Abstract
Objectives
The Future Proofing Study (FPS) was established to examine factors associated with the onset and course of mental health conditions during adolescence. This paper describes the design, methods, and baseline characteristics of the FPS cohort.
Methods
The FPS is an Australian school‐based prospective cohort study with an embedded cluster‐randomized controlled trial examining the effects of digital prevention programs on mental health. Data sources include self‐report questionnaires, cognitive functioning, linkage to health and education records, and smartphone sensor data. Participants are assessed annually for 5 years.
Results
The baseline cohort (N = 6388, M = 13.9 years) is broadly representative of the Australian adolescent population. The clinical profile of participants is comparable to other population estimates. Overall, 15.1% of the cohort met the clinical threshold for depression, 18.6% for anxiety, 31.6% for psychological distress, and 4.9% for suicidal ideation. These rates were significantly higher in adolescents who identified as female, gender diverse, sexuality diverse, or Aboriginal and/or Torres Strait Islander (all ps < 0.05).
Conclusions
This paper provides current and comprehensive data about the status of adolescent mental health in Australia. The FPS cohort is expected to provide significant insights into the risk, protective, and mediating factors associated with development of mental health conditions during adolescence.
Keywords: adolescent development, cohort profile, developmental psychology, mental health and wellbeing, school mental health
1. INTRODUCTION
The global prevalence of mental health conditions in young people is significant (Shorey et al., 2022). Approximately half of mental health conditions emerge before the age of 18 years, with peak age of onset at 14.5 years (Solmi et al., 2022). Among children and adolescents, depression and anxiety disorders are common, with global prevalence rates estimated to be up to 8% for depression (Shorey et al., 2022) and 6.5% for anxiety disorders (Polancyk et al., 2015). Evidence from Australian population surveys mirror this data, with 12‐month prevalence rates for depression and anxiety disorders estimated to be 8% and 7% respectively (Lawrence et al., 2015). There is a significant increase in the rate of mental health conditions and particularly depression with the transition from childhood to adolescence (Costello et al., 2011; Lawrence et al., 2015). Depression is the leading cause of disability in children and adolescents (Erskine et al., 2015) and both depression and anxiety disorders are major drivers of disease burden in this age group (Klaufus et al., 2022). Poor mental health is also associated with suicidality and self‐harm, both of which are significant issues for young people. According to Australian data, suicide is the leading cause of death in people aged 15–44 years (Australian Bureau of Statistics [ABS], 2020), and self‐harm rates are increasing, particularly among young women (ABS, 2022a).
While there are effective clinical treatments for depression and anxiety disorders, they are limited in availability and do not meet the current demand, particularly for young people (Lawrence et al., 2015; Slade et al., 2009). This is in part due to the stigma associated with service use, difficulties with access, and equity of care (Lawrence et al., 2015). In order to effectively address the global disease burden of mental ill‐health, there is growing recognition that prevention and early intervention approaches delivered before, or at, first onset should form part of the strategy, in addition to treatment approaches (Cuijpers et al., 2021). Research has established that prevention programs reduce symptoms and prevent incident episodes of depression and anxiety (e.g., Stockings et al., 2015; van Zoonen et al., 2014; Werner‐Seidler et al., 2021). Early intervention is critical because untreated mental illness with onset during childhood or adolescence is a key predictor of illness severity and recurrence during later adolescence (Neufeld et al., 2017) and into adulthood (Korczak & Goldstein, 2009). Therefore, delivering evidence‐based interventions early will not only reduce the duration and severity of the incident episode, but will also reduce the likelihood of future episodes later in life (Mueller et al., 1999).
Research to date has found small but consistent prevention effects for depression and anxiety interventions (Stockings et al., 2015; van Zoonen et al., 2014; Werner‐Seidler et al., 2021). These effects are likely to be small, at least in part, because contributing risk factors and trajectories of symptom development are not yet well understood (Forsman et al., 2015; Wittchen et al., 2014). An enhanced understanding of mental health risk and protective factors will lead to the development of more precise, targeted, and effective programs for prevention and early intervention. Prospective cohort studies are a key component to building this understanding.
Existing cohort studies that investigate child and adolescent mental health have provided important insights into understanding mental health risk and protection, but many have been associated with limitations. First, the large‐scale cohort studies in this area take a general focus on development and health, and accordingly, assess a broad range of outcomes for which mental health is just one, limiting the breadth, precision of measurement, and contribution of the overall study to mental health specifically (Harris, 2013; Sanson et al., 2002; Scholtens et al., 2015). For example, the Longitudinal Study of Australian Children is a study of 10,000 Australian children that collects a wide range of data including parenting, family relationships, education, and health (Sanson et al., 2002). While there is some measurement of social and emotional outcomes, these are limited in scope and do not provide the rich mental health data needed to identify mental health trajectories. A notable exception is the Adolescent Brain Cognitive Development Study in the USA, involving over 10,000 children aged 9–10 years (Garavan et al., 2018). This study has a dual focus on the neurobiological and psychological development of children through to adulthood, and includes a broad range of measures including neuroimaging, cognitive, biospecimen and individual mental and physical health factors (Karcher & Barch, 2020).
Second, of the cohort studies that do focus specifically on risk factors for adolescent mental illness, sample sizes are relatively small, ranging from 200 to 1200 participants (Beesdo‐Baum et al., 2020; De la Torre‐Luque et al., 2020; Ellis et al., 2017; Grootendorst‐van Mil et al., 2021). This limits the potential to examine risk factors associated with subgroups of adolescents, and may not accommodate for attrition rates, diminishing the potential for appropriately powered longitudinal analyses.
The Future Proofing Study (FPS) aims to overcome these limitations by utilizing large‐scale, comprehensive, and long‐term data relating to adolescent mental health, thereby advancing knowledge about the factors associated with the onset and developmental trajectories of a broad range of adolescent mental health conditions. The FPS was established as a 5‐year prospective cohort study with an embedded cluster‐randomized controlled trial (cRCT) conducted in Australian secondary schools. Full details of the trial protocol have been published elsewhere (Werner‐Seidler et al., 2020). A separate process evaluation incorporating teacher and school staff perspectives has also been conducted (Beames et al., 2021; Beames et al., submitted).
Future Proofing Study data sources include annual student self‐report questionnaires to assess mental health, wellbeing, sleep, and a wide range of other individual, environmental, and social factors. These are complemented by smartphone‐collected measures that will be examined as potential digital predictors and/or correlates of adolescent mental health and wellbeing. Smartphone‐collected measures include cognitive task performance (e.g., working memory, executive function), typing and speech characteristics, ecological momentary assessment (EMA), and passive device sensor data (e.g., Global Positioning System (GPS), accelerometry, gyroscope). Smartphone‐collected data will be monitored over time to explore associations with changes in adolescent mental health. For example, emerging research has shown that changes in activity levels as detected from smartphone sensors are associated with wellbeing, however, this has not yet been examined comprehensively (Muller et al., 2020). Modeling and machine learning approaches will be used to develop reliable and valid indicators for prediction of mental illness onset and disease trajectories (Barnett et al., 2019). Smartphone‐collected data will be examined together with other data sources to determine if superior and more accurate prediction can be achieved by combining data sources, compared to using individual measures. Ultimately, this may lead to data‐informed approaches for personalizing and enhancing intervention delivery. Finally, linkage to government records relating to health and education (e.g., emergency department attendance, hospital data from birth, academic data throughout schooling) will be utilized to provide objective information about risk factors, health outcomes, service utilization, and educational outcomes associated with adolescent mental health. To date, there have not been any mental health specific cohort studies of this scale which incorporate such a broad range of different data sources concurrently into the one study (Beesdo‐Baum et al., 2020; Ellis et al., 2017).
The broad questions we will address with this cohort are as follows:
-
(i)
What is the prevalence of mental health conditions in an adolescent sample, and how do these change at an individual level over time?
-
(ii)
What individual factors are associated with the development of, and protection against, mental health symptoms and conditions for a range of disorders (e.g., depression, anxiety, behavioral, and eating disorders), self‐harm, suicidal ideation, and suicidal behavior, cross‐sectionally and over time?
-
(iii)
What social and environmental factors (e.g., socioeconomic status, geographical location, school factors) are associated with the development of, and protection against, mental health symptoms and conditions cross‐sectionally and over time?
-
(iv)
Are there identifiable and distinct trajectories of mental ill‐health over time, and how can they be distinguished? Do these trajectories have different risk factors, and can these trajectories be predicted from risk factors measured at baseline or early life experience?
-
(v)
Does passively collected smartphone data or cognitive task data correlate with or predict mental illness and wellbeing, cross‐sectionally and over time?
-
(vi)
What is the relationship between mental health conditions and medical history, health service utilization and academic performance, as measured by linked government records, cross‐sectionally and over time?
The aim of the embedded cRCT is to investigate whether two digital prevention interventions, delivered during the first 2 years of the study, prevent or reduce depression and other mental health conditions, relative to a control group. Full details can be found in the protocol (Werner‐Seidler et al., 2020).
The purpose of the current paper is to provide a description and reference to the design, methods, and baseline characteristics of the FPS cohort.
2. METHOD
2.1. Design
The FPS is a prospective cohort study with an embedded cRCT (the trial protocol has been published elsewhere: Werner‐Seidler et al., 2020). Study variables were assessed at baseline and will be collected annually for 5 years. Ethics approvals were obtained from the University of New South Wales (NSW) Human Research Ethics Committee (HC180836), the State Education Research Applications Process for the NSW Department of Education (SERAP2019201), and relevant Catholic Schools Dioceses across Australia.
