developing regions [1, 2]. Epilepsy is identified by the International League Against Epilepsy by the following features: (1) at least two unprovoked (or reflex) seizures occurring more than 24 h apart, (2) one unprovoked (or reflex) seizure and a probability of additional seizures similar to the general recurrence risk (60% or higher) after two unprovoked seizures occurring over the next 10 years, and (3) a diagnosis of an epilepsy syndrome [3]. In Mexico, approximately 1.5–2 million inhabitants suffer from epileptic crises, with an estimated incidence of just over 100 patients per 1,000,000 inhabitants [4, 5]. Central nervous system infections, family history, trauma, neuronal diseases, and malformations are the most common causes of epilepsy. The objective of this study was to evaluate, for the first time, the effects of VPA on the oxidant‐antioxidant status in Mexican epileptic children before and after 6 and 12 months of treatment with this AED by determining plasmatic antioxidant activities and oxidant marker profiles (GLUTHATIONE reductase), gluthatione peroxidase, superoxide dismutase, and catalase, activities and malondialdehyde, hydrogen peroxide, 8‐hidroxy‐2‐2deoxyguanosine and 3‐nitrotyrosine levels. Moreover, evaluated the possible relationships between antioxidant or antioxidant markers and some clinicophatological factors. the samples were collected from service of emergency, military hospital of specialties of the woman and neonatology, samples of peripheral blood in EDTA were obtained from 16 healthy children and 32 patients diagnosed with epilepsy and used for plasma isolation. Ethical approval was provided by the Bioethics in research Committee of the military Hospital of Specilities. Vpa shows significant antioxidant effects by decreasing MDA, H202. 8‐OhdG, and 3‐NT oxidant.
References: [1] xxxx. [2] xxxx. [3] xxxx. [4] xxxx. [5] xxxx.

FIGURE 1.

FIGURE 2.
OTHER FIELDS OF NEUROPATHOLOGY OR METHOD DEVELOPMENT
S27‐OT‐T2
The value of extracerebral biopsies in the diagnosis of neurometabolic diseases in children
G. Anderson 1
1Great Ormond Street Hospital for Children, Histopathology Department, London, United Kingdom
Diseases involving lysosomal, peroxisomal and mitochondrial dysfunction probably accounts for about 50% of all metabolic disorders. The remainder collectively known as small molecule diseases are predominantly those involving metabolic errors of amino acids, organic acids or the urea cycle and diseases of fatty oxidation. Lysosomal storage diseases include over 60 monogenic disorders with a combined frequency of approximately 1:7000 live births. Many of them express their enzyme defect in circulating cells and due to the highly specialised nature of these investigations, referral to a regional or national centre offering biochemistry and molecular genetics is advised. Where these investigations are insufficient, a morphological approach to screening for lysosomal storage disorders can help. We examine least invasive samples such as blood, hair, urine, skin biopsy and, when necessary, bone marrow aspirate. Using routine histochemical and immunological procedures with electron microscopic investigation can provide specific and rapid information leading to the diagnosis of a storage disorder or its exclusion. These procedures are available in many laboratories but their accurate interpretation require specialist knowledge and experience.
S29‐OT‐A311
Novel zebrafish model for studying neurodevelopment in Timothy syndrome
N. S. Banono 1, K. Gawel2, T. Mäki‐Marttunen3,4, W. van der Ent1, W. Kukula‐Koch5, M. Fyhn3,6, G. T. Einevoll6,7,8, O. A. Andreassen9,10, S. M. Waszak1,11,12, C. V. Esguerra1,13
1Centre for Molecular Medicine Norway (NCMM), University of Oslo and Oslo University Hospital, Oslo, Norway, Faculty of Medicine, Oslo, Norway; 2Medical University of Lublin, Department of Experimental and Clinical Pharmacology, Lublin, Poland; 3University of Oslo, Department of Biosciences, Oslo, Norway; 4Tampere University, Faculty of Medicine and Health Technology, Tampere, Finland; 5Medical University of Lublin, Department of Pharmacognosy, Lublin, Poland; 6University of Oslo, Centre for Integrative Neuroplasticity, Oslo, Norway; 7University of Oslo, Department of Physics, Oslo, Norway; 8Norwegian University of Life Sciences, Department of Physics, Ås, Norway; 9University of Oslo, Institute of Clinical Medicine, Oslo, Norway; 10Oslo University Hospital, NORMENT, Division of Mental Health and Addiction, Oslo, Norway; 11École Polytechnique Fédérale de Lausanne (EPFL), Swiss Institute for Experimental Cancer Research (ISREC), Lausanne, Switzerland; 12University of California, San Francisco, Department of Neurology, San Francisco, CA, United States; 13University of Oslo, Section for Pharmacology and Pharmaceutical Biosciences, Department of Pharmacy, Faculty of Mathematics and Natural Sciences, Oslo, Norway
Introduction: Timothy syndrome (TS) is a rare genetic disorder characterized by cardiac and neurological symptoms, including autism spectrum disorder and epilepsy, caused by germline variants in the CACNA1C gene. While the role of CACNA1C variants in neuronal function has been studied, the specific effects on neurodevelopment remain unclear. Animal models and human‐induced pluripotent stem cells can help investigate the mechanisms and develop treatments for TS. However, there are limited large animal models for TS and no zebrafish model of TS has been described.
Objectives: This study aimed to create a zebrafish model for studying neurodevelopment in TS and investigate the underlying mechanisms of TS‐related neurodevelopmental defects.
Materials and Methods: The cacna1c mutants were generated using ENU mutagenesis and confirmed through genotyping. We employed behavioural, electrophysiological, and biochemical approaches to identify molecular and cellular changes associated with cacna1c mutations in the zebrafish brain.
Results: We showed that the TS zebrafish model exhibited morphological abnormalities in the head and tail regions, a shorter body length, and cardiac abnormalities. Behavioural analysis revealed hyperactivity and increased seizure‐like behaviour. Brain recordings showed lower spectral power and significant seizure‐like activity in the TS zebrafish model. Gene expression and HPLC analyses revealed significant changes in the expression levels of genes and neurotransmitters essential for neuronal development and survival, synaptic plasticity, and cognitive function.
Conclusion: We provide a new in vivo model for studying the neurodevelopmental defects associated with TS, which may provide insights into the mechanisms underlying neuronal dysfunction in patients with TS.
