Abstract
Background
To compare the survival rates of four timing of treatment initiation for people living with HIV/AIDS provided in China in 2006, 2011, 2015, and 2018, and to investigate the factors impacting survival time.
Methods
A people living with HIV/AIDS retrospective cohort study was in Liuzhou City from April 2006 to December 2020. The information was obtained from the National Comprehensive AIDS Prevention and Control Information System. Life tables and the Kaplan–Meier method were used to calculate participant survival rates and time. The univariate and multivariate Cox regression models were used to investigate the factors related to survival.
Results
18,543 participants were included in this study. In four periods, the 1-year survival rates were 81%, 87%, 95%, and 95%. The 2-year survival rates were 76%, 85%, 93%, and 94%. The 3-year survival rates were 73%, 84%, 92%, and 94%. Results of multivariate Cox regression showed that sex, age of HIV diagnosis, ethnicity, household registration, occupation, marital status, the timing of treatment, education level, route of HIV transmission, whether receiving antiretroviral therapy (ART), and the count of CD4+T cells at baseline (count of CD4+T cells at HIV diagnosis) were factors that are significantly correlated with mortality caused by HIV infection.
Conclusions
With the Guidelines updated from 2006 to 2020, the 1-, 2-, and 3-year survival rates of people living with HIV/AIDS in four periods tended to increase. The timing of treatment initiation of the updated edition of the AIDS Diagnostic and Treatment Guidelines (Guidelines) significantly prolonged the survival time of people living with HIV/AIDS.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15662-3.
Keywords: Antiretroviral therapy, Survival time, Cox regression model, People living with HIV/AIDS, Influencing factors
Background
Acquired immune deficiency syndrome (AIDS), a major infectious disease, is caused by the human immunodeficiency virus (HIV).Which seriously affects the physical and mental health of humans [1]. In 2019, there were 1.7 million newly diagnosed HIV infections, 690,000 HIV-related deaths and 38 million people living with HIV/AIDS globally [2].
The development of antiretroviral therapy (ART) is one of the most significant achievements of modern medicine, slowing the progression of AIDS and reducing AIDS-related mortality [3, 4]. Since the "Four Free and One Care" policy was issued in China from 2003, Chinese government provided free antiretroviral medication to all people living with HIV/AIDS diagnosed. The "Four Free and One Care" policy includes: free ART, free voluntary counseling and testing, free schooling, and reduction of mother-to-child transmission. As a result, an increasing number of people living with HIV/AIDS are taking antiretroviral drugs [5].
ART has greatly improved the life expectancy and the quality of life for people living with HIV/AIDS [6, 7]. The best time to start ART in people living with HIV/AIDS varies between countries. In the latest Guidelines of America [8, 9], ART is advised for all newly infected individuals regardless their count of CD4+T cells at diagnosis. The World Health Organization (WHO) recommends that ART should be initiated when the count of CD4+T cells is less than 500 cells/mm3 in people living with HIV/AIDS [8]. In Europe, ART is recommended when the CD4+T cells count in RPWHA is less than 350 cells/mm3 and should be considered for individuals with CD4+T cells count of 350–500 cells/mm3 [10]. To date, four editions of the AIDS Diagnostic and Treatment Guidelines (Guidelines) have been issued in China, and the timing of starting ART treatment for people living with HIV/AIDS changed as the Guidelines were updated. In April 2006, China published the first edition of the Guidelines, ART is recommended when the CD4+T cells count is less than 200 cells/mm3 in HIV-positive asymptomatic people [11]. According to the second edition Guidelines, issued in October 2011, ART started when the counts of CD4+ T cells was less than 350 cells/mm3 [12]. The third edition Guidelines, issued in October 2015, recommended that ART should be initiated when the count of CD4+T cells is less than 500 cells/mm3 in people living with HIV/AIDS [13]. The latest Guidelines, published in December 2018, suggested no matter their count of CD4+T cells at baseline, all people living with HIV/AIDS should receive ART [14]. According to the publication dates of different editions of the Guidelines, the time from April 2006 to December 2020 was divided into four periods. Period one: April 2006-September 2011. Period two: October 2011-September 2015. Period three: October 2015-November 2018. Period four: December 2018-December 2020. It is critical to compare the survival times and factors related survival of people living with HIV/AIDS in different Guidelines in order to make clinical decisions and plan health service interventions [15].
HIV infection has created a significant global disease burden [16]. In China, there were 1.053 million people living with HIV/AIDS and 351,000 people died from HIV infection in 2020 [17]. Guangxi, located in the southern border region of China, has the second-largest population of people living with HIV/AIDS in South-Central China [18]. From 2010 to 2020, there were about 10,000 newly diagnosed HIV infections and 5,000 AIDS-related fatalities each year in Guangxi, ranking first in the morbidity and mortality rate of HIV in China [19, 20]. Liuzhou, in Guangxi Province, has the highest rate of HIV infection [21].
This study compared survival rates and investigated the influential factors of the people living with HIV/AIDS in different treatment indications, and provided evidence on prolonging the life span and improving the physical and mental health of the people living with HIV/AIDS.
Methods
Study populations
Participants were chosen based on the following factors: (1) Above 18 years old; (2) whose current address was "Liuzhou City, Guangxi Province" in the National Integrated AIDS Control Information System; (3) Confirmed HIV-infected or AIDS patient; (4) With a clear start date of antiviral treatment; (5) Deaths in the National Integrated AIDS Control Information System are AIDS-related deaths.
Study design
A retrospective cohort study was conducted in Liuzhou. All information on HIV infectors aged 18 years old and above confirmed between 2006 and 2020 was extracted from National Integrated AIDS Control Information System. Data were reported to the Disease Control Department (CDC) by doctors with the consent of the patient. The CD4+ T cells count is the CD4+ T cells count at the time of the initial diagnosis, and for patients missing the initial CD4+ T cells count, we used the earliest primary CD4+ T cells count instead. The starting point of the study was the day participants were confirmed infected with HIV. The cohort follow-up deadline was December 31, 2020. The time from HIV diagnosis to death is defined as survival time, and the outcome variable was the death of the participant.
