Summary
Background
Childhood cancers are emerging as an essential concern in India where there is lack of a specific programme component or policy to address childhood cancer control. There is limited information on the status and quality of childhood cancer care services in India. This paper describes the childhood cancer care services available at secondary and tertiary-level hospitals in India through a cross sectional study design.
Methods
The survey was conducted in 137 tertiary-level and 92 secondary-level hospitals in 26 states and 4 Union Territories (UTs), ensuring a uniform representation of public and private care hospitals. The study tool collected data on the organisational infrastructure, type of oncology services, health workforce, equipment, treatment and referral protocols, and treatment guidelines. Descriptive statistics was used to primarily present the health service status and data on childhood cancer care services in proportions and mean.
Findings
A dedicated pediatric oncology department was available in 41.6% of the public, 48.6% of private, and 64% Non Government Organization (NGO) managed tertiary-level hospitals. In 36 (39%) of the 92 hospitals providing secondary care, childhood cancer care was provided. The availability of bone (41.5%) and positron emission tomography (PET) scans (25.9%) was lower in public tertiary hospitals, whereas histopathology, computerised tomography (CT scan), and magnetic resonance imaging (MRI) were lower in public secondary hospitals than private and NGO managed hospitals for the corresponding level of care. Most tertiary hospitals had the required supportive care facilities except for play therapy and hospice care. Less than 50% of the public tertiary hospitals had stocks of the four categories of cancer-treating drugs and essential infrastructure for radiotherapy and chemotherapy. Most secondary-level hospitals not treating childhood cancer had referral linkages with tertiary hospitals.
Interpretation
The situational analysis of childhood cancer care services in India showed the concentration of availability of childhood cancer care services at the tertiary level of health care. There were gaps in the availability of specialised pediatric oncology care in all the tertiary hospitals. The availability of childhood cancer care services was higher in private and NGO-managed hospitals than in public hospitals. Integration of childhood cancer as a part of the national cancer control response should be taken up as a matter of priority. The need of the hour is to formulate a childhood cancer policy that will enable timely access to care universally.
Funding
World Health Organization, India provided funding and technical support.
Keywords: Childhood cancer, Care, Health services, India
Research in context.
Evidence before this study
The first paediatric oncology unit in India was started as early as the 1960s and the number of such units has been increasing since the 1980s. A national survey of childhood cancer services conducted in 1988 observed that paediatric oncology cases were handled by adult oncologists in 50% of the surveyed centres. Most paediatric cancer care centres in India are urban-centric, leading to delayed access by the rural population. It is seen that children with cancer often present with an advanced-stage disease which worsens the outcome. We did a MEDLINE search for studies on the status of childhood cancer care services in India using the search terms “childhood” OR “children” AND “cancer” AND “care service” OR “health service” AND “situation” OR “situational analysis” OR “status” AND “India”. Most studies had been done in selected geographic settings and did not provide a comprehensive country presentation. Thus there is a limited information on the status and quality of childhood cancer care services in India.
Added value of this study
The situational analysis of childhood cancer care services in India was done in vast majority of states and Union Territories, covering a wide representative network of hospitals providing tertiary and secondary level of care. The study has generated evidence on the availability of childhood cancer related diagnostic, treatment and supportive care facilities, health workforce, referral pathways, physical infrastructure and drug availability.
Implications of all the available evidence
Developing evidence-based policies for childhood cancer requires a situational analysis of childhood cancer services in the country. Such interventions will enable high-quality care within limited health care resources, culminating in improved survival and quality of life of pediatric cancer patients in India.
Introduction
Childhood cancers rank ninth as a leading cause of childhood diseases globally, accounting for 11.5 million (10.6–12.3 95% CI) of the Disability Adjusted Life Years (DALYs').1 As many as 80% of children at risk of childhood cancer reside in low and middle-income countries (LMICs).2
In 2017, childhood cancer ranked fifth as a leading cause of death among children between five and 14 years.3 In high-income countries, while the five-year survival rate for childhood cancer exceeds 80%, such outcomes are not seen in the LMICs.4,5 The low survival rate is mainly attributed to weak health systems in LMICs'. Childhood treatment services are primarily available at tertiary care facilities and display an urban skewing regarding availability and ease of accessibility. Access to childhood cancer care is characterised by weak infrastructure, lack of supportive care and poorly defined care pathways. Many children present with advanced disease at the time of presentation.6,7
According to a recent National Cancer Registry Programme (NCRP) report in India, childhood cancers in the 0–14 age group accounted for 4.0% of all cancers.8 The Population Based Cancer Registry in Delhi reported the highest age-adjusted incidence rate (AAR) of 203.1 per million in boys and 125.4 per million in girls.9,10 Cancers of the eye and lymphoid leukaemia contributed to the highest disability-adjusted life years (DALYs) in 2016 among children in the 0–14 age group.11
The Ministry of Health and Family Welfare, Government of India, has been striving to achieve cancer control by implementing the National Programme for Prevention and Control of Non Communicable Diseases (NP-NCD). However, the country does not have a specific programme component or policy to address childhood cancer. There is limited information on the status, distribution, and quality of childhood cancer care services in India. Most studies have been done in selected geographic settings and do not provide a comprehensive country presentation.12, 13, 14 Developing a programme component or policy for childhood cancers requires a situational analysis of childhood cancer services. This paper describes the cross sectional survey results on the status of childhood cancer care services available at secondary and tertiary-level hospitals in India.
