Summary
Background
Childhood obesity is high in Republic of Marshall Islands (RMI). We report the prevalence and socio-demographic distribution of selected obesity-related risk factors among children in Majuro, RMI.
Methods
Sixteen elementary schools were approached and students and parents in Grades 1, 3, and 5 invited to participate in this cross-sectional population-based survey. Accelerometry and a questionnaire were used to collect data on children's physical activity (PA), sleep, screen time and dietary behaviours. Descriptive statistics and mixed-effects logistic regression were used to examine differences in the proportions of children meeting selected RMI Healthy Living Guidelines by sex, school grade and school sector.
Findings
Thirteen schools and 958 children were recruited, of which 892 (52.2% girls; mean age 9.3 ± 1.8 years) provided useable data. Around 90% met the PA, 29% screen time, 13% sleep, 69% sugar-sweetened beverage and 56% highly processed food guidelines. The proportion meeting individual guidelines was higher among children in Grade 1 compared with Grade 5. Being a girl (0.27; 95% CI 0.16, 0.46) was associated with lower odds of meeting the PA recommendation. Compared with children from Grade 1, those in Grade 5 had lower odds of meeting the PA (0.28; 95% CI 0.15, 0.55), screen time (0.60; 95% CI 0.40, 0.89), sleep duration (0.33; 95% CI 0.18, 0.59), sugar-sweetened beverage (0.35; 95% CI 0.23, 0.53), and consumption of highly processed foods recommendations (0.49; 95% CI 0.33, 0.72).
Interpretation
While most children in RMI are adequately active, resources are needed to promote healthier levels of screen time, sleep, sugar-sweetened beverage and highly processed food consumption, especially among older children.
Funding
This study was funded by World Diabetes Foundation; Canvasback Missions, RMI; NHMRC Australia (APP1176858); Pacific Community.
Keywords: Physical activity, Screen time, Sleep, Diet
Research in context.
Evidence before this study
To identify papers that reported the prevalence and sociodemographic correlates of physical activity, screen time, sleep and selected dietary factors among children from RMI we conducted a systematic review. We searched PubMed for papers published between 1 January 2000 and 19 November 2022. Our search terms included “physical activity” or “sedentary behaviour” or “screen time” or “sleep” or “diet” and “child∗” and “Marshall Islands”. Six original articles were located that were related to this study. These reported the prevalence of child overweight and obesity and acanthosis nigricans. One study reported the proportion of children who consumed fruit and vegetables in their diet. We examined two in-press papers from the Children's Health Living Program in the US-affiliated Pacific Region. These reported types of food and PA outlets in RMI, and the dietary intakes of children by food group, percentage of energy from macronutrients, and most frequently consumed foods. No study has reported the prevalence or sociodemographic distribution of meeting guidelines for physical activity, sedentary behaviour, sleep, and nutrition among children in RMI.
Added value of this study
This is the first study to report the prevalence and sociodemographic distribution of selected child health behaviours included in the 2022 RMI Guidelines for Healthy Living. Data were representative of children from Majuro, the largest and most populous atool in RMI. Eighty-one percent (13/16) elementary schools participated and within these schools, 59% of eligible students were recruited to the study. The proportion of children meeting the physical activity and dietary guidelines was high, with a much lower prevalence for the sleep and screen time guidelines. Older children were less likely to meet the guidelines that their younger counterparts.
Implications of all the available evidence
Healthy food habits and movement behaviours are important for children in RMI. The new RMI Healthy Living Guidelines provide a benchmark for monitoring and surveillance. The sub-optimal levels of screen time and sleep duration in RMI children reinforce the need for programs to educate parents and children. The study provides guidance for the RMI government on where priorities should be set to enhance the proportion of children meeting the guidelines. Reducing premature mortality caused by non-communicable diseases (NCDs) is a sustainable development goal. Prevention efforts must commence in childhood by targeting key NCD risk factors. Developing guidelines, as RMI have done, is an important first step. This study advocates regular monitoring and surveillance of the guidelines and the allocation of resources to support whole-of-community initiatives to promote healthy levels of physical activity, screen time, sleep and dietary behaviours.
Introduction
The Republic of the Marshall Islands (RMI) comprises 34 coral atolls and single coral islands located in the central north Pacific. The main urban centre is located in Majuro, where 52% (N = 27,797) of the total population of 53,069 live.1 RMI is an upper-middle-income country with an annual gross domestic product per capita growth of 4.4% in 2021.2 Forty-one per cent of the population is aged under 20 y.3 According to the Global Status Report for Physical Activity, no data exist on the surveillance of physical activity in children or adolescents in RMI.3 The 2020 Rapid High School Survey (N = 2621) reported the prevalence of selected NCD risk factors among students aged 13–19 y in RMI (substance use, sexual health and overweight).4 Just under 20% of students had smoked or chewed tobacco and 29% had consumed alcohol. This was lower than that reported in the Federated States of Micronesia (FSM) but higher than in peers from Guam and the Commonwealth of Northern Mariana Islands (CNMI). Just under 20% were overweight or obese, which was between 15 and 22 percentage points lower than that reported in FSM, Guam, CNMI, and the US.
Few studies have examined dietary and movement behaviours (physical activity [PA], sedentary behaviour, and sleep) among children in the Pacific US-affiliated states and territories. The Children's Healthy Living Study (CHL) comprised a community-based randomised controlled trial (RCT) in five jurisdictions (Alaska, American Samoa, CNMI, Guam, and Hawaii).5 Analysis of baseline data included 3108 children aged 2–8 y (1226 aged 6–8 y). The authors found that children slept an average of 9.75 h/d and spent 3.73 h/d in screen time. The CHL study also included a cross-sectional prevalence survey in the five jurisdictions involved in the RCT and an additional three (FSM, RMI, and Palau). Data from RMI found that 75% of children aged 6–8 y met the sleep guideline of 9–11 h/d, 41% of children aged 2–8 y met the screen time guideline of ≤2 h/d, and 77% met the US PA guideline of 60 min of moderate-to vigorous-intensity physical activity (MVPA) every day.6 A systematic review and meta-analysis of seven Pacific jurisdictions found that 43% of adolescent males and 35% of females met the guideline of 60 min MVPA every day.7 These lower proportions can be explained by the difference in guidelines (every day vs average per day) and the difference in ages. It is well-documented that adolescents are less active than children.8
Regarding dietary behaviours, Novotny et al.9 found that in the five participating countries of the CHL RCT, children at baseline consumed an average of 1.0 cup/d of fruit and 0.6 cup/d of vegetables. This was similar to that reported by Guerrero et al.10 in their independent analysis of data from Guam in the same study (0.9 cup/d fruit and 0.6 cup/d vegetables). These values are higher than those reported from the same study for RMI (0.3 cup/d fruit and 0.3 cup/d vegetables).6 These three studies also reported the average consumption of sugar-sweetened beverages (SSB) per day. The same value was found in the five-country RCT and the RMI study (0.6 cup/d), which was lower than that found in the Guam study (1.0 cup/d).
