Abstract
Simple Summary
This review discusses new findings for the roles of TNFR1 and TNFR2 in the development of aggressive lung squamous cell carcinoma and lung adenocarcinoma by diverse signaling pathways in lung epithelial tumor cells and leukocytes participating in immunosuppressive tumor microenvironment generation in animal models. These defined events were consistently identified in human lung SCCs and ADCs. The components in these molecular mechanisms may be considered potential therapeutics for lung cancer.
Abstract
TNFR1 and TNFR2, encoded by TNFRSF1A and TNFRSF1B, respectively, are the most well-characterized members among the TNFR superfamily. TNFR1 is expressed in most cell types, while TNFR2 has been reported to be preferentially expressed in leukocytes. Lung cancer remains the leading cause of cancer mortality worldwide but TNFRs’ activities in lung cancer development have not been fully evaluated. Recently, overexpressed TNFR1 was reported in a large proportion of human lung squamous cell carcinomas. Increased TNFR1 coupled with increased UBCH10 caused lung SCC cell dedifferentiation with epithelial–mesenchymal transition features and the metastasis in a combined spontaneous lung SCC and TNFR1 transgenic mouse model. UBCH10, an E2 ubiquitin-conjugating enzyme that is an oncogene, increased Sox2, c-Myc, Twist1, and Bcl2 levels. Increased TNFR1 upregulated UBCH10 expression by activating c-Rel and p65 NF-κB. Lung SCC patients overexpressing TNFRSF1A and one of these target genes died early compared to lung SCC patients expressing lower levels of these genes. Recently, we also revealed that TNFR2 was required for lung adenocarcinoma progression, delivering a signaling pathway of TNF/TNFR2/NF-κB-c-Rel, in which macrophage-produced ROS and TNF converted CD4 T cells to Foxp3 Treg cells, generating an immunosuppressive tumor microenvironment and promoting lung ADC progression. In human lung ADC cohorts, TNFRSF1B expression was highly correlated with TNF, FOXP3, and CD4 expression. Of note, TNF stimulated the activities of TNFR1 and TNFR2, two membrane-binding receptors, which accelerate tumorigenesis through diverse mechanisms. This review focuses on these new findings regarding the roles of TNFR1 and TNFR2 in lung SCC and ADC development in humans and mice, and highlights the potential therapeutic targets of human lung cancers.
Keywords: TNFR1, TNFR2, NF-κB, lung squamous cell carcinoma, lung adenocarcinoma
1. Introduction
Human lung cancer is still a leading cause of cancer mortality. Non-small cell lung carcinoma (NSCLC), which represents 80–90% of human lung cancer, includes lung adenocarcinoma (ADC) (50%), squamous cell carcinoma (SCC) (35%), and large cell carcinoma (15%) [1]. Lung SCC and ADC derive from different lung epithelial cells and exhibit distinct causes, morphology, and gene expression patterns [1,2,3,4]. Approximately 30–40% of human lung ADCs contain activated KRAS mutations at its residue 12, 13, or 61 [3,4]. Activated Kras mutations or chemical urethane carcinogen mediate lung ADC and many upregulated oncogenes and loss of tumor suppressors promote Kras- or chemical carcinogen-initiated lung ADCs [2,5,6]. On the other hand, activated KRAS, HRAS, and NRAS mutations were found in very few human lung SCC cases (cBioPortal for Cancer Genomics, lung cancer cohorts). To date, three distinct mechanisms for initiating lung SCC development in mice have been reported: (1) combined p53 deletion with Lkb1 or Kmt2d deletion [7,8]; (2) combined deletion of Pten and Cdkn2ab with overexpressed Sox2 [9]; and (3) kinase-dead Ikka knock-in (KA/KA) associated with pulmonary inflammation and IKKα reduction [1]. All these lung SCC animal models require the loss of one or two tumor suppressors. Recently, we reported that overexpressed tumor necrosis factor receptor 1 (TNFR1) induced lung SCC cell dedifferentiation and metastasis to the liver in KA/KA mice [10] and that TNFR2 in CD4 T cells was required for generating an immunosuppressive tumor microenvironment (iTME) for promoting lung ADC progression in KrasG12D;Ikka∆LU mice [11].
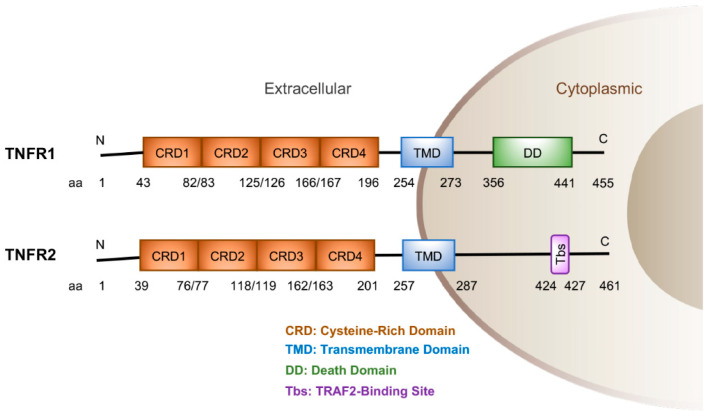
Members of the TNFR superfamily contain multiple cysteine rich domains in the N-terminal region and a transmembrane domain in the middle region (Figure 1). TNFR1, a 455-amino-acid-polypeptide, contains a death domain (DD) in its C-terminal region. TNFR2, containing 461 amino acids, does not contain this death domain, but, instead, includes a TRAF2 binding site (Tbs) at the C-terminal region. These indicate that TNFR1 and TNFR2 lead to different pathways for distinct events and activities based on specific cell types and their internal domains. TNF cytokine can stimulate TNFR1 and TNFR2 activities [10,11]. For example, TNF-activated TNFR1 induces IKK, which is composed of IKKα, IKKβ, and IKKγ, and NF-κB activation [12,13], although the individual physiological activity of these molecules in this pathway shows linear functions or diverse effects, depending on the cell types [14]. In this review, we mainly discuss the newly identified physiological roles and mechanisms of TNFR1 and TNFR2 in lung SCC and lung ADC development in humans and mice. These new findings highlight the possible therapeutic targets for lung cancer.
Figure 1.
Human TNFR1 and TNFR2 protein structures and amino acid (aa) numbers. N, N-terminal region; C, C-terminal region.