Statistical analysis
For statistical analysis, IBM SPSS software, version 23.0, was utilized. Life tables and the Kaplan–Meier were used to calculated survival rates and the average survival time. Log-rank test was used to compare the survival rates of the four periods. The Mann–Whitney U test or the Chi-Square test for trend was performed to identify differences among the four groups. If univariate analysis revealed differences of more than 0.05, multivariate COX regression analysis was performed. P < 0.05 was used as the significance level.
Results
General demographic characteristics of people living with HIV/AIDS in Liuzhou City during different periods from 2006 to 2020
18,543 individuals were included in this study, 5,890(31.76%), 6,062(32.69%), 3,226(17.40%), and 3,365(18.15%) HIV infectors were confirmed in four periods, respectively. In this study, the majority of people living with HIV/AIDS were male (69.64%) and Chinese-Han (54.76%), nearly 57.64% of participants were aged 31–60, and heterosexual behavior is the principal route of HIV transmission (87.82%). From 2006 to 2020, the main household registration of people living with HIV/AIDS was Liunan District (46.35%), over half (56.96%) were married, and 58.94% of participants were farmers. The majority education level of them was Junior high school or less. In period one, the count of CD4+T cells of most patients was greater than 500/mm3 (22.99%). In period two and period four, many patients had the count of CD4+T cells of less than 200/ mm3 (24.30% and 36.20%, respectively). In period three, most of the patients had the count of CD4+T cells of 200–350/ mm3 (26.44%). Most patients in four periods received ART, accounting for 66.72%, 73.39%, 81.06%, and 77.12%, respectively. (Table 1).
Table 1.
General demographic characteristics of people living with HIV/AIDS in Liuzhou City during different periods, 2006–2020
| Covariate | 2006–2020 (N%) | Period one (N%) | Period two (N%) | Period three (N%) | Period four (N%) | P-value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female | 5,630 (30.36) | 1,998 (33.92) | 1,796 (29.63) | 894 (27.71) | 942 (27.99) | < 0.001 |
| Male | 12,913 (69.64) | 3,892 (66.08) | 4,266 (70.37) | 2,332 (72.29) | 2,423 (72.01) | |
| Age of diagnosis, y | ||||||
| ≤ 30 | 3,347 (18.05) | 1,717 (29.15) | 928 (15.31) | 410 (12.71) | 292 (8.68) | < 0.001 |
| 31 ~ 60 | 10,688 (57.64) | 3,422 (58.10) | 3,575 (58.97) | 1,900 (58.90) | 1,791 (53.22) | |
| ≥ 61 | 4,508 (24.31) | 751 (12.75) | 1,559 (25.72) | 916 (28.39) | 1,282 (38.10) | |
| Household registration | ||||||
| Liunan District | 8,595 (46.40) | 2,427 (41.20) | 3,198 (52.80) | 1,456 (45.10) | 1,514 (45.00) | |
| Other districts in Liuzhou | 8,074 (43.50) | 2,621 (44.50) | 2,356 (38.90) | 1,493 (46.30) | 1,604 (47.70) | < 0.001 |
| Others | 1,874 (10.10) | 842 (14.30) | 508 (8.40) | 277 (8.60) | 247 (7.30) | |
| Occupation | ||||||
| Housekeeping | 3,516 (18.96) | 1,360 (23.09) | 963 (15.89) | 611 (19.94) | 582 (17.30) | 0.309 |
| Farmer | 10,928 (58.94) | 2,957 (50.20) | 3,922 (64.70) | 1,911 (59.24) | 2,138 (63.54) | |
| Laborer | 778 (4.20) | 299 (5.08) | 225 (3.71) | 162 (5.02) | 92 (2.73) | |
| Business Service Provider | 1,054 (5.68) | 240 (4.07) | 149 (2.46) | 90 (2.79) | 98 (2.90) | |
| Retirees | 1,690 (9.11) | 279 (4.74) | 351 (5.79) | 198 (6.14) | 226 (6.72) | |
| Others | 577 (3.11) | 755 (12.82) | 452 (7.46) | 254 (7.87) | 229 (6.81) | |
| Marital status | ||||||
| Unmarried | 4,350 (23.46) | 1,468 (24.92) | 3,330 (21.94) | 775 (24.02) | 777 (23.09) | < 0.001 |
| Married | 10,563 (56.96) | 3,559 (60.42) | 3,523 (58.12) | 1,753 (54.34) | 1,728 (51.35) | |
| Widowed/Divorced | 3,630 (19.58) | 863 (14.66) | 1,209 (19.94) | 698 (21.64) | 860 (25.56) | |
| Ethnicity | ||||||
| Han | 10,153 (54.76) | 3,422 (58.10) | 3,398 (56.05) | 1,667 (51.67) | 1,666 (49.51) | < 0.001 |
| Zhuang | 7,169 (38.66) | 2,223 (37.74) | 2,292 (37.81) | 1,287 (39.90) | 1,367 (40.62) | |
| Others | 1,221 (6.58) | 245 (4.16) | 372 (6.14) | 272 (8.43) | 332 (9.87) | |