S29‐OT‐A312
Normal development of cerebellar vermis in midgestation—A roadmap for pathological diagnosis
J. Ferrer‐Lozano 1, E. García‐Gómez1, J. Rubio‐Moll2, R. Llorens‐Salvador3
1Hospital Universitari i Politècnic La Fe, Department of Pathology, Valencia, Spain; 2Hospital Universitari i Politècnic La Fe, Department of Obstetrics and Gynecology, Valencia, Spain; 3Hospital Universitari i Politècnic La Fe, Department of Radiology, Valencia, Spain
Introduction and Objective: Histologic descriptions of the normal development of human cerebellar vermis (CVer) are scarce, which makes comparative analysis difficult in cases of suspected congenital defects. This work aims to build a detailed picture of the developing CVer in the second trimester of gestation.
Patients and Methods: Forty‐two fetuses between 12 and 24 gestational weeks (GW), submitted for pathological analysis after spontaneous termination of gestation, were studied. All cases had a clinical diagnosis of preterm labor and/or premature rupture of membranes. Routine prenatal genetic testing was available in seven cases, with no alterations found. No cases of intrauterine growth retardation were included. Any morphological congenital defect was discarded, both prenatally and after complete autopsy, with a final diagnosis of placental and/or membrane pathology rendered in every case. Prenatal ultrasonographic evaluations were recovered, and cerebellar and vermian measures (diameter, length, and height) compared with anatomic and histologic observations. Sagital sections of the CVer were scanned and their morphological appearance digitally analyzed. The proliferative activity in the vermian cortex was analyzed by Ki67 immunostain.
Results: The development of CVer followed a consistent, progressively complex pattern of foliation, which could be traced throughout the second trimester. The sequential appearance of fissures, position of rhombic lip, growth of the different cerebellar lobes and emergence of lobuli constituted a distinct image along every consecutive GW. The proliferative activity in the cerebellar cortex increased parallel to vermian development, especially in the external and internal granular layers.
Conclusions: Morphological features progressively acquired by the developing cerebellum allow a precise vision of its normal appearance during the second trimester of pregnancy, thus allowing a reliable identification of cases with a congenital defect.
S29‐OT‐A313
Somatic mosaicism of the PI3K‐AKT‐MTOR pathway causes hemimegalencephaly: Analyses of human fetal cases and animal models
K. Itoh 1,2, M. Tonosaki1, S. Fushiki1,2
1Kyoto Prefectural University of Medicine (KPUM), Pathology and Applied Neurobiology, Kyoto, Japan; 2Kyoto Chubu Medical Center, Diagnostic Pathology, Nantan, Japan
Introduction: It is known that somatic activation of PI3K‐AKT‐MTOR signaling causes malformations of cortical development varying from hemimegalencephaly to focal cortical dysplasia. However; there have been few reports of the fetal case and the underlying pathomechanisms remain unsolved.
Objectives: We report here two fetal cases of hemimegalencephaly with somatic mosaicism of activated PI3K‐AKT‐MTOR signaling and the experimental mice models were analyzed in order to get insight into the molecular mechanisms of brain malformation seen in human fetuses.
Patients and Methods: Two fetal cases of hemimegalencephaly, one associated with mosaic mutations in PIK3CA (c.1633G>A, p.(Glu545Lys)) and another in AKT1 (c.49G>A p.(Glu17Lys)) were analyzed. Next, we generated mouse model of somatic mosaicism using in utero electroporation of mutated AKT1E17K in fetal brains.
Results: Both fetal brains showed polymicrogyria, multiple subarachnoidal, subcortical and subventricular heterotopia, resulting from abnormal proliferation of neural stem/progenitor cells, cell differentiation and migration of neuroblasts. Scattered immature neurons immunoreactive for P‐RPS6 (Ser240/244) were observed in the polymicrogyria‐like cortical plate, intermediate zone and arachnoid space, suggesting that the PI3K‐AKT‐MTOR pathway was actually activated in these cells (Itoh et al., Neuropathology, 2022). The developing mouse brains after application of in utero electroporation of mutated AKT1 demonstrated abnormal migration and increased apoptosis, associated with aberrant expression of cortical layer‐specific transcription factors such as Ctip2 and Satb2 and enlarged cell size in the intermediate zone of fetal cortex.
Conclusion: We recapitulate human brain malformation in mice brain using in utero electroporation of mutated AKT1E17K. Further analyses could shed light on the mechanisms involved in disrupted brain development in the somatic mosaicism of the PI3K‐AKT‐MTOR pathway.
S29‐OT‐A314
Congenital stenosis of aqueduct of Sylvius secondary to mesencephalic vascular malformation—Autopsy case report in a fetus
M. T. Espinosa Romero 1, L. A. Téllez Manríquez1, W. R. Toscano‐Rengifo1, D. Villa Sepúlveda2, C. A. Durán López1, A. P. Chávez Hernández2, T. Rizo Pica2, L. G. Chávez Macías1, A. Escobar España1, E. Gómez Apo1
1Hospital General de México, Neuropathology, Mexico City, Mexico; 2Hospital General de México, Pathology, Mexico City, Mexico
Aqueduct of Sylvius is the most common site of cerebrospinal fluid flow obstruction. There is a wide spectrum of causes of obstruction of the aqueduct of Sylvius such as tumors, congenital malformations or infections; however, all show similar histological characteristics such as narrowing, retention and gliosis. To report the autopsy case of congenital stenosis of aqueduct of Sylvius secondary to mesencephalic vascular malformation. Fetus of 37.6 gestation weeks, product of the first pregnancy of a 22‐year‐old mother. The decision was made to terminate the pregnancy due to dysmorphic syndrome, polyhydramnios, and ventriculomegaly. The postmortem pathology service received the body of the female fetus, weighing 2910 kg, head‐heel length of 49 cm, cephalic perimeter of 34 cm, and foot length of 7.0 cm. The brain weighs 406 g (supratentorial 382 g and infratentorial 24 g). In consecutive coronal slices of the brain, dilated lateral ventricles are observed, the septum pellucidum is absent, the cerebellum is diminished in size, and the aqueduct of Silvio is narrow. In the histological sections of the midbrain, multiple aqueducts are observed, with partial occlusion of the Silvio aqueduct. In the rest of the sections of the midbrain, a conglomerate of tortuous vessels is observed, they have hybrid walls with an arterio‐venous appearance. Stenosis of aqueduct of Sylvius can be asymptomatic until it is diagnosed in adulthood, so its treatment is required when there is hydrocephalus that conditions some clinical manifestation. Obstruction due to vascular malformations is a rare cause of aqueductal stenosis, being more frequent due to venous angiomas. There are a few cases reported in the pediatric stage, only two of these cases were reported in newborns, like the present case.
