ABSTRACT.
During this age of climate change, the incidence of tropical diseases may change. This study compared the epidemiological characteristics and trends of leptospirosis in Japan between the endemic region, Okinawa, and the rest of the country. Infectious Diseases Weekly Reports were used to determine the numbers and crude incidence rates of leptospirosis. Data were stratified by sex, age, the estimated location of the infection, the notified regions, and the reporting month. A joinpoint regression analysis was performed to estimate the annual percentage change (APC). During the 16-year study period (2006–2021), 543 leptospirosis cases were reported, with male dominance (86.2%). Approximately half of these cases were reported from Okinawa (47.1%). The patients were relatively younger in Okinawa (20–29 years, 23.4%; 30–39 years, 20.7%) than outside Okinawa. The frequency of imported cases was significantly higher outside Okinawa (0.4% versus 14.3%). The incidences of leptospirosis in and outside Okinawa were apparently higher during the summer and typhoon seasons. The annual crude incidence ratios were 20–200 times higher in Okinawa than in the rest of the country. The average APCs for the entire study period in Okinawa and the rest of Japan were 1.6% (95% CI: −5.9 to 9.6) and −1.8% (95% CI: −7.8 to 4.6), respectively, without any particular trends. Collectively, the patient profile of leptospirosis differed between Okinawa (younger men) and outside Okinawa (middle- or older-aged men with a history of traveling abroad). The disease remains a neglected tropical disease; continuous surveillance with close monitoring is required.
INTRODUCTION
Leptospirosis is an acute zoonotic disease caused by bacteria from the genus Leptospira, which primarily affects people living in tropical and subtropical areas worldwide.1,2 Each year, one million cases of human leptospirosis are globally diagnosed, and 58,900 people die.1 The spirochetes colonize the proximal renal tubules of reservoir animals, mostly rats and possibly companion animals such as dogs, livestock such as cattle and pigs, and wild animals such as rats and boars.3,4 Humans are infected with bacteria percutaneously or permucosally through direct contact with the urine of host animals or indirect contact with soil or water contaminated with urine.5 The clinical signs and symptoms of leptospirosis range from mild flu-like conditions (e.g., fever, myalgia, and headache) to fatal states, such as Weil’s disease (jaundice and renal failure) and pulmonary hemorrhage syndrome. The diagnosis of leptospirosis depends on various laboratory methods, including polymerase chain reaction (PCR) testing of blood, urine, and cerebrospinal fluid and microscopic agglutination testing of paired serum samples.6
Although spirochete infection is quite rare in Japan, Okinawa Prefecture, the southwest subtropical islands, is known to be endemic to this tropical disease.6 The Yaeyama Islands in Okinawa were the site of a recent eco-epidemiology study that discovered a significant diversity of environment-derived Leptospira species,7 indicating that these fastidious microbes are endemic to the island regions. Freshwater exposure from outdoor activities in these regions is known to increase the risk of developing the disease.6,8 Interestingly, the seroconversion rate of marine personnel from the United States who participated in jungle training in Okinawa was 3.5% during their deployment,9 indicating a high risk of leptospiral infection in those endemic areas.
Given climate change and globalization,10,11 a domestic epidemiology of leptospirosis may be shifting. Although sporadic cases diagnosed outside Okinawa were previously considered those from the southwest subtropical islands,7 the literature have increasingly described non-imported domestic cases in other regions than Okinawa.12–14 In Tokyo, a wild rat bite was reported to cause the disease even in the winter season.15 We recently encountered a laboratory-confirmed case of leptospirosis that involved a previously healthy Japanese man living outside the islands with no history of traveling to Okinawa or overseas. These facts may indicate that an infectious risk of leptospirosis outside Okinawa is spreading across the country.
In this study, we examined the epidemiological characteristics and recent trends of leptospirosis cases in Japan using the national database for infectious diseases, particularly focusing on the difference between Okinawa and the rest of the regions.
MATERIALS AND METHODS
Data source.
