Abstract
Background: Delirium is difficult to measure in the Intensive Care Unit (ICU). It is possible that by considering the rate of screening, incidence, and rate of treatment with antipsychotic medications (APMs) for suspected delirium, a clearer picture can emerge. Methods: A retrospective, observational study was conducted at two ICUs in Australia, between April and June of 2020. All adult ICU patients were screened; those who spoke English and did not have previous neurocognitive pathology or intracranial pathology were included in the analysis. Data were collected from the hospitals’ electronic medical records. The primary outcome was incidence of delirium based on the use of the Confusion Assessment Method for ICU (CAM-ICU). Secondary outcomes included measures of screening for delirium, treatment of suspected delirium with APMs, and identifying clinical factors associated with both delirium and the use of APMs. Results: From 736 patients that were screened, 665 were included in the analysis. The incidence of delirium was 11.3% (75/665); on average, the Richmond Agitation and Sedation Scale (RASS) was performed every 2.9 h and CAM-ICU every 40 h. RASS was not performed in 8.4% (56/665) of patients and CAM-ICU was not performed in 40.6% (270/665) of patients. A total of 17% (113/665) of patients were prescribed an APM, with quetiapine being the most used. ICU length of stay (LOS), APACHE-III score, and the use of alpha-2 agonists were associated with the presence of delirium, while ICU LOS, the use of alpha-2 agonists, and the presence of delirium were associated with patients receiving APMs. Conclusions: The incidence of delirium was lower than previously reported, at 11.3%. The rate of screening for delirium was low, while the use of APMs for delirium was higher than the incidence of delirium. It is possible that the true incidence is higher than what was measured. Critical prospective assessment is required to optimize APM indications in the ICU.
Keywords: delirium, Intensive Care Unit, hospitalization, incidence, antipsychotic agents
1. Introduction
Delirium is a common neuropsychiatric syndrome characterized by acute fluctuations in mental status, inattention, and either disorganized thinking or an altered level of consciousness [1]. It is now widely accepted that the aetiology of delirium is likely multifactorial, with older age and cognitive impairment being some of the factors associated with delirium [2,3]. Other predictive factors include the presence of more than one condition associated with coma, sedative medications (like benzodiazepines), analgesics (like opioids and ketamine), increased severity of illness, type of admission (increased in emergency compared to planned), admission diagnosis (like neurological, neurosurgical, and trauma), the presence of infection, dehydration, malnutrition, renal failure, and the use of haemofiltration [4,5]. The pathophysiological pathway of delirium may depend on the cause. There are likely several pathways for the development of delirium, including GABAergic and cholinergic neurotransmitter systems [2]. This is suggested by the increased risk associated with GABA agonists and anticholinergic drugs [6]. Other pathways may include excess dopaminergic activity and inflammatory cytokines [2,4]. Delirium can be classified as hyperactive, hypoactive, or mixed, depending on the features of the symptoms [7]. The incidence of delirium in Intensive Care Units (ICUs) varies widely, ranging from 20% to 80%, depending on the patient population and the diagnostic criteria used [8,9]. Delirium in the ICU is associated with longer hospital stays, increased healthcare costs, and higher morbidity and mortality rates [10]. Prevention, early identification, and treatment of delirium are crucial when it comes to improving patient outcomes [10].
There are many tools used to screen for delirium, but The Richmond Agitation and Sedation Scale (RASS) and the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) are two of the most widely used [11,12]. Both screening tests are well-validated and are usually used together to assess sedation and diagnose delirium in ICU patients [13]. However, studies have shown that screening for delirium is inconsistent. This leads to delirium often going unrecognized and underdiagnosed in the ICU setting [14].
RASS and CAM-ICU are used in conjunction. RASS is used first to measure the level of arousal of patients. It can be used regardless of whether patients are receiving sedatives or not. The RASS score ranges from a score of −5, where a patient is deemed “unarousable”, to a score of +4, where a patient is “violent and immediate danger to staff”. If the RASS score is too low (less than −3), meaning that the patient is too drowsy or sedated, then the CAM-ICU cannot be performed [12]. The CAM-ICU test measures whether a patient is suffering from delirium at the time that the test is performed [12]. It uses a series of questions and commands to check if a patient is able to concentrate and undertake abstract thinking. Once delirium is identified, it is possible to grade its severity by using the CAM-S scale. By doing so, it is possible to determine its clinical trajectory as either improving or worsening [15].
Delirium is treated through both non-pharmacologic and pharmacologic strategies [16]. When pharmacologic strategies are needed, antipsychotic medications (APMs) are commonly prescribed, although their efficacy remains uncertain [17]. Some studies have suggested that APMs may be effective in reducing the duration and severity of delirium symptoms, while others have found no significant benefit [18,19]. The American Geriatrics Society guidelines for the management of delirium recommend the use of antipsychotic medications for patients with severe agitation or distress, but not for the routine treatment of delirium [20]. Despite the lack of definitive evidence and their considerable side effect profile, the use of APMs for delirium management in ICU patients is widespread [21].
