Abstract
Aim
The diagnosis of acute vertebral compression fractures (AVCFs) is often challenging. An alternative to magnetic resonance imaging, which may not always be available, includes a comparison of supine and sitting/standing position radiographs. However, this cannot be accomplished in patients with acute vertebral compression fractures who require emergency transport and are in severe pain. In this study, aimed to assess the diagnostic accuracy of comparing lateral‐view radiographs of the thoracolumbar spine in supine and 30° head‐elevated positions, which are less painful.
Methods
We retrospectively examined 30 patients with AVCFs who were transported by ambulance to our emergency department between June 2018 and May 2019. All underwent 30° head‐elevated lateral‐view thoracolumbar spine radiography and magnetic resonance imaging. We evaluated vertebral fractures by examining changes in vertebral wedging ratio (WR) from supine to 30° head‐elevated position (Δ WR) using the following equation: Δ WR = WR (30° head‐elevated) – WR (supine). We compared Δ WR to that of unfractured vertebrae as control.
Results
A total of 176 vertebrae were included (fractured, 32 and non‐fractured, 144). Δ WR of fractured vertebrae ranged between 5.1% and 24.4%, whereas non‐fractured vertebrae ranged between −6.7% and 4.3%. Median Δ WR of fractured vertebrae was significantly higher than non‐fractured vertebrae (12.6% versus −0.5%, p < 0.001). No patients reported pain during 30° head‐elevated positioning.
Conclusions
Lateral radiographs in supine and 30° head‐elevated positions can accurately diagnose of AVCF, without worsening pain. This study showed a Δ WR value of ≥5.1% for AVCFs.
Keywords: emergency medical service, lumbar vertebrae, magnetic resonance imaging, osteoporosis, thoracic vertebrae
This study showed a Δ wedging ratio (WR) (change of WR from supine to 30° head‐elevated position) value of ≥5.1% for acute vertebral compression fractures. WR (supine) = (b–a)/b × 100 (%), WR (30° head‐elevated) = (d–c)/d × 100 (%) Δ WR = WR (30° head‐elevated) – WR (supine) = (d–c)/d × 100–(b–a)/b × 100 (%).

INTRODUCTION
The incidence of acute vertebral compression fractures (AVCFs) in older patients raises with the aging global population's growth. 1 AVCFs due to osteoporosis are the most frequent fragility‐associated fractures. 2 Risk factors include advanced age, osteoporosis, menopause, and prior compression fractures. 2 Simple daily activities, such as lifting, descending stairs, slipping, coughing, or sneezing can cause these fractures. 3
Most frequent sites for AVCFs in older adults are the seventh, eighth, and twelfth thoracic vertebrae (T7, T8, and T12) and the first lumbar vertebra (L1). 4
X‐rays are commonly used for diagnosing AVCFs, 5 however, distinguishing new from previous fractures using X‐rays 6 is challenging. Aging‐associated degenerative spinal changes complicate AVCFs diagnosis. 7 , 8 Vertebral fractures have a high relative risk of death (1.4 in men and 1.1 in women), because of ensuing sarcopenia, emphasizing the need for early diagnosis. 9 , 10 Current guidelines recommend early magnetic resonance imaging (MRI) or computed tomography (CT) imaging to exclude new fractures, even without percussion pain. 11 However, MRI may be unavailable in certain medical settings or contraindicated because of factors such as claustrophobia or metallic implants. 12 Additionally, CT and MRI are expensive, and certain facilities do not have immediate access to these scanners. Furthermore, MRI scans require longer waiting and examination periods compared to CT scans, leading to extended hospital stays and increased crowding in emergency rooms. A previous study indicated the benefit of comparing lateral‐view radiographs in supine and sitting positions to observe the fractured vertebral body height changes. 13 However, obtaining sitting position radiographs can be painful for older adults with AVCFs. 14 For acute pain management, it is recommended to rest in bed, and the head should not be elevated beyond 30°. 15 Because MRI is not always immediately available for emergency patients with suspected AVCFs at our facility, the patients first undergo supine and 30° head‐elevated lateral radiographs. These radiographs often show collapsed vertebral bodies, but no previous studies have clarified whether these 30° head‐elevated lateral radiographs can accurately diagnose AVCFs.
We hypothesized that lateral radiographs of the patient in supine to 30° head ‐elevated position would be diagnostic of vertebral compression fractures.
In this study, we aimed to clarify the diagnostic accuracy of lateral‐view radiograph in a 30° head‐elevated position for AVCFs and explore its potential as an alternative to radiographs in the supine and sitting position.