In this retrospective observational analysis, data on the incidence of leptospirosis between 2006 and 2021 were obtained from the Infectious Diseases Weekly Reports of Japan, which have been accumulated at the National Institute of Infectious Diseases based on the Act on the Prevention of Infectious Diseases and Medical Care for Patients with Infectious Diseases (Infectious Diseases Control Law) since November 2003.16 Leptospirosis is listed in the law as a notifiable infectious disease that falls under category IV and must be reported soon after the diagnosis. Physicians are responsible for notifying public health facilities when individuals are diagnosed with leptospirosis. The National Epidemiologic Surveillance of Infectious Diseases subsequently compiled the submitted data and made it publicly accessible on a website.16 This study excluded clinically diagnosed cases of leptospirosis because the law stipulates that only cases detected by laboratory tests, such as PCR testing of blood, urine, and cerebrospinal fluid, or paired sera (microscopic agglutination testing) are required for reporting. Details and definition in the laboratory diagnosis (PCR testing and paired sera) are unavailable because this information has not been opened to the public by the National Institute of Infectious Diseases. In practice, because there is no commercially available test for leptospirosis in Japan, medical doctors need to submit patient samples to public health centers for laboratory diagnosis as administrative testing. This prevents reporting bias in the diagnosed cases.
Data processing and statistical analyses.
We obtained annual incidences of leptospirosis from 2006 to 2021 at the open website.16 We accessed data from each fiscal year and downloaded necessary data as excel files. The annual incidence was extracted from these datafiles by sex and age. Age data were available only in 10-year age groups, and the male-to-female incidence ratio was calculated. Data were stratified by reporting regions to calculate the annual incidence rates of leptospirosis in Okinawa Prefecture and outside Okinawa over time. In addition, the estimated places of the leptospirosis infection were available (domestic versus overseas), and we calculated the proportions of imported cases. The incidence ratio was calculated by dividing crude incidence rates of Okinawa by those of outside Okinawa of the relevant year. To assess the seasonality of the disease onset, we converted the weekly data into the monthly data as follows: January (weeks 1–5), February (weeks 6–9), March (weeks 10–14), April (weeks 15–18), May (weeks 19–23), June (weeks 24–27), July (weeks 28–32), August (weeks 33–36), September (weeks 37–41), October (weeks 42–45), November (weeks 46–49), and December (weeks 50–53). Data on the Japanese population were obtained from vital statistics provided by the Japanese Ministry of Health, Labor, and Welfare.17
Categorical variables were expressed as numbers and percentages and were assessed by Fisher’s exact test using EZR version 3.5.2, a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).18 The Joinpoint Regression Software (version 4.9.0.1, Statistical Research and Applications Branch, National Cancer Institute, Bethesda, MD) was used for the joinpoint regression model to estimate trends in crude incidence rates.19 We applied a default condition for the analysis in the joinpoint software; that is, minimum number of observations from a joinpoint to either end of the data, 2; minimum number of observations between two joinpoints, 2; minimum number of joinpoint, 0; maximum number of joinpoint, 2; and permutation test as model selection method. The annual percentage change (APC) values between trend change points, which are used to characterize trends in the rates over time, were determined using the 95% CI. A P value < 0.05 was set as the level of statistical significance.
Ethics approval.
Because the study involved a retrospective examination of anonymized open-source data, informed consent was not required. The Okayama University Ethics Institutional Review Board granted ethical approval (no. 1910–009).
RESULTS
Number of notified leptospirosis cases in Japan.
