Abstract
Longitudinal studies have shown that children with complex trauma (i.e., exposure to multiple or repeated traumatic events of an interpersonal nature) have poorer cognitive outcomes later in life than children without complex trauma. This association may be moderated by the timing of the trauma, which may explain, in part, some heterogeneity in the findings reported across previous investigations. The objective of the systematic review and meta-analyses was to compare the cognitive outcomes of children with complex trauma and controls and to explore whether the timing of trauma (i.e., its onset and recency) moderated this association. Electronic databases (APA PsycNET, Pubmed Central, ERIC, CINAHL, Embase) and gray literature were systematically searched. To be included, studies had to (1) have a longitudinal design, (2) comprise children with complex trauma and controls, and (3) include a cognitive assessment. Thirteen studies were identified. Meta-analyses were conducted to compare children with complex trauma and controls, while subgroup analyses and meta-regressions explored the impact of potential moderators. Children with complex trauma had poorer overall cognitive functioning than controls, and the timing of trauma (early onset and, to a greater extent, recency of trauma) moderated this association. Thus, findings suggest that children with complex trauma are at risk of cognitive difficulties quickly after trauma exposure. As such, systematic neuropsychological assessment and interventions supporting the optimal development of cognitive functioning among children with complex trauma should be investigated to determine whether prompt interventions lead to better cognitive functioning.
Keywords: child, child abuse, cognitive dysfunction, meta-analysis, longitudinal studies
The National Child Traumatic Stress Network (NCTSN; Cook et al., 2003) proposed the term “complex trauma” to encompass both children’s exposure to multiple, interpersonal traumatic events and the wide-ranging, long-term effects of this exposure. These events usually involve a parent or a caregiver, are severe and pervasive, and occur during sensitive developmental periods. They have multiple putative effects on child development, including dysregulation in attachment and relationships, affect dysregulation, dissociation, poor behavior control, and poor cognitive functioning (Ford & Courtois, 2013).
Experiences of maltreatment and severe deprivation in institutions (e.g., Romanian orphanages) may both be considered sources of complex trauma. Indeed, maltreatment tends to be repeated and experienced in multiple forms (e.g., physical, sexual and verbal abuse, neglect), and to occur early in life at the hand of a parent (Milot et al., 2018). Experiences of severe deprivation in institutions follow the early loss of a parent (e.g., death or abandonment) and are characterized by social and emotional deprivation and cognitive understimulation (Bick & Nelson, 2016; Carr et al., 2020; Sonuga-Barke et al., 2017). Institutional deprivation is also characterized by malnutrition, limited access to physical resources and facilities, poor hygiene, and overcrowding, conditions that may have incremental effects on child development (Carr et al., 2020; Sonuga-Barke et al., 2017). These notable differences notwithstanding, maltreatment and institutional deprivation both have multiple and similar effects on child development (e.g., dysregulation in attachment and relationships, affect dysregulation, poor cognitive functioning; Bick & Nelson, 2016; Carr et al., 2020; Milot et al., 2018). Thus, both experiences share common key features pertaining to complex trauma (in terms of exposure and impacts) and, in this review, were considered under this umbrella.
Complex Trauma, the Brain and Cognitive Functioning
It has been theorized that complex trauma may induce a toxic stress response because of the intense, repeated, or prolonged activation of the neurophysiological stress response systems (e.g., hypothalamic–pituitary–adrenocortical [HPA] axis) during sensitive developmental periods, when a caregiver’s protection is absent (Shonkoff, 2010). In the long run, such stress responses may damage the regulatory capacity of the HPA axis, causing a persistent tendency toward higher or lower cortisol secretion in stressful contexts (Bernard et al., 2017; Holochwost et al., 2020; Khoury et al., 2019). This may induce structural and functional brain alterations in various brain regions, including the prefrontal cortex, the amygdala and the hippocampus, which are responsible for a host of cognitive functions (Bick & Nelson, 2016; Lupien et al., 2009; Nemeroff, 2016; Rauch et al., 1998; Teicher et al., 2016; Yehuda et al., 2015). Notably, these regions undergo rapid maturation and organization during sensitive developmental periods, such as infancy and puberty (Bick & Nelson, 2016; Koss & Gunnar, 2018; Teicher et al., 2016). These periods are characterized by higher sensitivity of brain regions to adverse (or positive) experiences, partly because of the increased plasticity of the brain during these periods of intense maturation and organization (Bick & Nelson, 2016; Cowell et al., 2015; Lupien et al., 2009; Shonkoff, 2010; Zeanah et al., 2011). In sum, it is regularly argued that impaired HPA axis functioning and brain alterations act as putative stress-mediating mechanisms through which trauma occurring during sensitive developmental periods exerts a detrimental influence on cognitive functioning later in life.
Cognitive functioning comprises numerous interrelated cognitive functions, including intelligence, language, perceptual/visuospatial functions, memory as well as attention and executive functions (EF) (Lezak et al., 2004; Strauss et al., 2006). On the one hand, trauma may have a stronger or weaker impact on certain cognitive functions that are more or less vulnerable to toxic stress because they rely on brain regions with varying periods of vulnerability to toxic stress. On the other hand, given that toxic stress is expected to detrimentally impact numerous brain regions that are collectively responsible for many cognitive functions, trauma may have a pervasive impact on several aspects of cognitive functioning (Bick & Nelson, 2016; Lupien et al., 2009; Nemeroff, 2016; Teicher et al., 2016). As such, the umbrella construct “cognitive functioning” was used to underline this pervasive effect of complex trauma, as it has been used in previous work (e.g., Irigaray et al., 2013; Malarbi et al., 2017; Masson et al., 2015).
The Effect of the Timing of Trauma
Given the existence of sensitive periods of enhanced vulnerability to toxic stress, the timing of trauma, that is the onset and recency of trauma, has been recurrently hypothesized to differentially impact functioning across a variety of domains, including cognitive functioning. The early onset hypothesis rises from current knowledge of early sensitive developmental periods, which are characterized by higher sensitivity of brain regions to toxic stress (Bick & Nelson, 2016; Cowell et al., 2015; Lupien et al., 2009; Shonkoff, 2010; Zeanah et al., 2011). As such, trauma has been proposed to have the strongest impact when it occurs early in life (e.g., infancy). This hypothesis has been consistently supported across a host of domains (e.g., mental health outcomes, internalizing and externalizing problems), including cognitive functioning (Carr et al., 2020; Koss & Gunnar, 2018; Zeanah et al., 2011). For instance, Cowell et al. (2015) found that children maltreated during infancy had poorer EF than those maltreated after this period. Similarly, Hambrick et al. (2019) reported that among children between the ages of 8 and 10 years, overall cognitive functioning was more vulnerable to stress (e.g., domestic violence, caregiver drug use, neglect) during infancy (2–12 months), but also during childhood (>4 years). This increased vulnerability to stress during both infancy and childhood could suggest that the impact of trauma on cognitive functions is stronger not only when trauma occurs early in life, but also when it is more recent. Indeed, another hypothesis pertains to the recency of trauma (time elapsed since trauma at the time of the measurement of cognitive functioning—the recency hypothesis). Some evidence does suggest that the impact of trauma on cognitive functions may be stronger when trauma is more recent (Carr et al., 2020; Zeanah et al., 2011). For instance, in samples of children who experienced severe deprivation in institutions, the early gap in intelligence quotient [IQ] scores between institutionalized children and non-institutionalized children decreased over time, such that the two groups of children were no longer different at age 8 (Carr et al., 2020; Zeanah et al., 2011). In contrast, Cowell et al. (2015) did not find such an effect of recency on EF in maltreated children. However, because EF remain immature up to approximately age 25 (Center on the Developing Child at Harvard University, 2011), the impact of maltreatment on EF may manifest only later in development (referred to as a “sleeper” or “inoculation” effect; Bick & Nelson, 2016; Lupien et al., 2009; Rutter, 2013; Zeanah et al., 2011).
These putative effects pertaining to the recency hypothesis may however be captured only using prospective longitudinal designs. Longitudinal designs are ideally positioned to provide information on the short- and long-term effects of trauma on cognitive functions and, moreover, to control for unmeasured potential confounders (intra-individual perspective; Su et al., 2019). This information is crucial to knowing whether trauma has short- and long-term effects and whether these tend to be transient or rather persistent over time. To date, even though a few reviews have been published on cognitive outcomes of children with complex trauma (which are reviewed below), most studies included in these reviews have a cross-sectional design, and the effects of the onset and recency of trauma have not been formally investigated. This is one of the objectives of this systematic review of longitudinal studies.