MATERIALS AND METHODS
Study design and setting
We conducted a single‐center, retrospective pilot observational study in accordance with the principles of Declaration of Helsinki, after obtaining approval from the Ethics Review Committee of Minaminara General Medical Center (date of approval: October 2, 2019; approval number: 37). The need for informed consent was waived by the institutional board because of the retrospective nature of the study.
Participant selection
We included 30 consecutive patients (32 vertebrae) with AVCFs (classified as type A1 of AO) 16 who were transported to our emergency department by ambulance between June 2018 and May 2019. The inclusion criteria were: (1) ages 50 years or older, (2) acute low back pain complaints, and (3) stable vital signs. Patients with fever were excluded to omit possible vertebritis. We excluded high‐energy trauma cases, vertebral fractures other than A1 type of AO classification, and diffuse idiopathic skeletal hyperostosis (DISH) cases.
Diagnostic procedures
All patients with suspected AVCFs first underwent radiological examinations. For patients with difficulty in standing or sitting because of severe back pain, radiological examinations were routinely performed with 30° head‐elevation (i.e., the patient's head was raised by 30° according to a scale on a stretcher when the radiographs were taken in lateral view only). The radiographs were taken centering on the thoracolumbar junction without changing the positions of tube or cassette. Later, patients underwent MRI examination if they had no contraindications. The final diagnosis was based on the MRI results provided by the radiologists. T1‐weighted and T2‐weighted fat suppression images were used to interpret the MRI findings.
Measurements
The height of the vertebral body with AVCFs has been reported to decrease because of weight bearing positions. 15 , 17 To quantify the change in the fractured vertebral body from supine to 30° head‐elevated position, we calculated the change in wedging ratio (WR) from supine to 30° head‐elevated position (Δ WR). Δ WR was obtained using the following formula.
Two examiners (K.T. and T.U.) manually measured the leading edge (a) and the trailing edge (b) of the vertebral body in the supine position, along with the leading edge (c) and trailing edge (d) of the vertebral body at the 30° head‐elevated position (Figure 1) to calculate Δ WR. To minimize possible information bias, inter‐ and intraobserver reliability for Δ WR measurements were assessed. For the intraobserver reliability, the measurements were repeated 3 months later.
FIGURE 1.
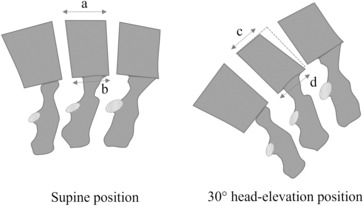
Measurement of Δ wedging ratio in supine and 30° head‐elevated positions. Δ wedging ratio = wedging ratio (30° head‐elevated) − wedging ratio (supine) = (a–b)/a × 100–(c–d)/c × 100 (%). (a) leading edge in supine position; (b) trailing edge in supine position; (c) leading edge at 30° head‐elevated position; (d) trailing edge at 30° head‐elevated position.
Vertebrae without fractures were assessed using MRI and used as the control group.
Statistical analysis
Consecutive numbers were described as median, interquartile range, minimum, and maximum values. Categorical variables were described as numbers (%).
Statistical comparisons were performed using Mann–Whitney U test. Inter‐ and intraobserver reliabilities are reported using the interclass correlation coefficient (ICC). All analyses were performed using Easy R software (Auckland University, Auckland, New Zealand). 18 Statistical significance was set at p < 0.05.
RESULTS
Table 1 shows the characteristics of all the study participants. The median age of the participants was 83 years (interquartile range, 56–92 years), and most of the participants were females (n = 22, 73.3%). Only four patients had known previous history of compression fractures (13.3%). Four patients (13.3%) were on medications for osteoporosis. The mechanisms of injury included: falling on their buttocks (n = 16, 53.3%), hitting their backs (n = 3, 10%), lifting heavy objects (n = 3, 10%), coughing (n = 1, 3.3%), twisting their waist (n = 1, 3.3%), and standing up (n = 1, 3.3%). Five patients (16.7%) had no memory of the exact mechanism. All 30 patients underwent lateral view radiography in a 30° head‐elevated position and MRI scanning; and were diagnosed with new vertebral compression fractures. None of the patients complained of low back pain while taking the lateral view radiographs. Two patients had two fractures each. Lateral view of L5 with a 30° head‐elevated position could not be obtained in six patients. Therefore, we evaluated Δ WR of 32 fractured vertebral bodies and 144 unfractured vertebrae. A statistically significant decrease (p < 0.01) in the Δ WR for new vertebral compression fractures was observed (Figure 2).
TABLE 1.
