Key Points
Question
Do trajectories of exposure to neighborhood social environments before and after first diagnosis of a serious mental illness (SMI) differ between case patients and matched control participants?
Findings
This nested case-control study of 26 729 case patients diagnosed with SMI and 26 729 birth year– and sex-matched control participants found gradients between living in more deprived neighborhoods during upbringing and subsequent risk of SMI; in contrast, risk was ameliorated in those who experienced early-life upward mobility. After diagnosis, few case patients moved into more deprived areas but remained disproportionately exposed to higher levels of deprivation.
Meaning
In this study, associations among deprivation, population density, and psychotic disorder were partially explained by social variables but were exacerbated after diagnosis by social immobility; social drift did not play a strong role.
This case-control study examines whether patients diagnosed with psychotic disorder or nonpsychotic bipolar disorder differed from a control group in their deprivation and population density trajectories.
Abstract
Importance
People with psychosis are more likely to be born and live in densely populated and socioeconomically deprived environments, but it is unclear whether these associations are a cause or consequence of disorder.
Objective
To investigate whether trajectories of exposure to deprivation and population density before and after diagnosis are associated with psychotic disorders or nonpsychotic bipolar disorder.
Design, Setting, and Participants
This nested case-control study included all individuals born in Sweden between January 1, 1982, and December 31, 2001, diagnosed for the first time with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) psychotic disorder or nonpsychotic bipolar disorder between their 15th birthday and cohort exit (December 31, 2016). One sex- and birth year–matched control participant per case was selected. Data analysis was performed from July 2021 to June 2023.
Exposures
The main exposures were quintiles of neighborhood-level deprivation and population density each year from birth to age 14 years and from first diagnosis until cohort exit.
Main Outcomes and Measures
The main outcomes were the odds of a serious mental illness outcome associated with trajectories of deprivation and population density, before and after diagnosis in cases. Group-based trajectory modeling was used to derive trajectories of each exposure in each period. Logistic regression was used to examine associations with outcomes.
Results
A total of 53 458 individuals (median [IQR] age at diagnosis in case patients, 23.2 [15.0-34.8] years; 30 746 [57.5%] female), including 26 729 case patients and 26 729 control participants, were studied. From birth to early adolescence, gradients were observed in exposure to deprivation and population density trajectories during upbringing and psychotic disorder, with those in the most vs least deprived (adjusted odds ratio [AOR], 1.17; 95% CI, 1.08-1.28) and most vs least densely populated (AOR, 1.49; 95% CI, 1.34-1.66) trajectories at greatest risk. A strong upward mobility trajectory to less deprived neighborhoods was associated with similar risk to living in the least deprived trajectory (AOR, 1.01; 95% CI, 0.91-1.12). Only 543 case patients (2.0%) drifted into more deprived areas after diagnosis; people with psychotic disorder were more likely to belong to this trajectory (AOR, 1.38; 95% CI, 1.16-1.65) or remain in the most deprived trajectory (AOR, 1.36; 95% CI, 1.24-1.48) relative to controls. Patterns were similar for nonpsychotic bipolar disorder and deprivation but weaker for population density.
Conclusions and Relevance
In this case-control study, greater exposure to deprivation during upbringing was associated with increased risk of serious mental illness, but upward mobility mitigated this association. People with serious mental illness disproportionately remained living in more deprived areas after diagnosis, highlighting issues of social immobility. Prevention and treatment should be proportionately located in deprived areas according to need.
Introduction
Elevated rates of serious mental illnesses (SMI), primarily nonaffective psychotic disorders, have been consistently observed in more socially deprived and densely populated areas.1,2,3,4,5,6,7,8,9,10,11 The direction of this association remains unclear. Social causation theory posits that exposure to socioenvironmental stressors cause increased psychosis risk.12,13,14,15 Conversely, noncausal selection-drift theories propose that downward social mobility explains the association between social adversity and SMI.8,16 These theories include social drift theory, which posits that psychosis negatively affects one’s ability to sustain living standards, resulting in intragenerational drift into more deprived areas; and social selection theory, which proposes that individuals with genetic predisposition to psychosis are selected into such environments before psychosis onset because of intergenerational transmission of genetic liability to psychosis,16,17,18,19,20 which may be an upstream common cause of other functional processes related to both exposure and outcome, such as cognition.21 Cognitive impairment is more strongly associated with psychotic disorders than other SMIs, such as bipolar disorder, which may explain the specificity of association between neighborhood social environments and nonaffective psychoses.20,22,23
Both selection and drift occur by active movement into more adverse neighborhoods or lower socioeconomic positions. A related third process may also exist: Individuals with psychosis may remain in the same neighborhood or socioeconomic position but experience social immobility relative to their unaffected peers, who are more likely to experience upward mobility by both place and status.
These explanations are not mutually exclusive. Longitudinal evidence of a dose-response association between urbanicity at birth and upbringing with future risk of psychotic disorders excludes intragenerational drift as the sole underlying mechanism.24,25 Some studies,20,22 though not all,26,27 have reported modest levels of social drift after psychosis onset, although whether this is due to social drift or relative social immobility among people with SMI remains unclear. Recently, genetically informed studies have sought to untangle potential social causation from intergenerational selection hypotheses. Genetic susceptibility to schizophrenia, measured by polygenic risk scores or shared familial influences, is associated with subsequent residence in more deprived areas before onset, irrespective of socioeconomic status at birth.28,29 However, a social causation interpretation remains possible via mediated pleiotropy,30 and not all studies have observed that polygenic risk scores for schizophrenia are associated with urban birth.31 Furthermore, urban birth and upbringing remain associated with later psychosis, despite adjustment for genetic risk.31,32,33,34 No study to date has investigated the specificity of longitudinal associations between neighborhood social environments and various SMI outcomes during upbringing and after first diagnosis; such an analysis would shed further light on social causation vs selection-drift-immobility hypotheses. The current study used national population–based register data from Sweden to investigate these issues. Our aims were to (1) identify and describe latent trajectories of neighborhood-level deprivation and population density from birth until age 14 years and from year of SMI diagnosis in cases and matched controls until the end of follow-up and (2) explore whether people diagnosed with a psychotic disorder or nonpsychotic bipolar disorder and controls differed in their deprivation and population density trajectories.