Existing Reviews on Cognitive Outcomes of Children with Complex Trauma
Existing reviews on cognitive outcomes of maltreated and institutionalized children provide clear evidence that these children have, overall, poorer cognitive outcomes than controls (i.e., children without complex trauma) (Irigaray et al., 2013; Kavanaugh et al., 2017; Perfect et al., 2016; Veltman & Browne, 2001; Young-Southward et al., 2020). However, evidence gathered from these reviews is less clear as to the specific cognitive functions affected in children with complex trauma. For instance, many reviews showed lower language skills in maltreated or trauma-exposed children in comparison with controls (Irigaray et al., 2013; Perfect et al., 2016; Veltman & Browne, 2001), but others did not (Kavanaugh et al., 2017). Kavanaugh et al. (2017) instead found strong evidence for poorer intelligence and attention/EF in maltreated children, whereas findings were not as conclusive for language and memory. In contrast, other reviews did highlight poorer memory in maltreated or trauma-exposed children compared to controls (Irigaray et al., 2013; Perfect et al., 2016). Some reviews further suggest poorer perceptual/visuospatial functions in maltreated children in comparison to controls (Irigaray et al., 2013; Kavanaugh et al., 2017). Thus, inconsistencies remain as to the specific cognitive functions affected in children with complex trauma. These inconsistencies may be explained or moderated by the type of trauma (e.g., abuse, neglect, institutional deprivation), the onset of trauma and the recency of trauma (given that cognitive functions rely on brain regions with varying periods of vulnerability to toxic stress) or the presence of post-traumatic stress disorder (PTSD), which may exacerbate the effect of trauma on cognitive functions (Kavanaugh et al., 2017; O’Higgins et al., 2017; Young-Southward et al., 2020). The previous reviews mostly included retrospective or cross-sectional design studies; only one systematic review focused exclusively on longitudinal studies (Su et al., 2019). It indicated that childhood maltreatment was associated with poorer overall cognitive functioning; however, despite their focus on longitudinal studies, Su et al. (2019) did not formally address the effect of the timing of trauma nor include a meta-analysis.
Reviews Including a Meta-Analysis
Meta-analysis and meta-regression can be used to identify specific cognitive functions affected in children with complex trauma and formally test whether the timing of trauma (and other factors) moderates this association. Only three existing reviews included a meta-analysis (Malarbi et al., 2017; Masson et al., 2015; Sylvestre et al., 2016). Sylvestre et al. (2016) shed light on the inconsistencies in previous reviews regarding the language skills of maltreated or trauma-exposed children. They showed that abused and neglected children had lower language skills than controls, and that the type of maltreatment (physical abuse, neglect or both) did not moderate the association between maltreatment and language skills. However, the year of publication did; children had poorer language skills in more recent studies. The year of publication may capture methodological differences between studies, such as cohort effects and changes in the conceptualization of maltreatment over the years. For instance, eligibility criteria may become more (or less) stringent, which could support (or undermine) the capacity of studies to robustly detect associations between complex trauma and cognitive functioning. Beyond language skills, Masson et al. (2015) systematically reviewed and conducted meta-analyses on the cognitive functioning of children, adolescents and adults with histories of childhood maltreatment. They found that those with such histories had lower scores in virtually all cognitive functions, and further identified that participants assessed at a younger age (0–5 years old vs. adulthood) had poorer cognitive functioning. Because childhood maltreatment was necessarily closer in time for participants assessed between the ages of 0 and 5 years (vs. adulthood), this points to a possible effect of recency—the impact of maltreatment on cognitive functions being stronger when trauma was more recent. Otherwise, similarly to Sylvestre et al. (2016), they did not find that the type of maltreatment moderated the association between childhood maltreatment and cognitive functioning. Lastly, Malarbi et al. (2017) compared trauma-exposed children with PTSD, trauma-exposed children without PTSD, and controls to try to disentangle the effects of trauma exposure itself versus those of PTSD. They found that trauma-exposed children with PTSD had poorer outcomes than controls in essentially all cognitive functions, whereas trauma-exposed children without PTSD only had poorer memory and EF than controls, which suggest that PTSD may exacerbate the impact of trauma on cognitive outcomes.
The Current Review
Past reviews have offered convincing evidence supporting the association between complex trauma, poorer cognitive functioning and difficulties in virtually all cognitive functions. However, uncertainty remains as to the putative effect of the timing of trauma, that is, the early onset and recency hypotheses, given that these hypotheses were never formally tested in systematic reviews and meta-analyses. Doing so may inform on the short- and long-term effects of trauma on cognitive functions, on whether these effects are transient or persisting, as well as on when the onset of trauma is expected to exert the strongest detrimental impact on cognitive functioning. Such information is needed for prevention and intervention efforts at moments where effects are expected to be the strongest and to offer neuropsychological assessments and interventions in a timely manner. As mentioned previously, longitudinal designs are ideally positioned to provide this information. This systematic review and meta-analyses were undertaken to fill this gap in knowledge by focusing on longitudinal studies. We sought to answer the following questions: (1) Do children with complex trauma have poorer cognitive outcomes than controls? (2) Does the timing of trauma moderate cognitive outcomes? (3) Do other factors (i.e., type of trauma, publication year and methodological quality) moderate cognitive outcomes in children with complex trauma?
Methods
Methods were based upon the PRISMA statement for reporting systematic reviews and meta-analyses (Liberati et al., 2009) and the JBI methodology (Moola et al., 2017). This systematic review is part of a larger project that was prospectively registered on PROSPERO (CRD42019121610) and pre-specified in a protocol (Matte-Landry & Collin-Vézina, 2020), as recommended by PRISMA.
Eligibility Criteria
To be included, studies had to (1) have a prospective longitudinal design with at least two time points, (2) comprise ≥1 group of children (0–18 years old) with complex trauma (hereafter, the trauma group), (3) comprise ≥1 group of children who had not been exposed to any trauma for comparison purposes (hereafter, the control group), and (4) include an assessment of cognitive functions with standardized tests with documented psychometric properties when the participants were 18 years old or younger.
Search Strategy
The search strategy was developed and conducted by the first author (a clinical neuropsychologist and researcher trained in systematic reviews and meta-analyses). The strategy was first developed for APA PsycNET, and then adapted to the syntax, subject headings and thesaurus of other databases (Pubmed Central, ERIC, CINAHL, Embase; see Appendix A). Additional studies were searched for by looking at reference lists of included studies and existing reviews. In addition, to limit the potential impact of a publication bias (the fact that studies with positive and significant results are more likely to be published following peer review), further efforts were made to locate unpublished studies and documents whose publication is not associated with peer review, following recommendations from Liberati et al. (2009) and Moola et al. (2017). Therefore, the search strategy was adapted and extended to the web (Google) and PROQUEST.
Study Selection and Data Extraction
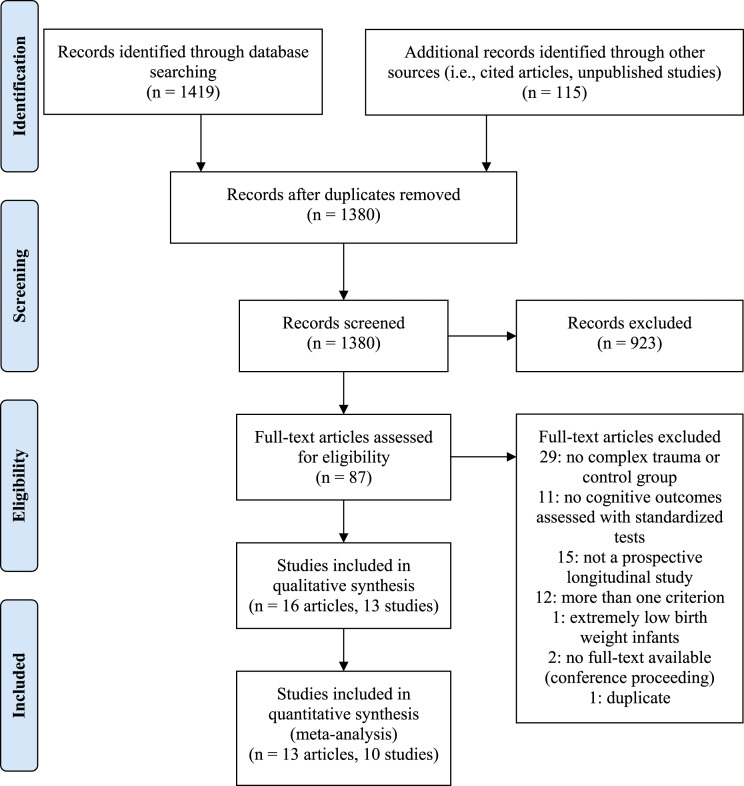
Study selection and data extraction were done by two evaluators (the first author and the second author, a graduate student in psychology), independently and in duplicate. Disagreements were resolved by discussion, and consensus was reached in all cases. The study selection and exclusion process is presented in a PRISMA flow diagram (Figure 1). First, articles yielded by the search were exported to DistillerSR, a systematic review software that automates the management of literature collection, triage and assessment (Evidence Partners, n.d.). Second, titles and abstracts were screened by the two evaluators. Third, full-text articles were read to determine eligibility. When articles met all eligibility criteria, the two evaluators extracted the following information from the articles (when available): authors; study language; publication status (published or unpublished) and year; study setting; recruitment procedures; number of assessments in the study; sample sizes; children’s characteristics (gender, ethnicity, family socioeconomic status [SES], behavioral and mental health problems, current placement, care history, interventions offered to children, PTSD diagnosis or symptoms); type(s) and duration of trauma; age(s) at the time of onset of trauma; age(s) at the time of cognitive assessment(s); cognitive functions assessed; and tests used.