By looking simultaneously at the patterns of screening for delirium, rates at which it occurs, and the treatment with APMs that patients with suspected delirium receive, clinicians might be able to obtain a more comprehensive picture of the overall landscape of delirium in the critical care setting. This more comprehensive evaluation might help determine whether the rates at which delirium is being identified are accurate and whether treatment is being administered appropriately. We hypothesize that screening rates for delirium are low and that the rates at which delirium is being identified are not similar to the rates at which delirium is being treated with APMs.
The overall aim of this study is to provide a comprehensive description of how critical care patients are burdened by delirium by looking at multiple parameters simultaneously, rather than a single measure. This study intends to achieve this aim by completing the objectives of describing the frequency of screening for delirium, describing the rates of delirium, including the incidence, and describing the treatment of suspected delirium with APMs.
2. Materials and Methods
This was a retrospective, observational study, conducted at two metropolitan ICUs in Australia. Patients admitted to the two participating ICUs between 1 April 2020 and 30 June 2020 were reviewed. Inclusion criteria were adult patients of 18 years of age or older, admitted to the John Hunter Hospital ICU or Calvary Mater Newcastle ICU, who could be assessed for delirium at least twice daily with RASS and CAM-ICU tools. Exclusion criteria were age less than 18 years old; comatose, defined as a Glasgow Coma Scale (GCS) score of less than 8 for reasons other than purely sedation; non-English-speaking; patients with known pre-existing psychiatric disorders already receiving APMs; and patients with pre-existing cognitive impairment. These criteria made it possible to identify patients that could be assessed adequately with the tools being utilised and who would be at risk of suffering from delirium and not another type of neurological dysfunction from a primary pathology like dementia, schizophrenia, or a traumatic brain injury.
The primary outcome of the study was the incidence of delirium in ICU. This was considered as the number of patients with a positive CAM-ICU result out of those who were not previously known to have neurocognitive failure before presenting to ICU (i.e., new cases). The secondary outcomes were as follows: 1. the rates of use of RASS and CAM-ICU; 2. the rates of delirium based on a positive CAM-ICU result out of those who completed CAM-ICU assessments, therefore providing a period prevalence; 3. the rates of administration of APMs in the ICU for the treatment of suspected delirium; 4. the correlation of clinical parameters with the incidence of delirium; and 5. the relationship between clinical indicators and the propensity for the administration of APMs in suspected delirium cases.
The hospitals’ Electronic Medical Record (EMR) systems were used to screen and identify patients. All data were de-identified and collected using a password-protected electronic database. Only the study team had access to the data and database. An effort to minimize selection bias was made by screening all patients who were admitted to the participating ICUs. The sample size was a convenience sample, determined by the number of patients who were admitted during the pre-determined study period and that were eligible. The study protocol was approved by the local Human Research Ethics Committee and Governance offices before it was initiated (AU202009-13; AU202103-13).
Patient data collected included demographics and baseline characteristics, treatment received in ICU, and outcome data. A measure of severity of illness was obtained by collecting Acute Physiology and Chronic Health Evaluation (APACHE) III scores. APACHE-III scores take into account a variety of clinical parameters and chronic health conditions within the first 24 h of admission to the ICU and are used to assess the prognosis of patients admitted to the ICU [22]. Sedation and delirium data were collected in the form of the RASS and CAM-ICU assessments performed by medical and nursing staff. Only data available for collection in the EMR were used. Since data regarding the type of delirium or severity of delirium were not routinely collected in the participating units, they did not form a part of this study.
Descriptive statistics were used with percentages and fractions. For determining which clinical factors are associated with delirium and with the use of APMs, multiple logistic regression was used. A p-value of <0.05 was considered significant.
