Summary
Non-suicidal self-injury behavior (NSSI) is a serious public health concern that requires immediate attention. Despite the high prevalence of NSSI among the Chinese population, there is a significant gap in research on the comprehensive picture of this field. Therefore, a scoping review was conducted to investigate the prevalence, methods, risk factors, and preventive intervention programs related to NSSI in China. The review found that the estimated lifetime prevalence of NSSI among Chinese youth population is alarmingly high at 24.7% (N = 1,088,433). Common methods of NSSI include scratching, hitting, and biting. Additionally, the review synthesized 249 risk factors based on the biopsychosocial-ecological framework, highlighting the urgent need for intervention. However, only 12 empirical studies focus on NSSI prevention or intervention programs were included. These findings underscore the necessity for more clinical practices and larger studies to identify effective interventions and ultimately alleviate the burden of NSSI on the Chinese population.
Funding
This review was supported by Humanity and Social Science Youth foundation of Ministry of Education (22YJCZH018), Science and Technology Innovation 2030 (STI2030-Major Projects:2021ZD0200702), National Natural Science Foundation of China (81825009), and Shuimu Tsinghua Scholar. No funding agencies were involved in the data collection, data analysis, and writing of this paper.
Keywords: Non-suicidal self-injury, Prevalence, Method, Risk factor, Prevention, Intervention, China
Introduction
Non-suicidal self-injury behavior (NSSI) is defined as the deliberate, self-inflicted destruction of body tissues without any suicidal intent and for specific purposes.1 Common examples include cutting, burning, scratching, and hitting.2 It has been observed as a serious public health problem across a variety of populations,3 including non-clinical children and adolescents, with a 22.1% lifetime prevalence,4,5 community adults (e.g., the pooled NSSI prevalence was 13.4%) and clinical samples with nearly 49.5% NSSI rate.6 The long-lasting negative effects of NSSI on individual's health outcomes have been documented. For example, previous study has highlighted that NSSI is associated with increased suicidal thoughts and attempts.7
A substantial body of research related to the NSSI has been conducted in developed countries.8 It has pointed out the urgent situation of NSSI, which needs great attention from the government, social agencies, public health practitioners, psychologists, and social workers.9 To date, no review has comprehensively addressed the prevalence, methods, risk factors, and intervention or prevention programs of NSSI in China,10 despite the complex sociocultural context of the issue. Urbanization and modernization in China have created a clash between traditional cultural values and modern culture, exerting significant pressure on individuals,11 particularly young people, who may experience low self-worth, loneliness, and a distorted sense of reality that increase the risk of NSSI.12 Furthermore, left-behind children, a group of children whose parents have migrated to cities, face unique challenges that have drawn widespread concern in Chinese society due to their negative long-term physical and mental health outcomes.13 Therefore, increased attention and research on NSSI in China are necessary.
In response to this challenge, this scoping review will be divided into three main sections: 1) the NSSI prevalence and methods in China; 2) the risk factors of NSSI in China; 3) the prevention and intervention programs targeting NSSI in China. In the first section, we aim to summarize evidence of NSSI prevalence and methods from different developmental stages, including childhood, adolescence, and adulthood, as well as from various genders and sexual orientations. These efforts could help raise awareness about the importance of NSSI and promote access to mental health services, which also provide important insights into global trends in NSSI. The second section will summarize the previous literature that focused on the risk factors of NSSI found in Chinese society, from a biopsychosocial-ecological system framework.14 This theoretical framework explains human developmental outcomes from a unified perspective, which highlights the importance of risk factors from the biological system, psychological system, community environment, built environment, and natural environment when considering an individual's maladaptive behaviors. Systematically summarizing the risk factors would help scholars and practitioners to alert to this emerging public health problem earlier, and address it in a more cost-effective way. Also, we will take a general review of all the actions that have been taken to prevent and intervene the incidence of NSSI. This section will help all stakeholders learn what “strength” and “improvement” for the design of a more implementation-guided program could be taken in the next step,15 which would effectively help prevent NSSI behaviors in China or globally nowadays.
Methods
Protocol registration
The study protocol was drafted based on the methods outlined in the PRISMA extension for scoping reviews (PRISMA-ScR) checklist. The final protocol was prospectively registered with the International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY) on 24 December 2022 (Identifier: DOI 10.37766/inplasy2022.12.0099).
Search strategy and selection criteria
Scoping review is an ideal tool to determine the scope or coverage of a body of literature on a given topic and give clear indication of the volume of literature and studies available as well as an overview (broad or detailed) of its focus.16 The purpose of the scoping review is to identify knowledge gaps, scope a body of literature, clarify concepts, investigate research conduct, or to inform a systematic review.17 Scoping review proves to be valuable for exploring developing evidence, especially when it remains uncertain what other specific inquiries can be raised and effectively tackled by a more exacting systematic review.
This scoping review followed the five-stage framework: 1) identifying the research question; 2) identifying relevant studies; 3) study selection; 4) charting the data; 5) collating, summarizing and reporting the results.18 The keywords and MeSH terms of NSSI included: self-injur∗, self-harm, self-mutilat∗, auto-mutilat∗, self-neglect, self-cut∗, parasuicid∗, self-destruct∗, auto-destruct∗, self-wound∗, self-inflicted injur∗, self-poisoning, skin-cut∗, self-burn∗, self-abus∗, “DSH”, “DSHI”, “NSSI”. For the first section regarding NSSI prevalence and methods, the keywords and MeSH terms also included: frequen∗, prevalen∗, inciden∗, occur∗, persist∗, trend∗, experience, number∗, count∗, “population at risk”, time∗, rate∗, percent∗, form∗, method∗, way∗, act∗, strateg∗. For the second section regarding risk factors of NSSI, the keywords and MeSH terms also included: predict∗, prospective, risk∗, relat∗, associat∗, attribut∗, precurs∗, correlat∗, determin∗, protect∗, factor∗, variable∗, casual∗, mediat∗, moderat∗. For the third section regarding current intervention and prevention programs of NSSI, the keywords and MeSH terms will also include: intervent∗, prevent∗, project∗, program∗, therap∗, solution∗, service∗, treat∗, train∗, manag∗. Throughout the search for all three sections, two keywords including China and Chinese will be added as the scoping review will focus on NSSI in China.
Three English-language databases (Web of Science, PubMed, and PsychINFO) and three Chinese-language databases (CNKI, Weipu, and Wanfang) were searched for peer-reviewed articles published between January 1, 2000, and December 30, 2022. For papers in Chinese, only articles published in high-quality journals were considered (i.e., Chinese Core Journals). The reference lists of the included papers/reports were reviewed to identify other potentially eligible studies and reports not identified in the electronic searches.
All studies meeting the following criteria were included in the current review: 1) studies conducted on Chinese participants; 2) studies focused on the prevalence, methods, risk factors, as well as intervention and prevention programs for NSSI behaviors in China; 3) empirical study, qualitative study or meta-analysis; 4) published in peer-reviewed journals. The general exclusion criteria were: 1) No outcomes relate to NSSI; 2) Unable to distinguish NSSI from suicidal thoughts and behaviors (STBs); 3) Not about Chinese population; 4) Not a peer-reviewed research article or review. For section one, the extra exclusion criteria were: 1) Not about NSSI prevalence or method; 2) Lack of details about NSSI prevalence or method; 3) Not an empirical study, qualitative study or meta-analysis. For section two, the extra exclusion criteria were: 1) papers not about risk factors associated with NSSI; 2) literature reviews did not include the empirical data. For section three, the extra exclusion criteria were: Not about NSSI prevention or intervention programs.
Peer-reviewed journal articles were retrieved and imported into Covidence, a well-used software for reviews, which automatically identified and removed duplicate records. The first round of screening was based on titles, keywords, and abstracts. The second round of review was based on the full text of potentially eligible papers and involved the peer-reviewed articles that met the inclusion and exclusion criteria. Both screening and full-text review were carried out by two independent researchers for each section (i.e., Section 1: ZX, DXE; Section 2: LBW, HYH; Section 3: CDY, YJA). Disagreements were discussed with third reviewers (first authors, QDY and WX) until a consensus was reached.
Data extraction
The items in the final data-collection form used for peer-reviewed articles are shown in the Supplementary section. An independent researcher (LDY) documented and cross-checked each section, with a total of six independent researchers (Section 1: ZX, DXE; Section 2: LBW, HYH; Section 3: CDY, YJA). Any disagreements were resolved by senior reviewers (QDY and WX).
Summarising and reporting the results
In Section 1, the spatiotemporal information of included publications were summarised, then the prevalence of NSSI and method of NSSI were further summarised and presented in tables by a leading analyst (WX). In Section 3, the prevention and intervention programs targeting NSSI in China were presented in tables by CDY. Data charting for each section were conducted by mapping the data extracted from the selected articles and guided by LDY.
Assessment of intervention quality
Two independent reviewers (CDY, YJA) appraised eligible studies for intervention quality in Section 3 using the appropriate standardized critical appraisal instruments from Joanna Briggs Institute System (JBI).19 Any disagreements that arisen between the reviewers were resolved through discussion or with a third reviewer (QDY). The result of the critical appraisal is reported in narrative form and refer to the table number. All studies, regardless of the results of their methodological quality, underwent data extraction and synthesis (where possible).
Results
Section 1: NSSI prevalence and methods in China
PRISMA flow diagram
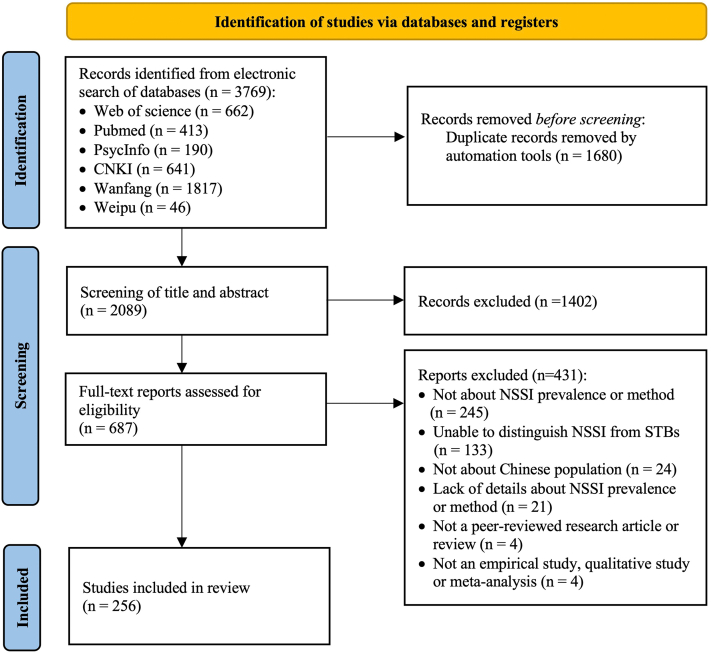
As is shown in the PRISMA flowchart (Fig. 1), we identified 3769 items in our initial literature search. After removing 1680 and 1402 duplicates or apparently irrelevant records, we examined 687 full-text articles. After full-text screening, 256 articles fulfilled the inclusion criteria, among which 123 (48.0%) were Chinese-language research articles. Of the reported studies, 209 (81.6%) were cross-sectional studies, 38 (14.8%) were longitudinal studies, 5 (2.0%) were meta/review studies, and 4 (1.6%) were qualitative studies. The characteristics and citations of each study are shown in the Supplementary Tables S3 and S4.
Fig. 1.
PRISMA flowchart of studies identified for inclusion in scoping review about NSSI prevalence and method in China.