| Educational level | ||||||
| Primary or below | 8,384 (45.21) | 2,339 (39.71) | 2,772 (45.73) | 1,507 (46.71) | 1,766 (52.48) | < 0.001 |
| Junior high school | 7,563 (40.79) | 2,741 (46.54) | 2,519 (41.55) | 1,217 (37.72) | 1,086 (32.27) | |
| Senior high school | 1,854 (10.00) | 665 (11.29) | 559 (9.22) | 319 (9.89) | 311 (9.24) | |
| College or above | 742 (4.00) | 145 (2.46) | 212 (3.50) | 183 (5.68) | 202 (6.01) | |
| Route of HIV transmission | ||||||
| Heterosexual behavior | 16,284 (87.82) | 4,527 (76.86) | 5,692 (93.90) | 2,935 (90.98) | 3,130 (93.02) | < 0.001 |
| Homosexual behavior | 523 (2.82) | 29 (0.49) | 115 (1.90) | 194 (6.01) | 185 (5.50) | |
| Injecting drug use | 1,233 (6.65) | 961 (16.32) | 175 (2.89) | 70 (2.17) | 27 (0.80) | |
| Others | 503 (2.71) | 373 (6.33) | 80 (1.32) | 27 (0.84) | 23 (0.68) | |
| Counts of CD4+ T cells (cells⁄mm 3) | ||||||
| Not Tested | 2,268 (12.23) | 1,065 (18.08) | 695 (11.46) | 188 (5.83) | 320 (9.51) | < 0.001 |
| ≤ 200 | 4,816 (25.97) | 1,332 (22.61) | 1,473 (24.30) | 793 (24.58) | 1,218 (36.20) | |
| 200 ~ 350 | 4,081 (22.01) | 1,103 (18.73) | 1,325 (21.86) | 853 (26.44) | 800 (23.77) | |
| 350 ~ 500 | 3,354 (18.09) | 1,036 (17.59) | 1,157 (19.09) | 627 (19.44) | 534 (15.87) | |
| > 500 | 4,024 (21.70) | 1,354 (22.99) | 1,412 (23.29) | 765 (23.71) | 493 (14.65) | |
| ART | ||||||
| Yes | 13,589 (73.28) | 3,930 (66.72) | 4,449 (73.39) | 2,615 (81.06) | 2,595 (77.12) | < 0.001 |
| No | 4,954 (26.72) | 1,960 (33.28) | 1,613 (26.61) | 611 (18.94) | 770 (22.88) | |
Data outside of parentheses are the number of cases, and data in parentheses are the composition ratio (%)
High-risk behaviors for HIV infection
With the Guidelines updated, the percentage of people having high-risk behavior changed. The proportion of patients having a history of injecting drugs tended to decline (Trend χ 2 = 911.272, P < 0.001). The percentage of patients with non-commercial sexuality has been increasing (Trend χ 2 = 3,855.978, P < 0.001). The rate of people living with HIV/AIDS with a history of commercial sexuality tended to increase (Trend χ 2 = 4,198.971, P < 0.001). The decreasing proportion of people living with HIV/AIDS whose mothers were HIV-positive (Trend χ 2 = 31.087, P < 0.001). Men who have sex with men (MSM) were becoming more prevalent. (Trend χ 2 = 285.489, P < 0.001). The rate of people living with HIV/AIDS who has a positive spouse/regular sex partner tended to decrease (Trend χ 2 = 53.615, P < 0.001). People living with HIV/AIDS with a history of surgery or blood donation showed a decreasing trend (Trend χ 2 = 42.881, P < 0.001). There was a decreasing trend in the proportion of patients with other exposure histories. (Trend χ 2 = 107.783, P < 0.001). (Table 2).
Table 2.
Description of high-risk exposure history for people living with HIV/AIDS in Liuzhou City, 2006–2020
| Covariate | Groupe | χ 2 test for trend | P-value for Trend | |||
|---|---|---|---|---|---|---|
| period one (N%) | period two (N%) | period three (N%) | period four (N%) | |||
| History of injecting drug use | ||||||
| No | 4,904 (83.26) | 5,869 (96.82) | 3,155 (97.80) | 3,331 (98.99) | 911.272 | < 0.001 |
| Yes | 986 (16.74) | 193 (3.18) | 71 (2.20) | 34 (1.01) | ||
| History of non-commercial sexuality | ||||||
| No | 5,778 (98.10) | 5,969 (98.47) | 2,119 (65.69) | 1,941 (57.68) | 3,855.978 | < 0.001 |
| Yes | 112 (1.90) | 93 (1.53) | 1,107 (34.31) | 1,424 (42.32) | ||
| History of commercial sexuality | ||||||
| No | 5,727 (97.23) | 5,970 (98.48) | 1,613 (50.00) | 1,889 (56.14) | 4,198.971 | < 0.001 |
| Yes | 163 (2.77) | 92 (1.52) | 1,613 (50.00) | 1,476 (43.86) | ||
| Mother was HIV positive | ||||||
| No | 5,816 (98.74) | 6,032 (99.51) | 3,208 (99.44) | 3,357 (99.76) | 31.087 | < 0.001 |
| Yes | 74 (1.26) | 30 (0.49) | 18 (0.56) | 8 (0.24) | ||
| MSM | ||||||
| No | 5,855 (99.41) | 5,942 (98.02) | 3,032 (93.99) | 3,177 (94.41) | 285.489 | < 0.001 |
| Yes | 35 (0.59) | 120 (1.98) | 194 (6.01) | 188 (5.59) | ||
