Summary
Background
The burden of cardiovascular diseases (CVDs) is on the rise in China, yet a comprehensive and systematic understanding of the temporal trends and distribution of CVD burden attributable to dietary factors across the provinces remains elusive. This study endeavors to provide a comprehensive depiction of the burden of CVDs attributable to dietary risk factors across China’s geographical regions from 2002 to 2018.
Methods
Data from the China National Nutrition Surveys, the China Chronic Disease and Risk Factor Surveillance, the Hypertension Survey, and the Chinese Centre for Disease Control and Prevention cause-of-death reporting system were used to estimate the intake of dietary factor, the number of deaths, and disability-adjusted life years (DALYs), mortality rate, for ischemic heart disease (IHD), ischemic stroke (IS), hemorrhage and other stroke (HOS) attributable to dietary factors at national and provincial levels in China from 2002 to 2018. Using a comparative risk assessment approach, we estimated the proportion of CVDs burden attributable to suboptimal intake of seven dietary factors, both individually and collectively, among Chinese citizens aged 20 years or older.
Finding
The mean consumption of whole grains, soybeans, nuts, vegetables, fruits, red meat, and sugar-sweetened beverages (SSBs) exhibited an upward trend from 2002 to 2018. However, with the exception of red meat and SSBs, the average intake remained below the levels recommended levels outlined in the Chinese national dietary guidelines. Inadequate fruit, whole grain, and vegetables intake were the leading dietary risk factors for IHD, IS and HOS in China, while nuts, soybean and SSB were only associated with IHD mortality. From 2002 to 2018, the number of deaths and mortality rate for CVDs attributable to suboptimal diet among Chinese males were greater than that of females. With increasing age, the diet-related mortality rate for CVDs increased substantially. In 2018, the nationwide mortality rate attributable to diet was found to be 77.9 (95% UI, 77.5–78.1) per 100,000 population for IHD, 34.1 (95% UI, 33.8–34.2) for IS, and 32.8 (95% UI, 32.4–32.8) for HOS. Suboptimal diet was responsible for 16.0 million (95% UI, 13.8–18.4) DALYs and 1137.1 (95% UI, 980.4–1312.3) DALYs per 100,000 population for stroke, and 13.9 million (95% UI, 11.8–16.3) DALYs and 990.2 (95% UI, 841.2–1158.6) DALYs for IHD. Across the provinces of China, in 2018, the highest age-standardized mortality rates of all diet-related deaths were observed in Shandong (92.8 [95% UI, 89.9–93.3]) for IHD, Heilongjiang (38.1 [95% UI, 36.2–38.8]) for IS, and Tibet (68.3 [95% UI, 65.0–70.1]) for HOS. The highest diet related DALYs were observed in Henan (1.4 million [95% UI, 1.2–1.6] for IS, and 1.3 million [95% UI, 1.1–1.5] for IHD).
Interpretation
This study provides a comprehensive picture of the geographic variation and temporal trends of the burden of CVDs attributable to dietary risk factors at the national and provincial levels from 2002 to 2018 in China, highlighting the need for geographically targeted intervention strategies to improve the quality of diet and reduce the diet-related burden of CVDs.
Funding
National Key Research and Development Program of China (2018YFC1315303), National Natural Science Foundation of China (82103966).
Keywords: Dietary, Disease burden, Cardiovascular disease, China
Research in context.
Evidence before this study
We searched PubMed, Embase, Web of Science, and Google Scholar for articles published up to October 31, 2022, using a combination of the following terms: (“dietary risk factors” OR “diet” OR “food” OR “nutrition”) AND (“cardiovascular disease” OR “heart disease” OR “stroke”) AND (“death” OR “mortality” OR “burden”) AND (“China” OR “Chinese”), with the language restricted to English and Chinese. Previous studies, including our own previous publications, has demonstrated that dietary factors were one of the leading behavioral risk factors for morbidity, mortality and the burden of cardiovascular disease associated with the dietary transition in China. However, these studies had limitations, such as non-representative samples or a failure to consider the diet-related burden of different types of cardiovascular disease. Given the substantial heterogeneity in cardiovascular disease burden across the 31 provinces of mainland China over time, it is necessary to conduct a comprehensive assessment of the burden of diet-related cardiovascular disease over an extended period of time at both national and provincial levels.
Added value of this study
We employed a unified definition of dietary factors and utilized nationally representative individual-level dietary data to comprehensively estimate the burden of cardiovascular diseases deaths related to suboptimal diet among Chinese citizens from 2002 to 2018. Nationally, the diet-related cardiovascular disease mortality rate increased for ischemic heart disease and ischemic stroke from 2002 to 2018. In recent years, suboptimal diet was responsible for 16.0 million disability-adjusted life years (DALYs) for stroke and 13.9 million DALYs for ischemic heart disease. There were notable geographical variations in the burden of cardiovascular disease and its subcategories attributable to suboptimal diet across the provinces of China. In 2018, the highest age-standardized mortality rates of all diet-related deaths were observed in Shandong for ischemic heart disease, Heilongjiang for ischemic stroke, and Tibet for hemorrhage and other stroke. The highest diet related DALYs were observed in Henan for both ischemic heart disease and ischemic stroke. The number of deaths and mortality rate for CVDs attributable to suboptimal diet were higher in male than that in female among Chinese from 2002 to 2018. Additionally, diet-related mortality rate for CVDs increased substantially with the increasing age.
Implications of all the available evidence
Suboptimal diet remains an important risk factor for cardiovascular disease in China. The geographic variation and temporal trends of the burden of different cardiovascular disease categories attributable to dietary risk factors observed emphasize the need for geographically targeted intervention strategies aimed at improving the quality of diet and reducing the diet-related burden of cardiovascular disease.
Introduction
Cardiovascular diseases (CVDs), primarily ischemic heart disease (IHD), hemorrhagic stroke and ischemic stroke (IS), are the leading cause of death in China, accounting for 43.0% of total deaths and 24.1% of total disability-adjusted life years (DALYs) for both genders combined in 2019.1 The estimated number of CVDs deaths in China rose from 3.1 million in 2005 to 4.6 million in 2020, and the burden of CVDs-related premature remained high.2 Diet plays an essential role among the many known risk factors for CVDs.3 In the past decades, efforts have been made to clarify the link between dietary and CVDs.4, 5, 6, 7, 8, 9, 10, 11, 12 Globally, suboptimal diet is the one of the leading behavioral factor of mortality, and optimal diets are believed to be an effective and modifiable lever for reducing the burden of CVDs.13,14
Due to the complexities of characterizing dietary consumption across different countries, and the transitions of dietary and demographic in China over the past several decades, the majority of existing results pertain to populations from other countries.12,15 According to previous study, in 2017, among the world’s 20 most populous countries, China had the highest age-standardized rates of diet-related cardiovascular disease deaths.3 In recent years, there is a growing emphasis on addressing the burden of diet-related CVDs in China. In addition, geographical patterns for the burden of total CVDs and their subcategories over time were observed to be markedly heterogeneity,2,16,17 whereas there was limited evidence for a comprehensive assessment of the temporal trend in the burden of diet-related CVDs at the provincial level. Knowledge of the burden of CVDs attributable to dietary risks at the province level will provide government and policy makers insight in framing health-care policies and implementing effective disease prevention strategies for CVDs at both national and provincial levels.
Therefore, the aim of this study is to comprehensively depict the burden of CVDs attributable to different dietary risk factors in the geographical profile across China from 2002 to 2018.
Methods
Study design and participants/overview
The analysis and findings regarding dietary intake presented in this study were derived from three national representative surveys: the China National Nutrition Surveys (CNNS),18 the China Chronic Disease and Risk Factor Surveillance (CCDRFS)19 and the China Hypertension Survey (CHPS).20 The data sources for the year 2002 were CNNS, for the year 2010 and 2015 were CNNS, CCDRFS and CHPS, and for the year 2018 were CCDRFS. Stratified and multi-stage cluster random sampling was used for all three surveys. We ensured the quality of the data by conducting a standardized training of investigators who have extensive experience in dietary investigations and have conducted epidemiological investigations for many years. For this analysis, we restricted the study sample to adults aged 20 years or older with food consumption information. Mortality data were obtained from the Chinese Centre for Disease Control and Prevention cause-of-death reporting system.17,21,22 All data utilized in this study were aggregated and did not have personally identifiable information. A comprehensive description of the design and data sources has been reported elsewhere18, 19, 20 and is summarized in Appendix 2 (pp 1–2).