Patient characteristics.
| Variables | Study patients (N = 30) | |
|---|---|---|
| Patient demographics | ||
| Age (years), median (IQR) | 83 | (56–92) |
| Sex (male), n (%) | 8 | (26.7) |
| Known history of compression fracture, n (%) | 4 | (13.3) |
| Medications history of osteoporosis, n (%) | 4 | (13.3) |
| Mechanism of injury, n (%) | ||
| Fall on their bottom, n (%) | 16 | (53.3) |
| Hit their back, n (%) | 3 | (10) |
| Lifting heavy objects, n (%) | 3 | (10) |
| Cough, n (%) | 1 | (3.3) |
| Twist their waist, n (%) | 1 | (3.3) |
| No particular cause, n (%) | 5 | (16.7) |
Abbreviation: IQR; interquartile range.
FIGURE 2.
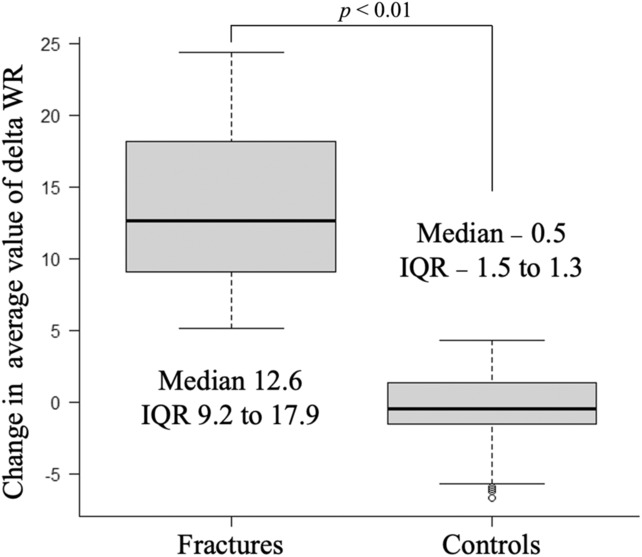
Comparison of wedging ratio between control and fracture images. This analysis shows a significant difference between the controls and fractures. IQR, interquartile range; WR, wedging ratio.
Measurement of the leading edge of fractured vertebrae ranged between 14.1 and 37.8 mm in supine positioned radiograph, whereas in the 30° head‐elevated position, it ranged between 10.0 and 32.7 mm. The median change in the leading edge was 3.6 mm (interquartile range, 2.7–5.8). The leading edge of unfractured vertebrae remained the same between supine and 30° head‐elevated positions (Tables S1 and S2).
Agreement of Δ WR values measured by two investigators was excellent with interobserver reliability of 0.90. Intraobserver reliability was also excellent and good, with values of 0.91 and 0.88, respectively. The median Δ WR of fractured vertebrae was 12.6% with interquartile range of 9.2% to 17.9% (minimum, 5.1%; maximum, 24.4%), which was significantly higher than that of non‐fractured vertebrae (median of −0.5%, interquartile range, −1.5% to 1.7%; minimum, −6.7% and maximum, 4.3%, p < 0.001) (Table 2).
TABLE 2.
Comparison of Δ wedging ratio between new fractures and no fractures.
| No. of new fractures | 32 | |
| Δ wedging ratio, median (IQR) | 12.6 | (9.2–17.9) |
| Over 5.1%, n | 32 | |
| Under 5.1%, n | 0 | |
| No. of no fractures | 144 | |
| Δ wedging ratio, median (IQR) | −0.5 | (−1.5 to 1.3) |
| Over 5.1%, n | 0 | |
| Under 5.1%, n | 144 |
Abbreviation: IQR; interquartile range.
DISCUSSION
This study showed that Δ WR of fractured vertebras was significantly higher compared to non‐fractured vertebrae when lateral radiographs in supine and 30° head‐elevated positions were compared. The Δ WR of fractured vertebrae was ≥5.1%.
A previous study investigated the efficacy of dynamic radiographs for diagnosing osteoporotic AVCFs in comparison to supine radiographs or sitting radiographs alone. The authors reported that evaluating the mobility of acute AVCFs in both supine and sitting positions was superior to using radiographs in either the supine or sitting position alone. They concluded that dynamic radiographs provided a convenient way to identify AVCFs. 15 This study showed that the mobility of fractured vertebrae could be identified using significant value of Δ WR in comparison to lateral X‐ray view in supine to 30° head‐elevated positions and not in sitting or standing position that can aggravate lower back pain.