Collectively, these studies show large variability in the findings for dietary and movement behaviours across the Pacific and within RMI. Limitations of previous studies in RMI include the small sample (accelerometry data were available on only 63 children aged 5–9 y) and that the data were collected in 2013, when screen time among children in RMI almost exclusively comprised only television and video viewing and computer games. There is a need to collect data from a larger, more representative sample that includes assessment of smartphones and tablets, which are widely used among children in RMI, and to determine the proportion who meet the new RMI Guidelines for Healthy Living.11
Childhood obesity is associated with a range of short- and long-term physical and mental health consequences.12 In response to the increasing prevalence of overweight and obesity among children in RMI (currently 13%) with higher level as children age,13 the RMI Government and key stakeholders formed a coalition to address childhood obesity. One recommendation from the coalition was to collect representative data on the prevalence and socio-demographic distribution of key behaviours associated with childhood obesity. In 2022, RMI released their first Healthy Living Guidelines.11 These provided recommendations for physical activity, sedentary screen time, sleep, food habits, and eating behaviours for children, teens, and adults. The guidelines have been helpful in raising awareness of the importance of healthy levels of these behaviours. The RMI Government has officially endorsed the guidelines and mandated that they be displayed in all restaurants and schools. Support has been provided by the UN Food and Agriculture Organization (FAO) for a national campaign based on the guidelines. The guidelines are driving legislational change in the areas of marketing of unhealthy foods to minors, and mandatory physical education classes in all schools. The purpose of this study was to report the proportion of children who met key recommendations of these guidelines and to see if these proportions varied by sex, age, or type of school attended.
Methods
Study design
This was a cross-sectional population-based survey with assessments occurring between March 2020 and May 2021. During this time, schools remained open and RMI remained free of any outbreak of COVID-19. The protocol of this study was developed based on local ethical considerations as advised by the locally-based research investigators (TS, MI, PE). Ethical approval was obtained from the Human Research Ethics Committee of the University of Wollongong (2019/467). The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.14
Setting
Principals from all 16 elementary schools (nine public and seven private) on Majuro atoll were verbally invited by the lead author to participate in the study. Participant information sheets and consent forms were provided in English and Marshallese by the study team and distributed to all eligible children. Written informed consent from parents and students were obtained to allow for their participation in the study. Permission to conduct the study in schools was obtained from the Republic of Marshall Islands Ministry of Health and Human Services and from the Ministry of Education.
Participants
All children in Grades 1, 3 and 5 in the participating schools were eligible and invited to participate; however, only those providing written parental consent were recruited into the study.
Data collection procedures
The data collection team consisted of the survey leader (TS) and ten physical education teachers, (under the supervision of PE) seconded to the project from the Ministry of Education. Prior to the study, these local staff received two full days of training and orientation in data collection methodology and use of the survey tools, provided by the senior author on Majuro in 2020. A detailed protocol manual was developed and distributed to each data collector. On the first day of training, all data collection procedures were explained in detail. This included watching videos and practising assessments on one another. On the second day, the data collection team visited a local school and practised all assessments with the children, under the guidance and feedback of the senior author. Data collectors then underwent a quiz on the correct methods of assessment and needed to score 100% prior to entering the field to collect data.
Measurements
Accelerometer
Physical activity (PA) and sleep duration were measured using the Axivity AX3 triaxial accelerometers (Axivity Ltd., Newcastle-Upon-Tyne, UK) worn on the non-dominant wrist. The accelerometers were initialised to collect data at 50 Hz for seven consecutive days (24 h per day). Data were downloaded in raw format as cwa files using OMGUI software (version 43; Open Movement, Newcastle, UK) and processed in R using the package GGIR (version 2.3-0),15 which performed 1) auto-calibration procedures using local gravity as a reference; 2) identified non-wear period(s); and 3) converted raw triaxial accelerometer signals into one omnidirectional measure of acceleration (Euclidean Norm Minus-One; ENMO).16,17 The ENMO values were averaged over 5-s epochs and expressed in milli-gravitational units (mg). Non-wear time was imputed by default in GGIR using the average data at similar time points on other days.15 Moderate-to vigorous-intensity physical activity (MVPA) was defined as ENMO values above 192 mg.18 Sleep duration was estimated from the sleep period time window detected using a polysomnography-validated algorithm.19 Accelerometer days with <16 h of wear time and ≤200 min of sleep were considered invalid and were excluded from the analysis. For data inclusion, the participants were required to have at least four valid days of data, including one weekend day. The daily time spent in MVPA and sleep was weighted at 5:2 for weekdays: weekend days.
Questionnaire
A standardised questionnaire (see Supplementary Material) was used to collect information on children's physical activity, screen time, food habits and dietary behaviours, with questions adopted from the existing movement behaviour and nutrition surveys (WHO Global School-based student Health Survey (GSHS)20 [Q1,2,3,4]; SUNRISE Study21 [Q4-11,13]; NSW Schools Physical Activity and Nutrition Survey 201022 [Q12]). The questionnaire was translated into Marshallese and took approximately 15 min to complete. The questionnaire was sent home with children in Grades 1 and 3 for their parents/caregivers to complete. For children in Grade 5, it was self-administered at school under the guidance of the data collectors. Data pertaining to children's participation in muscle- and bone-strengthening activities, bedtime and wake-up time consistency, screen use before bedtime, presence of screens in the bedroom, recreational screen time, and the consumption frequency of SSB, highly processed snack foods, fruits and vegetables were extracted and used in the analysis (see Table 1 for the questions and response categories).