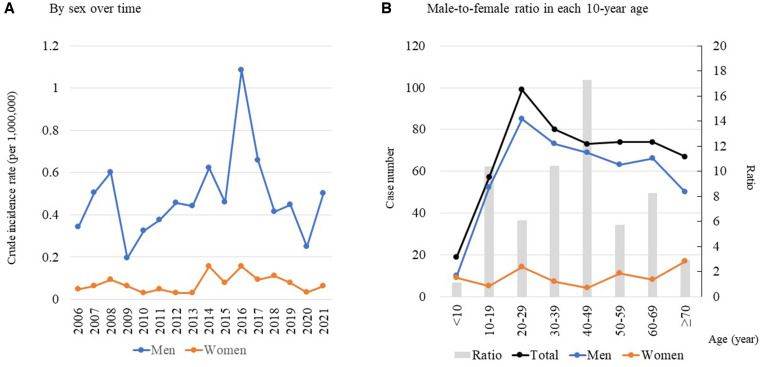
During the 16-year study period, 543 leptospirosis cases were reported. The number of male patients (468; 86.2%) was greater than the number of female patients (75; 13.8%). In Okinawa there were 256 leptospirosis cases (47.1%), and those diagnosed outside Okinawa were mostly reported in Tokyo (82; 15.1%), Miyazaki (31; 5.7%), and Kagoshima (23; 4.2%). Details of the total numbers in each prefecture are given in Supplemental Table 1. Over time, the total annual case number greatly varied from 16 cases in 2009 to 76 cases in 2016. The crude incidence rates per 1,000,000 did not reveal any increasing or decreasing trends in both sexes (Figure 1A). By age group, the fewest cases were notified in the under 10-year age group, and the highest number was observed in the twenties in both sexes, followed by equivalent numbers in older age groups (Figure 1B). The male-to-female ratio apparently varied by age category, ranging from 1.1 in the < 10 years age group to 17.3 in the 40–49 years age group. The numbers of overseas imported cases in each year were 0–6 during the study period. Calculating with the total case numbers, the proportion of overseas imported cases was relatively higher (> 10%) in the early 2010 s and 2019, indicating that the majority of the cases were diagnosed as domestic infections (Supplemental Table 2).
Figure 1.
Crude incidence rate (per 1,000,000) over time and case numbers of leptospirosis notified in Japan from 2006–2021, by sex (A) and age group (B).
Comparison between Okinawa and outside of Okinawa.
By region, we stratified the data according to Okinawa and the rest (Table 1). Overall, approximately half of the cases were reported from Okinawa (256 cases; 47.1%), and half of the cases (287 cases; 2.9%) were from the rest of Japan. Male cases were equally dominant in each of these regions (85.5% and 86.8%, respectively). By age group, patients in Okinawa were younger than those outside Okinawa. Proportion among persons aged 20–29 years were the highest in Okinawa, which was almost double of that of outside Okinawa (23.4% versus 13.6%). In comparison with this age group in their twenties, the proportions were significantly higher in older age groups outside of Okinawa, such as 50–59 years (10.2% versus 16.7%; P = 0.001), 60–69 years (5.5% versus 20.9%; P < 0.001), and ≥ 70 years (4.3% versus 19.5%; P < 0.001). Almost all (99.6%) leptospirosis cases reported in Okinawa were domestic cases, whereas 14.3% of those reported from outside Okinawa were imported cases from abroad (P < 0.001). Over time, the percentage reported from Okinawa was almost half of the total, which were comparatively lower in the early 2010 s and reached 70.6% in the final year of 2021 (Figure 2).
Table 1.
Comparison of the characteristics of patients with leptospirosis reported from Okinawa and outside Okinawa
| Characteristics | Okinawa, n (%) | Outside Okinawa, n (%) | P value* |
|---|---|---|---|
| Total | 256 (47.1) | 287 (52.9) | |
| Male/female | 219/37 (85.5/14.5) | 249/38 (86.8/13.2) | 0.71 |
| Age groups | |||
| < 10 years | 17 (6.6) | 2 (0.7) | 0.02 |
| 10–19 years | 39 (15.2) | 18 (6.3) | 0.39 |
| 20–29 years | 60 (23.4) | 39 (13.6) | reference |
| 30–39 years | 53 (20.7) | 27 (9.4) | 0.53 |
| 40–49 years | 36 (14.1) | 37 (12.9) | 0.16 |
| 50–59 years | 26 (10.2) | 48 (16.7) | 0.001 |
| 60–69 years | 14 (5.5) | 60 (20.9) | <0.001 |
| ≥ 70 years | 11 (4.3) | 56 (19.5) | <0.001 |
| Estimated place of infection | |||
| Japan | 255 (99.6) | 246 (85.7) | <0.001 |
| Overseas | 1 (0.4) | 41 (14.3) | |
Statistical analysis was performed using Fisher’s exact test.