Methods
Study setting
The survey was conducted in hospitals providing tertiary and secondary level of care in 26 states and 4 Union Territories (UTs). ICMR-NCDIR (National Centre for Disease Informatics and Research) played the role of a central coordinating unit through survey tool development, technical support, supervision, monitoring, feedback and data management. The study was conducted between July and October 2021.
A nodal childhood cancer treating hospital, preferably within the operational network of Hospital Based Cancer Registries (HBCRs') under the National Cancer Registry Programme (NCRP), managed by the ICMR- NCDIR in each state or Union Territory, was identified as the ‘hub centre’ to coordinate the survey in the state. The nodal hospital was asked to identify a representative network or the ‘spoke centres’ consisting of three to five cancer-treating hospitals (tertiary level) and two to three district/sub-district hospitals (secondary level), which were purposively selected. The ‘hub centres’ monitored and coordinated data collection from these hospitals and verified the data that was so collected. Besides, data was also collected from the hub centres themselves. Hospitals at the tertiary level comprised those at the third tier of the health system where specialised treatment and care were provided, usually based on a referral. Secondary-level hospitals were those at the second tier of the health system, which attended to patients referred from health centres at the primary level or back referrals from tertiary hospitals. Attempts were made to give uniform representation to the public (government owned and funded), private (owned by private players; largely for profit), and NGO (non-profit, funded through charitable organisations) managed hospitals. The tertiary hospitals included (a) Public: Regional Cancer Centres (RCC), Tertiary Cancer Care Centres TCCCs', State Cancer Institutes (SCI), medical colleges and super speciality hospitals (b) Private/NGO managed: super speciality and private medical colleges. The secondary level hospitals comprised (a) Public: District hospitals (without a medical college)/Sub-district hospitals (b) Private: Multispeciality hospitals (without a specialised cancer department).
Study tool
The study tool was adapted from the WHO Service Availability and Readiness Assessment (SARA), a health facility assessment tool designed to assess and monitor service availability and the WHO list of priority medical devices for cancer management, and the Indian Public Health Standards.15, 16, 17 The tool collected data on the organisational infrastructure, type of oncology services, health workforce, availability of diagnostic facilities and medicines at tertiary and secondary level hospitals. The availability of childhood cancer-treating medicines was categorised as (i) available, (ii) usually available but out of stock at the time of the study (iii) not available. Further data on physical infrastructure, pediatric oncology training and the impact of COVID-19 on childhood cancer care at tertiary hospitals were recorded. The questionnaire was administered through an online portal. The nodal hospitals that consented to participate in the survey were provided with secure login credentials to access the portal and enter relevant data in the questionnaires for the participating hospitals in the respective state/UT.
Data management and analysis
The collected data was scrutinised for irrational entries, anomalous and missing values. Data quality checklists were sent to the nodal hospitals for feedback and rectification. Data analysis was done using Microsoft Excel. Descriptive statistics was used primarily to present the data on childhood cancer care services in terms of proportions and mean. Responses to open-ended questions were analysed and presented as proportions.
Ethics approval
The study was approved by the Institutional Ethics Committee of the ICMR-NCDIR [NCDIR/IEC/3041/2021].
Role of the funding source
World Health Organization, India, provided funding and technical support for the study. They had no role in the conceptualisation and drafting of this manuscript.
Results
A total of 137 tertiary level hospitals and 101 secondary level hospitals had been approached for their participation, out of which all 137 (100%) tertiary level hospitals and 92 (91%) secondary level hospitals consented to participate. Supplementary Figure S1 shows the distribution of participating hospitals in the 26 states and 4 Union Territories. Among these-56.2% were government-run and 51.1% were medical college-associated hospitals. The categorisation of hospitals according to the primary ownership is presented in Table 1.
Table 1.
Categorisation of hospitals according to the major source of financial support.