Table 1.
Outcome measures for examining compliance with selected RMI Guidelines for Healthy Living.
| Guideline component | Recommendations | Measurement method | Use in analysis |
|---|---|---|---|
| Moderate- to vigorous-intensity physical activity (MVPA) | An average of 60 min per day of MVPA. | Measured using wrist-worn accelerometer (Axivity AX3) for seven consecutive days | Children with an average MVPA duration of 60 min/day were classified as meeting the guideline. |
| Muscle- and bone-strengthening activitiesa | At least 3 days a week. | Questionnaire: During the past seven days, on how many days did you do activities to strengthen your muscles and bones (e.g., push ups, sit-ups, lifting weights, lunges and squats; dance; martial arts or aerobics class)? 8 responses: 0 days, 1 day, 2 days, 3 days, 4 days, 5 days, 6 days, 7 days. |
Children who answered 3 or more days were classified as meeting the guideline. |
| Sleep duration | 9–11 h of sleep each night. | Measured using wrist-worn accelerometer (Axivity AX3) for seven consecutive days | Children with an average sleep duration of 9–11 h/day were classified as meeting the guideline. |
| Sleep consistency | Have a consistent bedtime and wake-up time. | Questionnaire:
|
Children who answered ‘Yes’ for both questions were classified as meeting the guideline. |
| Screen time before bed | Avoid screen time 1 h before sleep. | Questionnaire: Do you use electronic screen devices (e.g., TV, video game, computer, tablet or smartphone) in the 2 h before bedtime on a daily basis? (Yes/No/Don't know). If Yes, how close to bedtime do you usually use these devices? 3 responses: Closer than 30 min; 30 min–< 1 h; 1–2 h. |
Children who answered ‘No’ or who answered ‘Yes’ and then selected the option ‘1–2 h’ were classified as meeting the guideline. Children who answered ‘Don't know’ were excluded from the analysis. |
| Screens in bedrooms | Keep screens out of the bedroom. | Questionnaire: Do you have electronic screen devices in the room where you sleep (e.g., TV, video game, computer, tablet or smartphone) (Yes/No) | Children who answered ‘No’ were classified as meeting the guideline. |
| Recreational screen time | A maximum of 2 h per day. | Questionnaire: Over the past seven days, on how many days did you watch TV/videos/Internet (including on a smart phone or tablet) or play video or computer games for entertainment for less than 2 h while sitting or lying down? 8 responses: 0 days, 1 day, 2 days, 3 days, 4 days, 5 days, 6 days, 7 days. |
Children who answered ‘7 days’ were classified as meeting the guidelines. |
| Sugar-sweetened beverages consumption | Drink clean, safe water and avoid soda or sugar-sweetened beverages. | Questionnaire: How often do you drink sugary drinks (e.g., Cordials, flavoured milk, fruit juice, soda, soft drinks? 6 responses: Never, Rarely, Once a week, Most days, Every day, Don't know |
Children who answered ‘Never’, ‘Rarely’ or ‘Once a week’ were classified as meeting the guideline. Children who answered ‘Don't know’ were excluded from the analysis. |
| Highly processed food consumption | Limit highly processed foods with added salt, sugar and fat. Avoid foods with trans-fatty acids. | Questionnaire: How often do you have snacks like chips, biscuits, cakes, candies, chocolate, pastries, and sweets between meals? 6 responses: Never, Rarely, Once a week, Most days, Every day, Don't know |
Children who answered ‘Never’, ‘Rarely’ or ‘Once a week’ were classified as meeting the guideline. Children who answered ‘Don't know’ were excluded from the analysis. |
| Fruit consumption | Include local fruits with every meal. | Questionnaire: How often do you eat other fruits and vegetables (e.g., apple, banana, orange, pear) on a typical day/in a typical week? 6 responses: Every day, More than 3 times a week, Twice a week, Once a week, Never, Don't know |
Children who answered ‘Every day’ were classified as meeting the guidelines. Children who answered ‘Don't know’ were excluded from the analysis. |
| Vegetable consumption | Include local vegetables with every meal. | Questionnaire: How often do you eat Vitamin-A rich fruits and vegetables (e.g., green leafy vegetables, yellow and orange inside vegetables and orange non-citrus fruits)? 6 responses: Every day, More than 3 times a week, Twice a week, Once a week, Never, Don't know |
Children who answered ‘Every day’ were classified as meeting the guidelines. Children who answered ‘Don't know’ were excluded from the analysis. |
The recommendations for participation in muscle- and bone-strengthening activities are taken from the WHO Guidelines on Physical Activity and Sedentary Behaviour (World Health Organization 2020) as there was no clear recommendation for this component within the RMI Guidelines for Healthy Living.
Variables
Compliance with guidelines
This study focused on analysis of compliance with 11 of the individual guideline components from the RMI Guidelines for Healthy Living.11 These include children's participation in PA, sleep duration and consistency, screen time before bed, screens in bedroom, recreational screen time, and the consumption of SSB, highly processed foods, fruits and vegetables. The recommendations for participation in muscle- and bone-strengthening activities were taken from the WHO Guidelines on Physical Activity and Sedentary Behaviour23 as there was no clear recommendation for this component within the RMI Guidelines. Table 1 outlines the guideline recommendations and the outcome measures used for assessing and defining children's compliance with each guideline component.
Socio-demographic characteristics
Participants' dates of birth (for age calculation), sex (boy/girl), school grade (Grade 1/3/5), and school sector (public/private) were provided from the schools’ information management systems.
Statistical analysis
The analytical sample of this study included participants with valid accelerometry or questionnaire data available for assessing at least one guideline component. Descriptive statistics were presented as mean and standard deviation (SD) (for continuous data) or frequency and percentage (for categorical data). The proportions of children meeting the individual healthy living guidelines were calculated for the overall population and separately for each socio-demographic subgroup (sex, school grade, school sectors). Mixed-effects logistic regression models with school units as random effects (accounting for the cluster sampling by school) were used to calculate the adjusted odds ratios (aOR) with 95% confidence intervals (CI) of meeting the individual guidelines across all subgroups (sex, school grade, and school sector; one model for each guideline). Missing data were handled using pairwise deletion method to maximise the amount of data available for analysis. All statistical analyses were conducted using jamovi software version 2.3 (Sydney, Australia). Statistical significance was set at p < 0.05.