Figure 2.
Chronological changes in leptospirosis in Japan from 2006–2021, by regions.
Monthly case numbers of leptospirosis during the study period are depicted in Figure 3. During winter and spring seasons (roughly from December to May), there seem to be only sporadic cases mainly from outside Okinawa. Beginning in June, when the rainy season starts in the southern part of Japan, leptospirosis cases appear to increase in Okinawa. As the season turns to summer and typhoon season begins (July and August), the increasing trend escalated in both Okinawa and the rest of the regions, which peaks in September and then decreases thereafter.
Figure 3.
Monthly incidences of leptospirosis in Japan.
The annual crude incidence rates are summarized in Table 2. The crude incidence rates in Okinawa exceeded 10 per 1,000,000 population at sporadic intervals in 2007, 2008, 2014, 2016, 2017, 2018, and 2021. In contrast, those from outside Okinawa were lower roughly around 0.1–0.26 per 1,000,000 population. The incidence ratio ranged from 18.5 (95% CI: 6.3–54.1) in 2006 to 202.8 (95% CI: 97.0–424.0) in 2021.
Table 2.
Comparison of the annual crude incidence rates of leptospirosis in Okinawa and the other regions in Japan, per 1,000,000 population
| Year | Okinawa | Outside Okinawa | Incidence ratio* (95% CI) |
|---|---|---|---|
| 2006 | 2.92 | 0.16 | 18.5 (6.3–54.1) |
| 2007 | 15.28 | 0.11 | 138.3 (70.3–271.9) |
| 2008 | 20.32 | 0.12 | 171.6 (91.7–321.3) |
| 2009 | 5.05 | 0.07 | 71.1 (26.5–191.0) |
| 2010 | 7.18 | 0.09 | 75.8 (32.7–175.4) |
| 2011 | 4.99 | 0.15 | 33.2 (14.0–79.0) |
| 2012 | 4.25 | 0.19 | 22.4 (9.1–54.7) |
| 2013 | 4.93 | 0.17 | 28.3 (12.1–66.1) |
| 2014 | 19.64 | 0.16 | 123.5 (69.6–219.2) |
| 2015 | 9.07 | 0.16 | 57.0 (28.3–114.5) |
| 2016 | 29.82 | 0.26 | 113.5 (72.1–178.6) |
| 2017 | 15.19 | 0.19 | 79.4 (44.5–141.7) |
| 2018 | 10.32 | 0.14 | 76.0 (38.0–152.2) |
| 2019 | 8.89 | 0.15 | 58.5 (28.9–l18.5) |
| 2020 | 5.45 | 0.07 | 75.5 (29.1–195.8) |
| 2021 | 16.35 | 0.08 | 202.8 (97.0–424.0) |
The incidence ratio was calculated by dividing the crude incidence rates of Okinawa by those of outside Okinawa.
The results of the trend analysis are presented in Table 3. The average APC for the entire study period in Okinawa was 1.6% (95% CI: −5.9 to 9.6) without any increasing or decreasing trends. In contrast, the APC outside Okinawa initially showed a significantly increasing trend, with an increase of 7.2% (95% CI: 1.3–13.4) from 2006 to 2016, which decreased thereafter, with APC of −17.5% (95% CI: −31.2 to −1.1). However, the average APC did not show a significant overall trend (−1.8%; 95% CI: −7.8 to 4.6). Plotting and regression lines of annual percentage changes by the joinpoint regression model are provided in Supplemental Figure 1.
Table 3.
