Abstract
Glaucoma is a leading cause of irreversible blindness worldwide. While intraocular pressure (IOP) presents a major risk factor, the underlying pathophysiology still remains largely unclear. The correlation between vascular abnormalities and glaucoma has been deliberated for decades. Evidence for a role played by vascular factors in the pathogenesis of glaucomatous neurodegeneration has already been postulated. In addition, the fact that glaucoma causes both structural and functional changes to retinal blood vessels has been described. This review aims to investigate the published evidence concerning the relationship between vascular abnormalities and glaucoma, and to provide an overview of the “chicken or egg” dilemma in glaucoma. In this study, several biomarkers of glaucoma progression from a vascular perspective, including endothelin-1 (ET-1), nitric oxide, vascular endothelial growth factor (VEGF), and matrix metalloproteinases (MMPs), were identified and subsequently assessed for their potential as pharmacological intervention targets.
Keywords: glaucoma, vascular abnormalities, vascular biomarkers, neurodegeneration, intraocular pressure
1. Introduction
Glaucoma is characterized by the progressive death of retinal ganglion cells (RGCs) and consequential functional impairments of the visual field [1]. However, despite extensive research efforts, the precise pathogenesis of glaucoma remains inadequately understood. While elevated IOP has traditionally been recognized as the primary risk factor in glaucoma development, it is crucial to acknowledge that a significant proportion of patients experience disease progression despite successful normalization of IOP through therapeutic interventions [2].
There is a growing body of compelling evidence supporting the notion that vascular abnormalities, encompassing both vascular factors and systemic hemodynamics, play a substantial role in the complex etiology of glaucoma. The vascular theory in glaucomatous neurodegeneration postulates that diminished perfusion pressure, impaired vascular autoregulation, and disrupted neurovascular coupling serve as the underlying mechanisms. These factors collectively contribute to the progressive degeneration of the optic nerve and retinal ganglion cells in glaucoma [3,4].
Regarding hemodynamics, a notable association between glaucoma and systemic cardiovascular diseases, such as diabetes mellitus (DM) [5,6,7], high blood pressure (BP) [8,9], low BP [10], and nocturnal dipping [11] has been documented, suggesting an elevated incidence of glaucoma in affected individuals. These observations highlight the potential influence of hemodynamic factors on glaucoma development and progression [12,13]. Abnormal vascular function can also influence the secretion and drainage of aqueous humor (AH), thus affecting IOP regulation [14]. The elevated IOP resulting from vascular abnormalities can induce compression of RGCs and their axons, as well as diminished ocular blood supply. Consequently, these factors contribute to the pathogenesis and progression of glaucoma [15].
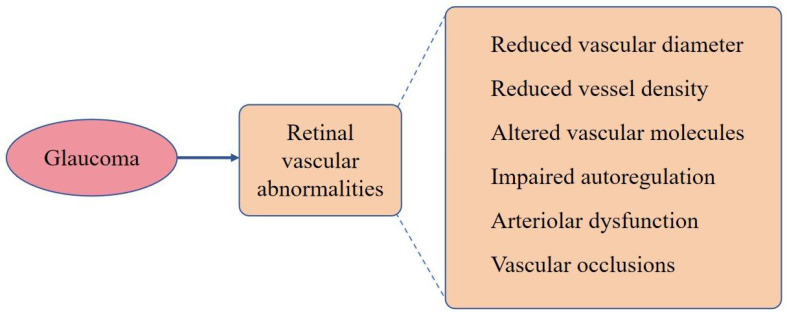
Retinal vascular dysfunction has been reported secondary to glaucoma, indicative of a bidirectional relationship between glaucoma and retinal vascular pathology [16]. These secondary manifestations of glaucoma include a reduction in retinal vascular diameter [17], decreased retinal vascular density [18], alterations in retinal vascular molecules [19], impaired autoregulation, arteriolar dysfunction within the retina [16], and even occurrences of retinal vein occlusion [17,20]. However, the answer to the question of whether vascular abnormalities drive glaucoma progression or if glaucoma serves as the instigator of vascular abnormalities remains elusive. In this comprehensive review, we investigate published evidence and provide a succinct summary of the vascular factors that potentially contribute to the pathogenesis of glaucoma. Additionally, we explore ocular vascular abnormalities that arise as a consequence of glaucoma. Furthermore, our analysis aims to identify potential vascular biomarkers that can serve as indicators for the progression and prognosis of glaucoma and the role of these biomarkers in refining current management strategies for glaucoma.
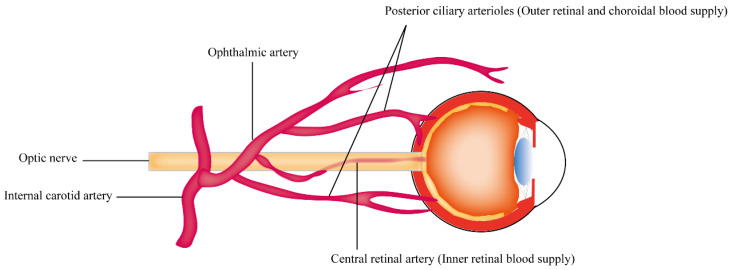
2. The Anatomy of Blood Supply in the Retina
The retina is a highly metabolically active tissue that requires a constant supply of nutrients and oxygen to function properly. The blood supply of the outer retina and inner retina comes from different circulatory pathways: the central retinal artery (CRA) and the choroidal circulation, respectively. This is summarized in Figure 1. The CRA is a branch of the ophthalmic artery, which arises from the internal carotid artery. The artery enters the eye through the optic nerve and travels through the center of the optic nerve to reach the retina. The CRA then divides into multiple smaller branches that supply blood to the inner retina, which includes the ganglion cells, inner plexiform layer, and inner nuclear layer [17,21]. The choroidal circulation is a network of blood vessels that lies between the retina and the sclera, the outermost layer of the eye. Blood from the choroidal circulation enters the retina through the outer retinal vessels and then flows towards the inner retina. The choroidal circulation supplies the outer retina, including the photoreceptors and the retinal pigment epithelium [22]. The high oxygen demands of the retina and the relatively sparse nature of the retinal vasculature are believed to be responsible for the particular vulnerability of the retina to vascular disease [22,23]. This indicates that neurons in the inner retina, such as RGCs, are susceptible to limited retinal inner blood supply in retinal diseases such as glaucoma and diabetic retinopathy [22,24]. Animal studies have demonstrated that bilateral occlusion of the common carotid arteries, leading to retinal hypoperfusion, causes a significant reduction in RGC density in rats due to apoptosis [25,26]. Clinical studies have also revealed a strong correlation between impaired ocular blood flow and glaucoma severity, particularly in patients with reduced perfusion in the optic nerve head (ONH) [27,28,29]. Such findings suggest that RGCs are particularly susceptible to reduced ocular blood flow.
Figure 1.
Anatomical depiction of the retinal blood supply.
3. The Role of Vascular Abnormalities in Glaucomatous Neurodegeneration
The vascular theory of glaucomatous neurodegeneration suggests that reduced perfusion pressure, faulty vascular autoregulation, and loss of neurovascular coupling play important roles in the relationship between vascular abnormalities and glaucomatous neurodegeneration [30,31]. In terms of hemodynamics, an increased incidence of glaucoma has been observed in patients with systemic cardiovascular diseases, such as DM [5,6] and high BP [8,9]. This observation underscores the potential impact of hemodynamic factors on the onset and advancement of glaucoma. Abnormal vascular function can also influence the secretion and drainage of aqueous humor, consequently increasing IOP and contributing to the pathogenesis and progression of glaucoma [14]. In this section, we provide a detailed discussion of these factors, elucidating their significance in the context of glaucoma. Additionally, we offer a comprehensive summary of the biomarkers that have been associated with glaucoma.
3.1. Ocular Perfusion Pressure and Its Role in Glaucomatous Neurodegeneration
The ocular perfusion pressure (OPP) refers to the pressure necessary to propel blood through the intraocular vasculature and represents the blood flow and oxygen supplying ONH [32]. Thus, it has long been proposed that a decrease in OPP may increase the vulnerability of the optic disc, leading to an increased risk of glaucoma development or progression [33,34,35,36]. In the Barbados Eye Study, individuals with low mean OPP exhibited a risk ratio of 2.6 for incident open-angle glaucoma (OAG) over a 9-year follow-up period [37]. The Singapore Malay Eye Study and the Los Angeles Latino Eye Study revealed a direct relationship between decreased OPP and increased prevalence of OAG [36,38]. The actual OPP should be determined by the difference between arterial pressure at the entrance to the eye and venous pressure at the exit of the eye. Since currently available methods cannot directly measure such pressures, OPP has been estimated by the difference between arterial pressure measured in the arm and IOP [33]. As a crucial modifiable part of OPP, systemic hemodynamics are supposed to play a role in the pathology and treatment of glaucoma, and this is further discussed in Section 3.4.