Estimating food consumption
The food frequency questionnaire (FFQ) was used to collect dietary information, as described in detail previously.18,19 Intake was treated as a continuous variable and expressed in grams (g) per person per day. Fourteen dietary risk factors were initially selected in the analysis, including refined grain, whole grain, tuber, soybean, nuts, total vegetable, fruit, red meat, red meat product, total dairy, low fat dairy, egg, fish, sugar-sweetened beverages (SSB). We selected whole grain, soybean, nuts, vegetable, fruit, red meat, and SSB from the 14 dietary risk factors associated with CVDs though pooled prospective cohort studies conducted in the global burden of disease (GBD) study. Linear model was used to interpolate the absent data for whole grains, soybeans and nuts intake in 2018.
Definitions of disease categories
Deaths and mortality from CVDs subcategories were classified based on the International Classification of Disease 10th revision (ICD-10). In this study, IHD includes diseases coded as I20–I25.9, IS includes diseases coded as I63–I63.9, I65–I66.9, I67.2–I67.3, I67.5–I67.6, I69.3, hemorrhage and other stroke (HOS) includes diseases coded as I60–I62.9, I67.0–I67.1, I68.1–I68.2, I69.0–I69.2.
Statistical analysis
To quantify the CVDs burden attributable to dietary risks, the number of deaths, age-standardized rate (ASR), population attributable fraction (PAF), and disability-adjusted life years (DALYs) and annual change were adopted. Age-standardized PAF mortality rates and DALYs rates were calculated based on the standard population in 2010 census data constructed by the National Bureau of Statistics. We estimated the PAF for individual components and the overall effect of all dietary factors relevant to each outcome based on the following formulas3,12:
where RR(x) stands for the relative risk of cause-specific mortality at exposure level x, P(x) stands for the population distribution of exposure, P′(x) stands for the counterfactual distribution of exposure, m stands for the maximum exposure level, i stands for the specific risk factor, and n stands for the total number of risk factor. The annual change based on the formula: , where final stands for the food intake of the ending year, start stands for the food intake of the start year, and n stands for the number of years. The numbers of deaths, PAFs, mortality rates, and DALYs for each of the causes of cardiovascular disease attributable to suboptimal diet were computed by age, sex, year, and province. Consistent with previous research in China,23,24 this study categorizes the 31 provinces into five health areas. Health area one includes provinces (Beijing, Shanghai, Tianjin, and Zhejiang) with lowest mortality and high life expectancies; health area two includes provinces (Fujian, Guangdong, Hainan, Hubei, Hunan, and Jiangsu) with relatively high life expectancy and the lowest mortality rates due to CVDs but higher mortality rates due to cancer or COPD; provinces in health area three (including Anhui, Hebei, Heilongjiang, Henan, Inner Mongolia, Jilin, Liaoning, Ningxia, Shaanxi, Shandong, and Shanxi) are characterized by middle life expectancy and higher levels of mortality due to CVDs; provinces in health area four (including Chongqing, Gansu, Jiangxi, Sichuan, and Yunnan) have lower than average life expectancy but low mortality from CVDs and high mortality from COPD; health area five (including Guangxi, Guizhou, Qinghai, Tibet, and Xinjiang) has low average life expectancy and high mortality.
The uncertainty of parameters was estimated using the Monte Carlo simulation method. All calculations were repeated 1000 times using one draw of each parameter at each iteration, assuming that the distribution of the food intake and the mortality rate data were normal based on the central limit theorem.25,26
All statistical analyses were performed using SAS software 9.4 (SAS Institute Inc., Cary, NC, USA), unless otherwise stated. Graphs were plotted using GraphPad Prism version 9 for Windows (San Diego, California, USA). The uncertainty interval was estimated using @RISK 8.1 (Palisade Corp., Ithaca, NY).
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
Results
Consumption of major foods, 2002–2018
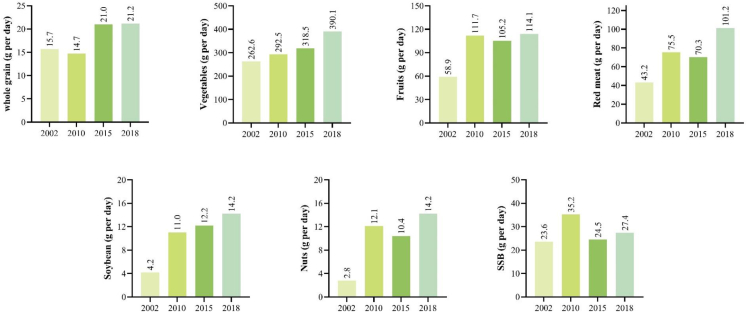
The average daily food intake varied by province and year (Fig. 1, Supplementary Table S1). In 2018, the average intake of whole grain was 21.2 g/d, varied from 3.7 g/d (Hunan) to 56.0 g/d (Hebei) by the provinces; vegetable intake was 390.1 g/d, varied from 286.3 g/d (Inner Mongolia) to 546.5 g/d (Hubei); and fruit intake was 114.1 g/d, varied from 76.8 g/d (Hainan) to 206.9 g/d (Tianjin). The average intake of red meat, soybeans, nuts, and sugar-sweetened beverages (SSB) by the provinces in 2018 ranged from 31.3 g/d (Shaanxi) to 341.6 g/d (Tibet), 4.1 g/d (Tibet) to 24.1 g/d (Shanxi), 5.1 g/d (Hainan) to 26.8 g/d (Xinjiang), and 12.2 g/d (Shanxi) to 67.0 g/d (Tibet), respectively (Supplementary Table S1).
Fig. 1.
Consumption of foods selected among Chinese adults in 2002, 2010, 2015, and 2018.
The average intake of these foods increased from 2002 to 2018 (Fig. 1), but with the exception of red meat and SSB, most of them are still below the Chinese national dietary recommendations. The disparities between current and optimal intake were widest for whole grains and fruits, with mean consumption at 14.1%∼42.4% and 32.6%∼57.1% of the optimal levels, respectively. Compared to 2002, the average intake of nuts was increased by 407.1%, soy by 238.1%, red meat by 134.3%, fruits by 93.7%, vegetables by 48.6%, whole grains by 35.0%, and SSB by 16.1% in 2018.
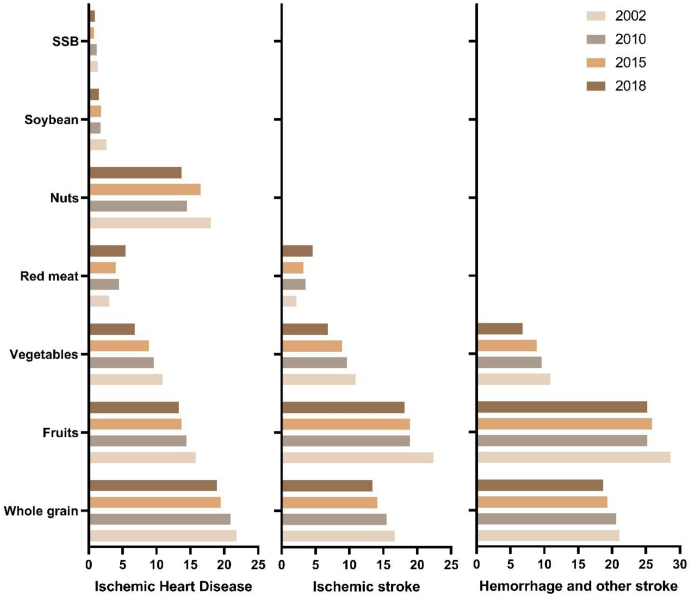
Population attributable fraction of CVDs mortality to selected foods, 2002–2018
Inadequate intake of fruit, whole grains, and vegetables intake were the primary dietary risk factors for ischemic heart disease, ischemic stroke, hemorrhage, and other stroke; low intake of nuts and soybean, and high intake of SSB were only associated with IHD mortality in China (Fig. 2). In 2018, diet low in fruits was the first leading dietary risk factor for IS and HOS, with respective PAFs of 18.1% and 25.2%, respectively, followed by diet low in whole grains (IS: 13.4%, HOS: 18.7%). While low whole grain intake was the first leading dietary risk factors for IHD and was associated with a PAF of 21.8% in 2002, it was associated with a PAF of 18.9% in 2018; and lower nuts intake was the second dietary risk factors for IHD and was associated with a PAF of 18.0% in 2002 and 13.7% in 2018. From 2002 to 2018, the population fraction of cardiovascular diseases mortality attributed to diet low in whole grains, fruits, vegetables, nuts, soybean, and diet high in SSB decreased, with the exception of diet high in red meat. In 2002, the population fraction of IHD and IS mortality attributed to diet high in red meat was 3.0% and 2.2%, respectively; by 2018, these proportions had increased to 5.4% and 4.6%, respectively.