| Type of hospital | Public |
Private |
NGO-managed |
N | % | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Tertiary level hospitals | ||||||||
| Medical college hospital | 53 | 68.8 | 11 | 31.4 | 6 | 24.0 | 70 | 51.1 |
| Super speciality (oncology) | 12 | 15.5 | 8 | 22.8 | 12 | 48.0 | 32 | 23.4 |
| Multispecialty with dedicated oncology unit | 12 | 15.5 | 16 | 45.7 | 7 | 28.0 | 35 | 25.5 |
| Total number of tertiary hospitals | 77 | 56.2 | 35 | 25.5 | 25 | 18.2 | 137 | 100 |
| Secondary level hospitals | 64 | 69.5 | 23 | 25.0 | 5 | 5.4 | 92 | 100 |
Childhood cancer management
Tertiary hospitals
A dedicated pediatric oncology department was available in 41.6% of the public, 48.6% of private, and 64% NGO managed tertiary level hospitals, as shown in Table 2. A pediatric oncologist was available in 48% of the public, 54.3% of private and 64% of the NGO-managed hospitals. A higher proportion of public tertiary hospitals provided childhood cancer treatment through general pediatric medicine (77.9%), pediatric surgery (62.3%), internal medicine (61%) and surgical departments (71.4%). Nurses trained in pediatric oncology were available in 41.5% of the public, 48.6% of private, and 72% of NGO-managed hospitals. Most tertiary hospitals had a blood bank, facilities for nutritional rehabilitation, physiotherapy, psychological counselling, dental care, immunisation, growth and development and parental education. However, less than a third of these hospitals provided play therapy and hospice care (Table 2).
Table 2.
Availability of childhood cancer treatment-related departments at tertiary hospitals.
| S. No. | Public |
Private |
NGO/charitable |
||||
|---|---|---|---|---|---|---|---|
| n = 77 |
n = 35 |
n = 25 |
|||||
| n | % | n | % | n | % | ||
| Cancer treatment departments | |||||||
| 1 | Pediatric Oncology | 32 | 41.6 | 17 | 48.6 | 16 | 64.0 |
| 2 | Medical Oncology | 35 | 45.5 | 22 | 62.9 | 15 | 60.0 |
| 3 | Radiation Oncology | 52 | 67.5 | 24 | 68.6 | 17 | 68.0 |
| 4 | Surgical Oncology | 41 | 53.2 | 24 | 68.6 | 17 | 68.0 |
| 5 | Pediatric medicine | 60 | 77.9 | 24 | 68.6 | 16 | 64.0 |
| 6 | Medicine | 47 | 61.0 | 20 | 57.1 | 11 | 44.0 |
| 7 | Haematology | 33 | 42.9 | 20 | 57.1 | 13 | 52.0 |
| 8 | Pediatric surgery | 48 | 62.3 | 20 | 57.1 | 11 | 44.0 |
| 9 | Surgery | 55 | 71.4 | 19 | 54.3 | 11 | 44.0 |
| 10 | Ophthalmology | 50 | 64.9 | 21 | 60.0 | 9 | 36.0 |
| 11 | Musculoskeletal oncology | 7 | 9.1 | 7 | 20.0 | 9 | 36.0 |
| 12 | Orthopaedics | 61 | 79.2 | 23 | 65.7 | 12 | 48.0 |
| 13 | Neurosurgery | 47 | 61.0 | 23 | 65.7 | 10 | 40.0 |
| 14 | Radiology | 66 | 85.7 | 31 | 88.6 | 22 | 88.0 |
| 15 | Nuclear medicine | 27 | 35.1 | 18 | 51.4 | 11 | 44.0 |
| 16 | Pathology | 71 | 92.2 | 31 | 88.6 | 24 | 96.0 |
| 17 | Palliative medicine | 37 | 48.1 | 20 | 57.1 | 18 | 72.0 |
| Supportive care facilities | |||||||
| 1. | Blood bank | 72 | 93.5 | 30 | 85.7 | 18 | 72.0 |
| 2. | Nutritional rehabilitation | 54 | 70.1 | 32 | 91.4 | 20 | 80.0 |
| 3. | Physiotherapy | 72 | 93.5 | 34 | 97.1 | 21 | 84.0 |
| 4. | Psychological counselling | 61 | 79.2 | 27 | 77.1 | 22 | 88.0 |
| 5. | Parental education | 58 | 75.3 | 25 | 71.4 | 17 | 68.0 |
| 6. | Occupational therapy | 39 | 50.6 | 19 | 54.3 | 14 | 56.0 |
| 7. | Hospice care | 26 | 33.8 | 13 | 37.1 | 6 | 24.0 |
| 8. | Dental care | 69 | 89.6 | 32 | 91.4 | 14 | 56.0 |
| 9. | Play therapy | 29 | 37.7 | 10 | 28.6 | 7 | 28.0 |
| 10. | Growth and development | 60 | 77.9 | 29 | 82.9 | 16 | 64.0 |
| 11. | Immunisation | 66 | 85.7 | 32 | 91.4 | 16 | 64.0 |
| 12. | Fertility Preservation services | 14 | 18.2 | 11 | 31.4 | 4 | 16.0 |
| 13. | Parental groups | 29 | 37.7 | 14 | 40.0 | 14 | 56.0 |
| 14. | Accommodation/lodging for patients and caregivers | 40 | 51.9 | 15 | 42.9 | 17 | 68.0 |
| Dedicated human resourcesfor childhood cancer treatment | |||||||
| 15 | Pediatric oncologist (Pediatrician working exclusively with childhood cancer) | 37 | 48.0 | 19 | 54.3 | 16 | 64 |
| 16 | Pediatric oncosurgeon | 11 | 14.2 | 6 | 17.1 | 7 | 28.0 |
| 17 | Nurses trained in pediatric cancer | 32 | 41.5 | 17 | 48.6 | 18 | 72.0 |
| 18 | Occupational therapist | 32 | 41.5 | 17 | 48.6 | 13 | 52.0 |
| 19 | Social worker | 59 | 76.6 | 24 | 68.6 | 20 | 80.0 |
| 20 | Counsellor | 50 | 64.9 | 24 | 68.6 | 19 | 76.0 |
Over two-thirds of the government tertiary hospitals had referral linkages with lower-tier hospitals not having specialised paediatric oncology services; however, such links were seen in less than half (45.7%) of the private tertiary hospitals. More public hospitals (76.6%) adopted a multidisciplinary treatment approach compared to 35% of private hospitals.