3. Results
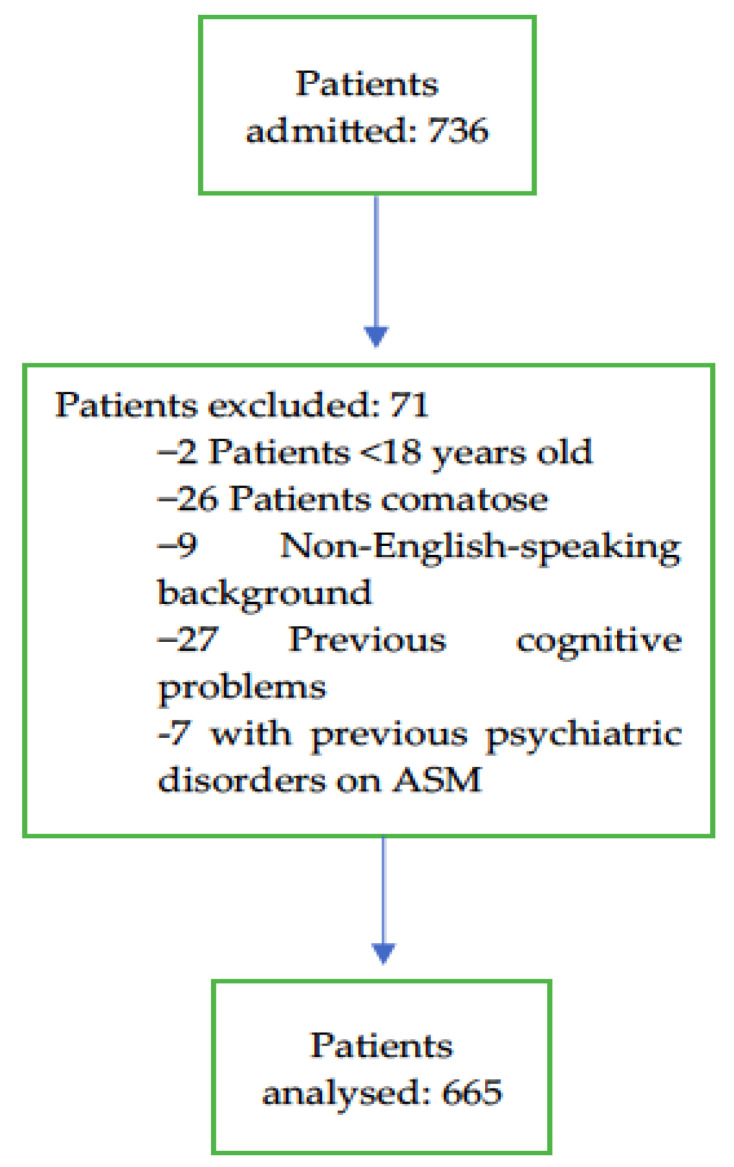
There were a total of 736 patients admitted to the participating ICUs during the study period. A total of 665 patients who met the inclusion criteria and had none of the exclusion criteria were included in the analysis (Figure 1). John Hunter Hospital is a tertiary-referral centre which provides comprehensive care with subspecialty teams that include cardiothoracic and vascular surgery, neurosurgery, interventional neuroradiology, trauma care, and extracorporeal therapies like haemodialysis, plasmapheresis, and ECMO. The Calvary Mater Newcastle Hospital is also a referral centre. It provides tertiary level care, including oncology, toxicology, and acute mental health illness services. The patients screened for this study were a cross-section of the population serviced by both hospitals’ ICUs.
Figure 1.
ICU admissions and exclusions, and the study population included in the final analysis.
The median age of the cohort was 64 (IQR 53–74) years, 62% (417/665) of the patients were male, the median APACHE-III score was 55 (IQR 40–75.5), and the median ICU LOS was 1.9 (IQR 1–3.6) days. The cohort’s baseline characteristics can be seen in Table 1.
Table 1.
Patient baseline characteristics.
| Characteristics | N = 665 |
|---|---|
| Age | |
| Median (IQR) | 64 (53–74) |
| Mean (SD) | 61 (17) |
| Sex (male) | 62.6% (417/665) |
| APACHE-III scores | |
| Median (IQR) | 55 (40–75.5) |
| Mean (SD) | 59 (26) |
| Admission type | |
| Medical | 48.6% (323/665) |
| Surgical | 51.4% (342/665) |
| ICU LOS (days) | |
| Median (IQR) | 1.9 (1–3.6) |
| Mean (SD) | 3.2 (5) |
| ICU LOS (hours) | |
| Median (IQR) | 46 (24–86) |
| Mean (SD) | 76.2 (120) |
| Received IMV at one point during ICU admission | |
| Yes | 55.9% (372/665) |
| No | 44.2% (293/665) |
| Sedative, any | 57.1% (380/665) |
| Benzodiazepine | 43% (286/665) |
| Alpha-2 agonist | 16.7% (111/665) |
| Opioid | 74% (492/665) |
| ICU mortality | 10.5% (70/665) |
APACHE-III: Acute Physiology and Chronic Health Evaluation- III; ICU: Intensive Care Unit; IMV: Invasive Mechanical Ventilation; IQR: Interquartile Range; LOS: length of stay; SD: Standard Deviation.