Spatiotemporal distribution of included publications
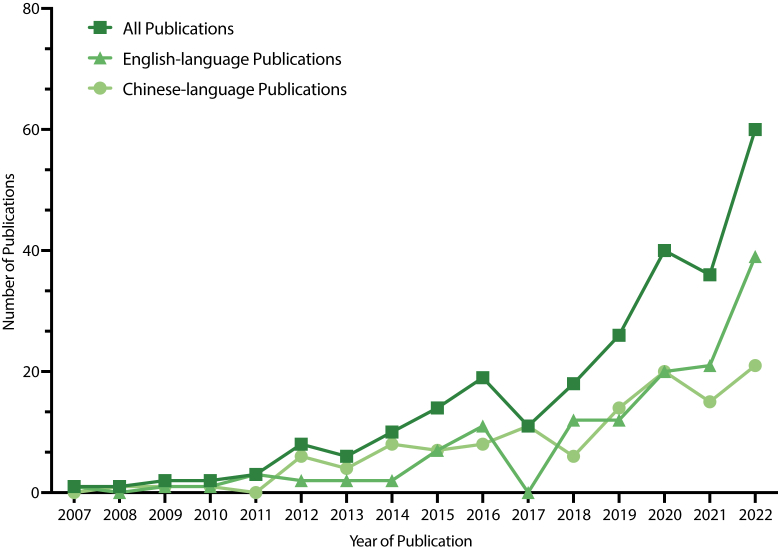
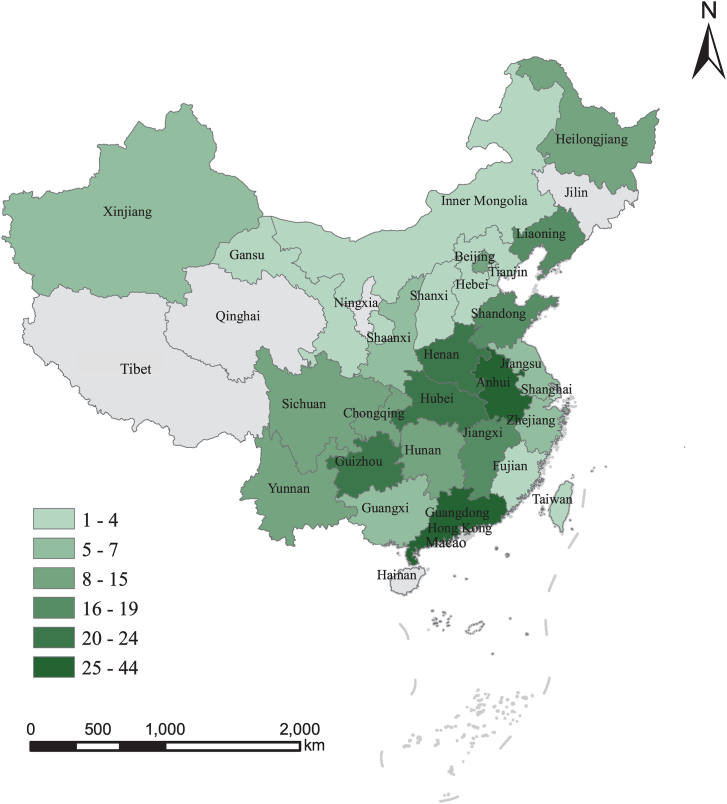
All the 256 publications were conducted between 2007 and 2022, from 28 provinces of China. As shown in Fig. 2, the number of studies about NSSI prevalence and methods conducted in China increased over time, particularly after 2017.
Fig. 2.
Annual number of articles included in the analysis published from 2007 to 2022.
Of 228 publications with geographic information, most publications were from institutions located in China's more developed eastern provinces and provincial-level municipalities, as is shown in Fig. 3. The top five locations were Guangdong (N = 44), Anhui (N = 39), Guizhou (N = 24), Henan (N = 23), and Hubei (N = 22).
Fig. 3.
Provincial distribution of 228 papers included in the analysis based on the location where the study was conducted.
After combining publications with the same sample (N = 42), a total of 205 cross-sectional and longitudinal studies with information about the prevalence of NSSI and NSSI methods were analyzed, which concluded 188 (91.7%) school samples and 11 (5.4%) clinical samples, 4 (1.9%) community samples and 2 (1.0%) other samples. Besides, 5 meta-analyses/reviews and 4 qualitative studies were also described.
NSSI prevalence among target populations
A total of 200 cross-sectional and longitudinal studies have provided information about the prevalence of NSSI. Among them, 187 specifically targeted students ranged from primary school to college, with some studies simultaneously included samples across multiple groups. Additionally, only 6 studies have reported NSSI prevalence among primary school students, and a total of 73 studies have reported specific NSSI prevalence for middle school students, while the number of studies decreased to 45 for high school students and 43 for college students. Notably, only 48 (24%) studies have provided the lifetime prevalence of NSSI. Based on the available data points, the lifetime prevalence of NSSI among primary, middle, high schools, and college is estimated to be 24.7% [IQR 18.7–38.0]. Moreover, the lifetime prevalence of NSSI remains high for children and adolescents, which is estimated to be 29.3% (28.5–30.1) for primary school students, 25.3% (20.7–41.9) for middle school students and 32.8% (26.6–35.6) for high school students. Importantly, college students reported the lowest lifetime NSSI prevalence 21.2% (15.8–30.4), suggesting an early onset trend of NSSI. Specifically, the age-specific prevalence estimates of NSSI among students are shown in Table 1. Additionally, 2 studies have reported the prevalence of self-neglect among older adults, which was 23.2% for community-dwelling older adults living alone in China and 30.3% for older adults admitted to the hospital in the COVID-19 pandemic era.20,21
Table 1.
Age-specific prevalence of NSSI among Chinese students.
| 6-month prevalence |
12-month prevalence |
Lifetime prevalence |
||||
|---|---|---|---|---|---|---|
| Range | IQRa | Range | IQRa | Range | IQRa | |
| Overall students | 6.9–34.4 | 17.4 (13.4–24.1) | 1.8–83.4 | 24.9 (14.0–33.4) | 0.4–47.3 | 24.7 (18.7–38.0) |
| Primary school | 3.8–38.6 | 19.3 (11.6–27.9) | 27.6–31.0 | 29.3 (28.5–30.1) | ||
| Middle school | 10.3–34.4 | 16.3 (13.6–29.2) | 4.6–51.6 | 30.4 (23.1–36.3) | 5.4–52.8 | 25.3 (20.7–41.9) |
| 7th grade | 12.2–48.1 | 31.0 (17.8–36.1) | 8.9–43.4 | 31.1 (20.0–37.2) | ||
| 8th grade | 7.0–51.1 | 29.9 (21.8–37.3) | 8.4–38.6 | 33.5 (20.9–36.1) | ||
| 9th grade | 4.1–35.1 | 22.4 (18.7–30.4) | 8.6–45.3 | 21.4 (9.7–35.9) | ||
| High school | 13.8–18.4 | 16.0 (14.9–17.2) | 4.3–41.0 | 27.6 (20.4–30.6) | 23.6–61.0 | 32.8 (26.6–35.6) |
| 10th grade | 27.7–47.9 | 33.0 (31.1–37.2) | 41.5 | 41.5 | ||
| 11th grade | 22.7–49.3 | 38.6 (36.1–44.0) | 8.9–38.3 | 23.6 (16.2–30.9) | ||
| 12th grade | 23.7 | 23.7 | 35.9 | 35.9 | ||
| College | 6.9–13.7 | 11.8 (8.2–12.6) | 1.8–56.5 | 11.8 (9.8–15.8) | 0.4–42.5 | 21.2 (15.8–30.4) |
Subgroup analysis was conducted according to period prevalence measure, mainly include 6 m, 12 m, and lifetime.
Data are median (IQR); range unless otherwise specified.
Besides, the lifetime NSSI prevalence is estimated to be 26.5% (20.0–37.0) among female students and 27.7% (19.0–36.9) among male students. 76 samples have shown significant sex differences for NSSI prevalence, while 44 samples have reported insignificant sex differences. The detailed sex-specific prevalence estimates of NSSI are shown in Table 2. Notably, three studies have provided NSSI prevalence during the last year among sexual minority individuals, which is 30.9%22 and 31.1%23,24 in community sample. Specific NSSI prevalence during the past year among gay (22.5%), lesbian (42.2%), and bisexual (43.5%) was also provided.23,24
Table 2.
Sex-specific prevalence of NSSI among Chinese students.
| 6-month prevalence |
12-month prevalence |
Lifetime prevalence |
||||
|---|---|---|---|---|---|---|
| Range | IQRa | Range | IQRa | Range | IQRa | |
| Female | 8.4–32.4 | 18.7 (14.6–24.5) | 2.2–83.3 | 24.3 (14.1–35.7) | 0.5–50.7 | 26.5 (20.0–37.0) |
| Primary school | – | – | 23.6 | 23.6 | 26.3 | 26.3 |
| Middle school | 13.9–32.4 | 29.4 (21.6–30.9) | 5.9–53.0 | 29.6 (23.4–41.2) | 8.6–47.6 | 41.6 (39.1–46.6) |
| High school | 16.6–20.8 | 18.7 (17.7–19.8) | 6.7–37.6 | 25.2 (14.1–29.2) | 33.9 | 33.9 |
| College | 8.4–14.8 | 11.6 (10.0–13.2) | 2.2–24.0 | 10.0 (8.7–14.0) | 0.5–37.0 | 20.4 (16.5–27.4) |
| Male | 5.8–30.6 | 14.0 (9.4–22.5) | 1.4–83.5 | 24.0 (15.3–30.9) | 0.3–46.9 | 27.7 (19.0–36.9) |
| Primary school | – | – | 25.1 | 25.1 | 28.8 | 28.8 |
| Middle school | 6.3–30.6 | 24.9 (15.6–27.8) | 3.0–39.2 | 27.8 (17.8–33.2) | 11.3–46.9 | 38.4 (37.6–39.4) |
| High school | 10.4–15.3 | 12.9 (11.6–14.1) | 6.9–30.9 | 19.3 (10.0–23.7) | 30.2 | 30.2 |
| College | 5.8–12.7 | 9.2 (7.5–11.0) | 1.4–24.8 | 14.7 (10.8–16.8) | 0.3–42.7 | 24.5 (17.0–33.9) |
Subgroup analysis was conducted according to period prevalence measure, mainly include 6 m, 12 m, and lifetime.
Data are median (IQR); range unless otherwise specified.
NSSI prevalence among other specific populations
The NSSI prevalence among Chinese left-behind children (LBC) remains high according to 21 related studies, which is estimated to be 32.0% (28.5–32.8) over the past six months, 19.8% (13.7–35.0) during the last year, and 27.5% (19.5–42.4) in a lifetime. Notably, 4 studies have provided more detailed information about parental migration, and those with two migrated parents demonstrated higher NSSI prevalence than one migrated parent.25, 26, 27, 28
Besides, 3 studies have reported NSSI prevalence in disabled students,29, 30, 31 among which deaf-mute middle school students demonstrated extremely high NSSI prevalence (83.4%) during the past year.29 For 5 studies that included clinical samples,32, 33, 34, 35, 36 NSSI prevalence among those diagnosed with mood disorders was estimated to be 62.6% (56.2–67.9) during the last year.