Results of the joinpoint regression analysis for the crude incidence rates of leptospirosis in Japan
| Period 1 | Period 2 | Entire study period | |||
|---|---|---|---|---|---|
| Regions | Years | APC (95% CI) | Years | APC (95% CI) | Average APC (95% CI) |
| Okinawa | 2006–2021 | 1.6% (−5.9 to 9.6) | 1.6% (−5.9 to 9.6) | ||
| Outside Okinawa | 2006–2016 | 7.2% (1.3 to 13.4)* | 2016–2021 | −17.5% (−31.2 to −1.1)* | −1.8% (−7.8 to 4.6) |
APC = annual percentage change.
statistically significant.
DISCUSSION
Herein, we demonstrated the epidemiological characteristics and trends in the incidence of leptospirosis in Japan. Overall, the total number of cases was 543 in 16 years, suggesting that leptospirosis remains a rare illness in Japan. However, about half of the cases were reported from Okinawa, with the crude incidence ratios being roughly 20–200 times higher than those in other Japanese regions. This reminded us that Okinawa is an endemic area for leptospirosis in Japan. With respect to sex, the number of cases was higher in men. In terms of age, the disease was diagnosed usually among adults aged ≥ 20 years. However, the patients diagnosed with leptospirosis outside Okinawa were older than those in Okinawa. Seasonality for the leptospirosis incidence was apparent in both Okinawa and the rest of Japan, with high frequencies in summer and typhoon seasons. Finally, in contrast to our expectation, the trend analysis suggested no increasing trend of leptospirosis in either Okinawa or the rest of the country in recent years.
We found that the patient profile of leptospirosis differed between Okinawa and the rest of Japan. A male-dominated incidence was observed in both regions, which has also been documented in the literature from other countries.1,20–23 The mean age of patients in Okinawa was biased toward a younger population (20–39 years), similar to reports from other countries.24–28 A recent retrospective study with detailed surveillance data demonstrated that majority of the patients contracted the disease in the northern part of Okinawa Main Island or the Yaeyama area,6 which are very rich in nature. Both visitors and local residents, especially those of younger ages, enjoy outdoor activities (e.g., swimming, canoeing, hiking, and canyoning) in the rivers in the regions that are regarded as the source of leptospirosis. Accordingly, we consider that proportions of leptospirosis cases in Okinawa are biased to younger populations, although those outside subtropical regions were older than 50 years in more than half of the cases. In addition, although relatively few, a significantly higher frequency of cases diagnosed outside Okinawa was reported as overseas imported cases. Based on these facts, we propose that leptospirosis should be included in the differential diagnosis in currently non-endemic regions in Japan when seeing febrile male patients in their fifties or older, especially those with a history of traveling abroad.
Unfortunately, our data may not reflect the epidemiology of leptospirosis in mainland Japan because the open database lacked information on the estimated place of infection in the country. For instance, when a patient infected with leptospirosis during domestic travel to Okinawa developed the disease after returning to the place of residence, that patient would be identified as a case at the resident place unless his or her traveling history was identified. This is possible considering the long incubation period (7–12 days to 1 month) of leptospirosis.29 Even though the physician elicited the traveling history of the patient and reported it in the notification form, that information was not reflected in the open data source. Therefore, we should note that cases reported outside Okinawa may include some of the cases imported from Okinawa itself.
To the best of our knowledge, this is the first attempt to elucidate the differences in epidemiological characteristics of leptospirosis between endemic islands and the rest of the regions in Japan. Additionally, our effort to uncover chronological trends is new to the literature. However, several limitations should be clarified. First, due to the nature of the data collection and methodology, underdiagnosis is potentially a major concern. Leptospirosis is an infrequent disease, and physicians usually do not recall it in their daily medical care. Leptospirosis can never be diagnosed without a specific laboratory test. Thus, a certain number of cases may have been clinically underreported. Contrarily, there were no reporting errors because the definitive diagnosis was made by administrative laboratory testing. Second, owing to the limited number of cases, we could not calculate the age-adjusted incidence rates. Third, due to the lack of clinical data, a detailed analysis of the clinical characteristics and prognosis of the patients was unavailable. Despite these limitations, we believe that the present data are worthy of being shared among physicians and researchers to comprehend this peculiar disease.