The incidence of delirium, the primary outcome of this study, was 11.3% (75/665). Regarding screening for delirium, there were a total of 17,273 episodes of RASSs performed and a total of 1248 episodes of CAM-ICU assessments performed. This represents 7.2% (1248/17,273) of RASS assessments that go on to have a CAM-ICU assessment. RASS was performed an average of 8.2 times per patient per ICU day, while CAM-ICU was performed an average of 0.6 times per patient per ICU day. The primary outcome and secondary outcomes of screening can be seen in Table 2.
Table 2.
Rates of delirium and frequencies of screening with RASS and CAM-ICU.
| Primary Outcome | |
| Incidence, or rate, of patients who were found to have delirium at least once during their admission. | 11.3% (75/665) |
| Secondary Outcomes of screening | |
| Total RASSs performed | 17,273 |
| Number of RASSs performed per patient per day (average number of RASSs/average ICU LOS) | 8.2 |
| Number of RASSs completed per patient during their ICU stays | |
| Median (IQR) | 12 (5–27) |
| Mean (SD) | 26 (52) |
| Time between RASS score evaluation (Average number of RASSs/24 h) | 2.9 h |
| Number of patients who were not assessed with RASS at any time during their ICU stays | 8.4% (56/665) |
| RASS score value | |
| Median (IQR) | −0.2 (−1.2 to 0.0) |
| Mean (SD) | −0.55 (1.5) |
| Number of patients with a mean RASS score < −3 (cannot be assessed with CAM-ICU) | 6.2% (41/665) |
| Total CAM-ICUs performed | 1248 |
| Number of CAM-ICUs performed per patient per day (Average number of CAM-ICUs/average ICU LOS) |
0.6 |
| Number of CAM-ICUs completed per patient during their ICU stays | |
| Median (IQR) | 1 (0–2) |
| Mean (SD) | 1.9 (3.1) |
| Time between CAM-ICU evaluation (Average number of CAM-ICUs/24 h) | 40 h |
| Number of patients who were | |
| assessed with CAM-ICU at least once while in the ICU | 59.4%(395/665) |
| not assessed with CAM-ICU at any time while in the ICU | 40.6% (270/665) |
| Rate of delirium based on assessments (Positive CAM-ICU results/Total CAM-ICU results) |
14.8% (185/1248) |
| Rate of patients who had at least one positive CAM-ICU result out of those who were assessed with CAM-ICU | 19% (75/395) |
CAM-ICU: Confusion Assessment Method-ICU; ICU: Intensive Care Unit; IQR: Interquartile Range; LOS: length of stay; RASS: Richmond Agitation Sedation Scale; SD: Standard Deviation.
Regarding the treatment for suspected delirium, in this cohort, 17% (113/665) of patients received an APM for the treatment of suspected or diagnosed delirium. Of the patients that received APMs, 36.3% (41/113) had not been screened for delirium. Of the patients who were screened for delirium and received an APM, 9.1% (29/320) had a negative CAM-ICU result. Quetiapine was the APM most used as a first-line agent, which was administered to 6% (40/665) of patients, followed by haloperidol, which was administered to 4.5% (30/665) of patients. When a second- or third-line agent was needed, haloperidol was the APM most used. The maximum recommended dose was administered to only 1.2% (8/665) of patients [23]. The use of APMs for the treatment of suspected delirium in the ICU can be seen in Table 3.
Table 3.
Treatment with antipsychotic medications in the ICU for suspected delirium.
| n = 665 | |
|---|---|
| APM prescribed | 17% (113/665) |
| Patients who received APMs | |
| After being screened for delirium | 63.7% (72/113) |
| After not being screened for delirium | 36.3% (41/113) |
| Patients who were screened for delirium who received APMs | |
| with a positive CAM-ICU result | 57.3% (43/75) |
| with a negative CAM-ICU result | 9.1% (29/320) |
| Patients that received | |
| one agent | 12.6% (84/665) |
| two agents | 3.5% (23/665) |
| three agents | 0.9% (6/665) |
| Most used APM | |
| Quetiapine | 6% (40/665) |
| Haloperidol | 4.5% (30/665) |
| Olanzepine | 3.3% (22/665) |
| Droperidol | 2.6% (17/665) |
| Risperidone | 0.5% (3/665) |
| Other | 0.2% (1/665) |
| Patients who received non-APM treatment with a benzodiazepine | |
| with a positive CAM-ICU result | 68% (51/75) |
| with a negative CAM-ICU result | 35% (114/320) |
| Patients who received non-APM treatment with an alpha-2 agonist | |
| with a positive CAM-ICU result | 45.3% (34/75) |
| with a negative CAM-ICU result | 13.4% (43/320) |
APMs: antipsychotic medications; CAM-ICU: Confusion Assessment Method for ICU; ICU: Intensive Care Unit.
