Abstract
The continuous evolution of cancer biology has led to the discovery of mammaglobin, a potential novel biomarker for breast carcinoma. This review aims to unravel the enigmatic aspects of mammaglobin and elucidate its potential role in redefining the paradigm of breast carcinoma biomarkers. We will thoroughly examine its expression in tumoral and peritumoral tissues and its circulating levels in the blood, thereby providing insights into its possible function in cancer progression and metastasis. Furthermore, the potential application of mammaglobin as a non-invasive diagnostic tool and a target for personalized treatment strategies will be discussed. Given the increasing incidence of breast carcinoma worldwide, the exploration of novel biomarkers such as mammaglobin is crucial in advancing our diagnostic capabilities and treatment modalities, ultimately contributing to improved patient outcomes.
Keywords: mammaglobin, breast carcinoma, biomarker, tumoral expression, peritumoral expression, cancer progression, metastasis, diagnosis, treatment strategies
1. Introduction
Breast carcinoma is one of the most prevalent malignancies affecting women worldwide, posing significant challenges to early detection, accurate prognosis, and effective treatment [1,2]. Despite considerable advances in medical technologies, the quest for reliable and sensitive biomarkers that can aid in the early detection and monitoring of breast carcinoma remains of paramount importance [3]. Biomarkers not only provide insights into the pathophysiology of diseases but can also guide individualized treatment strategies, hence contributing to the overall improvement of patient outcomes [4].
In this intriguing quest, mammaglobin, a member of the secretoglobin family, has emerged as a potential novel biomarker [5]. Mammaglobin, also known as mammaglobin-A or SCGB2A2, belongs to a cluster of small secretory proteins [6]. It was first discovered in 1996 through a differential screening of a human breast carcinoma cDNA library, with its expression being predominantly limited to the mammary gland [7,8]. While its exact function remains somewhat elusive, mammaglobin is believed to play roles in various biological processes, including cell signaling, immune response, chemotaxis, and potentially hormone transport [8]. The protein is known to bind steroid-like molecules and is part of the secretoglobin family, which comprises over 20 related proteins [6,8]. The SCGB2A2 gene, located on chromosome 11q13, encodes mammaglobin, a 93-amino-acid secretory protein [5]. It is believed to play a role in the secretory processes of the mammary gland under normal circumstances [8]. However, it is frequently upregulated in instances of breast cancer, emphasizing its potential as a therapeutic target for these tumors [9].
Human mammaglobin (hMAG) is primarily a small epithelial secretory protein and a member of the uteroglobin/Clara cell protein family [6,10]. It possesses two N-linked glycosylation sites, contributing to the addition of approximately 3 kDa carbohydrate chains [11]. In breast tissue, hMAG-A protein exists in two forms with molecular masses of around 18 kDa and 25 kDa, both of which are more commonly found in breast carcinomas compared with fibroadenomas or normal breast tissues [9,11]. Interestingly, the expression of mammaglobin appears to be independent of steroid hormones and is potentially regulated by mechanisms involving Phosphoprotein Enriched in Astrocytes 3 (PEA-3) expression [9]. Molecular modeling studies suggest a structural arrangement of mammaglobin, with four alpha helices per protein forming a hydrophobic core in a head-to-tail orientation [9]. The presence of N-linked glycosylation sites at opposite ends of the complex, as well as in flexible loop regions between the alpha helices, allows for the extension of large carbohydrate chains in either direction [12]. Additionally, mammaglobin forms covalent heterodimers with lipophilin B, exhibiting an anti-parallel arrangement that facilitates the formation of three disulfide bridges between them [13].
Mammaglobin overexpression, particularly specific to breast cancer cells, lends its compelling potential as a unique biomarker for breast carcinoma [14]. Its detectability in peritumoral tissue and circulation suggests possible uses in a variety of clinical applications, including diagnosis, prognosis, and potential therapeutic targeting [9,15]. Yet, the mechanisms driving its overexpression and its role in tumorigenesis and cancer progression are subjects of ongoing research. Although variably detected on the membrane fraction of breast cancer cells and present in both normal and cancer cell surfaces and cytoplasm, the precise function and significance of mammaglobin-A in breast cancer pathogenesis are yet to be fully understood [12].
Despite these gaps, mammaglobin-A’s clinical relevance is undeniable given its overexpression in breast cancer [7]. Its potential utility as a diagnostic and prognostic biomarker is backed by numerous studies linking mammaglobin levels with clinical parameters like tumor stage and lymph node status [16,17].
This review seeks to demystify mammaglobin, a potential gamechanger in the landscape of breast carcinoma biomarkers. It explores mammaglobin’s expression in tumoral and peritumoral tissues and its circulating levels in blood, along with its implications in cancer progression and metastasis. As a prospective non-invasive diagnostic tool, mammaglobin could revolutionize early cancer detection and prognostic prediction and guide therapeutic strategies [3]. Given the global rise in breast carcinoma, examining innovative biomarkers like mammaglobin is crucial.
2. The Pivotal Role of Biomarkers in Breast Carcinoma
Breast carcinoma is a significant global health concern, posing challenges in early detection, prognostication, and targeted therapies [18]. The risk of distant recurrence persists even five years post-diagnosis, necessitating the exploration of biomarkers for improved patient outcomes [19]. Biomarkers, measurable indicators of physiological or pathological processes, hold promise in revolutionizing breast cancer care by elucidating underlying disease mechanisms, facilitating early diagnosis, and tracking disease progression [20]. Their detection in non-invasive samples such as blood and urine enables early disease identification, thus promoting prompt intervention and a more favorable prognosis [3].
Various biomarkers like estrogen and progesterone receptors (ER and PR), gross cystic disease fluid protein-15 (GCDFP-15), and others have traditionally been employed in diagnosing and prognosticating breast cancer [21,22]. Yet, current markers, including carcinoembryonic antigen (CEA) and CA 15-3 (CA27-29), display limited sensitivity and specificity, necessitating improved diagnostic precision [23,24]. Numerous proposed biomarkers aim to improve detection but lack sufficient sensitivity and specificity to be clinically beneficial [3]. Prognostic indicators such as ER, PR, and HER2/neu and multigene panels like Oncotype DX have been instrumental in treatment planning and predicting disease outcomes, but they have limitations in accuracy and tissue specificity [25,26,27,28]. A comparative analysis of these traditional markers, including their specific remarks, can be found in Table 1. Consequently, research focuses on identifying innovative biomarkers with better sensitivity, specificity, and tissue specificity [29]. Human mammaglobin (hMAG), a promising candidate, is currently under investigation for its potential utility in diagnosis, prognosis, and therapy in breast cancer [9].
Table 1.
Comparative analysis of human mammaglobin and other breast cancer markers.
| Tumour Marker | Specific Remarks |
|---|---|
| Carcinoembryonic antigen (CEA) | Noted for its involvement in recurrence and correlation with circulating tumor cell discovery, yet its sensitivity is considered low [23]. |
| Cytokeratins (CK19 and CK20) | Known for their low sensitivity, these markers can be found in both normal cells and a variety of tumors [30]. |
| Epidermal growth factor receptor (EGFR) | Similar to cytokeratins, EGFR presents with low sensitivity and can be identified in normal cells and various tumors [31]. |
| Maspin | This marker is associated with a reduced risk of recurrence [32]. |
| Polymorphic epithelial mucin (MUC-1) | Adverse outcomes are linked to high pre-operative CA 15-3 levels. CA27-29 offers little utility. Low sensitivity and expression in normal cells and hematological tumors are its key characteristics [33,34]. |
| B726P | When used in tandem with hMAG, B726P could aid in distinguishing between mammary and non-mammary tissues [35]. |
| Urokinase plasminogen activator (uPA) | The presence of this marker might provide valuable information for prognosis [36]. |
| Plasminogen activator inhibitor 1 (PAI-1) | Similar to uPA, PAI-1 can be helpful in determining prognosis [37]. |
| Estrogen receptor (ER) | Detectable in primary lung adenocarcinomas, ER is used for predicting hormonal therapy responses in breast cancer despite its limited prognostic significance [38]. |
| Progesterone receptor (PR) | PR is considered a key factor for hormonal therapy [39]. |
| Human epidermal growth factor receptor-2 (HER-2) | Human epidermal growth factor receptor-2 (HER-2) is highly expressed in breast cancers with an amplified ERBB2 gene, i.e., those of the HER2 molecular subtype, making HER-2 instrumental in the selection process for Herceptin therapy [40]. |
| Breast cancer 1 and 2 early onset (BRAC-1 and BRAC-2) | These markers can assist in identifying high-risk patients [41]. |
| Small breast epithelial mucin (SBEM) | SBEM is detectable in roughly 52% of breast tumors, with no presence in non-breast tumors [42]. |
| Survivin | This marker does not have specificity for breast cancer [43]. |
| Ki67 | Ki67 is thought to act as an indicator of breast cancer progression [44]. |
| Gross cystic disease fluid protein 15 (GCDFP-15) | This marker is noted for its significant link with mammary differentiation and has shown a correlation with mammaglobin expression. Research is ongoing into its potential as a breast cancer biomarker [45]. |
| Human mammaglobin (hMAG) | hMAG exhibits high expression (80–90%) in breast tumors and is particularly sensitive (97%) in detecting residual disease [9]. |
3. Expression Patterns of Mammaglobin-A in Diverse Human Tissues
Studies by Watson and Fleming explored mammaglobin-A mRNA expression in a variety of human tissues, both fetal and adult, primarily through RT-PCR and Northern blotting techniques [12,14]. They found that mammaglobin-A’s expression is predominantly restricted to the adult mammary gland, believed to be associated with the gland’s proliferation and terminal differentiation [12]. Further research corroborated the overexpression of mammaglobin-A in breast tumors, with about 80% exhibiting this characteristic [9]. This overexpression was found to be unrelated to breast carcinogenesis, but increased expression in breast tumors was associated with less aggressive tumor phenotypes and significantly higher in estrogen receptor-positive tumors [46].