3.2. Vascular Autoregulation and Its Role in Glaucomatous Neurodegeneration
Vascular autoregulation, commonly known as vasoreactivity, represents the intrinsic capacity of the vascular system to adapt to varying physiological conditions and meet diverse metabolic demands by maintaining stable and sufficient blood flow [30,39]. A recent study suggested that the lower autoregulation limit is quite close to physiological OPP values [40]. This means that healthy optic nerves are prone to hypoperfusion with small fluctuations in BP or IOP. In pathological conditions [41], such as DM [42] and hypercholesterolemia [43], autoregulation in the ONH can be disrupted. In a study centered on autoregulation of the retrobulbar hemodynamics [44], it was observed that the unaltered flow velocities in the short posterior ciliary artery (SPCA) of healthy individuals, as a response to postural changes, suggest a strict autoregulatory control. However, in contrast, patients with normal-tension glaucoma (NTG) and primary open-angle glaucoma (POAG) demonstrated an insufficient compensatory response to postural changes. The authors of the study suggest that compromised autoregulatory control may represent another contributing factor in the pathogenesis of glaucomatous neurodegeneration. In fact, the disruption of vascular autoregulation in ONH has been reported to play a role in the etiology and progression of glaucoma for decades [30,45,46,47].
3.3. Neurovascular Coupling and Its Role in Glaucomatous Neurodegeneration
The central nervous system exhibits highly coordinated coupling between neuronal activity and blood flow. When there is a surge in neuronal activity, it triggers an increase in blood flow to the corresponding area, which is referred to as neurovascular coupling (NVC) [48]. NVC response has been demonstrated in the ONH blood flow and neuronal activity of RGCs with experiments investigating hemodynamic responses to flicker-light stimulation [49,50]. The NVC response in individuals with glaucoma is impaired [51], as the vasodilation response of the retina induced by flickering light [52] and the vasoconstrictive response to hyperoxia are attenuated [53]. Ischemia/hypoxia/perfusion instability may influence the astrocytes in the ONH and/or mitochondria of RGC axons, resulting in neurotoxic effects on RGCs [54,55,56].
3.4. Systematic Hemodynamics and Its Role in Glaucomatous Neurodegeneration
The role of systemic hemodynamics in glaucoma pathogenesis has been widely investigated. A “U-shaped” effect of BP on retinal function and structure has been revealed [8,57]. On the one hand, clinical studies have demonstrated that individuals with hypertension (HTN) [8,9] have a higher risk of developing glaucoma, with neural damage being more severe in glaucoma patients with HTN than those with normal BP [58]. Meanwhile, the treatment of HTN with beta-blockers can decrease the risk of glaucoma [59]. On the other hand, systemic hypotension and nocturnal dipping have also been associated with an increased risk of glaucoma [60]. The association between BP and neural deficits was shown to be mediated by decreased blood flow, increased vascular resistance, or lack of autoregulatory reserve [10,57,61]. Therefore, BP management in patients with concurrent systemic HTN and glaucoma is important. It is imperative to avoid excessive nocturnal BP dipping and to monitor potential retinal neuronal damage due to nocturnal hypotension induced by these treatments [11,60]. The recent TIME trial showed that the time of administration (morning or evening) for antihypertensive medication does not affect cardiovascular outcomes [62]. This suggests more flexibility in tailoring treatments for patients with concomitant glaucoma and HTN.
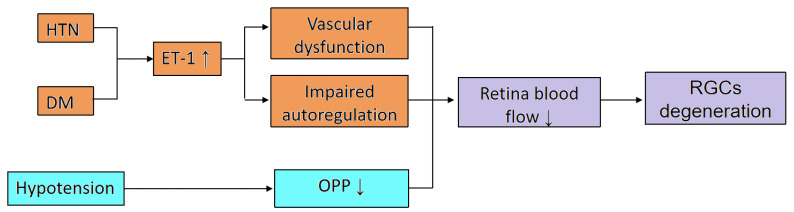
Apart from BP, it also has been reported that individuals with DM have a higher incidence of developing glaucoma [63]. Additionally, animal models have demonstrated that DM can trigger the degradation of RGCs [64,65]. One proposed mechanism is that DM [66,67] leads to a reduction in retinal blood flow, subsequently inducing retinal ischemia and hypoxia, and therefore RGC degeneration. In addition to exerting an influence upon systemic hemodynamics, DM can precipitate the onset of glaucoma through the elevation of IOP, a topic that is further discussed in Section 3.5. We summarize the systematic hemodynamic diseases contributing to reduced retinal blood flow and ganglion cell degeneration in Figure 2.
Figure 2.
The proposed mechanism of systematic hemodynamic diseases in reducing retinal blood flow (DM: diabetes mellitus; HTN: systematic hypertension; ET-1: endothelin-1; OPP: ocular perfusion pressure; RGCs: retinal ganglion cells).
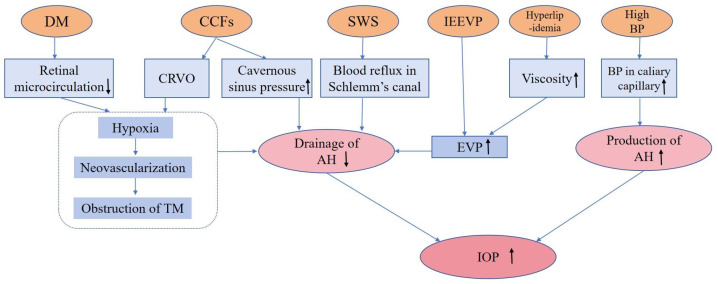
3.5. The Role of Vascular Abnormalities in Regulating IOP
IOP is the dynamic equilibrium between the production and drainage of AH [14,68]. The ciliary body in the posterior chamber secretes AH [69], which is primarily drained through the trabecular meshwork (TM) and collector canals before exiting into the episcleral veins and cavernous sinus [69]. Elevated IOP represents a significant etiological factor contributing to the onset and progression of glaucoma, while vascular abnormalities also precipitate elevated IOP, thereby fostering the pathogenesis of glaucoma [4,70].
It has been demonstrated that different vascular diseases are related to increased IOP. For instance, the pericyte loss of retinal blood vessels is a recognized marker of diabetic retinopathy (DR), which provokes capillary occlusion and overexpressed VEGF [70], potentially leading to neovascular glaucoma (NVG) [4,71,72]. In high-glucose conditions, the synthesis of extracellular matrix components including fibronectin is significantly increased, resulting in increased AH outflow resistance in TM, thus elevating IOP [73]. In addition, DM is considered to increase optic nerve head susceptibility to additional stress such as elevated IOP [7,74,75]. Arterial hypertension is another vascular disease that can increase IOP by elevating BP in the ciliary capillaries, leading to increased secretion of AH [76,77]. High BP can also raise episcleral venous pressure (EVP), which can increase resistance to AH drainage and further contribute to increased IOP [78,79]. Another vascular abnormality that can lead to increased IOP is hyperlipidemia. Studies have shown that hyperlipidemic patients are at an increased risk of glaucoma, potentially due to the increased viscosity of blood lipid levels, which in turn increases EVP [80,81]. Evidence supporting this hypothesis includes a lower incidence of glaucoma among patients receiving anti-hyperlipidemia therapy [82,83], as well as an increase in AH outflow facility observed in cultured porcine eyes treated with statins [84].
Sturge–Weber syndrome (SWS) is a rare, non-inherited neurovascular disorder characterized by abnormal vasculature in the brain, skin, and eye [85]. Glaucoma in SWS is another indication of elevated IOP caused by vascular abnormalities [86]. In glaucomatous eyes due to SWS, higher EVP was observed and thought to be the underlying pathophysiological mechanism of glaucoma [87,88]. Gonioscopy examination revealed reflux of blood in the Schlemm’s canal and episcleral hemangiomas, suggesting that Schlemm’s canal may be a component of hemangioma. Arteriovenous shunts in episcleral hemangioma may be the cause of elevated EVP, which consequently elevates IOP [88].
Carotid–cavernous fistulas (CCFs) are acquired vascular abnormalities with flow between the cavernous sinus and branches of either the external or internal carotid artery [89]. Elevated IOP and secondary glaucoma are common in CCFs [90]. Increased IOP in CCFs can be attributed to abnormal vascular shunts allowing carotid blood flow into cavernous fistulas, causing elevated pressure in the cavernous sinus and hindering the venous blood outflow from retinal and choroidal circulation, leading to anterior chamber (AC) shallowing and increased IOP [90,91,92]. Additionally, CCFs can result in neovascular glaucoma due to retinal hypoperfusion and ischemia [90,93,94]. While some cases of elevated EVP are due to identifiable etiologies, others are characterized as idiopathic elevated episcleral venous pressure (IEEVP) presenting with engorged episcleral veins, raised IOP, and/or glaucomatous visual field changes [94,95,96,97]. The elevated IOP due to vascular abnormities can cause compression of RGCs and their axons, as well as reduced ocular blood supply, leading to the development of glaucoma [15]. We summarize the different vascular abnormalities resulting in increased IOP in Figure 3.
Figure 3.
The possible roles of different vascular abnormalities in increasing IOP (DM: diabetes mellitus; CCFs: carotid-cavernous fistulas; SWS: Sturge–Weber syndrome; IEEVP: idiopathic elevated episcleral venous pressure; BP: blood pressure; TM: trabecular meshwork; AH: aqueous humor; EVP: episcleral venous pressure; IOP: intraocular pressure).
3.6. Biomarkers Associated with Ocular Blood Flow in Glaucoma
ET-1, a key regulator of vascular autoregulation [98,99], has been found to be overexpressed in the retina of diabetic individuals [98,100], and increased expression of ET-1 has also been observed in the plasma of patients with high BP [101,102]. Overexpression of ET-1 may therefore play a role in the impaired autoregulation of retinal vessels. Furthermore, increased ET-1 expression is a biomarker that has been implicated in retinal vascular dysfunction, which is another potential mechanism contributing to reduced retinal blood flow [103,104]. This hypothesis is supported by the finding that an ET-1 blocker can increase retinal blood flow [105]. Clinical studies have reported that glaucoma patients have higher levels of plasma ET-1 compared to healthy controls [106], and those with deteriorating visual fields have higher plasma ET-1 levels than those with normal visual fields [107]. Animal experiments have also shown that chronic administration of low doses of ET-1 in primates and rabbits can cause glaucomatous changes [108,109]. Thus, ET-1 may serve as a useful biomarker for predicting glaucoma progression or as a target for pharmacological intervention.