Figure 1.
PRISMA flow diagram.
The primary outcome for this meta-analytic review was “overall cognitive functioning,” an umbrella construct comprising the aggregation of scores from separate cognitive functions measured in the reviewed studies (i.e., intelligence, language, perceptual/visuospatial functions, memory and EF). Secondary outcomes were the above cognitive functions that made up overall cognitive functioning in this review: intelligence, language, perceptual/visuospatial functions, memory, and EF (Lezak et al., 2004; Strauss et al., 2006). Trauma and control groups’ mean and standard deviation scores on outcomes were extracted from the text, tables, graphs and/or figures. When the groups’ standard deviations were unavailable, the test’s standard deviation was used. When information could not be extracted from articles, authors of recent studies (<5 years) were contacted by email.
Risk of Bias Within Studies
Assessments of the risk of bias within studies were done independently and in duplicate by the two evaluators who completed study selection and data extraction. Once again, disagreements were resolved by discussion, and consensus was reached in all cases. The evaluators used the JBI Critical Appraisal Checklist for Cohort Studies that was developed by the JBI team and underwent peer review (Moola et al., 2017). It was chosen in accordance with the JBI methodology and because it matches the prospective longitudinal design of the studies reviewed. The evaluators assessed the presence (or absence) of the checklist’s 11 criteria regarding the equivalence of groups, exposure measurement, identification and management of confounders, outcome measurement, follow-up time, attrition, and statistical analyses.
Data Synthesis
For studies to be included in meta-analyses, we had to be able to calculate an effect size (Hedges’ g) from group means and standard deviations. In some of the reviewed studies, children were divided into independent subgroups, based on the timing of trauma, the type of maltreatment, or the type of intervention received. A single effect size was calculated and allowed per subgroup per meta-analysis, ensuring that estimates were independent. For the primary outcome (overall cognitive functioning), an aggregated effect size was calculated by averaging effect sizes of separate cognitive functions. For secondary outcomes, one effect size was calculated per cognitive function. When more than one score was reported for a specific cognitive function, an aggregated effect size was calculated for that function. When outcomes were assessed at multiple time points after trauma, only the scores from the first assessment after trauma were used to ensure that estimates were independent and to allow comparability across studies. Effect sizes were interpreted as follows: .20 small, .50 moderate, and .80 large mean difference between groups (Cohen, 1988).
For the first research question, we compared trauma and control groups using a meta-analysis for overall cognitive functioning, and then separate meta-analyses for each specific cognitive function. All meta-analyses were performed using random-effect models with the random-effects maximum likelihood (REML) method in STATA (StataCorp, 2019). This method uses the variance of the random effects to account for the between-study heterogeneity. Homogeneity tests, based on the Q statistic, were used to test whether heterogeneity was significant, and the I2 statistic (the percentage of variation across studies due to heterogeneity) was used to quantify heterogeneity: 25% low, 50% moderate, and 75% high (Higgins & Thompson, 2002).
For the second question, we performed subgroup analyses to determine whether the aspects pertaining to the timing of trauma moderated cognitive outcomes. Ages at the time of onset of trauma and cognitive assessment(s) varied greatly between and within the study samples, and age intervals were also often reported. Consequently, using the available information, we relied on two developmental periods (early childhood [0–5 years old] and childhood/adolescence [6–18 years old]), as did others (e.g., Cowell et al., 2015; Harpur et al., 2015; Masson et al., 2015). It was further deemed appropriate given the definition of complex trauma, that is, exposure to repeated and multiple traumatic events during sensitive developmental periods—not a unique traumatic event at a specific point in time (Cook et al., 2003). Trauma groups were thus constituted according to age at the time of trauma and cognitive assessment(s). Three subgroups were derived: (1) Early Onset/Recent Trauma group, in which the trauma and cognitive assessment both occurred during early childhood; (2) Early Onset/Less Recent Trauma group, referring to children with early onset trauma for whom the assessment was conducted during childhood/adolescence; and (3) Later Onset/Recent Trauma group whose trauma and assessments both took place during childhood/adolescence. Notably, both onset and recency of trauma were considered simultaneously this way, in order to disentangle the effect of the onset and recency of trauma. Indeed, we contrasted the Early Onset/Recent Trauma group with the Early Onset/Less Recent Trauma group to isolate the effect of the recency of trauma—testing the recency hypothesis. Similarly, we contrasted the Early Onset/Recent Trauma group with the Later Onset/Recent Trauma group to isolate the effect of early versus late onset—testing the early onset hypothesis.
For the third question, we performed subgroup analyses and meta-regressions for the following moderating factors: type of trauma (maltreatment vs. institutional deprivation), methodological quality (number of quality criteria not met), and study publication year (when there were multiple articles for the same study, the most recent publication year was used). Finally, a funnel plot was used to explore the presence of small-study effects that may be attributed to publication bias.
Results
Study Selection
The results of the study selection and exclusion process is presented in a PRISMA flow diagram (Figure 1). A total of 16 articles (13 independent study samples) were included. Inter-rater agreement was 91% (title and abstract screening) and 80% (full-text eligibility). None of the 20 unpublished studies and non-peer reviewed documents identified through the web (Google) and PROQUEST (e.g., government documents, theses, papers presented at conferences) met all the eligibility criteria, and thus none were included in this review.
Study Characteristics
All articles were published in English in peer-reviewed journals. Characteristics of the included studies are presented in detail in Appendix B. One study was a population-based longitudinal study (Mills et al., 2011), four were longitudinal studies of at-risk samples (e.g., low-income/disadvantaged families, high-risk sampling strategy, children at risk of maltreatment; Enlow et al., 2012; Font & Berger, 2015; Harpur et al., 2015; Jaffee et al., 2007), and two studies were conducted in samples of children adopted from Romanian institutions (Beckett et al., 2006; Tibu et al., 2016). In the remaining studies, community samples of maltreated children were recruited.
Group Characteristics
Characteristics of trauma and control groups are presented in Appendix C. Overall, 19,795 children were included as part of 13 independent studies. In most studies, the control group was matched to the sociodemographic characteristics of the trauma group so that there were no, or very few, differences between the groups in terms of children’s age, gender, and ethnicity, parent’s education and families’ SES, which was a methodological strength of the studies reviewed. The predominant ethnic group in trauma and control groups was Caucasian in six studies (Beckett et al., 2006; Fitch et al., 1976; Mills et al., 2011; Noll et al., 2010; Tibu et al., 2016; Weller et al., 2015) and African American in three studies (Cheatham et al., 2010; Font & Berger, 2015; Harpur et al., 2015). Ethnic group distribution was not specified for trauma and control groups separately in the four remaining studies (Enlow et al., 2012; Jaffee et al., 2007; Manly et al., 2013; Rieder & Cicchetti, 1989). In the majority of studies, the families’ SES was considered low in both trauma and control groups (e.g., parents having a high school diploma or less education, history of public assistance, low family income).
The majority of studies did not report precise information regarding children’s behavioral and mental health problems, current placement, care history, interventions, and duration of trauma, and no study reported the occurrence of a PTSD diagnosis or symptoms. Tibu et al. (2016) reported that approximately 20% of children with trauma had ADHD, whereas Jaffee et al. (2007) reported that approximately a quarter of children with trauma had well-adjusted temperaments. Weller et al. (2015) reported internalizing and externalizing symptoms among children with trauma. In four studies (including the two conducted in samples of children adopted from Romanian institutions), some or all of the children in trauma groups were living in out-of-home care (Beckett et al., 2006; Harpur et al., 2015; Tibu et al., 2016; Weller et al., 2015).