Role of the funding source
The funders had no role in the study design, data collection, data analysis interpretation or writing of the report.
Results
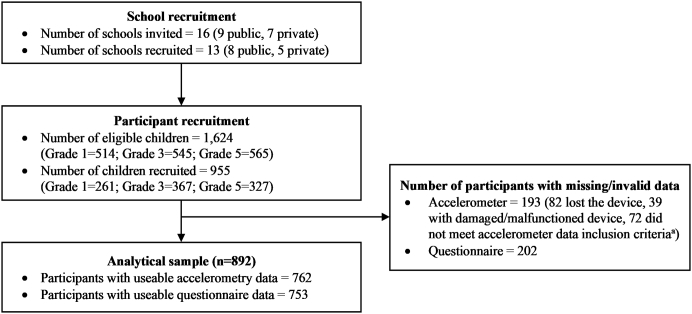
Fig. 1 displays the participant recruitment process for the study. Thirteen (eight public and five private) of the 16 elementary schools were recruited (81%). Of the 1624 eligible children enrolled in these schools, 955 provided written parent consent to participate (58.2% response rate). Of these, 892 (52.2% girls; mean age [SD] = 9.3 [1.8] years) had useable data from the accelerometers (N = 762; 79.8%) or questionnaires (N = 753; 78.8%) for assessing at least one of the guideline components, and were included in the analytical sample. As presented in Table 2, the analytical sample comprised a slightly larger proportion of children in Grade 5 than the consenting sample, but were similar in terms of their sex and school sector distributions. The age ranges for the children in each grade were: Grade 1 (5.4–9.4 y), Grade 3 (7.3–12.5 y) and Grade 5 (8.8–13.5 y).
Fig. 1.
Flowchart of the participant recruitment process.aWith at least four days (including one weekend day) of valid accelerometry data (≥16 h of wear time per day).
Table 2.
Descriptive characteristics of the study population.
| Socio-demographic characteristics | Total sample (n = 955) | Analytical sample (n = 892) |
|---|---|---|
| Age in years, mean (SD)a | 9.3 (1.8) | 9.3 (1.8) |
| Sex, n (%) | ||
| Boy | 461 (48.3) | 426 (47.8) |
| Girl | 494 (51.7) | 466 (52.2) |
| School grade, n (%) | ||
| Grade 1 | 261 (27.3) | 234 (26.2) |
| Grade 3 | 367 (38.4) | 341 (38.2) |
| Grade 5 | 327 (34.2) | 317 (35.5) |
| School type, n (%) | ||
| Public | 741 (77.6) | 690 (77.4) |
| Private | 214 (22.4) | 202 (22.6) |
Missing data for three children.
Table 3 presents the proportion of children meeting the individual healthy living guidelines. For the movement behaviour-related guideline components, most children met the PA recommendations (90.9% for muscle- and bone-strengthening activities and 88.7% for MVPA); far fewer met the screen time (28.7%) and sleep duration (13.3%) recommendations. A greater proportion of children met the recommendation for sleep consistency (58.3%) than the recommendations for screen time before bed (45.4%) and for the presence of screens in their bedroom (33.7%). For the diet-related guidelines, more than half the children met the recommended consumption frequency for SSB (68.5%) and highly processed foods (55.9%), while fewer met the recommendations for fruit (44.7%) and vegetable (30.7%) consumption. Stratification analyses showed that the proportions who met the individual guidelines were generally higher among girls (except for PA and screens in bedroom recommendations), children in the lower grade levels (Grade 1 and Grade 3; except for screen time before bed and fruit and vegetable consumption), and those from public schools (except for sleep duration and screen time recommendations). A detailed summary of descriptive statistics for each guideline measure can be found in the Supplementary Material (Table S1).
Table 3.
Number (percentage) of children meeting selected RMI Guidelines for Healthy Living by socio-demographic subgroups.
| Physical activity |
Sleep |
Screen use |
Diet |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MVPA | Muscle- and bone-strengthening activities | Duration | Consistency | Screen time before bed | Screens in bedroom | Recreational screen time | Sugar-sweetened beverages consumption | Highly processed food consumption | Fruit consumption | Vegetable consumption | |
| Sample size | 762 | 747 | 762 | 748 | 729 | 751 | 745 | 696 | 706 | 701 | 612 |
| Overall | 676 (88.7) | 679 (90.9) | 101 (13.3) | 436 (58.3) | 331 (45.4) | 253 (33.7) | 214 (28.7) | 477 (68.5) | 395 (55.9) | 313 (44.7) | 188 (30.7) |
| Sex | |||||||||||
| Boy | 341 (94.5) | 327 (92.1) | 46 (12.7) | 196 (54.7) | 158 (45.3) | 128 (35.7) | 99 (28.0) | 222 (66.9) | 184 (54.8) | 138 (41.7) | 79 (27.5) |
| Girl | 335 (83.5) | 352 (89.8) | 55 (13.7) | 240 (61.5) | 173 (45.5) | 125 (31.9) | 115 (29.4) | 255 (70.1) | 211 (57.0) | 175 (47.3) | 109 (33.5) |
| School grade | |||||||||||
| Grade 1 | 178 (92.7) | 177 (95.7) | 37 (19.3) | 101 (54.3) | 66 (36.5) | 61 (32.8) | 69 (37.3) | 132 (74.6) | 114 (63.7) | 67 (38.1) | 36 (26.1) |
| Grade 3 | 271 (91.2) | 261 (96.0) | 44 (14.8) | 166 (61.0) | 126 (47.4) | 104 (37.8) | 69 (25.6) | 210 (82.4) | 155 (60.3) | 95 (38.8) | 52 (24.9) |
| Grade 5 | 227 (83.2) | 241 (83.1) | 20 (7.3) | 169 (58.3) | 139 (49.3) | 88 (30.3) | 76 (26.2) | 135 (51.1) | 126 (46.7) | 151 (53.9) | 100 (37.7) |
| School sector | |||||||||||
| Public | 527 (90.9) | 532 (91.7) | 76 (13.1) | 355 (61.1) | 259 (46.0) | 209 (35.8) | 165 (28.5) | 379 (70.2) | 313 (57.2) | 247 (45.6) | 149 (32.3) |
| Private | 149 (81.9) | 147 (88.0) | 25 (13.7) | 81 (48.5) | 72 (43.4) | 44 (26.3) | 49 (29.3) | 98 (62.8) | 82 (51.6) | 66 (41.5) | 39 (26.0) |
Abbreviation: MVPA; Moderate-to vigorous-intensity physical activity.