| Positive spouse/regular sex partner | ||||||
| No | 5,012 (85.09) | 5,235 (86.36) | 2,882 (89.34) | 3,016 (89.63) | 53.615 | < 0.001 |
| Yes | 878 (14.91) | 827 (13.64) | 344 (10.66) | 349 (10.37) | ||
| History of surgery or blood donation | ||||||
| No | 5,808 (98.61) | 6,022 (99.34) | 3,213 (99.60) | 3,357 (99.76) | 42.881 | < 0.001 |
| Yes | 82 (1.39) | 40 (0.66) | 13 (0.40) | 8 (0.24) | ||
| History of other exposures | ||||||
| No | 5,752 (97.66) | 6,036 (99.57) | 3,215 (99.70) | 3,357 (99.76) | 107.783 | < 0.001 |
| Yes | 138 (2.34) | 26 (0.43) | 11 (0.34) | 8 (0.24) | ||
The survival rate of people living with HIV/AIDS in Liuzhou City from 2006 to 2020
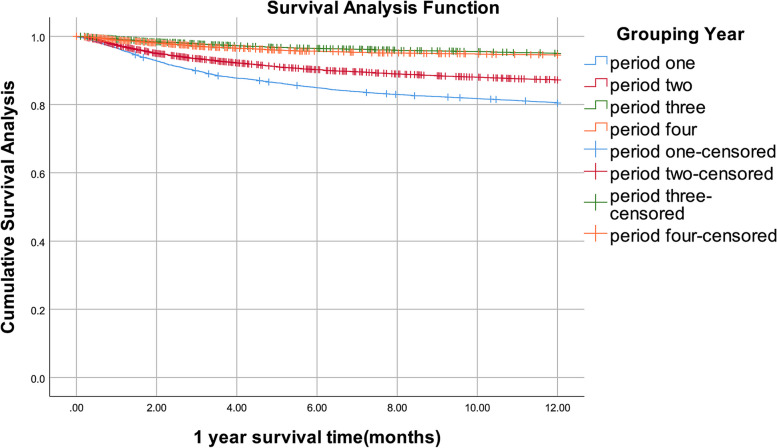
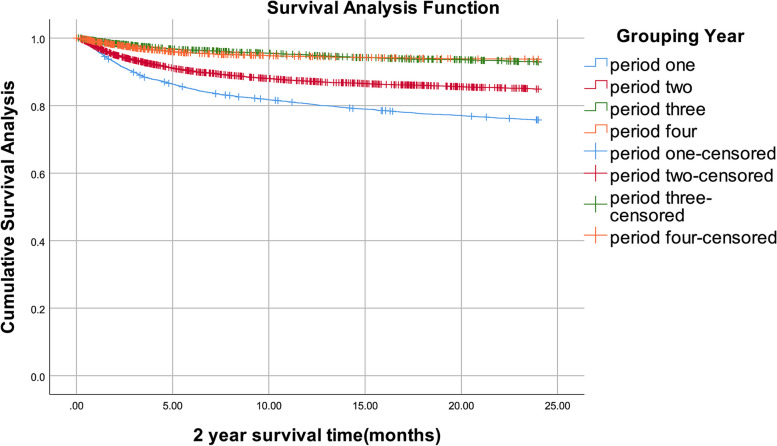
By December 31, 2020, of 18,543 people living with HIV/AIDS, 3,813 people had died. In four periods, 1-year survival rates were 81%, 87%, 95%, and 95%, respectively, 2-year survival rates were 76%, 85%, 93%, and 94%, 3-year survival rates were 73%, 84%, 92%, and 94%, respectively (Table 3). The survival curves demonstrated that the 1-, 2-, and 3-year survival rates all showed increasing trends. For infected patients with ART, in four periods, 1-year survival rates were 75%, 88%, 92%, and 98%, respectively, 2-year survival rates were 83%, 92%, 91%, and 100%, 3-year survival rates were 99%, 99%, 100%, and 100%, respectively. For infected patients no ART, in four periods, 1-year survival rates were 98%, 97%, 99%, and 98%, respectively, 2-year survival rates were 99%, 99%, 99%, and 99%, 3-year survival rates were 100%, 100%, 100%, and 100%, respectively (Supplementary Table 1). After log-rank test, the differences between groups were statistically significant in all four periods with ART, and also in no ART. (all P < 0.05). (Supplementary Table 2) The Kaplan–Meier method was used to assess the impact of four timing of treatment initiation on the people living with HIV/AIDS's survival time. In four periods, there were notable variations in 1-year survival rates. (P < 0.001). (Fig. 1). Similarly, the 2-year survival rates differed markedly between four periods. (P < 0.001). (Fig. 2). The 3-year survival rates in four periods varied dramatically. (P < 0.001). (Fig. 3). The timing of treatment for patients in period three and period four had a higher possibility of survival, suggesting the timing of treatment initiation of Guidelines (2018) and Guidelines (2015) significantly prolonged the survival time of patients.
Table 3.
People living with HIV/AIDS survival rate in Liuzhou City, 2006–2020
| Year | Time since diagnosis (months) | Number of Observers | Number of missed visits | Number of deaths | Mortality | Survival rate | Cumulative survival rate | Cumulative survival standard error |
|---|---|---|---|---|---|---|---|---|
| period one | 0 | 5,890 | 17 | 1,143 | 0.19 | 0.81 | 0. 81 | 0.01 |
| 12 | 4,730 | 14 | 281 | 0.06 | 0. 94 | 0.76 | 0.01 | |
| 24 | 4,435 | 16 | 162 | 0.04 | 0. 96 | 0.73 | 0.01 | |
| 36 | 4,257 | 3,752 | 505 | 0.21 | 0. 79 | 0.58 | 0.01 | |
| period two | 0 | 6,062 | 296 | 755 | 0.13 | 0. 87 | 0.87 | 0 |
| 12 | 5,011 | 172 | 134 | 0.03 | 0. 97 | 0.85 | 0 | |
| 24 | 4,705 | 145 | 65 | 0.01 | 0.99 | 0.84 | 0 | |
| 36 | 4,495 | 4,235 | 260 | 0.11 | 0.89 | 0.75 | 0.01 | |
| period three | 0 | 3,226 | 267 | 153 | 0.05 | 0. 95 | 0.95 | 0 |
| 12 | 2,806 | 99 | 59 | 0.02 | 0.98 | 0.93 | 0 | |
| 24 | 2,648 | 46 | 37 | 0.01 | 0.99 | 0.92 | 0.01 | |
| 36 | 2,565 | 2,515 | 50 | 0.04 | 0.96 | 0.88 | 0.01 | |
| period four | 0 | 3,365 | 247 | 177 | 0.05 | 0.95 | 0.95 | 0 |
| 12 | 2,941 | 34 | 25 | 0.01 | 0.99 | 0.94 | 0 | |
| 24 | 2,882 | 9 | 7 | 0.00 | 1.00 | 0.94 | 0 | |
| 36 | 2,866 | 2,866 | 0 | 0.00 | 1.00 | 0.94 | 0 |
Fig. 1.
1-year survival curves of patients with people living with HIV/AIDS in Liuzhou City with different treatment options from 2006 to 2020
Fig. 2.
2-year survival curves of patients with people living with HIV/AIDS in Liuzhou City with different treatment options, 2006–2020
Fig. 3.