We hypothesized under the social causation theory that individuals diagnosed with a psychotic disorder would be more likely to have lived in more deprived and densely populated areas before diagnosis compared with controls. We also hypothesized under the selection-drift-immobility theory that, after diagnosis, individuals with psychotic disorders would be more likely than controls to follow a downward trajectory to more deprived and densely populated areas. Finally, we hypothesized that these patterns would be weaker for nonpsychotic bipolar disorders, given previous evidence.23,35
Methods
Study Design
Using a nested case-control design, we matched cases and controls by birth year and sex, ensuring that trajectories of neighborhood change occurred during similar ages and periods. We first identified a cohort of individuals born in Sweden between January 1, 1982, and December 31, 2001, through Psychiatry Sweden, a register linkage of national longitudinal registries of routine data, linked via a civic registration number assigned to all Swedish residents at birth. Data on small area marketing statistics (SAMS) neighborhoods were available from 1982 onward. We followed up the cohort from birth until censorship due to an SMI diagnosis, death, emigration, or the study end date (December 31, 2016), whichever came first. All individuals who died, emigrated, or were diagnosed with SMI before age 15 years were excluded. This study was approved by the Stockholm Regional Ethical Review Board and the University College London Research Ethics Committee, and informed consent was waived as per Sweden’s legal framework for their welfare state, which allows national register data to be used for research purposes under strict data protection laws. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
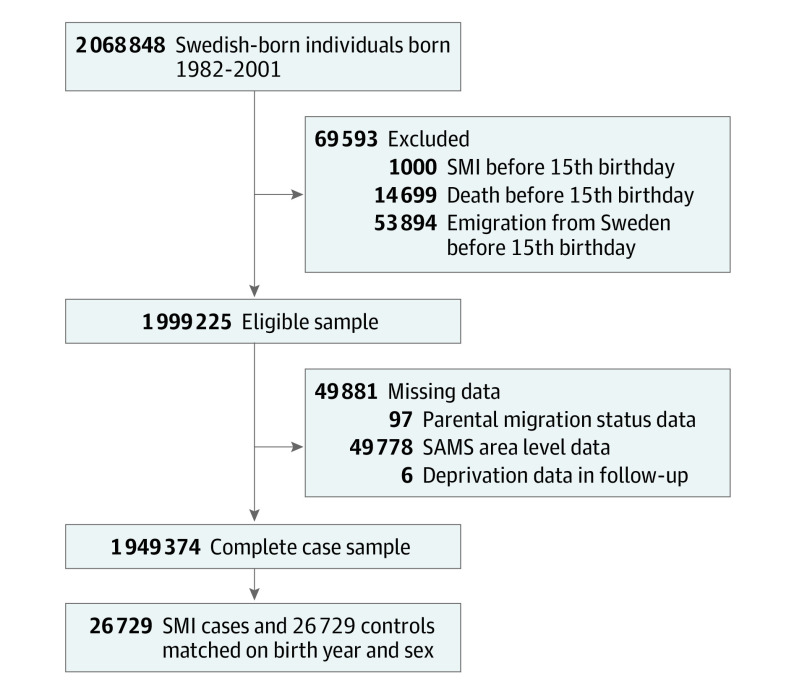
Selection of Cases and Controls
Within the base cohort, we excluded 49 784 individuals (2.5%) missing data on neighborhood of residence and 97 individuals (<0.1%) missing covariate data (Figure 1). We then identified all cases with a first SMI diagnosis after 15 years of age (earliest, January 1, 1997) recorded in the national patient register. The SMI diagnoses were defined using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and categorized into 2 groups: psychotic disorders (schizophrenia [ICD-10 code F20], nonaffective psychoses [ICD-10 codes F21-29], or affective psychotic disorders [ICD-10 codes F30.2, F31.2, F31.5, F32.3, and F33.3]) and nonpsychotic bipolar disorder (ICD-10 codes F30.x and F31.x, excluding F30.2, F31.2, F31.5). People who received both diagnoses were categorized in the psychotic disorder group, consistent with previous research.36 For each case, we randomly selected 1 sex- and birth year–matched control without an SMI diagnosis.
Figure 1. Flow of Participants Through the Study.
SAMS indicates small area marketing statistics; SMI, serious mental illness.
Exposures and Covariates
For each year of observation, we estimated area-level socioeconomic deprivation and population density using the SAMS register.29,37,38,39 Sweden is divided into 9209 SAMS neighborhoods for administrative purposes. The register holds annual information on area-level characteristics of each SAMS neighborhood. These are classified to be maximally socioeconomically homogeneous, but their deprivation and population density levels vary.29 Socioeconomic deprivation was derived from measures of income, social benefits, unemployment, and crime (eMethods in Supplement 1). These were z-standardized and summed to calculate a deprivation index (higher scores specifying greater deprivation).21,40 Population density was calculated as people per square kilometer in each SAMS neighborhood. For each year, we calculated quintiles of deprivation and population density. Individuals were linked to their SAMS area and respective quintile values for each year of observation. We included the following confounders: biological parental history of SMI, parental migrant status, parental disposable income quintile at birth, number of residential moves from birth until age 14 years, and number of residential moves from index year until end of follow-up for postdiagnosis analyses (eMethods in Supplement 1).
Statistical Analysis
Data analysis was performed from July 2021 to June 2023. First, we conducted group-based trajectory modeling to identify latent groups that followed similar trajectories of deprivation and population density exposure over time (see the eMethods in Supplement 1 for full details).41 Group-based trajectory modeling was conducted separately for each exposure for 2 different periods: prediagnosis (from birth year until 14th year of follow-up) and postdiagnosis (from index diagnosis year in cases until end of follow-up). For each model, we established the optimal number of trajectory groups and their shape, considering Bayesian Information Criterion values and other statistics.41,42,43 Each individual was then classified into a group according to the maximum posterior probability assignment rule.
Second, to determine the association between trajectory group membership and each SMI outcome, we conducted logistic regressions for the prediagnosis and postdiagnosis periods, separately. We fitted univariable models for each exposure-outcome association, bivariable analyses (mutually adjusted for population density and deprivation trajectories), and multivariable models adjusted for all covariates. Reference categories for each exposure were the least deprived and least densely populated trajectory groups. We reported adjusted odds ratios (AORs) with 95% CIs.
As post hoc analyses, we conducted reparameterized logistic regression models with the upward mobility and urban-rural movement trajectories as the reference categories to investigate the presence of relative social immobility for people with SMI (ie, remaining in more deprived or urban environments relative to their unaffected peers). Given minimal missing data (2.5%), we conducted complete-case analyses44 and compared the characteristics of those with and without complete data. All modeling was conducted in Stata, version 17 (StataCorp); group-based trajectory modeling was estimated using the traj user-written Stata package.45
Results
Sample Characteristics
From the complete sample of 1 949 374 individuals (97.5% of the cohort), 53 458 individuals (median [IQR] age at diagnosis in case patients, 23.2 [15.0-34.8] years; 30 746 [57.5%] female and 22 712 [42.5%] male), including 26 729 case patients (12 947 [48.4%] with psychotic disorders and 13 782 [51.6%] with nonpsychotic bipolar disorder) and 26 729 control participants, were studied (Figure 1 and Table 1; eTable 1 and the eResults in Supplement 1). Case patients with psychotic disorders were more likely to be male, to be second-generation immigrants, to be born in the most deprived and densely populated quintiles, and to have moved 5 or more times after index diagnosis year compared with cases with nonpsychotic bipolar disorder and controls (Table 1). All case patients were more likely to have a parental history of SMI and to have moved between birth and 14 years of age, consistent with previous findings.39 The median length of postdiagnosis follow-up was 5 (IQR, 2-7) years in both cases and controls.
Table 1. Sample Characteristics by Case Status.