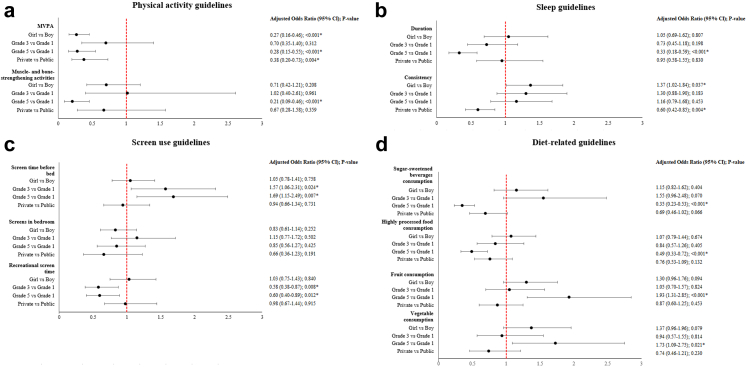
Fig. 2 shows that there were significant differences in the odds of meeting the individual healthy living guidelines across subgroups. Girls were more likely to meet the sleep consistency recommendation (adjusted odds ratio [aOR] 1.37; 95% CI 1.02, 1.84) but less likely to meet the MVPA recommendation (aOR 0.27; 95% CI 0.16, 0.46) than boys. Compared to children in Grade 1, those in Grade 5 were less likely to meet the recommendations for sleep duration (aOR 0.33; 95% CI 0.18, 0.59), MVPA (aOR 0.28; 95% CI 0.15, 0.55]), muscle- and bone-strengthening activities (aOR 0.21; 95% CI 0.09, 0.46), screen time (aOR 0.60; 95% CI 0.40, 0.89), consumption of SSB (aOR 0.35; 95% CI 0.23, 0.53) and highly processed foods (aOR 0.49; 95% CI 0.33, 0.72); but more likely to meet the recommendations for screen time before bed (aOR 1.69; 95% CI 1.15, 2.49), fruit (aOR 1.93; 95% CI 1.31, 2.85) and vegetable consumption (aOR 1.73; 95% CI 1.09, 2.75). Children in Grade 3 were less likely to meet the screen time recommendation (aOR 0.58; 95% CI 0.38, 0.87); but more likely to meet the screen time before bed recommendation (aOR 1.57; 95% CI 1.06, 2.31) than those in Grade 1. Children from private schools were less likely to meet the sleep consistency (aOR 0.60; 95% CI 0.42, 0.85) and MVPA (aOR 0.38; 95% CI 0.20, 0.73) guidelines than children from public schools.
Fig. 2.
Adjusted odds ratio (95% confidence intervals) of meeting selected RMI Guidelines for Health Living across socio-demographic subgroups. Abbreviation: MVPA, Moderate-to vigorous-intensity physical activity. Models adjusted for school clustering. Values with an asterisk (∗) mark indicate statistically significant (p < 0.05).
Discussion
This is the first known study to examine the proportion of children who meet the 2022 RMI Healthy Living Guidelines. Overall, nearly all children met the PA guidelines. This is higher than that reported for RMI (77%) by Novotny et al.6 The reason for this is the change in guidelines between the two studies. To meet the previous PA guideline, a child had to accumulate 60 min of MVPA on every day of the measurement period whereas to meet the current guideline requires accumulation of an average of 60 min per day. It has been shown that using the average method results in a higher prevalence compared with the every day method,24 which is consistent with our finding. Given the important independent relationships between physical activity and health outcomes in children, this high proportion meeting the guideline is promising and may be explained by the supportive environments provided for children in the community, school settings, parks and churches in RMI. Efforts to prevent the precipitous decline in PA during adolescence must be prioritised to ensure the future health of the population in Majuro.
We found that only 29% of children met the screen time guideline. This was lower than the 41% previously reported for RMI6 but higher than the 17% reported in Guam.10 This can be explained by differences in the operationalisation of the guidelines. The previous guidelines recommended up to and including 2 h/d, whereas the current guidelines recommend less than 2 h/d. Less than half the children met the guideline for not using screens before bedtime and only one-third met the recommendation to not have a screen in the room where they sleep. These low compliances are consistent with other studies25,26 and reflect how challenging it is for children to meet these recommendations. Around 40% of the population in RMI are regular internet users, including of social media, and 12% have smartphones, meaning children have relatively easy access to electronic media for entertainment.27 RMI has a stable internet, making it easy for children to spend large amounts of time online. Despite having an environment that supports year-round outdoor play and activity, the availability of screen devices makes them an attractive option for children in their leisure time. If both parents are working, and little parental supervision is present, especially during the after school period, this can make it difficult for children to limit their recreational sedentary screen time.
Around 15% of children met the sleep duration guideline. This is much lower than the 75% reported previously in RMI6 and the 40% in Guam.10 The reasons for this are the way sleep was assessed. We used accelerometry, which typically captures only sleep time, whereas the other studies used parent report, which tends to capture time in bed. This difference, referred to as the sleep onset latency period, appears to be around 20 min28,29 but may be as high as 60 min.30 Because the guidelines recommend sleep time, we felt it was more accurate to report this from accelerometry data. We also calculated the proportion who met the sleep guidelines using parent/self-reports. It was much higher (51.4%) and more commensurate with the findings from these other studies that used the same method. More work needs to be done in this area, as the evidence base upon which sleep guidelines were developed is predominantly based on studies which used parent/self-reports.31 Although more than half the children went to bed at a consistent time, this time was likely to be too late for them to accumulate enough sleep time to meet the recommendation.28 Reasons for children not meeting the sleep duration guideline are likely to be due to them staying up too late at night, most likely because of watching television or using other electronic devices.