2. TNFR1 Overexpression Promotes Lung SCC Cell Dedifferentiation and Metastasis
2.1. Background
The skin, lungs, esophagus, oral cavity, and uterine tubes are protected by a stratified or pseudostratified epithelial structure that is composed of several cell layers from the undifferentiated basal cells to functionally and terminally differentiated cells that protect the organs [1,15,16]. SCC derives from the basal epithelial cells or the epithelial cells with stemness properties, which can dedifferentiate or proliferate in these organs with loss of tumor suppressors or overexpression of oncogenes. TNFR1 is ubiquitously expressed in many types of cells in the body. The roles of TNF and TNFR1 have been examined for chemical carcinogen-induced skin carcinogenesis [17,18]. The 7,12-dimethylbenz[a]anthracene (DMBA) treatment induces Hras mutations at amino acid residue 12, 13, or 61, and 12-O-tetradecanoylphorbol-13-acetate (TPA) elicits inflammation in the skin. DMBA/TPA-induced skin tumorigenesis was dampened in Tnfr1-/- or Tnf-/- mice compared to WT mice [17,18]. Double Tnfr1-/-;Tnfr2-/- mutant mice inhibited DMBA/TPA-induced skin carcinogenesis in a bacterial count-dependent manner, which required a TLR5 pathway [19]. Furthermore, TNFR1 was required for obesity-induced tumor promotion in a diethylnitrosamine (chemical carcinogen)-initiated liver carcinogenesis setting [20]. Thus, TNFRs promote carcinogen-induced skin and liver tumor development. However, the role of TNFR1 in lung cancer has not been intensively investigated yet.
2.2. TNFR1 in Human Lung SCC
Lung SCC frequently occurs in the upper and center of the lungs and derives from the basal epithelial cells that are able to proliferate or dedifferentiate. NSCLC cohorts from The Cancer Genome Atlas Program (TCGA) with increased TNF expression showed significantly reduced survival compared to NSCLC patients with reduced TNF [21]. Increased expression of TNFRSF1A was associated with a reduced trend in lung SCC patients’ survival (media, Logrank p-value = 0.08, OncoLnc). In addition, immunohistochemical (IHC) staining showed increased TNFR1 expression in a large proportion of human lung SCCs [10]. Consistently, analyses with reverse-transcription polymerase chain reaction showed increased TNFR1 mRNA in a large proportion of human lung SCCs. These data suggest that increased TNF and TNFR1 levels may facilitate lung SCC development. Thus, there is an urgent need to identify TNFR1′s targets in human lung SCCs. We then hypothesize that patients with lung SCCs expressing a combination of increased TNFRSF1A and one of its targets may show significantly reduced survival. This remains to be confirmed by animal models.
2.3. A Lung SCC Mouse Model
Tumor suppressor genes of TP53, RB1, and LKB1 are frequently mutated in human lung SCCs [3]. A single deletion of either of these tumor suppressor genes does not induce spontaneous lung SCC in mice, but mice lacking double Lkb1 and p53 develop spontaneous lung SCCs or mixed SCCs and ADCs [7]. Of note, we previously reported that KA/KA mice, which express a mutated IKKα protein containing a single mutation at amino acid 44, an ATP binding site, with a replacement of an alanine (A) residue from a lysine (K), developed spontaneous lung SCCs. This KA/KA mutation destabilized IKKα proteins in the lung epithelial cells with increased ages and was associated with increased macrophage infiltration in mice, which contributed to spontaneous lung SCC development in KA/KA mice [1]. Reintroducing transgenic IKKα, in which an IKKα cDNA is controlled by a keratin 5 (K5) promoter, or depleting macrophages, diminished lung SCC development [1]. The lung SCCs derived from KA/KA mice exhibited the classical SCC features with keratin pearls and increased K5, p63, and Ki67 positive cells, and expressed reduced p53, Rb, and LKB1 tumor suppressors but elevated EGFR activity, ERK activity, c-Myc, Trim29, Rhov, Nanog, and ROS1 levels [1]. In addition, the pulmonary infiltrating macrophages within KA/KA lung SCCs expressed increased inducible nitric oxide synthase (iNOS), which is encoded by Nos2, and many cytokines including IL-3, IL-21, IL-22, and IL-24 [22,23]. KA/KA;Nos2-/- mice inhibited lung SCC development. Transfer with KA/KA and KA/KA;Nos2-/- bone marrow (BM) to irradiated wild-type (WT), KA/KA, or KA/KA;Nos2-/- mice demonstrated that iNOS in tumor cells and macrophages contributes to lung SCC development. iNOS levels are very low in normal cells. TNF is a strong inducer of iNOS expression [22], which provides a connection between iNOS and TNF/TNFRs in tumorigenesis.
2.4. TNFR1 Induction in Lung SCC Development in Human and Mice
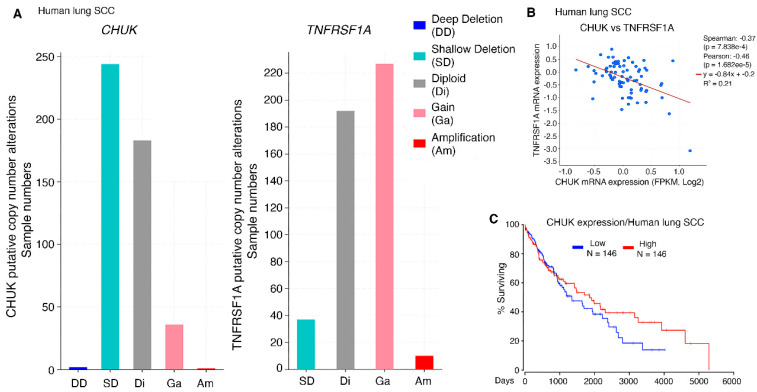
Increased TNFR1 protein and mRNA levels were detected in KA/KA lung SCCs that express reduced IKKα [10]. Although the mutation rate of CHUK in human lung SCC was low [3], its expression levels were reduced in a large proportion of human lung SCCs, which were reciprocal to TNFRSF1A expression patterns in human lung SCCs (Figure 2A). Indeed, the expression levels of CHUK and TNFRSF1A were totally opposite in human lung SCCs (Figure 2B). Again, high IKKα levels were correlated with an increased survival for lung SCC patients (Figure 2C). Downregulation of IKKα in human cancers is associated with the DNA methylation of the CHUK gene [24]. In addition, treatment with TNF cytokine downregulates IKKα levels in human SCC cell lines [16]. These suggest that multiple pathways determine IKKα expression and stability. Together, this KA/KA animal lung SCC model represents a relevant human lung cancer setting and the findings from these studies will provide therapeutic value.
Figure 2.
TNFRSF1A and CHUK correlations in human lung SCCs (cBioPortal, TCGA, PanCancer Atlas). (A). Distributions of CHUK (left) and TNFRSF1A (right) expression alterations in human lung SCC numbers. (B). Correlation of TNFRSF1A and CHUK expression in human lung SCCs (cBioPortal, CPTAC, Cell 2021). (C). Survival rate of human lung SCC patients with the top 30% and the bottom 30% of CHUK expression levels (OncoLnc), Logrank p-value = 0.3.