| Characteristic | Controls, No. (%) (n = 26 729 [50.0%]) | Cases, No. (%) (n = 26 729 [50.0%]) | χ2 | df | P value | |
|---|---|---|---|---|---|---|
| Psychotic disorder (n = 12 947 [48.4%]) | Nonpsychotic bipolar disorder (n = 13 782 [51.6%]) | |||||
| Sex | ||||||
| Male | 11 356 (42.5) | 7417 (57.3) | 3939 (28.6) | 2251.4 | 1 | <.001 |
| Female | 15 373 (57.5) | 5530 (42.7) | 9843 (71.4) | |||
| Parental migrant status | ||||||
| Swedish born | 22 324 (83.5) | 9724 (75.1) | 11 241 (81.6) | 405.0 | 2 | <.001 |
| Migrant | 4405 (16.5) | 3223 (24.9) | 2541 (18.4) | |||
| Other Europe | 1894 (7.1) | 1313 (10.1) | 1308 (9.5) | |||
| Asia | 134 (0.5) | 68 (0.5) | 22 (0.2) | |||
| North Africa and Middle East | 628 (2.4) | 375 (2.9) | 115 (0.8) | |||
| Sub-Saharan Africa | 93 (0.4) | 130 (1.0) | 12 (0.1) | |||
| Mixed | 1570 (5.9) | 1279 (9.9) | 1043 (7.6) | |||
| Othera | 8.6 (0.3) | 58 (0.5) | 41 (0.3) | |||
| Parental history of SMI | ||||||
| 0 | 25 827 (96.6) | 11 418 (88.2) | 11 952 (86.7) | 1559.9 | 2 | <.001 |
| 1 | 787 (2.9) | 1312 (10.1) | 1573 (11.4) | |||
| 2 | 115 (0.4) | 217 (1.7) | 257 (1.9) | |||
| Parental disposable income at birth | ||||||
| 1 (Lowest quintile) | 4814 (18.0) | 3137 (24.2) | 2967 (21.5) | 286.4 | 8 | <.001 |
| 2 | 5469 (20.5) | 2730 (21.2) | 3013 (21.9) | |||
| 3 | 5534 (20.7) | 2370 (18.3) | 2818 (20.5) | |||
| 4 | 5554 (20.8) | 2423 (18.7) | 2477 (18.0) | |||
| 5 (Highest quintile) | 5358 (20.1) | 2287 (17.7) | 2507 (18.2) | |||
| Deprivation at birth | ||||||
| 1 (Lowest quintile) | 4464 (16.7) | 1894 (14.6) | 2016 (14.6) | 239.2 | 8 | <.001 |
| 2 | 5362 (20.1) | 2291 (17.7) | 2536 (18.4) | |||
| 3 | 5708 (21.4) | 2546 (19.7) | 2813 (20.4) | |||
| 4 | 5581 (20.9) | 2696 (20.8) | 2997 (21.8) | |||
| 5 (Highest quintile) | 5614 (21.0) | 3520 (27.2) | 3420 (24.8) | |||
| Population density at birth | ||||||
| 1 (Lowest quintile) | 2703 (10.1) | 1025 (7.9) | 1357 (9.9) | 311.6 | 8 | <.001 |
| 2 | 3719 (13.9) | 1462 (11.3) | 1806 (13.1) | |||
| 3 | 4940 (18.5) | 2120 (16.4) | 2295 (16.7) | |||
| 4 | 7114 (26.6) | 3259 (25.2) | 3584 (26.0) | |||
| 5 (Highest quintile) | 8253 (30.9) | 5081 (39.2) | 4740 (34.4) | |||
| Moves between birth year and 14th year of follow-up | ||||||
| 0 | 11 761 (44.0) | 4435 (33.6) | 4502 (32.7) | 842.8 | 4 | <.001 |
| 1-4 | 14 141 (52.9) | 7825 (60.4) | 8387 (60.9) | |||
| ≥5 | 827 (3.1) | 777 (6.0) | 893 (6.5) | |||
| Moves between diagnosis year and end of follow-up | ||||||
| 0 | 12 889 (48.2) | 6441 (49.8) | 6530 (47.4) | 39.1 | 4 | <.001 |
| 1-4 | 13 125 (49.1) | 6067 (46.9) | 6879 (49.9) | |||
| ≥5 | 715 (2.7) | 439 (3.4) | 373 (2.7) | |||
| Diagnosis (ICD-10 code) | ||||||
| Schizophrenia (F20) or schizoaffective disorders (F25) | NA | 2942 (22.7) | NA | NA | NA | NA |
| Affective psychosis (F30-33) | NA | 3369 (26.0) | NA | |||
| Bipolar psychosis (F30-31) | NA | 1153 (8.9) | NA | |||
| Depressive psychosis (F32-33) | NA | 2216 (17.1) | NA | |||
| Other nonaffective psychosis (F2X) | NA | 6636 (51.3) | NA | |||
| Bipolar or mania without psychosis | NA | NA | 13 782 (100) | |||
Abbreviations: ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; NA, not applicable; SMI, severe mental illness.
Other includes any other part of the world not included in the aforementioned areas, such as Australasia and the Americas.
Trajectory Identification
Model fit statistics (eTables 2 and 3 in Supplement 1) indicated that we obtained trajectory models with good model fit. The trajectories for each exposure and period are described below.
Prediagnosis Period
For deprivation, a 6-group model provided optimal fit to the data. Four trajectories indicated temporally stable levels of exposure to deprivation (from low to high; trajectories 1, 2, 3, and 4) between birth and 14 years of age, accounting for 80.7% of the sample (Figure 2A). Trajectories 5 (8.0%) and 6 (11.2%) depicted groups that moved from more to less deprived areas, which we termed strong upward mobility and moderate upward mobility, respectively.
Figure 2. Group-Based Trajectory Modeling (GBTM) Trajectories for Each Neighborhood-Level Exposure and Each Time.
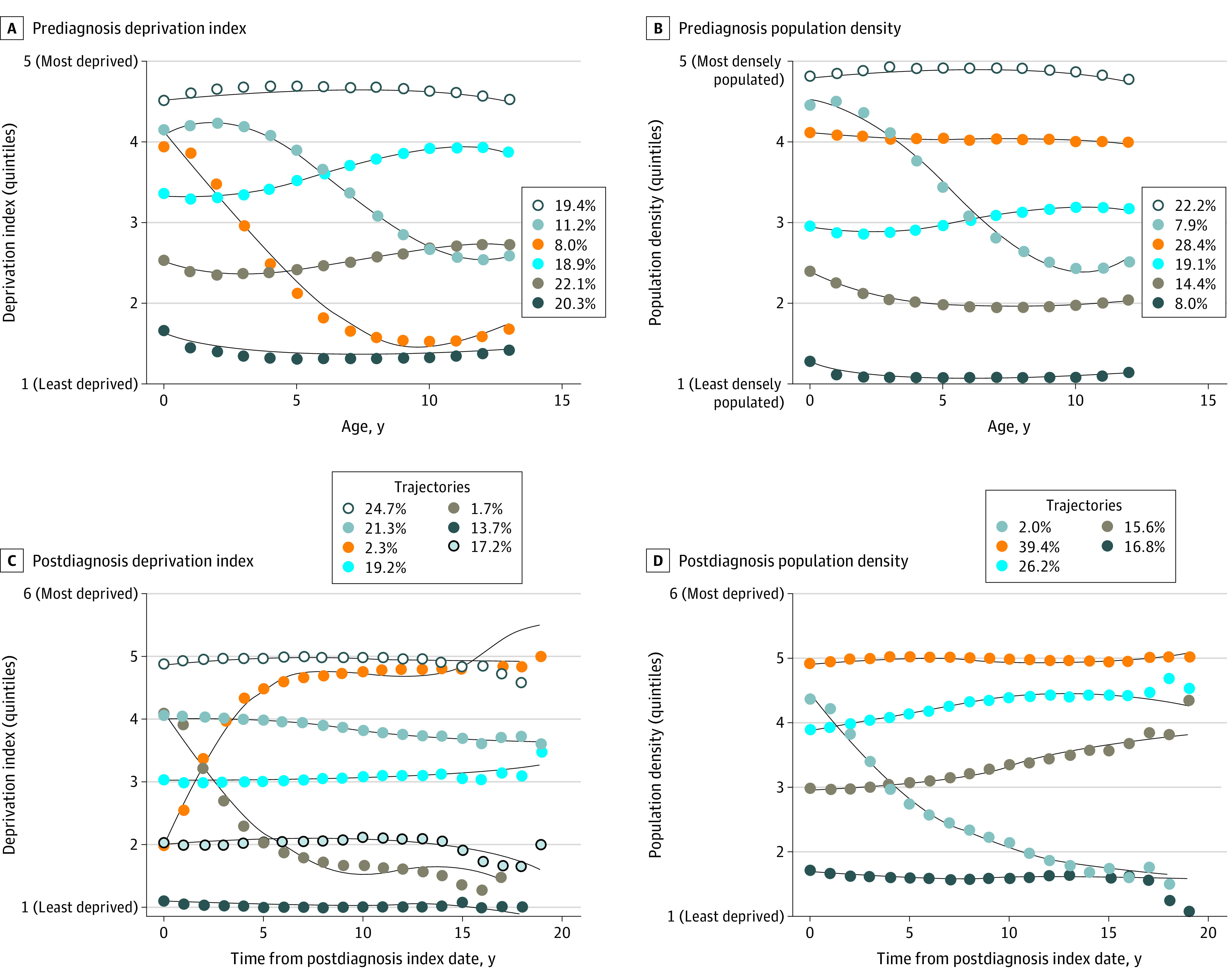
Numbers in the panel keys indicate the proportion of the sample assigned to each trajectory according to the maximum posterior probability assignment rule.