Fractured vertebrae are known to be mobile 19 and painful. 20 It has been reported that the average vertebral body height changes from supine to sitting position is ~9.0 mm. 19 , 20 Studies have reported that vertebral mobility of ≥2 mm from supine to sitting position showed sensitivity of 84% to 87% and specificity of 53%. 13 , 19
The measured vertebral height values, however, can have some inaccuracies between examiners; and it is troublesome to fix the measuring points on lateral views. Radiological conditions (i.e., tube and object‐to‐file distances) may also interfere with the measurements. To minimize these possible errors, we measured the difference of WR (Δ WR) to assess vertebral mobility. WR is the ratio of the vertebral leading edge to tailing edge, which can omit the need for fixing the measurement points. 20 Δ WR has been associated with severe pain assessed by the Visual Analogue Scale and is commonly used as an index for changes in vertebral body height and symptom improvement after vertebroplasty. 20 , 21
According to a study that evaluated the values of Δ WR among 77 preoperative patients with AVCF, the average of Δ WR among patients with a value of 2.5% or more (the study considered <2.5% was no mobility) was reported to be 9.9%. 21 However, no study has reported the cutoff or minimum values of Δ WR for AVCFs. The median height change of fractured vertebrae in our study participants was 3.6 mm, which was lower than the abovementioned reports. 19 , 21 However, the Δ WR from supine to 30° head‐elevated position ranged between 5.1% to 24.4%, whereas that of unfractured vertebrae was ≤4.3%, which was comparable to the previous report. 21
A previous report supports that comparing lateral radiographic views from supine to sitting positions can be useful diagnosing of AVCFs. 13 However, the majority of emergency transported patients with suspected AVCFs complain of severe pain, 22 are often immobile, and unable to sit or stand. In this study, none of the patients complained of pain exacerbation during 30° head‐elevated positioning. This finding indicates that this radiological evaluation would be easy to use in AVCFs patients complaining of severe back pain.
Lower back pain accounts for a significant proportion of emergency room visits, and this trend is on the rise. 23 , 24 Patients with vertebral compression fractures tend to stay longer in the emergency room because of difficulty in sitting and waiting, and this has been found to be even more prolonged among the older adult patients. 22 , 23 Our proposed method provides a simple and accurate diagnosis of vertebral compression fractures by using two lateral radiographs and could contribute to alleviating crowded emergency departments.
In addition to the substantial strengths of this study, we acknowledge a few limitations. First, this was a single‐center, retrospective observational study. Further studies with larger sample sizes are required to validate the value of Δ WR for generalizability. Additionally, sensitivity and specificity studies blinded with the MRI results are also needed. Second, all the study participants were transported to our emergency center by ambulance and were unable to sit because of severe back pain. Therefore, the severity and mobility of the fractured vertebrae among our study participants were likely to be greater compared to patients with AVCFs in previous reports. Third, none of the patients reported aggravated lower back pain during 30° head‐elevated positioning; however, pain during this procedure was not assessed using any pain scale. Additionally, we treated unfractured vertebrae as controls. A prospective study comparing patients with AVCF with healthy volunteers may be required. Finally, we must consider the potential information bias in this study. Although the two examiners were unaware of which vertebrae had AVCF when measuring Δ WR, they knew that the study participants had ACVF. To minimize this bias, we conducted both interobserver and intraobserver reliability for Δ WR measurements, which showed good to excellent ICCs. Nonetheless, it is still necessary to consider this potential bias when interpreting the study results.
CONCLUSIONS
Comparison of lateral radiographs in supine and 30° head‐elevated positions can provide accurately diagnose AVCF, without aggravating lower back pain. This study showed a Δ WR value of ≥5.1% for AVCFs.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Review Committee of Minaminara General Medical Center (date of approval: October 2, 2019/approval number: 37).
Informed consent: The participants were provided with the opportunity to opt‐out. None of the patients refused to participate.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Supporting information
Table S1
Table S2
Tsuruta K, Ueyama T, Watanabe T, Kobata Y, Nakano K, Fukushima H. A novel radiological assessment to identify acute vertebral compression fractures: A pilot observational study. Acute Med Surg. 2023;10:e891. 10.1002/ams2.891
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this published article.