Beyond breast tissue, mammaglobin-A has been detected in normal and cancerous tissues of the female genital tract and the sweat and salivary glands [8]. Its expression in breast tissue, however, significantly outpaces that in ovarian and endometrial tissues [8]. Immunostaining has revealed mammaglobin-A expression in a few normal tissue types like the luminal cells of the breast, endocervical glands, endometrium, and more [8,47]. Despite its presence in other tissues, mammaglobin-A’s expression is exceptionally specific to breast cancer, leading to its proposition as a potential marker for identifying circulating and disseminated tumor cells and verifying the breast origin of metastatic cancer [5,11].
4. Tumoral Expression of Mammaglobin
Mammaglobin, a potential biomarker for breast carcinoma, has drawn significant interest because of its overexpression in primary and metastatic breast cancer tissues and specificity to mammary tissue [7,9]. Numerous studies show high levels of mammaglobin in a considerable percentage of breast carcinomas, with variations based on tumor subtype and stage [8,46]. Its expression in other malignancies is largely minimal, heightening its appeal as a specific breast carcinoma biomarker [8]. There is a demonstrated correlation between high mammaglobin expression and adverse prognostic factors, implying a role in disease pathogenesis and progression [8,15]. However, the exact role and mechanisms of mammaglobin’s overexpression in breast carcinoma are unclear, and its non-universal overexpression could limit its standalone biomarker utility.
4.1. Mammaglobin in Breast Carcinoma Tissue: Its Potential Role as a Marker
Mammaglobin, known to exist in two isotypes, mammaglobin-A (MAM-A) and mammaglobin-B (MAM-B), presents distinct roles in cancer biology [48]. MAM-A, predominantly expressed in breast tissue, has been found in approximately 80% of breast tumors, showing an overexpression of up to 10 times compared with normal breast tissue [11,46]. This significant upregulation suggests that MAM-A is a potential molecular diagnostic marker for breast cancer [46]. Variability exists in the prevalence of MAM-A expression, with positivity rates ranging from 59% to 100% for lobular breast carcinomas and 25% to 94% for invasive breast carcinomas of no specific type [8]. On the other hand, MAM-B has been observed in a variety of cancer types, suggesting its role extends beyond breast cancer [46].
MAM-A, a highly specific marker for breast tissue, demonstrates significant potential, though it is not a perfect diagnostic marker, as it is not expressed in all breast cancer cell lines and tumors [5]. mRNA expression in mammaglobin in breast cancer cells is significantly elevated compared with non-malignant breast tissue [49]. This overexpression, likely modulated by intricate transcription mechanisms, has important implications [12]. Mammaglobin-A has been identified as an important predictor for bone metastases in breast cancer, and its expression pattern could aid in personalizing postoperative adjuvant treatment planning [15].
Interestingly, the mammaglobin protein complex in breast tumors appears to provoke an immune response, activating mammaglobin-reactive CD8+ and CD4+ T cells [50]. This immune response could reflect antitumor activity, with a potential correlation between the number of these cells and disease outcomes or recurrence. Antibodies against the mammaglobin complex have been found in the sera of breast cancer patients [11,51]. Levels of these antibodies correlate with disease stages, with higher antibody levels against a component called lipophilin B seen in advanced stages [52]. Antibodies specifically targeting mammaglobin are lower, possibly because of its high degree of glycosylation [11].
The overexpression of MAM-A is associated with high tumor grades, indicating its potential as a poor prognosis marker [53]. Numerous studies have demonstrated a positive correlation between MAM-A positivity and breast cancer stages [11,53]. Patients with MAM-A-positive invasive breast cancer typically present with larger tumors, higher histological grading, and a higher Ki-67 proliferation index, indicative of high cell proliferation [53].
The reduced expression of proteins typically found in tumor cells suggests tumor cell dedifferentiation, often linked to unfavorable tumor characteristics [54]. This might explain the associations between decreased MAM-A expression and high tumor grades or unfavorable molecular parameters in breast cancer [8]. Breast cancer patients with moderate MAM-A staining on their tumors have demonstrated the best patient outcomes, hinting that both the upregulation and downregulation of MAM-A could be linked to tumor progression [8]. The downregulation of MAM-A has been observed in 49% of breast cancers [8].
Mammaglobin Expression and Its Correlation with Hormone Receptor Status in Breast Cancer
Research has evidenced an association between elevated mammaglobin expression and the presence of pivotal hormone-responsive markers, specifically estrogen and progesterone receptors, in cases of breast cancer [51]. This elevated expression has also been connected to diploid DNA content, low cell proliferation rates, low nuclear grades, and the absence of axillary nodal invasion, hinting at a less aggressive tumor phenotype [11]. Additionally, several studies have indicated higher mammaglobin positivity rates in patients with estrogen receptor (ER)-positive tumors, suggesting a link between mammaglobin expression and estrogen responsiveness [53].
However, the connection between mammaglobin expression and ER status is complex, with some studies associating mammaglobin expression with negative ER status [55]. This inconsistency could be attributed to variations in study design, patient populations, or mammaglobin measurement methods. Consequently, further research is needed to elucidate the intricate relationship between mammaglobin and hormone receptor status in breast cancer.
4.2. Peritumoral Expression of Mammaglobin: A New Dimension in Breast Carcinoma Research
Peritumoral tissues, or tumor microenvironments, which are composed of various cell types and extracellular matrix components, play a vital role in cancer progression, influencing tumor growth, invasiveness, and metastatic potential [56]. The expression of mammaglobin in these tissues introduces an intriguing aspect to its potential as a biomarker [15]. Initial research has found mammaglobin to be present in these areas, suggesting a possible link to local invasion, metastasis, and aggressive disease phenotypes [15].
However, the exact role of mammaglobin in the peritumoral environment is still undefined. It is uncertain whether mammaglobin’s expression in these tissues results from the tumor’s influence or if it actively shapes the tumor microenvironment [15]. Likewise, the cell types expressing mammaglobin in the peritumoral environment and its potential role in modulating the local environment to support tumor growth and spread remain unclear. These questions highlight the need for further research in this area.
In a study investigating mammaglobin levels in breast cancer patients, it was found that mammaglobin concentrations were elevated in both peritumoral and carcinoma tissues compared with healthy individuals, showing a correlation between tumor size and the likelihood of lymphatic metastasis [15]. However, the study did not specify the cellular source of mammaglobin expression in these tissues.
In contrast, in a study conducted by Leygue et al. using in situ hybridization on 13 breast tumor tissues, mammaglobin expression was found specifically in tumor epithelial cells, with no expression detected in stromal or inflammatory cells [57].
While both studies underscore the presence and potential relevance of mammaglobin in breast cancer tissues, they highlight different aspects: one emphasizes its potential prognostic value and correlation with certain tumor characteristics, while the other identifies the specific cell type expressing mammaglobin within the tumor. The apparent discrepancy in the cellular source might be due to differences in the methodologies used or the specific tissue samples analyzed in each study.
As we delve deeper into the association between mammaglobin-A expression and various aspects of breast cancer, Table 2 provides a succinct summary of these relationships. The table categorizes key prognostic factors, including tumor subtype and stage, hormone receptor status, tumor grade, cell proliferation, and peritumoral expression. It outlines the correlation between these factors and mammaglobin-A expression, highlighting how varying expression levels can impact the pathogenesis and progression of the disease. This overview underscores the potential role of mammaglobin-A as a significant biomarker in breast cancer diagnosis and prognosis.
Table 2.
Mammaglobin-A expression and correlation with breast cancer prognostic factors.
| Prognostic Factor | Mammaglobin-A Expression |
|---|---|
| Tumor Subtype and Stage | Variable expression with positivity rates ranging from 59% to 100% for lobular breast carcinomas and 25% to 94% for invasive breast carcinomas |
| Hormone Receptor Status | Elevated levels correlate with estrogen receptor (ER) and progesterone receptor (PR) status |
| Tumor Grade | High tumor grade associated with overexpression of human mammaglobin (hMAM) |
| Cell Proliferation | Higher Ki-67 proliferation index observed in hMAM-positive invasive breast cancer |
| Peritumoral Expression | Presence detected, suggesting a possible link with local invasion, metastasis, and aggressive disease phenotypes |
5. Mammaglobin Expression in Metastatic Breast Carcinoma: Potential Implications for Disease Detection and Monitoring
Breast cancer is a prevalent disease among women in the United States and is the second leading cause of cancer-related deaths [58]. While early-stage diagnoses provide hopeful prospects for successful treatment through surgical intervention, about half of the patients experience recurrence, often because of undetectable microscopic metastases present at the initial diagnosis stage [59,60]. These micrometastases, although clinically hidden, pose a significant challenge, as they can continue to grow and potentially lead to disease relapse, thus undermining the effectiveness of current treatment strategies [61].