Logistic regression was used to analyse the relationship between delirium and selected variables including age, gender, ICU LOS, admission type, APACHE-III score, and use of invasive mechanical ventilation (IMV), sedatives, benzodiazepines, alpha-2 agonists, and opioids. The results can be found in Table 4.
Table 4.
Multiple logistic regression for the association of clinical factors with delirium.
| Variable | Odds Ratio | 95% CI (Profile Likelihood) |
|---|---|---|
| Intercept (Delirium) | 0.012 | 0.002217 to 0.05621 |
| Gender | 1.119 | 0.5980 to 2.132 |
| Age | 1.003 | 0.9832 to 1.024 |
| ICU LOS in hours | 1.006 | 1.003 to 1.009 |
| Admission type (surgical, medical) | 0.8267 | 0.4034 to 1.683 |
| APACHE-III score | 1.027 | 1.013 to 1.041 |
| Intubated | 0.9344 | 0.4105 to 2.157 |
| New sedative prescribed | 1.385 | 0.4597 to 4.087 |
| New benzo prescribed | 2.007 | 0.8929 to 4.778 |
| Alpha-2 agonist prescribed | 2.760 | 1.302 to 5.919 |
| New opioid prescribed | 0.6006 | 0.2525 to 1.418 |
APACHE-III: Acute Physiology and Chronic Health Evaluation III; APM: antipsychotic medication; CI: Confidence Interval; ICU: Intensive Care Unit; LOS: length of stay.
Logistic regression was also used to analyse the relationship between the use of APMs and important clinical characteristics. The results can be found in Table 5.
Table 5.
Multiple logistic regression for the association between clinical factors and the use of APMs.
| Variable | Odds Ratio | 95% CI (Profile Likelihood) |
|---|---|---|
| Intercept (APM use) | 0.08668 | 0.02639 to 0.2658 |
| Gender | 1.055 | 0.6059 to 1.865 |
| Age | 0.9856 | 0.9696 to 1.002 |
| ICU LOS in hours | 1.003 | 1.001 to 1.006 |
| Admission type (surgical, medical) | 1.503 | 0.8428 to 2.712 |
| APACHE-III score | 1.002 | 0.9906 to 1.014 |
| Intubated | 0.6482 | 0.3438 to 1.196 |
| Alpha-2 agonist (clonidine/dexmed) prescribed | 7.615 | 4.182 to 14.04 |
| Delirium | 3.537 | 1.747 to 7.066 |
APACHE-III: Acute Physiology and Chronic Health Evaluation III; APM: antipsychotic medication; CI: Confidence Interval; ICU: Intensive Care Unit; LOS: length of stay.
4. Discussion
This study provides a comprehensive view of the rates of screening and incidence of delirium, the patterns of use of APMs to treat suspected delirium, and factors associated with delirium. By including patients from two different institutions, a total of 2109 ICU days were analysed.
The patients included in this study had baseline characteristics that are similar to those encountered in most ICUs in Australia and New Zealand, as reported by the Australia and New Zealand Intensive Care Society (ANZICS) Centre for Outcome Resource Evaluation (CORE) [24]. This suggests that these results can be considered as generalizable.
In this study, the incidence of delirium was 11.3%, which is lower than the 20% to 80% that has been reported widely across the literature [25,26,27]. By taking into account the rate of screening and considering the number of positive CAM-ICUs over the number of CAM-ICUs performed (the rate of delirium), we see that the frequency with which delirium presents itself increases. The rate increases from an incidence of 11.3% to a rate of almost 15%. This highlights how delirium is difficult to measure, likely because of its fluctuating nature; it is possible that, to capture the true burden of delirium in critical care, Period-Prevalence might be a better measure than incidence [28,29,30].
Assessments with RASS were undertaken, on average, around every 3 h, when it is suggested that RASS provides the best utility when it is used every 1 to 2 h [22,23]. Assessments with CAM-ICU were performed, on average, every 40 h, when it is recommended that it is measured every 12 h [12]. This lower-than-recommended rate of screening is likely why the rates of delirium in this study were lower than those reported by other studies.
CAM-ICU was performed on only 7.2% of the occasions that a RASS was performed. As mentioned previously, if the RASS score is less than −3, then CAM-ICU cannot be performed because the patient is too sedated. The RASS score was less than −3 only 6.2% of the time, which means that the low rate of CAM-ICU assessments was unlikely to be due to oversedation. It can be hypothesized that other factors were preventing its use. It is difficult to determine what factors specifically from these data alone; thus, further research is needed.