An imbalance between the vasoconstrictor ET-1 and the vasodilator nitric oxide has been observed in glaucoma, leading to endothelial dysfunction and decreased ocular blood flow [30]. Nitric oxide is a molecule that dilates blood vessels and is thought to be involved in the regulation of ocular blood flow in glaucoma [110]. Several studies have shown that the availability of nitric oxide is reduced in glaucoma [110,111], leading to a shift in the balance between vasoconstriction and vasodilation and resulting in decreased blood flow in the optic nerve head [111]. Collectively, ET-1 and nitric oxide could be reliable biomarkers in predicting glaucoma progression and/or targeting pharmacological intervention from a vascular perspective.
3.7. Biomarkers Associated with Aqueous Humor Outflow or Trabecular Meshwork Function
VEGF is a primary factor contributing to vascular permeability and plays a pivotal role in the process of neovascularization [112]. In the context of NVG, an excessive quantity of VEGF is observed entering the AC through the posterior pole, leading to the development of neovascularization and fibrovascular membranes over the TM. This process results in the obstruction of the AH outflow through the TM, leading to elevated IOP, which can potentially lead to glaucomatous optic neuropathy [112].
Nitric oxide is generated by neuronal nitric oxide synthase and endothelial nitric oxide synthase in a Ca2+/calmodulin-dependent manner, which is essential for maintaining IOP homeostasis [113]. Neuronal nitric oxide synthase is predominantly expressed in ciliary processes and nerve endings, with high expression in the anterior segment of the eye, such as ciliary muscle, trabecular meshwork, Schlemm’s canal, and collecting channels [113,114]. These structures are crucial in regulating AH dynamics and IOP homeostasis in both physiological and pathological conditions [113]. Ocular hypertensive patients have reduced nitric oxide formation compared to healthy individuals, and exogenous nitric oxide administration has been shown to lower IOP in these patients [114]. Polymorphisms in endothelial nitric oxide synthase are associated with a higher risk of glaucoma [115]. Studies with endothelial nitric-oxide-synthase-deficient mice [116] or animals with impaired ganglion cell activity [117,118] show that these animals have higher IOP than their wild-type littermates, further demonstrating the importance of nitric oxide signaling in regulating IOP.
MMPs are enzymes that play a role in the breakdown of extracellular matrix proteins, and are thought to contribute to the IOP change in glaucoma [119]. The TM generates the main AH outflow resistance and its extracellular matrix is constantly remodeled by MMPs [120]. The activity of MMPs has been found to be positively correlated with the AH outflow rate. Specifically, increasing MMP activity has been shown to elevate the outflow rate, while inhibiting MMP activity leads to a decrease in the outflow rate [121]. A recent study conducted using a porcine model has reported similar results, demonstrating that reduced activity of MMP-2 and -9 is associated with elevated IOP [122].
Together, the biomolecules VEGF, nitric oxide, and MMPs hold promise as potential biomarkers for predicting the progression of glaucoma and as targets for pharmacologic intervention.
4. Glaucoma Can Also Be the Instigator of Retinal Vascular Abnormalities
Retinal vascular dysfunction has been observed as a secondary manifestation both in individuals diagnosed with glaucoma and animal models employed to study the disease, suggesting that glaucoma may also serve as the instigator of retinal vascular abnormalities [16]. These secondary manifestations encompass various alterations, such as a notable reduction in retinal vascular diameter [17], decreased retinal vascular density [18], disturbances in retinal vascular molecules [19], impaired autoregulation of blood flow, dysfunction of retinal arterioles [16], and instances of retinal vein occlusion [17,20]. In this section, we aim to provide a comprehensive and in-depth discussion of the aforementioned alterations observed in both glaucoma patients and animal models used for studying the disease.
4.1. Reduced Retinal Vascular Diameter in Glaucoma
A study conducted on individuals with early normal-tension glaucoma demonstrated that there were no significant differences in retinal arterial diameters compared to normal controls. This finding suggests that the narrowing of retinal arterioles observed in glaucoma patients is a consequence of the disease rather than being its underlying cause [123]. Further research conducted on adult Sprague Dawley rats involved the experimental elevation of IOP by cauterizing three episcleral veins. The findings from this study demonstrated a significant reduction in both vessel caliber and area within the glaucomatous optic nerves of the experimental rats [17]. In another glaucoma model, utilizing elevated IOP in Brown Norway rats through a vascular loop, an acute elevation of IOP caused a decrease in total retinal blood flow and average retinal blood vessel size [124]. One proposed mechanism underlying glaucomatous conditions suggests that the impaired RGCs necessitate a reduced blood supply, subsequently triggering retinal arteriolar constriction through the process of autoregulation [120,125,126,127,128]. This mechanism appears plausible, since retinal vascular constriction is observed not only in glaucoma but also in other optic nerve damage diseases [127,129,130,131,132].
4.2. Reduced Retinal Vascular Density in Glaucoma
In a case-control study, it was discovered that individuals afflicted with unilateral acute primary angle closure glaucoma (PACG) demonstrated a significant reduction in peripapillary retinal vessel density within affected eyes, as compared to contralateral unaffected eyes [18]. The notable decrease in vessel density was found to be significantly associated with visual field loss, thinning of the retinal nerve fiber layer, and ganglion cell complex in eyes affected by PACG. This association suggests that the loss of retinal vessel density is closely related to the presence and progression of glaucoma [18]. A series of case reports revealed that the reduction in IOP can lead to a re-increase in peripapillary capillary density in the retinal nerve fiber layer in ocular hypertensive and glaucomatous eyes [18]. Likewise, a prospective study demonstrated that trabeculectomy led to an improvement in peripapillary capillaries’ microvasculature observed through optical coherence tomography angiography in POAG patients [133]. However, this improvement proved incomplete as other studies showed that peripapillary retinal vessel density in resolved acute PACG eyes was still lower than the unaffected fellow eyes [18,134]. In a study conducted on C57BL/6J mice, transient elevated IOP was induced by injecting sodium hyaluronate into the AC. This manipulation resulted in a significant reduction in the number of capillary branches observed in both the superficial and intermediate vascular plexus of the retina [135]. The reduction in retinal capillaries observed in glaucomatous rats follows a similar pattern, with a more pronounced impact on capillary density in the inner layers of the retina in response to elevated IOP [136]. This phenomenon may provide an explanation for the observed decline in RGCs and thinning of the retinal nerve fiber layer during the progression of glaucoma.
4.3. Altered Retinal Vascular Molecules in the Retinas of Murine Models of Glaucoma
In experiments conducted on cultivated mouse retinas subjected to elevated intrachamber pressure, it was observed that the expression of tight adherens junction proteins, such as zonula occludens 1 (ZO-1), occludin, and the adherens junction protein VE-cadherin in retinal vessels, underwent alterations [19]. These findings strongly indicate that the integrity of the blood–retina barrier was compromised under conditions of elevated pressure [19]. In vivo and in vitro studies have demonstrated the expression of ß-III-tubulin, a neuron-specific biomarker, in both pericytes and endothelial cells in response to elevated IOP and intrachamber pressure, respectively [137]. This regulation of neuron-specific ß-III-tubulin is believed to be associated with retinal vascular remodeling under elevated IOP. Notably, the expression of ß-III-tubulin has also been observed during the remodeling of mesenteric vessels in rats, further supporting its involvement in vascular remodeling processes [138]. Furthermore, ß-III-tubulin is involved in oxidative stress [139], which can induce vascular endothelial dysfunction and impair the autoregulation of retinal arterioles [16].
4.4. Impaired Autoregulation and Arteriolar Dysfunction in the Retina of a Murine Model of Glaucoma
In a mouse model of glaucoma induced by unilateral cauterization of three episcleral veins [16,140], elevated IOP was observed to lead to impaired autoregulation and vascular dysfunction of retinal arterioles. This means that the ability of the retinal arterioles to regulate blood flow and maintain proper vascular function was compromised. [16]. The exact underlying mechanism for this phenomenon is believed to involve heightened oxidative stress and inflammation within the retina [16].
4.5. Glaucoma Is a Risk Factor for Retinal Vascular Occlusions
Multiple studies have reported a notable association between glaucoma, specifically open-angle glaucoma, and an increased incidence of retinal vascular occlusions [141,142]. In a comprehensive Korean nationwide population-based retrospective study, it was observed that individuals diagnosed with open-angle glaucoma exhibited a significantly elevated incidence of retinal vascular occlusions when compared to the general population [20]. A retrospective case-control study conducted by Schwaber et al. (2018) [143] found that glaucoma was a risk factor for incident retinal vascular occlusions with an odds ratio of 6.19 (p < 0.001). However, some studies did not find this association [144,145]. A meta-analysis by Yin et al. (2019) [146] reported that glaucoma is a risk factor for retinal vascular occlusions with an odds ratio of 4.01. Subgroup analysis within the study indicated that glaucoma was significantly associated with various types of retinal vascular occlusions, including central retinal vein occlusion, branch retinal vein occlusion, and hemiretinal vein occlusion. Furthermore, the analysis of glaucoma subgroups revealed an association between open-angle glaucoma and central retinal vein occlusion, as well as between PACG and central retinal vein occlusion. However, there was no significant association observed between PACG and branch retinal vein occlusion. We have summarized the different vascular abnormalities resulting from glaucoma in Figure 4.