Reference: [1] Paulson D, et al. Aqueductal developmental venous anomaly as an unusual cause of congenital hydrocephalus: a case report and review of the literature. J Med Case Rep. 2012;6(1):7.
S29‐OT‐A315
High‐dimensional characterisation of the cellular and molecular changes in the human brain after radiotherapy
T. Millner 1, P. Panday1, N. Pomella1, S. Bododi1, S. Marino1
1Queen Mary University of London, Blizard Institute, London, United Kingdom
Question: In the UK ~40,000 intrinsic and metastatic brain tumours are diagnosed each year. Although targeted radiotherapy (RT) is integral to increasing survival of cancer patients, it has significant side‐effects, the cellular and molecular mechanisms of which are not fully understood. During RT treatment epigenetic changes occur in the neoplastic tissue, but few studies have assessed these in non‐neoplastic brain tissue and results are highly variable.
Methods: To explore the effects of RT on patient‐specific methylation, we retrospectively identified 19 samples, mainly metastatic tumours, that had undergone stereotactic‐RT followed by resection, and contained peri‐lesional brain tissue, as well as 14 controls. Peri‐lesional brain was micro‐dissected, followed by DNA methylation profiling and RNA‐sequencing.
Results: Clustering of DNA methylation data showed distinct patterns between the two groups, while RNA‐seq revealed 1887 differentially expressed genes. Pathway analysis with GSEA identified differentially represented pathways, including: innate immune system, trans‐synaptic signalling, olfactory signalling, regulation of supramolecular fibre organisation, and pattern specification. Computational deconvolution of cellular composition showed increased activated dendritic cells and B‐cells, and reduced smooth muscle cells and several sub‐sets of astrocytes in the RT samples.
Conclusions: We are currently further investigating these findings using spatial transcriptomics and proteomics to produce the first high‐dimensional characterisation of the irradiated human brain. This will also provide the first direct evidence of epigenetic dysregulation after targeted‐RT, and assess novel epigenetically‐regulated genes, which will be validated with single cell tissue‐based imaging techniques. A range of epigenetic‐based drugs are undergoing clinical trials and we aim to identify targets for radiomitigation in brain tumour patients.
S29‐OT‐A316
Spinal cord is pathology is important in investigating abusive head trauma (AbHT) in children—A retrospective assessment of 40 cases
S. Al‐Sarraj 1, M. Colombari1, C. Troakes1
1King's College Hospital NHS Foundation Trust, Clinical Neuropathology, London, United Kingdom
Introduction: Abusive head trauma (AbHT) in children is a challenging diagnosis for which the current neuropathological diagnostic criteria (“the triad”) of ischaemic encephalopathy (IsE), subdural haematoma (SDH) and retinal haemorrhage (RH) has been argued to be insufficient. There is increasing evidence from the Neuroradiology of additional spinal cord injury in AbHT but this is so far, it has been poorly investigated neuropathologically.
Materials and Methods: We retrospectively reviewed 110 autopsy brain examination from children (62 males and 48 females, mean age 8 months) refereed for medico legal investigation over an 8‐year‐period. The review includes gross and histological examination of the brain and spinal cord alongside the circumstances of death and other pathological investigations.
Depending on the outcome of multidisciplinary forensic experts, 40 are diagnosed abusive head trauma (AbHT) and 9 accidental head trauma (AcHT). Eight cases were not clearly accidental or abusive (“undetermined” UHT) and 53 cases died from non‐traumatic brain injury (NTBI).
Results: The 40 AbHT cases (1 day to 3 years) show 100% mutlifocal and shallow cranial SDH 100%, IsE 100%, RH 93% and brain stem axonal injury 30%. The spinal cord shows SDH in 87%, subarachnoid haemorrhage (SAH) in 79% and spinal nerve roots axonal injury in 58% of the cases. The SDH/SAH at lumbar level was found to be significantly related to a diagnosis of abuse. When blood collection was detected at the cervical level it was consistently associated with blood collection at lower levels, suggesting a primary blood source in the spinal cord.
Conclusion: The results indicate that the spinal cord injury is common in AbHT that should be routinely examined together with the cervical spine and can be regarded as useful fourth criteria in addition to the triad in the diagnosis of abusive head trauma.
S29‐OT‐A317
Neuropathological findings in autopsy of a patient with MELAS‐like mitochondrial encephalopathy due to a new ATP8 mutation
J. Jiménez Almonacid 1, J. Ramírez Sánchez‐Ajofrín1, S. Moreno García1, C. Domínguez González1, A. Blázquez Encinar1, A. Hernández Lain1
1Hospital 12 de Octubre, Pathology, Madrid, Spain
Introduction: Mitochondrial diseases are a large and heterogeneous group of pathologies with systemic involvement especially in the central and peripheral nervous system. Among those that present with encephalopathy, Leigh's disease and MELAS (mitochondrial encephalomyopathy, lactic acidosis and stroke‐like episodes) stand out.
Objectives: We present the neuropathological findings of the autopsy of a 48‐year‐old patient with mitochondrial encephalopathy due to a new ATP8 mutation (m8424T>C) described in his family.
Materials and Methods: The subject is a 49‐year‐old male who died of status epilepticus preceded by sudden‐onset left hemianopsia. Previously, the patient had presented epileptic seizures since he was 42 years old and retinitis pigmentosa, showing ischemic lesions compatible with mitochondrial disease on magnetic resonance imaging. A genetic study detected a new mutation in the ATP8 gene. His mother died at the age of 69 due to status epilepticus, exhibiting cerebellar atrophy and structural alterations compatible with mitochondrial disease in the autopsy.
Results: Multiple foci of cortical laminar necrosis were observed more frequently in the parietal and occipital lobes that did not follow the distribution of a certain vascular territory in different evolutionary stages—acute, sub‐acute and chronic. Lesions with similar histological characteristics were observed in the basal ganglia. No alterations in the white matter were identified. Both hippocampi and amygdalae present significant atrophy and gliosis. Severe cortical atrophy and loss of Purkinje cells were observed in the cerebellum. The biopsy of the quadriceps muscle showed signs of denervation without blue ragged fibres with SDH and COX‐negative fibers.
Conclusions: The neuropathological findings in this case with MELAS‐like features broaden the spectrum of the clinical and morphological phenotype of mitochondrial diseases due to ATP8 gene mutations.