Cognitive Outcomes
Details on the assessment of cognitive outcomes are presented in Appendix D. Seven studies, though longitudinal, assessed cognitive functions only at one time point. Others did so at two or three time points (Beckett et al., 2006; Cheatham et al., 2010; Enlow et al., 2012; Fitch et al., 1976; Font & Berger, 2015; Noll et al., 2010), but only two included assessments of cognitive functions both before and after trauma (Cheatham et al., 2010; Font & Berger, 2015). The cognitive functions assessed included intelligence, language, perceptual/visuospatial functions, memory, and EF (Lezak et al., 2004; Strauss et al., 2006). In nine studies, only one function was assessed (intelligence or language), whereas two to four functions were assessed in the remaining studies (Fitch et al., 1976; Harpur et al., 2015; Manly et al., 2013; Tibu et al., 2016).
Risk of Bias Within Studies
Seven studies did not meet one of the 11 quality criteria, three studies did not meet two criteria (Fitch et al., 1976; Harpur et al., 2015; Mills et al., 2011), and three studies did not meet three criteria (Cheatham et al., 2010; Enlow et al., 2012; Rieder & Cicchetti, 1989). One criterion was not met by any study because evaluators answered “N/A” to item 6 (“Were the groups free of the outcome at the start of the study?”) for all studies. For 11 of the 13 studies, one (k = 3), two (k = 4), three (k = 2) or four (k = 2) items of the checklist were answered “Unclear” because information was not reported or not reported clearly enough to assess the presence or absence of the criteria. Overall, studies met most quality criteria and were considered to be of good quality.
Data Synthesis
To compare trauma and control groups, we performed meta-analyses for overall cognitive functioning, as well as for intelligence and language (other cognitive functions were not assessed in a sufficient number of studies to conduct meta-analyses for these specific functions). Three studies could not be included in meta-analyses because effect sizes could not be calculated (Font & Berger, 2015; Jaffee et al., 2007; Manly et al., 2013). Results not included in meta-analyses are presented in Appendix E.
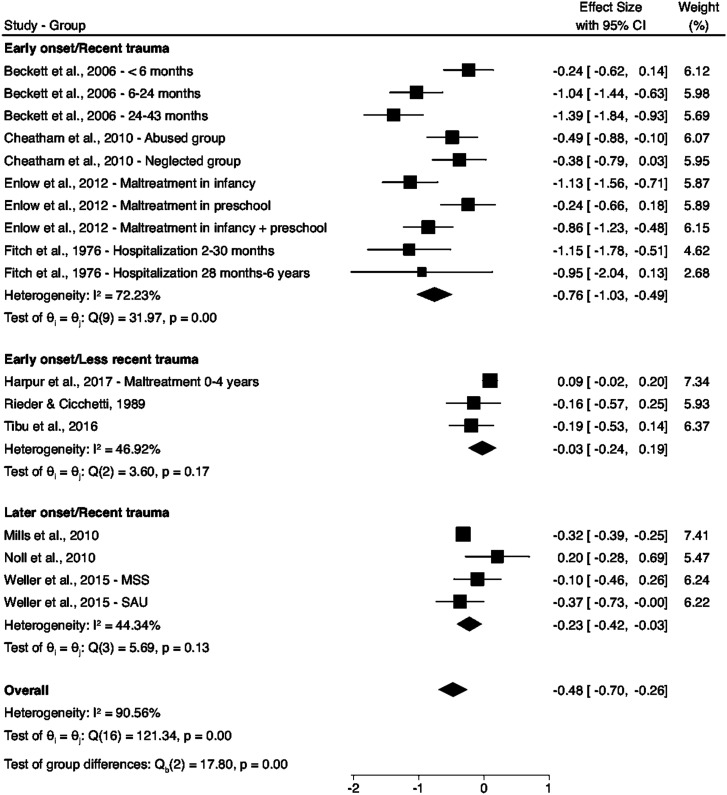
Overall Cognitive Functioning
Figure 2 shows results for the meta-analysis on overall cognitive functioning (“Overall” section at the bottom of the figure) as well as the results of the subgroup analyses for the onset and recency of trauma (three sections at the top of the figure). The overall effect size between children with complex trauma and controls was −.48, 95% CIs [−.70, −.26], p < .001, which suggests that children with complex trauma had poorer overall cognitive functioning than controls. Subgroup analyses for the onset and recency of trauma showed that when trauma was more recent, whether onset was in early childhood or childhood/adolescence, children with complex trauma had poorer overall cognitive functioning than controls. However, when trauma was less recent, children with complex trauma were similar to controls. Additionally, the test of group differences showed significant between-group differences among children with complex trauma: the Early Onset/Recent Trauma group had the poorest outcomes of all, whereas the two other groups (Early Onset/Less Recent Trauma group and Later Onset/Recent Trauma group) were similar in terms of their overall cognitive functioning. Between-study heterogeneity was significant and high in the overall meta-analysis (see I2 and Q statistics at the bottom of Figure 2), yet diminished when subgroup analyses were used (see I2 and Q statistics for each subgroup).
Figure 2.
Meta-analysis for overall cognitive functioning and subgroup analyses for the effect of onset and recency of trauma.
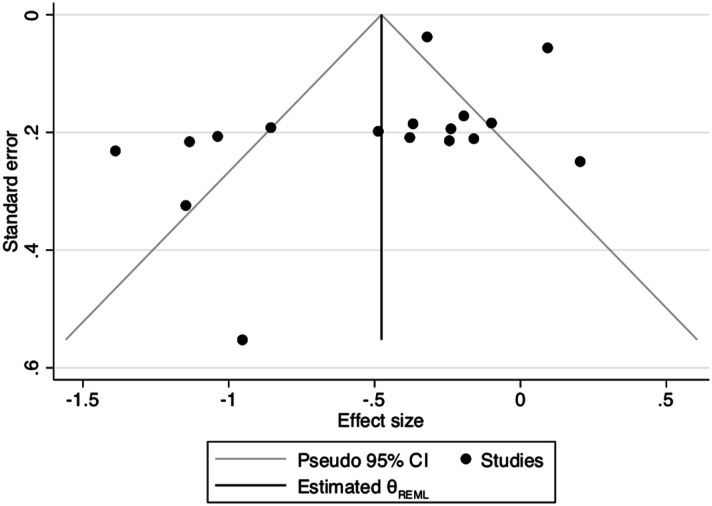
In subgroup analyses for type of trauma, we compared children with any form of maltreatment to children who experienced severe deprivation in Romanian institutions. We did not conduct subgroup analyses for the specific forms of maltreatment because children were exposed to a single form of maltreatment in only two studies (Cheatham et al., 2010; Noll et al., 2010). The effect size was similar between the samples of children who experienced severe deprivation in institutions and the samples of children exposed to maltreatment (Qb (1) = .92, p = .34), suggesting that the estimated impact of trauma on cognitive functioning is similar across samples, and lending support to the inclusion of both types of experiences in this review. Meta-regression analyses indicated that publication year (.01, 95% CI [−.1, .03], p = .372) and methodological quality (−0.05, 95% CI [−.31, .21], p = .703) were not significant moderators of the association between complex trauma and overall cognitive functioning. Although the funnel plot (Figure 3) was asymmetrical, visual exploration did not suggest a publication bias.
Figure 3.
. Funnel plot.
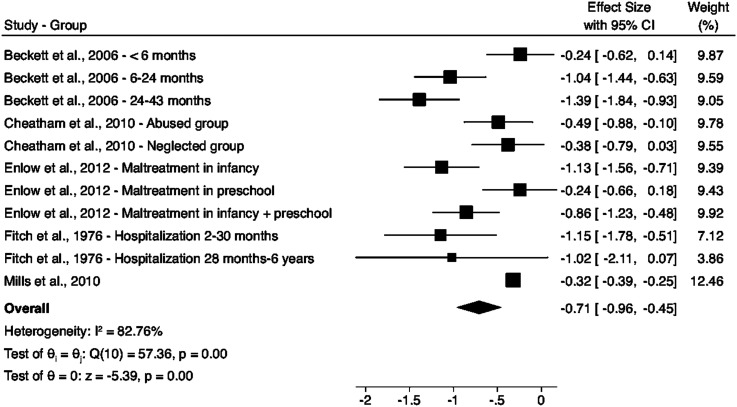
Intelligence
The overall effect size between the trauma and control groups was −.71, 95% CI [−.96, −.45], p < .001 (Figure 4), which suggests that children with complex trauma had lower IQ scores than controls. The between-study heterogeneity was significant and high (Q (10) = 57.36, p < .001, I2 = 82.76%). We did not conduct the subgroup analyses for onset and recency of trauma specifically for intelligence because intelligence was not measured in the samples for the Early Onset/Less Recent Trauma group, and in only one study in the samples for the Later Onset/Recent Trauma group.