We found that just under half the children (45%) met the fruit consumption guideline. This is lower than that reported in the CHL Study in RMI (18%).6 This can be explained by differences in methodologies. The CHL Study used food logs completed over two days, where exact quantities were recorded. In our study, a single item was used (see Table 1). Our results, however, were similar to the Guam CHL study (41%) which also used food logs to assess fruit consumption.10 Similar results were found for vegetable consumption, with 31% of our sample meeting the RMI guidelines compared with only 3% and 1% from the CHL RMI and Guam studies, respectively. In addition to the difference in methodologies, differences in the operationalisation of the guidelines can explain these variations. The RMI Guidelines recommend consuming five servings of fuit and vegetables each day, and ideally including some with every meal; the latter is how we determined compliance in this study. We were not able to determine from our question the amount of fruit and vegetables consumed, which was possible with the previous studies and was how compliance with the USDA guideline was measured.
Just over two-thirds of children met the RMI guideline for SSB and consumption of highly processed foods. The figure for SSB is lower than the 91% reported in the CHL RMI Study.6 This difference can be explained by the different guidelines in each study. The current RMI Guideline is to avoid soda or SSB, which we operationalised as those who consumed sugary drinks never, rarely, or once a week as meeting the guideline. The previous study used a guideline of 0–2 cups per day.
In summary, these dietary consumption figures reflect the change in dietary patterns among children in RMI. Traditional foods are being replaced with more unhealthy options. These unhealthy foods are becoming more accessible and are more widely available.32 Efforts are needed to prevent the marketing of these food to children and to limit their availability, especially in small stores around schools where children are likely to frequent on the way to and from school.
Girls were less likely than boys to meet the physical activity guideline. This is consistent with literature, which shows that boys are more active than girls.33 Reasons for this sex disparity are both biological and environmental.34 Biologically, girls tend to have lower fitness levels, coordination and a higher percentage of body fat than boys.34 Environmentally, girls often receive less positive reinforcement from school and family sources and have fewer opportunities to participate in sports compared to boys).34 This finding reinforces the need to prioritise initiatives to promote girls’ participation in physical activity. Higher compliance rates with the guidelines were also observed among younger children. This difference between age groups can be attributed to the natural decline in PA levels than occurs during the transition from childhood to adolescence.8
Compared with students who attended public schools, private school students were less likely to meet the guideline for MVPA. This is likely due to differences in the provision of physical education (PE), which is a key domain of physical activity in children.35 In Majuro, public schools have dedicated PE teachers at each school, whereas only a small number of the private schools have such staff. This is consistent with findings among adolescents in other countries with a similar education system.36 Students who attended private schools were also less likely to meet the guideline for sleep consistency than their public school peers. The reasons for this are unclear. Private school students have been found to have later bedtime and earlier wake-up times than their public school peers.37 Such sleeping patterns may be associated with poorer sleep consistency,38 although more research is needed in this area.
Girls were more likely to meet the sleep consistency guideline than boys. This is due to girls having a slightly higher consistency in their bed time (72% vs 69%) and going to bed slightly earlier. An earlier bed time has been associated with a higher sleep quality and better health outcomes.39 Reasons for having a more consistent bedtime are not clear, but may be partly explained by fewer girls having electronic devices in the room where they sleep compared with boys (32% vs 36%).
Students in Grades 3 and 5 were less likely to meet the recreational screen time guideline than students in Grade 1. Older students consistently have higher levels of screen time than younger students40 likely due to a greater proportion owning smartphones41 and being allowed to stay up later at night watching television and using electronic media devices.42 However, students in Grades 3 and 5 were more likely to meet screen time before bed guideline than students in Grade 1. This is harder to explain. It might be that because these students have higher ownership of smartphones, and for those in Grade 3, a higher number with a screen in the room where they sleep. It may reflect different patterns of screen use between older and younger students. Although older students had higher overall screen time, and were less likely to meet the recreational screen time guidelines, they may have accumulated most of their recreational screen time in the after school period (3–6pm) when the greatest amount of discretionary time is available. This would explain their lower levels of physical activity compared with their Grade 1 counterparts. Older students may have had more homework to complete in the evening or more domestic responsibilities, which would have reduced the time they could spend in recreational screen time before bed. It could also reflect that, because older children accumulate more of their recreational screen time from smartphones than from television43 that parents have less oversight into whether their children were engaged in recreational screen media use before bedtime, especially if these were being used in the child's bedroom. The CHL RCT reported a significant decrease in screen time among children in the intervention communities compared with those in control communities.9 We recommend examining this intervention to determine if a similar approach could be used to address the high levels of screen time among children in RMI.
Students in Grade 5 were less likely to meet the SSB guideline and consumption of highly processed foods guideline than students in Grade 1. This may be due to Grade 5 students having higher levels of recreational screen time, which has been shown to be linked to greater consumption of SSB and highly processed foods.44 Older students may also have more discretionary money available to spend at shops that sell these products. Grade 5 were more likely to meet fruit and vegetable consumption guidelines than their Grade 1 peers. This may be due to students self-reporting their consumption in Grade 5, compared with parents reporting in Grade 1, which may have led to over-reporting. These differences may also reflect older students confusing fruit-flavoured products with fruit. Grade 5 students and parents of Grades 1 and 3 students may also have different interpretations of whether local foods such as coconut, breadfruit, and pandanus are fruits. Students in Grade 5 may also have had more discretionary money to purchase these foods.
A strength of this study was the use of a device-based measure for accessing physical activity and sleep. This overcomes biases associated with self- or parent-reports of these behaviours and allows for a detailed assessment of movement behaviours over an extended period in free-living scenarios. It is worth noting that the accelerometry approach may not adequately measure certain types of activities (e.g., bicycling) and the outcome is highly dependent on the data collection and processing criteria. The use of wrist acceleration cutpoint, although validated, may have also resulted in some misclassification of MVPA as it reflects absolute rather than relative intensity for each participating children.