2.5. Increased TNFR1 in Lung SCC Cells Drives Cancer Stemness, Dedifferentiation, and Metastasis
IHC detected significantly increased TNFR1 in human lung SCC cells, suggesting an intrinsic activity of TNFR1 in lung SCC cells. To determine an overexpressed TNFR1′s role, we generated a transgenic mouse strain overexpressing Tg-K5.TNFR1, in which TNFR1 cDNA is controlled by a K5 promoter [10,25]. The lungs of Tg-K5.TNFR1 young mice are comparable to those of WT mice, but the lungs of the transgenic mice at 10 months of age show minor increased epithelial proliferation with slightly inflammatory cell infiltration. Furthermore, lung SCCs were detected in three-month-old K5.TNFR1;KA/KA mice, while 5–10-month-old KA/KA mice start to show lung SCCs, suggesting that overexpressed TNFR1 promoted lung SCC initiation. In addition, K5.TNFR1;KA/KA lung SCCs display dedifferentiated features and metastasize to the liver [10], suggesting that TNFR1 promotes lung SCC initiation, dedifferentiation, and metastasis.
To determine the mechanism by which intrinsic TNFR1 modulates tumor cell fates, we used Scal1 and CD24 stem cell markers to isolate KALLU+ lung SCC cells with high stemness (Scal1highCD24low) features and KALLU- cells with low stemness (Scal1lowCD24high) features from a previously reported parental KALLU lung SCC cell line derived from KA/KA lung SCCs [1,10]. Importantly, Scal1highCD24lowKALLU+ cells highly expressed TNFR1 and Sox2 compared to Scal1lowCD24highKALLU- cells [10]. Silencing TNFR1 downregulated Sox2 levels in KALLU+ cells. Sox2, a stem cell marker, is highly expressed in human lung SCCs [26]. Thus, TNFR1 levels are associated with cancer stemness potential. Consistently, the lung tumor burdens were significantly higher when induced by the KALLU+ cells via tail vein injection than by the KALLU- cells in WT and KA/KA mice, and KALLU+ cancers, but not KALLU- cancers, metastasized to the liver [10]. KALLU+ cell-derived lung spindle cell carcinomas, a final stage of SCCs, showed dedifferentiated and epithelial–mesenchymal transition (EMT) features with E-cadherin loss and K5 expression reduction [10,27]. KALLU- cell–derived well-differentiated lung SCCs expressed high levels of K5 and low levels of involucrin, an intermediate differentiation marker. Silencing TNFR1 in KALLU+ cells reduced the cell-derived tumor burdens and converted the spindle cell carcinomas to well-differentiated SCCs [10]. These results suggest that a high TNFR1 level drives dedifferentiation and metastasis of SCC cells. Interestingly, human and mouse lung SCCs contain full-length and cleaved TNFR1 proteins [10]. Cell-surface membrane-binding and Golgi-associated TNFR1s exist in cells [28,29]. The functions of these different forms of TNFR1 in tumorigenesis remain to be revealed.
While working to elucidate the molecular bases for the different oncogenic activities in KALLU+ and KALLU- cells, we identified higher levels of Sox2, c-Myc, Twist1, Bcl2, and UBCH10 in KALLU+ cells than in KALLU- cells. Silencing TNFR1 in KALLU+ cells downregulated the levels of these proteins. UBCH10, an E2 ubiquitin-conjugating enzyme, which is encoded by UBE2C, is an oncogene. Its targets include Sox2, c-Myc, Twist1, and Bcl2. Overexpressed UBCH10 causes chromosome missegregation and results in multiple types of spontaneous tumors [30,31,32,33]. Of note, TNF treatment of KALLU+ cells elevated UBCH10 and downregulated E-cadherin and K5 levels, whereas, knocking down UBCH10 elevated K5 and E-cadherin levels, indicating that TNF/TNFR1 and UBCH10 lead a program that switches differentiation and dedifferentiation or EMT of SCC cells, which determines a tumor’s regression or progression. Indeed, silencing TNF impaired KALLU+ cell–derived lung tumor development. Importantly, patients with lung SCCs expressing increased TNFRSF1A with TWIST1 or UBE2C died much earlier than lung SCC patients expressing low levels of these genes [10]. Thus, these molecular alterations are relevant to human cancer development.
Consistently, we used the same methods to isolate cancer stem cells from human H520 SCC cells with CD24 and CD44 markers [10]. TNFR1 expression levels were higher in CD24lowCD44+H520 cells than in CD24highCD44+H520 cells [10]. Subcutaneously injected CD24lowCD44+H520 cells developed tumors at the injection location and metastasis to the lungs but CD24highCD44+H520 cells did not develop tumors in these mice. These results indicate that TNFR1 shows similar activities in human and mouse lung SCCs.
2.6. TNFR1 Levels Correlate with Induced NF-κB Activity That is Required for UBE2C/Ube2c Promoter Activity
Previously, we reported that the CD45-CD31- lung epithelial cells isolated from KA/KA mice showed increased NF-κB activity compared to lung epithelial cells isolated from WT mice and that elevated NF-κB activity was correlated with decreased IKKα levels due to this KA/KA mutation that destabilizes IKKα proteins in KA/KA lung epithelial cells [1]. In addition, TNF treatment induced higher levels of nuclear p65 and p50 in parental KALLU cells than in M2C cells that are mouse transformed lung epithelial cells. Furthermore, the induced nuclear c-Rel, p65, and p50 NF-κB levels were higher in KALLU+ stem cells expressing high TNFR1 levels than in KALLU- cells expressing low TNFR1 levels. Research has noted that TNF promotes a cancer stem-like cell property [34]. Thus, TNFR1 levels correlate with increased NF-κB activities in response to cytokine stimulation and elevate cancer stem-like cell properties.