2.2. Setting
Enrollment in the FPS occurred in 134 secondary schools located across Australia, including government and non‐government (independent and Catholic) schools. Recruitment was conducted from March 2019 to March 2022. All NSW government and independent secondary schools and eligible NSW Catholic secondary schools were invited to participate. Independent schools in capital cities from around Australia were also invited to participate. The relative focus on NSW schools was by design, to minimize logistical barriers associated with in‐school data collection conducted by the research team. Schools were required to have a counselor, psychologist, or wellbeing staff member onsite during the data collection phase. Written informed consent was provided from a parent or guardian and the adolescent prior to study participation. Baseline data collection took place at schools across three separate Year 8 cohorts (students aged 13–14 years): the 2019 Cohort from August‐September 2019; the 2020 Cohort from August‐November 2020; the 2021 Cohort from April‐December 2021 (extended to March 2022 due to COVID‐19).
2.3. Participants
All adolescents enrolled in Year 8 at participating schools were invited to take part. To participate, students required a smartphone with iOS or Android operating system and an active phone number.
2.4. Measures
See Table 1 for the full list of measures administered. Details for measures of depression, anxiety, distress, and suicidal ideation are provided below. Details for measures of disordered eating, insomnia, sleep quality, internalizing and externalizing symptoms, wellbeing, quality of life, self‐harm, suicidal behavior, psychotic‐like symptoms, alcohol and substance use can be found in the Supplementary Materials. Other non‐clinical measures will be published separately in the future.
TABLE 1.
Summary of primary, secondary, and additional outcome measures, potential mediating and risk factors, and data collection timepoints
| Self‐report measures | Baseline | Post (Stage I) | 6 months | 12 months | Post (Stage II) a | 24 months | 36 months | 48 months | 60 months | |
|---|---|---|---|---|---|---|---|---|---|---|
| Participant characteristics | ||||||||||
| Demographics | Age, sex at birth, residential location, country of birth, language spoken most at home, perceived socioeconomic status, household makeup, Aboriginal and/or Torres Strait Islander identity | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Height and weight | Height (cm), weight (kg) | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Gender identity | Current gender identity | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Sexuality | Sexual identity and attraction | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Primary and secondary outcome measures | ||||||||||
| Depression | Patient health questionnaire: Adolescent version (PHQ‐A) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Psychological distress | Distress questionnaire 5 (DQ5) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Anxiety | Spence children's anxiety scale short form (CAS‐8) and CAS generalized anxiety and social phobia subscales | ✓ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Insomnia | Insomnia severity index (ISI) | ✓ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Suicidal ideation | Suicidal ideation attributes scale (SIDAS) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Additional outcome measures, potential mediating variables, risk factors | ||||||||||
| Diagnosed mental health condition | Reported diagnosed mental health condition | ✓ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ | ✓ | ✓ |
| Diagnosed disability | Reported diagnosed disability | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✓ | ‐ |
| Disordered eating | Screen for disordered eating (SDE) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Sleep quality | Pittsburgh sleep quality index (PSQI) | ✓ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Internalizing and externalizing symptoms | Strengths and difficulties questionnaire (SDQ) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Wellbeing | Short‐form Warwick‐Edinburgh mental wellbeing scale (SWEMWBS) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Quality of life | Child health utility 9D (CHU‐9D) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Self‐harm | Self‐harm questionnaire | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Suicidal behavior | Youth risk behavior survey (YRBS) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Psychotic‐like symptoms | Adolescent psychotic‐like symptom screener (APSS) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Alcohol use | Age of onset and frequency of alcohol use | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Other substance use | Use of cannabis, tobacco, and other substances | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Hospital admissions | Reported hospital admissions for physical and mental health | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Childhood trauma | Behavioral risk factor surveillance system ‐ Adverse childhood experience (BRFSS‐ACE) | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✓ | ‐ |
| Stressful life events | Exposure to stressful life events | ‐ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Personality | Big five inventory‐10 (BFI‐10) | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Social support | Schuster social support scale (SSSS) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| School connectedness | Items from programme for international student assessment (PISA) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ‐ |
| School climate | School climate measure | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ‐ |
| Bullying | Frequency and type of bullying | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Resilience | Connor‐Davidson resilience scale (CD‐RISC‐10) | ‐ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Screen time | Hours of recreational screen time per day | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Social media use | Maladaptive Facebook use survey (MFUS), adapted to apply to social media use more broadly | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Pubertal development | Menarche, voice breaking and Tanner stages | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Romantic relationships | Reported romantic relationships | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Sexual behavior | Reported sexual behavior | ‐ | ‐ | ‐ | ‐ | ‐ | ✓ | ‐ | ✓ | ‐ |
| COVID‐19 exposure | Experience of COVID‐19 pandemic and child traumatic stress questionnaire (CTSQ) | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ‐ | ‐ |
| Bushfire exposure | Bushfire exposure questionnaire (BEQ) and child traumatic stress questionnaire (CTSQ) | ✓ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Flood exposure | Exposure to Australian flood disaster in 2022 | ‐ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ‐ | ‐ |
| Top three concerns | Current top three issues of concern | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| Priorities for the future | Social and political issues of importance to young Australians | ‐ | ‐ | ‐ | ✓ | ‐ | ✓ | ✓ | ✓ | ✓ |
| School characteristics (imputed from ACARA schools database) | Baseline | Post (stage I) | 6 months | 12 months | Post (stage II) a | 24 months | 36 months | 48 months | 60 months | |
|---|---|---|---|---|---|---|---|---|---|---|
| Location | State, local government area | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Remoteness | Accessibility and remoteness index of Australia (ARIA+) | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Sector and type | Government or non‐government, combined or secondary | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Size | Full time equivalent students, full time equivalent teaching staff | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Socio‐educational advantage | Index of community socio‐educational advantage (ICSEA) | ✓ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Smartphone‐collected data | Baseline | Post (stage I) | 6 months | 12 months | Post (stage II) a | 24 months | 36 months | 48 months | 60 months | |
|---|---|---|---|---|---|---|---|---|---|---|
| Self‐rated mood | Ecological momentary mood rating on 5‐point scale | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Affective card sorting task | Wisconsin card sorting task, with/without affective distractors | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Affective backward span task | Digit span backwards, with/without affective distractors | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Typing task | Copying and free typing about every day and affective topics | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Voice task | Sentence narration, phonemes, recall and free speaking on provided topics | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Movement (opt‐in) | Accelerometery and gyroscope device sensor data | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Location (opt‐in) | GPS device sensor data | ✓ | ✓ | ‐ | ✓ | ‐ | ✓ | ‐ | ‐ | ‐ |
| Data linkage (opt‐in) | ||||||||||
| Birth and early development | Birth registrations, neonatal intensive care, perinatal care | |||||||||
| Health service utilization | Admission to hospital and emergency department, ambulance use, mental health ambulatory care, use of health services under Medicare and Pharmaceutical Benefits Scheme | |||||||||
| Physical health outcomes | Self‐harm and suicide attempt, cancer registry, notifiable conditions, death registrations | |||||||||
| Educational outcomes | Standardized test results from school years 3, 5, 7, 9, 10 and 12 | |||||||||
Note: References for the measures in Table 1 are available from the authors upon request.
Participants selected to take part in Stage II of the RCT only.
2.4.1. Participant school and individual characteristics
Participants' school characteristics were imputed from a publicly available database curated by the Australian Curriculum, Assessment and Reporting Authority (ACARA), and included state, remoteness (e.g., major cities, inner regional, outer regional; ascertained through the Accessibility and Remoteness Index of Australia, ARIA+; Australian Institute of Health and Welfare [AIHW], 2004), school sector, school size, and Index of Community Socio‐Educational Advantage (ICSEA: an index applied to all Australian schools, calculated from parent and community socio‐demographic data; ACARA, 2020). Participants' individual characteristics were assessed via self‐report questionnaires and included age, sex at birth, gender identity, sexuality, Aboriginal and/or Torres Strait Islander identity, country of birth, language spoken most at home, household makeup, perceived socioeconomic status, and mental health and disability diagnoses.
2.4.2. Depression
The Patient Health Questionnaire for Adolescents (PHQ‐A; Johnson et al., 2002) is an adaptation of the PHQ‐9, a nine‐item depression severity screening tool based on Diagnostic and Statistical Manual of Mental Disorders‐Fourth Edition criteria (range 0–27; higher score indicates greater depression). A threshold of ≥15, reflecting moderately severe symptoms, was used to determine caseness. The internal consistency of the PHQ‐A in the current study was excellent (Cronbach's α = 0.88).
2.4.3. Anxiety
The Children's Anxiety Scale Short‐Form (CAS‐8) is an eight‐item measure of anxiety, based on the Spence children's anxiety scale (CAS; Spence, 1998). The CAS‐8 incorporates questions assessing generalized anxiety and social anxiety. The CAS‐8 has demonstrated good reliability and provides population‐level, standardized norms, with a range of 0–24 (higher score indicates greater anxiety; Spence et al., 2003; Spence et al., 2014). A threshold of ≥14 was used to determine caseness. The internal consistency of the CAS‐8 was high in the current study (α = 0.88). An additional 7‐items from the CAS were administered to allow for calculation of the CAS Social Phobia and Generalized Anxiety subscales (each with total scores ranging 0–18).
2.4.4. Psychological distress
The Distress Questionnaire‐5 (DQ5; Batterham et al., 2016) is a five‐item screening tool assessing psychological distress. The scale has strong psychometric properties, a range of 5–25 (higher score indicates greater distress), and a threshold of ≥14 as the clinical cut‐off. The internal consistency of the DQ5 in the current study was good (α = 0.88).
2.4.5. Suicidal ideation
The Suicidal Ideation Attributes Scale (SIDAS) is a measure of suicidal ideation severity in the past month. It has high internal consistency and good convergent validity (Van Spijker et al., 2014). The score range is 0–50, with a higher score indicating higher suicidal ideation. A threshold of ≥21 was used to determine clinical levels of suicidal ideation. Internal consistency of the SIDAS was good in the current study (α = 0.78).