To combat this, research aims to enhance the early detection and monitoring of micrometastases, which could allow for earlier intervention and potentially prevent disease recurrence [62]. Hence, advancements in diagnostic methods are crucial for identifying these metastatic cells and creating targeted therapeutic strategies [63]. Understanding the mechanisms underlying micrometastasis progression and developing novel detection and elimination strategies are vital areas of research, carrying the potential to significantly improve patient outcomes by reducing recurrence risk and offering more effective treatment options [64].
The metastasis process in breast tumors is complex and involves multiple biological events, all of which are influenced by various factors, critical for both the diagnosis and prognosis of the disease [65]. The overexpression of mammaglobin has been observed in metastatic breast carcinoma, suggesting its potential role in the metastatic process and indicating its potential use in monitoring disease progression and responses to treatment [7,66]. However, the mechanisms underlying mammaglobin’s overexpression in primary and metastatic breast carcinoma are still unclear, warranting further research to comprehend its role in the initiation, progression, and metastasis of breast carcinoma.
In an effort to understand the broad implications of mammaglobin in the metastatic process, we summarize the current knowledge about its role in different metastatic contexts in Table 3. This table underscores the value of mammaglobin as a marker, the methods of its detection, specific findings, and potential implications in the management of metastatic breast carcinoma.
Table 3.
Mammaglobin as a marker in different contexts of metastatic breast carcinoma.
| Metastatic Context | Method of Detection | Specific Findings | Potential Implications |
|---|---|---|---|
| Lymph Node Metastasis | VivoTag-S 680, RT-PCR | Presence in positive lymph nodes, absent in normal/sentinel nodes | Guiding surgical decisions, improved prognosis |
| Circulating Mammaglobin | RT-PCR | Detected in 25% of patients | Potential diagnostic marker |
| Circulating Tumor Cells (CTCs) | RT-PCR (hMAM mRNA) | hMAM mRNA expressed in 70–80% of breast cancers | Indicates a higher number of CTCs and a higher risk of advanced disease progression |
| Bone Marrow Metastasis | Bone marrow aspirates, immunohistochemical staining | Mammaglobin expression is higher in patients with metastasis | Potential marker for metastasis |
In the following sections, we will further explore mammaglobin expression in different contexts, such as lymph node metastases, circulating tumor cells, and bone marrow metastases.
5.1. Mammaglobin: A Promising Marker for Lymph Node Metastasis in Breast Cancer
Metastasis detection in axillary lymph nodes is vital for breast cancer management, with a growing emphasis on sentinel lymph node biopsy for accurate prediction and clinical advantages [67]. Mammaglobin-A has emerged as a valuable marker for identifying breast cancer metastasis and micrometastases, offering superior sensitivity compared with other markers [7]. Its presence has been recognized in breast cancer-positive lymph node samples, whereas it is absent in normal or sentinel lymph nodes without detectable tumor cells [9]. The innovative use of a near-infrared fluorescent dye, VivoTag-S 680, conjugated to a monoclonal antibody against human mammaglobin-A, has shown promise in the non-invasive detection of metastasis in lymph nodes in animal models [68].
The application of multiple markers, including mammaglobin, cytokeratin 19, and carcinoembryonic antigen (CEA), has been proposed for guiding surgical decisions on axillary lymph node dissection in breast cancer [69,70]. In this context, while cytokeratin 19 has shown more specificity than mammaglobin in lymph node detection, mammaglobin’s detection in sentinel lymph nodes has been more informative than both cytokeratin 19 and CEA [71,72]. This suggests that mammaglobin could be a valuable molecular marker for detecting breast cancer in sentinel lymph nodes, potentially improving patient prognosis.
Innovative techniques like in vivo fluorescence imaging, leveraging a mammaglobin-A-specific monoclonal antibody conjugated to a near-infrared fluorescent dye, might reduce the need for surgical examination [73]. These techniques offer robust tools for studying tumor cells within the lymphatic system, detecting tumor cells in lymph nodes, and monitoring antitumor therapy [73]. Furthermore, the detection of minimal breast cancer mRNA markers like mammaglobin-A mRNA can aid in investigating node micrometastasis [12]. Real-time reverse transcription polymerase chain reaction (RT-PCR) can assist in detecting metastases in sentinel lymph nodes of breast cancer patients during surgery [12].
The use of RT-PCR to detect mammaglobin expression has been invaluable for identifying occult metastases in the lymph nodes of breast cancer patients [11]. Mammaglobin was first suggested as a marker for nodal metastases by Min et al., who found it to be expressed in all tested breast cancer cell lines but absent in normal lymph nodes [74]. Mammaglobin B (MAG-B) has also been identified as a useful marker for detecting histology-positive lymph node samples, despite its significant homology with mammaglobin-A [11].
Recent advancements in high-throughput RT-PCR protocols are promising for intraoperative sentinel lymph node analysis [70]. The practice of sentinel lymph node biopsy (SLNB) provides valuable prognostic information on metastatic spread with minimal associated morbidity [75]. In this regard, mammaglobin RT-PCR has displayed higher sensitivity compared with conventional histology [69]. Combining multiple markers, including mammaglobin, has been proposed for lymph node analysis, with real-time multigene RT-PCR assays showing excellent sensitivity and specificity [35]. Human mammaglobin (hMAM) mRNA overexpression has shown consistent alignment with lymph node metastasis, with hMAM protein levels found to be significantly high in patients with carcinoma in situ (CIS), invasive carcinoma (IC), and metastatic disease [49,51].
5.2. Circulating Mammaglobin: A Potential Diagnostic Marker for Breast Cancer
Mammaglobin has garnered growing research interest because of its presence in the bloodstream [12,15]. Notably, mammaglobin RT-PCR has been utilized to identify circulating mammary carcinoma cells in the blood samples of breast cancer patients [11,49]. One study reported sensitivity equivalent to detecting a single tumor cell among 106–107 white blood cells, with mammaglobin mRNA detected in 25% of patients, displaying variations based on clinical stages and disease status [76].
Researchers have also examined mammaglobin protein levels in the serum for potential diagnostic applications [11]. Utilizing monoclonal antibodies specific to recombinant mammaglobin, the protein was detected in 33% of primary breast cancer serum and 44% of metastatic breast cancer serum samples, suggesting that elevated mammaglobin protein levels could serve as a diagnostic marker [14].
Mammaglobin and Circulating Tumor Cells (CTCs): A Novel Diagnostic Avenue in Breast Cancer
Circulating tumor cells (CTCs), cancer cells that have detached from the primary tumor and entered the bloodstream, are significant contributors to cancer metastasis and are linked to worse clinical outcomes [77]. Recognized as crucial in cancer progression and patient prognosis, these cells provide insights into tumor molecular makeup and aid in personalized therapeutic decisions [78]. Mammaglobin, particularly its human form, hMAM mRNA, has gained attention as a potential marker for CTCs because of its breast-specific expression [49,53]. Elevated hMAM mRNA levels in leucocytes may indicate a higher number of CTCs, suggesting a higher risk of advanced disease progression [79].
The development of reverse transcriptase polymerase chain reaction (RT-PCR) technology has enabled the detection of specific tumor-related genes like mammaglobin in cancer patients’ blood, including those with metastatic breast cancer [53,80]. This has led to the identification and quantification of CTCs, offering valuable information about disease progression and overall survival [53]. However, hMAM mRNA detection methods can overlook tumor cells from hMAM-negative tumors, given that hMAM mRNA is only expressed in 70–80% of primary and metastatic breast cancer tissues [53]. To overcome this, a multi-gene RT-PCR assay has been proposed for the more sensitive and reliable detection of circulating breast cancer cells, showing increased detection sensitivity and providing significant prognostic information [53].
5.3. Mammaglobin: A Potential Indicator for Bone Marrow Metastasis in Breast Cancer
Breast cancer research advances have significantly improved patient survival rates over the past few decades, especially for localized disease [81]. However, survival rates decrease dramatically with metastatic lesions, highlighting the need for reliable early detection methods [82]. Mammaglobin, a breast-tissue-specific antigen found in the bone marrow of breast cancer patients, is under investigation as a potential marker for breast cancer metastasis given its higher expression rates in patients with metastasis and progressive disease [83].
While some reports suggest that cytokines might induce mammaglobin expression in non-cancerous bone marrow and peripheral stem cells, leading to false positives, research by Silva et al. did not detect mammaglobin transcripts in bone marrow samples from normal donors [83,84]. Instead, they identified mammaglobin expression in bone marrow aspirates from breast cancer patients, particularly those with metastatic disease [84]. Despite mammaglobin’s potential as a metastasis marker, more research is needed to confirm its specificity and establish its clinical utility, especially as immunohistochemical staining for MAM-A in bone marrow could be more sensitive in detecting early bone marrow micrometastases.
6. Mammaglobin in Breast Cancer: A Multifaceted Entity
In the complex and multifarious landscape of breast cancer, mammaglobin plays a critical yet not entirely understood role [9]. This member of the secretoglobin family has shown significant promise in various capacities, from contributing to our understanding of the biological underpinnings of breast cancer to potentially guiding prognosis and therapy [51]. In the following sections, we delve into the intricate biological function of mammaglobin and how its varied expression might impact the prognosis of breast cancer patients. We will further explore mammaglobin’s potential role as a therapeutic target, while also examining its expression in other carcinomas. By comprehensively examining these different dimensions, we aim to offer a nuanced perspective of mammaglobin in the context of breast cancer.