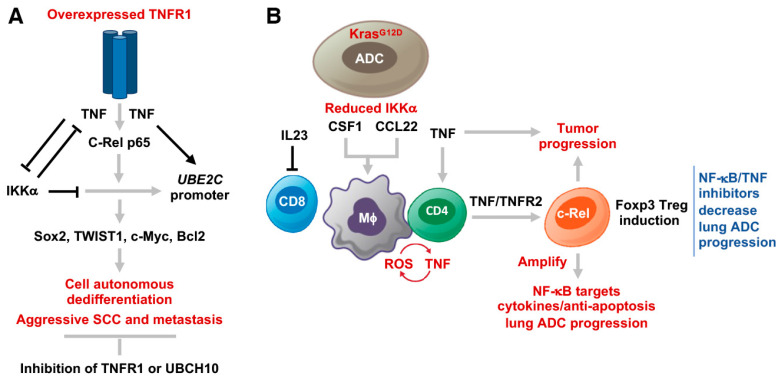
The c-Rel DNA-binding motifs are found in the promoter region of Ube2c/UBE2C [10,35]. The p65 and c-Rel enrichments were found with the Ube2c/UBE2C gene in mouse KALLU+ and human SW900 SCC cells, which were associated with increased H3K27ac, an activated transcriptional marker [10]. TNF treatment, indeed, increased the levels of NF-κB enrichment on the Ubec2c promoter. Interestingly, the IKKα enrichment also formed the complex with the Ube2c promoter, but TNF treatment reduced levels of the IKKα enrichment. The enrichment levels of NF-κB and IKKα were reciprocal. Consistently, IKKα repressed UBCH10 protein and mRNA levels in KALLU+ cells, although IKKα did not significantly repress TNFR1 levels. Overexpressed IKKα repressed KALLU+ cell–derived tumor burdens in mice [10]. Clearly, in this case, increased NF-κB activity was correlated with high TNFR1 levels in KALLU+ cells compared to KALLU- cells after TNF treatment, whereas IKKα inhibited tumorigenesis through repressing downstream targets of overexpressed TNFR1 (Figure 4A). Overall, TNF/TNFR1/NF-κB regulated UBCH10, which further mediated TWIST1, Sox2, and Bcl2 levels, contributing to SCC dedifferentiation, EMT, and metastasis (Figure 4A). In addition, patients with lung SCCs expressing high levels of TNFRSF1A and REL died earlier than patients with lung SCC expressing low levels of these genes [10]. Intriguingly, a report showed that transgenic Tg-K5.mIκBα mice, in which a mutated IκBα at its serine residues 32 and 36 is controlled by the K5 promoter, developed severe skin hyperplasia and inflammation [36]. The skin phenotype was rescued by Tnfr1 deletion in Tg-K5.mIκBα;Tnfr1-/- mice [37]. Furthermore, our unpublished data suggest that this mIκBα, an un-degraded form, may interact with IKKα, impairing normal IKKα activity in the skin cells [14,15,38,39], which may contribute to the skin phenotypes in K5.mIκBα mice.
3. Role of TNFR2 in Lung Adenocarcinoma Progression
3.1. Background
Lung ADC, a major type of human lung cancer, derives from lung type II alveolar epithelial cells [2]. TCGA human cancer database analysis revealed that increased TNFRSF1A is correlated with significantly reduced survival of lung ADC patients [21]. TNFR1 is an upstream regulator of NF-κB. Increased NF-κB activity promotes KrasG12D-initiated lung ADC development with accelerating p53 loss [40]. In contrast, treatment with a NF-κB inhibitors (bortezomib and bay-117082) repressed lung ADC development [41]. TNFR1, as an upstream transducer of NF-κB, may use the NF-κB pathway to promote lung ADC development. The internal domains of TNFR1 and TNFR2 are different at their C-terminal regions (Figure 1). Through the DD, TNFR1 stimulation at the plasma membrane forms complex I or complex II, which leads to diverse consequences. Complex I, containing TNFR1, TRADD, RIP1, TRAF2, and cIAP1, activates NF-κB and promotes cell survival. Complex II further recruits TRADD and RIP1 associated with FADD and caspase-8, resulting in cell death [42,43]. These suggest that TNF/TNFR1/NF-κB is sufficient to promote lung ADC as well as SCC development. Consistently, our unpublished data detected increased cIAP1 levels in some human lung SCCs. Because complex I and complex II lead to opposite results, it will be important to test whether alterations in components of TNFR1 complex I and TNFR II may change lung cancer fates in the future [42,43]. If so, the findings will provide new insight into lung cancer therapy. Indeed, patients with lung ADCs overexpressing TNFRSF1A died earlier than lung ADC patients expressing low TNFRSF1A levels [21].
TNFR2 shows the cell-type specific activities, such as those leukocytes, compared to TNFR1. Tnfr2-/- mice have a defect in Foxp3+ Treg cell development [44]. Foxp3, a transcriptional factor, is a crucial regulator for Treg cell induction [45]. There are three highly conserved noncoding sequences (CNS), CNS1 to CNS3, in the Foxp3 locus, which are required for Foxp3 expression [45]. NF-κB c-Rel binds to CNS3 to induce Foxp3 expression [45]. Mice with a deletion of Nfkb p65 or c-Rel in Foxp3+ cells show a defect in Treg cell induction, resulting in autoimmune diseases [46,47]. Increased NF-κB-induced Treg cell numbers generate an iTME for tumor promotion. Foxp3+ Treg cells suppressed antitumor T-cell responses, facilitating KrasG12D-mediated lung ADC development [48]. Thus, we examined whether TNFR2 in CD4 T cells via NF-κB is required for Treg induction to generate the iTME for lung ADC progression [11].
3.2. TNFR2 in CD4 T Cells Is Required for Generating an iTME with Increased Treg Numbers
Approximately 35–40% of human lung ADCs contain activated mutations at KRAS residue 12, 13, or 61 [4] (human lung ADC cohorts, cBioPortal for Cancer Genomics). KrasG12D is a lung ADC driver in mice [6]. Ikka deletion or reduction in lung cells with activated KrasG12D promoted KrasG12D-mediated ADC progression in Ikka∆LU;KrasG12D and Ikka∆LU/+;KrasG12D mice compared to KrasG12D mice [2]. Consistently, Ikka deletion in type II alveolar epithelial cells in the lungs, which was mediated by a pulmonary-associated surfactant protein C Cre, promoted urethane-induced lung ADC [5]. In the two models, although Ikka was ablated, NF-κB activity was not impaired in lung ADC epithelial cells.