For population density, we were unable to execute the trajectory modeling for the entire follow-up period because of convergence issues. Therefore, we restricted the model from birth to 13 years of age and selected a 6-group model. Population density remained stable for 5 trajectories (from low to high; trajectories 1, 2, 3, 4, and 5; 92.1% of the sample) (Figure 2B). Trajectory 6 (7.9%) depicted an urban-rural movement group, which moved from more urban to rural environments in childhood.
Postdiagnosis Period
We chose a 7-group model for deprivation trajectories up to 19 years after the index diagnosis year (eTable 2 in Supplement 1). Deprivation remained stable for 5 trajectories (from low to high; trajectories 1, 2, 3, 4, and 5; 96.1% of the sample) (Figure 2C). Two further trajectories included a downward drift group (trajectory 6; 2.3%), moving from less to more deprived areas in the first 5 to 6 years after diagnosis, and, conversely, an upward mobility group (trajectory 7; 1.7%).
We modeled population density using a 5-group model. Population density remained largely stable after diagnosis for 4 trajectories (from low to high; trajectories 1, 2, 3, and 4; 98.0% of the sample) (Figure 2D). Trajectory 5 (2.0%) represented an urban-rural movement group, which moved from the most to least densely populated areas.
Association Between Trajectories and SMI Outcomes
Prediagnosis Period
In unadjusted and bivariable models, we observed strong gradients between living in greater deprivation trajectories from birth to 14 years of age and odds of psychotic disorder after 15 years of age (Table 2), which persisted in fully adjusted models (ie, trajectory 3: AOR, 1.17; 95% CI, 1.06-1.26; trajectory 4: AOR, 1.17; 95% CI, 1.08-1.28). A similar association was observed for nonpsychotic bipolar disorder (ie, trajectory 2: AOR, 1.14; 95% CI, 1.06-1.24; trajectory 3: AOR, 1.25, 95% CI, 1.16-1.36; trajectory 4: AOR, 1.23; 95% CI, 1.13-1.34). In fully adjusted models, odds of either outcome were ameliorated in the strong and moderately upward mobility trajectories (Table 2), with the strongest amelioration in the strong upward mobility group for both psychotic disorders (AOR, 1.01; 95% CI, 0.91-1.12) and nonpsychotic bipolar disorder (AOR, 1.08; 95% CI, 0.97-1.19).
Table 2. Prediagnosis Logistic Regression Models for Psychotic Disorder and Nonpsychotic Bipolar Disorder.
| Exposure | OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| Psychotic disorder | Nonpsychotic bipolar disorder | |||||
| Univariable model | Bivariable modela | Multivariable modelb | Univariable model | Bivariable modela | Multivariable modelb | |
| Deprivation index | ||||||
| Trajectory 1 (least deprived) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Trajectory 2 | 1.10 (1.02-1.19) | 1.16 (1.07-1.25) | 1.03 (0.95-1.12) | 1.21 (1.13-1.30) | 1.26 (1.17-1.36) | 1.14 (1.06-1.24) |
| Trajectory 3 | 1.38 (1.27-1.49) | 1.45 (1.34-1.57) | 1.17 (1.06-1.26) | 1.42 (1.32-1.53) | 1.51 (1.40-1.63) | 1.25 (1.16-1.36) |
| Trajectory 4 (most deprived) | 1.62 (1.50-1.75) | 1.56 (1.43-1.69) | 1.17 (1.08-1.28) | 1.42 (1.32-1.53) | 1.50 (1.39-1.63) | 1.23 (1.13-1.34) |
| Trajectory 5 (strong upward mobility) | 1.25 (1.12-1.38) | 1.22 (1.10-1.35) | 1.01 (0.91-1.12) | 1.29 (1.17-1.42) | 1.26 (1.14-1.39) | 1.08 (0.97-1.19) |
| Trajectory 6 (moderate upward mobility) | 1.46 (1.33-1.60) | 1.46 (1.33-1.60) | 1.11 (1.01-1.23) | 1.50 (1.38-1.64) | 1.53 (1.40-1.68) | 1.21 (1.10-1.33) |
| Population density | ||||||
| Trajectory 1 (least densely populated) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Trajectory 2 | 1.14 (1.02-1.28) | 1.22 (1.09-1.36) | 1.08 (0.96-1.21) | 1.13 (1.02-1.26) | 1.19 (1.07-1.32) | 1.07 (0.97-1.19) |
| Trajectory 3 | 1.26 (1.14-1.40) | 1.42 (1.28-1.58) | 1.17 (1.05-1.31) | 1.12 (1.01-1.23) | 1.25 (1.13-1.38) | 1.06 (0.96-1.18) |
| Trajectory 4 | 1.36 (1.23-1.50) | 1.55 (140-1.71) | 1.21 (1.08-1.34) | 1.23 (1.12-1.35) | 1.41 (1.28-1.55) | 1.16 (1.05-1.28) |
| Trajectory 5 (most densely populated) | 1.96 (1.77-2.16) | 1.98 (1.79-2.19) | 1.49 (1.34-1.66) | 1.23 (1.12-1.36) | 1.27 (1.15-1.41) | 1.08 (0.97-1.20) |
| Trajectory 6 (urban-rural movement) | 1.69 (1.49-1.91) | 1.82 (1.60-2.06) | 1.29 (1.13-1.47) | 1.58 (1.40-1.78) | 1.69 (1.49-1.90) | 1.24 (1.09-1.41) |
| Parental migrant status | 1.73 (1.63-1.84) | NA | 1.43 (1.33-1.52) | 1.12 (1.05-1.19) | NA | 1.02 (0.96-1.09) |
| Parental history of SMI | 3.94 (3.52-4.40) | NA | 3.44 (3.08-3.85) | 4.28 (3.86-4.75) | NA | 3.87 (3.48-4.30) |
| Parental disposable income at birth | ||||||
| 1 (Lowest quintile) | 1 [Reference] | NA | 1 [Reference] | 1 [Reference] | NA | 1 [Reference] |
| 2 | 0.72 (0.67-0.78) | NA | 0.83 (0.77-0.90) | 0.95 (0.88-1.02) | NA | 1.05 (0.97-1.14) |
| 3 | 0.64 (0.59-0.69) | NA | 0.80 (0.74-0.87) | 0.85 (0.79-0.91) | NA | 0.99 (0.92-1.07) |
| 4 | 0.66 (0.61-0.71) | NA | 0.86 (0.79-0.93) | 0.73 (0.68-0.79) | NA | 0.90 (0.83-0.97) |
| 5 (Highest quintile) | 0.63 (0.58-0.68) | NA | 0.83 (0.76-0.90) | 0.79 (0.73-0.85) | NA | 1.01 (0.93-1.10) |
| Moves between birth and 14th year | 1.21 (1.19-1.24) | NA | 1.16 (1.14-1.18) | 1.21 (1.19-1.23) | NA | 1.16 (1.14-1.18) |
Abbreviations: NA, not applicable; OR, odds ratio; SMI, severe mental illness.