Secondary hospitals
Childhood cancer treatment was provided in 36 (39%) of the 92 hospitals providing a secondary level of care; the proportion was higher for private hospitals (56.5%) and NGO-managed hospitals (40%) than in public hospitals (32.8%). The pediatric medicine departments managed childhood cancers at these hospitals in over 70% of these hospitals (Supplementary Figure S2). Most secondary-level hospitals had blood banks, physiotherapy, counselling and dietary services facilities. However, a lower percentage of public (33.3%) and private (16.7%) secondary hospitals had provisions for occupational therapy (Supplementary Figure S3). Among the secondary-level hospitals (56) that were not treating childhood cancers, all the NGOs managed, and 74.4% of public hospitals, compared to 60% of private hospitals, had referral linkages with tertiary hospitals (Supplementary Figure S4).
Diagnostic facilities
Tertiary hospitals
Over 90% of the tertiary hospitals had facilities for histopathology diagnosis; however, a lower proportion of public tertiary hospitals had facilities for advanced diagnostic modalities (flowcytometric Immunophenotyping-33.7%, cytogenetics-19.4%). More than 80% of the tertiary hospitals had Computed Tomography (CT) scans, Magnetic Resonance Imaging (MRI) and ultrasound scan facilities. In contrast, the availability of bone and PET scans was lower, especially in public tertiary hospitals (Supplementary Table S1).
Secondary hospitals
Most childhood cancer treating secondary-level hospitals had facilities for basic laboratory and radiologic investigations. Compared to private hospitals, histopathology, CT scan, and MRI availability was lower in public secondary-level hospitals (Supplementary Table S2).
Cancer treatment drugs
Tertiary hospitals
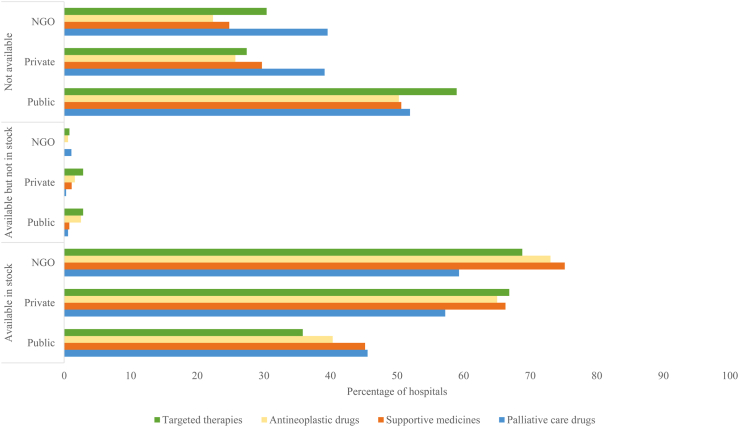
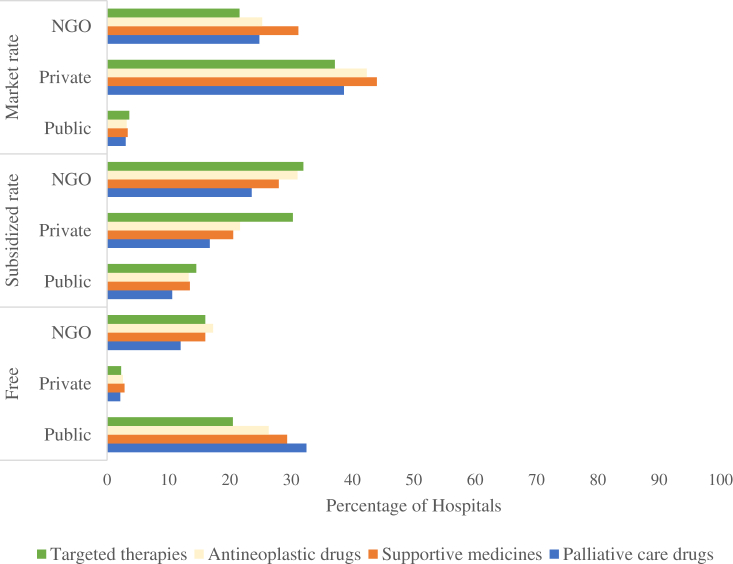
Regarding childhood cancer-treating drugs, less than 50% of the public tertiary hospitals had stocks available for the four categories of cancer-treating medications (Fig. 1), while majority of the private and NGO managed hospitals had supplies of all four drugs available. The availability of targeted therapies was the lowest (35.4% in public tertiary hospitals, compared to 66.8% in private and 68.8% in NGO managed hospitals). Free medicines were available in less than 40% of the tertiary hospitals, the lowest availability being in private hospitals (Fig. 2). In public tertiary hospitals, palliative drugs were free of cost at about one-third of the hospitals, followed by supportive medicines (29.3%), antineoplastic medicines (26.3%) and targeted therapies (20.5%).