When patients were suspected of or diagnosed with delirium and pharmacological treatment was utilised, an APM was prescribed 17% of the time. This rate is already higher than both the incidence and the rate of delirium found in this cohort. This makes us suspect, once more, that the burden of illness from delirium is higher than what is suggested by the previous figures. More than one third of the patients who received APMs had not been assessed for delirium with CAM-ICU. Along with that, in patients who had been screened for delirium but had a negative CAM-ICU result, almost 10% of these received an APM. It is difficult to know from these data alone why APMs were being used in these circumstances. It is possible that they were suffering from delirium and that this was recognised by clinicians, but this was not captured by the screening. This would also suggest that there is a significant unreported burden of illness from delirium in the critically ill population.
In this cohort, APMs were used frequently and even on some patients who had no delirium. Along with APMs, it is important to note that patients suspected of delirium received non-APM treatments for delirium. Of the patients with a positive CAM-ICU result, 68% received benzodiazepines, most commonly as infusions. This was likely carried out for sedation while receiving IMV. Benzodiazepines have been associated with increased rates of delirium so it is surprising to see how their use is still relatively prevalent [27,31]. Of the patients with a positive CAM-ICU result, 45% received alpha-2 agonists as either boluses with clonidine or infusions with dexmedetomidine. Dexmedetomidine has shown promise for treating delirium, but the evidence is mixed [25,26,27]. It was unexpected that the rate of treatment with both APM and non-APM medications was higher than the actual documented rates of delirium.
When attempting to identify factors that are associated with delirium, in this cohort only three were statistically significantly associated with delirium: ICU LOS, APACHE-III score, and the use of alpha-2 agonists. The factors analysed are all tightly interconnected, therefore making it difficult to determine how individual factors can increase the likelihood of developing delirium. Previous findings vary in terms of factors associated with delirium in the ICU [19,28]. With longer ICU LOS and a higher APACHE-III score, it is easy to see how organ failure like delirium can occur. It is possible that those with delirium were more likely to be prescribed alpha-2 agonists, rather than these causing the delirium. The timing of prescribing can help determine this in future studies. The only potentially modifiable factor associated with delirium, as long as the temporal relationship coincides, is the use of alpha-2 agonists. Future studies can continue to look for modifiable factors associated with delirium to help improve patient outcomes.
APMs are not without adverse effects; some of them, like prolonged QT intervals and dystonic reactions, are serious [29,30]. Minimizing their use puts patients at less risk, which is why identifying characteristics associated with a higher likelihood of receiving APMs could help clinicians plan how to best manage delirium when it occurs. From these data, we can see that a longer ICU LOS is associated with a higher chance of receiving APMs. Delirium itself is associated with a higher chance of receiving APMs, but receiving an alpha-2 agonist is also strongly associated. This means that, in the current environment, patients with delirium who have already received an alpha-2 agonist and continue to suffer from delirium are the most likely of all to receive an APM.
Some of the strengths of this study are that, by looking at delirium holistically (screening, rates, and treatment), we can potentially extract stronger insights about the complete landscape of this type of organ failure in the critical care population. This is a characteristic that makes this study unique when compared to most others, as it is common to focus on one aspect of the illness rather than looking at it from different angles. This can be more insightful for clinicians than a unidimensional perspective. Another strength is that including more than one centre makes the findings more generalisable. The limitations of this study are the same as those of other retrospective observational studies. While this is a limitation, the retrospective nature of the study allows for an assessment of the true adherence to delirium screening, which would have been harder to assess in a prospective study due to the study potentially altering usual practice. This study was undertaken at the beginning of the COVID-19 pandemic, so it might be representative of a period in history where the priorities of critical care practitioners were different to what they normally are, and treating patients with suspected delirium could have been different in terms of relying more on heavy sedation. We did not collect data around how many of the patients included here were admitted to the ICU due to COVID-19, so we cannot determine how this would have affected outcomes. At the height of the pandemic, with resources stretched, no patient was recruited into any type of study. This would have been valuable information but was not within the scope of the study. Data around the type of delirium were not available for collection. How the type of delirium affects outcomes could have made this report stronger. The timing and indications of medications and their relationship to the suspected or diagnosed delirium are difficult to determine due to the retrospective design. We were interested in short-term outcomes, although long-term outcomes using functional assessment scales would have also been insightful but were not available to us.
5. Conclusions
The incidence of delirium in this study was 11.3%. The screening rates with RASS and CAM-ICU were lower than recommended. The use of APMs is more frequent than the rate at which delirium is being diagnosed. A critical prospective assessment is required to optimize APM use in the ICU. Through ongoing attempts at determining its true burden of illness, delirium might become a type of organ failure that is less confusing for clinicians.
Acknowledgments
The authors would like to thank Thomas Woodcock, and Sarah Dalton for their valuable contribution in the development of this study, they have consented to this acknowledgement. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the position of the Hunter New England Local Health District.