Figure 4.
Meta-analysis for intelligence.
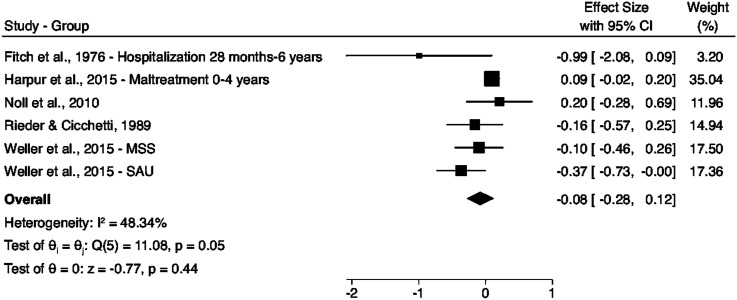
Language
Figure 5 shows that the overall effect size between children with complex trauma and controls was −.08, 95% CI [−.28, −.12], p = .44, suggesting no difference between children with complex trauma and controls in terms of language skills. The between-study heterogeneity was moderate (I2 = 43.34%) and on the brink of significance (Q (5) = 11.08, p = .05). For the same reasons as for intelligence, subgroup analyses for onset and recency of trauma were not conducted specifically for language.
Figure 5.
Meta-analysis for language.
Discussion
The objectives of this review were to compare the cognitive outcomes of children with complex trauma and controls and to explore potential moderators that may influence this association. We conducted meta-analyses on the data drawn from 10 longitudinal studies of good empirical quality and found that children with complex trauma had lower overall cognitive functioning and IQ scores than controls, whereas their language skills were similar to those of controls. Subgroup analyses showed that the timing of trauma moderated the association between complex trauma and overall cognitive functioning. Indeed, when trauma was more recent (i.e., closer in time to the cognitive assessment), children had poorer overall cognitive functioning than controls, regardless of whether the onset of trauma occurred in early childhood or childhood/adolescence. Moreover, among all children with complex trauma, it was the Early Onset/Recent Trauma group who had the poorest overall cognitive functioning. These findings point to the possibility that early onset and, to a greater extent, the recency of trauma are associated with poorer cognitive outcomes (see Table 1 for critical findings).
Table 1.
Critical Findings.
|
|
|
|
Cognitive Outcomes of Children with Complex Trauma
The finding that children with complex trauma had lower overall cognitive functioning and intelligence than controls is in line with previous reviews (e.g., Kavanaugh et al., 2017; Perfect et al., 2016; Young-Southward et al., 2020) and meta-analyses (Malarbi et al., 2017; Masson et al., 2015). In this review, the global effect sizes for overall cognitive functioning and intelligence were very similar to those reported by Malarbi et al. (2017) and Masson et al. (2015). Compared to controls, children with complex trauma appeared to have moderate cognitive difficulties. Concretely, this represents approximately −7.5 IQ points on IQ scales, such as the Wechsler’s scales (Wechsler et al., 2014). In contrast, we found no difference in language skills between children with complex trauma and controls. Despite methodological similarities (except the focus on longitudinal studies), this contrasts with Sylvestre et al. (2016) who showed that maltreated children had lower language skills than controls. Yet, it should be noted that Sylvestre et al. (2016) found significant heterogeneity across the studies they included in their meta-analytic review: nine of the 23 studies had non-significant effect sizes, suggesting the absence of difference between the maltreated and control children. Kavanaugh et al. (2017) also reported mixed findings with regards to language skills. It is possible that the onset and recency of trauma explain in part this heterogeneity in language skills among children with complex trauma, along with other factors such as the chronicity of trauma or the additional presence of PTSD or other behavioral and mental health problems (Irigaray et al., 2013; Kavanaugh et al., 2017; O’Higgins et al., 2017; Perfect et al., 2016; Young-Southward et al., 2020). However, these hypotheses could not be tested in this review because of the unavailability of this information in the reviewed studies. Building on new studies that include this key information, future meta-analyses will be able to further shed light on what lies behind the heterogeneity of cognitive outcomes among children with complex trauma.
The Timing of Trauma
This was the first meta-analysis to formally test whether the onset and recency of trauma moderated cognitive outcomes in children with complex trauma. Previous meta-analyses considered only the age at the time of assessment because of a lack of information or differences in reporting of information pertaining to the timing of trauma across included studies. Nevertheless, we derived from the available information (age at onset and age at assessment) three subgroups—Early Onset/Recent Trauma group, Early Onset/Less Recent Trauma group, and Later Onset/Recent Trauma group—capturing the combined information on the onset and recency of trauma. We showed that early onset and, to a greater extent, the recency of trauma were associated with poorer overall cognitive functioning.
Following the early onset hypothesis, we had anticipated that participants with early onset trauma would have poorer cognitive functioning given that early childhood is a sensitive period of enhanced vulnerability to toxic stress (Cowell et al., 2015; Hambrick et al., 2019; Koss & Gunnar, 2018; Shonkoff, 2010; Zeanah et al., 2011). Regarding the recency hypothesis, previous evidence was less clear as to whether the impact of trauma would be stronger (or weaker) when trauma was more (or less) recent (Carr et al., 2020; Sonuga-Barke et al., 2017; Zeanah et al., 2011). Our findings suggest the former—that the impact of trauma may be stronger when trauma is more recent. We speculate that this uncovered effect of the recency of trauma may be driven by transient effects of trauma on cognitive functions, which may be more apparent shortly after trauma and then lessen with time. This is in line with findings from samples of institutionalized children indicating that the early gap between their IQ scores and those of controls decreased over time, such that the two groups of children were no longer distinguishable later in life (Carr et al., 2020; Zeanah et al., 2011). However, future studies are needed to explain the mechanisms underlying these potential transient effects of trauma on cognitive functioning.
Yet, a first putative explanation may be individual (e.g., previous cognitive functioning, self-regulation abilities, brain plasticity) and environmental (e.g., social support) characteristics present before and after trauma that may support resilience (Cicchetti, 2013; Miller-Graff, 2020; Rutter, 2013; Sonuga-Barke et al., 2017). The resilience literature suggests that some resilience promoters would operate prior to the adverse experiences (e.g., success in situations demanding autonomy and responsibility), increasing a child’s personal sense of agency and helping them to cope with adverse experiences, while other resilience promoters would operate after the occurrence of the experiences (e.g., social support from peers or the extended family, or interventions by mental health professionals or educators), providing resources and opportunities in the environment to support resilience (Rutter, 2013).
Accordingly, what appears to be a transient effect of trauma on cognitive functions may reflect successful placement following trauma. As a matter of fact, among the Early Onset/Less Recent Trauma group, two of the three samples comprised children who had been adopted or were living in out-of-home care at the time of the cognitive assessment (Harpur et al., 2015; Tibu et al., 2016). It is possible that the placement and/or interventions that took place may have provided the children a greater sense of safety, predictability, and control. This may have helped to normalize HPA axis activity, limiting the extent of brain exposure to stress hormones and, more generally, creating more optimal conditions to promote cognitive functioning (e.g., Cicchetti, 2013; Lupien et al., 2009; Rutter, 2013; Zeanah et al., 2011). At school-age, the educational context may have further provided opportunities to promote a sense of safety as well as optimal conditions for cognitive functioning, through caring and encouraging environments, social and educational activities and the school curriculum (Rutter, 2013; Scales & Roehlkepartain, 2003; Yule et al., 2019). These hypotheses remain, however, speculative in nature and should be further investigated in longitudinal studies that systematically document the timing of trauma as well as individual and environmental resilience promoters (e.g., previous cognitive functioning, sense of agency, social support, or interventions) in various ecological contexts.
