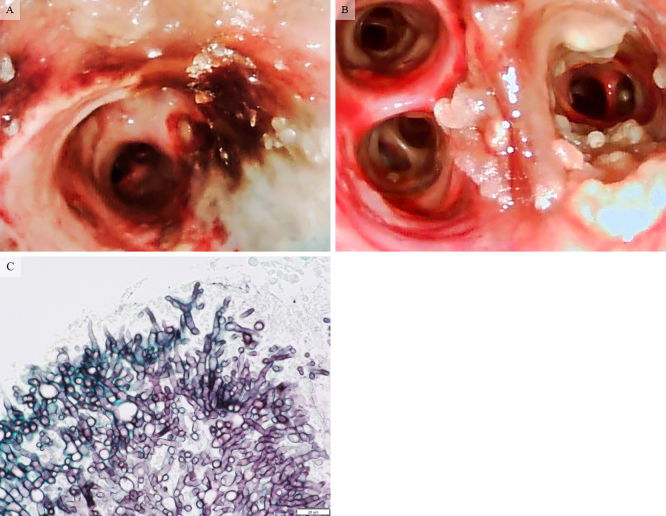
A 70-year-old woman with diabetes and renal failure presented with a fever and hypoxemia and was diagnosed with coronavirus disease 2019 (COVID-19) infection and hospitalized. On day 1, dexamethasone at 6 mg once daily and remdesivir and tocilizumab were started. However, on day 7, her condition deteriorated, and she required a ventilator. However, her respiratory status improved only temporarily, so tocilizumab was re-instituted, and dexamethasone was continued. On day 16, bronchoscopy performed for acute hypoxemia revealed pseudomembranes and ulceration on multiple bronchial walls (Picture A, B), so an endobronchial biopsy was performed. Laboratory studies showed elevation of β-D-glucan to 238 pg/mL. Chest computed tomography revealed bilateral diffuse ground-glass opacification. Suspecting COVID-19-asscociated Aspergillus tracheobronchitis, voriconazole was administered. However, she never improved and eventually died from respiratory failure. Later, the results of a biopsy evaluation showed Aspergillus (Picture C: Grocott's methenamine silver staining), confirming a diagnosis of Aspergillus tracheobronchitis. Cases of COVID-19 infection requiring steroid therapy in the intensive-care unit should be aggressively considered for bronchoscopy, with Aspergillus tracheobronchitis also kept in mind.
Picture.
The authors state that they have no Conflict of Interest (COI).