Notably, the lifetime NSSI prevalence (0.78%) among soldiers was relatively low reported by one study.37 Another group of interest is Chinese heroin-dependent patients, although there are many studies on NSSI behaviors in this group, the vast majority do not provide a clear definition of NSSI, so we only involved one relevant empirical study and one systematic review in this scoping review, which reported that the prevalence of NSSI was 13.8% for heroin-dependent patients receiving methadone maintenance treatment and 4.4% for heroin-dependent patients receiving detoxification treatment.38,39 In addition, one study reported the prevalence of NSSI (14.8%) during the past year among male prisoners.40
NSSI methods among target populations
A total of 68 cross-sectional and longitudinal studies have provided information about specific NSSI methods, which concluded 57 (83.8%) school samples, 8 (11.8%) clinical samples, 2 (2.9%) community samples, and another (1.5%) sample.
In order to integrate information from more articles, we summarized the relative ranking of the methods here, since only some of the articles provided the prevalence of NSSI methods. Based on the available data points, the NSSI methods commonly used by primary, middle, high schools, and college students include scratching, hitting, biting, pulling hair, cutting, pinching, banging, interfering with wound healing, carving, inserting objects to the nail or skin, burning, punching, stabbing, and striking.
Among these, scratching (N = 30), hitting (N = 27), biting (N = 22), pulling hair (N = 20), cutting (N = 19), and pinching (N = 18) are considered to be the top six most used NSSI methods in Chinese students in most of the studies. 14 studies have reported specific NSSI methods conducted by middle school students, while the number of studies decreased to 11 for high school students and 9 for college students. Moreover, scratching, cutting, and biting have been shown as common methods for secondary school students, while scratching (N = 5), hitting (N = 5) and biting (N = 4) have been reported as common methods for college students. Specifically, the age-specific NSSI methods are shown in Table 3. Additionally, one study has reported NSSI methods used by older adults, including substance abusing, failing to maintain a minimum level of hygiene and sanitation, and refusing to ask for any kind of assistance although they were exposed to unsafe environments.21
Table 3.
Age-specific and sex-specific method of NSSI among Chinese students.
| Top three NSSI methods |
|---|
| Overall students (N = 52) |
| scratching (N = 30), hitting (N = 27), biting (N = 22), pulling hair (N = 20), cutting (N = 19), pinching (N = 18), banging (N = 9), interfering (N = 3), carving (N = 2), inserting (N = 2), burning, punching, stabbing, striking |
| Middle school (N = 14) |
| scratching (N = 9), biting (N = 9), cutting (N = 6), hitting (N = 5), pinching (N = 4), pulling hair (N = 4), interfering (N = 2), banging, carving |
| High school (N = 11) |
| scratching (N = 9), cutting (N = 5), pulling hair (N = 5), biting (N = 4), hitting (N = 3), pinching, banging, carving, electrocuting, strangling |
| College (N = 9) |
| scratching (N = 5), hitting (N = 5), biting (N = 4), pulling hair (N = 4), pinching (N = 3), banging (N = 3), cutting (N = 2), punching (N = 2), inserting, dripping acid, carving, ripping |
| Female (N = 24) |
| scratching (N = 12), biting (N = 11), cutting (N = 10), pinching (N = 9), hitting (N = 8), pulling hair (N = 8), interfering (N = 3), burning (N = 3), punching (N = 2), carving (N = 2), banging (N = 2), inserting, pricking, ripping, strangling, striking, stabbing |
| Male (N = 24) |
| banging (N = 12), hitting (N = 12), scratching (N = 10), biting (N = 9), pulling hair (N = 9), cutting (N = 5), pinching (N = 4), punching (N = 4), burning (N = 2), stabbing (N = 2), electrocuting, exposing heat/hot, ingesting, interfering, ripping, rubbing, strangling, dripping acid, carving |
As shown in Table 3, common NSSI methods include scratching (N = 12), biting (N = 11), cutting (N = 10), pinching (N = 9), pulling hair (N = 8), and hitting (N = 8) for female students. As for male students, banging (N = 12), hitting (N = 12), scratching (N = 10), biting (N = 9), and pulling hair (N = 9) are common NSSI methods. Notably, two studies have provided NSSI methods conducted by sexual minority individuals, among which pulling hair, scratching, and cutting were shown as the top three methods.23,24
NSSI methods among other specific populations
In total, 6 studies have reported NSSI methods conducted by those diagnosed with mood disorders, among which cutting and scratching were consistently shown to be the most common methods for this population.32,33,35,36,41,42 Meanwhile, 2 studies have reported sex-specific NSSI methods among individuals with mood disorders.36,41 For female, scratching and pinching were most commonly used methods, while for male, scratching and hitting were most commonly used methods.
Notably, burning was shown to be the most common NSSI method for deaf-mute middle school students, heroin-dependent patients receiving methadone maintenance treatment and male prisoners.29,39,40
Section 2: risk factors of NSSI in China
PRISMA flow diagram
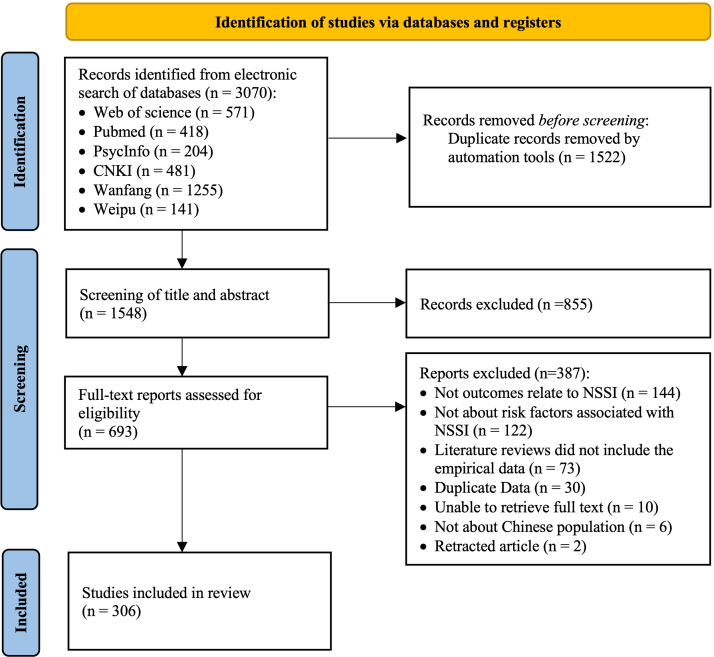
The details of search processes are summarized in Fig. 4. A total of 3070 records were sourced in our initial literature search, of which only 1548 records were deemed eligible after title, abstract and keyword screening. After removal of 855 apparently irrelevant records, we examined 693 full-text articles. After full-text screening, 306 articles fulfilled the inclusion criteria, among which 159 (52.0%) were Chinese-language research articles. Of the reported studies, 263 (85.9%) were cross-sectional studies, 36 (11.8%) were longitudinal studies, 3 (1.0%) were cohort studies, 3 (1.0%) were qualitative studies, and 1 (0.3%) was a meta-review. The characteristics and citations of each study are shown in the Supplementary Table S4.
Fig. 4.
PRISMA flowchart of studies identified for inclusion in scoping review about the risk factors of NSSI.
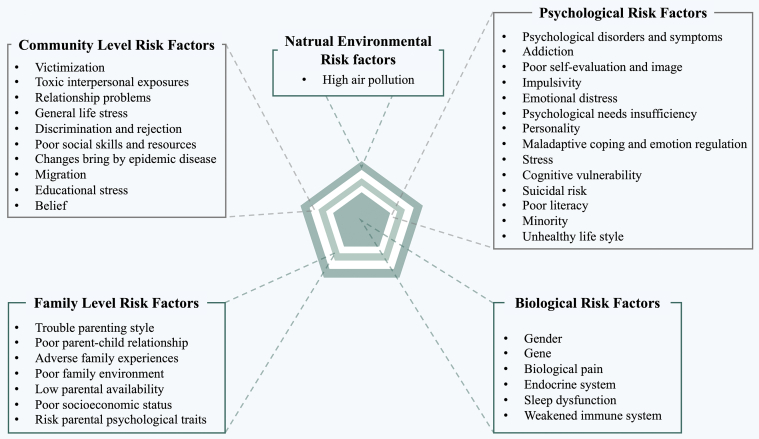
The risk factors of NSSI from biopsychosocial-ecological approach
The biopsychosocial-ecological framework is a comprehensive model that recognizes the interplay of biological, psychological, social, and ecological factors in shaping human health and well-being. This framework acknowledges that health and illness are not solely determined by biological or genetic factors but are also influenced by various social and environmental factors such as culture, community, and the physical environment.43 As showed in Fig. 5, the risk factors of NSSI in China identified in the reviewed studies are presented using five broad themes based on the framework of biopsychosocial-ecological approach. Given that stating all the 249 factors would be extensive, we referred to previous literature and categorized them accordingly.44,45
Fig. 5.
The risk factors of NSSI from biopsychosocial-ecological framework.
Biological risk factors
The first level identifies factors at biological level that increase the likelihood of a Chinese individual's NSSI behaviors. Among the 306 articles included in the review, 46 (15.0%) reported the association of biological risk factors and NSSI behaviors. There are 6 categories and 19 factors included at this level. The categories of biological risk are gender (N = 27), sleep dysfunction (N = 8), gene (N = 7), endocrine system abnormality (N = 3), biological pain (N = 1), and weakened immune system (N = 1).
Psychological risk factors
The second level identifies factors at psychological level that increase the likelihood of a Chinese individual's NSSI behaviors. 209 (68.3%) studies included in the review reported psychological risk factors of NSSI, with a total of 14 categories and 114 factors. The categories of psychological risk include psychological disorders and symptoms (N = 88), poor self-evaluation and image (N = 36), emotional distress (N = 33), maladaptive coping and emotion regulation (N = 30), cognitive vulnerability (N = 24), addiction (N = 24), personality (N = 16), impulsivity (N = 15), stress (N = 8), suicidal risk (N = 7), poor literacy (N = 5), psychological needs insufficiency (N = 5), minority (N = 4), and unhealthy lifestyle (N = 1).
Family level risk factors
This level identifies factors at family level, which may also trigger higher risk of individual's NSSI behaviors. A total of 110 (35.9%) studies reported the associations of family level risk factors and NSSI. There are 7 categories and 63 factors included at this level. The categories of family-level risk level include adverse family experiences (N = 41), trouble parenting style (N = 28), poor family environment (N = 21), poor parent–child relationship (N = 20), low parental availability (N = 7), poor socioeconomic status (N = 5), and risk parental personality traits (N = 2).
Community level risk factors
In this level, a broader societal relationship factors that increase individual's possibilities of NSSI behaviors have been reviewed. There were 113 (36.9%) studies reporting associations between community-level risk and NSSI, including 10 categories and 52 factors. The categories of community risk include victimization (N = 32), general life stress (N = 30), relationship problems (N = 26), discrimination and rejection (N = 10), migration (N = 10), educational stress (N = 10), toxic interpersonal exposures (N = 5), poor social skills and resources (N = 2), changes bring by epidemic disease (N = 2), and belief (N = 1).
Natural environmental risk factor
The natural environmental risk factor refers to the potential risks posed by natural elements such as climate change and other natural disasters. Evidence of the relationship between high air pollution and high NSSI was found in 1 record. Air pollution is the release of pollutants into the air that can harm human health and the environment. This study identified particulate matter 2.5 (PM2.5), ozone 3 (O3), and carbon monoxide (CO) as the air pollutants that increase the risk of NSSI.