Other Moderating Factors
In this review, samples of maltreated or institutionalized children were considered to have complex trauma. Although some previous reviews qualitatively compared these samples (e.g., Bick & Nelson, 2016; Young-Southward et al., 2020), this was the first review to formally test whether their cognitive functions were indeed similar. We found similar overall effect sizes for both maltreated and institutionalized children, suggesting they have similar cognitive outcomes. This may potentially indicate that similar mechanisms underlie difficulties in children exposed to severe deprivation and those exposed to maltreatment. Indeed, impairment of HPA axis functioning and ensuing structural and functional alterations in the prefrontal cortex, the amygdala, and the hippocampus were found in both contexts (Bick & Nelson, 2016; McLaughlin et al., 2015). Otherwise, year of publication and methodological quality were not significant moderators of the association between complex trauma and cognitive functions, suggesting no cohort effect and that effect sizes do not vary as a function of methodological quality. Other moderating factors of interest (e.g., the chronicity of trauma or the additional presence of PTSD or other behavioral and mental health problems; Irigaray et al., 2013; Kavanaugh et al., 2017; Perfect et al., 2016; O’Higgins et al., 2017; Young-Southward et al., 2020) could not be tested in this review because of the unavailability of this information in the reviewed studies.
Limitations and Future Directions
The studies reviewed present some limitations that had direct implications for this review. First, this review relied on between-group comparisons and could not provide information on causal associations between trauma and cognitive functioning because only 2 of the 13 studies reviewed included cognitive assessments before and after trauma (Cheatham et al., 2010; Font & Berger, 2015). Therefore, our findings could be explained in part by confounders, such as previous cognitive functioning, SES, or other behavior and mental health problems that were present prior to the onset of trauma (O’Higgins et al., 2017). Longitudinal studies in at-risk samples that repeatedly assess cognitive functioning are an important future line of research to clarify the temporal sequence of the proposed association and to better account for potential confounders. Second, some key information or variables were not measured or available in reviewed studies. For instance, cognitive functions other than intelligence and language were not measured; none of the reviewed studies reported the occurrence of PTSD in samples; and the chronicity of trauma was reported in only three studies. Thus, we could not test whether the impact of trauma was stronger on some cognitive functions (beyond intelligence and language), in the presence of PTSD or when trauma was chronic, as evidenced by others (Bick & Nelson, 2016; Lupien et al., 2009; Malarbi et al., 2017; Nemeroff, 2016; O’Higgins et al., 2017; Teicher et al., 2016). As such, it is essential that future longitudinal studies document various cognitive functions and assess children’s PTSD status and the chronicity of trauma to test these anticipated moderating factors and enable more complete and robust subsequent meta-analyses. In the same vein, we considered large developmental periods to test the effect of the timing of trauma because of the lack of information or inconsistencies in reporting of information on the onset and recency of trauma in the studies reviewed. Although developmental periods were large, this choice was deemed in line with the definition of complex trauma, that is exposure to repeated and multiple traumatic events, rather than a unique traumatic event at a specific point in time (Cook et al., 2003). While a post-hoc examination of narrower developmental periods highlighted that results of studies with children between the ages of 6 and 12 years at the time of assessment (Harpur et al., 2015; Noll et al., 2010; Rieder & Cicchetti, 1989; Tibu et al., 2016) did not differ from those with children between the ages of 13 and 18 years (Mills et al., 2011; Weller et al., 2015), the question merits further attention in future studies. These studies will need to document the precise age at onset of trauma and at assessment to consider narrower developmental periods and to test more reliably the respective role of the onset and recency of trauma on cognitive functioning. Alternatively, heterogeneity within subgroups of children between the ages of 6 and 18 years at the time of assessment was rather low (I2 = 46.92% and 44.34%) and non-significant (p = .17 and p = .13), suggesting that a large age range may not have induced disproportionate noise. Lastly, another limitation of the reviewed studies is that samples were not ethnically diverse (mostly Caucasians), which limits generalization of the findings to other ethnic groups, although they may be at increased risk of complex trauma (Cook et al., 2003).
The limitations of the meta-analyses themselves comprise the rather small number of studies included and the moderate to high heterogeneity in the main meta-analysis. The number of studies included in our meta-analyses was smaller than in previous meta-analyses, which is obviously due to the fact that we limited our search to longitudinal studies. This was, however, a strength and a novel aspect of this review given that longitudinal designs are ideally positioned to inform whether trauma has short- and long-term effects and whether it tends to be transient or, rather, persistent over time. Moreover, longitudinal designs help to control for unmeasured potential confounders (intra-individual perspective; Su et al., 2019). Accordingly, this review expands and complements knowledge on the association between trauma and cognitive functions. Heterogeneity among studies in the meta-analyses was diminished by using subgroups based on the onset and recency of trauma and by separating cognitive functions (intelligence and language). High heterogeneity was recurrent in previous reviews and meta-analyses (Masson et al., 2015; Su et al., 2019; Sylvestre et al., 2016), and even prevented Su et al. (2019) from including a meta-analysis in their review of longitudinal studies. We included meta-analyses despite heterogeneity to extend the literature and still provide a quantitative synthesis of the cognitive outcomes of children with complex trauma in longitudinal studies. In addition, random-effect models using the REML method were used to account for heterogeneity.
Conclusions: Practice and Policy Implications
In conclusion, this review yields two main implications for practice and policy (see Table 2 for the implications of the review for practice, policy and research). First, given the effect of the recency of trauma highlighted in this review, we suggest that interventions could be implemented rapidly following trauma to promote overall cognitive functioning. It is already well established that infancy and early childhood are sensitive periods during which the brain and cognitive functions are particularly vulnerable to the toxic stress that complex trauma represents. Conversely, these developmental epochs also open windows for interventions and resilience (Cicchetti, 2013). Even though results also indicate that effects might be transient, other long-lasting consequences may stem from the impact of trauma on cognitive functions, given that cognitive functions support learning, social interactions, as well as emotion and behavior regulation (Weissman et al., 2019). To intervene rapidly following trauma, and in line with increasingly influential trauma-informed approaches (Substance Abuse and Mental Health Services Administration, 2014), individuals in communities (e.g., neighbors) and organizations (e.g., teachers, professionals) need to recognize the signs and symptoms of trauma in children, realize the widespread impact of trauma, understand potential paths for recovery, and respond accordingly, notably by supporting resilience factors.
Table 2.
Implications of the Review for Practice, Policy and Research.
| Practice and policy implications |
| • Given the effect of the recency of trauma highlighted in this review, we suggest that interventions could be implemented rapidly following trauma to promote overall cognitive functioning. |
| • Moreover, given that, overall, children with complex trauma were found to be at risk of cognitive difficulties, all children who experienced trauma, or who are at risk of experiencing it, could be screened or fully assessed for cognitive difficulties by a clinical neuropsychologist. |
| • In addition to neuropsychological screening and/or assessment, some activities (e.g., sports, music, theatre, and arts) and enriched school curriculum that promote cognitive development could potentially be beneficial to children with complex trauma. |
| Research implications |
| • This review of longitudinal studies highlighted that there is a need for additional longitudinal studies on the cognitive outcomes of children with complex trauma (e.g., maltreated or institutionalized children). |
| • These studies will need to document the precise age at onset of trauma and at assessment to consider narrower developmental periods and to test more reliably the respective role of the onset and recency of trauma on cognitive functioning. |
| • Longitudinal studies in at-risk samples that repeatedly assess various cognitive functions are an important future line of research to clarify the temporal sequence of the proposed association between trauma and cognitive functioning, to test anticipated moderating factors (e.g., children’s PTSD status and the chronicity of trauma), and to better account for potential confounders. |
| • Neuropsychological screening, assessment and interventions supporting the optimal development of cognitive functioning among children with complex trauma should be investigated to determine whether prompt interventions lead to better cognitive functioning. |
Second, given that, overall, children with complex trauma were found to be at risk of cognitive difficulties, all children who experienced trauma, or who are at risk of experiencing it, could be screened or fully assessed for cognitive difficulties by a clinical neuropsychologist. Even though results indicate that effects of trauma on cognitive functioning might be transient, neuropsychological screening or assessment could help depicting an accurate portrait of the child’s cognitive difficulties in order to tailor interventions and the school curriculum to his needs and particular neuropsychological profile. Neuropsychological services are unfortunately rarely offered within child welfare and child protection agencies. In many jurisdictions, these agencies do not employ neuropsychologists. Consequently, when cognitive difficulties are suspected, the child is referred to a neuropsychologist practicing in another setting (e.g., psychiatric setting or private practice), and there may be a waiting period of a few months, or even years, before the child can be fully assessed for cognitive difficulties. Hopefully, growing awareness of the neurobiological and cognitive impacts of trauma will increase access to these services within these systems in the near future. In addition to neuropsychological screening and/or assessment, some activities (e.g., sports, music, theater, and arts) and enriched school curriculum that promote cognitive development (e.g., Montessori, Tools of the Mind) could potentially be beneficial to children with complex trauma to support their cognitive functioning, and, more broadly, their resilience (Center on the Developing Child at Harvard University, 2011; Diamond & Ling, 2019). The mechanisms by which these programs are expected to support cognitive functioning and resilience following trauma should, however, be the target of future investigations.