Adjusted for deprivation index and population density trajectory membership and controlling for birth year and sex by matching cases and controls.
Adjusted as in the bivariable model and for parental migrant status, parental history of SMI, parental disposable income at birth, and number of moves (between birth and 14th year).
A gradated association was also observed between population density and psychotic disorder risk (ie, trajectory 3: AOR, 1.17; 95% CI, 1.05-1.31; trajectory 4: AOR, 1.21; 95% CI, 1.08-1.34; trajectory 5: AOR, 1.49; 95% CI, 1.34-1.66) (Table 2) but not nonpsychotic bipolar disorder. Those in the urban-rural movement trajectory had increased odds of psychotic disorder (AOR, 1.29; 95% CI, 1.13-1.47) and nonpsychotic bipolar disorder (AOR, 1.24; 95% CI, 1.09-1.41).
Postdiagnosis Period
After diagnosis, case patients with both psychotic disorders (trajectory 4: AOR, 1.19; 95% CI, 1.09-130; trajectory 5: AOR, 1.36; 95% CI, 1.24-1.48) and nonpsychotic bipolar disorder (trajectory 4: AOR, 1.21; 95% CI, 1.11-1.32; trajectory 5: AOR, 1.39; 95% CI, 1.28-1.51) were at greater odds of living in more deprived trajectories compared with controls (Table 3). Case patients with psychotic disorder were also more likely to belong to the downward drift trajectory than controls (OR, 1.38; 95% CI, 1.16-1.65), but not case patients with nonpsychotic bipolar disorder. Upward mobility was not associated with either outcome. Nonetheless, only 543 case patients (2.0%) drifted into more deprived areas after diagnosis.
Table 3. Postdiagnosis Logistic Regression Models for Psychotic Disorder and Nonpsychotic Bipolar Disorder.
| Exposures | OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| Psychotic disorder | Nonpsychotic bipolar disorder | |||||
| Univariable model | Bivariable modela | Multivariable modelb | Univariable model | Bivariable modela | Multivariable modelb | |
| Deprivation index | ||||||
| Trajectory 1 (least deprived) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Trajectory 2 | 1.00 (0.91-1.09) | 1.03 (0.94-1.12) | 1.02 (0.93-1.12) | 1.04 (0.96-1.13) | 1.04 (0.96-1.14) | 1.04 (0.95-1.14) |
| Trajectory 3 | 1.03 (0.94-1.12) | 1.07 (0.98-1.17) | 1.04 (0.95-1.14) | 1.16 (1.06-1.26) | 1.16 (1.07-1.26) | 1.11 (1.02-1.21) |
| Trajectory 4 | 1.23 (1.13-1.34) | 1.27 (1.16-1.38) | 1.19 (1.09-1.30) | 1.28 (1.18-1.39) | 1.29 (1.19-1.40) | 1.21 (1.11-1.32) |
| Trajectory 5 (most deprived) | 1.55 (1.43-1.69) | 1.57 (1.44-1.70) | 1.36 (1.24-1.48) | 1.51 (1.39-1.64) | 1.52 (1.40-1.65) | 1.39 (1.28-1.51) |
| Trajectory 6 (downward drift) | 1.29 (1.09-1.53) | 1.28 (1.08-1.51) | 1.38 (1.16-1.65) | 1.28 (1.03-1.57) | 1.28 (1.04-1.58) | 1.06 (0.85-1.33) |
| Trajectory 7 (upward mobility) | 0.85 (0.80-0.91) | 0.86 (0.70-1.06) | 0.91 (0.74-1.13) | 1.29 (1.01-1.65) | 1.30 (1.01-1.67) | 1.11 (0.86-1.44) |
| Population density | ||||||
| Trajectory 1 (least densely populated) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Trajectory 2 | 1.25 (1.14-1.36) | 1.25 (1.14-1.36) | 1.21 (1.10-1.32) | 1.03 (0.95-1.11) | 1.03 (0.95-1.12) | 1.02 (0.93-1.11) |
| Trajectory 3 | 1.34 (1.24-1.45) | 1.33 (1.23-1.44) | 1.27 (1.18-1.38) | 1.02 (0.95-1.09) | 1.02 (0.95-1.10) | 0.99 (0.91-1.07) |
| Trajectory 4 (most densely populated) | 1.35 (1.26-1.45) | 1.26 (1.17-1.36) | 1.15 (1.07-1.25) | 1.06 (0.99-1.14) | 1.01 (0.94-1.08) | 0.97 (0.90-1.04) |
| Trajectory 5 (urban-rural movement) | 1.15 (0.94-1.40) | 1.13 (0.93-1.39) | 1.15 (0.93-1.42) | 1.06 (0.85-1.32) | 0.99 (0.79-1.24) | 0.87 (0.69-1.10) |
| Parental migrant status | 1.73 (1.63-1.84) | NA | 1.51 (1.41-1.61) | 1.12 (1.05-1.19) | NA | 1.03 (0.97-1.10) |
| Parental history of SMI | 3.94 (3.52-4.40) | NA | 3.47 (3.10-3.88) | 4.28 (3.86-4.75) | NA | 3.86 (3.47-4.29) |
| Parental disposable income at birth | ||||||
| 1 (Lowest quintile) | 1 [Reference] | NA | 1 [Reference] | 1 [Reference] | NA | 1 [Reference] |
| 2 | 0.72 (0.67-0.78) | NA | 0.82 (0.76-0.89) | 0.95 (0.88-1.02) | NA | 1.05 (0.97-1.13) |
| 3 | 0.64 (0.59-0.69) | NA | 0.79 (0.73-0.86) | 0.85 (0.79-0.91) | NA | 0.99 (0.92-1.07) |
| 4 | 0.66 (0.61-0.71) | NA | 0.85 (0.78-0.92) | 0.73 (0.68-0.79) | NA | 0.90 (0.83-0.97) |
| 5 (Highest quintile) | 0.63 (0.58-0.68) | NA | 0.83 (0.76-0.90) | 0.79 (0.73-0.85) | NA | 1.01 (0.93-1.10) |
| Moves between birth and 14th year | 1.21 (1.19-1.24) | NA | 1.17 (1.15-1.19) | 1.21 (1.19-1.23) | NA | 1.17 (1.15-1.19) |
| Moves between diagnosis and end of follow-up | 0.97 (0.95-0.99) | NA | 0.95 (0.94-0.97) | 1.08 (1.06-1.09) | NA | 1.06 (1.04-1.08) |
Abbreviations: NA, not applicable; OR, odds ratio; SMI, severe mental illness.
Adjusted for deprivation index and population density trajectory membership and controlling for birth year and sex by matching cases and controls.
Adjusted as in the bivariable model and for parental migrant status, parental history of SMI, parental disposable income at birth, number of moves between birth and 14th year, and number of moves between diagnosis and end of follow-up.
People with psychotic disorder were more likely to belong to more densely populated postdiagnosis trajectories than controls, although no dose-response pattern was evident (trajectory 2: AOR, 1.21, 95% CI, 1.10-1.32; trajectory 3: AOR, 1.27; 95% CI, 1.18-1.38; trajectory 4: AOR, 1.15; 95% CI, 1.07-1.25) (Table 3). There was no association between the urban-rural movement trajectory and psychotic disorder or between postdiagnosis population density trajectories and nonpsychotic bipolar disorder.
Post Hoc Analyses
Individuals with psychotic disorder were more likely to be in more deprived trajectories following diagnosis than in the upward mobility trajectory compared with controls (trajectory 4: AOR, 1.30; 95% CI, 1.06-1.60; trajectory 5: AOR, 1.49; 95% CI, 1.21-1.83) (eTable 5 in Supplement 1), indicative of relative social immobility among people with a psychotic disorder. This finding was not observed for nonpsychotic bipolar disorder or for either outcome regarding population density with urban-rural movement as the reference category (eTable 5 in Supplement 1).