There were a number of limitations with this study. There was a low consent rate (58%), but this was not uncommon in this population and our analyses showed that the socio-demographic distribution of the analytical samples were similar to that of the elementary school-aged population in Majuro. Although this was a population-based sample (all schools on Majuro invited to participate), the results may not be necessarily generalise to all elementary school children in Majuro as the influence of other socio-economic indicators (e.g., parental education level, household income) were not examined in this study. It was not feasible to collect data on parental income, education level, or level of disadvantage, which would have been beneficial in describing the socio-demographic profile of the participants. We relied on self-reported data, which is subject to social desirability and recall bias, to assess screen time and dietary outcomes. The diet-related questions were not specifically designed to assess compliance with the RMI guidelines (which were developed after the survey), so the results should be interpreted with caution.
Our findings provide the first known evidence on the proportion of children in Majuro who meet the 2023 RMI Guidelines for Healthy Living. While some behaviours such as physical activity, processed food and SSB consumption show good levels of compliance with the guidelines, other behaviours such as sleep, screen time and fruit and vegetable consumption are sub-optimal. We are encouraged that the RMI government and key stakeholders have legislated changes around food marketing to children and mandatory quality physical education classes. These two types of interventions have a strong evidence base for their efficacy in promoting healthy eating and physical activity levels. We recommend consideration of other evidence-based interventions such as the Children's Healthy Living Program45 and that further data be collected at regular intervals to assess the proportion of children meeting the guidelines and to evaluate the effectiveness of the initiatives being implemented.
Contributors
All authors contributed to the design and conceptualisation of the study. TS led the data collection team and was supported by MI and PS. PC and KHC contributed to data curation. KHC conducted the data analyses. ADO and KHC prepared the draft manuscript. All authors reviewed and approved the final version of the manuscript.
Data sharing statement
The data presented in this study are not openly available as participants did not provide informed consent for data sharing.
Declaration of interests
TS received funds from the World Diabetes Foundation (WDF16-1418) and Pacific Community to support the data collection activities related to this study. ADO is supported by a National Health and Medical Research Council of Australia Investigator Grant (APP1176858). The authors have no competing interests to declare.
Acknowledgements
This study was funded by the Canvasback Missions, Inc. Republic of Marshall Islands, World Diabetes Federation, Pacific Community (SPC), and National Health and Medical Research Council of Australia (APP1176858). The funders had no role in the design of the study; in the collection, analyses, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication. The authors would like to thank Dr Jane Matanaicake-Lum On at the RMI Ministry of Health and Human Services for their critical review of the manuscript. The authors would also like to thank Dr Bradley Wakefield of the Statistical Consulting Centre at the University of Wollongong for providing statistical advice. We thank the participants and their families and schools who made this study possible. The authors also acknowledge the contribution and support of all data collectors involved in the study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100783.
Contributor Information
Tanner Smith, Email: tannersmith@canvasback.org.
Kar Hau Chong, Email: khchong@uow.edu.au.
Penny Cross, Email: pcross@uow.edu.au.
Maybelline Ipil, Email: miepi.projects@gmail.com.
Pranson Eliou, Email: peliou@pss.edu.mh.
Rachel Novotny, Email: novotny@hawaii.edu.
Anthony D. Okely, Email: tokely@uow.edu.au.
Appendix A. Supplementary data
References
- 1.The World Bank Population total - Marshall Islands. 2020. https://data.worldbank.org/indicator/SP.POP.TOTL?end=2021&locations=MH&start=1960&view=chart
- 2.The World Bank GDP per capita growth (annual %) - Marshall Islands. 2021. https://data.worldbank.org/indicator/NY.GDP.PCAP.KD.ZG?end=2021&locations=MH&start=1990&view=chart
- 3.World Health Organisation . World Health Organization; Geneva: 2022. Global status report on physical activity 2022: country profiles. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 4.Ministry of Health & Human Services Republic of the Marshall Islands Marshall Islands rapid youth survey Majuro. 2020. https://www.pihoa.org/wp-content/uploads/2022/05/RMI-Rapid-Youth-Survey-0-Final_05_21_21.pdf
- 5.Wilken L.R., Novotny R., Fialkowski M.K., et al. Children's Healthy Living (CHL) program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity. BMC Public Health. 2013;13(1):1–13. doi: 10.1186/1471-2458-13-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Novotny R. Children's healthy living program for remote underserved minority populations in the Pacific region: republic of the Marshall Islands prevalence survey results. 2013. https://chl-pacific.org/wp-content/uploads/2016/09/RMI_CHL-Comprehensive-Community-Reports.pdf Available from:
- 7.Richards Adams I.K., Okoli C.T.C., Krok-Schoen J.L., et al. Physical activity among native Hawaiins and Pacific Islanders: a systematic review and meta-analysis. J Nutr Educ Behav. 2019;51:245–258. doi: 10.1016/j.jneb.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Sallis J.F. Age-related decline in physical activity: a synthesis of human and animal studies. Med Sci Sports Exerc. 2000;32:1598–1600. doi: 10.1097/00005768-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Novotny R., Davis J., Butel J., et al. Effect of the children's healthy living program on young child overweight, obesity, and acanthosis nigricans in the us-affiliated Pacific region: a randomized clinical trial. JAMA Netw Open. 2018;1(6) doi: 10.1001/jamanetworkopen.2018.3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leon Guerrero R.T., Barber L.R., Aflague T.F., et al. Prevalence and predictors of overweight and obesity among young children in the Children's Healthy Living Study on Guam. Nutrients. 2020;12 doi: 10.3390/nu12092527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pacific Community Public Health Division . Pacific Community (SPC); Suva, Fiji: 2022. RMI Guidelines for Healthy Living: a handbook for community members. [Google Scholar]
- 12.Reilly J.J., Methven E., McDowell Z.C., et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Passmore E., Smith T. Dual burden of stunting and obesity among elementary school children on Majuro, republic of Marshall Islands. Hawaii J Health Soc Welf. 2019;78(8):262. [PMC free article] [PubMed] [Google Scholar]