Fig. 1.
Availability of childhood cancer treating drugs at tertiary hospitals (%).
Fig. 2.
Cost of childhood cancer treating medicines available at tertiary hospitals (%).
Secondary hospitals
Among the childhood cancer treating secondary level hospitals, the proportion of public hospitals with sufficient stock of routine chemotherapeutic and symptom-relieving medication was lower than private and NGO-managed centres (Fig. 3a). Less than half of public hospitals had adequate supplies of Dexamethasone, Vincristine, 6—Mercaptopurine, L Asparaginase, Methotrexate injection and tablet, Cytarabine and Cyclophosphamide (Fig. 3b).
Fig. 3.
a) Availability of drugs for treating childhood cancers at secondary level public hospitals (%). b) Availability of drugs for treating childhood cancers at secondary level private hospitals (%).
Physical infrastructure
Concerning the infrastructure for treating childhood cancers, less than 50% of the public tertiary hospitals had a separate room for managing children with severe neutropenia, safety measures for preparing chemotherapy drugs and daycare beds with infusion chairs (Fig. 4). The proportion of availability was higher for the private and NGO-managed hospitals.
Fig. 4.
Availability of infrastructure relevant to managing childhood cancer services at the tertiary hospitals.
Capacity building
Less than 10% of the tertiary-level hospitals had provision for training courses in pediatric oncology, as seen in Table 3. While none of the surveyed private hospitals provided D.M. pediatric oncology, a higher proportion of private hospitals had facilities for FNB in pediatric oncology and IAP PHO Fellowship (8.6% for both versus 5.2% in public tertiary hospitals).
Table 3.
Availability of pediatric oncology training courses at tertiary hospitals.
| Courses | Public (N = 77) |
Private (N = 35) |
NGO/charitable (N = 25) |
Total |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Doctorate of Medicine in Pediatric oncology | 4 | 5.2 | 0 | 0.0 | 1 | 4.0 | 5 | 3.7 |
| Fellow of National Board in Pediatric Oncology | 4 | 5.2 | 3 | 8.6 | 2 | 8.0 | 9 | 6.7 |
| Indian Academy of Pediatrics-Pediatric Hematology Oncology Fellowship | 4 | 5.2 | 3 | 8.6 | 4 | 16.0 | 11 | 8.1 |
| Fellowship in pediatric oncology (Besides FNB and IAP PHO) | 3 | 3.9 | 2 | 5.7 | 4 | 16.0 | 9 | 6.7 |
| Diploma in oncologic nursing | 6 | 7.8 | 3 | 8.6 | 3 | 12.0 | 12 | 8.9 |
| Certificate course in pediatric oncology for nurses/doctors | 4 | 5.2 | 2 | 5.7 | 2 | 8.0 | 8 | 5.9 |
| Any other | 4 | 5.2 | 4 | 11.4 | 4 | 16.0 | 12 | 8.9 |
Impact of COVID-19 on the delivery of childhood cancer treatment
COVID-19 impacted the delivery of childhood cancer care services at over half of the tertiary-level hospitals [Table 4]. There was a decrease in new paediatric cancer diagnoses, increased treatment abandonment, reduced surgical care and interruptions in radiotherapy at most hospitals. Some frequently employed approaches to address childhood cancer care included telemedicine and modifications in chemotherapy regimens.
Table 4.
Impact of COVID-19 pandemic on the delivery of childhood cancer care services at tertiary hospitals.