6.1. The Biological Function of Mammaglobin in Breast Carcinoma: A Dual Role
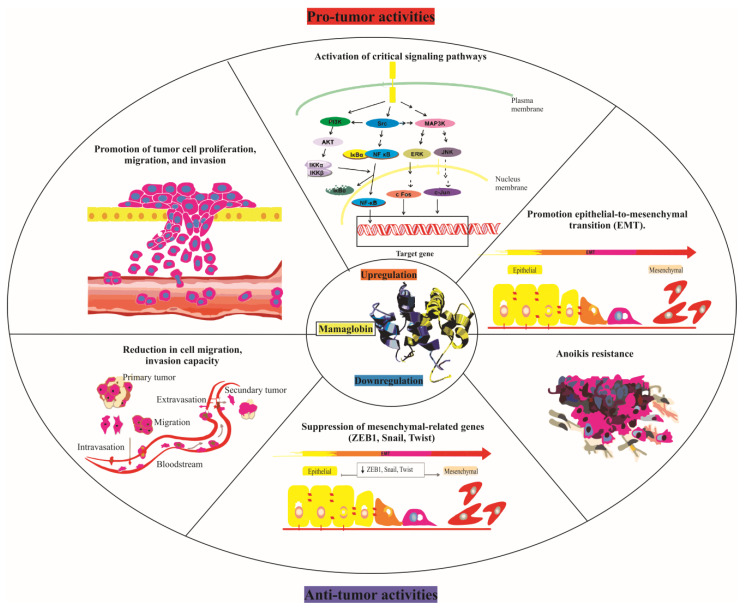
The role of mammaglobin, especially mammaglobin-A, in breast cancer is complex, modulating processes like cell proliferation, migration, and invasion [8]. Although it exhibits both pro-tumor and anti-tumor activities, the mechanisms behind the impact of its upregulation on cancer aggressiveness remain to be fully understood (Figure 1). A study by Picot et al. suggested that mammaglobin-A can promote tumor cell proliferation, migration, and invasion, activating several critical signaling pathways such as mitogen-activated protein kinase (MAPK), focal adhesion kinase (FAK), matrix metalloproteinases (MMPs), and nuclear factor kappa B (NF-κB), all essential in cancer development and metastasis [85].
Figure 1.
Pro-tumor and anti-tumor activities of mammaglobin-A. The upper half of the figure depicts the pro-tumor activities triggered by mammaglobin-A upregulation. This includes the promotion of tumor cell proliferation, migration, and invasion; the activation of critical signaling pathways such as MAPK, FAK, MMPs, and NF-κB; and the initiation of epithelial-to-mesenchymal transition (EMT). Conversely, the lower half illustrates the anti-tumor activities resulting from mammaglobin-A downregulation. This encompasses the suppression of mesenchymal-related genes (ZEB1, Snail, Twist) and a decrease in cell migration, invasion capacity, and anoikis resistance subsequent to hMAG-A suppression. This figure thereby underlines the dual and contrasting roles of mammaglobin-A in tumor dynamics, dependent on its regulation.
Mammaglobin-A also seems to regulate the epithelial-to-mesenchymal transition (EMT), a process tied to increased cancer cell invasiveness and metastatic potential [17]. This idea is supported by the observed suppression of mesenchymal-related genes like Zinc Finger E-box-binding Homeobox 1 (ZEB1), Snail, and Twist following the inhibition of mammaglobin-A expression. Mammaglobin-A (MAG-A) also appears to play a significant role in breast cancer cell growth and survival, with the suppression of MAG-A expression in the aggressive MB231 breast cancer cell line resulting in attenuated cell growth [85].
Additionally, reduced MAG-A expression has been linked to decreased cell migration, invasion capacity, and anoikis resistance in the MB231 cell line [85]. This reduction correlates with decreased matrix metalloproteinases (MMP-9 and MMP-2) and decreased focal adhesion kinase (FAK) activity, proteins known for promoting invasive behavior [85]. MAG-A also seems to influence gene expression profiles associated with epithelial-mesenchymal transition (EMT) and mesenchymal–epithelial transition (MET) [85].
Interestingly, decreased mammaglobin expression has been associated with increased resistance to apoptosis and altered responses to chemotherapeutic drugs in breast cancer cells [85]. Furthermore, chronic treatment with trastuzumab, a common breast cancer drug, has been linked to increased MAG-A expression in HER2-positive/ER-negative breast cancer cells, potentially enhancing their proliferation, migration, and invasion capacities and potentially contributing to trastuzumab resistance [86]. In conclusion, mammaglobin, particularly MAG-A, plays a multifaceted role in breast cancer, influencing tumor aggressiveness, chemosensitivity, apoptosis resistance, and metastatic disease progression, which warrants further investigation.
6.2. Expression of Mammaglobin-A in Other Carcinomas
Mammaglobin-A, a protein markedly present in an array of tumors, is predominantly observed in cancers originating from the salivary glands, breasts, endometrium, and ovaries [8]. Its detection relies on a method known as immunohistochemistry. Nearly 99% of tumors that test positive for mammaglobin-A are found within these four organs [8]. Nonetheless, this protein is also detected, although to a lesser degree, in other, less frequent cancer types [8].
Aside from breast cancer, varying degrees of mammaglobin-A presence have been documented in cancers like uterine endometrium carcinomas, ovarian carcinomas, and prostatic adenocarcinomas [8]. The observed variations in mammaglobin-A expression are attributed to differences in the antibodies used, the immunostaining protocols implemented, and the criteria set for defining the staining outcomes. Remarkably, there is an absolute absence of mammaglobin-A immunostaining in several non-breast and non-gynecological cancers, underlining the diagnostic utility of mammaglobin-A immunohistochemistry, especially for gynecological tumors [8].
Interestingly, studies have shown links between low or non-existent mammaglobin-A immunostaining and advanced tumor stages across various types of cancers [12]. However, these associations do not necessarily translate to correlations with overall survival. Differing results across various studies examining mammaglobin-A expression in tumors are primarily due to disparities in the antibodies used, staining protocols followed, and what constitutes a “positive” case. Despite this, the expression pattern of mammaglobin-A in tumors generally mirrors that in normal tissues, providing invaluable insights into the role of mammaglobin-A across a spectrum of cancers [8].
6.3. Mammaglobin-A as a Promising Therapeutic Target in Breast Cancer
Mammaglobin-A (MAM-A), a secretoglobin protein consisting of 93 amino acids, offers promising potential as a target for breast cancer vaccine therapy because of its high expression in breast cancers and minimal presence in healthy tissues [87]. Its high immunogenicity allows for the generation of MAM-A-specific CD8+ and CD4+ T cells that recognize and target MAM-A-expressing breast cancers [88]. However, the endogenous immune response to MAM-A seems insufficient to eliminate developing breast cancers, potentially because of insufficient MAM-A-specific T cells, inadequate infiltration into the tumor microenvironment (TME), or downregulation due to immunoregulatory elements [87].
Previous research has managed to induce MAM-A-specific CD8+ T cells through DNA vaccination, with a phase 1 clinical trial involving 15 patients demonstrating no severe toxicities and an increase in peripheral MAM-A-specific T cells [89]. This trial also reported an increase in ICOShiCD4+ T cells and a decrease in Foxp3+CD4+ T cells six months post-vaccination [89]. In eight vaccinated patients expressing HLA-A 0201, a significant increase in MAM-A-specific CD8 T cells was noted, and their cytotoxic activity against breast cancer cell lines displayed efficacy dependent on certain parameters [89].
The effectiveness of MAM-A-specific CD8+ T cells hinges not only on population expansion but also on the modulation of regulatory networks within the TME [87]. Associations have been made between lower levels of certain tumor-associated macrophages and lymphocytes and longer recurrence-free survival [87]. Despite encouraging preliminary results, further research is needed to elucidate interactions between the MAM-A vaccine and the TME’s regulatory networks and to explore the specific signaling pathways involved in the expression of MAM-A in breast cancer tissues.
6.4. Mammaglobin as a Potential Target for Breast Cancer Immunotherapy
Mammaglobin, a mammary-specific antigen, has been spotlighted as a promising target for breast cancer immunotherapy because of its elevated expression in breast cancer tissues relative to normal tissues [9]. This heightened expression enhances the prospects of developing effective targeted therapies, including vaccine-based approaches such as the MAM-A DNA vaccine [90,91]. Such vaccines are crafted to stimulate the immune system, prompting it to recognize and attack tumor cells by presenting tumor-associated antigens. The overarching goal is to halt tumor progression and eradicate existing malignancies, offering a new horizon in the therapeutic landscape for breast cancer.
Human MAM-A holds promise in spearheading effective therapies and vaccines against breast cancer cells. This potential arises from targeting mammaglobin-derived epitopes on cytotoxic T-lymphocytes for the effective delivery of targeted interventions. The strategic focus includes utilizing a transmembrane N-terminal domain of MAM-A or MAM-A-derived epitopes in association with HLA-A-2, HLA-A-3, and HLA-A-24 to evoke CD8-restricted responses [90,91,92,93,94,95].