2.5. Study size
The sample size was based on an estimate to detect small (d = 0.29) between‐group differences in the cRCT component of the study on symptoms of depression (the primary outcome), with power set at 0.80 (for details, see Werner‐Seidler et al., 2020). The target sample size was set at 10,000 participants. A cluster‐randomization approach was employed at the school level with a 1:1 allocation, projected to be 5000 participants in each arm (Werner‐Seidler et al., 2020). The intention was to use the control arm as the cohort study sample and to combine the two arms if the cRCT results showed no effects of the interventions on mental health.
2.6. Study apps
2.6.1. Future Proofing app
The Future Proofing app was developed by the Black Dog Institute and Deakin University for data collection. Cognitive functioning (executive function and working memory), typing, speech, and EMA data are actively collected via app‐specific tasks. Passively collected sensor data includes location data (GPS) and movement data (accelerometery, gyroscope; Barnett et al., 2019).
2.6.2. SPARX‐Future Proofing (SPARX‐FP)
SPARX‐FP is an app‐based, gamified Cognitive Behavioral Therapy (CBT) prevention program. SPARX‐FP was adapted in both format and content from a web‐based depression treatment program to an app‐based prevention program (Merry et al., 2012; Perry et al., 2017). The prevention version has been found to reduce symptoms of depression (d = 0.29) in school students (Perry et al., 2017).
2.6.3. Sleep Ninja
Sleep Ninja is an app that delivers CBT for insomnia. Sleep Ninja has been shown to be effective in improving sleep difficulties (d = 0.41) and reducing symptoms of depression (d = 0.28) and anxiety (d = 0.27) in adolescents (Werner‐Seidler et al., 2019; Werner‐Seidler et al., submitted).
See protocol (Werner‐Seidler et al., 2020) for further details about these interventions and their delivery in FPS.
2.7. Procedure
Figure 1 shows the study timeline and flow. A total of 1036 Australian secondary schools were invited to participate in the study by letter, email, and phone. Concurrently, the study was advertised on social media and promoted at school conferences. Interested schools provided a signed letter of support from their executive and were then randomized (at the school level) using a computer‐generated randomization schedule into the intervention or control condition for the cRCT component of the study, stratified by school size, school remoteness, co‐educational versus single sex enrollment, and index of socio‐educational advantage (ICSEA). In the school term prior to study commencement, recruitment materials were provided to schools to share with Year 8 families inviting parents to provide consent for their child's participation. To minimize sampling bias, recruitment materials were produced in several languages (English, Arabic, Chinese) and parental consent was accepted online, on paper forms, or by phone. Additional opt‐in consent was obtained from parents for collection of sensor data via the Future Proofing app, and for participation in the data linkage component of the study.
FIGURE 1.
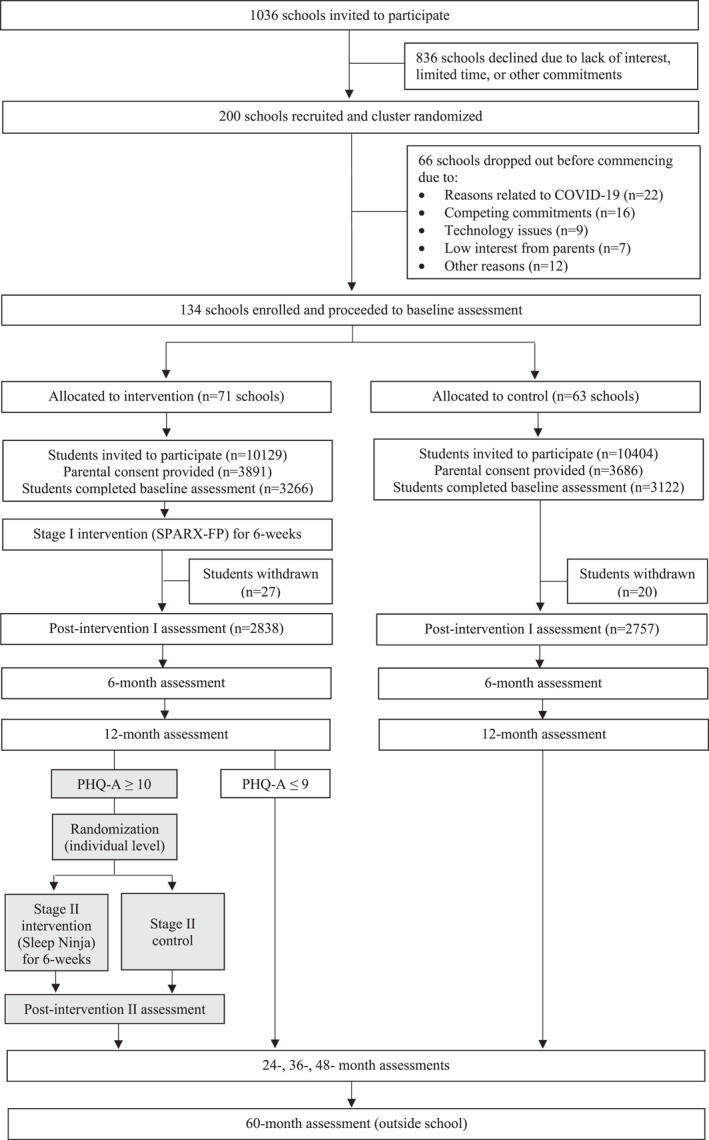
Participant flow diagram
On the date of the baseline assessment, participating students were invited to attend a group session at school facilitated by the study team. Students were introduced to the study and then logged in to the study website to provide individual consent and complete the baseline questionnaire on their own computer, smartphone, or tablet. They then downloaded the Future Proofing app on their smartphones to complete cognitive tasks, typing, speech, and EMA measures. All questionnaires and study tasks were completed independently, without input from the study team. Students in the intervention arm were subsequently invited to download and commence using the depression prevention program (SPARX‐FP), which they could access for 6 weeks (Stage I of the RCT). Most baseline assessments were facilitated in person by the study team (57% of all sessions). Assessments that coincided with physical distancing restrictions imposed due to COVID‐19 were facilitated remotely over Zoom, with students joining either from school (41% of all sessions) or home (2% of all sessions). At 12 months (Stage II of the RCT), students in the intervention arm with moderate to high levels of depression were independently re‐randomized to either the Sleep Ninja intervention or a control group. Those who received the Sleep Ninja intervention had access to the program for 6 weeks.
Follow‐up assessments are conducted primarily at school to minimize loss at follow‐up, and are scheduled for 6‐weeks, 6‐months, 12‐months, 24‐months, 36‐months, 48‐months, and 60‐months post‐baseline. At the 6‐week assessment, all students received a $20 gift card to reimburse personal data costs. Linkage with government records relating to health and educational outcomes will be conducted in 2023 and 2026.
2.8. Statistical analysis
Data quality was routinely monitored by the study Data Manager. Data were automatically collected using a bespoke study‐specific platform, hosted on the Black Dog Institute Research Engine. Data from the Research Engine were exported to Excel for preparation and then imported to SPSS Statistics v28 for analyses.
The focus of this paper is to present characteristics of the cohort and their mental health symptoms at baseline, using descriptive and frequency statistics. Data are presented overall and segmented by key demographic characteristics known to be associated with mental health conditions (ABS, 2022a; Lawrence et al., 2015). An analysis of variance approach was used to investigate gender differences in baseline mental health symptoms, wellbeing, and quality of life, using Bonferroni adjustments. Mental health symptom profiles for primary and secondary outcomes are presented, together with the proportion of participants above scale specified clinical cut‐offs. Chi‐square analyses were used to compare participants based on their school remoteness and ICSEA, and for participants who were gender or sexuality diverse, Aboriginal and/or Torres Strait Islander, or spoke English as a second language, and to compare these subgroups on mental health symptoms. Reported effect sizes are partial eta squared (η p 2) for continuous outcomes where 0.01 is small, 0.06 is medium and 0.14 is large, and phi (φ) for categorical outcomes where 0.10 is small, 0.30 is medium and 0.50 is large (Cohen, 1988; Keppel, 1991).
3. RESULTS
A total of 200 schools consented to participate and were randomized. However, as baseline data collection coincided with multiple COVID‐19 lockdowns, a total of 66 schools withdrew from the study (see Figure 1 for reasons). There were 134 schools enrolled in the final sample, of which 77 (57.5%) were government schools and 57 (42.5%) were non‐government schools. From these 134 schools, 20,533 Year 8 students were invited to participate. Consent was obtained from 7577 parents, and baseline data were collected from a total of 6388 students. There were 3266 students randomized to the intervention arm, and 3122 students randomized to the control arm.
3.1. Participant school and individual characteristics
Table 2 shows participant school and individual characteristics. Table 3 shows a comparison of the key demographics from our cohort with youth population estimates in Australia.