Author Contributions
Conceptualization: F.E.M., R.T. and Z.J.B.; methodology: F.E.M.; statistical analysis: F.E.M.; data collection: R.T., A.-L.P., L.J. and L.B.; formal analysis: F.E.M. and Z.J.B.; supervision: F.E.M. and A.-L.P.; writing, review, and editing: F.E.M. and Z.J.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This research underwent review and was approved by the Hunter New England Human Research Ethics Committee (AU202009-13; AU202103-13).
Informed Consent Statement
Patient consent was waived due to the minimal risk due to retrospective observational nature of the study and de-identified quality of the data.
Data Availability Statement
Data collected and presented here can be made available on direct request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. APA; Washington, DC, USA: 2013. [(accessed on 25 June 2016)]. Available online: http://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596. [Google Scholar]
- 2.Fiest K.M., Soo A., Hee Lee C., Niven D.J., Ely E.W., Doig C.J., Stelfox H.T. Long-Term Outcomes in ICU Patients with Delirium: A Population-based Cohort Study. Am. J. Respir. Crit. Care Med. 2021;204:412–420. doi: 10.1164/rccm.202002-0320OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO|ICD-10 Online Versions. [(accessed on 17 April 2020)]. Available online: http://www.who.int/classifications/icd/icdonlineversions/en/
- 4.Wolters A.E., van Dijk D., Pasma W., Cremer O.L., Looije M.F., de Lange D.W., Veldhuijzen D.S., Slooter A.J. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness: A prospective cohort study. Crit. Care. 2014;18:R125. doi: 10.1186/cc13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De J., Wand A.P. Delirium Screening: A Systematic Review of Delirium Screening Tools in Hospitalized Patients. Gerontologist. 2015;55:1079–1099. doi: 10.1093/geront/gnv100. [DOI] [PubMed] [Google Scholar]
- 6.Monitoring Delirium in the ICU. [(accessed on 13 March 2023)]. Available online: https://www.icudelirium.org/medical-professionals/delirium/monitoring-delirium-in-the-icu.
- 7.Barman A., Pradhan D., Bhattacharyya P., Dey S., Bhattacharjee A., Tesia S.S., Mitra J.K. Diagnostic accuracy of delirium assessment methods in critical care patients. J. Crit. Care. 2018;44:82–86. doi: 10.1016/j.jcrc.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Riekerk B., Pen E.J., Hofhuis J.G.M., Rommes J.H., Schultz M.J., Spronk P.E. Limitations and practicalities of CAM-ICU implementation, a delirium scoring system, in a Dutch intensive care unit. Intensive Crit. Care Nurs. 2009;25:242–249. doi: 10.1016/j.iccn.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Burry L., Hutton B., Williamson D.R., Mehta S., Adhikari N.K., Cheng W., Ely E.W., Egerod I., Fergusson D.A., Rose L. Pharmacological interventions for the treatment of delirium in critically ill adults. Cochrane Database Syst. Rev. 2019;2019:CD011749. doi: 10.1002/14651858.CD011749.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Girard T.D., Exline M.C., Carson S.S., Hough C.L., Rock P., Gong M.N., Douglas I.S., Malhotra A., Owens R.L., Feinstein D.J., et al. Haloperidol and Ziprasidone for Treatment of Delirium in Critical Illness. N. Engl. J. Med. 2018;379:2506–2516. doi: 10.1056/NEJMoa1808217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andersen-Ranberg N.C., Poulsen L.M., Perner A., Wetterslev J., Estrup S., Hästbacka J., Morgan M., Citerio G., Caballero J., Lange T., et al. Haloperidol for the Treatment of Delirium in ICU Patients. N. Engl. J. Med. 2022;387:2425–2435. doi: 10.1056/NEJMoa2211868. [DOI] [PubMed] [Google Scholar]
- 12.American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J. Am. Geriatr. Soc. 2015;63:142–150. doi: 10.1111/jgs.13281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markowitz J.D., Narasimhan M. Delirium and Antipsychotics: A Systematic Review of Epidemiology and Somatic Treatment Options. Psychiatry. 2008;5:29–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Haloperidol—Australian Medicines Handbook. [(accessed on 27 June 2023)]. Available online: https://amhonline.amh.net.au.acs.hcn.com.au/chapters/psychotropic-drugs/antipsychotics/haloperidol?menu=hints.