Being a membrane-associated protein, MAM-A might serve as an invaluable molecular marker for devising targeted drug therapies specific to breast cancer [96]. Furthermore, its potential is also underscored in crafting experimental vaccines against breast cancer cells [90]. Techniques such as stimulating CD4+CD25− T cells in vitro with MAM-A-pulsed antigen-presenting cells or transducing dendritic cells with Tat-MAM-A have been explored [91,97]. Notably, the ability of MAM-A to bind to breast cancer cells has also raised intriguing propositions regarding its potential role in guiding radioisotopes or toxins to specifically target these malignant cells [98].
Several therapeutic strategies leveraging MAM-A have been proposed, including the innovative use of the MAM-A promoter to facilitate gene therapy. This approach might deliver oncolytic viruses or toxic genes directly to mammary tumors [99]. Additionally, combining targets like MAM-A with other markers such as HER-2/neu in active immunotherapy could potentially amplify the therapeutic vaccine’s efficacy and bolster specific T cells for adoptive immunotherapy, especially in treating established metastatic diseases [100]. It is worth noting, however, that recent findings suggest inducing the overexpression of MAM-a in breast cancer cells might diminish their metastatic potential, offering another intriguing avenue for managing aggressive forms of breast cancer [101].
7. Current Challenges and Future Perspectives
Despite the optimistic potential of mammaglobin as a breast carcinoma biomarker, several crucial challenges persist:
Sensitivity and Specificity: Enhancing the sensitivity and specificity of mammaglobin detection in breast carcinoma is imperative. Future studies need to concentrate on refining the techniques used in mammaglobin detection to boost accuracy.
Method Standardization: Currently, a universal protocol for detecting and quantifying mammaglobin across diverse sample types is absent, creating hurdles for comparison between studies. The establishment of shared protocols should be prioritized.
Biological Role Comprehension: The biological role mammaglobin plays in breast carcinoma is not entirely clear. Clarifying its exact function could offer critical insights into its effectiveness as a diagnostic and prognostic marker and potential as a therapeutic target.
Moving forward, the realm of mammaglobin research reveals a number of thrilling prospects:
Early Detection and Diagnosis: Enhanced detection methods could pave the way for the use of mammaglobin as a non-invasive biomarker for the early detection and diagnosis of breast carcinoma.
Prognostic Marker: Mammaglobin may become a valuable prognostic marker if larger prospective studies substantiate the link between its levels and disease progression/outcomes.
Personalized Therapy: If mammaglobin is proven to be integral to the pathogenesis of breast carcinoma, it could be considered a target for personalized therapies.
Companion Diagnostic Tool: In conjunction with other established biomarkers, mammaglobin could serve as a companion diagnostic tool to improve diagnostic accuracy and inform treatment choices.
The potential for mammaglobin to serve as a biomarker for breast carcinoma holds promise, yet its realization hinges on rigorous, continued research to surmount current obstacles and validate its clinical application. Should these challenges be resolved, mammaglobin could herald a new phase in breast carcinoma management, offering tools for early detection, precise prognosis, and personalized treatment.
Table 4 summarizes the main challenges and prospects associated with mammaglobin as a biomarker for breast carcinoma. It provides an overview of current obstacles to its implementation, as well as its potential future applications, highlighting the need for ongoing research in this field.
Table 4.
Challenges and prospects of mammaglobin in breast carcinoma.
| Area | Challenge/Prospect | Description |
|---|---|---|
| Sensitivity and Specificity | Challenge | Enhancing the detection accuracy of mammaglobin in breast carcinoma |
| Method Standardization | Challenge | Establishing a universal protocol for detecting and quantifying mammaglobin |
| Biological Role Comprehension | Challenge | Understanding the exact role of mammaglobin in breast carcinoma |
| Early Detection and Diagnosis | Prospect | Using mammaglobin as a non-invasive biomarker for early detection and diagnosis |
| Prognostic Marker | Prospect | Establishing mammaglobin as a valuable prognostic marker through larger prospective studies |
| Personalized Therapy | Prospect | Exploring mammaglobin as a potential target for personalized therapies |
| Companion Diagnostic Tool | Prospect | Utilizing mammaglobin alongside other established biomarkers to improve diagnostic accuracy and inform treatment choices |
8. Conclusions
Mammaglobin, a breast-tissue-specific biomarker, offers transformative potential in breast carcinoma diagnosis, prognosis, and treatment, albeit with a few challenges. While its detection in various samples, including tumor tissues, peritumoral regions, and circulating blood, promises a broad application, improving its detection sensitivity and specificity, standardizing detection protocols, and understanding its biological role are essential steps toward realizing its full potential. Despite these hurdles, mammaglobin research holds exciting promise for breast carcinoma management, offering a vision of early detection, accurate prognosis, and personalized treatment. In the face of challenges and opportunities, continued investment in mammaglobin research is essential, driving us toward the ultimate goal of improved patient outcomes in breast carcinoma.
Acknowledgments
The authors would like to express their gratitude to the Faculty of Medical Sciences, University of Kragujevac, for their unwavering support. The resources and facilities provided by the institution have been instrumental in the completion of this work.
Author Contributions
In this review article, B.M. and B.S. contributed equally to the work. They were responsible for the conceptualization, organization, and analysis of the reviewed literature. A.C., I.J. and M.S. (Marko Spasic) contributed to the selection of relevant studies and data extraction. M.D.S., D.L., V.S. and M.S. (Marija Sekulic) provided critical insights and interpretations of the reviewed data. M.S. (Marko Spasic), B.S.S. and N.Z. were responsible for the writing and editing of the manuscript. M.M., D.L., J.S., M.V. and D.C. were responsible for the overall project administration and supervision. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
As this is a review article, it does not contain any new, original research data. Instead, it synthesizes and analyzes previously published data and information. All data and materials discussed in this review are cited appropriately and can be found in the referenced articles and resources. Therefore, a data availability statement is not applicable to this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Financial support for this study was provided by the Ministry of Science, Technological Development, and Innovation of the Republic of Serbia, under the agreement referenced as contract number 451-03-47/2023-01/200111, and additionally from the Junior Project of the Faculty of Medical Sciences at the University of Kragujevac, Serbia (JP17/19).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Łukasiewicz S., Czeczelewski M., Forma A., Baj J., Sitarz R., Stanisławek A. Breast Cancer-Epidemiology, Risk Factors, Classification, Prognostic Markers, and Current Treatment Strategies—An Updated Review. Cancers. 2021;13:4287. doi: 10.3390/cancers13174287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim Y.X., Lim Z.L., Ho P.J., Li J. Breast Cancer in Asia: Incidence, Mortality, Early Detection, Mammography Programs, and Risk-Based Screening Initiatives. Cancers. 2022;14:4218. doi: 10.3390/cancers14174218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li J., Guan X., Fan Z., Ching L.M., Li Y., Wang X., Cao W.M., Liu D.X. Non-Invasive Biomarkers for Early Detection of Breast Cancer. Cancers. 2020;12:2767. doi: 10.3390/cancers12102767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patani N., Martin L.A., Dowsett M. Biomarkers for the clinical management of breast cancer: International perspective. Int. J. Cancer. 2013;133:1–13. doi: 10.1002/ijc.27997. [DOI] [PubMed] [Google Scholar]