S15‐OT‐A318
Quantitative proteomics analysis of single brain organoids and patient‐derived neurospheres using TMT10plex isobaric tags
M. Junqueira 1
1Universidade Federal do Rio de Janeiro, Biochemistry, Rio de Janeiro, Brazil
Neurodegenerative and neuropsychiatric disorders involve changes in a range of molecular pathways. Advanced cell‐based models, such as brain organoids and patient‐derived neurospheres, provide new opportunities for understanding these disorders at the molecular level. However, analyzing the complex proteomic data generated from these models remains a challenge. Here, we present a quantitative proteomics approach using isobaric tags for relative and absolute quantification (iTRAQ) and tandem mass spectrometry (MS/MS) to analyze individual brain organoids and neurospheres from patients with various neuropathological conditions. Specifically, we used the TMT10plex isobaric tags to improve sensitivity, precision, and cost‐effectiveness. Our results demonstrate that the TMT10plex approach effectively quantified thousands of proteins across individual samples, and identified differentially expressed proteins and enriched biological pathways associated with neurodegeneration and neuropsychiatric disorders. This method was developed for single organoids and neurospheres, enabling a reduction in cost while increasing sensitivity and throughput. Additionally, miniaturization of the process improved the coverage of the proteome in each sample. The approach provides novel opportunities for studying the molecular underpinnings of these complex diseases using advanced cell‐based models.
PS10‐OT‐A320
Dual correlative light and electron microscopy (CLEM) of human autopsy specimens by gold enhancement of quantum dots
T. Uchihara 1,2,3, M. Uematsu2,4, K. Mikami2, A. Nakamura2, T. Yokota3, K. Hirokawa1
1Nitobe Memorial Nakano General Hospital, Tokyo, Japan; 2Tokyo Metropolitan Institute of Medical Science, Tokyo, Japan; 3Tokyo Medical and Dental University, Neurology and Neurological Science, Tokyo, Japan; 4Osaka Metropolitan University, Immunology and Genomics, Osaka, Japan
Cadmium selenide quantum dots (QDs) are fluorescent and electron‐dense nanoparticles that, when used as reporters for immunolabeling, allow direct comparison of fluorescent signals on light microscopy (LM) and ultrastructure on electron microscopy (EM) as correlated light and electron microscopy (CLEM). In this study, QD particles on the EM grid were enhanced with gold to increase the electron density of the particles. The rod‐shaped QD655 was gold enhanced at both ends of the particle, whereas the spherical QD565 was gold enhanced spherically, so that QDs with different original shapes could be more clearly distinguished on EM by the different gold enhancement patterns. This distinction by EM was also clear in tissue sections double immunolabeled with QD565 (green fluorescence) and QD655 (red fluorescence) as reporter pairs, and mutual comparison of LM and EM confirmed the specific labeling of each epitope. Target structures labeled with gold‐enhanced QDs were identifiable by brightfield microscopy due to their coloration, which facilitated trimming of the target structure on the final EM sections. Double labeling CLEM with gold‐enhanced QDs is a simple and feasible strategy that does not require special equipment. This method can be applied to formalin‐fixed human brain samples and paves the way to investigate how different molecules are woven into complex.
PS10‐OT‐A321
On the structure and microenvironment of cortical microvascular “raspberries” and their association with major neurocognitive disorders—A histopathological and immunohistochemical study
H. Ek Olofsson 1, M. Haglund1, E. Englund1
1Lund University, Division of Pathology, Department of Clinical Sciences Lund, Lund, Sweden
Introduction: A raspberry is a cerebral microvascular formation defined as >3 arteriolar lumen surrounded by a common space (Figure 1). Correlating the neocortical raspberry density to data retrieved from medical records and autopsy reports has demonstrated associations with vascular dementia (VaD) and cerebral atherosclerosis [1, 2].
Objectives: Unpublished data motivate further examination of potential associations between raspberries, frontotemporal lobar degeneration (FTLD) and Lewy body disease (LBD). In parallel, it is motivated to characterise the structure of raspberries and their surrounding microenvironment.
Materials and Methods: Our research is based on formalin‐fixed paraffin‐embedded brain tissue from clinical neuropathological autopsies. Cortical raspberry density is quantified manually on haematoxylin and eosin‐stained tissue sections. Immunohistochemical analyses are performed on selected sections. Primary antibodies are being evaluated: CD31, COL4, aSMA, CD68, GFAP, APP, IGG. All tissue sections are scanned and assessed digitally.
Results: Preliminary data indicate an increased raspberry density in FTLD similar to VaD. The raspberry density in LBD is indicated to be lower, corresponding to Alzheimer's disease. Immunohistochemical analyses are underway.
Conclusion: Results to date suggest associations between raspberries and ischaemia but further research is required to unveil the pathogenesis of this entity.
References: [1] Ek Olofsson H, Englund E. A cortical microvascular structure in vascular dementia, Alzheimer's disease, frontotemporal lobar degeneration and nondemented controls: a sign of angiogenesis due to brain ischaemia? Neuropathol Appl Neurobiol. 2019;45(6):557–69. [2] Ek Olofsson H, Haglund M, Englund E. On the regional distribution of cerebral microvascular raspberries and their association with cerebral atherosclerosis and acute circulatory failure. Cereb Circ Cognit Behav. 2023:100157.

FIGURE 1. A raspberry. Diameter: 45 μm.
PS10‐OT‐A322
A case of AL amyloidosis died from intracranial hemorrhage
Y. Ito 1, J. Suzuki1, N. Nakai1, M. Ueda2, H. Miyahara3, Y. Iwasaki3, M. Yoshida3
1TOYOTA Memorial Hospital, Neurology, Toyota, Japan; 2Kumamoto University, Neurology, Kumamoto, Japan; 3Medical Science of Aging, Aichi Medical University Hospital, Neuropathology, Nagakute, Japan
Background: A disease entity in which amyloid deposits in brain tissue and/or cerebral vessels is known as cerebral amyloidosis or cerebral amyloid angiopathy. Alzheimer's disease and cerebrovascular amyloid angiopathy (CAA) in which Aβ accumulates are representative, as well as transthyretin (ATTR) and cystatin C. On the other hand, there have been few reports of intracranial lesions of AL amyloidosis (ALA), in which amyloid deposits throughout the body.