Figure 4.
Different vascular abnormalities resulting from glaucoma.
5. Conclusions
The introduction of the vascular theory, as well as the hemodynamics surrounding it, has spurred a growing body of scientific investigations aimed at unraveling the intricate relationship between vascular abnormalities and the underlying pathophysiology of glaucoma. It has become increasingly apparent that vascular abnormalities are closely associated with the observed neurodegeneration in glaucoma. However, it is important to recognize that glaucoma itself can initiate retinal vascular abnormalities. Nevertheless, given the multifactorial nature of glaucoma, it is acknowledged that vascular abnormalities represent just one of many contributing factors to the neurodegenerative processes observed in this disease. In addition to determining the causality between vascular abnormalities and glaucoma, longitudinal studies are necessary to disentangle the temporal association between loss of neural structure and loss of vascularization.
Acknowledgments
We thank Valerio Ganci for carefully proofreading the manuscript.
Abbreviations
The following abbreviations are used in this manuscript:
| AH | Aqueous humor |
| AC | Anterior chamber |
| BP | Blood pressure |
| CCFs | Carotid–cavernous fistulas |
| CRA | Central retinal artery |
| DM | Diabetes mellitus |
| DR | Diabetic retinopathy |
| ET-1 | Endothelin-1 |
| EVP | Episcleral venous pressure |
| HTN | Hypertension |
| IEEVP | Idiopathic elevated episcleral venous pressure |
| IOP | Intraocular pressure |
| MMPs | Matrix metalloproteinases |
| NVC | Neurovascular coupling |
| NVG | Neovascular glaucoma |
| OCTA | Optical coherence tomography angiography |
| ONH | Optic nerve head |
| OPP | Ocular perfusion pressure |
| PACG | Primary angle closure glaucoma |
| POAG | Primary open-angle glaucoma |
| RGCs | Retinal ganglion cells |
| SPCA | Short posterior ciliary artery |
| SWS | Sturge–Weber syndrome |
| TM | Trabecular meshwork |
| VEGF | Vascular endothelial growth factor |
| ZO-1 | Zonula occludens 1 |
Author Contributions
Conceptualization, V.P. and H.L.; writing—original draft preparation, X.W. and M.W.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the Deutsche Forschungsgemeinschaft (DFG) with grant PR1569/1-1.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Raman P., Khy Ching Y., Sivagurunathan P.D., Ramli N., Mohd Khalid K.H. The Association between Visual Field Reliability Indices and Cognitive Impairment in Glaucoma Patients. J. Glaucoma. 2019;28:685–690. doi: 10.1097/IJG.0000000000001269. [DOI] [PubMed] [Google Scholar]
- 2.Leske M.C., Heijl A., Hussein M., Bengtsson B., Hyman L., Komaroff E., Early Manifest Glaucoma Trial Group Factors for glaucoma progression and the effect of treatment: The early manifest glaucoma trial. Arch. Ophthalmol. 2003;121:48–56. doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 3.Fan X., Ying Y., Zhai R., Sheng Q., Sun Y., Xu H., Kong X. The characteristics of fundus microvascular alterations in the course of glaucoma: A narrative review. Ann. Transl. Med. 2022;10:527. doi: 10.21037/atm-21-5695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alarcon-Martinez L., Shiga Y., Villafranca-Baughman D., Belforte N., Quintero H., Dotigny F., Cueva Vargas J.L., Di Polo A. Pericyte dysfunction and loss of interpericyte tunneling nanotubes promote neurovascular deficits in glaucoma. Proc. Natl. Acad. Sci. USA. 2022;119:e2110329119. doi: 10.1073/pnas.2110329119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou M., Wang W., Huang W., Zhang X. Diabetes mellitus as a risk factor for open-angle glaucoma: A systematic review and meta-analysis. PLoS ONE. 2014;9:e102972. doi: 10.1371/journal.pone.0102972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pasquale L.R., Kang J.H., Manson J.E., Willett W.C., Rosner B.A., Hankinson S.E. Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women. Ophthalmology. 2006;113:1081–1086. doi: 10.1016/j.ophtha.2006.01.066. [DOI] [PubMed] [Google Scholar]
- 7.Chopra V., Varma R., Francis B.A., Wu J., Torres M., Azen S.P., Los Angeles Latino Eye Study Group Type 2 diabetes mellitus and the risk of open-angle glaucoma the Los Angeles Latino Eye Study. Ophthalmology. 2008;115:227–232. doi: 10.1016/j.ophtha.2007.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuang T.M., Xirasagar S., Kao Y.W., Shia B.C., Lin H.C. Association of Systemic Hypertension with Primary Open-angle Glaucoma: A Population-based Case-Control Study. Am. J. Ophthalmol. 2020;218:99–104. doi: 10.1016/j.ajo.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Phillips C.I. The association of blood pressure and primary open-angle glaucoma: A meta-analysis. Am. J. Ophthalmol. 2014;158:1363. doi: 10.1016/j.ajo.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 10.Chung H.J., Hwang H.B., Lee N.Y. The Association between Primary Open-Angle Glaucoma and Blood Pressure: Two Aspects of Hypertension and Hypotension. BioMed Res. Int. 2015;2015:827516. doi: 10.1155/2015/827516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Moraes C.G., Cioffi G.A., Weinreb R.N., Liebmann J.M. New Recommendations for the Treatment of Systemic Hypertension and their Potential Implications for Glaucoma Management. J. Glaucoma. 2018;27:567–571. doi: 10.1097/IJG.0000000000000981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rim T.H., Lee S.Y., Bae H.W., Seong G.J., Kim S.S., Kim C.Y. Increased risk of open-angle glaucoma among patients with diabetes mellitus: A 10-year follow-up nationwide cohort study. Acta Ophthalmol. 2018;96:e1025–e1030. doi: 10.1111/aos.13805. [DOI] [PubMed] [Google Scholar]
- 13.Cui Y.K., Pan L., Lam T., Wen C.Y., Do C.W. Mechanistic links between systemic hypertension and open angle glaucoma. Clin. Exp. Optom. 2022;105:362–371. doi: 10.1080/08164622.2021.1964332. [DOI] [PubMed] [Google Scholar]
- 14.van Zyl T., Yan W., McAdams A., Peng Y.R., Shekhar K., Regev A., Juric D., Sanes J.R. Cell atlas of aqueous humor outflow pathways in eyes of humans and four model species provides insight into glaucoma pathogenesis. Proc. Natl. Acad. Sci. USA. 2020;117:10339–10349. doi: 10.1073/pnas.2001250117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yanagi M., Kawasaki R., Wang J.J., Wong T.Y., Crowston J., Kiuchi Y. Vascular risk factors in glaucoma: A review. Clin. Exp. Ophthalmol. 2011;39:252–258. doi: 10.1111/j.1442-9071.2010.02455.x. [DOI] [PubMed] [Google Scholar]
- 16.Gericke A., Mann C., Zadeh J.K., Musayeva A., Wolff I., Wang M., Pfeiffer N., Daiber A., Li H., Xia N., et al. Elevated Intraocular Pressure Causes Abnormal Reactivity of Mouse Retinal Arterioles. Oxid. Med. Cell. Longev. 2019;2019:9736047. doi: 10.1155/2019/9736047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mann C., Anders F., Liu H., Brockhaus K., Liu A., Grus F.H., Pfeiffer N., Thanos S., Prokosch V. Morphological and Quantitative Changes in Retinal and Optic Nerve Vessels in Experimental Glaucoma Model with Elevated IOP for 7 Weeks. Klin. Monbl. Augenheilkd. 2019;236:871–876. doi: 10.1055/s-0044-101617. [DOI] [PubMed] [Google Scholar]
- 18.Zhang S., Wu C., Liu L., Jia Y., Zhang Y., Zhang Y., Zhang H., Zhong Y., Huang D. Optical Coherence Tomography Angiography of the Peripapillary Retina in Primary Angle-Closure Glaucoma. Am. J. Ophthalmol. 2017;182:194–200. doi: 10.1016/j.ajo.2017.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brockhaus K., Melkonyan H., Prokosch-Willing V., Liu H., Thanos S. Alterations in Tight- and Adherens-Junction Proteins Related to Glaucoma Mimicked in the Organotypically Cultivated Mouse Retina under Elevated Pressure. Investig. Ophthalmol. Vis. Sci. 2020;61:46. doi: 10.1167/iovs.61.3.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Na K.I., Jeoung J.W., Kim Y.K., Lee W.J., Park K.H. Incidence of retinal vein occlusion in open-angle glaucoma: A nationwide, population-based study using the Korean Health Insurance Review and Assessment Database. Clin. Exp. Ophthalmol. 2018;46:637–644. doi: 10.1111/ceo.13157. [DOI] [PubMed] [Google Scholar]
- 21.Kocabiyik N., Yalcin B., Ozan H. The morphometric analysis of the central retinal artery. Ophthalmic Physiol. Opt. 2005;25:375–378. doi: 10.1111/j.1475-1313.2005.00286.x. [DOI] [PubMed] [Google Scholar]