Section 3: prevention and intervention programs targeting NSSI in China
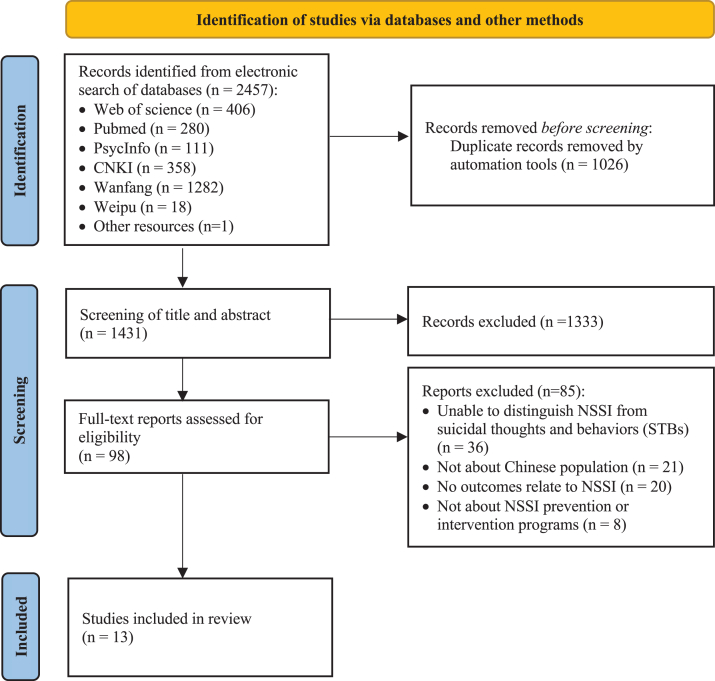
PRISMA flow diagram
As shown in the PRISMA flowchart (Fig. 6), a total of 2457 records were sourced, of which only 1431 records were deemed eligible after titles, abstracts, and keywords screening. After full-text screening, a total of 13 records were included for this review, and data was charted accordingly.
Fig. 6.
PRISMA flowchart of studies identified for inclusion in scoping review about the prevention and intervention programs targeting NSSI in China.
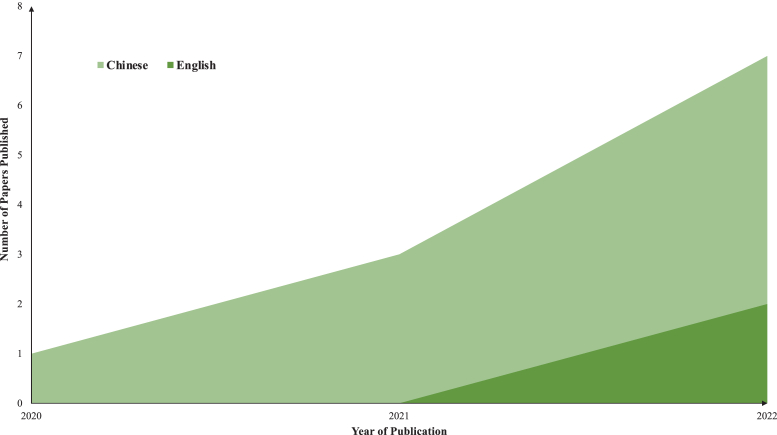
The number of publications
A total of 13 papers reported on the prevention and intervention programs targeting NSSI in China, and the number of published literatures sharply increases year by year (Fig. 7); 12 out of 13 (92%) were empirical studies, while one study was a review study (8%). Two papers (15.8%) were published in English journals and 11 papers (84.6%) in Chinese journals. The relevant literatures were published in the last two years (from 2020 to 2022), and the number of publications reached 9 out of 12 in year 2022.
Fig. 7.
The number of publications that report the prevention and intervention programs targeting NSSI in China.
The intervention population
Generally, 8 out of 12 (66.7%) empirical studies targeted teenagers (e.g., aged from 12 to 18 years old), while 3 studies (25%) focused on adults, and 1 study (8.3%) did no specify the age of participants. In addition, 10 studies (83.3%) were aimed at outpatients or inpatients, and 2 studies (16.7%) were community samples. The sample sizes were generally small, with almost all below 50.
Meanwhile, 8 studies (66.7%) were primarily focused on depressive symptoms, and one study (8.3%) targeted the borderline personality disorder. Significantly, only three of the interventions (25%) were developed specifically for individuals with NSSI behaviors, despite evidence suggesting that this might be a more effective intervention strategy.
The intervention strategies
In terms of treatment aim, 11 of 12 empirical studies (91.7%) were intervention studies and one study (8.3%) was preventive study. As for treatment format, 8 of 12 empirical studies (66.7%) used individual therapy alone, 1 study (8.3%) used group therapy alone, 2 studies (16.7%) mixed individual therapy with group therapy, and 1 study (8.3%) mixed individual therapy, group therapy, and family therapy.
As shown in Table 4, eight intervention strategies were used in the intervention programs targeting NSSI in China. The most commonly used intervention strategies were cognitive behavioral therapy (CBT; N = 2, 16.7%) and dialectical behavior therapy (DBT; N = 2, 16.7%), followed by acceptance and commitment therapy (ACT; N = 1, 8.3%), emotion regulation skills (ERS; N = 1, 8.3%), cognitive therapy (CT; N = 1, 8.3%), sensory integration therapy (N = 1, 8.3%), Hazard analysis and critical control point therapy (N = 1, 8.3%) and Colaizzi analysis (N = 1, 8.3%). Additionally, 4 studies (33.3%) did not specify any particular intervention strategy.
Table 4.
Summary of studies about the prevention and intervention programs targeting NSSI in China.
| No | Authors | Language | Sample | Settings | Size (I:C) | Treatment (I) | Treatment (C) | Strategies | Format | Durations (Sessions; Session/Week; Mins/Session) | Study Type | Main outcomes | Pre/post (Months/Weeks) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ding et al., 202146 | Chinese | Adolescent with depression | Inpatient | (45:45) | PIa | TAU (MT & PT) | CT; ERS | Personal | 7/2/60 | RCT | NSSI | Yes (3 M) |
| 2 | Xue et al., 202247 | Chinese | Adolescent with NSSI | Outpatient | (60:60) | PIa | TAU (MT& PIb) | ACT | Personal/Group/Family | 6/1/30-50 | CCT | NSSI | Yes (post) |
| 3 | Quan et al., 202048 | Chinese | Adolescent with depression | Outpatient | (40:40) | PTa | TAU (MT) | Sensory integration | Personal/Group/Family | 36/3/90 | RCT | Depression | Yes (4/2/12 W) |
| 4 | Yu et al., 202149 | Chinese | Adolescent with depression | Inpatient; Outpatient | (18:18) | PTa | TAU (MT) | NA | Personal | 10/5/20 | RCT | NSSI | Yes (2 W) |
| 5 | Zeng et al., 202250 | Chinese | Adult with depression | Inpatient | (43:42) | PTa | TAU (MT) | NA | Personal | 9/3/NA | CCT | NSSI | Yes (6 M) |
| 6 | Chen et al., 202251 | English | Vocational students with depression | Community | (320:1728) | PI | NA | NA | Personal | NA/NA/NA | RS | NSSI | Yes (6 M) |
| 7 | Lin et al., 202152 | Chinese | Adult with depression | Inpatient; Outpatient | (14:14) | PIa | TAU (MT) | DBT | Personal | 6/1/50 | RCT | NSSI | Yes (post) |
| 8 | Su et al., 202253 | Chinese | Adolescent with NSSI | Outpatient | (45:45) | PIa | TAU (MT) | DBT | Personal | NA/NA/NA | RCT | NSSI | Yes (1/3/6 W) |
| 9 | Zhang et al., 202254 | Chinese | Adults with BPD | Inpatient | (175:182) | MAa | TAU (PI + MT + PT) | HZ | Personal/Family | NA; NA; NA | CCT | NSSI | Yes (post) |
| 10 | Huang et al., 202255 | Chinese | Adolescent with NSSI | Patient | (63:63) | MAa | TAU (PI) | CBT; CA | Personal/Group/Family | 5/NA/NA | RCT | NSSI | Yes (post) |
| 11 | Lu et al., 202256 | Chinese | Adult with depression | Outpatient | (45:45) | PIa/MA | TAU (NA) | CBT | Personal | 8/1/NA | RCT | NSSI | Yes(12 W) |
| 12 | Zhang et al., 202257 | English | Adult with depression | Community | (42:42) | PIa | TAU (MT) | NA | Group | 6/1/90 | RCT | NSSI | Yes (post) |
I = Intervention; C = Control group; CT = Cognitive therapy; CBT = Cognitive behavioral therapy; ACT = Acceptance and commitment therapy; DBT = Dialectical behavior therapy; ERS = Emotion regulation skills; Personal = Individual intervention/treatment; NA = Not addressed; PI = Psychotherapeutic interventions; PT = Physical therapy; RCT = Randomized Controlled Trial; CCT = Clinical Controlled Trial; RS = Retrospective Study; MT = Psychopharmacology treatment; BPD = Borderline Personality disorder; MA = Management; HZ = Hazard analysis and critical control point; CA = Colaizzi analysis.
represent this is the added treatment in regular settings.
represent cognitive therapy.
The overall quality of published studies
The quality of published empirical studies about the prevention and intervention programs targeting NSSI in China is shown in Supplementary Fig. S1. The overall quality is acceptable, but eight articles (66.6%) with a RCT design did not fully comply with the reporting standards of RCT. There were three articles (25%) that utilized CCT design without randomization control, and one article (7.6%) which specified the approach of personalized intervention did not specify their operational strategies.
Discussion
To our knowledge, this is the very first attempt to synthesize evidence from a broad literature that examines the full picture of NSSI, including its frequency, method, risk factors, and prevention and intervention programs among Chinese population. In the first section, an overview of NSSI prevalence and NSSI methods in China are provided. Our study confirms that students were the most well-investigated population in China, and NSSI is highly prevalent among Chinese students. Common forms of NSSI among Chinese students included scratching, hitting, biting, cutting, pulling hair, and pinching. We not only provide the latest evidence on the prevalence of NSSI in Chinese population, but also describe the characteristics of NSSI method in China. At the same time, some specific groups came into our perspective during the scoping review of the general Chinese population, especially for some vulnerable groups (e.g., left-behind children, the disabled), as there are multiple empirical studies describing their NSSI characteristics. Thus, we conducted multiple subgroup analyses of these populations here. Our subgroup analyses of special populations allow us to gain a deeper understanding of mental health issues among these populations, thus providing more precise guidance and recommendations for relevant policies and interventions. In contrast to meta-analysis, our scoping review concludes multiple research methods (i.e., empirical studies, reviews, qualitative studies) and study designs (i.e., cross-sectional studies, longitudinal studies), and initially provides a more comprehensive and detailed overview of the prevalence and methods of NSSI by extensively collecting and synthesizing the existing literature in China.
In the second section, we identified several risk factors of NSSI from a biopsychosocial-ecological approach among Chinese population. This theoretical framework explains human developmental outcomes from a unified perspective, which highlights the importance of risk factors from the biological system (e.g., genes), psychological system (e.g., emotional distress), family environment (e.g., family experience), community environment (e.g., lower social support), built environment, and natural environment (e.g., pollution) when considering an individual's maladaptive behaviors. Although no factors have been found within the built environment, it is worth pointing out that, several risk factors from community environment are unique under the Chinese cultural context, for example, “the only child situation”, “left-behind children”, “academic stress”, and “internal rural-to-urban migration” which clearly raised a call for further exploration. To the best of our knowledge, to date, no single article has consolidated the research on Chinese population who practice NSSI behaviors from such a comprehensive framework. In the last section, we examined the existing prevention or intervention programs that have been developed for Chinese population to reduce their NSSI behaviors, as well as analyzed their efficacy. The biggest gap identified in the literature is the lack of NSSI prevention programs designed for Chinese population.