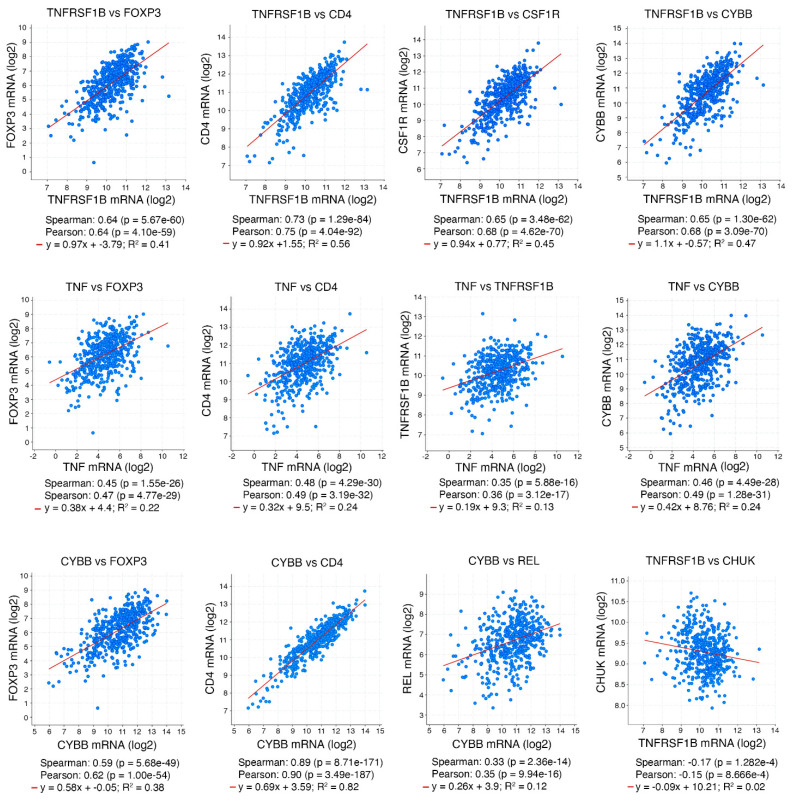
TME regulates tumorigenesis. We detected a correlated increase in numbers of macrophages and Foxp3+ Treg cells in Ikka∆LU;KrasG12D ADCs that were associated with increased tumor burdens and reduced CD8 cell numbers compared to KrasG12D ADCs [11]. Macrophage-produced reactive oxygen species (ROS) are required for Treg cell induction [11]. Depleting macrophages decreased Treg cell numbers and inhibited lung ADC development, and depleting Treg cells indeed dampened lung ADC development in Ikka∆LU;KrasG12D mice, indicating that increased Treg cell number is a mechanism for ADC progression. Furthermore, macrophage-produced ROS and TNF stimulated TNFR2 and NF-κB activation in CD4 T cells, which converted CD4 T cells to Treg cells. Inhibition of NF-κB c-Rel decreased Treg cell induction in vivo and reduced lung tumorigenesis. In addition, Ikka∆LU;Tnfrsf1b-/-;KrasG12D mice reduced lung ADC burdens with reduced Treg cell numbers compared to Ikka∆LU;KrasG12D mice. Intratracheal injection of a lung ADC cell line to Tnf-/- mice showed reduced lung ADC burdens, which were associated with decreased Treg cell induction, compared to WT mice [11], confirming that TNF/TNFR2/NF-κB is required for Treg cell induction in TME. Interestingly, the co-culture of WT macrophage and Tnfrsf1b-/- CD4 T cells treated with TNF showed a partial reduction in Treg cell numbers compared to WT CD4 T cells in the co-culture, suggesting that TNFR1 may contribute to Treg induction in the absence of TNFR2 [11]. Because macrophage-ROS and TNF/TNFR2/NF-κB play a role that affects Treg cell induction associated with ADC burdens in Ikka∆LU;KrasG12D mice, we further analyzed the expression of the associated genes to determine the relevance of this pathway in human lung ADC cohorts (cBioPortal for Cancer Genomics). Patients with lung ADCs expressing reduced CHUK and increased TNFRSF1B died earlier than lung ADC patients expressing increased CHUK and decreased TNFRSF1B [11]. Furthermore, human lung ADC cohorts showed that TNFRSF1B expression levels were highly correlated with FOXP3, CD4, CSF1R, and CYBB expression; that TNF expression levels were highly correlated with FOXP3, CD4, TNFSF1B, and CYBB expression; and that CYBB expression levels were highly correlated with FOXP3, CD4, and REL expression (Figure 3). On the other hand, TNFRSF1B expression levels were opposite to CHUK expression levels (cBioPortal for Cancer Genomics). Reintroduction of IKKα repressed lung tumorigenesis in this animal system and IKKα reduction upregulated the expression of TNF, CSF1, CCL22, and IL-23A. CSF1 and CCL22 recruited macrophages and IL-23A blocked CD8 T-cell infiltration [49]. Thus, the increased cytokines generated a milieu to facilitate the development of an iTME. The tight correlation between the ROS/TNF/TNFR2/NF-κB pathway and Treg cell induction in human and mouse lung ADCs indicates the medical significance of this finding.
Figure 3.
Expression correlations of genes related to FOXP3 Treg cell induction in human lung ADCs (cBioPortal for Cancer Genomics, TCGA, PanCancer Atlas).
4. Conclusions and Therapeutic Perspective
Overall, TNFR1 and TNFR2 have been demonstrated to promote aggressive lung SCC development and metastasis and accelerate lung ADC progression through distinct mechanisms in different mouse models (Figure 4A,B). In addition, Ikka ablation is a cancer driver in these lung cancer animal models, and reintroduction of IKKα inhibited the ADC and SCC development. Although IKKα does not directly regulate TNFR1 or TNFR2 expression, we found that IKKα inhibited the expression of the targets of TNFR1 and TNFR2 in carcinogenesis. However, a puzzling relationship between IKKα and IKK activity as downstream targets of TNFRs in carcinogenesis remains to be investigated in the future.
Figure 4.
(A) and (B) The mechanisms of TNFR1 and TNFR2 in the promotion of lung SCC metastasis and lung ADC progression.
Several literature reviews have discussed the multiple mechanisms by which TNF and TNFRs regulate immune responses and lung cancer development [50,51]. Of note, TNF has been suggested to inhibit tumor development, but phase I and phase II clinical trials for treating cancer patients with TNF were not successful [52,53,54]. Here, our studies provided new insights into the roles of TNF, TNFR1, and TNFR2 in promoting lung cancer development, including the following: (1) Tnfr1 deletion prevented lung SCC development in KA/KA;Tnfr1-/- mice compared to KA/KA mice; (2) silencing TNFR1 in KALLU+ lung SCC cells reduced stemness and Bcl2 anti-apoptotic protein levels but increased differentiation markers and E-cadherin that is expressed on the surface of well-differentiated SCC compared to parental KALLU+ cells, and TNF regulated the differentiation and EMT markers in SCC cells [10,55]; (3) KALLU+ cells expressing downregulated TNFR1 inhibited lung SCC burdens and blocked the SCC transition from well-differentiated lung SCCs to spindle cell carcinomas, a final stage of SCC, and metastasis compared to the parental KALLU+ cell-induced lung tumors in WT and KA/KA mice; (4) silencing TNF in KALLU+ cells inhibited lung tumor development compared to parental KALLU+ cells in WT and KA/KA mice; (5) the numbers of tumor infiltrating Treg cells and lung ADC burdens were reduced in Tnfr2-/-;KrasG12D;Ikka∆LU mice compared to KrasG12D;Ikka∆LU mice; and (6) the lung ADC burden induced by injected lung ADC cells and tumor infiltrating Treg numbers were significantly lower in Tnf-/- mice than in WT mice [10,11]. These findings suggest that TNF, TNFR1, and TNFR2 regulate intratumoral oncogenic pathways and modulate TME. Thus, these molecules may be considered to be potential therapeutic targets. To date, the commercial antibodies, antagonists, and small-molecule inhibitors against TNF, TNFR, TNFR1, and TNFR2 have been successfully used to treat several human autoimmune diseases, such as rheumatoid arthritis, inflammatory bowel disease, and psoriasis [56,57,58,59,60]. Taken together, to increase the efficacy of anti-tumor treatment with anti-TNFR-related reagents, it may be important to examine the alterations in TNFR1, TNFR2, and TNF levels and Treg cell numbers in human lung tumors. Then, the anti-TNFR1/TNF or anti-TNFR2/TNF therapeutic approach could be used to treat those selected patients with lung cancers expressing the relevant markers.