- 22.Country M.W. Retinal metabolism: A comparative look at energetics in the retina. Brain Res. 2017;1672:50–57. doi: 10.1016/j.brainres.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 23.Yu D.Y., Cringle S.J. Oxygen Distribution and Consumption within the Retina in Vascularised and Avascular Retinas and in Animal Models of Retinal Disease. Prog. Retin. Eye Res. 2001;20:175–208. doi: 10.1016/S1350-9462(00)00027-6. [DOI] [PubMed] [Google Scholar]
- 24.Chen N., Jiang K., Yan G.G. Effect of fenofibrate on diabetic retinopathy in rats via SIRT1/NF-kappaB signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 2019;23:8630–8636. doi: 10.26355/eurrev_201910_19180. [DOI] [PubMed] [Google Scholar]
- 25.Qin Y., Ji M., Deng T., Luo D., Zi Y., Pan L., Wang Z., Jin M. Functional and morphologic study of retinal hypoperfusion injury induced by bilateral common carotid artery occlusion in rats. Sci. Rep. 2019;9:80. doi: 10.1038/s41598-018-36400-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lavinsky D., Arterni N.S., Achaval M., Netto C.A. Chronic bilateral common carotid artery occlusion: A model for ocular ischemic syndrome in the rat. Graefes Arch. Clin. Exp. Ophthalmol. 2006;244:199–204. doi: 10.1007/s00417-005-0006-7. [DOI] [PubMed] [Google Scholar]
- 27.Schumann J., Orgül S., Gugleta K., Dubler B., Flammer J. Interocular difference in progression of glaucoma correlates with interocular differences in retrobulbar circulation. Am. J. Ophthalmol. 2000;129:728–733. doi: 10.1016/S0002-9394(99)00481-X. [DOI] [PubMed] [Google Scholar]
- 28.Baek S.U., Kim Y.K., Ha A., Kim Y.W., Lee J., Kim J.S., Jeoung J.W., Park K.H. Diurnal change of retinal vessel density and mean ocular perfusion pressure in patients with open-angle glaucoma. PLoS ONE. 2019;14:e0215684. doi: 10.1371/journal.pone.0215684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fındık H., Çeliker M., Aslan M.G., Çeliker F.B., İnecikli M.F., Dursun E., Okutucu M., Şahin Ü. The relation between retrobulbar blood flow and posterior ocular changes measured using spectral-domain optical coherence tomography in patients with obstructive sleep apnea syndrome. Int. Ophthalmol. 2019;39:1013–1025. doi: 10.1007/s10792-018-0892-4. [DOI] [PubMed] [Google Scholar]
- 30.Leung D.Y.L., Tham C.C. Normal-tension glaucoma: Current concepts and approaches—A review. Clin. Exp. Ophthalmol. 2022;50:247–259. doi: 10.1111/ceo.14043. [DOI] [PubMed] [Google Scholar]
- 31.Ahmad S.S. Controversies in the vascular theory of glaucomatous optic nerve degeneration. Taiwan J. Ophthalmol. 2016;6:182–186. doi: 10.1016/j.tjo.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caprioli J., Coleman A.L. Blood pressure, perfusion pressure, and glaucoma. Am. J. Ophthalmol. 2010;149:704–712. doi: 10.1016/j.ajo.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 33.Kim K.E., Oh S., Baek S.U., Ahn S.J., Park K.H., Jeoung J.W. Ocular Perfusion Pressure and the Risk of Open-Angle Glaucoma: Systematic Review and Meta-analysis. Sci. Rep. 2020;10:10056. doi: 10.1038/s41598-020-66914-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tham Y.C., Lim S.H., Gupta P., Aung T., Wong T.Y., Cheng C.Y. Inter-relationship between ocular perfusion pressure, blood pressure, intraocular pressure profiles and primary open-angle glaucoma: The Singapore Epidemiology of Eye Diseases study. Br. J. Ophthalmol. 2018;102:1402–1406. doi: 10.1136/bjophthalmol-2017-311359. [DOI] [PubMed] [Google Scholar]
- 35.Barbosa-Breda J., Abegão-Pinto L., Van Keer K., Jesus D.A., Lemmens S., Vandewalle E., Rocha-Sousa A., Stalmans I. Heterogeneity in arterial hypertension and ocular perfusion pressure definitions: Towards a consensus on blood pressure-related parameters for glaucoma studies. Acta Ophthalmol. 2019;97:e487–e492. doi: 10.1111/aos.13942. [DOI] [PubMed] [Google Scholar]
- 36.Zheng Y.F., Wong T.Y., Matchell P., Friedman D.S., HE M., Aung T. Distribution of Ocular Perfusion Pressure and Its Relationship with Open-Angle Glaucoma: The Singapore Malay Eye Study. Investig. Ophthalmol. Vis. Sci. 2010;51:3399–3404. doi: 10.1167/iovs.09-4867. [DOI] [PubMed] [Google Scholar]
- 37.Leske M.C., Wu S.Y., Hennis A., Honkanen R., Nemesure B., BESs Study Group Risk factors for incident open-angle glaucoma: The Barbados Eye Studies. Ophthalmology. 2008;115:85–93. doi: 10.1016/j.ophtha.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 38.Memarzadeh F., Ying L., Chung J., Azen S.P., Varma R. Blood Pressure, Perfusion Pressure, and Open-Angle Glaucoma: The Los Angeles Latino Eye Study. Investig. Ophthalmol. Vis. Sci. 2010;51:2872–2877. doi: 10.1167/iovs.08-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stewart W.C., Kolker A.E., Sharpe E.D., Day D.G., Holmes K.T., Leech J.N., Johnson M., Cantrell J.B. Factors associated with long-term progression or stability in primary open-angle glaucoma. Am. J. Ophthalmol. 2000;130:274–279. doi: 10.1016/S0002-9394(00)00487-6. [DOI] [PubMed] [Google Scholar]
- 40.Pappelis K., Choritz L., Jansonius N.M. Microcirculatory model predicts blood flow and autoregulation range in the human retina: In vivo investigation with laser speckle flowgraphy. Am. J. Physiol. Heart Circ. Physiol. 2020;319:H1253–H1273. doi: 10.1152/ajpheart.00404.2020. [DOI] [PubMed] [Google Scholar]
- 41.Anderson D.R. Introductory comments on blood flow autoregulation in the optic nerve head and vascular risk factors in glaucoma. Surv. Ophthalmol. 1999;43:S5–S9. doi: 10.1016/S0039-6257(99)00046-6. [DOI] [PubMed] [Google Scholar]
- 42.Phene S., Dunn R.C., Hammel N., Liu Y., Krause J., Kitade N., Schaekermann M., Sayres R., Wu D.J., Bora A. Deep Learning and Glaucoma Specialists: The Relative Importance of Optic Disc Features to Predict Glaucoma Referral in Fundus Photographs. Ophthalmology. 2019;126:1627–1639. doi: 10.1016/j.ophtha.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 43.Shibata M., Sugiyama T., Hoshiga M., Hotchi J., Okuno T., Oku H., Hanafusa T., Ikeda T. Changes in optic nerve head blood flow, visual function, and retinal histology in hypercholesterolemic rabbits. Exp. Eye Res. 2011;93:818–824. doi: 10.1016/j.exer.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 44.Galambos P., Vafiadis J., Vilchez S.E., Wagenfeld L., Matthiessen E.T., Richard G., Klemm M., Zeitz O. Compromised autoregulatory control of ocular hemodynamics in glaucoma patients after postural change. Ophthalmology. 2006;113:1832–1836. doi: 10.1016/j.ophtha.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 45.Chung H.S., Harris A., Evans D.W., Kagemann L., Garzozi H.J., Martin B. Vascular aspects in the pathophysiology of glaucomatous optic neuropathy. Surv. Ophthalmol. 1999;43:43–50. doi: 10.1016/S0039-6257(99)00050-8. [DOI] [PubMed] [Google Scholar]
- 46.Loo J.H., Wang Z., Chong R.S. Caveolin-1 in vascular health and glaucoma: A critical vascular regulator and potential therapeutic target. Front. Med. 2023;10:1087123. doi: 10.3389/fmed.2023.1087123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yabana T., Sato K., Shiga Y., Himori N., Omodaka K., Nakazawa T. The relationship between glutathione levels in leukocytes and ocular clinical parameters in glaucoma. PLoS ONE. 2019;14:e0227078. doi: 10.1371/journal.pone.0227078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Drew P.J. Neurovascular coupling: Motive unknown. Trends Neurosci. 2022;45:809–819. doi: 10.1016/j.tins.2022.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Riva C.E., Grunwald J.E., Petrig B.L. Autoregulation of human retinal blood flow. An investigation with laser Doppler velocimetry. Investig. Ophthalmol. Vis. Sci. 1986;27:1706–1712. [PubMed] [Google Scholar]