TABLE 2.
| School characteristics | |
|---|---|
| School state, n (%) | |
| New South Wales | 5465 (85.6) |
| Victoria | 455 (7.1) |
| Queensland | 196 (3.1) |
| Western Australia | 183 (2.9) |
| South Australia | 89 (1.4) |
| School remoteness, n (%) | |
| Major cities | 4855 (76.0) |
| Inner regional | 1409 (22.1) |
| Outer regional | 124 (1.9) |
| School sector, n (%) | |
| Government school | 3252 (50.9) |
| Non‐government school | 3136 (49.1) |
| School size, mean (SD) | |
| FTE students | 952 (279) |
| FTE teaching staff | 76 (25) |
| ICSEA, median (SD) | 1048 (79.6) |
| Individual characteristics | |
| Age, mean (SD) | 13.90 (0.51) |
| Sex at birth, n (%) | |
| Female | 3329 (52.1) |
| Male | 2970 (46.5) |
| Not sure | 33 (0.5) |
| Another term | <5 (<1) |
| Prefer not to say | 52 (0.8) |
| Gender identity, n (%) | |
| Female | 3122 (48.9) |
| Male | 2973 (46.5) |
| Nonbinary | 117 (1.8) |
| Other | 67 (1.0) |
| Prefer not to say | 109 (1.7) |
| Gender diversity, n (%) | |
| Cisgender | 6019 (94.2) |
| Gender diverse | 202 (3.2) |
| Mischievous or uninterpretable response | 37 (0.6) |
| Prefer not to say | 130 (2.0) |
| Sexuality, n (%) | |
| Heterosexual | 4471 (73) |
| Gay or lesbian | 103 (1.7) |
| Bisexual | 414 (6.8) |
| Pansexual | 119 (1.9) |
| Asexual | 67 (1.1) |
| Other | 96 (1.6) |
| Not sure | 561 (9.2) |
| Prefer not to say | 296 (4.8) |
| Sexuality diverse | 764 (12.5) |
| Aboriginal and/or Torres Strait Islander identity, n (%) | |
| Not Aboriginal and/or Torres Strait Islander | 5899 (92.3) |
| Aboriginal and/or Torres Strait Islander | 338 (5.3) |
| Prefer not to say | 151 (2.4) |
| Country of birth, n (%) | |
| Australia | 5842 (91.5) |
| Others | 545 (8.5) |
| Language spoken most at home, n (%) | |
| English | 5982 (93.7) |
| Others | 405 (6.3) |
| Household makeup, n (%) | |
| Two parents | 5009 (78.4) |
| Stepfamily | 648 (10.1) |
| Single parent | 669 (10.5) |
| Other | 62 (1.0) |
| Perceived socioeconomic status, n (%) | |
| High | 2866 (44.9) |
| Medium | 2083 (32.6) |
| Low | 529 (8.3) |
| Prefer not to say | 910 (14.2) |
| Mental health diagnosis, n (%) | |
| Major depression | 239 (3.7) |
| Social anxiety disorder | 383 (6.0) |
| Generalized anxiety disorder | 501 (7.8) |
| Obsessive compulsive disorder | 85 (1.3) |
| Panic disorder | 120 (1.9) |
| Separation anxiety disorder | 97 (1.5) |
| Alcohol use disorder | 8 (0.1) |
| Substance use disorder | 10 (0.2) |
| Attention deficit hyperactivity disorder | 395 (6.2) |
| Post‐traumatic stress disorder | 88 (1.4) |
| Schizophrenia/Psychosis | 16 (0.3) |
| No diagnosis | 5253 (82.2) |
| Disability diagnosis, n (%) | |
| Autism | 170 (2.7) |
| Intellectual disability | 29 (0.5) |
| Learning disability | 135 (2.1) |
| Tourette syndrome | 41 (0.6) |
| Cerebral palsy | 9 (0.1) |
| Brain injury | 16 (0.3) |
| Neurological disability | 57 (0.9) |
| Hearing impairment | 90 (1.4) |
| Visual impairment | 376 (5.9) |
| No diagnosis | 5591 (87.5) |
Note: N for each measure = 6388 except sexuality (N = 6127), country of birth (N = 6387), and language spoken most at home (N = 6387).
Abbreviations: FTE, Full time equivalent; Gender diverse, gender identity incongruent with sex at birth (includes nonbinary gender); ICSEA, Index of Community Socio‐Educational Advantage; Sexuality diverse, gay or lesbian, bisexual, pansexual, asexual, and free text responses to ‘other’ where valid terms describing non‐heterosexual identity were provided. To protect the identities of individuals, values less than 5 are censored and reported as ‘<5’.
TABLE 3.
Comparison of Future Proofing Study (FPS) cohort to Australian youth population estimates
| FPS Cohort (%) | Australian Population (%) | |
|---|---|---|
| Female | 48.9 | 48.6 a |
| Born in Australia | 91.5 | 84.0 b |
| Reside in major cities | 76.0 | 75.0 c |
| Aboriginal and/or Torres Strait Islander | 5.3 | 5.6 d |
| Sexuality diverse | 12.5 | 12.2 e –21.1 f |
| Gender diverse | 3.2 | 2.3 f –3.7 g |
| Attends government secondary school | 50.9 | 58.9 h |
Australian Census, reference sample 10–14 years (ABS, 2022e).
Australian Census, reference sample 10–14 years (ABS, 2022d).
Australian Institute of Health and Welfare, reference sample 15–24 years (AIHW, 2021).
Australian Census, reference sample 5–14 years (ABS, 2022c).
Victorian Agency for Health Information, reference sample 18–24 years (VAHI, 2020).
Australian Research Centre in Sex, Health and Society, reference sample 15–18 years (Fisher et al., 2019).
Mission Australia Youth Survey Report, reference sample 15–19 years (Mission Australia, 2021).
Australian Curriculum, Assessment and Reporting Authority, reference sample 12–18 years (ACARA, 2021).
Study participants were in Year 8 (M = 13.9 years; SD = 0.51). Most students (85.6%) attended schools located in NSW, the same state as the study team. Approximately three quarters of students attended schools in major cities and 24% attended schools located in inner and outer regional areas, reflecting the spread of the Australian population (AIHW, 2021). Approximately half of participating students attended government secondary schools (50.9%), which is slightly lower than the proportion of students attending government secondary schools in the Australian population (58.9%; ACARA, 2021). Schools attended by study participants had a mean number of 952 students and 76 full‐time equivalent teaching staff, with a student to teaching staff ratio of 12.5 students to one teacher, similar to the national average (ABS, 2022b). Participants attended schools with a median ICSEA of 1048, which is slightly higher than the Australian population median of 1000 (ACARA, 2020).
Participants mostly identified as female (48.9%) or male (46.5%), with 4.5% indicating that they were nonbinary, other, or preferred not to say. Most participants were cisgender (94.2%) and 3.2% were gender diverse (participants whose gender identity was incongruent with their sex at birth). In terms of sexuality, 73% indicated heterosexual identity, 12.5% indicated either ‘gay or lesbian’, ‘bisexual’, ‘pansexual’, ‘asexual’, or provided a free text response to ‘other’ describing non‐heterosexual identity using another term, 9.2% indicated ‘not sure’, and 4.8% preferred not to say. Although there is limited Australian data regarding LGBTQA + identity in young adolescents, our cohort were comparable to Australian estimates for people aged 15–24 years (Fisher et al., 2019; Victorian Agency for Health Information [VAHI], 2020; Mission Australia, 2021). A small proportion of the cohort (5.3%) identified as Aboriginal and/or Torres Strait Islander, representative of recent census estimates (ABS, 2022c). Participants were predominantly born in Australia (91.5%) and spoke mostly English at home (93.7%), higher than recent census estimates suggesting that 84% of children aged 10–14 years were Australian born (ABS, 2022d). Approximately 20% of participants lived with a stepfamily or a single‐parent family, with the majority (78.4%) in two‐parent households.
Participants provided self‐report responses to questions about lifetime mental health or disability diagnosis given by a health professional. In line with population prevalence estimates (Lawrence et al., 2015), most participants reported never having received a diagnosis of a mental health condition (82.2%) or a disability (87.5%). A depression diagnosis was reported by 3.7% of participants, which was slightly lower than the 5% prevalence level reported by young people (11–17 years) in the most recent Australian population mental health survey (Lawrence et al., 2015). For anxiety disorders, Generalized Anxiety Disorder and Social Anxiety Disorder were most common (7.8% and 6%, respectively). A diagnosis of Attention Deficit Hyperactivity Disorder was reported by 6.2% of the cohort. The most common disabilities were visual impairment (5.9%), autism (2.7%) and learning disability (2.1%; see Table 2).
3.2. Participant symptoms on clinical measures, wellbeing and quality of life
Participant symptom data are presented in Table 4. Data are presented overall and separated by gender identity (male, female, nonbinary). Mental health symptom levels differed significantly as a function of gender on all variables, all ps < 0.001 (depression, η p 2 = 0.10; anxiety, η p 2 = 0.17; psychological distress, η p 2 = 0.15; suicidal ideation, η p 2 = 0.05; disordered eating, η p 2 = 0.14; insomnia, η p 2 = 0.07; sleep quality, η p 2 = 0.06; externalizing symptoms, η p 2 = 0.03; internalizing symptoms, η p 2 = 0.12), with female gender being associated with higher symptom levels relative to male gender (all ps < 0.001). This pattern was replicated for wellbeing (η p 2 = 0.04) and quality of life (η p 2 = 0.12), with female gender being associated with lower levels of wellbeing and quality of life, relative to males (ps < 0.001). Adolescents who identified as nonbinary had significantly higher symptoms relative to males and females across all variables (ps < 0.001), except for disordered eating, where there was no difference between those who identified as nonbinary and females (p = 0.07).
TABLE 4.
Symptoms on clinical measures, wellbeing, and quality of life in overall cohort and in male, female, and nonbinary participants
| Total | Male | Female | Nonbinary | |
|---|---|---|---|---|
| N = 6388 | n = 2973 | n = 3122 | n = 117 | |
| PHQ‐A | 7.36 (6.3) | 5.4 (5.3) | 8.58 (6.3) | 15.9 (7.1) |
| CAS‐8 | 8.26 (5.5) | 5.84 (4.5) | 10.11 (5.3) | 13.82 (5.9 |
| CAS‐SP | 7.21 (4.6) | 5.17 (3.8) | 8.81 (4.3) | 11.41 (4.7) |
| CAS‐GAD | 6.51 (4.5) | 4.5 (3.6) | 8.1 (4.4) | 10.56 (4.5) |
| DQ5 | 11.34 (5.1) | 9.33 (4.2) | 12.76 (5) | 17.54 (5) |
| SIDAS | 2.84 (7.5) | 1.6 (5.4) | 3.49 (8.3) | 12.45 (13.8) |
| SDE | 1.48 (1.5) | 0.9 (1.2) | 1.96 (1.5) | 2.28 (1.5) |
| ISI | 7.06 (5.5) | 5.61 (4.9) | 8.00 (5.6) | 13.53 (6.5) |
| PSQI | 6.12 (3.7) | 5.33 (3.5) | 6.55 (3.6) | 10.38 (4) |
| SDQ‐total | 12.72 (6.9) | 10.63 (6.2) | 14.05 (6.9) | 20.72 (6.6) |
| SDQ‐internalizing | 5.9 (3.94) | 4.48 (3.46) | 6.89 (3.82) | 10.27 (3.93) |
| SDQ‐externalizing | 6.81 (4.0) | 6.15 (3.76) | 7.16 (4.08) | 10.46 (3.58) |
| SWEMWBS | 21.2 (4.9) | 22.2 (5.2) | 20.6 (4.4) | 17.3 (4.3) |
| CHU‐9D | 0.65 (0.26) | 0.75 (0.23) | 0.59 (0.26) | 0.38 (0.24) |
Note: Data are mean (SD). Higher scores reflect greater levels of the variable being measured.