Discussion
Principal Findings
In this nested case-control study, from birth until early adolescence, we observed strong gradients between living in more deprived and densely populated areas and future odds of psychosis, congruent with the social causation theory. These odds were ameliorated in proportion with the degree of upward mobility experienced during upbringing. Similar findings were observed with respect to deprivation but not population density for nonpsychotic bipolar disorder.
After diagnosis, people with psychotic disorder were more likely than controls to drift downward into more deprived areas, although this was only experienced by 2.7% of those with psychotic disorder. Relative social immobility was a bigger driver of exposure to deprivation after diagnosis than social drift, with people with SMI disproportionately remaining in the most deprived trajectory quintile.
Meaning of the Findings
Our findings are consistent with research that shows elevated incidence of psychosis in those who are born or reside in deprived and densely populated areas before diagnosis.3,8,46,47 Although early residential mobility may increase psychosis risk through disruption to social networks,39,48 our findings show that upward mobility reduces future SMI risk, consistent with work from Denmark, where children who moved to less urban areas during upbringing had a reduced schizophrenia risk.3 We extend that work by showing that this effect appears specific to deprivation and was evident in early childhood for both psychotic disorders and nonpsychotic bipolar disorder. Furthermore, our trajectory modeling approach suggests that social deprivation is a modifiable risk factor for SMI: the earlier participants experienced upward mobility, the lower their subsequent SMI risk. Potential mechanisms include both a critical window of susceptibility to deprivation in childhood and a cumulative exposure hypothesis. It is also possible that threshold effects also exist. In our analyses, exposure to deprivation during childhood only increased the odds of psychosis in the 2 highest quintiles of persistent exposure to deprivation, consistent with earlier research.49,50 Alternatively, a noncausal explanation would arise if case patients and control participants who experienced upward mobility were systematically different on unobserved confounders, including genetic liability to SMI, from those who remained in more deprived trajectories during upbringing. Nonetheless, we controlled for several covariates, including parental history of SMI, lending credence to a causal interpretation. If our results were causal, this would suggest that socioeconomic interventions that lift people out of more deprived environments earlier in childhood would mitigate future SMI risk. Recent research provides potential clues, including evidence that children exposed to greater deprivation have lower total brain volumes and other structural brain differences,51 that greater deprivation is associated with biomarkers of allostatic load,52 and that cognition partially mediates the effect of deprivation on nonaffective psychosis.21
We also identified gradients between population density during upbringing and later risk of psychotic disorders, as previously observed.3,8,46 This finding was less evident for nonpsychotic bipolar disorders, consistent with previous evidence.23 Interestingly, we observed that those moving from more urban to rural areas remained at increased SMI risk, suggesting that early exposure to factors associated with population density can have a lasting impact on mental health. Marcelis et al53 also reported stronger associations of urban birth than later residency with schizophrenia risk. These findings suggest that deprivation and population density may have different critical windows or may operate differently to influence SMI risk. Further theoretical development and empirical studies are required to disentangle these potentially causal explanations.
Our study adds to the evidence base that limited social drift occurs after SMI diagnosis.20,22 A recent Welsh study also did not observe such a process during a 10-year period26 but could not exclude relative social immobility (termed “passive social drift” in their article), which has been demonstrated to be a more predominant social process in our study and in others.20 People with psychotic disorders but not nonpsychotic bipolar disorder were more likely to live in more urban areas after diagnosis, but no dose-response relationship was observed; any urban area may offer better access to mental health care services than the most rural communities in our analyses.
Strengths and Limitations
Using registry data, our sample was largely representative of the Swedish-born population, with a low likelihood of selection bias given minimal missing data (2.5%). Our exposures were well validated and prospectively measured, minimizing recall bias.21,40 Registry-based diagnostic codes have good concurrent validity with SMI diagnoses.54 The use of trajectory modeling allowed us to identify distinct longitudinal patterns of neighborhood-level exposures. Although all participants had complete data on prediagnosis trajectories until 14 years of age, our postdiagnosis trajectories included differential lengths of follow-up data, which became sparser beyond 15 years (Figure 2). Modeling quintile data may have captured less variability than possible through continuous data.
We controlled for several potential confounders, including age, period, and cohort and sex effects by design, as well as parental migrant status, number of residential moves, and parental history of SMI. The last, a marker of shared familial liability, did not substantively confound our findings. However, direct measures of genetic liability, such as polygenic risk scores for schizophrenia, were unavailable. These measures have previously been associated with residence in more urban environments,28 and thus intergenerational selection may explain our results.29 However, we believe this is unlikely because associations between neighborhood deprivation or urbanicity and psychosis have remained in several studies after controlling for different genetic risk indexes.31,32,33 We also did not have data on other potential confounders, such as individual-level socioeconomic status, birth order, or adverse childhood experiences.55,56,57,58
Implications for Policy, Practice, and Future Research
For policy makers, our results highlight which population groups are most likely to experience psychotic disorders and nonpsychotic bipolar disorders. We also observed that people with SMI tend to disproportionately remain living in the most deprived quintiles up to 20 years after diagnosis and, for people with psychotic disorders, in the most densely populated environments. This finding can inform provisions of early intervention for psychosis services and of health care resources in these communities, building on existing efforts to translate psychiatric epidemiology into effective resource allocation models.59 For public mental health, our results should guide prevention efforts that are preferentially located in more deprived and densely populated areas and linked with socioeconomic support.
Social deprivation appears to have its strongest influence on SMI risk in childhood and early adolescence, but our results crucially suggest its impact is modifiable through upward mobility. This finding provides vital clues for intervention research and suggests that ambitious trials are now warranted to investigate whether moving people out of more deprived environments can ameliorate SMI risk. To our knowledge, no trial has tested such interventions regarding SMI, although the Moving to Opportunity trial has shown evidence that moving to higher-quality neighborhoods resulted in lower psychological distress in adolescence,60 although this may also have introduced unintended harms for some groups, including increased mental health risks for boys.61
Our results also have implications for etiological research. We support calls for more interdisciplinary approaches to understand and target potential environmental risk factors that link early-life exposure to deprivation and urbanicity with later SMI risk.62 Future studies should also investigate these trajectories in more diverse samples, including immigrant communities and settings outside the Global North, where emerging evidence suggests that the greater concentration of psychosis in urban areas may not hold.63 We also need to better understand whether trajectories of exposure immediately before diagnosis are influenced by drift processes before onset. Whether SMI risk associated with exposure to different trajectories applies to all individuals or may be stronger or weaker for some groups (such as by income, migrant, or ethnic status) also requires further investigation. Finally, future studies could investigate functional and clinical outcomes within each trajectory to identify those in greatest need of support.