- 50.Loo J.H., Lee Y.S., Woon C.Y., Yong V.H.K., Tan B., Schmetterer L., Chong R.S. Loss of Caveolin-1 Impairs Light Flicker-Induced Neurovascular Coupling at the Optic Nerve Head. Front. Neurosci. 2021;15:764898. doi: 10.3389/fnins.2021.764898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Q., Qu X., Chen W., Wang H., Huang C., Li T., Wang N., Xian J. Altered coupling of cerebral blood flow and functional connectivity strength in visual and higher order cognitive cortices in primary open angle glaucoma. J. Cereb. Blood Flow Metab. 2021;41:901–913. doi: 10.1177/0271678X20935274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou W., Sabel B.A. Vascular dysregulation in glaucoma: Retinal vasoconstriction and normal neurovascular coupling in altitudinal visual field defects. EPMA J. 2023;14:87–99. doi: 10.1007/s13167-023-00316-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kiyota N., Shiga Y., Suzuki S., Sato M., Takada N., Maekawa S., Omodaka K., Maruyama K., Kunikata H., Nakazawa T. The Effect of Systemic Hyperoxia on Optic Nerve Head Blood Flow in Primary Open-Angle Glaucoma Patients. Investig. Ophthalmol. Vis. Sci. 2017;58:3181–3188. doi: 10.1167/iovs.17-21648. [DOI] [PubMed] [Google Scholar]
- 54.Ghosh A.K., Rao V.R., Wisniewski V.J., Zigrossi A.D., Floss J., Koulen P., Stubbs E.B., Kaja S. Differential Activation of Glioprotective Intracellular Signaling Pathways in Primary Optic Nerve Head Astrocytes after Treatment with Different Classes of Antioxidants. Antioxidants. 2020;9:324. doi: 10.3390/antiox9040324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patabendige A., Singh A., Jenkins S., Sen J., Chen R. Astrocyte Activation in Neurovascular Damage and Repair Following Ischaemic Stroke. Int. J. Mol. Sci. 2021;22:4280. doi: 10.3390/ijms22084280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pronin A., Pham D., An W., Dvoriantchikova G., Reshetnikova G., Qiao J., Kozhekbaeva Z., Reiser A.E., Slepak V.Z., Shestopalov V.I. Inflammasome Activation Induces Pyroptosis in the Retina Exposed to Ocular Hypertension Injury. Front. Mol. Neurosci. 2019;12:36. doi: 10.3389/fnmol.2019.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pappelis K., Jansonius N.M. U-Shaped Effect of Blood Pressure on Structural OCT Metrics and Retinal Perfusion in Investigative Ophthalmology and Visual Science. EPMA J. 2021;62:5. doi: 10.1167/iovs.62.12.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khatri A., Shrestha J.K., Thapa M., Khatri B.K., Kharel M. Severity of primary open-angle glaucoma in patients with hypertension and diabetes. Diabetes Metab. Syndr. Obes. Targets Ther. 2018;11:209–215. doi: 10.2147/DMSO.S160978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu A., Khawaja A.P., Pasquale L.R., Stein J.D. A review of systemic medications that may modulate the risk of glaucoma. Eye. 2020;34:12–28. doi: 10.1038/s41433-019-0603-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shukla A.G., Razeghinejad R., Myers J.S. Balancing treatments for patients with systemic hypertension and glaucoma. Expert Opin. Pharmacother. 2020;21:2225–2230. doi: 10.1080/14656566.2020.1810235. [DOI] [PubMed] [Google Scholar]
- 61.Kim Y.-S., Han N.-R., Seo K.H. Changes of intraocular pressure and ocular perfusion pressure during controlled hypotension in patients undergoing arthroscopic shoulder surgery: A prospective, randomized, controlled study comparing propofol, and desflurane anesthesia. Medicine. 2019;98:e15461. doi: 10.1097/MD.0000000000015461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pappelis K., Apostolos A., Konstantinou K. TIME to discuss the optic nerve? Eye. 2023 doi: 10.1038/s41433-023-02555-3. online ahead of print . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.AlDarrab A., Al Jarallah O.J., Al Balawi H.B. Association of diabetes, fasting glucose, and the risk of glaucoma: A systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2023;27:2419–2427. doi: 10.26355/eurrev_202303_31776. [DOI] [PubMed] [Google Scholar]
- 64.Yang Y., Mao D., Chen X., Zhao L., Tian Q., Liu C., Zhou B.L. Decrease in retinal neuronal cells in streptozotocin-induced diabetic mice. Mol. Vis. 2012;18:1411–1420. [PMC free article] [PubMed] [Google Scholar]
- 65.Barber A.J., Antonetti D.A., Kern T.S., Reiter C.E., Soans R.S., Krady J.K., Levison S.W., Gardner T.W., Bronson S.K. The Ins2Akita mouse as a model of early retinal complications in diabetes. Investig. Ophthalmol. Vis. Sci. 2005;46:2210–2218. doi: 10.1167/iovs.04-1340. [DOI] [PubMed] [Google Scholar]
- 66.Takagi C., King G.L., Clermont A.C., Cummins D.R., Takagi H., Bursell S.E. Reversal of abnormal retinal hemodynamics in diabetic rats by acarbose, an alpha-glucosidase inhibitor. Curr. Eye Res. 1995;14:741–749. doi: 10.3109/02713689508995795. [DOI] [PubMed] [Google Scholar]
- 67.Higashi S., Clermont A.C., Dhir V., Bursell S.E. Reversibility of retinal flow abnormalities is disease-duration dependent in diabetic rats. Diabetes. 1998;47:653–659. doi: 10.2337/diabetes.47.4.653. [DOI] [PubMed] [Google Scholar]
- 68.Greenfield D.S. Glaucoma associated with elevated episcleral venous pressure. J. Glaucoma. 2000;9:190–194. doi: 10.1097/00061198-200004000-00012. [DOI] [PubMed] [Google Scholar]
- 69.Fautsch M.P., Johnson D.H. Aqueous humor outflow: What do we know? Where will it lead us? Investig. Ophthalmol. Vis. Sci. 2006;47:4181–4187. doi: 10.1167/iovs.06-0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Trost A., Bruckner D., Rivera F.J., Reitsamer H.A. Pericytes in the Retina. Adv. Exp. Med. Biol. 2019;1122:1–26. doi: 10.1007/978-3-030-11093-2_1. [DOI] [PubMed] [Google Scholar]
- 71.Barac I.R., Pop M.D., Gheorghe A.I., Taban C. Neovascular Secondary Glaucoma, Etiology and Pathogenesis. Rom. J. Ophthalmol. 2015;59:24–28. [PMC free article] [PubMed] [Google Scholar]
- 72.Konareva-Kostianeva M. Neovascular glaucoma. Folia Med. 2005;47:5–11. [PubMed] [Google Scholar]
- 73.Sato T., Roy S. Effect of high glucose on fibronectin expression and cell proliferation in trabecular meshwork cells. Investig. Ophthalmol. Vis. Sci. 2002;43:170–175. [PubMed] [Google Scholar]
- 74.Jung K.I., Woo J.E., Park C.K. Intraocular pressure fluctuation and neurodegeneration in the diabetic rat retina. Br. J. Pharmacol. 2020;177:3046–3059. doi: 10.1111/bph.15033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Freeman E.E., Bastasic J., Grant A., Leung G., Li G., Buhrmann R., Roy-Gagnon M.H. Inverse Association of APOE ϵ4 and Glaucoma Modified by Systemic Hypertension: The Canadian Longitudinal Study on Aging. Investig. Ophthalmol. Vis. Sci. 2022;63:9. doi: 10.1167/iovs.63.13.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Charlson M.E., de Moraes C.G., Link A., Wells M.T., Harmon G., Peterson J.C., Ritch R., Liebmann J.M. Nocturnal systemic hypotension increases the risk of glaucoma progression. Ophthalmology. 2014;121:2004–2012. doi: 10.1016/j.ophtha.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dziedziak J., Zaleska-Żmijewska A., Szaflik J.P., Cudnoch-Jędrzejewska A. Impact of Arterial Hypertension on the Eye: A Review of the Pathogenesis, Diagnostic Methods, and Treatment of Hypertensive Retinopathy. Med. Sci. Monit. 2022;28:e935135. doi: 10.12659/MSM.935135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhao D., Cho J., Kim M.H., Guallar E. The association of blood pressure and primary open-angle glaucoma: A meta-analysis. Am. J. Ophthalmol. 2014;158:615–627.e9. doi: 10.1016/j.ajo.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 79.Krasińska B., Karolczak-Kulesza M., Krasiński Z., Pawlaczyk-Gabriel K., Lopatka P., Głuszek J., Tykarski A. Effects of the time of antihypertensive drugs administration on the stage of primary open-angle glaucoma in patients with arterial hypertension. Blood Press. 2012;21:240–248. doi: 10.3109/08037051.2012.666423. [DOI] [PubMed] [Google Scholar]
- 80.Wang S., Bao X. Hyperlipidemia, Blood Lipid Level, and the Risk of Glaucoma: A Meta-Analysis. Investig. Ophthalmol. Vis. Sci. 2019;60:1028–1043. doi: 10.1167/iovs.18-25845. [DOI] [PubMed] [Google Scholar]
- 81.Shiose Y., Kawase Y. A new approach to stratified normal intraocular pressure in a general population. Am. J. Ophthalmol. 1986;101:714–721. doi: 10.1016/0002-9394(86)90776-2. [DOI] [PubMed] [Google Scholar]
- 82.Vaughan C.J., Delanty N. Neuroprotective properties of statins in cerebral ischemia and stroke. Stroke. 1999;30:1969–1973. doi: 10.1161/01.STR.30.9.1969. [DOI] [PubMed] [Google Scholar]
- 83.McGwin G., McNeal S., Jr., Owsley C., Girkin C., Epstein D., Lee P.P. Statins and other cholesterol-lowering medications and the presence of glaucoma. Arch. Ophthalmol. 2004;122:822–826. doi: 10.1001/archopht.122.6.822. [DOI] [PubMed] [Google Scholar]