Supplemental Material
Supplemental Material for Cognitive Outcomes of Children With Complex Trauma: A Systematic Review and Meta-Analyses of Longitudinal Studies by Alexandra Matte-Landry, Marie-Ève Grisé Bolduc, Laurence Tanguay-Garneau, Delphine Collin-Vézina and Isabelle Ouellet-Morin in Trauma, Violence, & Abuse
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The first author’s work was supported by the Centre de recherche universitaire sur les jeunes et les familles of Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale and the Social Sciences and Humanities Research Council of Canada.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Alexandra Matte-Landry https://orcid.org/0000-0003-3070-321X
References
- Beckett C., Maughan B., Rutter M., Castle J., Colvert E., Groothues C., Kreppner J., Stevens S., O’Connor T. G., Sonuga-Barke E. J. S. (2006). Do the effects of early severe deprivation on cognition persist into early adolescence? Findings from the English and romanian adoptees study. Child Development, 77(3), 696–711. 10.1111/j.1467-8624.2006.00898.x [DOI] [PubMed] [Google Scholar]
- Bernard K., Frost A., Bennett C. B., Lindhiem O. (2017). Maltreatment and diurnal cortisol regulation: A meta-analysis. Psychoneuroendocrinology, 78, 57–67. 10.1016/j.psyneuen.2017.01.005 [DOI] [PubMed] [Google Scholar]
- Bick J., Nelson C. A. (2016). Early adverse experiences and the developing brain. Neuropsychopharmacology, 41(1), 177–196. 10.1038/npp.2015.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr A., Duff H., Craddock F. (2020). A systematic review of reviews of the outcome of severe neglect in underresourced childcare institutions. Trauma, Violence and Abuse, 21(3), 484–497. 10.1177/1524838018777788 [DOI] [PubMed] [Google Scholar]
- Center on the Developing Child at Harvard University (2011). Building the brain’s “air traffic control” system: How early experiences shape the development of executive function. Working paper no. 11. https://developingchild.harvard.edu/wp-content/uploads/2011/05/How-Early-Experiences-Shape-the-Development-of-Executive-Function.pdf [Google Scholar]
- Cheatham C. L., Larkina M., Bauer P. J., Toth S. L., Cicchetti D. (2010). Declarative memory in abused and neglected infants. Advances in Child Development and Behavior, 38, 161–182. 10.1016/b978-0-12-374471-5.00007-6 [DOI] [PubMed] [Google Scholar]
- Cicchetti D. (2013). Annual research review: Resilient functioning in maltreated children –past, present, and future perspectives. Journal of Child Psychology and Psychiatry, 54(4), 402–422. 10.1111/j.1469-7610.2012.02608.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Cook A., Blaustein M., Spinazzola J., van der Kolk B. (2003). Complex trauma in children and adolescents. https://www.nctsn.org/sites/default/files/resources//complex_trauma_in_children_and_adolescents.pdf [Google Scholar]
- Cowell R. A., Cicchetti D., Rogosch F. A., Toth S. L. (2015). Childhood maltreatment and its effect on neurocognitive functioning: Timing and chronicity matter. Development and Psychopathology, 27(2), 521–533. 10.1017/S0954579415000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A., Ling D. S. (2019). Review of the evidence on, and fundamental questions about, efforts to improve executive functions, including working memory. In Novick J. M., Bunting M. F., Dougherty M. R., Engle R. W. (Eds.), Cognitive and working memory training: Perspectives from psychology, neuroscience, and human development (pp. 143–431). Oxford University Press. 10.1093/oso/9780199974467.003.0008 [DOI] [Google Scholar]
- Enlow M. B., Egeland B., Blood E. A., Wright R. O., Wright R. J. (2012). Interpersonal trauma exposure and cognitive development in children to age 8 years: A longitudinal study. Journal of Epidemiology and Community Health, 66(11), 1005–1010. 10.1136/jech-2011-200727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evidence Partners . (n.d.). DistillerSR. https://www.evidencepartners.com/products/distillersr-systematic-review-software [Google Scholar]
- Fitch M. J., Cadol R. V., Goldson E., Wendell T., Swartz D., Jackson E. (1976). Cognitive development of abused and failure-to-thrive children. Journal of Pedicatric Psychology, 1(2), 32–37. https://doi.org/https://doi.org/10.1093/jpepsy/1.2.32 [Google Scholar]
- Font S. A., Berger L. M. (2015). Child maltreatment and children’s developmental trajectories in early to middle childhood. Child Development, 86(2), 536–556. 10.1111/cdev.12322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford J. D., Courtois C. A. (2013). Treating complex traumatic stress disorders in children and adolescents: Scientific foundations and therapeutic models. The Guilford Press. [Google Scholar]
- Hambrick E. P., Brawner T. W., Perry B. D. (2019). Timing of early-life stress and the development of brain-related capacities. Frontiers in Behavioral Neuroscience, 13, 183. 10.3389/fnbeh.2019.00183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpur L. J., Polek E., van Harmelen A. L. (2015). The role of timing of maltreatment and child intelligence in pathways to low symptoms of depression and anxiety in adolescence. Child Abuse & Neglect, 47, 24–37. 10.1016/j.chiabu.2015.05.019 [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Thompson S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medecine, 21(11), 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Holochwost S. J., Wang G., Kolacz J., Mills-Koonce W. R., Klika J. B., Jaffee S. R. (2020). The neurophysiological embedding of child maltreatment (pp. 1–31). Development and Psychopathology. 10.1017/S0954579420000383 [DOI] [PubMed] [Google Scholar]
- Irigaray T. Q., Pacheco J. B., Grassi-Oliveira R., Fonseca R. P., Leite J. C. C., Kristensen C. H. (2013). Child maltreatment and later cognitive functioning: A systematic review. Psicologia: Reflexão e Crítica, 26(2), 376–387. [DOI] [Google Scholar]
- Jaffee S. R., Caspi A., Moffitt T. E., Polo-Tomás M., Taylor A. (2007). Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: A cumulative stressors model. Child Abuse and Neglect, 31(3), 231–253. 10.1016/j.chiabu.2006.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanaugh B. C., Dupont-Frechette J. A., Jerskey B. A., Holler K. A. (2017). Neurocognitive deficits in children and adolescents following maltreatment: Neurodevelopmental consequences and neuropsychological implications of traumatic stress. Applied Neuropsychology: Child, 6(1), 64–78. 10.1080/21622965.2015.1079712 [DOI] [PubMed] [Google Scholar]
- Khoury J. E., Bosquet Enlow M., Plamondon A., Lyons-Ruth K. (2019). The association between adversity and hair cortisol levels in humans: A meta-analysis. Psychoneuroendocrinology, 103(2–3), 104–117. 10.1016/j.psyneuen.2019.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss K. J., Gunnar M. R. (2018). Annual research review: Early adversity, the hypothalamic–pituitary–adrenocortical axis, and child psychopathology. Journal of Child Psychology and Psychiatry, 59(4), 327–346. 10.1111/jcpp.12784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak M. D., Howieson D. B., Loring D. W., Fischer J. S. (2004). Neuropsychological assessment. Oxford University Press. [Google Scholar]
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P., Clarke M., Devereaux P. J., Kleijnen J., Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med, 6(7), Article e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien S. J., McEwen B. S., Gunnar M. R., Heim C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10(6), 434–445. 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- Malarbi S., Abu-Rayya H. M., Muscara F., Stargatt R. (2017). Neuropsychological functioning of childhood trauma and post-traumatic stress disorder: A meta-analysis. Neuroscience and Biobehavioral Reviews, 72, 68–86. 10.1016/j.neubiorev.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Manly J. T., Lynch M., Oshri A., Herzog M., Wortel S. N. (2013). The impact of neglect on initial adaptation to school. Child Maltreatment, 18(3), 155–170. 10.1177/1077559513496144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masson M., Bussières È.-L., East-Richard C., R.-Mercier A., Cellard C. (2015). Neuropsychological profile of children, adolescents and adults experiencing maltreatment: A meta-analysis. The Clinical Neuropsychologist, 29(5), 573–594. 10.1080/13854046.2015.1061057 [DOI] [PubMed] [Google Scholar]