NSSI prevalence in China
In the first section, we found that 200 studies reported the prevalence of NSSI covering 1,096,825 Chinese (excluded 5 review studies to avoid duplication), among which 187 studies were related to school samples (N = 1,088,433). We found that almost one in four (24.7%) students in primary, middle, high schools, and college (aged between 5 and 25 years) reported NSSI behaviors in their lifetime. These studies focused on four age groups in China, which we summarized as primary school children (5–12 years), middle school students (12–15 years), high school students (15–18 years), and college students (18–24 years). The lifetime prevalence of NSSI was found as 29.3% in primary school children, 25.3% in middle school students, 32.8% in high school students, and 21.2% in college students. Besides, the sex-specific lifetime prevalence of NSSI was 26.5% among female students and 27.7% among male students.
Practically, 4 meta-analyses of NSSI prevalence in China have already been conducted, and the prevalence of NSSI among middle school, high school, and college students was calculated separately. Lang et al. reviewed 26 studies in 2018 and reported the pooled NSSI prevalence (22.4% [95% CI: 18.8%–25.7%]) among secondary school students, which was 21.9% [17.6%–26.2%] for females and 20.6% [16.1%–25.0%] for males.58 Yang et al. reviewed 33 studies in 2018 and estimated the pooled NSSI prevalence among secondary school students (female: 23.5%, male: 22.2%) and college students (female: 23.4%, male: 30.7%).59 Han et al. reviewed 22 studies in 2017 and reported the pooled NSSI prevalence (27.4% [24.5%–30.2%]) among secondary school students, which was 25.6% [22.3%–28.9%] for females and 27.2% [23.5%–30.9%] for males.60 Pan et al. reviewed 23 studies in 2016 and estimated the pooled NSSI prevalence (16.6% [10.7%–24.7%]) among college students, which was 17.8% [10.8%–27.8%] for females and 16.2% [9.7%–25.9%] for males.61 Above studies and our study have consistently documented a high prevalence of NSSI among Chinese students. Also, our study provides evidence for the existence of unique gender patterns in the NSSI, namely, a female bias among middle school and high school students, and a male bias among college students.59
NSSI methods in China
Common forms of NSSI include scratching, hitting, biting, cutting, pulling hair, cutting and pinching among Chinese students. According to 4 qualitative studies, cutting has also been reported as the most common NSSI method (65.0%–95.7%) among Chinese adolescents.62, 63, 64, 65 Moreover, approximately half of the existing articles reported that scratching and biting were more prevalent NSSI methods in females, while banging and hitting were more prevalent methods in males. Given that these findings were based on a substantially smaller subset of studies (N = 24), it is hard to draw firm conclusions that there is a difference in the way females and males conduct NSSI. Thus, future research should continue to examine the possibility of gender difference in NSSI methods.
To the best of our knowledge, this is the first Chinese review to date that provides a review of NSSI methods and performs a subgroup analysis of gender and age. However, researchers must carefully consider the use of more standardized terms when measuring and describing different NSSI methods, and clarify terms to encode the same NSSI method under Chinese and English contexts. For example, semantically similar NSSI methods including the following five categories: 1) NSSI methods involving physical impact: striking, hitting, and banging; 2) NSSI methods involving contacting with objects or surfaces: scraping, rubbing, erasing, abrading, and friction; 3) NSSI methods involving piercing the skin with a sharp object: stabbing, pricking, and probing with needle; 4) biting and gnawing; 5) burning and scalding. There are differences in severity and intent between each of the specific behaviors in these five categories of NSSI behaviors, but they are rarely distinguished carefully among the Chinese articles.
The risk factor of NSSI from a biopsychosocial-ecological perspective
Biological risk
This primary and most direct level identifies factors at the biological level that increase the likelihood of a Chinese individual engaging in NSSI behaviors, including gender, sleep dysfunction, gene, endocrine system abnormality, biological pain, and weakened immune system. These findings align with the previous studies focused on Western populations.66
Following the proposed model in the previous meta-analysis, which suggested the risk factors and mechanisms involved in NSSI can be distinguished into both trait and state factors,67 our studies pointed out the fact that the majority of the current studies among Chinese population only focused on the trait factors rather than state markers (e.g., a transient biological marker that reflect individual's current statues; the experimental exposure to stress, HPA axis). More studies exploring these associations are required.68
Psychological risk
The second level identifies factors at psychological level that increase the likelihood of a Chinese individual's NSSI behaviors. In total, 114 risk factors were identified and classified into 14 categories, including psychological disorders and symptoms, addition behavior, poor self-evaluation or image, impulsivity, limited development need, personality, poor coping styles, high level of stress, cognitive vulnerability, suicidal risk, poor literacy, minority group, and unhealthy lifestyle. Several findings are consistent with the current meta-analysis, which included 25 articles and found that mental disorders, low health literacy, problem behaviors at this level appear to be risk factors for NSSI among adolescents.69
The findings also provide new evidence for the four functional model of NSSI, that is, individuals with emotional disorders or symptoms may lack effective coping strategies and are more likely to engage in NSSI behaviors, as a maladaptive way for relief or triggering feelings, and getting rid of or getting attention from social reinforcement.70
However, the specific pathways to explain the onset and maintenance of NSSI are still missing. Especially, the revised cognitive emotional model of NSSI (CEM-NSSI) has indicated how cognitive and emotion regulation work jointly to govern NSSI, but more empirical studies are still required.71
Family level risk
Individuals are not developed in isolation, but are instead shaped by their family systems. Therefore, this level identifies factors at family level, for example, trouble parenting style, poor parent–child relationship, adverse family experiences, poor family environment, low parental availability, socioeconomic status (SES), and risk parental personality traits, which may also trigger higher risk of an individual's NSSI behaviors. These findings are in line with previous meta-analyses, and the large impact of the family on individual's NSSI behaviors has been well acknowledged.72 Our findings also align well with the NSSI family distress cascade theory, which indicates a dynamic and reciprocal patterns of influence between parents' NSSI behaviors and their children's.73
However, most research still relied on self-report measurements, which may not capture the ongoing and instantaneous interaction within family members. Using multiple informants or qualitative research might better capture these complex associations. For example, the Lausanne Trilogue Play (LTP) has been proposed as a new observational assessment tool for testing the dynamic interaction between family members and family behaviors.74 Furthermore, it has been observed that certain research findings are inconsistent. Specifically, regarding the frequency of NSSI, high paternal education level is a protective factor for single NSSI, while it is a risk factor for repeated NSSI.75 These conflicting results highlight the necessity for additional research to elucidate these relationships.
Community level risk
At this level, there has been a focus on broader societal relationship factors (e.g., peer relationships, school relationships and community level factors) that increase individuals’ possibilities of NSSI behaviors. That includes victimization, toxic interpersonal exposures, relationship problems, general life stress, discrimination and rejection, poor social skills and resources, changes bring by epidemic disease, migration, educational stress, and belief.
In the current review, one empirical study found that a higher level of religious belief predicted a higher level of NSSI behaviors. This counterintuitive finding of belief is not consistent with the mainstream findings in Western cultures, which identified religiosity or spiritual beliefs as a significant protective factor against NSSI behaviors.76 However, it is worth noting that the results of this meta-analysis showed a small effect. Therefore, further clarification is urgently needed to understand the possible underlying mechanisms between these associations, including a cultural-oriented perspective analysis.
The social safety theory hypothesizes that developing and maintaining friendly social bonds is a basic principle of human behaviors. Threats to general social safety, such as bullying or toxic relationships, may lead to self-harm behaviors. However, the complex underlying mechanisms between exposures to environmental stress and NSSI remain unclear. For example, NSSI may reversely represent a behavioral trigger that induces neuroinflammation, worsening an individual's perception of social threats and increasing their propensity to engage in self-harm behaviors.77 Therefore, future research may further consider the possibilities of the interactions between risk factors within or across levels regarding later NSSI behaviors.
Built environmental risk and natural environmental risk
The built environmental level identifies risk factors in an overlapping zone between culture and nature, namely, man-made environment, for example, landscapes. However, to best of our knowledge, no study has focused on the impact of risk factors at this level on Chinese population's NSSI behaviors. For example, a previous study pointed out the fact that a desirable urban environment can make people feel at ease and comfortable, which may further promote the positive public emotions. While emotion is considered one of the most important triggers for NSSI, to what extent this indirect association may contribute to these maladaptive behaviors remains unclear.78
In addition, only one risk factor at natural environmental level has been highlighted, that is, high air pollution pertinent to particulate matter 2.5 (PM2.5), ozone 3 (O3), and carbon monoxide (CO). Air pollution is one of the greatest threats to human health. Inhaling particles from pollution can damage an individual's serotonergic and dopaminergic activity.79 However, the mechanisms underlying the association between air pollution and an individual's NSSI behaviors still require further explorations.
The current NSSI prevention and intervention program in China
In order to conduct a more comprehensive review of the existing prevention or intervention programs, several programs that were not specifically designed for NSSI issues have also been included,46,48,49,52, 53, 54, 55, 56,80 as long as they proved effective in reducing the symptoms of NSSI in the Chinese population. However, the number of programs is still extremely limited. After reviewing 1431 articles, only 12 empirical studies and 1 review met the inclusion criteria. This may be out of the reason that, we only focused on studies with clear distinctions between NSSI and STBs. In other words, studies did not specify that they focused on individual's self-harm behaviors without any intention to die were not included. This further highlights a crucial need for studies to use clear operational definitions, and more comprehensive measures that disentangle STBs from NSSI.
In addition, we found that almost all relevant literatures were published in the recent two years (from 2020 to 2022), and the number of published literatures sharply increased year by year. As illustrated in Fig. 1, the number of publications reached 9 out of 12 in year 2022. However, there is a significant difference in the number of studies compared with the previous reviews focusing on the Western populations. In total, two papers were published in English journals51,57 and 11 were in Chinese journals.46, 47, 48, 49, 50,52, 53, 54, 55, 56,80 In conclusion, the recent increase in papers reflects the growing interest in developing evidence-based prevention or intervention programs to decrease Chinese population's NSSI behaviors, following the global trends in recent years. The growing number of publications in year 2022 implies the fact that this trend will continue as more findings are published in the coming years. However, the limited numbers of publications regarding prevention and intervention programs also highlights lager research gaps in this filed, and this fact calls for more localized prevention and intervention programs to reduce these serious problems among the Chinese population. Another commonly observation was that most articles were published in local journals, in this case, more articles with international influence are highly demanded in the future.
The different formats of treatments
The majority of studies used the combination of medication and other treatments (e.g., psychotherapeutic intervention, physical therapy, and management treatment),46, 47, 48,50,52, 53, 54,80 given the clinical samples were recruited. In this case, the underlying mechanism and individual effect of these treatments on NSSI prevention or intervention need to be further explored.
Additionally, several studies did not specify any underpinning theoretical models related to the NSSI problems. Although the intervention strategies have been selected from dialectical behavior therapy (DBT),52,53 cognitive behavioral therapy (CBT),55,56 emotional strategies,46 sensory integration therapy,48 as well as acceptance and commitment therapy (ACT),47 the effective combinations between intervention approaches and theoretical frameworks into practice are still missing. In other words, the blending of theories with practices as an immensely beneficial way is still lacking in the current studies. Given the complex underlying mechanism or functions of NSSI, for example, Nock believes that it can be divided into four dimensions, which indicated the necessity to design the different intervention components following these theoretical bases, as a way to promote the effectiveness of an intervention.70 In addition, Hasking and colleagues proposed the cognitive-emotional mode of NSSI, this novelty model offered an explanation of how emotion regulation and cognition can work in concert to promote NSSI,71 which paves a new way for the prevention and intervention programs of governing this problems. In this case, a current review has pointed out that, cutting down program (CDP), a project designed for young people with a self-harm history based on the foundation of CBT, was shown to be one of the most effective strategies at reducing NSSI.81 But this NSSI-specific psychotherapeutic intervention program was not used in Chinese context yet. What is the clear front-runner treatment for NSSI, and how to practice them in an effective way, remain unaddressed for future research to answer.