Fig. 2.
Proportion of cardiovascular diseases mortality attributed to selected foods among Chinese adults in 2002, 2010, 2015, and 2018.
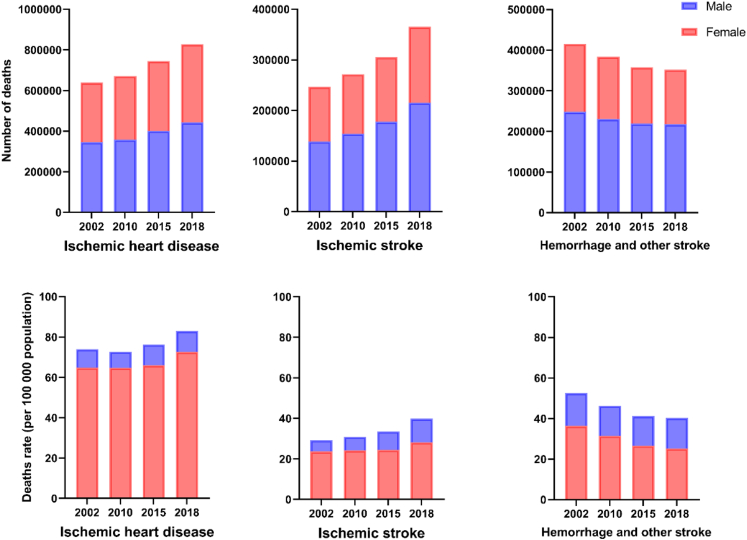
Overall impact of diet on the burden of CVDs in 2002–2018 across China and its province
In 2018, diet related IHD deaths (827,474) were highest among CVDs followed by IS (365,475), and HOS (351,905). The diet-related mortality rate was 77.9 (95% UI, 77.5–78.1) per 100,000 population for IHD, 34.1 (95% UI, 33.8–34.2) for IS, and 32.8 (95% UI, 32.4–32.8) for HOS, respectively (Fig. 3). Suboptimal diet was responsible for 16.0 million (95% UI, 13.8–18.4) DALYs and 1137.1 (95% UI, 980.4–1312.3) DALYs per 100,000 population for stroke, and 13.9 million (95% UI, 11.8–16.3) DALYs and 990.2 (95% UI, 841.2–1158.6) DALYs for IHD.
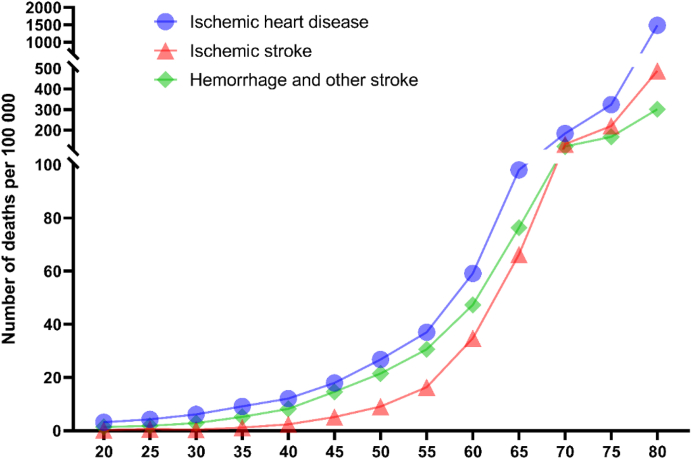
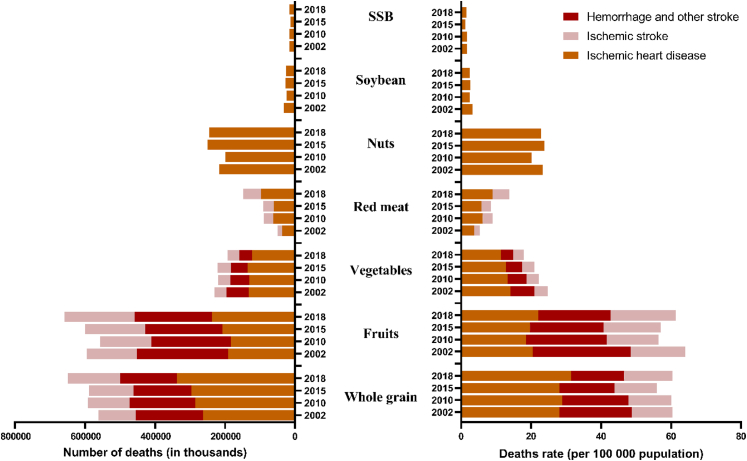
Fig. 3.
Number of deaths and deaths rate attributed to suboptimal dietary intake of all the 7 kinds of food by sex in 2002, 2010, 2015, and 2018.
The number of deaths and mortality rate for IHD, IS and HOS attributable to suboptimal diet were all higher in male than female among Chinese from 2002 to 2018. The diet-related mortality rate for IHD, IS and HOS increased substantially with the increasing age, which was 3.2 (95% UI, 2.8–3.4) for IHD, 0.2 (95% UI, 0.1–0.3) for IS and 1.4 (95% UI, 1.2–1.6) for HOS at age 20–25 years, to 1483.4 (95% UI, 1482.9–1489.6) for IHD, 488.6 (95% UI, 486.1–490.1) for IS and 301.7 (95% UI, 300.6–303.7) for HOS among Chinese adults aged order than 80 years (Fig. 4).
Fig. 4.
Mortality of ischemic heart disease, ischemic stroke, and intracerebral hemorrhage associated with overall suboptimal dietary intake in 2018.
Across the provinces of China, in 2018, the highest age-standardized mortality rates among Chinese adults aged 20 years or older attributable to suboptimal diet were observed in health area three for both IHD and IS. Shandong and Heilongjiang had the highest age-standardized mortality rates and diet-related deaths for IHD and IS, with 92.8 [95% UI, 89.9–93.3] deaths and 38.1 [95% UI, 36.2–38.8] deaths per 100,000 population, respectively. High HOS age-standardized mortality rates attributable to suboptimal diet were observed in health areas five and four, with the highest diet attributable age-standardized mortality rates found in Tibet (68.3 [95% UI, 65.0–70.1]). The lowest age-standardized mortality rates of all diet-related deaths among Chinese adults (aged 20 years or older) were observed in Tibet (26.5 [95% UI, 24.4–27.5]) for IHD, Qinghai (11.6 [95% UI, 11.6–13.9]) for IS, and Shanghai (6.1 [95% UI, 5.9–7.3]) for HOS, respectively (Table 1).
Table 1.