Acknowledgments
This research was funded by National Cancer Institute (ZIA BC011212 and ZIABC011212) to Y.H.
Author Contributions
Conceptualization, G.S. and Y.H.; software, G.S.; writing—original draft preparation, G.S. and Y.H.; writing—review and editing, G.S. and Y.H.; funding acquisition, Y.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by National Cancer Institute (ZIA BC011212 and ZIA BC011212) to Y.H. This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Xiao Z., Jiang Q., Willette-Brown J., Xi S., Zhu F., Burkett S., Back T., Song N.Y., Datla M., Sun Z., et al. The Pivotal Role of IKKalpha in the Development of Spontaneous Lung Squamous Cell Carcinomas. Cancer Cell. 2013;23:527–540. doi: 10.1016/j.ccr.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song N.Y., Zhu F., Wang Z., Willette-Brown J., Xi S., Sun Z., Su L., Wu X., Ma B., Nussinov R., et al. IKKalpha inactivation promotes Kras-initiated lung adenocarcinoma development through disrupting major redox regulatory pathways. Proc. Natl. Acad. Sci. USA. 2018;115:E812–E821. doi: 10.1073/pnas.1717520115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammerman P.S., Hayes D.N., Wilkerson M.D., Schultz N., Bose R., Chu A., Collisson E.A., Cope L., Creighton C.J., Getz G., et al. Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489:519–525. doi: 10.1038/nature11404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cancer Genome Atlas Research N. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–550. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chavdoula E., Habiel D.M., Roupakia E., Markopoulos G.S., Vasilaki E., Kokkalis A., Polyzos A.P., Boleti H., Thanos D., Klinakis A., et al. CHUK/IKK-alpha loss in lung epithelial cells enhances NSCLC growth associated with HIF up-regulation. Life Sci. Alliance. 2019;2:e201900460. doi: 10.26508/lsa.201900460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DuPage M., Dooley A.L., Jacks T. Conditional mouse lung cancer models using adenoviral or lentiviral delivery of Cre recombinase. Nat. Protoc. 2009;4:1064–1072. doi: 10.1038/nprot.2009.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ji H., Ramsey M.R., Hayes D.N., Fan C., McNamara K., Kozlowski P., Torrice C., Wu M.C., Shimamura T., Perera S.A., et al. LKB1 modulates lung cancer differentiation and metastasis. Nature. 2007;448:807–810. doi: 10.1038/nature06030. [DOI] [PubMed] [Google Scholar]
- 8.Pan Y., Han H., Hu H., Wang H., Song Y., Hao Y., Tong X., Patel A.S., Misirlioglu S., Tang S., et al. KMT2D deficiency drives lung squamous cell carcinoma and hypersensitivity to RTK-RAS inhibition. Cancer Cell. 2023;41:88–105.e108. doi: 10.1016/j.ccell.2022.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferone G., Song J.Y., Sutherland K.D., Bhaskaran R., Monkhorst K., Lambooij J.P., Proost N., Gargiulo G., Berns A. SOX2 Is the Determining Oncogenic Switch in Promoting Lung Squamous Cell Carcinoma from Different Cells of Origin. Cancer Cell. 2016;30:519–532. doi: 10.1016/j.ccell.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao Z., Shi G., Xi S., Singh A.K., Willette-Brown J., Li X., Zhu F., Su L., Wu X., Schrump D.S., et al. A TNFR1-UBCH10 axis drives lung squamous cell carcinoma dedifferentiation and metastasis through a cell-autonomous signaling loop. Cell Death Dis. 2022;13:885. doi: 10.1038/s41419-022-05308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song N.Y., Li X., Ma B., Willette-Brown J., Zhu F., Jiang C., Su L., Shetty J., Zhao Y., Shi G., et al. IKKalpha-deficient lung adenocarcinomas generate an immunosuppressive microenvironment by overproducing Treg-inducing cytokines. Proc. Natl. Acad. Sci. USA. 2022;119:e2120956119. doi: 10.1073/pnas.2120956119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z.W., Chu W., Hu Y., Delhase M., Deerinck T., Ellisman M., Johnson R., Karin M. The IKKb subunit of IkB kinase (IKK) is essential for nuclear factor kB activation and prevention of apoptosis. J. Exp. Med. 1999;189:1839–1845. doi: 10.1084/jem.189.11.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu Y., Baud V., Oga T., Kim K.I., Yoshida K., Karin M. IKKa controls formation of the epidermis independently of NF-kB. Nature. 2001;410:710–714. doi: 10.1038/35070605. [DOI] [PubMed] [Google Scholar]
- 14.Li X., Hu Y. Attribution of NF-kappaB Activity to CHUK/IKKalpha-Involved Carcinogenesis. Cancers. 2021;13:1411. doi: 10.3390/cancers13061411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu B., Xia X., Zhu F., Park E., Carbajal S., Kiguchi K., DiGiovanni J., Fischer S.M., Hu Y. IKKalpha is required to maintain skin homeostasis and prevent skin cancer. Cancer Cell. 2008;14:212–225. doi: 10.1016/j.ccr.2008.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu F., Willette-Brown J., Song N.Y., Lomada D., Song Y., Xue L., Gray Z., Zhao Z., Davis S.R., Sun Z., et al. Autoreactive T Cells and Chronic Fungal Infection Drive Esophageal Carcinogenesis. Cell Host Microbe. 2017;21:478–493.e477. doi: 10.1016/j.chom.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suganuma M., Okabe S., Marino M.W., Sakai A., Sueoka E., Fujiki H. Essential role of tumor necrosis factor alpha (TNF-alpha) in tumor promotion as revealed by TNF-alpha-deficient mice. Cancer Res. 1999;59:4516–4518. [PubMed] [Google Scholar]
- 18.Moore R.J., Owens D.M., Stamp G., Arnott C., Burke F., East N., Holdsworth H., Turner L., Rollins B., Pasparakis M., et al. Mice deficient in tumor necrosis factor-alpha are resistant to skin carcinogenesis. Nat. Med. 1999;5:828–831. doi: 10.1038/10552. [DOI] [PubMed] [Google Scholar]