Interestingly, the physical treatment (e.g., low frequency repetitive transcranial magnetic stimulation) has also been observed previously as a way to manage the NSSI problems, for example, the reduction rate for NSSI was 84.6% in the rTMS combined with medication group and only 38.9% in the single medication group.49 These findings are consistent with neurobiological models implicating the ventral medial prefrontal cortex (vmPFC) systems in NSSI.82
Unfortunately, there is a paucity on a larger sample size and longer follow-up of these studies. More clinical practices are needed to further clarify the efficacy and safety of physical treatment for individuals with NSSI. Moreover, although there are three studies that tried to design personalized intervention through the management strategies,54, 55, 56 which is in line with the new wave of interventions,83 these studies still emphasized on the monitoring process and system construction. The extent to which specified intervention component works remains to be explored.
Overall quality of publish empirical studies
The overall quality is acceptable, but there is still several missing information or the limitation in the reporting methods of these published articles. Specifically, although 8 articles used RCTs,46,48,49,52,53,55, 56, 57 they did not fully comply with the reporting standards of RCTs, especially for the blinding process. In addition, three articles used CCT design,47,50,54 for example, a study recruited patients from January to June 2020 as the control group and patients from June to December 2020 as the intervention group.47 Although the significant intervention effect was found, but the lack of randomized control may lead to the insufficient empirical evidence of these studies. Furthermore, one article utilized the approach of personalized intervention.55 But the operation strategies were unclear so that far more limited the possibilities of replications and robust interpretations of which underlying mechanism is effective,84 which is one of the most longstanding concerns in the intervention field.85 This again pointed out a necessity for a precision reporting of intervention details, as to gaining scientific credibility and facilitating replications in the emerging scientific areas.
Limitation and implication for future studies
In Section 1, our work further incorporated richer and newer studies, systematically integrated the epidemiological characteristics of NSSI among students of various age groups and different genders, and strictly distinguished NSSI period (i.e., 6 m, 12 m, and lifetime) which could provide more rigorous evidence for the prevalence of NSSI among Chinese students, and provide a more comprehensive guidance for subsequent NSSI-related epidemiological surveys. Notably, the reported prevalence has varied greatly, possibly due to differences in NSSI definition, assessment criteria, sample size (ranged from 112 to 25,378), and geographical area (e.g., rural and urban, western and eastern area). Given this variation, it is difficult to fully understand the current situation with respect to NSSI in the Chinese population. At the same time, given the vast population and vast geography of China, studies from more regions are needed to provide a more comprehensive picture of NSSI epidemiological characteristics in China. More importantly, uniform evaluation criteria should also be established. Further advancement and improvement of these studies will contribute to more significant progress and development of public health in China.
Secondly, the lack of a review of NSSI methods in China means that our understanding of NSSI is incomplete, which may hinder effective prevention and intervention efforts. Practically, a deeper understanding of NSSI methods can inform the development of targeted prevention and intervention strategies that can effectively prevent and reduce NSSI. Besides, research on the most common NSSI approaches in China could not only help scholars conduct in-depth research on NSSI, but also raise vigilance and awareness of these behaviors among the general public. This is especially important for those who are exposed to a high risk of NSSI or who are engaging in NSSI behaviors. By reducing the stigma surrounding NSSI behavior and emphasizing the importance of seeking mental health care, we can better prevent and intervene in NSSI cases.
In Section 2, three main findings were identified. First, our review found that research examining the risk of NSSI in Chinese population beyond the use of correlations is still in its infancy. Although a growing number of studies have acknowledged the necessity to use longitudinal designs, as the cross-sectional design limits the possibilities to determine the direction of effect, still, the mainstream of studies (nearly 263 out of 306) in this review collected data at the same time. The underlying mechanism that contributes to the development and/or maintenance of NSSI behavior is still unclear. Where possible, longitudinal designs over the course of development will be ideal for examining how things evolve before, during, and after the onset, remission, and persistence of NSSI, identifying predictors that may guide later treatment strategies.86 Given the high rates during adolescence, these directional findings would provide more guidance for early intervention, and better avert aberrant processes while promoting the healthy development of adolescents. In recent years, the development of ecological momentary assessment may also be particularly useful to studying the mechanisms implied in this behavior. This measurement strategy brings opportunities to advance scientific understanding of the dynamic course of NSSI, the ecological validity of the framework, and capturing of risk factors for predicting NSSI behaviors under the acute risk and the functional mechanisms of NSSI.87
Secondly, only a few studies in this review examined the risk factors at the macro level, for example, the built environmental and natural environmental risk factors, which limits our understanding of behavior in a more comprehensive way, as several risk factors within ecological frameworks may be interdependent.88 Where possible, future research should also address how these factors interact with each other and contribute to these behaviors within or beyond of the existing framework. This would provide more empirical evidence and framework for governments, social agencies, practitioners, and health workers in this area.
Thirdly, with the fast-than-ever development of computer internet technology, several researchers have shifted their focus to the association between online media and NSSI behaviors.89 For example, a recent review found that spending more time on online social networking promotes more frequent self-harm behaviors among adolescents.90 In addition, the digital self-harm as a new format has been proposed in the current studies,91 which involves the individual using digital platforms to present themselves as the target of interpersonal aggression. In the future, more empirical studies will be required to test the potential underlying mechanisms.
The barriers to the implementation of NSSI prevention and intervention could be classified into three major areas, that is, study population, study methodologies, and therapeutic framework. For instance, in China, a preventive intervention program is lacking for the high prevalence rates of NSSI among teenagers, and it is not being implemented in schools or communities. Targeted, evidence-based preventive efforts are therefore urgently needed, as a most cost-effective way to prevent the risk prior to the onset of this serious public health problem.92 In addition, the majority of existing studies focused on clinical samples, while the practical approach for general population is inadequate, as this previous empirical evidence cannot be transformed and simply applied to another population with different context. The small sample size, short-term follow-up and short of randomized design are other drawbacks related to current prevention and intervention programs for NSSI among Chinese population.
In addition, four studies tried to involve the present of family members,47, 48, 54, 55 and one even further identified the higher involvement of parents (e.g., the improve of family closeness) may also intrigue better treatment outcomes.48 This is in line with the calling of combination between individual treatment and family treatment together,93 which has been shown effectively in increasing the participants’ adherence and the maintenance of clinical gains.94
Previous studies have also showed a high co-occurrence rate between NSSI and personality disorders,95 since NSSI has been historically intertwined with borderline personality disorders as one of its prototypical symptoms.96 However, the treatment for this complex condition should receive special attention rather than simply using existing interventions for NSSI. This might be a way to getting “clean”, in other words, this is a more effective way to prevent the high prevalence of repetitive or recurrent NSSI nowadays.97
As aforementioned, several studies have attempted to design personalized interventions and provide timely healthcare to individuals with different needs. For example, Huang and colleagues explored the effect of Colaizzi analysis (e.g., seven steps strategies to generate individual's core thoughts and relevant suggestions are put forward according to the mechanism of the problem to achieve targeted changes in the treatment) with the combination of CBT for adolescents with NSSI, and found a significant effect in decreasing the incidence of NSSI.55 These exploratory studies are consistent with the calling for personalized and process-based intervention for youth mental health in the recent years,70,83,98 that is, how can we understand the needs of the individual more effectively, as a way to produce better intervention outcomes. However, the effective measurement and intervention evaluation for this field need to be expanded. As general issues across the field, the overcoming of these questions may largely promote the progress in this new area.
Besides, it should be noted that certain intervention studies possessing distinct Chinese characteristics, such as the utilization of traditional Chinese medicine to treat NSSI, were not incorporated into this review due to the dearth of quantifiable outcomes. Such an omission underscores the necessity for future studies to enhance the rigor of efficacy verification. Moreover, it also highlights the prospect of identifying alternative intervention programs in this realm, further emphasizing the continual evolution of research in this field.
Conclusion
This current study addressed trends and potential directions in future studies of non-suicidal self-injury (NSSI), including a deeper understanding of Chinese-specific NSSI methods, functions and different levels of risk factors for NSSI from biological to natural environmental levels. By gaining familiarity with this existing phenomenon, researchers can acquire new insights into it. In the third section, we would like to further emphasize the urgent need and the importance to address the lack of NSSI prevention and intervention programs in China. It is important to develop more culture-specific prevention and intervention programs that address the China-specific community and built environmental contexts. For example, future NSSI prevention and intervention programs should address the needs of individuals who are left-behind children or internal rural-to-urban immigrants.
With such efforts, we anticipate that researchers can better understand the mechanisms that induce NSSI and provide empirical evidence for policymakers. We also believe that there is a great social and translational significance derived from the current research. To allay the severe public health burden induced by NSSI in Chinese society, the promotion of population well-being through different approaches targeting different levels of risk factors is a crucial task for future researchers, practitioners, and policymakers.
Contributors
DYQ: Conceptualisation, Formal analysis, Investigation, Methodology, Project administration, Visualisation, Writing–review & editing; XW: Conceptualisation, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualisation, Writing–review & editing; BWL: Conceptualisation, Investigation, Methodology, Project administration, Visualisation, Writing–review & editing; XZ: Conceptualization, Data curation, Investigation, Methodology, Project administration, Validation, Writing–review & editing; YHH:Investigation, Methodology, Investigation, Validation, Visualisation; DYC: Investigation, Methodology, Project administration, Validation, Visualization; XED: Formal analysis, Investigation, Methodology; JAY: Methodology, Validation; DYL: Conceptualisation, Visualisation, Writing–review & editing; XQZ: Methodology, Resources, Data interpretation, Project administration; JJO: Methodology, Data interpretation; JSZ: Data interpretation, Clinical suggestions, Writing–review & editing; ZXC: Methodology, Resources; JA: Methodology, Data interpretation, Writing–review & editing; YYW: Methodology, Data interpretation, Project administration, Writing–review & editing; XYZ: Data interpretation, Writing–review & editing; TFY: Data interpretation, Resources, Writing–review & editing; JT: Methodology, Data interpretation, Writing–review & editing; Supervision; WHY: Conceptualisation, Methodology, Resources, Writing–review & editing; Supervision; RSC: Conceptualisation, Data curation, Investigation, Methodology, Project administration, Resources, Funding, Supervision, Writing–review & editing.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
There are no conflicts of interests associated with this paper.
Acknowledgements
Funding: This review was supported by Humanity and Social Science Youth foundation of Ministry of Education (22YJCZH018), Science and Technology Innovation 2030 (STI2030-Major Projects: 2021ZD0200702), National Natural Science Foundation of China (81825009), and Shuimu Tsinghua Scholar. No funding agencies were involved in the data collection, data analysis, and writing of this paper.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100794.
Contributor Information
Weihua Yue, Email: dryue@bjmu.edu.cn.
Runsen Chen, Email: runsenchen@tsinghua.edu.cn.