Overall impact of diet attributable age-standardized mortality rates of CVDs by provinces of China (per 100,000 population).
| IHD |
IS |
HOS |
CVDs |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2002 | 2018 | Annual change (%) | 2002 | 2018 | Annual change (%) | 2002 | 2018 | Annual change (%) | 2002 | 2018 | Annual change (%) | |
| Health area one | ||||||||||||
| Shanghai | 35.6 (34.7, 40.6) | 50.3 (47.8, 51.3) | 2.19 | 25.0 (23.2, 27.8) | 21.2 (19.9, 22.1) | −1.02 | 12.2 (10.3, 13.6) | 6.1 (5.9, 7.3) | −4.24 | 72.9 (72.1, 80.2) | 77.7 (75.5, 80.1) | 0.40 |
| Tianjin | 122.9 (116.1, 128.7) | 64.0 (62.3, 66.3) | −4.00 | 41.4 (35.9, 42.8) | 25.9 (24.6, 27.1) | −2.88 | 37.3 (35.8, 42.8) | 12.8 (12.0, 13.7) | −6.45 | 201.6 (191.7, 207.0) | 102.7 (101.2, 106.0) | −4.13 |
| Zhejiang | 51.9 (50.6, 56.8) | 33.2 (30.9, 33.4) | −2.75 | 20.5 (19.0, 23.1) | 23.3 (22.7, 24.9) | 0.80 | 39.0 (35.8, 41.3) | 16.4 (14.5, 16.4) | −5.28 | 111.4 (110.1, 119.4) | 72.9 (71.0, 74.8) | −2.62 |
| Beijing | 75.2 (69.7, 77.3) | 59.3 (56.7, 60.3) | −1.47 | 29.0 (25.6, 30.4) | 16.5 (15.4, 17.4) | −3.46 | 19.3 (17.9, 22.0) | 6.3 (5.6, 6.8) | −6.81 | 123.5 (118.7, 129.0) | 82.1 (81.6, 86.0) | −2.52 |
| Health area two | ||||||||||||
| Jiangsu | 46.7 (44.4, 48.6) | 39.6 (37.6, 39.9) | −1.02 | 40.8 (36.9, 40.8) | 28.9 (28.3, 30.3) | −2.12 | 35.4 (34.4, 38.0) | 17.7 (16.3, 17.8) | −4.22 | 122.9 (119.5, 126.0) | 86.3 (84.3, 87.8) | −2.18 |
| Hainan | 82.5 (80.6, 95.0) | 73.1 (70.4, 75.1) | −0.75 | 40.7 (30.1, 40.7) | 34.6 (32.7, 36.2) | −1.00 | 37.7 (35.3, 45.8) | 30.3 (28.1, 31.0) | −1.36 | 160.9 (145.2, 165.1) | 138.0 (131.3, 138.0) | −0.95 |
| Guangdong | 72.5 (68.6, 73.6) | 56.0 (55.1, 57.7) | −1.61 | 22.0 (21.3, 24.1) | 24.1 (23.3, 25.1) | 0.57 | 26.8 (25.1, 28.1) | 14.9 (14.6, 16.0) | −3.58 | 121.3 (114.5, 121.3) | 95.0 (92.6, 96.1) | −1.52 |
| Fujian | 50.3 (47.1, 54.1) | 42.1 (40.9, 43.8) | −1.10 | 23.8 (22.7, 27.9) | 20.7 (19.1, 21.0) | −0.87 | 37.2 (33.4, 39.5) | 20.6 (20.2, 22.2) | −3.64 | 111.3 (107.6, 118.5) | 83.4 (81.7, 85.8) | −1.79 |
| Hubei | 72.4 (69.8, 75.7) | 54.0 (52.9, 55.9) | −1.81 | 29.8 (27.2, 31.0) | 22.1 (21.6, 23.4) | −1.85 | 59.2 (54.3, 59.3) | 32.2 (30.1, 32.3) | −3.73 | 161.4 (157.5, 166.3) | 108.4 (106.4, 110.5) | −2.46 |
| Hunan | 89.5 (82.4, 89.5) | 60.0 (58.8, 61.5) | −2.46 | 29.4 (28.6, 33.0) | 25.7 (24.9, 26.8) | −0.83 | 28.3 (26.4, 30.4) | 23.4 (22.3, 24.0) | −1.20 | 147.2 (138.0, 147.2) | 109.1 (107.4, 111.0) | −1.85 |
| Health area three | ||||||||||||
| Shandong | 107.0 (102.6, 109.3) | 92.8 (89.9, 93.3) | −0.89 | 33.4 (31.8, 35.5) | 29.4 (27.7, 29.7) | −0.80 | 42.2 (41.7, 45.7) | 23.0 (21.7, 23.5) | −3.74 | 182.6 (175.9, 184.1) | 145.1 (143.0, 147.4) | −1.43 |
| Hebei | 97.3 (93.3, 100.3) | 64.6 (62.8, 65.6) | −2.53 | 39.0 (37.9, 42.2) | 27.1 (26.2, 28.0) | −2.24 | 48.9 (45.3, 50.2) | 29.7 (29.7, 31.8) | −3.06 | 185.1 (182.0, 190.9) | 121.5 (118.9, 122.9) | −2.60 |
| Ningxia | 75.9 (74.4, 81.3) | 60.6 (59.8, 64.0) | −1.40 | 19.9 (19.1, 22.6) | 22.4 (21.0, 23.6) | 0.75 | 31.4 (28.0, 32.2) | 24.5 (23.9, 26.6) | −1.55 | 127.3 (119.1, 128.2) | 107.5 (106.7, 112.4) | −1.05 |
| Jilin | 106.4 (93.1, 106.4) | 80.7 (79.4, 83.3) | −1.71 | 40.6 (36.7, 44.5) | 34.4 (33.8, 36.5) | −1.02 | 53.2 (51.0, 60.0) | 30.7 (29.8, 32.2) | −3.39 | 200.3 (192.0, 209.7) | 145.9 (141.2, 146.5) | −1.96 |
| Liaoning | 109.7 (105.4, 111.9) | 91.5 (91.4, 95.2) | −1.13 | 49.1 (45.8, 50.1) | 34.1 (32.8, 35.0) | −2.24 | 51.3 (48.0, 52.6) | 25.7 (24.5, 26.4) | −4.24 | 210.1 (207.5, 216.8) | 151.3 (147.6, 152.4) | −2.03 |
| Shanxi | 57.0 (55.0, 60.1) | 56.9 (55.1, 58.4) | −0.01 | 26.4 (25.5, 29.3) | 24.5 (23.1, 25.4) | −0.48 | 36.3 (33.4, 37.6) | 21.5 (20.0, 22.1) | −3.21 | 119.6 (117.5, 125.1) | 102.9 (100.7, 105.3) | −0.94 |
| Shaanxi | 92.2 (85.5, 92.2) | 55.5 (54.1, 57.2) | −3.12 | 30.5 (26.9, 30.5) | 26.4 (25.3, 27.4) | −0.92 | 67.3 (63.5, 68.3) | 29.6 (27.9, 30.1) | −5.00 | 190.0 (187.8, 195.9) | 111.4 (109.0, 113.3) | −3.28 |
| Henan | 91.0 (87.2, 92.9) | 85.6 (83.5, 86.6) | −0.38 | 31.5 (28.8, 32.1) | 31.0 (30.7, 32.7) | −0.08 | 66.1 (64.5, 69.3) | 37.3 (35.5, 37.6) | −3.52 | 188.6 (184.1, 192.0) | 153.9 (151.3, 155.7) | −1.26 |
| Anhui | 71.0 (67.2, 74.2) | 63.7 (62.8, 65.7) | −0.67 | 23.9 (22.8, 26.9) | 36.7 (34.7, 37.0) | 2.72 | 59.3 (57.2, 63.1) | 40.1 (38.5, 40.9) | −2.41 | 154.2 (153.0, 163.7) | 140.6 (137.5, 142.0) | −0.58 |