Abbreviations: CAS‐8, Children's Anxiety Scale Short Form‐8 (Anxiety); CAS‐GAD, Spence Children's Anxiety Scale—Generalized Anxiety Disorder subscale; CAS‐SP, Spence Children's Anxiety Scale—Social Phobia subscale; CHU‐9D, Child Health Utility 9D (Quality of Life); DQ5, Distress Questionnaire 5 (Psychological Distress); ISI, Insomnia Severity Index; PHQ‐A, Patient Health Questionnaire for Adolescents (Depression); PSQI, Pittsburgh Sleep Quality Index; SDE, Screen for Disordered Eating; SDQ‐externalizing, Strengths and Difficulties Questionnaire—Externalizing subscale; SDQ‐internalizing, Strengths and Difficulties Questionnaire—Internalizing subscale; SDQ‐total, Strengths and Difficulties Questionnaire—Total Difficulties Score; SIDAS, Suicidal Ideation Attributes Scale; SWEMWBS, Short Warwick‐Edinburgh Mental Wellbeing Scale. Data are presented by gender identity.
Participant data were collected from 2019 to 2022 so we conducted ANOVAs on the outcomes reported in Table 4 with baseline year entered as a fixed factor. The overall tests were significant, suggesting higher levels of mental health symptoms in later years. However, the effect sizes were all η p 2<0.003 demonstrating negligible effects as a function of baseline year.
The proportion of participants meeting clinical thresholds on primary and secondary measures (depression, anxiety, psychological distress, suicidal ideation) are presented in Table 5. Data are presented overall and broken down by school remoteness, school ICSEA, gender identity, gender diversity, sexuality diversity, Aboriginal and/or Torres Strait Islander identity, and English as a second language. Participants who attended school in regional areas were more likely to meet the clinical threshold for depression (p = 0.046, φ = 0.03) and anxiety (p = 0.002, φ = 0.04) relative to participants who attended school in major cities but did not significantly differ in symptom profile for psychological distress (p = 0.41) or suicidal ideation (p = 0.52). Participants who attended less advantaged schools (ICSEA≤1000) were significantly more likely to reach the clinical threshold for depression (p = 0.001, φ = −0.04), anxiety (p < 0.000, φ = −0.06) and psychological distress (p = 0.017, φ = −0.03) relative to participants who attended more advantaged schools (ICSEA≥1001) but did not significantly differ on suicidal ideation (p = 0.26). Gender diverse participants were significantly more likely to reach the clinical threshold for depression (φ = 0.23), anxiety (φ = 0.17), psychological distress (φ = 0.18), and suicidal ideation (φ = 0.19) relative to cisgender participants (all ps < 0.0001). Similarly, sexuality diverse participants were significantly more likely to reach the clinical threshold for depression (φ = 0.33), anxiety (φ = 0.26), psychological distress (φ = 0.32), and suicidal ideation (φ = 0.23) relative to those who were heterosexual (all ps < 0.0001). Participants who identified as Aboriginal and/or Torres Strait Islander were significantly more likely to meet the clinical threshold for depression (p = 0.001, φ = 0.04), anxiety (p = 0.028, φ = 0.03), psychological distress (p = 0.014, φ = 0.03) and suicidal ideation (p < 0.000, φ = 0.05) relative to participants who did not identify as Aboriginal and/or Torres Strait Islander. There were no significant differences in the symptom profile of participants with English as a second language for depression, psychological distress, or suicidal ideation (all ps > 0.05) relative to participants who spoke mostly English at home, and participants with English as a second language were significantly less likely to meet the clinical threshold for anxiety (p = 0.032, φ = −0.03).
TABLE 5.
Proportion of cohort meeting clinical cut‐offs for depression, anxiety, psychological distress, and suicidal ideation overall and by demographic characteristics
| PHQ‐A (%) | CAS‐8 (%) | DQ5 (%) | SIDAS (%) | |
|---|---|---|---|---|
| Total | 15.1 | 18.6 | 31.6 | 4.9 |
| Major cities | 14.6 | 17.7 | 31.3 | 4.8 |
| Regional areas | 16.7 | 21.2 | 32.4 | 5.2 |
| ICSEA ≥ 1001 | 14.1 | 17.0 | 30.7 | 4.7 |
| ICSEA ≤ 1000 | 17.5 | 22.3 | 33.7 | 5.4 |
| Male | 7.6 | 6.9 | 16.6 | 2.4 |
| Female | 19.1 | 26.9 | 42.0 | 6.1 |
| Gender diverse | 58.9 | 53.5 | 76.2 | 28.7 |
| Sexuality diverse | 43.5 | 43.1 | 66.5 | 17.7 |
| Aboriginal and/or Torres Strait Islander | 21.0 | 23.1 | 37.6 | 9.5 |
| English is second language | 15.8 | 14.6 | 32.6 | 5.3 |
Note: Data are percentages of the cohort meeting clinical cut‐offs across the PHQ‐A (depression), CAS‐8 (anxiety), DQ5 (psychological distress) and SIDAS (suicidal ideation). Gender diverse, gender identity incongruent with sex at birth (includes nonbinary gender); Sexuality diverse, gay or lesbian, bisexual, pansexual, asexual, and free text responses to ‘other’ where valid terms describing non‐heterosexual identity were provided.
Abbreviations: CAS‐8, children'’s anxiety scale; DQ5, distress questionnaire‐5; ICSEA, Index of Community Socio‐Educational Advantage; PHQ‐A, Patient Health Questionnaire for Adolescents; SIDAS, Suicidal Ideation Attributes Scale.
3.3. Additional variables
See Table 6 for descriptive data on self‐harm, suicidal behavior, psychotic‐like symptoms, alcohol and substance use. Data are presented overall and separated by gender identity (male, female, nonbinary).
TABLE 6.
Self‐harm, suicidal behavior, psychotic‐like symptoms, alcohol and substance use in overall cohort and in male, female, and nonbinary participants
| Total | Male | Female | Nonbinary | |
|---|---|---|---|---|
| Ever self‐harmed, n (%) | N = 6373 | n = 2963 | n = 3118 | n = 117 |
| Never | 4966 (77.9) | 2528 (85.3) | 2311 (74.1) | 48 (41.0) |
| Once | 654 (10.3) | 244 (8.2) | 372 (11.9) | 14 (12.0) |
| 2, 3 or 4 times | 403 (6.3) | 115 (3.9) | 241 (7.7) | 24 (20.5) |
| 5 or more times | 350 (5.5) | 76 (2.6) | 194 (6.2) | 31 (26.5) |
| Suicidal behavior in past 12 months, n (%) | N = 6370 | n = 2960 | n = 3118 | n = 117 |
| Suicidal ideation | 499 (7.8) | 159 (5.4) | 277 (8.9) | 29 (24.8) |
| Suicide plan | 413 (6.5) | 135 (4.6) | 230 (7.4) | 27 (23.1) |
| Suicide attempt | 307 (4.8) | 99 (3.3) | 169 (5.4) | 19 (16.9) |
| Psychotic‐like symptoms, n (%) | N = 6163 | n = 2832 | n = 3047 | n = 114 |
| Paranoia | 778 (12.8) | 176 (6.2) | 516 (16.9) | 45 (39.5) |
| Auditory hallucinations | 1039 (16.9) | 317 (11.2) | 607 (19.9) | 53 (46.5) |
| Visual hallucinations | 808 (13.1) | 276 (9.7) | 449 (14.7) | 33 (28.9) |
| Alcohol use, n (%) | n = 6161 | n = 2831 | n = 3046 | n = 114 |
| Ever had standard drink | 860 (14.0) | 427 (15.1) | 381 (12.5) | 24 (21.1) |
| Standard drink in past 6 months | 634 (10.3) | 313 (11.0) | 289 (9.5) | 13 (11.4) |
| Ever had 5+ standard drinks | 211 (3.4) | 108 (3.8) | 93 (3.1) | <5 (<5) |
| Substance use in past 6 months, n (%) | N = 6156 | n = 2830 | n = 3042 | n = 114 |
| No drug use | 5333 (86.6) | 2430 (85.9) | 2664 (87.6) | 98 (86.0) |
| Cannabis | 140 (2.3) | 104 (3.7) | 83 (2.7) | 9 (7.9) |
| Tobacco | 215 (3.5) | 104 (3.7) | 88 (2.9) | 10 (8.8) |
| Amphetamines | 18 (0.3) | 9 (0.3) | <5 (<1) | <5 (<5) |
| Ecstasy | 33 (0.5) | 14 (0.5) | 13 (0.4) | <5 (<5) |
| Hallucinogens | 30 (0.5) | 13 (0.5) | 12 (0.4) | <5 (<5) |
| Sedatives | 26 (0.4) | 11 (0.4) | 12 (0.4) | <5 (<5) |
| Inhalants | 45 (0.7) | 20 (0.7) | 20 (0.7) | <5 (<5) |
| Other substance/s | 249 (4.0) | 93 (3.3) | 139 (4.6) | 7 (6.1) |
Note: Data are n and %. To protect the identities of individuals, values less than 5 are censored and reported as ‘<5'. Data are presented by gender identity.