| S. No. | Delivery of childhood cancer care services | Public (n = 77) |
Private (n = 35) |
NGO/charitable (n = 25) |
|||
|---|---|---|---|---|---|---|---|
| n |
% |
n |
% |
n |
% |
||
| 44 | 57.1 | 18 | 51.4 | 13 | 52.0 | ||
| 1. | Complete closure of paediatric cancer care services | 3 | 6.8 | 0 | 0 | 1 | 7.6 |
| 2. | Ceased evaluating new cases of suspected cancers | 14 | 31.8 | 3 | 16.6 | 3 | 23.0 |
| 3. | Decrease in new paediatric cancer diagnoses | 31 | 70.4 | 11 | 61.1 | 10 | 76.9 |
| 4. | Increase in treatment abandonment | 32 | 72.7 | 9 | 50.0 | 9 | 69.2 |
| 5. | Reduced surgical care | 20 | 45.4 | 8 | 44.4 | 4 | 30.7 |
| 6. | Modifications in chemotherapy regimens | 25 | 56.8 | 8 | 44.4 | 9 | 69.2 |
| 7. | Interruptions in radiotherapy | 21 | 47.7 | 9 | 50.0 | 5 | 38.4 |
| 8. | Unavailability of chemotherapy agents | 17 | 38.6 | 6 | 33.3 | 3 | 23.0 |
| 9. | Shortage of blood products | 21 | 47.7 | 9 | 50.0 | 9 | 69.2 |
| 10. | Telemedicine use | 21 | 47.7 | 4 | 22.2 | 6 | 46.1 |
Discussion
The results from this first kind of national survey provide a comprehensive description of childhood cancer care services in tertiary and secondary level hospitals in most states and Union Territories in India. A pediatric oncologist was available in less than half of the tertiary hospitals. The availability of pediatric oncologists has been shown to vary in a baseline survey conducted in ten LMICs'.18 Ukraine had the highest ratio of pediatric oncologists per childhood cancer patient (1:4), followed by the Philippines (1:10), Egypt (1:23) and Venezuela (1:28). The ratio ranged from 1:50 to 1:750 for the other LMICs' (Bangladesh, Honduras, Morocco, Senegal, Tanzania and Vietnam). Pediatric oncology is in an emerging phase in India and is still lacking in terms of international standards.19 Earlier studies have shown that pediatric oncologists were available in 10% of the cancer centres in the late 80s'.20 Despite this notable improvement, the mortality-to-incidence ratio for childhood cancers ranges from 17 to 72% in India, compared to 20–24% in the United States and Britain.21,22
Besides a shortage of trained doctors, the issue of poor childhood cancer outcomes is compounded by resource constraints. In our study, public tertiary hospitals reported low availability of nurses trained in pediatric oncology, advanced diagnostic modalities, bone and PET scans, childhood cancer dedicated beds and physical infrastructure for chemotherapy administration, and insufficient stock of chemotherapeutic medicines compared with private hospitals. Similar gaps in public hospitals compared to private and NGO-managed hospitals were observed in a qualitative study conducted in seven tertiary hospitals in Delhi and Hyderabad.12 Childhood cancer care services in public hospitals were characterised by inadequate human resources and patient navigation services. Likewise, insufficient infrastructure and human resources concerning childhood cancer care were encountered in other LMICs' including Iraq, Jordan, Egypt, Lebanon and Pakistan.23
Providing optimal supportive care services help ensures favourable outcomes in childhood cancer patients. Even after the primary treatment is completed, childhood cancer survivors need long-term follow-up and supportive care even into adult life to address the delayed adverse effects of chemotherapeutic agents. In our study, most tertiary hospitals provided a wide range of support services, except for play therapy and hospice care. The proportion of public tertiary hospitals that adopted a multidisciplinary treatment approach was twice that of private hospitals. In countries with limited resources, a multidisciplinary treatment approach is shown to double the five-year event-free survival rate from 32% to 63% and improve the quality of life of childhood cancer patients due to a shift in focus from ‘survival’ to ‘thriving'.24 Our survey shows that many childhood cancer-treating medicines were unavailable at public tertiary hospitals. Access to essential and affordable pediatric cancer-treating medication ensures a continuum of care and prevents follow-up loss. In India, 70% of the out-of-pocket (OOP) healthcare expenditure is for medicines alone.25 OOP expenditure for cancer treatment is the highest compared to other diseases in India.26 The central and state governments have launched health insurance schemes to provide financial packages that offer coverage for various health expenditures on childhood cancer care. The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY) was launched in 2018 to provide financial assistance for secondary and tertiary care hospitalisation and comprises oncology benefit packages for paediatric cancer.
The availability of childhood cancer care at the secondary level of care hospitals showed a wide gap, with a little over one-third having childhood cancer care services. While tertiary hospitals are the core source of childhood cancer treatment, secondary-level hospitals could play a crucial role in early diagnosis, referral and follow-up. On a positive note, over three-quarters of the public secondary hospitals had formal referral linkages with tertiary-level hospitals.
The situational analysis of childhood cancer care services in India showed a concentration of the availability of childhood cancer care services at the tertiary level of health care. There were gaps in the availability of specialised pediatric oncology care in all the tertiary hospitals. The availability of oncology departments, advanced diagnostics, dedicated beds for childhood cancer patients, physical facilities for chemotherapy, and available medicines in stock were higher for private tertiary hospitals. An ideal pediatric oncology unit consists of dedicated clinicians and nurses trained in pediatric cancer management with sufficient health facility infrastructure, supportive care and availability of chemotherapy drugs in stock. The functioning of a pediatric care unit should also be extended to providing follow-up and palliative care to patients and training and capacity building for health care professionals.
While setting up a specialised unit may not be feasible in every hospital, providing these services through existing infrastructure with the necessary facilities for diagnosis and treatment may be the best way forward.19 Pediatric oncology service could be expanded by strengthening referral and back referral linkages between a tertiary nodal hospital and secondary health facilities. This could also be achieved through a robust end-to-end technological connectivity between the cancer-treating hospital and the district hospital using telemedicine services to enable early diagnosis and initiation of treatment. Expanding pediatric oncology training courses and programmes for health professionals, including doctors and nurses, should receive strong support from professional organisations for building a robust childhood cancer-treating health workforce.