Case: A 76‐year‐old male at the time of death, At the age of 50, he was introduced on dialysis with renal failure due to chronic glomerulonephritis. Multiple myeloma (MM) was diagnosed at the age of 76. One hour after the first bortezomib therapy for MM, he suddenly developed decreased consciousness, left conjugate deviation, and right hemiparalysis Cranial MRI revealed acute cerebral infarction in the left middle cerebral artery region and right cerebellar hemisphere. After alteplase administration and thrombectomy therapy, partial recanalization was observed, but there was little improvement in neurological symptoms. CT showed subarachnoid hemorrhage and right cerebellar hemorrhage the next day, and the patient died.
Pathological Findings: General pathological findings showed a plasma cell neoplasm in the bone marrow, and multiple nodules due to amyloid in the dialysis kidney, myocardium and lungs. Amyloid deposits were also observed in systemic blood vessels, and the common carotid artery was severely stenosed due to amyloid deposits. L chain (κtype) deposition was confirmed and systemic amyloidosis caused by ALA was diagnosed. There is no amyloid in the central nervous system, deposition is observed in sites lacking the blood–brain barrier, such as the choroid plexus and infundibulum, and deposition is also observed in the cortex and meningeal vessels. Discussion: Hematogenous dissemination was suggested as a mechanism of the AL amyloid deposition.
PS10‐OT‐A323
Chiari anomalies—What are they?
A. Hori 1,2
1Hannover Medical School, Neuropathology, Hannover, Germany
Currently Defined: Chiari anomaly type 1: Chronic herniation of the cerebellar tonsils (neocerebellum!) without increased intracranial pressure and may be accompanied by syringomyelia. Chiari anomaly type 2: Chronic herniation of the cerebellar vermis (paleo‐cerebellum!) with variable morphological manifestations: herniation of the lower brain stem, “peg” of the dorsal medulla oblongata, anterograde course of the cervical nerve roots, anterograde herniation of the dorsal cerebellar hemispheres, “reverse cerebellum” and so forth, and may be accompanied by spina bifida. Chiari anomaly type 3: Cerebellar herniation into the spina bifida cervicalis. Chiari anomaly type 4: Cerebellar aplasia/hypoplasia in cases of congenital hydrocephalus. This is no herniation of the cerebellum, therefore diagnosis of Chiari anomaly type 4 is not used anymore.
Consensus Today: Pathogenesis of Chiari anomalies (type 1 and 2) is a developmental space conflict between posterior fossa/craniovertebral junction and cerebellum/lower medulla oblongata during later fetal period.
Discussion: Cerebellar herniation is found in neo‐cerebellum in Chiari type 1 and in paleo‐cerebellum in Chiari type 2. If the posterior fossa is too small, paleo‐cerebellum should search for the space for the increasing volume during the developmental period in the second trimester and later (type 2). Because of shortness of the cervical canal, peg of the medulla oblongata and/or anterograde course of the cervical nerve roots may occur. On the other hand, if the posterior fossa is not severely hypoplastic, this will be pre‐occupied by the earlier developing paleo‐cerebellum, so that the later developing neocerebellum must seek for the space (type 1).
Conclusion: Chiari anomalies type 1 and type 2 are simply features of one disorder. (Is this a malformation or a deformation?) Chiari anomaly type 3 should be discussed in relation to Friede's “tectocerebellar dysraphia with occipital encephalocele.”
PS10‐OT‐A324
Tumefactive centrum semiovale and splenium demyelination in a case of suspected Perrault syndrome type 3
J. Klonoski 1, D. Sudarshan2, L. Robinson2, E. Goold2, C. Palmer2, C. Davidson2
1Incyte Diagnostics, Spokane Valley, WA, United States; 2University of Utah, Pathology, Salt Lake City, UT, United States
A 3‐year‐old girl with a history of prenatal intrauterine growth restriction, congenital hearing loss, bilateral cochlear implants, global development delay, lower limb spasticity, undetectable anti‐Mullerian hormone and chronic constipation was admitted for regression of milestones, neurological impairment and abdominal pain. MRI showed bilateral tumefactive white matter lesions in the frontal lobes and around the atria. Following optimization of her medications, pain and comfort, she was discharged. Eighteen days later she was readmitted for worsening discomfort and irritability. MRI showed increased size of the white matter lesions. Due to her functional decline, ineffective airway clearance and irregular breathing, she was transitioned to comfort care and passed at home. Autopsy showed bilateral white matter lesions extending from the frontal to the parietal lobes and an additional lesion in the splenium. Sections demonstrated myelin loss, preservation of axons and aggregates of macrophages within the white matter lesions. Whole genome sequencing demonstrated heterozygous mutations (maternal c.355A>T p.Ile119Phe and paternal c.484G>A p.Gly162Ser) in the Caseinolytic mitochondrial matrix Peptidase Proteolytic subunit (CLPP) gene. Perrault syndrome is a rare autosomal recessive disorder defined by the association of 46XX ovarian dysgenesis, neurosensory deafness in both sexes and mutations in one of at least six genes (CLPP, ERAL1, HARS2, HSD17B4, LARS2 or TWNK). Glycine to serine mutations at position 162 of CLPP are pathogenic and are known to disrupt the hydrophobic pocket responsible for ATPase interactions and proteolytic activity. Here we present, for the first time, that a missense mutation at position 119 is likely pathogenic in trans with an established pathogenic variant. Furthermore, our findings strengthen the literature of radiographic white matter abnormalities in Perrault syndrome type 3 by providing pathologic evidence of demyelination.

FIGURE 1.

FIGURE 2.
PS10‐OT‐A325
Spinal calcifying pseudoneoplasm of the neuraxis (CAPNON) associated with facet joint pathology
F. Fareez 1, J. Moodley2, C. Fong3, J. Provias1, S. Popovic1, A. Cenic4, J. Q. Lu1
1McMaster University, Pathology and Molecular Medicine, Hamilton, Canada; 2Massachusetts General Hospital, Harvard Medical School, Pathology, Boston, MA, United States; 3McMaster University, Radiology, Hamilton, Canada; 4McMaster University, Surgery/Neurosurgery, Hamilton, Canada
Introduction: Calcifying pseudoneoplasm of the neuraxis (CAPNON) is a rare tumor‐like fibro‐osseous lesion that can develop anywhere in the neuraxis. Approximately a half of all reported CAPNONs developed in the spinal region, mostly epidural and close to the facet joint. The pathogenesis of CAPNON remains elusive, although increasing evidence suggests a reactive proliferative process. A few case reports demonstrate CAPNONs in collision or association with other lesions such as tumors and inflammatory lesions. This study aims to explore the pathogenesis and diagnosis of spinal CAPNONs.