Conclusion
The findings of this nested case-control study suggest that social causation and relative social immobility may play distinct roles in the onset and subsequent exposure to more deprived and urban environments for people with SMI. Importantly, our findings suggest upward social mobility may mitigate the impact of early-life deprivation.
eMethods. Supplemental Methods
eResults. Supplemental Results
eTable 1. Baseline Characteristics of Cases and Controls With Complete and Missing Data
eTable 2. BIC and Entropy Values for Each GBTM Model
eTable 3. Model Fit Statistics for Each Final GBTM Model
eTable 4. Proportion of Cases and Controls Assigned to Each Trajectory Group for Each Model
eTable 5. Post-diagnosis Logistic Regression Models for Psychotic and Nonpsychotic SMI With Upward Mobility and Urban-Rural Movement of the Reference Groups
eReferences
Data Sharing Statement
References
- 1.Faris REL, Dunham HW. Mental Disorders in Urban Areas: An Ecological Study of Schizophrenia and Other Psychoses. University of Chicago Press; 1939. [Google Scholar]
- 2.Kirkbride JB, Jones PB, Ullrich S, Coid JW. Social deprivation, inequality, and the neighborhood-level incidence of psychotic syndromes in East London. Schizophr Bull. 2014;40(1):169-180. doi: 10.1093/schbul/sbs151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry. 2001;58(11):1039-1046. doi: 10.1001/archpsyc.58.11.1039 [DOI] [PubMed] [Google Scholar]
- 4.Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression: follow-up study of 4.4 million women and men in Sweden. Br J Psychiatry. 2004;184(4):293-298. doi: 10.1192/bjp.184.4.293 [DOI] [PubMed] [Google Scholar]
- 5.Allardyce J, Boydell J. Review: the wider social environment and schizophrenia. Schizophr Bull. 2006;32(4):592-598. doi: 10.1093/schbul/sbl008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly BD, O’Callaghan E, Waddington JL, et al. Schizophrenia and the city: a review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr Res. 2010;116(1):75-89. doi: 10.1016/j.schres.2009.10.015 [DOI] [PubMed] [Google Scholar]
- 7.Kirkbride JB, Errazuriz A, Croudace TJ, et al. Incidence of schizophrenia and other psychoses in England, 1950-2009: a systematic review and meta-analyses. PLoS One. 2012;7(3):e31660. doi: 10.1371/journal.pone.0031660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev. 2008;30(1):84-100. doi: 10.1093/epirev/mxn006 [DOI] [PubMed] [Google Scholar]
- 9.O’Donoghue B, Roche E, Lane A. Neighbourhood level social deprivation and the risk of psychotic disorders: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2016;51(7):941-950. doi: 10.1007/s00127-016-1233-4 [DOI] [PubMed] [Google Scholar]
- 10.Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38(6):1118-1123. doi: 10.1093/schbul/sbs096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pedersen CB, Antonsen S, Timmermann A, et al. Urban-rural differences in schizophrenia risk: multilevel survival analyses of individual- and neighborhood-level indicators, urbanicity and population density in a Danish national cohort study. Schizophr Bull Open. 2021;3(1):sgab056. doi: 10.1093/schizbullopen/sgab056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper B. Immigration and schizophrenia: the social causation hypothesis revisited. Br J Psychiatry. 2005;186(5):361-363. doi: 10.1192/bjp.186.5.361 [DOI] [PubMed] [Google Scholar]
- 13.Brenner MH. Mental Illness and the Economy. Harvard University Press; 1973. [Google Scholar]
- 14.Cantor-Graae E, Selten J-P. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162(1):12-24. doi: 10.1176/appi.ajp.162.1.12 [DOI] [PubMed] [Google Scholar]
- 15.Verheij RA, van de Mheen HD, de Bakker DH, Groenewegen PP, Mackenbach JP. Urban-rural variations in health in The Netherlands: does selective migration play a part? J Epidemiol Community Health. 1998;52(8):487-493. doi: 10.1136/jech.52.8.487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox JW. Social class, mental illness, and social mobility: the social selection-drift hypothesis for serious mental illness. J Health Soc Behav. 1990;31(4):344-353. doi: 10.2307/2136818 [DOI] [PubMed] [Google Scholar]
- 17.Dunham HW. Community and Schizophrenia: An Epidemiological Analysis. Wayne State University Press; 1965. [Google Scholar]
- 18.Goldberg EM, Morrison SL. Schizophrenia and social class. Br J Psychiatry. 1963;109(463):785-802. doi: 10.1192/bjp.109.463.785 [DOI] [PubMed] [Google Scholar]
- 19.Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75(1):3-18. doi: 10.1037/0002-9432.75.1.3 [DOI] [PubMed] [Google Scholar]
- 20.Hudson CG. Patterns of residential mobility of people with schizophrenia: multi-level tests of downward geographic drift. J Sociol Soc Welf. 2012;39:149. doi: 10.15453/0191-5096.3688 [DOI] [Google Scholar]
- 21.Lewis G, Dykxhoorn J, Karlsson H, et al. Assessment of the role of IQ in associations between population density and deprivation and nonaffective psychosis. JAMA Psychiatry. 2020;77(7):729-736. doi: 10.1001/jamapsychiatry.2020.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ngamini Ngui A, Cohen AA, Courteau J, et al. Does elapsed time between first diagnosis of schizophrenia and migration between health territories vary by place of residence? a survival analysis approach. Health Place. 2013;20:66-74. doi: 10.1016/j.healthplace.2012.12.003 [DOI] [PubMed] [Google Scholar]
- 23.Pedersen CB, Mortensen PB. Urbanicity during upbringing and bipolar affective disorders in Denmark. Bipolar Disord. 2006;8(3):242-247. doi: 10.1111/j.1399-5618.2006.00307.x [DOI] [PubMed] [Google Scholar]
- 24.Lewis G, David A, Andréasson S, Allebeck P. Schizophrenia and city life. Lancet. 1992;340(8812):137-140. doi: 10.1016/0140-6736(92)93213-7 [DOI] [PubMed] [Google Scholar]
- 25.Mortensen PB, Pedersen CB, Westergaard T, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340(8):603-608. doi: 10.1056/NEJM199902253400803 [DOI] [PubMed] [Google Scholar]
- 26.Lee SC, DelPozo-Banos M, Lloyd K, et al. Area deprivation, urbanicity, severe mental illness and social drift—a population-based linkage study using routinely collected primary and secondary care data. Schizophr Res. 2020;220:130-140. doi: 10.1016/j.schres.2020.03.044 [DOI] [PubMed] [Google Scholar]
- 27.Pignon B, Eaton S, Schürhoff F, Szöke A, McGorry P, O’Donoghue B. Residential social drift in the two years following a first episode of psychosis. Schizophr Res. 2019;210:323-325. doi: 10.1016/j.schres.2019.06.008 [DOI] [PubMed] [Google Scholar]
- 28.Colodro-Conde L, Couvy-Duchesne B, Whitfield JB, et al. Association between population density and genetic risk for schizophrenia. JAMA Psychiatry. 2018;75(9):901-910. doi: 10.1001/jamapsychiatry.2018.1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sariaslan A, Fazel S, D’Onofrio BM, et al. Schizophrenia and subsequent neighborhood deprivation: revisiting the social drift hypothesis using population, twin and molecular genetic data. Transl Psychiatry. 2016;6(5):e796. doi: 10.1038/tp.2016.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gage SH, Davey Smith G, Munafò MR. Schizophrenia and neighbourhood deprivation. Transl Psychiatry. 2016;6(12):e979. doi: 10.1038/tp.2016.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Solmi F, Lewis G, Zammit S, Kirkbride JB. Neighborhood characteristics at birth and positive and negative psychotic symptoms in adolescence: findings from the ALSPAC birth cohort. Schizophr Bull. 2020;46(3):581-591. doi: 10.1093/schbul/sbz049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paksarian D, Trabjerg BB, Merikangas KR, et al. The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychol Med. 2018;48(2):305-314. doi: 10.1017/S0033291717001696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Newbury JB, Arseneault L, Caspi A, et al. Association between genetic and socioenvironmental risk for schizophrenia during upbringing in a UK longitudinal cohort. Psychol Med. 2022;52(8):1527-1537. doi: 10.1017/S0033291720003347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fan CC, McGrath JJ, Appadurai V, et al. Spatial fine-mapping for gene-by-environment effects identifies risk hot spots for schizophrenia. Nat Commun. 2018;9(1):5296. doi: 10.1038/s41467-018-07708-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaymaz N, Krabbendam L, de Graaf R, Nolen W, Ten Have M, van Os J. Evidence that the urban environment specifically impacts on the psychotic but not the affective dimension of bipolar disorder. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):679-685. doi: 10.1007/s00127-006-0086-7 [DOI] [PubMed] [Google Scholar]