| Inner Mongolia | 62.8 (53.5, 62.9) | 71.9 (71.2, 74.8) | 0.85 | 25.5 (22.9, 29.5) | 24.2 (23.9, 26.1) | −0.31 | 45.2 (39.7, 48.0) | 28.7 (28.0, 30.4) | −2.80 | 133.5 (132.9, 147.8) | 124.8 (122.1, 127.0) | −0.42 |
| Heilongjiang | 109.5 (100.0, 109.9) | 91.8 (90.8, 94.9) | −1.10 | 38.0 (36.5, 42.7) | 38.1 (36.2, 38.8) | 0.00 | 57.4 (53.8, 61.0) | 29.3 (28.4, 30.6) | −4.11 | 204.9 (193.2, 207.5) | 159.2 (155.9, 161.1) | −1.57 |
| Health area four | ||||||||||||
| Jiangxi | 62.8 (58.5, 66.8) | 42.9 (41.8, 44.6) | −2.36 | 17.2 (15.1, 19.5) | 20.5 (19.4, 21.4) | 1.12 | 57.9 (57.2, 65.4) | 26.0 (24.8, 27.0) | −4.88 | 137.9 (128.6, 140.3) | 89.4 (88.6, 92.5) | −2.67 |
| Chongqing | 73.9 (66.6, 73.9) | 51.6 (50.7, 53.9) | −2.22 | 22.6 (21.1, 25.1) | 25.6 (24.4, 26.6) | 0.78 | 64.2 (59.9, 66.5) | 34.4 (32.6, 35.1) | −3.82 | 160.7 (151.2, 161.8) | 111.6 (109.5, 114.2) | −2.25 |
| Yunnan | 66.9 (62.0, 67.9) | 39.9 (39.2, 41.9) | −3.18 | 24.4 (23.1, 26.8) | 26.3 (25.0, 27.2) | 0.46 | 40.4 (38.9, 43.7) | 32.0 (31.2, 33.6) | −1.46 | 131.7 (125.6, 134.1) | 98.1 (96.1, 100.3) | −1.83 |
| Gansu | 73.6 (69.4, 78.0) | 52.0 (50.4, 53.9) | −2.15 | 17.4 (16.7, 21.0) | 21.4 (19.7, 21.9) | 1.29 | 58.2 (55.1, 62.7) | 35.7 (33.6, 36.6) | −3.01 | 149.3 (142.6, 154.7) | 109.1 (106.6, 111.7) | −1.94 |
| Sichuan | 57.1 (51.7, 57.1) | 52.2 (50.2, 52.9) | −0.57 | 19.2 (18.2, 21.2) | 20.5 (19.8, 21.4) | 0.43 | 64.8 (62.4, 68.1) | 47.4 (46.1, 48.6) | −1.93 | 141.1 (134.1, 142.1) | 120.1 (116.1, 120.2) | −1.00 |
| Health area five | ||||||||||||
| Tibet | 19.6 (15.3, 23.0) | 26.5 (24.4, 27.5) | 1.88 | 9.7 (7.2, 12.3) | 13.9 (11.7, 13.9) | 2.27 | 92.2 (83.5, 100.3) | 68.3 (65.0, 70.1) | −1.86 | 121.5 (115.9, 134.4) | 108.6 (104.4, 110.8) | −0.70 |
| Xinjiang | 84.5 (79.6, 90.5) | 54.5 (53.3, 57.0) | −2.71 | 15.8 (13.9, 18.7) | 13.9 (12.8, 14.6) | −0.81 | 49.3 (43.7, 52.0) | 22.1 (20.3, 22.7) | −4.89 | 149.6 (143.0, 157.7) | 90.5 (89.8, 94.6) | −3.09 |
| Qinghai | 38.3 (31.5, 38.3) | 38.6 (35.3, 39.0) | 0.06 | 6.6 (5.6, 8.8) | 11.6 (11.6, 13.9) | 3.57 | 60.7 (56.5, 66.0) | 41.7 (40.0, 43.7) | −2.32 | 105.5 (104.1, 116.7) | 91.9 (86.2, 91.9) | −0.86 |
| Guangxi | 82.6 (82.3, 90.7) | 62.8 (61.8, 65.2) | −1.70 | 32.6 (29.1, 34.4) | 36.2 (35.1, 37.5) | 0.65 | 46.2 (42.7, 48.9) | 37.6 (35.2, 37.8) | −1.27 | 161.4 (158.2, 169.7) | 136.6 (131.3, 136.6) | −1.04 |
| Guizhou | 60.3 (57.7, 63.6) | 40.9 (39.3, 42.7) | −2.40 | 29.8 (29.1, 33.5) | 30.5 (28.8, 31.6) | 0.14 | 85.9 (84.6, 92.0) | 41.8 (41.2, 44.5) | −4.40 | 176.1 (171.3, 181.4) | 113.2 (111.1, 116.5) | −2.72 |
The diet-related mortality rates for IHD increased in the majority of provinces except for Tianjin, Xinjiang, Yunnan, Shaanxi, Guizhou, Guangxi, Hebei, Hainan, Gansu, Hunan, Zhejiang, Chongqing, and Jiangxi in 2018 when compared to the rates in 2002, with Shanghai having the highest increase and Guangdong having the lowest. For IS, the diet-related mortality rates were higher in almost all provinces in 2018 compared to 2002, with the highest increase observed in Qinghai and the lowest in Xinjiang. However, the diet-related mortality rates for HOS decreased in most provinces in 2018, except for Ningxia, Hunan, and Sichuan, with the highest decrease observed in Tianjin and the lowest in Yunnan (Table 1).
Across the provinces of China, in 2018, the highest diet related DALYs among Chinese adults were observed in Henan (1.4 million [95% UI, 1.2–1.6] for stroke, 1.3 million [95% UI, 1.1–1.5] for IHD), and the lowest were observed in Tibet (0.05 million [95% UI, 0.043–0.063] for stroke, 0.03 million [95% UI, 0.028–0.042] for IHD). The DALYs rate for stroke and IHD attributable to suboptimal diet were the highest in health areas three and five, with the highest observed in Heilongjiang (1879.3 [95% UI, 1595.8–2182.6] DALYs per 100,000 population for stroke, 2012.8 [95% UI, 1692.2, 2362.7] DALYs for IHD). The DALYs rate for stroke and IHD attributable to suboptimal diet were the lowest in health areas one, with the lowest observed in Shanghai (353.2 [95% UI, 302.9–406.2] DALYs for stroke, 359.7 [95% UI, 307.2–421.0] DALYs for IHD) (Table 2).
Table 2.
Overall impact of diet on CVDs DALYs and DALYs rates by provinces of China.