The need of the hour is to formulate a National Childhood Cancer Policy that comprises early detection, access to affordable care, and comprehensive supportive care services through well-defined care pathways at public health facilities. Adopting the shared care model approach incorporating palliative care into the practice of pediatric oncology could enable the development of a national collaborative policy that would address disparities in access to childhood cancer care.27 It is desirable that all concerned stakeholders, including governing authorities, policymakers, health care providers, civil society organisations and communities, take proactive and collated efforts, considering WHO's global initiative for childhood cancer survival goal of 60% by 2030.28,29 Regarding addressing financial distress associated with childhood cancer, policymakers could take a cue from Kerala, the first state to introduce the ‘Cancer Suraksha Scheme’-a programme under which free cancer treatment is provided to childhood cancer patients below 18 years of age. Scaling up of Universal Health Coverage (UHC) through the robust implementation of the Ayushman Bharat (PMJAY), India's national health protection scheme, would enable a successful continuum of care through high-quality healthcare services.30 The Integration of childhood cancer as a part of the national cancer control response should be considered by integrating childhood cancer diagnosis with health programmes such as the Reproductive and Child Health programme (RCH) and ‘Rashtriya Bal Swasthya Karyakram’ (RBSK). Likewise, a component of childhood cancer care could be included in the National Programme for Prevention and Control of Non Communicable Diseases (NP-NCD) and school health programmes.
This study was systematically conducted in 26 States and 4 Union Territories in a network of tertiary and secondary-level hospitals. Adequate caution was exercised in giving uniform representation to public/private and NGO-managed hospitals. The study tool comprehensively captured the availability of treatment modalities, human resources, physical infrastructure and drug availability. One of the limitations was that the study could not assess state-wise disparities in the distribution of childhood cancer treatment services since the sample of hospitals was selected by purposive sampling in each state/UT, which could have introduced selection bias, nevertheless, the inclusion of different hospital types could have sufficed to represent the coverage of a diverse population.
Contributors
AN Data curation, formal analysis, methodology, validation, writing-original draftwriting-review and editing, PM: Conceptualization, funding acquistion, supervsion, methodology, writing-review and editing, SKL Software, data curation, validation,writing-review and editing, GKR and LM Data curation, formal analysis, writing-review and editing, RA, RS, SKD,GC: Methodology, writing-review and editing, RPSB, TSW,VKB, AB, NKC, VCR, DSD, SG, CH, MH, SNG, GK, VK, RK, AK, SKDM, GM, SM, SM, AMN, CM, AKP, SP, PP, JLD, VSR, CR, MR, NR, VR, AS, SBS, VS, PS, DS, RS, AT, PKT, ST, LT: Investigation, validation, writing-review and editing.
Data sharing statement
The complete report on ‘Situational analysis of childhood cancer care services in India’ can be accessed at https://www.ncdirindia.org/All_Reports/Childhood_Cancer/Default.aspx. Further data will be made available upon a reasonable request over email to the corresponding author.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None to declare.
Acknowledgement
We would like to acknowledge the staff of all the participating hospitals for their contribution towards data collection for this study at the respective hospital.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100235.
Appendix A. Supplementary data
References
- 1.GBD 2017 Childhood Cancer Collaborators The global burden of childhood and adolescent cancer in 2017: an analysis of the Global Burden of Disease Study 2017. Lancet Oncol. 2019;20:1211–1225. doi: 10.1016/S1470-2045(19)30339-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhakta N., Force L.M., Allemani C., et al. Childhood cancer burden: a review of global estimates. Lancet Oncol. 2019;20:e42–e53. doi: 10.1016/S1470-2045(18)30761-7. [DOI] [PubMed] [Google Scholar]
- 3.Institute for Health Metrics and Evaluation (IHME) University of Washington, IHME; Seattle: 2017. GBD compare.https://vizhub.healthdata.org/gbd-compare/ Available on: [Google Scholar]
- 4.Gatta G., Botta L., Rossi S., et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5—a population-based study. Lancet Oncol. 2014;15:35–47. doi: 10.1016/S1470-2045(13)70548-5. [DOI] [PubMed] [Google Scholar]
- 5.Allemani C., Matsuda T., Di Carlo V., et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganguly S., Kinsey S., Bakhshi S. Childhood cancer in India. Cancer Epidemiol. 2021;71 doi: 10.1016/j.canep.2020.101679. [DOI] [PubMed] [Google Scholar]
- 7.Chawla B., Hasan F., Azad R., et al. Clinical presentation and survival of retinoblastoma in Indian childrenBritish. J Ophthalmol. 2016;100:172–178. doi: 10.1136/bjophthalmol-2015-306672. [DOI] [PubMed] [Google Scholar]