Methods: We examined 11 spinal CAPNONs (including a recurrent one) from 10 patients (ages: 51–81 years; eight females, and two males; three with an autoimmune connective tissue disease, and one with autoimmune hepatitis). The spinal lesions were surgically resected for symptomatic relief and pathologic examination.
Results: These cases showed foci of CAPNONs (11/11) as well as facet joint degenerative changes including calcified/calcifying synovial cysts (6/11 including 1 recurrent) and degenerated ligaments with calcification (11/11). CAPNONs exhibited diagnostic features including calcifying cores with peripheral palisading of macrophages including multinucleated giant cells, variable fibrous stroma, and positive immunostaining for Neurofilament light chain (NF‐L); they abutted calcifying/calcified foci of synovial tissue or degenerated ligaments, with limited to no peripheral palisading of cells. The complex foci contained focally abundant CD68+ macrophages and variable CD8+ T‐cells.
Conclusions: The findings of our present and previous studies [Lu et al., Pathology. 2022;54:573–9] suggest that spinal CAPNONs may occur in transition from or in association with calcifying degenerative lesions of facet joint ligaments and/or synovial cysts when a reactive proliferative process is complemented by other pathogenic changes such as immune‐mediated pathology and NF‐L expression.
PS10‐OT‐A326
A quality improvement project on the collection and process of cerebrospinal fluid (CSF) for cytology
A. K. L. Liu 1, L. van Hillegondsberg2, M. Zonda2, S. Cragg2, H. Keyser2, M. Hofer2
1University of Oxford, Nuffield Department of Clinical Neurosciences, Oxford, United Kingdom; 2Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Introduction: Despite advancement in neuroimaging and various diagnostic techniques, cytological analysis of cerebrospinal fluid (CSF) remains an integral part of a diagnostic workup. In 2019, the Royal College of Pathologists produced a set of Best Practice Recommendations (G177) that stated “cytological examination should only be performed on cases with a suspicion of malignancy or aseptic meningitis.” Appropriate collection, identification and delivery of CSF samples are also essential to ensure the accuracy and prompt reporting of results.
Objectives: We aim to ensure appropriate collection of CSF in order to minimise unnecessary workload burden to ward clinicians, technical staff and neuropathologists. We also aim to produce an updated set of local trust guidelines with the aim to inform and educate medical staff on appropriate collection of CSF for cytology.
Materials and Methods: We analysed CSF samples sent to neuropathology for cytological analysis from 2/7/21 to 1/7/22 and included samples taken with lumbar puncture (LP) on patients over the age of 18 (n = 222). We extracted information including volume of CSF samples collected, indications for cytological analysis and whether the samples were positive for malignancy or aseptic meningitis. We also reviewed the turnaround time for CSF sample.
Results: We found only 23% of all requests had correct indications (decrease from previous audit), but 97.3% had a turnaround time of <48 h on working days. CSF volume was appropriate (>0.5 mL) in 206/222 (93%) of samples and 22/222 (10%) sent volumes >10 mL.
Conclusions: We have updated our trust guideline to further advice clinicians and are in the process of producing a lanyard card and an update to the electronic system for CSF cytology requests. Completion of the audit cycle is planned for summer 2023.
S14‐OT‐A327
Conumee 2.0—Enhanced copy‐number variation analysis from DNA methylation arrays for humans and mice
B. Daenekas 1,2,3, E. Pérez2, D. Capper2,4, M. Zapatka5, V. Hovestadt1,3
1Dana‐Farber Cancer Institute, Pediatric Oncology, Boston, MA, United States; 2Charité—Universitätsmedizin Berlin, Department of Neuropathology, Berlin, Germany; 3Broad Institute of MIT and Harvard, Boston, MA, United States; 4German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Partner Site Berlin, Berlin, Germany; 5German Cancer Research Center (DKFZ), Division of Molecular Genetics, Heidelberg, Germany
Background and Objectives: In neuropathology, the detection of genomic copy‐number variations (CNVs) may influence clinical decision making. Due to the recent machine learning‐based patient classification system for brain tumors (the Heidelberg classifier), the generation of DNA methylation profiles is already integrated in routine workflows worldwide. We update our established R package “conumee” that allows to infer CNV profiles from methylation arrays. We aim to identify diagnostically relevant focal CNVs, increase the performance, implement new array types and add new plotting functionality.
Methods: Our approach combines tangent normalization, an adjustable genomic binning heuristic, and weighted circular binary segmentation to reduce technical biases and batch effects. High‐level alterations are detected de novo using a novel segmented block bootstrapping approach (Figure 1). The segmentation results are validated on the lung squamous carcinoma dataset from TCGA that comprises both DNA methylation array data and CNV segmentations derived from SNP arrays for 367 paired samples. The detection of high‐level alterations is assessed on TCGA low‐grade glioma dataset (n = 239).
Results: Conumee 2.0 achieved a significantly lower noise parameter compared to the old version (p < 0.001). On the gene‐level, highest correlation between segmentation results from both data types was observed for matching samples, achieving an average Pearson's correlation coefficient of r = 0.91 (r = 0.3 in non‐matching samples). For the detection of homozygous deletions affecting CDKN2A/B we achieved a sensitivity of 78.3% and a specificity of 87% (sensitivity: 90%; specificity 87.8% for RB1).
Conclusion: Our package conumee 2.0 enables enhanced CNV analysis from Illumina DNA methylation array data from human (including the EPICv2 array) and mouse samples. Diagnostically relevant high‐level alterations are frequently detected and may add an important layer of information in clinical settings.

FIGURE 1.