- 36.Dykxhoorn J, Hollander AC, Lewis G, Magnusson C, Dalman C, Kirkbride JB. Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status, region of origin, and age-at-migration: a national cohort study of 1.8 million people. Psychol Med. 2019;49(14):2354-2363. doi: 10.1017/S0033291718003227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crump C, Sundquist K, Sundquist J, Winkleby MA. Neighborhood deprivation and psychiatric medication prescription: a Swedish national multilevel study. Ann Epidemiol. 2011;21(4):231-237. doi: 10.1016/j.annepidem.2011.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lofors J, Sundquist K. Low-linking social capital as a predictor of mental disorders: a cohort study of 4.5 million Swedes. Soc Sci Med. 2007;64(1):21-34. doi: 10.1016/j.socscimed.2006.08.024 [DOI] [PubMed] [Google Scholar]
- 39.Price C, Dalman C, Zammit S, Kirkbride JB. Association of residential mobility over the life course with nonaffective psychosis in 1.4 million young people in Sweden. JAMA Psychiatry. 2018;75(11):1128-1136. doi: 10.1001/jamapsychiatry.2018.2233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Terhune J, Dykxhoorn J, Mackay E, Hollander AC, Kirkbride JB, Dalman C. Migrant status and risk of compulsory admission at first diagnosis of psychotic disorder: a population-based cohort study in Sweden. Psychol Med. 2022;52(2):362-371. doi: 10.1017/S0033291720002068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nagin DS, Nagin D. Group-Based Modeling of Development. Harvard University Press; 2005. doi: 10.4159/9780674041318 [DOI] [Google Scholar]
- 42.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109-138. doi: 10.1146/annurev.clinpsy.121208.131413 [DOI] [PubMed] [Google Scholar]
- 43.Shearer DM, Thomson WM, Broadbent JM, McLean R, Poulton R, Mann J. High-risk glycated hemoglobin trajectories established by mid-20s: findings from a birth cohort study. BMJ Open Diabetes Res Care. 2016;4(1):e000243. doi: 10.1136/bmjdrc-2016-000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dong Y, Peng CY. Principled missing data methods for researchers. Springerplus. 2013;2(1):222. doi: 10.1186/2193-1801-2-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones BL, Nagin DS. A note on a stata plugin for estimating group-based trajectory models. Sociol Methods Res. 2013;42(4):608-613. doi: 10.1177/0049124113503141 [DOI] [Google Scholar]
- 46.Heinz A, Deserno L, Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. 2013;12(3):187-197. doi: 10.1002/wps.20056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Werner S, Malaspina D, Rabinowitz J. Socioeconomic status at birth is associated with risk of schizophrenia: population-based multilevel study. Schizophr Bull. 2007;33(6):1373-1378. doi: 10.1093/schbul/sbm032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Paksarian D, Eaton WW, Mortensen PB, Pedersen CB. Childhood residential mobility, schizophrenia, and bipolar disorder: a population-based study in Denmark. Schizophr Bull. 2015;41(2):346-354. doi: 10.1093/schbul/sbu074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirkbride JB, Hameed Y, Ankireddypalli G, et al. The epidemiology of first-episode psychosis in early intervention in psychosis services: findings from the Social Epidemiology of Psychoses in East Anglia [SEPEA] study. Am J Psychiatry. 2017;174(2):143-153. doi: 10.1176/appi.ajp.2016.16010103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Croudace TJ, Kayne R, Jones PB, Harrison GL. Non-linear relationship between an index of social deprivation, psychiatric admission prevalence and the incidence of psychosis. Psychol Med. 2000;30(1):177-185. doi: 10.1017/S0033291799001464 [DOI] [PubMed] [Google Scholar]
- 51.Mackes NK, Golm D, Sarkar S, et al. ; ERA Young Adult Follow-up team . Early childhood deprivation is associated with alterations in adult brain structure despite subsequent environmental enrichment. Proc Natl Acad Sci U S A. 2020;117(1):641-649. doi: 10.1073/pnas.1911264116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ribeiro AI, Fraga S, Kelly-Irving M, et al. Neighbourhood socioeconomic deprivation and allostatic load: a multi-cohort study. Sci Rep. 2019;9(1):8790. doi: 10.1038/s41598-019-45432-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marcelis M, Takei N, van Os J. Urbanization and risk for schizophrenia: does the effect operate before or around the time of illness onset? Psychol Med. 1999;29(5):1197-1203. doi: 10.1017/S0033291799008983 [DOI] [PubMed] [Google Scholar]
- 54.Ekholm B, Ekholm A, Adolfsson R, et al. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry. 2005;59(6):457-464. doi: 10.1080/08039480500360906 [DOI] [PubMed] [Google Scholar]
- 55.Haukka JK, Suvisaari J, Lönnqvist J. Family structure and risk factors for schizophrenia: case-sibling study. BMC Psychiatry. 2004;4:41. doi: 10.1186/1471-244X-4-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661-671. doi: 10.1093/schbul/sbs050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Luo Y, Zhang L, He P, Pang L, Guo C, Zheng X. Individual-level and area-level socioeconomic status (SES) and schizophrenia: cross-sectional analyses using the evidence from 1.9 million Chinese adults. BMJ Open. 2019;9(9):e026532. doi: 10.1136/bmjopen-2018-026532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hakulinen C, Webb RT, Pedersen CB, Agerbo E, Mok PLH. Association between parental income during childhood and risk of schizophrenia later in life. JAMA Psychiatry. 2020;77(1):17-24. doi: 10.1001/jamapsychiatry.2019.2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McDonald K, Ding T, Ker H, et al. Using epidemiological evidence to forecast population need for early treatment programmes in mental health: a generalisable bayesian prediction methodology applied to and validated for first-episode psychosis in England. Br J Psychiatry. 2021;219(1):383-391. doi: 10.1192/bjp.2021.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmidt NM, Glymour MM, Osypuk TL. Does the temporal pattern of moving to a higher-quality neighborhood across a 5-year period predict psychological distress among adolescents? results from a federal housing experiment. Am J Epidemiol. 2021;190(6):998-1008. doi: 10.1093/aje/kwaa256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rudolph KE, Gimbrone C, Díaz I. Helped into harm: mediation of a housing voucher intervention on mental health and substance use in boys. Epidemiology. 2021;32(3):336-346. doi: 10.1097/EDE.0000000000001334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abrahamyan Empson L, Baumann PS, Söderström O, Codeluppi Z, Söderström D, Conus P. Urbanicity: the need for new avenues to explore the link between urban living and psychosis. Early Interv Psychiatry. 2020;14(4):398-409. doi: 10.1111/eip.12861 [DOI] [PubMed] [Google Scholar]
- 63.Roberts T, Susser E, Lee Pow J, et al. ; INTREPID Group . Urbanicity and rates of untreated psychotic disorders in three diverse settings in the Global South. Psychol Med. Published online January 16, 2023. doi: 10.1017/S0033291722003749 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplemental Methods
eResults. Supplemental Results
eTable 1. Baseline Characteristics of Cases and Controls With Complete and Missing Data
eTable 2. BIC and Entropy Values for Each GBTM Model
eTable 3. Model Fit Statistics for Each Final GBTM Model
eTable 4. Proportion of Cases and Controls Assigned to Each Trajectory Group for Each Model
eTable 5. Post-diagnosis Logistic Regression Models for Psychotic and Nonpsychotic SMI With Upward Mobility and Urban-Rural Movement of the Reference Groups
eReferences
Data Sharing Statement