- 14.Von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med. 2007;45(4):247–251. doi: 10.1016/j.ypmed.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Migueles J.H., Rowlands A.V., Huber F., Sabia S., van Hees V.T. GGIR: a research community–driven open source R package for generating physical activity and sleep outcomes from multi-day raw accelerometer data. J Meas Phys Behav. 2019;2(3):188–196. [Google Scholar]
- 16.Van Hees V.T., Fang Z., Langford J., et al. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol. 2014;117(7):738–744. doi: 10.1152/japplphysiol.00421.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Hees V.T., Gorzelniak L., Dean León E.C., et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS One. 2013;8(4) doi: 10.1371/journal.pone.0061691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hildebrand M., VAN Hees V.T., Hansen B.H., Ekelund U. Age group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–1824. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 19.van Hees V.T., Sabia S., Jones S.E., et al. Estimating sleep parameters using an accelerometer without sleep diary. Sci Rep. 2018;8(1):1–11. doi: 10.1038/s41598-018-31266-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . World Health Organization; Geneva: 2009. Global school-based student health survey (GSHS) [Google Scholar]
- 21.Okely A.D., Reilly J.J., Tremblay M., Kariippanon K. Examining 24-hour movement behaviours in the early years in urban and rural settings in low-, middle-, and high-income countries: the SUNRISE Study Protocol. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-049267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hardy L.L., King L., Espinel P., Cosgrove C., Bauman A. NSW Ministry of Health; Sydney, NSW: 2010. NSW schools physical activity and nutrition survey (SPANS) 2010: full report. [Google Scholar]
- 23.World Health Organization . World Health Organization: Licence: CC BY-NC-SA 3.0 IGO; Geneva: 2020. WHO guidelines on physical activity and sedentary behaviour. [Google Scholar]
- 24.Ridgers N.D., Timperio A., Crawford D., Salmon J. Validity of a brief self-report instrument for assessing compliance with physical activity guidelines amongst adolescents. J Sci Med Sport. 2012;15(2):136–141. doi: 10.1016/j.jsams.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Friel C.P., Duran A.T., Shechter A., Diaz K.M. U.S. children meeting physical activity, screen time, and sleep guidelines. Am J Prev Med. 2020;59(4):513–521. doi: 10.1016/j.amepre.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas G., Bennie J.A., De Cocker K., Castro O., Biddle S.J. A descriptive epidemiology of screen-based devices by children and adolescents: a scoping review of 130 surveillance studies since 2000. Child Indicat Res. 2020;13(3):935–950. [Google Scholar]
- 27.Kemp S. Digital 2021: the Marshall Islands. 2021. https://datareportal.com/reports/digital-2021-marshall-islands
- 28.Crabtree V.M., Williams N.A. Normal sleep in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2009;18(4):799–811. doi: 10.1016/j.chc.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 29.Galland B.C., Taylor B.J., Elder D.E., Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012;16(3):213–222. doi: 10.1016/j.smrv.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Goodwin J.L., Silva G.E., Kaemingk K.L., Sherrill D.L., Morgan W.J., Quan S.F. Comparison between reported and recorded total sleep time and sleep latency in 6-to 11-year-old children: the Tucson Children's Assessment of Sleep Apnea Study (TuCASA) Sleep Breath. 2007;11:85–92. doi: 10.1007/s11325-006-0086-6. [DOI] [PubMed] [Google Scholar]
- 31.Chaput J.P., Gray C.E., Poitras V.J., et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41:S266–S282. doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- 32.Novotny R., Yamanaka A.B., Dela Cruz R., et al. Food group, macronutrient intake, and metabolic status in the US-affiliated Pacific's Children's Healthy Living (CHL) program. J Nutr. 2022;152(12):2898–2912. doi: 10.1093/jn/nxac173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trost S.G., Pate R.R., Sallis J.F., et al. Age and gender differences in objectively measured physical activity in youth. Med Sci Sports Exerc. 2002;34:350–355. doi: 10.1097/00005768-200202000-00025. [DOI] [PubMed] [Google Scholar]
- 34.Telford R.M., Telford R.D., Olive L.S., Cochrane T., Davey R. Why are girls less physically active than boys? Findings from the LOOK Longitudinal Study. PLoS One. 2016;11(3) doi: 10.1371/journal.pone.0150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sallis J.F., McKenzie T.L. Physical education's role in public health. Res Q Exerc Sport. 1991;62:124–137. doi: 10.1080/02701367.1991.10608701. [DOI] [PubMed] [Google Scholar]
- 36.Pearman S.N., Valois R.F., Thatcher W.G., Drane J.W. Physical activity behaviors of adolescents in public and private high schools. Am J Health Behav. 2001;25(1):42–49. doi: 10.5993/ajhb.25.1.5. [DOI] [PubMed] [Google Scholar]
- 37.Mathew G., Varghese A.D., Benjamin A.I. A comparative study assessing sleep duration and associated factors among adolescents studying in different types of schools in an urban area of Kerala, India. Indian J Community Med. 2019;44(Suppl 1):S10–S13. doi: 10.4103/ijcm.IJCM_19_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chaput J.-P., Dutil C., Featherstone R., et al. Sleep timing, sleep consistency, and health in adults: a systematic review. Appl Physiol Nutr Metab. 2020;45(10):S232–S247. doi: 10.1139/apnm-2020-0032. [DOI] [PubMed] [Google Scholar]
- 39.Golley R.K., Maher C., Matricciani L., Olds T. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37(4):546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- 40.Chong K.H., Parrish A.M., Cliff D.P., Dumuid D., Okely A.D. Changes in 24-hour movement behaviours during the transition from primary to secondary school among Australian children. Eur J Sport Sci. 2021;22:1–11. doi: 10.1080/17461391.2021.1903562. [DOI] [PubMed] [Google Scholar]
- 41.Lenhart A. Pew Internet & American Life Project; Washington, DC: 2009. Teens and mobile phones over the past five years: pew Internet looks back. [Google Scholar]
- 42.Sormunen M., Turunen H., Tossavainen K. Self-reported bedtimes, television-viewing habits and parental restrictions among Finnish schoolchildren (aged 10–11 years, and 2 years later aged 12–13 years): perspectives for health. Euro J Commun. 2016;31(3):283–298. [Google Scholar]
- 43.UNICEF . UNICEF; New York: 2017. The state of the worlds children 2017: children in a digital world. [Google Scholar]
- 44.Stiglic N., Viner R.M. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.SNAP-Ed Toolkit: obesity prevention interventions and evaluation framework. The children's healthy living program. 2022. https://snapedtoolkit.org/interventions/programs/the-childrens-healthy-living-chl-program/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.