S14‐OT‐A328
Detection of structural DNA variations in pediatric brain tumors using optical genome mapping
N. Kubon 1, D. Picard2, C. Knobbe‐Thomsen1, D. Pauck1, J. Felsberg1, M. Remke2, G. Reifenberger1
1University Hospital Düsseldorf, Institute of Neuropathology, Duesseldorf, Germany; 2University Hospital Düsseldorf, Department of Pediatric Oncology, Hematology and Clinical Immunology, Duesseldorf, Germany
Medulloblastoma (MB) and atypical teratoid‐rhabdoid tumor (ATRT) are the most common malignant central nervous system tumors in children characterized by distinct patterns of genetic and epigenetic alterations. In addition to single nucleotide variations, large structural DNA variations (SVs) may contribute to cancer pathogenesis, in particular in tumors with relatively low mutational burden like medulloblastoma and ATRT. However, large‐scale profiling for SVs is challenging, as established methods such as karyotyping, fluorescence in situ hybridization and short‐read next‐generation sequencing are limited by low sensitivity or restriction to detection of pre‐defined SVs. To further assess the role of large structural DNA variations in malignant brain tumors from pediatric patients, we applied a novel technique for genome‐wide SV detection, namely optical genome mapping (OGM) using the Bionano Genomics Saphyr™ OGM instrument. This approach is based on the analysis of ultra‐high molecular weight DNA molecules and provides a high‐resolution genome‐wide profile highlighting DNA copy number and structural anomalies from 500 base pairs to one or more megabase pairs in length, including deletions, insertions, inversions, duplications and translocations. For classification and subtyping of the investigated tumors and tumor‐derived cell lines as well as for validation of the OGM findings, we performed 850 k DNA methylation and copy number profiling of all cases. Thereby, we found that OGM reliably detects previously known SVs in medulloblastoma and ATRT, as demonstrated by 850 k copy number profiling. In addition, OGM allowed to characterize novel recurrent SVs affecting cancer‐associated genes as well as non‐coding DNA regions. Thus, OGM represents a novel approach for large‐scale profiling and identification of SVs in pediatric brain tumors. Further validation of the OGM findings using PacBio HiFi long‐read sequencing and RNAseq of selected tumor cases is still ongoing.

eP‐OT‐A329
Migration disorder of the cerebral cortex caused by coactivation of LIN28A and CTNNB1 in neural precursor cells
J. Navolic 1, M. Middelkamp2, M. Moritz2, J. Hahn2, P. Sumislawski2, L. Ruck2, C. Krisp2, M. Dottermusch2, S. Godbole2, H. Schlüter2, J. E. Neumann2
1University Medical Center Hamburg‐Eppendorf, Center for Molecular Neurobiology Hamburg, Hamburg, Germany; 2University Medical Center Hamburg‐Eppendorf, Hamburg, Germany
LIN28A overexpression and mutations of the Wnt pathway gene CTNNB1 have been described in rare malignant brain tumors of early childhood. In order to investigate the interplay of the oncogenic proteins during embryonal brain development, we overexpressed these components in murine neural progenitor cells in vivo. The sole overexpression of either Lin28A, stabilized Ctnnb1 (Ctnnb1Δex3) or the combination of both in hGFAP‐positive forebrain precursor cells did not lead to brain tumor formation but resulted in distinct phenotypes in the cerebral cortex during embryonal development. In contrast to control mice and LIN28A expressing mice (GL) the cortical layering in hGFAP‐cre::Ctnnb1Δex3fl/+ (GB) and hGFAP‐cre::Ctnnb1Δex3fl/+::IsI‐Lin28A (GBL) mice was highly disturbed. Cell fate mapping of BrdU‐positive cells during development revealed impaired migration in the cerebral cortex of GB and GBL mice. GB mice displayed cerebral hypoplasia with a thinned cortex, while the GBL cortices showed variable thickness. Immunostainings with the pial marker LAMININ and dendritic marker MAP2C revealed a porous pia mater and aggregations of neurons above the pial border in the GBL model at embryonal day 14 (E14.5). At later embryonal stage (E18.5), the GBL model showed large blood vessels located in deeper cortical layers. Bulk and spatially resolved proteome analysis of the cortices in respective genotypes revealed distinct alterations of protein profiles associated with cerebral layers. These results indicate that the co‐expression of Lin28A and Ctnnb1Δex3 in neural precursor cells is not sufficient for tumor formation, but results in a neuronal migration disorder with ectopic neurons in the subarachnoid area. Whereas the GB phenotype is reminiscent of human lissencephaly type I, GBL brain morphology showed similarities to neuronal overmigration observed in the migration disorder of human Cobblestone (Type II) Lissencephaly.
eP‐OT‐A330
Protein malnutrition during gestation or early postnatal period is associated with reduced dendritic spine density and increased markers of synaptic pruning in Wistar rats
C. F. Romera‐Lopes1, S. R. Perosa1, J. P. Leite2, C. E. N. Girardi3, J. E. Peixoto‐Santos 1
1Unifesp, Neurology and Neurosurgery, São Paulo, Brazil; 2University of Sao Paulo, Neurosciences and Behavioral Sciences, Ribeirao Preto, Brazil; 3Unifesp, Psychobiology, São Paulo, Brazil
Question: The present study evaluated whether gestational/early postnatal protein malnutrition affects the expression of microglial synaptic pruning receptor CX3CR1 and dendritic spine density in rats.
Methods: Pregnant female adult Wistar rats were randomly assigned to three groups on gestation day 0: short prenatal malnutrition (Pre, females kept in protein restriction from G0 to postnatal day 1—PND1); short postnatal malnutrition (Pos, females kept in restricted diet between PND1 and PND21); and controls (Ctrl, female kept in standard diet). For protein restriction, pregnant females were fed ad libitum with a low‐protein isocaloric diet (5% protein) while those without restriction received a 20% protein diet. Male offspring from the restricted and control females were euthanized at PND21, and brains were extracted, formalin‐fixed, and paraffin‐embedded. Sections from the dorsal hippocampus and prelimbic cortex were immunostained for CX3CR1 expression or submitted to immunofluorescence for the dendritic protein drebrin, and sections were evaluated for microglial CX3CR1 immunopositive area or dendritic spine density, respectively.
Results: Protein restriction reduced offspring body weight, with both groups presenting lower weight than controls, and Pos presenting lower weight than Pre. Visual inspection did not reveal morphologic differences in brain structure but restricted animals had lower brain volume than controls. Only the hippocampal fascia dentata had differences between the groups, with increased CX3CR1 expression in microglia and decreased dendritic spine density in Pre and Pos compared to control, without differences between the groups under protein restriction.