| DALYs (in thousands) |
DALYs rate (per 100,000 population) |
|||
|---|---|---|---|---|
| Stroke | IHD | Stroke | IHD | |
| Health area one | ||||
| Shanghai | 99 (85, 113) | 101 (86, 118) | 353.20 (302.87, 406.20) | 359.72 (307.16, 420.95) |
| Tianjin | 141 (121, 163) | 151 (130, 178) | 926.21 (795.07, 1068.1) | 991.01 (849.36, 1168.2) |
| Zhejiang | 372 (322, 430) | 232 (196, 274) | 610.16 (526.53, 702.62) | 378.58 (321.26, 448.20) |
| Beijing | 119 (101, 138) | 165 (138, 195) | 492.53 (419.38, 570.90) | 687.30 (574.75, 807.82) |
| Health area two | ||||
| Jiangsu | 720 (628, 818) | 456 (390, 523) | 882.04 (767.83, 1002.6) | 556.11 (477.57, 641.89) |
| Hainan | 76 (64, 90) | 65 (53, 79) | 792.48 (667.79, 933.10) | 673.87 (555.28, 823.91) |
| Guangdong | 732 (634, 844) | 841 (718, 979) | 625.40 (542.27, 722.33) | 717.75 (615.23, 837.63) |
| Fujian | 267 (231, 307) | 208 (178, 246) | 677.46 (585.26, 779.22) | 528.84 (450.29, 622.68) |
| Hubei | 830 (715, 952) | 582 (498, 675) | 1499.6 (1296.2, 1719.0) | 1051.1 (901.17, 1219.9) |
| Hunan | 950 (824, 1096) | 916 (789, 1079) | 1417.1 (1224.6, 1633.7) | 1368.2 (1176.4, 1603.8) |
| Health area three | ||||
| Shandong | 992 (855, 1144) | 1148 (983, 1338) | 998.40 (859.96, 1152.4) | 1155.5 (987.53, 1348.3) |
| Hebei | 1188 (1035, 1358) | 945 (804, 1095) | 1554.3 (1356.6, 1778.5) | 1235.9 (1051.4, 1430.1) |
| Ningxia | 61 (52, 72) | 73 (60, 88) | 867.44 (736.21, 1021.4) | 1042.5 (859.43, 1257.7) |
| Jilin | 432 (361, 500) | 438 (365, 513) | 1549.0 (1293.4, 1793.1) | 1570.7 (1306.7, 1831.7) |
| Liaoning | 699 (602, 812) | 683 (576, 802) | 1564.0 (1343.9, 1815.6) | 1533.3 (1290.1, 1798.6) |
| Shanxi | 347 (292, 407) | 351 (289, 418) | 902.87 (756.69, 1054.5) | 909.71 (748.06, 1087.5) |
| Shaanxi | 430 (362, 510) | 411 (341, 492) | 1089.5 (916.78, 1291.6) | 1040.0 (864.03, 1243.1) |
| Henan | 1379 (1199, 1572) | 1274 (1093, 1487) | 1430.5 (1244.7, 1633.3) | 1321.4 (1135.3, 1546.1) |
| Anhui | 752 (664, 854) | 571 (494, 658) | 1232.0 (1083.0, 1398.3) | 933.71 (807.44, 1075.5) |
| Inner Mongolia | 380 (332, 438) | 433 (370, 503) | 1468.2 (1280.6, 1687.6) | 1673.7 (1427.6, 1943.2) |
| Heilongjiang | 736 (626, 858) | 788 (664, 926) | 1879.3 (1595.8, 2182.6) | 2012.8 (1692.2, 2362.7) |
| Health area four | ||||
| Jiangxi | 464 (406, 535) | 377 (324, 444) | 980.65 (853.25, 1127.1) | 793.83 (681.67, 932.93) |
| Chongqing | 308 (258, 367) | 200 (166, 238) | 1152.6 (965.04, 1373.0) | 746.45 (623.07, 891.87) |
| Yunnan | 636 (551, 746) | 462 (391, 545) | 1295.8 (1117.1, 1520.4) | 939.43 (796.68, 1109.4) |
| Gansu | 359 (309, 417) | 307 (259, 356) | 1351.7 (1164.5, 1568.2) | 1153.1 (974.84, 1339.0) |
| Sichuan | 1080 (914, 1241) | 689 (583, 790) | 1292.7 (1097.2, 1486.7) | 823.56 (701.44, 947.96) |
| Health area five | ||||
| Tibet | 51 (43, 63) | 33 (28, 42) | 1460.7 (1225.4, 1812.2) | 961.28 (796.07, 1202.7) |
| Xinjiang | 251 (216, 292) | 287 (241, 340) | 1030.9 (885.29, 1198.9) | 1178.7 (990.49, 1393.0) |
| Qinghai | 89 (74, 103) | 67 (55, 79) | 1412.4 (1182.9, 1633.3) | 1069.9 (884.18, 1251.8) |
| Guangxi | 604 (523, 710) | 524 (446, 622) | 1250.9 (1079.9, 1468.5) | 1085.3 (921.88, 1287.2) |
| Guizhou | 581 (498, 663) | 281 (235, 330) | 1713.4 (1468.9, 1962.2) | 831.53 (695.51, 976.91) |
Impact of individual components of diet on the burden of CVDs across China and its provinces
More than two-thirds of diet-related deaths and mortality rates can be attributed to low intake of whole grains, nuts, fruits, and vegetables (Fig. 5). Low intake of fruits was the leading dietary risk factor for deaths and mortality rate of IS and HOS among men and women, followed by inadequate intake of whole grains; while low intake of whole grain ranked first for IHD deaths and mortality rate followed by inadequate nuts and fruits intake (Supplementary Tables S2 and S3).
Fig. 5.
Number of deaths and mortality rate attributable to individual dietary risks in 2002, 2010, 2015, and 2018.
In 2018, low intake of fruit was the leading risk for DALYs and DALYs rate of stroke among Chinese adults followed by low intake of whole grains, inadequate fruits intake was responsible for 9.4 million (95% UI, 8.1–10.8) DALYs and 668.1 (95% UI, 576.0–771.0) DALYs per 100,000 population. While inadequate whole grain intake ranked first for DALYs and DALYs rate of IHD followed by inadequate nuts and fruits intake. Low intake of whole grains was responsible for 5.7 million (95% UI, 4.8–6.6) DALYs and 402.7 (95% UI, 342.1–471.1) DALYs per 100,000 population; low intake of nuts was responsible for 4.1 million (95% UI, 3.5–4.8) DALYs and 293.2 (95% UI, 249.0–343.0) DALYs; and low intake of fruits was responsible 4.0 million (95% UI, 3.4–4.7) DALYs and 283.7 (95% UI, 241.0–331.9) DALYs (Supplementary Figure S1).
Across the provinces of China, in 2018, IHD morality rates attributable to diet low in whole grains, vegetables, fruits, soybeans, nuts, and diet high in SSB and IS morality rates attributable to diet low in whole grains, vegetables, and fruits were highest in health area three, whereas IHD and IS morality rates attributable to diet high in red meat were highest in health areas five and two, respectively. Health area five had the highest HOS morality rates attributable to diet low in whole grains, vegetables, and fruits (Supplementary Table S4). Specifically, in Heilongjiang, Liaoning, Shandong, Beijing, Jilin, and Henan, diet low in whole grains, nuts, and fruits were the leading dietary risk for IHD-related deaths, DALYs, and DALYs rate. In Anhui, Jilin, and Heilongjiang, diet low in fruits and whole grain were the leading dietary risk for IS-related deaths and DALYs. In Tibet, diet low in whole grain and fruits were the leading dietary risk for HOS-related deaths and DALYs (Supplementary Tables S4–S6).
Discussion
The present study provides a comprehensive picture of the geographic variation and temporal trends of the burden of CVDs attributable to dietary risk factors at the national and provincial levels from 2002 to 2018. The diet-related mortality rates for IHD and IS were increased over time, and the diet-related burden of CVDs were varied across the Chinese provinces, with the highest mortality rates in Shandong, Heilongjiang, and Tibet for IHD, IS and HOS, respectively, and the lowest mortality rates in Tibet, Qinghai, and Beijing. Moreover, the burden of CVDs attributable to suboptimal diet among Chinese males was higher than that of female from 2002 to 2018 and increased substantially with the increasing age. Inadequate intakes fruits, whole grains, and vegetables intake were the primary dietary risk factors for IHD, IS, and HOS; low intake of nuts and soybean, and high intake of SSB only associated with IHD in China.
Despite the PAF of whole grains, fruits, vegetables, nuts, soybean and SSB associated with CVDs mortality were decreased from 2002 to 2018, the absolute deaths numbers and mortality rates of IHD and IS still increased substantially in the majority of provinces and the entire country, which can be primarily explained by the shift in age structure and the change of the background mortality rate. As of 2019, there were 26 million Chinese citizens 80 and 164.5 million Chinese citizens over the age of 65 (termed the elderly).27 According to the findings of this study, the number of deaths and mortality rate for CVDs attributable to suboptimal diet in China increased substantially with the increasing age, particularly in those over the age of 80 (the diet-related mortality rate for IHD, IS and HOS were 1483.4, 488.6, and 301.7 per 100,000 population, respectively). Interventions aimed at modifying suboptimal dietary behaviors and programs devoted to the detection and management of dietary risk factors are urgently required in China to reduce the diet-related burden of CVDs.