- 15.ANZICS CORE Reports. [(accessed on 14 March 2023)]. Available online: https://www.anzics.com.au/annual-reports/
- 16.Wang C., Qin Y., Wan X., Song L., Li Z., Li H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J. Orthop. Surg. 2018;13:186. doi: 10.1186/s13018-018-0897-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van den Boogaard M., Schoonhoven L., van der Hoeven J.G., van Achterberg T., Pickkers P. Incidence and short-term consequences of delirium in critically ill patients: A prospective observational cohort study. Int. J. Nurs. Stud. 2012;49:775–783. doi: 10.1016/j.ijnurstu.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Williams E.C., Estime S., Kuza C.M. Delirium in trauma ICUs: A review of incidence, risk factors, outcomes, and management. Curr. Opin. Anesthesiol. 2023;36:137–146. doi: 10.1097/ACO.0000000000001233. [DOI] [PubMed] [Google Scholar]
- 19.Vasilevskis E.E., Han J.H., Hughes C.G., Ely E.W. Epidemiology and risk factors for delirium across hospital settings. Best Pract. Res. Clin. Anaesthesiol. 2012;26:277–287. doi: 10.1016/j.bpa.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watt C.L., Momoli F., Ansari M.T., Sikora L., Bush S.H., Hosie A., Kabir M., Rosenberg E., Kanji S., Lawlor P.G. The incidence and prevalence of delirium across palliative care settings: A systematic review. Palliat. Med. 2019;33:865–877. doi: 10.1177/0269216319854944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martinez F.E., Ho V.W., Brogan G., Pickering C., Leung G., Parrey J., Charlton A. Period-Prevalence and Risk Factors for Delirium in a Tertiary Referral ICU: A prospective cohort study. Acute Med. 2021;20:168–173. doi: 10.52964/AMJA.0860. [DOI] [PubMed] [Google Scholar]
- 22.Taran Z., Namadian M., Faghihzadeh S., Naghibi T. The Effect of Sedation Protocol Using Richmond Agitation-Sedation Scale (RASS) on Some Clinical Outcomes of Mechanically Ventilated Patients in Intensive Care Units: A Randomized Clinical Trial. J. Caring Sci. 2019;8:199–206. doi: 10.15171/jcs.2019.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeGrado J.R., Anger K.E., Szumita P.M., Pierce C.D., Massaro A.F. Evaluation of a local ICU sedation guideline on goal-directed administration of sedatives and analgesics. J. Pain Res. 2011;4:127–134. doi: 10.2147/JPR.S18161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pandharipande P., Shintani A., Peterson J., Pun B.T., Wilkinson G.R., Dittus R.S., Bernard G.R., Ely E.W. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104:21–26. doi: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Shehabi Y., Howe B.D., Bellomo R., Arabi Y.M., Bailey M., Bass F.E., Bin Kadiman S., McArthur C.J., Murray L., Reade M.C., et al. Early Sedation with Dexmedetomidine in Critically Ill Patients. N. Engl. J. Med. 2019;380:2506–2517. doi: 10.1056/NEJMoa1904710. [DOI] [PubMed] [Google Scholar]
- 26.Riker R.R., Shehabi Y., Bokesch P.M., Ceraso D., Wisemandle W., Koura F., Whitten P., Margolis B.D., Byrne D.W., Ely E.W., et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: A randomized trial. JAMA. 2009;301:489–499. doi: 10.1001/jama.2009.56. [DOI] [PubMed] [Google Scholar]
- 27.Pandharipande P.P., Pun B.T., Herr D.L., Maze M., Girard T.D., Miller R.R., Shintani A.K., Thompson J.L., Jackson J.C., Deppen S.A., et al. Effect of Sedation With Dexmedetomidine vs Lorazepam on Acute Brain Dysfunction in Mechanically Ventilated Patients: The MENDS Randomized Controlled Trial. JAMA. 2007;298:2644–2653. doi: 10.1001/jama.298.22.2644. [DOI] [PubMed] [Google Scholar]
- 28.Zaal I.J., Devlin J.W., Peelen L.M., Slooter A.J.C. A Systematic Review of Risk Factors for Delirium in the ICU. Crit. Care Med. 2015;43:40–47. doi: 10.1097/CCM.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 29.Park Y., Bateman B.T., Kim D.H., Hernandez-Diaz S., Patorno E., Glynn R.J., Mogun H., Huybrechts K.F. Use of haloperidol versus atypical antipsychotics and risk of in-hospital death in patients with acute myocardial infarction: Cohort study. BMJ. 2018;360:k1218. doi: 10.1136/bmj.k1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huhn M., Nikolakopoulou A., Schneider-Thoma J., Krause M., Samara M., Peter N., Arndt T., Bäckers L., Rothe P., Cipriani A., et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: A systematic review and network meta-analysis. Lancet. 2019;394:939–951. doi: 10.1016/S0140-6736(19)31135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGinn K., Davis S.N., Terrry E., Simmons J., Brevard S. Elimination of Routine Benzodiazepine Administration for Nonprocedural Sedation in a Trauma Intensive Care Unit is Feasible. Am. Surg. 2018;84:947–951. doi: 10.1177/000313481808400646. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data collected and presented here can be made available on direct request to the corresponding author.