- 19.Hoste E., Arwert E.N., Lal R., South A.P., Salas-Alanis J.C., Murrell D.F., Donati G., Watt F.M. Innate sensing of microbial products promotes wound-induced skin cancer. Nat. Commun. 2015;6:5932. doi: 10.1038/ncomms6932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park E.J., Lee J.H., Yu G.Y., He G., Ali S.R., Holzer R.G., Osterreicher C.H., Takahashi H., Karin M. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell. 2010;140:197–208. doi: 10.1016/j.cell.2009.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gong K., Guo G., Beckley N., Zhang Y., Yang X., Sharma M., Habib A.A. Tumor necrosis factor in lung cancer: Complex roles in biology and resistance to treatment. Neoplasia. 2021;23:189–196. doi: 10.1016/j.neo.2020.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang X., Gray Z., Willette-Brown J., Zhu F., Shi G., Jiang Q., Song N.Y., Dong L., Hu Y. Macrophage inducible nitric oxide synthase circulates inflammation and promotes lung carcinogenesis. Cell Death Discov. 2018;4:46. doi: 10.1038/s41420-018-0046-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gray Z., Shi G., Wang X., Hu Y. Macrophage inducible nitric oxide synthase promotes the initiation of lung squamous cell carcinoma by maintaining circulated inflammation. Cell Death Dis. 2018;9:642. doi: 10.1038/s41419-018-0653-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maeda G., Chiba T., Kawashiri S., Satoh T., Imai K. Epigenetic inactivation of IkappaB Kinase-alpha in oral carcinomas and tumor progression. Clin. Cancer Res. 2007;13:5041–5047. doi: 10.1158/1078-0432.CCR-07-0463. [DOI] [PubMed] [Google Scholar]
- 25.Xia X., Park E., Liu B., Willette-Brown J., Gong W., Wang J., Mitchell D., Fischer S.M., Hu Y. Reduction of IKKalpha expression promotes chronic ultraviolet B exposure-induced skin inflammation and carcinogenesis. Am. J. Pathol. 2010;176:2500–2508. doi: 10.2353/ajpath.2010.091041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bass A.J., Watanabe H., Mermel C.H., Yu S., Perner S., Verhaak R.G., Kim S.Y., Wardwell L., Tamayo P., Gat-Viks I., et al. SOX2 is an amplified lineage-survival oncogene in lung and esophageal squamous cell carcinomas. Nat. Genet. 2009;41:1238–1242. doi: 10.1038/ng.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang H., Unternaehrer J.J. Epithelial-mesenchymal Transition and Cancer Stem Cells: At the Crossroads of Differentiation and Dedifferentiation. Dev. Dyn. 2019;248:10–20. doi: 10.1002/dvdy.24678. [DOI] [PubMed] [Google Scholar]
- 28.Lobito A.A., Kimberley F.C., Muppidi J.R., Komarow H., Jackson A.J., Hull K.M., Kastner D.L., Screaton G.R., Siegel R.M. Abnormal disulfide-linked oligomerization results in ER retention and altered signaling by TNFR1 mutants in TNFR1-associated periodic fever syndrome (TRAPS) Blood. 2006;108:1320–1327. doi: 10.1182/blood-2005-11-006783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karathanasis C., Medler J., Fricke F., Smith S., Malkusch S., Widera D., Fulda S., Wajant H., van Wijk S.J.L., Dikic I., et al. Single-molecule imaging reveals the oligomeric state of functional TNFalpha-induced plasma membrane TNFR1 clusters in cells. Sci. Signal. 2020;13:eaax5647. doi: 10.1126/scisignal.aax5647. [DOI] [PubMed] [Google Scholar]
- 30.van Ree J.H., Jeganathan K.B., Malureanu L., van Deursen J.M. Overexpression of the E2 ubiquitin-conjugating enzyme UbcH10 causes chromosome missegregation and tumor formation. J. Cell Biol. 2010;188:83–100. doi: 10.1083/jcb.200906147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hao Z., Zhang H., Cowell J. Ubiquitin-conjugating enzyme UBE2C: Molecular biology, role in tumorigenesis, and potential as a biomarker. Tumour Biol. 2012;33:723–730. doi: 10.1007/s13277-011-0291-1. [DOI] [PubMed] [Google Scholar]
- 32.Wang X., Yin L., Yang L., Zheng Y., Liu S., Yang J., Cui H., Wang H. Silencing ubiquitin-conjugating enzyme 2C inhibits proliferation and epithelial-mesenchymal transition in pancreatic ductal adenocarcinoma. FEBS J. 2019;286:4889–4909. doi: 10.1111/febs.15134. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y., Zhao R., Chi S., Zhang W., Xiao C., Zhou X., Zhao Y., Wang H. UBE2C Is Upregulated by Estrogen and Promotes Epithelial-Mesenchymal Transition via p53 in Endometrial Cancer. Mol. Cancer Res. 2020;18:204–215. doi: 10.1158/1541-7786.MCR-19-0561. [DOI] [PubMed] [Google Scholar]
- 34.Liu W., Lu X., Shi P., Yang G., Zhou Z., Li W., Mao X., Jiang D., Chen C. TNF-alpha increases breast cancer stem-like cells through up-regulating TAZ expression via the non-canonical NF-kappaB pathway. Sci. Rep. 2020;10:1804. doi: 10.1038/s41598-020-58642-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kunsch C., Ruben S.M., Rosen C.A. Selection of optimal kappa B/Rel DNA-binding motifs: Interaction of both subunits of NF-kappa B with DNA is required for transcriptional activation. Mol. Cell Biol. 1992;12:4412–4421. doi: 10.1128/MCB.12.10.4412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Hogerlinden M., Rozell B.L., Ahrlund-Richter L., Toftgard R. Squamous cell carcinomas and increased apoptosis in skin with inhibited Rel/nuclear factor-kB signaling. Cancer Res. 1999;59:3299–3303. [PubMed] [Google Scholar]
- 37.Lind M.H., Rozell B., Wallin R.P., van Hogerlinden M., Ljunggren H.G., Toftgard R., Sur I. Tumor necrosis factor receptor 1-mediated signaling is required for skin cancer development induced by NF-kappaB inhibition. Proc. Natl. Acad. Sci. USA. 2004;101:4972–4977. doi: 10.1073/pnas.0307106101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park E., Zhu F., Liu B., Xia X., Shen J., Bustos T., Fischer S.M., Hu Y. Reduction in IkappaB kinase alpha expression promotes the development of skin papillomas and carcinomas. Cancer Res. 2007;67:9158–9168. doi: 10.1158/0008-5472.CAN-07-0590. [DOI] [PubMed] [Google Scholar]