- 5.Zafrakas M., Petschke B., Donner A., Fritzsche F., Kristiansen G., Knüchel R., Dahl E. Expression analysis of mammaglobin A (SCGB2A2) and lipophilin B (SCGB1D2) in more than 300 human tumors and matching normal tissues reveals their co-expression in gynecologic malignancies. BMC Cancer. 2006;6:88. doi: 10.1186/1471-2407-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jackson B.C., Thompson D.C., Wright M.W., McAndrews M., Bernard A., Nebert D.W., Vasiliou V. Update of the human secretoglobin (SCGB) gene superfamily and an example of ‘evolutionary bloom’ of androgen-binding protein genes within the mouse Scgb gene superfamily. Hum. Genom. 2011;5:691–702. doi: 10.1186/1479-7364-5-6-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Z., Spaulding B., Sienko A., Liang Y., Li H., Nielsen G., Yub Gong G., Ro J.Y., Jim Zhai Q. Mammaglobin, a valuable diagnostic marker for metastatic breast carcinoma. Int. J. Clin. Exp. Pathol. 2009;2:384–389. [PMC free article] [PubMed] [Google Scholar]
- 8.Gorbokon N., Timm P., Dum D., Menz A., Büscheck F., Völkel C., Hinsch A., Lennartz M., Luebke A.M., Hube-Magg C., et al. Mammaglobin-A Expression Is Highly Specific for Tumors Derived from the Breast, the Female Genital Tract, and the Salivary Gland. Diagnostics. 2023;13:1202. doi: 10.3390/diagnostics13061202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Joudi F.S. Human mammaglobin in breast cancer: A brief review of its clinical utility. Indian J. Med. Res. 2014;139:675–685. [PMC free article] [PubMed] [Google Scholar]
- 10.Klug J., Beier H., Bernard A., Chilton B., Fleming T., Lehrer R., Miele L., Pattabiraman N., Singh G. Uteroglobin/Clara Cell 10—kDa Family of Proteins: Nomenclature Committee Report. Ann. New York Acad. Sci. 2000;923:348–354. doi: 10.1111/j.1749-6632.2000.tb05549.x. [DOI] [PubMed] [Google Scholar]
- 11.Zehentner B.K., Carter D. Mammaglobin: A candidate diagnostic marker for breast cancer. Clin. Biochem. 2004;37:249–257. doi: 10.1016/j.clinbiochem.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Ghersevich S., Ceballos M.P. Mammaglobin A: Review and clinical utility. Adv. Clin. Chem. 2014;64:241–268. [PubMed] [Google Scholar]
- 13.Carter D., Valliere-Douglass J., Cornellison C., Retter M., Johnson J., Bennington A., Fleming T., Reed S., Houghton R., Diamond D., et al. Purification and Characterization of the Mammaglobin/Lipophilin B Complex, a Promising Diagnostic Marker for Breast Cancer. Biochemistry. 2002;41:6714–6722. doi: 10.1021/bi0159884. [DOI] [PubMed] [Google Scholar]
- 14.Fleming T.P., Watson M.A. Mammaglobin, a breast-specific gene, and its utility as a marker for breast cancer. Ann. N. Y. Acad. Sci. 2000;923:78–89. doi: 10.1111/j.1749-6632.2000.tb05521.x. [DOI] [PubMed] [Google Scholar]
- 15.Milosevic B., Cvetkovic A., Ninkovic S., Markovic S., Mitrovic S., Stojanovic B., Radunovic A., Vulovic M., Cvetkovic D. Mammaglobin expression in tissue as a predictor of breast carcinoma aggressiveness. Vojnosanit. Pregl. 2021;78:160–170. doi: 10.2298/VSP190129046M. [DOI] [Google Scholar]
- 16.Monsalve-Lancheros A., Ibáñez-Pinilla M., Ramírez-Clavijo S. Detection of mammagloblin by RT-PCR as a biomarker for lymph node metastasis in breast cancer patients: A systematic review and meta-analysis. PLoS ONE. 2019;14:e0216989. doi: 10.1371/journal.pone.0216989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu Y., Liu P., Wu D., Jiang Y. Prognostic role of plasma mammaglobin A expression in breast carcinoma patients: A meta-analysis. Onco Targets Ther. 2018;11:3245–3255. doi: 10.2147/OTT.S156556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilkinson L., Gathani T. Understanding breast cancer as a global health concern. Br. J. Radiol. 2022;95:20211033. doi: 10.1259/bjr.20211033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richman J., Dowsett M. Beyond 5 years: Enduring risk of recurrence in oestrogen receptor-positive breast cancer. Nat. Rev. Clin. Oncol. 2019;16:296–311. doi: 10.1038/s41571-018-0145-5. [DOI] [PubMed] [Google Scholar]
- 20.Li G., Hu J., Hu G. Biomarker Studies in Early Detection and Prognosis of Breast Cancer. Adv. Exp. Med. Biol. 2017;1026:27–39. doi: 10.1007/978-981-10-6020-5_2. [DOI] [PubMed] [Google Scholar]
- 21.Darb-Esfahani S., von Minckwitz G., Denkert C., Ataseven B., Högel B., Mehta K., Kaltenecker G., Rüdiger T., Pfitzner B., Kittel K., et al. Gross cystic disease fluid protein 15 (GCDFP-15) expression in breast cancer subtypes. BMC Cancer. 2014;14:546. doi: 10.1186/1471-2407-14-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caselli E., Pelliccia C., Teti V., Bellezza G., Mandarano M., Ferri I., Hartmann K., Laible M., Sahin U., Varga Z., et al. Looking for more reliable biomarkers in breast cancer: Comparison between routine methods and RT-qPCR. PLoS ONE. 2021;16:e0255580. doi: 10.1371/journal.pone.0255580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anoop T.M., Joseph P.R., Soman S., Chacko S., Mathew M. Significance of serum carcinoembryonic antigen in metastatic breast cancer patients: A prospective study. World J. Clin. Oncol. 2022;13:529–539. doi: 10.5306/wjco.v13.i6.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin D., Genzen J. Comparison of Breast Cancer Tumor Marker Test Results: A Retrospective Analysis of Paired CA 15-3 and CA 27.29 Testing at a National Reference Laboratory. Am. J. Clin. Pathol. 2017;147:S156. doi: 10.1093/ajcp/aqw191.009. [DOI] [Google Scholar]
- 25.Pal M., Muinao T., Boruah H.P.D., Mahindroo N. Current advances in prognostic and diagnostic biomarkers for solid cancers: Detection techniques and future challenges. Biomed. Pharmacother. 2022;146:112488. doi: 10.1016/j.biopha.2021.112488. [DOI] [PubMed] [Google Scholar]
- 26.Győrffy B., Hatzis C., Sanft T., Hofstatter E., Aktas B., Pusztai L. Multigene prognostic tests in breast cancer: Past, present, future. Breast Cancer Res. 2015;17:11. doi: 10.1186/s13058-015-0514-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sinn P., Aulmann S., Wirtz R., Schott S., Marmé F., Varga Z., Lebeau A., Kreipe H., Schneeweiss A. Multigene Assays for Classification, Prognosis, and Prediction in Breast Cancer: A Critical Review on the Background and Clinical Utility. Geburtshilfe Frauenheilkd. 2013;73:932–940. doi: 10.1055/s-0033-1350831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thibodeau S., Voutsadakis I.A. The Oncotype Dx Assay in ER-Positive, HER2-Negative Breast Cancer Patients: A Real Life Experience from a Single Cancer Center. Eur. J. Breast Health. 2019;15:163–170. doi: 10.5152/ejbh.2019.4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarhadi V.K., Armengol G. Molecular Biomarkers in Cancer. Biomolecules. 2022;12:1021. doi: 10.3390/biom12081021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehrpouya M., Pourhashem Z., Yardehnavi N., Oladnabi M. Evaluation of cytokeratin 19 as a prognostic tumoral and metastatic marker with focus on improved detection methods. J. Cell. Physiol. 2019;234:21425–21435. doi: 10.1002/jcp.28768. [DOI] [PubMed] [Google Scholar]
- 31.Masuda H., Zhang D., Bartholomeusz C., Doihara H., Hortobagyi G.N., Ueno N.T. Role of epidermal growth factor receptor in breast cancer. Breast Cancer Res. Treat. 2012;136:331–345. doi: 10.1007/s10549-012-2289-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferrucci P.F., Rabascio C., Gigli F., Corsini C., Giordano G., Bertolini F., Martinelli G. A new comprehensive gene expression panel to study tumor micrometastasis in patients with high-risk breast cancer. Int. J. Oncol. 2007;30:955–962. doi: 10.3892/ijo.30.4.955. [DOI] [PubMed] [Google Scholar]
- 33.Duffy M.J. Serum tumor markers in breast cancer: Are they of clinical value? Clin. Chem. 2006;52:345–351. doi: 10.1373/clinchem.2005.059832. [DOI] [PubMed] [Google Scholar]
- 34.Corradini P., Voena C., Astolfi M., Delloro S., Pilotti S., Arrigoni G., Bregni M., Pileri A., Gianni A.M. Maspin and mammaglobin genes are specific markers for RT-PCR detection of minimal residual disease in patients with breast cancer. Ann. Oncol. 2001;12:1693–1698. doi: 10.1023/A:1013573108945. [DOI] [PubMed] [Google Scholar]
- 35.Zehentner B.K., Persing D.H., Deme A., Toure P., Hawes S.E., Brooks L., Feng Q., Hayes D.C., Critichlow C.W., Houghton R.L., et al. Mammaglobin as a novel breast cancer biomarker: Multigene reverse transcription-PCR assay and sandwich ELISA. Clin. Chem. 2004;50:2069–2076. doi: 10.1373/clinchem.2004.038687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Banys-Paluchowski M., Witzel I., Aktas B., Fasching P.A., Hartkopf A., Janni W., Kasimir-Bauer S., Pantel K., Schön G., Rack B., et al. The prognostic relevance of urokinase-type plasminogen activator (uPA) in the blood of patients with metastatic breast cancer. Sci. Rep. 2019;9:2318. doi: 10.1038/s41598-018-37259-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duffy M.J. Urokinase plasminogen activator and its inhibitor, PAI-1, as prognostic markers in breast cancer: From pilot to level 1 evidence studies. Clin. Chem. 2002;48:1194–1197. doi: 10.1093/clinchem/48.8.1194. [DOI] [PubMed] [Google Scholar]