In conclusion, the present data suggest no evidence of an increase in leptospirosis in Japan, both in Okinawa and outside Okinawa, even in this progressing climate change.30 However, our data analysis reconfirmed the fact that leptospirosis in Okinawa is far more common, especially among young populations, than in the rest of the country. Notably, more than half (57.1%) of the patients diagnosed outside the southwestern subtropical islands were aged ≥ 50 years. Leptospirosis may remain a neglected tropical disease in Japan. However, in today’s climate change and globalizing society, continuous monitoring and active surveillance of the disease is necessary.
Supplemental Materials
ACKNOWLEDGMENT
We thank Editage (www.editage.jp) for the English language editing.
Note: Supplemental material appears at www.ajtmh.org.
REFERENCES
- 1. Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI, 2015. Global morbidity and mortality of leptospirosis: a systematic review. PLoS Negl Trop Dis 9: e0003898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boey K, Shiokawa K, Rajeev S, 2019. Leptospira infection in rats: a literature review of global prevalence and distribution. PLoS Negl Trop Dis 13: e0007499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yamaguchi T, Higa N, Okura N, Matsumoto A, Hermawan I, Yamashiro T, Suzuki T, Toma C, 2018. Characterizing interactions of Leptospira interrogans with proximal renal tubule epithelial cells. BMC Microbiol 18: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guglielmini J, Bourhy P, Schiettekatte O, Zinini F, Brisse S, Picardeau M, 2019. Genus-wide Leptospira core genome multilocus sequence typing for strain taxonomy and global surveillance. PLoS Negl Trop Dis 13: e0007374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levett PN, 2001. Leptospirosis. Clin Microbiol Rev 14: 296–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kakita T, Okano S, Kyan H, Miyahira M, Taira K, Kitashoji E, Koizumi N, 2021. Laboratory diagnostic, epidemiological, and clinical characteristics of human leptospirosis in Okinawa Prefecture, Japan, 2003-2020. PLoS Negl Trop Dis 15: e0009993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sato Y, Hermawan I, Kakita T, Okano S, Imai H, Nagai H, Kimura R, Yamashiro T, Kajita T, Toma C, 2022. Analysis of human clinical and environmental Leptospira to elucidate the eco-epidemiology of leptospirosis in Yaeyama, subtropical Japan. PLoS Negl Trop Dis 16: e0010234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Narita M, Fujitani S, Haake DA, Paterson DL, 2005. Leptospirosis after recreational exposure to water in the Yaeyama Islands, Japan. Am J Trop Med Hyg 73: 652–656. [PMC free article] [PubMed] [Google Scholar]
- 9. Chen H-W, Zhang Z, Belinskaya T, Williams M, Ching W-M, 2020. Leptospirosis seroconversion surveillance among US marines assigned to Japan, 2011-2015. Mil Med 185: 624–627. [DOI] [PubMed] [Google Scholar]
- 10. Rossati A, 2017. Global warming and its health impact. Int J Occup Environ Med 8: 7–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bandara M, Ananda M, Wickramage K, Berger E, Agampodi S, 2014. Globalization of leptospirosis through travel and migration. Global Health 10: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suzuki R, Terayama M, Tanda M, 2021. Severe leptospirosis infection in a non-epidemic area. IDCases 26: e01345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Saitoh H. et al. , 2015. Leptospirosis in the Tohoku region: re-emerging infectious disease. Tohoku J Exp Med 236: 33–37. [DOI] [PubMed] [Google Scholar]
- 14. Mutoh Y, Koizumi N, Morino E, Hayakawa K, Kato Y, Ohmagari N, 2017. Leptospirosis cases in the Tokyo metropolitan area, Japan. Jpn J Infect Dis 70: 669–671. [DOI] [PubMed] [Google Scholar]
- 15. Suzuki T, Morioka S, Kikuchi T, Sato L, Nomoto H, Yamamoto K, Koizumi N, Hayakawa K, Kutsuna S, Ohmagari N, 2022. Case report: leptospirosis by wild rat bite in winter in Tokyo metropolitan area, Japan. Am J Trop Med Hyg 107: 100–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Institute of Infectious Diseases , 2023. Infectious Diseases Weekly Report. Available at: https://www.niid.go.jp/niid/ja/idwr.html. Accessed February 21, 2023.