Appendix A. Supplementary data
References
- 1.Cipriano A., Cella S., Cotrufo P. Nonsuicidal self-injury: a systematic review. Front Psychol. 2017;8:1946. doi: 10.3389/fpsyg.2017.01946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klonsky E.D., Victor S.E., Saffer B.Y. Nonsuicidal self-injury: what we know, and what we need to know. Can J Psychiatry. 2014;59(11):565–568. doi: 10.1177/070674371405901101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baer M.M., Tull M.T., Forbes C.N., Richmond J.R., Gratz K.L. Methods matter: nonsuicidal self-injury in the form of cutting is uniquely associated with suicide attempt severity in patients with substance use disorders. Suicide Life Threat Behav. 2020;50(2):397–407. doi: 10.1111/sltb.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim K.S., Wong C.H., McIntyre R.S., et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. 2019;16(22):4581. doi: 10.3390/ijerph16224581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swannell S.V., Martin G.E., Page A., Hasking P., St John N.J. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44(3):273–303. doi: 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- 6.Glenn C.R., Klonsky E.D. Nonsuicidal self-injury disorder: an empirical investigation in adolescent psychiatric patients. J Clin Child Adolesc Psychol. 2013;42(4):496–507. doi: 10.1080/15374416.2013.794699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poudel A., Lamichhane A., Magar K.R., Khanal G.P. Non suicidal self injury and suicidal behavior among adolescents: co-occurrence and associated risk factors. BMC Psychiatry. 2022;22(1):96. doi: 10.1186/s12888-022-03763-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mars B., Heron J., Klonsky E.D., et al. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry. 2019;6(4):327. doi: 10.1016/S2215-0366(19)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Westers N.J., Culyba A.J. Nonsuicidal self-injury: a neglected public health problem among adolescents. Am J Public Health. 2018;108(8):981–983. doi: 10.2105/AJPH.2018.304550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mannekote Thippaiah S., Shankarapura Nanjappa M., Gude J.G., et al. Non-suicidal self-injury in developing countries: a review. Int J Soc Psychiatry. 2021;67(5):472–482. doi: 10.1177/0020764020943627. [DOI] [PubMed] [Google Scholar]
- 11.Trueba H.T., Jacobs L., Kirton E. Routledge; 2014. Cultural conflict & adaptation; p. 184. [Google Scholar]
- 12.Wang Q., Zhang Y., Liu X. Perceived discrimination, loneliness, and non-suicidal self-injury in Chinese migrant children: the moderating roles of parent-child cohesion and gender. J Soc Pers Relatsh. 2021;38(3):825–847. [Google Scholar]
- 13.Sun X., Tian Y., Zhang Y., Xie X., Heath M.A., Zhou Z. Psychological development and educational problems of left-behind children in rural China. Sch Psychol Int. 2015;36(3):227–252. [Google Scholar]
- 14.Stineman M.G., Streim J.E. The biopsycho-ecological paradigm: a foundational theory for medicine. PM R. 2010;2(11):1035–1045. doi: 10.1016/j.pmrj.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner B.J., Austin S.B., Chapman A.L. Treating nonsuicidal self-injury: a systematic review of psychological and pharmacological interventions. Can J Psychiatry. 2014;59(11):576–585. doi: 10.1177/070674371405901103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong R., Hall B.J., Doyle J., Waters E. ‘Scoping the scope’of a cochrane review. J Public Health. 2011;33(1):147–150. doi: 10.1093/pubmed/fdr015. [DOI] [PubMed] [Google Scholar]
- 17.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 19.Tufanaru C., Munn Z., Aromataris E., Campbell J., Hopp L. Joanna Briggs Institute reviewer's manual. The Joanna Briggs Institute Adelaide; Australia: 2017. Systematic reviews of effectiveness; pp. 3–10. [Google Scholar]
- 20.Xu L., Sun H., Xu H., et al. Self-neglect among older adults admitted to a Chinese comprehensive hospital in the COVID-19 pandemic era: a cross-sectional study. J Elder Abuse Negl. 2022;34(4):241–258. doi: 10.1080/08946566.2022.2095319. [DOI] [PubMed] [Google Scholar]
- 21.Yu M., Gu L., Jiao W., Xia H., Wang W. Predictors of self-neglect among community-dwelling older adults living alone in China. Geriatr Nurs. 2019;40(5):457–462. doi: 10.1016/j.gerinurse.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Ying J., Liu S., Chen D., Xu Z., Gao Q., You J. Gender differences in the relationship between maladaptive perfectionism, negative body image, anxiety, and nonsuicidal self-injury in Chinese lesbian, gay, and bisexual populations. Sex Res Soc Policy. 2022;19(4):2024–2036. [Google Scholar]
- 23.Guo J., Ying J., Zhou X., Wang C., Lin N., You J. Double hurt: the impact of interpersonal-level stigma on nonsuicidal self-injury among lesbian, gay, and bisexual individuals. Curr Psychol. 2022:1–14. [Google Scholar]
- 24.Chen D., Ying J., Zhou X., Wu H., Shen Y., You J. Sexual minority stigma and nonsuicidal self-injury among sexual minorities: the mediating roles of sexual orientation concealment, self-criticism, and depression. Sex Res Soc Policy. 2022;19(4):1690–1701. doi: 10.1007/s13178-022-00745-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang F., Lu J., Lin L., Cai J., Xu J., Zhou X. Impact of parental divorce versus separation due to migration on mental health and self-injury of Chinese children: a cross sectional survey. Child Adolesc Psychiatry Ment Health. 2021;15(1):1–11. doi: 10.1186/s13034-021-00424-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Q., Xiong Y., Liu X. Family unity or money? The roles of parent-child cohesion and socioeconomic status in the relationship between stressful life events and nonsuicidal self-injury among Chinese left-behind children. Suicide Life Threat Behav. 2020;50(5):963–974. doi: 10.1111/sltb.12650. [DOI] [PubMed] [Google Scholar]
- 27.Wang Y., Zhang M., Chen H. Self-injury among left-behind adolescents in rural China: the role of parental migration and parent-child attachment. Front Psychol. 2019;9:2672. doi: 10.3389/fpsyg.2018.02672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma Y., Guo H., Guo S., et al. Association of the labor migration of parents with nonsuicidal self-injury and suicidality among their offspring in China. JAMA Netw Open. 2021;4(11) doi: 10.1001/jamanetworkopen.2021.33596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shao Y.P., Guo A.G. Self-harm behaviors among deaf and mute middle school students. (in Chinese) Chin J Sch Health. 2016;3(37):451–452. [Google Scholar]
- 30.Gao Q., Xiang H., Xiang Y.T., Zhu H. Deliberate self-harm among children with disabilities in China: a matched case-control study. Pediatr Res. 2019;85(3):275–282. doi: 10.1038/s41390-018-0258-7. [DOI] [PubMed] [Google Scholar]
- 31.Zhu H., Abudusaimaiti X., Xiang J., Gao Q. Deliberate self-harm among Chinese children with different types and severity of disabilities. Int J Env Res Public Health. 2019;16(17):3149. doi: 10.3390/ijerph16173149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang Q., Qi N., Wang Y.T., Li J., Huang H.F., Xu T.Z. The impact of school bullying on non-suicidal self-injury behaviors among adolescents with depression (in Chinese) J Psychiatry. 2022;35(2):176–180. [Google Scholar]
- 33.Xu M.R., Liu S.M., Chen J., et al. Relationships among life events, emotional symptoms and non-suicidal self-injury behaviors in adolescents with depression. J Psychiatry. 2020;33(6):420–423. [Google Scholar]
- 34.Wang Y.X., Lai J.B., Hu C.C., Meng H.B., Hu S.H., Lyu D. Non-suicidal self-harm is linked to suicidal thoughts in Chinese adolescents with mood disorders: a cross-sectional report. J Zhejiang Univ Sci B. 2021;22(3):233–240. doi: 10.1631/jzus.B2000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng Y.G., Xiao L., Wang H.L., Chen Z.H., Wang G.H. A retrospective research on non-suicidal self-injurious behaviors among young patients diagnosed with mood disorders. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.895892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang L., Liu J., Yang Y., Zou H. Prevalence and risk factors for non-suicidal self-injury among patients with depression or bipolar disorder in China. BMC Psychiatry. 2021;21(1):1–12. doi: 10.1186/s12888-021-03392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shi K.T., Wei X.L., Gao qi, Liu T.S. The relationship between non-suicidal self-injury and childhood maltreatment in soldiers. Acad J Chin PLA Med Sch. 2022;9(43):982–987. [Google Scholar]
- 38.Zhong B.L., Xu Y.M., Xie W.X., Chen W.C., Lu J. Prevalence of deliberate self-harm among Chinese patients with heroin dependence: a meta-analysis. Front Psychiatry. 2018;9:325. doi: 10.3389/fpsyt.2018.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhong B.L., Xu Y.M., Zhu J.H., Liu X.J. Non-suicidal self-injury in Chinese heroin-dependent patients receiving methadone maintenance treatment: prevalence and associated factors. Drug Alcohol Depend. 2018;189:161–165. doi: 10.1016/j.drugalcdep.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Gu H., Lu Y., Cheng Y. Negative life events and nonsuicidal self-injury in prisoners: the mediating role of hopelessness and moderating role of belief in a just world. J Clin Psychol. 2021;77(1):145–155. doi: 10.1002/jclp.23015. [DOI] [PubMed] [Google Scholar]
- 41.Li G.H., Zhou Y.J., Huang W., et al. Gender differences in non-suicidal self-injury behavior among adolescents with mood disorder. Chin Prev Med. 2021;9(22):699–703. [Google Scholar]
- 42.Meng L., Qu D., Bu H., et al. The psychosocial correlates of non-suicidal self-injury within a sample of adolescents with mood disorder. Front Public Health. 2022;10:78. doi: 10.3389/fpubh.2022.768400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maier K.J., al'Absi M. Toward a biopsychosocial ecology of the human microbiome, brain-gut axis, and health. Psychosom Med. 2017;79(8):947. doi: 10.1097/PSY.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 44.Hooley J.M., Franklin J.C. Why do people hurt themselves? A new conceptual model of nonsuicidal self-injury. Clin Psychol Sci. 2018;6(3):428–451. [Google Scholar]
- 45.Gallant J., Snyder G.S., von der Embse N.P. Characteristics and psychosocial predictors of adolescent nonsuicidal self-injury in residential care. Prev Sch Fail Altern Educ Child Youth. 2014;58(1):26–31. [Google Scholar]
- 46.Ding H., Yang F., He X. Effect of emotional regulation strategy on non-suicidal self-injury behavior of adolescents with depressive disorder. J Nurs Sci. 2021;8(36):62–65. [Google Scholar]
- 47.Xue Y., Zhou X., Fan Z., Wu Q., Liu H. Application of family participatory acceptance and commitment therapy in the adolescent patients with non-suicidal self-injury. Chongqing Med. 2022;51(7):1131–1134. [Google Scholar]
- 48.Quan L., Zhao Y., Ying D. Clinical effect of sensory integration therapy on adolescent depression. Chin J Rehabiliation Med. 2020;5(35):551–555+612. [Google Scholar]
- 49.Yu H., Long S., Zhou Y. A clinical study of low frequency rTMS stimulation in the right ventromedial prefrontal cortex (VMPFC) combined with Sertraline on the treatment of the adolescents with nonsuicidal self-injurious behaviors. J Int Psychol. 2021;48(6):987–990,993. [Google Scholar]
- 50.Zeng J., Zhou X. Effect of modified electroconvulsive therapy on self injury behavior in patients with depression. J Clin Psychiatry. 2022;32(2):141–143. [Google Scholar]
- 51.Chen C., Li X., Deng Y. Effect of emotional distress monitoring and intervention in preventing non-suicidal self-injury (NSSI) of college students. Health Behav Policy Rev. 2022;9(3):846–852. [Google Scholar]