Conclusions: Overall, our results indicate that PM reduces offspring dendritic spine density, and one factor related to this reduction can be increased synaptic pruning.
eP‐OT‐A331
An autopsy report of a patient with simultaneous multiple hypertensive intracerebral hematomas (SMHICHs) in the left putamen and thalamus 11 years after the right putaminal hemorrhage
S. Takeda 1, T. Miyakawa2, H. Takahashi3, K. Yamazaki2, K. Onda2
1Niigata Neurosurgical Hospital, Department of Pathology, Niigata, Japan; 2Niigata Neurosurgical Hospital, Neurosurgery, Niigata, Japan; 3Niigata Neurosurgical Hospital, Laboratory Medicine, Niigata, Japan
SMHJCHs associated with central gray matter are rare. Most of them have been reported as clinical examples. A 54‐year‐old Japanese woman, who had a past history of a right putaminal hemorrhage with ventricular rupture at the age of 43, developed a left putaminal hemorrhage, showing a bizarre spread on CT and accompanied ventricular rupture. She died the next day. The brain (1360g) was examined routinely and several sections were applied for synaptophysin andα‐smooth muscle actin immunohistochemistry. The right putaminal hematoma (PH) changed into a cystic lesion with iron‐positive granules, extending from the lateral region of the putamen to the dorsal region of the caudate nucleus, and being continuous to the lateral ventricle. In the left cerebral hemisphere, two fresh hematomas, that is, PH and thalamic hematoma (TH) were found. The PH destroyed most of the putamen, crossed the internal capsule and caudate nucleus in a tongue‐like manner, and ruptured into the left lateral ventricle. Such an extension pattern of the PH toward the midline of the brain differed from that of the usual PH. The globus pallidus was relatively preserved. The TH destroyed the dorsal and medial structures of the thalamus, and ruptured into the left lateral and third ventricles. A large amount of thalamic tissue debris was found in the hematoma within the ventricles. The TH also extended to the pons, although the ventral region of the thalamus was relatively preserved. Microvacuolar changes were found with similar appearance frequency in the brain tissues around the PH and TH. No aneurysms, AVMs, or angiomas were found. Present case shows that (1) when SMHICHs occur in the ipsilateral putamen and thalamus, the extension pattern may differ from those of usual HICHs, especially hypertensive PHs, and that (2) SMHICHs occurring in the ipsilateral putamen and thalamus differ in form from the hematomas seen in so‐called hypertensive mixed‐type hemorrhage.
eP‐OT‐A332
Age‐related increase in white matter vascular bagging independently from Alzheimer‐related pathology
D. Yilmazer‐Hanke 1, K. S. Georgieva1
1Ulm University, Clinical Neuroanatomy, Neurology, Ulm, Germany
Introduction: Aging is associated with basement membrane splitting and duplication in the smallest cerebral vessels. In our studies, we could show for the first time that the duplicated basement membranes of white matter cerebral microvessels develop bags filled with plasma proteins in the human brain, indicating endothelial damage and consecutive blood–brain barrier (BBB) disruption. A second indicator of endothelial damage in cerebral microvessels is enhanced string vessel formation.
Objectives: The objectives are to analyze vascular bagging with BBB disruption and string vessel formation in aging and AD.
Materials and Methods: Autopsy tissue from a non‐selected aged autopsy cohort and from age‐matched cohort with different stages of AD‐related pathology were compared. A mid‐hemispheric formalin‐fixed tissue block was embedded in polyethylene glycol and 100 m‐thick hemisphere sections were obtained. Vascular bags and string vessels were studied using double‐label immunohistochemistry for the simultaneous visualization of collagen IV‐positive membranes and endothelial cell layer with UEA‐l lectin. Findings were correlated with markers of neuroinflammation such as microglial markers.
Results: Quantitative analyses of vascular bagging in the frontoparietal white matter indicated a statistically significant correlation between age and the degree of vascular bagging and string vessel formation associated with the emergence of CD68‐positive macrophages. In contrast, vascular bagging was not increased in the white matter of randomly selected cases with a pathologically confirmed diagnosis of AD.
Conclusion: The risk for developing vascular bagging and string vessels in the cerebral white matter increases with age. However, our data suggest that vascular bagging is an age‐related vascular pathology in the human brain that develops independently from AD pathology.
eP‐OT‐A333
Establishment of Brain Bank for Neurodevelopmental, Neurological and Psychiatric Disorders (BBNNPD), Osaka in collaboration with Brain Bank for Aging Research (BBAR), Tokyo, Japan
S. Murayama 1,2,3, Y. Saito3, G. Beck1,2, K. Inoue4, M. Yamadera4, M. Taniike1, H. Matsumoto5, E. Morii6, H. Mochizuki1,2
1Osaka University, Division of Brain Bank and Bioresource, Molecular Research Center for Child Development, Postgraduate School of Child Development, Osaka, Japan; 2Osaka University, Department of Neurology, Postgraduate School of Medicine, Osaka, Japan; 3Tokyo Metropolitan Institute for Geriatric and Gerontology, Department of Neuropathology (Brain Bank for Aging Research), Tokyo, Japan; 4Osaka Toneyama Medical Center, National Hospital Organization, Osaka, Japan; 5Osaka University, Department of Legal Medicine, Postgraduate School of Medicine, Osaka, Japan; 6Osaka University, Department of Pathology, Postgraduate School of Medicine, Osaka, Japan
Introduction: We established BBAR in 1999, based on (1) brain and body donation; (2) quality control of resource with pathological consensus; and (3) open resource. BBAR guided to build up the national brain bank network with the Brain Bank Committee, the Japanese Society of Neuropathology (JSNP).
Objectives: BBAR could not accumulate resource of neurodevelopmental disorders including autism and mood disorders. We newly established BBNNPD in 2020 and received funding of Japanese Brain Net by Japan Agency for Medical Research and Development (AMED, PI: Professor Masaki Takao), whose aim is to recover postmortem brains of psychiatric disorders, in collaboration with Osaka University (OU) and National Hospital Organization (NHO). The aim of BBNNPD is to establish brain and body donation system in Osaka and try to build up the registry for Japanese equivalent of suicide bank, sudden death bank and autism brain net.
Materials and Methods: We recruited brain and body donors in Kansai area. The autopsy was done on site or transferred to OU Department of Pathology or NHO Osaka Toneyama Medical Center (OTMC). Neuropathological diagnosis was quality controlled by every week internet conference connected with OU Department of Neurology, OTMC and BBAR. In addition, in order to recruit young brain bank doctors, we started JSNP board certification of neuropathologists in 2020.
Results: We succeeded in establishing OU division of brain bank in 2020 and began to fulfill the donors’ will. Although our effort was seriously affected by dramatic decrease of autopsy numbers by COVID19 pandemic, we could accumulate resource of at least 15 cases a year and publish original research papers continuously. About registry of legal autopsy, we still experienced difficulty in IRB approval. This year we welcomed a board‐certified neuropathologist to BBNNPD and two to BBAR after the first qualified examination.
Conclusion: We are building up the Japanese Brain Bank Network and succeeded in establishing the Kansai Base. We are still in the middle of our effort.
Acknowledgement: This work was supported by AMED under Grant Number JP21wm0425019.