- 17. Japanese Ministry of Health, Labor, and Welfare , 2023. Vital Statistics. Available at: https://www.e-stat.go.jp/dbview?sid=0003411884. Accessed February 21, 2023.
- 18. Kanda Y, 2013. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48: 452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. National Cancer Institute , 2023. Annual Percent Change (APC) and Confidence Interval. Available at: https://surveillance.cancer.gov/help/joinpoint/setting-parameters/method-and-parameters-tab/apc-aapc-tau-confidence-intervals/estimate-average-percent-change-apc-and-confidence-interval. Accessed February 21, 2023.
- 20. Katz AR, Ansdell VE, Effler PV, Middleton CR, Sasaki DM, 2001. Assessment of the clinical presentation and treatment of 353 cases of laboratory-confirmed leptospirosis in Hawaii, 1974-1998. Clin Infect Dis 33: 1834–1841. [DOI] [PubMed] [Google Scholar]
- 21. Tubiana S, Mikulski M, Becam J, Lacassin F, Lefèvre P, Gourinat A-C, Goarant C, D’Ortenzio E, 2013. Risk factors and predictors of severe leptospirosis in New Caledonia. PLoS Negl Trop Dis 7: e1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Philip N. et al. , 2020. Leptospira interrogans and Leptospira kirschneri are the dominant Leptospira species causing human leptospirosis in central Malaysia. PLoS Negl Trop Dis 14: e0008197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kamath R, Swain S, Pattanshetty S, Nair NS, 2014. Studying risk factors associated with human leptospirosis. J Glob Infect Dis 6: 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Daher EF, Lima RS, Júnior GB, Silva EC, Karbage NN, Kataoka RS, Júnior PC, Magalhães MM, Mota RM, Libório AB, 2010. Clinical presentation of leptospirosis: a retrospective study of 201 patients in a metropolitan city of Brazil. Braz J Infect Dis 14: 3–10. [PubMed] [Google Scholar]
- 25. Klement-Frutos E, Tarantola A, Gourinat A-C, Floury L, Goarant C, 2020. Age-specific epidemiology of human leptospirosis in New Caledonia, 2006-2016. PLoS One 15: e0242886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tique V, Mattar S, Miranda J, Oviedo M, Noda A, Montes E, Rodriguez V, 2018. Clinical and epidemiological status of leptospirosis in a tropical Caribbean area of Colombia. BioMed Res Int 2018: 6473851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Le Turnier P. et al. , 2018. Epidemiology of human leptospirosis in French Guiana (2007-2014): a retrospective study. Am J Trop Med Hyg 99: 590–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jauréguiberry S, Roussel M, Brinchault-Rabin G, Gacouin A, Le Meur A, Arvieux C, Michelet C, Tattevin P, 2005. Clinical presentation of leptospirosis: a retrospective study of 34 patients admitted to a single institution in metropolitan France. Clin Microbiol Infect 11: 391–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haake DA, Adler B. Leptospirosis in humans. Berlin, Germany: Springer, 65–97. [Google Scholar]
- 30. Ministry of Education, Culture, Sports, Science and Technology, Japan Meteorological Agency , 2020. Climate Change in Japan. Available at: https://www.data.jma.go.jp/cpdinfo/ccj/2020/pdf/cc2020_gaiyo_en.pdf. Accessed February 21, 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.