4. DISCUSSION
The FPS cohort at baseline provides the most comprehensive, up‐to‐date Australian information about mental health during the early adolescent years since the last national survey, conducted almost a decade ago (Lawrence et al., 2015). Participant characteristics reported in this paper indicate that the FPS cohort is comparable to the Australian adolescent population in relation to gender, remoteness, Aboriginal and/or Torres Strait Islander identity, and LGBTQA + identity (see Table 3 for reference samples). To the best of our knowledge, this cohort provides the most comprehensive gender diversity prevalence data for adolescents under the age of 15 in Australia, something that has been omitted from previous studies, and similarly, furthers the field by providing detailed, large‐scale prevalence data about sexuality diversity for adolescents under 15 (Fisher et al., 2019; Mission Australia, 2021; VAHI, 2020).
The FPS cohort includes a relatively high proportion of Australian‐born adolescents who report speaking mostly English at home. It is well‐documented that culturally and linguistically diverse populations are underrepresented in health research for a range of reasons (Hughson et al., 2016; Smith et al., 2018). In the case of mental health research, these reasons may include language and communication barriers, as well as the stigma associated with accessing mental health services (Wohler & Dantas, 2017). The FPS cohort also includes more students who attend non‐government schools with a higher median ICSEA relative to students in the overall Australian population. Despite our best attempts to attract a representative sample by advertising widely, approaching all school types, and producing recruitment materials in multiple languages and formats, there is likely to be some degree of sampling bias due to the opt‐in nature of the study. Government schools represent 57.5% of the schools participating in the study, however, the opt‐in consent rate was higher from parents at non‐government schools. Having resources available at schools to devote to study recruitment, as well as household factors and parental availability, likely contributed to these differential consent rates, which is consistent with perspectives provided by school staff on this issue (Beames et al., submitted). Related to this point is that smartphone ownership was necessary for study inclusion, raising the possibility of sampling bias. At study commencement, estimates suggest 90% of Australian teenagers owned a smartphone (Nielsen, 2019), providing some parameters around the extent of this sampling bias risk.
Key findings from our initial baseline analyses showed that female and nonbinary adolescents had elevated symptom levels across all clinical measures relative to their male counterparts with effect sizes ranging from small (e.g., externalizing symptoms) to large (e.g., depression, anxiety, distress), with nonbinary participants faring worse than their female peers. Participants attending school in regional areas were more likely to reach clinical thresholds for depression and anxiety, and those attending less advantaged schools were more likely to report symptoms above clinical thresholds for depression, anxiety, and psychological distress, although the size of these effects for both variables were negligible. These results are in line with national data indicating that despite increased risk factors outside of metropolitan areas, prevalence rates for common mental illnesses do not differ between those living in metropolitan and regional areas of Australia (ABS, 2008). Members of minority and marginalized groups, including Aboriginal and/or Torres Strait Islander people and adolescents who were gender and/or sexuality diverse, were significantly more likely to report symptoms above clinical thresholds for depression, anxiety, psychological distress, and suicidal ideation. These effect sizes were in the small‐to‐medium range for gender and sexuality diversity and very small for Aboriginal and/or Torres Strait Islander identity, and align with existing estimates showing elevated mental health symptom levels among these groups (ABS, 2019; Russell & Fish, 2016; Strauss et al., 2020; VAHI, 2020). The FPS data extends what is known about young people by providing a reliable, population‐level estimate of the degree to which these groups show heightened symptoms, during the critical developmental phase of early adolescence.
The main strengths of the data reported in this study include the comprehensiveness of the self‐report information across a range of mental health and demographic domains, the representativeness of the sample, and the reporting of current prevalence estimates for common mental health symptoms and suicidality among Australian adolescents. There were significant mental health symptom levels reported in this cohort, with higher rates for some population groups (e.g., gender and sexuality diverse adolescents). The FPS will continue to monitor prevalence levels in these high‐risk groups, as well as the whole population, and will provide evidence about how mental health morbidity changes over time in adolescents.
The FPS cohort will advance knowledge by leveraging a broad range of data sources (e.g., self‐report, cognitive task performance, passively collected sensor data, government health and education records) to create a rich and detailed picture of the development of adolescent mental health conditions. Moreover, the large FPS sample will provide sound statistical power for future studies to examine predictors and mediators of mental health outcomes, and the ability to use advanced statistical approaches (e.g., latent class analysis, growth curve modeling) to identify subgroups of adolescents and individual trajectories of mental health and wellbeing. Data from the FPS cohort are likely to inform the targets of prevention and early intervention strategies well into the future, providing focus for more personalized and precision‐based approaches to mental health. While not the focus of the current paper, the embedded cRCT is one of the largest of its kind and will be able to answer questions about the effectiveness of digital prevention approaches, at scale (Werner‐Seidler et al., 2020).
There are several limitations associated with the FPS that need to be considered. First, using an opt‐in school, parent, and participant consent process likely led to some sampling biases which included a slightly more advantaged and less linguistically diverse sample relative to the general Australian population. Nonetheless, the study still reflects the Australian population with respect to gender, remoteness, and other diversity characteristics. Relatedly, adolescents who were not in formal schooling were not included in this cohort study. Second, by coincidence, baseline data were collected during 2019–2022. From 2020 to 2021, many regions of Australia were subject to varying levels of COVID‐19 related lockdowns and restrictions. It is within this context that the baseline data need to be considered. While a potential limitation given this broader context, this timeframe provides a unique opportunity to assess how young people fare over the long term after such significant disruption. Finally, the embedded cRCT may be a limitation of the cohort study if intervention effects on mental health outcomes are detected. If this is the case, the control arm (n = 3122) will comprise the sample to answer our core cohort study research questions. Although a limitation to the pure cohort study, if effects of the interventions are detected, there will be an opportunity to examine potential interaction of risk and protective factors on intervention effects.
The FPS cohort is expected to provide a major contribution to understanding different aspects of development, experience, and behavior as risk and/or protective factors for mental ill‐health and wellbeing during the adolescent years.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
We would like to offer our heartfelt thanks to the wonderful young people, their families and school communities who are participating in this study. This study would not have been possible without the enthusiasm, dedication and commitment from the wellbeing staff from our partner schools, including deputy principals, year advisors, school counselors, and student support officers among many others. A study of this scale also would not have been possible without the committed Black Dog Institute volunteers who have given up their time to support and facilitate the implementation of this study. We would also like to thank the Black Dog Institute Education, Marketing and Communications, and Information Technology teams, and the Deakin University team. This project was funded by a NHMRC Project Grant awarded to Helen Christensen (GNT1138405), a Ramsay Health Philanthropic Grant awarded to Helen Christensen and Aliza Werner‐Seidler, a donation made by General Pants Co, a NHMRC Emerging Leader Fellowship awarded to Aliza Werner‐Seidler (GNT1197074), a NHMRC Emerging Leader II Fellowship awarded to Alison Calear (GNT1173146), a SPRF NHMRC Fellowship to Helen Christensen (GNT1155614), a NHMRC Fellowship 1158707 to Philip Batterham, a NHMRC Emerging Leader II Fellowship awarded to Michelle Torok (GNT2007731), and funding from Financial Markets Foundation for Children awarded to Raghu Lingam.