- 84.Song J., Deng P.F., Stinnett S.S., Epstein D.L., Rao P.V. Effects of cholesterol-lowering statins on the aqueous humor outflow pathway. Investig. Ophthalmol. Vis. Sci. 2005;46:2424–2432. doi: 10.1167/iovs.04-0776. [DOI] [PubMed] [Google Scholar]
- 85.Yeom S., Comi A.M. Updates on Sturge-Weber Syndrome. Stroke. 2022;53:3769–3779. doi: 10.1161/STROKEAHA.122.038585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Silverstein M., Salvin J. Ocular manifestations of Sturge-Weber syndrome. Curr. Opin. Ophthalmol. 2019;30:301–305. doi: 10.1097/ICU.0000000000000597. [DOI] [PubMed] [Google Scholar]
- 87.Shiau T., Armogan N., Yan D.B., Thomson H.G., Levin A.V. The role of episcleral venous pressure in glaucoma associated with Sturge-Weber syndrome. J. AAPOS. 2012;16:61–64. doi: 10.1016/j.jaapos.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 88.Phelps C.D. The pathogenesis of glaucoma in Sturge-Weber syndrome. Ophthalmology. 1978;85:276–286. doi: 10.1016/S0161-6420(78)35667-0. [DOI] [PubMed] [Google Scholar]
- 89.Shen C.C., Tsuei Y.S., Yang M.Y., You W.C., Sun M.H., Sheu M.L., Pan L.Y., Sheehan J., Pan H.C. Gamma Knife Radiosurgery for Indirect Dural Carotid-Cavernous Fistula: Long-Term Ophthalmological Outcome. Life. 2022;12:1175. doi: 10.3390/life12081175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Khurana M., Alam M.S., Balekudaru S., Vijaya L., Madhuri M.B., Halbe S.V., Noronha V.O., George R.J., Mukherjee B. Intraocular Pressure in the Eyes of Patients with Carotid-Cavernous Fistulas: Profile, Intereye Asymmetry, and Treatment Outcomes. J. Glaucoma. 2019;28:1074–1078. doi: 10.1097/IJG.0000000000001392. [DOI] [PubMed] [Google Scholar]
- 91.Buus D.R., Tse D.T., Parrish R.K. Spontaneous carotid cavernous fistula presenting with acute angle closure glaucoma. Arch. Ophthalmol. 1989;107:596–597. doi: 10.1001/archopht.1989.01070010610039. [DOI] [PubMed] [Google Scholar]
- 92.Fujitani A., Hayasaka S. Concurrent acute angle-closure glaucoma, choroidal detachment and exudative retinal detachment in a patient with spontaneous carotid cavernous fistula. Ophthalmologica. 1995;209:220–222. doi: 10.1159/000310618. [DOI] [PubMed] [Google Scholar]
- 93.Barke R.M., Yoshizumi M.O., Hepler R.S., Krauss H.R., Jabour B.A. Spontaneous dural carotid-cavernous fistula with central retinal vein occlusion and iris neovascularization. Ann. Ophthalmol. 1991;23:11–17. [PubMed] [Google Scholar]
- 94.Sugar H.S. Neovascular glaucoma after carotid-cavernous fistula formation. Ann. Ophthalmol. 1979;11:1667–1669. [PubMed] [Google Scholar]
- 95.Cymbor M., Knapp E., Carlin F. Idiopathic elevated episcleral venous pressure with secondary glaucoma. Optom. Vis. Sci. 2013;90:213–217. doi: 10.1097/OPX.0b013e31829689a6. [DOI] [PubMed] [Google Scholar]
- 96.Ganesh N., Alam M.S., George R.J., Balekudaru S., Vijaya L. Outcomes of medical and surgical management in eyes with idiopathic elevated episcleral venous pressure. Indian J. Ophthalmol. 2022;70:3316–3319. doi: 10.4103/ijo.IJO_2931_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Usha Tejaswini S., Sivakumar P., Upadhyaya S., Venkatesh R. Elevated episcleral venous pressure and its implications: A case of Radius-Maumenee syndrome. Indian J. Ophthalmol. 2020;68:1683–1685. doi: 10.4103/ijo.IJO_2407_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang S., Li X., Liu S., Zhang W., Li M., Qiao C. Research progress on the role of ET-1 in diabetic kidney disease. J. Cell. Physiol. 2023;10:1002. doi: 10.1002/jcp.31023. [DOI] [PubMed] [Google Scholar]
- 99.Imig J.D. Eicosanoid blood vessel regulation in physiological and pathological states. Clin. Sci. 2020;134:2707–2727. doi: 10.1042/CS20191209. [DOI] [PubMed] [Google Scholar]
- 100.Feng J., Liang L., Chen Y., Tian P., Zhao X., Huang B., Wu Y., Wang J., Guan J., Huang L. Big Endothelin-1 as a Predictor of Reverse Remodeling and Prognosis in Dilated Cardiomyopathy. J. Clin. Med. 2023;12:1363. doi: 10.3390/jcm12041363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lu Y.P., Hasan A.A., Zeng S., Hocher B. Plasma ET-1 Concentrations Are Elevated in Pregnant Women with Hypertension -Meta-Analysis of Clinical Studies. Kidney Blood Press. Res. 2017;42:654–663. doi: 10.1159/000482004. [DOI] [PubMed] [Google Scholar]
- 102.Gu X., Li H., Zhu X., Gu H., Chen J., Wang L., Harding P., Xu W. Inverse Correlation Between Plasma Adropin and ET-1 Levels in Essential Hypertension: A Cross-Sectional Study. Medicine. 2015;94:e1712. doi: 10.1097/MD.0000000000001712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Almeida I.N.F., Taniguchi E., Tito C.V.A., Dias D.T., Ushida M., Dorairaj S., Ritch R., Teixeira S.H., Paranhos A., Gracitelli C.P., Jr. Vascular parameters and endothelin-1 measurements in glaucoma patients with low- and high-tension optic disc hemorrhages. Sci. Rep. 2023;13:5023. doi: 10.1038/s41598-023-31682-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wenner M.M., Welti L.M., Dow C.A., Greiner J.J., Stauffer B.L., DeSouza C.A. Aerobic Exercise Training Reduces ET-1 mediated Vasoconstriction and Improves Endothelium-Dependent Vasodilation in Postmenopausal Women. Am. J. Physiol. Heart Circ. Physiol. 2023;324:732–738. doi: 10.1152/ajpheart.00674.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Van der Graaff D., Chotkoe S., De Winter B., De Man J., Casteleyn C., Timmermans J.P., Pintelon I., Vonghia L., Kwanten W.J., Francque S. Vasoconstrictor antagonism improves functional and structural vascular alterations and liver damage in rats with early NAFLD. JHEP Rep. Innov. Hepatol. 2022;4:100412. doi: 10.1016/j.jhepr.2021.100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lommatzsch C., Rothaus K., Schopmeyer L., Feldmann M., Bauer D., Grisanti S., Heinz C., Kasper M. Elevated endothelin-1 levels as risk factor for an impaired ocular blood flow measured by OCT-A in glaucoma. Sci. Rep. 2022;12:11801. doi: 10.1038/s41598-022-15401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Emre M., Orgül S., Haufschild T., Shaw S.G., Flammer J. Increased plasma endothelin-1 levels in patients with progressive open angle glaucoma. Br. J. Ophthalmol. 2005;89:60–63. doi: 10.1136/bjo.2004.046755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Orgül S., Cioffi G.A., Bacon D.R., Van Buskirk E.M. An endothelin-1-induced model of chronic optic nerve ischemia in rhesus monkeys. J. Glaucoma. 1996;5:135–138. [PubMed] [Google Scholar]
- 109.Orgül S., Cioffi G.A., Wilson D.J., Bacon D.R., Van Buskirk E.M. An endothelin-1 induced model of optic nerve ischemia in the rabbit. Investig. Ophthalmol. Vis. Sci. 1996;37:1860–1869. [PubMed] [Google Scholar]
- 110.Orgül S., Cioffi G.A., Wilson D.J., Bacon D.R., Van Buskirk E.M. Nitric oxide donating anti-glaucoma drugs: Advances and prospects. Chin. J. Nat. Med. 2020;18:275–283. doi: 10.1016/S1875-5364(20)30035-2. [DOI] [PubMed] [Google Scholar]
- 111.Toda N., Nakanishi-Toda M. Nitric oxide: Ocular blood flow, glaucoma, and diabetic retinopathy. Prog. Retin. Eye Res. 2007;26:205–238. doi: 10.1016/j.preteyeres.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 112.Urbonavičiūtė D., Buteikienė D., Janulevičienė I. A Review of Neovascular Glaucoma: Etiology, Pathogenesis, Diagnosis, and Treatment. Medicina. 2022;58:1870. doi: 10.3390/medicina58121870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Impagnatiello F., Bastia E., Almirante N., Brambilla S., Duquesroix B., Kothe A.C., Bergamini M.V.W. Prostaglandin analogues and nitric oxide contribution in the treatment of ocular hypertension and glaucoma. Br. J. Pharmacol. 2019;176:1079–1089. doi: 10.1111/bph.14328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nathanson J.A., McKee M. Alterations of ocular nitric oxide synthase in human glaucoma. Investig. Ophthalmol. Vis. Sci. 1995;36:1774–1784. [PubMed] [Google Scholar]