- 38.Zhou Y., Zhou J., Xiao J., Wang Y., Wang H., Shi H., Yue C., Jia F., Li P., Hu Z., et al. Prognostic Relevance of Estrogen Receptor Status in Circulating Tumor Cells in Breast Cancer Patients Treated With Endocrine Therapy. Front. Oncol. 2022;12:866293. doi: 10.3389/fonc.2022.866293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li Z., Wei H., Li S., Wu P., Mao X. The Role of Progesterone Receptors in Breast Cancer. Drug Des. Dev. Ther. 2022;16:305–314. doi: 10.2147/DDDT.S336643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Iqbal N., Iqbal N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol. Biol. Int. 2014;2014:852748. doi: 10.1155/2014/852748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mehrgou A., Akouchekian M. The importance of BRCA1 and BRCA2 genes mutations in breast cancer development. Med. J. Islam. Repub. Iran. 2016;30:369. [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Z.Z., Xie X.D., Qu S.X., Zheng Z.D., Wang Y.K. Small breast epithelial mucin (SBEM) has the potential to be a marker for predicting hematogenous micrometastasis and response to neoadjuvant chemotherapy in breast cancer. Clin. Exp. Metastasis. 2010;27:251–259. doi: 10.1007/s10585-010-9323-2. [DOI] [PubMed] [Google Scholar]
- 43.Lv Y.G., Yu F., Yao Q., Chen J.H., Wang L. The role of survivin in diagnosis, prognosis and treatment of breast cancer. J. Thorac. Dis. 2010;2:100–110. [PMC free article] [PubMed] [Google Scholar]
- 44.Davey M.G., Hynes S.O., Kerin M.J., Miller N., Lowery A.J. Ki-67 as a Prognostic Biomarker in Invasive Breast Cancer. Cancers. 2021;13:4455. doi: 10.3390/cancers13174455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kinoshita M., Sawabe M., Soejima Y., Mieno M.N., Arai T., Honma N. Gross Cystic Disease Fluid Protein-15 (GCDFP-15) Expression Characterizes Breast Mucinous Carcinomas in Older Women. Diagnostics. 2022;12:3129. doi: 10.3390/diagnostics12123129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker E., Whiteoak N., Hall L., France J., Wilson D., Bhaskar P. Mammaglobin-A, VEGFR3, and Ki67 in Human Breast Cancer Pathology and Five Year Survival. Breast Cancer. 2019;13:1178223419858957. doi: 10.1177/1178223419858957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Onuma K., Dabbs D.J., Bhargava R. Mammaglobin expression in the female genital tract: Immunohistochemical analysis in benign and neoplastic endocervix and endometrium. Int. J. Gynecol. Pathol. 2008;27:418–425. doi: 10.1097/PGP.0b013e31815d05ec. [DOI] [PubMed] [Google Scholar]
- 48.Watson M.A., Fleming T.P. Mammaglobin, a mammary-specific member of the uteroglobin gene family, is overexpressed in human breast cancer. Cancer Res. 1996;56:860–865. [PubMed] [Google Scholar]
- 49.Nguyen H.M., Dao M.Q. Detection of human mammaglobin mRNA in breast cancer cells among Vietnamese women. Breast Cancer. 2019;11:143–150. doi: 10.2147/BCTT.S193777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaramillo A., Majumder K., Manna P.P., Fleming T.P., Doherty G., Dipersio J.F., Mohanakumar T. Identification of HLA-A3-restricted CD8+ T cell epitopes derived from mammaglobin-A, a tumor-associated antigen of human breast cancer. Int. J. Cancer. 2002;102:499–506. doi: 10.1002/ijc.10736. [DOI] [PubMed] [Google Scholar]
- 51.Galvis-Jiménez J.M., Curtidor H., Patarroyo M.A., Monterrey P., Ramírez-Clavijo S.R. Mammaglobin peptide as a novel biomarker for breast cancer detection. Cancer Biol. Ther. 2013;14:327–332. doi: 10.4161/cbt.23614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carter D., Dillon D.C., Reynolds L.D., Retter M.W., Fanger G., Molesh D.A., Sleath P.R., McNeill P.D., Vedvick T.S., Reed S.G., et al. Serum antibodies to lipophilin B detected in late stage breast cancer patients. Clin. Cancer Res. 2003;9:749–754. [PubMed] [Google Scholar]
- 53.Li G., Zhang J., Jin K., He K., Wang H., Lu H., Teng L. Human mammaglobin: A superior marker for reverse-transcriptase PCR in detecting circulating tumor cells in breast cancer patients. Biomark. Med. 2011;5:249–260. doi: 10.2217/bmm.11.20. [DOI] [PubMed] [Google Scholar]
- 54.Friedmann-Morvinski D., Verma I.M. Dedifferentiation and reprogramming: Origins of cancer stem cells. EMBO Rep. 2014;15:244–253. doi: 10.1002/embr.201338254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O’Brien N., Maguire T.M., O’Donovan N., Lynch N., Hill A.D., McDermott E., O’Higgins N., Duffy M.J. Mammaglobin a: A promising marker for breast cancer. Clin. Chem. 2002;48:1362–1364. doi: 10.1093/clinchem/48.8.1362. [DOI] [PubMed] [Google Scholar]
- 56.Neophytou C.M., Panagi M., Stylianopoulos T., Papageorgis P. The Role of Tumor Microenvironment in Cancer Metastasis: Molecular Mechanisms and Therapeutic Opportunities. Cancers. 2021;13:2053. doi: 10.3390/cancers13092053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leygue E., Snell L., Dotzlaw H., Hole K., Troup S., Hiller-Hitchcock T., Murphy L.C., Watson P.H. Mammaglobin, a potential marker of breast cancer nodal metastasis. J. Pathol. 1999;189:28–33. doi: 10.1002/(SICI)1096-9896(199909)189:1<28::AID-PATH389>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 58.Ataollahi M.R., Sharifi J., Paknahad M.R., Paknahad A. Breast cancer and associated factors: A review. J. Med. Life. 2015;8:6–11. [PMC free article] [PubMed] [Google Scholar]
- 59.Birnbaum J.K., Duggan C., Anderson B.O., Etzioni R. Early detection and treatment strategies for breast cancer in low-income and upper middle-income countries: A modelling study. Lancet Glob. Health. 2018;6:e885–e893. doi: 10.1016/S2214-109X(18)30257-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Riggio A.I., Varley K.E., Welm A.L. The lingering mysteries of metastatic recurrence in breast cancer. Br. J. Cancer. 2021;124:13–26. doi: 10.1038/s41416-020-01161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zanghì G., Di Stefano G., Caponnetto A., Vecchio R., Lanaia A., La Terra A., Leanza V., Basile F. Breast cancer and sentinel lymph node micrometastases: Indications for lymphadenectomy and literature review. G. Chir. 2014;35:260–265. [PMC free article] [PubMed] [Google Scholar]
- 62.Graham L.J., Shupe M.P., Schneble E.J., Flynt F.L., Clemenshaw M.N., Kirkpatrick A.D., Gallagher C., Nissan A., Henry L., Stojadinovic A., et al. Current approaches and challenges in monitoring treatment responses in breast cancer. J. Cancer. 2014;5:58–68. doi: 10.7150/jca.7047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ganesh K., Massagué J. Targeting metastatic cancer. Nat. Med. 2021;27:34–44. doi: 10.1038/s41591-020-01195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fares J., Fares M.Y., Khachfe H.H., Salhab H.A., Fares Y. Molecular principles of metastasis: A hallmark of cancer revisited. Signal Transduct. Target. Ther. 2020;5:28. doi: 10.1038/s41392-020-0134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Redig A.J., McAllister S.S. Breast cancer as a systemic disease: A view of metastasis. J. Intern. Med. 2013;274:113–126. doi: 10.1111/joim.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chivukula M., Dabbs D.J. Chapter 21—Immunocytology. In: Dabbs D.J., editor. Diagnostic Immunohistochemistry. 3rd ed. W.B. Saunders; Philadelphia, PA, USA: 2011. pp. 890–918. [Google Scholar]
- 67.Maguire A., Brogi E. Sentinel lymph nodes for breast carcinoma: An update on current practice. Histopathology. 2016;68:152–167. doi: 10.1111/his.12853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leung K. Molecular Imaging and Contrast Agent Database (MICAD) National Center for Biotechnology Information (US); Bethesda, MD, USA: 2004. VivoTag-S 680-anti-human mammaglobin-A monoclonal antibody. [PubMed] [Google Scholar]
- 69.Gillanders W.E., Mikhitarian K., Hebert R., Mauldin P.D., Palesch Y., Walters C., Urist M.M., Mann G.B., Doherty G., Herrmann V.M., et al. Molecular detection of micrometastatic breast cancer in histopathology-negative axillary lymph nodes correlates with traditional predictors of prognosis: An interim analysis of a prospective multi-institutional cohort study. Ann. Surg. 2004;239:828–837; discussion 837–840. doi: 10.1097/01.sla.0000128687.59439.d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shang J., Zhao M., Deng H., Liu C., Cai L., Liu Y. A clinical diagnostic test on the detection of sentinel lymph node metastasis in breast neoplasms using a 1-step RT-PCR. Gland. Surg. 2022;11:1628–1638. doi: 10.21037/gs-22-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Berger J., Mueller-Holzner E., Fiegl H., Marth C., Daxenbichler G. Evaluation of three mRNA markers for the detection of lymph node metastases. Anticancer Res. 2006;26:3855–3860. [PubMed] [Google Scholar]