3-year survival curves for patients with people living with HIV/AIDS in Liuzhou City with different treatment options, 2006–2020
Factors influencing survival time
The Cox regression model was utilized to investigate the connection between baseline data and mortality. Factors influencing survival time in people living with HIV/AIDS were sex, age at diagnosis, household registration, the timing of treatment, occupation, marriage status, ethnicity, education level, route of transmission, whether receiving ART, and the count of CD4+T cells at baseline. Mortality risk tended to increase with increasing age at diagnosis. Among household registration, high mortality was seen in Liunan District. A lower degree of education was linked to a higher chance of dying. The survival time was significantly longer for patients in period four. Patients who didn't receive ART have a high mortality rate. Patients with a low count of CD4+ T cells have a higher mortality rate. (Table 4).
Table 4.
Survival time of people living with HIV/AIDS in Liuzhou City, 2006–2020: Univariate and Multivariate Cox Regression
| Covariate | Number of cases(N%) | Univariate cox regression | Multivariate cox regression | ||
|---|---|---|---|---|---|
| P-value | RR value (95% CI) | P-value | RR value (95% CI) | ||
| Sex | |||||
| Female | 5,630 (30.36) | 1.000 | 1.000 | ||
| Male | 12,913 (69.64) | < 0.001 | 1.965(1.815 ~ 2.1276) | < 0.001 | 1.239(1.138 ~ 1.348) |
| Age at diagnosis, y | |||||
| ≤ 30 | 3,347 (18.05) | 1.000 | 1.000 | ||
| 31 ~ 60 | 10,688 (57.64) | < 0.001 | 1.457(1.321 ~ 1.607) | < 0.001 | 1.306(1.175 ~ 1.452) |
| ≥ 61 | 4,508 (24.31) | < 0.001 | 2.449(2.206 ~ 2.719) | < 0.001 | 1.583(1.387 ~ 1.808) |
| Occupation | |||||
| Housekeeping/housework/ standby jobs | 1,360 (23.09) | 1.000 | |||
| Farmer | 2,957 (50.20) | < 0.001 | 1.239(1.135 ~ 1.352) | 0.075 | 1.090(0.991 ~ 1.199) |
| Laborer | 299 (5.08) | 0.267 | 0.899(0.745 ~ 1.085) | 0.157 | 1.148(0.948 ~ 1.391) |
| Business Service Provider | 240 (4.07) | < 0.001 | 2.094(1.837 ~ 2.387) | 0.027 | 1.180(1.019 ~ 1.366) |
| Retirees | 279 (4.74) | 0.085 | 1.121(0.984 ~ 1.278) | 0.914 | 0.993(0.869 ~ 1.134) |
| Others | 755 (12.82) | 0.001 | 0.664(0.522 ~ 0.844) | 0.687 | 0.951(0.744 ~ 1.215) |
| Household registration | |||||
| Liunan District | 8,595 (46.40) | 1.000 | 1.000 | ||
| Other districts in Liuzhou | 8,074 (43.50) | < 0.001 | 1.393(1.238 ~ 1.568) | < 0.001 | 1.461(1.293 ~ 1.650) |
| Others | 1,874 (10.10) | < 0.001 | 1.256(1.115 ~ 1.415) | < 0.001 | 1.340(1.186 ~ 1.515) |
| Timing of treatment | |||||
| Period four | 3,365 (18.15) | 1.000 | |||
| Period three | 3,226 (17.40) | < 0.001 | 1.393(1.167 ~ 1.663) | < 0.001 | 2.334(1.954 ~ 2.789) |
| Period two | 6,062 (32.69) | < 0.001 | 3.045(2.629 ~ 3.528) | < 0.001 | 3.701(3.191 ~ 4.294) |
| Period one | 5,890 (31.76) | < 0.001 | 5.452(4.727 ~ 6.287) | < 0.001 | 5.388(4.649 ~ 6.244) |
| Marital status | |||||
| Unmarried | 4,350 (23.46) | 1.000 | |||
| Married | 10,563 (56.96) | 0.270 | 0.957(0.886 ~ 1.034) | 0.932 | 1.004(0.920 ~ 1.096) |
| Widowed/Divorced | 3,630 (19.58) | 0.152 | 1.073(0.975 ~ 1.181) | 0.867 | 0.965(0.867 ~ 1.074) |
| Ethnicity | |||||
| Han | 10,153 (54.76) | 1.000 | 1.000 | ||
| Zhuang | 7,169 (38.66) | < 0.001 | 0.815(0.762 ~ 0.871) | < 0.001 | 0.881(0.822 ~ 0.944) |
| Others | 1,221 (6.58) | < 0.001 | 0.427(0.356 ~ 0.511) | < 0.001 | 0.642(0.535 ~ 0.771) |
| Educational level | |||||
| College or above | 742 (4.00) | 1.000 | 1.000 | ||
| Junior high school | 1,854 (10.00) | < 0.001 | 2.403(1.785 ~ 3.234) | 0.019 | 1.410(1.059 ~ 1.876) |
| Senior high school | 7,563 (40.79) | < 0.001 | 2.957(2.236 ~ 3.909) | 0.092 | 1.277(0.961 ~ 1.698) |
| Primary or below | 8,384 (45.21) | < 0.001 | 4.132 (3.129 ~ 5.456) | 0.019 | 1.432(1.061 ~ 1.933) |
| Route of transmission | |||||
| Heterosexual | 16,284 (87.82) | 1.000 | 1.000 | ||
| Homosexual | 523 (2.82) | < 0.001 | 0.145(0.089 ~ 0.237) | 0.006 | 0.496(0.300 ~ 0.819) |
| Injecting drug use | 1,233 (6.65) | < 0.001 | 2.187(1.991 ~ 2.403) | 0.109 | 0.915(0.822 ~ 1.020) |
| Others | 503 (2.71) | < 0.001 | 2.448(2.126 ~ 2.819) | < 0.001 | 1.374(1.187 ~ 1.591) |
| ART | |||||
| Yes | 13,589 (73.28) | 1.000 | 1.000 | ||
| No | 4,954 (26.72) | < 0.001 | 15.815(14.689 ~ 17.027) | < 0.001 | 5.987(5.478 ~ 6.543) |
| Count of CD4+ T cells (cells⁄mm 3) | |||||
| Not Tested | 2,268 (12.23) | 1.000 | 1.000 | ||
| ≤ 200 | 4,816 (25.97) | < 0.001 | 0.013(0.011 ~ 0.016) | < 0.001 | 0.832(0.769 ~ 0.899) |
| 200 ~ < 350 | 4,081 (22.01) | < 0.001 | 0.271(0.252 ~ 0.291) | < 0.001 | 0.197(0.173 ~ 0.225) |
| 350 ~ < 500 | 3,354 (18.09) | < 0.001 | 0.046(0.041 ~ 0.051) | < 0.001 | 0.115(0.097 ~ 0.137) |
| > 500 | 4,024 (21.70) | < 0.001 | 0.024(0.028 ~ 0.020) | < 0.001 | 0.070(0.057 ~ 0.087) |
The number of cases was partially missing in the multifactorial analysis
Discussion