Werner‐Seidler, A. , Maston, K. , Calear, A. L. , Batterham, P. J. , Larsen, M. E. , Torok, M. , O’Dea, B. , Huckvale, K. , Beames, J. R. , Brown, L. , Fujimoto, H. , Bartholomew, A. , Bal, D. , Schweizer, S. , Skinner, S. R. , Steinbeck, K. , Ratcliffe, J. , Oei, J.‐L. , Venkatesh, S. , … Christensen, H. (2023). The Future Proofing Study: Design, methods and baseline characteristics of a prospective cohort study of the mental health of Australian adolescents. International Journal of Methods in Psychiatric Research, 32(3), e1954. 10.1002/mpr.1954
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- Australian Bureau of Statistics (ABS) . (2008). National survey of mental health and wellbeing 2007: Summary of results. ABS cat no. 4326.0. Australian Bureau of Statistics. Retrieved from https://www.abs.gov.au/statistics/health/mental‐health/national‐study‐mental‐health‐and‐wellbeing/2007 [Google Scholar]
- Australian Bureau of Statistics (ABS) . (2019). National Aboriginal and Torres Strait Islander Health Survey: Statistics about long‐term health conditions, disability, lifestyle factors, physical harm and use of health services. Retrieved from https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/national‐aboriginal‐and‐torres‐strait‐islander‐health‐survey/latest‐release
- Australian Bureau of Statistics (ABS) . (2020). Causes of death. Retrieved from https://www.abs.gov.au/statistics/health/causes‐death/causes‐death‐australia/2020
- Australian Bureau of Statistics (ABS) . (2022a). National study of mental health and wellbeing. Retrived from https://www.abs.gov.au/statistics/health/mental‐health/national‐study‐mental‐health‐and‐wellbeing/latest‐release
- Australian Bureau of Statistics (ABS) . (2022b). Data on students, staff, schools, rates and ratios for government and non‐government schools, for all Australian states and territories. Retrieved from https://www.abs.gov.au/statistics/people/education/schools/latest‐release
- Australian Bureau of Statistics (ABS) . (2022c). Census 2021: Information on Aboriginal and Torres Strait Islander peoples including language and ancestry. Retrieved from https://www.abs.gov.au/statistics/people/aboriginal‐and‐torres‐strait‐islander‐peoples/aboriginal‐and‐torres‐strait‐islander‐people‐census/latest‐release
- Australian Bureau of Statistics (ABS) . (2022d). Census 2021: Information on country of birth, year of arrival, ancestry, language and religion. Retrieved from https://www.abs.gov.au/statistics/people/people‐and‐communities/cultural‐diversity‐census/latest‐release
- Australian Bureau of Statistics (ABS) . (2022e). Census 2021: Information on sex and age. Retrieved from https://www.abs.gov.au/statistics/people/population/population‐census/2021
- Australian Curriculum, Assessment and Reporting Authority (ACARA) . (2020). Guide to understanding the index of community socio‐educational advantage (ICSEA). Retrieved from https://www.myschool.edu.au/media/1820/guide‐to‐understanding‐icsea‐values.pdf
- Australian Curriculum, Assessment and Reporting Authority (ACARA) . (2021). Number and proportion of students enrolled in schools by school level and school sector. Retrieved from https://www.acara.edu.au/reporting/national%2Dreport%2Don%2Dschooling%2Din%2Daustralia/national%2Dreport%2Don%2Dschooling%2Din%2Daustralia%2Ddata%2Dportal/student%2Dnumbers%23view1
- Australian Institute of Health and Welfare (AIHW) . (2004). Rural, regional and remote health: A guide to remoteness classifications. AIHW cat. no. PHE 53. AIHW. Retrieved from https://www.aihw.gov.au/reports/rural‐remote‐australians/guide‐to‐remoteness‐classifications/summary [Google Scholar]
- Australian Institute of Health and Welfare (AIHW) . (2021). Demographics of Australian young people and their families. Retrieved from https://www.aihw.gov.au/reports/children‐youth/australias‐youth/contents/demographics
- Barnett, S. , Huckvale, K. , Christensen, H. , Venkatesh, S. , Mouzakis, K. , & Vasa, R. (2019). Intelligent sensing to inform and learn (InSTIL): A scalable and governance‐aware platform for universal, smartphone‐based digital phenotyping for research and clinical applications. Journal of Medical Internet Research, 21(11), e16399. 10.2196/16399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham, P. J. , Sunderland, M. , Carragher, N. , Calear, A. L. , Mackinnon, A. J. , & Slade, T. (2016). The Distress Questionnaire‐5: Population screener for psychological distress was more accurate than the K6/K10. Journal of Clinical Epidemiology, 71, 35–42. 10.1016/j.jclinepi.2015.10.005 [DOI] [PubMed] [Google Scholar]
- Beames, J. R. , Lingam, R. , Boydell, K. , Calear, A. L. , Torok, M. , Maston, K. , Zbukvic, I. , Huckvale, K. , Batterham, P. J. , Christensen, H. , & Werner‐Seidler, A. (2021). Protocol for the process evaluation of a complex intervention delivered in schools to prevent adolescent depression: The future proofing study. BMJ Open, 11(1), e042133. 10.1136/bmjopen-2020-042133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beames, J. R. , Werner‐Seidler, A. , Hodgins, M. , Brown, L. , Fujimoto, H. , Bartholomew, A. , Maston, K. , Huckvale, K. , Zbukvic, I. , Torok, M. , Christensen, H. , Batterham, PJ. , Calear, AL. , Lingam, R. , & Boydell, K. M. (submitted Sept 2022). A qualitative inquiry of implementation factors in the Future Proofing study, a depression prevention program for Australian secondary schools. [DOI] [PMC free article] [PubMed]
- Beesdo‐Baum, K. , Voss, C. , Venz, J. , Hoyer, J. , Berwanger, J. , Kische, H. , Ollmann, T. M. , & Pieper, L. (2020). The Behavior and Mind Health (BeMIND) study: Methods, design and baseline sample characteristics of a cohort study among adolescents and young adults. International Journal of Methods in Psychiatric Research, 29(1), e1804. 10.1002/mpr.1804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. Statistical power and anlysis for the behavoiural sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Costello, E. J. , Copeland, W. , & Angold, A. (2011). Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, 52(10), 1015–1025. 10.1111/j.1469-7610.2011.02446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P. , Pineda, B. S. , Quero, S. , Karyotaki, E. , Struijs, S. Y. , Figueroa, C. A. , Llamas, J. A. , Furukawa, T. A. , & Munoz, R. F. (2021). Psychological interventions to prevent the onset of depressive disorders: A meta‐analysis of randomized controlled trials. Clinical Psychological Review, 83, 101955. 10.1016/j.cpr.2020.101955 [DOI] [PubMed] [Google Scholar]
- De la Torre‐Luque, A. , Fiol‐Veny, A. , Balle, M. , Nelemans, S. A. , & Bornas, X. (2020). Anxiety in early adolescence: Heterogeneous developmental trajectories, associations with risk factors and depressive symptoms. Child Psychiatry and Human Development, 51(4), 527–541. 10.1007/s10578-019-00936-y [DOI] [PubMed] [Google Scholar]
- Ellis, R. E. , Seal, M. L. , Simmons, J. G. , Whittle, S. , Schwartz, O. S. , Byrne, M. L. , & Allen, N. B. (2017). Longitudinal trajectories of depression symptoms in adolescence: Psychosocial risk factors and outcomes. Child Psychiatry and Human Development, 48(4), 554–571. 10.1007/s10578-016-0682-z [DOI] [PubMed] [Google Scholar]
- Erskine, H. E. , Moffitt, T. E. , Copeland, W. E. , Costello, E. J. , Ferrari, A. J. , Patton, G. , Degenhardt, L. , Vos, T. , Whiteford, H. A. , & Scott, J. G. (2015). A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychological Medicine, 45(7), 1551–1563. 10.1017/s0033291714002888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, C. M. , Waling, A. , Kerr, L. , Bellamy, R. , Ezer, P. , Mikolajczak, G. , Brown, G. , Carman, M. , & Lucke, J. (2019). 6th national survey of Australian secondary students and sexual health 2018. Australian Research Centre in Sex, Health & Society, La Trobe University. (ARCSHS Monograph Series No. 113). [Google Scholar]
- Forsman, A. K. , Wahlbeck, K. , Aarø, L. E. , Alonso, J. , Barry, M. M. , Brunn, M. , Cardoso, G. , Cattan, M. , de Girolamo, G. , Eberhard‐Gran, M. , Evans‐Lacko, S. , Fiorillo, A. , Hansson, L. , Haro, J. M. , Hazo, J.‐B. , Hegerl, U. , Katschnig, H. , Knappe, S. , Luciano, M. , … Roamer Consortium (2015). Research priorities for public mental health in Europe: Recommendations of the ROAMER project. The European Journal of Public Health, 25(2), 249–254. 10.1093/eurpub/cku232 [DOI] [PubMed] [Google Scholar]
- Garavan, H. , Bartsch, H. , Conway, K. , Decastro, A. , Goldstein, R. Z. , Heeringa, S. , Jernigan, T. , Potter, A. , Thompson, W. , & Zahs, D. (2018). Recruiting the ABCD sample: Design considerations and procedures. Developmental Cognitive Neuroscience, 32, 16–22. 10.1016/j.dcn.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grootendorst‐van Mil, N. H. , Bouter, D. C. , Hoogendijk, W. J. , van Jaarsveld, S. F. , Tiemeier, H. , Mulder, C. L. , & Roza, S. J. (2021). The iBerry study: A longitudinal cohort study of adolescents at high risk of psychopathology. European Journal of Epidemiology, 36(4), 453–464. 10.1007/s10654-021-00740-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, K. M. (2013). The add health study: Design and accomplishments. 10.17615/C6TW87 (Accessed 15 March 2022). [DOI]
- Hughson, J.‐a. , Woodward‐Kron, R. , Parker, A. , Hajek, J. , Bresin, A. , Knoch, U. , Phan, T. , & Story, D. (2016). A review of approaches to improve participation of culturally and linguistically diverse populations in clinical trials. Trials, 17(1), 1–10. 10.1186/s13063-016-1384-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, J. G. , Harris, E. S. , Spitzer, R. L. , & Williams, J. B. (2002). The patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. Journal of Adolescent Health, 30(3), 196–204. 10.1016/s1054-139x(01)00333-0 [DOI] [PubMed] [Google Scholar]
- Karcher, N. R. , & Barch, D. M. (2020). The ABCD study: Understanding the development of risk for mental and physical health outcomes. Neuropsychopharmacology, 15, 1–12. 10.1038/s41386-020-0736-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keppel, G. Design and analysis: A reseacher’s handbook. Prentice Hall. [Google Scholar]