- Matte-Landry A., Collin-Vézina D. (2020). Cognitive outcomes of children who have experienced complex trauma. JBI Evidence Synthesis, 18(3), 543–552. 10.11124/jbisrir-d-19-00036 [DOI] [PubMed] [Google Scholar]
- McLaughlin K. A., Sheridan M. A., Tibu F., Fox N. A., Zeanah C. H., Nelson C. A. (2015). Causal effects of the early caregiving environment on development of stress response systems in children. Proceedings of the National Academy of Sciences, 112(18), 5637–5642. 10.1073/pnas.1423363112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Graff L. E. (2020). The multidimensional taxonomy of individual resilience. Trauma, violence and abuse. 10.1177/1524838020967329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R., Alati R., O’Callaghan M., Najman J. M., Williams G. M., Bor W., Strathearn L. (2011). Child abuse and neglect and cognitive function at 14 years of age: Findings from a birth cohort. Pediatrics, 127(1), 4–10. 10.1542/peds.2009-3479 [DOI] [PubMed] [Google Scholar]
- Milot T., Collin-Vézina D., Godbout N. (2018). Qu’est-ce que le trauma complexe? [What is complex trauma? In Milot T., Collin-Vézina D., Godbout N. (Eds.), Trauma complexe: Comprendre, évaluer et intervenir [complex trauma: Understanding, assessment and intervention] (pp. 9–36). Presses de l’Université du Québec. [Google Scholar]
- Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetcu R., Currie M., Lisy K., Qureshi R., Mattis P., Mu P. (2017). Systematic reviews of etiology and risk. In Aromataris E., Munn Z. (Eds.), JBI manual for evidence synthesis. The Joanna Briggs Institute. https://reviewersmanual.joannabriggs.org/ [DOI] [PubMed] [Google Scholar]
- Nemeroff C. B. (2016). Paradise lost: The neurobiological and clinical consequences of child abuse and neglect. Neuron, 89(5), 892–909. 10.1016/j.neuron.2016.01.019 [DOI] [PubMed] [Google Scholar]
- Noll J. G., Shenk C. E., Yeh M. T., Ji J., Putnam F. W., Trickett P. K. (2010). Receptive language and educational attainment for sexually abused females. Pediatrics, 126(3), Artcile e615–622. 10.1542/peds.2010-0496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Higgins A., Sebba J., Gardner F. (2017). What are the factors associated with educational achievement for children in kinship or foster care: A systematic review. Children and Youth Services Review, 79, 198–220. 10.1016/j.childyouth.2017.06.004 [DOI] [Google Scholar]
- Perfect M. M., Turley M. R., Carlson J. S., Yohanna J., Saint Gilles M. P. (2016). School-related outcomes of traumatic event exposure and traumatic stress symptoms in students: A systematic review of research from 1990 to 2015. School Mental Health, 8(1), 7–43. 10.1007/s12310-016-9175-2 [DOI] [Google Scholar]
- Rauch S. L., Shin L. M., Whalen P. J., Pitman R. K. (1998). Neuroimaging and the neuroanatomy of posttraumatic stress disorder. CNS Spectrums, 3(S2), 30–41. 10.1017/S1092852900007306 [DOI] [Google Scholar]
- Rieder C., Cicchetti D. (1989). Organizational perspective on cognitive control functioning and cognitive-affective balance in maltreated children. Developmental Psychology, 25(3), 382–393. https://doi.org/https://doi.org/10.1037/0012-1649.25.3.382 [Google Scholar]
- Rutter M. (2013). Annual research review: Resilience – clinical implications. The Journal of Child Psychology and Psychiatry, 54(4), 474–487. 10.1111/j.1469-7610.2012.02615.x [DOI] [PubMed] [Google Scholar]
- Scales P. C., Roehlkepartain E. C. (2003). Boosting student achievement: New research on the power of developmental assets. Search Institute Insights & Evidence, 1(1), 1–10. [Google Scholar]
- Shonkoff J. P. (2010). Building a new biodevelopmental framework to guide the future of early childhood policy. Child Development, 81(1), 357–367. 10.1111/j.1467-8624.2009.01399.x [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke E. J. S., Kennedy M., Kumsta R., Knights N., Golm D., Rutter M., Maughan B., Schlotz W., Kreppner J. (2017). Child-to-adult neurodevelopmental and mental health trajectories after early life deprivation: The young adult follow-up of the longitudinal English and Romanian adoptees study. Lancet, 389(10078), 1539–1548. 10.1016/s0140-6736(17)30045-4 [DOI] [PubMed] [Google Scholar]
- StataCorp . (2019). Stata statistical software: Release 16. StataCorp LLC. [Google Scholar]
- Strauss E., Sherman E. M., Spreen O. (2006). A compendium of neuropsychological tests: Administration, norms, and commentary. American Chemical Society. [Google Scholar]
- Substance Abuse and Mental Health Servcies Administration . (2014). SAMHSA concept of trauma and guidance for a trauma-informed approach. http://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf [Google Scholar]
- Su Y., D’Arcy C., Yuan S., Meng X. (2019). How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. Journal of Affective Disorders, 252(suppl 2), 278–293. 10.1016/j.jad.2019.04.026 [DOI] [PubMed] [Google Scholar]
- Sylvestre A., Bussières È.-L., Bouchard C. (2016). Language problems among abused and neglected children: A meta-analytic review. Child Maltreatment, 21(1), 47–58. 10.1177/1077559515616703 [DOI] [PubMed] [Google Scholar]
- Teicher M. H., Samson J. A., Anderson C. M., Ohashi K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17(10), 652–666. 10.1038/nrn.2016.111 [DOI] [PubMed] [Google Scholar]
- Tibu F., Sheridan M. A., McLaughlin K. A., Nelson C. A., Fox N. A., Zeanah C. H. (2016). Disruptions of working memory and inhibition mediate the association between exposure to institutionalization and symptoms of attention deficit hyperactivity disorder. Psychological Medecine, 46(3), 529–541. 10.1017/S0033291715002020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veltman M. W. M., Browne K. D. (2001). Three decades of child maltreatment research: Implications for the school years. Trauma, Violence & Abuse, 2(3), 215–239. https://doi.org/https://doi.org/10.1177/1524838001002003002 [Google Scholar]
- Wechsler D. (2014). WISC-V: Wechsler intelligence scale for children (5th ed.). Pearson Education Inc., & Psychological CorporationPsychCorp. [Google Scholar]
- Weissman D. G., Bitran D., Miller A. B., Schaefer J. D., Sheridan M. A., McLaughlin K. A. (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 31(3), 899–915. 10.1017/S0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller J. A., Leve L. D., Kim H. K., Bhimji J., Fisher P. A. (2015). Plasticity of risky decision making among maltreated adolescents: Evidence from a randomized controlled trial. Development and Psychopathology, 27(2), 535–551. 10.1017/S0954579415000140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R., Hoge C. W., McFarlane A. C., Vermetten E., Lanius R. A., Nievergelt C. M., Hobfoll S. E., Koenen K. C., Neylan T. C., Hyman S. E. (2015). Post-traumatic stress disorder. Nature Reviews Disease Primers, 8(1), 15057. 10.1038/nrdp.2015.57 [DOI] [PubMed] [Google Scholar]
- Young-Southward G., Eaton C., O’Connor R., Minnis H. (2020). Investigating the causal relationship between maltreatment and cognition in children: A systematic review. Child Abuse & Neglect, 107, 104603. 10.1016/j.chiabu.2020.104603 [DOI] [PubMed] [Google Scholar]
- Yule K., Houston J., Grych J. (2019). Resilience in children exposed to violence: A meta-analysis of protective factors across ecological contexts. Clinical Child and Family Psychology Review, 22(3), 406–431. 10.1007/s10567-019-00293-1 [DOI] [PubMed] [Google Scholar]
- Zeanah C. H., Gunnar M. R., McCall R. B., Kreppner J. M., Fox N. A. (2011). Sensitive periods. Monographs of the Society for Research in Child Development, 76(4), 147–162. 10.1111/j.1540-5834.2011.00631.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Cognitive Outcomes of Children With Complex Trauma: A Systematic Review and Meta-Analyses of Longitudinal Studies by Alexandra Matte-Landry, Marie-Ève Grisé Bolduc, Laurence Tanguay-Garneau, Delphine Collin-Vézina and Isabelle Ouellet-Morin in Trauma, Violence, & Abuse