Patients in this study with the following characteristics constituted the majority of people living with HIV/AIDS in Liuzhou: male, 31–60 years old, farmer, married, primary school education or less, Han Chinese, heterosexual transmission, receiving ART, CD4+ T cell count below 200/mm3 at baseline, which is consistent with other studies [22, 23]. Notably, the count of CD4+T cells of most patients was less than 200/mm3, which could be owing to patients' late diagnosis. The count of CD4+T cells at baseline is critical for prognosis, as a low count of CD4+T cells at baseline may result in high mortality [24]. We found that the survival rate increased with the Guidelines updated, further suggesting the value of the current Guidelines is better than the previous one, in both ART and no-ART infected patients there were such results. There were many factors impacting on people living with HIV/AIDS's chances of survival. The risk of death was higher in males, consistent with the previous report [25]. Patients with the age of diagnosis of older than 30 years had a higher possibility of death. This may be due to the fact that as people get older, their immune systems weaken, making them more susceptible to disease and increasing their risk of dying. This is consistent with previous studies [26, 27]. Chinese-Han people died at a higher rate than other ethnic groupings. Higher-educated people living with HIV/AIDS had a lower mortality rate, which is in line with the results of studies in Yunnan Province [22].
We found the number of participants decreased by half from period two to three. Firstly, in our manuscript, the duration of period two was 48 months, and the duration of period three was 36 months, so the number of people in period three has been reduced. Secondly, in order to curb the development of AIDS, Guangxi Province implemented the "AIDS alleviation program" from 2010 to 2015 [28], especially the AIDS extended detection was done in the whole Province of Guangxi, so the number of new diagnoses was bigger in period two than period three, this period coincides with the period two in our manuscript. Finally, after expanded HIV testing, almost all existing HIV-infected patients have been diagnosed, so the number of newly diagnosed cases of HIV infection in period three has decreased.
In this manuscript, the CD4+ T cells count was the CD4+ T cells count at the time of HIV confirmed, it was not the CD4+ T cells count when infected persons start ART, and for participants who missing the initial CD4+ T cells count, the earliest primary CD4+ T cells count was used to replace it.
In this manuscript, the CD4+ T cells counts were not getting higher with the guidelines updated, which may related to the proportion of aged (≥ 61 years of age) HIV infected persons were increased in the four periods(trendχ 2 = 759.183, P < 0.001), An article pointed out that [29] the CD4+ T cells counts was lower in older HIV infected persons.
"Homosexual transmission" gave the lowest possibility of death in people living with HIV/AIDS. This may be ascribed to increased knowledge of HIV in MSM, they had more awareness of self-protection. The higher count of the CD4+T cells at baseline, the lower risk of death, which is consistent with the previous report [30]. People living with HIV/AIDS who didn't receive ART were at greater risk of death.
Studies [31–33] have shown that drugs such as methamphetamine and ketamine act on the central nervous system of the human body, producing strong euphoric effects that induce high-risk behavior and increase the spread of AIDS. According to this study, the proportion of patients with a history of intravenous drug use decreased from 2006 to 2020, indicating that HIV-related interventions in Liuzhou City are effective in recent years. However, it still cannot be ignored, and the publicity work on drugs and AIDS should be strengthened.
We observed a gradual increase in the survival rate of 18,543 people living with HIV/AIDS in four periods. According to the result of the univariate Cox regression model, whether receiving ART can impact the survival time of people living with HIV/AIDS, similar findings emerged with the multivariate Cox regression model. The timing of treatment also affected survival, which may be related to the increase in the count of CD4+T cells at baseline in the Guidelines for starting ART. In period one, only people whose count of CD4+T cells at baseline less than 200/mm3 were eligible for ART. Consistent with foreign studies [34, 35], individuals whose count of CD4+T cells at baseline was greater than 200/mm3 perished due to a failure to receive ART on time, this may account for the increased mortality rate [36]. The importance of early initiation of antiretroviral therapy is demonstrated.
In summary, the new Guidelines are better than previous ones. With the Guidelines updated from 2006 to 2020, the 1-, 2-, and 3-year survival rates tended to rise. Numerous elements impacted the people living with HIV/AIDS's survival time, and HIV education should be improved to raise public awareness and decrease the risk of HIV infection. Treatment initiated early, intensively, extensively, and continuously has the best potential to minimize mortality. This study further highlights the importance of early detection, diagnosis, and treatment. Therefore, HIV testing should be intensified so that an early diagnosis can be made.
There are some limitations to this study. Firstly, the data for this manuscript were extracted from National Integrated AIDS Control Information System, more information related to the mortality of HIV infected persons were not collected, such as adherence of ART, substance abuse and dietary habit. Secondly, Liuzhou has a special ethnic agglomeration, so it is difficult to extrapolate this result to other areas.
Supplementary Information
Additional file 1: SupplementaryTable 1. Survival rates of people living with HIV/AIDSwith different treatment status in Liuzhou, 2006-2020. Supplementary Table 2. Comparisonof survival rates of infected patients in four periods with different treatmentstatus in Liuzhou, 2006-2020.