- Klaufus, L. , Verlinden, E. , van der Wal, M. , Cuijpers, P. , Chinapaw, M. , & Smit, F. (2022). Adolescent anxiety and depression: Burden of disease study in 53,894 secondary school pupils in The Netherlands. BMC Psychiatry, 22(1), 225. 10.1186/s12888-022-03868-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korczak, D. J. , & Goldstein, B. I. (2009). Childhood onset major depressive disorder: Course of illness and psychiatric comorbidity in a community sample. The Journal of Pediatrics, 155(1), 118–123. 10.1016/j.jpeds.2009.01.061 [DOI] [PubMed] [Google Scholar]
- Lawrence, D. , Johnson, S. , Hafekost, J. , de Hann, K. B. , Sawyer, M. , Ainley, J. , & Zubrick, S. R. (2015). The mental health of children and adolescents: Report on the second Australian child and adolescent survey of mental health and wellbeing. Department of Health. Retrieved from https://www.health.gov.au/sites/default/files/documents/2020/11/the‐mental‐health‐of‐children‐and‐adolescents_0.pdf [Google Scholar]
- Merry, S. N. , Stasiak, K. , Shepherd, M. , Frampton, C. , Fleming, T. , & Lucassen, M. F. (2012). The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: Randomised controlled non‐inferiority trial. BMJ, 344, e2598. 10.1136/bmj.e2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mission Australia . (2021). Mission Australia youth survey report. Retrieved from https://www.missionaustralia.com.au/what‐we‐do/research‐impact‐policy‐advocacy/youth‐survey
- Mueller, T. I. , Leon, A. C. , Keller, M. B. , Solomon, D. A. , Endicott, J. , Coryell, W. , Warshaw, M. , & Maser, J. D. (1999). Recurrence after recovery from major depressive disorder during 15 years of observational follow‐up. American Journal of Psychiatry, 156(7), 1000–1006. 10.1176/ajp.156.7.1000 [DOI] [PubMed] [Google Scholar]
- Muller, S. R. , Peters, H. , Matz, S. C. , Wang, W. , & Harari, G. M. (2020). Investigating the relationships between mobility behaviours and indicators of subjective well‐being using smartphone‐based experience sampling and GPS tracking. European Journal of Personality, 34(5), 714–732. 10.1002/per.2262 [DOI] [Google Scholar]
- Neufeld, S. A. S. , Dunn, V. J. , Jones, P. B. , Croudace, T. J. , & Goodyer, I. M. (2017). Reduction in adolescent depression after contact with mental health services: A longitudinal cohort study in the UK. The Lancet Psychiatry, 4(2), 120–127. 10.1016/s2215-0366(17)30140-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen and iab Australia . (2019). Device ownership & trends. Retrieved from https://iabaustralia.com.au/wp‐content/uploads/2019/12/IAB_Device‐Ownership_July‐2019.pdf
- Perry, Y. , Werner‐Seidler, A. , Calear, A. , Mackinnon, A. , King, C. , Scott, J. , Merry, S. , Fleming, T. , Stasiak, K. , Christensen, H. , & Batterham, P. J. (2017). Preventing depression in final year secondary students: School‐based randomized controlled trial. Journal of Medical Internet Research, 19(11), e369. 10.2196/jmir.8241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanczyk, G. V. , Salum, G. A. , Sugaya, L. S. , Caye, A. , & Rohde, L. A. (2015). Annual research review: A meta‐analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Psychology and Psychiatry, 53(3), 345–365. 10.1111/jcpp.12381 [DOI] [PubMed] [Google Scholar]
- Russell, S. T. , & Fish, J. N. (2016). Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annual Review of Clinical Psychology, 12(1), 465–487. 10.1146/annurev-clinpsy-021815-093153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanson, A. , Nicholson, J. , Ungerer, J. , Zubrick, S. , Wilson, K. , Ainley, J. , Berthelsen, D. , Bittman, M. , Broom, D. , Harrison, L. , Rodgers, B. , Sawyer, M. , Silburn, S. , Strazdins, L. , Vimpani, G. , & Wake, M. (2002). Introducing the longitudinal study of Australian children. LSAC Discussion Paper No.1. Retrieved from https://growingupinaustralia.gov.au/sites/default/files/discussionpaper1.pdf
- Scholtens, S. , Smidt, N. , Swertz, M. A. , Bakker, S. J. , Dotinga, A. , Vonk, J. M. , Van Dijk, F. , van Zon, S. K. , Wijmenga, C. , Wolffenbuttel, B. H. , & Stolk, R. P. (2015). Cohort profile: LifeLines, a three‐generation cohort study and biobank. International Journal of Epidemiology, 44(4), 1172–1180. 10.1093/ije/dyu229 [DOI] [PubMed] [Google Scholar]
- Shorey, S. , Ng, E. D. , & Wong, C. H. J. (2022). Global prevalence of depression and elevated depressive symptoms among adolescents: A systematic review and meta‐analysis. British Journal of Clinical Psychology, 61(2), 287‐305. 10.1111/bjc.12333 [DOI] [PubMed] [Google Scholar]
- Slade, T. , Johnston, A. , Oakley Browne, M. A. , Andrews, G. , & Whiteford, H. (2009). 2007 national survey of mental health and wellbeing: Methods and key findings. Australian and New Zealand Journal of Psychiatry, 43(7), 594–605. 10.1080/00048670902970882 [DOI] [PubMed] [Google Scholar]
- Smith, A. B. , Agar, M. , Delaney, G. , Descallar, J. , Dobell‐Brown, K. , Grand, M. , Aung, J. , Patel, P. , Kaadan, N. , & Girgis, A. (2018). Lower trial participation by culturally and linguistically diverse (CALD) cancer patients is largely due to language barriers. Asia‐Pacific Journal of Clinical Oncology, 14(1), 52–60. 10.1111/ajco.12818 [DOI] [PubMed] [Google Scholar]
- Solmi, M. , Radua, J. , Olivola, M. , Croce, E. , Soardo, L. , Salazar de Pablo, G. , Il Shin, J. , Kirkbride, J. B. , Jones, P. , Kim, J. H. , Kim, J. Y. , Carvalho, A. F. , Seeman, M. V. , Correll, C. U. , & Fusar‐Poli, P. (2022). Age at onset of mental disorders worldwide: Large‐scale meta‐analysis of 192 epidemiological studies. Molecular Psychiatry, 27(1), 281–295. 10.1038/s41380-021-01161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence, S. H. (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36(5), 545–566. 10.1016/s0005-7967(98)00034-5 [DOI] [PubMed] [Google Scholar]
- Spence, S. H. , Barrett, P. M. , & Turner, C. M. (2003). Psychometric properties of the spence children's anxiety scale with young adolescents. Journal of Anxiety Disorders, 17(6), 605–625. 10.1016/s0887-6185(02)00236-0 [DOI] [PubMed] [Google Scholar]
- Spence, S. H. , Sawyer, M. G. , Sheffield, J. , Patton, G. , Bond, L. , Graetz, B. , & Kay, D. (2014). Does the absence of a supportive family environment influence the outcome of a universal intervention for the prevention of depression? International Journal of Environmental Research and Public Health, 11(5), 5113–5132. 10.3390/ijerph110505113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings, E. , Degenhardt, L. , Dobbins, T. , Lee, Y. , Erskine, H. , Whiteford, H. , & Patton, G. (2015). Preventing depression and anxiety in young people: A review of the joint efficacy of universal, selective and indicated prevention. Psychological Medicine, 46(1), 11–26. 10.1017/s0033291715001725 [DOI] [PubMed] [Google Scholar]
- Strauss, P. , Cook, A. , Winter, S. , Watson, V. , Wright Toussaint, D. , & Lin, A. (2020). Mental health issues and complex experiences of abuse among trans and gender diverse young people: Findings from Trans Pathways. LGBT Health, 7(3), 128–136. 10.1089/lgbt.2019.0232 [DOI] [PubMed] [Google Scholar]
- Van Spijker, B. A. , Batterham, P. J. , Calear, A. L. , Farrer, L. , Christensen, H. , Reynolds, J. , & Kerkhof, A. J. (2014). The suicidal ideation attributes scale (SIDAS): Community‐based validation study of a new scale for the measurement of suicidal ideation. Suicide and Life‐Threatening Behavior, 44(4), 408–419. 10.1111/sltb.12084 [DOI] [PubMed] [Google Scholar]
- van Zoonen, K. , Buntrock, C. , Ebert, D. D. , Smit, F. , Reynolds, C. F. , Beekman, A. T. F. , & Cuijpers, P. (2014). Preventing the onset of major depressive disorder: A meta‐analytic review of psychological interventions. International Journal of Epidemiology, 43(2), 318–329. 10.1093/ije/dyt175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victorian Agency for Health Information (VAHI) . (2020). The health and wellbeing of the lesbian, gay, bisexual, transgender, intersex and queer population in Victoria: Findings from the Victorian Population Health Survey 2017. Retrieved from https://www.safercare.vic.gov.au/sites/default/files/2020‐09/The‐health‐and‐wellbeing‐of‐the‐LGBTIQ‐population‐in‐Victoria.pdf
- Werner‐Seidler, A. , Huckvale, K. , Larsen, M. E. , Calear, A. L. , Maston, K. , Johnston, L. , Torok, M. , O’Dea, B. , Batterham, P. J. , Schweizer, S. , Skinner, S. R. , Steinbeck, K. , Ratcliffe, J. , Oei, J. , Patton, G. , Wong, I. , Beames, J. , Wong, Q. J. , Lingham, R. , … Christensen, H. (2020). A trial protocol for the effectiveness of digital interventions for preventing depression in adolescents: The Future Proofing Study. Trials, 21(1), 1–21. 10.1186/s13063-019-3901-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner‐Seidler, A. , Li, S. H. , Spanos, S. , Johnston, L. , O’Dea, B. , Torok, M. , Ritterband, L. , Newby, J. M. , Mackinnon, A. J. , & Christensen, H. (submitted). The effects of a sleep‐focused smartphone application on insomnia and depressive symptoms: A randomised controlled trial and mediation analysis. [DOI] [PMC free article] [PubMed]
- Werner‐Seidler, A. , Spanos, S. , Calear, A. L. , Perry, Y. , Torok, M. , O'Dea, B. , Christensen, H. , & Newby, J. M. (2021). School‐based depression and anxiety prevention programs: An updated systematic review and meta‐analysis. Clinical Psychology Review, 89, 102079. 10.1016/j.cpr.2021.102079 [DOI] [PubMed] [Google Scholar]
- Werner‐Seidler, A. , Wong, Q. , Johnston, L. , O'Dea, B. , Torok, M. , & Christensen, H. (2019). A pilot evaluation of the sleep Ninja – A smartphone‐application for adolescent insomnia symptoms. BMJ Open, 9(5), e026502. 10.1136/bmjopen-2018-026502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen, H. U. , Knappe, S. , & Schumann, G. (2014). The psychological perspective on mental health and mental disorder research: Introduction to the ROAMER work package 5 consensus document. International Journal of Methods in Psychiatric Research, 23(S1), 15–27. 10.1002/mpr.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohler, Y. , & Dantas, J. A. (2017). Barriers accessing mental health services among culturally and linguistically diverse (CALD) immigrant women in Australia: Policy implications. Journal of Immigrant and Minority Health, 19(3), 697–701. 10.1007/s10903-016-0402-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