- 52.Lin X., Li K. Analysis on the efficacy of dialectical behavior therapy combined with sertraline drug therapy on adolescent depression with non-suicidal self-harm. Anal Effic Dialect Behav. 2021;48(3):439–442,465. [Google Scholar]
- 53.Su X., He J., Zhang X., Zhang L., Men J. Application of dialectical behavior therapy in adolescents with non-suicidal self-injury. Chin Nurs Res. 2022;21(36):3922–3925. [Google Scholar]
- 54.Zhang R., Wang Y. Nursing management of non-suicidal self-injury in inpatients with borderline personality disorder based on hazard analysis critical control point. J Nursingchina. 2022;22(29):20–25. [Google Scholar]
- 55.Huang J., Cheng X., Zhu X., Li X. Colaizzi analysis combined with cognitive -behavior therapy for adolescent non -suicidal self -injury and its effect on Barratt score and MOAS. J Pract Med. 2022;38(3):360–365. [Google Scholar]
- 56.Lu H., Liu Y., Huang Z., et al. Development and application effect of knowledge-to-action framework-based health management in adolescents with depressive disorder in remote counties. Chin Gen Pract. 2022;11(25):1373–1377+1382. [Google Scholar]
- 57.Zhang Y., Huang K., Cong H., Wang M. Effects of group psychological counseling on nonsuicidal self-injury (NSSI) behaviors of college students with depression. Psychiatr Danub. 2022;34(2):229–235. doi: 10.24869/psyd.2022.229. [DOI] [PubMed] [Google Scholar]
- 58.Lang J., Yao Y. Prevalence of nonsuicidal self-injury in Chinese middle school and high school students: a meta-analysis. Med Baltim. 2018;97(42) doi: 10.1097/MD.0000000000012916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang X., Feldman M.W. A reversed gender pattern? A meta-analysis of gender differences in the prevalence of non-suicidal self-injurious behaviour among Chinese adolescents. BMC Public Health. 2017;18(1):66. doi: 10.1186/s12889-017-4614-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Han A.Z., Xu G., Su P.Y. A Meta-analysis of characteristics of non-suicidal self-injury among middle school students in mainland China. Chin J Sch Health. 2017;38(11):1665–1670. [Google Scholar]
- 61.Pan Z., Mao S.J., Tang H.M., et al. Meta-analysis on non-suicidal self-injury among college students in China. Chin J Sch Health. 2016;6(37):878–881. [Google Scholar]
- 62.Shang C.N., Wang J.Y., Song T., Zhang J.L., Zhang D.H. The psychological experience of adolescent patients with mood disorder accompanied by non-suicidal self-injury: a qualitative study. Chin J Nurs. 2022;7(57):827–834. [Google Scholar]
- 63.Duan S., Wang H., Wilson A., et al. Developing a text messaging intervention to reduce deliberate self-harm in Chinese adolescents: qualitative study. JMIR Mhealth Uhealth. 2020;8(6) doi: 10.2196/16963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fu X., Yang J., Liao X., et al. Parents' attitudes toward and experience of non-suicidal self-injury in adolescents: a qualitative study. Front Psychiatry. 2020;11:651. doi: 10.3389/fpsyt.2020.00651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen R., Wang Y., Liu L., et al. A qualitative study of how self-harm starts and continues among Chinese adolescents. BJPsych Open. 2020;7(1) doi: 10.1192/bjo.2020.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maciejewski D.F., Renteria M.E., Abdellaoui A., et al. The association of genetic predisposition to depressive symptoms with non-suicidal and suicidal self-injuries. Behav Genet. 2017;47(1):3–10. doi: 10.1007/s10519-016-9809-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kaess M., Hooley J.M., Klimes-Dougan B., et al. Advancing a temporal framework for understanding the biology of nonsuicidal self- injury: an expert review. Neurosci Biobehav Rev. 2021;130:228–339. doi: 10.1016/j.neubiorev.2021.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schreiner M.W., Klimes-Dougan B., Begnel E.D., Cullen K.R. Conceptualizing the neurobiology of non-suicidal self-injury from the perspective of the research domain criteria project. Neurosci Biobehav Rev. 2015;57:381–931. doi: 10.1016/j.neubiorev.2015.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang Y.J., Li X., Ng C.H., Xu D.W., Hu S., Yuan T.F. Risk factors for non-suicidal self-injury (NSSI) in adolescents: a meta-analysis. eClinicalMedicine. 2022;46 doi: 10.1016/j.eclinm.2022.101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bentley K.H., Nock M.K., Barlow D.H. The four-function model of nonsuicidal self-injury: key directions for future research. Clin Psychol Sci. 2014;2(5):638–656. [Google Scholar]
- 71.Hasking P., Whitlock J., Voon D., Rose A. A cognitive-emotional model of NSSI: using emotion regulation and cognitive processes to explain why people self-injure. Cogn Emot. 2017;31(8):1543–1556. doi: 10.1080/02699931.2016.1241219. [DOI] [PubMed] [Google Scholar]
- 72.Martin J., Bureau J.F., Yurkowski K., Fournier T.R., Lafontaine M.F., Cloutier P. Family-based risk factors for non-suicidal self-injury: considering influences of maltreatment, adverse family-life experiences, and parent–child relational risk. J Adolesc. 2016;49:170–180. doi: 10.1016/j.adolescence.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 73.Waals L., Baetens I., Rober P., et al. The NSSI family distress cascade theory. Child Adolesc Psychiatry Ment Health. 2018;12(1):52. doi: 10.1186/s13034-018-0259-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gatta M., Miscioscia M., Sisti M., Comis I., Battistella P.A. Interactive family dynamics and Non-Suicidal Self-Injury in psychiatric adolescent patients: a single case study. Front Psychol. 2017;8:46. doi: 10.3389/fpsyg.2017.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wan Y.H., Hu C.L., Hao J.H., Sun Y., Tao F.B. Deliberate self-harm behaviors in Chinese adolescents and young adults. Eur Child Adolesc Psychiatry. 2011;20(10):517–525. doi: 10.1007/s00787-011-0213-1. [DOI] [PubMed] [Google Scholar]
- 76.Haney A.M. Nonsuicidal self-injury and religiosity: a meta-analytic investigation. Am J Orthopsychiatry. 2020;90:78–89. doi: 10.1037/ort0000395. [DOI] [PubMed] [Google Scholar]
- 77.Slavich G.M. Social safety theory: a biologically based evolutionary perspective on life stress, health, and behavior. Annu Rev Clin Psychol. 2020;16(1):265–295. doi: 10.1146/annurev-clinpsy-032816-045159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ma Y., Yang Y., Jiao H. Exploring the impact of urban built environment on public emotions based on social media data: a case study of wuhan. Land. 2021;10(9):986. [Google Scholar]
- 79.Landrigan P.J. Air pollution and health. Lancet Public Health. 2017;2(1):e4–e5. doi: 10.1016/S2468-2667(16)30023-8. [DOI] [PubMed] [Google Scholar]
- 80.Zhang W., Hu D., Ding X., et al. Nursing of adolescents with non-suicidal self-injury: a review. J Nurs Sci. 2022;7(37):109–1013. [Google Scholar]
- 81.Calvo N., García-González S., Perez-Galbarro C., et al. Psychotherapeutic interventions specifically developed for NSSI in adolescence: a systematic review. Eur Neuropsychopharmacol. 2022;58:86–98. doi: 10.1016/j.euroneuro.2022.02.009. [DOI] [PubMed] [Google Scholar]
- 82.Case J.A.C., Mattoni M., Olino T.M. Examining the neurobiology of non-suicidal self-injury in children and adolescents: the role of reward responsivity. J Clin Med. 2021;10(16):3561. doi: 10.3390/jcm10163561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hayes S.C., Ciarrochi J., Hofmann S.G., Chin F., Sahdra B. Evolving an idionomic approach to processes of change: towards a unified personalized science of human improvement. Behav Res Ther. 2022;156 doi: 10.1016/j.brat.2022.104155. [DOI] [PubMed] [Google Scholar]
- 84.Van Agteren J., Iasiello M., Ali K., et al. Using the intervention mapping approach to develop a mental health intervention: a case study on improving the reporting standards for developing psychological interventions. Front Psychol. 2021;12:3773. doi: 10.3389/fpsyg.2021.648678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hillary F.G., Medaglia J.D. What the replication crisis means for intervention science. Int J Psychophysiol. 2020;154:3–5. doi: 10.1016/j.ijpsycho.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rodríguez-Blanco L., Carballo J.J., Baca-García E. Use of ecological momentary assessment (EMA) in non-suicidal self-injury (NSSI): a systematic review. Psychiatry Res. 2018;263:212–219. doi: 10.1016/j.psychres.2018.02.051. [DOI] [PubMed] [Google Scholar]
- 87.Kiekens G., Robinson K., Tatnell R., Kirtley O.J. Opening the black box of daily life in nonsuicidal self-injury research: with great opportunity comes great responsibility. JMIR Ment Health. 2021;8(11) doi: 10.2196/30915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lan Z., Pau K., Mohd Yusof H., Huang X. Hierarchical topological model of the factors influencing adolescents' non-suicidal self-injury behavior based on the DEMATEL-TAISM method. Sci Rep. 2022;12(1) doi: 10.1038/s41598-022-21377-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lewis S.P., Heath N.L., Michal N.J., Duggan J.M. Non-suicidal self-injury, youth, and the Internet: what mental health professionals need to know. Child Adolesc Psychiatry Ment Health. 2012;6(1):13. doi: 10.1186/1753-2000-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Memon A.M., Sharma S.G., Mohite S.S., Jain S. The role of online social networking on deliberate self-harm and suicidality in adolescents: a systematized review of literature. Indian J Psychiatry. 2018;60(4):384. doi: 10.4103/psychiatry.IndianJPsychiatry_414_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Soengkoeng R., Moustafa A.A. Digital self-harm: an examination of the current literature with recommendations for future research. Discov Psychol. 2022;2(1):19. [Google Scholar]
- 92.Fazel M., Kohrt B.A. Prevention versus intervention in school mental health. Lancet Psychiatry. 2019;6(12):969–971. doi: 10.1016/S2215-0366(19)30440-7. [DOI] [PubMed] [Google Scholar]
- 93.Ma C.F., Chan S.K.W., Chien W.T., et al. Cognitive behavioural family intervention for people diagnosed with severe mental illness and their families: a systematic review and meta-analysis of randomized controlled trials. J Psychiatr Ment Health Nurs. 2020;27(2):128–139. doi: 10.1111/jpm.12567. [DOI] [PubMed] [Google Scholar]
- 94.Peris T.S., Thamrin H., Rozenman M.S. Family intervention for child and adolescent anxiety: a meta-analytic review of therapy targets, techniques, and outcomes. J Affect Disord. 2021;286:282–295. doi: 10.1016/j.jad.2021.02.053. [DOI] [PubMed] [Google Scholar]
- 95.Buelens T., Costantini G., Luyckx K., Claes L. Comorbidity between non-suicidal self-injury disorder and borderline personality disorder in adolescents: a graphical network approach. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.580922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stead V.E., Boylan K., Schmidt L.A. Longitudinal associations between non-suicidal self-injury and borderline personality disorder in adolescents: a literature review. Borderline Personal Disord Emot Dysregul. 2019;6(1):3. doi: 10.1186/s40479-019-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Himelein-Wachowiak M., Giorgi S., Kwarteng A., et al. Getting “clean” from nonsuicidal self-injury: experiences of addiction on the subreddit r/selfharm. J Behav Addict. 2022;11(1):128–139. doi: 10.1556/2006.2022.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ng M.Y., Weisz J.R. Building a science of personalized intervention for youth mental health. J Child Psychol Psychiatry. 2016;57(3):216–236. doi: 10.1111/jcpp.12470. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.