Acknowledgements
Not applicable.
Abbreviations
- AIDS
Acquired immune deficiency syndrome
- ART
Antiretroviral therapy
- HIV
Human immunodeficiency virus
- WHO
World Health Organization
Authors’ contributions
The main manuscript was written by and revised by Susu Ke, and the data preprocessing and analysis were performed by Quan Fang, Jianguo Lan, Nini Qiao, and Xinhong Zhang, under the supervision of Changping Xie and Yinguang Fan The final text has been reviewed and approved by all authors.
Funding
This work was supported by the Key Project of Natural Science Research in Universities of Anhui Province (KJ2020A0151).
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by Anhui Medical University Ethics Committee (Approval number: 20200594). Information was reported to the CDC by doctors after seeking informed consent from patients. All methods of the study were implemented in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Susu Ke and Quan Fang contributed equally to this work.
Changping Xie and Yinguang Fan contributed equally as co-corresponding authors.
Contributor Information
Changping Xie, Email: ping164007@126.com.
Yinguang Fan, Email: fanyinguang@163.com.
References
- 1.Li Y, Zhang XW, Liao B, Liang J, He WJ, Liu J, Yang Y, Zhang YH, Ma T, Wang JY. Social support status and associated factors among people living with HIV/AIDS in Kunming city, China. BMC Public Health. 2021;21(1):1413. doi: 10.1186/s12889-021-11253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. The 2020 Global AIDS Prevention and Control Progress Report was released: the 2020 AIDS goal will not be achieved [EB/OL].(2020–07–20)[2022–11–1]. http://www.unaids.org.cn/page122?article_id=1200.
- 3.Judd A, Chappell E, Turkova A, Le Coeur S, Noguera-Julian A, Goetghebuer T, Doerholt K, Galli L, Pajkrt D, Marquess L, et al. Long-term trends in mortality and AIDS-defining events after combination ART initiation among children and adolescents with perinatal HIV infection in 17 middle- and high-income countries in Europe and Thailand: a cohort study. PLos Med. 2018;15(1):e1002491. doi: 10.1371/journal.pmed.1002491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trickey A, May MT, Vehreschild JJ, Obel N, Gill MJ, Crane HM, Boesecke C, Patterson S, Grabar S, Cazanave C, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4(8):E349–E356. doi: 10.1016/S2352-3018(17)30066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang HX, Han MJ, Zhou Y, Xiu XF, Xu F, Wang L. Interrupted time series analysis for influence on HIV related fatality of implementation of 'Four Free Services One Care' policy in China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2020;41(3):406–411. doi: 10.3760/cma.j.issn.0254-6450.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 6.Hogg R, Lima V, Sterne JAC, Grabar S, Battegay M, Bonarek M, Monforte AD, Esteve A, Gill MJ, Harris R, et al. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palella FJ, Jr, Deloria-Knoll M, Chmiel JS, Moorman AC, Wood KC, Greenberg AE, Holmberg SD. Investigators HIVOS: Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Ann Intern Med. 2003;138(8):620–626. doi: 10.7326/0003-4819-138-8-200304150-00007. [DOI] [PubMed] [Google Scholar]
- 8.G BJ. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. The Department of Health and Human Services Panel on Antiretroviral Guidelines for Adult and Adolescents. 2008:42–3. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/archive/AdultandAdolescentGL000988.pdf.
- 9.Gunthard HF, Aberg JA, Eron JJ, Hoy JF, Telenti A, Benson CA, Burger DM, Cahn P, Gallant JE, Glesby MJ, et al. Antiretroviral Treatment of Adult HIV Infection 2014 Recommendations of the International Antiviral Society-USA Panel. JAMA-J Am Med Assoc. 2014;312(4):410–425. doi: 10.1001/jama.2014.8722. [DOI] [PubMed] [Google Scholar]
- 10.Lodi S, Phillips A, Logan R, Olson A, Costagliola D, Abgrall S, van Sighem A, Reiss P, Miro JM, Ferrer E, et al. Comparative effectiveness of immediate antiretroviral therapy versus CD4-based initiation in HIV-positive individuals in high-income countries: observational cohort study. Lancet HIV. 2015;2(8):E335–E343. doi: 10.1016/S2352-3018(15)00108-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang AX, Wang FS, Wang QY, Jian W, Feng TJ, Lu HZ, Sun HQ, Sun YT, Ye HH, Li TS, et al. Guidelines for diagnosis and treatment of HIV/AIDS in China (2005) Chin Med J. 2006;119(19):1589–1608. doi: 10.1097/00029330-200610010-00002. [DOI] [PubMed] [Google Scholar]
- 12.Wang AX WF, Mao Q. Guidelines for diagnosis and treatment of AIDS. Proceedings of the Fifth National Conference on HIV/AIDS, Viral Hepatitis C and National Tropical Diseases of the Chinese Medical Association. 2011. pp. 57–78. [Google Scholar]
- 13.Sun J-J, Lu H-Z. Highlights of the third edition of Chinese guidelines for AIDS diagnosis and treatment(2015). Zhejiang da xue xue bao Yi xue ban = J Zhejiang Univ Med Sci. 2015;44(6):597–602. doi: 10.3785/j.issn.1008-9292.2015.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aids, Hepatitis C Professional Group SoIDCMA, Chinese Center for Disease C, Prevention Chinese guidelines for diagnosis and treatment of HIV/AIDS (2018) Zhonghua Nei Ke Za Zhi. 2018;57(12):867–884. doi: 10.3760/cma.j.issn.0578-1426.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Dare DJ. HIV antiretroviral therapy in Ethiopia: Overcoming implementation challenges. Dissertation for the degree of philosophiae doctor (PhD). Norway: University of Bergen; 2007. https://www.researchgate.net/publication/330039998_HIV_antiretroviral_therapy_in_Ethiopia_Overcoming_implementation_challenges.