- 39.Liu B., Park E., Zhu F., Bustos T., Liu J., Shen J., Fischer S.M., Hu Y. A critical role for I{kappa}B kinase {alpha} in the development of human and mouse squamous cell carcinomas. Proc. Natl. Acad. Sci. USA. 2006;103:17202–17207. doi: 10.1073/pnas.0604481103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meylan E., Dooley A.L., Feldser D.M., Shen L., Turk E., Ouyang C., Jacks T. Requirement for NF-kappaB signalling in a mouse model of lung adenocarcinoma. Nature. 2009;462:104–107. doi: 10.1038/nature08462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xue W., Meylan E., Oliver T.G., Feldser D.M., Winslow M.M., Bronson R., Jacks T. Response and resistance to NF-kappaB inhibitors in mouse models of lung adenocarcinoma. Cancer Discov. 2011;1:236–247. doi: 10.1158/2159-8290.CD-11-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Micheau O., Tschopp J. Induction of TNF receptor I-mediated apoptosis via two sequential signaling complexes. Cell. 2003;114:181–190. doi: 10.1016/S0092-8674(03)00521-X. [DOI] [PubMed] [Google Scholar]
- 43.Muppidi J.R., Tschopp J., Siegel R.M. Life and death decisions: Secondary complexes and lipid rafts in TNF receptor family signal transduction. Immunity. 2004;21:461–465. doi: 10.1016/j.immuni.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 44.Chen X., Wu X., Zhou Q., Howard O.M., Netea M.G., Oppenheim J.J. TNFR2 is critical for the stabilization of the CD4+Foxp3+ regulatory T. cell phenotype in the inflammatory environment. J. Immunol. 2013;190:1076–1084. doi: 10.4049/jimmunol.1202659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Long M., Park S.G., Strickland I., Hayden M.S., Ghosh S. Nuclear factor-kappaB modulates regulatory T cell development by directly regulating expression of Foxp3 transcription factor. Immunity. 2009;31:921–931. doi: 10.1016/j.immuni.2009.09.022. [DOI] [PubMed] [Google Scholar]
- 46.Grinberg-Bleyer Y., Oh H., Desrichard A., Bhatt D.M., Caron R., Chan T.A., Schmid R.M., Klein U., Hayden M.S., Ghosh S. NF-kappaB c-Rel Is Crucial for the Regulatory T Cell Immune Checkpoint in Cancer. Cell. 2017;170:1096–1108.e1013. doi: 10.1016/j.cell.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oh H., Grinberg-Bleyer Y., Liao W., Maloney D., Wang P., Wu Z., Wang J., Bhatt D.M., Heise N., Schmid R.M., et al. An NF-kappaB Transcription-Factor-Dependent Lineage-Specific Transcriptional Program Promotes Regulatory T Cell Identity and Function. Immunity. 2017;47:450–465.e455. doi: 10.1016/j.immuni.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joshi N.S., Akama-Garren E.H., Lu Y., Lee D.Y., Chang G.P., Li A., DuPage M., Tammela T., Kerper N.R., Farago A.F., et al. Regulatory T Cells in Tumor-Associated Tertiary Lymphoid Structures Suppress Anti-tumor T Cell Responses. Immunity. 2015;43:579–590. doi: 10.1016/j.immuni.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Langowski J.L., Zhang X., Wu L., Mattson J.D., Chen T., Smith K., Basham B., McClanahan T., Kastelein R.A., Oft M. IL-23 promotes tumour incidence and growth. Nature. 2006;442:461–465. doi: 10.1038/nature04808. [DOI] [PubMed] [Google Scholar]
- 50.Benoot T., Piccioni E., De Ridder K., Goyvaerts C. TNFalpha and Immune Checkpoint Inhibition: Friend or Foe for Lung Cancer? Int. J. Mol. Sci. 2021;22:8691. doi: 10.3390/ijms22168691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steeland S., Libert C., Vandenbroucke R.E. A New Venue of TNF Targeting. Int. J. Mol. Sci. 2018;19:1442. doi: 10.3390/ijms19051442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Creaven P.J., Plager J.E., Dupere S., Huben R.P., Takita H., Mittelman A., Proefrock A. Phase I clinical trial of recombinant human tumor necrosis factor. Cancer Chemother. Pharmacol. 1987;20:137–144. doi: 10.1007/BF00253968. [DOI] [PubMed] [Google Scholar]
- 53.Feinberg B., Kurzrock R., Talpaz M., Blick M., Saks S., Gutterman J.U. A phase I trial of intravenously-administered recombinant tumor necrosis factor-alpha in cancer patients. J. Clin. Oncol. 1988;6:1328–1334. doi: 10.1200/JCO.1988.6.8.1328. [DOI] [PubMed] [Google Scholar]
- 54.Roberts N.J., Zhou S., Diaz L.A., Jr., Holdhoff M. Systemic use of tumor necrosis factor alpha as an anticancer agent. Oncotarget. 2011;2:739–751. doi: 10.18632/oncotarget.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schipper J.H., Frixen U.H., Behrens J., Unger A., Jahnke K., Birchmeier W. E-cadherin expression in squamous cell carcinomas of head and neck: Inverse correlation with tumor dedifferentiation and lymph node metastasis. Cancer Res. 1991;51:6328–6337. [PubMed] [Google Scholar]
- 56.Richter F., Williams S.K., John K., Huber C., Vaslin C., Zanker H., Fairless R., Pichi K., Marhenke S., Vogel A., et al. The TNFR1 Antagonist Atrosimab Is Therapeutic in Mouse Models of Acute and Chronic Inflammation. Front. Immunol. 2021;12:705485. doi: 10.3389/fimmu.2021.705485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis J.M., Colangelo J. Small-molecule inhibitors of the interaction between TNF and TNFR. Future Med. Chem. 2013;5:69–79. doi: 10.4155/fmc.12.192. [DOI] [PubMed] [Google Scholar]
- 58.Fu H., Wu H., Zhang X., Huang J., He X., Chen L., Guo W., Guo X., Hao B., Li Y. Pre-clinical study of a TNFR1-targeted (18)F probe for PET imaging of breast cancer. Amino Acids. 2018;50:409–419. doi: 10.1007/s00726-017-2526-y. [DOI] [PubMed] [Google Scholar]
- 59.Tsimberidou A.M., Waddelow T., Kantarjian H.M., Albitar M., Giles F.J. Pilot study of recombinant human soluble tumor necrosis factor (TNF) receptor (p75) fusion protein (TNFR:Fc; Enbrel) in patients with refractory multiple myeloma: Increase in plasma TNF alpha levels during treatment. Leuk. Res. 2003;27:375–380. doi: 10.1016/S0145-2126(02)00082-6. [DOI] [PubMed] [Google Scholar]
- 60.Sprott H., Glatzel M., Michel B.A. Treatment of myositis with etanercept (Enbrel), a recombinant human soluble fusion protein of TNF-alpha type II receptor and IgG1. Rheumatology. 2004;43:524–526. doi: 10.1093/rheumatology/keh062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.