Similar to previous results of the diet-related burden of CVDs,14,28,29 results of this study indicate that the leading dietary risk factors for mortality are diet low in whole grains, diet low in nuts, diet low in fruits and vegetables. These findings support the scientific statement for 2021 dietary guidance to improve cardiovascular health from the American Heart Association.30 These food groups contain biologically active compounds, such as dietary fiber, minerals, antioxidants, vitamins, and other phytochemical composition, which may affect CVDs risk by altering endothelial function, antioxidant activity, oxidative stress, lipids and lipoproteins profile, and some other mechanisms.31, 32, 33, 34 The ranking of food groups in terms of their impact on CVDs may have significant implications for the development of future food-based dietary guidelines aimed at enhancing population health. For instance, effective strategies should be implemented to increase intakes of whole grains, vegetables, fruits, nuts, soybean while decreasing intakes of SSB and red mead should be, such as media campaigns, adjusting taxes by food type, food reformulation, etc.35, 36, 37
The association between adherence to a healthy diet and a lower risk of mortality and CVDs supports the important of nutrition in reducing disease burden.38,39 CVDs prevention and treatment programs need to incorporate healthy eating habits and give this information substantial consideration based on regional dietary patterns and the burdens of each CVD component. The present study revealed that provinces with medium level of economic development and life expectancy had higher burden of CVD-related mortality due to suboptimal diet. However, in provinces with a high economically development, high life expectancy and low mortality, such as Shanghai and Zhejiang, as well as provinces with low economic development and high mortality, such as Tibet and Qinghai, the age-standardized death rates for IS and IHD attributable to suboptimal diet were low. Provinces with established economies had the lowest DALYs rates for both stroke and IHD, including Shanghai, Zhejiang, Beijing, and Jiangsu. Previous studies in China have pointed out that the prevalence of CVDs in China is in a continuous rising stage, with mortality in rural areas exceeding that in urban areas since 2009.40 In China, there are also significant regional disparities and variable inequalities in primary and secondary CVD prevention. Healthy China 2030 proposes to reduce disparities in health levels between urban and rural areas, regions, and people, achieve universal health coverage and promote social equity, and The China’s Fourteenth Five Year Plan proposes promoting the construction of a healthy China comprehensively as a major task. Our findings provide evidence to support the development of province-specific strategies for CVDs prevention and reduction the burden of disease for each CVDs component.
Targeting specific dietary factors may not only be cost-effective but cost-saving, according to cost-effectiveness analyses of a range of population-level dietary interventions.41, 42, 43, 44, 45, 46, 47 Moreover, the specificity of the nutritional interventions should be considered; there is no one-size-fits-all approach. This study found that the diet-related burden of CVDs and the ranking of dietary risk factors for CVDs varied among the provinces of China; consequently, specific nutrition intervention strategies should be adjusted based on the dietary characteristics of each province. For example, in majority provinces, particularly in the province of Heilongjiang, Liaoning, and Shandong, low intake of whole grains was the first leading risk factors for CVDs; therefore, strategies that target increasing intakes of whole grains would be an effective strategy for these provinces. However, low intake of nuts was the primary risk factors for CVDs in Beijing, so strategies target increasing intakes of nuts would be more cost-effective than those aimed at increasing intakes of whole grains, vegetables, and fruits. The specific nutrition interventions are only cost-effective and cost-saving when they are tailored to the regional dietary characteristics. Unfortunately, the cost-effectiveness analyses of dietary interventions on whole grains, vegetables, fruits, nuts, etc., which are important dietary factors for the burden of CVDs among Chinese citizens, are lacking in evidence.
Several potential limitations should be considered when interpreting and using the findings of this study. Since dietary intakes were estimated using the food frequency questionnaire, it was not possible to evaluate the impact of nutrients (such as sodium, marine omega-3 fatty acids, polyunsaturated fatty acid, trans fats and so forth). In addition, we presumed that the distribution of dietary intakes is independent when estimating the PAFs for the overall effect of all dietary factors relevant to each outcome, which might have led to uncertainty regarding the combined effect of dietary factors. To quantify the effect of correlation of dietary factors, GBD diet Collaborators have estimated the overall burden of dietary risks with and without taking into account the correlation of dietary factors, and found that the absolute difference in the joint population attributable fractions was less than 2% on average.3 Additionally, provincial deaths data may limit the generalizability of our findings and prevent us from deriving more specific conclusions regarding the influence of subgroups such as residency (urban/rural) and socio-economic status (education and income) on the outcomes of interest; and deaths and dietary data collected at the same year may affect the precision of our result because it should take years for the effects of suboptimal diet to generate fatal consequences. Consequently, the findings of our study should be interpreted with caution, and further research is required to confirm and expand upon them. Finally, the effects of diet on CVDs mortality were derived primarily from meta-analyses of studies, and the effects could be mediated by raising blood pressure, increasing body mass index, etc., despite the fact that the studies included in the meta-analyses adjusted for potential confounding variables. When additional meta-analyses from Chinese population become available in the future, further estimations will be expected.
In summary, the present study found that suboptimal diets are a major contributor to CVDs mortality in China and the diet-related burden can vary substantially across provinces. This finding highlights the need for geographically targeted intervention strategies to improve the quality of human diet and reduces the diet-related burden of CVDs.
Contributors
YH, ZW, and MZ contributed to the conceive and design of the study. YF, JX, YL, CY, and YH conducted the data analysis. JX and YF prepared the first draft. YF, MZ, ZZ, and YK participated in data preparation and verification. YF, JX, YL, PY, MZ, ZZ, CY, and YH participated in data interpretation. PY, ZW, YH, and MZ provided important comments on the manuscript. All authors reviewed the drafted manuscript and approved the final manuscript and take responsibility for accuracy and integrity of the manuscript.
Data sharing statement
The data used for the analyses are available by email request to the corresponding author.
Declaration of interests
All authors declare no competing interests.
Acknowledgements
We acknowledge funding by the National Key Research and Development Program of China (2018YFC1315303), and the National Natural Science Foundation of China (82103966).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100784.
Contributor Information
Maigeng Zhou, Email: zhoumaigeng@ncncd.chinacdc.cn.
Yuna He, Email: heyn@ninh.chinacdc.cn.