- 115.Kang J.H., Wiggs J.L., Rosner B.A., Hankinson S.E., Abdrabou W., Fan B.J., Haines J., Pasquale L.R. Endothelial nitric oxide synthase gene variants and primary open-angle glaucoma: Interactions with sex and postmenopausal hormone use. Investig. Ophthalmol. Vis. Sci. 2010;51:971–979. doi: 10.1167/iovs.09-4266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lei Y., Zhang X., Song M., Wu J., Sun X. Aqueous Humor Outflow Physiology in NOS3 Knockout Mice. Investig. Ophthalmol. Vis. Sci. 2015;56:4891–4898. doi: 10.1167/iovs.15-16564. [DOI] [PubMed] [Google Scholar]
- 117.Muenster S., Lieb W.S., Fabry G., Allen K.N., Kamat S.S., Guy A.H., Dordea A.C., Teixeira L., Tainsh R.E., Yu B. The Ability of Nitric Oxide to Lower Intraocular Pressure Is Dependent on Guanylyl Cyclase. Investig. Ophthalmol. Vis. Sci. 2017;58:4826–4835. doi: 10.1167/iovs.17-22168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Buys E.S., Potter L.R., Pasquale L.R., Ksander B.R. Regulation of intraocular pressure by soluble and membrane guanylate cyclases and their role in glaucoma. Front. Mol. Neurosci. 2014;7:38. doi: 10.3389/fnmol.2014.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim M.H., Lim S.-H. Matrix Metalloproteinases and Glaucoma. Biomolecules. 2022;12:1368. doi: 10.3390/biom12101368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kaufman P.L. Deconstructing aqueous humor outflow—The last 50 years. Exp. Eye Res. 2020;197:108105. doi: 10.1016/j.exer.2020.108105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bradley J.M., Vranka J., Colvis C.M., Conger D.M., Alexander J.P., Fisk A.S., Samples J.R., Acott T.S. Effect of matrix metalloproteinases activity on outflow in perfused human organ culture. Investig. Ophthalmol. Vis. Sci. 1998;39:2649–2658. [PubMed] [Google Scholar]
- 122.Snider E.J., Hardie B.A., Li Y., Gao K., Splaine F., Kim R.K., Vannatta R.T., Read A.T., Ethier C.R. A Porcine Organ-Culture Glaucoma Model Mimicking Trabecular Meshwork Damage Using Oxidative Stress. Investig. Ophthalmol. Vis. Sci. 2021;62:18. doi: 10.1167/iovs.62.3.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Arend O., Remky A., Plange N., Martin B.J., Harris A. Capillary density and retinal diameter measurements and their impact on altered retinal circulation in glaucoma: A digital fluorescein angiographic study. Br. J. Ophthalmol. 2002;86:429–433. doi: 10.1136/bjo.86.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tan B., MacLellan B., Mason E., Bizheva K.K. The Effect of Acutely Elevated Intraocular Pressure on the Functional and Blood Flow Responses of the Rat Retina to Flicker Stimulation. Investig. Ophthalmol. Vis. Sci. 2017;58:5532–5540. doi: 10.1167/iovs.17-22412. [DOI] [PubMed] [Google Scholar]
- 125.Jonas J.B., Nguyen X.N., Naumann G.O. Parapapillary retinal vessel diameter in normal and glaucoma eyes. I. Morphometric data. Investig. Ophthalmol. Vis. Sci. 1989;30:1599–1603. [PubMed] [Google Scholar]
- 126.Jonas J.B., Fernandez M.C., Naumann G.O. Parapapillary atrophy and retinal vessel diameter in nonglaucomatous optic nerve damage. Investig. Ophthalmol. Vis. Sci. 1991;32:2942–2947. [PubMed] [Google Scholar]
- 127.Rader J., Feuer W.J., Anderson D.R. Peripapillary vasoconstriction in the glaucomas and the anterior ischemic optic neuropathies. Am. J. Ophthalmol. 1994;117:72–80. doi: 10.1016/S0002-9394(14)73017-X. [DOI] [PubMed] [Google Scholar]
- 128.Papastathopoulos K.I., Jonas J.B. Follow up of focal narrowing of retinal arterioles in glaucoma. Br. J. Ophthalmol. 1999;83:285–289. doi: 10.1136/bjo.83.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zheng Y., Cheung N., Aung T., Mitchell P., He M., Wong T.Y. Relationship of retinal vascular caliber with retinal nerve fiber layer thickness: The singapore malay eye study. Investig. Ophthalmol. Vis. Sci. 2009;50:4091–4096. doi: 10.1167/iovs.09-3444. [DOI] [PubMed] [Google Scholar]
- 130.Frisen L., Claesson M. Narrowing of the retinal arterioles in descending optic atrophy. A quantitative clinical study. Ophthalmology. 1984;91:1342–1346. doi: 10.1016/S0161-6420(84)34144-6. [DOI] [PubMed] [Google Scholar]
- 131.Rankin S.J., Drance S.M. Peripapillary focal retinal arteriolar narrowing in open angle glaucoma. J. Glaucoma. 1996;5:22–28. doi: 10.1097/00061198-199602000-00005. [DOI] [PubMed] [Google Scholar]
- 132.Papastathopoulos K.I., Jonas J.B. Focal narrowing of retinal arterioles in optic nerve atrophy. Ophthalmology. 1995;102:1706–1711. doi: 10.1016/S0161-6420(95)30805-6. [DOI] [PubMed] [Google Scholar]
- 133.Shin J.W., Sung K.R., Uhm K.B., Jo J., Moon Y., Song M.K., Song J.Y. Peripapillary Microvascular Improvement and Lamina Cribrosa Depth Reduction after Trabeculectomy in Primary Open-Angle Glaucoma. Investig. Ophthalmol. Vis. Sci. 2017;58:5993–5999. doi: 10.1167/iovs.17-22787. [DOI] [PubMed] [Google Scholar]
- 134.Wang X., Jiang C., Kong X., Yu X., Sun X. Peripapillary retinal vessel density in eyes with acute primary angle closure: An optical coherence tomography angiography study. Graefe Arch. Clin. Exp. Ophthalmol. 2017;255:1013–1018. doi: 10.1007/s00417-017-3593-1. [DOI] [PubMed] [Google Scholar]
- 135.Tao X., Sigireddi R.R., Westenskow P.D., Channa R., Frankfort B.J. Single transient intraocular pressure elevations cause prolonged retinal ganglion cell dysfunction and retinal capillary abnormalities in mice. Exp. Eye Res. 2020;201:108296. doi: 10.1016/j.exer.2020.108296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zhao D., He Z., Wang L., Fortune B., Lim J.K.H., Wong V.H.Y., Nguyen C.T.O., Bui B.V. Response of the Trilaminar Retinal Vessel Network to Intraocular Pressure Elevation in Rat Eyes. Investig. Ophthalmol. Vis. Sci. 2020;61:2. doi: 10.1167/iovs.61.2.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Prokosch V., Brockhaus K., Anders F., Liu H., Mercieca K., Gericke A., Melkonyan H., Thanos S. Elevated intraocular pressure induces neuron-specific beta-III-tubulin expression in non-neuronal vascular cells. Acta Ophthalmol. 2020;98:617–630. doi: 10.1111/aos.14333. [DOI] [PubMed] [Google Scholar]
- 138.Stapor P.C., Murfee W.L. Identification of class III beta-tubulin as a marker of angiogenic perivascular cells. Microvasc. Res. 2012;83:257–262. doi: 10.1016/j.mvr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 139.Shao W., Sun K., Ma T., Jiang H., Hahn M., Ma Z., Jiao C., Yin Y. SUMOylation regulates low-temperature survival and oxidative DNA damage tolerance in Botrytis cinerea. New Phytol. 2023;238:817–834. doi: 10.1111/nph.18748. [DOI] [PubMed] [Google Scholar]
- 140.Ruiz-Ederra J., Verkman A.S. Mouse model of sustained elevation in intraocular pressure produced by episcleral vein occlusion. Exp. Eye Res. 2006;82:879–884. doi: 10.1016/j.exer.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 141.Kingston E.J., Lusthaus J.A. Two-year outcomes of patients presenting to Sydney Eye Hospital with neovascular glaucoma. Int. Ophthalmol. 2023;10:1007. doi: 10.1007/s10792-023-02675-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jabbehdari S., Yazdanpanah G., Cantor L.B., Hajrasouliha A.R. A narrative review on the association of high intraocular pressure and glaucoma in patients with retinal vein occlusion. Ann. Transl. Med. 2022;10:1072. doi: 10.21037/atm-22-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schwaber E.J., Fogelman N., Sobol E.K., Mehrotra D., Powell J.A., Mian U., Gritz D.C. Associations with retinal vascular occlusions in a diverse, urban population. Ophthalmic. Epidemiol. 2018;25:220–226. doi: 10.1080/09286586.2017.1406530. [DOI] [PubMed] [Google Scholar]
- 144.Klein R., Klein B.E., Moss S.E., Meuer S.M. The epidemiology of retinal vein occlusion: The Beaver Dam Eye Study. Trans. Am. Ophthalmol. Soc. 2000;98:133–143. [PMC free article] [PubMed] [Google Scholar]
- 145.Shin Y.U., Cho H., Kim J.M., Bae K., Kang M.H., Shin J.P., Nam E., Kang S.W., Epidemiologic Survey Committee of the Korean Ophthalmological Society Prevalence and associated factors of retinal vein occlusion in the Korean National Health and Nutritional Examination Survey, 2008–2012: A cross-sectional observational study. Medicine. 2016;95:e5185. doi: 10.1097/MD.0000000000005185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Yin X., Li J., Zhang B., Lu P. Association of glaucoma with risk of retinal vein occlusion: A meta-analysis. Acta Ophthalmol. 2019;97:652–659. doi: 10.1111/aos.14141. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.