- 72.Gimbergues P., Dauplat M.M., Cayre A., Durando X., Le Bouedec G., Finat-Duclos F., Portefaix G., Kwiatkowski F., Dauplat J., Penault-Llorca F., et al. Correlation between molecular metastases in sentinel lymph nodes of breast cancer patients and St Gallen risk category. Eur. J. Surg. Oncol. 2007;33:16–22. doi: 10.1016/j.ejso.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 73.Tafreshi N.K., Enkemann S.A., Bui M.M., Lloyd M.C., Abrahams D., Huynh A.S., Kim J., Grobmyer S.R., Carter W.B., Vagner J., et al. A mammaglobin-A targeting agent for noninvasive detection of breast cancer metastasis in lymph nodes. Cancer Res. 2011;71:1050–1059. doi: 10.1158/0008-5472.CAN-10-3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Min C.J., Tafra L., Verbanac K.M. Identification of superior markers for polymerase chain reaction detection of breast cancer metastases in sentinel lymph nodes. Cancer Res. 1998;58:4581–4584. [PubMed] [Google Scholar]
- 75.Harrison B. Update on sentinel node pathology in breast cancer. Semin. Diagn. Pathol. 2022;39:355–366. doi: 10.1053/j.semdp.2022.06.016. [DOI] [PubMed] [Google Scholar]
- 76.Zach O., Kasparu H., Krieger O., Hehenwarter W., Girschikofsky M., Lutz D. Detection of circulating mammary carcinoma cells in the peripheral blood of breast cancer patients via a nested reverse transcriptase polymerase chain reaction assay for mammaglobin mRNA. J. Clin. Oncol. 1999;17:2015–2019. doi: 10.1200/JCO.1999.17.7.2015. [DOI] [PubMed] [Google Scholar]
- 77.Lin D., Shen L., Luo M., Zhang K., Li J., Yang Q., Zhu F., Zhou D., Zheng S., Chen Y., et al. Circulating tumor cells: Biology and clinical significance. Signal Transduct. Target. Ther. 2021;6:404. doi: 10.1038/s41392-021-00817-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pantel K., Alix-Panabières C. Crucial roles of circulating tumor cells in the metastatic cascade and tumor immune escape: Biology and clinical translation. J. Immunother. Cancer. 2022;10:e005615. doi: 10.1136/jitc-2022-005615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li C., Zhang T. Human mammaglobin: A specific marker for breast cancer prognosis. J. Buon. 2016;21:35–41. [PubMed] [Google Scholar]
- 80.Fabisiewicz A., Kulik J., Kober P., Brewczyńska E., Pieńkowski T., Siedlecki J.A. Detection of circulating breast cancer cells in peripheral blood by a two-marker reverse transcriptase-polymerase chain reaction assay. Acta Biochim. Pol. 2004;51:747–755. doi: 10.18388/abp.2004_3559. [DOI] [PubMed] [Google Scholar]
- 81.Guo F., Kuo Y.F., Shih Y.C.T., Giordano S.H., Berenson A.B. Trends in breast cancer mortality by stage at diagnosis among young women in the United States. Cancer. 2018;124:3500–3509. doi: 10.1002/cncr.31638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ginsburg O., Yip C.H., Brooks A., Cabanes A., Caleffi M., Dunstan Yataco J.A., Gyawali B., McCormack V., McLaughlin de Anderson M., Mehrotra R., et al. Breast cancer early detection: A phased approach to implementation. Cancer. 2020;126((Suppl. S10)):2379–2393. doi: 10.1002/cncr.32887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Talaat I.M., Hachim M.Y., Hachim I.Y., Ibrahim R.A.E., Ahmed M., Tayel H.Y. Bone marrow mammaglobin-1 (SCGB2A2) immunohistochemistry expression as a breast cancer specific marker for early detection of bone marrow micrometastases. Sci. Rep. 2020;10:13061. doi: 10.1038/s41598-020-70012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Silva A.L., Tomé M.J., Correia A.E., Passos-Coelho J.L. Human mammaglobin RT-PCR assay for detection of occult breast cancer cells in hematopoietic products. Ann. Oncol. 2002;13:422–429. doi: 10.1093/annonc/mdf107. [DOI] [PubMed] [Google Scholar]
- 85.Picot N., Guerrette R., Beauregard A.P., Jean S., Michaud P., Harquail J., Benzina S., Robichaud G.A. Mammaglobin 1 promotes breast cancer malignancy and confers sensitivity to anticancer drugs. Mol. Carcinog. 2016;55:1150–1162. doi: 10.1002/mc.22358. [DOI] [PubMed] [Google Scholar]
- 86.Kusumastuti R., Kumagai Y., Ishihara S., Enomoto A., Murakami T., Yasuda M., Haga H. Mammaglobin 1 mediates progression of trastuzumab-resistant breast cancer cells through regulation of cyclins and NF-κB. FEBS Open Bio. 2022;12:1797–1813. doi: 10.1002/2211-5463.13468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kim S.W., Goedegebuure P., Gillanders W.E. Mammaglobin-A is a target for breast cancer vaccination. Oncoimmunology. 2016;5:e1069940. doi: 10.1080/2162402X.2015.1069940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Riazi Rad F., Ajdary S., Omranipour R., Alimohammadian M.H., Hassan Z.M. Comparative analysis of CD4+ and CD8+ T cells in tumor tissues, lymph nodes and the peripheral blood from patients with breast cancer. Iran Biomed. J. 2015;19:35–44. doi: 10.6091/ibj.1289.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tiriveedhi V., Fleming T.P., Goedegebuure P.S., Naughton M., Ma C., Lockhart C., Gao F., Gillanders W.E., Mohanakumar T. Mammaglobin-A cDNA vaccination of breast cancer patients induces antigen-specific cytotoxic CD4+ICOShi T cells. Breast Cancer Res. Treat. 2013;138:109–118. doi: 10.1007/s10549-012-2110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bharat A., Benshoff N., Fleming T.P., Dietz J.R., Gillanders W.E., Mohanakumar T. Characterization of the role of CD8+T cells in breast cancer immunity following mammaglobin-A DNA vaccination using HLA-class-I tetramers. Breast Cancer Res. Treat. 2008;110:453–463. doi: 10.1007/s10549-007-9741-2. [DOI] [PubMed] [Google Scholar]
- 91.Narayanan K., Jaramillo A., Benshoff N.D., Campbell L.G., Fleming T.P., Dietz J.R., Mohanakumar T. Response of established human breast tumors to vaccination with mammaglobin-A cDNA. J. Natl. Cancer Inst. 2004;96:1388–1396. doi: 10.1093/jnci/djh261. [DOI] [PubMed] [Google Scholar]
- 92.Ilias Basha H., Tiriveedhi V., Fleming T.P., Gillanders W.E., Mohanakumar T. Identification of immunodominant HLA-B7-restricted CD8+ cytotoxic T cell epitopes derived from mammaglobin-A expressed on human breast cancers. Breast Cancer Res. Treat. 2011;127:81–89. doi: 10.1007/s10549-010-0975-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tanaka Y., Amos K.D., Fleming T.P., Eberlein T.J., Goedegebuure P.S. Mammaglobin-A is a tumor-associated antigen in human breast carcinoma. Surgery. 2003;133:74–80. doi: 10.1067/msy.2003.92. [DOI] [PubMed] [Google Scholar]
- 94.Jaramillo A., Narayanan K., Campbell L.G., Benshoff N.D., Lybarger L., Hansen T.H., Fleming T.P., Dietz J.R., Mohanakumar T. Recognition of HLA-A2-restricted mammaglobin-A-derived epitopes by CD8+ cytotoxic T lymphocytes from breast cancer patients. Breast Cancer Res. Treat. 2004;88:29–41. doi: 10.1007/s10549-004-8918-1. [DOI] [PubMed] [Google Scholar]
- 95.Manna P.P., Jaramillo A., Majumder K., Campbell L.G., Fleming T.P., Dietz J.R., Dipersio J.F., Mohanakumar T. Generation of CD8+ cytotoxic T lymphocytes against breast cancer cells by stimulation with mammaglobin-A-pulsed dendritic cells. Breast Cancer Res. Treat. 2003;79:133–136. doi: 10.1023/A:1023323509888. [DOI] [PubMed] [Google Scholar]
- 96.Zuo L., Li L., Wang Q., Fleming T.P., You S. Mammaglobin as a potential molecular target for breast cancer drug delivery. Cancer Cell Int. 2009;9:8. doi: 10.1186/1475-2867-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Viehl C.T., Tanaka Y., Chen T., Frey D.M., Tran A., Fleming T.P., Eberlein T.J., Goedegebuure P.S. Tat mammaglobin fusion protein transduced dendritic cells stimulate mammaglobin-specific CD4 and CD8 T cells. Breast Cancer Res. Treat. 2005;91:271–278. doi: 10.1007/s10549-005-0450-4. [DOI] [PubMed] [Google Scholar]
- 98.Goedegebuure P.S., Watson M.A., Viehl C.T., Fleming T.P. Mammaglobin-based strategies for treatment of breast cancer. Curr. Cancer Drug Targets. 2004;4:531–542. doi: 10.2174/1568009043332862. [DOI] [PubMed] [Google Scholar]
- 99.Shi C.X., Long M.A., Liu L., Graham F.L., Gauldie J., Hitt M.M. The human SCGB2A2 (mammaglobin-1) promoter/enhancer in a helper-dependent adenovirus vector directs high levels of transgene expression in mammary carcinoma cells but not in normal nonmammary cells. Mol. Ther. 2004;10:758–767. doi: 10.1016/j.ymthe.2004.06.849. [DOI] [PubMed] [Google Scholar]
- 100.Baxevanis C.N., Voutsas I.F., Gritzapis A.D., Perez S.A., Papamichail M. HER-2/neu as a target for cancer vaccines. Immunotherapy. 2010;2:213–226. doi: 10.2217/imt.09.89. [DOI] [PubMed] [Google Scholar]
- 101.Koh E.H., Cho Y.W., Mun Y.J., Ryu J.H., Kim E.J., Choi D.S., Maeng K.Y., Han J., Kang D. Upregulation of human mammaglobin reduces migration and invasion of breast cancer cells. Cancer Investig. 2014;32:22–29. doi: 10.3109/07357907.2013.861473. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As this is a review article, it does not contain any new, original research data. Instead, it synthesizes and analyzes previously published data and information. All data and materials discussed in this review are cited appropriately and can be found in the referenced articles and resources. Therefore, a data availability statement is not applicable to this paper.