REFERENCES
- 1. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. [DOI] [PubMed] [Google Scholar]
- 2. Diacinti D, Guglielmi G. How to define an osteoporotic vertebral fracture? Quant Imaging Med Surg. 2019;9:1485–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Old JL, Calvert M. Vertebral compression fractures in the elderly. Am Fam Physician. 2004;69:111–116. [PubMed] [Google Scholar]
- 4. Siminoski K, Lee KC, Jen H, et al. Anatomical distribution of vertebral fractures: comparison of pediatric and adult spines. Osteoporos Int. 2012;23:1999–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee YW, Jang JH, Kim JJ, Lim YS, Hyun SY, Yang HJ. The value of X‐ray compared with magnetic resonance imaging in the diagnosis of traumatic vertebral fractures. J Trauma Injury. 2017;30:158–165. [Google Scholar]
- 6. Lenski M, Büser N, Scherer M. Concomitant and previous osteoporotic vertebral fractures. Acta Orthop. 2017;88:192–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bernhard P, Aleksander K, Andreas MW, et al. Vertebral compression fractures: third‐generation dual‐energy CT for detection of bone marrow edema at visual and quantitative analyses. Radiology. 2017;284:161–168. [DOI] [PubMed] [Google Scholar]
- 8. Expert Panels on Neurological Imaging, Interventional Radiology, and Musculoskeletal Imaging , Shah LM, Jennings JW, et al. ACR appropriateness criteria® management of vertebral compression fractures. J Am Coll Radiol. 2018;15:S347–S364. [DOI] [PubMed] [Google Scholar]
- 9. Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, et al. Vertebral fracture and cause‐specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow‐up. Eur Spine J. 2011;20:2181–2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hida T, Shimokata H, Sakai Y, Ito S, Matsui Y, Takemura M, et al. Sarcopenia and sarcopenic leg as potential risk factors for acute osteoporotic vertebral fracture among older women. Eur Spine J. 2016;25:3424–3431. [DOI] [PubMed] [Google Scholar]
- 11. Toyoda K. The diagnostic value of percussion pain on spinal process for osteoporotic vertebral fracture. J Jpn Soc Lumbar Spine Disord. 2006;12:127–1299. [Google Scholar]
- 12. Dewey M, Schink T, Dewey CF. Claustrophobia during magnetic resonance imaging: cohort study in over 55,000 patients. J Magn Reason Imaging. 2007;26:1322–1327. [DOI] [PubMed] [Google Scholar]
- 13. Niimi R, Kono T, Nishihara A, Hasegawa M, Matsumine A, Kono T, et al. Efficacy of the dynamic radiographs for diagnosing acute osteoporotic vertebral fractures. Osteoporos Int. 2014;25:605–612. [DOI] [PubMed] [Google Scholar]
- 14. Wong CC, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013;6:205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rapado A. General management of vertebral fractures. Bone. 1996;18:191S–196S. [DOI] [PubMed] [Google Scholar]
- 16. Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, et al. AO spine thoracolumbar spine injury classification system. Fracture description, neurological status, and key modifiers. Spine. 2013;38:2028–2037. [DOI] [PubMed] [Google Scholar]
- 17. Bae IS, Moon BG, Kang HI, Kim JH, Jwa C, Kim DR. Difference in the cobb angle between standing and supine position as a prognostic factor after vertebral augmentation in osteoporotic vertebral compression fractures. Neurospine. 2022;19:357–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kanda Y. Investigation of the freely available easy‐to‐use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen YJ, Lo DF, Chang CH, Chen HT, Hsu HC. The value of dynamic radiographs in diagnosing painful vertebrae in osteoporotic compression fractures. AJNR Am J Neuroradiol. 2011;32:121–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Toyone T, Tanaka T, Wada Y, et al. Changes in vertebral wedging rate between supine and standing position and its association with back pain. Spine. 2006;31:2963–2966. [DOI] [PubMed] [Google Scholar]
- 21. Qian L, Pan J, Liu ZD, Li LJ, Tan J, Cheng LM, et al. The correlation between vertebral wedge‐shaped changes in X‐ray imaging at supine and standing positions and the efficacy of operative treatment of thoracolumbar spinal fracture in the elderly. Spinal Cord. 2013;51:904–908. [DOI] [PubMed] [Google Scholar]
- 22. Federico L, Andrew MK, Ogilvie R, Wilson M, Magee K, Hayden JA. Low back pain in a Nova Scotian emergency department: prevalence and patient characteristics in the older adult patient population. Can J Aging. 2021;41:145–153. [DOI] [PubMed] [Google Scholar]
- 23. Edwards J, Hayden J, Asbridge M, Magee K. The prevalence of low back pain in the emergency departments: a descriptive study set in the Charles V. Keating emergency and trauma center Halifax, Nova Scotia, Canada. BMC Musculoskelet Disord. 2018;19:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Capsey M, Ryan C, Alexanders J, Martin D. Ambulance service use by patients with lower back pain: an observational study. Br Paramed J. 2022;6:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Table S2
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