- 8.Clinicopathological profile of cancers in India: a report of the hospital based cancer registries. 2021. https://ncdirindia.org/All_Reports/HBCR_2021/Default.aspx Available on: [Google Scholar]
- 9.Report of national cancer Registry programme (ICMR-NCDIR) 2020. https://www.ncdirindia.org/All_Reports/Report_2020/default.aspx Bengaluru, India. Available on: [Google Scholar]
- 10.Mathur P., Sathishkumar K., Chaturvedi M., et al. Cancer statistics, 2020: report from national cancer Registry programme, India. JCO Glob Oncol. 2020;6:1063–1075. doi: 10.1200/GO.20.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulothungan V., Sathishkumar K., Leburu S., et al. Burden of cancers in India–estimates of cancer crude incidence, YLLs, YLDs and DALYs for 2021 and 2025 based on National Cancer Registry Program. BMC Cancer. 2022;22:1–2. doi: 10.1186/s12885-022-09578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faruqui N., Bernays S., Martiniuk A., et al. Access to care for childhood cancers in India: perspectives of health care providers and the implications for universal health coverage. BMC Public Health. 2020;20:1641. doi: 10.1186/s12889-020-09758-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pati S., Hussain M.A., Chauhan A.S., Mallick D., Nayak S. Patient navigation pathway and barriers to treatment seeking in cancer in India: a qualitative inquiry. Cancer Epidemiol. 2013;37:973–978. doi: 10.1016/j.canep.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Faruqui N., Joshi R., Martiniuk A., et al. A health care labyrinth: perspectives of caregivers on the journey to accessing timely cancer diagnosis and treatment for children in India. BMC Public Health. 2019;19:1613. doi: 10.1186/s12889-019-7911-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Service Availability and Readiness Assessment (SARA)-An annual monitoring system for service delivery. Reference Manual. 2015.
- 16.WHO list of priority medical devices for cancer management. World Health Organization; 2017. https://www.who.int/publications/i/item/9789241565462./ Available on: [DOI] [PubMed] [Google Scholar]
- 17.Indian public health standards. https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=971&lid=154./ Available on:
- 18.Ribeiro R.C., Steliarova-Foucher E., Magrath I., et al. Baseline status of paediatric oncology care in ten low-income or mid-income countries receiving My Child Matters support: a descriptive study. Lancet Oncol. 2008;9:721–729. doi: 10.1016/S1470-2045(08)70194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arora B., Banavali S.D. Pediatric oncology in India: past, present and future. Indian J Med Paediatr Oncol. 2009;30:121–123. doi: 10.4103/0971-5851.65333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shenoy S., Christo G.G., Venkatesh A. Pediatric cancer care in India: a national survey. Indian J Cancer. 1990;27:91–96. [PubMed] [Google Scholar]
- 21.Gurney J.G., Bondy M.L. In: Principles and practice of pediatric oncology. 5th ed. Pizzo P.A., Poplack D.G., editors. Lippincott Williams and Wilkins; Philadelphia: 2006. Epidemiology of childhood cancer; pp. 2–14. [Google Scholar]
- 22.Stiller C. Oxford University Press; Oxford: 2007. Childhood cancer in Britain: incidence survival, mortality. [Google Scholar]
- 23.Basbous M., Al-Jadiry M., Belgaumi A., et al. Childhood cancer care in the Middle East, North Africa, and West/Central Asia: a snapshot across five countries from the POEM network. Cancer Epidemiol. 2021;71(Part B) doi: 10.1016/j.canep.2020.101727. [DOI] [PubMed] [Google Scholar]
- 24.Cantrell M.A., Ruble K. Multidisciplinary care in pediatric oncology. J Multidiscip Healthc. 2011;4:171–181. doi: 10.2147/JMDH.S7108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prinja S., Bahuguna P., Tripathy J.P., Kumar R. Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacol Toxicol. 2015;16:43. doi: 10.1186/s40360-015-0043-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhankhar A., Kumari R., Bahurupi Y.A. Out-of-Pocket, catastrophic health expenditure and distress financing on non-communicable diseases in India: a systematic review with meta-analysis. Asian Pac J Cancer Prev. 2021;22:671–680. doi: 10.31557/APJCP.2021.22.3.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arun Kumar A.R., Aruna Kumari B.S., Ramachandra C., et al. National childhood cancer comprehensive management policy-a road map. Oncology Radiother. 2020;14:1–5. [Google Scholar]
- 28.World Health Organization . World Health Organization; 2021. CureAll framework: WHO global initiative for childhood cancer: increasing access, advancing quality, saving lives.https://apps.who.int/iris/handle/10665/347370 [Google Scholar]
- 29.Pediatric Hematology Oncology Chapter of Indian Academy of Pediatrics (PHO IAP) Indian Pediatric Oncology Group (InPOG) Cankids Kidscan representing Civil Society & Patient Groups WHO global initiative for childhood cancer – India responds pediatric hematology. J Pediatr Hematol Oncol. 2020;5:145–150. [Google Scholar]
- 30.Ayushman Bharat . Ministry of Health and Family Welfare, Government of India; New Delhi: 2018. Comprehensive primary health care through health and wellness centers. Operational guidelines. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.