- 16.Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulle AM, Abebo TA, Abera SF, Aboyans V, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260–1344. doi: 10.1016/S0140-6736(17)32130-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun JP. International exchange and cooperation help China to provide free AIDS antiviral treatment. Chin J AIDS STD. 2022;28(6):634–637. doi: 10.13419/j.cnki.aids.2022.06.02. [DOI] [Google Scholar]
- 18.Zhang YJFX, Fan YG, et al. HIV transmission and related risk factors among serodiscordant couples in Liuzhou. China J Med Virol. 2015;87(4):553–556. doi: 10.1002/jmv.24093. [DOI] [PubMed] [Google Scholar]
- 19.Lan GHSZ, Ge XM, et al. Review and prospect of comprehensive prevention, control and management of acquired immune deficiency syndrome in Guangxi. Chinese J New Clin Med. 2021;14(10):1674–3806. [Google Scholar]
- 20.Wang LQQ, Ding ZHW, et al. Current case reporting of HIV/A IDS epidemic in China 2010. Chin J AIDS STD. 2011;17(3):275–278. [Google Scholar]
- 21.Fu YS, Ashuro AA, Feng XX, Wang T, Zhang SC, Ye DQ, Fan YG. Willingness to use HIV pre-exposure prophylaxis and associated factors among men who have sex with men in Liuzhou, China. Aids Res Ther. 2021;18(1):46. doi: 10.1186/s12981-021-00374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dong XY HA, Li ZHX, et al. Survival analysis among HIV-infected individual and AIDS patients in Baoshan, Yunnan, 1990–2020. J Trop Med. 2021;21(11):1075–80. [Google Scholar]
- 23.Jiang XM WH. Analysis of survival time and factors influencing HIV/AIDS in Nanping City, 1998–2020. Strait J Prev Med. 2021;27(04):28–31. [Google Scholar]
- 24.Egger M, May M, Chene G, Phillips AN, Ledergerber B, Dabis F, Costagliola D, D'Arminio Monforte A, de Wolf F, Reiss P, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet (London, England) 2002;360(9327):119–129. doi: 10.1016/S0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 25.Li M, Tang WM, Bu K, Mahapatra T, Zhang XY, Feng YB, Chen FF, Guo W, Wang LY, Ding ZW, et al. Mortality among people living with HIV and AIDS in China: implications for enhancing linkage. Sci Rep. 2016;6:28005. doi: 10.1038/srep28005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carriquiry G, Fink V, Koethe JR, Giganti MJ, Jayathilake K, Blevins M, Cahn P, Grinsztejn B, Wolff M, Pape JW, et al. Mortality and loss to follow-up among HIV-infected persons on long-term antiretroviral therapy in Latin America and the Caribbean. J Int AIDS Soc. 2015;18:20016. doi: 10.7448/IAS.18.1.20016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim YC, Ahn JY, Kim HY, Song JY, Park DW, Kim MJ, Choi HJ, Kim SW, Kee MK, Han MG, et al. Survival trend of HIV/AIDS patients starting antiretroviral therapy in South Korea between 2001 and 2015. Yonsei Med J. 2020;61(8):705–711. doi: 10.3349/ymj.2020.61.8.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang ZHS. Study on risk factors for failure and death of antiviral treatment in HIV/AIDS patients with initial HAART in Liuzhou City[D].Guangxi Medical University,2014. https://kns.cnki.net/kcms2/article/abstract?v=3uoqIhG8C447WN1SO36whLpCgh0R0Z-i4Lc0kcI_HPe7ZYqSOTP4QqdCOl7mBRR6JmcC84PTes9XXILbtGp5WwWKlSPpz22d&uniplatform=NZKPT
- 29.Cheng D, Fan W, Shan YF. The first detection results of CD4* T lymphocytes in newly confirmed HIV infected persons/AIDS patients in Xinxiang city from 2015 to 2020. J Trop Med. 2023;23(02):263–266. [Google Scholar]
- 30.Crabtree-Ramirez BE, Caro-Vega Y, Belaunzaran-Zamudio PF, Shepherd BE, Rebeiro PF, Veloso V, Cortes CP, Padgett D, Gotuzzo E, Sierra-Madero J, et al. Temporal changes in ART initiation in adults with high CD4 counts in Latin America: a cohort study. J Int AIDS Soc. 2019;22(12):6. doi: 10.1002/jia2.25413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoenigl M, Chaillon A, Moore DJ, Morris SR, Smith DM, Little SJ. Clear links between starting methamphetamine and increasing sexual risk behavior: a cohort study among men who have sex with men. JAIDS. 2016;71(5):551–557. doi: 10.1097/QAI.0000000000000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu DC, Jiang ZX, Xiu CZ, Li ZZ, Song Q, Wang ZH. Sexually transmitted infection prevalence and related risk factors among heterosexual male methamphetamine users in China. Int J STD AIDS. 2017;28(12):1208–1214. doi: 10.1177/0956462417693165. [DOI] [PubMed] [Google Scholar]
- 33.Robertson AM, Syvertsen JL, Ulibarri MD, Rangel MG, Martinez G, Strathdee SA. Prevalence and correlates of HIV and sexually transmitted infections among female sex workers and their non-commercial male partners in two Mexico-USA Border Cities. J Urban Health. 2014;91(4):752–767. doi: 10.1007/s11524-013-9855-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, Ouassa T, Ouattara E, Anzian A, Ntakpe JB, Minga A, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–822. doi: 10.1056/NEJMoa1507198. [DOI] [PubMed] [Google Scholar]
- 35.May M, Gompels M, Delpech V, Porter K, Post F, Johnson M, Dunn D, Palfreeman A, Gilson R, Gazzard B, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ-Br Med J. 2011;343:d6016. doi: 10.1136/bmj.d6016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lundgren D, Babiker AG, Gordin F, Emery S, Sharma S, Avihingsanon AC, Cooper DA, Fatkenheuer G, Llibre JM, Moli-Na JM, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: SupplementaryTable 1. Survival rates of people living with HIV/AIDSwith different treatment status in Liuzhou, 2006-2020. Supplementary Table 2. Comparisonof survival rates of infected patients in four periods with different treatmentstatus in Liuzhou, 2006-2020.
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.