Appendix A. Supplementary data
References
- 1.Global Burden of Disease Study . 2019. GBD results.https://vizhub.healthdata.org/gbd-results/ [Google Scholar]
- 2.Wang W., Liu Y., Liu J., et al. Mortality and years of life lost of cardiovascular diseases in China, 2005–2020: empirical evidence from national mortality surveillance system. Int J Cardiol. 2021;340:105–112. doi: 10.1016/j.ijcard.2021.08.034. [DOI] [PubMed] [Google Scholar]
- 3.Afshin A., Sur P.J., Fay K.A., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho F.K., Gray S.R., Welsh P., et al. Associations of fat and carbohydrate intake with cardiovascular disease and mortality: prospective cohort study of UK Biobank participants. BMJ. 2020;368 doi: 10.1136/bmj.m688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen K.S., Kris-Etherton P.M. Diet quality assessment and the relationship between diet quality and cardiovascular disease risk. Nutrients. 2021;13:4305. doi: 10.3390/nu13124305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Shaar L., Satija A., Wang D.D., et al. Red meat intake and risk of coronary heart disease among US men: prospective cohort study. BMJ. 2020;371 doi: 10.1136/bmj.m4141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Godos J., Micek A., Brzostek T., et al. Egg consumption and cardiovascular risk: a dose–response meta-analysis of prospective cohort studies. Eur J Nutr. 2021;60:1833–1862. doi: 10.1007/s00394-020-02345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petermann-Rocha F., Ho F.K., Foster H., et al. Nonlinear associations between cumulative dietary risk factors and cardiovascular diseases, cancer, and all-cause mortality: a prospective cohort study from UK Biobank. Mayo Clin Proc. 2021;96:2418–2431. doi: 10.1016/j.mayocp.2021.01.036. [DOI] [PubMed] [Google Scholar]
- 9.Clermont A., Sufra R., Pierre J.L., et al. Dietary risk factors for cardiovascular disease among low-income Haitian adults: findings from a population-based cohort. Nutrients. 2022;14:787. doi: 10.3390/nu14040787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim C.G.Y., Tai E.S., van Dam R.M. Replacing dietary carbohydrates and refined grains with different alternatives and risk of cardiovascular diseases in a multi-ethnic Asian population. Am J Clin Nutr. 2022;115:854–863. doi: 10.1093/ajcn/nqab403. [DOI] [PubMed] [Google Scholar]
- 11.Senftleber N.K., Albrechtsen A., Lauritzen L., et al. Omega-3 fatty acids and risk of cardiovascular disease in Inuit: first prospective cohort study. Atherosclerosis. 2020;312:28–34. doi: 10.1016/j.atherosclerosis.2020.08.032. [DOI] [PubMed] [Google Scholar]
- 12.He Y., Li Y., Yang X., et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019;7:540–548. doi: 10.1016/S2213-8587(19)30152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dong C., Bu X., Liu J., Wei L., Ma A., Wang T. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: a systematic analysis of the Global Burden of Disease Study. Nutr Metab Cardiovasc Dis. 2022;32:897–907. doi: 10.1016/j.numecd.2021.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Huang L., Wang Z., Wang H., et al. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr. 2021;75:247–252. doi: 10.1038/s41430-020-0674-8. [DOI] [PubMed] [Google Scholar]
- 16.Ma Q., Li R., Wang L., et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2021;6:e897–e906. doi: 10.1016/S2468-2667(21)00228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou M., Wang H., Zeng X., et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He Y., Zhao W., Zhang J., et al. Data resource profile: China National Nutrition Surveys. Int J Epidemiol. 2019;48 doi: 10.1093/ije/dyy289. 368–368f. [DOI] [PubMed] [Google Scholar]
- 19.Zhang M., Wang L., Wu J., et al. Data resource profile: China Chronic Disease and Risk Factor Surveillance (CCDRFS) Int J Epidemiol. 2022;51:e1–e8. doi: 10.1093/ije/dyab255. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z., Zhang L., Chen Z., et al. Survey on prevalence of hypertension in China: background, aim, method and design. Int J Cardiol. 2014;174:721–723. doi: 10.1016/j.ijcard.2014.03.117. [DOI] [PubMed] [Google Scholar]
- 21.Liu S., Wu X., Lopez A.D., et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94:46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y., Li X., Zhou M., et al. Under-5 mortality in 2851 Chinese counties, 1996–2012: a subnational assessment of achieving MDG 4 goals in China. Lancet. 2016;387:273–283. doi: 10.1016/S0140-6736(15)00554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cao X., Zhao Z., Kang Y., et al. The burden of cardiovascular disease attributable to high systolic blood pressure across China, 2005–18: a population-based study. Lancet Public Health. 2022;7:e1027–e1040. doi: 10.1016/S2468-2667(22)00232-8. [DOI] [PubMed] [Google Scholar]
- 24.Zhou M., Wang H., Zhu J., et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 25.Efron B., Tibshirani R.J. 0 edn. Chapman and Hall/CRC; 1994. An introduction to the Bootstrap. [Google Scholar]
- 26.Gardiner J.C. The asymptotic distribution of mortality rates in competing risks analyses. Scand J Stat. 1982;9:31–36. [Google Scholar]
- 27.Fang E.F., Xie C., Schenkel J.A., et al. A research agenda for ageing in China in the 21st century (2nd edition): focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;64 doi: 10.1016/j.arr.2020.101174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwingshackl L., Knüppel S., Michels N., et al. Intake of 12 food groups and disability-adjusted life years from coronary heart disease, stroke, type 2 diabetes, and colorectal cancer in 16 European countries. Eur J Epidemiol. 2019;34:765–775. doi: 10.1007/s10654-019-00523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meier T., Gräfe K., Senn F., et al. Cardiovascular mortality attributable to dietary risk factors in 51 countries in the WHO European Region from 1990 to 2016: a systematic analysis of the Global Burden of Disease Study. Eur J Epidemiol. 2019;34:37–55. doi: 10.1007/s10654-018-0473-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lichtenstein A.H., Appel L.J., Vadiveloo M., et al. 2021 dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144:e472–e487. doi: 10.1161/CIR.0000000000001031. [DOI] [PubMed] [Google Scholar]
- 31.Swaminathan S., Dehghan M., Raj J.M., et al. Associations of cereal grains intake with cardiovascular disease and mortality across 21 countries in Prospective Urban and Rural Epidemiology study: prospective cohort study. BMJ. 2021;372 doi: 10.1136/bmj.m4948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bitok E., Sabaté J. Nuts and cardiovascular disease. Prog Cardiovasc Dis. 2018;61:33–37. doi: 10.1016/j.pcad.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Miller V., Mente A., Dehghan M., et al. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet. 2017;390:2037–2049. doi: 10.1016/S0140-6736(17)32253-5. [DOI] [PubMed] [Google Scholar]
- 34.Liu W., Hu B., Dehghan M., et al. Fruit, vegetable, and legume intake and the risk of all-cause, cardiovascular, and cancer mortality: a prospective study. Clin Nutr. 2021;40:4316–4323. doi: 10.1016/j.clnu.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Peñalvo J.L., Cudhea F., Micha R., et al. The potential impact of food taxes and subsidies on cardiovascular disease and diabetes burden and disparities in the United States. BMC Med. 2017;15:208. doi: 10.1186/s12916-017-0971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Backholer K., Martin J. Sugar-sweetened beverage tax: the inconvenient truths. Public Health Nutr. 2017;20:3225–3227. doi: 10.1017/S1368980017003330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang Y., Pomeranz J., Wilde P., et al. Adoption and design of emerging dietary policies to improve cardiometabolic health in the US. Curr Atheroscler Rep. 2018;20:25. doi: 10.1007/s11883-018-0726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang X., Lu J., Wu C., et al. Healthy lifestyle behaviours and all-cause and cardiovascular mortality among 0.9 million Chinese adults. Int J Behav Nutr Phys Act. 2021;18:162. doi: 10.1186/s12966-021-01234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gong Q., Zhang P., Wang J., et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol. 2019;7:452–461. doi: 10.1016/S2213-8587(19)30093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Writing Committee of the Report on Cardiovascular Health and Diseases in China Report on cardiovascular health and diseases in China 2021: an updated summary. Biomed Environ Sci. 2022;35:573–603. doi: 10.3967/bes2022.079. [DOI] [PubMed] [Google Scholar]
- 41.Basto-Abreu A., Barrientos-Gutiérrez T., Vidaña-Pérez D., et al. Cost-effectiveness of the sugar-sweetened beverage excise tax in Mexico. Health Aff. 2019;38:1824–1831. doi: 10.1377/hlthaff.2018.05469. [DOI] [PubMed] [Google Scholar]
- 42.Fayet-Moore F., George A., Cassettari T., Yulin L., Tuck K., Pezzullo L. Healthcare expenditure and productivity cost savings from reductions in cardiovascular disease and type 2 diabetes associated with increased intake of cereal fibre among Australian adults: a cost of illness analysis. Nutrients. 2018;10:34. doi: 10.3390/nu10010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang J., Lee Bravatti M.A., Johnson E.J., Raman G. Daily almond consumption in cardiovascular disease prevention via LDL-C change in the U.S. population: a cost-effectiveness analysis. BMC Public Health. 2020;20:558. doi: 10.1186/s12889-020-08642-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim D.D., Wilde P.E., Michaud D.S., et al. Cost effectiveness of nutrition policies on processed meat: implications for cancer burden in the U.S. Am J Prev Med. 2019;57:e143–e152. doi: 10.1016/j.amepre.2019.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wolfenden L., Barnes C., Jones J., et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev. 2020;2 doi: 10.1002/14651858.CD011779.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huse O., Ananthapavan J., Sacks G., et al. The potential cost-effectiveness of mandatory restrictions on price promotions for sugar-sweetened beverages in Australia. Int J Obes. 2020;44:1011–1020. doi: 10.1038/s41366-019-0495-9. [DOI] [PubMed] [Google Scholar]
- 47.Fattore G., Federici C., Drummond M., et al. Economic evaluation of nutrition interventions: does one size fit all? Health Policy. 2021;125:1238–1246. doi: 10.1016/j.healthpol.2021.06.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.